User login
Lymphoma rate in RA patients is falling
MAUI, HAWAII – The incidence of lymphoma in patients with RA appears to have been dropping during the past 2 decades – and for rheumatologists, that’s news you can use.
“I think this is encouraging data about where we’re headed with therapy. And it’s encouraging data for your patients, that maybe more effective therapies can lead to a lower risk of cancer,” John J. Cush, MD, commented at the 2019 Rheumatology Winter Clinical Symposium.
“Patients are always worried about cancer,” observed symposium director Arthur Kavanaugh, MD. “I think this is very useful data to bring to a discussion with patients.”
The study they highlighted was presented at the 2018 annual meeting of the American College of Rheumatology by Namrata Singh, MD, of the University of Iowa, Iowa City and coinvestigators from Veterans Affairs medical centers around the country. They analyzed the incidence of lymphomas as well as all-site cancers in 50,870 men with RA in the national VA health care system during 2001-2015 and compared the rates with the background rates in the general U.S. population as captured in the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program.
The key finding: While the standardized incidence ratio for the development of lymphoma in the RA patients during 2001-2005 was 190% greater than in the SEER population, the SIR dropped to 1.6 in 2006-2010 and stayed low in 2011-2015.
“These are the only data I’m aware of that say maybe lymphomas are becoming less frequent among RA patients,” said Dr. Kavanaugh, professor of medicine at the University of California, San Diego.
Historically, RA has been associated with roughly a 100% increased risk of lymphoma. The source of the increased risk has been a matter of controversy: Is it the result of immunostimulation triggered by high RA disease activity, or a side effect of the drugs employed in treatment of the disease? The clear implication of the VA study is that it’s all about disease activity.
“The lymphoma rate is higher early in the use of our new therapies, in 2001-2005, because the patients who went on TNF [tumor necrosis factor] inhibitors then had the most disease activity. But with time, patients are getting those treatments earlier. Does this [lower lymphoma rate] reflect a change in the practice of rheumatology? I think it does,” according to Dr. Cush, professor of medicine and rheumatology at Baylor University Medical Center, Dallas.
Dr. Kavanaugh agreed. “Now, if we’re treating early and treating to target, we should see less lymphomas than we did back in the day.”
The rate of cancers at all sites in the VA RA patients has been going down as well, with the SIR dropping from 1.8 in 2001-2005 to close to 1, the background rate in the general population.
“What’s great about this study is this is a large data set. You really can’t compare an RA population on and off treatment. The right comparison is to a normal population – and SEER accounts for something like 14% of the U.S. population,” Dr. Cush said.
Previous support for the notion that the increased lymphoma risk associated with RA was a function of disease activity came from a Swedish study of 378 RA patients in the prebiologic era who developed lymphoma and a matched cohort of 378 others without lymphoma. The investigators found that patients with moderate overall RA disease activity were at a 700% increased risk of lymphoma, compared with those with low overall disease activity, and that patients with high RA disease activity were at a 6,900% increased risk (Arthritis Rheum. 2006 Mar;54[3]:692-701). But that was a cross-sectional study, whereas the VA study examined trends over time.
The VA RA cohort had a mean age of 64 years. About 60% were current or ex-smokers, 65% were positive for rheumatoid factor, and 62% were positive for anticyclic citrullinated peptide.
Dr. Kavanaugh said that, because of the potential for referral bias in the VA study, he’s eager to see the findings reproduced in another data set.
Both Dr. Cush and Dr. Kavanaugh reported serving as a consultant to and/or receiving research funding from numerous pharmaceutical companies.
MAUI, HAWAII – The incidence of lymphoma in patients with RA appears to have been dropping during the past 2 decades – and for rheumatologists, that’s news you can use.
“I think this is encouraging data about where we’re headed with therapy. And it’s encouraging data for your patients, that maybe more effective therapies can lead to a lower risk of cancer,” John J. Cush, MD, commented at the 2019 Rheumatology Winter Clinical Symposium.
“Patients are always worried about cancer,” observed symposium director Arthur Kavanaugh, MD. “I think this is very useful data to bring to a discussion with patients.”
The study they highlighted was presented at the 2018 annual meeting of the American College of Rheumatology by Namrata Singh, MD, of the University of Iowa, Iowa City and coinvestigators from Veterans Affairs medical centers around the country. They analyzed the incidence of lymphomas as well as all-site cancers in 50,870 men with RA in the national VA health care system during 2001-2015 and compared the rates with the background rates in the general U.S. population as captured in the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program.
The key finding: While the standardized incidence ratio for the development of lymphoma in the RA patients during 2001-2005 was 190% greater than in the SEER population, the SIR dropped to 1.6 in 2006-2010 and stayed low in 2011-2015.
“These are the only data I’m aware of that say maybe lymphomas are becoming less frequent among RA patients,” said Dr. Kavanaugh, professor of medicine at the University of California, San Diego.
Historically, RA has been associated with roughly a 100% increased risk of lymphoma. The source of the increased risk has been a matter of controversy: Is it the result of immunostimulation triggered by high RA disease activity, or a side effect of the drugs employed in treatment of the disease? The clear implication of the VA study is that it’s all about disease activity.
“The lymphoma rate is higher early in the use of our new therapies, in 2001-2005, because the patients who went on TNF [tumor necrosis factor] inhibitors then had the most disease activity. But with time, patients are getting those treatments earlier. Does this [lower lymphoma rate] reflect a change in the practice of rheumatology? I think it does,” according to Dr. Cush, professor of medicine and rheumatology at Baylor University Medical Center, Dallas.
Dr. Kavanaugh agreed. “Now, if we’re treating early and treating to target, we should see less lymphomas than we did back in the day.”
The rate of cancers at all sites in the VA RA patients has been going down as well, with the SIR dropping from 1.8 in 2001-2005 to close to 1, the background rate in the general population.
“What’s great about this study is this is a large data set. You really can’t compare an RA population on and off treatment. The right comparison is to a normal population – and SEER accounts for something like 14% of the U.S. population,” Dr. Cush said.
