User login
BRCA2 mutations linked to childhood NHL
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
FROM JAMA ONCOLOGY
Study outlines survival factors with nivolumab
Predictors of long-term survival of patients with advanced melanoma, renal cell carcinoma (RCC), non–small cell lung cancer (NSCLC), and other malignancies treated with nivolumab include the absence of liver or bone metastases, excellent baseline performance status, and the presence of grade 3 or greater treatment-related adverse events, investigators have found.
A secondary analysis of the phase 1 CA209-003 trial with expansion cohorts showed that, among 270 heavily pretreated patients with melanoma, RCC, and NSCLC who received single-agent nivolumab (Opdivo) during this trial, those with liver or bone metastases had a 69% higher risk for death within 5 years.
In contrast, patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0 had a nearly threefold higher chance for survival, compared with patients with less favorable performance status scores, reported Suzanne L. Topalian, MD, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore and colleagues.
“The results of this study suggest that survival benefits reported in the more limited follow-up of recent nivolumab randomized clinical trials may persist for prolonged periods in some patients, extending to at least 5 years,” they wrote in JAMA Oncology.
In the CA209-003 trial, investigators enrolled patients 18 years or older with documented evidence of advanced melanoma, RCC, NSCLC, castration-resistant prostate cancer, or colorectal cancer. To be eligible, patients needed to have received 1-5 previous systemic therapies for advanced or recurrent cancer, measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0, and an ECOG performance status of 0-2. The current survival analysis included data on 107 patients with melanoma, 34 with RCC, and 129 with NSCLC.
Estimated 5-year overall survival rates were 34.2% for patients with melanoma, 27.7% for patients with RCC, and 15.6% for patients with NSCLC. A multivariable analysis controlling for age, sex, performance status, metastatic disease, and number of prior therapies showed that the presence of either liver or bone metastases was associated with an odds ratio for 5-year survival of 0.31 (P = .02 and .04, respectively).
One factor favorably associated with survival included ECOG performance status 0 (OR, 2.74; P = .003). The investigators also found that treatment-related adverse events (AEs) were associated with longer overall survival, with a median of 19.8 months for patients with any grade of treatment-related event and 20.3 months for patients with grade 3 or greater events, compared with a median of 5.8 months for patients with no treatment-related events (P less than .001 for each comparison based on hazard ratios).
“Of note, patients in our study who developed treatment-related AEs, regardless of whether the AEs were deemed to have an immune-mediated causality, had significantly higher ORRs [overall response rates] and prolonged 5-year OS. These findings are reminiscent of some reports of anti–CTLA-4 therapy and align with other studies of anti–PD-1 therapies, “ Dr. Topalian and associates wrote.
The study and the secondary analysis were supported by Bristol-Myers Squibb. Dr. Topalian disclosed grants and travel reimbursements from Bristol-Myers Squibb and consulting fees with other entities. Multiple co-authors reported similar relationships. Four of the co-authors are Bristol-Myers Squibb employees.
SOURCE: Topalian SL et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2187.
Although the existence of a subset of patients experiencing long-term survival certainly substantiates the role of PD-1/ PD-L1 checkpoint blockade in cancer immunotherapy, it is noteworthy to consider that these agents as monotherapy have not yielded sufficient activity and efficacy to replace standard-of-care therapy in the first line of therapy in advanced solid tumors, with the exception of NSCLC expressing high levels of PD-L1 and melanoma; emerging results also restrict monotherapy to stringently defined subsets of patients with gastric, esophageal, head and neck, and bladder cancers. Baseline predictive biomarkers have demonstrated distinct shortcomings, the first being their poor discriminatory ability and low negative predictive value. The clinician keen on securing the best possible outcome for his patients is thus left with the necessity for indiscriminate administration of PD-1/PD-L1 checkpoint inhibitors.
Unsurprisingly, the field of combination therapies using PD-1/PD-L1 checkpoint blockade as a backbone has been growing exponentially; a recent review shows more than 2,250 immunotherapy trials, 1,716 of which are investigating PD-1/ PD-L1 checkpoint inhibitors with more than 240 combination partners. Analysis of the pipeline also reveals a 67% increase in the number of active agents, amounting to more than 3,300, between September 2017 and September 2018. A noteworthy development is a 113% increase in cell therapies, and an increase of agents targeting neoantigens identified through bioinformatics analysis of an individual patient’s tumor, suggesting a shift toward increased personalization of immunotherapy. The observation that clinical development of immunotherapy agents has outstripped our understanding of the cancer-immune interactions advocates for renewed collective efforts in standardizing immune monitoring methods in clinical trials to identify immune evasion pathways that are dominant and to build novel trial designs able to efficiently enhance matching of patients with therapy.
Stefan Zimmermann, MD, and Solange Peters, MD, PhD, are from the Centre Hospitalier Universitaire Vaudois in Lausanne,Switzerland. Their remarks are excerpted and adapted from an editorial accompanying the study (JAMA Oncol. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2186). Dr. Zimmerman disclosed fees for advisory roles, travel grants, and clinical research support from Bristol-Myers Squibb and others. Dr. Peters disclosed fees for advisory board participation and/or lectures from Bristol-Myers Squibb and others.
Although the existence of a subset of patients experiencing long-term survival certainly substantiates the role of PD-1/ PD-L1 checkpoint blockade in cancer immunotherapy, it is noteworthy to consider that these agents as monotherapy have not yielded sufficient activity and efficacy to replace standard-of-care therapy in the first line of therapy in advanced solid tumors, with the exception of NSCLC expressing high levels of PD-L1 and melanoma; emerging results also restrict monotherapy to stringently defined subsets of patients with gastric, esophageal, head and neck, and bladder cancers. Baseline predictive biomarkers have demonstrated distinct shortcomings, the first being their poor discriminatory ability and low negative predictive value. The clinician keen on securing the best possible outcome for his patients is thus left with the necessity for indiscriminate administration of PD-1/PD-L1 checkpoint inhibitors.
Unsurprisingly, the field of combination therapies using PD-1/PD-L1 checkpoint blockade as a backbone has been growing exponentially; a recent review shows more than 2,250 immunotherapy trials, 1,716 of which are investigating PD-1/ PD-L1 checkpoint inhibitors with more than 240 combination partners. Analysis of the pipeline also reveals a 67% increase in the number of active agents, amounting to more than 3,300, between September 2017 and September 2018. A noteworthy development is a 113% increase in cell therapies, and an increase of agents targeting neoantigens identified through bioinformatics analysis of an individual patient’s tumor, suggesting a shift toward increased personalization of immunotherapy. The observation that clinical development of immunotherapy agents has outstripped our understanding of the cancer-immune interactions advocates for renewed collective efforts in standardizing immune monitoring methods in clinical trials to identify immune evasion pathways that are dominant and to build novel trial designs able to efficiently enhance matching of patients with therapy.
Stefan Zimmermann, MD, and Solange Peters, MD, PhD, are from the Centre Hospitalier Universitaire Vaudois in Lausanne,Switzerland. Their remarks are excerpted and adapted from an editorial accompanying the study (JAMA Oncol. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2186). Dr. Zimmerman disclosed fees for advisory roles, travel grants, and clinical research support from Bristol-Myers Squibb and others. Dr. Peters disclosed fees for advisory board participation and/or lectures from Bristol-Myers Squibb and others.
Although the existence of a subset of patients experiencing long-term survival certainly substantiates the role of PD-1/ PD-L1 checkpoint blockade in cancer immunotherapy, it is noteworthy to consider that these agents as monotherapy have not yielded sufficient activity and efficacy to replace standard-of-care therapy in the first line of therapy in advanced solid tumors, with the exception of NSCLC expressing high levels of PD-L1 and melanoma; emerging results also restrict monotherapy to stringently defined subsets of patients with gastric, esophageal, head and neck, and bladder cancers. Baseline predictive biomarkers have demonstrated distinct shortcomings, the first being their poor discriminatory ability and low negative predictive value. The clinician keen on securing the best possible outcome for his patients is thus left with the necessity for indiscriminate administration of PD-1/PD-L1 checkpoint inhibitors.
Unsurprisingly, the field of combination therapies using PD-1/PD-L1 checkpoint blockade as a backbone has been growing exponentially; a recent review shows more than 2,250 immunotherapy trials, 1,716 of which are investigating PD-1/ PD-L1 checkpoint inhibitors with more than 240 combination partners. Analysis of the pipeline also reveals a 67% increase in the number of active agents, amounting to more than 3,300, between September 2017 and September 2018. A noteworthy development is a 113% increase in cell therapies, and an increase of agents targeting neoantigens identified through bioinformatics analysis of an individual patient’s tumor, suggesting a shift toward increased personalization of immunotherapy. The observation that clinical development of immunotherapy agents has outstripped our understanding of the cancer-immune interactions advocates for renewed collective efforts in standardizing immune monitoring methods in clinical trials to identify immune evasion pathways that are dominant and to build novel trial designs able to efficiently enhance matching of patients with therapy.
Stefan Zimmermann, MD, and Solange Peters, MD, PhD, are from the Centre Hospitalier Universitaire Vaudois in Lausanne,Switzerland. Their remarks are excerpted and adapted from an editorial accompanying the study (JAMA Oncol. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2186). Dr. Zimmerman disclosed fees for advisory roles, travel grants, and clinical research support from Bristol-Myers Squibb and others. Dr. Peters disclosed fees for advisory board participation and/or lectures from Bristol-Myers Squibb and others.
