User login
Docs Around the Clock
Docs Around the Clock
Our hospitalist group presently takes out-of-house call at night, but our hospital is pressuring us to move into the hospital 24/7. What should we do?
Afraid of the Dark,
Provo, Utah
Dr. Hospitalist responds: It can be a real challenge to find sufficient providers to staff the hospital nightly. But I encourage you to take this step. I believe there is a quality advantage to having hospitalists in house 24/7 versus having physicians on call at night from outside the hospital.
Hospitalized patients are no less likely to become acutely ill at night as during the day. From a quality perspective, it has never made sense to me why hospitals do not routinely have a physician in house 24/7. Many hospitals say they cannot afford to pay a physician to work in house at night because there are few opportunities to generate revenue. But in today’s environment, can you afford not to have a hospitalist in at night?
Hospitals without hospitalists in at night often encounter issues with patient throughput each morning. Nurses are waiting for physician orders, and physicians are scrambling to write admission notes on patients admitted overnight. This delays morning discharges and admissions, leading to other problems including overcrowding in the emergency department.
Hospitalized patients are now sicker than ever. Delays in evaluations can mean adverse outcomes. Just because the doctor is not in the hospital does not relieve them of any responsibility if a patient suffers an adverse outcome as a result of delay in care. Patients and payers are not only scrutinizing the care patients receive in the hospital but also paying based on performance. Can you and your hospital afford to not provide the timeliest care possible?
Right Night Solution?
Do you think it is better to have dedicated nocturnist(s) or have hospitalist staff members take turns working nights?
Sleepless in San Diego
Dr. Hospitalist responds: There are advantages and disadvantages of having a dedicated nocturnist versus having a rotation model with regular hospitalist staff members taking turns working nights in the hospital. If your hospital has different groups of nurses for days and nights, there may be an advantage to having nocturnists.
This model allows the doctors and nurses to work closely and develop a cohesive team. This would be more difficult if the doctor at night changes frequently. Using nocturnists to staff nights can also make daytime staffing easier or more difficult.
Consider this analogy. At the end of this baseball season, the New York Yankees faced the decision of whether or not to re-sign arguably the best player on the planet, Alex Rodriguez. With A-Rod’s high price tag ($30 million-plus annually), would the Yankees be better served taking this money and signing several players (because we assume no single player could match his talent)? What would happen if they signed A-Rod and he got hurt? Wouldn’t that leave a hole in the lineup the size of the Milky Way?
How different are nocturnists in today’s hospitalist workplace? Most hospitalist programs covet them. They can do things others can’t—work a large number of nights on the schedule. This means fewer or no nights for colleagues, which makes them happier. Nocturnists command a high salary, and if one leaves for your program for any reason, they leave a gaping hole in the schedule.
My advice is to hire a nocturnist but don’t rely solely on nocturnists to cover nights. Covering your night schedule with a mix of nocturnists and staff hospitalists will allow everyone to appreciate the nocturnist but won’t put you in the uncomfortable position of relying solely on nocturnists to keep your program running effectively.
Performance Anxiety
I just started working as a hospitalist. I was told that the federal government surveys patients about the care I provide in the hospital. Is this true?
Newbie in Fort Lauderdale
Dr. Hospitalist responds: I believe you are referring to the Consumer Assessment of Healthcare Providers and Systems (CAHPS) hospital survey. It is a standardized instrument designed to measure patients’ perspective of care in acute care hospitals.
Hospital participation is optional. Many hospitals survey patients about their perceptions of care after they leave the hospital. Press Ganey Associates works with hospitals nationwide to conduct the surveys. The Centers for Medicare and Medicaid Services (CMS) and the Joint Commission encourage hospitals to incorporate the CAHPS questions into any other surveys being performed. The survey has 27 questions that cover seven topic areas:
- Communication with doctors;
- Communication with nurses;
- Hospital staff responsiveness;
- Pain management;
- Communication about medicines;
- Hospital environment; and
- Discharge information.
Three questions ask about communication with doctors:
- How often did the doctors treat you with courtesy and respect?
- How often did doctors listen carefully to you?
- How often did doctors explain things so you could understand?
The survey will produce data that not only will “allow comparison between hospitals, it will create an incentive for hospitals to improve quality of care and to increase accountability by increasing transparency.” Data collection for the initial period from October 2006 to June 2007 will be publicly reported in March 2008 on the Hospital Compare Web site: www.hospitalcompare.hhs.gov. For additional information, go to www.hcaphsonline.org. TH
Docs Around the Clock
Our hospitalist group presently takes out-of-house call at night, but our hospital is pressuring us to move into the hospital 24/7. What should we do?
Afraid of the Dark,
Provo, Utah
Dr. Hospitalist responds: It can be a real challenge to find sufficient providers to staff the hospital nightly. But I encourage you to take this step. I believe there is a quality advantage to having hospitalists in house 24/7 versus having physicians on call at night from outside the hospital.
Hospitalized patients are no less likely to become acutely ill at night as during the day. From a quality perspective, it has never made sense to me why hospitals do not routinely have a physician in house 24/7. Many hospitals say they cannot afford to pay a physician to work in house at night because there are few opportunities to generate revenue. But in today’s environment, can you afford not to have a hospitalist in at night?
Hospitals without hospitalists in at night often encounter issues with patient throughput each morning. Nurses are waiting for physician orders, and physicians are scrambling to write admission notes on patients admitted overnight. This delays morning discharges and admissions, leading to other problems including overcrowding in the emergency department.
Hospitalized patients are now sicker than ever. Delays in evaluations can mean adverse outcomes. Just because the doctor is not in the hospital does not relieve them of any responsibility if a patient suffers an adverse outcome as a result of delay in care. Patients and payers are not only scrutinizing the care patients receive in the hospital but also paying based on performance. Can you and your hospital afford to not provide the timeliest care possible?
Right Night Solution?
Do you think it is better to have dedicated nocturnist(s) or have hospitalist staff members take turns working nights?
Sleepless in San Diego
Dr. Hospitalist responds: There are advantages and disadvantages of having a dedicated nocturnist versus having a rotation model with regular hospitalist staff members taking turns working nights in the hospital. If your hospital has different groups of nurses for days and nights, there may be an advantage to having nocturnists.
This model allows the doctors and nurses to work closely and develop a cohesive team. This would be more difficult if the doctor at night changes frequently. Using nocturnists to staff nights can also make daytime staffing easier or more difficult.
Consider this analogy. At the end of this baseball season, the New York Yankees faced the decision of whether or not to re-sign arguably the best player on the planet, Alex Rodriguez. With A-Rod’s high price tag ($30 million-plus annually), would the Yankees be better served taking this money and signing several players (because we assume no single player could match his talent)? What would happen if they signed A-Rod and he got hurt? Wouldn’t that leave a hole in the lineup the size of the Milky Way?
How different are nocturnists in today’s hospitalist workplace? Most hospitalist programs covet them. They can do things others can’t—work a large number of nights on the schedule. This means fewer or no nights for colleagues, which makes them happier. Nocturnists command a high salary, and if one leaves for your program for any reason, they leave a gaping hole in the schedule.
My advice is to hire a nocturnist but don’t rely solely on nocturnists to cover nights. Covering your night schedule with a mix of nocturnists and staff hospitalists will allow everyone to appreciate the nocturnist but won’t put you in the uncomfortable position of relying solely on nocturnists to keep your program running effectively.
Performance Anxiety
I just started working as a hospitalist. I was told that the federal government surveys patients about the care I provide in the hospital. Is this true?
Newbie in Fort Lauderdale
Dr. Hospitalist responds: I believe you are referring to the Consumer Assessment of Healthcare Providers and Systems (CAHPS) hospital survey. It is a standardized instrument designed to measure patients’ perspective of care in acute care hospitals.
Hospital participation is optional. Many hospitals survey patients about their perceptions of care after they leave the hospital. Press Ganey Associates works with hospitals nationwide to conduct the surveys. The Centers for Medicare and Medicaid Services (CMS) and the Joint Commission encourage hospitals to incorporate the CAHPS questions into any other surveys being performed. The survey has 27 questions that cover seven topic areas:
- Communication with doctors;
- Communication with nurses;
- Hospital staff responsiveness;
- Pain management;
- Communication about medicines;
- Hospital environment; and
- Discharge information.
Three questions ask about communication with doctors:
- How often did the doctors treat you with courtesy and respect?
- How often did doctors listen carefully to you?
- How often did doctors explain things so you could understand?
The survey will produce data that not only will “allow comparison between hospitals, it will create an incentive for hospitals to improve quality of care and to increase accountability by increasing transparency.” Data collection for the initial period from October 2006 to June 2007 will be publicly reported in March 2008 on the Hospital Compare Web site: www.hospitalcompare.hhs.gov. For additional information, go to www.hcaphsonline.org. TH
Docs Around the Clock
Our hospitalist group presently takes out-of-house call at night, but our hospital is pressuring us to move into the hospital 24/7. What should we do?
Afraid of the Dark,
Provo, Utah
Dr. Hospitalist responds: It can be a real challenge to find sufficient providers to staff the hospital nightly. But I encourage you to take this step. I believe there is a quality advantage to having hospitalists in house 24/7 versus having physicians on call at night from outside the hospital.
Hospitalized patients are no less likely to become acutely ill at night as during the day. From a quality perspective, it has never made sense to me why hospitals do not routinely have a physician in house 24/7. Many hospitals say they cannot afford to pay a physician to work in house at night because there are few opportunities to generate revenue. But in today’s environment, can you afford not to have a hospitalist in at night?
Hospitals without hospitalists in at night often encounter issues with patient throughput each morning. Nurses are waiting for physician orders, and physicians are scrambling to write admission notes on patients admitted overnight. This delays morning discharges and admissions, leading to other problems including overcrowding in the emergency department.
Hospitalized patients are now sicker than ever. Delays in evaluations can mean adverse outcomes. Just because the doctor is not in the hospital does not relieve them of any responsibility if a patient suffers an adverse outcome as a result of delay in care. Patients and payers are not only scrutinizing the care patients receive in the hospital but also paying based on performance. Can you and your hospital afford to not provide the timeliest care possible?
Right Night Solution?
Do you think it is better to have dedicated nocturnist(s) or have hospitalist staff members take turns working nights?
Sleepless in San Diego
Dr. Hospitalist responds: There are advantages and disadvantages of having a dedicated nocturnist versus having a rotation model with regular hospitalist staff members taking turns working nights in the hospital. If your hospital has different groups of nurses for days and nights, there may be an advantage to having nocturnists.
This model allows the doctors and nurses to work closely and develop a cohesive team. This would be more difficult if the doctor at night changes frequently. Using nocturnists to staff nights can also make daytime staffing easier or more difficult.
Consider this analogy. At the end of this baseball season, the New York Yankees faced the decision of whether or not to re-sign arguably the best player on the planet, Alex Rodriguez. With A-Rod’s high price tag ($30 million-plus annually), would the Yankees be better served taking this money and signing several players (because we assume no single player could match his talent)? What would happen if they signed A-Rod and he got hurt? Wouldn’t that leave a hole in the lineup the size of the Milky Way?
How different are nocturnists in today’s hospitalist workplace? Most hospitalist programs covet them. They can do things others can’t—work a large number of nights on the schedule. This means fewer or no nights for colleagues, which makes them happier. Nocturnists command a high salary, and if one leaves for your program for any reason, they leave a gaping hole in the schedule.
My advice is to hire a nocturnist but don’t rely solely on nocturnists to cover nights. Covering your night schedule with a mix of nocturnists and staff hospitalists will allow everyone to appreciate the nocturnist but won’t put you in the uncomfortable position of relying solely on nocturnists to keep your program running effectively.
Performance Anxiety
I just started working as a hospitalist. I was told that the federal government surveys patients about the care I provide in the hospital. Is this true?
Newbie in Fort Lauderdale
Dr. Hospitalist responds: I believe you are referring to the Consumer Assessment of Healthcare Providers and Systems (CAHPS) hospital survey. It is a standardized instrument designed to measure patients’ perspective of care in acute care hospitals.
Hospital participation is optional. Many hospitals survey patients about their perceptions of care after they leave the hospital. Press Ganey Associates works with hospitals nationwide to conduct the surveys. The Centers for Medicare and Medicaid Services (CMS) and the Joint Commission encourage hospitals to incorporate the CAHPS questions into any other surveys being performed. The survey has 27 questions that cover seven topic areas:
- Communication with doctors;
- Communication with nurses;
- Hospital staff responsiveness;
- Pain management;
- Communication about medicines;
- Hospital environment; and
- Discharge information.
Three questions ask about communication with doctors:
- How often did the doctors treat you with courtesy and respect?
- How often did doctors listen carefully to you?
- How often did doctors explain things so you could understand?
The survey will produce data that not only will “allow comparison between hospitals, it will create an incentive for hospitals to improve quality of care and to increase accountability by increasing transparency.” Data collection for the initial period from October 2006 to June 2007 will be publicly reported in March 2008 on the Hospital Compare Web site: www.hospitalcompare.hhs.gov. For additional information, go to www.hcaphsonline.org. TH
Avoid Bottlenecks
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Fight the Losing Battle
With shirt buttons bulging and my panniculus spilling like the top of an oversized muffin over my belt—which was essentially a tourniquet strangling my lower extremities—I examined my options.
After hours of grazing through the snack food pyramid and consuming significant portions of a dinosaur-size turkey, an acromegalic dollop of dressing, a bog of cranberries, and a field of mashed potatoes, I was faced with the proposition of shoveling in another 500 calories cleverly disguised as a heaping slice of pumpkin pie.
The intensity of the situation was palpable. My in-laws sat mouths agape, stunned by the amount and rate at which I forked thousands of calories into my gullet. They fidgeted as I stared with steely, miotic pupils and furrowed, sweat-beaded brow at my prospective ingestion.
The tension heightened as my lower two shirt buttons gave up the cause, careening across the table and striking, respectively, a deserted bowl of creamed corn and the forehead of a comatose relative who had long ago lost interest in watching my acute food intoxication. As my cousins brokered bets over the likelihood of my impending demise, I sat and deliberated, fork hovering over my sugary prey.
Obesity Epidemic
As healthcare practitioners, we are well aware of the dangers of obesity, yet seem paralyzed to make change. However, hospitalists are perfectly positioned to help patients resolve to lose their weight.
A body mass index (BMI) of 30 or more indicates obesity; its slimmer overweight cousin weighs in with a BMI of 25-29.
Overweight or obese people are at increased risk of osteoarthritis, dyslipidemia, obstructive sleep apnea, hypertension, coronary artery disease, stroke, cancer, and diabetes. Obesity accounts for 300,000 excess deaths per year in the U.S., along with about 10% of all healthcare expenditures, according to the Centers for Disease Control and Prevention (CDC). It affects all ages, races, and professions—including physicians. It is perhaps the most significant health issue facing our nation.
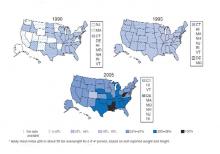
Despite this awareness, we keep getting bigger. In the past 20 years we have seen an epic swelling of American waistlines. In 1990 the CDC reported that among adult residents, 10 states had a prevalence rate of obesity less than 10%, and no states had a rate more than 15% (see Fig. 1, above). By 2006, no state had a prevalence of obesity less than 10%, while only four states clocked in with a rate less than 20%. A whopping 22 states found at least 25% of their inhabitants obese. Since 2005 we’ve become so big the CDC had to create a new category for states with more than 30% of their residents being obese. When the BMI cutoff is dropped to 25 or more, 66% meet of U.S. adults meet this definition for being overweight or obese.
Recent CDC data reveal a glimmer of hope. There was no statistically significant increase in the prevalence of obesity in 2005-2006, compared with 2003-2004. In the earlier time period, 31.1% of men and 33.2% of women were obese, compared with 33.3% of men and 35.3% of women in the most recent time period.
Still, one of every three U.S. adults is obese. That’s 100 million Americans. More than 50% of non-Hispanic black and Mexican-American women age 40-59 are obese. Sixty-one percent of non-Hispanic black women older than 60 are obese.
A complex mix of components, including environment and genetics, determines weight gain. The rapid rate of weight gain in recent years is unlikely to be explained by genetics alone—the population’s genetic composition cannot change that quickly. Thus the bulk of the recent increase in obesity is likely related to cultural and environmental determinants. A 2007 paper by Christakis, et al., found that social networks play a large role in the spread of obesity.1 The study followed 12,067 people for more than 30 years. Those with a friend, sibling, or spouse who became obese over that period were 57%, 40%, and 37% more likely, respectively, to become obese. The authors hypothesize that obesity may become less stigmatized and more tolerable for those surrounded by obese associates. Another theory is that peer groups tend to adopt similar behaviors, such as smoking, eating fast food, and inactivity.
The average person gains about one to two pounds a year.2 When distilled to its simplest form, weight gain occurs anytime calories in exceed calories out—that is, a positive energy balance or gap.
The six weeks from Thanksgiving to New Year’s is an especially vulnerable time for weight gain. In a 2000 study of 195 subjects, the average person gained about one pound during the holiday season. When these subjects were followed up with six months later, there was no statistically significant loss of peri-holiday weight gain. This holiday pound may seem trivial (and keep in mind these subjects gained weight despite being closely watched in a weight-gain study). But this weight appears hard to shed and results in much of the weight gained during adulthood.
However, unlike my Thanksgiving gorging, the hallmark of obesity is the small but frequent positive energy gaps, that is, days of 50 to 100 calories of intake greater than use. Over the course of the year, these small daily caloric gaps are anabolically transformed into pounds.
Resolve to Lose
By now, like me, many of you may have added a holiday pound or two. This may be in addition to a nefarious pound or two added throughout the rest of the year. As you ponder scribing your annual resolutions, consider making weight loss a top priority for your patients and yourself, if appropriate.
Unfortunately no magic bullet will turn your New Year’s resolution into reality, just hard work. The key is to tilt the energy balance toward weight loss by reducing caloric intake and increasing activity. Fortunately this can be done in non-Draconian ways. Just as weight gain can snowball from small daily caloric overdoses, it can be removed the same way. Instead of setting or recommending insurmountable goals to your patients—like reducing intake to 1,000 calories a day or adhering to a triathletic training regimen—the CDC suggests a simpler, more sustainable approach to shedding those pounds, namely tipping your energy balance to a negative 150 calories per day.
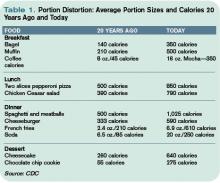
A net negative energy balance of 150 calories per day will at worst stabilize your weight (depending on your current energy balance) and at best net five to 10 pounds of weight loss per year. For most this can result from something as simple as switching your daily Coke to a Diet Coke. Even more ground can be gained by reducing portion size. The super-sizing of the American menu over the past 20 years is one of the prime drivers of the obesity epidemic (see Table 1, p. 64). Consider cutting back in small ways. For example, continue to enjoy that gourmet chocolate chip cookie but downsize it to a smaller version and reduce your intake by 150 to 200 calories.
As important as reducing caloric intake is the need for activity. Adding moderate amounts of exercise five days a week can burn an additional 150 calories per day, reducing overall weight by another five to 10 pounds in a year. This can include things like walking for 30 minutes, swimming for 20 minutes, or biking for 15 minutes. More adventurous (dancing for 30 minutes), parental (pushing a stroller for 30 minutes), agricultural (gardening for 30 minutes), or chore-oriented (shoveling 15 minutes) options also help.
Much to the dismay of my cousin Mike, who bet that I’d eat at least half the piece of Thanksgiving pie, I put down my fork. After packing away a winter’s worth of calories I was feeling diaphoretic and pathetic. I wobbled away from the table and began charting my course to redemption. It would begin the next day with an apple instead of a bagel, an extra hour at the gym—and a trip to the cleaners to get those buttons replaced. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Editor’s note: The author’s driver license claims a weight of 165 pounds. Physical evidence, as well as his wife’s report, paints a substantially different picture.
References
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370-379.
- Yanovksi JA, Yanovski SZ, Sovik KN, et al. A prospective study of holiday weight gain. N Engl J Med. 2000;342:861-867.
With shirt buttons bulging and my panniculus spilling like the top of an oversized muffin over my belt—which was essentially a tourniquet strangling my lower extremities—I examined my options.
After hours of grazing through the snack food pyramid and consuming significant portions of a dinosaur-size turkey, an acromegalic dollop of dressing, a bog of cranberries, and a field of mashed potatoes, I was faced with the proposition of shoveling in another 500 calories cleverly disguised as a heaping slice of pumpkin pie.
The intensity of the situation was palpable. My in-laws sat mouths agape, stunned by the amount and rate at which I forked thousands of calories into my gullet. They fidgeted as I stared with steely, miotic pupils and furrowed, sweat-beaded brow at my prospective ingestion.
The tension heightened as my lower two shirt buttons gave up the cause, careening across the table and striking, respectively, a deserted bowl of creamed corn and the forehead of a comatose relative who had long ago lost interest in watching my acute food intoxication. As my cousins brokered bets over the likelihood of my impending demise, I sat and deliberated, fork hovering over my sugary prey.
Obesity Epidemic
As healthcare practitioners, we are well aware of the dangers of obesity, yet seem paralyzed to make change. However, hospitalists are perfectly positioned to help patients resolve to lose their weight.
A body mass index (BMI) of 30 or more indicates obesity; its slimmer overweight cousin weighs in with a BMI of 25-29.
