User login
Daily Care Conundrums
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Medicare, Money, More
The new payment system for hospitalized Medicare patients spells big changes for hospitals and hospitalists.
On Aug. 1, 2006, the Centers for Medicare and Medicaid (CMS) issued final regulations for Medicare payments to hospitals in 2008. This update to the hospital inpatient prospective payment system (IPPS) is designed to improve the accuracy of Medicare payments and includes a new reporting system with new incentives for participating hospitals, restructured inpatient diagnosis-related groups (DRGs), and the exclusion of some hospital-acquired conditions.
The IPPS contains a number of provisions that will affect hospital medicine, and the incentives paid will come from many hospitalist-treated patients. “Realistically, the majority of patients that hospitalists admit are Medicare patients,” says Eric Siegal, MD, regional medical director of Cogent Healthcare in Madison, Wis., and chair of SHM’s Public Policy Committee.
27 Quality Measures
Under the IPPS, hospitals must now report on 27 quality measures to receive their full update. These include 30-day mortality measures for acute myocardial infarction and heart failure for Medicare patients, three measures related to surgical care, and the Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction survey.
The set of measures will be expanded for 2009 to include a 30-day mortality measure for pneumonia and four additional measures related to surgical care, contingent on their endorsement by the National Quality Forum (NQF).
More Precise DRGs
The new IPPS uses restructured DRGs to better account for the severity of each patient’s condition. Now, 745 severity-adjusted DRGs have replaced the previous 538. This means hospitals that serve more severely ill patients will receive increased payments in an effort to prevent rewards for cherry-picking the healthiest patients.
“At least conceptually, this is a better way of doing things,” says Dr. Siegal. “Hospitals have been effectively penalized for taking care of really sick patients, because the DRGs weren’t really differentiating degrees of serious illness. Now that hospital comparison is becoming a big deal, people look at a statistic like mortality rates,” and the figures don’t specify which patients were mortally ill upon admission.
What’s Not Covered?
One interesting aspect to IPPS is that it specifies that Medicare will not cover additional costs of eight preventable, hospital-acquired conditions. These conditions include an object mistakenly left in a patient during surgery, air embolism, blood incompatibility, falls, mediastinitis, catheter-associated urinary tract infections (UTIs), pressure ulcers, and vascular catheter associated infections. For 2009, CMS will also propose excluding ventilator associated pneumonia, staphylococcus aureus septicemia, and deep-vein thrombosis/pulmonary embolism.
“Some of this stuff will be easy. Some cases, like ‘object left in patient during surgery’ are so obvious as to be laughable,” says Dr. Siegal. “Others are a tougher call, such as a catheter-associated UTI. These are not always as clear-cut as [CMS] says they will be. Philosophically, I think this is the right thing to do—it’s not right to pay a hospital for treating something they caused.”
Hospitalists and hospital staff are likely to see added paperwork as a result of this rule. “I can guarantee that there will be an added checklist for these conditions on admission,” says Dr. Siegal. “We’ll have to check for pressure ulcer, UTI, etc.—and that’s not necessarily a bad thing.”
Key Role for Hospitalists
When hospital payment based on reporting is involved, hospitalists are quickly drawn in. “This puts more money for hospitals at risk,” explains Dr. Siegal. “There’s a clear imperative to document better, and to identify who’s really sick. This will all land squarely on the shoulders of hospitalists—and, in fact, it already [has].”
On average, hospitals that comply with all provisions of the rule will earn an additional 3.5% in Medicare payments. This is really a result of the 3.3% market basket increase.
“The difference between doing this well and doing it poorly can add up to the margin for some hospitals,” stresses Dr. Siegal. “There’s absolutely no question that if I’m a hospital and I’m shelling out for a hospital medicine program, the single thing I want them to do and do well is report properly on these measures.”
Careful documentation includes the DRGs. Dr. Siegal points out that there’s a $4,000 swing between the DRG for low-acuity heart failure (a $3,900 payment) and high-acuity heart failure (a $7,900 payment). “Clearly, there will be a shift in reimbursement to those hospitals with sicker patients—or those that do a better job of documenting those patients,” he says. “You can bet that hospitals will make this a priority. They’re going to get much more finicky about how we document.”
Here’s an example: If presented with a patient with sepsis and a UTI, different physicians will have different diagnoses—or rather, use different terms, whether it’s sepsis, severe sepsis, urosepsis, SIRS, or something else. “Hospitals will try to force all physicians to get more crisp in their definitions,” says Dr. Siegal. “This could be good, because we’ll all be using the same language. But some aspects of this will just be a pain … like any other broadly applied rule. If you admit someone with chest pains, you will no longer be able to note ‘chest pains’; you’ll have to describe the pains.”
Starting now, the new IPPS will force hospitalists to perform more—and more careful—documentation for each patient. “It feels like one more hoop to jump through,” says Dr. Siegal. “But there should be no doubt that this is the future of healthcare, like it or not.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
The new payment system for hospitalized Medicare patients spells big changes for hospitals and hospitalists.
On Aug. 1, 2006, the Centers for Medicare and Medicaid (CMS) issued final regulations for Medicare payments to hospitals in 2008. This update to the hospital inpatient prospective payment system (IPPS) is designed to improve the accuracy of Medicare payments and includes a new reporting system with new incentives for participating hospitals, restructured inpatient diagnosis-related groups (DRGs), and the exclusion of some hospital-acquired conditions.
