User login
Are anti-TNF drugs safe for pregnant women with inflammatory bowel disease?
Yes, anti-tumor necrosis factor (anti-TNF) therapy for inflammatory bowel disease (IBD) can be continued during pregnancy.
IBD is often diagnosed and treated in women during their reproductive years. Consequently, these patients face important decisions about the management of their disease and the safety of their baby. Clinicians should be prepared to offer guidance by discussing the risks and benefits of anti-TNF agents with their pregnant patients who have IBD, as well as with those considering pregnancy.
STUDIES OF THE POTENTIAL RISKS
Anti-TNF agents are monoclonal antibodies. Infliximab, adalimumab, and golimumab are actively transported into the fetal circulation via the placenta, mainly during the second and third trimesters. Certolizumab crosses the placenta only by passive means, because it lacks the fragment crystallizable (Fc) region required for placental transfer.1
Effects on pregnancy outcomes
In a 2016 meta-analysis,2 of 1,242 pregnancies in women with IBD, 482 were in women on anti-TNF therapy. It found no statistically significant difference in rates of adverse pregnancy outcomes including congenital abnormality, preterm birth, and low birth weight.
A meta-analysis of 1,216 pregnant women with IBD found no statistically significant differences in rates of spontaneous or elective abortion, preterm birth, low birth weight, or congenital malformation in those on anti-TNF therapy vs controls.3
A systematic review of 58 studies including more than 1,500 pregnant women with IBD who were exposed to anti-TNF agents concluded that there was no association with adverse pregnancy outcomes such as spontaneous abortion, preterm delivery, stillbirth, low birth weight, congenital malformation, or infection.4
A retrospective cohort study of 66 pregnant patients with IBD from several centers in Spain found that anti-TNF or thiopurine therapy during pregnancy did not increase the risk of pregnancy complications or neonatal complications.5
Effects on newborns
Cord blood studies have shown that maternal use of infliximab and adalimumab results in a detectable serum level in newborns, while cord blood levels of certolizumab are much lower.1,6 In some studies, anti-TNF drugs were detectable in infants for up to 6 months after birth, whereas other studies found that detectable serum levels dropped soon after birth.1,7
Addressing concern about an increased risk of infection or dysfunctional immune development in newborns exposed to anti-TNF drugs in utero, a systematic review found no increased risk.4 A retrospective multicenter cohort study of 841 children also reported no association between in utero exposure to anti-TNF agents and risk of severe infection in the short term or long term (mean of 4 years).8 Additional studies are under way to determine long-term risk to the newborn.7
THE TORONTO CONSENSUS GUIDELINES
The Toronto consensus guidelines strongly recommend continuing anti-TNF therapy during pregnancy in women with IBD who began maintenance therapy before conception.6
If a patient strongly prefers to stop therapy during pregnancy to limit fetal exposure, the Toronto consensus recommends giving the last dose at 22 to 24 weeks of gestation. However, this should only be considered in patients whose IBD is in remission and at low risk of relapse.6,9
Although anti-TNF drugs may differ in terms of placental transfer, agents should not be switched in stable patients, as switching increases the risk of relapse.10
BENEFITS OF CONTINUING THERAPY
Active IBD poses a significantly greater risk to the mother and the baby than continuing anti-TNF therapy during pregnancy.1,7 The primary benefit of continuing therapy is to maintain disease remission.
Among women with active IBD at the time of conception, one-third will have improvement in disease activity during the course of their pregnancy, one-third will have no change, and one-third will have worsening of disease activity. But if IBD is in remission at the time of conception, it will remain in remission in nearly 80% of women during pregnancy.1
Women with active IBD are at increased risk of preterm delivery, low birth weight, and intrauterine growth restriction.1,2,5 Also, women with IBD have an increased risk of venous thromboembolism, particularly if they have active disease during pregnancy.1 Therefore, achieving and maintaining remission are vital in the management of the pregnant patient with IBD.
CONSIDERATIONS AFTER BIRTH: BREAST-FEEDING AND VACCINATION
Breast-feeding is considered safe. Minuscule amounts of infliximab or adalimumab are transferred in breast milk but are unlikely to result in systemic immune suppression in the infant.7
Live-attenuated vaccines should be avoided for the first 6 months in infants exposed to anti-TNF agents in utero.1,7,11 All other vaccines, including hepatitis B virus vaccine, should be given according to standard schedules.6
OUR RECOMMENDATIONS
The goal of managing IBD in women of reproductive age is to minimize the risk of adverse outcomes for both mother and baby. We recommend a team approach, working closely with a gastroenterologist and a high-risk-pregnancy obstetrician, if available.
Patients should continue anti-TNF therapy during pregnancy because evidence supports its safety. If a woman wants to stop therapy and is at low risk of relapse, we recommend giving the last dose at 22 to 24 weeks of gestation, then promptly resuming therapy postpartum.
Live-attenuated vaccines (eg, influenza, rotavirus) should be avoided for the first 6 months in babies born to mothers on anti-TNF therapy.
- Ananthakrishnan AN, Xavier RJ, Podolsky DK. Inflammatory Bowel Diseases: A Clinician’s Guide. Chichester, UK: Wiley; 2017. doi:10.1002/9781119077633
- Shihab Z, Yeomans ND, De Cruz P. Anti-tumour necrosis factor alpha therapies and inflammatory bowel disease pregnancy outcomes: a meta-analysis. J Crohns Colitis 2016; 10(8):979–988. doi:10.1093/ecco-jcc/jjv234
- Narula N, Al-Dabbagh, Dhillon A, Sands BE, Marshall JK. Anti-TNF alpha therapies are safe during pregnancy in women with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 2014; 20(10):1862–1869. doi:10.1097/MIB.0000000000000092
- Nielsen OH, Loftus EV Jr, Jess T. Safety of TNF-alpha inhibitors during IBD pregnancy: a systematic review. BMC Med 2013; 11:174. doi:10.1186/1741-7015-11-174
- Casanova MJ, Chaparro M, Domenech E, et al. Safety of thiopurines and anti-TNF-alpha drugs during pregnancy in patients with inflammatory bowel disease. Am J Gastroenterol 2013; 108(3):433–440. doi:10.1038/ajg.2012.430
- Nguyen GC, Seow CH, Maxwell C, et al; IBD in Pregnancy Consensus Group; Canadian Association of Gastroenterology. The Toronto consensus statements for the management of inflammatory bowel disease in pregnancy. Gastroenterology 2016; 150(3):734–757.e1. doi:10.1053/j.gastro.2015.12.003
- Gisbert JP, Chaparro, M. Safety of anti-TNF agents during pregnancy and breastfeeding in women with inflammatory bowel disease. Am J Gastroenterol 2013; 108(9):1426–1438. doi:10.1038/ajg.2013.171
- Chaparro M, Verreth A, Lobaton T, et al. Long-term safety of in utero exposure to anti-TNF alpha drugs for the treatment of inflammatory bowel disease: results from the multicenter European TEDDY Study. Am J Gastroenterol 2018; 113(3):396–403. doi:10.1038/ajg.2017.501
- de Lima A, Zelinkova Z, van der Ent C, Steegers EA, van der Woude CJ. Tailored anti-TNF therapy during pregnancy in patients with IBD: maternal and fetal safety. Gut 2016; 65(8):1261–1268. doi:10.1136/gutjnl-2015-309321
- Van Assche G, Vermeire S, Ballet V, et al. Switch to adalimumab in patients with Crohn’s disease controlled by maintenance infliximab: prospective randomised SWITCH trial. Gut 2012; 61(2):229–234. doi:10.1136/gutjnl-2011-300755
- Saha S. Medication management in the pregnant IBD patient. Am J Gastroenterol 2017; 112(5):667–669. doi:10.1038/ajg.2017.22
Yes, anti-tumor necrosis factor (anti-TNF) therapy for inflammatory bowel disease (IBD) can be continued during pregnancy.
IBD is often diagnosed and treated in women during their reproductive years. Consequently, these patients face important decisions about the management of their disease and the safety of their baby. Clinicians should be prepared to offer guidance by discussing the risks and benefits of anti-TNF agents with their pregnant patients who have IBD, as well as with those considering pregnancy.
STUDIES OF THE POTENTIAL RISKS
Anti-TNF agents are monoclonal antibodies. Infliximab, adalimumab, and golimumab are actively transported into the fetal circulation via the placenta, mainly during the second and third trimesters. Certolizumab crosses the placenta only by passive means, because it lacks the fragment crystallizable (Fc) region required for placental transfer.1
Effects on pregnancy outcomes
In a 2016 meta-analysis,2 of 1,242 pregnancies in women with IBD, 482 were in women on anti-TNF therapy. It found no statistically significant difference in rates of adverse pregnancy outcomes including congenital abnormality, preterm birth, and low birth weight.
A meta-analysis of 1,216 pregnant women with IBD found no statistically significant differences in rates of spontaneous or elective abortion, preterm birth, low birth weight, or congenital malformation in those on anti-TNF therapy vs controls.3
A systematic review of 58 studies including more than 1,500 pregnant women with IBD who were exposed to anti-TNF agents concluded that there was no association with adverse pregnancy outcomes such as spontaneous abortion, preterm delivery, stillbirth, low birth weight, congenital malformation, or infection.4
A retrospective cohort study of 66 pregnant patients with IBD from several centers in Spain found that anti-TNF or thiopurine therapy during pregnancy did not increase the risk of pregnancy complications or neonatal complications.5
Effects on newborns
Cord blood studies have shown that maternal use of infliximab and adalimumab results in a detectable serum level in newborns, while cord blood levels of certolizumab are much lower.1,6 In some studies, anti-TNF drugs were detectable in infants for up to 6 months after birth, whereas other studies found that detectable serum levels dropped soon after birth.1,7
Addressing concern about an increased risk of infection or dysfunctional immune development in newborns exposed to anti-TNF drugs in utero, a systematic review found no increased risk.4 A retrospective multicenter cohort study of 841 children also reported no association between in utero exposure to anti-TNF agents and risk of severe infection in the short term or long term (mean of 4 years).8 Additional studies are under way to determine long-term risk to the newborn.7
THE TORONTO CONSENSUS GUIDELINES
The Toronto consensus guidelines strongly recommend continuing anti-TNF therapy during pregnancy in women with IBD who began maintenance therapy before conception.6
If a patient strongly prefers to stop therapy during pregnancy to limit fetal exposure, the Toronto consensus recommends giving the last dose at 22 to 24 weeks of gestation. However, this should only be considered in patients whose IBD is in remission and at low risk of relapse.6,9
Although anti-TNF drugs may differ in terms of placental transfer, agents should not be switched in stable patients, as switching increases the risk of relapse.10
BENEFITS OF CONTINUING THERAPY
Active IBD poses a significantly greater risk to the mother and the baby than continuing anti-TNF therapy during pregnancy.1,7 The primary benefit of continuing therapy is to maintain disease remission.
Among women with active IBD at the time of conception, one-third will have improvement in disease activity during the course of their pregnancy, one-third will have no change, and one-third will have worsening of disease activity. But if IBD is in remission at the time of conception, it will remain in remission in nearly 80% of women during pregnancy.1
Women with active IBD are at increased risk of preterm delivery, low birth weight, and intrauterine growth restriction.1,2,5 Also, women with IBD have an increased risk of venous thromboembolism, particularly if they have active disease during pregnancy.1 Therefore, achieving and maintaining remission are vital in the management of the pregnant patient with IBD.
CONSIDERATIONS AFTER BIRTH: BREAST-FEEDING AND VACCINATION
Breast-feeding is considered safe. Minuscule amounts of infliximab or adalimumab are transferred in breast milk but are unlikely to result in systemic immune suppression in the infant.7
Live-attenuated vaccines should be avoided for the first 6 months in infants exposed to anti-TNF agents in utero.1,7,11 All other vaccines, including hepatitis B virus vaccine, should be given according to standard schedules.6
OUR RECOMMENDATIONS
The goal of managing IBD in women of reproductive age is to minimize the risk of adverse outcomes for both mother and baby. We recommend a team approach, working closely with a gastroenterologist and a high-risk-pregnancy obstetrician, if available.
Patients should continue anti-TNF therapy during pregnancy because evidence supports its safety. If a woman wants to stop therapy and is at low risk of relapse, we recommend giving the last dose at 22 to 24 weeks of gestation, then promptly resuming therapy postpartum.
Live-attenuated vaccines (eg, influenza, rotavirus) should be avoided for the first 6 months in babies born to mothers on anti-TNF therapy.
Yes, anti-tumor necrosis factor (anti-TNF) therapy for inflammatory bowel disease (IBD) can be continued during pregnancy.
IBD is often diagnosed and treated in women during their reproductive years. Consequently, these patients face important decisions about the management of their disease and the safety of their baby. Clinicians should be prepared to offer guidance by discussing the risks and benefits of anti-TNF agents with their pregnant patients who have IBD, as well as with those considering pregnancy.
STUDIES OF THE POTENTIAL RISKS
Anti-TNF agents are monoclonal antibodies. Infliximab, adalimumab, and golimumab are actively transported into the fetal circulation via the placenta, mainly during the second and third trimesters. Certolizumab crosses the placenta only by passive means, because it lacks the fragment crystallizable (Fc) region required for placental transfer.1
Effects on pregnancy outcomes
In a 2016 meta-analysis,2 of 1,242 pregnancies in women with IBD, 482 were in women on anti-TNF therapy. It found no statistically significant difference in rates of adverse pregnancy outcomes including congenital abnormality, preterm birth, and low birth weight.
A meta-analysis of 1,216 pregnant women with IBD found no statistically significant differences in rates of spontaneous or elective abortion, preterm birth, low birth weight, or congenital malformation in those on anti-TNF therapy vs controls.3
A systematic review of 58 studies including more than 1,500 pregnant women with IBD who were exposed to anti-TNF agents concluded that there was no association with adverse pregnancy outcomes such as spontaneous abortion, preterm delivery, stillbirth, low birth weight, congenital malformation, or infection.4
A retrospective cohort study of 66 pregnant patients with IBD from several centers in Spain found that anti-TNF or thiopurine therapy during pregnancy did not increase the risk of pregnancy complications or neonatal complications.5
Effects on newborns
Cord blood studies have shown that maternal use of infliximab and adalimumab results in a detectable serum level in newborns, while cord blood levels of certolizumab are much lower.1,6 In some studies, anti-TNF drugs were detectable in infants for up to 6 months after birth, whereas other studies found that detectable serum levels dropped soon after birth.1,7
Addressing concern about an increased risk of infection or dysfunctional immune development in newborns exposed to anti-TNF drugs in utero, a systematic review found no increased risk.4 A retrospective multicenter cohort study of 841 children also reported no association between in utero exposure to anti-TNF agents and risk of severe infection in the short term or long term (mean of 4 years).8 Additional studies are under way to determine long-term risk to the newborn.7
THE TORONTO CONSENSUS GUIDELINES
The Toronto consensus guidelines strongly recommend continuing anti-TNF therapy during pregnancy in women with IBD who began maintenance therapy before conception.6
If a patient strongly prefers to stop therapy during pregnancy to limit fetal exposure, the Toronto consensus recommends giving the last dose at 22 to 24 weeks of gestation. However, this should only be considered in patients whose IBD is in remission and at low risk of relapse.6,9
Although anti-TNF drugs may differ in terms of placental transfer, agents should not be switched in stable patients, as switching increases the risk of relapse.10
BENEFITS OF CONTINUING THERAPY
Active IBD poses a significantly greater risk to the mother and the baby than continuing anti-TNF therapy during pregnancy.1,7 The primary benefit of continuing therapy is to maintain disease remission.
Among women with active IBD at the time of conception, one-third will have improvement in disease activity during the course of their pregnancy, one-third will have no change, and one-third will have worsening of disease activity. But if IBD is in remission at the time of conception, it will remain in remission in nearly 80% of women during pregnancy.1
Women with active IBD are at increased risk of preterm delivery, low birth weight, and intrauterine growth restriction.1,2,5 Also, women with IBD have an increased risk of venous thromboembolism, particularly if they have active disease during pregnancy.1 Therefore, achieving and maintaining remission are vital in the management of the pregnant patient with IBD.
CONSIDERATIONS AFTER BIRTH: BREAST-FEEDING AND VACCINATION
Breast-feeding is considered safe. Minuscule amounts of infliximab or adalimumab are transferred in breast milk but are unlikely to result in systemic immune suppression in the infant.7
Live-attenuated vaccines should be avoided for the first 6 months in infants exposed to anti-TNF agents in utero.1,7,11 All other vaccines, including hepatitis B virus vaccine, should be given according to standard schedules.6
OUR RECOMMENDATIONS
The goal of managing IBD in women of reproductive age is to minimize the risk of adverse outcomes for both mother and baby. We recommend a team approach, working closely with a gastroenterologist and a high-risk-pregnancy obstetrician, if available.
Patients should continue anti-TNF therapy during pregnancy because evidence supports its safety. If a woman wants to stop therapy and is at low risk of relapse, we recommend giving the last dose at 22 to 24 weeks of gestation, then promptly resuming therapy postpartum.