Overweight or obese people are at increased risk of osteoarthritis, dyslipidemia, obstructive sleep apnea, hypertension, coronary artery disease, stroke, cancer, and diabetes. Obesity accounts for 300,000 excess deaths per year in the U.S., along with about 10% of all healthcare expenditures, according to the Centers for Disease Control and Prevention (CDC). It affects all ages, races, and professions—including physicians. It is perhaps the most significant health issue facing our nation.
Despite this awareness, we keep getting bigger. In the past 20 years we have seen an epic swelling of American waistlines. In 1990 the CDC reported that among adult residents, 10 states had a prevalence rate of obesity less than 10%, and no states had a rate more than 15% (see Fig. 1, above). By 2006, no state had a prevalence of obesity less than 10%, while only four states clocked in with a rate less than 20%. A whopping 22 states found at least 25% of their inhabitants obese. Since 2005 we’ve become so big the CDC had to create a new category for states with more than 30% of their residents being obese. When the BMI cutoff is dropped to 25 or more, 66% meet of U.S. adults meet this definition for being overweight or obese.
Recent CDC data reveal a glimmer of hope. There was no statistically significant increase in the prevalence of obesity in 2005-2006, compared with 2003-2004. In the earlier time period, 31.1% of men and 33.2% of women were obese, compared with 33.3% of men and 35.3% of women in the most recent time period.
Still, one of every three U.S. adults is obese. That’s 100 million Americans. More than 50% of non-Hispanic black and Mexican-American women age 40-59 are obese. Sixty-one percent of non-Hispanic black women older than 60 are obese.
A complex mix of components, including environment and genetics, determines weight gain. The rapid rate of weight gain in recent years is unlikely to be explained by genetics alone—the population’s genetic composition cannot change that quickly. Thus the bulk of the recent increase in obesity is likely related to cultural and environmental determinants. A 2007 paper by Christakis, et al., found that social networks play a large role in the spread of obesity.1 The study followed 12,067 people for more than 30 years. Those with a friend, sibling, or spouse who became obese over that period were 57%, 40%, and 37% more likely, respectively, to become obese. The authors hypothesize that obesity may become less stigmatized and more tolerable for those surrounded by obese associates. Another theory is that peer groups tend to adopt similar behaviors, such as smoking, eating fast food, and inactivity.
The average person gains about one to two pounds a year.2 When distilled to its simplest form, weight gain occurs anytime calories in exceed calories out—that is, a positive energy balance or gap.
The six weeks from Thanksgiving to New Year’s is an especially vulnerable time for weight gain. In a 2000 study of 195 subjects, the average person gained about one pound during the holiday season. When these subjects were followed up with six months later, there was no statistically significant loss of peri-holiday weight gain. This holiday pound may seem trivial (and keep in mind these subjects gained weight despite being closely watched in a weight-gain study). But this weight appears hard to shed and results in much of the weight gained during adulthood.
However, unlike my Thanksgiving gorging, the hallmark of obesity is the small but frequent positive energy gaps, that is, days of 50 to 100 calories of intake greater than use. Over the course of the year, these small daily caloric gaps are anabolically transformed into pounds.
Resolve to Lose
By now, like me, many of you may have added a holiday pound or two. This may be in addition to a nefarious pound or two added throughout the rest of the year. As you ponder scribing your annual resolutions, consider making weight loss a top priority for your patients and yourself, if appropriate.
Unfortunately no magic bullet will turn your New Year’s resolution into reality, just hard work. The key is to tilt the energy balance toward weight loss by reducing caloric intake and increasing activity. Fortunately this can be done in non-Draconian ways. Just as weight gain can snowball from small daily caloric overdoses, it can be removed the same way. Instead of setting or recommending insurmountable goals to your patients—like reducing intake to 1,000 calories a day or adhering to a triathletic training regimen—the CDC suggests a simpler, more sustainable approach to shedding those pounds, namely tipping your energy balance to a negative 150 calories per day.
A net negative energy balance of 150 calories per day will at worst stabilize your weight (depending on your current energy balance) and at best net five to 10 pounds of weight loss per year. For most this can result from something as simple as switching your daily Coke to a Diet Coke. Even more ground can be gained by reducing portion size. The super-sizing of the American menu over the past 20 years is one of the prime drivers of the obesity epidemic (see Table 1, p. 64). Consider cutting back in small ways. For example, continue to enjoy that gourmet chocolate chip cookie but downsize it to a smaller version and reduce your intake by 150 to 200 calories.
As important as reducing caloric intake is the need for activity. Adding moderate amounts of exercise five days a week can burn an additional 150 calories per day, reducing overall weight by another five to 10 pounds in a year. This can include things like walking for 30 minutes, swimming for 20 minutes, or biking for 15 minutes. More adventurous (dancing for 30 minutes), parental (pushing a stroller for 30 minutes), agricultural (gardening for 30 minutes), or chore-oriented (shoveling 15 minutes) options also help.
Much to the dismay of my cousin Mike, who bet that I’d eat at least half the piece of Thanksgiving pie, I put down my fork. After packing away a winter’s worth of calories I was feeling diaphoretic and pathetic. I wobbled away from the table and began charting my course to redemption. It would begin the next day with an apple instead of a bagel, an extra hour at the gym—and a trip to the cleaners to get those buttons replaced. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Editor’s note: The author’s driver license claims a weight of 165 pounds. Physical evidence, as well as his wife’s report, paints a substantially different picture.
References
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370-379.
- Yanovksi JA, Yanovski SZ, Sovik KN, et al. A prospective study of holiday weight gain. N Engl J Med. 2000;342:861-867.
With shirt buttons bulging and my panniculus spilling like the top of an oversized muffin over my belt—which was essentially a tourniquet strangling my lower extremities—I examined my options.
After hours of grazing through the snack food pyramid and consuming significant portions of a dinosaur-size turkey, an acromegalic dollop of dressing, a bog of cranberries, and a field of mashed potatoes, I was faced with the proposition of shoveling in another 500 calories cleverly disguised as a heaping slice of pumpkin pie.
The intensity of the situation was palpable. My in-laws sat mouths agape, stunned by the amount and rate at which I forked thousands of calories into my gullet. They fidgeted as I stared with steely, miotic pupils and furrowed, sweat-beaded brow at my prospective ingestion.
The tension heightened as my lower two shirt buttons gave up the cause, careening across the table and striking, respectively, a deserted bowl of creamed corn and the forehead of a comatose relative who had long ago lost interest in watching my acute food intoxication. As my cousins brokered bets over the likelihood of my impending demise, I sat and deliberated, fork hovering over my sugary prey.
Obesity Epidemic
As healthcare practitioners, we are well aware of the dangers of obesity, yet seem paralyzed to make change. However, hospitalists are perfectly positioned to help patients resolve to lose their weight.
A body mass index (BMI) of 30 or more indicates obesity; its slimmer overweight cousin weighs in with a BMI of 25-29.
Overweight or obese people are at increased risk of osteoarthritis, dyslipidemia, obstructive sleep apnea, hypertension, coronary artery disease, stroke, cancer, and diabetes. Obesity accounts for 300,000 excess deaths per year in the U.S., along with about 10% of all healthcare expenditures, according to the Centers for Disease Control and Prevention (CDC). It affects all ages, races, and professions—including physicians. It is perhaps the most significant health issue facing our nation.
Despite this awareness, we keep getting bigger. In the past 20 years we have seen an epic swelling of American waistlines. In 1990 the CDC reported that among adult residents, 10 states had a prevalence rate of obesity less than 10%, and no states had a rate more than 15% (see Fig. 1, above). By 2006, no state had a prevalence of obesity less than 10%, while only four states clocked in with a rate less than 20%. A whopping 22 states found at least 25% of their inhabitants obese. Since 2005 we’ve become so big the CDC had to create a new category for states with more than 30% of their residents being obese. When the BMI cutoff is dropped to 25 or more, 66% meet of U.S. adults meet this definition for being overweight or obese.
Recent CDC data reveal a glimmer of hope. There was no statistically significant increase in the prevalence of obesity in 2005-2006, compared with 2003-2004. In the earlier time period, 31.1% of men and 33.2% of women were obese, compared with 33.3% of men and 35.3% of women in the most recent time period.
Still, one of every three U.S. adults is obese. That’s 100 million Americans. More than 50% of non-Hispanic black and Mexican-American women age 40-59 are obese. Sixty-one percent of non-Hispanic black women older than 60 are obese.
A complex mix of components, including environment and genetics, determines weight gain. The rapid rate of weight gain in recent years is unlikely to be explained by genetics alone—the population’s genetic composition cannot change that quickly. Thus the bulk of the recent increase in obesity is likely related to cultural and environmental determinants. A 2007 paper by Christakis, et al., found that social networks play a large role in the spread of obesity.1 The study followed 12,067 people for more than 30 years. Those with a friend, sibling, or spouse who became obese over that period were 57%, 40%, and 37% more likely, respectively, to become obese. The authors hypothesize that obesity may become less stigmatized and more tolerable for those surrounded by obese associates. Another theory is that peer groups tend to adopt similar behaviors, such as smoking, eating fast food, and inactivity.
The average person gains about one to two pounds a year.2 When distilled to its simplest form, weight gain occurs anytime calories in exceed calories out—that is, a positive energy balance or gap.
The six weeks from Thanksgiving to New Year’s is an especially vulnerable time for weight gain. In a 2000 study of 195 subjects, the average person gained about one pound during the holiday season. When these subjects were followed up with six months later, there was no statistically significant loss of peri-holiday weight gain. This holiday pound may seem trivial (and keep in mind these subjects gained weight despite being closely watched in a weight-gain study). But this weight appears hard to shed and results in much of the weight gained during adulthood.
However, unlike my Thanksgiving gorging, the hallmark of obesity is the small but frequent positive energy gaps, that is, days of 50 to 100 calories of intake greater than use. Over the course of the year, these small daily caloric gaps are anabolically transformed into pounds.
Resolve to Lose
By now, like me, many of you may have added a holiday pound or two. This may be in addition to a nefarious pound or two added throughout the rest of the year. As you ponder scribing your annual resolutions, consider making weight loss a top priority for your patients and yourself, if appropriate.
Unfortunately no magic bullet will turn your New Year’s resolution into reality, just hard work. The key is to tilt the energy balance toward weight loss by reducing caloric intake and increasing activity. Fortunately this can be done in non-Draconian ways. Just as weight gain can snowball from small daily caloric overdoses, it can be removed the same way. Instead of setting or recommending insurmountable goals to your patients—like reducing intake to 1,000 calories a day or adhering to a triathletic training regimen—the CDC suggests a simpler, more sustainable approach to shedding those pounds, namely tipping your energy balance to a negative 150 calories per day.
A net negative energy balance of 150 calories per day will at worst stabilize your weight (depending on your current energy balance) and at best net five to 10 pounds of weight loss per year. For most this can result from something as simple as switching your daily Coke to a Diet Coke. Even more ground can be gained by reducing portion size. The super-sizing of the American menu over the past 20 years is one of the prime drivers of the obesity epidemic (see Table 1, p. 64). Consider cutting back in small ways. For example, continue to enjoy that gourmet chocolate chip cookie but downsize it to a smaller version and reduce your intake by 150 to 200 calories.
As important as reducing caloric intake is the need for activity. Adding moderate amounts of exercise five days a week can burn an additional 150 calories per day, reducing overall weight by another five to 10 pounds in a year. This can include things like walking for 30 minutes, swimming for 20 minutes, or biking for 15 minutes. More adventurous (dancing for 30 minutes), parental (pushing a stroller for 30 minutes), agricultural (gardening for 30 minutes), or chore-oriented (shoveling 15 minutes) options also help.
Much to the dismay of my cousin Mike, who bet that I’d eat at least half the piece of Thanksgiving pie, I put down my fork. After packing away a winter’s worth of calories I was feeling diaphoretic and pathetic. I wobbled away from the table and began charting my course to redemption. It would begin the next day with an apple instead of a bagel, an extra hour at the gym—and a trip to the cleaners to get those buttons replaced. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Editor’s note: The author’s driver license claims a weight of 165 pounds. Physical evidence, as well as his wife’s report, paints a substantially different picture.
References
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370-379.
- Yanovksi JA, Yanovski SZ, Sovik KN, et al. A prospective study of holiday weight gain. N Engl J Med. 2000;342:861-867.
In The Driver’s Seat
It’s a refrain I have heard too many times in too many places: “Don’t do it.”
You have probably heard it, too—that plaintive cry from some practicing physicians trying to discourage young people from entering a career in medicine. I understand why so many doctors seem so pessimistic about medicine’s future. They’re grappling with a healthcare industry that struggles with overwhelming complexity. They face unrelenting cost pressures, misaligned incentives and policies, massive shortfalls in quality and service, fragmented systems, and disunity among peers.
I understand the pessimism, but I cannot agree with it. At the midpoint of my term as SHM president, I reflect upon the strengths that distinguish our specialty and our society from the general malaise of the broader healthcare industry. These strengths compel me to redouble my resolve to deliver on the promise of hospital medicine.
What is that promise? Hospitalists are poised to lead the way toward a better healthcare system in two critical ways. They are situated to help advance quality control and they are uniquely situated to promote medicine as a team effort, a shared vision with the hospital.
Now, quality control and teamwork are not in the standard curriculum. Medical school training focuses on disease. But in the real world of the hospital, quality control and the teamwork it takes to ensure it are vital issues. This is where hospitalists must prove themselves. This is where our special skills align with the priorities of hospital CEOs nationwide. We must advance the quality agenda and engage other physicians in a shared vision with the hospital.
These factors set us apart from other specialties and allow us to lead from the core of our strength. We lead:
- Through quality rather than narrow professional self-interests;
- While valuing the team over the individual; and
- With openness and inclusiveness to all medical personnel involved patient care, from pharmacists to nurses, to nonphysician providers, to management.
This is our great promise—but only if we exercise it. As the brilliant author and scientist Johann Wolfgang von Goethe cautioned 200 years ago: “Knowing is not enough. We must apply.”
Honesty requires physicians to admit there is sometimes a gap between what we know and what we apply. Many quality metrics measure our performance. For example, we know we must get aspirin to a heart attack victim quickly. But the clinical strides that dictate the care patients ought to get must be moved into the operational area, where optimal care is sometimes lacking.
We next need to work out the systems to ensure that care, turning best practices into routine practice. Hospitalists are in the vanguard on that front, just as other specialties have been on the cutting edge of academic medicine. Our specialty will always need to weigh in on the development and vetting of quality and safety metrics related to hospital care.
We are also poised to advance the implementation and application of systems that drive improvement in those metrics.
Ours is a young specialty—the average hospitalist is 37, the leadership 41. While we have accomplished much in our 10 years of existence, there is much more to do. Hospitalists must meet the extraordinarily high expectations of hospitals and the other physicians who work in them. We must help manage emergency patients, surgical patients, and the in-hospital patient census of primary care physicians.
But there is a shortage of physicians in our specialty because demand is so great. It’s hard to sustain our growth as a specialty and work on quality control at the same time.
We are in the financial crosshairs, as well. Administrators want to see value—that is, money saved. But the fact that we see and manage patients does not generate savings per se because insurance companies do not allow reimbursement as such for our services. “Prove your value,” they say. “Show us the money.” That translates into driving down length of stay, cutting nursing expenses, and reducing pharmacy costs though better quality control and more coordinated care.
But administrators also know that to accomplish these goals and bring other physicians on board, their best ally is the hospitalist.
Our patients demand more of us, too. In “Zen and the Art of Physician Autonomy Maintenance” in Annals of Internal Medicine in 2003, author Jim Reinertsen clearly stated the public’s perspective. “You claim that your profession is based on science … now show us that you can use all the science you know, for our benefit,” he writes. He asks us to “join together—as a profession—with our colleagues, in venues large and small to decide on and apply the best science.”
It is the least we can do as physicians. But in practice, working together to apply the best science is difficult.
All of which brings me to my final point: SHM’s commitment to our members. In October, SHM sponsored two summits, the first on healthcare quality, the second on leadership development. Two themes emerged. First, it takes an unwavering commitment to teamwork to accomplish anything of substance. Second, the educational needs of our workforce are tremendous. SHM’s focus on acquiring skills and applying knowledge are the society’s greatest accomplishment and greatest ongoing opportunity. To that end, we are working on four fronts.
First, we are developing alliances with other like-minded organizations such as the Case Management Association of America, the American Nursing Association, the American Hospital Association, and the Institute for Healthcare Improvement. Through these alliances we hope to foster the teams that will improve the monitoring of parameters of hospital care, and the care itself.
Second, we are committed to creating the tools to equip hospitalists to make the changes that will lead to improvements in the front lines of hospital medicine. We have taken several such steps. SHM has developed a discharge checklist for physicians to use before sending patients home or to other facilities. The checklist, somewhat like those used by pilots, ensures nothing is forgotten or overlooked upon discharge. We believe it will become an invaluable tool.
SHM has also added Resource Rooms to our Web site (www.hospitalmedicine.org). Here, our members can look up and download information on disease states like heart failure or venous thromboembolism.
Third, SHM is funding a group of quality-control mentors available to visit hospitals. These mentors will evaluate and advise on quality-control programs at SHM’s expense.
Finally, SHM wants to train its next generation of leaders. Quality control is a never-ending quest; it can always be better. That is what we at SHM strive for. That is what we owe our patients.
All these tools have one goal: Make quality easy. With so many other pressures of physicians and hospital staff, making it easy is also the key to making it work.
“Knowing is not enough,” Goethe said. “We must apply.” I say: “Willing is not enough. We must do.” TH
Dr. Holman is president of SHM.
It’s a refrain I have heard too many times in too many places: “Don’t do it.”
You have probably heard it, too—that plaintive cry from some practicing physicians trying to discourage young people from entering a career in medicine. I understand why so many doctors seem so pessimistic about medicine’s future. They’re grappling with a healthcare industry that struggles with overwhelming complexity. They face unrelenting cost pressures, misaligned incentives and policies, massive shortfalls in quality and service, fragmented systems, and disunity among peers.
I understand the pessimism, but I cannot agree with it. At the midpoint of my term as SHM president, I reflect upon the strengths that distinguish our specialty and our society from the general malaise of the broader healthcare industry. These strengths compel me to redouble my resolve to deliver on the promise of hospital medicine.
What is that promise? Hospitalists are poised to lead the way toward a better healthcare system in two critical ways. They are situated to help advance quality control and they are uniquely situated to promote medicine as a team effort, a shared vision with the hospital.
Now, quality control and teamwork are not in the standard curriculum. Medical school training focuses on disease. But in the real world of the hospital, quality control and the teamwork it takes to ensure it are vital issues. This is where hospitalists must prove themselves. This is where our special skills align with the priorities of hospital CEOs nationwide. We must advance the quality agenda and engage other physicians in a shared vision with the hospital.
These factors set us apart from other specialties and allow us to lead from the core of our strength. We lead:
- Through quality rather than narrow professional self-interests;
- While valuing the team over the individual; and
- With openness and inclusiveness to all medical personnel involved patient care, from pharmacists to nurses, to nonphysician providers, to management.
This is our great promise—but only if we exercise it. As the brilliant author and scientist Johann Wolfgang von Goethe cautioned 200 years ago: “Knowing is not enough. We must apply.”
Honesty requires physicians to admit there is sometimes a gap between what we know and what we apply. Many quality metrics measure our performance. For example, we know we must get aspirin to a heart attack victim quickly. But the clinical strides that dictate the care patients ought to get must be moved into the operational area, where optimal care is sometimes lacking.
We next need to work out the systems to ensure that care, turning best practices into routine practice. Hospitalists are in the vanguard on that front, just as other specialties have been on the cutting edge of academic medicine. Our specialty will always need to weigh in on the development and vetting of quality and safety metrics related to hospital care.
We are also poised to advance the implementation and application of systems that drive improvement in those metrics.
Ours is a young specialty—the average hospitalist is 37, the leadership 41. While we have accomplished much in our 10 years of existence, there is much more to do. Hospitalists must meet the extraordinarily high expectations of hospitals and the other physicians who work in them. We must help manage emergency patients, surgical patients, and the in-hospital patient census of primary care physicians.
But there is a shortage of physicians in our specialty because demand is so great. It’s hard to sustain our growth as a specialty and work on quality control at the same time.
We are in the financial crosshairs, as well. Administrators want to see value—that is, money saved. But the fact that we see and manage patients does not generate savings per se because insurance companies do not allow reimbursement as such for our services. “Prove your value,” they say. “Show us the money.” That translates into driving down length of stay, cutting nursing expenses, and reducing pharmacy costs though better quality control and more coordinated care.
But administrators also know that to accomplish these goals and bring other physicians on board, their best ally is the hospitalist.
Our patients demand more of us, too. In “Zen and the Art of Physician Autonomy Maintenance” in Annals of Internal Medicine in 2003, author Jim Reinertsen clearly stated the public’s perspective. “You claim that your profession is based on science … now show us that you can use all the science you know, for our benefit,” he writes. He asks us to “join together—as a profession—with our colleagues, in venues large and small to decide on and apply the best science.”
It is the least we can do as physicians. But in practice, working together to apply the best science is difficult.
All of which brings me to my final point: SHM’s commitment to our members. In October, SHM sponsored two summits, the first on healthcare quality, the second on leadership development. Two themes emerged. First, it takes an unwavering commitment to teamwork to accomplish anything of substance. Second, the educational needs of our workforce are tremendous. SHM’s focus on acquiring skills and applying knowledge are the society’s greatest accomplishment and greatest ongoing opportunity. To that end, we are working on four fronts.