Predictors of long-term survival of patients with advanced melanoma, renal cell carcinoma (RCC), non–small cell lung cancer (NSCLC), and other malignancies treated with nivolumab include the absence of liver or bone metastases, excellent baseline performance status, and the presence of grade 3 or greater treatment-related adverse events, investigators have found.
A secondary analysis of the phase 1 CA209-003 trial with expansion cohorts showed that, among 270 heavily pretreated patients with melanoma, RCC, and NSCLC who received single-agent nivolumab (Opdivo) during this trial, those with liver or bone metastases had a 69% higher risk for death within 5 years.
In contrast, patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0 had a nearly threefold higher chance for survival, compared with patients with less favorable performance status scores, reported Suzanne L. Topalian, MD, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore and colleagues.
“The results of this study suggest that survival benefits reported in the more limited follow-up of recent nivolumab randomized clinical trials may persist for prolonged periods in some patients, extending to at least 5 years,” they wrote in JAMA Oncology.
In the CA209-003 trial, investigators enrolled patients 18 years or older with documented evidence of advanced melanoma, RCC, NSCLC, castration-resistant prostate cancer, or colorectal cancer. To be eligible, patients needed to have received 1-5 previous systemic therapies for advanced or recurrent cancer, measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0, and an ECOG performance status of 0-2. The current survival analysis included data on 107 patients with melanoma, 34 with RCC, and 129 with NSCLC.
Estimated 5-year overall survival rates were 34.2% for patients with melanoma, 27.7% for patients with RCC, and 15.6% for patients with NSCLC. A multivariable analysis controlling for age, sex, performance status, metastatic disease, and number of prior therapies showed that the presence of either liver or bone metastases was associated with an odds ratio for 5-year survival of 0.31 (P = .02 and .04, respectively).
One factor favorably associated with survival included ECOG performance status 0 (OR, 2.74; P = .003). The investigators also found that treatment-related adverse events (AEs) were associated with longer overall survival, with a median of 19.8 months for patients with any grade of treatment-related event and 20.3 months for patients with grade 3 or greater events, compared with a median of 5.8 months for patients with no treatment-related events (P less than .001 for each comparison based on hazard ratios).
“Of note, patients in our study who developed treatment-related AEs, regardless of whether the AEs were deemed to have an immune-mediated causality, had significantly higher ORRs [overall response rates] and prolonged 5-year OS. These findings are reminiscent of some reports of anti–CTLA-4 therapy and align with other studies of anti–PD-1 therapies, “ Dr. Topalian and associates wrote.
The study and the secondary analysis were supported by Bristol-Myers Squibb. Dr. Topalian disclosed grants and travel reimbursements from Bristol-Myers Squibb and consulting fees with other entities. Multiple co-authors reported similar relationships. Four of the co-authors are Bristol-Myers Squibb employees.
SOURCE: Topalian SL et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2187.
Predictors of long-term survival of patients with advanced melanoma, renal cell carcinoma (RCC), non–small cell lung cancer (NSCLC), and other malignancies treated with nivolumab include the absence of liver or bone metastases, excellent baseline performance status, and the presence of grade 3 or greater treatment-related adverse events, investigators have found.
A secondary analysis of the phase 1 CA209-003 trial with expansion cohorts showed that, among 270 heavily pretreated patients with melanoma, RCC, and NSCLC who received single-agent nivolumab (Opdivo) during this trial, those with liver or bone metastases had a 69% higher risk for death within 5 years.
In contrast, patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0 had a nearly threefold higher chance for survival, compared with patients with less favorable performance status scores, reported Suzanne L. Topalian, MD, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore and colleagues.
“The results of this study suggest that survival benefits reported in the more limited follow-up of recent nivolumab randomized clinical trials may persist for prolonged periods in some patients, extending to at least 5 years,” they wrote in JAMA Oncology.
In the CA209-003 trial, investigators enrolled patients 18 years or older with documented evidence of advanced melanoma, RCC, NSCLC, castration-resistant prostate cancer, or colorectal cancer. To be eligible, patients needed to have received 1-5 previous systemic therapies for advanced or recurrent cancer, measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0, and an ECOG performance status of 0-2. The current survival analysis included data on 107 patients with melanoma, 34 with RCC, and 129 with NSCLC.
Estimated 5-year overall survival rates were 34.2% for patients with melanoma, 27.7% for patients with RCC, and 15.6% for patients with NSCLC. A multivariable analysis controlling for age, sex, performance status, metastatic disease, and number of prior therapies showed that the presence of either liver or bone metastases was associated with an odds ratio for 5-year survival of 0.31 (P = .02 and .04, respectively).
One factor favorably associated with survival included ECOG performance status 0 (OR, 2.74; P = .003). The investigators also found that treatment-related adverse events (AEs) were associated with longer overall survival, with a median of 19.8 months for patients with any grade of treatment-related event and 20.3 months for patients with grade 3 or greater events, compared with a median of 5.8 months for patients with no treatment-related events (P less than .001 for each comparison based on hazard ratios).
“Of note, patients in our study who developed treatment-related AEs, regardless of whether the AEs were deemed to have an immune-mediated causality, had significantly higher ORRs [overall response rates] and prolonged 5-year OS. These findings are reminiscent of some reports of anti–CTLA-4 therapy and align with other studies of anti–PD-1 therapies, “ Dr. Topalian and associates wrote.
The study and the secondary analysis were supported by Bristol-Myers Squibb. Dr. Topalian disclosed grants and travel reimbursements from Bristol-Myers Squibb and consulting fees with other entities. Multiple co-authors reported similar relationships. Four of the co-authors are Bristol-Myers Squibb employees.
SOURCE: Topalian SL et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2187.
FROM JAMA ONCOLOGY
Novel translocation inhibitor shows efficacy in treatment-naive HIV-1–infected adults
The first-in-class antiretroviral therapy islatravir (Merck) was well tolerated and had promising efficacy in a phase 2B study including treatment-naive adults with HIV-1 infection, supporting plans to initiate a phase 3 trial, an investigator said at the International AIDS Society Conference on HIV Science.
The proportion of patients achieving viral suppression at week 48 with combinations including the nucleoside transcriptase translocation inhibitor (NRTTI) was comparable to what was achieved with a standard triple regimen, said investigator Jean-Michel Molina, MD, professor of infectious diseases at the University of Paris Diderot, and head of the infectious diseases department at the Saint-Louis Hospital in Paris
The treatment was effective not only as part of a three-drug combination of islatravir, doravirine, and lamivudine over 24 weeks, but also over an additional 24 weeks in patients who achieved viral suppression and were switched to dual therapy with islatravir and doravirine, according to Dr. Molina.
“These are promising data that will encourage the company to move to a phase 3 trial to see how these results can be confirmed in a larger study set, and also to assess the potency of the dual combination for maintenance therapy in the future, providing also novel options for people with a drug that has a high genetic barrier to resistance and efficacy that seems to be quite interesting,” Dr. Molina said in an IAS press conference in Mexico City.
This drug has very potent activity not only against wild-type HIV-1 viruses, but also multiresistant viruses, according to Dr. Molina.
“It has a high inhibitory quotient at a very low dose, so you give people a tiny amount of drug – in the range of 1 milligram per day, instead of a few hundred milligrams with other, regular drugs,” he said.
Another attribute of islatravir is its long half-life of approximately 120 hours, allowing not only for once-daily dosing, but potentially for evaluation as once-weekly or once-monthly dosing in the future, he said, adding that a subdermal islatravir-eluting implant under investigation for preexposure prophylaxis has potential as a once-yearly option.
The international, multicenter, 121-patient clinical trial that Dr. Molina described included adults with HIV-1 infection naive to antiretroviral therapy randomized to islatravir (in one of three doses) plus doravirine and lamivudine, or to the combination of doravirine, lamivudine, and tenofovir (Delstrigo, Merck).
After at least 24 weeks of treatment, subjects in the islatravir treatment groups were transitioned to the two-drug combination of islatravir and doravirine if they had HIV-1 RNA levels less than 50 copies/mL and did not meet any protocol-defined criteria for virologic failure.
Those participants in the islatravir arms who received 48 weeks of treatment had “very good response” and safety that was comparable to the control arm, according to Dr. Molina.
At 48 weeks, the proportion of patients with HIV-1 RNA less than 50 copies/mL were 89.7%, 90%, and 77.4% for regimens containing islatravir 0.25 mg, 0.75 mg, and 2.25 mg, respectively, and 83.9% for those receiving the standard triple therapy, according to reported data.
All patients with protocol-defined virologic failure (greater than or equal to 50 copies/mL) in the study actually had very low viral load, below 80 copies/mL, Dr. Molina said.
The study was supported by Merck. Dr. Molina has been on the Merck advisory board and speaker’s bureau.
SOURCE: Molina J-M et al. IAS 2019, Abstract WEAB0402LB.
The first-in-class antiretroviral therapy islatravir (Merck) was well tolerated and had promising efficacy in a phase 2B study including treatment-naive adults with HIV-1 infection, supporting plans to initiate a phase 3 trial, an investigator said at the International AIDS Society Conference on HIV Science.
The proportion of patients achieving viral suppression at week 48 with combinations including the nucleoside transcriptase translocation inhibitor (NRTTI) was comparable to what was achieved with a standard triple regimen, said investigator Jean-Michel Molina, MD, professor of infectious diseases at the University of Paris Diderot, and head of the infectious diseases department at the Saint-Louis Hospital in Paris
The treatment was effective not only as part of a three-drug combination of islatravir, doravirine, and lamivudine over 24 weeks, but also over an additional 24 weeks in patients who achieved viral suppression and were switched to dual therapy with islatravir and doravirine, according to Dr. Molina.