Live-attenuated vaccines (eg, influenza, rotavirus) should be avoided for the first 6 months in babies born to mothers on anti-TNF therapy.
- Ananthakrishnan AN, Xavier RJ, Podolsky DK. Inflammatory Bowel Diseases: A Clinician’s Guide. Chichester, UK: Wiley; 2017. doi:10.1002/9781119077633
- Shihab Z, Yeomans ND, De Cruz P. Anti-tumour necrosis factor alpha therapies and inflammatory bowel disease pregnancy outcomes: a meta-analysis. J Crohns Colitis 2016; 10(8):979–988. doi:10.1093/ecco-jcc/jjv234
- Narula N, Al-Dabbagh, Dhillon A, Sands BE, Marshall JK. Anti-TNF alpha therapies are safe during pregnancy in women with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 2014; 20(10):1862–1869. doi:10.1097/MIB.0000000000000092
- Nielsen OH, Loftus EV Jr, Jess T. Safety of TNF-alpha inhibitors during IBD pregnancy: a systematic review. BMC Med 2013; 11:174. doi:10.1186/1741-7015-11-174
- Casanova MJ, Chaparro M, Domenech E, et al. Safety of thiopurines and anti-TNF-alpha drugs during pregnancy in patients with inflammatory bowel disease. Am J Gastroenterol 2013; 108(3):433–440. doi:10.1038/ajg.2012.430
- Nguyen GC, Seow CH, Maxwell C, et al; IBD in Pregnancy Consensus Group; Canadian Association of Gastroenterology. The Toronto consensus statements for the management of inflammatory bowel disease in pregnancy. Gastroenterology 2016; 150(3):734–757.e1. doi:10.1053/j.gastro.2015.12.003
- Gisbert JP, Chaparro, M. Safety of anti-TNF agents during pregnancy and breastfeeding in women with inflammatory bowel disease. Am J Gastroenterol 2013; 108(9):1426–1438. doi:10.1038/ajg.2013.171
- Chaparro M, Verreth A, Lobaton T, et al. Long-term safety of in utero exposure to anti-TNF alpha drugs for the treatment of inflammatory bowel disease: results from the multicenter European TEDDY Study. Am J Gastroenterol 2018; 113(3):396–403. doi:10.1038/ajg.2017.501
- de Lima A, Zelinkova Z, van der Ent C, Steegers EA, van der Woude CJ. Tailored anti-TNF therapy during pregnancy in patients with IBD: maternal and fetal safety. Gut 2016; 65(8):1261–1268. doi:10.1136/gutjnl-2015-309321
- Van Assche G, Vermeire S, Ballet V, et al. Switch to adalimumab in patients with Crohn’s disease controlled by maintenance infliximab: prospective randomised SWITCH trial. Gut 2012; 61(2):229–234. doi:10.1136/gutjnl-2011-300755
- Saha S. Medication management in the pregnant IBD patient. Am J Gastroenterol 2017; 112(5):667–669. doi:10.1038/ajg.2017.22
- Ananthakrishnan AN, Xavier RJ, Podolsky DK. Inflammatory Bowel Diseases: A Clinician’s Guide. Chichester, UK: Wiley; 2017. doi:10.1002/9781119077633
- Shihab Z, Yeomans ND, De Cruz P. Anti-tumour necrosis factor alpha therapies and inflammatory bowel disease pregnancy outcomes: a meta-analysis. J Crohns Colitis 2016; 10(8):979–988. doi:10.1093/ecco-jcc/jjv234
- Narula N, Al-Dabbagh, Dhillon A, Sands BE, Marshall JK. Anti-TNF alpha therapies are safe during pregnancy in women with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 2014; 20(10):1862–1869. doi:10.1097/MIB.0000000000000092
- Nielsen OH, Loftus EV Jr, Jess T. Safety of TNF-alpha inhibitors during IBD pregnancy: a systematic review. BMC Med 2013; 11:174. doi:10.1186/1741-7015-11-174
- Casanova MJ, Chaparro M, Domenech E, et al. Safety of thiopurines and anti-TNF-alpha drugs during pregnancy in patients with inflammatory bowel disease. Am J Gastroenterol 2013; 108(3):433–440. doi:10.1038/ajg.2012.430
- Nguyen GC, Seow CH, Maxwell C, et al; IBD in Pregnancy Consensus Group; Canadian Association of Gastroenterology. The Toronto consensus statements for the management of inflammatory bowel disease in pregnancy. Gastroenterology 2016; 150(3):734–757.e1. doi:10.1053/j.gastro.2015.12.003
- Gisbert JP, Chaparro, M. Safety of anti-TNF agents during pregnancy and breastfeeding in women with inflammatory bowel disease. Am J Gastroenterol 2013; 108(9):1426–1438. doi:10.1038/ajg.2013.171
- Chaparro M, Verreth A, Lobaton T, et al. Long-term safety of in utero exposure to anti-TNF alpha drugs for the treatment of inflammatory bowel disease: results from the multicenter European TEDDY Study. Am J Gastroenterol 2018; 113(3):396–403. doi:10.1038/ajg.2017.501
- de Lima A, Zelinkova Z, van der Ent C, Steegers EA, van der Woude CJ. Tailored anti-TNF therapy during pregnancy in patients with IBD: maternal and fetal safety. Gut 2016; 65(8):1261–1268. doi:10.1136/gutjnl-2015-309321
- Van Assche G, Vermeire S, Ballet V, et al. Switch to adalimumab in patients with Crohn’s disease controlled by maintenance infliximab: prospective randomised SWITCH trial. Gut 2012; 61(2):229–234. doi:10.1136/gutjnl-2011-300755
- Saha S. Medication management in the pregnant IBD patient. Am J Gastroenterol 2017; 112(5):667–669. doi:10.1038/ajg.2017.22
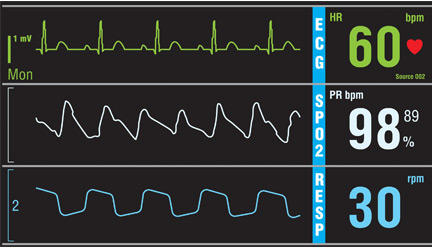
Do all hospital inpatients need cardiac telemetry?
No. Continuous monitoring for changes in heart rhythm with cardiac telemetry is recommended for all patients admitted to an intensive care unit (ICU). But routine telemetry monitoring for patients in non-ICU beds is not recommended, as it leads to unnecessary testing and treatment, increasing the cost of care and hospital length of stay.
RISK STRATIFICATION AND INDICATIONS
Telemetry is generally recommended for patients admitted with any type of heart disease, including:
- Acute myocardial infarction with ST-segment elevation or Q waves on 12-lead electrocardiography (ECG)
- Acute ischemia suggested by ST-segment depression or T-wave inversion on ECG
- Systolic blood pressure less than 100 mm Hg
- Acute decompensated heart failure with bilateral rales above the lung bases
- Chest pain that is worse than or the same as that in prior angina or myocardial infarction.1,2
Indications for telemetry are less clear in patients with no history of heart disease. The American Heart Association (AHA)3 has classified admitted patients based on the presence or absence of heart disease3:
- Class I (high risk of arrhythmia): acute coronary syndrome, new arrhythmia (eg, atrial fibrillation or flutter), severe electrolyte imbalance; telemetry is warranted
- Class II (moderate risk): acute decompensated heart failure with stable hemodynamic status, a surgical or medical diagnosis with underlying paced rhythms (ie, with a pacemaker), and chronic arrhythmia (atrial fibrillation or flutter); in these cases, telemetry monitoring may be considered
- Class III (low risk): no history of cardiac disease or arrhythmias, admitted for medical or surgical reasons; in these cases, telemetry is generally not indicated3
Telemetry should also be considered in patients admitted with syncope or stroke, critical illness, or palpitations.
Syncope and stroke
Despite the wide use of telemetry for patients admitted with syncope, current evidence does not support this practice. However, the AHA recommends routine telemetry for patients admitted with idiopathic syncope when there is a high level of suspicion for underlying cardiac arrhythmias as a cause of syncope (risk class II-b).3 In 30% of patients admitted with stroke or transient ischemic attack, the cause is cardioembolic. Therefore, telemetry is indicated to rule out an underlying cardiac cause.4
Critical illness
Patients hospitalized with major trauma, acute respiratory failure, sepsis, shock, or acute pulmonary embolism or for major noncardiac surgery (especially elderly patients with coronary artery disease or at high risk of coronary events) require cardiac telemetry (risk class I-b). Patients admitted with kidney failure, significant electrolyte abnormalities, drug or substance toxicity (especially with known arrhythmogenic drugs) also require cardiac telemetry at the time of admission (risk class I-b).
Recurrent palpitations, arrhythmia
Most patients with palpitations can be evaluated in an outpatient setting.5 However, patients hospitalized for recurrent palpitations or for suspected underlying cardiac disease require telemetric monitoring (risk class II-b).3 Patients with high-degree atrioventricular block admitted after percutaneous temporary pacemaker implantation should be monitored, as should patients with a permanent pacemaker for 12 to 24 hours after implantation (risk class I-c). Also, patients hospitalized after implantable cardioverter-defibrillator (ICD) shock need to be monitored.3,6
Patients with a paced rhythm who do not meet the above criteria do not require routine telemetric monitoring (risk class III-c).7
TELEMETRY IS OVERUSED
Off-site telemetry monitoring can identify significant arrhythmias during hospitalization. It also saves time on nursing staff to focus on bedside patient care. However, its convenience can lower the threshold for ordering it. This can lead to overuse with a major impact on healthcare costs.
Routine use of cardiac telemetry is associated with increased hospitalization costs with little benefit.8 The use of off-site services for continuous monitoring can activate many alarms throughout the day, triggering unnecessary workups and leading to densensitization to alarms (“alarm fatigue”).9
Despite the precise indications outlined in the AHA updated practice standards for inpatient electrocardiographic monitoring,10 telemetry use is expanding to non-ICU units without evidence of benefit,8 and this overuse can result in harmful clinical outcomes and a financial burden. Telemetry monitoring of low-risk patients can cause delays in emergency department and ICU admissions and transfers8,11 of patients who may be sicker and need intensive care.
In a prospective observational study,12 only 11 (6%) of 182 patients admitted to a general medical floor met AHA class I criteria for telemetry; very few patients developed a significant telemetry event such as atrial fibrillation or flutter that necessitated a change in management. Most overprescribers of telemetry monitoring reason that it will catch arrhythmias early.12 In fact, in a study of patients in a cardiac unit, telemetry detected just 50% of in-house cardiac arrest cases, with a potential survival benefit of only 0.02%.13
Another study showed that only 0.01% of all telemetry alarms represented a real emergency. Only 37.2% of emergency alarms were classified as clinically important, and only 48.3% of these led to a change in management within 1 hour.14
Moreover, in a report of trauma patients with abnormal results on ECG at the time of admission, telemetry had negligible clinical benefit.15 And in a study of 414 patients, only 4% of those admitted with chest pain and normal initial ECG had cardiac interventions.16
Another study8 showed that hospital intervention to restrict the use of telemetry guided by AHA recommendations resulted in a 43% reduction in telemetry orders, a 47% reduction in telemetry duration, and a 70% reduction in the mean daily number of patients monitored, with no changes in hospital census or rates of code blue, death, or rapid response team activation.8
The financial cost can be seen in the backup of patients in the emergency department. A study showed that 91% of patients being admitted for chest pain were delayed by more than 3 hours while waiting for monitored beds. This translated into an annual cost of $168,300 to the hospital.17 Adherence to guidelines for appropriate use of telemetry can significantly decrease costs. Applying a simple algorithm for telemetry use was shown8 to decrease daily non-ICU cardiac telemetry costs from $18,971 to $5,772.
CURRENT GUIDELINES ARE LIMITED
The current American College of Cardiology and AHA guidelines are based mostly on expert opinion rather than randomized clinical trials, while most telemetry trials have been performed on patients with a cardiac or possible cardiac diagnosis.3 Current guidelines need to be updated, and more studies are needed to specify the optimal duration of cardiac monitoring in indicated cases. Many noncardiac conditions raise a legitimate concern of dysrhythmia, an indication for cardiac monitoring, but precise recommendations for telemetry for such conditions are lacking.
RECOMMENDATIONS
Raising awareness of the clinical and financial burdens associated with unwise telemetry utilization is critical. We suggest use of a pop-up notification in the electronic medical record to remind the provider of the existing telemetry order and to specify the duration of telemetry monitoring when placing the initial order. The goal is to identify patients in true need of a telemetry bed, to decrease unnecessary testing, and to reduce hospitalization costs.
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol 1991; 18(6):1431–1433. pmid:1939942
- Goldman L, Cook EF, Johnson PA, Brand DA, Rouan GW, Lee TH. Prediction of the need for intensive care in patients who come to emergency departments with acute chest pain. N Engl J Med 1996; 334(23):1498–1504. doi:10.1056/NEJM199606063342303
- Drew BJ, Califf RM, Funk M, et al; American Heart Association; Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004;110(17):2721–2746. doi:10.1161/01.CIR.0000145144.56673.59
- Ustrell X, Pellise A. Cardiac workup of ischemic stroke. Curr Cardiol Rev 2010; 6(3):175-183. doi:10.2174/157340310791658721
- Olson JA, Fouts AM, Padanilam BJ, Prystowsky EN. Utility of mobile cardiac outpatient telemetry for the diagnosis of palpitations, presyncope, syncope, and the assessment of therapy efficacy. J Cardiovasc Electrophysiol 2007; 18(5):473–477. doi:10.1111/j.1540-8167.2007.00779.x
- Chen EH, Hollander JE. When do patients need admission to a telemetry bed? J Emerg Med 2007; 33(1):53–60. doi:10.1016/j.jemermed.2007.01.017
- Sandau KE, Funk M, Auerbach A, et al; American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Cardiovascular Disease in the Young. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med 2014; 174(11):1852–1854. doi:10.1001/jamainternmed.2014.4491
- Cantillon DJ, Loy M, Burkle A, et al. Association between off-site central monitoring using standardized cardiac telemetry and clinical outcomes among non–critically ill patients. JAMA 2016; 316(5):519–524. doi:10.1001/jama.2016.10258
- Sandau KE, Funk M, Auerbach A, et al. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GR, Lee CK. ALARMED: adverse events in low-risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study. Am J Emerg Med 2006; 24(1):62–67. doi:10.1016/j.ajem.2005.05.015
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med 2012; 172(17):1349–1350. doi:10.1001/archinternmed.2012.3163
- Schull MJ, Redelmeier DA. Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients. Acad Emerg Med 2000; 7(6):647–652. pmid:10905643
- Kansara P, Jackson K, Dressler R, et al. Potential of missing life-threatening arrhythmias after limiting the use of cardiac telemetry. JAMA Intern Med 2015; 175(8):1416–1418. doi:10.1001/jamainternmed.2015.2387
- Nagy KK, Krosner SM, Roberts RR, Joseph KT, Smith RF, Barrett J. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg 2001; 25(1):108–111. pmid:11213149
- Snider A, Papaleo M, Beldner S, et al. Is telemetry monitoring necessary in low-risk suspected acute chest pain syndromes? Chest 2002; 122(2):517–523. pmid:12171825
- Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med 2005; 45(2):110–117. doi:10.1016/j.annemergmed.2004.09.010
No. Continuous monitoring for changes in heart rhythm with cardiac telemetry is recommended for all patients admitted to an intensive care unit (ICU). But routine telemetry monitoring for patients in non-ICU beds is not recommended, as it leads to unnecessary testing and treatment, increasing the cost of care and hospital length of stay.
RISK STRATIFICATION AND INDICATIONS
Telemetry is generally recommended for patients admitted with any type of heart disease, including:
- Acute myocardial infarction with ST-segment elevation or Q waves on 12-lead electrocardiography (ECG)
- Acute ischemia suggested by ST-segment depression or T-wave inversion on ECG
- Systolic blood pressure less than 100 mm Hg
- Acute decompensated heart failure with bilateral rales above the lung bases
- Chest pain that is worse than or the same as that in prior angina or myocardial infarction.1,2
Indications for telemetry are less clear in patients with no history of heart disease. The American Heart Association (AHA)3 has classified admitted patients based on the presence or absence of heart disease3:
- Class I (high risk of arrhythmia): acute coronary syndrome, new arrhythmia (eg, atrial fibrillation or flutter), severe electrolyte imbalance; telemetry is warranted
- Class II (moderate risk): acute decompensated heart failure with stable hemodynamic status, a surgical or medical diagnosis with underlying paced rhythms (ie, with a pacemaker), and chronic arrhythmia (atrial fibrillation or flutter); in these cases, telemetry monitoring may be considered
- Class III (low risk): no history of cardiac disease or arrhythmias, admitted for medical or surgical reasons; in these cases, telemetry is generally not indicated3
Telemetry should also be considered in patients admitted with syncope or stroke, critical illness, or palpitations.
