User login
Volume directly tied to mitral valve procedure success
SAN FRANCISCO – Volume matters when it comes to mitral valve repair/replacement for primary mitral regurgitation. in the Society of Thoracic Surgeons Adult Cardiac Surgery Database.
Investigators “found a clear inflection point at approximately 75 cases” for hospitals and 35 cases for individual surgeons when the curves for successful mitral repair and 30-day operative mortality start to level out. Nationwide, 148 hospitals (14%) in the analysis did 75 or more mitral cases a year, and 303 surgeons (13%) did at least 35.
Lead investigator Vinay Badhwar, MD, professor and chair of cardiovascular and thoracic surgery at West Virginia University, Morgantown, estimated that about 90% of Americans have access to a regional hospital that does at least 25 mitral procedures annually, and about 82% can use a regional hospital that does at least 40. Meanwhile, the rate of mitral valve repair for primary mitral regurgitation was 81% (44,692/55,311) in the study, up from about 60% a decade ago.
“We are getting there; we are getting better,” Dr. Badhwar said at the Transcatheter Cardiovascular Therapeutics annual meeting. By defining volume cut points, he said the findings could be useful in future guidelines to steer referrals to higher-volume centers.
“We really needed these data, because we’ve had so many other pieces pointing to the volume repair rates and technical success, which clearly is related to volume. Now we have the outcome data we’ve been looking for; this ties it together. There really is an impact on patient outcomes,” Robert Bonow, MD, a professor of cardiology at Northwestern University, Chicago, commented.
The team divided annual case volume into quartiles. The lowest hospital quartile did fewer than 11 cases a year, and the highest more than 46. The lowest-quartile surgeons did fewer than 6 cases a year, and the highest more than 20. Lowest-quartile surgeons and hospitals, versus the highest, had higher operative mortality and 30-day morbidity and mortality, and lower 1-year survival.
Patients in the lowest quartile were also more likely to be black or Hispanic (14.8% versus 10.2%); have no insurance (4.0% versus 2.4%); and more severe symptom presentation (31.9% versus 23.8% class III or IV heart failure). The differences were highly statistically significant.
Study moderator Ajay Kirtane, MD, an interventional cardiologist and associate professor of medicine at Columbia University, New York, said there’s a role for advocacy to get more people to high-volume centers. “Just because you live in an area that has a good program doesn’t mean that you are actually going to get referred to that program. We find a lot that it’s advocacy that is important,” especially with the disparities noted in the study. “Not everybody has an advocate who says, ‘Don’t do it here; do it someplace else,’ ” he said at the meeting sponsored by the Cardiovascular Research Foundation.
And not everyone has an advocate to get them to the right surgeon, even if they get to the right program. “There are cardiac procedures that most surgeons can do well. Mitral valve surgery is one of those that should be super specialized,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at Baylor Scott and White Health System, Dallas.
No industry funding was reported. Dr. Badhwar had no relevant disclosures.
SOURCE: Badhwar V et al. TCT 2019.
SAN FRANCISCO – Volume matters when it comes to mitral valve repair/replacement for primary mitral regurgitation. in the Society of Thoracic Surgeons Adult Cardiac Surgery Database.
Investigators “found a clear inflection point at approximately 75 cases” for hospitals and 35 cases for individual surgeons when the curves for successful mitral repair and 30-day operative mortality start to level out. Nationwide, 148 hospitals (14%) in the analysis did 75 or more mitral cases a year, and 303 surgeons (13%) did at least 35.
Lead investigator Vinay Badhwar, MD, professor and chair of cardiovascular and thoracic surgery at West Virginia University, Morgantown, estimated that about 90% of Americans have access to a regional hospital that does at least 25 mitral procedures annually, and about 82% can use a regional hospital that does at least 40. Meanwhile, the rate of mitral valve repair for primary mitral regurgitation was 81% (44,692/55,311) in the study, up from about 60% a decade ago.
“We are getting there; we are getting better,” Dr. Badhwar said at the Transcatheter Cardiovascular Therapeutics annual meeting. By defining volume cut points, he said the findings could be useful in future guidelines to steer referrals to higher-volume centers.
“We really needed these data, because we’ve had so many other pieces pointing to the volume repair rates and technical success, which clearly is related to volume. Now we have the outcome data we’ve been looking for; this ties it together. There really is an impact on patient outcomes,” Robert Bonow, MD, a professor of cardiology at Northwestern University, Chicago, commented.
The team divided annual case volume into quartiles. The lowest hospital quartile did fewer than 11 cases a year, and the highest more than 46. The lowest-quartile surgeons did fewer than 6 cases a year, and the highest more than 20. Lowest-quartile surgeons and hospitals, versus the highest, had higher operative mortality and 30-day morbidity and mortality, and lower 1-year survival.
Patients in the lowest quartile were also more likely to be black or Hispanic (14.8% versus 10.2%); have no insurance (4.0% versus 2.4%); and more severe symptom presentation (31.9% versus 23.8% class III or IV heart failure). The differences were highly statistically significant.
Study moderator Ajay Kirtane, MD, an interventional cardiologist and associate professor of medicine at Columbia University, New York, said there’s a role for advocacy to get more people to high-volume centers. “Just because you live in an area that has a good program doesn’t mean that you are actually going to get referred to that program. We find a lot that it’s advocacy that is important,” especially with the disparities noted in the study. “Not everybody has an advocate who says, ‘Don’t do it here; do it someplace else,’ ” he said at the meeting sponsored by the Cardiovascular Research Foundation.
And not everyone has an advocate to get them to the right surgeon, even if they get to the right program. “There are cardiac procedures that most surgeons can do well. Mitral valve surgery is one of those that should be super specialized,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at Baylor Scott and White Health System, Dallas.
No industry funding was reported. Dr. Badhwar had no relevant disclosures.
SOURCE: Badhwar V et al. TCT 2019.
SAN FRANCISCO – Volume matters when it comes to mitral valve repair/replacement for primary mitral regurgitation. in the Society of Thoracic Surgeons Adult Cardiac Surgery Database.
Investigators “found a clear inflection point at approximately 75 cases” for hospitals and 35 cases for individual surgeons when the curves for successful mitral repair and 30-day operative mortality start to level out. Nationwide, 148 hospitals (14%) in the analysis did 75 or more mitral cases a year, and 303 surgeons (13%) did at least 35.
Lead investigator Vinay Badhwar, MD, professor and chair of cardiovascular and thoracic surgery at West Virginia University, Morgantown, estimated that about 90% of Americans have access to a regional hospital that does at least 25 mitral procedures annually, and about 82% can use a regional hospital that does at least 40. Meanwhile, the rate of mitral valve repair for primary mitral regurgitation was 81% (44,692/55,311) in the study, up from about 60% a decade ago.
“We are getting there; we are getting better,” Dr. Badhwar said at the Transcatheter Cardiovascular Therapeutics annual meeting. By defining volume cut points, he said the findings could be useful in future guidelines to steer referrals to higher-volume centers.
“We really needed these data, because we’ve had so many other pieces pointing to the volume repair rates and technical success, which clearly is related to volume. Now we have the outcome data we’ve been looking for; this ties it together. There really is an impact on patient outcomes,” Robert Bonow, MD, a professor of cardiology at Northwestern University, Chicago, commented.
The team divided annual case volume into quartiles. The lowest hospital quartile did fewer than 11 cases a year, and the highest more than 46. The lowest-quartile surgeons did fewer than 6 cases a year, and the highest more than 20. Lowest-quartile surgeons and hospitals, versus the highest, had higher operative mortality and 30-day morbidity and mortality, and lower 1-year survival.
Patients in the lowest quartile were also more likely to be black or Hispanic (14.8% versus 10.2%); have no insurance (4.0% versus 2.4%); and more severe symptom presentation (31.9% versus 23.8% class III or IV heart failure). The differences were highly statistically significant.
Study moderator Ajay Kirtane, MD, an interventional cardiologist and associate professor of medicine at Columbia University, New York, said there’s a role for advocacy to get more people to high-volume centers. “Just because you live in an area that has a good program doesn’t mean that you are actually going to get referred to that program. We find a lot that it’s advocacy that is important,” especially with the disparities noted in the study. “Not everybody has an advocate who says, ‘Don’t do it here; do it someplace else,’ ” he said at the meeting sponsored by the Cardiovascular Research Foundation.
And not everyone has an advocate to get them to the right surgeon, even if they get to the right program. “There are cardiac procedures that most surgeons can do well. Mitral valve surgery is one of those that should be super specialized,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at Baylor Scott and White Health System, Dallas.
No industry funding was reported. Dr. Badhwar had no relevant disclosures.
SOURCE: Badhwar V et al. TCT 2019.
REPORTING FROM TCT 2019
Women undergoing hysterectomy, myomectomy have similar short-term outcomes
PHILADELPHIA – despite different baseline characteristics, according to recent results from the COMPARE-UF study presented at the annual meeting of the American Society for Reproductive Medicine.
“Both hysterectomy and myomectomy can substantially improve women’s quality of life scores and substantially reduce symptom severity,” reported Wanda K. Nicholson, MD, MPH, lead investigator for COMPARE-UF and professor of general obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Researchers included 1,295 women in the COMPARE-UF study who were at least 30 years old, not attempting pregnancy, and undergoing hysterectomy or myomectomy for treatment of fibroids. Overall, 727 patients underwent hysterectomy, and 568 patients underwent myomectomy.