“These are promising data that will encourage the company to move to a phase 3 trial to see how these results can be confirmed in a larger study set, and also to assess the potency of the dual combination for maintenance therapy in the future, providing also novel options for people with a drug that has a high genetic barrier to resistance and efficacy that seems to be quite interesting,” Dr. Molina said in an IAS press conference in Mexico City.
This drug has very potent activity not only against wild-type HIV-1 viruses, but also multiresistant viruses, according to Dr. Molina.
“It has a high inhibitory quotient at a very low dose, so you give people a tiny amount of drug – in the range of 1 milligram per day, instead of a few hundred milligrams with other, regular drugs,” he said.
Another attribute of islatravir is its long half-life of approximately 120 hours, allowing not only for once-daily dosing, but potentially for evaluation as once-weekly or once-monthly dosing in the future, he said, adding that a subdermal islatravir-eluting implant under investigation for preexposure prophylaxis has potential as a once-yearly option.
The international, multicenter, 121-patient clinical trial that Dr. Molina described included adults with HIV-1 infection naive to antiretroviral therapy randomized to islatravir (in one of three doses) plus doravirine and lamivudine, or to the combination of doravirine, lamivudine, and tenofovir (Delstrigo, Merck).
After at least 24 weeks of treatment, subjects in the islatravir treatment groups were transitioned to the two-drug combination of islatravir and doravirine if they had HIV-1 RNA levels less than 50 copies/mL and did not meet any protocol-defined criteria for virologic failure.
Those participants in the islatravir arms who received 48 weeks of treatment had “very good response” and safety that was comparable to the control arm, according to Dr. Molina.
At 48 weeks, the proportion of patients with HIV-1 RNA less than 50 copies/mL were 89.7%, 90%, and 77.4% for regimens containing islatravir 0.25 mg, 0.75 mg, and 2.25 mg, respectively, and 83.9% for those receiving the standard triple therapy, according to reported data.
All patients with protocol-defined virologic failure (greater than or equal to 50 copies/mL) in the study actually had very low viral load, below 80 copies/mL, Dr. Molina said.
The study was supported by Merck. Dr. Molina has been on the Merck advisory board and speaker’s bureau.
SOURCE: Molina J-M et al. IAS 2019, Abstract WEAB0402LB.
The first-in-class antiretroviral therapy islatravir (Merck) was well tolerated and had promising efficacy in a phase 2B study including treatment-naive adults with HIV-1 infection, supporting plans to initiate a phase 3 trial, an investigator said at the International AIDS Society Conference on HIV Science.
The proportion of patients achieving viral suppression at week 48 with combinations including the nucleoside transcriptase translocation inhibitor (NRTTI) was comparable to what was achieved with a standard triple regimen, said investigator Jean-Michel Molina, MD, professor of infectious diseases at the University of Paris Diderot, and head of the infectious diseases department at the Saint-Louis Hospital in Paris
The treatment was effective not only as part of a three-drug combination of islatravir, doravirine, and lamivudine over 24 weeks, but also over an additional 24 weeks in patients who achieved viral suppression and were switched to dual therapy with islatravir and doravirine, according to Dr. Molina.
“These are promising data that will encourage the company to move to a phase 3 trial to see how these results can be confirmed in a larger study set, and also to assess the potency of the dual combination for maintenance therapy in the future, providing also novel options for people with a drug that has a high genetic barrier to resistance and efficacy that seems to be quite interesting,” Dr. Molina said in an IAS press conference in Mexico City.
This drug has very potent activity not only against wild-type HIV-1 viruses, but also multiresistant viruses, according to Dr. Molina.
“It has a high inhibitory quotient at a very low dose, so you give people a tiny amount of drug – in the range of 1 milligram per day, instead of a few hundred milligrams with other, regular drugs,” he said.
Another attribute of islatravir is its long half-life of approximately 120 hours, allowing not only for once-daily dosing, but potentially for evaluation as once-weekly or once-monthly dosing in the future, he said, adding that a subdermal islatravir-eluting implant under investigation for preexposure prophylaxis has potential as a once-yearly option.
The international, multicenter, 121-patient clinical trial that Dr. Molina described included adults with HIV-1 infection naive to antiretroviral therapy randomized to islatravir (in one of three doses) plus doravirine and lamivudine, or to the combination of doravirine, lamivudine, and tenofovir (Delstrigo, Merck).
After at least 24 weeks of treatment, subjects in the islatravir treatment groups were transitioned to the two-drug combination of islatravir and doravirine if they had HIV-1 RNA levels less than 50 copies/mL and did not meet any protocol-defined criteria for virologic failure.
Those participants in the islatravir arms who received 48 weeks of treatment had “very good response” and safety that was comparable to the control arm, according to Dr. Molina.
At 48 weeks, the proportion of patients with HIV-1 RNA less than 50 copies/mL were 89.7%, 90%, and 77.4% for regimens containing islatravir 0.25 mg, 0.75 mg, and 2.25 mg, respectively, and 83.9% for those receiving the standard triple therapy, according to reported data.
All patients with protocol-defined virologic failure (greater than or equal to 50 copies/mL) in the study actually had very low viral load, below 80 copies/mL, Dr. Molina said.
The study was supported by Merck. Dr. Molina has been on the Merck advisory board and speaker’s bureau.
SOURCE: Molina J-M et al. IAS 2019, Abstract WEAB0402LB.
FROM IAS 2019
Results support first-line T-DM1 in HER2+ breast cancer
Trastuzumab emtansine (T-DM1) is a suitable first-line therapy for patients with HER2-positive, advanced breast cancer who cannot receive taxane-based therapy, according to researchers.
Final results from the phase 3 MARIANNE trial revealed similar overall survival (OS) in patients who received T-DM1, T-DM1 plus pertuzumab, or trastuzumab plus a taxane (HT). All three regimens resulted in a median OS exceeding 50 months.
The incidence of grade 3 or higher adverse events (AEs) was highest in patients who received HT.
Edith A. Perez, MD, of Mayo Clinic Cancer Center in Jacksonville, Fla., and colleagues reported these results in Cancer.
The MARIANNE trial (NCT01120184) enrolled 1,095 adults with HER2-positive, advanced breast cancer. They were randomized to receive HT, T-DM1, or T-DM1 plus pertuzumab. Patients in the HT arm received trastuzumab plus paclitaxel or docetaxel according to the investigator’s discretion.
In all, 352 patients received HT (257 on docetaxel and 96 on paclitaxel), 361 patients received T-DM1 plus placebo, and 366 received T-DM1 plus pertuzumab.
Response and OS
In the primary analysis, the median OS was not reached in any treatment arm at a median follow-up of 35 months. The rate of objective response was 67.9% in the HT arm, 64.2% in the T-DM1 plus pertuzumab arm, and 59.7% in the T-DM1 arm. The median duration of response was 12.5 months, 21.2 months, and 20.7 months, respectively.
For the final OS analysis, the median duration of follow-up was 54 months. Roughly 70% of patients in each arm had received at least one treatment regimen during follow-up.
The final median OS was similar across the treatment arms – 50.9 months in the HT arm, 53.7 months in the T-DM1 arm, and 51.8 months in the T-DM1 plus pertuzumab arm. With the HT arm as a reference, the stratified hazard ratio was 0.93 for the T-DM1 arm and 0.86 for the T-DM1 plus pertuzumab arm.
OS results were consistent across subgroups. Although there were some differences in hazard ratios, “none of the examined subgroups showed a clear benefit with one treatment regimen in comparison with the others,” the researchers wrote.
The researchers also analyzed OS by response status at 6.5 months after randomization. Among nonresponders, the median OS was 41.9 months in the T-DM1 plus pertuzumab arm, 45.7 months in the T-DM1 arm, and 48.1 months in the HT arm. Among responders, the median OS was not reached in the T-DM1 plus pertuzumab arm, 64.4 months, and 56.3 months, respectively.
There were no baseline characteristics or biomarkers that were strongly associated with response by treatment group. However, in the HT and T-DM1 arms, patients with above-median HER2 messenger RNA expression were more likely to respond.
Safety
Rates of grade 3 or higher AEs were 55.8% in the HT arm, 47.1% in the T-DM1 arm, and 48.6% in the T-DM1 plus pertuzumab arm. The most common grade 3 or higher AEs were as follows:
- HT arm – neutropenia (19.3%), febrile neutropenia (6.5%), and diarrhea (4.2%).
- T-DM1 arm – increased aspartate aminotransferase (6.9%), thrombocytopenia (6.6%), and anemia (5.0%).
- T-DM1 plus pertuzumab arm – thrombocytopenia (9.0%), anemia (7.1%), and increased alanine aminotransferase (6.0%).
Rates of AE-related treatment discontinuation were 20.8% in the T-DM1 arm, 23.0% in the T-DM1 plus pertuzumab arm, and 30.6% in the HT arm. Rates of AE-related death were 1.4%, 1.9%, and 2.0%, respectively.
This study was funded by F. Hoffmann–La Roche. Dr. Perez was previously employed by Genentech/Roche. Her fellow authors disclosed relationships with Roche and many other companies.
SOURCE: Perez EA et al. Cancer. 2019 Jul 18. doi: 10.1002/cncr.32392.
Trastuzumab emtansine (T-DM1) is a suitable first-line therapy for patients with HER2-positive, advanced breast cancer who cannot receive taxane-based therapy, according to researchers.
