User login
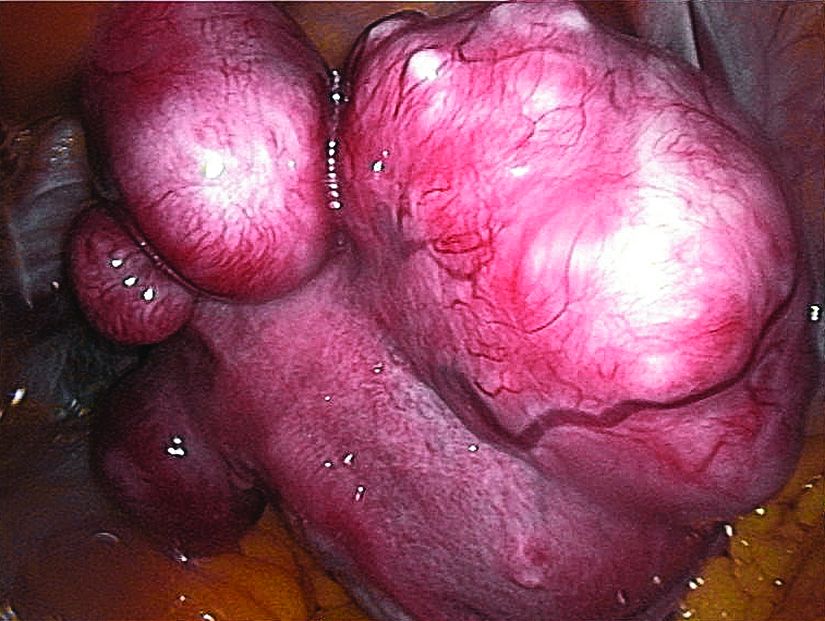
Ulipristal acetate tops placebo for uterine leiomyomas
according to a study of the intention-to-treat populations of the randomized, double-blind, phase III VENUS I and VENUS II trials.
In these pivotal studies, ulipristal (Ella) at either 5 mg or 10 mg significantly improved both rate of and time to amenorrhea, noted Andrea S. Lukes, MD, of Carolina Women’s Research and Wellness Center in Durham, N.C. To assess effects on quality of life, she and her associates analyzed baseline and 12-week responses to the widely validated Uterine Fibroid Symptom Health-Related Quality of Life (UFS-QOL) questionnaire, which examined factors such as symptom severity, energy and mood, physical and social activities, self-consciousness, and sexual functioning.
Among 589 patients in the analysis, 169 received placebo, 215 received 5 mg ulipristal, and 205 received 10 mg ulipristal. At baseline, average total quality of life scores on UFS-QOL were 33 (standard deviation, 220), 32 (SD, 21), and 36 (SD, 23), respectively, the researchers wrote in Obstetrics & Gynecology.
After 12 weeks of treatment, both doses of ulipristal were associated with significantly greater improvements on all UFS-QOL scales, compared with placebo (P less than .001). For example, on a scale of 0-100, symptom severity improved by a mean of 23 with ulipristal 5 mg and by a mean of 30 with ulipristal 10 mg (both P less than .001 versus placebo).
“Although a small proportion of patients experienced no change or some worsening in these outcomes, the majority of women reported clear improvements; for example, more than 70% of patients in the ulipristal treatment arms achieved a meaningful improvement of 30 or more points on the Revised Activities subscale,” the researchers wrote.
Additionally, significantly greater improvements in physical and social activities were seen for both ulipristal doses, compared with placebo, from baseline to the end of treatment.
The VENUS II trial included two 12-week treatment courses. In this trial, women who switched from ulipristal to placebo experienced some worsening in quality of life, while those who switched from placebo to ulipristal improved their UFS-QOL scores, the investigators said. Patients who stayed on ulipristal throughout continued to benefit from one treatment course to the next.
The researchers concluded that the findings, “taken together with the significant improvements in amenorrhea, suggest that ulipristal is a promising, noninvasive treatment option for women suffering from symptomatic uterine leiomyomas.”
Allergan provided funding. Dr. Lukes disclosed ties to Allergan, AbbVie, Myovant, Merck, and several other companies. Four of the coauthors are employees of Allergan, and the two remaining coauthors had links to a number of pharmaceutical companies.
SOURCE: Lukes AS et al. Obstet Gynecol 2019;133 (5):869-78.
In this study, 77%-87% of women who received ulipristal acetate reported more than a 20-point improvement in health-related quality of life, compared with only 36% of placebo recipients, Joanna L. Hatfield, MD, wrote in an accompanying editorial.
“However, women with leiomyomas report a 51-point mean improvement after hysterectomy,” she noted. “Clinicians need to keep this difference in mind when counseling women with leiomyomas.”
Ulipristal can cause fatigue and weight gain leading to treatment discontinuation, she noted. Very rare cases of liver failure also have been reported, and there is no evidence that liver enzyme screening identifies patients at risk.
Nonetheless, for the approximately half of women with symptomatic leiomyomas who desire uterine-sparing treatment, selective progesterone receptor modulators like ulipristal offer “a noninvasive way to manage bleeding and bulk symptoms,” Dr. Hatfield said.
She advocated for long-term safety studies and a large pregnancy registry, calling ulipristal “neither a panacea nor a Pandora’s box,” but a choice that “lies somewhere in the middle, just [like] nearly all options that present themselves in a woman’s life.”
Dr. Hatfield is director of the fibroid program at Oregon Health & Science University in Portland. She did not report having conflicts of interest. She wrote an editorial accompanying the article by AS Lukes et al. (Obstet Gynecol. 2019 May;133[5]:867-8).
In this study, 77%-87% of women who received ulipristal acetate reported more than a 20-point improvement in health-related quality of life, compared with only 36% of placebo recipients, Joanna L. Hatfield, MD, wrote in an accompanying editorial.
“However, women with leiomyomas report a 51-point mean improvement after hysterectomy,” she noted. “Clinicians need to keep this difference in mind when counseling women with leiomyomas.”
Ulipristal can cause fatigue and weight gain leading to treatment discontinuation, she noted. Very rare cases of liver failure also have been reported, and there is no evidence that liver enzyme screening identifies patients at risk.
Nonetheless, for the approximately half of women with symptomatic leiomyomas who desire uterine-sparing treatment, selective progesterone receptor modulators like ulipristal offer “a noninvasive way to manage bleeding and bulk symptoms,” Dr. Hatfield said.
She advocated for long-term safety studies and a large pregnancy registry, calling ulipristal “neither a panacea nor a Pandora’s box,” but a choice that “lies somewhere in the middle, just [like] nearly all options that present themselves in a woman’s life.”
Dr. Hatfield is director of the fibroid program at Oregon Health & Science University in Portland. She did not report having conflicts of interest. She wrote an editorial accompanying the article by AS Lukes et al. (Obstet Gynecol. 2019 May;133[5]:867-8).
In this study, 77%-87% of women who received ulipristal acetate reported more than a 20-point improvement in health-related quality of life, compared with only 36% of placebo recipients, Joanna L. Hatfield, MD, wrote in an accompanying editorial.
“However, women with leiomyomas report a 51-point mean improvement after hysterectomy,” she noted. “Clinicians need to keep this difference in mind when counseling women with leiomyomas.”
Ulipristal can cause fatigue and weight gain leading to treatment discontinuation, she noted. Very rare cases of liver failure also have been reported, and there is no evidence that liver enzyme screening identifies patients at risk.
Nonetheless, for the approximately half of women with symptomatic leiomyomas who desire uterine-sparing treatment, selective progesterone receptor modulators like ulipristal offer “a noninvasive way to manage bleeding and bulk symptoms,” Dr. Hatfield said.
She advocated for long-term safety studies and a large pregnancy registry, calling ulipristal “neither a panacea nor a Pandora’s box,” but a choice that “lies somewhere in the middle, just [like] nearly all options that present themselves in a woman’s life.”
Dr. Hatfield is director of the fibroid program at Oregon Health & Science University in Portland. She did not report having conflicts of interest. She wrote an editorial accompanying the article by AS Lukes et al. (Obstet Gynecol. 2019 May;133[5]:867-8).
according to a study of the intention-to-treat populations of the randomized, double-blind, phase III VENUS I and VENUS II trials.
In these pivotal studies, ulipristal (Ella) at either 5 mg or 10 mg significantly improved both rate of and time to amenorrhea, noted Andrea S. Lukes, MD, of Carolina Women’s Research and Wellness Center in Durham, N.C. To assess effects on quality of life, she and her associates analyzed baseline and 12-week responses to the widely validated Uterine Fibroid Symptom Health-Related Quality of Life (UFS-QOL) questionnaire, which examined factors such as symptom severity, energy and mood, physical and social activities, self-consciousness, and sexual functioning.
Among 589 patients in the analysis, 169 received placebo, 215 received 5 mg ulipristal, and 205 received 10 mg ulipristal. At baseline, average total quality of life scores on UFS-QOL were 33 (standard deviation, 220), 32 (SD, 21), and 36 (SD, 23), respectively, the researchers wrote in Obstetrics & Gynecology.
After 12 weeks of treatment, both doses of ulipristal were associated with significantly greater improvements on all UFS-QOL scales, compared with placebo (P less than .001). For example, on a scale of 0-100, symptom severity improved by a mean of 23 with ulipristal 5 mg and by a mean of 30 with ulipristal 10 mg (both P less than .001 versus placebo).
“Although a small proportion of patients experienced no change or some worsening in these outcomes, the majority of women reported clear improvements; for example, more than 70% of patients in the ulipristal treatment arms achieved a meaningful improvement of 30 or more points on the Revised Activities subscale,” the researchers wrote.