Previous support for the notion that the increased lymphoma risk associated with RA was a function of disease activity came from a Swedish study of 378 RA patients in the prebiologic era who developed lymphoma and a matched cohort of 378 others without lymphoma. The investigators found that patients with moderate overall RA disease activity were at a 700% increased risk of lymphoma, compared with those with low overall disease activity, and that patients with high RA disease activity were at a 6,900% increased risk (Arthritis Rheum. 2006 Mar;54[3]:692-701). But that was a cross-sectional study, whereas the VA study examined trends over time.
The VA RA cohort had a mean age of 64 years. About 60% were current or ex-smokers, 65% were positive for rheumatoid factor, and 62% were positive for anticyclic citrullinated peptide.
Dr. Kavanaugh said that, because of the potential for referral bias in the VA study, he’s eager to see the findings reproduced in another data set.
Both Dr. Cush and Dr. Kavanaugh reported serving as a consultant to and/or receiving research funding from numerous pharmaceutical companies.
MAUI, HAWAII – The incidence of lymphoma in patients with RA appears to have been dropping during the past 2 decades – and for rheumatologists, that’s news you can use.
“I think this is encouraging data about where we’re headed with therapy. And it’s encouraging data for your patients, that maybe more effective therapies can lead to a lower risk of cancer,” John J. Cush, MD, commented at the 2019 Rheumatology Winter Clinical Symposium.
“Patients are always worried about cancer,” observed symposium director Arthur Kavanaugh, MD. “I think this is very useful data to bring to a discussion with patients.”
The study they highlighted was presented at the 2018 annual meeting of the American College of Rheumatology by Namrata Singh, MD, of the University of Iowa, Iowa City and coinvestigators from Veterans Affairs medical centers around the country. They analyzed the incidence of lymphomas as well as all-site cancers in 50,870 men with RA in the national VA health care system during 2001-2015 and compared the rates with the background rates in the general U.S. population as captured in the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program.
The key finding: While the standardized incidence ratio for the development of lymphoma in the RA patients during 2001-2005 was 190% greater than in the SEER population, the SIR dropped to 1.6 in 2006-2010 and stayed low in 2011-2015.
“These are the only data I’m aware of that say maybe lymphomas are becoming less frequent among RA patients,” said Dr. Kavanaugh, professor of medicine at the University of California, San Diego.
Historically, RA has been associated with roughly a 100% increased risk of lymphoma. The source of the increased risk has been a matter of controversy: Is it the result of immunostimulation triggered by high RA disease activity, or a side effect of the drugs employed in treatment of the disease? The clear implication of the VA study is that it’s all about disease activity.
“The lymphoma rate is higher early in the use of our new therapies, in 2001-2005, because the patients who went on TNF [tumor necrosis factor] inhibitors then had the most disease activity. But with time, patients are getting those treatments earlier. Does this [lower lymphoma rate] reflect a change in the practice of rheumatology? I think it does,” according to Dr. Cush, professor of medicine and rheumatology at Baylor University Medical Center, Dallas.
Dr. Kavanaugh agreed. “Now, if we’re treating early and treating to target, we should see less lymphomas than we did back in the day.”
The rate of cancers at all sites in the VA RA patients has been going down as well, with the SIR dropping from 1.8 in 2001-2005 to close to 1, the background rate in the general population.
“What’s great about this study is this is a large data set. You really can’t compare an RA population on and off treatment. The right comparison is to a normal population – and SEER accounts for something like 14% of the U.S. population,” Dr. Cush said.
Previous support for the notion that the increased lymphoma risk associated with RA was a function of disease activity came from a Swedish study of 378 RA patients in the prebiologic era who developed lymphoma and a matched cohort of 378 others without lymphoma. The investigators found that patients with moderate overall RA disease activity were at a 700% increased risk of lymphoma, compared with those with low overall disease activity, and that patients with high RA disease activity were at a 6,900% increased risk (Arthritis Rheum. 2006 Mar;54[3]:692-701). But that was a cross-sectional study, whereas the VA study examined trends over time.
The VA RA cohort had a mean age of 64 years. About 60% were current or ex-smokers, 65% were positive for rheumatoid factor, and 62% were positive for anticyclic citrullinated peptide.
Dr. Kavanaugh said that, because of the potential for referral bias in the VA study, he’s eager to see the findings reproduced in another data set.
Both Dr. Cush and Dr. Kavanaugh reported serving as a consultant to and/or receiving research funding from numerous pharmaceutical companies.
REPORTING FROM RWCS 2019
Systematic review: Patient navigation programs improve outcomes, have financial benefits
finds a systematic review.
The study, which was published in Cancer (2019 Apr 29. doi: 10.1002/cncr.32147) also found methodologic limitations and gaps in the research regarding cancer sites and steps in care, highlighting areas needing more focus.
The patient navigation model, introduced in 1990 to address poverty-related disparities in cancer care (Cancer. 2011;117(15 Suppl):3539-42), is now widely used in chronic illness management and has support from legislation as well as public and private funding. However, a 2011 review of patient navigation programs used in cancer care identified only 33 articles assessing impact and yielded mixed results, suggesting improvement in some out-comes but not others (CA Cancer J Clin. 2011;61:237-49), and there has been scant research on their cost-effectiveness.
Investigators led by Brittany M. Bernardo, MPH, Division of Population Sciences, Comprehensive Cancer Center, The Ohio State University, Columbus, Ohio, searched PubMed and EMBASE databases for studies investigating the efficacy and cost-effectiveness of patient navigation across the cancer continuum, with aims of summarizing their results, assessing quality, determining gaps, and identifying avenues for future research.
Ultimately, the investigators included 113 articles published between August 1, 2010, and February 1, 2018. A total of 14 reported on the cost-effectiveness of patient navigation programs.
Results reported in Cancer showed that the largest share of the articles focused on the effectiveness of patient navigation in screening (50%) and diagnosis (27%), while few focused on treatment (15%), survivorship (9%), clinical trial enrollment (2 articles), and prevention (1 article). With respect to cancer site, the majority of programs pertained to breast cancer (52%) and colorectal cancer (51%).
Overall, studies reported patient navigation programs had positive outcomes. For example, they improved uptake of and adherence to cancer screenings, timely diagnostic resolution and follow-up, completion rates for cancer therapy, and rates of attending medical appointments.
The 14 studies focusing on cost-effectiveness suggested that patient navigation programs had financial benefits as well. Two found that the programs generated net revenue for clinics and hospitals. Programs additionally reduced medical treatment costs, improved life expectancy and quality-adjusted life-years, and decreased health care use.