Final results from the phase 3 MARIANNE trial revealed similar overall survival (OS) in patients who received T-DM1, T-DM1 plus pertuzumab, or trastuzumab plus a taxane (HT). All three regimens resulted in a median OS exceeding 50 months.
The incidence of grade 3 or higher adverse events (AEs) was highest in patients who received HT.
Edith A. Perez, MD, of Mayo Clinic Cancer Center in Jacksonville, Fla., and colleagues reported these results in Cancer.
The MARIANNE trial (NCT01120184) enrolled 1,095 adults with HER2-positive, advanced breast cancer. They were randomized to receive HT, T-DM1, or T-DM1 plus pertuzumab. Patients in the HT arm received trastuzumab plus paclitaxel or docetaxel according to the investigator’s discretion.
In all, 352 patients received HT (257 on docetaxel and 96 on paclitaxel), 361 patients received T-DM1 plus placebo, and 366 received T-DM1 plus pertuzumab.
Response and OS
In the primary analysis, the median OS was not reached in any treatment arm at a median follow-up of 35 months. The rate of objective response was 67.9% in the HT arm, 64.2% in the T-DM1 plus pertuzumab arm, and 59.7% in the T-DM1 arm. The median duration of response was 12.5 months, 21.2 months, and 20.7 months, respectively.
For the final OS analysis, the median duration of follow-up was 54 months. Roughly 70% of patients in each arm had received at least one treatment regimen during follow-up.
The final median OS was similar across the treatment arms – 50.9 months in the HT arm, 53.7 months in the T-DM1 arm, and 51.8 months in the T-DM1 plus pertuzumab arm. With the HT arm as a reference, the stratified hazard ratio was 0.93 for the T-DM1 arm and 0.86 for the T-DM1 plus pertuzumab arm.
OS results were consistent across subgroups. Although there were some differences in hazard ratios, “none of the examined subgroups showed a clear benefit with one treatment regimen in comparison with the others,” the researchers wrote.
The researchers also analyzed OS by response status at 6.5 months after randomization. Among nonresponders, the median OS was 41.9 months in the T-DM1 plus pertuzumab arm, 45.7 months in the T-DM1 arm, and 48.1 months in the HT arm. Among responders, the median OS was not reached in the T-DM1 plus pertuzumab arm, 64.4 months, and 56.3 months, respectively.
There were no baseline characteristics or biomarkers that were strongly associated with response by treatment group. However, in the HT and T-DM1 arms, patients with above-median HER2 messenger RNA expression were more likely to respond.
Safety
Rates of grade 3 or higher AEs were 55.8% in the HT arm, 47.1% in the T-DM1 arm, and 48.6% in the T-DM1 plus pertuzumab arm. The most common grade 3 or higher AEs were as follows:
- HT arm – neutropenia (19.3%), febrile neutropenia (6.5%), and diarrhea (4.2%).
- T-DM1 arm – increased aspartate aminotransferase (6.9%), thrombocytopenia (6.6%), and anemia (5.0%).
- T-DM1 plus pertuzumab arm – thrombocytopenia (9.0%), anemia (7.1%), and increased alanine aminotransferase (6.0%).
Rates of AE-related treatment discontinuation were 20.8% in the T-DM1 arm, 23.0% in the T-DM1 plus pertuzumab arm, and 30.6% in the HT arm. Rates of AE-related death were 1.4%, 1.9%, and 2.0%, respectively.
This study was funded by F. Hoffmann–La Roche. Dr. Perez was previously employed by Genentech/Roche. Her fellow authors disclosed relationships with Roche and many other companies.
SOURCE: Perez EA et al. Cancer. 2019 Jul 18. doi: 10.1002/cncr.32392.
Trastuzumab emtansine (T-DM1) is a suitable first-line therapy for patients with HER2-positive, advanced breast cancer who cannot receive taxane-based therapy, according to researchers.
Final results from the phase 3 MARIANNE trial revealed similar overall survival (OS) in patients who received T-DM1, T-DM1 plus pertuzumab, or trastuzumab plus a taxane (HT). All three regimens resulted in a median OS exceeding 50 months.
The incidence of grade 3 or higher adverse events (AEs) was highest in patients who received HT.
Edith A. Perez, MD, of Mayo Clinic Cancer Center in Jacksonville, Fla., and colleagues reported these results in Cancer.
The MARIANNE trial (NCT01120184) enrolled 1,095 adults with HER2-positive, advanced breast cancer. They were randomized to receive HT, T-DM1, or T-DM1 plus pertuzumab. Patients in the HT arm received trastuzumab plus paclitaxel or docetaxel according to the investigator’s discretion.
In all, 352 patients received HT (257 on docetaxel and 96 on paclitaxel), 361 patients received T-DM1 plus placebo, and 366 received T-DM1 plus pertuzumab.
Response and OS
In the primary analysis, the median OS was not reached in any treatment arm at a median follow-up of 35 months. The rate of objective response was 67.9% in the HT arm, 64.2% in the T-DM1 plus pertuzumab arm, and 59.7% in the T-DM1 arm. The median duration of response was 12.5 months, 21.2 months, and 20.7 months, respectively.
For the final OS analysis, the median duration of follow-up was 54 months. Roughly 70% of patients in each arm had received at least one treatment regimen during follow-up.
The final median OS was similar across the treatment arms – 50.9 months in the HT arm, 53.7 months in the T-DM1 arm, and 51.8 months in the T-DM1 plus pertuzumab arm. With the HT arm as a reference, the stratified hazard ratio was 0.93 for the T-DM1 arm and 0.86 for the T-DM1 plus pertuzumab arm.
OS results were consistent across subgroups. Although there were some differences in hazard ratios, “none of the examined subgroups showed a clear benefit with one treatment regimen in comparison with the others,” the researchers wrote.
The researchers also analyzed OS by response status at 6.5 months after randomization. Among nonresponders, the median OS was 41.9 months in the T-DM1 plus pertuzumab arm, 45.7 months in the T-DM1 arm, and 48.1 months in the HT arm. Among responders, the median OS was not reached in the T-DM1 plus pertuzumab arm, 64.4 months, and 56.3 months, respectively.
There were no baseline characteristics or biomarkers that were strongly associated with response by treatment group. However, in the HT and T-DM1 arms, patients with above-median HER2 messenger RNA expression were more likely to respond.
Safety
Rates of grade 3 or higher AEs were 55.8% in the HT arm, 47.1% in the T-DM1 arm, and 48.6% in the T-DM1 plus pertuzumab arm. The most common grade 3 or higher AEs were as follows:
- HT arm – neutropenia (19.3%), febrile neutropenia (6.5%), and diarrhea (4.2%).
- T-DM1 arm – increased aspartate aminotransferase (6.9%), thrombocytopenia (6.6%), and anemia (5.0%).
- T-DM1 plus pertuzumab arm – thrombocytopenia (9.0%), anemia (7.1%), and increased alanine aminotransferase (6.0%).
Rates of AE-related treatment discontinuation were 20.8% in the T-DM1 arm, 23.0% in the T-DM1 plus pertuzumab arm, and 30.6% in the HT arm. Rates of AE-related death were 1.4%, 1.9%, and 2.0%, respectively.
This study was funded by F. Hoffmann–La Roche. Dr. Perez was previously employed by Genentech/Roche. Her fellow authors disclosed relationships with Roche and many other companies.
SOURCE: Perez EA et al. Cancer. 2019 Jul 18. doi: 10.1002/cncr.32392.
FROM CANCER
Antiretroviral-eluting implant could provide HIV prophylaxis for a year or more
An implant that elutes an investigational antiretroviral agent provided drug release that should be sufficient for HIV prophylaxis for 12 months or more, according to results of a phase 1 clinical trial just presented here at the International AIDS Society Conference on HIV Science.
The islatravir-eluting arm implant was safe and generally well tolerated, with drug concentrations that remained above the target level needed for protection throughout the randomized, placebo-controlled study, said investigator Randolph P. Matthews, MD, PhD, senior principal scientist at Merck, Kenilworth, N.J.
“Based on this study, the islatravir-eluting implant appears to be a potentially important option for preexposure prophylaxis (PrEP) as an agent that could be effective with yearly dosing,” Dr. Matthews said in an IAS press conference.
This drug-eluting implant, inserted subdermally in the skin of the upper arm, could represent a “meaningful option” for many individuals at high risk of HIV infection, particularly those who have adherence challenges, said Dr. Matthews.
“Many at-risk individuals face adherence challenges with the existing daily oral PrEP therapy,” he added. “A high degree of adherence is required for it to be effective, and daily adherence is challenging for many, particularly for women.”
Islatravir, formerly known as MK-8591, is a nucleoside reverse transcriptase translocation inhibitor (NRTTI) being evaluated in clinical trials not only for PrEP, but also for treatment of HIV-1 infection in combination with other antiretrovirals.
In preclinical trials, islatravir demonstrated high potency, a high barrier to resistance, and a long half-life, according to Dr. Matthews.
The phase 1, single-site, double-blind study included a total of 16 healthy adult volunteers who received implants of islatravir at one of two doses (54 mg and 62 mg) or placebo for 12 weeks.
Both active doses of islatravir led to concentrations above the target level at 12 weeks, and based on data modeling, the higher-dose implant would still be above the target level for at least a year, Dr. Matthews said in the press conference.
The projected duration above the target ranged from 12 to 16 months for the 62-mg dose of islatravir, and from 8 to 10 months for the 54-mg dose, according to the reported data.