Syncope and stroke
Despite the wide use of telemetry for patients admitted with syncope, current evidence does not support this practice. However, the AHA recommends routine telemetry for patients admitted with idiopathic syncope when there is a high level of suspicion for underlying cardiac arrhythmias as a cause of syncope (risk class II-b).3 In 30% of patients admitted with stroke or transient ischemic attack, the cause is cardioembolic. Therefore, telemetry is indicated to rule out an underlying cardiac cause.4
Critical illness
Patients hospitalized with major trauma, acute respiratory failure, sepsis, shock, or acute pulmonary embolism or for major noncardiac surgery (especially elderly patients with coronary artery disease or at high risk of coronary events) require cardiac telemetry (risk class I-b). Patients admitted with kidney failure, significant electrolyte abnormalities, drug or substance toxicity (especially with known arrhythmogenic drugs) also require cardiac telemetry at the time of admission (risk class I-b).
Recurrent palpitations, arrhythmia
Most patients with palpitations can be evaluated in an outpatient setting.5 However, patients hospitalized for recurrent palpitations or for suspected underlying cardiac disease require telemetric monitoring (risk class II-b).3 Patients with high-degree atrioventricular block admitted after percutaneous temporary pacemaker implantation should be monitored, as should patients with a permanent pacemaker for 12 to 24 hours after implantation (risk class I-c). Also, patients hospitalized after implantable cardioverter-defibrillator (ICD) shock need to be monitored.3,6
Patients with a paced rhythm who do not meet the above criteria do not require routine telemetric monitoring (risk class III-c).7
TELEMETRY IS OVERUSED
Off-site telemetry monitoring can identify significant arrhythmias during hospitalization. It also saves time on nursing staff to focus on bedside patient care. However, its convenience can lower the threshold for ordering it. This can lead to overuse with a major impact on healthcare costs.
Routine use of cardiac telemetry is associated with increased hospitalization costs with little benefit.8 The use of off-site services for continuous monitoring can activate many alarms throughout the day, triggering unnecessary workups and leading to densensitization to alarms (“alarm fatigue”).9
Despite the precise indications outlined in the AHA updated practice standards for inpatient electrocardiographic monitoring,10 telemetry use is expanding to non-ICU units without evidence of benefit,8 and this overuse can result in harmful clinical outcomes and a financial burden. Telemetry monitoring of low-risk patients can cause delays in emergency department and ICU admissions and transfers8,11 of patients who may be sicker and need intensive care.
In a prospective observational study,12 only 11 (6%) of 182 patients admitted to a general medical floor met AHA class I criteria for telemetry; very few patients developed a significant telemetry event such as atrial fibrillation or flutter that necessitated a change in management. Most overprescribers of telemetry monitoring reason that it will catch arrhythmias early.12 In fact, in a study of patients in a cardiac unit, telemetry detected just 50% of in-house cardiac arrest cases, with a potential survival benefit of only 0.02%.13
Another study showed that only 0.01% of all telemetry alarms represented a real emergency. Only 37.2% of emergency alarms were classified as clinically important, and only 48.3% of these led to a change in management within 1 hour.14
Moreover, in a report of trauma patients with abnormal results on ECG at the time of admission, telemetry had negligible clinical benefit.15 And in a study of 414 patients, only 4% of those admitted with chest pain and normal initial ECG had cardiac interventions.16
Another study8 showed that hospital intervention to restrict the use of telemetry guided by AHA recommendations resulted in a 43% reduction in telemetry orders, a 47% reduction in telemetry duration, and a 70% reduction in the mean daily number of patients monitored, with no changes in hospital census or rates of code blue, death, or rapid response team activation.8
The financial cost can be seen in the backup of patients in the emergency department. A study showed that 91% of patients being admitted for chest pain were delayed by more than 3 hours while waiting for monitored beds. This translated into an annual cost of $168,300 to the hospital.17 Adherence to guidelines for appropriate use of telemetry can significantly decrease costs. Applying a simple algorithm for telemetry use was shown8 to decrease daily non-ICU cardiac telemetry costs from $18,971 to $5,772.
CURRENT GUIDELINES ARE LIMITED
The current American College of Cardiology and AHA guidelines are based mostly on expert opinion rather than randomized clinical trials, while most telemetry trials have been performed on patients with a cardiac or possible cardiac diagnosis.3 Current guidelines need to be updated, and more studies are needed to specify the optimal duration of cardiac monitoring in indicated cases. Many noncardiac conditions raise a legitimate concern of dysrhythmia, an indication for cardiac monitoring, but precise recommendations for telemetry for such conditions are lacking.
RECOMMENDATIONS
Raising awareness of the clinical and financial burdens associated with unwise telemetry utilization is critical. We suggest use of a pop-up notification in the electronic medical record to remind the provider of the existing telemetry order and to specify the duration of telemetry monitoring when placing the initial order. The goal is to identify patients in true need of a telemetry bed, to decrease unnecessary testing, and to reduce hospitalization costs.
No. Continuous monitoring for changes in heart rhythm with cardiac telemetry is recommended for all patients admitted to an intensive care unit (ICU). But routine telemetry monitoring for patients in non-ICU beds is not recommended, as it leads to unnecessary testing and treatment, increasing the cost of care and hospital length of stay.
RISK STRATIFICATION AND INDICATIONS
Telemetry is generally recommended for patients admitted with any type of heart disease, including:
- Acute myocardial infarction with ST-segment elevation or Q waves on 12-lead electrocardiography (ECG)
- Acute ischemia suggested by ST-segment depression or T-wave inversion on ECG
- Systolic blood pressure less than 100 mm Hg
- Acute decompensated heart failure with bilateral rales above the lung bases
- Chest pain that is worse than or the same as that in prior angina or myocardial infarction.1,2
Indications for telemetry are less clear in patients with no history of heart disease. The American Heart Association (AHA)3 has classified admitted patients based on the presence or absence of heart disease3:
- Class I (high risk of arrhythmia): acute coronary syndrome, new arrhythmia (eg, atrial fibrillation or flutter), severe electrolyte imbalance; telemetry is warranted
- Class II (moderate risk): acute decompensated heart failure with stable hemodynamic status, a surgical or medical diagnosis with underlying paced rhythms (ie, with a pacemaker), and chronic arrhythmia (atrial fibrillation or flutter); in these cases, telemetry monitoring may be considered
- Class III (low risk): no history of cardiac disease or arrhythmias, admitted for medical or surgical reasons; in these cases, telemetry is generally not indicated3
Telemetry should also be considered in patients admitted with syncope or stroke, critical illness, or palpitations.
Syncope and stroke
Despite the wide use of telemetry for patients admitted with syncope, current evidence does not support this practice. However, the AHA recommends routine telemetry for patients admitted with idiopathic syncope when there is a high level of suspicion for underlying cardiac arrhythmias as a cause of syncope (risk class II-b).3 In 30% of patients admitted with stroke or transient ischemic attack, the cause is cardioembolic. Therefore, telemetry is indicated to rule out an underlying cardiac cause.4
Critical illness
Patients hospitalized with major trauma, acute respiratory failure, sepsis, shock, or acute pulmonary embolism or for major noncardiac surgery (especially elderly patients with coronary artery disease or at high risk of coronary events) require cardiac telemetry (risk class I-b). Patients admitted with kidney failure, significant electrolyte abnormalities, drug or substance toxicity (especially with known arrhythmogenic drugs) also require cardiac telemetry at the time of admission (risk class I-b).
Recurrent palpitations, arrhythmia
Most patients with palpitations can be evaluated in an outpatient setting.5 However, patients hospitalized for recurrent palpitations or for suspected underlying cardiac disease require telemetric monitoring (risk class II-b).3 Patients with high-degree atrioventricular block admitted after percutaneous temporary pacemaker implantation should be monitored, as should patients with a permanent pacemaker for 12 to 24 hours after implantation (risk class I-c). Also, patients hospitalized after implantable cardioverter-defibrillator (ICD) shock need to be monitored.3,6
Patients with a paced rhythm who do not meet the above criteria do not require routine telemetric monitoring (risk class III-c).7
TELEMETRY IS OVERUSED
Off-site telemetry monitoring can identify significant arrhythmias during hospitalization. It also saves time on nursing staff to focus on bedside patient care. However, its convenience can lower the threshold for ordering it. This can lead to overuse with a major impact on healthcare costs.
Routine use of cardiac telemetry is associated with increased hospitalization costs with little benefit.8 The use of off-site services for continuous monitoring can activate many alarms throughout the day, triggering unnecessary workups and leading to densensitization to alarms (“alarm fatigue”).9
Despite the precise indications outlined in the AHA updated practice standards for inpatient electrocardiographic monitoring,10 telemetry use is expanding to non-ICU units without evidence of benefit,8 and this overuse can result in harmful clinical outcomes and a financial burden. Telemetry monitoring of low-risk patients can cause delays in emergency department and ICU admissions and transfers8,11 of patients who may be sicker and need intensive care.
In a prospective observational study,12 only 11 (6%) of 182 patients admitted to a general medical floor met AHA class I criteria for telemetry; very few patients developed a significant telemetry event such as atrial fibrillation or flutter that necessitated a change in management. Most overprescribers of telemetry monitoring reason that it will catch arrhythmias early.12 In fact, in a study of patients in a cardiac unit, telemetry detected just 50% of in-house cardiac arrest cases, with a potential survival benefit of only 0.02%.13
Another study showed that only 0.01% of all telemetry alarms represented a real emergency. Only 37.2% of emergency alarms were classified as clinically important, and only 48.3% of these led to a change in management within 1 hour.14
Moreover, in a report of trauma patients with abnormal results on ECG at the time of admission, telemetry had negligible clinical benefit.15 And in a study of 414 patients, only 4% of those admitted with chest pain and normal initial ECG had cardiac interventions.16
Another study8 showed that hospital intervention to restrict the use of telemetry guided by AHA recommendations resulted in a 43% reduction in telemetry orders, a 47% reduction in telemetry duration, and a 70% reduction in the mean daily number of patients monitored, with no changes in hospital census or rates of code blue, death, or rapid response team activation.8
The financial cost can be seen in the backup of patients in the emergency department. A study showed that 91% of patients being admitted for chest pain were delayed by more than 3 hours while waiting for monitored beds. This translated into an annual cost of $168,300 to the hospital.17 Adherence to guidelines for appropriate use of telemetry can significantly decrease costs. Applying a simple algorithm for telemetry use was shown8 to decrease daily non-ICU cardiac telemetry costs from $18,971 to $5,772.
CURRENT GUIDELINES ARE LIMITED
The current American College of Cardiology and AHA guidelines are based mostly on expert opinion rather than randomized clinical trials, while most telemetry trials have been performed on patients with a cardiac or possible cardiac diagnosis.3 Current guidelines need to be updated, and more studies are needed to specify the optimal duration of cardiac monitoring in indicated cases. Many noncardiac conditions raise a legitimate concern of dysrhythmia, an indication for cardiac monitoring, but precise recommendations for telemetry for such conditions are lacking.
RECOMMENDATIONS
Raising awareness of the clinical and financial burdens associated with unwise telemetry utilization is critical. We suggest use of a pop-up notification in the electronic medical record to remind the provider of the existing telemetry order and to specify the duration of telemetry monitoring when placing the initial order. The goal is to identify patients in true need of a telemetry bed, to decrease unnecessary testing, and to reduce hospitalization costs.
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol 1991; 18(6):1431–1433. pmid:1939942
- Goldman L, Cook EF, Johnson PA, Brand DA, Rouan GW, Lee TH. Prediction of the need for intensive care in patients who come to emergency departments with acute chest pain. N Engl J Med 1996; 334(23):1498–1504. doi:10.1056/NEJM199606063342303
- Drew BJ, Califf RM, Funk M, et al; American Heart Association; Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004;110(17):2721–2746. doi:10.1161/01.CIR.0000145144.56673.59
- Ustrell X, Pellise A. Cardiac workup of ischemic stroke. Curr Cardiol Rev 2010; 6(3):175-183. doi:10.2174/157340310791658721
- Olson JA, Fouts AM, Padanilam BJ, Prystowsky EN. Utility of mobile cardiac outpatient telemetry for the diagnosis of palpitations, presyncope, syncope, and the assessment of therapy efficacy. J Cardiovasc Electrophysiol 2007; 18(5):473–477. doi:10.1111/j.1540-8167.2007.00779.x
- Chen EH, Hollander JE. When do patients need admission to a telemetry bed? J Emerg Med 2007; 33(1):53–60. doi:10.1016/j.jemermed.2007.01.017
- Sandau KE, Funk M, Auerbach A, et al; American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Cardiovascular Disease in the Young. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med 2014; 174(11):1852–1854. doi:10.1001/jamainternmed.2014.4491
- Cantillon DJ, Loy M, Burkle A, et al. Association between off-site central monitoring using standardized cardiac telemetry and clinical outcomes among non–critically ill patients. JAMA 2016; 316(5):519–524. doi:10.1001/jama.2016.10258
- Sandau KE, Funk M, Auerbach A, et al. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GR, Lee CK. ALARMED: adverse events in low-risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study. Am J Emerg Med 2006; 24(1):62–67. doi:10.1016/j.ajem.2005.05.015
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med 2012; 172(17):1349–1350. doi:10.1001/archinternmed.2012.3163
- Schull MJ, Redelmeier DA. Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients. Acad Emerg Med 2000; 7(6):647–652. pmid:10905643
- Kansara P, Jackson K, Dressler R, et al. Potential of missing life-threatening arrhythmias after limiting the use of cardiac telemetry. JAMA Intern Med 2015; 175(8):1416–1418. doi:10.1001/jamainternmed.2015.2387
- Nagy KK, Krosner SM, Roberts RR, Joseph KT, Smith RF, Barrett J. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg 2001; 25(1):108–111. pmid:11213149
- Snider A, Papaleo M, Beldner S, et al. Is telemetry monitoring necessary in low-risk suspected acute chest pain syndromes? Chest 2002; 122(2):517–523. pmid:12171825
- Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med 2005; 45(2):110–117. doi:10.1016/j.annemergmed.2004.09.010
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol 1991; 18(6):1431–1433. pmid:1939942
- Goldman L, Cook EF, Johnson PA, Brand DA, Rouan GW, Lee TH. Prediction of the need for intensive care in patients who come to emergency departments with acute chest pain. N Engl J Med 1996; 334(23):1498–1504. doi:10.1056/NEJM199606063342303
- Drew BJ, Califf RM, Funk M, et al; American Heart Association; Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004;110(17):2721–2746. doi:10.1161/01.CIR.0000145144.56673.59
- Ustrell X, Pellise A. Cardiac workup of ischemic stroke. Curr Cardiol Rev 2010; 6(3):175-183. doi:10.2174/157340310791658721
- Olson JA, Fouts AM, Padanilam BJ, Prystowsky EN. Utility of mobile cardiac outpatient telemetry for the diagnosis of palpitations, presyncope, syncope, and the assessment of therapy efficacy. J Cardiovasc Electrophysiol 2007; 18(5):473–477. doi:10.1111/j.1540-8167.2007.00779.x
- Chen EH, Hollander JE. When do patients need admission to a telemetry bed? J Emerg Med 2007; 33(1):53–60. doi:10.1016/j.jemermed.2007.01.017
- Sandau KE, Funk M, Auerbach A, et al; American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Cardiovascular Disease in the Young. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med 2014; 174(11):1852–1854. doi:10.1001/jamainternmed.2014.4491
- Cantillon DJ, Loy M, Burkle A, et al. Association between off-site central monitoring using standardized cardiac telemetry and clinical outcomes among non–critically ill patients. JAMA 2016; 316(5):519–524. doi:10.1001/jama.2016.10258
- Sandau KE, Funk M, Auerbach A, et al. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation 2017; 136(19):e273–e344. doi:10.1161/CIR.0000000000000527
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GR, Lee CK. ALARMED: adverse events in low-risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study. Am J Emerg Med 2006; 24(1):62–67. doi:10.1016/j.ajem.2005.05.015
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med 2012; 172(17):1349–1350. doi:10.1001/archinternmed.2012.3163
- Schull MJ, Redelmeier DA. Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients. Acad Emerg Med 2000; 7(6):647–652. pmid:10905643
- Kansara P, Jackson K, Dressler R, et al. Potential of missing life-threatening arrhythmias after limiting the use of cardiac telemetry. JAMA Intern Med 2015; 175(8):1416–1418. doi:10.1001/jamainternmed.2015.2387
- Nagy KK, Krosner SM, Roberts RR, Joseph KT, Smith RF, Barrett J. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg 2001; 25(1):108–111. pmid:11213149
- Snider A, Papaleo M, Beldner S, et al. Is telemetry monitoring necessary in low-risk suspected acute chest pain syndromes? Chest 2002; 122(2):517–523. pmid:12171825
- Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med 2005; 45(2):110–117. doi:10.1016/j.annemergmed.2004.09.010
Telemedicine: Past, present, and future
Telemedicine has been used successfully to improve patient access to medical care while reducing healthcare costs. In 2016, an estimated 61% of US healthcare institutions and 40% to 50% of US hospitals used telemedicine.1 From 2012 to 2013, the telemedicine market grew by 60%. However, its widespread use has been limited by low reimbursement rates and interstate licensing and practice issues.
In this commentary, we discuss the history of telemedicine, current uses and challenges, and areas of future growth.