Additionally, significantly greater improvements in physical and social activities were seen for both ulipristal doses, compared with placebo, from baseline to the end of treatment.
The VENUS II trial included two 12-week treatment courses. In this trial, women who switched from ulipristal to placebo experienced some worsening in quality of life, while those who switched from placebo to ulipristal improved their UFS-QOL scores, the investigators said. Patients who stayed on ulipristal throughout continued to benefit from one treatment course to the next.
The researchers concluded that the findings, “taken together with the significant improvements in amenorrhea, suggest that ulipristal is a promising, noninvasive treatment option for women suffering from symptomatic uterine leiomyomas.”
Allergan provided funding. Dr. Lukes disclosed ties to Allergan, AbbVie, Myovant, Merck, and several other companies. Four of the coauthors are employees of Allergan, and the two remaining coauthors had links to a number of pharmaceutical companies.
SOURCE: Lukes AS et al. Obstet Gynecol 2019;133 (5):869-78.
according to a study of the intention-to-treat populations of the randomized, double-blind, phase III VENUS I and VENUS II trials.
In these pivotal studies, ulipristal (Ella) at either 5 mg or 10 mg significantly improved both rate of and time to amenorrhea, noted Andrea S. Lukes, MD, of Carolina Women’s Research and Wellness Center in Durham, N.C. To assess effects on quality of life, she and her associates analyzed baseline and 12-week responses to the widely validated Uterine Fibroid Symptom Health-Related Quality of Life (UFS-QOL) questionnaire, which examined factors such as symptom severity, energy and mood, physical and social activities, self-consciousness, and sexual functioning.
Among 589 patients in the analysis, 169 received placebo, 215 received 5 mg ulipristal, and 205 received 10 mg ulipristal. At baseline, average total quality of life scores on UFS-QOL were 33 (standard deviation, 220), 32 (SD, 21), and 36 (SD, 23), respectively, the researchers wrote in Obstetrics & Gynecology.
After 12 weeks of treatment, both doses of ulipristal were associated with significantly greater improvements on all UFS-QOL scales, compared with placebo (P less than .001). For example, on a scale of 0-100, symptom severity improved by a mean of 23 with ulipristal 5 mg and by a mean of 30 with ulipristal 10 mg (both P less than .001 versus placebo).
“Although a small proportion of patients experienced no change or some worsening in these outcomes, the majority of women reported clear improvements; for example, more than 70% of patients in the ulipristal treatment arms achieved a meaningful improvement of 30 or more points on the Revised Activities subscale,” the researchers wrote.
Additionally, significantly greater improvements in physical and social activities were seen for both ulipristal doses, compared with placebo, from baseline to the end of treatment.
The VENUS II trial included two 12-week treatment courses. In this trial, women who switched from ulipristal to placebo experienced some worsening in quality of life, while those who switched from placebo to ulipristal improved their UFS-QOL scores, the investigators said. Patients who stayed on ulipristal throughout continued to benefit from one treatment course to the next.
The researchers concluded that the findings, “taken together with the significant improvements in amenorrhea, suggest that ulipristal is a promising, noninvasive treatment option for women suffering from symptomatic uterine leiomyomas.”
Allergan provided funding. Dr. Lukes disclosed ties to Allergan, AbbVie, Myovant, Merck, and several other companies. Four of the coauthors are employees of Allergan, and the two remaining coauthors had links to a number of pharmaceutical companies.
SOURCE: Lukes AS et al. Obstet Gynecol 2019;133 (5):869-78.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: For women with symptomatic uterine leiomyomas, ulipristal at either 5 mg or 10 mg significantly improved both the rate of and time to amenorrhea, compared with placebo.
Major finding: Patients who received 5 or 10 mg ulipristal showed significant improvements in Uterine Fibroid Symptom Health-Related Quality of Life scales, compared with those who received placebo (P less than .001).
Study details: VENUS I and II, 12-week randomized controlled trials of ulipristal acetate or placebo in 589 women with symptomatic uterine leiomyomas and abnormal uterine bleeding.
Disclosures: Allergan provided funding. Dr. Lukes disclosed ties to Allergan, AbbVie, Myovant, Merck, and several other companies. Four of the coauthors are employees of Allergan, and the two remaining coauthors had links to a number of pharmaceutical companies.
Source: Lukes AS et al. Obstet Gynecol. 2019 May;133(5):869-78.
More data point to potency of genes in development of psychosis
Early findings suggest that positive environment is not protective
ORLANDO – A genetic profile that’s considered risky for psychosis matters more for patients who come from an environmental background that is considered good, while it doesn’t seem to make much of a difference among those whose environmental background is more adverse, according to research presented at the annual congress of the Schizophrenia International Research Society.
Researchers at the University of Pennsylvania, Philadelphia, are examining a wide variety of data – from socioeconomic factors to neuroimaging – to assess how these data all feed into the psychosis picture, asking whether some factors matter more than others and which factors can be used to predict the development of psychosis in the future.
“The goal of all of the research ... is to try and capture people earlier in the course of development where we can try and tweak the developmental trajectory,” said Raquel Gur, MD, PhD, professor of psychiatry, neurology, and radiology at the university.
The findings come from the Philadelphia Neurodevelopmental Cohort, a community sample of about 9,500 children and young adults aged 8-21 years, with an average age of 15 years, collected through pediatricians. About 1,600 had neuroimaging. Researchers followed 961 participants who had baseline measurements recorded and were seen at follow-up visits after 2 years and 4 years, or longer.
Participants had clinical testing done to determine traumatic stressful events and to look for symptoms seen as precursors to psychosis. They also had neurocognitive battery tests performed. Neuroimaging, genomics testing, and information from their electronic medical record were also examined.
One of the most salient findings so far in their ongoing analysis involved the relationship between polygenic risk score (PRS) and their environmental risk score (ERS), which factored in items such as household income from their geographic area, percentage of married adults in their area, crime rates in their area, and traumatic stressful events experienced personally. The ERS scores were grouped into “good” scores and “bad” scores.
Researchers saw a trend in which, among those with good ERS scores, the average PRS was higher for those with psychotic spectrum symptoms than for those with normal development, with very little overlapping of 95% confidence intervals. But among those with bad ERS scores, the average PRS was about the same for those with psychotic spectrum symptoms and those with normal development.
“If you have genetic vulnerability, a good environment is not going to protect you. You’re going to manifest it,” Dr. Gur said. “However, in a negative environment that has adversity that includes both a poor environment and traumatic events, the polygenic risk score matters less.”
They are continuing to explore and assess these findings.
The researchers also found differences in cognitive functioning among those with poor environmental scores, which dovetail with defects seen in schizophrenia, such as executive functioning.
“Neurocognitive functioning can be established with brief computerized testing,” Dr. Gur said, “and shows deficit in the psychosis spectrum group in domains that have been implicated in schizophrenia.”
Dr. Gur reported no relevant financial disclosures.
Early findings suggest that positive environment is not protective
Early findings suggest that positive environment is not protective
ORLANDO – A genetic profile that’s considered risky for psychosis matters more for patients who come from an environmental background that is considered good, while it doesn’t seem to make much of a difference among those whose environmental background is more adverse, according to research presented at the annual congress of the Schizophrenia International Research Society.
Researchers at the University of Pennsylvania, Philadelphia, are examining a wide variety of data – from socioeconomic factors to neuroimaging – to assess how these data all feed into the psychosis picture, asking whether some factors matter more than others and which factors can be used to predict the development of psychosis in the future.
“The goal of all of the research ... is to try and capture people earlier in the course of development where we can try and tweak the developmental trajectory,” said Raquel Gur, MD, PhD, professor of psychiatry, neurology, and radiology at the university.
The findings come from the Philadelphia Neurodevelopmental Cohort, a community sample of about 9,500 children and young adults aged 8-21 years, with an average age of 15 years, collected through pediatricians. About 1,600 had neuroimaging. Researchers followed 961 participants who had baseline measurements recorded and were seen at follow-up visits after 2 years and 4 years, or longer.
Participants had clinical testing done to determine traumatic stressful events and to look for symptoms seen as precursors to psychosis. They also had neurocognitive battery tests performed. Neuroimaging, genomics testing, and information from their electronic medical record were also examined.
One of the most salient findings so far in their ongoing analysis involved the relationship between polygenic risk score (PRS) and their environmental risk score (ERS), which factored in items such as household income from their geographic area, percentage of married adults in their area, crime rates in their area, and traumatic stressful events experienced personally. The ERS scores were grouped into “good” scores and “bad” scores.
Researchers saw a trend in which, among those with good ERS scores, the average PRS was higher for those with psychotic spectrum symptoms than for those with normal development, with very little overlapping of 95% confidence intervals. But among those with bad ERS scores, the average PRS was about the same for those with psychotic spectrum symptoms and those with normal development.
“If you have genetic vulnerability, a good environment is not going to protect you. You’re going to manifest it,” Dr. Gur said. “However, in a negative environment that has adversity that includes both a poor environment and traumatic events, the polygenic risk score matters less.”
They are continuing to explore and assess these findings.
The researchers also found differences in cognitive functioning among those with poor environmental scores, which dovetail with defects seen in schizophrenia, such as executive functioning.
“Neurocognitive functioning can be established with brief computerized testing,” Dr. Gur said, “and shows deficit in the psychosis spectrum group in domains that have been implicated in schizophrenia.”
Dr. Gur reported no relevant financial disclosures.
ORLANDO – A genetic profile that’s considered risky for psychosis matters more for patients who come from an environmental background that is considered good, while it doesn’t seem to make much of a difference among those whose environmental background is more adverse, according to research presented at the annual congress of the Schizophrenia International Research Society.