All drug-related adverse events were mild or moderate in severity, and none of the volunteers discontinued the study because of an adverse event, Dr. Matthews said.
Taken together, these data support the continued progression of the implant clinical development program, said Dr. Matthews, who is an employee of Merck, which sponsored the study.
SOURCE: Matthews RP et al. IAS 2019, Abstract TUAC0401LB.
An implant that elutes an investigational antiretroviral agent provided drug release that should be sufficient for HIV prophylaxis for 12 months or more, according to results of a phase 1 clinical trial just presented here at the International AIDS Society Conference on HIV Science.
The islatravir-eluting arm implant was safe and generally well tolerated, with drug concentrations that remained above the target level needed for protection throughout the randomized, placebo-controlled study, said investigator Randolph P. Matthews, MD, PhD, senior principal scientist at Merck, Kenilworth, N.J.
“Based on this study, the islatravir-eluting implant appears to be a potentially important option for preexposure prophylaxis (PrEP) as an agent that could be effective with yearly dosing,” Dr. Matthews said in an IAS press conference.
This drug-eluting implant, inserted subdermally in the skin of the upper arm, could represent a “meaningful option” for many individuals at high risk of HIV infection, particularly those who have adherence challenges, said Dr. Matthews.
“Many at-risk individuals face adherence challenges with the existing daily oral PrEP therapy,” he added. “A high degree of adherence is required for it to be effective, and daily adherence is challenging for many, particularly for women.”
Islatravir, formerly known as MK-8591, is a nucleoside reverse transcriptase translocation inhibitor (NRTTI) being evaluated in clinical trials not only for PrEP, but also for treatment of HIV-1 infection in combination with other antiretrovirals.
In preclinical trials, islatravir demonstrated high potency, a high barrier to resistance, and a long half-life, according to Dr. Matthews.
The phase 1, single-site, double-blind study included a total of 16 healthy adult volunteers who received implants of islatravir at one of two doses (54 mg and 62 mg) or placebo for 12 weeks.
Both active doses of islatravir led to concentrations above the target level at 12 weeks, and based on data modeling, the higher-dose implant would still be above the target level for at least a year, Dr. Matthews said in the press conference.
The projected duration above the target ranged from 12 to 16 months for the 62-mg dose of islatravir, and from 8 to 10 months for the 54-mg dose, according to the reported data.
All drug-related adverse events were mild or moderate in severity, and none of the volunteers discontinued the study because of an adverse event, Dr. Matthews said.
Taken together, these data support the continued progression of the implant clinical development program, said Dr. Matthews, who is an employee of Merck, which sponsored the study.
SOURCE: Matthews RP et al. IAS 2019, Abstract TUAC0401LB.
An implant that elutes an investigational antiretroviral agent provided drug release that should be sufficient for HIV prophylaxis for 12 months or more, according to results of a phase 1 clinical trial just presented here at the International AIDS Society Conference on HIV Science.
The islatravir-eluting arm implant was safe and generally well tolerated, with drug concentrations that remained above the target level needed for protection throughout the randomized, placebo-controlled study, said investigator Randolph P. Matthews, MD, PhD, senior principal scientist at Merck, Kenilworth, N.J.
“Based on this study, the islatravir-eluting implant appears to be a potentially important option for preexposure prophylaxis (PrEP) as an agent that could be effective with yearly dosing,” Dr. Matthews said in an IAS press conference.
This drug-eluting implant, inserted subdermally in the skin of the upper arm, could represent a “meaningful option” for many individuals at high risk of HIV infection, particularly those who have adherence challenges, said Dr. Matthews.
“Many at-risk individuals face adherence challenges with the existing daily oral PrEP therapy,” he added. “A high degree of adherence is required for it to be effective, and daily adherence is challenging for many, particularly for women.”
Islatravir, formerly known as MK-8591, is a nucleoside reverse transcriptase translocation inhibitor (NRTTI) being evaluated in clinical trials not only for PrEP, but also for treatment of HIV-1 infection in combination with other antiretrovirals.
In preclinical trials, islatravir demonstrated high potency, a high barrier to resistance, and a long half-life, according to Dr. Matthews.
The phase 1, single-site, double-blind study included a total of 16 healthy adult volunteers who received implants of islatravir at one of two doses (54 mg and 62 mg) or placebo for 12 weeks.
Both active doses of islatravir led to concentrations above the target level at 12 weeks, and based on data modeling, the higher-dose implant would still be above the target level for at least a year, Dr. Matthews said in the press conference.
The projected duration above the target ranged from 12 to 16 months for the 62-mg dose of islatravir, and from 8 to 10 months for the 54-mg dose, according to the reported data.
All drug-related adverse events were mild or moderate in severity, and none of the volunteers discontinued the study because of an adverse event, Dr. Matthews said.
Taken together, these data support the continued progression of the implant clinical development program, said Dr. Matthews, who is an employee of Merck, which sponsored the study.
SOURCE: Matthews RP et al. IAS 2019, Abstract TUAC0401LB.
FROM IAS 2019
Efficacy of DOACs vs. warfarin in high-risk atrial fibrillation patients
Background: DOACs have been shown to be efficacious in randomized, controlled trials, but these trials did not include high-risk patients. This trial studies the efficacy and safety of DOACs in elderly patients with new-onset atrial fibrillation who are at high risk of both ischemic stroke and major bleeding.
Study design: Retrospective comparative effectiveness analysis.
Setting: Data from a population-based Medicare beneficiaries database.
Synopsis: Data from 213,705 Medicare beneficiaries with new-onset atrial fibrillation on rivaroxaban, dabigatran, or warfarin were analyzed. The investigators calculated CHA2DS2-VASc, HAS-BLED, and Gagne Index comorbidity scores for each participant to assess comorbidity burden and categorize patients into low-, medium-, and high-morbidity categories.
Researchers then used three-way propensity matching, accounting for each morbidity category and anticoagulation medication to compare outcomes. Cox proportion regression models were used to adjust for risk and compare outcomes of ischemic stroke and major hemorrhage in matched participants in each anticoagulant group.
Primary outcomes of the study were ischemic stroke and major hemorrhage, which were determined based on ICD-9 codes. The investigators did not find a significant difference among anticoagulants regardless of the morbidity level for risk-adjusted ischemic stroke rates. Participants in the dabigatran group had lower rates of risk-adjusted major hemorrhage, compared with the warfarin group, regardless of morbidity category. The dabigatran group also had lower major hemorrhage risk, compared with the rivaroxaban group, especially in moderate- and high-morbidity category. Lastly, risk-adjusted rates of mortality were lower in the dabigatran and rivaroxaban groups, compared with the warfarin group, and there was no difference between the dabigatran and rivaroxaban groups with regards to mortality.
Bottom line: Rivaroxaban and dabigatran are each equally effective, compared with warfarin, in preventing ischemic strokes in elderly patients with new-onset atrial fibrillation and multiple comorbidities. However, patients on dabigatran appear to be at less risk of major bleeding, compared with warfarin and rivaroxaban.
Citation: Mentias A et al. Assessment of outcomes of treatment with oral anticoagulants in patients with atrial fibrillation and multiple chronic conditions. JAMA Netw Open. 2018 Sep 28;1(5):e182870.
Dr. Puri is assistant professor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
Background: DOACs have been shown to be efficacious in randomized, controlled trials, but these trials did not include high-risk patients. This trial studies the efficacy and safety of DOACs in elderly patients with new-onset atrial fibrillation who are at high risk of both ischemic stroke and major bleeding.
Study design: Retrospective comparative effectiveness analysis.
Setting: Data from a population-based Medicare beneficiaries database.
Synopsis: Data from 213,705 Medicare beneficiaries with new-onset atrial fibrillation on rivaroxaban, dabigatran, or warfarin were analyzed. The investigators calculated CHA2DS2-VASc, HAS-BLED, and Gagne Index comorbidity scores for each participant to assess comorbidity burden and categorize patients into low-, medium-, and high-morbidity categories.
Researchers then used three-way propensity matching, accounting for each morbidity category and anticoagulation medication to compare outcomes. Cox proportion regression models were used to adjust for risk and compare outcomes of ischemic stroke and major hemorrhage in matched participants in each anticoagulant group.
Primary outcomes of the study were ischemic stroke and major hemorrhage, which were determined based on ICD-9 codes. The investigators did not find a significant difference among anticoagulants regardless of the morbidity level for risk-adjusted ischemic stroke rates. Participants in the dabigatran group had lower rates of risk-adjusted major hemorrhage, compared with the warfarin group, regardless of morbidity category. The dabigatran group also had lower major hemorrhage risk, compared with the rivaroxaban group, especially in moderate- and high-morbidity category. Lastly, risk-adjusted rates of mortality were lower in the dabigatran and rivaroxaban groups, compared with the warfarin group, and there was no difference between the dabigatran and rivaroxaban groups with regards to mortality.
Bottom line: Rivaroxaban and dabigatran are each equally effective, compared with warfarin, in preventing ischemic strokes in elderly patients with new-onset atrial fibrillation and multiple comorbidities. However, patients on dabigatran appear to be at less risk of major bleeding, compared with warfarin and rivaroxaban.
Citation: Mentias A et al. Assessment of outcomes of treatment with oral anticoagulants in patients with atrial fibrillation and multiple chronic conditions. JAMA Netw Open. 2018 Sep 28;1(5):e182870.