When the quality of studies was assessed with the Quality Assessment Tool for Quantitative Studies, just 5% had strong methodology (having no weak components) and 30% had moderate methodology (having 1 weak component), while 65% had weak methodology (greater than or equal to 2 weak components).
“[Patient navigation] continues to be an effective method for overcoming barriers to care and should be integrated into more health care systems,” Ms. Bernardo and coinvestigators concluded. “With the encouraging results of this review and past reviews, it is hoped that new research will be conducted to fill in the remaining gaps and further elucidate the benefits of [patient navigation] in health care.”
One investigator disclosed having grant funding from the Merck Foundation and being a stockholder in Pfizer and a member of the American Cancer Society Patient Navigation Round Table; the other investigators made no disclosures. The study was supported by the Susan G. Komen Foundation and the Bradley Charles Cooper Foundation.
SOURCE: Bernardo BM et al. Cancer. 2019 Apr 29. doi: 10.1002/cncr.32147.
finds a systematic review.
The study, which was published in Cancer (2019 Apr 29. doi: 10.1002/cncr.32147) also found methodologic limitations and gaps in the research regarding cancer sites and steps in care, highlighting areas needing more focus.
The patient navigation model, introduced in 1990 to address poverty-related disparities in cancer care (Cancer. 2011;117(15 Suppl):3539-42), is now widely used in chronic illness management and has support from legislation as well as public and private funding. However, a 2011 review of patient navigation programs used in cancer care identified only 33 articles assessing impact and yielded mixed results, suggesting improvement in some out-comes but not others (CA Cancer J Clin. 2011;61:237-49), and there has been scant research on their cost-effectiveness.
Investigators led by Brittany M. Bernardo, MPH, Division of Population Sciences, Comprehensive Cancer Center, The Ohio State University, Columbus, Ohio, searched PubMed and EMBASE databases for studies investigating the efficacy and cost-effectiveness of patient navigation across the cancer continuum, with aims of summarizing their results, assessing quality, determining gaps, and identifying avenues for future research.
Ultimately, the investigators included 113 articles published between August 1, 2010, and February 1, 2018. A total of 14 reported on the cost-effectiveness of patient navigation programs.
Results reported in Cancer showed that the largest share of the articles focused on the effectiveness of patient navigation in screening (50%) and diagnosis (27%), while few focused on treatment (15%), survivorship (9%), clinical trial enrollment (2 articles), and prevention (1 article). With respect to cancer site, the majority of programs pertained to breast cancer (52%) and colorectal cancer (51%).
Overall, studies reported patient navigation programs had positive outcomes. For example, they improved uptake of and adherence to cancer screenings, timely diagnostic resolution and follow-up, completion rates for cancer therapy, and rates of attending medical appointments.
The 14 studies focusing on cost-effectiveness suggested that patient navigation programs had financial benefits as well. Two found that the programs generated net revenue for clinics and hospitals. Programs additionally reduced medical treatment costs, improved life expectancy and quality-adjusted life-years, and decreased health care use.
When the quality of studies was assessed with the Quality Assessment Tool for Quantitative Studies, just 5% had strong methodology (having no weak components) and 30% had moderate methodology (having 1 weak component), while 65% had weak methodology (greater than or equal to 2 weak components).
“[Patient navigation] continues to be an effective method for overcoming barriers to care and should be integrated into more health care systems,” Ms. Bernardo and coinvestigators concluded. “With the encouraging results of this review and past reviews, it is hoped that new research will be conducted to fill in the remaining gaps and further elucidate the benefits of [patient navigation] in health care.”
One investigator disclosed having grant funding from the Merck Foundation and being a stockholder in Pfizer and a member of the American Cancer Society Patient Navigation Round Table; the other investigators made no disclosures. The study was supported by the Susan G. Komen Foundation and the Bradley Charles Cooper Foundation.
SOURCE: Bernardo BM et al. Cancer. 2019 Apr 29. doi: 10.1002/cncr.32147.
finds a systematic review.
The study, which was published in Cancer (2019 Apr 29. doi: 10.1002/cncr.32147) also found methodologic limitations and gaps in the research regarding cancer sites and steps in care, highlighting areas needing more focus.
The patient navigation model, introduced in 1990 to address poverty-related disparities in cancer care (Cancer. 2011;117(15 Suppl):3539-42), is now widely used in chronic illness management and has support from legislation as well as public and private funding. However, a 2011 review of patient navigation programs used in cancer care identified only 33 articles assessing impact and yielded mixed results, suggesting improvement in some out-comes but not others (CA Cancer J Clin. 2011;61:237-49), and there has been scant research on their cost-effectiveness.
Investigators led by Brittany M. Bernardo, MPH, Division of Population Sciences, Comprehensive Cancer Center, The Ohio State University, Columbus, Ohio, searched PubMed and EMBASE databases for studies investigating the efficacy and cost-effectiveness of patient navigation across the cancer continuum, with aims of summarizing their results, assessing quality, determining gaps, and identifying avenues for future research.
Ultimately, the investigators included 113 articles published between August 1, 2010, and February 1, 2018. A total of 14 reported on the cost-effectiveness of patient navigation programs.
Results reported in Cancer showed that the largest share of the articles focused on the effectiveness of patient navigation in screening (50%) and diagnosis (27%), while few focused on treatment (15%), survivorship (9%), clinical trial enrollment (2 articles), and prevention (1 article). With respect to cancer site, the majority of programs pertained to breast cancer (52%) and colorectal cancer (51%).
Overall, studies reported patient navigation programs had positive outcomes. For example, they improved uptake of and adherence to cancer screenings, timely diagnostic resolution and follow-up, completion rates for cancer therapy, and rates of attending medical appointments.
The 14 studies focusing on cost-effectiveness suggested that patient navigation programs had financial benefits as well. Two found that the programs generated net revenue for clinics and hospitals. Programs additionally reduced medical treatment costs, improved life expectancy and quality-adjusted life-years, and decreased health care use.
When the quality of studies was assessed with the Quality Assessment Tool for Quantitative Studies, just 5% had strong methodology (having no weak components) and 30% had moderate methodology (having 1 weak component), while 65% had weak methodology (greater than or equal to 2 weak components).
