User login
Change is upon us
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
New HHS physical activity guidelines break fresh ground
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Children with poor cardiorespiratory fitness have a higher risk of type 2 diabetes and cardiovascular disease
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
FROM THE SCANDINAVIAN JOURNAL OF MEDICINE & SCIENCE IN SPORTS
Key clinical point: Peak oxygen uptake less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
Major finding: Cardiorespiratory fitness scaled by body mass could be used to screen for cardiometabolic risk in children.
Study details: An analysis of 352 Finnish children, all aged 9-11 years, who took a maximal exercise test as part of an ongoing physical activity and dietary intervention study.
Disclosures: The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area, Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
Source: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
Congenital Syphilis Is on the Rise
Diagnoses of primary and secondary syphilis, the most infectious stages of the disease, jumped 76% from 2013 to 2017. And reported cases of congenital syphilis—passed from mother to infant during pregnancy—rose 44% between 2016 and 2017, from 16 cases to 23 cases per 100,000 live births, according to the CDC’s annual Sexually Transmitted Disease Surveillance Report. Those data highlight the need for better prenatal care that includes syphilis testing at the first visit and follow-up testing for women at high risk of the infection, the CDC says. Syphilis can cause miscarriage, newborn death, and severe lifelong physical and mental health problems.
The 918 cases reported in 2017 represent the highest number of recorded cases in 20 years. Cases were reported in 37 states, primarily western and southern states. The report notes that the surge in cases parallels similar increases in syphilis among women of reproductive age and outpaces national increases in sexually transmitted dieseases (STDs) overall.
Syphilis during pregnancy is easily cured with the right antibiotics. Left untreated, a pregnant woman with syphilis has as much as an 80% chance of passing it to the baby.
Early testing, prompt treatment, and follow-up are key. Recent CDC research found that 1 in 3 women who gave birth to a baby with syphilis in 2016 had in fact been tested during pregnancy but either acquired syphilis after that test or was not treated in time to cure the infection in the fetus.
“Too many women are falling through the cracks of the system,” said Gail Bolan, MD, director of the CDC’s Division of STD Prevention. The CDC recommends that all pregnant women be treated for syphilis at the first prenatal visit. But for many women, 1 test may not be enough. Woman at high risk, or those who live in high-prevalence areas, should be tested again early in the third trimester and at delivery.
“To protect every baby,” Bolan says, “we have to start by protecting every mother.”
Diagnoses of primary and secondary syphilis, the most infectious stages of the disease, jumped 76% from 2013 to 2017. And reported cases of congenital syphilis—passed from mother to infant during pregnancy—rose 44% between 2016 and 2017, from 16 cases to 23 cases per 100,000 live births, according to the CDC’s annual Sexually Transmitted Disease Surveillance Report. Those data highlight the need for better prenatal care that includes syphilis testing at the first visit and follow-up testing for women at high risk of the infection, the CDC says. Syphilis can cause miscarriage, newborn death, and severe lifelong physical and mental health problems.
The 918 cases reported in 2017 represent the highest number of recorded cases in 20 years. Cases were reported in 37 states, primarily western and southern states. The report notes that the surge in cases parallels similar increases in syphilis among women of reproductive age and outpaces national increases in sexually transmitted dieseases (STDs) overall.
Syphilis during pregnancy is easily cured with the right antibiotics. Left untreated, a pregnant woman with syphilis has as much as an 80% chance of passing it to the baby.
Early testing, prompt treatment, and follow-up are key. Recent CDC research found that 1 in 3 women who gave birth to a baby with syphilis in 2016 had in fact been tested during pregnancy but either acquired syphilis after that test or was not treated in time to cure the infection in the fetus.
“Too many women are falling through the cracks of the system,” said Gail Bolan, MD, director of the CDC’s Division of STD Prevention. The CDC recommends that all pregnant women be treated for syphilis at the first prenatal visit. But for many women, 1 test may not be enough. Woman at high risk, or those who live in high-prevalence areas, should be tested again early in the third trimester and at delivery.