DEFINITION AND HISTORY
The World Health Organization defines telemedicine as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”2
Modern telemedicine began in the early 1900s in the Netherlands with the transmission of heart rhythms over the telephone,3 which was followed by transmissions to radio consultation centers in Europe in the 1920s. In the 1940s, radiographic images were transmitted by telephone between cities in Pennsylvania.4
Today, telemedicine is used in a variety of specialties including radiology, neurology, and pathology5 and by organizations in the United States ranging from the National Aeronautics and Space Administration and Kaiser Permanente to the US Department of Veterans Affairs (VA). The VA, in particular, is a leader in telemedicine. In 2012, it reduced mental health hospitalizations by over 40%, heart failure hospitalizations by 25%, and diabetes and chronic obstructive pulmonary disease hospitalizations by about 20% using telemedicine programs.6 In 2015, it provided about 2.1 million telemedicine consultations to 677,000 veterans.7
TYPES OF TELEMEDICINE PROGRAMS
There are 2 types of telemedicine programs.
Synchronous programs take place in real time and are a live 2-way interaction between the patient and healthcare provider. This includes virtual appointments that are conducted using the patient’s smartphone, tablet, or computer with a camera. When using a smartphone or tablet, patients must first download an app that connects them with a provider.
Asynchronous programs, also known as “store and forward” applications, are not live and involve the transfer of images, videos, and other clinical information that a healthcare provider views and responds to at a later time. In this case, patients may wear medical devices to monitor and track health information (eg, blood pressure) in a personal health application that they forward to their healthcare provider.
IMPROVING PATIENT ACCESS TO CARE WHILE REDUCING COSTS
Telemedicine allows patients living in both rural and urban areas to access healthcare when they need it. Currently, about 59 million Americans reside in health professional-shortage areas, which are rural and urban areas with shortages of primary care providers.1 These patients often experience long delays when attempting to schedule a healthcare visit7 and may experience issues with continuity of care if they are unable to see the same care provider at every visit.
It also provides access to care to patients without reliable transportation or those who may be too sick to travel long distances. For some patients, such as those with cystic fibrosis who do not want to come to the hospital for fear of contracting multiple antibiotic-resistant bacteria, a virtual office visit may be safer.
At the same time, telemedicine helps reduce healthcare costs. For example, it:
- Optimizes staff distribution and healthcare resources within a healthcare facility and across an entire system
- Enables primary care providers to conduct appointments without additional office staff at any time, thereby extending office hours and availability
- Reduces the financial impact of patient no-shows
- Improves patient engagement and outcomes
- Reduces unnecessary office and emergency room visits and hospital admissions.
The last point is especially important for senior living and skilled nursing centers whose residents are known to have high rates of hospital admissions.8,9 In these facilities, 24-hour medical assistance may not be available, and telemedicine can help troubleshoot common problems.
LOW REIMBURSEMENT RATES CURTAIL USE
Limited reimbursement has curtailed the widespread use of telemedicine. Although rules for reimbursement are evolving, telemedicine still represents a small amount of total healthcare expenditures. In 2015, Medicare spent approximately $14.4 million on services delivered via telemedicine—less than 0.01% of total spending on healthcare services.1
Currently, 31 states and the District of Columbia have telemedicine parity laws that mandate private commercial insurers to pay for telemedicine services.10 Unfortunately, there is a lack of uniformity in the specifics of these laws, resulting in variations in reimbursement rates. Furthermore, a large number of larger insurers such as Medicare and Medicaid and many self-insured plans do not fall under these mandates.
Another factor that affects reimbursement for telemedicine services is the setting of the medical encounter. Medicare reimburses providers for telemedicine services only when they are conducted at specific sites such as physician’s offices, hospitals, rural health centers, and skilled nursing facilities. Additionally, Medicare only reimburses for services in areas with a shortage of healthcare professionals and in non-metropolitan areas, which excludes many urban patients.11
In contrast, more commercial reimbursement is occurring for online urgent care, and options for commercial reimbursement of online behavioral services are being explored.
INTERSTATE LICENSURE ISSUES
Current licensure laws also limit the ability of many healthcare providers to offer telemedicine services. Federal law requires providers to be fully licensed to practice medicine in the state where the patient is physically located. In cases of health systems that have locations in more than one state, providers may need to apply for and pay to maintain multiple licenses (current interstate licensing laws vary across states).
Interstate licensure is one way to solve this problem. Thus far, a number of states have joined the Interstate Medical Licensure Compact that intends to allow physicians to obtain expedited licenses to practice in multiple states.12
The federal TELE-MED Act was introduced in 2015 but not passed. It proposed to “allow a Medicare provider to provide telemedicine services to a Medicare beneficiary who is in a different state from the one in which the provider is licensed or authorized to provide healthcare services.”
CAN TELEMEDICINE FOSTER A GOOD PROVIDER-PATIENT RELATIONSHIP?
In-person encounters provide healthcare providers with the opportunity to build a therapeutic relationship with their patients. Face-to-face encounters also increase patient satisfaction scores and outcomes. As such, critics fear that patient relationships may suffer with the use of telemedicine. However, using video technology for new patient encounters may help overcome this challenge. During a video encounter, the provider can see the patient’s facial expressions and take cues from nonverbal behaviors.
At times, the element of distance may enhance the encounter. For example, in behavioral health, patients often feel more comfortable in their home environment than in a sterile office environment.
Telemedicine patients often have positive experiences, given the speed of access, precision, time savings, and the ability to stay in contact with healthcare providers from the comfort of their homes. Ultimately, these virtual visits may help improve compliance with follow-up consultations since the barriers of distance and transportation are circumvented.
WHO CAN CONDUCT TELEMEDICINE VISITS?
Although a patient’s healthcare team is likely to consist of members who are not physicians, including nurse practitioners, physician assistants, social workers, and psychologists, not everyone can, by law, conduct telemedicine visits. Currently, the rules and regulations addressing ancillary team members’ participation in telemedicine vary from state to state.
TELEMEDICINE VISITS AT CLEVELAND CLINIC
Our health system has several telemedicine programs, including our eHospital program. Launched in 2014, this program provides patients at 4 hospitals with input from staff intensivists and experienced critical care nurses during the night (7 pm to 7 am) via remote monitoring. These remote caregivers have full access to patient charts and, when signalled, can activate an in-room camera to initiate 2-way audio communication with patients, their families, and bedside caregivers.
In addition, new patient consults are being offered via telemedicine for several services including dermatology, where pictures of skin lesions are reviewed and triaged, and management recommendations are provided accordingly.
In 2016, Cleveland Clinic launched its Remote Hypertension Improvement Program—an enterprise-wide initiative to minimize hypertension-associated mortality and morbidity with the assistance of telehealth services. The program was first piloted in a group of 80 high-risk hypertensive patients who were monitored and followed through a Bluetooth-enabled remote monitoring tool, which exported blood pressure readings to a central dashboard. A multidisciplinary team of doctors, nurses, and pharmacists used this dashboard to adjust medication when needed and provide virtual lifestyle coaching. Over a 24-week period, the patients’ systolic blood pressure decreased by an average of 7.5 mm Hg and diastolic blood pressure by 3.1 mm Hg (unpublished data).
Beginning this year, blood pressure readings will be directly exported from the remote monitoring tool into the patient’s electronic medical record, providing the healthcare team with the information needed to make informed decisions to remotely manage patients with hypertension.
Remote monitoring of patients with hypertension is also being used at other institutions such as the VA. In 2016, almost 19,000 veterans were using the remote monitoring system, and this number is expected to increase with the enhanced adaptation of telemedicine services.13
FUTURE DIRECTIONS
About 50% of all adults in the United States have at least 1 chronic disease. In all, chronic disease accounts for roughly 75% of the total healthcare expenditure and 70% of all deaths.7,14 Recent data suggest that virtual chronic disease management represents an untapped market for telemedicine, given its relative underutilization compared to other services such as telebehavorial health and specialty telemedicine. These patients require frequent visits to the doctor, and targeting this patient population with telemedicine may decrease the number of emergency room visits and hospital admissions.
Another growing area in the field of telemedicine is the “hospital at home” model in which patients who meet the criteria for hospitalization but are otherwise stable are treated at home for diseases such as chronic obstructive pulmonary disease, pneumonia, and heart failure. Studies have shown that the hospital-at-home model, when used appropriately, is not only more cost-effective than hospitalization but results in a shorter treatment duration and lower rates of delirium.15–17
Finally, in the acute setting, we have seen wide success with telemedicine programs in stroke care, radiology, intensive care, and psychiatry, and several studies have shown mortality rates comparable to those with the traditional model.18,19 These encounters often require specialized skills and are the focus of multiple ongoing studies.
Acknowledgment: The authors would like to acknowledge and thank Matthew Faiman, MD, for providing information regarding the Remote Hypertension Program.
- US Department of Health and Human Services. Report to Congress: e-health and telemedicine. aspe.hhs.gov/system/files/pdf/206751/TelemedicineE-HealthReport.pdf. Accessed September 1, 2018.
- World Health Organization (WHO). A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics, 11–16 December, Geneva 1997. World Health Organization, Geneva, 1998.
- Bashshur RL, Shannon GW. History of telemedicine: evolution, context, and transformation. Mary Ann Liebert, Inc.: New Rochelle (NY), 2009.
- Bashshur RL, Goldberg MA. The origins of telemedicine and e-Health. Telemed J E Health 2014; 20(3):190–191. doi:10.1089/tmj.2014.9996
- Bashshur RL, Shannon G, Krupinski EA, Grigsby J. Sustaining and realizing the promise of telemedicine. Telemed J E Health 2013; 19(5):339–345. doi:10.1089/tmj.2012.0282
- American Hospital Association (AHA). Issue Brief. Telehealth: helping hospitals deliver cost-effective care. www.aha.org/system/files/content/16/16telehealthissuebrief.pdf. Accessed September 10, 2018.
- Congressional Research Service. Telehealth and Telemedicine: description and issues. March 29, 2016. www.senate.gov/CRSpubs/757e3b90-ff10-497c-8e8c-ac1bdbdb3aaf.pdf. Accessed August 8, 2018.
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev 2008; 65(1):3–39. doi:10.1177/1077558707308754
- Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff (Millwood) 2014; 33(2):244–250. doi:10.1377/hlthaff.2013.0922
- Jones K. If not parity, clarity—getting doctors paid for telehealth. www.forbes.com/sites/realspin/2016/09/15/if-not-parity-clarity-getting-doctors-paid-for-telehealth/#43928587777f. Accessed September 1, 2018.
- Neufeld JD, Doarn CR. Telemedicine spending by Medicare: a snapshot from 2012. Telemed J E Health 2015; 21(8):686–693. doi:10.1089/tmj.2014.0185
- Chaudhry HJ, Robin LA, Fish EM, Polk DH, Gifford JD. Improving access and mobility—the Interstate Medical Licensure Compact. N Engl J Med 2015; 372(17):1581–1583. doi:10.1056/NEJMp1502639
- United States Government Accountability Office. Report to Congressional Committees. Healthcare: telehealth and remote patient monitoring use in Medicare and selected federal programs. www.gao.gov/assets/690/684115.pdf. Accessed September 1, 2018.
- Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health 2014; 20(9):769–800. doi:10.1089/tmj.2014.9981
- Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood) 2012; 31:1237–1243. doi:10.1377/hlthaff.2011.1132
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med 2005; 143(11):798–808. pmid:16330791
- Leff B, Soones T, DeCherrie L. The hospital at home program for older adults. JAMA Intern Med 2016; 176(11):1724–1725. doi:10.1001/jamainternmed.2016.6307
- Wechsler LR, Demaerschalk BM, Schwamm LH, et al; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48(1):e3–e25. doi:10.1161/STR.0000000000000114
- Wilcox ME, Wiener-Kronish JP. Telemedicine in the intensive care unit: effect of a remote intensivist on outcomes. JAMA Intern Med 2014; 174(7):1167–1169. doi:10.1001/jamainternmed.2014.289
Telemedicine has been used successfully to improve patient access to medical care while reducing healthcare costs. In 2016, an estimated 61% of US healthcare institutions and 40% to 50% of US hospitals used telemedicine.1 From 2012 to 2013, the telemedicine market grew by 60%. However, its widespread use has been limited by low reimbursement rates and interstate licensing and practice issues.
In this commentary, we discuss the history of telemedicine, current uses and challenges, and areas of future growth.
DEFINITION AND HISTORY
The World Health Organization defines telemedicine as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”2
Modern telemedicine began in the early 1900s in the Netherlands with the transmission of heart rhythms over the telephone,3 which was followed by transmissions to radio consultation centers in Europe in the 1920s. In the 1940s, radiographic images were transmitted by telephone between cities in Pennsylvania.4
Today, telemedicine is used in a variety of specialties including radiology, neurology, and pathology5 and by organizations in the United States ranging from the National Aeronautics and Space Administration and Kaiser Permanente to the US Department of Veterans Affairs (VA). The VA, in particular, is a leader in telemedicine. In 2012, it reduced mental health hospitalizations by over 40%, heart failure hospitalizations by 25%, and diabetes and chronic obstructive pulmonary disease hospitalizations by about 20% using telemedicine programs.6 In 2015, it provided about 2.1 million telemedicine consultations to 677,000 veterans.7
TYPES OF TELEMEDICINE PROGRAMS
There are 2 types of telemedicine programs.
Synchronous programs take place in real time and are a live 2-way interaction between the patient and healthcare provider. This includes virtual appointments that are conducted using the patient’s smartphone, tablet, or computer with a camera. When using a smartphone or tablet, patients must first download an app that connects them with a provider.
Asynchronous programs, also known as “store and forward” applications, are not live and involve the transfer of images, videos, and other clinical information that a healthcare provider views and responds to at a later time. In this case, patients may wear medical devices to monitor and track health information (eg, blood pressure) in a personal health application that they forward to their healthcare provider.
IMPROVING PATIENT ACCESS TO CARE WHILE REDUCING COSTS
Telemedicine allows patients living in both rural and urban areas to access healthcare when they need it. Currently, about 59 million Americans reside in health professional-shortage areas, which are rural and urban areas with shortages of primary care providers.1 These patients often experience long delays when attempting to schedule a healthcare visit7 and may experience issues with continuity of care if they are unable to see the same care provider at every visit.
It also provides access to care to patients without reliable transportation or those who may be too sick to travel long distances. For some patients, such as those with cystic fibrosis who do not want to come to the hospital for fear of contracting multiple antibiotic-resistant bacteria, a virtual office visit may be safer.
At the same time, telemedicine helps reduce healthcare costs. For example, it:
- Optimizes staff distribution and healthcare resources within a healthcare facility and across an entire system
- Enables primary care providers to conduct appointments without additional office staff at any time, thereby extending office hours and availability
- Reduces the financial impact of patient no-shows
- Improves patient engagement and outcomes
- Reduces unnecessary office and emergency room visits and hospital admissions.
The last point is especially important for senior living and skilled nursing centers whose residents are known to have high rates of hospital admissions.8,9 In these facilities, 24-hour medical assistance may not be available, and telemedicine can help troubleshoot common problems.
LOW REIMBURSEMENT RATES CURTAIL USE
Limited reimbursement has curtailed the widespread use of telemedicine. Although rules for reimbursement are evolving, telemedicine still represents a small amount of total healthcare expenditures. In 2015, Medicare spent approximately $14.4 million on services delivered via telemedicine—less than 0.01% of total spending on healthcare services.1
Currently, 31 states and the District of Columbia have telemedicine parity laws that mandate private commercial insurers to pay for telemedicine services.10 Unfortunately, there is a lack of uniformity in the specifics of these laws, resulting in variations in reimbursement rates. Furthermore, a large number of larger insurers such as Medicare and Medicaid and many self-insured plans do not fall under these mandates.
Another factor that affects reimbursement for telemedicine services is the setting of the medical encounter. Medicare reimburses providers for telemedicine services only when they are conducted at specific sites such as physician’s offices, hospitals, rural health centers, and skilled nursing facilities. Additionally, Medicare only reimburses for services in areas with a shortage of healthcare professionals and in non-metropolitan areas, which excludes many urban patients.11
In contrast, more commercial reimbursement is occurring for online urgent care, and options for commercial reimbursement of online behavioral services are being explored.
INTERSTATE LICENSURE ISSUES
Current licensure laws also limit the ability of many healthcare providers to offer telemedicine services. Federal law requires providers to be fully licensed to practice medicine in the state where the patient is physically located. In cases of health systems that have locations in more than one state, providers may need to apply for and pay to maintain multiple licenses (current interstate licensing laws vary across states).
Interstate licensure is one way to solve this problem. Thus far, a number of states have joined the Interstate Medical Licensure Compact that intends to allow physicians to obtain expedited licenses to practice in multiple states.12
The federal TELE-MED Act was introduced in 2015 but not passed. It proposed to “allow a Medicare provider to provide telemedicine services to a Medicare beneficiary who is in a different state from the one in which the provider is licensed or authorized to provide healthcare services.”
CAN TELEMEDICINE FOSTER A GOOD PROVIDER-PATIENT RELATIONSHIP?