Dr. Puri is assistant professor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
Background: DOACs have been shown to be efficacious in randomized, controlled trials, but these trials did not include high-risk patients. This trial studies the efficacy and safety of DOACs in elderly patients with new-onset atrial fibrillation who are at high risk of both ischemic stroke and major bleeding.
Study design: Retrospective comparative effectiveness analysis.
Setting: Data from a population-based Medicare beneficiaries database.
Synopsis: Data from 213,705 Medicare beneficiaries with new-onset atrial fibrillation on rivaroxaban, dabigatran, or warfarin were analyzed. The investigators calculated CHA2DS2-VASc, HAS-BLED, and Gagne Index comorbidity scores for each participant to assess comorbidity burden and categorize patients into low-, medium-, and high-morbidity categories.
Researchers then used three-way propensity matching, accounting for each morbidity category and anticoagulation medication to compare outcomes. Cox proportion regression models were used to adjust for risk and compare outcomes of ischemic stroke and major hemorrhage in matched participants in each anticoagulant group.
Primary outcomes of the study were ischemic stroke and major hemorrhage, which were determined based on ICD-9 codes. The investigators did not find a significant difference among anticoagulants regardless of the morbidity level for risk-adjusted ischemic stroke rates. Participants in the dabigatran group had lower rates of risk-adjusted major hemorrhage, compared with the warfarin group, regardless of morbidity category. The dabigatran group also had lower major hemorrhage risk, compared with the rivaroxaban group, especially in moderate- and high-morbidity category. Lastly, risk-adjusted rates of mortality were lower in the dabigatran and rivaroxaban groups, compared with the warfarin group, and there was no difference between the dabigatran and rivaroxaban groups with regards to mortality.
Bottom line: Rivaroxaban and dabigatran are each equally effective, compared with warfarin, in preventing ischemic strokes in elderly patients with new-onset atrial fibrillation and multiple comorbidities. However, patients on dabigatran appear to be at less risk of major bleeding, compared with warfarin and rivaroxaban.
Citation: Mentias A et al. Assessment of outcomes of treatment with oral anticoagulants in patients with atrial fibrillation and multiple chronic conditions. JAMA Netw Open. 2018 Sep 28;1(5):e182870.
Dr. Puri is assistant professor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
FDA approves Baqsimi nasal powder for emergency hypoglycemia treatment
in patients aged 4 years and older.
Injectable glucagon has been approved in the United States for several decades.
The safety and efficacy of the Baqsimi powder was assessed in two studies with adults with diabetes and one with pediatric patients. In all three studies, a single dose of Baqsimi was compared with a single dose of glucagon injection, and Baqsimi adequately raised blood sugar levels in response to insulin-induced hypoglycemia.
The most common adverse events associated with Baqsimi include nausea, vomiting, headache, upper respiratory tract irritation, watery eyes, redness of eyes, and itchiness. The safety profile is similar to that of injectable glucagon, with the addition of nasal- and eye-related symptoms because of the method of delivery.
“There are many products on the market for those who need insulin, but until now, people suffering from a severe hypoglycemic episode had to be treated with a glucagon injection that first had to be mixed in a several-step process. This new way to administer glucagon may simplify the process, which can be critical during an episode, especially since the patient may have lost consciousness or may be having a seizure. In those situations, we want the process to treat the suffering person to be as simple as possible,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.
in patients aged 4 years and older.
Injectable glucagon has been approved in the United States for several decades.
The safety and efficacy of the Baqsimi powder was assessed in two studies with adults with diabetes and one with pediatric patients. In all three studies, a single dose of Baqsimi was compared with a single dose of glucagon injection, and Baqsimi adequately raised blood sugar levels in response to insulin-induced hypoglycemia.
The most common adverse events associated with Baqsimi include nausea, vomiting, headache, upper respiratory tract irritation, watery eyes, redness of eyes, and itchiness. The safety profile is similar to that of injectable glucagon, with the addition of nasal- and eye-related symptoms because of the method of delivery.
“There are many products on the market for those who need insulin, but until now, people suffering from a severe hypoglycemic episode had to be treated with a glucagon injection that first had to be mixed in a several-step process. This new way to administer glucagon may simplify the process, which can be critical during an episode, especially since the patient may have lost consciousness or may be having a seizure. In those situations, we want the process to treat the suffering person to be as simple as possible,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.
in patients aged 4 years and older.
Injectable glucagon has been approved in the United States for several decades.
The safety and efficacy of the Baqsimi powder was assessed in two studies with adults with diabetes and one with pediatric patients. In all three studies, a single dose of Baqsimi was compared with a single dose of glucagon injection, and Baqsimi adequately raised blood sugar levels in response to insulin-induced hypoglycemia.
The most common adverse events associated with Baqsimi include nausea, vomiting, headache, upper respiratory tract irritation, watery eyes, redness of eyes, and itchiness. The safety profile is similar to that of injectable glucagon, with the addition of nasal- and eye-related symptoms because of the method of delivery.
“There are many products on the market for those who need insulin, but until now, people suffering from a severe hypoglycemic episode had to be treated with a glucagon injection that first had to be mixed in a several-step process. This new way to administer glucagon may simplify the process, which can be critical during an episode, especially since the patient may have lost consciousness or may be having a seizure. In those situations, we want the process to treat the suffering person to be as simple as possible,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.
Meeting just 2 of 7 ‘simple’ goals lowers HF risk
Turns out the American Heart Association is onto something when it urges people to embrace its “Life’s Simple 7” (LS7) recommendations, a series of strategies designed to boost cardiovascular health. A new European study finds that people who follow the recommendations were more than half as likely to develop heart failure (HF) and that mastering just two of the seven criteria makes a big difference, compared with mastering none at all.
“Focusing on particular components of the American Heart Association LS7 could be seen as a way to improve cardiovascular health,” wrote the authors of the study, which appears in JACC: Heart Failure.
The LS7 encourages the following strategies:
- Manage blood pressure.
- Control cholesterol.
- Reduce blood sugar.
- Get active.
- Eat better.
- Lose weight.
- Stop smoking.
For the new study, researchers led by Alicia Uijl, MSc, of University College London and University Medical Center Utrecht (the Netherlands) retrospectively tracked 37,803 participants in a prospective Dutch study of cancer and nutrition.
The subjects, 75% women, had a mean age of 49 years. The group was much thinner, with a mean body mass index of 25 kg/m2, than typical American men and women, whose mean BMIs are 29 and 30, per CDC statistics (Natl Health Stat Report. 2018 Dec;122:1-16)
Researchers gave the subjects an LS7 score (0-14) at baseline from 1993-1997. The score was based on whether they fully (2 points), partially (1) or not at all (0) met each of the LC7 criteria.
Most of the subjects failed to reach the ideal level of healthiness, which was defined as scores 11-14 and was achieved by 23%. The others were in the intermediate group (scores, 9-10 points; 35%) and inadequate group (scores, 0-8; 42%).
Over a median follow-up of 15 years, 2% of participants (690) developed HF. In an adjusted model, subjects in the top two groups (ideal and intermediate) were less likely to develop HF than were those in the lowest group (hazard ratios, 0.45 and 0.53, respectively).
The researchers found that diet, exercise, and cholesterol had lesser impacts on risk of HF than did the other elements. And they discovered that meeting the ideal level for just 2 of the 7 strategies would lower HF risk by 52%, compared with reaching no ideal levels.
What now? The high number of subjects in the lowest category suggests “there is ample room for improvements in healthy lifestyle behavior that may reduce HF in the general population,” the researchers wrote. “Given the robust associations between a healthy lifestyle and reduced incidence of HF, this study provides evidence that prevention of incident HF could be accomplished by implementing healthy lifestyle patterns.”
The study is funded by the European Commission, European Union/European Federation of Pharmaceutical Industries and Associations, and several other research organizations. The study authors reported no relevant disclosures.
SOURCE: Uijl A et al. JACC: Heart Fail. 2019 Jul 10. doi: 10.1016/j.jchf.2019.03.009
Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, of Baylor College of Medicine, Houston, made these comments in an accompanying editorial. Dr. Ballantyne discloses grant/research support/consulting for Abbott and Roche and a provisional patent. Dr. Nambi discloses research site primary investigator work for Merck and a provisional patent.
Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, of Baylor College of Medicine, Houston, made these comments in an accompanying editorial. Dr. Ballantyne discloses grant/research support/consulting for Abbott and Roche and a provisional patent. Dr. Nambi discloses research site primary investigator work for Merck and a provisional patent.
Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, of Baylor College of Medicine, Houston, made these comments in an accompanying editorial. Dr. Ballantyne discloses grant/research support/consulting for Abbott and Roche and a provisional patent. Dr. Nambi discloses research site primary investigator work for Merck and a provisional patent.
Turns out the American Heart Association is onto something when it urges people to embrace its “Life’s Simple 7” (LS7) recommendations, a series of strategies designed to boost cardiovascular health. A new European study finds that people who follow the recommendations were more than half as likely to develop heart failure (HF) and that mastering just two of the seven criteria makes a big difference, compared with mastering none at all.
“Focusing on particular components of the American Heart Association LS7 could be seen as a way to improve cardiovascular health,” wrote the authors of the study, which appears in JACC: Heart Failure.
The LS7 encourages the following strategies:
- Manage blood pressure.
- Control cholesterol.
- Reduce blood sugar.
- Get active.
- Eat better.
- Lose weight.
- Stop smoking.
For the new study, researchers led by Alicia Uijl, MSc, of University College London and University Medical Center Utrecht (the Netherlands) retrospectively tracked 37,803 participants in a prospective Dutch study of cancer and nutrition.