Researchers at the University of Pennsylvania, Philadelphia, are examining a wide variety of data – from socioeconomic factors to neuroimaging – to assess how these data all feed into the psychosis picture, asking whether some factors matter more than others and which factors can be used to predict the development of psychosis in the future.
“The goal of all of the research ... is to try and capture people earlier in the course of development where we can try and tweak the developmental trajectory,” said Raquel Gur, MD, PhD, professor of psychiatry, neurology, and radiology at the university.
The findings come from the Philadelphia Neurodevelopmental Cohort, a community sample of about 9,500 children and young adults aged 8-21 years, with an average age of 15 years, collected through pediatricians. About 1,600 had neuroimaging. Researchers followed 961 participants who had baseline measurements recorded and were seen at follow-up visits after 2 years and 4 years, or longer.
Participants had clinical testing done to determine traumatic stressful events and to look for symptoms seen as precursors to psychosis. They also had neurocognitive battery tests performed. Neuroimaging, genomics testing, and information from their electronic medical record were also examined.
One of the most salient findings so far in their ongoing analysis involved the relationship between polygenic risk score (PRS) and their environmental risk score (ERS), which factored in items such as household income from their geographic area, percentage of married adults in their area, crime rates in their area, and traumatic stressful events experienced personally. The ERS scores were grouped into “good” scores and “bad” scores.
Researchers saw a trend in which, among those with good ERS scores, the average PRS was higher for those with psychotic spectrum symptoms than for those with normal development, with very little overlapping of 95% confidence intervals. But among those with bad ERS scores, the average PRS was about the same for those with psychotic spectrum symptoms and those with normal development.
“If you have genetic vulnerability, a good environment is not going to protect you. You’re going to manifest it,” Dr. Gur said. “However, in a negative environment that has adversity that includes both a poor environment and traumatic events, the polygenic risk score matters less.”
They are continuing to explore and assess these findings.
The researchers also found differences in cognitive functioning among those with poor environmental scores, which dovetail with defects seen in schizophrenia, such as executive functioning.
“Neurocognitive functioning can be established with brief computerized testing,” Dr. Gur said, “and shows deficit in the psychosis spectrum group in domains that have been implicated in schizophrenia.”
Dr. Gur reported no relevant financial disclosures.
REPORTING FROM SIRS 2019
Version success more likely in lower BMI, multiparous breech pregnancies
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Multiparity, larger forebag size, and lower BMI are predictors of external cephalic version success.
Major finding: Model of external cephalic version success shows prediction accuracy of 92%.
Study details: A single-center retrospective cohort study in 250 women with breech presentation.
Disclosures: None of the authors declared any relevant financial disclosures, and there was no external funding.
Source: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
CAR T-cell therapy bb2121 performs well in phase 1 trial of refractory multiple myeloma
Chimeric antigen receptor (CAR) T-cell therapy bb2121, which targets B-cell maturation agent (BCMA), appears safe and effective for treating patients with refractory multiple myeloma, according to results of a phase 1 trial.
The objective response rate of 85% among 33 heavily pretreated patients suggests “promising efficacy,” reported lead author Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston and colleagues.
“Although comparisons among studies are complicated by differences in patient populations, CAR constructs, administered doses, and grading scales of toxic effects, the results observed with bb2121 indicate a favorable safety profile,” the investigators wrote in a study published in the New England Journal of Medicine.
The study initially involved 36 patients with refractory multiple myeloma who had received at least three lines of prior therapy, including an immunomodulatory agent and a proteasome inhibitor. Although leukapheresis and therapy manufacturing were successful in all patients, three patients were excluded from receiving the infusion because of disease progression.
The 33 remaining patients were lymphodepleted with fludarabine and cyclophosphamide. Bridging therapy was allowed during the manufacturing process but was stopped at least 2 weeks prior to infusion. In the dose-escalation phase of the study, b2121 was delivered as a single infusion at one of four dose levels: 50 × 106, 150 × 106, 450 × 106, or 800 × 106 CAR T cells. In the expansion phase, the treatment was given at either 150 x 106 or 450 x 106 CAR T cells. The primary endpoint was safety; the secondary endpoints were response rate and duration of response.
After a median follow-up of 11.3 months, most patients (85%) had responded to therapy, and almost half (45%) had achieved a complete response. Of the 15 complete responders, 6 relapsed. The median progression-free survival was 11.8 months; stated differently, two out of five patients (40%) had not experienced disease progression after 1 year. CAR T cells were detectable 1 month after infusion in 96% of patients; however, this value dropped to 86% at 3 months, 57% at 6 months, and 20% at 12 months. The investigators noted that CAR T-cell persistence was associated with treatment response.
All patients had adverse events. Most (85%) had grade 3 or higher hematologic toxicity, which the investigators considered to be the “expected toxic effects of lymphodepleting chemotherapy.” Although other adverse events occurred in the majority of patients, these were generally mild to moderate. Cytokine release syndrome occurred in 25 patients (76%), including two instances of grade 3 toxicity but none of grade 4 or higher. Fourteen patients (42%) developed neurologic toxicities: Most were grade 1 or 2, but one patient had a grade 4 toxicity that resolved after a month. Infections occurred at the same rate (42%), although, again, most were grade 1 or 2.
The study was funded by Bluebird Bio and Celgene. The investigators disclosed financial relationships with Bluebird and other drug companies.
SOURCE: Raje N et al. NEJM. 1 May 2019. doi: 10.1056/NEJMoa1817226.
Chimeric antigen receptor (CAR) T-cell therapy bb2121, which targets B-cell maturation agent (BCMA), appears safe and effective for treating patients with refractory multiple myeloma, according to results of a phase 1 trial.
The objective response rate of 85% among 33 heavily pretreated patients suggests “promising efficacy,” reported lead author Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston and colleagues.
“Although comparisons among studies are complicated by differences in patient populations, CAR constructs, administered doses, and grading scales of toxic effects, the results observed with bb2121 indicate a favorable safety profile,” the investigators wrote in a study published in the New England Journal of Medicine.
The study initially involved 36 patients with refractory multiple myeloma who had received at least three lines of prior therapy, including an immunomodulatory agent and a proteasome inhibitor. Although leukapheresis and therapy manufacturing were successful in all patients, three patients were excluded from receiving the infusion because of disease progression.
The 33 remaining patients were lymphodepleted with fludarabine and cyclophosphamide. Bridging therapy was allowed during the manufacturing process but was stopped at least 2 weeks prior to infusion. In the dose-escalation phase of the study, b2121 was delivered as a single infusion at one of four dose levels: 50 × 106, 150 × 106, 450 × 106, or 800 × 106 CAR T cells. In the expansion phase, the treatment was given at either 150 x 106 or 450 x 106 CAR T cells. The primary endpoint was safety; the secondary endpoints were response rate and duration of response.
After a median follow-up of 11.3 months, most patients (85%) had responded to therapy, and almost half (45%) had achieved a complete response. Of the 15 complete responders, 6 relapsed. The median progression-free survival was 11.8 months; stated differently, two out of five patients (40%) had not experienced disease progression after 1 year. CAR T cells were detectable 1 month after infusion in 96% of patients; however, this value dropped to 86% at 3 months, 57% at 6 months, and 20% at 12 months. The investigators noted that CAR T-cell persistence was associated with treatment response.
All patients had adverse events. Most (85%) had grade 3 or higher hematologic toxicity, which the investigators considered to be the “expected toxic effects of lymphodepleting chemotherapy.” Although other adverse events occurred in the majority of patients, these were generally mild to moderate. Cytokine release syndrome occurred in 25 patients (76%), including two instances of grade 3 toxicity but none of grade 4 or higher. Fourteen patients (42%) developed neurologic toxicities: Most were grade 1 or 2, but one patient had a grade 4 toxicity that resolved after a month. Infections occurred at the same rate (42%), although, again, most were grade 1 or 2.
The study was funded by Bluebird Bio and Celgene. The investigators disclosed financial relationships with Bluebird and other drug companies.
SOURCE: Raje N et al. NEJM. 1 May 2019. doi: 10.1056/NEJMoa1817226.
Chimeric antigen receptor (CAR) T-cell therapy bb2121, which targets B-cell maturation agent (BCMA), appears safe and effective for treating patients with refractory multiple myeloma, according to results of a phase 1 trial.
The objective response rate of 85% among 33 heavily pretreated patients suggests “promising efficacy,” reported lead author Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston and colleagues.
“Although comparisons among studies are complicated by differences in patient populations, CAR constructs, administered doses, and grading scales of toxic effects, the results observed with bb2121 indicate a favorable safety profile,” the investigators wrote in a study published in the New England Journal of Medicine.
The study initially involved 36 patients with refractory multiple myeloma who had received at least three lines of prior therapy, including an immunomodulatory agent and a proteasome inhibitor. Although leukapheresis and therapy manufacturing were successful in all patients, three patients were excluded from receiving the infusion because of disease progression.
The 33 remaining patients were lymphodepleted with fludarabine and cyclophosphamide. Bridging therapy was allowed during the manufacturing process but was stopped at least 2 weeks prior to infusion. In the dose-escalation phase of the study, b2121 was delivered as a single infusion at one of four dose levels: 50 × 106, 150 × 106, 450 × 106, or 800 × 106 CAR T cells. In the expansion phase, the treatment was given at either 150 x 106 or 450 x 106 CAR T cells. The primary endpoint was safety; the secondary endpoints were response rate and duration of response.
After a median follow-up of 11.3 months, most patients (85%) had responded to therapy, and almost half (45%) had achieved a complete response. Of the 15 complete responders, 6 relapsed. The median progression-free survival was 11.8 months; stated differently, two out of five patients (40%) had not experienced disease progression after 1 year. CAR T cells were detectable 1 month after infusion in 96% of patients; however, this value dropped to 86% at 3 months, 57% at 6 months, and 20% at 12 months. The investigators noted that CAR T-cell persistence was associated with treatment response.