“[Patient navigation] continues to be an effective method for overcoming barriers to care and should be integrated into more health care systems,” Ms. Bernardo and coinvestigators concluded. “With the encouraging results of this review and past reviews, it is hoped that new research will be conducted to fill in the remaining gaps and further elucidate the benefits of [patient navigation] in health care.”
One investigator disclosed having grant funding from the Merck Foundation and being a stockholder in Pfizer and a member of the American Cancer Society Patient Navigation Round Table; the other investigators made no disclosures. The study was supported by the Susan G. Komen Foundation and the Bradley Charles Cooper Foundation.
SOURCE: Bernardo BM et al. Cancer. 2019 Apr 29. doi: 10.1002/cncr.32147.
FROM CANCER
Novel strategies may help curb bariatric SSI
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
REPORTING FROM SAGES 2019
Key clinical point: .
Major findings: The BariWound predictive model had an accuracy of area under the curve of 0.73; wound infection rates decreased from 6% to 1.3% after the change in practice.
Study details: Analysis of 274,187 cases from the 2015 MBSAQIP database; and a retrospective analysis of 333 bariatric cases performed from January 2016 to March 2018 at a single center.
Disclosures: Dr. Dang has no relationships to disclose. Dr. Weber has no disclosures, although coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
Sources: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
Neurodevelopmental concerns may emerge later in Zika-exposed infants
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
REPORTING FROM PAS 2019
Key clinical point: .
Major finding: Zika-exposed infants with normal fetal MRI neuroimaging showed increasingly lower mobility and social cognition skills as they approached their first birthday.
Study details: The findings are based on neurodevelopmental assessments of 72 Zika-exposed Colombian children at 4-18 months old.
Disclosures: The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
Marijuana during prenatal OUD treatment increases premature birth
BALTIMORE – Marijuana is a not a good idea during pregnancy, and it’s an even worse idea when women are being treated for opioid addiction, according to an investigation from East Tennessee State University, Mountain Home.
Marijuana use may become more common as legalization rolls out across the country, and legalization, in turn, may add to the perception that pot is harmless, and maybe a good way to take the edge off during pregnancy and prevent morning sickness, said neonatologist Darshan Shaw, MD, of the department of pediatrics at the university.
Dr. Shaw wondered how that trend might impact treatment of opioid use disorder (OUD) during pregnancy, which has also become more common. The take-home is that “if you have a pregnant patient on medically assistant therapy” for opioid addition, “you should warn them against use of marijuana. It increases the risk of prematurity and low birth weight,” he said at the Pediatric Academic Societies annual meeting.
He and his team reviewed 2,375 opioid-exposed pregnancies at six hospitals in south-central Appalachia from July 2011 to June 2016. All of the women had used opioids during pregnancy, some illegally and others for opioid use disorder (OUD) treatment or other medical issues; 108 had urine screens that were positive for tetrahydrocannabinol (THC) at the time of delivery.
Infants were born a mean of 3 days earlier in the marijuana group, and a mean of 265 g lighter. They were also more likely to be born before 37 weeks’ gestation (14% versus 6.5%); born weighing less than 2,500 g (17.6% versus 7.3%); and more likely to be admitted to the neonatal ICU (17.5% versus 7.1%).
On logistic regression to control for parity, maternal status, and tobacco and benzodiazepine use, prenatal marijuana exposure more than doubled the risk of prematurity (odds ratio, 2.35; 95% confidence interval, 1.3-4.23); tobacco and benzodiazepines did not increase the risk. Marijuana also doubled the risk of low birth weight (OR, 2.02; 95% CI, 1.18-3.47), about the same as tobacco and benzodiazepines.
The study had limitations. There was no controlling for a major confounder: the amount of opioids woman took while pregnant. These data were not available, Dr. Shaw said.
Neonatal abstinence syndrome was more common in the marijuana group (33.3% versus 18.1%), so it’s possible that women who used marijuana also used more opioids. “We suspect that opioid exposure was not uniform among all infants,” he said. There were also no data on the amount or way marijuana was used.
Marijuana-positive women were more likely to be unmarried, nulliparous, and use tobacco and benzodiazepines.
There was no industry funding for the work, and Dr. Shaw had no disclosures.
BALTIMORE – Marijuana is a not a good idea during pregnancy, and it’s an even worse idea when women are being treated for opioid addiction, according to an investigation from East Tennessee State University, Mountain Home.
Marijuana use may become more common as legalization rolls out across the country, and legalization, in turn, may add to the perception that pot is harmless, and maybe a good way to take the edge off during pregnancy and prevent morning sickness, said neonatologist Darshan Shaw, MD, of the department of pediatrics at the university.
Dr. Shaw wondered how that trend might impact treatment of opioid use disorder (OUD) during pregnancy, which has also become more common. The take-home is that “if you have a pregnant patient on medically assistant therapy” for opioid addition, “you should warn them against use of marijuana. It increases the risk of prematurity and low birth weight,” he said at the Pediatric Academic Societies annual meeting.
He and his team reviewed 2,375 opioid-exposed pregnancies at six hospitals in south-central Appalachia from July 2011 to June 2016. All of the women had used opioids during pregnancy, some illegally and others for opioid use disorder (OUD) treatment or other medical issues; 108 had urine screens that were positive for tetrahydrocannabinol (THC) at the time of delivery.
Infants were born a mean of 3 days earlier in the marijuana group, and a mean of 265 g lighter. They were also more likely to be born before 37 weeks’ gestation (14% versus 6.5%); born weighing less than 2,500 g (17.6% versus 7.3%); and more likely to be admitted to the neonatal ICU (17.5% versus 7.1%).
On logistic regression to control for parity, maternal status, and tobacco and benzodiazepine use, prenatal marijuana exposure more than doubled the risk of prematurity (odds ratio, 2.35; 95% confidence interval, 1.3-4.23); tobacco and benzodiazepines did not increase the risk. Marijuana also doubled the risk of low birth weight (OR, 2.02; 95% CI, 1.18-3.47), about the same as tobacco and benzodiazepines.
The study had limitations. There was no controlling for a major confounder: the amount of opioids woman took while pregnant. These data were not available, Dr. Shaw said.