“To protect every baby,” Bolan says, “we have to start by protecting every mother.”
Diagnoses of primary and secondary syphilis, the most infectious stages of the disease, jumped 76% from 2013 to 2017. And reported cases of congenital syphilis—passed from mother to infant during pregnancy—rose 44% between 2016 and 2017, from 16 cases to 23 cases per 100,000 live births, according to the CDC’s annual Sexually Transmitted Disease Surveillance Report. Those data highlight the need for better prenatal care that includes syphilis testing at the first visit and follow-up testing for women at high risk of the infection, the CDC says. Syphilis can cause miscarriage, newborn death, and severe lifelong physical and mental health problems.
The 918 cases reported in 2017 represent the highest number of recorded cases in 20 years. Cases were reported in 37 states, primarily western and southern states. The report notes that the surge in cases parallels similar increases in syphilis among women of reproductive age and outpaces national increases in sexually transmitted dieseases (STDs) overall.
Syphilis during pregnancy is easily cured with the right antibiotics. Left untreated, a pregnant woman with syphilis has as much as an 80% chance of passing it to the baby.
Early testing, prompt treatment, and follow-up are key. Recent CDC research found that 1 in 3 women who gave birth to a baby with syphilis in 2016 had in fact been tested during pregnancy but either acquired syphilis after that test or was not treated in time to cure the infection in the fetus.
“Too many women are falling through the cracks of the system,” said Gail Bolan, MD, director of the CDC’s Division of STD Prevention. The CDC recommends that all pregnant women be treated for syphilis at the first prenatal visit. But for many women, 1 test may not be enough. Woman at high risk, or those who live in high-prevalence areas, should be tested again early in the third trimester and at delivery.
“To protect every baby,” Bolan says, “we have to start by protecting every mother.”
Obesity curbs decades of CVD progress
Also today, there is an increased risk of atrial fibrillation with migraine aura, adjunctive testosterone may reduce depressive symptoms in men, and the American Academy of Pediatrics advises moderate physical and cognitive activity after sports concussions.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there is an increased risk of atrial fibrillation with migraine aura, adjunctive testosterone may reduce depressive symptoms in men, and the American Academy of Pediatrics advises moderate physical and cognitive activity after sports concussions.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there is an increased risk of atrial fibrillation with migraine aura, adjunctive testosterone may reduce depressive symptoms in men, and the American Academy of Pediatrics advises moderate physical and cognitive activity after sports concussions.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Are Doctors Willing to PrEP Young Patients?
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
In 2015, young people aged 13 to 24 years—disproportionately young men and boys—accounted for 23% of new HIV infections. Pre-exposure prophylaxis (PrEP) can prevent HIV, and has been found safe and effective for young people, but are health care providers who treat adolescents willing to prescribe it?
Researchers from University of California, San Francisco say internal medicine and infectious disease providers have expressed concerns about adherence, development of resistant HIV strains, higher risk sexual behavior, cost, toxicity, and lack of evidence. Data are lacking, though, among youth providers. To find out how aware those clinicians are about PrEP, and how willing they are to prescribe it, the researchers conducted an online survey of members of the Society of Adolescent Health and Medicine.
Almost all of the 162 respondents had heard of PrEP, and agreed that it prevents HIV. Of the respondents, 57 (35%) had prescribed PrEP. Although 73% said they had treated few to no young patients with HIV, 65% were willing to prescribe PrEP to adolescents (aged 13-17 years) and young adults. Only 30 providers said they would refer adolescents and 25 would refer young adults.
Among the providers who would refer or were not willing to prescribe to adolescents, 35 (67%) would prescribe PrEP if it were FDA-approved for adolescents.
Willingness to prescribe was associated with the provider having enough knowledge to safely provide PrEP to adolescents and a belief that adolescents would adhere to a daily medication regimen. Some also said they would prefer to know that they could ensure confidentiality.