First, we are developing alliances with other like-minded organizations such as the Case Management Association of America, the American Nursing Association, the American Hospital Association, and the Institute for Healthcare Improvement. Through these alliances we hope to foster the teams that will improve the monitoring of parameters of hospital care, and the care itself.
Second, we are committed to creating the tools to equip hospitalists to make the changes that will lead to improvements in the front lines of hospital medicine. We have taken several such steps. SHM has developed a discharge checklist for physicians to use before sending patients home or to other facilities. The checklist, somewhat like those used by pilots, ensures nothing is forgotten or overlooked upon discharge. We believe it will become an invaluable tool.
SHM has also added Resource Rooms to our Web site (www.hospitalmedicine.org). Here, our members can look up and download information on disease states like heart failure or venous thromboembolism.
Third, SHM is funding a group of quality-control mentors available to visit hospitals. These mentors will evaluate and advise on quality-control programs at SHM’s expense.
Finally, SHM wants to train its next generation of leaders. Quality control is a never-ending quest; it can always be better. That is what we at SHM strive for. That is what we owe our patients.
All these tools have one goal: Make quality easy. With so many other pressures of physicians and hospital staff, making it easy is also the key to making it work.
“Knowing is not enough,” Goethe said. “We must apply.” I say: “Willing is not enough. We must do.” TH
Dr. Holman is president of SHM.
It’s a refrain I have heard too many times in too many places: “Don’t do it.”
You have probably heard it, too—that plaintive cry from some practicing physicians trying to discourage young people from entering a career in medicine. I understand why so many doctors seem so pessimistic about medicine’s future. They’re grappling with a healthcare industry that struggles with overwhelming complexity. They face unrelenting cost pressures, misaligned incentives and policies, massive shortfalls in quality and service, fragmented systems, and disunity among peers.
I understand the pessimism, but I cannot agree with it. At the midpoint of my term as SHM president, I reflect upon the strengths that distinguish our specialty and our society from the general malaise of the broader healthcare industry. These strengths compel me to redouble my resolve to deliver on the promise of hospital medicine.
What is that promise? Hospitalists are poised to lead the way toward a better healthcare system in two critical ways. They are situated to help advance quality control and they are uniquely situated to promote medicine as a team effort, a shared vision with the hospital.
Now, quality control and teamwork are not in the standard curriculum. Medical school training focuses on disease. But in the real world of the hospital, quality control and the teamwork it takes to ensure it are vital issues. This is where hospitalists must prove themselves. This is where our special skills align with the priorities of hospital CEOs nationwide. We must advance the quality agenda and engage other physicians in a shared vision with the hospital.
These factors set us apart from other specialties and allow us to lead from the core of our strength. We lead:
- Through quality rather than narrow professional self-interests;
- While valuing the team over the individual; and
- With openness and inclusiveness to all medical personnel involved patient care, from pharmacists to nurses, to nonphysician providers, to management.
This is our great promise—but only if we exercise it. As the brilliant author and scientist Johann Wolfgang von Goethe cautioned 200 years ago: “Knowing is not enough. We must apply.”
Honesty requires physicians to admit there is sometimes a gap between what we know and what we apply. Many quality metrics measure our performance. For example, we know we must get aspirin to a heart attack victim quickly. But the clinical strides that dictate the care patients ought to get must be moved into the operational area, where optimal care is sometimes lacking.
We next need to work out the systems to ensure that care, turning best practices into routine practice. Hospitalists are in the vanguard on that front, just as other specialties have been on the cutting edge of academic medicine. Our specialty will always need to weigh in on the development and vetting of quality and safety metrics related to hospital care.
We are also poised to advance the implementation and application of systems that drive improvement in those metrics.
Ours is a young specialty—the average hospitalist is 37, the leadership 41. While we have accomplished much in our 10 years of existence, there is much more to do. Hospitalists must meet the extraordinarily high expectations of hospitals and the other physicians who work in them. We must help manage emergency patients, surgical patients, and the in-hospital patient census of primary care physicians.
But there is a shortage of physicians in our specialty because demand is so great. It’s hard to sustain our growth as a specialty and work on quality control at the same time.
We are in the financial crosshairs, as well. Administrators want to see value—that is, money saved. But the fact that we see and manage patients does not generate savings per se because insurance companies do not allow reimbursement as such for our services. “Prove your value,” they say. “Show us the money.” That translates into driving down length of stay, cutting nursing expenses, and reducing pharmacy costs though better quality control and more coordinated care.
But administrators also know that to accomplish these goals and bring other physicians on board, their best ally is the hospitalist.
Our patients demand more of us, too. In “Zen and the Art of Physician Autonomy Maintenance” in Annals of Internal Medicine in 2003, author Jim Reinertsen clearly stated the public’s perspective. “You claim that your profession is based on science … now show us that you can use all the science you know, for our benefit,” he writes. He asks us to “join together—as a profession—with our colleagues, in venues large and small to decide on and apply the best science.”
It is the least we can do as physicians. But in practice, working together to apply the best science is difficult.
All of which brings me to my final point: SHM’s commitment to our members. In October, SHM sponsored two summits, the first on healthcare quality, the second on leadership development. Two themes emerged. First, it takes an unwavering commitment to teamwork to accomplish anything of substance. Second, the educational needs of our workforce are tremendous. SHM’s focus on acquiring skills and applying knowledge are the society’s greatest accomplishment and greatest ongoing opportunity. To that end, we are working on four fronts.
First, we are developing alliances with other like-minded organizations such as the Case Management Association of America, the American Nursing Association, the American Hospital Association, and the Institute for Healthcare Improvement. Through these alliances we hope to foster the teams that will improve the monitoring of parameters of hospital care, and the care itself.
Second, we are committed to creating the tools to equip hospitalists to make the changes that will lead to improvements in the front lines of hospital medicine. We have taken several such steps. SHM has developed a discharge checklist for physicians to use before sending patients home or to other facilities. The checklist, somewhat like those used by pilots, ensures nothing is forgotten or overlooked upon discharge. We believe it will become an invaluable tool.
SHM has also added Resource Rooms to our Web site (www.hospitalmedicine.org). Here, our members can look up and download information on disease states like heart failure or venous thromboembolism.
Third, SHM is funding a group of quality-control mentors available to visit hospitals. These mentors will evaluate and advise on quality-control programs at SHM’s expense.
Finally, SHM wants to train its next generation of leaders. Quality control is a never-ending quest; it can always be better. That is what we at SHM strive for. That is what we owe our patients.
All these tools have one goal: Make quality easy. With so many other pressures of physicians and hospital staff, making it easy is also the key to making it work.
“Knowing is not enough,” Goethe said. “We must apply.” I say: “Willing is not enough. We must do.” TH
Dr. Holman is president of SHM.
Ahead of the Curve
Twenty years before the term “hospitalist” was coined, and not long after serving as a battlefield surgeon in Vietnam, Tracy Spencer III, MD, selected a path few—if any—had chosen before.
Fresh from his combat experience, he became chief resident at the University of Colorado School of Medicine in Denver in 1975. He dreaded clinic hours but enjoyed the hospital. The flash, dash, and adrenaline of battlefield medicine were still in his blood; he wanted challenges.
“I didn’t want an outpatient practice with the overhead of an office,” says Dr. Spencer, 63, “I wanted to do internal medicine in a hospital setting. I had tons of energy to deal with the unassigned patients who came in the ER, and [I liked] the idea of being a hospital-based physician.”
He began searching for the right setting for his skills and temperament. Eventually, the third-generation physician made a bold leap—he started a hospital-based internal medicine practice in Everett, Wash.
Grass-roots Campaign
In 1976, Dr. Spencer knocked on lots of doors and convinced scores of Everett’s primary care physicians that his caring for their hospitalized patients would free them to build their practices. Although many of those physicians thought it bizarre that Dr. Spencer had no outpatients, they readily turned over their inpatients to him.
“I believe he was one of the first, if not the first, hospitalist in the state of Washington, and perhaps the country,” says John Cramer, MD, MBA, an intern at the University of Colorado 1974-1975 when Dr. Spencer was chief resident. Their relationship has endured more than three decades—with a twist. Now the former intern, who joined Dr. Spencer as a hospitalist in 1979, supervises his former boss in the growing 32-physician hospitalist group at Providence Everett Medical Center.
“Tracy is a member of the team, dispensing wisdom to the younger docs,” says Dr. Cramer. “I have never seen him happier professionally than he is now.”
Early Influence
Dr. Spencer’s medical training and early experiences shed light on how he came to be an inpatient physician two decades before hospitalist medicine formally emerged.
Theodore Woodward, MD, nominated for a Nobel Prize in 1948 for his work on typhus and typhoid, was Dr. Spencer’s professor at the University of Maryland, Baltimore. He impressed Dr. Woodward with “an old-fashioned, knowledge-based, and holistic approach to patients.”
Later, Thomas Petty, MD, an eminent pulmonologist who headed a respiratory team at the University of Colorado Medical Center and became chairman of the National Lung Educational Program, introduced the young physician to a team-based approach to hospital care. During his 1968-1969 internship at the University of Colorado under Dr. Petty, Dr. Spencer found he enjoyed working on a hospital team and the discipline of the hospital hierarchy.
After graduating from medical school, Dr. Spencer was drafted in 1970 by the Marines and was sent to Dà Nang, Vietnam. As a regimental doctor, he worked alone—and didn’t like it. “There was no collegiality for field combat docs,” he recalls. “There were ship-based specialists who didn’t even talk to us. The most serious cases we triaged were [taken] to the ship, and I didn’t see them again. I was dissatisfied and felt that the doctors in the field deserved more respect.”
Maurice Ramirez, DO, an emergency physician and federal medical officer with the Department of Homeland Security, suggests the military’s command structure may have influenced Dr. Spencer more than he realizes. “Before hospitalist medicine, physicians were like British aristocrats in their fiefdoms, ordering their lessers about,” explains Dr. Ramirez. “[The] hospitalist movement has changed all that.”
Turning Point
Dr. Spencer returned from his tour of duty and began his chief resident stint at the University of Colorado in 1975.
That year, Boyd Bigelow, MD, “a maverick with a plane” by Dr. Spencer’s account, hired him to admit and manage patients at Denver’s St. Anthony’s Central Hospital, which had no house staff. “To compete with big hospitals, we’d fly referrals into Stapleton [Air Force Base],” Dr. Spencer says. Dr. Bigelow became medical director of Flight for Life, the first civilian airborne emergency medical service, which has flown more than 65,000 patients to critical care facilities. He would swoop down from the sky through Colorado’s whirling snow, delivering patients to Dr. Spencer.
In 1976 Dr. Spencer took stock of his career and recognized he wanted to be a hospital-based physician. He contacted John Hoidal, MD, from his University of Colorado days, expecting to buddy up, move both of their families to Everett, and cover inpatients at two hospitals 24/7. But Dr. Hoidal chose not to go.
“It would have been easier if the two of us had started the hospitalist practice together, but it wasn’t right for him,” says Dr. Spencer. “I saw that I could do it on my own. I had energy to burn and ambition to succeed.”
Undaunted, he soldiered on to Everett.
“It is an absolutely gorgeous place to live,” he says. “When we arrived I found Everett loaded with GPs in their busy offices, and I had the expertise they needed to manage their inpatients. I hooked them with my three A’s: availability, affability, and ability.”
Everett Hospital hired him to provide 24/7 coverage for respiratory care, the intensive care unit, medical/surgical consults, and overall inpatient management. He worked solo for more than a year and grew exhausted. He hired a second physician in 1977, then Dr. Cramer in 1979.
Also in 1977, Dr. Spencer forged what has become a 30-year professional relationship with Eric Larson, MD, MPH, executive director of the Center for Health Studies Group in Everett.
“In 1977 I was chief resident at Providence General [which merged with Everett Hospital to become Providence Everett Medical Center in 1994],” Dr. Larson says. “Tracy introduced himself as a hospitalist and said he took care of patients in the hospital for GPs. It seemed like an interesting solo practice model.”
What struck Dr. Larson at the time was the contrast between the commotion of a teaching hospital with medical students, interns, residents, and attendings “tripping all over each other” and Dr. Spencer’s approach.
“He embodied the principle of keeping things simple and was organized and methodical in his approach to patients,” Dr. Larson says. “He was superb in pulmonary medicine and the ICU.”
Challenging Times
The hospitalist practice and Everett’s medical community kept growing through the early ’80s, with specialists joining general practitioners in using Dr. Spencer’s group for consults and co-management. Then came managed care in the mid-’80s, and the hospitalists’ gains seemed threatened. “Managed care’s tight controls and preauthorizes of inpatient services were terribly frustrating,” says Dr. Larson. Dr. Spencer found himself competing for managed-care contracts rather than seeing patients.
By the time managed care loosened its grip in the 1990s and the hospitalist movement was officially launched, there were new challenges and frustrations. Dr. Spencer felt worn out administrating rather than doctoring. Dr. Larson felt something else: futility. “One of the hardest things about being a hospitalist is dealing with the futility of treating old people with multiple co-morbidities who shouldn’t even be in a hospital,” explains Dr. Larson. “Hospitals are now so protocolized. Once a patient gets in the hospital he’s almost on automatic.”
Frustrated and tired 25 years after becoming the first hospitalist, Dr. Spencer retired in April 2001. Then he realized he wasn’t finished with medicine. Six months later he joined the hospitalist cadre led by his former intern, Dr. Cramer, at the Everett Clinic, a multispecialty group with 250 physicians and 65 midlevel providers.
Putting 30 years of hospitalist experience to work, Dr. Spencer recruits young hospitalists, teaches best practices, and continues to build relationships with general practitioners and specialists. From his unique vantage point, he sees hospital medicine as a maturing discipline gone mainstream.
“There’s still so much to do,” he says. He plans to explore a variety of hospitalist growth areas, such as efficient use of diagnostic testing, higher intensity medicine with patients of markedly higher acuity, step-down cardiac telemetry, more involvement with ICUs, and managing complex patients living with multiple co-morbidities.
But Dr. Ramirez says that with all he’s already accomplished, Dr. Spencer has earned a place of note: “I hope that hospitalists recognize he was three decades and six generations of physicians ahead of his time.” TH
Marlene Piturro is a medical writer based in New York.
Twenty years before the term “hospitalist” was coined, and not long after serving as a battlefield surgeon in Vietnam, Tracy Spencer III, MD, selected a path few—if any—had chosen before.
Fresh from his combat experience, he became chief resident at the University of Colorado School of Medicine in Denver in 1975. He dreaded clinic hours but enjoyed the hospital. The flash, dash, and adrenaline of battlefield medicine were still in his blood; he wanted challenges.
“I didn’t want an outpatient practice with the overhead of an office,” says Dr. Spencer, 63, “I wanted to do internal medicine in a hospital setting. I had tons of energy to deal with the unassigned patients who came in the ER, and [I liked] the idea of being a hospital-based physician.”
He began searching for the right setting for his skills and temperament. Eventually, the third-generation physician made a bold leap—he started a hospital-based internal medicine practice in Everett, Wash.
Grass-roots Campaign
In 1976, Dr. Spencer knocked on lots of doors and convinced scores of Everett’s primary care physicians that his caring for their hospitalized patients would free them to build their practices. Although many of those physicians thought it bizarre that Dr. Spencer had no outpatients, they readily turned over their inpatients to him.
“I believe he was one of the first, if not the first, hospitalist in the state of Washington, and perhaps the country,” says John Cramer, MD, MBA, an intern at the University of Colorado 1974-1975 when Dr. Spencer was chief resident. Their relationship has endured more than three decades—with a twist. Now the former intern, who joined Dr. Spencer as a hospitalist in 1979, supervises his former boss in the growing 32-physician hospitalist group at Providence Everett Medical Center.
“Tracy is a member of the team, dispensing wisdom to the younger docs,” says Dr. Cramer. “I have never seen him happier professionally than he is now.”
Early Influence
Dr. Spencer’s medical training and early experiences shed light on how he came to be an inpatient physician two decades before hospitalist medicine formally emerged.
Theodore Woodward, MD, nominated for a Nobel Prize in 1948 for his work on typhus and typhoid, was Dr. Spencer’s professor at the University of Maryland, Baltimore. He impressed Dr. Woodward with “an old-fashioned, knowledge-based, and holistic approach to patients.”
Later, Thomas Petty, MD, an eminent pulmonologist who headed a respiratory team at the University of Colorado Medical Center and became chairman of the National Lung Educational Program, introduced the young physician to a team-based approach to hospital care. During his 1968-1969 internship at the University of Colorado under Dr. Petty, Dr. Spencer found he enjoyed working on a hospital team and the discipline of the hospital hierarchy.
After graduating from medical school, Dr. Spencer was drafted in 1970 by the Marines and was sent to Dà Nang, Vietnam. As a regimental doctor, he worked alone—and didn’t like it. “There was no collegiality for field combat docs,” he recalls. “There were ship-based specialists who didn’t even talk to us. The most serious cases we triaged were [taken] to the ship, and I didn’t see them again. I was dissatisfied and felt that the doctors in the field deserved more respect.”
Maurice Ramirez, DO, an emergency physician and federal medical officer with the Department of Homeland Security, suggests the military’s command structure may have influenced Dr. Spencer more than he realizes. “Before hospitalist medicine, physicians were like British aristocrats in their fiefdoms, ordering their lessers about,” explains Dr. Ramirez. “[The] hospitalist movement has changed all that.”
Turning Point
Dr. Spencer returned from his tour of duty and began his chief resident stint at the University of Colorado in 1975.
That year, Boyd Bigelow, MD, “a maverick with a plane” by Dr. Spencer’s account, hired him to admit and manage patients at Denver’s St. Anthony’s Central Hospital, which had no house staff. “To compete with big hospitals, we’d fly referrals into Stapleton [Air Force Base],” Dr. Spencer says. Dr. Bigelow became medical director of Flight for Life, the first civilian airborne emergency medical service, which has flown more than 65,000 patients to critical care facilities. He would swoop down from the sky through Colorado’s whirling snow, delivering patients to Dr. Spencer.
In 1976 Dr. Spencer took stock of his career and recognized he wanted to be a hospital-based physician. He contacted John Hoidal, MD, from his University of Colorado days, expecting to buddy up, move both of their families to Everett, and cover inpatients at two hospitals 24/7. But Dr. Hoidal chose not to go.
“It would have been easier if the two of us had started the hospitalist practice together, but it wasn’t right for him,” says Dr. Spencer. “I saw that I could do it on my own. I had energy to burn and ambition to succeed.”
Undaunted, he soldiered on to Everett.
“It is an absolutely gorgeous place to live,” he says. “When we arrived I found Everett loaded with GPs in their busy offices, and I had the expertise they needed to manage their inpatients. I hooked them with my three A’s: availability, affability, and ability.”
Everett Hospital hired him to provide 24/7 coverage for respiratory care, the intensive care unit, medical/surgical consults, and overall inpatient management. He worked solo for more than a year and grew exhausted. He hired a second physician in 1977, then Dr. Cramer in 1979.
Also in 1977, Dr. Spencer forged what has become a 30-year professional relationship with Eric Larson, MD, MPH, executive director of the Center for Health Studies Group in Everett.
“In 1977 I was chief resident at Providence General [which merged with Everett Hospital to become Providence Everett Medical Center in 1994],” Dr. Larson says. “Tracy introduced himself as a hospitalist and said he took care of patients in the hospital for GPs. It seemed like an interesting solo practice model.”
What struck Dr. Larson at the time was the contrast between the commotion of a teaching hospital with medical students, interns, residents, and attendings “tripping all over each other” and Dr. Spencer’s approach.
“He embodied the principle of keeping things simple and was organized and methodical in his approach to patients,” Dr. Larson says. “He was superb in pulmonary medicine and the ICU.”
Challenging Times
The hospitalist practice and Everett’s medical community kept growing through the early ’80s, with specialists joining general practitioners in using Dr. Spencer’s group for consults and co-management. Then came managed care in the mid-’80s, and the hospitalists’ gains seemed threatened. “Managed care’s tight controls and preauthorizes of inpatient services were terribly frustrating,” says Dr. Larson. Dr. Spencer found himself competing for managed-care contracts rather than seeing patients.
By the time managed care loosened its grip in the 1990s and the hospitalist movement was officially launched, there were new challenges and frustrations. Dr. Spencer felt worn out administrating rather than doctoring. Dr. Larson felt something else: futility. “One of the hardest things about being a hospitalist is dealing with the futility of treating old people with multiple co-morbidities who shouldn’t even be in a hospital,” explains Dr. Larson. “Hospitals are now so protocolized. Once a patient gets in the hospital he’s almost on automatic.”
Frustrated and tired 25 years after becoming the first hospitalist, Dr. Spencer retired in April 2001. Then he realized he wasn’t finished with medicine. Six months later he joined the hospitalist cadre led by his former intern, Dr. Cramer, at the Everett Clinic, a multispecialty group with 250 physicians and 65 midlevel providers.
Putting 30 years of hospitalist experience to work, Dr. Spencer recruits young hospitalists, teaches best practices, and continues to build relationships with general practitioners and specialists. From his unique vantage point, he sees hospital medicine as a maturing discipline gone mainstream.
“There’s still so much to do,” he says. He plans to explore a variety of hospitalist growth areas, such as efficient use of diagnostic testing, higher intensity medicine with patients of markedly higher acuity, step-down cardiac telemetry, more involvement with ICUs, and managing complex patients living with multiple co-morbidities.
But Dr. Ramirez says that with all he’s already accomplished, Dr. Spencer has earned a place of note: “I hope that hospitalists recognize he was three decades and six generations of physicians ahead of his time.” TH
Marlene Piturro is a medical writer based in New York.