In-person encounters provide healthcare providers with the opportunity to build a therapeutic relationship with their patients. Face-to-face encounters also increase patient satisfaction scores and outcomes. As such, critics fear that patient relationships may suffer with the use of telemedicine. However, using video technology for new patient encounters may help overcome this challenge. During a video encounter, the provider can see the patient’s facial expressions and take cues from nonverbal behaviors.
At times, the element of distance may enhance the encounter. For example, in behavioral health, patients often feel more comfortable in their home environment than in a sterile office environment.
Telemedicine patients often have positive experiences, given the speed of access, precision, time savings, and the ability to stay in contact with healthcare providers from the comfort of their homes. Ultimately, these virtual visits may help improve compliance with follow-up consultations since the barriers of distance and transportation are circumvented.
WHO CAN CONDUCT TELEMEDICINE VISITS?
Although a patient’s healthcare team is likely to consist of members who are not physicians, including nurse practitioners, physician assistants, social workers, and psychologists, not everyone can, by law, conduct telemedicine visits. Currently, the rules and regulations addressing ancillary team members’ participation in telemedicine vary from state to state.
TELEMEDICINE VISITS AT CLEVELAND CLINIC
Our health system has several telemedicine programs, including our eHospital program. Launched in 2014, this program provides patients at 4 hospitals with input from staff intensivists and experienced critical care nurses during the night (7 pm to 7 am) via remote monitoring. These remote caregivers have full access to patient charts and, when signalled, can activate an in-room camera to initiate 2-way audio communication with patients, their families, and bedside caregivers.
In addition, new patient consults are being offered via telemedicine for several services including dermatology, where pictures of skin lesions are reviewed and triaged, and management recommendations are provided accordingly.
In 2016, Cleveland Clinic launched its Remote Hypertension Improvement Program—an enterprise-wide initiative to minimize hypertension-associated mortality and morbidity with the assistance of telehealth services. The program was first piloted in a group of 80 high-risk hypertensive patients who were monitored and followed through a Bluetooth-enabled remote monitoring tool, which exported blood pressure readings to a central dashboard. A multidisciplinary team of doctors, nurses, and pharmacists used this dashboard to adjust medication when needed and provide virtual lifestyle coaching. Over a 24-week period, the patients’ systolic blood pressure decreased by an average of 7.5 mm Hg and diastolic blood pressure by 3.1 mm Hg (unpublished data).
Beginning this year, blood pressure readings will be directly exported from the remote monitoring tool into the patient’s electronic medical record, providing the healthcare team with the information needed to make informed decisions to remotely manage patients with hypertension.
Remote monitoring of patients with hypertension is also being used at other institutions such as the VA. In 2016, almost 19,000 veterans were using the remote monitoring system, and this number is expected to increase with the enhanced adaptation of telemedicine services.13
FUTURE DIRECTIONS
About 50% of all adults in the United States have at least 1 chronic disease. In all, chronic disease accounts for roughly 75% of the total healthcare expenditure and 70% of all deaths.7,14 Recent data suggest that virtual chronic disease management represents an untapped market for telemedicine, given its relative underutilization compared to other services such as telebehavorial health and specialty telemedicine. These patients require frequent visits to the doctor, and targeting this patient population with telemedicine may decrease the number of emergency room visits and hospital admissions.
Another growing area in the field of telemedicine is the “hospital at home” model in which patients who meet the criteria for hospitalization but are otherwise stable are treated at home for diseases such as chronic obstructive pulmonary disease, pneumonia, and heart failure. Studies have shown that the hospital-at-home model, when used appropriately, is not only more cost-effective than hospitalization but results in a shorter treatment duration and lower rates of delirium.15–17
Finally, in the acute setting, we have seen wide success with telemedicine programs in stroke care, radiology, intensive care, and psychiatry, and several studies have shown mortality rates comparable to those with the traditional model.18,19 These encounters often require specialized skills and are the focus of multiple ongoing studies.
Acknowledgment: The authors would like to acknowledge and thank Matthew Faiman, MD, for providing information regarding the Remote Hypertension Program.
Telemedicine has been used successfully to improve patient access to medical care while reducing healthcare costs. In 2016, an estimated 61% of US healthcare institutions and 40% to 50% of US hospitals used telemedicine.1 From 2012 to 2013, the telemedicine market grew by 60%. However, its widespread use has been limited by low reimbursement rates and interstate licensing and practice issues.
In this commentary, we discuss the history of telemedicine, current uses and challenges, and areas of future growth.
DEFINITION AND HISTORY
The World Health Organization defines telemedicine as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”2
Modern telemedicine began in the early 1900s in the Netherlands with the transmission of heart rhythms over the telephone,3 which was followed by transmissions to radio consultation centers in Europe in the 1920s. In the 1940s, radiographic images were transmitted by telephone between cities in Pennsylvania.4
Today, telemedicine is used in a variety of specialties including radiology, neurology, and pathology5 and by organizations in the United States ranging from the National Aeronautics and Space Administration and Kaiser Permanente to the US Department of Veterans Affairs (VA). The VA, in particular, is a leader in telemedicine. In 2012, it reduced mental health hospitalizations by over 40%, heart failure hospitalizations by 25%, and diabetes and chronic obstructive pulmonary disease hospitalizations by about 20% using telemedicine programs.6 In 2015, it provided about 2.1 million telemedicine consultations to 677,000 veterans.7
TYPES OF TELEMEDICINE PROGRAMS
There are 2 types of telemedicine programs.
Synchronous programs take place in real time and are a live 2-way interaction between the patient and healthcare provider. This includes virtual appointments that are conducted using the patient’s smartphone, tablet, or computer with a camera. When using a smartphone or tablet, patients must first download an app that connects them with a provider.
Asynchronous programs, also known as “store and forward” applications, are not live and involve the transfer of images, videos, and other clinical information that a healthcare provider views and responds to at a later time. In this case, patients may wear medical devices to monitor and track health information (eg, blood pressure) in a personal health application that they forward to their healthcare provider.
IMPROVING PATIENT ACCESS TO CARE WHILE REDUCING COSTS
Telemedicine allows patients living in both rural and urban areas to access healthcare when they need it. Currently, about 59 million Americans reside in health professional-shortage areas, which are rural and urban areas with shortages of primary care providers.1 These patients often experience long delays when attempting to schedule a healthcare visit7 and may experience issues with continuity of care if they are unable to see the same care provider at every visit.
It also provides access to care to patients without reliable transportation or those who may be too sick to travel long distances. For some patients, such as those with cystic fibrosis who do not want to come to the hospital for fear of contracting multiple antibiotic-resistant bacteria, a virtual office visit may be safer.
At the same time, telemedicine helps reduce healthcare costs. For example, it:
- Optimizes staff distribution and healthcare resources within a healthcare facility and across an entire system
- Enables primary care providers to conduct appointments without additional office staff at any time, thereby extending office hours and availability
- Reduces the financial impact of patient no-shows
- Improves patient engagement and outcomes
- Reduces unnecessary office and emergency room visits and hospital admissions.
The last point is especially important for senior living and skilled nursing centers whose residents are known to have high rates of hospital admissions.8,9 In these facilities, 24-hour medical assistance may not be available, and telemedicine can help troubleshoot common problems.
LOW REIMBURSEMENT RATES CURTAIL USE
Limited reimbursement has curtailed the widespread use of telemedicine. Although rules for reimbursement are evolving, telemedicine still represents a small amount of total healthcare expenditures. In 2015, Medicare spent approximately $14.4 million on services delivered via telemedicine—less than 0.01% of total spending on healthcare services.1
Currently, 31 states and the District of Columbia have telemedicine parity laws that mandate private commercial insurers to pay for telemedicine services.10 Unfortunately, there is a lack of uniformity in the specifics of these laws, resulting in variations in reimbursement rates. Furthermore, a large number of larger insurers such as Medicare and Medicaid and many self-insured plans do not fall under these mandates.
Another factor that affects reimbursement for telemedicine services is the setting of the medical encounter. Medicare reimburses providers for telemedicine services only when they are conducted at specific sites such as physician’s offices, hospitals, rural health centers, and skilled nursing facilities. Additionally, Medicare only reimburses for services in areas with a shortage of healthcare professionals and in non-metropolitan areas, which excludes many urban patients.11
In contrast, more commercial reimbursement is occurring for online urgent care, and options for commercial reimbursement of online behavioral services are being explored.
INTERSTATE LICENSURE ISSUES
Current licensure laws also limit the ability of many healthcare providers to offer telemedicine services. Federal law requires providers to be fully licensed to practice medicine in the state where the patient is physically located. In cases of health systems that have locations in more than one state, providers may need to apply for and pay to maintain multiple licenses (current interstate licensing laws vary across states).
Interstate licensure is one way to solve this problem. Thus far, a number of states have joined the Interstate Medical Licensure Compact that intends to allow physicians to obtain expedited licenses to practice in multiple states.12
The federal TELE-MED Act was introduced in 2015 but not passed. It proposed to “allow a Medicare provider to provide telemedicine services to a Medicare beneficiary who is in a different state from the one in which the provider is licensed or authorized to provide healthcare services.”
CAN TELEMEDICINE FOSTER A GOOD PROVIDER-PATIENT RELATIONSHIP?
In-person encounters provide healthcare providers with the opportunity to build a therapeutic relationship with their patients. Face-to-face encounters also increase patient satisfaction scores and outcomes. As such, critics fear that patient relationships may suffer with the use of telemedicine. However, using video technology for new patient encounters may help overcome this challenge. During a video encounter, the provider can see the patient’s facial expressions and take cues from nonverbal behaviors.
At times, the element of distance may enhance the encounter. For example, in behavioral health, patients often feel more comfortable in their home environment than in a sterile office environment.
Telemedicine patients often have positive experiences, given the speed of access, precision, time savings, and the ability to stay in contact with healthcare providers from the comfort of their homes. Ultimately, these virtual visits may help improve compliance with follow-up consultations since the barriers of distance and transportation are circumvented.
WHO CAN CONDUCT TELEMEDICINE VISITS?
Although a patient’s healthcare team is likely to consist of members who are not physicians, including nurse practitioners, physician assistants, social workers, and psychologists, not everyone can, by law, conduct telemedicine visits. Currently, the rules and regulations addressing ancillary team members’ participation in telemedicine vary from state to state.
TELEMEDICINE VISITS AT CLEVELAND CLINIC
Our health system has several telemedicine programs, including our eHospital program. Launched in 2014, this program provides patients at 4 hospitals with input from staff intensivists and experienced critical care nurses during the night (7 pm to 7 am) via remote monitoring. These remote caregivers have full access to patient charts and, when signalled, can activate an in-room camera to initiate 2-way audio communication with patients, their families, and bedside caregivers.
In addition, new patient consults are being offered via telemedicine for several services including dermatology, where pictures of skin lesions are reviewed and triaged, and management recommendations are provided accordingly.
In 2016, Cleveland Clinic launched its Remote Hypertension Improvement Program—an enterprise-wide initiative to minimize hypertension-associated mortality and morbidity with the assistance of telehealth services. The program was first piloted in a group of 80 high-risk hypertensive patients who were monitored and followed through a Bluetooth-enabled remote monitoring tool, which exported blood pressure readings to a central dashboard. A multidisciplinary team of doctors, nurses, and pharmacists used this dashboard to adjust medication when needed and provide virtual lifestyle coaching. Over a 24-week period, the patients’ systolic blood pressure decreased by an average of 7.5 mm Hg and diastolic blood pressure by 3.1 mm Hg (unpublished data).
Beginning this year, blood pressure readings will be directly exported from the remote monitoring tool into the patient’s electronic medical record, providing the healthcare team with the information needed to make informed decisions to remotely manage patients with hypertension.
Remote monitoring of patients with hypertension is also being used at other institutions such as the VA. In 2016, almost 19,000 veterans were using the remote monitoring system, and this number is expected to increase with the enhanced adaptation of telemedicine services.13
FUTURE DIRECTIONS
About 50% of all adults in the United States have at least 1 chronic disease. In all, chronic disease accounts for roughly 75% of the total healthcare expenditure and 70% of all deaths.7,14 Recent data suggest that virtual chronic disease management represents an untapped market for telemedicine, given its relative underutilization compared to other services such as telebehavorial health and specialty telemedicine. These patients require frequent visits to the doctor, and targeting this patient population with telemedicine may decrease the number of emergency room visits and hospital admissions.
Another growing area in the field of telemedicine is the “hospital at home” model in which patients who meet the criteria for hospitalization but are otherwise stable are treated at home for diseases such as chronic obstructive pulmonary disease, pneumonia, and heart failure. Studies have shown that the hospital-at-home model, when used appropriately, is not only more cost-effective than hospitalization but results in a shorter treatment duration and lower rates of delirium.15–17
Finally, in the acute setting, we have seen wide success with telemedicine programs in stroke care, radiology, intensive care, and psychiatry, and several studies have shown mortality rates comparable to those with the traditional model.18,19 These encounters often require specialized skills and are the focus of multiple ongoing studies.
Acknowledgment: The authors would like to acknowledge and thank Matthew Faiman, MD, for providing information regarding the Remote Hypertension Program.
- US Department of Health and Human Services. Report to Congress: e-health and telemedicine. aspe.hhs.gov/system/files/pdf/206751/TelemedicineE-HealthReport.pdf. Accessed September 1, 2018.
- World Health Organization (WHO). A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics, 11–16 December, Geneva 1997. World Health Organization, Geneva, 1998.
- Bashshur RL, Shannon GW. History of telemedicine: evolution, context, and transformation. Mary Ann Liebert, Inc.: New Rochelle (NY), 2009.
- Bashshur RL, Goldberg MA. The origins of telemedicine and e-Health. Telemed J E Health 2014; 20(3):190–191. doi:10.1089/tmj.2014.9996
- Bashshur RL, Shannon G, Krupinski EA, Grigsby J. Sustaining and realizing the promise of telemedicine. Telemed J E Health 2013; 19(5):339–345. doi:10.1089/tmj.2012.0282
- American Hospital Association (AHA). Issue Brief. Telehealth: helping hospitals deliver cost-effective care. www.aha.org/system/files/content/16/16telehealthissuebrief.pdf. Accessed September 10, 2018.
- Congressional Research Service. Telehealth and Telemedicine: description and issues. March 29, 2016. www.senate.gov/CRSpubs/757e3b90-ff10-497c-8e8c-ac1bdbdb3aaf.pdf. Accessed August 8, 2018.
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev 2008; 65(1):3–39. doi:10.1177/1077558707308754
- Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff (Millwood) 2014; 33(2):244–250. doi:10.1377/hlthaff.2013.0922
- Jones K. If not parity, clarity—getting doctors paid for telehealth. www.forbes.com/sites/realspin/2016/09/15/if-not-parity-clarity-getting-doctors-paid-for-telehealth/#43928587777f. Accessed September 1, 2018.
- Neufeld JD, Doarn CR. Telemedicine spending by Medicare: a snapshot from 2012. Telemed J E Health 2015; 21(8):686–693. doi:10.1089/tmj.2014.0185
- Chaudhry HJ, Robin LA, Fish EM, Polk DH, Gifford JD. Improving access and mobility—the Interstate Medical Licensure Compact. N Engl J Med 2015; 372(17):1581–1583. doi:10.1056/NEJMp1502639
- United States Government Accountability Office. Report to Congressional Committees. Healthcare: telehealth and remote patient monitoring use in Medicare and selected federal programs. www.gao.gov/assets/690/684115.pdf. Accessed September 1, 2018.
- Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health 2014; 20(9):769–800. doi:10.1089/tmj.2014.9981
- Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood) 2012; 31:1237–1243. doi:10.1377/hlthaff.2011.1132
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med 2005; 143(11):798–808. pmid:16330791
- Leff B, Soones T, DeCherrie L. The hospital at home program for older adults. JAMA Intern Med 2016; 176(11):1724–1725. doi:10.1001/jamainternmed.2016.6307
- Wechsler LR, Demaerschalk BM, Schwamm LH, et al; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48(1):e3–e25. doi:10.1161/STR.0000000000000114
- Wilcox ME, Wiener-Kronish JP. Telemedicine in the intensive care unit: effect of a remote intensivist on outcomes. JAMA Intern Med 2014; 174(7):1167–1169. doi:10.1001/jamainternmed.2014.289
- US Department of Health and Human Services. Report to Congress: e-health and telemedicine. aspe.hhs.gov/system/files/pdf/206751/TelemedicineE-HealthReport.pdf. Accessed September 1, 2018.
- World Health Organization (WHO). A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics, 11–16 December, Geneva 1997. World Health Organization, Geneva, 1998.
- Bashshur RL, Shannon GW. History of telemedicine: evolution, context, and transformation. Mary Ann Liebert, Inc.: New Rochelle (NY), 2009.
- Bashshur RL, Goldberg MA. The origins of telemedicine and e-Health. Telemed J E Health 2014; 20(3):190–191. doi:10.1089/tmj.2014.9996
- Bashshur RL, Shannon G, Krupinski EA, Grigsby J. Sustaining and realizing the promise of telemedicine. Telemed J E Health 2013; 19(5):339–345. doi:10.1089/tmj.2012.0282
- American Hospital Association (AHA). Issue Brief. Telehealth: helping hospitals deliver cost-effective care. www.aha.org/system/files/content/16/16telehealthissuebrief.pdf. Accessed September 10, 2018.