The researchers say their findings highlight potential opportunities to reduce HIV incidence among young people by shaping educational and implementation tools to improve provider self-efficacy and youth adherence.
R-CHOP effective as first-line treatment in FL
Long-term data suggest R-CHOP can be effective as first-line treatment for patients with follicular lymphoma (FL).
In a phase 2-3 trial, investigators compared R-CHOP-21 and R-CHOP-14 in a cohort of patients with indolent lymphomas, most of whom had FL.
Ten-year survival rates were similar between the R-CHOP-21 and R-CHOP-14 groups, with progression-free survival (PFS) rates of 33% and 39%, respectively, and overall survival (OS) rates of 81% and 85%, respectively.
The investigators did note that 9% of patients in each treatment group developed secondary malignancies, and grade 3 infections were a concern as well.
Takashi Watanabe, MD, PhD, of Mie University in Japan, and his colleagues reported these results in The Lancet Haematology.
The trial (JCOG0203) included 300 patients with stage III or IV indolent B-cell lymphomas from 44 Japanese hospitals.
Most patients (n=248) had grade 1-3a FL, 17 had grade 3b FL, 6 had marginal zone lymphoma, 6 had diffuse large B-cell lymphoma, 4 had mantle cell lymphoma, 2 had small lymphocytic lymphoma, 1 had plasmacytoma, 13 had other indolent B-cell lymphomas, and 3 had other lymphomas.
The patients were randomly assigned to receive six cycles of R-CHOP 21 (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone every 3 weeks) or R-CHOP 14 (R-CHOP every 2 weeks with granulocyte-colony stimulating factor support). Neither group received rituximab maintenance.
Overall results
The median follow-up was 11.2 years (interquartile range, 10.1 to 12.7 years).
The 10-year PFS was 33% in the R-CHOP-21 group and 39% in the R-CHOP-14 group (hazard ratio=0.89). The 10-year OS was 81% and 85%, respectively (hazard ratio=0.87).
At 10 years, the incidence of secondary malignancies was 9% in both the R-CHOP-21 group (14/148) and the R-CHOP-14 group (14/151).
The most frequent solid tumor malignancies were stomach (n=5), lung (n=4), colon (n=3), bladder (n=2), and prostate (n=2) cancers. Hematologic malignancies included myelodysplastic syndromes (n=6), acute myeloid leukemia (n=2), acute lymphoblastic leukemia (n=1), and chronic myeloid leukemia (n=1).
There were nine deaths from secondary malignancies, four in the R-CHOP-21 group and five in the R-CHOP-14 group.
The rate of grade 3 adverse events was 18% (n=53) for the entire cohort. Grade 3 infections occurred in 23% of the R-CHOP-21 group and 12% of the R-CHOP-14 group.
Focus on grade 1-3a FL
Among the 248 patients with grade 1-3a FL, the PFS (for both treatment groups) was 45% at 5 years, 39% at 8 years, and 36% at 10 years. The OS was 94% at 5 years, 87% at 8 years, and 85% at 10 years.
Histological transformation was observed in 11% of the patients who had grade 1-3a FL at enrollment. The cumulative incidence of histological transformation was 2.4% at 3 years, 3.2% at 5 years, 8.5% at 8 years, and 9.3% at 10 years.
Secondary malignancies occurred in 10% (12/125) of the R-CHOP-21 group and 11% (13/123) of the R-CHOP-14 group.
The cumulative incidence of hematologic secondary malignancies at 10 years was 2.9%.
The investigators noted that the actual incidence of secondary solid tumors or hematologic malignancies apart from the setting of autologous stem cell transplants is not known. They emphasized that patients should be followed beyond 10 years to ensure the risk of secondary malignancies is not underestimated.