The researchers measured QoL and symptom severity using the Uterine Fibroid Scale-QoL, the EQ-5D, and Visual Analog Scale (VAS). The UFS-QoL contained subscales for concern, activities, energy and mood, control, self-consciousness, and sexual function, while the EQ-5D had subscales for mobility, self-care, usual activities, pain or discomfort, and anxiety or depression.
After surgery, UFS-QoL overall scores were similar in both hysterectomy and myomectomy groups between 6 weeks and 12 weeks (77 vs. 76), but there was less postsurgery symptom severity in the hysterectomy group over the same time period (16 vs. 20; P less than .05). However, both groups had a significant improvement in overall UFS-QoL post surgery (hysterectomy, 31; myomectomy, 30) and in UFS-QoL symptom severity (hysterectomy, 41; myomectomy, 37), Dr. Nicholson noted. EQ-5D VAS scores also were similar in both hysterectomy and myomectomy groups after treatment (82 vs. 79), and showed a 10.9 score improvement in hysterectomy patients and an 8.6 score improvement in myomectomy patients.
“This is really important, because it shows that, regardless of which procedure that you’ve chosen, at least at short-term follow up, it appears that you will have improvement in quality of life,” she said.
When researchers analyzed the UFS-QoL subscale scores, they found patients who underwent abdominal myomectomy scored better than abdominal hysterectomy on the activities subscale (79 vs. 72; P equals .01) and energy/mood subscale (82 vs. 75; P equals .03). In examining minimally invasive procedures, Dr. Nicholson and colleagues found higher improvements in health-related QoL scores among patients undergoing minimally invasive hysterectomy (45-80 vs. 45 vs. 75), and these patients also had lower symptom severity, compared with patients who underwent myomectomy (59-13 vs. 58-21).
“At least at the short-term follow-up, we think that some of that difference that we see in minimally invasive procedures vs. nonminimally invasive may be in part due to women’s perceptions or what their expectations are having minimally invasive surgery, and how they might feel in the short-term follow-up period,” said Dr. Nicholson.
These similar short-term outcomes occurred even though there were significant differences in baseline patient characteristics for the hysterectomy and myomectomy groups, with women undergoing hysterectomy being significantly younger (40 years) than patients undergoing hysterectomy (45 years). Differences also were significant between hysterectomy and myomectomy groups in the percentage of patients who were white (50% vs. 41%; P less than .01), African-American (38% vs. 41%; P less than .01) or other races (12% vs. 18%; P less than .01). There also were significant differences in baseline body mass index between hysterectomy (31 kg/m2) and myomectomy (29 kg/m2) groups.
Patients in both groups further differed in presurgery quality-of-life (QoL) scores.
Women in the hysterectomy group had lower presurgery overall QoL (44 vs. 50), greater symptom severity (60 vs. 52), and lower VAS (69 vs. 73) scores, compared with the myomectomy group (P less than .05). This difference continued in the UFS-QoL subscale scores, where women in the hysterectomy group had significantly lower scores in the concern (38 vs. 45), activities (46 vs. 52), energy/mood (45 vs. 51), control (48 vs. 52), self-consciousness (41 vs. 50), and sexual function (45 vs. 50) subscales, compared with women in the myomectomy group (P less than .05). The researchers used propensity scoring to adjust for baseline characteristics, and inverse propensity weighting to adjust for potential confounding in the multivariate analysis.
COMPARE-UF is funded by the Agency for Healthcare Research and Quality (AHRQ), Patient-Centered Outcomes Research Institute (PCORI), and the National Institutes of Health. Dr. Nicholson reported no relevant conflicts of interest.
SOURCE: Nicholson WK et al. ASRM 2019, Abstract SYT07.
PHILADELPHIA – despite different baseline characteristics, according to recent results from the COMPARE-UF study presented at the annual meeting of the American Society for Reproductive Medicine.
“Both hysterectomy and myomectomy can substantially improve women’s quality of life scores and substantially reduce symptom severity,” reported Wanda K. Nicholson, MD, MPH, lead investigator for COMPARE-UF and professor of general obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Researchers included 1,295 women in the COMPARE-UF study who were at least 30 years old, not attempting pregnancy, and undergoing hysterectomy or myomectomy for treatment of fibroids. Overall, 727 patients underwent hysterectomy, and 568 patients underwent myomectomy.
The researchers measured QoL and symptom severity using the Uterine Fibroid Scale-QoL, the EQ-5D, and Visual Analog Scale (VAS). The UFS-QoL contained subscales for concern, activities, energy and mood, control, self-consciousness, and sexual function, while the EQ-5D had subscales for mobility, self-care, usual activities, pain or discomfort, and anxiety or depression.
After surgery, UFS-QoL overall scores were similar in both hysterectomy and myomectomy groups between 6 weeks and 12 weeks (77 vs. 76), but there was less postsurgery symptom severity in the hysterectomy group over the same time period (16 vs. 20; P less than .05). However, both groups had a significant improvement in overall UFS-QoL post surgery (hysterectomy, 31; myomectomy, 30) and in UFS-QoL symptom severity (hysterectomy, 41; myomectomy, 37), Dr. Nicholson noted. EQ-5D VAS scores also were similar in both hysterectomy and myomectomy groups after treatment (82 vs. 79), and showed a 10.9 score improvement in hysterectomy patients and an 8.6 score improvement in myomectomy patients.
“This is really important, because it shows that, regardless of which procedure that you’ve chosen, at least at short-term follow up, it appears that you will have improvement in quality of life,” she said.
When researchers analyzed the UFS-QoL subscale scores, they found patients who underwent abdominal myomectomy scored better than abdominal hysterectomy on the activities subscale (79 vs. 72; P equals .01) and energy/mood subscale (82 vs. 75; P equals .03). In examining minimally invasive procedures, Dr. Nicholson and colleagues found higher improvements in health-related QoL scores among patients undergoing minimally invasive hysterectomy (45-80 vs. 45 vs. 75), and these patients also had lower symptom severity, compared with patients who underwent myomectomy (59-13 vs. 58-21).
“At least at the short-term follow-up, we think that some of that difference that we see in minimally invasive procedures vs. nonminimally invasive may be in part due to women’s perceptions or what their expectations are having minimally invasive surgery, and how they might feel in the short-term follow-up period,” said Dr. Nicholson.
These similar short-term outcomes occurred even though there were significant differences in baseline patient characteristics for the hysterectomy and myomectomy groups, with women undergoing hysterectomy being significantly younger (40 years) than patients undergoing hysterectomy (45 years). Differences also were significant between hysterectomy and myomectomy groups in the percentage of patients who were white (50% vs. 41%; P less than .01), African-American (38% vs. 41%; P less than .01) or other races (12% vs. 18%; P less than .01). There also were significant differences in baseline body mass index between hysterectomy (31 kg/m2) and myomectomy (29 kg/m2) groups.
Patients in both groups further differed in presurgery quality-of-life (QoL) scores.
Women in the hysterectomy group had lower presurgery overall QoL (44 vs. 50), greater symptom severity (60 vs. 52), and lower VAS (69 vs. 73) scores, compared with the myomectomy group (P less than .05). This difference continued in the UFS-QoL subscale scores, where women in the hysterectomy group had significantly lower scores in the concern (38 vs. 45), activities (46 vs. 52), energy/mood (45 vs. 51), control (48 vs. 52), self-consciousness (41 vs. 50), and sexual function (45 vs. 50) subscales, compared with women in the myomectomy group (P less than .05). The researchers used propensity scoring to adjust for baseline characteristics, and inverse propensity weighting to adjust for potential confounding in the multivariate analysis.
COMPARE-UF is funded by the Agency for Healthcare Research and Quality (AHRQ), Patient-Centered Outcomes Research Institute (PCORI), and the National Institutes of Health. Dr. Nicholson reported no relevant conflicts of interest.
SOURCE: Nicholson WK et al. ASRM 2019, Abstract SYT07.
PHILADELPHIA – despite different baseline characteristics, according to recent results from the COMPARE-UF study presented at the annual meeting of the American Society for Reproductive Medicine.
“Both hysterectomy and myomectomy can substantially improve women’s quality of life scores and substantially reduce symptom severity,” reported Wanda K. Nicholson, MD, MPH, lead investigator for COMPARE-UF and professor of general obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Researchers included 1,295 women in the COMPARE-UF study who were at least 30 years old, not attempting pregnancy, and undergoing hysterectomy or myomectomy for treatment of fibroids. Overall, 727 patients underwent hysterectomy, and 568 patients underwent myomectomy.
The researchers measured QoL and symptom severity using the Uterine Fibroid Scale-QoL, the EQ-5D, and Visual Analog Scale (VAS). The UFS-QoL contained subscales for concern, activities, energy and mood, control, self-consciousness, and sexual function, while the EQ-5D had subscales for mobility, self-care, usual activities, pain or discomfort, and anxiety or depression.
After surgery, UFS-QoL overall scores were similar in both hysterectomy and myomectomy groups between 6 weeks and 12 weeks (77 vs. 76), but there was less postsurgery symptom severity in the hysterectomy group over the same time period (16 vs. 20; P less than .05). However, both groups had a significant improvement in overall UFS-QoL post surgery (hysterectomy, 31; myomectomy, 30) and in UFS-QoL symptom severity (hysterectomy, 41; myomectomy, 37), Dr. Nicholson noted. EQ-5D VAS scores also were similar in both hysterectomy and myomectomy groups after treatment (82 vs. 79), and showed a 10.9 score improvement in hysterectomy patients and an 8.6 score improvement in myomectomy patients.