Twenty years before the term “hospitalist” was coined, and not long after serving as a battlefield surgeon in Vietnam, Tracy Spencer III, MD, selected a path few—if any—had chosen before.
Fresh from his combat experience, he became chief resident at the University of Colorado School of Medicine in Denver in 1975. He dreaded clinic hours but enjoyed the hospital. The flash, dash, and adrenaline of battlefield medicine were still in his blood; he wanted challenges.
“I didn’t want an outpatient practice with the overhead of an office,” says Dr. Spencer, 63, “I wanted to do internal medicine in a hospital setting. I had tons of energy to deal with the unassigned patients who came in the ER, and [I liked] the idea of being a hospital-based physician.”
He began searching for the right setting for his skills and temperament. Eventually, the third-generation physician made a bold leap—he started a hospital-based internal medicine practice in Everett, Wash.
Grass-roots Campaign
In 1976, Dr. Spencer knocked on lots of doors and convinced scores of Everett’s primary care physicians that his caring for their hospitalized patients would free them to build their practices. Although many of those physicians thought it bizarre that Dr. Spencer had no outpatients, they readily turned over their inpatients to him.
“I believe he was one of the first, if not the first, hospitalist in the state of Washington, and perhaps the country,” says John Cramer, MD, MBA, an intern at the University of Colorado 1974-1975 when Dr. Spencer was chief resident. Their relationship has endured more than three decades—with a twist. Now the former intern, who joined Dr. Spencer as a hospitalist in 1979, supervises his former boss in the growing 32-physician hospitalist group at Providence Everett Medical Center.
“Tracy is a member of the team, dispensing wisdom to the younger docs,” says Dr. Cramer. “I have never seen him happier professionally than he is now.”
Early Influence
Dr. Spencer’s medical training and early experiences shed light on how he came to be an inpatient physician two decades before hospitalist medicine formally emerged.
Theodore Woodward, MD, nominated for a Nobel Prize in 1948 for his work on typhus and typhoid, was Dr. Spencer’s professor at the University of Maryland, Baltimore. He impressed Dr. Woodward with “an old-fashioned, knowledge-based, and holistic approach to patients.”
Later, Thomas Petty, MD, an eminent pulmonologist who headed a respiratory team at the University of Colorado Medical Center and became chairman of the National Lung Educational Program, introduced the young physician to a team-based approach to hospital care. During his 1968-1969 internship at the University of Colorado under Dr. Petty, Dr. Spencer found he enjoyed working on a hospital team and the discipline of the hospital hierarchy.
After graduating from medical school, Dr. Spencer was drafted in 1970 by the Marines and was sent to Dà Nang, Vietnam. As a regimental doctor, he worked alone—and didn’t like it. “There was no collegiality for field combat docs,” he recalls. “There were ship-based specialists who didn’t even talk to us. The most serious cases we triaged were [taken] to the ship, and I didn’t see them again. I was dissatisfied and felt that the doctors in the field deserved more respect.”
Maurice Ramirez, DO, an emergency physician and federal medical officer with the Department of Homeland Security, suggests the military’s command structure may have influenced Dr. Spencer more than he realizes. “Before hospitalist medicine, physicians were like British aristocrats in their fiefdoms, ordering their lessers about,” explains Dr. Ramirez. “[The] hospitalist movement has changed all that.”
Turning Point
Dr. Spencer returned from his tour of duty and began his chief resident stint at the University of Colorado in 1975.
That year, Boyd Bigelow, MD, “a maverick with a plane” by Dr. Spencer’s account, hired him to admit and manage patients at Denver’s St. Anthony’s Central Hospital, which had no house staff. “To compete with big hospitals, we’d fly referrals into Stapleton [Air Force Base],” Dr. Spencer says. Dr. Bigelow became medical director of Flight for Life, the first civilian airborne emergency medical service, which has flown more than 65,000 patients to critical care facilities. He would swoop down from the sky through Colorado’s whirling snow, delivering patients to Dr. Spencer.
In 1976 Dr. Spencer took stock of his career and recognized he wanted to be a hospital-based physician. He contacted John Hoidal, MD, from his University of Colorado days, expecting to buddy up, move both of their families to Everett, and cover inpatients at two hospitals 24/7. But Dr. Hoidal chose not to go.
“It would have been easier if the two of us had started the hospitalist practice together, but it wasn’t right for him,” says Dr. Spencer. “I saw that I could do it on my own. I had energy to burn and ambition to succeed.”
Undaunted, he soldiered on to Everett.
“It is an absolutely gorgeous place to live,” he says. “When we arrived I found Everett loaded with GPs in their busy offices, and I had the expertise they needed to manage their inpatients. I hooked them with my three A’s: availability, affability, and ability.”
Everett Hospital hired him to provide 24/7 coverage for respiratory care, the intensive care unit, medical/surgical consults, and overall inpatient management. He worked solo for more than a year and grew exhausted. He hired a second physician in 1977, then Dr. Cramer in 1979.
Also in 1977, Dr. Spencer forged what has become a 30-year professional relationship with Eric Larson, MD, MPH, executive director of the Center for Health Studies Group in Everett.
“In 1977 I was chief resident at Providence General [which merged with Everett Hospital to become Providence Everett Medical Center in 1994],” Dr. Larson says. “Tracy introduced himself as a hospitalist and said he took care of patients in the hospital for GPs. It seemed like an interesting solo practice model.”
What struck Dr. Larson at the time was the contrast between the commotion of a teaching hospital with medical students, interns, residents, and attendings “tripping all over each other” and Dr. Spencer’s approach.
“He embodied the principle of keeping things simple and was organized and methodical in his approach to patients,” Dr. Larson says. “He was superb in pulmonary medicine and the ICU.”
Challenging Times
The hospitalist practice and Everett’s medical community kept growing through the early ’80s, with specialists joining general practitioners in using Dr. Spencer’s group for consults and co-management. Then came managed care in the mid-’80s, and the hospitalists’ gains seemed threatened. “Managed care’s tight controls and preauthorizes of inpatient services were terribly frustrating,” says Dr. Larson. Dr. Spencer found himself competing for managed-care contracts rather than seeing patients.
By the time managed care loosened its grip in the 1990s and the hospitalist movement was officially launched, there were new challenges and frustrations. Dr. Spencer felt worn out administrating rather than doctoring. Dr. Larson felt something else: futility. “One of the hardest things about being a hospitalist is dealing with the futility of treating old people with multiple co-morbidities who shouldn’t even be in a hospital,” explains Dr. Larson. “Hospitals are now so protocolized. Once a patient gets in the hospital he’s almost on automatic.”
Frustrated and tired 25 years after becoming the first hospitalist, Dr. Spencer retired in April 2001. Then he realized he wasn’t finished with medicine. Six months later he joined the hospitalist cadre led by his former intern, Dr. Cramer, at the Everett Clinic, a multispecialty group with 250 physicians and 65 midlevel providers.
Putting 30 years of hospitalist experience to work, Dr. Spencer recruits young hospitalists, teaches best practices, and continues to build relationships with general practitioners and specialists. From his unique vantage point, he sees hospital medicine as a maturing discipline gone mainstream.
“There’s still so much to do,” he says. He plans to explore a variety of hospitalist growth areas, such as efficient use of diagnostic testing, higher intensity medicine with patients of markedly higher acuity, step-down cardiac telemetry, more involvement with ICUs, and managing complex patients living with multiple co-morbidities.
But Dr. Ramirez says that with all he’s already accomplished, Dr. Spencer has earned a place of note: “I hope that hospitalists recognize he was three decades and six generations of physicians ahead of his time.” TH
Marlene Piturro is a medical writer based in New York.
Birth of the Beth
Were you born at “the Beth?” Generations are proud to have entered the world at Newark Beth Israel Medical Center, a 673-bed teaching hospital that offers comprehensive healthcare to its communities and is a major referral and treatment center for patients throughout the northern New Jersey metropolitan area.
The lively history of Newark Beth Israel Medical Center, an affiliate of the Saint Barnabas Health Care System, is typical of the histories of the voluntary nonprofit Jewish hospitals in the United States from the mid-19th to mid-20th centuries.
The Need for Healthcare
At the turn of the 20th century, Newark, N.J. was a city filled with tanneries, breweries, varnish factories, fine silver manufacturers, and inventors who hoped to emulate its most famous resident—Thomas Edison.
City officials struggled to overcome the myriad industrial accidents, sanitation problems, and epidemics of diphtheria, typhus, and smallpox that had made Newark the nation’s unhealthiest city.
With population exceeding 100,000 in the 1890 census, Newark would endure one of the first outbreaks of polio in 1916. Because of its proximity to Fort Dix, the city was an epicenter of the 1918 influenza pandemic.
On Oct. 22, 1900, Newark residents first learned of the possibility of a Jewish hospital when newsboys held up copies of the Newark Evening News and shouted, “There’s Trouble in the Beth Israel Hospital Association!” When the men of the association voted to open a storefront dispensary, the women broke away, renaming themselves the Daughters of Israel and purchasing a crumbling mansion that opened as a 28-bed hospital on Aug. 31, 1902. For six years, the dispensary and hospital operated separate facilities. They merged their services in 1908, when a 110-bed, four-story facility opened on the site of the old mansion.
Expression of Assimilation
“They come to the United States, eager to breathe the air of freedom, anxious to repay the country for this blessing that she offers,” said Reform Rabbi Solomon Foster at the dedication ceremony Jan. 30, 1908. For the Eastern European Jews who passed through Ellis Island from 1880 to 1920, the founding of a Jewish hospital became their expression of becoming Americans.
In Newark, more than 87 Jewish societies, workmen’s lodges, and synagogues provided funds for the hospital. The 1908 opening was celebrated with a massive parade through the immigrant neighborhood, where tenements were festooned with American flag bunting.
The Beth practiced a nonsectarian policy in hospital admissions, the extension of hospital privileges to doctors, and the hiring of hospital staff. “While this hospital will be mainly supported by Jews, it will open its doors just as wide as they can swing to receive all who may desire to enter, and his religious sentiments shall be carefully safeguarded,” the policy stated. Kosher meals were available upon request, and Christmas decorations were displayed to cheer patients.
Community-based Care
In 1924, a new, modern image of the hospital appeared on billboards and newspapers: Miss Beth, who launched a campaign for a new hospital with the question: “Is your heart with the hospital?”
The third hospital—a 350-bed yellow-brick tower with a Spanish tile roof—rose nearly 200 feet from its foundation like a sentinel beckoning its community. The new hospital opened in 1928, relocated from the city center to the southern tip of the city north of Lake Weequahic.
The Jewish community followed its hospital to settle in the surrounding streets, transforming it into a vibrant Jewish neighborhood celebrated by Philip Roth in his many novels about Newark.
The Beth was committed to providing training and research opportunities to doctors—Jewish and non-Jewish—who were denied privileges at other hospitals early in the 20th century.
The commitment to providing high-caliber training was evident in its accreditation from the American College of Surgeons in 1919 and the AMA Council approval for the internships in 1921.
By 1930, the laboratory, physical therapy, social work, and dietary departments were offering technical training programs. During World War II, it was designated as one of 1,000 depots that stored penicillin.
During the Great Depression, despite financial difficulties that nearly bankrupted the hospital, the Beth maintained an animal house for research. It was at the Beth that the Rh factor was identified as the cause of erythroblastosis fetalis.
A Laboratory Research Foundation was created to provide funding for research projects and support publication of a hospital journal. The journal published the earliest research results of the Beth Cardiopulmonary Laboratory, which became a leading center for the development of the pacemaker.
In the mid-1960s, as the Newark Jewish community resettled in the outlying New Jersey suburbs, hospital leaders decided to remain on Lyons Avenue and expand into a regional medical center.
Like other industrial cities, Newark suffered through a turbulent decade, requiring the hospital to redefine itself in its mission to serve its neighborhood and waves of immigrants settling into the region.
Federal grant programs and loans from the Prudential Life Insurance Corp. enabled the phased construction of a fourth hospital complex next to the old hospital, providing inpatient and ambulatory care services.
In 1996, Newark Beth Israel Hospital and Medical Center became an affiliate of Barnabas Health Care—New Jersey’s largest integrated healthcare system.
The Beth Today
These days, Newark Beth Israel Hospital and Medical Center is a major teaching affiliate of the Mount Sinai School of Medicine in New York City, the New York College of Osteopathic Medicine in Old Westbury, N.Y, and St. George’s University School of Medicine in Grenada.
The Beth’s division of cardiology continues pioneering work on therapeutic cardiac services and offers the most comprehensive robotic surgical center in the state.
And, honoring a 75-year-old tradition, the center still holds the outreach health screening and health fairs program begun by the Maternity Guild as a citywide public health initiative.
At its inception, the “Born at the Beth” program meant every baby born in the hospital was eligible to join a Babies’ Alumni Club. The $1 annual dues paid on their behalf entitled them to attend an annual babies’ health fair at which they enjoyed Dixie cups of ice cream and free examinations from the hospital staff. Now, the hospital offers the Born at the Beth Wall of Recognition to pay tribute to all those who greeted life within the hospital’s walls.
The Star of David remains at the front entrance, an enduring symbol of the hospital’s heritage. And the hospital’s creed—first displayed in 1928—still asserts the commitment of its staff: “The value of the human touch as a power for healing is never lost sight of at Beth Israel.” TH
The Krauts are coauthors of “Covenant of Care: Newark Beth Israel Hospital and the Jewish Hospital in America.”
Were you born at “the Beth?” Generations are proud to have entered the world at Newark Beth Israel Medical Center, a 673-bed teaching hospital that offers comprehensive healthcare to its communities and is a major referral and treatment center for patients throughout the northern New Jersey metropolitan area.
The lively history of Newark Beth Israel Medical Center, an affiliate of the Saint Barnabas Health Care System, is typical of the histories of the voluntary nonprofit Jewish hospitals in the United States from the mid-19th to mid-20th centuries.
The Need for Healthcare
At the turn of the 20th century, Newark, N.J. was a city filled with tanneries, breweries, varnish factories, fine silver manufacturers, and inventors who hoped to emulate its most famous resident—Thomas Edison.
City officials struggled to overcome the myriad industrial accidents, sanitation problems, and epidemics of diphtheria, typhus, and smallpox that had made Newark the nation’s unhealthiest city.
With population exceeding 100,000 in the 1890 census, Newark would endure one of the first outbreaks of polio in 1916. Because of its proximity to Fort Dix, the city was an epicenter of the 1918 influenza pandemic.
On Oct. 22, 1900, Newark residents first learned of the possibility of a Jewish hospital when newsboys held up copies of the Newark Evening News and shouted, “There’s Trouble in the Beth Israel Hospital Association!” When the men of the association voted to open a storefront dispensary, the women broke away, renaming themselves the Daughters of Israel and purchasing a crumbling mansion that opened as a 28-bed hospital on Aug. 31, 1902. For six years, the dispensary and hospital operated separate facilities. They merged their services in 1908, when a 110-bed, four-story facility opened on the site of the old mansion.
Expression of Assimilation
“They come to the United States, eager to breathe the air of freedom, anxious to repay the country for this blessing that she offers,” said Reform Rabbi Solomon Foster at the dedication ceremony Jan. 30, 1908. For the Eastern European Jews who passed through Ellis Island from 1880 to 1920, the founding of a Jewish hospital became their expression of becoming Americans.
In Newark, more than 87 Jewish societies, workmen’s lodges, and synagogues provided funds for the hospital. The 1908 opening was celebrated with a massive parade through the immigrant neighborhood, where tenements were festooned with American flag bunting.
The Beth practiced a nonsectarian policy in hospital admissions, the extension of hospital privileges to doctors, and the hiring of hospital staff. “While this hospital will be mainly supported by Jews, it will open its doors just as wide as they can swing to receive all who may desire to enter, and his religious sentiments shall be carefully safeguarded,” the policy stated. Kosher meals were available upon request, and Christmas decorations were displayed to cheer patients.
Community-based Care
In 1924, a new, modern image of the hospital appeared on billboards and newspapers: Miss Beth, who launched a campaign for a new hospital with the question: “Is your heart with the hospital?”
The third hospital—a 350-bed yellow-brick tower with a Spanish tile roof—rose nearly 200 feet from its foundation like a sentinel beckoning its community. The new hospital opened in 1928, relocated from the city center to the southern tip of the city north of Lake Weequahic.
The Jewish community followed its hospital to settle in the surrounding streets, transforming it into a vibrant Jewish neighborhood celebrated by Philip Roth in his many novels about Newark.
The Beth was committed to providing training and research opportunities to doctors—Jewish and non-Jewish—who were denied privileges at other hospitals early in the 20th century.
The commitment to providing high-caliber training was evident in its accreditation from the American College of Surgeons in 1919 and the AMA Council approval for the internships in 1921.
By 1930, the laboratory, physical therapy, social work, and dietary departments were offering technical training programs. During World War II, it was designated as one of 1,000 depots that stored penicillin.
During the Great Depression, despite financial difficulties that nearly bankrupted the hospital, the Beth maintained an animal house for research. It was at the Beth that the Rh factor was identified as the cause of erythroblastosis fetalis.
A Laboratory Research Foundation was created to provide funding for research projects and support publication of a hospital journal. The journal published the earliest research results of the Beth Cardiopulmonary Laboratory, which became a leading center for the development of the pacemaker.
In the mid-1960s, as the Newark Jewish community resettled in the outlying New Jersey suburbs, hospital leaders decided to remain on Lyons Avenue and expand into a regional medical center.
Like other industrial cities, Newark suffered through a turbulent decade, requiring the hospital to redefine itself in its mission to serve its neighborhood and waves of immigrants settling into the region.
Federal grant programs and loans from the Prudential Life Insurance Corp. enabled the phased construction of a fourth hospital complex next to the old hospital, providing inpatient and ambulatory care services.
In 1996, Newark Beth Israel Hospital and Medical Center became an affiliate of Barnabas Health Care—New Jersey’s largest integrated healthcare system.
The Beth Today
These days, Newark Beth Israel Hospital and Medical Center is a major teaching affiliate of the Mount Sinai School of Medicine in New York City, the New York College of Osteopathic Medicine in Old Westbury, N.Y, and St. George’s University School of Medicine in Grenada.
The Beth’s division of cardiology continues pioneering work on therapeutic cardiac services and offers the most comprehensive robotic surgical center in the state.
And, honoring a 75-year-old tradition, the center still holds the outreach health screening and health fairs program begun by the Maternity Guild as a citywide public health initiative.
At its inception, the “Born at the Beth” program meant every baby born in the hospital was eligible to join a Babies’ Alumni Club. The $1 annual dues paid on their behalf entitled them to attend an annual babies’ health fair at which they enjoyed Dixie cups of ice cream and free examinations from the hospital staff. Now, the hospital offers the Born at the Beth Wall of Recognition to pay tribute to all those who greeted life within the hospital’s walls.
The Star of David remains at the front entrance, an enduring symbol of the hospital’s heritage. And the hospital’s creed—first displayed in 1928—still asserts the commitment of its staff: “The value of the human touch as a power for healing is never lost sight of at Beth Israel.” TH
The Krauts are coauthors of “Covenant of Care: Newark Beth Israel Hospital and the Jewish Hospital in America.”
Were you born at “the Beth?” Generations are proud to have entered the world at Newark Beth Israel Medical Center, a 673-bed teaching hospital that offers comprehensive healthcare to its communities and is a major referral and treatment center for patients throughout the northern New Jersey metropolitan area.
The lively history of Newark Beth Israel Medical Center, an affiliate of the Saint Barnabas Health Care System, is typical of the histories of the voluntary nonprofit Jewish hospitals in the United States from the mid-19th to mid-20th centuries.
The Need for Healthcare
At the turn of the 20th century, Newark, N.J. was a city filled with tanneries, breweries, varnish factories, fine silver manufacturers, and inventors who hoped to emulate its most famous resident—Thomas Edison.
City officials struggled to overcome the myriad industrial accidents, sanitation problems, and epidemics of diphtheria, typhus, and smallpox that had made Newark the nation’s unhealthiest city.
With population exceeding 100,000 in the 1890 census, Newark would endure one of the first outbreaks of polio in 1916. Because of its proximity to Fort Dix, the city was an epicenter of the 1918 influenza pandemic.
On Oct. 22, 1900, Newark residents first learned of the possibility of a Jewish hospital when newsboys held up copies of the Newark Evening News and shouted, “There’s Trouble in the Beth Israel Hospital Association!” When the men of the association voted to open a storefront dispensary, the women broke away, renaming themselves the Daughters of Israel and purchasing a crumbling mansion that opened as a 28-bed hospital on Aug. 31, 1902. For six years, the dispensary and hospital operated separate facilities. They merged their services in 1908, when a 110-bed, four-story facility opened on the site of the old mansion.
Expression of Assimilation
“They come to the United States, eager to breathe the air of freedom, anxious to repay the country for this blessing that she offers,” said Reform Rabbi Solomon Foster at the dedication ceremony Jan. 30, 1908. For the Eastern European Jews who passed through Ellis Island from 1880 to 1920, the founding of a Jewish hospital became their expression of becoming Americans.
In Newark, more than 87 Jewish societies, workmen’s lodges, and synagogues provided funds for the hospital. The 1908 opening was celebrated with a massive parade through the immigrant neighborhood, where tenements were festooned with American flag bunting.
The Beth practiced a nonsectarian policy in hospital admissions, the extension of hospital privileges to doctors, and the hiring of hospital staff. “While this hospital will be mainly supported by Jews, it will open its doors just as wide as they can swing to receive all who may desire to enter, and his religious sentiments shall be carefully safeguarded,” the policy stated. Kosher meals were available upon request, and Christmas decorations were displayed to cheer patients.