“Clinicians choosing a first-line treatment for patients with follicular lymphoma should be cautious of secondary malignancies caused by immunochemotherapy and severe complications of infectious diseases in the long-term follow-up—both of which could lead to death,” the investigators wrote.
This study was supported by the Ministry of Health, Labour and Welfare of Japan and the National Cancer Center Research and Development Fund of Japan.
Dr. Wantanabe has received honoraria from Bristol-Myers Squibb, Takeda, Taisho Toyama, Celgene, Nippon Shinyaku, and Novartis and funding resources from TakaraBio and United Immunity to support the Department of Immuno-Gene Therapy at Mie University. Multiple co-authors reported similar relationships.
Long-term data suggest R-CHOP can be effective as first-line treatment for patients with follicular lymphoma (FL).
In a phase 2-3 trial, investigators compared R-CHOP-21 and R-CHOP-14 in a cohort of patients with indolent lymphomas, most of whom had FL.
Ten-year survival rates were similar between the R-CHOP-21 and R-CHOP-14 groups, with progression-free survival (PFS) rates of 33% and 39%, respectively, and overall survival (OS) rates of 81% and 85%, respectively.
The investigators did note that 9% of patients in each treatment group developed secondary malignancies, and grade 3 infections were a concern as well.
Takashi Watanabe, MD, PhD, of Mie University in Japan, and his colleagues reported these results in The Lancet Haematology.
The trial (JCOG0203) included 300 patients with stage III or IV indolent B-cell lymphomas from 44 Japanese hospitals.
Most patients (n=248) had grade 1-3a FL, 17 had grade 3b FL, 6 had marginal zone lymphoma, 6 had diffuse large B-cell lymphoma, 4 had mantle cell lymphoma, 2 had small lymphocytic lymphoma, 1 had plasmacytoma, 13 had other indolent B-cell lymphomas, and 3 had other lymphomas.
The patients were randomly assigned to receive six cycles of R-CHOP 21 (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone every 3 weeks) or R-CHOP 14 (R-CHOP every 2 weeks with granulocyte-colony stimulating factor support). Neither group received rituximab maintenance.
Overall results
The median follow-up was 11.2 years (interquartile range, 10.1 to 12.7 years).
The 10-year PFS was 33% in the R-CHOP-21 group and 39% in the R-CHOP-14 group (hazard ratio=0.89). The 10-year OS was 81% and 85%, respectively (hazard ratio=0.87).
At 10 years, the incidence of secondary malignancies was 9% in both the R-CHOP-21 group (14/148) and the R-CHOP-14 group (14/151).
The most frequent solid tumor malignancies were stomach (n=5), lung (n=4), colon (n=3), bladder (n=2), and prostate (n=2) cancers. Hematologic malignancies included myelodysplastic syndromes (n=6), acute myeloid leukemia (n=2), acute lymphoblastic leukemia (n=1), and chronic myeloid leukemia (n=1).
There were nine deaths from secondary malignancies, four in the R-CHOP-21 group and five in the R-CHOP-14 group.
The rate of grade 3 adverse events was 18% (n=53) for the entire cohort. Grade 3 infections occurred in 23% of the R-CHOP-21 group and 12% of the R-CHOP-14 group.
Focus on grade 1-3a FL
Among the 248 patients with grade 1-3a FL, the PFS (for both treatment groups) was 45% at 5 years, 39% at 8 years, and 36% at 10 years. The OS was 94% at 5 years, 87% at 8 years, and 85% at 10 years.
Histological transformation was observed in 11% of the patients who had grade 1-3a FL at enrollment. The cumulative incidence of histological transformation was 2.4% at 3 years, 3.2% at 5 years, 8.5% at 8 years, and 9.3% at 10 years.
Secondary malignancies occurred in 10% (12/125) of the R-CHOP-21 group and 11% (13/123) of the R-CHOP-14 group.
The cumulative incidence of hematologic secondary malignancies at 10 years was 2.9%.