“This is really important, because it shows that, regardless of which procedure that you’ve chosen, at least at short-term follow up, it appears that you will have improvement in quality of life,” she said.
When researchers analyzed the UFS-QoL subscale scores, they found patients who underwent abdominal myomectomy scored better than abdominal hysterectomy on the activities subscale (79 vs. 72; P equals .01) and energy/mood subscale (82 vs. 75; P equals .03). In examining minimally invasive procedures, Dr. Nicholson and colleagues found higher improvements in health-related QoL scores among patients undergoing minimally invasive hysterectomy (45-80 vs. 45 vs. 75), and these patients also had lower symptom severity, compared with patients who underwent myomectomy (59-13 vs. 58-21).
“At least at the short-term follow-up, we think that some of that difference that we see in minimally invasive procedures vs. nonminimally invasive may be in part due to women’s perceptions or what their expectations are having minimally invasive surgery, and how they might feel in the short-term follow-up period,” said Dr. Nicholson.
These similar short-term outcomes occurred even though there were significant differences in baseline patient characteristics for the hysterectomy and myomectomy groups, with women undergoing hysterectomy being significantly younger (40 years) than patients undergoing hysterectomy (45 years). Differences also were significant between hysterectomy and myomectomy groups in the percentage of patients who were white (50% vs. 41%; P less than .01), African-American (38% vs. 41%; P less than .01) or other races (12% vs. 18%; P less than .01). There also were significant differences in baseline body mass index between hysterectomy (31 kg/m2) and myomectomy (29 kg/m2) groups.
Patients in both groups further differed in presurgery quality-of-life (QoL) scores.
Women in the hysterectomy group had lower presurgery overall QoL (44 vs. 50), greater symptom severity (60 vs. 52), and lower VAS (69 vs. 73) scores, compared with the myomectomy group (P less than .05). This difference continued in the UFS-QoL subscale scores, where women in the hysterectomy group had significantly lower scores in the concern (38 vs. 45), activities (46 vs. 52), energy/mood (45 vs. 51), control (48 vs. 52), self-consciousness (41 vs. 50), and sexual function (45 vs. 50) subscales, compared with women in the myomectomy group (P less than .05). The researchers used propensity scoring to adjust for baseline characteristics, and inverse propensity weighting to adjust for potential confounding in the multivariate analysis.
COMPARE-UF is funded by the Agency for Healthcare Research and Quality (AHRQ), Patient-Centered Outcomes Research Institute (PCORI), and the National Institutes of Health. Dr. Nicholson reported no relevant conflicts of interest.
SOURCE: Nicholson WK et al. ASRM 2019, Abstract SYT07.
REPORTING FROM ASRM 2019
Rifabutin-based triple therapy for H. pylori gets high marks
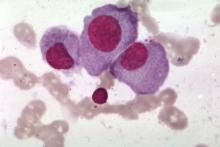
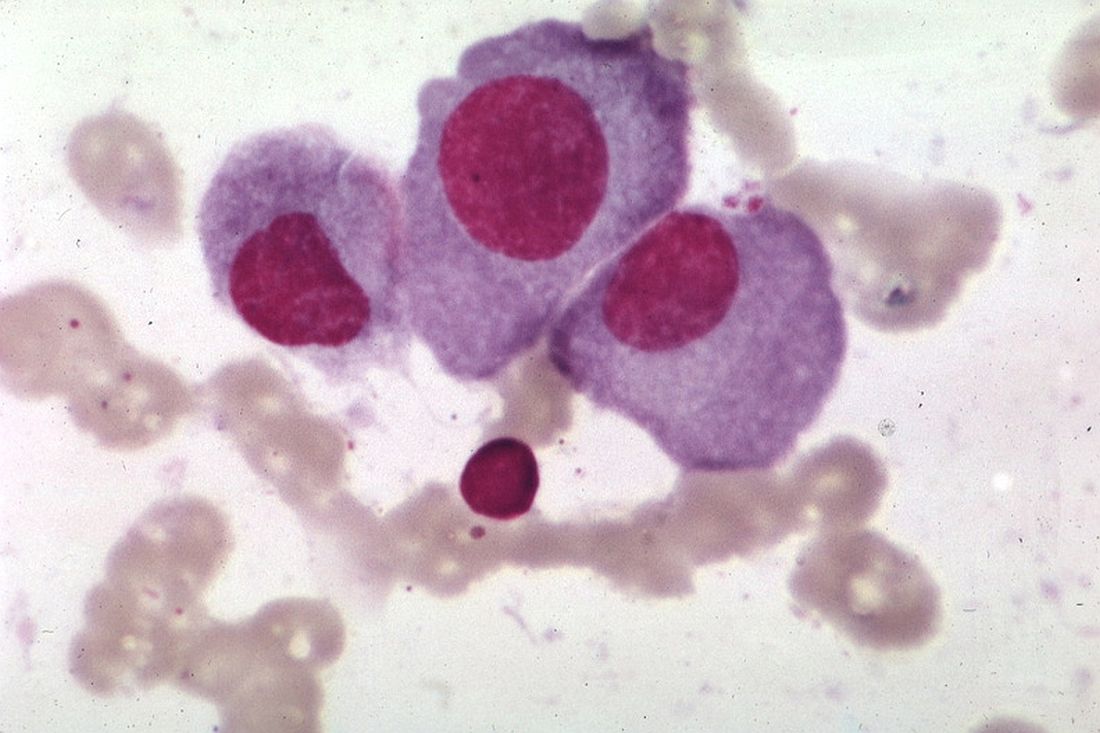
SAN ANTONIO – David Y. Graham, MD, asserted at the annual meeting of the American College of Gastroenterology.
The drug, recently approved as Talicia, is a rifabutin-based triple therapy. Each capsule contains 50 mg of rifabutin, 1,000 mg of amoxicillin, and 40 mg of omeprazole. As in the pivotal phase 3 trial led by Dr. Graham, the approved treatment regimen calls for adults to take four capsules every 8 hours for 14 days.
The impetus for developing the new therapy centers on the growing problem of resistance to long-standard agents for H. pylori eradication, including metronidazole and clarithromycin. The World Health Organization has declared H. pylori eradication to be a high priority for therapeutic development. Rifabutin resistance is rare: In one study, 413 of 414 strains of H. pylori were sensitive to the antibiotic, noted Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
He presented the results of the pivotal phase 3, double-blind, multicenter, active comparator trial, known as ERADICATE Hp2, in which 455 participants with confirmed H. pylori infection were randomized to a course of the all-in-one-capsule triple drug combo or to dual therapy with four capsules, each containing 1,000 mg of amoxicillin and 40 mg of omeprazole, every 8 hours for 14 days.
The primary endpoint was H. pylori eradication as documented by a negative urea breath test obtained 4-6 weeks after completing 14 days of treatment. The rate was 84% with the rifabutin-based combo, compared with 58% seen with the high-dose dual therapy. Moreover, in a prespecified secondary analysis restricted to the 391 participants who were confirmed to be actually taking their medication as evidenced by a positive blood level measured on day 13, the eradication rates rose to 90% and 65%, respectively.
The antimicrobial resistance rates documented in this study were eye opening: 17% of patients’ strains were resistant to clarithromycin, 44% to metronidazole, and 10.5% to both. Of concern, 6.4% of participants’ strains were amoxicillin resistant.
“For the first time we saw a low level – but a definite level – of amoxicillin resistance. That’s something we had not seen previously,” Dr. Graham said.
No rifabutin resistance was detected before or after treatment.
The side effect profiles of the two treatment regimens were similar. Diarrhea was reported by 9% of participants, headache by 7%, and nausea by 5%. No serious adverse events occurred in the 14-day study.
The efficacy of the rifabutin-based therapy wasn’t affected by metronidazole or clarithromycin resistance.
The ERADICATE Hp2 trial was sponsored by RedHill Biopharma of Tel Aviv. Dr. Graham reported having no financial conflicts.
SAN ANTONIO – David Y. Graham, MD, asserted at the annual meeting of the American College of Gastroenterology.
The drug, recently approved as Talicia, is a rifabutin-based triple therapy. Each capsule contains 50 mg of rifabutin, 1,000 mg of amoxicillin, and 40 mg of omeprazole. As in the pivotal phase 3 trial led by Dr. Graham, the approved treatment regimen calls for adults to take four capsules every 8 hours for 14 days.
The impetus for developing the new therapy centers on the growing problem of resistance to long-standard agents for H. pylori eradication, including metronidazole and clarithromycin. The World Health Organization has declared H. pylori eradication to be a high priority for therapeutic development. Rifabutin resistance is rare: In one study, 413 of 414 strains of H. pylori were sensitive to the antibiotic, noted Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
He presented the results of the pivotal phase 3, double-blind, multicenter, active comparator trial, known as ERADICATE Hp2, in which 455 participants with confirmed H. pylori infection were randomized to a course of the all-in-one-capsule triple drug combo or to dual therapy with four capsules, each containing 1,000 mg of amoxicillin and 40 mg of omeprazole, every 8 hours for 14 days.
The primary endpoint was H. pylori eradication as documented by a negative urea breath test obtained 4-6 weeks after completing 14 days of treatment. The rate was 84% with the rifabutin-based combo, compared with 58% seen with the high-dose dual therapy. Moreover, in a prespecified secondary analysis restricted to the 391 participants who were confirmed to be actually taking their medication as evidenced by a positive blood level measured on day 13, the eradication rates rose to 90% and 65%, respectively.