Community-based Care
In 1924, a new, modern image of the hospital appeared on billboards and newspapers: Miss Beth, who launched a campaign for a new hospital with the question: “Is your heart with the hospital?”
The third hospital—a 350-bed yellow-brick tower with a Spanish tile roof—rose nearly 200 feet from its foundation like a sentinel beckoning its community. The new hospital opened in 1928, relocated from the city center to the southern tip of the city north of Lake Weequahic.
The Jewish community followed its hospital to settle in the surrounding streets, transforming it into a vibrant Jewish neighborhood celebrated by Philip Roth in his many novels about Newark.
The Beth was committed to providing training and research opportunities to doctors—Jewish and non-Jewish—who were denied privileges at other hospitals early in the 20th century.
The commitment to providing high-caliber training was evident in its accreditation from the American College of Surgeons in 1919 and the AMA Council approval for the internships in 1921.
By 1930, the laboratory, physical therapy, social work, and dietary departments were offering technical training programs. During World War II, it was designated as one of 1,000 depots that stored penicillin.
During the Great Depression, despite financial difficulties that nearly bankrupted the hospital, the Beth maintained an animal house for research. It was at the Beth that the Rh factor was identified as the cause of erythroblastosis fetalis.
A Laboratory Research Foundation was created to provide funding for research projects and support publication of a hospital journal. The journal published the earliest research results of the Beth Cardiopulmonary Laboratory, which became a leading center for the development of the pacemaker.
In the mid-1960s, as the Newark Jewish community resettled in the outlying New Jersey suburbs, hospital leaders decided to remain on Lyons Avenue and expand into a regional medical center.
Like other industrial cities, Newark suffered through a turbulent decade, requiring the hospital to redefine itself in its mission to serve its neighborhood and waves of immigrants settling into the region.
Federal grant programs and loans from the Prudential Life Insurance Corp. enabled the phased construction of a fourth hospital complex next to the old hospital, providing inpatient and ambulatory care services.
In 1996, Newark Beth Israel Hospital and Medical Center became an affiliate of Barnabas Health Care—New Jersey’s largest integrated healthcare system.
The Beth Today
These days, Newark Beth Israel Hospital and Medical Center is a major teaching affiliate of the Mount Sinai School of Medicine in New York City, the New York College of Osteopathic Medicine in Old Westbury, N.Y, and St. George’s University School of Medicine in Grenada.
The Beth’s division of cardiology continues pioneering work on therapeutic cardiac services and offers the most comprehensive robotic surgical center in the state.
And, honoring a 75-year-old tradition, the center still holds the outreach health screening and health fairs program begun by the Maternity Guild as a citywide public health initiative.
At its inception, the “Born at the Beth” program meant every baby born in the hospital was eligible to join a Babies’ Alumni Club. The $1 annual dues paid on their behalf entitled them to attend an annual babies’ health fair at which they enjoyed Dixie cups of ice cream and free examinations from the hospital staff. Now, the hospital offers the Born at the Beth Wall of Recognition to pay tribute to all those who greeted life within the hospital’s walls.
The Star of David remains at the front entrance, an enduring symbol of the hospital’s heritage. And the hospital’s creed—first displayed in 1928—still asserts the commitment of its staff: “The value of the human touch as a power for healing is never lost sight of at Beth Israel.” TH
The Krauts are coauthors of “Covenant of Care: Newark Beth Israel Hospital and the Jewish Hospital in America.”
Can CT coronary angiography effectively rule out coronary disease in a patient admitted with chest pain?
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
The HM Wishlist
What’s on your wish list for 2008? For many hospitalists, the list is full of cultural changes they’d like to see sweep through their institutions, prying loose old, entrenched habits and replacing them with new, efficient methods and practices. They’re changes that would improve patient safety and care and create better working conditions for physicians.
Those ideas don’t have to remain wishes. We’ve compiled a list of some of the top changes hospitalists say they’d like to see in the coming year, including ideas for how to implement them and some success stories to prove change is possible. Of course, it’s not easy.
“We had to work, and we had to work hard,” says Dr. William Ford, MD, director of the hospitalist program at Temple University in Philadelphia. It took major collaboration and a lot of face-to-face talks to create the cultural shifts he wanted to see at Temple, which partnered with Cogent Healthcare in 2006. But the work paid off, winning support for an observation unit from key stakeholders, such as residency program leaders and nurses.
Dr. Ford’s experience might inspire hospitalists who wish to improve the following critical facets of how hospital medicine is done:
1) Integrate hospitalists into policy-making bodies of institutions. Hospitalists work right in the thick of things, yet don’t often have a voice in their institution’s strategic planning, says Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California, Irvine. Bringing hospitalists onto major committees would benefit everyone, he says.
Hospitalists have a vested interest in their institutions and a deep knowledge of it. They should be involved in operations, business development, and growth, Dr. Amin notes. That can mean growing the surgical business, increasing referrals, or meeting joint commission goals and requirements of the Accreditation Council for Graduate Medical Education (ACGME).
“Many of the bylaws of an institution have been created 10, 20 years ago, when there wasn’t such a thing as hospitalists,” so they don’t automatically get a seat at the table, Dr. Amin says.
But that should change, he argues, because today hospitalists affect every part of an institution. Hospitalists should sit on medical executive committees and contribute to discussions about bylaws, planning, business strategy, and more.
“The hospitalist is integral to helping a hospital improve operations and patient safety,” Dr. Amin says. “Having a permanent seat on the medical executive committee seems like a natural role for the hospitalist director to have.”
2) Reduce paperwork. Mark Thoelke, MD, clinical director of the hospitalist program and associate professor of medicine at Washington University School of Medicine in St. Louis, would love to put down his pen.
“I’ve been doing this job for 15 years now,” he says. “When I started, there was one piece of paper I’d fill out for admissions. [Now] we have to fill out 15 separate pieces of paper when we admit a patient to the hospital.”
Worthwhile and well-meaning patient process improvement groups tend to generate more paperwork for physicians, he points out.
“Nobody seems to want to complain about this because you’re going to be perceived as someone who’s against patient safety,” Dr. Thoelke says. “I feel very strongly about providing excellent patient care. But it makes it harder for me to take care of patients if I’m concerned about filling out multiple pieces of paper.”
To combat the paper flood, his institution has been using Lean Six Sigma, a business improvement strategy that addresses speed and quality. Admission forms are now in a single large packet available in one spot. Dr. Thoelke would like to see even more improvements.
“The end result of any committee is a new piece of paper that the physician has to fill out,” Dr. Thoelke says. “The perception is, it’s just one piece of paper. But it adds up to an incredible amount of time.”
3) Eliminate 24-hour shifts. Chris Landrigan, MD, MPH, studies the relationship between workplace safety and patient care, particularly the long hours residents tend to work.
In general, residents’ shifts are restricted to no more than 24 consecutive hours, plus up to six hours for paperwork and arranging patient care, according to the ACGME. Residents are to have 10-hour rest periods between duty shifts, and can work no more than 80 hours a week, averaged over four weeks.
“There’s no question that traditional shifts of 24 or more hours endanger residents and their patients,” says Dr. Landrigan director of the Sleep and Patient Safety Program, Brigham and Women’s Hospital, and research and fellowship director, Inpatient Pediatrics Service, Children’s Hospital Boston. “Twenty-four hour shifts are associated with an increased rate of serious medical errors, and residents frequently crash their cars on the way home from working these marathon shifts. In the last few years, I know of eight residents at Children’s alone who have had post-call crashes on the way home from work.”
In accordance with ACGME standards limiting residents’ work hours, hospitalists can encourage a cultural shift that would improve workplace safety and patient care, he says. “Hospitalists in some cases are the residency directors, or some of the key teachers, and have a lot of influence there,” he says. “They’re in a position to begin to challenge the traditional model, just as they have in other ways.”
Dr. Landrigan acknowledges this massive change will be slow to catch on, but it’s already started. At Brigham and Women’s Hospital, 24-hour shifts for surgical residents have been eliminated on most rotations, he says, and a few programs in New York, Ohio, and elsewhere have done the same. “The department of surgery at Brigham and Women’s viewed the data themselves, and they felt that this was an important issue,” Dr. Landrigan says. He plans to study the impact of eliminating 24-hour shifts in the surgical intensive care units at Brigham and Women’s.
4) Include leadership training in medical school curriculum. “When you go to medical school, you [learn] to make a diagnosis and interact with a patient essentially on a one-on-one level,” says Eric Howell, MD, assistant professor of medicine, faculty leader, Helen B. Taussig College, Johns Hopkins University School of Medicine in Baltimore, and the chairman of SHM’s leadership committee.
“But in the hospital, that teaching is almost counterproductive,” he explains. There, the physician-patient relationship expands into one with multiple players. The physician leads a team with the patient at its center that can include case managers, nurses, administrative staff, ancillary staff, social workers, and others.
Physicians get no training in school about how to manage multidisciplinary teams, or how to create change where change is needed; instead, they learn on the job, Dr. Howell says. At a summit in Chicago this fall, the Leadership Committee discussed the possibility of providing scholarships for residents to attend SHM’s leadership academies.
“That got a lot of positive reviews, even unofficially,” Dr. Howell says. “The other thing we’re doing is we’re trying to get the word out that many hospitalists have the tools to lead teams, and to manage teams, to non-hospitalist groups,” such as hospital administrators and the American College of Healthcare Executives. “We’re trying to get the word out that there are physicians in hospitals available to lead.”
5) Make “hospitalist” a specialty. Dr. Ford would like to see “hospitalist” recognized as a medical sub-specialty in 2008. As specialists, hospitalists would have specific training requirements and other benefits, he says.
“Right now, we’re a big black box,” Dr. Ford says. “There are no clearly defined guidelines for what we can and can’t do.”
A formal credential for hospitalists is closer to reality. The American Board of Internal Medicine (ABIM) has officially approved the creation of a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system. The ABIM’s formal proposal to the American Board of Medical Specialties (ABMS) is expected to be approved by September 2008. SHM began pursuing certification three years ago and intends to reach out to the pediatric and family medicine boards so certification can be available to all hospitalists.
The move would help make “hospitalist” a more recognizable term in the medical community and in the public arena, says Dr. Ford. “We’re not just your stereotypical general practice doctor. I think we’re more than that. I’d like to promote more of a global perspective of what hospitals are: We make the best use of resources as well as provide the most up-to-date care.”
6) Break down silos and collaborate more. “Medicine in general really is traditionally a siloed field, and at our institution there has been a lot of effort to break down those silos and work collaboratively,” Dr. Howell says.
In 1999 and 2000, the Johns Hopkins Bayview Medical Center, where Dr. Howell works, addressed a major patient throughput issue by bringing together two large groups for negotiation: the emergency department (ED) and the department of medicine. Together they reduced ED waiting time by 90 minutes, Dr. Howell says. The collaborative process received national recognition and resulted in joint publications. They did it again seven years later, this time bringing five large groups to the negotiating table and reducing the wait time even more.
“Each of those groups had to give up something,” such as control over the process, and they had to agree to greater transparency, Dr. Howell concedes. “But in return, they got a lot more.”
Bayview used collaboration again to tackle the issue of ambulance diversion, known as Red Alert, to dramatic effect. In fiscal year 2006, the campus had 2,025 Red Alert hours. The following year, it was 503. Fiscal year 2008 had, as of October, zero Red Alert hours.
“For years, we had been trying to solve the problems individually,” Dr. Howell says. “Imagine if everybody were approaching problems from the teamwork perspective right away. This is a cultural shift that’s going to have to change, and I think it’s going to take a long time. But for hospitalist medicine, these things are already happening.”
7) Improve staffing and retention rates. It almost doesn’t matter how sophisticated hospital culture is overall if the institution still battles one crucial weakness: burnout.
“There is a true burnout factor to hospitalists,” Dr. Amin says. “A lot of institutions are challenged with having the appropriate staffing of hospitalists. Part of that boils down to economics.”
Dr. Amin understands that bumping up staffing is tough to promote when the additions don’t correspond with increased revenue. An appropriate staffing model takes into account a number of variables, including patient load, vacation schedules, and non-clinical duties such as teaching, academics, research, administration, and quality-improvement efforts, he says.
Hiring hospitalists is not like hiring a new primary care doctor or another specialist who might attract new patients to the institution, he says. “A hospitalist program will have the same volume of patients that need to be covered regardless. If a hospitalist goes on vacation, one can’t close the hospital.”
Yet stop-gap measures, such as double shifts when someone’s on vacation, only work for so long, he points out. “You can’t continue to keep doing that as you’re being asked to see more and more patients, do more and more teaching, do more and more oversight, and still do it with the same number of people.”
Hospitalists’ great reputations for providing more efficient care and decreasing length of stay may convince institutions it’s worth it to change their staffing models and add more people. “Hospitals are running at capacity,” he says. “You still need quality.”
8) Improve communication: Pick up the phone. “One of the big things we’ve been working on is physician-to-physician communication,” Dr. Thoelke says. “That’s another problem area at many large academic institutions, and I think at most community institutions as well.”
Every consult should lead to a phone call, not just a note in a chart that another doctor might not see until the next day. It’s not only for courtesy’s sake: Dr. Thoelke believes that better, more direct communication will further decrease length of stay.
“You gather so much more information even in brief conversations from one doctor to another,” Dr. Thoelke says. “I object personally when I have a consultant schedule my patient for a test that they don’t make me aware of. I’m on the phone saying, ‘This is not appropriate.’ I’m the person who’s going to be dealing with the complications of this procedure. So I’m pushing back directly to physicians.”
He’s also working hand in hand with hospital administration to encourage a culture of communication.
A standardized hand-off of every patient, every time, would also help, says Dr. Landrigan.
“As it stands now, there’s a lot of looseness,” Dr. Landrigan says. Physicians sometimes assume that the next clinician can simply take over. “The reality is that when clinicians know the patients less well, care suffers.”
An SHM task force has created basic standards for hospitalists to use for hand-offs (The Hospitalist August 2007, p.18).
9) Meet face to face with all those involved when you want to make change. No matter what’s on your wish list for 2008, your chances of making it happen improve if you communicate directly, according to Dr. Ford.
“I would recommend this not just for hospital medicine, but for anything,” Dr. Ford says. “You really have to go and meet with people. You really have to communicate, and not just by e-mail. E-mail is a good way to set up times to meet.”
To build support for the changes he wanted to make at Temple when Cogent Healthcare began managing its hospitalist program, Ford brought everyone into the discussion, from medical department chairs to representatives from nursing, administration, the labs, and more. “All the key stakeholders,” he says.
Now, Temple’s overall culture focuses on the institution’s financial health as well as on patient health. It also has an observation unit run entirely by hospitalists, freeing residents to work on other cases and still comply with ACGME rules.
“We did get a lot of resistance,” Dr. Ford admits. “University faculty weren’t very receptive to having a non-university faction running this unit. We had to break down the stereotypes that we weren’t a for-profit monster. We had to gain the trust of the emergency department [and others] to allow us to take care of their patients.” TH
Liz Tascio is a journalist based in New York.
What’s on your wish list for 2008? For many hospitalists, the list is full of cultural changes they’d like to see sweep through their institutions, prying loose old, entrenched habits and replacing them with new, efficient methods and practices. They’re changes that would improve patient safety and care and create better working conditions for physicians.
Those ideas don’t have to remain wishes. We’ve compiled a list of some of the top changes hospitalists say they’d like to see in the coming year, including ideas for how to implement them and some success stories to prove change is possible. Of course, it’s not easy.
“We had to work, and we had to work hard,” says Dr. William Ford, MD, director of the hospitalist program at Temple University in Philadelphia. It took major collaboration and a lot of face-to-face talks to create the cultural shifts he wanted to see at Temple, which partnered with Cogent Healthcare in 2006. But the work paid off, winning support for an observation unit from key stakeholders, such as residency program leaders and nurses.
Dr. Ford’s experience might inspire hospitalists who wish to improve the following critical facets of how hospital medicine is done:
1) Integrate hospitalists into policy-making bodies of institutions. Hospitalists work right in the thick of things, yet don’t often have a voice in their institution’s strategic planning, says Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California, Irvine. Bringing hospitalists onto major committees would benefit everyone, he says.
Hospitalists have a vested interest in their institutions and a deep knowledge of it. They should be involved in operations, business development, and growth, Dr. Amin notes. That can mean growing the surgical business, increasing referrals, or meeting joint commission goals and requirements of the Accreditation Council for Graduate Medical Education (ACGME).
“Many of the bylaws of an institution have been created 10, 20 years ago, when there wasn’t such a thing as hospitalists,” so they don’t automatically get a seat at the table, Dr. Amin says.
But that should change, he argues, because today hospitalists affect every part of an institution. Hospitalists should sit on medical executive committees and contribute to discussions about bylaws, planning, business strategy, and more.
“The hospitalist is integral to helping a hospital improve operations and patient safety,” Dr. Amin says. “Having a permanent seat on the medical executive committee seems like a natural role for the hospitalist director to have.”
2) Reduce paperwork. Mark Thoelke, MD, clinical director of the hospitalist program and associate professor of medicine at Washington University School of Medicine in St. Louis, would love to put down his pen.
“I’ve been doing this job for 15 years now,” he says. “When I started, there was one piece of paper I’d fill out for admissions. [Now] we have to fill out 15 separate pieces of paper when we admit a patient to the hospital.”
Worthwhile and well-meaning patient process improvement groups tend to generate more paperwork for physicians, he points out.
“Nobody seems to want to complain about this because you’re going to be perceived as someone who’s against patient safety,” Dr. Thoelke says. “I feel very strongly about providing excellent patient care. But it makes it harder for me to take care of patients if I’m concerned about filling out multiple pieces of paper.”
To combat the paper flood, his institution has been using Lean Six Sigma, a business improvement strategy that addresses speed and quality. Admission forms are now in a single large packet available in one spot. Dr. Thoelke would like to see even more improvements.
“The end result of any committee is a new piece of paper that the physician has to fill out,” Dr. Thoelke says. “The perception is, it’s just one piece of paper. But it adds up to an incredible amount of time.”
3) Eliminate 24-hour shifts. Chris Landrigan, MD, MPH, studies the relationship between workplace safety and patient care, particularly the long hours residents tend to work.
In general, residents’ shifts are restricted to no more than 24 consecutive hours, plus up to six hours for paperwork and arranging patient care, according to the ACGME. Residents are to have 10-hour rest periods between duty shifts, and can work no more than 80 hours a week, averaged over four weeks.
“There’s no question that traditional shifts of 24 or more hours endanger residents and their patients,” says Dr. Landrigan director of the Sleep and Patient Safety Program, Brigham and Women’s Hospital, and research and fellowship director, Inpatient Pediatrics Service, Children’s Hospital Boston. “Twenty-four hour shifts are associated with an increased rate of serious medical errors, and residents frequently crash their cars on the way home from working these marathon shifts. In the last few years, I know of eight residents at Children’s alone who have had post-call crashes on the way home from work.”
In accordance with ACGME standards limiting residents’ work hours, hospitalists can encourage a cultural shift that would improve workplace safety and patient care, he says. “Hospitalists in some cases are the residency directors, or some of the key teachers, and have a lot of influence there,” he says. “They’re in a position to begin to challenge the traditional model, just as they have in other ways.”
Dr. Landrigan acknowledges this massive change will be slow to catch on, but it’s already started. At Brigham and Women’s Hospital, 24-hour shifts for surgical residents have been eliminated on most rotations, he says, and a few programs in New York, Ohio, and elsewhere have done the same. “The department of surgery at Brigham and Women’s viewed the data themselves, and they felt that this was an important issue,” Dr. Landrigan says. He plans to study the impact of eliminating 24-hour shifts in the surgical intensive care units at Brigham and Women’s.
4) Include leadership training in medical school curriculum. “When you go to medical school, you [learn] to make a diagnosis and interact with a patient essentially on a one-on-one level,” says Eric Howell, MD, assistant professor of medicine, faculty leader, Helen B. Taussig College, Johns Hopkins University School of Medicine in Baltimore, and the chairman of SHM’s leadership committee.
“But in the hospital, that teaching is almost counterproductive,” he explains. There, the physician-patient relationship expands into one with multiple players. The physician leads a team with the patient at its center that can include case managers, nurses, administrative staff, ancillary staff, social workers, and others.
Physicians get no training in school about how to manage multidisciplinary teams, or how to create change where change is needed; instead, they learn on the job, Dr. Howell says. At a summit in Chicago this fall, the Leadership Committee discussed the possibility of providing scholarships for residents to attend SHM’s leadership academies.
“That got a lot of positive reviews, even unofficially,” Dr. Howell says. “The other thing we’re doing is we’re trying to get the word out that many hospitalists have the tools to lead teams, and to manage teams, to non-hospitalist groups,” such as hospital administrators and the American College of Healthcare Executives. “We’re trying to get the word out that there are physicians in hospitals available to lead.”
5) Make “hospitalist” a specialty. Dr. Ford would like to see “hospitalist” recognized as a medical sub-specialty in 2008. As specialists, hospitalists would have specific training requirements and other benefits, he says.
“Right now, we’re a big black box,” Dr. Ford says. “There are no clearly defined guidelines for what we can and can’t do.”
A formal credential for hospitalists is closer to reality. The American Board of Internal Medicine (ABIM) has officially approved the creation of a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system. The ABIM’s formal proposal to the American Board of Medical Specialties (ABMS) is expected to be approved by September 2008. SHM began pursuing certification three years ago and intends to reach out to the pediatric and family medicine boards so certification can be available to all hospitalists.