The subjects, 75% women, had a mean age of 49 years. The group was much thinner, with a mean body mass index of 25 kg/m2, than typical American men and women, whose mean BMIs are 29 and 30, per CDC statistics (Natl Health Stat Report. 2018 Dec;122:1-16)
Researchers gave the subjects an LS7 score (0-14) at baseline from 1993-1997. The score was based on whether they fully (2 points), partially (1) or not at all (0) met each of the LC7 criteria.
Most of the subjects failed to reach the ideal level of healthiness, which was defined as scores 11-14 and was achieved by 23%. The others were in the intermediate group (scores, 9-10 points; 35%) and inadequate group (scores, 0-8; 42%).
Over a median follow-up of 15 years, 2% of participants (690) developed HF. In an adjusted model, subjects in the top two groups (ideal and intermediate) were less likely to develop HF than were those in the lowest group (hazard ratios, 0.45 and 0.53, respectively).
The researchers found that diet, exercise, and cholesterol had lesser impacts on risk of HF than did the other elements. And they discovered that meeting the ideal level for just 2 of the 7 strategies would lower HF risk by 52%, compared with reaching no ideal levels.
What now? The high number of subjects in the lowest category suggests “there is ample room for improvements in healthy lifestyle behavior that may reduce HF in the general population,” the researchers wrote. “Given the robust associations between a healthy lifestyle and reduced incidence of HF, this study provides evidence that prevention of incident HF could be accomplished by implementing healthy lifestyle patterns.”
The study is funded by the European Commission, European Union/European Federation of Pharmaceutical Industries and Associations, and several other research organizations. The study authors reported no relevant disclosures.
SOURCE: Uijl A et al. JACC: Heart Fail. 2019 Jul 10. doi: 10.1016/j.jchf.2019.03.009
Turns out the American Heart Association is onto something when it urges people to embrace its “Life’s Simple 7” (LS7) recommendations, a series of strategies designed to boost cardiovascular health. A new European study finds that people who follow the recommendations were more than half as likely to develop heart failure (HF) and that mastering just two of the seven criteria makes a big difference, compared with mastering none at all.
“Focusing on particular components of the American Heart Association LS7 could be seen as a way to improve cardiovascular health,” wrote the authors of the study, which appears in JACC: Heart Failure.
The LS7 encourages the following strategies:
- Manage blood pressure.
- Control cholesterol.
- Reduce blood sugar.
- Get active.
- Eat better.
- Lose weight.
- Stop smoking.
For the new study, researchers led by Alicia Uijl, MSc, of University College London and University Medical Center Utrecht (the Netherlands) retrospectively tracked 37,803 participants in a prospective Dutch study of cancer and nutrition.
The subjects, 75% women, had a mean age of 49 years. The group was much thinner, with a mean body mass index of 25 kg/m2, than typical American men and women, whose mean BMIs are 29 and 30, per CDC statistics (Natl Health Stat Report. 2018 Dec;122:1-16)
Researchers gave the subjects an LS7 score (0-14) at baseline from 1993-1997. The score was based on whether they fully (2 points), partially (1) or not at all (0) met each of the LC7 criteria.
Most of the subjects failed to reach the ideal level of healthiness, which was defined as scores 11-14 and was achieved by 23%. The others were in the intermediate group (scores, 9-10 points; 35%) and inadequate group (scores, 0-8; 42%).
Over a median follow-up of 15 years, 2% of participants (690) developed HF. In an adjusted model, subjects in the top two groups (ideal and intermediate) were less likely to develop HF than were those in the lowest group (hazard ratios, 0.45 and 0.53, respectively).
The researchers found that diet, exercise, and cholesterol had lesser impacts on risk of HF than did the other elements. And they discovered that meeting the ideal level for just 2 of the 7 strategies would lower HF risk by 52%, compared with reaching no ideal levels.
What now? The high number of subjects in the lowest category suggests “there is ample room for improvements in healthy lifestyle behavior that may reduce HF in the general population,” the researchers wrote. “Given the robust associations between a healthy lifestyle and reduced incidence of HF, this study provides evidence that prevention of incident HF could be accomplished by implementing healthy lifestyle patterns.”
The study is funded by the European Commission, European Union/European Federation of Pharmaceutical Industries and Associations, and several other research organizations. The study authors reported no relevant disclosures.
SOURCE: Uijl A et al. JACC: Heart Fail. 2019 Jul 10. doi: 10.1016/j.jchf.2019.03.009
FROM JACC: HEART FAILURE
Postpartum care: State scorecard for Medicaid enrollees
Timely postpartum care for Medicaid enrollees varies considerably, ranging from 17% to 74% among the states, according to the Centers for Medicare & Medicaid Services.
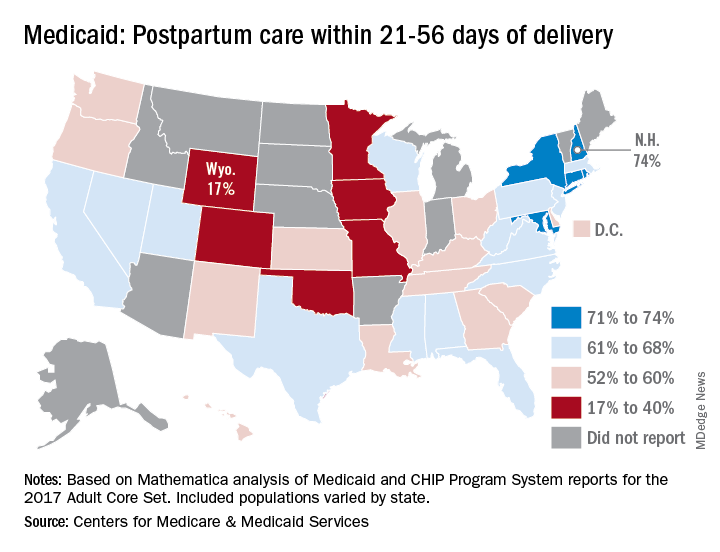
A national median of 60% of women saw a health care provider within 21-56 days of their delivery, CMS reported in its Medicaid and Children’s Health Insurance Program Scorecard.
“Medicaid is the largest payer for maternity care in the United States. The program has an important role to play in improving maternal and perinatal health outcomes,” the CMS noted.
New Hampshire’s rate of 74% was the highest of any state, just edging out Maryland and Rhode Island, each at 73%. The only other states over 70% were Connecticut and New York, which both reported rates of 71%, scorecard data show.
In Wyoming, the state with the lowest rate, 17% of Medicaid enrollees received timely postpartum care. The other four states with rates below 40% were Oklahoma (22%), Colorado (35%), Iowa (37%), and Missouri (38%), the CMS said after a recent refresh of data in the scorecard.
“The included populations … can vary by state. For example, some states report data on certain populations such as those covered under managed care but not those covered under fee for service. This variation in data and calculation methods can affect measure performance and comparisons between states,” the CMS said.
The scorecard is based on Mathematica analysis of Medicaid and CHIP Program System reports for the 2017 Adult Core Set, and the measurement period was Nov. 6, 2015, to Nov. 5, 2016. Twelve states did not report data on postpartum care to the CMS.
“More and more states are voluntarily reporting their health outcomes in the scorecard, and the new data is leading us into an era of increased transparency and accountability, so that together we can improve the quality of care we give to the vulnerable Americans that depend on this vital program,” CMS Administrator Seema Verma said in a written statement.
Timely postpartum care for Medicaid enrollees varies considerably, ranging from 17% to 74% among the states, according to the Centers for Medicare & Medicaid Services.
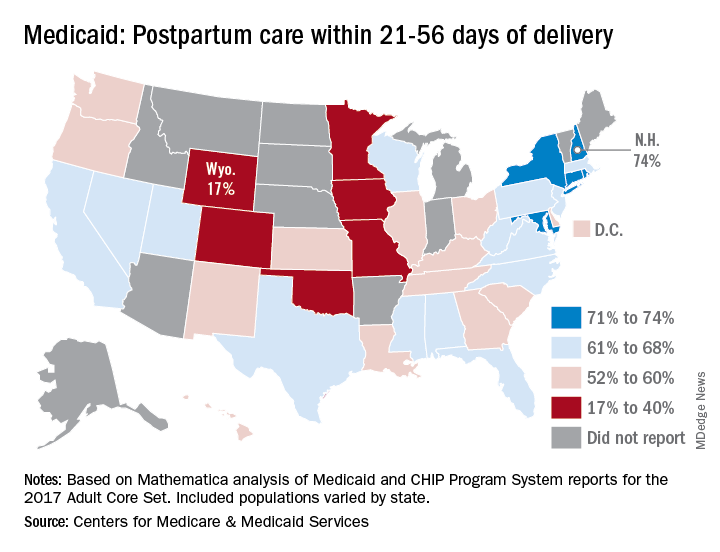
A national median of 60% of women saw a health care provider within 21-56 days of their delivery, CMS reported in its Medicaid and Children’s Health Insurance Program Scorecard.
“Medicaid is the largest payer for maternity care in the United States. The program has an important role to play in improving maternal and perinatal health outcomes,” the CMS noted.
New Hampshire’s rate of 74% was the highest of any state, just edging out Maryland and Rhode Island, each at 73%. The only other states over 70% were Connecticut and New York, which both reported rates of 71%, scorecard data show.
In Wyoming, the state with the lowest rate, 17% of Medicaid enrollees received timely postpartum care. The other four states with rates below 40% were Oklahoma (22%), Colorado (35%), Iowa (37%), and Missouri (38%), the CMS said after a recent refresh of data in the scorecard.