Neonatal abstinence syndrome was more common in the marijuana group (33.3% versus 18.1%), so it’s possible that women who used marijuana also used more opioids. “We suspect that opioid exposure was not uniform among all infants,” he said. There were also no data on the amount or way marijuana was used.
Marijuana-positive women were more likely to be unmarried, nulliparous, and use tobacco and benzodiazepines.
There was no industry funding for the work, and Dr. Shaw had no disclosures.
BALTIMORE – Marijuana is a not a good idea during pregnancy, and it’s an even worse idea when women are being treated for opioid addiction, according to an investigation from East Tennessee State University, Mountain Home.
Marijuana use may become more common as legalization rolls out across the country, and legalization, in turn, may add to the perception that pot is harmless, and maybe a good way to take the edge off during pregnancy and prevent morning sickness, said neonatologist Darshan Shaw, MD, of the department of pediatrics at the university.
Dr. Shaw wondered how that trend might impact treatment of opioid use disorder (OUD) during pregnancy, which has also become more common. The take-home is that “if you have a pregnant patient on medically assistant therapy” for opioid addition, “you should warn them against use of marijuana. It increases the risk of prematurity and low birth weight,” he said at the Pediatric Academic Societies annual meeting.
He and his team reviewed 2,375 opioid-exposed pregnancies at six hospitals in south-central Appalachia from July 2011 to June 2016. All of the women had used opioids during pregnancy, some illegally and others for opioid use disorder (OUD) treatment or other medical issues; 108 had urine screens that were positive for tetrahydrocannabinol (THC) at the time of delivery.
Infants were born a mean of 3 days earlier in the marijuana group, and a mean of 265 g lighter. They were also more likely to be born before 37 weeks’ gestation (14% versus 6.5%); born weighing less than 2,500 g (17.6% versus 7.3%); and more likely to be admitted to the neonatal ICU (17.5% versus 7.1%).
On logistic regression to control for parity, maternal status, and tobacco and benzodiazepine use, prenatal marijuana exposure more than doubled the risk of prematurity (odds ratio, 2.35; 95% confidence interval, 1.3-4.23); tobacco and benzodiazepines did not increase the risk. Marijuana also doubled the risk of low birth weight (OR, 2.02; 95% CI, 1.18-3.47), about the same as tobacco and benzodiazepines.
The study had limitations. There was no controlling for a major confounder: the amount of opioids woman took while pregnant. These data were not available, Dr. Shaw said.
Neonatal abstinence syndrome was more common in the marijuana group (33.3% versus 18.1%), so it’s possible that women who used marijuana also used more opioids. “We suspect that opioid exposure was not uniform among all infants,” he said. There were also no data on the amount or way marijuana was used.
Marijuana-positive women were more likely to be unmarried, nulliparous, and use tobacco and benzodiazepines.
There was no industry funding for the work, and Dr. Shaw had no disclosures.
REPORTING FROM PAS 2019
Key clinical point: Warn pregnant women being treated for opioid use disorder to stay away from marijuana.
Major finding: Marijuana use more than doubled the risk of prematurity and low birth weight.
Study details: Review of 2,375 opioid-exposed pregnancies at six hospitals
Disclosures: There was no industry funding for the work, and the lead investigator had no disclosures.
VIDEO: Givosiran cuts acute intermittent porphyria attacks in pivotal trial
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
REPORTING FROM ILC 2019
Key clinical point: Givosiran cut acute hepatic porphyria attacks in its pivotal trial.
Major finding: Patients treated with givosiran had 74% fewer acute porphyria attacks, compared with patients on placebo.
Study details: ENVISION, an international pivotal trial with 94 patients.
Disclosures: ENVISION was funded by Alnylam, the company developing givosiran. Dr. Balwani has been an advisor to and has received research funding from Alnylam. The center where Dr. Balwani works, the Icahn School of Medicine at Mount Sinai, in New York, holds patents related to givosiran that it has licensed to Amnylam.
Source: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
Staging tool predicts post-RYGB complications
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
REPORTING FROM SAGES 2019
Key clinical point: The Edmonton Obesity Staging System is predictive of complications after Roux-en-Y gastric bypass surgery.
Major finding: Patients with a score greater than 3 had a threefold greater incidence of complications at 1 year.
Study details: Retrospective chart review of 378 patients who had RYGB at a single center from 2009 through 2015.
Disclosures: Mr. Skulsky has no financial relationships to disclose.
Source: Skulsky SL et al. SAGES 2018, Session SS12.
Long-term antibiotic use may heighten stroke, CHD risk
, according to a study in the European Heart Journal.
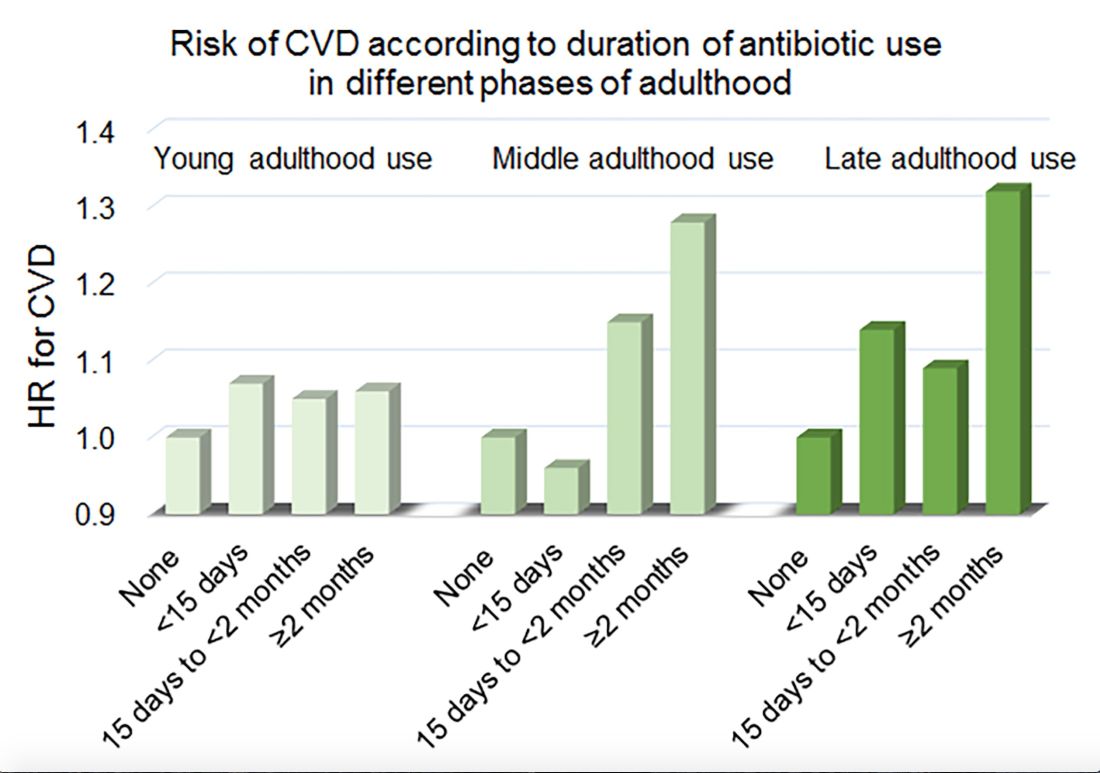
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
, according to a study in the European Heart Journal.