The move would help make “hospitalist” a more recognizable term in the medical community and in the public arena, says Dr. Ford. “We’re not just your stereotypical general practice doctor. I think we’re more than that. I’d like to promote more of a global perspective of what hospitals are: We make the best use of resources as well as provide the most up-to-date care.”
6) Break down silos and collaborate more. “Medicine in general really is traditionally a siloed field, and at our institution there has been a lot of effort to break down those silos and work collaboratively,” Dr. Howell says.
In 1999 and 2000, the Johns Hopkins Bayview Medical Center, where Dr. Howell works, addressed a major patient throughput issue by bringing together two large groups for negotiation: the emergency department (ED) and the department of medicine. Together they reduced ED waiting time by 90 minutes, Dr. Howell says. The collaborative process received national recognition and resulted in joint publications. They did it again seven years later, this time bringing five large groups to the negotiating table and reducing the wait time even more.
“Each of those groups had to give up something,” such as control over the process, and they had to agree to greater transparency, Dr. Howell concedes. “But in return, they got a lot more.”
Bayview used collaboration again to tackle the issue of ambulance diversion, known as Red Alert, to dramatic effect. In fiscal year 2006, the campus had 2,025 Red Alert hours. The following year, it was 503. Fiscal year 2008 had, as of October, zero Red Alert hours.
“For years, we had been trying to solve the problems individually,” Dr. Howell says. “Imagine if everybody were approaching problems from the teamwork perspective right away. This is a cultural shift that’s going to have to change, and I think it’s going to take a long time. But for hospitalist medicine, these things are already happening.”
7) Improve staffing and retention rates. It almost doesn’t matter how sophisticated hospital culture is overall if the institution still battles one crucial weakness: burnout.
“There is a true burnout factor to hospitalists,” Dr. Amin says. “A lot of institutions are challenged with having the appropriate staffing of hospitalists. Part of that boils down to economics.”
Dr. Amin understands that bumping up staffing is tough to promote when the additions don’t correspond with increased revenue. An appropriate staffing model takes into account a number of variables, including patient load, vacation schedules, and non-clinical duties such as teaching, academics, research, administration, and quality-improvement efforts, he says.
Hiring hospitalists is not like hiring a new primary care doctor or another specialist who might attract new patients to the institution, he says. “A hospitalist program will have the same volume of patients that need to be covered regardless. If a hospitalist goes on vacation, one can’t close the hospital.”
Yet stop-gap measures, such as double shifts when someone’s on vacation, only work for so long, he points out. “You can’t continue to keep doing that as you’re being asked to see more and more patients, do more and more teaching, do more and more oversight, and still do it with the same number of people.”
Hospitalists’ great reputations for providing more efficient care and decreasing length of stay may convince institutions it’s worth it to change their staffing models and add more people. “Hospitals are running at capacity,” he says. “You still need quality.”
8) Improve communication: Pick up the phone. “One of the big things we’ve been working on is physician-to-physician communication,” Dr. Thoelke says. “That’s another problem area at many large academic institutions, and I think at most community institutions as well.”
Every consult should lead to a phone call, not just a note in a chart that another doctor might not see until the next day. It’s not only for courtesy’s sake: Dr. Thoelke believes that better, more direct communication will further decrease length of stay.
“You gather so much more information even in brief conversations from one doctor to another,” Dr. Thoelke says. “I object personally when I have a consultant schedule my patient for a test that they don’t make me aware of. I’m on the phone saying, ‘This is not appropriate.’ I’m the person who’s going to be dealing with the complications of this procedure. So I’m pushing back directly to physicians.”
He’s also working hand in hand with hospital administration to encourage a culture of communication.
A standardized hand-off of every patient, every time, would also help, says Dr. Landrigan.
“As it stands now, there’s a lot of looseness,” Dr. Landrigan says. Physicians sometimes assume that the next clinician can simply take over. “The reality is that when clinicians know the patients less well, care suffers.”
An SHM task force has created basic standards for hospitalists to use for hand-offs (The Hospitalist August 2007, p.18).
9) Meet face to face with all those involved when you want to make change. No matter what’s on your wish list for 2008, your chances of making it happen improve if you communicate directly, according to Dr. Ford.
“I would recommend this not just for hospital medicine, but for anything,” Dr. Ford says. “You really have to go and meet with people. You really have to communicate, and not just by e-mail. E-mail is a good way to set up times to meet.”
To build support for the changes he wanted to make at Temple when Cogent Healthcare began managing its hospitalist program, Ford brought everyone into the discussion, from medical department chairs to representatives from nursing, administration, the labs, and more. “All the key stakeholders,” he says.
Now, Temple’s overall culture focuses on the institution’s financial health as well as on patient health. It also has an observation unit run entirely by hospitalists, freeing residents to work on other cases and still comply with ACGME rules.
“We did get a lot of resistance,” Dr. Ford admits. “University faculty weren’t very receptive to having a non-university faction running this unit. We had to break down the stereotypes that we weren’t a for-profit monster. We had to gain the trust of the emergency department [and others] to allow us to take care of their patients.” TH
Liz Tascio is a journalist based in New York.
What’s on your wish list for 2008? For many hospitalists, the list is full of cultural changes they’d like to see sweep through their institutions, prying loose old, entrenched habits and replacing them with new, efficient methods and practices. They’re changes that would improve patient safety and care and create better working conditions for physicians.
Those ideas don’t have to remain wishes. We’ve compiled a list of some of the top changes hospitalists say they’d like to see in the coming year, including ideas for how to implement them and some success stories to prove change is possible. Of course, it’s not easy.
“We had to work, and we had to work hard,” says Dr. William Ford, MD, director of the hospitalist program at Temple University in Philadelphia. It took major collaboration and a lot of face-to-face talks to create the cultural shifts he wanted to see at Temple, which partnered with Cogent Healthcare in 2006. But the work paid off, winning support for an observation unit from key stakeholders, such as residency program leaders and nurses.
Dr. Ford’s experience might inspire hospitalists who wish to improve the following critical facets of how hospital medicine is done:
1) Integrate hospitalists into policy-making bodies of institutions. Hospitalists work right in the thick of things, yet don’t often have a voice in their institution’s strategic planning, says Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California, Irvine. Bringing hospitalists onto major committees would benefit everyone, he says.
Hospitalists have a vested interest in their institutions and a deep knowledge of it. They should be involved in operations, business development, and growth, Dr. Amin notes. That can mean growing the surgical business, increasing referrals, or meeting joint commission goals and requirements of the Accreditation Council for Graduate Medical Education (ACGME).
“Many of the bylaws of an institution have been created 10, 20 years ago, when there wasn’t such a thing as hospitalists,” so they don’t automatically get a seat at the table, Dr. Amin says.
But that should change, he argues, because today hospitalists affect every part of an institution. Hospitalists should sit on medical executive committees and contribute to discussions about bylaws, planning, business strategy, and more.
“The hospitalist is integral to helping a hospital improve operations and patient safety,” Dr. Amin says. “Having a permanent seat on the medical executive committee seems like a natural role for the hospitalist director to have.”
2) Reduce paperwork. Mark Thoelke, MD, clinical director of the hospitalist program and associate professor of medicine at Washington University School of Medicine in St. Louis, would love to put down his pen.
“I’ve been doing this job for 15 years now,” he says. “When I started, there was one piece of paper I’d fill out for admissions. [Now] we have to fill out 15 separate pieces of paper when we admit a patient to the hospital.”
Worthwhile and well-meaning patient process improvement groups tend to generate more paperwork for physicians, he points out.
“Nobody seems to want to complain about this because you’re going to be perceived as someone who’s against patient safety,” Dr. Thoelke says. “I feel very strongly about providing excellent patient care. But it makes it harder for me to take care of patients if I’m concerned about filling out multiple pieces of paper.”
To combat the paper flood, his institution has been using Lean Six Sigma, a business improvement strategy that addresses speed and quality. Admission forms are now in a single large packet available in one spot. Dr. Thoelke would like to see even more improvements.
“The end result of any committee is a new piece of paper that the physician has to fill out,” Dr. Thoelke says. “The perception is, it’s just one piece of paper. But it adds up to an incredible amount of time.”
3) Eliminate 24-hour shifts. Chris Landrigan, MD, MPH, studies the relationship between workplace safety and patient care, particularly the long hours residents tend to work.
In general, residents’ shifts are restricted to no more than 24 consecutive hours, plus up to six hours for paperwork and arranging patient care, according to the ACGME. Residents are to have 10-hour rest periods between duty shifts, and can work no more than 80 hours a week, averaged over four weeks.
“There’s no question that traditional shifts of 24 or more hours endanger residents and their patients,” says Dr. Landrigan director of the Sleep and Patient Safety Program, Brigham and Women’s Hospital, and research and fellowship director, Inpatient Pediatrics Service, Children’s Hospital Boston. “Twenty-four hour shifts are associated with an increased rate of serious medical errors, and residents frequently crash their cars on the way home from working these marathon shifts. In the last few years, I know of eight residents at Children’s alone who have had post-call crashes on the way home from work.”
In accordance with ACGME standards limiting residents’ work hours, hospitalists can encourage a cultural shift that would improve workplace safety and patient care, he says. “Hospitalists in some cases are the residency directors, or some of the key teachers, and have a lot of influence there,” he says. “They’re in a position to begin to challenge the traditional model, just as they have in other ways.”
Dr. Landrigan acknowledges this massive change will be slow to catch on, but it’s already started. At Brigham and Women’s Hospital, 24-hour shifts for surgical residents have been eliminated on most rotations, he says, and a few programs in New York, Ohio, and elsewhere have done the same. “The department of surgery at Brigham and Women’s viewed the data themselves, and they felt that this was an important issue,” Dr. Landrigan says. He plans to study the impact of eliminating 24-hour shifts in the surgical intensive care units at Brigham and Women’s.
4) Include leadership training in medical school curriculum. “When you go to medical school, you [learn] to make a diagnosis and interact with a patient essentially on a one-on-one level,” says Eric Howell, MD, assistant professor of medicine, faculty leader, Helen B. Taussig College, Johns Hopkins University School of Medicine in Baltimore, and the chairman of SHM’s leadership committee.
“But in the hospital, that teaching is almost counterproductive,” he explains. There, the physician-patient relationship expands into one with multiple players. The physician leads a team with the patient at its center that can include case managers, nurses, administrative staff, ancillary staff, social workers, and others.
Physicians get no training in school about how to manage multidisciplinary teams, or how to create change where change is needed; instead, they learn on the job, Dr. Howell says. At a summit in Chicago this fall, the Leadership Committee discussed the possibility of providing scholarships for residents to attend SHM’s leadership academies.
“That got a lot of positive reviews, even unofficially,” Dr. Howell says. “The other thing we’re doing is we’re trying to get the word out that many hospitalists have the tools to lead teams, and to manage teams, to non-hospitalist groups,” such as hospital administrators and the American College of Healthcare Executives. “We’re trying to get the word out that there are physicians in hospitals available to lead.”
5) Make “hospitalist” a specialty. Dr. Ford would like to see “hospitalist” recognized as a medical sub-specialty in 2008. As specialists, hospitalists would have specific training requirements and other benefits, he says.
“Right now, we’re a big black box,” Dr. Ford says. “There are no clearly defined guidelines for what we can and can’t do.”
A formal credential for hospitalists is closer to reality. The American Board of Internal Medicine (ABIM) has officially approved the creation of a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system. The ABIM’s formal proposal to the American Board of Medical Specialties (ABMS) is expected to be approved by September 2008. SHM began pursuing certification three years ago and intends to reach out to the pediatric and family medicine boards so certification can be available to all hospitalists.
The move would help make “hospitalist” a more recognizable term in the medical community and in the public arena, says Dr. Ford. “We’re not just your stereotypical general practice doctor. I think we’re more than that. I’d like to promote more of a global perspective of what hospitals are: We make the best use of resources as well as provide the most up-to-date care.”
6) Break down silos and collaborate more. “Medicine in general really is traditionally a siloed field, and at our institution there has been a lot of effort to break down those silos and work collaboratively,” Dr. Howell says.
In 1999 and 2000, the Johns Hopkins Bayview Medical Center, where Dr. Howell works, addressed a major patient throughput issue by bringing together two large groups for negotiation: the emergency department (ED) and the department of medicine. Together they reduced ED waiting time by 90 minutes, Dr. Howell says. The collaborative process received national recognition and resulted in joint publications. They did it again seven years later, this time bringing five large groups to the negotiating table and reducing the wait time even more.
“Each of those groups had to give up something,” such as control over the process, and they had to agree to greater transparency, Dr. Howell concedes. “But in return, they got a lot more.”
Bayview used collaboration again to tackle the issue of ambulance diversion, known as Red Alert, to dramatic effect. In fiscal year 2006, the campus had 2,025 Red Alert hours. The following year, it was 503. Fiscal year 2008 had, as of October, zero Red Alert hours.
“For years, we had been trying to solve the problems individually,” Dr. Howell says. “Imagine if everybody were approaching problems from the teamwork perspective right away. This is a cultural shift that’s going to have to change, and I think it’s going to take a long time. But for hospitalist medicine, these things are already happening.”
7) Improve staffing and retention rates. It almost doesn’t matter how sophisticated hospital culture is overall if the institution still battles one crucial weakness: burnout.
“There is a true burnout factor to hospitalists,” Dr. Amin says. “A lot of institutions are challenged with having the appropriate staffing of hospitalists. Part of that boils down to economics.”
Dr. Amin understands that bumping up staffing is tough to promote when the additions don’t correspond with increased revenue. An appropriate staffing model takes into account a number of variables, including patient load, vacation schedules, and non-clinical duties such as teaching, academics, research, administration, and quality-improvement efforts, he says.
Hiring hospitalists is not like hiring a new primary care doctor or another specialist who might attract new patients to the institution, he says. “A hospitalist program will have the same volume of patients that need to be covered regardless. If a hospitalist goes on vacation, one can’t close the hospital.”
Yet stop-gap measures, such as double shifts when someone’s on vacation, only work for so long, he points out. “You can’t continue to keep doing that as you’re being asked to see more and more patients, do more and more teaching, do more and more oversight, and still do it with the same number of people.”
Hospitalists’ great reputations for providing more efficient care and decreasing length of stay may convince institutions it’s worth it to change their staffing models and add more people. “Hospitals are running at capacity,” he says. “You still need quality.”
8) Improve communication: Pick up the phone. “One of the big things we’ve been working on is physician-to-physician communication,” Dr. Thoelke says. “That’s another problem area at many large academic institutions, and I think at most community institutions as well.”
Every consult should lead to a phone call, not just a note in a chart that another doctor might not see until the next day. It’s not only for courtesy’s sake: Dr. Thoelke believes that better, more direct communication will further decrease length of stay.
“You gather so much more information even in brief conversations from one doctor to another,” Dr. Thoelke says. “I object personally when I have a consultant schedule my patient for a test that they don’t make me aware of. I’m on the phone saying, ‘This is not appropriate.’ I’m the person who’s going to be dealing with the complications of this procedure. So I’m pushing back directly to physicians.”
He’s also working hand in hand with hospital administration to encourage a culture of communication.
A standardized hand-off of every patient, every time, would also help, says Dr. Landrigan.
“As it stands now, there’s a lot of looseness,” Dr. Landrigan says. Physicians sometimes assume that the next clinician can simply take over. “The reality is that when clinicians know the patients less well, care suffers.”
An SHM task force has created basic standards for hospitalists to use for hand-offs (The Hospitalist August 2007, p.18).
9) Meet face to face with all those involved when you want to make change. No matter what’s on your wish list for 2008, your chances of making it happen improve if you communicate directly, according to Dr. Ford.
“I would recommend this not just for hospital medicine, but for anything,” Dr. Ford says. “You really have to go and meet with people. You really have to communicate, and not just by e-mail. E-mail is a good way to set up times to meet.”
To build support for the changes he wanted to make at Temple when Cogent Healthcare began managing its hospitalist program, Ford brought everyone into the discussion, from medical department chairs to representatives from nursing, administration, the labs, and more. “All the key stakeholders,” he says.
Now, Temple’s overall culture focuses on the institution’s financial health as well as on patient health. It also has an observation unit run entirely by hospitalists, freeing residents to work on other cases and still comply with ACGME rules.
“We did get a lot of resistance,” Dr. Ford admits. “University faculty weren’t very receptive to having a non-university faction running this unit. We had to break down the stereotypes that we weren’t a for-profit monster. We had to gain the trust of the emergency department [and others] to allow us to take care of their patients.” TH
Liz Tascio is a journalist based in New York.
Niche at Night
The middle-age man came to Kaiser Foundation Hospital’s emergency department (ED) in the middle of the night in the late stages of a heart attack.
No catheterization lab operates at night at the Santa Clara, Calif., teaching hospital. The emergency team called a cardiologist for advice and gave the man clot-busting medication.
Still, he did not respond well to treatment.
Jean Laumeyer, MD, of the hospitalist staff, was called in. She had seen many similar cases in her 11 years of working the night shift. Within an hour, Dr. Laumeyer stabilized the man’s condition with “a combination of blood thinners, beta-blockers, pain medications … i.e., general medical management.”
The next day, a woman walked up to Dr. Laumeyer’s husband at a car wash and told him his wife had saved her husband’s life.
“Cases like that are what makes me feel good about working at night,” says Dr. Laumeyer. “I’d seen many cases like it and when you do something a lot, you get good at it. And at night you really have to work well as a team, and we did.”
Dr. Laumeyer is one of the growing number of hospitalists working at night. They are filling critical roles in patient care as hospital medicine becomes more complex and oriented to acute care.
Focus on Quality
Whether they work other shifts or are dedicated nocturnalists like Dr. Laumeyer, a mother of three, night-shift hospitalists are increasingly playing key roles in admissions, medication reconciliation, co-management of surgical patients, and more. They are becoming increasingly important to patient care, to outpatient colleagues’ practices, and the effectiveness of today’s hospitals (see The Hospitalist, May 2006, p. 22).
“These days, a patient typically has to be very sick to be in a hospital,” says Janet Nagamine, MD, who has also been a hospitalist at Kaiser, and, years ago, an intensive care nurse. “Many patients who would have been in intensive care units 20 years ago are in step-down units today.” Now, she is primarily involved in risk management and consulting on quality and safety. She chairs SHM’s Hospital Quality and Patient Safety Committee.
Dr. Nagamine believes typical night-staffing patterns established decades ago may not always be what is needed for optimal patient care, especially lab and ancillary services (see The Hospitalist, April 2007, p 39). “The hospitalists working at night are on the front lines of dealing with this,” she says.
Dahlia Rizk, MD, director of the hospitalist program at Beth Israel Medical Center in New York’s Union Square facility, agrees hospitalists are grappling with some vexing issues in hospital medicine. “We’re involved in every medical issue within quality improvement and patient satisfaction,” says Dr. Rizk. “We are the go-to people for administrators dealing with these issues, on the training of new doctors, and in promoting good communication with other professionals and the community.”
Dr. Rizk is building a 24-hour, seven-day hospitalist program at Beth Israel, where the hospitalist staff has grown from two to 12 full-time physicians in 6 1/2 years. That staff handles nights with an on-call system.
The Challenges
Recent research does not indicate a statistically significant difference in patient outcomes when comparing day and night shifts. But some studies find challenges at night, including in EDs and with discharges.
A 2006 study in Academic Emergency Medicine found that while there are no marked deficits in ED patient care at night, there is a small but measurable increase in early mortality.1
Another 2006 study, published by the Medical Journal of Australia, found that over an 11-year period, more patients were discharged from the ICU in the afternoon and night and that they had an increased risk of death.2 Similar results were reported in a study published in December 2006 by Critical Care Medicine.3
ICUs and EDs are areas where night-shift hospitalists often work, treating patients who typically have symptoms of cardiac or respiratory distress, abdominal pain, and infectious diseases. They are often elderly.
As a result, night-shift hospitalists must work to build excellent relationships with the ED staff and doctors, other hospital staff, and the specialists who will pick up care of the admitted patients, says Robert Newborn, MD, medical director of the adult hospitalist program at Northern Westchester Hospital (NWH), a 175-bed community hospital in Mount Kisco, N.Y.
Dr. Newborn became director of NWH’s hospitalist program in 2004 when it was launched. He had served nearly 10 years as an attending physician in the ED and before that as associate director of the ED at NY Hospital-Cornell Medical Center in New York. NWH’s adult hospitalist program has five full-time physicians reporting to Dr. Newborn. Two pediatric hospitalists work during the day.
The adult-disease hospitalists work the nights in shifts, which Dr. Newborn believes is good for their professional development. “Rotating shifts are beneficial because you learn to work in all environments,” he says.
The NWH hospitalists work 12-hour shifts with face-to-face hand-offs with colleagues at the beginning and end. They review the census of patients (typically about 35) and get a thorough run-down on potential new admissions.
A Critical Shift
To Corina Suciu, MD, a hospitalist at NWH for 16 months, these sessions are obviously critical for patient care, but also for building a tight-knit group of physician colleagues.
Recently she began an 8 p.m. to 8 a.m. shift with a hand-off from the earlier shift. It looked like a pretty typical night.
Dr. Suciu began with the pending admission of a 26-year-old schizophrenic male who was acutely paranoid and needed a full medical exam.
After that, she needed to determine the medication status of a 90-year-old man who had suffered from diarrhea for days and had been falling at home—particularly dangerous because he was taking blood-thinning medication. The patient was taking five or six medications for heart rate, asthma, cholesterol, and more.