All patients had adverse events. Most (85%) had grade 3 or higher hematologic toxicity, which the investigators considered to be the “expected toxic effects of lymphodepleting chemotherapy.” Although other adverse events occurred in the majority of patients, these were generally mild to moderate. Cytokine release syndrome occurred in 25 patients (76%), including two instances of grade 3 toxicity but none of grade 4 or higher. Fourteen patients (42%) developed neurologic toxicities: Most were grade 1 or 2, but one patient had a grade 4 toxicity that resolved after a month. Infections occurred at the same rate (42%), although, again, most were grade 1 or 2.
The study was funded by Bluebird Bio and Celgene. The investigators disclosed financial relationships with Bluebird and other drug companies.
SOURCE: Raje N et al. NEJM. 1 May 2019. doi: 10.1056/NEJMoa1817226.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Study compares tapering strategies in rheumatoid arthritis
Patients whose rheumatoid arthritis was in sustained remission had similar rates of flare for the first 9 months after they tapered off either their conventional synthetic disease-modifying antirheumatic drug (DMARD), or their tumor necrosis factor (TNF) inhibitor, researchers reported.
After the first year, first author Elise van Mulligen of Erasmus University Medical Center in Rotterdam, the Netherlands, and her associates found that flares rates were 10% lower among patients who first tapered conventional synthetic DMARDs, a difference that was not statistically significant. Because secondary endpoints also were similar between groups, patients should consider first tapering off their TNF inhibitor to save costs and reduce side effects, the researchers wrote in Annals of the Rheumatic Diseases.
Over the past decade, better drugs, treat-to-target approaches, and earlier disease detection have vastly improved outcomes in rheumatoid arthritis. As more patients achieve sustained remission, they are tapering off therapy in accordance with current guidelines. This multicenter, single-blinded, randomized trial (Tapering Strategies in Rheumatoid Arthritis [TARA]) is one of the first to compare tapering strategies, rather than looking at only whether tapering is feasible.
The study included 189 patients from the Netherlands whose rheumatoid arthritis was in sustained remission (Disease Activity Score [DAS] less than 2.4 and swollen joint count less than 1 for at least 3 months) on a conventional synthetic DMARD plus a TNF inhibitor. Patients were randomly assigned to either halve the conventional synthetic DMARD dose, or to double the TNF-inhibitor dosing interval. After 3 months, they cut the dose of their assigned taper medication to 25% of baseline. If they stayed in remission, they stopped the medication 3 months later. They avoided glucocorticoids throughout.
There were no serious adverse events related to tapering. Cumulative rates of flare at 1 year (DAS greater than 2.4 or swollen joint count greater than 1) were 33% for conventional synthetic DMARD taper (95% confidence interval, 24%-43%) and 43% (95% CI, 33%-53%) for TNF-inhibitor taper (P = .17). The two groups also had similar scores at 1 year on the DAS, Health Assessment Questionnaire-Disability Index, and European Quality of Life-5 Dimensions index.
The suggestion to first taper off TNF inhibitors reflects current European League Against Rheumatism guidelines, which advise first tapering glucocorticoids, then biologic DMARDS, and finally conventional synthetic DMARDs. “Our results and the fact that TNF blockers are more expensive than conventional synthetic DMARDs support the aforementioned tapering order,” the researchers concluded.
An unrestricted grant from ZonMW supported the work. The investigators reported having no conflicts of interest.
SOURCE: Mulligen E et al. Ann Rheum Dis. 2019 Apr 6. doi: 10.1136/annrheumdis-2018-214970.
Patients whose rheumatoid arthritis was in sustained remission had similar rates of flare for the first 9 months after they tapered off either their conventional synthetic disease-modifying antirheumatic drug (DMARD), or their tumor necrosis factor (TNF) inhibitor, researchers reported.
After the first year, first author Elise van Mulligen of Erasmus University Medical Center in Rotterdam, the Netherlands, and her associates found that flares rates were 10% lower among patients who first tapered conventional synthetic DMARDs, a difference that was not statistically significant. Because secondary endpoints also were similar between groups, patients should consider first tapering off their TNF inhibitor to save costs and reduce side effects, the researchers wrote in Annals of the Rheumatic Diseases.
Over the past decade, better drugs, treat-to-target approaches, and earlier disease detection have vastly improved outcomes in rheumatoid arthritis. As more patients achieve sustained remission, they are tapering off therapy in accordance with current guidelines. This multicenter, single-blinded, randomized trial (Tapering Strategies in Rheumatoid Arthritis [TARA]) is one of the first to compare tapering strategies, rather than looking at only whether tapering is feasible.
The study included 189 patients from the Netherlands whose rheumatoid arthritis was in sustained remission (Disease Activity Score [DAS] less than 2.4 and swollen joint count less than 1 for at least 3 months) on a conventional synthetic DMARD plus a TNF inhibitor. Patients were randomly assigned to either halve the conventional synthetic DMARD dose, or to double the TNF-inhibitor dosing interval. After 3 months, they cut the dose of their assigned taper medication to 25% of baseline. If they stayed in remission, they stopped the medication 3 months later. They avoided glucocorticoids throughout.
There were no serious adverse events related to tapering. Cumulative rates of flare at 1 year (DAS greater than 2.4 or swollen joint count greater than 1) were 33% for conventional synthetic DMARD taper (95% confidence interval, 24%-43%) and 43% (95% CI, 33%-53%) for TNF-inhibitor taper (P = .17). The two groups also had similar scores at 1 year on the DAS, Health Assessment Questionnaire-Disability Index, and European Quality of Life-5 Dimensions index.
The suggestion to first taper off TNF inhibitors reflects current European League Against Rheumatism guidelines, which advise first tapering glucocorticoids, then biologic DMARDS, and finally conventional synthetic DMARDs. “Our results and the fact that TNF blockers are more expensive than conventional synthetic DMARDs support the aforementioned tapering order,” the researchers concluded.
An unrestricted grant from ZonMW supported the work. The investigators reported having no conflicts of interest.
SOURCE: Mulligen E et al. Ann Rheum Dis. 2019 Apr 6. doi: 10.1136/annrheumdis-2018-214970.
Patients whose rheumatoid arthritis was in sustained remission had similar rates of flare for the first 9 months after they tapered off either their conventional synthetic disease-modifying antirheumatic drug (DMARD), or their tumor necrosis factor (TNF) inhibitor, researchers reported.
After the first year, first author Elise van Mulligen of Erasmus University Medical Center in Rotterdam, the Netherlands, and her associates found that flares rates were 10% lower among patients who first tapered conventional synthetic DMARDs, a difference that was not statistically significant. Because secondary endpoints also were similar between groups, patients should consider first tapering off their TNF inhibitor to save costs and reduce side effects, the researchers wrote in Annals of the Rheumatic Diseases.
Over the past decade, better drugs, treat-to-target approaches, and earlier disease detection have vastly improved outcomes in rheumatoid arthritis. As more patients achieve sustained remission, they are tapering off therapy in accordance with current guidelines. This multicenter, single-blinded, randomized trial (Tapering Strategies in Rheumatoid Arthritis [TARA]) is one of the first to compare tapering strategies, rather than looking at only whether tapering is feasible.
The study included 189 patients from the Netherlands whose rheumatoid arthritis was in sustained remission (Disease Activity Score [DAS] less than 2.4 and swollen joint count less than 1 for at least 3 months) on a conventional synthetic DMARD plus a TNF inhibitor. Patients were randomly assigned to either halve the conventional synthetic DMARD dose, or to double the TNF-inhibitor dosing interval. After 3 months, they cut the dose of their assigned taper medication to 25% of baseline. If they stayed in remission, they stopped the medication 3 months later. They avoided glucocorticoids throughout.
There were no serious adverse events related to tapering. Cumulative rates of flare at 1 year (DAS greater than 2.4 or swollen joint count greater than 1) were 33% for conventional synthetic DMARD taper (95% confidence interval, 24%-43%) and 43% (95% CI, 33%-53%) for TNF-inhibitor taper (P = .17). The two groups also had similar scores at 1 year on the DAS, Health Assessment Questionnaire-Disability Index, and European Quality of Life-5 Dimensions index.
The suggestion to first taper off TNF inhibitors reflects current European League Against Rheumatism guidelines, which advise first tapering glucocorticoids, then biologic DMARDS, and finally conventional synthetic DMARDs. “Our results and the fact that TNF blockers are more expensive than conventional synthetic DMARDs support the aforementioned tapering order,” the researchers concluded.
An unrestricted grant from ZonMW supported the work. The investigators reported having no conflicts of interest.
SOURCE: Mulligen E et al. Ann Rheum Dis. 2019 Apr 6. doi: 10.1136/annrheumdis-2018-214970.
FROM ANNALS OF THE RHEUMATIC DISEASES
Interosseous tendon inflammation is common prior to RA
MAUI, HAWAII – Inflammation of the hand interosseous tendons found on MRI is a novel target in efforts to preempt the development and progression of rheumatoid arthritis, Paul Emery, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He and his coinvestigators have previously shown there is a high prevalence of interosseous tendon inflammation in the hands of patients with established RA, but now they’ve demonstrated that this phenomenon also occurs in anti–cyclic citrullinated peptide (CCP)–positive individuals at increased risk for RA, even before onset of clinical synovitis.