- Congressional Research Service. Telehealth and Telemedicine: description and issues. March 29, 2016. www.senate.gov/CRSpubs/757e3b90-ff10-497c-8e8c-ac1bdbdb3aaf.pdf. Accessed August 8, 2018.
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev 2008; 65(1):3–39. doi:10.1177/1077558707308754
- Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff (Millwood) 2014; 33(2):244–250. doi:10.1377/hlthaff.2013.0922
- Jones K. If not parity, clarity—getting doctors paid for telehealth. www.forbes.com/sites/realspin/2016/09/15/if-not-parity-clarity-getting-doctors-paid-for-telehealth/#43928587777f. Accessed September 1, 2018.
- Neufeld JD, Doarn CR. Telemedicine spending by Medicare: a snapshot from 2012. Telemed J E Health 2015; 21(8):686–693. doi:10.1089/tmj.2014.0185
- Chaudhry HJ, Robin LA, Fish EM, Polk DH, Gifford JD. Improving access and mobility—the Interstate Medical Licensure Compact. N Engl J Med 2015; 372(17):1581–1583. doi:10.1056/NEJMp1502639
- United States Government Accountability Office. Report to Congressional Committees. Healthcare: telehealth and remote patient monitoring use in Medicare and selected federal programs. www.gao.gov/assets/690/684115.pdf. Accessed September 1, 2018.
- Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health 2014; 20(9):769–800. doi:10.1089/tmj.2014.9981
- Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood) 2012; 31:1237–1243. doi:10.1377/hlthaff.2011.1132
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med 2005; 143(11):798–808. pmid:16330791
- Leff B, Soones T, DeCherrie L. The hospital at home program for older adults. JAMA Intern Med 2016; 176(11):1724–1725. doi:10.1001/jamainternmed.2016.6307
- Wechsler LR, Demaerschalk BM, Schwamm LH, et al; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48(1):e3–e25. doi:10.1161/STR.0000000000000114
- Wilcox ME, Wiener-Kronish JP. Telemedicine in the intensive care unit: effect of a remote intensivist on outcomes. JAMA Intern Med 2014; 174(7):1167–1169. doi:10.1001/jamainternmed.2014.289
KEY POINTS
- An estimated 7 million patients in the United States will use telemedicine services this year alone; demand will continue to rise.
- Low reimbursement rates and current lack of interstate licensure laws limit the ability of many health care providers to offer telemedicine services.
- The rules and regulations addressing ancillary team members’ participation in telemedicine vary from state to state.
- Areas of future growth include chronic disease management and “hospital at home” care.
New Marks of Distinction for SVS Members
The SVS Executive Board announced in November that all Active SVS Members in good standing will now be considered Fellows of the Society for Vascular Surgery™ (FSVS™). The trademarked designation is one of the benefits of SVS membership and is a public acknowledgement that a surgeon has met the high standards required by the SVS of its members and has shown and professional commitment to the field of vascular surgery. Active Members in good standing may add the initials FSVS™ after their name in any usage, such as signature lines, letterhead, door signage and so on. Distinguished Fellows of the Society for Vascular Surgery™ also may use the trademarked designation of DFSVS™. Read the official announcement here.
The SVS Executive Board announced in November that all Active SVS Members in good standing will now be considered Fellows of the Society for Vascular Surgery™ (FSVS™). The trademarked designation is one of the benefits of SVS membership and is a public acknowledgement that a surgeon has met the high standards required by the SVS of its members and has shown and professional commitment to the field of vascular surgery. Active Members in good standing may add the initials FSVS™ after their name in any usage, such as signature lines, letterhead, door signage and so on. Distinguished Fellows of the Society for Vascular Surgery™ also may use the trademarked designation of DFSVS™. Read the official announcement here.
The SVS Executive Board announced in November that all Active SVS Members in good standing will now be considered Fellows of the Society for Vascular Surgery™ (FSVS™). The trademarked designation is one of the benefits of SVS membership and is a public acknowledgement that a surgeon has met the high standards required by the SVS of its members and has shown and professional commitment to the field of vascular surgery. Active Members in good standing may add the initials FSVS™ after their name in any usage, such as signature lines, letterhead, door signage and so on. Distinguished Fellows of the Society for Vascular Surgery™ also may use the trademarked designation of DFSVS™. Read the official announcement here.
Cannabis for chronic pain: Not a simple solution
The narrative review by Modesto-Lowe et al1 in this issue on the potential therapeutic use of cannabis for peripheral neuropathy is only the latest in a vogue string of examinations on how medical marijuana may be used to manage complex conditions. While the authors should be lauded for acknowledging that the role of cannabis in treating peripheral neuropathy is far from settled (“the unknown” in their title), the high stakes involved warrant even more stringent scrutiny than they suggest.
We are in the midst of an epidemic of chronic opioid use with massive repercussions, and it did not start overnight. Mounting calls for liberalizing narcotic use across a broad range of pain conditions accumulated gradually during the patient-advocacy era of the 1990s, with supporting “evidence” coming mostly from small uncontrolled studies, anecdotal reports, and industry pressure.2 Although cannabis and opioids are not interchangeable, we should be cautious about concluding that cannabis is effective and that it should be used to treat chronic pain.
CHRONIC PAIN IS COMPLICATED
Peripheral neuropathy, by definition, is a chronic pain condition. Unlike acute pain, chronic pain is characterized by biologic, psychologic, and social complexities that require nuance to manage and study.
Such nuance is lacking in most recent reviews of the medical use of cannabis. The conditions in question are often studied as if they were transient and acute, eg, employing short-term studies and rudimentary measures such as numeric pain-rating scales or other snapshots of pain intensity. Results of these shortsighted assessments are impossible to extrapolate to long-term outcomes.
Whether cannabis therapy for chronic pain conditions is sustainable remains to be seen. Outcomes in chronic pain should not be defined simply by pain reduction, but by other dimensions such as changes in pain-related disability and quality of life, development of pharmacologic tolerance or dependence, adverse effects, and other “collateral damage.” We are far from understanding these issues, which require highly controlled and regulated longitudinal studies.
A recent Cochrane review3 of the efficacy of cannabis-based medicines for chronic neuropathic pain found that harms might outweigh the benefits. The quality of evidence was rated as very low to moderate; the reviewers cited small sample sizes and exclusion of important subgroups of patients (eg, those with substance abuse or other psychiatric comorbidities). Such exclusions are the crux of a major problem with cannabis research: studies are not naturalistic. The gritty reality of chronic pain management is paramount, and failing to consider the high-risk biopsychosocial factors typical of patients with chronic pain is naïve and, frankly, dangerous.
COGNITIVE AND MOTIVATIONAL PROBLEMS
The true danger of cannabis lies in what we already know with certainty. As the authors discuss, cannabis undisputedly results in dose-dependent cognitive and motivational problems. If we are preaching physical therapy and home exercise to counter deconditioning, socialization to reverse depression, cognitive-behavioral therapy to increase coping, returning to work to prevent prolonged disability, and other active measures to prevent pain from becoming chronic, then why would we suggest treatments known to blunt motivation, energy, concentration, and overall mood? As a general central nervous system suppressant,4 cannabis works broadly against our best efforts to rehabilitate patients and restore their overall function.
ALL CANNABIS IS NOT THE SAME
The authors use the general term cannabis in their title, yet rightly unpack the differences between medical marijuana, tetrahydrocannabinol (THC), and cannabidiol (CBD). However, in the minds of untrained and pain-stricken patients seeking rapid relief and practical solutions, such distinctions are likely irrelevant.
The danger in the barrage of publications examining cannabis vs medical marijuana vs THC vs CBD is that they all communicate an unintentional yet problematic message: that marijuana of some sort for pain is acceptable to try. And in the face of financial pressures, changing legal landscapes, insurance coverage volatility, and access issues, are patients really going to always secure prescriptions for well-regulated CBD (lacking psychoactive THC) from thoughtful and well-informed physicians, or will they turn to convenient street suppliers?
Simplified perceptions of safety and efficacy across all cannabis products do not help. More troublesome would be to extrapolate safety to other forms of marijuana known to be dangerous, such as synthetic cannabinoids, which in some instances have been associated with catastrophic outcomes.5 The slippery slope is real: if the message becomes that some (or most) marijuana is benign or even therapeutic, what is to curb a widespread and unregulated epidemic?
YOUTH AT RISK
Some groups are more vulnerable than others to the potential negative effects of cannabis. In a study at a medical cannabis dispensary in San Francisco,6 adolescents and young adults used more marijuana than older users did and had higher rates of “use when bored” and eventual pharmacologic dependence. Sustained use of marijuana by young people places them at risk of serious psychiatric disorders, with numerous studies demonstrating the unfolding of schizophrenia, depression, bipolar disorder, and more.7
As the authors point out, cannabis may be contraindicated in those already burdened with mental health problems. If we recall that comorbid psychiatric disorders are the norm rather than the exception in chronic pain conditions,8 can we recommend cannabis therapy for most patients with chronic pain with confidence that it will not cause unintended problems? Evidence already shows that even well-established medical marijuana services attract (and perhaps unintentionally debilitate) a certain high-risk demographic: young, socioeconomically disadvantaged men with other comorbid psychiatric and substance use disorders, who ultimately rank poorly in functional health measures compared with the general population.9
NOT REEFER MADNESS, BUT REEFER CAUTION
I am not advocating the fear-mongering misinformation campaigns of the past. We should not exaggerate and warn about “reefer madness” or equate marijuana with untruths about random violence or complete bedlam. Nonetheless, concerns for widespread amotivation, worsening psychiatric states, chronic disability, and chemical dependence are very real.
Needed are tightly regulated, well-controlled, and long-term prospective studies involving isolated CBD formulations lacking THC. Over time, perhaps only formulations approved by the US Food and Drug Administration will be embraced. In the meantime, more comprehensive approaches should be recommended, such as team-based interdisciplinary rehabilitation programs that have shown efficacy in handling chronic pain complexities.10,11
If such steps are unlikely, physicians should nonetheless stand united in sending a message of cautious optimism regarding medical marijuana, educating their patients not only about recently advertised potential yet inconclusive benefits, but also about the well-known and actual certitudes of its harms for use in chronic pain management. There is plenty of bad and worse information to share with patients, and there is a slippery slope of epidemic proportions to be wary about.
- Modesto-Lowe V, Bojka R, Alvarado C. Cannabis for peripheral neuropathy: The good, the bad, and the unknown. Cleve Clin J Med 2018; 85(12):943–949. doi:10.3949/ccjm.85a.17115
- Wailoo K. Pain: A Political History. Baltimore, MD: Johns Hopkins University Press; 2014.
- Mucke M, Phillips T, Radbruch L, Petzke F, Hauser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev 2018; 3:CD012182. doi:10.1002/14651858.CD012182.pub2
- Lucas CJ, Galettis P, Schneider J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol 2018. Epub ahead of print. doi:10.1111/bcp.13710
- Patel NA, Jerry JM, Jimenez XF, Hantus ST. New-onset refractory status epilepticus associated with the use of synthetic cannabinoids. Psychosomatics 2017; 58(2):180–186. doi:10.1016/j.psym.2016.10.006
- Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn-Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav 2017; 72:14–20. doi:10.1016/j.addbeh.2017.03.006
- Mammen G, Rueda S, Roerecke M, Bonato S, Lev-Ran S, Rehm J. Association of cannabis with long-term clinical symptoms in anxiety and mood disorders: a systematic review of prospective studies. J Clin Psychiatry 2018; 79(4)pii:17r11839. doi:10.4088/JCP.17r11839
- Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry 2017; pii:S0278–5846(17)30194–X. doi:10.1016/j.pnpbp.2017.05.012
- Fischer B, Ialomiteanu AR, Aeby S, Rudzinski K, Kurdyak P, Rehm J. Substance use, health, and functioning characteristics of medical marijuana program participants compared to the general adult population in Ontario (Canada). J Psychoactive Drugs 2017; 49(1):31–38. doi:10.1080/02791072.2016.1264648
- Shah A, Craner J, Cunningham JL. Medical cannabis use among patients with chronic pain in an interdisciplinary pain rehabilitation program: characterization and treatment outcomes. J Subst Abuse Treat 2017; 77:95–100. doi:10.1016/j.jsat.2017.03.012
- Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep 2012; 16(2):147–152. doi:10.1007/s11916-012-0252-4
The narrative review by Modesto-Lowe et al1 in this issue on the potential therapeutic use of cannabis for peripheral neuropathy is only the latest in a vogue string of examinations on how medical marijuana may be used to manage complex conditions. While the authors should be lauded for acknowledging that the role of cannabis in treating peripheral neuropathy is far from settled (“the unknown” in their title), the high stakes involved warrant even more stringent scrutiny than they suggest.
We are in the midst of an epidemic of chronic opioid use with massive repercussions, and it did not start overnight. Mounting calls for liberalizing narcotic use across a broad range of pain conditions accumulated gradually during the patient-advocacy era of the 1990s, with supporting “evidence” coming mostly from small uncontrolled studies, anecdotal reports, and industry pressure.2 Although cannabis and opioids are not interchangeable, we should be cautious about concluding that cannabis is effective and that it should be used to treat chronic pain.
CHRONIC PAIN IS COMPLICATED
Peripheral neuropathy, by definition, is a chronic pain condition. Unlike acute pain, chronic pain is characterized by biologic, psychologic, and social complexities that require nuance to manage and study.
Such nuance is lacking in most recent reviews of the medical use of cannabis. The conditions in question are often studied as if they were transient and acute, eg, employing short-term studies and rudimentary measures such as numeric pain-rating scales or other snapshots of pain intensity. Results of these shortsighted assessments are impossible to extrapolate to long-term outcomes.
Whether cannabis therapy for chronic pain conditions is sustainable remains to be seen. Outcomes in chronic pain should not be defined simply by pain reduction, but by other dimensions such as changes in pain-related disability and quality of life, development of pharmacologic tolerance or dependence, adverse effects, and other “collateral damage.” We are far from understanding these issues, which require highly controlled and regulated longitudinal studies.
A recent Cochrane review3 of the efficacy of cannabis-based medicines for chronic neuropathic pain found that harms might outweigh the benefits. The quality of evidence was rated as very low to moderate; the reviewers cited small sample sizes and exclusion of important subgroups of patients (eg, those with substance abuse or other psychiatric comorbidities). Such exclusions are the crux of a major problem with cannabis research: studies are not naturalistic. The gritty reality of chronic pain management is paramount, and failing to consider the high-risk biopsychosocial factors typical of patients with chronic pain is naïve and, frankly, dangerous.
COGNITIVE AND MOTIVATIONAL PROBLEMS
The true danger of cannabis lies in what we already know with certainty. As the authors discuss, cannabis undisputedly results in dose-dependent cognitive and motivational problems. If we are preaching physical therapy and home exercise to counter deconditioning, socialization to reverse depression, cognitive-behavioral therapy to increase coping, returning to work to prevent prolonged disability, and other active measures to prevent pain from becoming chronic, then why would we suggest treatments known to blunt motivation, energy, concentration, and overall mood? As a general central nervous system suppressant,4 cannabis works broadly against our best efforts to rehabilitate patients and restore their overall function.
ALL CANNABIS IS NOT THE SAME
The authors use the general term cannabis in their title, yet rightly unpack the differences between medical marijuana, tetrahydrocannabinol (THC), and cannabidiol (CBD). However, in the minds of untrained and pain-stricken patients seeking rapid relief and practical solutions, such distinctions are likely irrelevant.
The danger in the barrage of publications examining cannabis vs medical marijuana vs THC vs CBD is that they all communicate an unintentional yet problematic message: that marijuana of some sort for pain is acceptable to try. And in the face of financial pressures, changing legal landscapes, insurance coverage volatility, and access issues, are patients really going to always secure prescriptions for well-regulated CBD (lacking psychoactive THC) from thoughtful and well-informed physicians, or will they turn to convenient street suppliers?
Simplified perceptions of safety and efficacy across all cannabis products do not help. More troublesome would be to extrapolate safety to other forms of marijuana known to be dangerous, such as synthetic cannabinoids, which in some instances have been associated with catastrophic outcomes.5 The slippery slope is real: if the message becomes that some (or most) marijuana is benign or even therapeutic, what is to curb a widespread and unregulated epidemic?
YOUTH AT RISK
Some groups are more vulnerable than others to the potential negative effects of cannabis. In a study at a medical cannabis dispensary in San Francisco,6 adolescents and young adults used more marijuana than older users did and had higher rates of “use when bored” and eventual pharmacologic dependence. Sustained use of marijuana by young people places them at risk of serious psychiatric disorders, with numerous studies demonstrating the unfolding of schizophrenia, depression, bipolar disorder, and more.7
As the authors point out, cannabis may be contraindicated in those already burdened with mental health problems. If we recall that comorbid psychiatric disorders are the norm rather than the exception in chronic pain conditions,8 can we recommend cannabis therapy for most patients with chronic pain with confidence that it will not cause unintended problems? Evidence already shows that even well-established medical marijuana services attract (and perhaps unintentionally debilitate) a certain high-risk demographic: young, socioeconomically disadvantaged men with other comorbid psychiatric and substance use disorders, who ultimately rank poorly in functional health measures compared with the general population.9
NOT REEFER MADNESS, BUT REEFER CAUTION
I am not advocating the fear-mongering misinformation campaigns of the past. We should not exaggerate and warn about “reefer madness” or equate marijuana with untruths about random violence or complete bedlam. Nonetheless, concerns for widespread amotivation, worsening psychiatric states, chronic disability, and chemical dependence are very real.