The man was not able to accurately report his full medication regimen. Neither was his wife. Dr. Suciu could not reach other family members by phone.
Dr. Suciu knew she needed precise dosages on the patient’s blood thinning (Coumadin) and heart rate (digoxin) medications, at least, in order to proceed with a treatment plan. “Medication reconciliation is an important part of a hospitalist’s job and it is hard, especially at night when there usually isn’t a pharmacist,” she says.
That night, everyone was lucky. The patient had his medications in-hand and the pharmacist was still on-site at 9:30 p.m. He determined the dosage and Dr. Suciu continued with the admission and treatment plan.
As she worked the phone and computer for the 90-year-old, Dr. Suciu got beeped by the emergency staff regarding a less typical case. A 21-year-old woman came to the ED unable to speak. A stroke was suspected. The patient had been in a year earlier, but tests at the time proved inconclusive. The emergency team admitted her for further testing.
Dr. Suciu talked by phone and face to face with nurses familiar with the patient. Then she headed to the ED to examine the young woman and talk to her family.
On the way, she ran into the patient’s neurologist. After discussion, they agreed the patient’s status was inconclusive, so testing was needed as soon as possible.
After gathering more information from the emergency team, Dr. Suciu spent 30 minutes examining the patient and talking to the patient’s family. Next she ordered testing, including a stroke work-up. She planned to monitor the woman through the night.
At 10:45 p.m., the patient was ready to be moved from the ED for a battery of tests to determine if she was suffering a stroke.
By her 8 a.m. hand-off, Dr. Suciu reported that the initial tests on the 21-year-old were fine. Her condition may have been related to a migraine headache. The 90-year-old man was stable.
Communication is Key
Facilitating admissions, moving treatment forward, and reconciling medications are typical duties for a night-shift hospitalist. A critical skill is communicating with the specialists and other outpatient doctors who will care for the patients longer-term.
“I always call the consulting specialists at night because 90% of the time they help a lot,” says Dr. Suciu. “We help them because we give immediate care, which improves the patient’s condition, even saves lives, and gets the patient ready for treatment the next day by the specialist.”
Dr. Laumeyer, who started working nights when it was impossible to juggle the needs of her children—then ages 1, 4, and 6—with her 2,400-patient clinic work, says hospitalists must work hard at night to determine the right time to call a specialist.
“I don’t call a specialist until a patient is stabilized,” she says. “Then I try to have clear questions, a sense of when the patient will be admitted, what I will have done, and what needs to come next. Even if they have to come in before morning, I try to make one call.”
An advantage to working nights often, Dr. Laumeyer says, is that hospitalists can learn what specific physicians like to know, how they want to work, and at what point they want to be involved. “Our chief cardiologist says she starts getting dressed as soon as she knows it’s me on the phone because she knows she’ll have to come in,” she says. “I take pride in that.”
While she feels strongly that hospitalists need to be prepared and clear when they call specialists at night, they should never hesitate to call. “If they’re sleepy or cranky, it doesn’t matter,” Dr. Laumeyer says. “What matters is advancing patient care.”
Her Kaiser colleague, Dr. Nagamine, teaches teamwork and communication skills. “This is critical for hospitalists,” she says. Especially at night, “they must be specific about what they need and its urgency.”
Dr. Nagamine believes structured communication systems, such as those used by the military and in aviation, would benefit medical professionals and patients. One example is the Navy’s situation, background, assessment, and recommendations system. “We’re pretty good at background, but we don’t always clearly state the situation and expectations,” she says. “We assume the person will take the information we’ve given them and come up with the same thinking we have. But just by being present in a situation, you know more.”
Dr. Nagamine believes the onus is on night-shift hospitalists to convey a clear picture of what is needed from a colleague because, obviously, “communication failures take patients down.”
She believes the healthcare industry needs to better understand these issues and notes that the Joint Commission on Accreditation of Hospitals urges a standardized structure for communicating that reduces variability in information. “A shy, inexperienced person will say less,” she says. “These systems help to take the person out of the conversation to be sure communications are effective.”
NWH’s Dr. Newborn believes his staff, and hospitalists in general, are “skilled at appropriately triaging the need for specialists to come in at night.”
In his experience, most specialists are happy to have hospitalists on board because they improve patient care and the specialists’ lives and practices. “They are glad that treatment for their patients doesn’t wait until 7 a.m., that they don’t have to come in at night as often, that they don’t have to do all their admissions and that they get patient referrals,” he says. “As a result, they’re generally happy to take hospitalists’ calls in the middle of the night.”
Lab and ancillary services have increased, too. In the ED, advanced imaging, blood drawing, and electrocardiograms are available all night, says Dr. Newborn. There is a computerized system of patient and medication information that can warn doctors and other staff about potential medication problems.
Nevertheless, night-shift hospitalists are on their own more than their day-time colleagues.
At Beth Israel in Manhattan, the day-shift hospitalists are part of a teaching service. “The hospitalist communicates with the resident who is the in-house physician, or the ICU intensivist, or the fellows who are post-residents training in a specialty,” says Dr. Rizk.
The Beth Israel hospitalists are on a team or are assigned patients based on floors or wards rather than shifts. “The advantage is that one hospitalist cares for a given patient for a longer term, working with all the acquired knowledge,” says Dr. Rizk. “We minimize the number of providers working with a patient and the physician knows the goals for care and the treatment plan well.”
At night, the Beth Israel hospitalists are on-call, but because of the hospital’s growth, Dr. Rizk is working to establish a 24-hour, seven-day hospitalist program that will not be a teaching service. She is recruiting for two night-shift hospitalists who will staff the units.
She knows from her efforts to expand her staff in general that recruitment of night hospitalists will be a challenge. Dr. Rizk agrees with many who think night-shift hospitalists must be given incentives such as higher salaries, more time off, or hybrid schedules (such as one month of night shifts per year).
Yet there are benefits to working at night, she and others agree. “Since it’s shift work, when your beeper is off, you are off,” she says. “You can have more time off, and it can suit personal needs and lifestyles.”
It can be quieter at night with few meetings and little committee work. It can be a good fit for a physician who is between residency and working toward further specialization.
Most importantly, she says, it makes it possible to really focus on patients.
“It’s medicine without the committee,” says Dr. Laumeyer at Kaiser. “At night, there are fewer people to run decisions by, but you can learn and make a big difference.”
She cautions, however, “You have to be comfortable with what you can do on your own and get help with what you can’t.”
Dr. Nagamine agrees. “The most important thing is to recognize the limits of your experience and the scope of your practice. You also must be very aware that what you’re doing at night may be different than it would at 2 p.m. As long as you recognize a discrepancy, you can decide if you need to take another step to ensure the best patient care.” TH
Karla Feuer is a journalist based in New York.
References
- Silbergleit R, Kronick SL, Philpott S, Lowell MJ, Wagner C. Quality of emergency care on the night shift. Acad Emerg Med. 2006 Mar;13(3):325-330.
- Tobin AE, Santamaria JD. After-hours discharges from intensive care are associated with increased mortality. Med J Aust. 2006;184(7):334-337.
- Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med. 2006 Dec;34(12):2946-2951.
The middle-age man came to Kaiser Foundation Hospital’s emergency department (ED) in the middle of the night in the late stages of a heart attack.
No catheterization lab operates at night at the Santa Clara, Calif., teaching hospital. The emergency team called a cardiologist for advice and gave the man clot-busting medication.
Still, he did not respond well to treatment.
Jean Laumeyer, MD, of the hospitalist staff, was called in. She had seen many similar cases in her 11 years of working the night shift. Within an hour, Dr. Laumeyer stabilized the man’s condition with “a combination of blood thinners, beta-blockers, pain medications … i.e., general medical management.”
The next day, a woman walked up to Dr. Laumeyer’s husband at a car wash and told him his wife had saved her husband’s life.
“Cases like that are what makes me feel good about working at night,” says Dr. Laumeyer. “I’d seen many cases like it and when you do something a lot, you get good at it. And at night you really have to work well as a team, and we did.”
Dr. Laumeyer is one of the growing number of hospitalists working at night. They are filling critical roles in patient care as hospital medicine becomes more complex and oriented to acute care.
Focus on Quality
Whether they work other shifts or are dedicated nocturnalists like Dr. Laumeyer, a mother of three, night-shift hospitalists are increasingly playing key roles in admissions, medication reconciliation, co-management of surgical patients, and more. They are becoming increasingly important to patient care, to outpatient colleagues’ practices, and the effectiveness of today’s hospitals (see The Hospitalist, May 2006, p. 22).
“These days, a patient typically has to be very sick to be in a hospital,” says Janet Nagamine, MD, who has also been a hospitalist at Kaiser, and, years ago, an intensive care nurse. “Many patients who would have been in intensive care units 20 years ago are in step-down units today.” Now, she is primarily involved in risk management and consulting on quality and safety. She chairs SHM’s Hospital Quality and Patient Safety Committee.
Dr. Nagamine believes typical night-staffing patterns established decades ago may not always be what is needed for optimal patient care, especially lab and ancillary services (see The Hospitalist, April 2007, p 39). “The hospitalists working at night are on the front lines of dealing with this,” she says.
Dahlia Rizk, MD, director of the hospitalist program at Beth Israel Medical Center in New York’s Union Square facility, agrees hospitalists are grappling with some vexing issues in hospital medicine. “We’re involved in every medical issue within quality improvement and patient satisfaction,” says Dr. Rizk. “We are the go-to people for administrators dealing with these issues, on the training of new doctors, and in promoting good communication with other professionals and the community.”
Dr. Rizk is building a 24-hour, seven-day hospitalist program at Beth Israel, where the hospitalist staff has grown from two to 12 full-time physicians in 6 1/2 years. That staff handles nights with an on-call system.
The Challenges
Recent research does not indicate a statistically significant difference in patient outcomes when comparing day and night shifts. But some studies find challenges at night, including in EDs and with discharges.
A 2006 study in Academic Emergency Medicine found that while there are no marked deficits in ED patient care at night, there is a small but measurable increase in early mortality.1
Another 2006 study, published by the Medical Journal of Australia, found that over an 11-year period, more patients were discharged from the ICU in the afternoon and night and that they had an increased risk of death.2 Similar results were reported in a study published in December 2006 by Critical Care Medicine.3
ICUs and EDs are areas where night-shift hospitalists often work, treating patients who typically have symptoms of cardiac or respiratory distress, abdominal pain, and infectious diseases. They are often elderly.
As a result, night-shift hospitalists must work to build excellent relationships with the ED staff and doctors, other hospital staff, and the specialists who will pick up care of the admitted patients, says Robert Newborn, MD, medical director of the adult hospitalist program at Northern Westchester Hospital (NWH), a 175-bed community hospital in Mount Kisco, N.Y.
Dr. Newborn became director of NWH’s hospitalist program in 2004 when it was launched. He had served nearly 10 years as an attending physician in the ED and before that as associate director of the ED at NY Hospital-Cornell Medical Center in New York. NWH’s adult hospitalist program has five full-time physicians reporting to Dr. Newborn. Two pediatric hospitalists work during the day.
The adult-disease hospitalists work the nights in shifts, which Dr. Newborn believes is good for their professional development. “Rotating shifts are beneficial because you learn to work in all environments,” he says.
The NWH hospitalists work 12-hour shifts with face-to-face hand-offs with colleagues at the beginning and end. They review the census of patients (typically about 35) and get a thorough run-down on potential new admissions.
A Critical Shift
To Corina Suciu, MD, a hospitalist at NWH for 16 months, these sessions are obviously critical for patient care, but also for building a tight-knit group of physician colleagues.
Recently she began an 8 p.m. to 8 a.m. shift with a hand-off from the earlier shift. It looked like a pretty typical night.
Dr. Suciu began with the pending admission of a 26-year-old schizophrenic male who was acutely paranoid and needed a full medical exam.
After that, she needed to determine the medication status of a 90-year-old man who had suffered from diarrhea for days and had been falling at home—particularly dangerous because he was taking blood-thinning medication. The patient was taking five or six medications for heart rate, asthma, cholesterol, and more.
The man was not able to accurately report his full medication regimen. Neither was his wife. Dr. Suciu could not reach other family members by phone.
Dr. Suciu knew she needed precise dosages on the patient’s blood thinning (Coumadin) and heart rate (digoxin) medications, at least, in order to proceed with a treatment plan. “Medication reconciliation is an important part of a hospitalist’s job and it is hard, especially at night when there usually isn’t a pharmacist,” she says.
That night, everyone was lucky. The patient had his medications in-hand and the pharmacist was still on-site at 9:30 p.m. He determined the dosage and Dr. Suciu continued with the admission and treatment plan.
As she worked the phone and computer for the 90-year-old, Dr. Suciu got beeped by the emergency staff regarding a less typical case. A 21-year-old woman came to the ED unable to speak. A stroke was suspected. The patient had been in a year earlier, but tests at the time proved inconclusive. The emergency team admitted her for further testing.
Dr. Suciu talked by phone and face to face with nurses familiar with the patient. Then she headed to the ED to examine the young woman and talk to her family.
On the way, she ran into the patient’s neurologist. After discussion, they agreed the patient’s status was inconclusive, so testing was needed as soon as possible.
After gathering more information from the emergency team, Dr. Suciu spent 30 minutes examining the patient and talking to the patient’s family. Next she ordered testing, including a stroke work-up. She planned to monitor the woman through the night.
At 10:45 p.m., the patient was ready to be moved from the ED for a battery of tests to determine if she was suffering a stroke.
By her 8 a.m. hand-off, Dr. Suciu reported that the initial tests on the 21-year-old were fine. Her condition may have been related to a migraine headache. The 90-year-old man was stable.
Communication is Key
Facilitating admissions, moving treatment forward, and reconciling medications are typical duties for a night-shift hospitalist. A critical skill is communicating with the specialists and other outpatient doctors who will care for the patients longer-term.
“I always call the consulting specialists at night because 90% of the time they help a lot,” says Dr. Suciu. “We help them because we give immediate care, which improves the patient’s condition, even saves lives, and gets the patient ready for treatment the next day by the specialist.”
Dr. Laumeyer, who started working nights when it was impossible to juggle the needs of her children—then ages 1, 4, and 6—with her 2,400-patient clinic work, says hospitalists must work hard at night to determine the right time to call a specialist.
“I don’t call a specialist until a patient is stabilized,” she says. “Then I try to have clear questions, a sense of when the patient will be admitted, what I will have done, and what needs to come next. Even if they have to come in before morning, I try to make one call.”
An advantage to working nights often, Dr. Laumeyer says, is that hospitalists can learn what specific physicians like to know, how they want to work, and at what point they want to be involved. “Our chief cardiologist says she starts getting dressed as soon as she knows it’s me on the phone because she knows she’ll have to come in,” she says. “I take pride in that.”
While she feels strongly that hospitalists need to be prepared and clear when they call specialists at night, they should never hesitate to call. “If they’re sleepy or cranky, it doesn’t matter,” Dr. Laumeyer says. “What matters is advancing patient care.”
Her Kaiser colleague, Dr. Nagamine, teaches teamwork and communication skills. “This is critical for hospitalists,” she says. Especially at night, “they must be specific about what they need and its urgency.”
Dr. Nagamine believes structured communication systems, such as those used by the military and in aviation, would benefit medical professionals and patients. One example is the Navy’s situation, background, assessment, and recommendations system. “We’re pretty good at background, but we don’t always clearly state the situation and expectations,” she says. “We assume the person will take the information we’ve given them and come up with the same thinking we have. But just by being present in a situation, you know more.”
Dr. Nagamine believes the onus is on night-shift hospitalists to convey a clear picture of what is needed from a colleague because, obviously, “communication failures take patients down.”
She believes the healthcare industry needs to better understand these issues and notes that the Joint Commission on Accreditation of Hospitals urges a standardized structure for communicating that reduces variability in information. “A shy, inexperienced person will say less,” she says. “These systems help to take the person out of the conversation to be sure communications are effective.”
NWH’s Dr. Newborn believes his staff, and hospitalists in general, are “skilled at appropriately triaging the need for specialists to come in at night.”
In his experience, most specialists are happy to have hospitalists on board because they improve patient care and the specialists’ lives and practices. “They are glad that treatment for their patients doesn’t wait until 7 a.m., that they don’t have to come in at night as often, that they don’t have to do all their admissions and that they get patient referrals,” he says. “As a result, they’re generally happy to take hospitalists’ calls in the middle of the night.”
Lab and ancillary services have increased, too. In the ED, advanced imaging, blood drawing, and electrocardiograms are available all night, says Dr. Newborn. There is a computerized system of patient and medication information that can warn doctors and other staff about potential medication problems.
Nevertheless, night-shift hospitalists are on their own more than their day-time colleagues.
At Beth Israel in Manhattan, the day-shift hospitalists are part of a teaching service. “The hospitalist communicates with the resident who is the in-house physician, or the ICU intensivist, or the fellows who are post-residents training in a specialty,” says Dr. Rizk.
The Beth Israel hospitalists are on a team or are assigned patients based on floors or wards rather than shifts. “The advantage is that one hospitalist cares for a given patient for a longer term, working with all the acquired knowledge,” says Dr. Rizk. “We minimize the number of providers working with a patient and the physician knows the goals for care and the treatment plan well.”
At night, the Beth Israel hospitalists are on-call, but because of the hospital’s growth, Dr. Rizk is working to establish a 24-hour, seven-day hospitalist program that will not be a teaching service. She is recruiting for two night-shift hospitalists who will staff the units.
She knows from her efforts to expand her staff in general that recruitment of night hospitalists will be a challenge. Dr. Rizk agrees with many who think night-shift hospitalists must be given incentives such as higher salaries, more time off, or hybrid schedules (such as one month of night shifts per year).
Yet there are benefits to working at night, she and others agree. “Since it’s shift work, when your beeper is off, you are off,” she says. “You can have more time off, and it can suit personal needs and lifestyles.”
It can be quieter at night with few meetings and little committee work. It can be a good fit for a physician who is between residency and working toward further specialization.
Most importantly, she says, it makes it possible to really focus on patients.
“It’s medicine without the committee,” says Dr. Laumeyer at Kaiser. “At night, there are fewer people to run decisions by, but you can learn and make a big difference.”
She cautions, however, “You have to be comfortable with what you can do on your own and get help with what you can’t.”
Dr. Nagamine agrees. “The most important thing is to recognize the limits of your experience and the scope of your practice. You also must be very aware that what you’re doing at night may be different than it would at 2 p.m. As long as you recognize a discrepancy, you can decide if you need to take another step to ensure the best patient care.” TH
Karla Feuer is a journalist based in New York.
References
- Silbergleit R, Kronick SL, Philpott S, Lowell MJ, Wagner C. Quality of emergency care on the night shift. Acad Emerg Med. 2006 Mar;13(3):325-330.
- Tobin AE, Santamaria JD. After-hours discharges from intensive care are associated with increased mortality. Med J Aust. 2006;184(7):334-337.
- Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med. 2006 Dec;34(12):2946-2951.
The middle-age man came to Kaiser Foundation Hospital’s emergency department (ED) in the middle of the night in the late stages of a heart attack.
No catheterization lab operates at night at the Santa Clara, Calif., teaching hospital. The emergency team called a cardiologist for advice and gave the man clot-busting medication.
Still, he did not respond well to treatment.
Jean Laumeyer, MD, of the hospitalist staff, was called in. She had seen many similar cases in her 11 years of working the night shift. Within an hour, Dr. Laumeyer stabilized the man’s condition with “a combination of blood thinners, beta-blockers, pain medications … i.e., general medical management.”
The next day, a woman walked up to Dr. Laumeyer’s husband at a car wash and told him his wife had saved her husband’s life.
“Cases like that are what makes me feel good about working at night,” says Dr. Laumeyer. “I’d seen many cases like it and when you do something a lot, you get good at it. And at night you really have to work well as a team, and we did.”
Dr. Laumeyer is one of the growing number of hospitalists working at night. They are filling critical roles in patient care as hospital medicine becomes more complex and oriented to acute care.
Focus on Quality
Whether they work other shifts or are dedicated nocturnalists like Dr. Laumeyer, a mother of three, night-shift hospitalists are increasingly playing key roles in admissions, medication reconciliation, co-management of surgical patients, and more. They are becoming increasingly important to patient care, to outpatient colleagues’ practices, and the effectiveness of today’s hospitals (see The Hospitalist, May 2006, p. 22).
“These days, a patient typically has to be very sick to be in a hospital,” says Janet Nagamine, MD, who has also been a hospitalist at Kaiser, and, years ago, an intensive care nurse. “Many patients who would have been in intensive care units 20 years ago are in step-down units today.” Now, she is primarily involved in risk management and consulting on quality and safety. She chairs SHM’s Hospital Quality and Patient Safety Committee.
Dr. Nagamine believes typical night-staffing patterns established decades ago may not always be what is needed for optimal patient care, especially lab and ancillary services (see The Hospitalist, April 2007, p 39). “The hospitalists working at night are on the front lines of dealing with this,” she says.
Dahlia Rizk, MD, director of the hospitalist program at Beth Israel Medical Center in New York’s Union Square facility, agrees hospitalists are grappling with some vexing issues in hospital medicine. “We’re involved in every medical issue within quality improvement and patient satisfaction,” says Dr. Rizk. “We are the go-to people for administrators dealing with these issues, on the training of new doctors, and in promoting good communication with other professionals and the community.”
Dr. Rizk is building a 24-hour, seven-day hospitalist program at Beth Israel, where the hospitalist staff has grown from two to 12 full-time physicians in 6 1/2 years. That staff handles nights with an on-call system.