This finding is consistent with the notion that, even though RA is classically considered a disease of the synovial joints, the joint involvement is a relatively late phenomenon in the disease development process and extracapsular structures may be important early targets of RA-related inflammation. Indeed, the MRI finding of tenosynovitis of the wrist and finger flexor tendons is known to be the strongest predictor of progression to arthritis in patients with recent-onset arthralgia or other musculoskeletal symptoms but no clinical synovitis, according to Dr. Emery, professor of rheumatology and director of the University of Leeds (England) Musculoskeletal Biomedical Research Center.
Because the interosseous muscles of the hands play a critical role in hand function – pianists and other musicians not infrequently present to rheumatologists with overuse injuries of the muscles and their tendons – Dr. Emery and his coworkers decided to take a comprehensive look at interosseous tendon inflammation across the full spectrum of RA and pre-RA. They conducted a retrospective study of clinical and hand MRI data on 93 CCP-positive patients who presented with new-onset musculoskeletal symptoms but no clinical synovitis; 47 patients with early RA, all of whom were disease-modifying antirheumatic drug–naive; 28 patients with late RA as defined by at least 1 year of symptoms, anti-CCP and/or rheumatoid factor positivity, a Disease Activity Score in 28 joints (DAS28) of 3.2 or more, plus a history of exposure to one or more DMARDs at the time of their hand imaging; and 20 healthy controls.
The key finding is that the proportion of subjects with MRI evidence of interosseous tendon inflammation rose along the advancing RA continuum. It was present in 19% of the CCP-positive patients without clinical synovitis; 49% of the DMARD-naive early RA group; 57% of the late RA group; and in none of the healthy controls. Moreover, the number of inflamed interosseous tendons per patient also increased with RA progression.
A total of 12% of 507 nontender metacarpophalangeal joints showed MRI evidence of interosseous tendon inflammation, as did 28% of 141 tender ones (Ann Rheum Dis. 2019 Mar 23. doi: 10.1136/annrheumdis-2018-214331).
As part of the study, Dr. Emery and coinvestigators performed cadaveric dissections that demonstrated that the interosseous tendons don’t possess a tendon sheath and don’t directly communicate with the joint capsule.
A prospective study is warranted in order to confirm the observed association between interosseous tendon inflammation and clinical and subclinical synovitis and to establish the predictive value of hand MRI as a harbinger of RA, he noted.
Dr. Emery reported having no financial conflicts regarding his presentation.
MAUI, HAWAII – Inflammation of the hand interosseous tendons found on MRI is a novel target in efforts to preempt the development and progression of rheumatoid arthritis, Paul Emery, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He and his coinvestigators have previously shown there is a high prevalence of interosseous tendon inflammation in the hands of patients with established RA, but now they’ve demonstrated that this phenomenon also occurs in anti–cyclic citrullinated peptide (CCP)–positive individuals at increased risk for RA, even before onset of clinical synovitis.
This finding is consistent with the notion that, even though RA is classically considered a disease of the synovial joints, the joint involvement is a relatively late phenomenon in the disease development process and extracapsular structures may be important early targets of RA-related inflammation. Indeed, the MRI finding of tenosynovitis of the wrist and finger flexor tendons is known to be the strongest predictor of progression to arthritis in patients with recent-onset arthralgia or other musculoskeletal symptoms but no clinical synovitis, according to Dr. Emery, professor of rheumatology and director of the University of Leeds (England) Musculoskeletal Biomedical Research Center.
Because the interosseous muscles of the hands play a critical role in hand function – pianists and other musicians not infrequently present to rheumatologists with overuse injuries of the muscles and their tendons – Dr. Emery and his coworkers decided to take a comprehensive look at interosseous tendon inflammation across the full spectrum of RA and pre-RA. They conducted a retrospective study of clinical and hand MRI data on 93 CCP-positive patients who presented with new-onset musculoskeletal symptoms but no clinical synovitis; 47 patients with early RA, all of whom were disease-modifying antirheumatic drug–naive; 28 patients with late RA as defined by at least 1 year of symptoms, anti-CCP and/or rheumatoid factor positivity, a Disease Activity Score in 28 joints (DAS28) of 3.2 or more, plus a history of exposure to one or more DMARDs at the time of their hand imaging; and 20 healthy controls.
The key finding is that the proportion of subjects with MRI evidence of interosseous tendon inflammation rose along the advancing RA continuum. It was present in 19% of the CCP-positive patients without clinical synovitis; 49% of the DMARD-naive early RA group; 57% of the late RA group; and in none of the healthy controls. Moreover, the number of inflamed interosseous tendons per patient also increased with RA progression.
A total of 12% of 507 nontender metacarpophalangeal joints showed MRI evidence of interosseous tendon inflammation, as did 28% of 141 tender ones (Ann Rheum Dis. 2019 Mar 23. doi: 10.1136/annrheumdis-2018-214331).
As part of the study, Dr. Emery and coinvestigators performed cadaveric dissections that demonstrated that the interosseous tendons don’t possess a tendon sheath and don’t directly communicate with the joint capsule.
A prospective study is warranted in order to confirm the observed association between interosseous tendon inflammation and clinical and subclinical synovitis and to establish the predictive value of hand MRI as a harbinger of RA, he noted.
Dr. Emery reported having no financial conflicts regarding his presentation.
MAUI, HAWAII – Inflammation of the hand interosseous tendons found on MRI is a novel target in efforts to preempt the development and progression of rheumatoid arthritis, Paul Emery, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He and his coinvestigators have previously shown there is a high prevalence of interosseous tendon inflammation in the hands of patients with established RA, but now they’ve demonstrated that this phenomenon also occurs in anti–cyclic citrullinated peptide (CCP)–positive individuals at increased risk for RA, even before onset of clinical synovitis.
This finding is consistent with the notion that, even though RA is classically considered a disease of the synovial joints, the joint involvement is a relatively late phenomenon in the disease development process and extracapsular structures may be important early targets of RA-related inflammation. Indeed, the MRI finding of tenosynovitis of the wrist and finger flexor tendons is known to be the strongest predictor of progression to arthritis in patients with recent-onset arthralgia or other musculoskeletal symptoms but no clinical synovitis, according to Dr. Emery, professor of rheumatology and director of the University of Leeds (England) Musculoskeletal Biomedical Research Center.
Because the interosseous muscles of the hands play a critical role in hand function – pianists and other musicians not infrequently present to rheumatologists with overuse injuries of the muscles and their tendons – Dr. Emery and his coworkers decided to take a comprehensive look at interosseous tendon inflammation across the full spectrum of RA and pre-RA. They conducted a retrospective study of clinical and hand MRI data on 93 CCP-positive patients who presented with new-onset musculoskeletal symptoms but no clinical synovitis; 47 patients with early RA, all of whom were disease-modifying antirheumatic drug–naive; 28 patients with late RA as defined by at least 1 year of symptoms, anti-CCP and/or rheumatoid factor positivity, a Disease Activity Score in 28 joints (DAS28) of 3.2 or more, plus a history of exposure to one or more DMARDs at the time of their hand imaging; and 20 healthy controls.
The key finding is that the proportion of subjects with MRI evidence of interosseous tendon inflammation rose along the advancing RA continuum. It was present in 19% of the CCP-positive patients without clinical synovitis; 49% of the DMARD-naive early RA group; 57% of the late RA group; and in none of the healthy controls. Moreover, the number of inflamed interosseous tendons per patient also increased with RA progression.
A total of 12% of 507 nontender metacarpophalangeal joints showed MRI evidence of interosseous tendon inflammation, as did 28% of 141 tender ones (Ann Rheum Dis. 2019 Mar 23. doi: 10.1136/annrheumdis-2018-214331).
As part of the study, Dr. Emery and coinvestigators performed cadaveric dissections that demonstrated that the interosseous tendons don’t possess a tendon sheath and don’t directly communicate with the joint capsule.
A prospective study is warranted in order to confirm the observed association between interosseous tendon inflammation and clinical and subclinical synovitis and to establish the predictive value of hand MRI as a harbinger of RA, he noted.
Dr. Emery reported having no financial conflicts regarding his presentation.
REPORTING FROM RWCS 2019
Bringing hospitalist coverage to critical access hospitals
“As a hospitalist, I believe that my specialty improves care for inpatients,” said Ethan Kuperman, MD, MS, FHM, clinical associate professor of medicine at University of Iowa Health Care in Iowa City. “I want hospitalists involved with as many hospitals as possible because I believe we will lead to better patient outcomes.”
But, he adds, it’s not feasible to place dedicated hospitalists in every rural hospital in the United States – especially those running far below the average hospitalist census. “As a university, academic hospitalist, I wanted to make sure that the innovations and knowledge of the University of Iowa could penetrate into the greater community, and I wanted to strengthen the continuity of care between our partners in rural Iowa and our physical location in Iowa City,” he said.
Enter the virtual hospitalist: A telemedicine “virtual hospitalist” may expand capabilities at a fractional cost of an on-site provider.
Dr. Kuperman’s 6-month pilot program provided “virtual hospitalist” coverage to patients at a critical access hospital in rural Iowa.
“Our rural partners want to ensure that they are providing high-quality care within their communities and aren’t transferring patients without a good indication to larger centers,” he said. “For patients, this program means more of them can remain in their communities, surrounded by their families. I don’t think the virtual hospitalist program delivers equivalent care to the university hospital – I think we deliver better care because of that continuity with local providers and the ability of patients to remain in contact with their support structures.”
The study concludes that the virtual hospitalist model increased the percentage of ED patients who could safely receive their care locally, and a single virtual hospitalist may be able to cover multiple critical access hospitals simultaneously.
“We have the technology to deliver hospitalist expertise to rural hospitals through telehealth in a way that benefits patients, rural hospitals, and academic hospitals,” he said.