The antimicrobial resistance rates documented in this study were eye opening: 17% of patients’ strains were resistant to clarithromycin, 44% to metronidazole, and 10.5% to both. Of concern, 6.4% of participants’ strains were amoxicillin resistant.
“For the first time we saw a low level – but a definite level – of amoxicillin resistance. That’s something we had not seen previously,” Dr. Graham said.
No rifabutin resistance was detected before or after treatment.
The side effect profiles of the two treatment regimens were similar. Diarrhea was reported by 9% of participants, headache by 7%, and nausea by 5%. No serious adverse events occurred in the 14-day study.
The efficacy of the rifabutin-based therapy wasn’t affected by metronidazole or clarithromycin resistance.
The ERADICATE Hp2 trial was sponsored by RedHill Biopharma of Tel Aviv. Dr. Graham reported having no financial conflicts.
SAN ANTONIO – David Y. Graham, MD, asserted at the annual meeting of the American College of Gastroenterology.
The drug, recently approved as Talicia, is a rifabutin-based triple therapy. Each capsule contains 50 mg of rifabutin, 1,000 mg of amoxicillin, and 40 mg of omeprazole. As in the pivotal phase 3 trial led by Dr. Graham, the approved treatment regimen calls for adults to take four capsules every 8 hours for 14 days.
The impetus for developing the new therapy centers on the growing problem of resistance to long-standard agents for H. pylori eradication, including metronidazole and clarithromycin. The World Health Organization has declared H. pylori eradication to be a high priority for therapeutic development. Rifabutin resistance is rare: In one study, 413 of 414 strains of H. pylori were sensitive to the antibiotic, noted Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
He presented the results of the pivotal phase 3, double-blind, multicenter, active comparator trial, known as ERADICATE Hp2, in which 455 participants with confirmed H. pylori infection were randomized to a course of the all-in-one-capsule triple drug combo or to dual therapy with four capsules, each containing 1,000 mg of amoxicillin and 40 mg of omeprazole, every 8 hours for 14 days.
The primary endpoint was H. pylori eradication as documented by a negative urea breath test obtained 4-6 weeks after completing 14 days of treatment. The rate was 84% with the rifabutin-based combo, compared with 58% seen with the high-dose dual therapy. Moreover, in a prespecified secondary analysis restricted to the 391 participants who were confirmed to be actually taking their medication as evidenced by a positive blood level measured on day 13, the eradication rates rose to 90% and 65%, respectively.
The antimicrobial resistance rates documented in this study were eye opening: 17% of patients’ strains were resistant to clarithromycin, 44% to metronidazole, and 10.5% to both. Of concern, 6.4% of participants’ strains were amoxicillin resistant.
“For the first time we saw a low level – but a definite level – of amoxicillin resistance. That’s something we had not seen previously,” Dr. Graham said.
No rifabutin resistance was detected before or after treatment.
The side effect profiles of the two treatment regimens were similar. Diarrhea was reported by 9% of participants, headache by 7%, and nausea by 5%. No serious adverse events occurred in the 14-day study.
The efficacy of the rifabutin-based therapy wasn’t affected by metronidazole or clarithromycin resistance.
The ERADICATE Hp2 trial was sponsored by RedHill Biopharma of Tel Aviv. Dr. Graham reported having no financial conflicts.
REPORTING FROM ACG 2019
Spray-painted bandages and pharma sings ‘Dough Canada!’
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
Oral anticancer spending in Part D tied in major part to price increases
Price increases are the main source of the increase in spending on oral anticancer drugs in the Medicare Part D prescription drug program, according to new research.
“Annualized spending on the same oral anticancer drugs more than doubled in a 5-year period,” Kira Seiger from Harvard Medical School, Boston, and colleagues wrote in a research letter published online in JAMA Oncology.
“Use increased substantially, likely owing to expanded drug indications, increased Medicare Part D enrollment, and declining cancer mortality yielding longer treatment courses,” the authors continued. “However, increased spending was predominantly driven (56%) by rising drug costs, which is reflective of pharmaceutical pricing strategies.”
Increased use of these drugs accounted for 44% of the annualized spending on the 56 oral anticancer drugs in this study.
Researchers found that from 2007 through 2013, “anticancer drugs prices increased 5% above inflation annually, plus 10% per subsequent indication approved. Results of this study demonstrated a continued rise from 2013 through 2017 with a compound annual growth rate of 13% above inflation for drug cost per beneficiary.”
Ms. Seiger and colleagues noted that, from 2013 through 2017, more than $41.4 billion was spent on the 56 oral anticancer drugs examined for the study. These drugs carried an average out-of-pocket cost of $551, accounting for $2.1 billion of the amount spent on these drugs.
“High drug prices on market entry are often attributed to research and development expenses, though research and development may not explain the subsequent increases in drug costs demonstrated in this study,” the researchers stated.
They recommended policy makers consider capping price increases at a set percentage above inflation, “especially given that rising use reflects increased need for these therapies.”
The study was sponsored in part by the department of dermatology at Brigham and Women’s Hospital, Boston. Three of the five authors reported received fees from pharmaceutical manufacturers, and one reported serving as chair for the National Comprehensive Cancer Network.
SOURCE: Kira Seiger et al. JAMA Oncology. doi: 10.1001/jamaoncol.2019.4906.
Price increases are the main source of the increase in spending on oral anticancer drugs in the Medicare Part D prescription drug program, according to new research.
“Annualized spending on the same oral anticancer drugs more than doubled in a 5-year period,” Kira Seiger from Harvard Medical School, Boston, and colleagues wrote in a research letter published online in JAMA Oncology.
“Use increased substantially, likely owing to expanded drug indications, increased Medicare Part D enrollment, and declining cancer mortality yielding longer treatment courses,” the authors continued. “However, increased spending was predominantly driven (56%) by rising drug costs, which is reflective of pharmaceutical pricing strategies.”
Increased use of these drugs accounted for 44% of the annualized spending on the 56 oral anticancer drugs in this study.
Researchers found that from 2007 through 2013, “anticancer drugs prices increased 5% above inflation annually, plus 10% per subsequent indication approved. Results of this study demonstrated a continued rise from 2013 through 2017 with a compound annual growth rate of 13% above inflation for drug cost per beneficiary.”
Ms. Seiger and colleagues noted that, from 2013 through 2017, more than $41.4 billion was spent on the 56 oral anticancer drugs examined for the study. These drugs carried an average out-of-pocket cost of $551, accounting for $2.1 billion of the amount spent on these drugs.
“High drug prices on market entry are often attributed to research and development expenses, though research and development may not explain the subsequent increases in drug costs demonstrated in this study,” the researchers stated.
They recommended policy makers consider capping price increases at a set percentage above inflation, “especially given that rising use reflects increased need for these therapies.”
The study was sponsored in part by the department of dermatology at Brigham and Women’s Hospital, Boston. Three of the five authors reported received fees from pharmaceutical manufacturers, and one reported serving as chair for the National Comprehensive Cancer Network.
SOURCE: Kira Seiger et al. JAMA Oncology. doi: 10.1001/jamaoncol.2019.4906.
Price increases are the main source of the increase in spending on oral anticancer drugs in the Medicare Part D prescription drug program, according to new research.
“Annualized spending on the same oral anticancer drugs more than doubled in a 5-year period,” Kira Seiger from Harvard Medical School, Boston, and colleagues wrote in a research letter published online in JAMA Oncology.
“Use increased substantially, likely owing to expanded drug indications, increased Medicare Part D enrollment, and declining cancer mortality yielding longer treatment courses,” the authors continued. “However, increased spending was predominantly driven (56%) by rising drug costs, which is reflective of pharmaceutical pricing strategies.”
Increased use of these drugs accounted for 44% of the annualized spending on the 56 oral anticancer drugs in this study.
Researchers found that from 2007 through 2013, “anticancer drugs prices increased 5% above inflation annually, plus 10% per subsequent indication approved. Results of this study demonstrated a continued rise from 2013 through 2017 with a compound annual growth rate of 13% above inflation for drug cost per beneficiary.”
Ms. Seiger and colleagues noted that, from 2013 through 2017, more than $41.4 billion was spent on the 56 oral anticancer drugs examined for the study. These drugs carried an average out-of-pocket cost of $551, accounting for $2.1 billion of the amount spent on these drugs.
“High drug prices on market entry are often attributed to research and development expenses, though research and development may not explain the subsequent increases in drug costs demonstrated in this study,” the researchers stated.
They recommended policy makers consider capping price increases at a set percentage above inflation, “especially given that rising use reflects increased need for these therapies.”
The study was sponsored in part by the department of dermatology at Brigham and Women’s Hospital, Boston. Three of the five authors reported received fees from pharmaceutical manufacturers, and one reported serving as chair for the National Comprehensive Cancer Network.
SOURCE: Kira Seiger et al. JAMA Oncology. doi: 10.1001/jamaoncol.2019.4906.
FROM JAMA ONCOLOGY
Sentinel node biopsy safe for women with vulval cancer
Women with vulval cancer who have a negative sentinel node biopsy have a low risk of recurrence and good disease-specific survival outcomes, investigators report.
One of two current standard treatment approaches for early-stage vulval cancer is radical excision of the tumor and inguinofemoral lymph node dissection, wrote Ligita P. Froeding, MD, of Copenhagen University Hospital Rigshospitalet, and coauthors. Their report is in Gynecologic Oncology. However, this procedure is associated with the disabling complication of leg lymphedema, which can significantly affect a woman’s quality of life.