The Challenges
Recent research does not indicate a statistically significant difference in patient outcomes when comparing day and night shifts. But some studies find challenges at night, including in EDs and with discharges.
A 2006 study in Academic Emergency Medicine found that while there are no marked deficits in ED patient care at night, there is a small but measurable increase in early mortality.1
Another 2006 study, published by the Medical Journal of Australia, found that over an 11-year period, more patients were discharged from the ICU in the afternoon and night and that they had an increased risk of death.2 Similar results were reported in a study published in December 2006 by Critical Care Medicine.3
ICUs and EDs are areas where night-shift hospitalists often work, treating patients who typically have symptoms of cardiac or respiratory distress, abdominal pain, and infectious diseases. They are often elderly.
As a result, night-shift hospitalists must work to build excellent relationships with the ED staff and doctors, other hospital staff, and the specialists who will pick up care of the admitted patients, says Robert Newborn, MD, medical director of the adult hospitalist program at Northern Westchester Hospital (NWH), a 175-bed community hospital in Mount Kisco, N.Y.
Dr. Newborn became director of NWH’s hospitalist program in 2004 when it was launched. He had served nearly 10 years as an attending physician in the ED and before that as associate director of the ED at NY Hospital-Cornell Medical Center in New York. NWH’s adult hospitalist program has five full-time physicians reporting to Dr. Newborn. Two pediatric hospitalists work during the day.
The adult-disease hospitalists work the nights in shifts, which Dr. Newborn believes is good for their professional development. “Rotating shifts are beneficial because you learn to work in all environments,” he says.
The NWH hospitalists work 12-hour shifts with face-to-face hand-offs with colleagues at the beginning and end. They review the census of patients (typically about 35) and get a thorough run-down on potential new admissions.
A Critical Shift
To Corina Suciu, MD, a hospitalist at NWH for 16 months, these sessions are obviously critical for patient care, but also for building a tight-knit group of physician colleagues.
Recently she began an 8 p.m. to 8 a.m. shift with a hand-off from the earlier shift. It looked like a pretty typical night.
Dr. Suciu began with the pending admission of a 26-year-old schizophrenic male who was acutely paranoid and needed a full medical exam.
After that, she needed to determine the medication status of a 90-year-old man who had suffered from diarrhea for days and had been falling at home—particularly dangerous because he was taking blood-thinning medication. The patient was taking five or six medications for heart rate, asthma, cholesterol, and more.
The man was not able to accurately report his full medication regimen. Neither was his wife. Dr. Suciu could not reach other family members by phone.
Dr. Suciu knew she needed precise dosages on the patient’s blood thinning (Coumadin) and heart rate (digoxin) medications, at least, in order to proceed with a treatment plan. “Medication reconciliation is an important part of a hospitalist’s job and it is hard, especially at night when there usually isn’t a pharmacist,” she says.
That night, everyone was lucky. The patient had his medications in-hand and the pharmacist was still on-site at 9:30 p.m. He determined the dosage and Dr. Suciu continued with the admission and treatment plan.
As she worked the phone and computer for the 90-year-old, Dr. Suciu got beeped by the emergency staff regarding a less typical case. A 21-year-old woman came to the ED unable to speak. A stroke was suspected. The patient had been in a year earlier, but tests at the time proved inconclusive. The emergency team admitted her for further testing.
Dr. Suciu talked by phone and face to face with nurses familiar with the patient. Then she headed to the ED to examine the young woman and talk to her family.
On the way, she ran into the patient’s neurologist. After discussion, they agreed the patient’s status was inconclusive, so testing was needed as soon as possible.
After gathering more information from the emergency team, Dr. Suciu spent 30 minutes examining the patient and talking to the patient’s family. Next she ordered testing, including a stroke work-up. She planned to monitor the woman through the night.
At 10:45 p.m., the patient was ready to be moved from the ED for a battery of tests to determine if she was suffering a stroke.
By her 8 a.m. hand-off, Dr. Suciu reported that the initial tests on the 21-year-old were fine. Her condition may have been related to a migraine headache. The 90-year-old man was stable.
Communication is Key
Facilitating admissions, moving treatment forward, and reconciling medications are typical duties for a night-shift hospitalist. A critical skill is communicating with the specialists and other outpatient doctors who will care for the patients longer-term.
“I always call the consulting specialists at night because 90% of the time they help a lot,” says Dr. Suciu. “We help them because we give immediate care, which improves the patient’s condition, even saves lives, and gets the patient ready for treatment the next day by the specialist.”
Dr. Laumeyer, who started working nights when it was impossible to juggle the needs of her children—then ages 1, 4, and 6—with her 2,400-patient clinic work, says hospitalists must work hard at night to determine the right time to call a specialist.
“I don’t call a specialist until a patient is stabilized,” she says. “Then I try to have clear questions, a sense of when the patient will be admitted, what I will have done, and what needs to come next. Even if they have to come in before morning, I try to make one call.”
An advantage to working nights often, Dr. Laumeyer says, is that hospitalists can learn what specific physicians like to know, how they want to work, and at what point they want to be involved. “Our chief cardiologist says she starts getting dressed as soon as she knows it’s me on the phone because she knows she’ll have to come in,” she says. “I take pride in that.”
While she feels strongly that hospitalists need to be prepared and clear when they call specialists at night, they should never hesitate to call. “If they’re sleepy or cranky, it doesn’t matter,” Dr. Laumeyer says. “What matters is advancing patient care.”
Her Kaiser colleague, Dr. Nagamine, teaches teamwork and communication skills. “This is critical for hospitalists,” she says. Especially at night, “they must be specific about what they need and its urgency.”
Dr. Nagamine believes structured communication systems, such as those used by the military and in aviation, would benefit medical professionals and patients. One example is the Navy’s situation, background, assessment, and recommendations system. “We’re pretty good at background, but we don’t always clearly state the situation and expectations,” she says. “We assume the person will take the information we’ve given them and come up with the same thinking we have. But just by being present in a situation, you know more.”
Dr. Nagamine believes the onus is on night-shift hospitalists to convey a clear picture of what is needed from a colleague because, obviously, “communication failures take patients down.”
She believes the healthcare industry needs to better understand these issues and notes that the Joint Commission on Accreditation of Hospitals urges a standardized structure for communicating that reduces variability in information. “A shy, inexperienced person will say less,” she says. “These systems help to take the person out of the conversation to be sure communications are effective.”
NWH’s Dr. Newborn believes his staff, and hospitalists in general, are “skilled at appropriately triaging the need for specialists to come in at night.”
In his experience, most specialists are happy to have hospitalists on board because they improve patient care and the specialists’ lives and practices. “They are glad that treatment for their patients doesn’t wait until 7 a.m., that they don’t have to come in at night as often, that they don’t have to do all their admissions and that they get patient referrals,” he says. “As a result, they’re generally happy to take hospitalists’ calls in the middle of the night.”
Lab and ancillary services have increased, too. In the ED, advanced imaging, blood drawing, and electrocardiograms are available all night, says Dr. Newborn. There is a computerized system of patient and medication information that can warn doctors and other staff about potential medication problems.
Nevertheless, night-shift hospitalists are on their own more than their day-time colleagues.
At Beth Israel in Manhattan, the day-shift hospitalists are part of a teaching service. “The hospitalist communicates with the resident who is the in-house physician, or the ICU intensivist, or the fellows who are post-residents training in a specialty,” says Dr. Rizk.
The Beth Israel hospitalists are on a team or are assigned patients based on floors or wards rather than shifts. “The advantage is that one hospitalist cares for a given patient for a longer term, working with all the acquired knowledge,” says Dr. Rizk. “We minimize the number of providers working with a patient and the physician knows the goals for care and the treatment plan well.”
At night, the Beth Israel hospitalists are on-call, but because of the hospital’s growth, Dr. Rizk is working to establish a 24-hour, seven-day hospitalist program that will not be a teaching service. She is recruiting for two night-shift hospitalists who will staff the units.
She knows from her efforts to expand her staff in general that recruitment of night hospitalists will be a challenge. Dr. Rizk agrees with many who think night-shift hospitalists must be given incentives such as higher salaries, more time off, or hybrid schedules (such as one month of night shifts per year).
Yet there are benefits to working at night, she and others agree. “Since it’s shift work, when your beeper is off, you are off,” she says. “You can have more time off, and it can suit personal needs and lifestyles.”
It can be quieter at night with few meetings and little committee work. It can be a good fit for a physician who is between residency and working toward further specialization.
Most importantly, she says, it makes it possible to really focus on patients.
“It’s medicine without the committee,” says Dr. Laumeyer at Kaiser. “At night, there are fewer people to run decisions by, but you can learn and make a big difference.”
She cautions, however, “You have to be comfortable with what you can do on your own and get help with what you can’t.”
Dr. Nagamine agrees. “The most important thing is to recognize the limits of your experience and the scope of your practice. You also must be very aware that what you’re doing at night may be different than it would at 2 p.m. As long as you recognize a discrepancy, you can decide if you need to take another step to ensure the best patient care.” TH
Karla Feuer is a journalist based in New York.
References
- Silbergleit R, Kronick SL, Philpott S, Lowell MJ, Wagner C. Quality of emergency care on the night shift. Acad Emerg Med. 2006 Mar;13(3):325-330.
- Tobin AE, Santamaria JD. After-hours discharges from intensive care are associated with increased mortality. Med J Aust. 2006;184(7):334-337.
- Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med. 2006 Dec;34(12):2946-2951.
Your First Job
Within the next few months, many of you will have a new job as an attending hospitalist. As daunting as that may seem, now is the time to think about what you can do to ensure a smooth transition and successful beginning to your career.
Although residency prepared you to face the medical challenges ahead, here are 10 pointers that may help as you move to the next stage of your professional life.
1) Familiarize yourself with the licensing/credentialing process: Do not underestimate the amount of time it takes to get this paperwork approved—up to six months in some cases. Many new hires’ first days on the job are delayed because they didn’t complete this step. Check with state licensing boards for special requirements unique to that state. Also, every hospital has its own gauntlet of infectious disease, HIPAA, and information- technology hoops to jump through. Getting your applications in as early as possible puts you in position to begin on your planned start date and prevent last-minute catastrophes for your new program.
2) Gain valuable insight through observation: Study your current hospitalist group to gain perspective that will help in your new setting. All programs and hospitals operate differently and have room for quality/process improvement. Interview hospitalists, ask questions, and observe the workflow in your current hospital(s) to help in your new job.
3) Contemplate your career direction: Think strategically about your strengths and plans. Although you will learn an incredible amount about hospital medicine careers after you begin, having a sense of direction will help your new group and its leadership get you where you want to be. Making connections and making your goals known within your new program before you start will put your new career on the right path.
4) Seek mentors: Having mentors from your prior program and your new program is a key to a healthy and happy career. Choose people you respect and pick their brains about their careers, how they acquired their skills, and how they would advise you to do the same. Good mentors will help you for many years, and the most valuable may be the ones who have known you throughout your residency. Nurture and maintain these relationships even if you are moving on to new horizons. Inquire whether your new program has a mentorship structure or if your new group leader can recommend someone who shares common interests and goals.
5) Study SHM’s Core Com-petencies: Although you may have trepidation about your medical skills and knowledge as you move into uncharted waters, step back and relax. Know that you are prepared. That said, you can always learn more. One excellent resource is The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (available on SHM’s Web site, www.hospitalmedicine.org). This is a set of standards with which programs can teach hospital medicine and you can learn the scope of expectations and competencies for someone in your position.
6) Understand the nuts and bolts of your new program: Although there are many things you will learn on the job, gain an appreciation for some of the following before your first day:
- Billing: If this is your responsibility, you need to learn a little about this before you start, preferably from one of your future colleagues.
- Reimbursement structure: Find out how your productivity is tracked and rewarded. You’d be amazed how variable this can be.
- Time allotment: How are administrative, research, committee and teaching time balanced against your clinical time?
7) Get to know your new hospital: Before hitting the wards it pays to do a little homework on your new workplace. Do you have access to a medical library, journals, UpToDate, or other online databases? If not, do you need to purchase this access on your own? Many programs have academic funds allotted so you can use those resources. Also, familiarize yourself with the local antibiogram, formularies, guidelines, and order sets. Most facilities have tools specific to their hospital. Know how these affect you in your new role. Prior to starting, you will also want to be sufficiently oriented to any computer systems and understand how they’re used for documentation and order entry, and for viewing lab, radiology, and microbiology results.
8) Shadow a hospitalist: Spending a few hours with someone during a typical hospitalist work day will give you an idea of the pace of the work, the layout of the hospital and floors, the medical and ancillary staff you will work with, and the patient population. This will prompt questions you hadn’t thought of previously.
9) Prepare for each specific role: Hospitalists wear many hats, including teaching attending, non-teaching attending, consultant, researcher, committee member, and hospital medicine leader. Each role carries specific responsibilities and expectations. Prior to each new role, train with someone who leads that service or knows the job intimately.
10) Comprehend your benefits: Does your employer have a retirement program? Do they match retirement contributions? How does the malpractice insurance work? A meeting with human resources will usually help you arrange your health, dental, malpractice, and disability insurance prior to your start date. TH
Dr. Chacko is chair of SHM’s young physician committee and the hospitalist program medical director for Preferred Health Partners in New York City. Dr. Markoff is an assistant professor of medicine and associate director of the hospitalist service at the Mount Sinai Hospital in New York City. Dr. Sliwka is a hospitalist and assistant professor of clinical medicine at the University of California, San Francisco Medical Center.
Within the next few months, many of you will have a new job as an attending hospitalist. As daunting as that may seem, now is the time to think about what you can do to ensure a smooth transition and successful beginning to your career.
Although residency prepared you to face the medical challenges ahead, here are 10 pointers that may help as you move to the next stage of your professional life.
1) Familiarize yourself with the licensing/credentialing process: Do not underestimate the amount of time it takes to get this paperwork approved—up to six months in some cases. Many new hires’ first days on the job are delayed because they didn’t complete this step. Check with state licensing boards for special requirements unique to that state. Also, every hospital has its own gauntlet of infectious disease, HIPAA, and information- technology hoops to jump through. Getting your applications in as early as possible puts you in position to begin on your planned start date and prevent last-minute catastrophes for your new program.
2) Gain valuable insight through observation: Study your current hospitalist group to gain perspective that will help in your new setting. All programs and hospitals operate differently and have room for quality/process improvement. Interview hospitalists, ask questions, and observe the workflow in your current hospital(s) to help in your new job.
3) Contemplate your career direction: Think strategically about your strengths and plans. Although you will learn an incredible amount about hospital medicine careers after you begin, having a sense of direction will help your new group and its leadership get you where you want to be. Making connections and making your goals known within your new program before you start will put your new career on the right path.
4) Seek mentors: Having mentors from your prior program and your new program is a key to a healthy and happy career. Choose people you respect and pick their brains about their careers, how they acquired their skills, and how they would advise you to do the same. Good mentors will help you for many years, and the most valuable may be the ones who have known you throughout your residency. Nurture and maintain these relationships even if you are moving on to new horizons. Inquire whether your new program has a mentorship structure or if your new group leader can recommend someone who shares common interests and goals.
5) Study SHM’s Core Com-petencies: Although you may have trepidation about your medical skills and knowledge as you move into uncharted waters, step back and relax. Know that you are prepared. That said, you can always learn more. One excellent resource is The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (available on SHM’s Web site, www.hospitalmedicine.org). This is a set of standards with which programs can teach hospital medicine and you can learn the scope of expectations and competencies for someone in your position.
6) Understand the nuts and bolts of your new program: Although there are many things you will learn on the job, gain an appreciation for some of the following before your first day:
- Billing: If this is your responsibility, you need to learn a little about this before you start, preferably from one of your future colleagues.
- Reimbursement structure: Find out how your productivity is tracked and rewarded. You’d be amazed how variable this can be.
- Time allotment: How are administrative, research, committee and teaching time balanced against your clinical time?
7) Get to know your new hospital: Before hitting the wards it pays to do a little homework on your new workplace. Do you have access to a medical library, journals, UpToDate, or other online databases? If not, do you need to purchase this access on your own? Many programs have academic funds allotted so you can use those resources. Also, familiarize yourself with the local antibiogram, formularies, guidelines, and order sets. Most facilities have tools specific to their hospital. Know how these affect you in your new role. Prior to starting, you will also want to be sufficiently oriented to any computer systems and understand how they’re used for documentation and order entry, and for viewing lab, radiology, and microbiology results.
8) Shadow a hospitalist: Spending a few hours with someone during a typical hospitalist work day will give you an idea of the pace of the work, the layout of the hospital and floors, the medical and ancillary staff you will work with, and the patient population. This will prompt questions you hadn’t thought of previously.
9) Prepare for each specific role: Hospitalists wear many hats, including teaching attending, non-teaching attending, consultant, researcher, committee member, and hospital medicine leader. Each role carries specific responsibilities and expectations. Prior to each new role, train with someone who leads that service or knows the job intimately.
10) Comprehend your benefits: Does your employer have a retirement program? Do they match retirement contributions? How does the malpractice insurance work? A meeting with human resources will usually help you arrange your health, dental, malpractice, and disability insurance prior to your start date. TH
Dr. Chacko is chair of SHM’s young physician committee and the hospitalist program medical director for Preferred Health Partners in New York City. Dr. Markoff is an assistant professor of medicine and associate director of the hospitalist service at the Mount Sinai Hospital in New York City. Dr. Sliwka is a hospitalist and assistant professor of clinical medicine at the University of California, San Francisco Medical Center.
Within the next few months, many of you will have a new job as an attending hospitalist. As daunting as that may seem, now is the time to think about what you can do to ensure a smooth transition and successful beginning to your career.
Although residency prepared you to face the medical challenges ahead, here are 10 pointers that may help as you move to the next stage of your professional life.
1) Familiarize yourself with the licensing/credentialing process: Do not underestimate the amount of time it takes to get this paperwork approved—up to six months in some cases. Many new hires’ first days on the job are delayed because they didn’t complete this step. Check with state licensing boards for special requirements unique to that state. Also, every hospital has its own gauntlet of infectious disease, HIPAA, and information- technology hoops to jump through. Getting your applications in as early as possible puts you in position to begin on your planned start date and prevent last-minute catastrophes for your new program.
2) Gain valuable insight through observation: Study your current hospitalist group to gain perspective that will help in your new setting. All programs and hospitals operate differently and have room for quality/process improvement. Interview hospitalists, ask questions, and observe the workflow in your current hospital(s) to help in your new job.
3) Contemplate your career direction: Think strategically about your strengths and plans. Although you will learn an incredible amount about hospital medicine careers after you begin, having a sense of direction will help your new group and its leadership get you where you want to be. Making connections and making your goals known within your new program before you start will put your new career on the right path.
4) Seek mentors: Having mentors from your prior program and your new program is a key to a healthy and happy career. Choose people you respect and pick their brains about their careers, how they acquired their skills, and how they would advise you to do the same. Good mentors will help you for many years, and the most valuable may be the ones who have known you throughout your residency. Nurture and maintain these relationships even if you are moving on to new horizons. Inquire whether your new program has a mentorship structure or if your new group leader can recommend someone who shares common interests and goals.
5) Study SHM’s Core Com-petencies: Although you may have trepidation about your medical skills and knowledge as you move into uncharted waters, step back and relax. Know that you are prepared. That said, you can always learn more. One excellent resource is The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (available on SHM’s Web site, www.hospitalmedicine.org). This is a set of standards with which programs can teach hospital medicine and you can learn the scope of expectations and competencies for someone in your position.
6) Understand the nuts and bolts of your new program: Although there are many things you will learn on the job, gain an appreciation for some of the following before your first day:
- Billing: If this is your responsibility, you need to learn a little about this before you start, preferably from one of your future colleagues.
- Reimbursement structure: Find out how your productivity is tracked and rewarded. You’d be amazed how variable this can be.
- Time allotment: How are administrative, research, committee and teaching time balanced against your clinical time?
7) Get to know your new hospital: Before hitting the wards it pays to do a little homework on your new workplace. Do you have access to a medical library, journals, UpToDate, or other online databases? If not, do you need to purchase this access on your own? Many programs have academic funds allotted so you can use those resources. Also, familiarize yourself with the local antibiogram, formularies, guidelines, and order sets. Most facilities have tools specific to their hospital. Know how these affect you in your new role. Prior to starting, you will also want to be sufficiently oriented to any computer systems and understand how they’re used for documentation and order entry, and for viewing lab, radiology, and microbiology results.
8) Shadow a hospitalist: Spending a few hours with someone during a typical hospitalist work day will give you an idea of the pace of the work, the layout of the hospital and floors, the medical and ancillary staff you will work with, and the patient population. This will prompt questions you hadn’t thought of previously.
9) Prepare for each specific role: Hospitalists wear many hats, including teaching attending, non-teaching attending, consultant, researcher, committee member, and hospital medicine leader. Each role carries specific responsibilities and expectations. Prior to each new role, train with someone who leads that service or knows the job intimately.
10) Comprehend your benefits: Does your employer have a retirement program? Do they match retirement contributions? How does the malpractice insurance work? A meeting with human resources will usually help you arrange your health, dental, malpractice, and disability insurance prior to your start date. TH
Dr. Chacko is chair of SHM’s young physician committee and the hospitalist program medical director for Preferred Health Partners in New York City. Dr. Markoff is an assistant professor of medicine and associate director of the hospitalist service at the Mount Sinai Hospital in New York City. Dr. Sliwka is a hospitalist and assistant professor of clinical medicine at the University of California, San Francisco Medical Center.