Reference
Kuperman E et al. The Virtual Hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. Journal of Hospital Medicine. Published online first 2018 Sep 26. doi: 10.12788/jhm.3061. Accessed 2018 Oct 2.
“As a hospitalist, I believe that my specialty improves care for inpatients,” said Ethan Kuperman, MD, MS, FHM, clinical associate professor of medicine at University of Iowa Health Care in Iowa City. “I want hospitalists involved with as many hospitals as possible because I believe we will lead to better patient outcomes.”
But, he adds, it’s not feasible to place dedicated hospitalists in every rural hospital in the United States – especially those running far below the average hospitalist census. “As a university, academic hospitalist, I wanted to make sure that the innovations and knowledge of the University of Iowa could penetrate into the greater community, and I wanted to strengthen the continuity of care between our partners in rural Iowa and our physical location in Iowa City,” he said.
Enter the virtual hospitalist: A telemedicine “virtual hospitalist” may expand capabilities at a fractional cost of an on-site provider.
Dr. Kuperman’s 6-month pilot program provided “virtual hospitalist” coverage to patients at a critical access hospital in rural Iowa.
“Our rural partners want to ensure that they are providing high-quality care within their communities and aren’t transferring patients without a good indication to larger centers,” he said. “For patients, this program means more of them can remain in their communities, surrounded by their families. I don’t think the virtual hospitalist program delivers equivalent care to the university hospital – I think we deliver better care because of that continuity with local providers and the ability of patients to remain in contact with their support structures.”
The study concludes that the virtual hospitalist model increased the percentage of ED patients who could safely receive their care locally, and a single virtual hospitalist may be able to cover multiple critical access hospitals simultaneously.
“We have the technology to deliver hospitalist expertise to rural hospitals through telehealth in a way that benefits patients, rural hospitals, and academic hospitals,” he said.
Reference
Kuperman E et al. The Virtual Hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. Journal of Hospital Medicine. Published online first 2018 Sep 26. doi: 10.12788/jhm.3061. Accessed 2018 Oct 2.
“As a hospitalist, I believe that my specialty improves care for inpatients,” said Ethan Kuperman, MD, MS, FHM, clinical associate professor of medicine at University of Iowa Health Care in Iowa City. “I want hospitalists involved with as many hospitals as possible because I believe we will lead to better patient outcomes.”
But, he adds, it’s not feasible to place dedicated hospitalists in every rural hospital in the United States – especially those running far below the average hospitalist census. “As a university, academic hospitalist, I wanted to make sure that the innovations and knowledge of the University of Iowa could penetrate into the greater community, and I wanted to strengthen the continuity of care between our partners in rural Iowa and our physical location in Iowa City,” he said.
Enter the virtual hospitalist: A telemedicine “virtual hospitalist” may expand capabilities at a fractional cost of an on-site provider.
Dr. Kuperman’s 6-month pilot program provided “virtual hospitalist” coverage to patients at a critical access hospital in rural Iowa.
“Our rural partners want to ensure that they are providing high-quality care within their communities and aren’t transferring patients without a good indication to larger centers,” he said. “For patients, this program means more of them can remain in their communities, surrounded by their families. I don’t think the virtual hospitalist program delivers equivalent care to the university hospital – I think we deliver better care because of that continuity with local providers and the ability of patients to remain in contact with their support structures.”
The study concludes that the virtual hospitalist model increased the percentage of ED patients who could safely receive their care locally, and a single virtual hospitalist may be able to cover multiple critical access hospitals simultaneously.
“We have the technology to deliver hospitalist expertise to rural hospitals through telehealth in a way that benefits patients, rural hospitals, and academic hospitals,” he said.
Reference
Kuperman E et al. The Virtual Hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. Journal of Hospital Medicine. Published online first 2018 Sep 26. doi: 10.12788/jhm.3061. Accessed 2018 Oct 2.
Medicare-for-All gets first legislative hearing
Medicare-for-All – the health care proposal that could play a key role in the 2020 presidential elections – got its first airing on Capitol Hill April 30 as the House Rules Committee discussed H.R. 1384.
The Medicare for All Act of 2019, introduced Feb. 27 by Rep. Pramila Jayapal (D-Wash.) and Rep. Debbie Dingell (D-Mich.), would provide universal coverage at the time of birth in the United States or upon the establishment of residency. The bill would make it unlawful for a private health insurer to sell coverage that duplicates the benefits of the Medicare-for-All system, and would prohibit employers from providing health insurance coverage that is provided by the Medicare-for-All system. At press time, the bill currently had 108 cosponsors, all Democrats.
Given the challenges the bill will face getting through the Democrat-controlled House – and the likelihood that the Republican-controlled Senate won’t even touch it – one Rules Committee member questioned why the hearing was being held.
Rep. Debbie Lesko (D-Ariz.) acknowledged that there are problems with health care and called for bipartisanship, noting problems of this magnitude need both sides of the aisle working together, but said she does not think H.R. 1384 has any chance of passage.
“Most, if not all, Republicans in the House are probably going to vote against it if it gets up for a vote and certainly the Senate is not going to hear it,” Rep. Lesko said. “I don’t know why we are doing this.”
Witnesses called by the committee offered differing takes on whether Medicare-for-All is feasible in the United States.
“A Medicare-for-All system of the type envisioned in the Jayapal bill is a huge step from our current system, which relies largely on private insurers,” according to Dean Baker, PhD, senior economist at the Center for Economic and Policy Research. “The list of transition problems that would arise is too long to address here. However, I would argue that it is essential that any move to such a system be done piecemeal since a quick changeover would virtually guarantee confusion and quite possibly lead to some people going without care.”
Indeed, many ideas contained in a number of different Medicare-for-All proposals could be implemented “without a major reorganization of the health care system,” according to Sara Collins, PhD, vice president of health care coverage and access at The Commonwealth Fund. “For example, paying providers in commercial plans at prices closer to those in Medicare or allowing the secretary of Health and Human Services to negotiate prescription drug prices have potential to slow health care cost growth and would not require an immediate shift to a single-payer system.
“On the other hand,” she continued, “moving piecemeal also involves trade-offs including the possibility, based on the experience of the [Affordable Care Act], that additional steps may take some time to achieve.”
Grace-Marie Turner, president of the Galen Institute, noted that many people, regardless of whether their coverage is public or private or not at all, have frustrations with the current health care delivery system.
“But it is hard to see how consumers would be more empowered when dealing with a single government payer,” she said. “In a country that values diversity, will one program with one list of benefits and set of rules work for everyone?”
If physician payment under Medicare-for-All were closer to what Medicare currently pays, “physicians would see 30% cuts. These payment reductions would gradually grow over time,” Ms. Turner testified.
Despite discussion of pay cuts, doctors invited to testify spoke in favor of a single-payer system.
“All I want is to practice medicine in a world where I no longer have to watch a patient walk out of the ER without medical care that could save their life because they are worried about going bankrupt,” said Farzon Nahvi, MD, an emergency physician at New York University Medical Center who serves on the board of directors for the New York Metro chapter of Physicians for a National Health Program. “From my perspective on the ground, the solution has to involve approaching medical care in just the same way we approach educating our children, maintaining our roads, and supporting our troops. This means treating health care like any other public good and creating a universal health care system like Medicare-for-All so that when they’re at their most vulnerable, my patients never have to make any consideration except to simply do what they need to do in order to get better.”
Doris Browne, MD, immediate past president of the National Medical Association agreed, calling for the adoption of “a system of universal coverage that minimizes administrative medical costs. It does not matter what label is used. Such an undertaking must include preventive care, screening, early detection, and treatment. The coverage would allow patients the ability to chose their provider, primary care or specialist. Care should be the same no matter where you live, rural or urban, California or Mississippi, and not be restricted based on language, age, gender, or race/ethnicity.”
Rep. Jim McGovern (D-Mass.), chairman of the Rules Committee, wrapped up the hearing noting that, even with some dissenting viewpoints, “what we have shown today, I believe, is that Medicare-for-All is possible; that we can build on the principles of the Affordable Care Act to make even bolder reforms. Reforms that would give doctors like Dr. Browne and Dr. Nahvi the ability to treat patients and give them the best care every time without letting cost dictate medical decisions. ... If you walk away with nothing else today, know that we have the ability to do that. Medicare-for-All is possible. It is reasonable. It can move forward and I think it should.”
Medicare-for-All – the health care proposal that could play a key role in the 2020 presidential elections – got its first airing on Capitol Hill April 30 as the House Rules Committee discussed H.R. 1384.
The Medicare for All Act of 2019, introduced Feb. 27 by Rep. Pramila Jayapal (D-Wash.) and Rep. Debbie Dingell (D-Mich.), would provide universal coverage at the time of birth in the United States or upon the establishment of residency. The bill would make it unlawful for a private health insurer to sell coverage that duplicates the benefits of the Medicare-for-All system, and would prohibit employers from providing health insurance coverage that is provided by the Medicare-for-All system. At press time, the bill currently had 108 cosponsors, all Democrats.
Given the challenges the bill will face getting through the Democrat-controlled House – and the likelihood that the Republican-controlled Senate won’t even touch it – one Rules Committee member questioned why the hearing was being held.
Rep. Debbie Lesko (D-Ariz.) acknowledged that there are problems with health care and called for bipartisanship, noting problems of this magnitude need both sides of the aisle working together, but said she does not think H.R. 1384 has any chance of passage.
“Most, if not all, Republicans in the House are probably going to vote against it if it gets up for a vote and certainly the Senate is not going to hear it,” Rep. Lesko said. “I don’t know why we are doing this.”
Witnesses called by the committee offered differing takes on whether Medicare-for-All is feasible in the United States.