Radical excision with sentinel biopsy is also an option, but the authors said large, population-based studies on the safety of this procedure when performed outside multicenter clinical trials were lacking.
In a prospective, nationwide cohort study, researchers analyzed data from 190 patients with vulval cancer who underwent the sentinel node procedure and had a negative biopsy. Of these, 73 patients had a unilateral procedure and 117 had a bilateral biopsy.
Over a median follow-up of 30 months’ follow-up, 32 patients (16.8%) died – 12 (37.5%) of vulval cancer and 20 (62.5%) from other causes. The 3-year overall survival rate was 84% and disease-specific survival was 93%.
The overall rate of recurrence in these sentinel node–negative women was 12.1% during the follow-up period. Fourteen patients (7.4%) experienced an isolated local vulval recurrence at a median time of 16 months after their primary treatment, and eight of these patients subsequently underwent inguinofemoral lymph node dissection following treatment of the recurrence. Three patients in this group died from vulval cancer, so the 3-year overall survival rate for patients with recurrent disease was 58%.
Four patients developed an isolated groin recurrence at a median of 12 months, and were treated with a combination of inguinofemoral lymph node dissection and chemoradiation. Two then developed a second recurrence.
Histopathological revision of original sentinel node specimens from the four women who experienced groin recurrences revealed that two patients actually had metastases at the time of the sentinel node procedure. In one case there were scattered tumor cells measuring less than 0.1 mm, while in the other there was a metastasis measuring 0.9 mm that was seen in six consecutive slides.
The authors noted that the failure to detect these metastases occurred despite strict adherence to histopathological procedure protocols. They suggested the first misdiagnosis may have been the result of the pathologist’s reluctance to make a histological diagnosis with so few tumor cells present. The second slide was originally screened microscopically by a specially trained medical laboratory technician, before being signed out by a pathologist, which “potentially decreases the pathologist’s diagnostic awareness,” they suggested.
“In conclusion, our study showed that the SN procedure is safe in selected VC patients when the current guidelines are strictly followed, and the procedure is performed in specialized gynecological oncology centers with a high volume of patients.”
No conflicts of interest were declared.
SOURCE: Froeding L et al. Gynecol Oncol 2019 Nov 8. doi: 10.1016/j.ygyno.2019.10.024.
Women with vulval cancer who have a negative sentinel node biopsy have a low risk of recurrence and good disease-specific survival outcomes, investigators report.
One of two current standard treatment approaches for early-stage vulval cancer is radical excision of the tumor and inguinofemoral lymph node dissection, wrote Ligita P. Froeding, MD, of Copenhagen University Hospital Rigshospitalet, and coauthors. Their report is in Gynecologic Oncology. However, this procedure is associated with the disabling complication of leg lymphedema, which can significantly affect a woman’s quality of life.
Radical excision with sentinel biopsy is also an option, but the authors said large, population-based studies on the safety of this procedure when performed outside multicenter clinical trials were lacking.
In a prospective, nationwide cohort study, researchers analyzed data from 190 patients with vulval cancer who underwent the sentinel node procedure and had a negative biopsy. Of these, 73 patients had a unilateral procedure and 117 had a bilateral biopsy.
Over a median follow-up of 30 months’ follow-up, 32 patients (16.8%) died – 12 (37.5%) of vulval cancer and 20 (62.5%) from other causes. The 3-year overall survival rate was 84% and disease-specific survival was 93%.
The overall rate of recurrence in these sentinel node–negative women was 12.1% during the follow-up period. Fourteen patients (7.4%) experienced an isolated local vulval recurrence at a median time of 16 months after their primary treatment, and eight of these patients subsequently underwent inguinofemoral lymph node dissection following treatment of the recurrence. Three patients in this group died from vulval cancer, so the 3-year overall survival rate for patients with recurrent disease was 58%.
Four patients developed an isolated groin recurrence at a median of 12 months, and were treated with a combination of inguinofemoral lymph node dissection and chemoradiation. Two then developed a second recurrence.
Histopathological revision of original sentinel node specimens from the four women who experienced groin recurrences revealed that two patients actually had metastases at the time of the sentinel node procedure. In one case there were scattered tumor cells measuring less than 0.1 mm, while in the other there was a metastasis measuring 0.9 mm that was seen in six consecutive slides.
The authors noted that the failure to detect these metastases occurred despite strict adherence to histopathological procedure protocols. They suggested the first misdiagnosis may have been the result of the pathologist’s reluctance to make a histological diagnosis with so few tumor cells present. The second slide was originally screened microscopically by a specially trained medical laboratory technician, before being signed out by a pathologist, which “potentially decreases the pathologist’s diagnostic awareness,” they suggested.
“In conclusion, our study showed that the SN procedure is safe in selected VC patients when the current guidelines are strictly followed, and the procedure is performed in specialized gynecological oncology centers with a high volume of patients.”
No conflicts of interest were declared.
SOURCE: Froeding L et al. Gynecol Oncol 2019 Nov 8. doi: 10.1016/j.ygyno.2019.10.024.
Women with vulval cancer who have a negative sentinel node biopsy have a low risk of recurrence and good disease-specific survival outcomes, investigators report.
One of two current standard treatment approaches for early-stage vulval cancer is radical excision of the tumor and inguinofemoral lymph node dissection, wrote Ligita P. Froeding, MD, of Copenhagen University Hospital Rigshospitalet, and coauthors. Their report is in Gynecologic Oncology. However, this procedure is associated with the disabling complication of leg lymphedema, which can significantly affect a woman’s quality of life.
Radical excision with sentinel biopsy is also an option, but the authors said large, population-based studies on the safety of this procedure when performed outside multicenter clinical trials were lacking.
In a prospective, nationwide cohort study, researchers analyzed data from 190 patients with vulval cancer who underwent the sentinel node procedure and had a negative biopsy. Of these, 73 patients had a unilateral procedure and 117 had a bilateral biopsy.
Over a median follow-up of 30 months’ follow-up, 32 patients (16.8%) died – 12 (37.5%) of vulval cancer and 20 (62.5%) from other causes. The 3-year overall survival rate was 84% and disease-specific survival was 93%.
The overall rate of recurrence in these sentinel node–negative women was 12.1% during the follow-up period. Fourteen patients (7.4%) experienced an isolated local vulval recurrence at a median time of 16 months after their primary treatment, and eight of these patients subsequently underwent inguinofemoral lymph node dissection following treatment of the recurrence. Three patients in this group died from vulval cancer, so the 3-year overall survival rate for patients with recurrent disease was 58%.
Four patients developed an isolated groin recurrence at a median of 12 months, and were treated with a combination of inguinofemoral lymph node dissection and chemoradiation. Two then developed a second recurrence.
Histopathological revision of original sentinel node specimens from the four women who experienced groin recurrences revealed that two patients actually had metastases at the time of the sentinel node procedure. In one case there were scattered tumor cells measuring less than 0.1 mm, while in the other there was a metastasis measuring 0.9 mm that was seen in six consecutive slides.
The authors noted that the failure to detect these metastases occurred despite strict adherence to histopathological procedure protocols. They suggested the first misdiagnosis may have been the result of the pathologist’s reluctance to make a histological diagnosis with so few tumor cells present. The second slide was originally screened microscopically by a specially trained medical laboratory technician, before being signed out by a pathologist, which “potentially decreases the pathologist’s diagnostic awareness,” they suggested.
“In conclusion, our study showed that the SN procedure is safe in selected VC patients when the current guidelines are strictly followed, and the procedure is performed in specialized gynecological oncology centers with a high volume of patients.”
No conflicts of interest were declared.
SOURCE: Froeding L et al. Gynecol Oncol 2019 Nov 8. doi: 10.1016/j.ygyno.2019.10.024.
FROM GYNECOLOGIC ONCOLOGY
‘Tis the season to reflect and take stock
‘Tis the season to reflect and take stock: Maybe you had a baby, or learned a new procedure, or bought a Tesla? Of course, you made (loads of?) money and treated many patients. Imagine if I asked you this in person, what would you reply? And what made you most proud? I’d tell you this story.
Last week I saw a 50-something-year-old woman for her annual skin screening. She asked if I remembered her mother, who was also my patient. Squinting through my dermatoscope at the nevi on her back, I tried to recall. “Yes, I think so.” (Actually, I was unsure.)
“Well she passed away last week from breast cancer,” she said.
“Oh, I’m sorry to hear that,” I replied.
She added: “Yes, yet she lived much longer than we thought. I want you to know we believe it was in large part because of you.”
I stopped and wheeled around to face her. How could that possibly be true? I had only treated her for a simple skin cancer. She explained that I had seen her mom about a year ago and cut out a skin cancer on her face. Her mom was afraid of needles and of surgery. Apparently when she asked me if it would hurt, I replied: “Well, most patients, yes, but not you.” Pausing, I added: “Because you’re a tough old bird.” She laughed. Apparently that warmth I conveyed and display of confidence in her was just what she needed at that moment. She didn’t flinch.
Not long after, she was diagnosed with breast cancer. When given the news with her children present, she replied, “well, I’ll just fight it. I’m a tough old bird.” It was just what they needed in that moment. “I’m a tough old bird” became their rally cry. Apparently with each stage, surgery, radiation, chemo, they fell back on it. Her son had “Tough Old Bird” made into a magnet and prominently posted on the refrigerator door where she would see it every day.