Needed are tightly regulated, well-controlled, and long-term prospective studies involving isolated CBD formulations lacking THC. Over time, perhaps only formulations approved by the US Food and Drug Administration will be embraced. In the meantime, more comprehensive approaches should be recommended, such as team-based interdisciplinary rehabilitation programs that have shown efficacy in handling chronic pain complexities.10,11
If such steps are unlikely, physicians should nonetheless stand united in sending a message of cautious optimism regarding medical marijuana, educating their patients not only about recently advertised potential yet inconclusive benefits, but also about the well-known and actual certitudes of its harms for use in chronic pain management. There is plenty of bad and worse information to share with patients, and there is a slippery slope of epidemic proportions to be wary about.
The narrative review by Modesto-Lowe et al1 in this issue on the potential therapeutic use of cannabis for peripheral neuropathy is only the latest in a vogue string of examinations on how medical marijuana may be used to manage complex conditions. While the authors should be lauded for acknowledging that the role of cannabis in treating peripheral neuropathy is far from settled (“the unknown” in their title), the high stakes involved warrant even more stringent scrutiny than they suggest.
We are in the midst of an epidemic of chronic opioid use with massive repercussions, and it did not start overnight. Mounting calls for liberalizing narcotic use across a broad range of pain conditions accumulated gradually during the patient-advocacy era of the 1990s, with supporting “evidence” coming mostly from small uncontrolled studies, anecdotal reports, and industry pressure.2 Although cannabis and opioids are not interchangeable, we should be cautious about concluding that cannabis is effective and that it should be used to treat chronic pain.
CHRONIC PAIN IS COMPLICATED
Peripheral neuropathy, by definition, is a chronic pain condition. Unlike acute pain, chronic pain is characterized by biologic, psychologic, and social complexities that require nuance to manage and study.
Such nuance is lacking in most recent reviews of the medical use of cannabis. The conditions in question are often studied as if they were transient and acute, eg, employing short-term studies and rudimentary measures such as numeric pain-rating scales or other snapshots of pain intensity. Results of these shortsighted assessments are impossible to extrapolate to long-term outcomes.
Whether cannabis therapy for chronic pain conditions is sustainable remains to be seen. Outcomes in chronic pain should not be defined simply by pain reduction, but by other dimensions such as changes in pain-related disability and quality of life, development of pharmacologic tolerance or dependence, adverse effects, and other “collateral damage.” We are far from understanding these issues, which require highly controlled and regulated longitudinal studies.
A recent Cochrane review3 of the efficacy of cannabis-based medicines for chronic neuropathic pain found that harms might outweigh the benefits. The quality of evidence was rated as very low to moderate; the reviewers cited small sample sizes and exclusion of important subgroups of patients (eg, those with substance abuse or other psychiatric comorbidities). Such exclusions are the crux of a major problem with cannabis research: studies are not naturalistic. The gritty reality of chronic pain management is paramount, and failing to consider the high-risk biopsychosocial factors typical of patients with chronic pain is naïve and, frankly, dangerous.
COGNITIVE AND MOTIVATIONAL PROBLEMS
The true danger of cannabis lies in what we already know with certainty. As the authors discuss, cannabis undisputedly results in dose-dependent cognitive and motivational problems. If we are preaching physical therapy and home exercise to counter deconditioning, socialization to reverse depression, cognitive-behavioral therapy to increase coping, returning to work to prevent prolonged disability, and other active measures to prevent pain from becoming chronic, then why would we suggest treatments known to blunt motivation, energy, concentration, and overall mood? As a general central nervous system suppressant,4 cannabis works broadly against our best efforts to rehabilitate patients and restore their overall function.
ALL CANNABIS IS NOT THE SAME
The authors use the general term cannabis in their title, yet rightly unpack the differences between medical marijuana, tetrahydrocannabinol (THC), and cannabidiol (CBD). However, in the minds of untrained and pain-stricken patients seeking rapid relief and practical solutions, such distinctions are likely irrelevant.
The danger in the barrage of publications examining cannabis vs medical marijuana vs THC vs CBD is that they all communicate an unintentional yet problematic message: that marijuana of some sort for pain is acceptable to try. And in the face of financial pressures, changing legal landscapes, insurance coverage volatility, and access issues, are patients really going to always secure prescriptions for well-regulated CBD (lacking psychoactive THC) from thoughtful and well-informed physicians, or will they turn to convenient street suppliers?
Simplified perceptions of safety and efficacy across all cannabis products do not help. More troublesome would be to extrapolate safety to other forms of marijuana known to be dangerous, such as synthetic cannabinoids, which in some instances have been associated with catastrophic outcomes.5 The slippery slope is real: if the message becomes that some (or most) marijuana is benign or even therapeutic, what is to curb a widespread and unregulated epidemic?
YOUTH AT RISK
Some groups are more vulnerable than others to the potential negative effects of cannabis. In a study at a medical cannabis dispensary in San Francisco,6 adolescents and young adults used more marijuana than older users did and had higher rates of “use when bored” and eventual pharmacologic dependence. Sustained use of marijuana by young people places them at risk of serious psychiatric disorders, with numerous studies demonstrating the unfolding of schizophrenia, depression, bipolar disorder, and more.7
As the authors point out, cannabis may be contraindicated in those already burdened with mental health problems. If we recall that comorbid psychiatric disorders are the norm rather than the exception in chronic pain conditions,8 can we recommend cannabis therapy for most patients with chronic pain with confidence that it will not cause unintended problems? Evidence already shows that even well-established medical marijuana services attract (and perhaps unintentionally debilitate) a certain high-risk demographic: young, socioeconomically disadvantaged men with other comorbid psychiatric and substance use disorders, who ultimately rank poorly in functional health measures compared with the general population.9
NOT REEFER MADNESS, BUT REEFER CAUTION
I am not advocating the fear-mongering misinformation campaigns of the past. We should not exaggerate and warn about “reefer madness” or equate marijuana with untruths about random violence or complete bedlam. Nonetheless, concerns for widespread amotivation, worsening psychiatric states, chronic disability, and chemical dependence are very real.
Needed are tightly regulated, well-controlled, and long-term prospective studies involving isolated CBD formulations lacking THC. Over time, perhaps only formulations approved by the US Food and Drug Administration will be embraced. In the meantime, more comprehensive approaches should be recommended, such as team-based interdisciplinary rehabilitation programs that have shown efficacy in handling chronic pain complexities.10,11
If such steps are unlikely, physicians should nonetheless stand united in sending a message of cautious optimism regarding medical marijuana, educating their patients not only about recently advertised potential yet inconclusive benefits, but also about the well-known and actual certitudes of its harms for use in chronic pain management. There is plenty of bad and worse information to share with patients, and there is a slippery slope of epidemic proportions to be wary about.
- Modesto-Lowe V, Bojka R, Alvarado C. Cannabis for peripheral neuropathy: The good, the bad, and the unknown. Cleve Clin J Med 2018; 85(12):943–949. doi:10.3949/ccjm.85a.17115
- Wailoo K. Pain: A Political History. Baltimore, MD: Johns Hopkins University Press; 2014.
- Mucke M, Phillips T, Radbruch L, Petzke F, Hauser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev 2018; 3:CD012182. doi:10.1002/14651858.CD012182.pub2
- Lucas CJ, Galettis P, Schneider J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol 2018. Epub ahead of print. doi:10.1111/bcp.13710
- Patel NA, Jerry JM, Jimenez XF, Hantus ST. New-onset refractory status epilepticus associated with the use of synthetic cannabinoids. Psychosomatics 2017; 58(2):180–186. doi:10.1016/j.psym.2016.10.006
- Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn-Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav 2017; 72:14–20. doi:10.1016/j.addbeh.2017.03.006
- Mammen G, Rueda S, Roerecke M, Bonato S, Lev-Ran S, Rehm J. Association of cannabis with long-term clinical symptoms in anxiety and mood disorders: a systematic review of prospective studies. J Clin Psychiatry 2018; 79(4)pii:17r11839. doi:10.4088/JCP.17r11839
- Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry 2017; pii:S0278–5846(17)30194–X. doi:10.1016/j.pnpbp.2017.05.012
- Fischer B, Ialomiteanu AR, Aeby S, Rudzinski K, Kurdyak P, Rehm J. Substance use, health, and functioning characteristics of medical marijuana program participants compared to the general adult population in Ontario (Canada). J Psychoactive Drugs 2017; 49(1):31–38. doi:10.1080/02791072.2016.1264648
- Shah A, Craner J, Cunningham JL. Medical cannabis use among patients with chronic pain in an interdisciplinary pain rehabilitation program: characterization and treatment outcomes. J Subst Abuse Treat 2017; 77:95–100. doi:10.1016/j.jsat.2017.03.012
- Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep 2012; 16(2):147–152. doi:10.1007/s11916-012-0252-4
- Modesto-Lowe V, Bojka R, Alvarado C. Cannabis for peripheral neuropathy: The good, the bad, and the unknown. Cleve Clin J Med 2018; 85(12):943–949. doi:10.3949/ccjm.85a.17115
- Wailoo K. Pain: A Political History. Baltimore, MD: Johns Hopkins University Press; 2014.
- Mucke M, Phillips T, Radbruch L, Petzke F, Hauser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev 2018; 3:CD012182. doi:10.1002/14651858.CD012182.pub2
- Lucas CJ, Galettis P, Schneider J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol 2018. Epub ahead of print. doi:10.1111/bcp.13710
- Patel NA, Jerry JM, Jimenez XF, Hantus ST. New-onset refractory status epilepticus associated with the use of synthetic cannabinoids. Psychosomatics 2017; 58(2):180–186. doi:10.1016/j.psym.2016.10.006
- Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn-Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav 2017; 72:14–20. doi:10.1016/j.addbeh.2017.03.006
- Mammen G, Rueda S, Roerecke M, Bonato S, Lev-Ran S, Rehm J. Association of cannabis with long-term clinical symptoms in anxiety and mood disorders: a systematic review of prospective studies. J Clin Psychiatry 2018; 79(4)pii:17r11839. doi:10.4088/JCP.17r11839
- Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry 2017; pii:S0278–5846(17)30194–X. doi:10.1016/j.pnpbp.2017.05.012
- Fischer B, Ialomiteanu AR, Aeby S, Rudzinski K, Kurdyak P, Rehm J. Substance use, health, and functioning characteristics of medical marijuana program participants compared to the general adult population in Ontario (Canada). J Psychoactive Drugs 2017; 49(1):31–38. doi:10.1080/02791072.2016.1264648
- Shah A, Craner J, Cunningham JL. Medical cannabis use among patients with chronic pain in an interdisciplinary pain rehabilitation program: characterization and treatment outcomes. J Subst Abuse Treat 2017; 77:95–100. doi:10.1016/j.jsat.2017.03.012
- Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep 2012; 16(2):147–152. doi:10.1007/s11916-012-0252-4
Prostate cancer screening
To the Editor: In their article on men’s health,1Chaitoff and colleagues present the scenario of a 60-year-old patient, with no other history given, whose recent screening prostate-specific antigen (PSA) level was 5.1 ng/mL, and who asks his doctor:
- Should I have agreed to the screening?
- How effective is the screening?
- What are the next steps?
These questions are consistent with the patient having read the latest US Preventive Services Task Force (USPSTF) report on PSA screening, which states: “Screening offers a small potential benefit of reducing the chance of death from prostate cancer in some men. However, many men will experience potential harms of screening, including false-positive results…”2
I would tell the patient that he can expect greater benefit from PSA screening than reported by the USPSTF simply by adhering to the screening protocol. Intention-to-treat analysis applied to the trial results diminished the apparent benefits of PSA screening by counting fatal prostate cancers experienced by nonadherent study participants as screening failures.3 In other words, screening works better in those who actually get screened!
The authors state1 that “in 2014, an estimated 172,258 men in the United States were diagnosed with prostate cancer, but only 28,343 men died of it.” Nevertheless, prostate cancer remains the second most common cause of cancer deaths in American men, after lung cancer.4 In addition to the reduction in prostate cancer-specific mortality with screening, patients should consider the reduction in morbidity from painful bone metastases and pathologic fractures, which are common in advanced prostate cancer.
A false-positive elevated PSA can be caused by reversible benign conditions, such as prostate infection or trauma, which can resolve over time, returning the PSA to its baseline level. Studies have demonstrated that simply repeating the PSA test a few weeks later will significantly reduce the number of false-positive PSA screening tests.5
Also, it is not optimal to screen for prostate cancer using a single PSA measurement. This patient’s PSA of 5.1 ng/mL cannot distinguish between chronic benign prostatic hyperplasia and a fast-growing but still curable malignancy. If the patient’s PSA had been tested annually and was known to be stable at its current level, a benign or indolent condition would be most likely, allowing for the possibility of continuing noninvasive observation. If his PSA was 1.1 ng/mL a year ago, and his PSA remains elevated when retested in a few weeks, the likelihood of malignancy would increase, increasing the yield of biopsy.
Lastly, consider false-negatives. A man with a PSA of 2.0 ng/mL would not have undergone biopsy in any of the trials, but if he had a history of several consecutive annual PSA levels less than 1.0 ng/mL, the doubling of his PSA during an interval less than or equal to 1 year could signal an early aggressive prostate cancer. Increases in PSA velocity can reveal the rapid proliferation of malignant prostate cells before the tumor is large enough to cross a static threshold PSA. We have zero data indicating how much benefit can be derived from the use of PSA velocity in this fashion. However, clinicians who carefully track serial PSA changes in each patient have anecdotes of success in early detection and cure of aggressive prostate cancers that would not have been detected by the trial protocols using fixed PSA thresholds. Until such trials are done, we can only tell patients that the ability to compute PSA velocity may be another source of benefit of annual screening of PSA.
- Chaitoff A, Killeen TC, Nielsen C. Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880. doi:10.3949/ccjm.85a.18011
- US Preventive Services Task Force. Prostate cancer: screening. May 2018. www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/prostate-cancer-screening1?ds=1&s=PSA. Accessed November 6, 2018.
- Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res 2011; 2(3):109–112. doi:10.4103/2229-3485.83221
- Cancer.Net. Prostate cancer: statistics. www.cancer.net/cancer-types/prostate-cancer/statistics. Accessed November 6, 2018.
- Lavallée LT, Binette A, Witiuk K, et al. Reducing the harm of prostate cancer screening: repeated prostate-specific antigen testing. Mayo Clin Proc 2016; 91(1):17–22. doi:10.1016/j.mayocp.2015.07.030
To the Editor: In their article on men’s health,1Chaitoff and colleagues present the scenario of a 60-year-old patient, with no other history given, whose recent screening prostate-specific antigen (PSA) level was 5.1 ng/mL, and who asks his doctor:
- Should I have agreed to the screening?
- How effective is the screening?
- What are the next steps?
These questions are consistent with the patient having read the latest US Preventive Services Task Force (USPSTF) report on PSA screening, which states: “Screening offers a small potential benefit of reducing the chance of death from prostate cancer in some men. However, many men will experience potential harms of screening, including false-positive results…”2
I would tell the patient that he can expect greater benefit from PSA screening than reported by the USPSTF simply by adhering to the screening protocol. Intention-to-treat analysis applied to the trial results diminished the apparent benefits of PSA screening by counting fatal prostate cancers experienced by nonadherent study participants as screening failures.3 In other words, screening works better in those who actually get screened!
The authors state1 that “in 2014, an estimated 172,258 men in the United States were diagnosed with prostate cancer, but only 28,343 men died of it.” Nevertheless, prostate cancer remains the second most common cause of cancer deaths in American men, after lung cancer.4 In addition to the reduction in prostate cancer-specific mortality with screening, patients should consider the reduction in morbidity from painful bone metastases and pathologic fractures, which are common in advanced prostate cancer.
A false-positive elevated PSA can be caused by reversible benign conditions, such as prostate infection or trauma, which can resolve over time, returning the PSA to its baseline level. Studies have demonstrated that simply repeating the PSA test a few weeks later will significantly reduce the number of false-positive PSA screening tests.5
Also, it is not optimal to screen for prostate cancer using a single PSA measurement. This patient’s PSA of 5.1 ng/mL cannot distinguish between chronic benign prostatic hyperplasia and a fast-growing but still curable malignancy. If the patient’s PSA had been tested annually and was known to be stable at its current level, a benign or indolent condition would be most likely, allowing for the possibility of continuing noninvasive observation. If his PSA was 1.1 ng/mL a year ago, and his PSA remains elevated when retested in a few weeks, the likelihood of malignancy would increase, increasing the yield of biopsy.