“A Medicare-for-All system of the type envisioned in the Jayapal bill is a huge step from our current system, which relies largely on private insurers,” according to Dean Baker, PhD, senior economist at the Center for Economic and Policy Research. “The list of transition problems that would arise is too long to address here. However, I would argue that it is essential that any move to such a system be done piecemeal since a quick changeover would virtually guarantee confusion and quite possibly lead to some people going without care.”
Indeed, many ideas contained in a number of different Medicare-for-All proposals could be implemented “without a major reorganization of the health care system,” according to Sara Collins, PhD, vice president of health care coverage and access at The Commonwealth Fund. “For example, paying providers in commercial plans at prices closer to those in Medicare or allowing the secretary of Health and Human Services to negotiate prescription drug prices have potential to slow health care cost growth and would not require an immediate shift to a single-payer system.
“On the other hand,” she continued, “moving piecemeal also involves trade-offs including the possibility, based on the experience of the [Affordable Care Act], that additional steps may take some time to achieve.”
Grace-Marie Turner, president of the Galen Institute, noted that many people, regardless of whether their coverage is public or private or not at all, have frustrations with the current health care delivery system.
“But it is hard to see how consumers would be more empowered when dealing with a single government payer,” she said. “In a country that values diversity, will one program with one list of benefits and set of rules work for everyone?”
If physician payment under Medicare-for-All were closer to what Medicare currently pays, “physicians would see 30% cuts. These payment reductions would gradually grow over time,” Ms. Turner testified.
Despite discussion of pay cuts, doctors invited to testify spoke in favor of a single-payer system.
“All I want is to practice medicine in a world where I no longer have to watch a patient walk out of the ER without medical care that could save their life because they are worried about going bankrupt,” said Farzon Nahvi, MD, an emergency physician at New York University Medical Center who serves on the board of directors for the New York Metro chapter of Physicians for a National Health Program. “From my perspective on the ground, the solution has to involve approaching medical care in just the same way we approach educating our children, maintaining our roads, and supporting our troops. This means treating health care like any other public good and creating a universal health care system like Medicare-for-All so that when they’re at their most vulnerable, my patients never have to make any consideration except to simply do what they need to do in order to get better.”
Doris Browne, MD, immediate past president of the National Medical Association agreed, calling for the adoption of “a system of universal coverage that minimizes administrative medical costs. It does not matter what label is used. Such an undertaking must include preventive care, screening, early detection, and treatment. The coverage would allow patients the ability to chose their provider, primary care or specialist. Care should be the same no matter where you live, rural or urban, California or Mississippi, and not be restricted based on language, age, gender, or race/ethnicity.”
Rep. Jim McGovern (D-Mass.), chairman of the Rules Committee, wrapped up the hearing noting that, even with some dissenting viewpoints, “what we have shown today, I believe, is that Medicare-for-All is possible; that we can build on the principles of the Affordable Care Act to make even bolder reforms. Reforms that would give doctors like Dr. Browne and Dr. Nahvi the ability to treat patients and give them the best care every time without letting cost dictate medical decisions. ... If you walk away with nothing else today, know that we have the ability to do that. Medicare-for-All is possible. It is reasonable. It can move forward and I think it should.”
Medicare-for-All – the health care proposal that could play a key role in the 2020 presidential elections – got its first airing on Capitol Hill April 30 as the House Rules Committee discussed H.R. 1384.
The Medicare for All Act of 2019, introduced Feb. 27 by Rep. Pramila Jayapal (D-Wash.) and Rep. Debbie Dingell (D-Mich.), would provide universal coverage at the time of birth in the United States or upon the establishment of residency. The bill would make it unlawful for a private health insurer to sell coverage that duplicates the benefits of the Medicare-for-All system, and would prohibit employers from providing health insurance coverage that is provided by the Medicare-for-All system. At press time, the bill currently had 108 cosponsors, all Democrats.
Given the challenges the bill will face getting through the Democrat-controlled House – and the likelihood that the Republican-controlled Senate won’t even touch it – one Rules Committee member questioned why the hearing was being held.
Rep. Debbie Lesko (D-Ariz.) acknowledged that there are problems with health care and called for bipartisanship, noting problems of this magnitude need both sides of the aisle working together, but said she does not think H.R. 1384 has any chance of passage.
“Most, if not all, Republicans in the House are probably going to vote against it if it gets up for a vote and certainly the Senate is not going to hear it,” Rep. Lesko said. “I don’t know why we are doing this.”
Witnesses called by the committee offered differing takes on whether Medicare-for-All is feasible in the United States.
“A Medicare-for-All system of the type envisioned in the Jayapal bill is a huge step from our current system, which relies largely on private insurers,” according to Dean Baker, PhD, senior economist at the Center for Economic and Policy Research. “The list of transition problems that would arise is too long to address here. However, I would argue that it is essential that any move to such a system be done piecemeal since a quick changeover would virtually guarantee confusion and quite possibly lead to some people going without care.”
Indeed, many ideas contained in a number of different Medicare-for-All proposals could be implemented “without a major reorganization of the health care system,” according to Sara Collins, PhD, vice president of health care coverage and access at The Commonwealth Fund. “For example, paying providers in commercial plans at prices closer to those in Medicare or allowing the secretary of Health and Human Services to negotiate prescription drug prices have potential to slow health care cost growth and would not require an immediate shift to a single-payer system.
“On the other hand,” she continued, “moving piecemeal also involves trade-offs including the possibility, based on the experience of the [Affordable Care Act], that additional steps may take some time to achieve.”
Grace-Marie Turner, president of the Galen Institute, noted that many people, regardless of whether their coverage is public or private or not at all, have frustrations with the current health care delivery system.
“But it is hard to see how consumers would be more empowered when dealing with a single government payer,” she said. “In a country that values diversity, will one program with one list of benefits and set of rules work for everyone?”
If physician payment under Medicare-for-All were closer to what Medicare currently pays, “physicians would see 30% cuts. These payment reductions would gradually grow over time,” Ms. Turner testified.
Despite discussion of pay cuts, doctors invited to testify spoke in favor of a single-payer system.
“All I want is to practice medicine in a world where I no longer have to watch a patient walk out of the ER without medical care that could save their life because they are worried about going bankrupt,” said Farzon Nahvi, MD, an emergency physician at New York University Medical Center who serves on the board of directors for the New York Metro chapter of Physicians for a National Health Program. “From my perspective on the ground, the solution has to involve approaching medical care in just the same way we approach educating our children, maintaining our roads, and supporting our troops. This means treating health care like any other public good and creating a universal health care system like Medicare-for-All so that when they’re at their most vulnerable, my patients never have to make any consideration except to simply do what they need to do in order to get better.”
Doris Browne, MD, immediate past president of the National Medical Association agreed, calling for the adoption of “a system of universal coverage that minimizes administrative medical costs. It does not matter what label is used. Such an undertaking must include preventive care, screening, early detection, and treatment. The coverage would allow patients the ability to chose their provider, primary care or specialist. Care should be the same no matter where you live, rural or urban, California or Mississippi, and not be restricted based on language, age, gender, or race/ethnicity.”
Rep. Jim McGovern (D-Mass.), chairman of the Rules Committee, wrapped up the hearing noting that, even with some dissenting viewpoints, “what we have shown today, I believe, is that Medicare-for-All is possible; that we can build on the principles of the Affordable Care Act to make even bolder reforms. Reforms that would give doctors like Dr. Browne and Dr. Nahvi the ability to treat patients and give them the best care every time without letting cost dictate medical decisions. ... If you walk away with nothing else today, know that we have the ability to do that. Medicare-for-All is possible. It is reasonable. It can move forward and I think it should.”
REPORTING FROM THE HOUSE RULES COMMITTEE
Out-of-pocket costs for neurologic medications rise sharply
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
FROM NEUROLOGY
Empty words, Captain Bacteria, and the perils of vampire facials
And now, 37 words from our sponsor
If you’re looking for gluten-free news of the health and medical sciences that’s low in sugar, we here at LOTME Farms promise to use no artificial colors or flavors to tell you about a study of the health claims on cereal boxes.
Researchers identified 37 such claims that appeared on the boxes of 460 different breakfast cereals and grouped them into four categories: adding positives (high fiber, probiotics), not adding negatives (GMO free, no high-fructose corn syrup), removing negatives (low cholesterol, no trans fat), and not removing positives (made with whole grains, fresh).
What they found is that words matter: None of the 37 claims explicitly said that the product inside would make people healthier or help them lose weight, but that was how respondents interpreted them. There is, of course, a reason none of the products claimed to improve health. “The correlation between the type of ‘healthy’ claim made and the actual nutritional quality of the breakfast cereal was almost zero,” investigator Pierre Chandon said.
This is, perhaps, not such a surprise. But we here at the pure, all-natural LOTME deal with facts, which are low in calories and contain no artificial growth hormones, and we would never insult (NEW LOTME LIGHT! NO ARTIFICIAL SWEETENERS!) our wholesome, low-fat readers by resorting (TRY FRESH LOTME ORGANIC!) to hyperbole or doublespeak. Not a chance (MMM … HOMEMADE LOTME).
Now, who’s up for a bowl of Froot Loops?
Captain Bacteria: Civil War
In the never-ending struggle of bacteria versus the world, Clostridium difficile has become a particularly stubborn foe. It is far more likely to be resistant to antibiotics, and the antibiotics that can do the job are either incredibly expensive or destroy the patient’s entire microbiota. However, we may have a new ally in the fight against C. diff: other bacteria.
Specifically, we’re talking about fecal transplants. According to an article published in the Journal of the American Osteopathic Association, the wide variety of bacteria that get transferred into the body along with the poop can block C. diff’s ability to germinate and produce the toxins that affect the human body. The treatment is especially beneficial for patients with C. diff whose microbiotas have been compromised by some other treatment, like chemotherapy, antibiotics, or proton pump inhibitors.