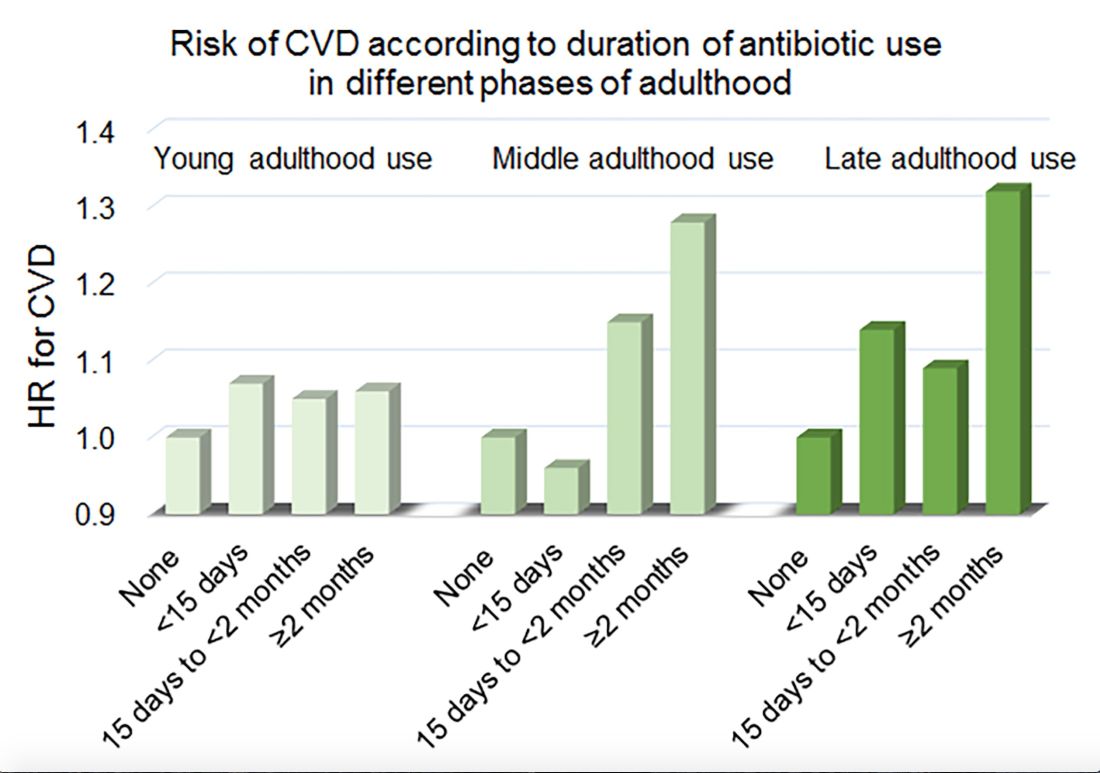
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
, according to a study in the European Heart Journal.
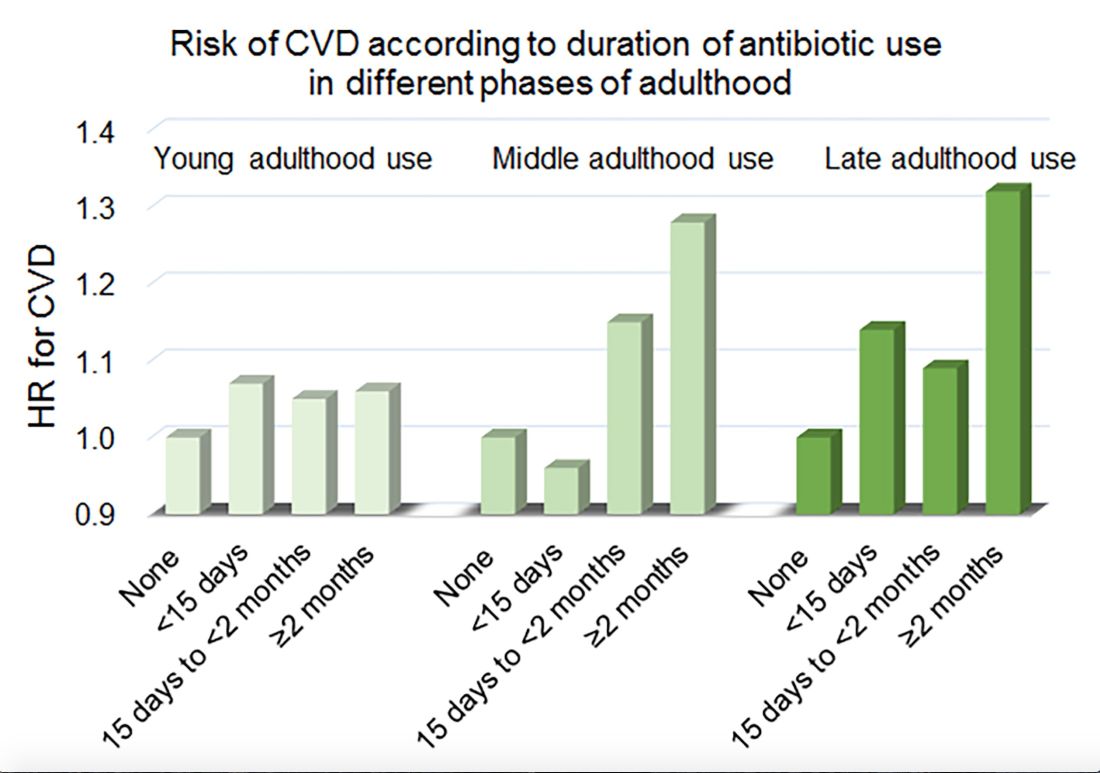
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
FROM THE EUROPEAN HEART JOURNAL
Key clinical point: Among middle-aged and older women, 2 or more months’ exposure to antibiotics is associated with an increased risk of coronary heart disease or stroke.