The investigators noted that the actual incidence of secondary solid tumors or hematologic malignancies apart from the setting of autologous stem cell transplants is not known. They emphasized that patients should be followed beyond 10 years to ensure the risk of secondary malignancies is not underestimated.
“Clinicians choosing a first-line treatment for patients with follicular lymphoma should be cautious of secondary malignancies caused by immunochemotherapy and severe complications of infectious diseases in the long-term follow-up—both of which could lead to death,” the investigators wrote.
This study was supported by the Ministry of Health, Labour and Welfare of Japan and the National Cancer Center Research and Development Fund of Japan.
Dr. Wantanabe has received honoraria from Bristol-Myers Squibb, Takeda, Taisho Toyama, Celgene, Nippon Shinyaku, and Novartis and funding resources from TakaraBio and United Immunity to support the Department of Immuno-Gene Therapy at Mie University. Multiple co-authors reported similar relationships.
Long-term data suggest R-CHOP can be effective as first-line treatment for patients with follicular lymphoma (FL).
In a phase 2-3 trial, investigators compared R-CHOP-21 and R-CHOP-14 in a cohort of patients with indolent lymphomas, most of whom had FL.
Ten-year survival rates were similar between the R-CHOP-21 and R-CHOP-14 groups, with progression-free survival (PFS) rates of 33% and 39%, respectively, and overall survival (OS) rates of 81% and 85%, respectively.
The investigators did note that 9% of patients in each treatment group developed secondary malignancies, and grade 3 infections were a concern as well.
Takashi Watanabe, MD, PhD, of Mie University in Japan, and his colleagues reported these results in The Lancet Haematology.
The trial (JCOG0203) included 300 patients with stage III or IV indolent B-cell lymphomas from 44 Japanese hospitals.
Most patients (n=248) had grade 1-3a FL, 17 had grade 3b FL, 6 had marginal zone lymphoma, 6 had diffuse large B-cell lymphoma, 4 had mantle cell lymphoma, 2 had small lymphocytic lymphoma, 1 had plasmacytoma, 13 had other indolent B-cell lymphomas, and 3 had other lymphomas.
The patients were randomly assigned to receive six cycles of R-CHOP 21 (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone every 3 weeks) or R-CHOP 14 (R-CHOP every 2 weeks with granulocyte-colony stimulating factor support). Neither group received rituximab maintenance.
Overall results
The median follow-up was 11.2 years (interquartile range, 10.1 to 12.7 years).
The 10-year PFS was 33% in the R-CHOP-21 group and 39% in the R-CHOP-14 group (hazard ratio=0.89). The 10-year OS was 81% and 85%, respectively (hazard ratio=0.87).
At 10 years, the incidence of secondary malignancies was 9% in both the R-CHOP-21 group (14/148) and the R-CHOP-14 group (14/151).
The most frequent solid tumor malignancies were stomach (n=5), lung (n=4), colon (n=3), bladder (n=2), and prostate (n=2) cancers. Hematologic malignancies included myelodysplastic syndromes (n=6), acute myeloid leukemia (n=2), acute lymphoblastic leukemia (n=1), and chronic myeloid leukemia (n=1).
There were nine deaths from secondary malignancies, four in the R-CHOP-21 group and five in the R-CHOP-14 group.
The rate of grade 3 adverse events was 18% (n=53) for the entire cohort. Grade 3 infections occurred in 23% of the R-CHOP-21 group and 12% of the R-CHOP-14 group.
Focus on grade 1-3a FL
Among the 248 patients with grade 1-3a FL, the PFS (for both treatment groups) was 45% at 5 years, 39% at 8 years, and 36% at 10 years. The OS was 94% at 5 years, 87% at 8 years, and 85% at 10 years.
Histological transformation was observed in 11% of the patients who had grade 1-3a FL at enrollment. The cumulative incidence of histological transformation was 2.4% at 3 years, 3.2% at 5 years, 8.5% at 8 years, and 9.3% at 10 years.