“The included populations … can vary by state. For example, some states report data on certain populations such as those covered under managed care but not those covered under fee for service. This variation in data and calculation methods can affect measure performance and comparisons between states,” the CMS said.
The scorecard is based on Mathematica analysis of Medicaid and CHIP Program System reports for the 2017 Adult Core Set, and the measurement period was Nov. 6, 2015, to Nov. 5, 2016. Twelve states did not report data on postpartum care to the CMS.
“More and more states are voluntarily reporting their health outcomes in the scorecard, and the new data is leading us into an era of increased transparency and accountability, so that together we can improve the quality of care we give to the vulnerable Americans that depend on this vital program,” CMS Administrator Seema Verma said in a written statement.
Timely postpartum care for Medicaid enrollees varies considerably, ranging from 17% to 74% among the states, according to the Centers for Medicare & Medicaid Services.
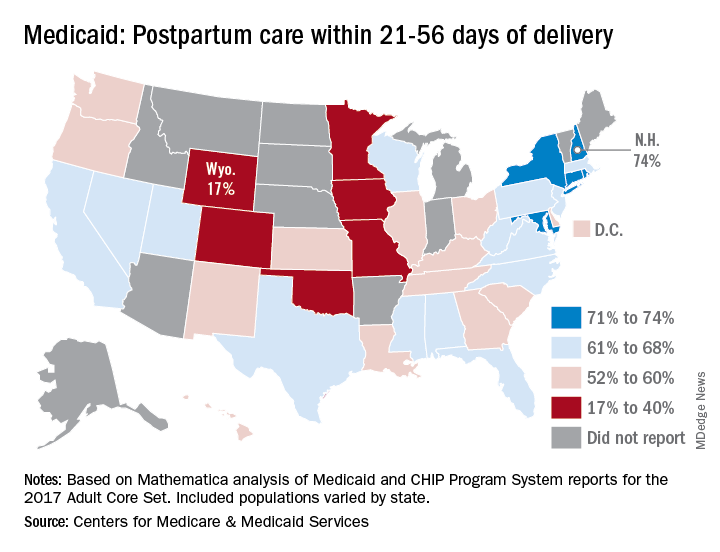
A national median of 60% of women saw a health care provider within 21-56 days of their delivery, CMS reported in its Medicaid and Children’s Health Insurance Program Scorecard.
“Medicaid is the largest payer for maternity care in the United States. The program has an important role to play in improving maternal and perinatal health outcomes,” the CMS noted.
New Hampshire’s rate of 74% was the highest of any state, just edging out Maryland and Rhode Island, each at 73%. The only other states over 70% were Connecticut and New York, which both reported rates of 71%, scorecard data show.
In Wyoming, the state with the lowest rate, 17% of Medicaid enrollees received timely postpartum care. The other four states with rates below 40% were Oklahoma (22%), Colorado (35%), Iowa (37%), and Missouri (38%), the CMS said after a recent refresh of data in the scorecard.
“The included populations … can vary by state. For example, some states report data on certain populations such as those covered under managed care but not those covered under fee for service. This variation in data and calculation methods can affect measure performance and comparisons between states,” the CMS said.
The scorecard is based on Mathematica analysis of Medicaid and CHIP Program System reports for the 2017 Adult Core Set, and the measurement period was Nov. 6, 2015, to Nov. 5, 2016. Twelve states did not report data on postpartum care to the CMS.
“More and more states are voluntarily reporting their health outcomes in the scorecard, and the new data is leading us into an era of increased transparency and accountability, so that together we can improve the quality of care we give to the vulnerable Americans that depend on this vital program,” CMS Administrator Seema Verma said in a written statement.
How common is accelerated knee OA?
TORONTO – Accelerated knee osteoarthritis – a particularly noxious form of the joint disease – occurred in more than one in seven women who developed knee osteoarthritis in the prospective, long-term Chingford Cohort Study, Jeffrey B. Driban, PhD, reported at the OARSI 2019 World Congress.
This finding from a unique prospective study of 1,003 middle-aged U.K. women who were followed for the development of knee osteoarthritis (OA) for 15 years is important because the participants represented a typical community-based population sample. And yet the Chingford results are consistent with and confirmatory of those found earlier in the Osteoarthritis Initiative, a U.S. cohort study of nearly 4,800 individuals, even though the Osteoarthritis Initiative featured a population enriched with established risk factors for knee OA, Dr. Driban explained at the meeting, sponsored by the Osteoarthritis Research Society International.
In Chingford, accelerated knee OA accounted for 15% of all incident cases of knee OA during follow-up, and for 17% of all newly affected knees, whereas 20% of incident knee OA in the Osteoarthritis Initiative was accelerated knee OA, noted Dr. Driban of Tufts University, Boston.
Accelerated knee OA is defined by rapidly progressive structural damage. Affected individuals streak from no radiographic evidence of knee OA to advanced-stage disease marked by a Kellgren-Lawrence score of 3 or more within 4 years, whereas the typical form of knee OA follows a more gradual course. Also, accelerated knee OA features greater pain and disability.
In the Chingford study, the cumulative incidence of accelerated knee OA was 3.9%, while typical knee OA occurred in 21.7% of women. During years 6-15 of follow-up, 21% of women with accelerated knee OA underwent total knee replacement, compared with 2% of those with typical knee OA and 0.9% of women without knee OA.
Dr. Driban reported having no financial conflicts regarding his analysis of the Chingford Cohort Study and the Osteoarthritis Initiative, supported by Arthritis Research UK and the National Institutes of Health, respectively.
SOURCE: Driban JB et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S250-S251, Abstract 352.
TORONTO – Accelerated knee osteoarthritis – a particularly noxious form of the joint disease – occurred in more than one in seven women who developed knee osteoarthritis in the prospective, long-term Chingford Cohort Study, Jeffrey B. Driban, PhD, reported at the OARSI 2019 World Congress.
This finding from a unique prospective study of 1,003 middle-aged U.K. women who were followed for the development of knee osteoarthritis (OA) for 15 years is important because the participants represented a typical community-based population sample. And yet the Chingford results are consistent with and confirmatory of those found earlier in the Osteoarthritis Initiative, a U.S. cohort study of nearly 4,800 individuals, even though the Osteoarthritis Initiative featured a population enriched with established risk factors for knee OA, Dr. Driban explained at the meeting, sponsored by the Osteoarthritis Research Society International.
In Chingford, accelerated knee OA accounted for 15% of all incident cases of knee OA during follow-up, and for 17% of all newly affected knees, whereas 20% of incident knee OA in the Osteoarthritis Initiative was accelerated knee OA, noted Dr. Driban of Tufts University, Boston.
Accelerated knee OA is defined by rapidly progressive structural damage. Affected individuals streak from no radiographic evidence of knee OA to advanced-stage disease marked by a Kellgren-Lawrence score of 3 or more within 4 years, whereas the typical form of knee OA follows a more gradual course. Also, accelerated knee OA features greater pain and disability.
In the Chingford study, the cumulative incidence of accelerated knee OA was 3.9%, while typical knee OA occurred in 21.7% of women. During years 6-15 of follow-up, 21% of women with accelerated knee OA underwent total knee replacement, compared with 2% of those with typical knee OA and 0.9% of women without knee OA.
Dr. Driban reported having no financial conflicts regarding his analysis of the Chingford Cohort Study and the Osteoarthritis Initiative, supported by Arthritis Research UK and the National Institutes of Health, respectively.
SOURCE: Driban JB et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S250-S251, Abstract 352.
TORONTO – Accelerated knee osteoarthritis – a particularly noxious form of the joint disease – occurred in more than one in seven women who developed knee osteoarthritis in the prospective, long-term Chingford Cohort Study, Jeffrey B. Driban, PhD, reported at the OARSI 2019 World Congress.
This finding from a unique prospective study of 1,003 middle-aged U.K. women who were followed for the development of knee osteoarthritis (OA) for 15 years is important because the participants represented a typical community-based population sample. And yet the Chingford results are consistent with and confirmatory of those found earlier in the Osteoarthritis Initiative, a U.S. cohort study of nearly 4,800 individuals, even though the Osteoarthritis Initiative featured a population enriched with established risk factors for knee OA, Dr. Driban explained at the meeting, sponsored by the Osteoarthritis Research Society International.
In Chingford, accelerated knee OA accounted for 15% of all incident cases of knee OA during follow-up, and for 17% of all newly affected knees, whereas 20% of incident knee OA in the Osteoarthritis Initiative was accelerated knee OA, noted Dr. Driban of Tufts University, Boston.
Accelerated knee OA is defined by rapidly progressive structural damage. Affected individuals streak from no radiographic evidence of knee OA to advanced-stage disease marked by a Kellgren-Lawrence score of 3 or more within 4 years, whereas the typical form of knee OA follows a more gradual course. Also, accelerated knee OA features greater pain and disability.
In the Chingford study, the cumulative incidence of accelerated knee OA was 3.9%, while typical knee OA occurred in 21.7% of women. During years 6-15 of follow-up, 21% of women with accelerated knee OA underwent total knee replacement, compared with 2% of those with typical knee OA and 0.9% of women without knee OA.
Dr. Driban reported having no financial conflicts regarding his analysis of the Chingford Cohort Study and the Osteoarthritis Initiative, supported by Arthritis Research UK and the National Institutes of Health, respectively.
SOURCE: Driban JB et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S250-S251, Abstract 352.
REPORTING FROM OARSI 2019