Major finding: Long-term antibiotic use in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Study details: An analysis of data from nearly 36,500 women in the Nurses’ Health Study.
Disclosures: The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
Source: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
Smoking found not protective against uveitis attacks in axSpA patients
Smoking does not appear to have protective effects against anterior uveitis attacks in patients with axial spondyloarthritis, according to prospective registry study data.
Both current and ex-smokers had increased uveitis rates versus never-smokers in the study, suggesting that the supposed protective effect of smoking found in previous axial spondyloarthritis studies was not causal, Sizheng Steven Zhao, MD, and his colleagues reported in the Annals of the Rheumatic Diseases.
“Spurious relationships can emerge when studies restrict to a disease population,” the researchers wrote.
The present analysis by Dr. Zhao and colleagues included 2,420 patients with axial spondyloarthritis in the British Society for Rheumatology Biologics Registry for Ankylosing Spondylitis. Of that group, 632 (26%) had a diagnosis of acute anterior uveitis over a total of 1,457 patient-years of follow-up.
Researchers looked specifically at the number of uveitis episodes per 12-month period, which ranged from 0 to 15 in the overall study cohort.
Current smokers had a 33% higher incidence of acute anterior uveitis episodes versus never-smokers, while ex-smokers had a 19% higher incidence, although the findings did not reach statistical significance, according to the researchers.
Because some studies have suggested that smoking may influence response to biologic therapy, Dr. Zhao and coinvestigators stratified patients into biologic and nonbiologic cohorts. In the biologic cohort, they found a 76% higher incidence per year of uveitis attacks for current smokers versus never-smokers, and a 29% increased incidence for ex-smokers versus never-smokers.
These findings are “consistent with increased risk of uveitis observed among smokers in the general population,” the researchers said. “Although nicotine may have anti-inflammatory properties, cigarette smoking is overall pro-inflammatory.”
Those results provide “yet another line of evidence” that should compel spondyloarthritis patients to quit smoking, the researchers added. Previous studies have suggested that smoking may increase radiographic progression and may reduce response to treatment.
The authors declared no competing interests. The registry study is supported by the British Society for Rheumatology, which has received funding from Pfizer, AbbVie, and UCB for the study.
SOURCE: Zhao SS et al. Ann Rheum Dis. 2019 Apr 20. doi: 10.1136/annrheumdis-2019-215348
Smoking does not appear to have protective effects against anterior uveitis attacks in patients with axial spondyloarthritis, according to prospective registry study data.
Both current and ex-smokers had increased uveitis rates versus never-smokers in the study, suggesting that the supposed protective effect of smoking found in previous axial spondyloarthritis studies was not causal, Sizheng Steven Zhao, MD, and his colleagues reported in the Annals of the Rheumatic Diseases.
“Spurious relationships can emerge when studies restrict to a disease population,” the researchers wrote.
The present analysis by Dr. Zhao and colleagues included 2,420 patients with axial spondyloarthritis in the British Society for Rheumatology Biologics Registry for Ankylosing Spondylitis. Of that group, 632 (26%) had a diagnosis of acute anterior uveitis over a total of 1,457 patient-years of follow-up.
Researchers looked specifically at the number of uveitis episodes per 12-month period, which ranged from 0 to 15 in the overall study cohort.
Current smokers had a 33% higher incidence of acute anterior uveitis episodes versus never-smokers, while ex-smokers had a 19% higher incidence, although the findings did not reach statistical significance, according to the researchers.
Because some studies have suggested that smoking may influence response to biologic therapy, Dr. Zhao and coinvestigators stratified patients into biologic and nonbiologic cohorts. In the biologic cohort, they found a 76% higher incidence per year of uveitis attacks for current smokers versus never-smokers, and a 29% increased incidence for ex-smokers versus never-smokers.
These findings are “consistent with increased risk of uveitis observed among smokers in the general population,” the researchers said. “Although nicotine may have anti-inflammatory properties, cigarette smoking is overall pro-inflammatory.”
Those results provide “yet another line of evidence” that should compel spondyloarthritis patients to quit smoking, the researchers added. Previous studies have suggested that smoking may increase radiographic progression and may reduce response to treatment.
The authors declared no competing interests. The registry study is supported by the British Society for Rheumatology, which has received funding from Pfizer, AbbVie, and UCB for the study.
SOURCE: Zhao SS et al. Ann Rheum Dis. 2019 Apr 20. doi: 10.1136/annrheumdis-2019-215348
Smoking does not appear to have protective effects against anterior uveitis attacks in patients with axial spondyloarthritis, according to prospective registry study data.
Both current and ex-smokers had increased uveitis rates versus never-smokers in the study, suggesting that the supposed protective effect of smoking found in previous axial spondyloarthritis studies was not causal, Sizheng Steven Zhao, MD, and his colleagues reported in the Annals of the Rheumatic Diseases.
“Spurious relationships can emerge when studies restrict to a disease population,” the researchers wrote.
The present analysis by Dr. Zhao and colleagues included 2,420 patients with axial spondyloarthritis in the British Society for Rheumatology Biologics Registry for Ankylosing Spondylitis. Of that group, 632 (26%) had a diagnosis of acute anterior uveitis over a total of 1,457 patient-years of follow-up.
Researchers looked specifically at the number of uveitis episodes per 12-month period, which ranged from 0 to 15 in the overall study cohort.
Current smokers had a 33% higher incidence of acute anterior uveitis episodes versus never-smokers, while ex-smokers had a 19% higher incidence, although the findings did not reach statistical significance, according to the researchers.