Secondary malignancies occurred in 10% (12/125) of the R-CHOP-21 group and 11% (13/123) of the R-CHOP-14 group.
The cumulative incidence of hematologic secondary malignancies at 10 years was 2.9%.
The investigators noted that the actual incidence of secondary solid tumors or hematologic malignancies apart from the setting of autologous stem cell transplants is not known. They emphasized that patients should be followed beyond 10 years to ensure the risk of secondary malignancies is not underestimated.
“Clinicians choosing a first-line treatment for patients with follicular lymphoma should be cautious of secondary malignancies caused by immunochemotherapy and severe complications of infectious diseases in the long-term follow-up—both of which could lead to death,” the investigators wrote.
This study was supported by the Ministry of Health, Labour and Welfare of Japan and the National Cancer Center Research and Development Fund of Japan.
Dr. Wantanabe has received honoraria from Bristol-Myers Squibb, Takeda, Taisho Toyama, Celgene, Nippon Shinyaku, and Novartis and funding resources from TakaraBio and United Immunity to support the Department of Immuno-Gene Therapy at Mie University. Multiple co-authors reported similar relationships.
FDA approves generic drugs for APL
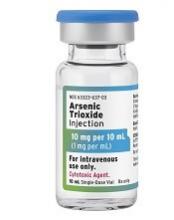
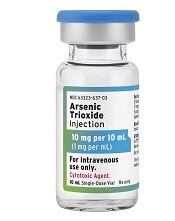
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.
FDA approves generic decitabine for MDS
The U.S. Food and Drug Administration has approved Lupin’s decitabine product, a generic version of Otsuka Pharmaceutical Co. Ltd.’s Dacogen, to treat patients with myelodysplastic syndromes (MDS).
Lupin’s decitabine for injection (50 mg, single-dose vial) is approved to treat patients with intermediate-1, intermediate-2, and high-risk MDS.
This includes previously treated, untreated, de novo, and secondary MDS of all French-American-British subtypes—refractory anemia, refractory anemia with ringed sideroblasts, refractory anemia with excess blasts, refractory anemia with excess blasts in transformation, and chronic myelomonocytic leukemia.
The U.S. Food and Drug Administration has approved Lupin’s decitabine product, a generic version of Otsuka Pharmaceutical Co. Ltd.’s Dacogen, to treat patients with myelodysplastic syndromes (MDS).
Lupin’s decitabine for injection (50 mg, single-dose vial) is approved to treat patients with intermediate-1, intermediate-2, and high-risk MDS.
This includes previously treated, untreated, de novo, and secondary MDS of all French-American-British subtypes—refractory anemia, refractory anemia with ringed sideroblasts, refractory anemia with excess blasts, refractory anemia with excess blasts in transformation, and chronic myelomonocytic leukemia.
The U.S. Food and Drug Administration has approved Lupin’s decitabine product, a generic version of Otsuka Pharmaceutical Co. Ltd.’s Dacogen, to treat patients with myelodysplastic syndromes (MDS).
Lupin’s decitabine for injection (50 mg, single-dose vial) is approved to treat patients with intermediate-1, intermediate-2, and high-risk MDS.
This includes previously treated, untreated, de novo, and secondary MDS of all French-American-British subtypes—refractory anemia, refractory anemia with ringed sideroblasts, refractory anemia with excess blasts, refractory anemia with excess blasts in transformation, and chronic myelomonocytic leukemia.
Free advice seems to be history
The 2 short years in the cocoon of residency ended, and I was flying solo on the picturesque but sparsely populated coast of Maine. My colleagues and I were fulfilling our 2-year military obligations at the Brunswick Naval Air Station, hundreds of miles from the support systems our tertiary care centers had provided. As the only pediatrician on the dispensary staff, I felt particularly vulnerable.