Sadly, she ultimately succumbed to her disease, but did so later than had been expected and having fought all the way. My patient teared up and asked if she could give me a hug on behalf of her mom. “Thank you, Dr. Benabio. We won’t forget what you did for her.”
I did recall her now, remembering even what exam room she was in when I said it. Yet, I had no idea what I had done. I wonder how many others there were. Of the many things you accomplished this year, try to recall these achievements. Not the psoriasis cleared, or tumor extirpated, or new homes bought. But the comfort and care you brought to the mother with worry, the father with anguish, the daughter with anxieties, or the son with misdeeds.
It is a beautiful, hard, and joyous life we have as physicians, for our “happiness lies in the absorption in some vocation which satisfies the soul; that we are here to add what we can to, not get what we can from life.”* How fortunate are we. Take stock.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Reference
*William Osler, “Doctor and Nurse.” Address given at Training School for Nurses at Johns Hopkins Hospital, June 4, 1891
‘Tis the season to reflect and take stock: Maybe you had a baby, or learned a new procedure, or bought a Tesla? Of course, you made (loads of?) money and treated many patients. Imagine if I asked you this in person, what would you reply? And what made you most proud? I’d tell you this story.
Last week I saw a 50-something-year-old woman for her annual skin screening. She asked if I remembered her mother, who was also my patient. Squinting through my dermatoscope at the nevi on her back, I tried to recall. “Yes, I think so.” (Actually, I was unsure.)
“Well she passed away last week from breast cancer,” she said.
“Oh, I’m sorry to hear that,” I replied.
She added: “Yes, yet she lived much longer than we thought. I want you to know we believe it was in large part because of you.”
I stopped and wheeled around to face her. How could that possibly be true? I had only treated her for a simple skin cancer. She explained that I had seen her mom about a year ago and cut out a skin cancer on her face. Her mom was afraid of needles and of surgery. Apparently when she asked me if it would hurt, I replied: “Well, most patients, yes, but not you.” Pausing, I added: “Because you’re a tough old bird.” She laughed. Apparently that warmth I conveyed and display of confidence in her was just what she needed at that moment. She didn’t flinch.
Not long after, she was diagnosed with breast cancer. When given the news with her children present, she replied, “well, I’ll just fight it. I’m a tough old bird.” It was just what they needed in that moment. “I’m a tough old bird” became their rally cry. Apparently with each stage, surgery, radiation, chemo, they fell back on it. Her son had “Tough Old Bird” made into a magnet and prominently posted on the refrigerator door where she would see it every day.
Sadly, she ultimately succumbed to her disease, but did so later than had been expected and having fought all the way. My patient teared up and asked if she could give me a hug on behalf of her mom. “Thank you, Dr. Benabio. We won’t forget what you did for her.”
I did recall her now, remembering even what exam room she was in when I said it. Yet, I had no idea what I had done. I wonder how many others there were. Of the many things you accomplished this year, try to recall these achievements. Not the psoriasis cleared, or tumor extirpated, or new homes bought. But the comfort and care you brought to the mother with worry, the father with anguish, the daughter with anxieties, or the son with misdeeds.
It is a beautiful, hard, and joyous life we have as physicians, for our “happiness lies in the absorption in some vocation which satisfies the soul; that we are here to add what we can to, not get what we can from life.”* How fortunate are we. Take stock.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Reference
*William Osler, “Doctor and Nurse.” Address given at Training School for Nurses at Johns Hopkins Hospital, June 4, 1891
‘Tis the season to reflect and take stock: Maybe you had a baby, or learned a new procedure, or bought a Tesla? Of course, you made (loads of?) money and treated many patients. Imagine if I asked you this in person, what would you reply? And what made you most proud? I’d tell you this story.
Last week I saw a 50-something-year-old woman for her annual skin screening. She asked if I remembered her mother, who was also my patient. Squinting through my dermatoscope at the nevi on her back, I tried to recall. “Yes, I think so.” (Actually, I was unsure.)
“Well she passed away last week from breast cancer,” she said.
“Oh, I’m sorry to hear that,” I replied.
She added: “Yes, yet she lived much longer than we thought. I want you to know we believe it was in large part because of you.”
I stopped and wheeled around to face her. How could that possibly be true? I had only treated her for a simple skin cancer. She explained that I had seen her mom about a year ago and cut out a skin cancer on her face. Her mom was afraid of needles and of surgery. Apparently when she asked me if it would hurt, I replied: “Well, most patients, yes, but not you.” Pausing, I added: “Because you’re a tough old bird.” She laughed. Apparently that warmth I conveyed and display of confidence in her was just what she needed at that moment. She didn’t flinch.
Not long after, she was diagnosed with breast cancer. When given the news with her children present, she replied, “well, I’ll just fight it. I’m a tough old bird.” It was just what they needed in that moment. “I’m a tough old bird” became their rally cry. Apparently with each stage, surgery, radiation, chemo, they fell back on it. Her son had “Tough Old Bird” made into a magnet and prominently posted on the refrigerator door where she would see it every day.
Sadly, she ultimately succumbed to her disease, but did so later than had been expected and having fought all the way. My patient teared up and asked if she could give me a hug on behalf of her mom. “Thank you, Dr. Benabio. We won’t forget what you did for her.”
I did recall her now, remembering even what exam room she was in when I said it. Yet, I had no idea what I had done. I wonder how many others there were. Of the many things you accomplished this year, try to recall these achievements. Not the psoriasis cleared, or tumor extirpated, or new homes bought. But the comfort and care you brought to the mother with worry, the father with anguish, the daughter with anxieties, or the son with misdeeds.
It is a beautiful, hard, and joyous life we have as physicians, for our “happiness lies in the absorption in some vocation which satisfies the soul; that we are here to add what we can to, not get what we can from life.”* How fortunate are we. Take stock.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Reference
*William Osler, “Doctor and Nurse.” Address given at Training School for Nurses at Johns Hopkins Hospital, June 4, 1891
Foundation launches direct-to-patient registry in multiple myeloma
The Multiple Myeloma Research Foundation (MMRF) recently launched its Direct-to-Patient registry, in what the organization’s leaders are describing as a “disruptive” step toward improving outcomes for patients with multiple myeloma.
The new registry is intended to build upon CoMMpass, a program started 8 years ago that now represents the largest genomic database of any type of cancer. Although CoMMpass includes data from about 1,150 patients with myeloma, it’s not enough information, according to the chief marketing and development officer at the MMRF, Anne Quinn Young.
“For a disease as heterogenous as myeloma is, we need more, particularly because we don’t have all the samples for later-stage disease,” Ms. Quinn Young said in an interview. “And even with the clinical data, given the patient population, both [in terms of] demographics and the nature of the disease, the numbers of patients still living after multiple relapses is rather small.”
In an earlier effort to gather more data, the MMRF first turned to other organizations for help, but this approach fell short because of scarcity of data, and in some cases, unwillingness to share. Steven Labkoff, MD, chief data officer at the MMRF, described this experience in an interview.
“When the MMRF was looking around for different data sources for myeloma data, it was always the claim that, ‘Sure, we have plenty of patients, we have plenty of data, and it’s rich and really complete.’ However, as we approached an array of organizations – big organizations – as we dug into the details and reviewed patient counts or data completeness, they either didn’t have a sufficient number of patients, they didn’t have sufficiently complete data for our needs, and in the case where some did have sufficient numbers and complete data sets, they simply weren’t in a position to share that data outside their institution,” Dr. Labkoff said.
Undeterred, the MMRF switched tactics to the current, patient-centric approach.
“We’re leveraging one aspect of the HIPAA legislation,” Dr. Labkoff said, referring to patients’ rights to request their own medical records and an institution’s legal obligation to provide those records.
In the short-term, the registry will collect three types of data: patient donated data (answers from a patient survey), electronic medical records abstracted from all relevant past providers, and genomic test results. Participating patients will have blood drawn at home by a phlebotomist for the genomic assay. Additional tubes of blood will be concurrently collected and biobanked. This will eventually allow for immune profiling, Dr. Labkoff said.
Future goals include a patient-reported outcomes module and the ability to link data with medical claims.
So far, 79 patients have participated in the pilot program, according to the MMRF. As the database builds, Ms. Quinn Young and Dr. Labkoff anticipate that it will yield answers to a variety of real-world questions.
Dr. Labkoff offered two examples. “Of all the patients who have been exposed to ‘name your drug,’ what were the costs of their therapy, and what were the outcomes?” he said. In addition, researchers will be able to query clinical trial inclusion criteria to search for data on a specific patient profile, such as patients with a 4:14 translocation, who have had a bone marrow transplant in the last 2 years, and have been exposed to a certain drug regimen.
Ms. Quinn Young noted that doctors may be able to use the database to reliably identify high-risk patients and guide agent selection. Common patient questions also will be addressed, she said, including best treatment regimens for certain types of patients.
“For patients who may have run out of all commercially available options, or for patients who are perhaps seen at a community center, where certainly this type of profiling is not standard, it’s opening up a whole new set of options for them,” Ms. Quinn Young said. “And if their physician doesn’t pursue those options, they have the report that they can use to seek a second opinion.”
The Direct-to-Patient registry is unique because it aims to empower patients in a way that hasn’t been done before, Ms. Quinn Young said. “We are committed ... ever since we conceived of this project, to giving results back to patients. That is disruptive because right now that doesn’t exist.”