We here at LOTME would like to take a moment to salute the brave bacteria in our guts, fighting the good fight against those who would do us harm, and to the fecal transplants that let our own bacteria join the battle. Poop, you never let us down!
Dracula side effects
The Kim Kardashian effect is having dire ramifications. Back in 2013, the social media influencer posted a photo of herself getting a “vampire facial” – a dermatologic procedure in which a person’s own blood is injected into their face as a way to freshen and rejuvenate their skin. At least they aren’t drinking it.
Vampire facials have skyrocketed in popularity since, despite the ick factor. Unfortunately, it seems to be as dangerous as an encounter with a real vampire: Recently, two people in New Mexico were diagnosed with HIV after getting vampire facials.
The New Mexico Department of Health noted that both cases have been traced to the same spa, which was shut down in 2018 after at least three government agencies noted its lack of attention to hygiene and cleanliness. Warning to all: Just because a Kardashian does it doesn’t mean you should, too.
Shave that beard, Fido
The adage “a dog’s mouth is cleaner than a person’s” is getting an upgrade and this time it’s backed by science. A clinic in Zurich looked at the pathogenic microorganisms that reside in men’s beards and dogs’ fur and guess what – the beards were dirtier.
Despite beards’ manly cache among Millennials and hipsters, the results many have some reaching for the razor. The clinicians took a look at the bacterial load of colony-forming units of human-pathogenic microorganisms, and compared samples of beards and dog’s necks (since dogs don’t have beards, but how cute would that be?). They found high microbial counts in all beard samples, but only 23 of 30 dogs’ hair samples. Half of the human subjects carried so much bacteria that they were in danger of illness, the researchers noted.
Does this mean men are dirty? Or are dogs clean? The clinicians didn’t survey the men on their habits so it could be likely that they spend lots of time rolling around in the grass or drinking water from the toilet. More research is definitely needed here.
And now, 37 words from our sponsor
If you’re looking for gluten-free news of the health and medical sciences that’s low in sugar, we here at LOTME Farms promise to use no artificial colors or flavors to tell you about a study of the health claims on cereal boxes.
Researchers identified 37 such claims that appeared on the boxes of 460 different breakfast cereals and grouped them into four categories: adding positives (high fiber, probiotics), not adding negatives (GMO free, no high-fructose corn syrup), removing negatives (low cholesterol, no trans fat), and not removing positives (made with whole grains, fresh).
What they found is that words matter: None of the 37 claims explicitly said that the product inside would make people healthier or help them lose weight, but that was how respondents interpreted them. There is, of course, a reason none of the products claimed to improve health. “The correlation between the type of ‘healthy’ claim made and the actual nutritional quality of the breakfast cereal was almost zero,” investigator Pierre Chandon said.
This is, perhaps, not such a surprise. But we here at the pure, all-natural LOTME deal with facts, which are low in calories and contain no artificial growth hormones, and we would never insult (NEW LOTME LIGHT! NO ARTIFICIAL SWEETENERS!) our wholesome, low-fat readers by resorting (TRY FRESH LOTME ORGANIC!) to hyperbole or doublespeak. Not a chance (MMM … HOMEMADE LOTME).
Now, who’s up for a bowl of Froot Loops?
Captain Bacteria: Civil War
In the never-ending struggle of bacteria versus the world, Clostridium difficile has become a particularly stubborn foe. It is far more likely to be resistant to antibiotics, and the antibiotics that can do the job are either incredibly expensive or destroy the patient’s entire microbiota. However, we may have a new ally in the fight against C. diff: other bacteria.
Specifically, we’re talking about fecal transplants. According to an article published in the Journal of the American Osteopathic Association, the wide variety of bacteria that get transferred into the body along with the poop can block C. diff’s ability to germinate and produce the toxins that affect the human body. The treatment is especially beneficial for patients with C. diff whose microbiotas have been compromised by some other treatment, like chemotherapy, antibiotics, or proton pump inhibitors.
We here at LOTME would like to take a moment to salute the brave bacteria in our guts, fighting the good fight against those who would do us harm, and to the fecal transplants that let our own bacteria join the battle. Poop, you never let us down!
Dracula side effects
The Kim Kardashian effect is having dire ramifications. Back in 2013, the social media influencer posted a photo of herself getting a “vampire facial” – a dermatologic procedure in which a person’s own blood is injected into their face as a way to freshen and rejuvenate their skin. At least they aren’t drinking it.
Vampire facials have skyrocketed in popularity since, despite the ick factor. Unfortunately, it seems to be as dangerous as an encounter with a real vampire: Recently, two people in New Mexico were diagnosed with HIV after getting vampire facials.
The New Mexico Department of Health noted that both cases have been traced to the same spa, which was shut down in 2018 after at least three government agencies noted its lack of attention to hygiene and cleanliness. Warning to all: Just because a Kardashian does it doesn’t mean you should, too.
Shave that beard, Fido
The adage “a dog’s mouth is cleaner than a person’s” is getting an upgrade and this time it’s backed by science. A clinic in Zurich looked at the pathogenic microorganisms that reside in men’s beards and dogs’ fur and guess what – the beards were dirtier.
Despite beards’ manly cache among Millennials and hipsters, the results many have some reaching for the razor. The clinicians took a look at the bacterial load of colony-forming units of human-pathogenic microorganisms, and compared samples of beards and dog’s necks (since dogs don’t have beards, but how cute would that be?). They found high microbial counts in all beard samples, but only 23 of 30 dogs’ hair samples. Half of the human subjects carried so much bacteria that they were in danger of illness, the researchers noted.
Does this mean men are dirty? Or are dogs clean? The clinicians didn’t survey the men on their habits so it could be likely that they spend lots of time rolling around in the grass or drinking water from the toilet. More research is definitely needed here.
And now, 37 words from our sponsor
If you’re looking for gluten-free news of the health and medical sciences that’s low in sugar, we here at LOTME Farms promise to use no artificial colors or flavors to tell you about a study of the health claims on cereal boxes.
Researchers identified 37 such claims that appeared on the boxes of 460 different breakfast cereals and grouped them into four categories: adding positives (high fiber, probiotics), not adding negatives (GMO free, no high-fructose corn syrup), removing negatives (low cholesterol, no trans fat), and not removing positives (made with whole grains, fresh).
What they found is that words matter: None of the 37 claims explicitly said that the product inside would make people healthier or help them lose weight, but that was how respondents interpreted them. There is, of course, a reason none of the products claimed to improve health. “The correlation between the type of ‘healthy’ claim made and the actual nutritional quality of the breakfast cereal was almost zero,” investigator Pierre Chandon said.
This is, perhaps, not such a surprise. But we here at the pure, all-natural LOTME deal with facts, which are low in calories and contain no artificial growth hormones, and we would never insult (NEW LOTME LIGHT! NO ARTIFICIAL SWEETENERS!) our wholesome, low-fat readers by resorting (TRY FRESH LOTME ORGANIC!) to hyperbole or doublespeak. Not a chance (MMM … HOMEMADE LOTME).
Now, who’s up for a bowl of Froot Loops?
Captain Bacteria: Civil War
In the never-ending struggle of bacteria versus the world, Clostridium difficile has become a particularly stubborn foe. It is far more likely to be resistant to antibiotics, and the antibiotics that can do the job are either incredibly expensive or destroy the patient’s entire microbiota. However, we may have a new ally in the fight against C. diff: other bacteria.
Specifically, we’re talking about fecal transplants. According to an article published in the Journal of the American Osteopathic Association, the wide variety of bacteria that get transferred into the body along with the poop can block C. diff’s ability to germinate and produce the toxins that affect the human body. The treatment is especially beneficial for patients with C. diff whose microbiotas have been compromised by some other treatment, like chemotherapy, antibiotics, or proton pump inhibitors.
We here at LOTME would like to take a moment to salute the brave bacteria in our guts, fighting the good fight against those who would do us harm, and to the fecal transplants that let our own bacteria join the battle. Poop, you never let us down!
Dracula side effects
The Kim Kardashian effect is having dire ramifications. Back in 2013, the social media influencer posted a photo of herself getting a “vampire facial” – a dermatologic procedure in which a person’s own blood is injected into their face as a way to freshen and rejuvenate their skin. At least they aren’t drinking it.
Vampire facials have skyrocketed in popularity since, despite the ick factor. Unfortunately, it seems to be as dangerous as an encounter with a real vampire: Recently, two people in New Mexico were diagnosed with HIV after getting vampire facials.
The New Mexico Department of Health noted that both cases have been traced to the same spa, which was shut down in 2018 after at least three government agencies noted its lack of attention to hygiene and cleanliness. Warning to all: Just because a Kardashian does it doesn’t mean you should, too.
Shave that beard, Fido
The adage “a dog’s mouth is cleaner than a person’s” is getting an upgrade and this time it’s backed by science. A clinic in Zurich looked at the pathogenic microorganisms that reside in men’s beards and dogs’ fur and guess what – the beards were dirtier.
Despite beards’ manly cache among Millennials and hipsters, the results many have some reaching for the razor. The clinicians took a look at the bacterial load of colony-forming units of human-pathogenic microorganisms, and compared samples of beards and dog’s necks (since dogs don’t have beards, but how cute would that be?). They found high microbial counts in all beard samples, but only 23 of 30 dogs’ hair samples. Half of the human subjects carried so much bacteria that they were in danger of illness, the researchers noted.
Does this mean men are dirty? Or are dogs clean? The clinicians didn’t survey the men on their habits so it could be likely that they spend lots of time rolling around in the grass or drinking water from the toilet. More research is definitely needed here.