At least I was in the same time zone in which I had trained. I still knew most of the beeper numbers or could remember the extensions and the first names of the department secretaries. Usually within minutes, the familiar and calming voice of one of my favorite subspecialists or pediatric mentors would set me on the path to the correct diagnosis and management plan. Of course, I could have asked one of the pediatricians in town for advice, and eventually, I did. But, in the beginning, I was embarrassed to reveal my soft underbelly to the townies.
Within a few months, I was moonlighting for a local pediatrician and, after 2 years, I joined him as a partner. However, it took another several years to wean myself off my dependency on the subspecialists at the big-city medical center where I had trained. To some extent, this was because in the 1970s and 1980s, Maine had few pediatric subspecialists.
Eventually, I developed my own list of favorite local consultants. While the quality of advice was the prime determinant in my choice of a consultant, availability was a close second. How easy was it to get the specialist on the phone? If the clinical situation was not terribly time sensitive and I knew the consultant always was painfully overbooked, I would ask my question in a short typed note, and even include a S.A.S.E. (self-addressed stamped envelope). This – of course – was before email had been invented.
How likely was the consultant going to provide the answer I wanted to hear? If I thought the patient needed P-E (pressure equalizer) tubes, I could choose any ENT specialist. If, on the other hand, I felt that watching and waiting was the better option, I would choose the physician I knew was least likely to advise surgery.
I am unaware that any of the physicians I consulted ever charged the patient for my phone calls or notes. In some cases, their reward came in the opportunity to perform surgery. I rarely received small gifts during the holidays from consultants who were trying to build their practices. And I never gave tokens of appreciation to consultants or their staff to secure their timely response to my pleas for help. However, I always included a personal thank-you note with the self-designed holiday cards I sent to my favorites. And when a consultant had bailed me out of a particularly challenging situation, I often sent a handwritten note in follow-up.
But, for me, the care and grooming of a good stable of consultants began with acknowledging that their time was at least as valuable as mine. The more carefully I crafted my question and the more complete the history I could provide, the more efficiently the consultant could provide me with the answer I needed.
Regrettably, but predictably, those days of free advice are fading away. The new revision of the CPT codes includes at least twelve codes for “interprofessional consultation.” Time is – and has always been – money. As everyone’s time is increasingly being gobbled up by electronic advancements that promised to save us time, no one seems to have time to make or answer that call that begins, “Can I ask you a quick question about a patient?”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
The 2 short years in the cocoon of residency ended, and I was flying solo on the picturesque but sparsely populated coast of Maine. My colleagues and I were fulfilling our 2-year military obligations at the Brunswick Naval Air Station, hundreds of miles from the support systems our tertiary care centers had provided. As the only pediatrician on the dispensary staff, I felt particularly vulnerable.
At least I was in the same time zone in which I had trained. I still knew most of the beeper numbers or could remember the extensions and the first names of the department secretaries. Usually within minutes, the familiar and calming voice of one of my favorite subspecialists or pediatric mentors would set me on the path to the correct diagnosis and management plan. Of course, I could have asked one of the pediatricians in town for advice, and eventually, I did. But, in the beginning, I was embarrassed to reveal my soft underbelly to the townies.
Within a few months, I was moonlighting for a local pediatrician and, after 2 years, I joined him as a partner. However, it took another several years to wean myself off my dependency on the subspecialists at the big-city medical center where I had trained. To some extent, this was because in the 1970s and 1980s, Maine had few pediatric subspecialists.
Eventually, I developed my own list of favorite local consultants. While the quality of advice was the prime determinant in my choice of a consultant, availability was a close second. How easy was it to get the specialist on the phone? If the clinical situation was not terribly time sensitive and I knew the consultant always was painfully overbooked, I would ask my question in a short typed note, and even include a S.A.S.E. (self-addressed stamped envelope). This – of course – was before email had been invented.
How likely was the consultant going to provide the answer I wanted to hear? If I thought the patient needed P-E (pressure equalizer) tubes, I could choose any ENT specialist. If, on the other hand, I felt that watching and waiting was the better option, I would choose the physician I knew was least likely to advise surgery.