Because some studies have suggested that smoking may influence response to biologic therapy, Dr. Zhao and coinvestigators stratified patients into biologic and nonbiologic cohorts. In the biologic cohort, they found a 76% higher incidence per year of uveitis attacks for current smokers versus never-smokers, and a 29% increased incidence for ex-smokers versus never-smokers.
These findings are “consistent with increased risk of uveitis observed among smokers in the general population,” the researchers said. “Although nicotine may have anti-inflammatory properties, cigarette smoking is overall pro-inflammatory.”
Those results provide “yet another line of evidence” that should compel spondyloarthritis patients to quit smoking, the researchers added. Previous studies have suggested that smoking may increase radiographic progression and may reduce response to treatment.
The authors declared no competing interests. The registry study is supported by the British Society for Rheumatology, which has received funding from Pfizer, AbbVie, and UCB for the study.
SOURCE: Zhao SS et al. Ann Rheum Dis. 2019 Apr 20. doi: 10.1136/annrheumdis-2019-215348
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: Current smokers had a 33% higher incidence of acute anterior uveitis episodes versus never-smokers, while ex-smokers had a 19% higher incidence.
Study details: Analysis including 2,420 patients with axial spondyloarthritis in the British Society for Rheumatology Biologics Registry for Ankylosing Spondylitis.
Disclosures: The authors declared no competing interests. The study is supported by the British Society for Rheumatology, which has received funding from Pfizer, AbbVie, and UCB for the study.
Source: Zhao SS et al. Ann Rheum Dis. 2019 Apr 20. doi: 10.1136/annrheumdis-2019-215348.
Perceived Physical Functioning Predicts Mortality
Researchers from Erasmus University, The Netherlands, and Monash University, Australia, say theirs is the first study to determine the independent association of various measures of subjective health with mortality. Previously, few studies had showed an effect of physical functioning independent of other subjective measures.
The researchers evaluated data on 5,538 adults who took part in the Rotterdam Study and who were followed for a mean of 12 years. One-third had cardiovascular disease; 8% had chronic obstructive pulmonary disease, and 38% had joint problems.
The researchers investigated 6 different measures of subjective health and how they related to all-cause mortality. They conceptualized subjective health—often associated with health and well-being—as a continuum with physical functioning at one end and mental health at the other. Physical functioning included basic activities of daily living (BADL), such as eating and grooming. Instrumental activities of daily living (IADL) included the cognitive attributes of performing self-reliant daily tasks, such as meal preparation and shopping. The researchers assessed mental health with scales measuring positive and negative effects as well as somatic symptoms (the physical manifestations of dysthymia) and quality of life.
“Importantly,” the researchers say, any of those indicators is affected strongly by both physical and mental aspects of health. For example, physical and functional decline are related to higher scores on dysthymia questionnaires.
During 48,534 person-years of follow-up, 2,021 people died. Only impairment in physical functioning assessed by either self-report of BADL or IADL was related to mortality. Quality of life, positive affect, somatic symptoms, and negative affect did not predict mortality once self-rated physical functioning was accounted for.
Clinically speaking, the researchers say, it might be good to focus interventions aimed at improving survival on subjective indicators of physical well-being: in other words, activities of daily living and what it takes to perform them.
Researchers from Erasmus University, The Netherlands, and Monash University, Australia, say theirs is the first study to determine the independent association of various measures of subjective health with mortality. Previously, few studies had showed an effect of physical functioning independent of other subjective measures.
The researchers evaluated data on 5,538 adults who took part in the Rotterdam Study and who were followed for a mean of 12 years. One-third had cardiovascular disease; 8% had chronic obstructive pulmonary disease, and 38% had joint problems.
The researchers investigated 6 different measures of subjective health and how they related to all-cause mortality. They conceptualized subjective health—often associated with health and well-being—as a continuum with physical functioning at one end and mental health at the other. Physical functioning included basic activities of daily living (BADL), such as eating and grooming. Instrumental activities of daily living (IADL) included the cognitive attributes of performing self-reliant daily tasks, such as meal preparation and shopping. The researchers assessed mental health with scales measuring positive and negative effects as well as somatic symptoms (the physical manifestations of dysthymia) and quality of life.
“Importantly,” the researchers say, any of those indicators is affected strongly by both physical and mental aspects of health. For example, physical and functional decline are related to higher scores on dysthymia questionnaires.
During 48,534 person-years of follow-up, 2,021 people died. Only impairment in physical functioning assessed by either self-report of BADL or IADL was related to mortality. Quality of life, positive affect, somatic symptoms, and negative affect did not predict mortality once self-rated physical functioning was accounted for.
Clinically speaking, the researchers say, it might be good to focus interventions aimed at improving survival on subjective indicators of physical well-being: in other words, activities of daily living and what it takes to perform them.
Researchers from Erasmus University, The Netherlands, and Monash University, Australia, say theirs is the first study to determine the independent association of various measures of subjective health with mortality. Previously, few studies had showed an effect of physical functioning independent of other subjective measures.
The researchers evaluated data on 5,538 adults who took part in the Rotterdam Study and who were followed for a mean of 12 years. One-third had cardiovascular disease; 8% had chronic obstructive pulmonary disease, and 38% had joint problems.
The researchers investigated 6 different measures of subjective health and how they related to all-cause mortality. They conceptualized subjective health—often associated with health and well-being—as a continuum with physical functioning at one end and mental health at the other. Physical functioning included basic activities of daily living (BADL), such as eating and grooming. Instrumental activities of daily living (IADL) included the cognitive attributes of performing self-reliant daily tasks, such as meal preparation and shopping. The researchers assessed mental health with scales measuring positive and negative effects as well as somatic symptoms (the physical manifestations of dysthymia) and quality of life.
“Importantly,” the researchers say, any of those indicators is affected strongly by both physical and mental aspects of health. For example, physical and functional decline are related to higher scores on dysthymia questionnaires.
During 48,534 person-years of follow-up, 2,021 people died. Only impairment in physical functioning assessed by either self-report of BADL or IADL was related to mortality. Quality of life, positive affect, somatic symptoms, and negative affect did not predict mortality once self-rated physical functioning was accounted for.
Clinically speaking, the researchers say, it might be good to focus interventions aimed at improving survival on subjective indicators of physical well-being: in other words, activities of daily living and what it takes to perform them.