Lastly, consider false-negatives. A man with a PSA of 2.0 ng/mL would not have undergone biopsy in any of the trials, but if he had a history of several consecutive annual PSA levels less than 1.0 ng/mL, the doubling of his PSA during an interval less than or equal to 1 year could signal an early aggressive prostate cancer. Increases in PSA velocity can reveal the rapid proliferation of malignant prostate cells before the tumor is large enough to cross a static threshold PSA. We have zero data indicating how much benefit can be derived from the use of PSA velocity in this fashion. However, clinicians who carefully track serial PSA changes in each patient have anecdotes of success in early detection and cure of aggressive prostate cancers that would not have been detected by the trial protocols using fixed PSA thresholds. Until such trials are done, we can only tell patients that the ability to compute PSA velocity may be another source of benefit of annual screening of PSA.
To the Editor: In their article on men’s health,1Chaitoff and colleagues present the scenario of a 60-year-old patient, with no other history given, whose recent screening prostate-specific antigen (PSA) level was 5.1 ng/mL, and who asks his doctor:
- Should I have agreed to the screening?
- How effective is the screening?
- What are the next steps?
These questions are consistent with the patient having read the latest US Preventive Services Task Force (USPSTF) report on PSA screening, which states: “Screening offers a small potential benefit of reducing the chance of death from prostate cancer in some men. However, many men will experience potential harms of screening, including false-positive results…”2
I would tell the patient that he can expect greater benefit from PSA screening than reported by the USPSTF simply by adhering to the screening protocol. Intention-to-treat analysis applied to the trial results diminished the apparent benefits of PSA screening by counting fatal prostate cancers experienced by nonadherent study participants as screening failures.3 In other words, screening works better in those who actually get screened!
The authors state1 that “in 2014, an estimated 172,258 men in the United States were diagnosed with prostate cancer, but only 28,343 men died of it.” Nevertheless, prostate cancer remains the second most common cause of cancer deaths in American men, after lung cancer.4 In addition to the reduction in prostate cancer-specific mortality with screening, patients should consider the reduction in morbidity from painful bone metastases and pathologic fractures, which are common in advanced prostate cancer.
A false-positive elevated PSA can be caused by reversible benign conditions, such as prostate infection or trauma, which can resolve over time, returning the PSA to its baseline level. Studies have demonstrated that simply repeating the PSA test a few weeks later will significantly reduce the number of false-positive PSA screening tests.5
Also, it is not optimal to screen for prostate cancer using a single PSA measurement. This patient’s PSA of 5.1 ng/mL cannot distinguish between chronic benign prostatic hyperplasia and a fast-growing but still curable malignancy. If the patient’s PSA had been tested annually and was known to be stable at its current level, a benign or indolent condition would be most likely, allowing for the possibility of continuing noninvasive observation. If his PSA was 1.1 ng/mL a year ago, and his PSA remains elevated when retested in a few weeks, the likelihood of malignancy would increase, increasing the yield of biopsy.
Lastly, consider false-negatives. A man with a PSA of 2.0 ng/mL would not have undergone biopsy in any of the trials, but if he had a history of several consecutive annual PSA levels less than 1.0 ng/mL, the doubling of his PSA during an interval less than or equal to 1 year could signal an early aggressive prostate cancer. Increases in PSA velocity can reveal the rapid proliferation of malignant prostate cells before the tumor is large enough to cross a static threshold PSA. We have zero data indicating how much benefit can be derived from the use of PSA velocity in this fashion. However, clinicians who carefully track serial PSA changes in each patient have anecdotes of success in early detection and cure of aggressive prostate cancers that would not have been detected by the trial protocols using fixed PSA thresholds. Until such trials are done, we can only tell patients that the ability to compute PSA velocity may be another source of benefit of annual screening of PSA.
- Chaitoff A, Killeen TC, Nielsen C. Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880. doi:10.3949/ccjm.85a.18011
- US Preventive Services Task Force. Prostate cancer: screening. May 2018. www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/prostate-cancer-screening1?ds=1&s=PSA. Accessed November 6, 2018.
- Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res 2011; 2(3):109–112. doi:10.4103/2229-3485.83221
- Cancer.Net. Prostate cancer: statistics. www.cancer.net/cancer-types/prostate-cancer/statistics. Accessed November 6, 2018.
- Lavallée LT, Binette A, Witiuk K, et al. Reducing the harm of prostate cancer screening: repeated prostate-specific antigen testing. Mayo Clin Proc 2016; 91(1):17–22. doi:10.1016/j.mayocp.2015.07.030
- Chaitoff A, Killeen TC, Nielsen C. Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880. doi:10.3949/ccjm.85a.18011
- US Preventive Services Task Force. Prostate cancer: screening. May 2018. www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/prostate-cancer-screening1?ds=1&s=PSA. Accessed November 6, 2018.
- Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res 2011; 2(3):109–112. doi:10.4103/2229-3485.83221
- Cancer.Net. Prostate cancer: statistics. www.cancer.net/cancer-types/prostate-cancer/statistics. Accessed November 6, 2018.
- Lavallée LT, Binette A, Witiuk K, et al. Reducing the harm of prostate cancer screening: repeated prostate-specific antigen testing. Mayo Clin Proc 2016; 91(1):17–22. doi:10.1016/j.mayocp.2015.07.030
Correction: Men’s health 2018
In the article by Chaitoff et al (Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880, doi:10.3949/ccjm.85a.18011), the prostate-specific antigen level of a 60-year-old man was given as 5.1 mg/dL. The unit of measure should have been 5.1 ng/mL. This has been corrected online.
In the article by Chaitoff et al (Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880, doi:10.3949/ccjm.85a.18011), the prostate-specific antigen level of a 60-year-old man was given as 5.1 mg/dL. The unit of measure should have been 5.1 ng/mL. This has been corrected online.
In the article by Chaitoff et al (Men’s health 2018: BPH, prostate cancer, erectile dysfunction, supplements. Cleve Clin J Med 2018; 85(11):871–880, doi:10.3949/ccjm.85a.18011), the prostate-specific antigen level of a 60-year-old man was given as 5.1 mg/dL. The unit of measure should have been 5.1 ng/mL. This has been corrected online.
Cognitive tests and flawed results
Also today, disease-modifying anti-rheumatic drugs improve vascular abnormalities in early RA, mandating insurance coverage of PrEP for HIV prevention, and polycystic ovary syndrome is linked to increased cancer risk in pre-menopausal women.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, disease-modifying anti-rheumatic drugs improve vascular abnormalities in early RA, mandating insurance coverage of PrEP for HIV prevention, and polycystic ovary syndrome is linked to increased cancer risk in pre-menopausal women.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, disease-modifying anti-rheumatic drugs improve vascular abnormalities in early RA, mandating insurance coverage of PrEP for HIV prevention, and polycystic ovary syndrome is linked to increased cancer risk in pre-menopausal women.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Luspatercept reduced transfusion burden in MDS patients
SAN DIEGO—Results of the randomized, phase 3 Medalist trial show that the erythroid maturation agent luspatercept can reduce transfusion burden in patients with anemia due to myelodysplastic syndromes (MDS) and ring sideroblasts.
Almost 38% of luspatercept-treated patients achieved red blood cell (RBC) transfusion independence for 8 weeks or more, compared with 13% of patients receiving placebo.
And 28% of luspatercept-treated patients achieved transfusion independence for 12 weeks or more, compared to 8% in the placebo group.
Investigators reported these results as abstract 1 at the 2018 ASH Annual Meeting.
Treatment with luspatercept was “very well tolerated,” and responses were durable, with approximately 40% of patients remaining transfusion-free after 1 year of therapy, said senior investigator Alan F. List, MD, of Moffitt Cancer Center in Tampa, Florida, during a press conference at the meeting.
The first-in-class erythroid maturation agent is being developed as a treatment for anemia related to MDS and beta-thalassemia, Dr. List said.
“Luspatercept is a potential new therapy that we think could be very effective in patients with lower-risk MDS with ring sideroblasts who are red blood cell transfusion-dependent,” Dr. List affirmed.
Luspatercept is a soluble receptor chimera that binds to an array of ligands in the TGF-β superfamily, which is known to be very important in suppressing erythropoiesis in patients with MDS, Dr. List noted.
The Medalist study (NCT02631070) included patients with very low-, low-, or intermediate-risk disease and ring sideroblasts who were RBC transfusion-dependent and were refractory to, unresponsive to, or ineligible for first-line treatment with an erythropoiesis-stimulating agent (ESA).
A total of 153 patients were randomized to receive luspatercept at 1.0 mg/kg, administered subcutaneously every 21 days for at least 24 weeks, while 76 were randomized to placebo every 21 days.
The primary endpoint was the proportion of patients achieving RBC transfusion independence for at least 8 weeks during the first 24 weeks of treatment.
The primary endpoint was achieved by 37.9% of luspatercept-treated patients and 13.2% of placebo-treated patients (P<0.0001).
The luspatercept-treated patients also had a higher rate of erythroid response compared with the placebo group, at 52.9% and 11.8%, respectively (P<0.0001).
The investigators reported no differences in treatment-emergent adverse events, severe adverse events, or frequency of progression of acute myeloid leukemia (AML).
The safety profile was consistent with that of the phase 2 PACE-MDS study, which included treatment-related grade 3 myalgia (2%), increased blast cell count (2%), and general physical health deterioration (2%).
“This was a very clean drug and a very safe drug,” Dr. List said.
The decision to study luspatercept in patients with ring sideroblasts was based on results of the phase 2 PACE study showing a higher response rate in that subset of MDS patients, according to Dr. List.
The PACE study also included a small number of patients who had not previously received an ESA.
Currently underway is a phase 3 trial (NCT03682536) investigating luspatercept in ESA-naïve lower-risk MDS patients with anemia who require RBC transfusions.
Luspatercept would be a useful therapy to have in clinic for patients with ring sideroblasts, which represent about 25% of patients overall, according to MDS expert David Steensma, MD, of Dana-Farber Cancer Institute and Harvard Medical School in Boston, Massachusetts.
“It’s been 12 years since we had an FDA-approved drug in MDS, and there have been 7 in acute myeloid leukemia in the last year and a half, so it’s our turn, I think,” said Dr. Steensma, who moderated the press conference.
The Medalist study was sponsored by Celgene in collaboration with Acceleron Pharma, Inc.
Dr. List reported research funding from Celgene.
SAN DIEGO—Results of the randomized, phase 3 Medalist trial show that the erythroid maturation agent luspatercept can reduce transfusion burden in patients with anemia due to myelodysplastic syndromes (MDS) and ring sideroblasts.
Almost 38% of luspatercept-treated patients achieved red blood cell (RBC) transfusion independence for 8 weeks or more, compared with 13% of patients receiving placebo.
And 28% of luspatercept-treated patients achieved transfusion independence for 12 weeks or more, compared to 8% in the placebo group.
Investigators reported these results as abstract 1 at the 2018 ASH Annual Meeting.
Treatment with luspatercept was “very well tolerated,” and responses were durable, with approximately 40% of patients remaining transfusion-free after 1 year of therapy, said senior investigator Alan F. List, MD, of Moffitt Cancer Center in Tampa, Florida, during a press conference at the meeting.
The first-in-class erythroid maturation agent is being developed as a treatment for anemia related to MDS and beta-thalassemia, Dr. List said.
“Luspatercept is a potential new therapy that we think could be very effective in patients with lower-risk MDS with ring sideroblasts who are red blood cell transfusion-dependent,” Dr. List affirmed.
Luspatercept is a soluble receptor chimera that binds to an array of ligands in the TGF-β superfamily, which is known to be very important in suppressing erythropoiesis in patients with MDS, Dr. List noted.
The Medalist study (NCT02631070) included patients with very low-, low-, or intermediate-risk disease and ring sideroblasts who were RBC transfusion-dependent and were refractory to, unresponsive to, or ineligible for first-line treatment with an erythropoiesis-stimulating agent (ESA).
A total of 153 patients were randomized to receive luspatercept at 1.0 mg/kg, administered subcutaneously every 21 days for at least 24 weeks, while 76 were randomized to placebo every 21 days.
The primary endpoint was the proportion of patients achieving RBC transfusion independence for at least 8 weeks during the first 24 weeks of treatment.
The primary endpoint was achieved by 37.9% of luspatercept-treated patients and 13.2% of placebo-treated patients (P<0.0001).
The luspatercept-treated patients also had a higher rate of erythroid response compared with the placebo group, at 52.9% and 11.8%, respectively (P<0.0001).
The investigators reported no differences in treatment-emergent adverse events, severe adverse events, or frequency of progression of acute myeloid leukemia (AML).
The safety profile was consistent with that of the phase 2 PACE-MDS study, which included treatment-related grade 3 myalgia (2%), increased blast cell count (2%), and general physical health deterioration (2%).
“This was a very clean drug and a very safe drug,” Dr. List said.
The decision to study luspatercept in patients with ring sideroblasts was based on results of the phase 2 PACE study showing a higher response rate in that subset of MDS patients, according to Dr. List.
The PACE study also included a small number of patients who had not previously received an ESA.
Currently underway is a phase 3 trial (NCT03682536) investigating luspatercept in ESA-naïve lower-risk MDS patients with anemia who require RBC transfusions.
Luspatercept would be a useful therapy to have in clinic for patients with ring sideroblasts, which represent about 25% of patients overall, according to MDS expert David Steensma, MD, of Dana-Farber Cancer Institute and Harvard Medical School in Boston, Massachusetts.
“It’s been 12 years since we had an FDA-approved drug in MDS, and there have been 7 in acute myeloid leukemia in the last year and a half, so it’s our turn, I think,” said Dr. Steensma, who moderated the press conference.
The Medalist study was sponsored by Celgene in collaboration with Acceleron Pharma, Inc.
Dr. List reported research funding from Celgene.
SAN DIEGO—Results of the randomized, phase 3 Medalist trial show that the erythroid maturation agent luspatercept can reduce transfusion burden in patients with anemia due to myelodysplastic syndromes (MDS) and ring sideroblasts.
Almost 38% of luspatercept-treated patients achieved red blood cell (RBC) transfusion independence for 8 weeks or more, compared with 13% of patients receiving placebo.
And 28% of luspatercept-treated patients achieved transfusion independence for 12 weeks or more, compared to 8% in the placebo group.
Investigators reported these results as abstract 1 at the 2018 ASH Annual Meeting.
Treatment with luspatercept was “very well tolerated,” and responses were durable, with approximately 40% of patients remaining transfusion-free after 1 year of therapy, said senior investigator Alan F. List, MD, of Moffitt Cancer Center in Tampa, Florida, during a press conference at the meeting.
The first-in-class erythroid maturation agent is being developed as a treatment for anemia related to MDS and beta-thalassemia, Dr. List said.
“Luspatercept is a potential new therapy that we think could be very effective in patients with lower-risk MDS with ring sideroblasts who are red blood cell transfusion-dependent,” Dr. List affirmed.
Luspatercept is a soluble receptor chimera that binds to an array of ligands in the TGF-β superfamily, which is known to be very important in suppressing erythropoiesis in patients with MDS, Dr. List noted.
The Medalist study (NCT02631070) included patients with very low-, low-, or intermediate-risk disease and ring sideroblasts who were RBC transfusion-dependent and were refractory to, unresponsive to, or ineligible for first-line treatment with an erythropoiesis-stimulating agent (ESA).
A total of 153 patients were randomized to receive luspatercept at 1.0 mg/kg, administered subcutaneously every 21 days for at least 24 weeks, while 76 were randomized to placebo every 21 days.
The primary endpoint was the proportion of patients achieving RBC transfusion independence for at least 8 weeks during the first 24 weeks of treatment.
The primary endpoint was achieved by 37.9% of luspatercept-treated patients and 13.2% of placebo-treated patients (P<0.0001).
The luspatercept-treated patients also had a higher rate of erythroid response compared with the placebo group, at 52.9% and 11.8%, respectively (P<0.0001).
The investigators reported no differences in treatment-emergent adverse events, severe adverse events, or frequency of progression of acute myeloid leukemia (AML).
The safety profile was consistent with that of the phase 2 PACE-MDS study, which included treatment-related grade 3 myalgia (2%), increased blast cell count (2%), and general physical health deterioration (2%).
“This was a very clean drug and a very safe drug,” Dr. List said.
The decision to study luspatercept in patients with ring sideroblasts was based on results of the phase 2 PACE study showing a higher response rate in that subset of MDS patients, according to Dr. List.
The PACE study also included a small number of patients who had not previously received an ESA.
Currently underway is a phase 3 trial (NCT03682536) investigating luspatercept in ESA-naïve lower-risk MDS patients with anemia who require RBC transfusions.
Luspatercept would be a useful therapy to have in clinic for patients with ring sideroblasts, which represent about 25% of patients overall, according to MDS expert David Steensma, MD, of Dana-Farber Cancer Institute and Harvard Medical School in Boston, Massachusetts.
“It’s been 12 years since we had an FDA-approved drug in MDS, and there have been 7 in acute myeloid leukemia in the last year and a half, so it’s our turn, I think,” said Dr. Steensma, who moderated the press conference.
The Medalist study was sponsored by Celgene in collaboration with Acceleron Pharma, Inc.
Dr. List reported research funding from Celgene.
New VTE guidelines include over 150 recommendations
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.