But the cost of implementing the registry, which has an approximate budget of $20 million, stands in the way of a completely free flow of anonymized data. MMRF leaders are exploring different strategies to sustain funding for the program.
Another MMRF program, CoMMpass, uses a precompetitive consortium model, in which several pharmaceutical companies pay for a preview of the data 6 months in advance of nonprofit researchers. A similar model may be used with the Direct-to-Patient registry, but this has yet to be determined, according to Dr. Labkoff and Ms. Quinn Young.
For now, Ms. Quinn Young said she hopes that physicians will be receptive to the program. “[The short term goal is that] when patients come to their doctors asking about this, that there is support and open-mindedness,” she said.
Looking to the future, Dr. Labkoff described how the registry could accelerate myeloma research, ultimately toward a cure.
“It is generally accepted that it can take 17 years to get something – a therapy, a new drug, or a guideline – from the bench to the bedside,” he said. “It’s my hope that we can take next generation sequencing and the results of this registry and bend that curve, maybe ... to 10 [years], or very aggressively, to 7 or 5 [years], where doctors are able to use the information in these reports for the patients that have literally given themselves, and use this to help guide the choices of their therapy or the trials they apply for, to help them get a better outcome in general.”
The Direct-to-Patient registry is a collaborative effort between the MMRF and multiple organizations, including the health care technology company COTA, the Broad Institute of Harvard and MIT, Prometheus Research, Tempus, and the Dana Farber Cancer Institute.
The Multiple Myeloma Research Foundation (MMRF) recently launched its Direct-to-Patient registry, in what the organization’s leaders are describing as a “disruptive” step toward improving outcomes for patients with multiple myeloma.
The new registry is intended to build upon CoMMpass, a program started 8 years ago that now represents the largest genomic database of any type of cancer. Although CoMMpass includes data from about 1,150 patients with myeloma, it’s not enough information, according to the chief marketing and development officer at the MMRF, Anne Quinn Young.
“For a disease as heterogenous as myeloma is, we need more, particularly because we don’t have all the samples for later-stage disease,” Ms. Quinn Young said in an interview. “And even with the clinical data, given the patient population, both [in terms of] demographics and the nature of the disease, the numbers of patients still living after multiple relapses is rather small.”
In an earlier effort to gather more data, the MMRF first turned to other organizations for help, but this approach fell short because of scarcity of data, and in some cases, unwillingness to share. Steven Labkoff, MD, chief data officer at the MMRF, described this experience in an interview.
“When the MMRF was looking around for different data sources for myeloma data, it was always the claim that, ‘Sure, we have plenty of patients, we have plenty of data, and it’s rich and really complete.’ However, as we approached an array of organizations – big organizations – as we dug into the details and reviewed patient counts or data completeness, they either didn’t have a sufficient number of patients, they didn’t have sufficiently complete data for our needs, and in the case where some did have sufficient numbers and complete data sets, they simply weren’t in a position to share that data outside their institution,” Dr. Labkoff said.
Undeterred, the MMRF switched tactics to the current, patient-centric approach.
“We’re leveraging one aspect of the HIPAA legislation,” Dr. Labkoff said, referring to patients’ rights to request their own medical records and an institution’s legal obligation to provide those records.
In the short-term, the registry will collect three types of data: patient donated data (answers from a patient survey), electronic medical records abstracted from all relevant past providers, and genomic test results. Participating patients will have blood drawn at home by a phlebotomist for the genomic assay. Additional tubes of blood will be concurrently collected and biobanked. This will eventually allow for immune profiling, Dr. Labkoff said.
Future goals include a patient-reported outcomes module and the ability to link data with medical claims.
So far, 79 patients have participated in the pilot program, according to the MMRF. As the database builds, Ms. Quinn Young and Dr. Labkoff anticipate that it will yield answers to a variety of real-world questions.
Dr. Labkoff offered two examples. “Of all the patients who have been exposed to ‘name your drug,’ what were the costs of their therapy, and what were the outcomes?” he said. In addition, researchers will be able to query clinical trial inclusion criteria to search for data on a specific patient profile, such as patients with a 4:14 translocation, who have had a bone marrow transplant in the last 2 years, and have been exposed to a certain drug regimen.
Ms. Quinn Young noted that doctors may be able to use the database to reliably identify high-risk patients and guide agent selection. Common patient questions also will be addressed, she said, including best treatment regimens for certain types of patients.
“For patients who may have run out of all commercially available options, or for patients who are perhaps seen at a community center, where certainly this type of profiling is not standard, it’s opening up a whole new set of options for them,” Ms. Quinn Young said. “And if their physician doesn’t pursue those options, they have the report that they can use to seek a second opinion.”
The Direct-to-Patient registry is unique because it aims to empower patients in a way that hasn’t been done before, Ms. Quinn Young said. “We are committed ... ever since we conceived of this project, to giving results back to patients. That is disruptive because right now that doesn’t exist.”
But the cost of implementing the registry, which has an approximate budget of $20 million, stands in the way of a completely free flow of anonymized data. MMRF leaders are exploring different strategies to sustain funding for the program.
Another MMRF program, CoMMpass, uses a precompetitive consortium model, in which several pharmaceutical companies pay for a preview of the data 6 months in advance of nonprofit researchers. A similar model may be used with the Direct-to-Patient registry, but this has yet to be determined, according to Dr. Labkoff and Ms. Quinn Young.
For now, Ms. Quinn Young said she hopes that physicians will be receptive to the program. “[The short term goal is that] when patients come to their doctors asking about this, that there is support and open-mindedness,” she said.
Looking to the future, Dr. Labkoff described how the registry could accelerate myeloma research, ultimately toward a cure.
“It is generally accepted that it can take 17 years to get something – a therapy, a new drug, or a guideline – from the bench to the bedside,” he said. “It’s my hope that we can take next generation sequencing and the results of this registry and bend that curve, maybe ... to 10 [years], or very aggressively, to 7 or 5 [years], where doctors are able to use the information in these reports for the patients that have literally given themselves, and use this to help guide the choices of their therapy or the trials they apply for, to help them get a better outcome in general.”
The Direct-to-Patient registry is a collaborative effort between the MMRF and multiple organizations, including the health care technology company COTA, the Broad Institute of Harvard and MIT, Prometheus Research, Tempus, and the Dana Farber Cancer Institute.
The Multiple Myeloma Research Foundation (MMRF) recently launched its Direct-to-Patient registry, in what the organization’s leaders are describing as a “disruptive” step toward improving outcomes for patients with multiple myeloma.
The new registry is intended to build upon CoMMpass, a program started 8 years ago that now represents the largest genomic database of any type of cancer. Although CoMMpass includes data from about 1,150 patients with myeloma, it’s not enough information, according to the chief marketing and development officer at the MMRF, Anne Quinn Young.
“For a disease as heterogenous as myeloma is, we need more, particularly because we don’t have all the samples for later-stage disease,” Ms. Quinn Young said in an interview. “And even with the clinical data, given the patient population, both [in terms of] demographics and the nature of the disease, the numbers of patients still living after multiple relapses is rather small.”
In an earlier effort to gather more data, the MMRF first turned to other organizations for help, but this approach fell short because of scarcity of data, and in some cases, unwillingness to share. Steven Labkoff, MD, chief data officer at the MMRF, described this experience in an interview.
“When the MMRF was looking around for different data sources for myeloma data, it was always the claim that, ‘Sure, we have plenty of patients, we have plenty of data, and it’s rich and really complete.’ However, as we approached an array of organizations – big organizations – as we dug into the details and reviewed patient counts or data completeness, they either didn’t have a sufficient number of patients, they didn’t have sufficiently complete data for our needs, and in the case where some did have sufficient numbers and complete data sets, they simply weren’t in a position to share that data outside their institution,” Dr. Labkoff said.
Undeterred, the MMRF switched tactics to the current, patient-centric approach.
“We’re leveraging one aspect of the HIPAA legislation,” Dr. Labkoff said, referring to patients’ rights to request their own medical records and an institution’s legal obligation to provide those records.
In the short-term, the registry will collect three types of data: patient donated data (answers from a patient survey), electronic medical records abstracted from all relevant past providers, and genomic test results. Participating patients will have blood drawn at home by a phlebotomist for the genomic assay. Additional tubes of blood will be concurrently collected and biobanked. This will eventually allow for immune profiling, Dr. Labkoff said.
Future goals include a patient-reported outcomes module and the ability to link data with medical claims.
So far, 79 patients have participated in the pilot program, according to the MMRF. As the database builds, Ms. Quinn Young and Dr. Labkoff anticipate that it will yield answers to a variety of real-world questions.
Dr. Labkoff offered two examples. “Of all the patients who have been exposed to ‘name your drug,’ what were the costs of their therapy, and what were the outcomes?” he said. In addition, researchers will be able to query clinical trial inclusion criteria to search for data on a specific patient profile, such as patients with a 4:14 translocation, who have had a bone marrow transplant in the last 2 years, and have been exposed to a certain drug regimen.
Ms. Quinn Young noted that doctors may be able to use the database to reliably identify high-risk patients and guide agent selection. Common patient questions also will be addressed, she said, including best treatment regimens for certain types of patients.
“For patients who may have run out of all commercially available options, or for patients who are perhaps seen at a community center, where certainly this type of profiling is not standard, it’s opening up a whole new set of options for them,” Ms. Quinn Young said. “And if their physician doesn’t pursue those options, they have the report that they can use to seek a second opinion.”