I am unaware that any of the physicians I consulted ever charged the patient for my phone calls or notes. In some cases, their reward came in the opportunity to perform surgery. I rarely received small gifts during the holidays from consultants who were trying to build their practices. And I never gave tokens of appreciation to consultants or their staff to secure their timely response to my pleas for help. However, I always included a personal thank-you note with the self-designed holiday cards I sent to my favorites. And when a consultant had bailed me out of a particularly challenging situation, I often sent a handwritten note in follow-up.
But, for me, the care and grooming of a good stable of consultants began with acknowledging that their time was at least as valuable as mine. The more carefully I crafted my question and the more complete the history I could provide, the more efficiently the consultant could provide me with the answer I needed.
Regrettably, but predictably, those days of free advice are fading away. The new revision of the CPT codes includes at least twelve codes for “interprofessional consultation.” Time is – and has always been – money. As everyone’s time is increasingly being gobbled up by electronic advancements that promised to save us time, no one seems to have time to make or answer that call that begins, “Can I ask you a quick question about a patient?”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
The 2 short years in the cocoon of residency ended, and I was flying solo on the picturesque but sparsely populated coast of Maine. My colleagues and I were fulfilling our 2-year military obligations at the Brunswick Naval Air Station, hundreds of miles from the support systems our tertiary care centers had provided. As the only pediatrician on the dispensary staff, I felt particularly vulnerable.
At least I was in the same time zone in which I had trained. I still knew most of the beeper numbers or could remember the extensions and the first names of the department secretaries. Usually within minutes, the familiar and calming voice of one of my favorite subspecialists or pediatric mentors would set me on the path to the correct diagnosis and management plan. Of course, I could have asked one of the pediatricians in town for advice, and eventually, I did. But, in the beginning, I was embarrassed to reveal my soft underbelly to the townies.
Within a few months, I was moonlighting for a local pediatrician and, after 2 years, I joined him as a partner. However, it took another several years to wean myself off my dependency on the subspecialists at the big-city medical center where I had trained. To some extent, this was because in the 1970s and 1980s, Maine had few pediatric subspecialists.
Eventually, I developed my own list of favorite local consultants. While the quality of advice was the prime determinant in my choice of a consultant, availability was a close second. How easy was it to get the specialist on the phone? If the clinical situation was not terribly time sensitive and I knew the consultant always was painfully overbooked, I would ask my question in a short typed note, and even include a S.A.S.E. (self-addressed stamped envelope). This – of course – was before email had been invented.
How likely was the consultant going to provide the answer I wanted to hear? If I thought the patient needed P-E (pressure equalizer) tubes, I could choose any ENT specialist. If, on the other hand, I felt that watching and waiting was the better option, I would choose the physician I knew was least likely to advise surgery.
I am unaware that any of the physicians I consulted ever charged the patient for my phone calls or notes. In some cases, their reward came in the opportunity to perform surgery. I rarely received small gifts during the holidays from consultants who were trying to build their practices. And I never gave tokens of appreciation to consultants or their staff to secure their timely response to my pleas for help. However, I always included a personal thank-you note with the self-designed holiday cards I sent to my favorites. And when a consultant had bailed me out of a particularly challenging situation, I often sent a handwritten note in follow-up.
But, for me, the care and grooming of a good stable of consultants began with acknowledging that their time was at least as valuable as mine. The more carefully I crafted my question and the more complete the history I could provide, the more efficiently the consultant could provide me with the answer I needed.
Regrettably, but predictably, those days of free advice are fading away. The new revision of the CPT codes includes at least twelve codes for “interprofessional consultation.” Time is – and has always been – money. As everyone’s time is increasingly being gobbled up by electronic advancements that promised to save us time, no one seems to have time to make or answer that call that begins, “Can I ask you a quick question about a patient?”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.