The Direct-to-Patient registry is unique because it aims to empower patients in a way that hasn’t been done before, Ms. Quinn Young said. “We are committed ... ever since we conceived of this project, to giving results back to patients. That is disruptive because right now that doesn’t exist.”
But the cost of implementing the registry, which has an approximate budget of $20 million, stands in the way of a completely free flow of anonymized data. MMRF leaders are exploring different strategies to sustain funding for the program.
Another MMRF program, CoMMpass, uses a precompetitive consortium model, in which several pharmaceutical companies pay for a preview of the data 6 months in advance of nonprofit researchers. A similar model may be used with the Direct-to-Patient registry, but this has yet to be determined, according to Dr. Labkoff and Ms. Quinn Young.
For now, Ms. Quinn Young said she hopes that physicians will be receptive to the program. “[The short term goal is that] when patients come to their doctors asking about this, that there is support and open-mindedness,” she said.
Looking to the future, Dr. Labkoff described how the registry could accelerate myeloma research, ultimately toward a cure.
“It is generally accepted that it can take 17 years to get something – a therapy, a new drug, or a guideline – from the bench to the bedside,” he said. “It’s my hope that we can take next generation sequencing and the results of this registry and bend that curve, maybe ... to 10 [years], or very aggressively, to 7 or 5 [years], where doctors are able to use the information in these reports for the patients that have literally given themselves, and use this to help guide the choices of their therapy or the trials they apply for, to help them get a better outcome in general.”
The Direct-to-Patient registry is a collaborative effort between the MMRF and multiple organizations, including the health care technology company COTA, the Broad Institute of Harvard and MIT, Prometheus Research, Tempus, and the Dana Farber Cancer Institute.
ATTEST: AFib ablation slows progression to persistence
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
REPORTING FROM THE ESC 2019 CONGRESS
Short Takes
E-cigarettes with behavioral support more effective than nicotine replacement for smoking cessation
A study of 886 randomized United Kingdom National Health Service stop-smoking service attendees showed better 1-year abstinence rates in the e-cigarette (18%) vs. nicotine replacement product (9%) group (risk ratio,1.83; 95% confidence interval, 1.30-2.58) when both groups received behavioral support.
Citation: Hajek P et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Eng J Med. 2019 Feb 14;380:629-37.
New scoring system more accurate in diagnosing sepsis than qSOFA
Using retrospective data from 2,759,529 ED patients in 49 urban hospitals, and a supervised machine-learning process, the authors developed a Risk of Sepsis score, which demonstrated significantly higher sensitivity for detecting sepsis than the qSOFA (Quick Sequential Organ Failure Assessment) score.
Citation: Delahanty R et al. Development and evaluation of a machine learning model for the early identification of patients at risk for sepsis. Ann Emerg Med. 2019 Apr;73(4):334-44.
Shared decision making may decrease risk of legal action
A randomized, controlled simulation experiment using a clinical vignette with an adverse outcome showed that when engaged in shared decision making, participants were less likely to consider taking legal action.
Citation: Schoenfeld EM et al. The effect of shared decision making on patients’ likelihood of filing a complaint or lawsuit: A simulation study. Ann Emerg Med. 2019 Jan 3. doi: 10.1016/j.annemergmed.2018.11.017.
ADA issues new inpatient diabetes care recommendations
The American Diabetes Association recommends that insulin therapy be initiated for a majority of inpatients who have persistent hyperglycemia greater than 180 mg/dL to target a blood glucose range of 140-180 mg/dL. They recommend the use of basal insulin or basal plus bolus insulin and discourage the sole use of sliding scale insulin.
Citation: American Diabetes Association. 15. Diabetes care in the hospital: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl. 1):S173-81.
Beta-blocker use may reduce risk of COPD hospitalization
In a retrospective longitudinal study of 301,542 patients newly prescribed beta-blockers and 1,000,633 patients newly prescribed any other antihypertensive drug, patients who were treated with beta-blockers continuously for more than 6 months had a significantly lower risk of chronic obstructive pulmonary disease (COPD) hospitalization, all-cause mortality, and COPD death than did patients who received alternative antihypertensives. Patients with a history of COPD hospitalization were excluded from this study.
Citation: Nielsen AO et al. Beta-blocker therapy and risk of chronic obstructive pulmonary disease: A Danish nationwide study of 1.3 million individuals. EClinicalMedicine. 2019;7:21-6. doi: 10.1016/j.eclinm.2019.01.004.
E-cigarettes with behavioral support more effective than nicotine replacement for smoking cessation
A study of 886 randomized United Kingdom National Health Service stop-smoking service attendees showed better 1-year abstinence rates in the e-cigarette (18%) vs. nicotine replacement product (9%) group (risk ratio,1.83; 95% confidence interval, 1.30-2.58) when both groups received behavioral support.
Citation: Hajek P et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Eng J Med. 2019 Feb 14;380:629-37.
New scoring system more accurate in diagnosing sepsis than qSOFA
Using retrospective data from 2,759,529 ED patients in 49 urban hospitals, and a supervised machine-learning process, the authors developed a Risk of Sepsis score, which demonstrated significantly higher sensitivity for detecting sepsis than the qSOFA (Quick Sequential Organ Failure Assessment) score.
Citation: Delahanty R et al. Development and evaluation of a machine learning model for the early identification of patients at risk for sepsis. Ann Emerg Med. 2019 Apr;73(4):334-44.
Shared decision making may decrease risk of legal action
A randomized, controlled simulation experiment using a clinical vignette with an adverse outcome showed that when engaged in shared decision making, participants were less likely to consider taking legal action.
Citation: Schoenfeld EM et al. The effect of shared decision making on patients’ likelihood of filing a complaint or lawsuit: A simulation study. Ann Emerg Med. 2019 Jan 3. doi: 10.1016/j.annemergmed.2018.11.017.
ADA issues new inpatient diabetes care recommendations
The American Diabetes Association recommends that insulin therapy be initiated for a majority of inpatients who have persistent hyperglycemia greater than 180 mg/dL to target a blood glucose range of 140-180 mg/dL. They recommend the use of basal insulin or basal plus bolus insulin and discourage the sole use of sliding scale insulin.
Citation: American Diabetes Association. 15. Diabetes care in the hospital: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl. 1):S173-81.
Beta-blocker use may reduce risk of COPD hospitalization
In a retrospective longitudinal study of 301,542 patients newly prescribed beta-blockers and 1,000,633 patients newly prescribed any other antihypertensive drug, patients who were treated with beta-blockers continuously for more than 6 months had a significantly lower risk of chronic obstructive pulmonary disease (COPD) hospitalization, all-cause mortality, and COPD death than did patients who received alternative antihypertensives. Patients with a history of COPD hospitalization were excluded from this study.
Citation: Nielsen AO et al. Beta-blocker therapy and risk of chronic obstructive pulmonary disease: A Danish nationwide study of 1.3 million individuals. EClinicalMedicine. 2019;7:21-6. doi: 10.1016/j.eclinm.2019.01.004.
E-cigarettes with behavioral support more effective than nicotine replacement for smoking cessation
A study of 886 randomized United Kingdom National Health Service stop-smoking service attendees showed better 1-year abstinence rates in the e-cigarette (18%) vs. nicotine replacement product (9%) group (risk ratio,1.83; 95% confidence interval, 1.30-2.58) when both groups received behavioral support.
Citation: Hajek P et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Eng J Med. 2019 Feb 14;380:629-37.
New scoring system more accurate in diagnosing sepsis than qSOFA
Using retrospective data from 2,759,529 ED patients in 49 urban hospitals, and a supervised machine-learning process, the authors developed a Risk of Sepsis score, which demonstrated significantly higher sensitivity for detecting sepsis than the qSOFA (Quick Sequential Organ Failure Assessment) score.
Citation: Delahanty R et al. Development and evaluation of a machine learning model for the early identification of patients at risk for sepsis. Ann Emerg Med. 2019 Apr;73(4):334-44.
Shared decision making may decrease risk of legal action
A randomized, controlled simulation experiment using a clinical vignette with an adverse outcome showed that when engaged in shared decision making, participants were less likely to consider taking legal action.
Citation: Schoenfeld EM et al. The effect of shared decision making on patients’ likelihood of filing a complaint or lawsuit: A simulation study. Ann Emerg Med. 2019 Jan 3. doi: 10.1016/j.annemergmed.2018.11.017.
ADA issues new inpatient diabetes care recommendations
The American Diabetes Association recommends that insulin therapy be initiated for a majority of inpatients who have persistent hyperglycemia greater than 180 mg/dL to target a blood glucose range of 140-180 mg/dL. They recommend the use of basal insulin or basal plus bolus insulin and discourage the sole use of sliding scale insulin.
Citation: American Diabetes Association. 15. Diabetes care in the hospital: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl. 1):S173-81.
Beta-blocker use may reduce risk of COPD hospitalization
In a retrospective longitudinal study of 301,542 patients newly prescribed beta-blockers and 1,000,633 patients newly prescribed any other antihypertensive drug, patients who were treated with beta-blockers continuously for more than 6 months had a significantly lower risk of chronic obstructive pulmonary disease (COPD) hospitalization, all-cause mortality, and COPD death than did patients who received alternative antihypertensives. Patients with a history of COPD hospitalization were excluded from this study.
Citation: Nielsen AO et al. Beta-blocker therapy and risk of chronic obstructive pulmonary disease: A Danish nationwide study of 1.3 million individuals. EClinicalMedicine. 2019;7:21-6. doi: 10.1016/j.eclinm.2019.01.004.