The IPPS contains a number of provisions that will affect hospital medicine, and the incentives paid will come from many hospitalist-treated patients. “Realistically, the majority of patients that hospitalists admit are Medicare patients,” says Eric Siegal, MD, regional medical director of Cogent Healthcare in Madison, Wis., and chair of SHM’s Public Policy Committee.
27 Quality Measures
Under the IPPS, hospitals must now report on 27 quality measures to receive their full update. These include 30-day mortality measures for acute myocardial infarction and heart failure for Medicare patients, three measures related to surgical care, and the Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction survey.
The set of measures will be expanded for 2009 to include a 30-day mortality measure for pneumonia and four additional measures related to surgical care, contingent on their endorsement by the National Quality Forum (NQF).
More Precise DRGs
The new IPPS uses restructured DRGs to better account for the severity of each patient’s condition. Now, 745 severity-adjusted DRGs have replaced the previous 538. This means hospitals that serve more severely ill patients will receive increased payments in an effort to prevent rewards for cherry-picking the healthiest patients.
“At least conceptually, this is a better way of doing things,” says Dr. Siegal. “Hospitals have been effectively penalized for taking care of really sick patients, because the DRGs weren’t really differentiating degrees of serious illness. Now that hospital comparison is becoming a big deal, people look at a statistic like mortality rates,” and the figures don’t specify which patients were mortally ill upon admission.
What’s Not Covered?
One interesting aspect to IPPS is that it specifies that Medicare will not cover additional costs of eight preventable, hospital-acquired conditions. These conditions include an object mistakenly left in a patient during surgery, air embolism, blood incompatibility, falls, mediastinitis, catheter-associated urinary tract infections (UTIs), pressure ulcers, and vascular catheter associated infections. For 2009, CMS will also propose excluding ventilator associated pneumonia, staphylococcus aureus septicemia, and deep-vein thrombosis/pulmonary embolism.
“Some of this stuff will be easy. Some cases, like ‘object left in patient during surgery’ are so obvious as to be laughable,” says Dr. Siegal. “Others are a tougher call, such as a catheter-associated UTI. These are not always as clear-cut as [CMS] says they will be. Philosophically, I think this is the right thing to do—it’s not right to pay a hospital for treating something they caused.”
Hospitalists and hospital staff are likely to see added paperwork as a result of this rule. “I can guarantee that there will be an added checklist for these conditions on admission,” says Dr. Siegal. “We’ll have to check for pressure ulcer, UTI, etc.—and that’s not necessarily a bad thing.”
Key Role for Hospitalists
When hospital payment based on reporting is involved, hospitalists are quickly drawn in. “This puts more money for hospitals at risk,” explains Dr. Siegal. “There’s a clear imperative to document better, and to identify who’s really sick. This will all land squarely on the shoulders of hospitalists—and, in fact, it already [has].”
On average, hospitals that comply with all provisions of the rule will earn an additional 3.5% in Medicare payments. This is really a result of the 3.3% market basket increase.
“The difference between doing this well and doing it poorly can add up to the margin for some hospitals,” stresses Dr. Siegal. “There’s absolutely no question that if I’m a hospital and I’m shelling out for a hospital medicine program, the single thing I want them to do and do well is report properly on these measures.”
Careful documentation includes the DRGs. Dr. Siegal points out that there’s a $4,000 swing between the DRG for low-acuity heart failure (a $3,900 payment) and high-acuity heart failure (a $7,900 payment). “Clearly, there will be a shift in reimbursement to those hospitals with sicker patients—or those that do a better job of documenting those patients,” he says. “You can bet that hospitals will make this a priority. They’re going to get much more finicky about how we document.”
Here’s an example: If presented with a patient with sepsis and a UTI, different physicians will have different diagnoses—or rather, use different terms, whether it’s sepsis, severe sepsis, urosepsis, SIRS, or something else. “Hospitals will try to force all physicians to get more crisp in their definitions,” says Dr. Siegal. “This could be good, because we’ll all be using the same language. But some aspects of this will just be a pain … like any other broadly applied rule. If you admit someone with chest pains, you will no longer be able to note ‘chest pains’; you’ll have to describe the pains.”
Starting now, the new IPPS will force hospitalists to perform more—and more careful—documentation for each patient. “It feels like one more hoop to jump through,” says Dr. Siegal. “But there should be no doubt that this is the future of healthcare, like it or not.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
The new payment system for hospitalized Medicare patients spells big changes for hospitals and hospitalists.
On Aug. 1, 2006, the Centers for Medicare and Medicaid (CMS) issued final regulations for Medicare payments to hospitals in 2008. This update to the hospital inpatient prospective payment system (IPPS) is designed to improve the accuracy of Medicare payments and includes a new reporting system with new incentives for participating hospitals, restructured inpatient diagnosis-related groups (DRGs), and the exclusion of some hospital-acquired conditions.
The IPPS contains a number of provisions that will affect hospital medicine, and the incentives paid will come from many hospitalist-treated patients. “Realistically, the majority of patients that hospitalists admit are Medicare patients,” says Eric Siegal, MD, regional medical director of Cogent Healthcare in Madison, Wis., and chair of SHM’s Public Policy Committee.
27 Quality Measures
Under the IPPS, hospitals must now report on 27 quality measures to receive their full update. These include 30-day mortality measures for acute myocardial infarction and heart failure for Medicare patients, three measures related to surgical care, and the Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction survey.
The set of measures will be expanded for 2009 to include a 30-day mortality measure for pneumonia and four additional measures related to surgical care, contingent on their endorsement by the National Quality Forum (NQF).
More Precise DRGs
The new IPPS uses restructured DRGs to better account for the severity of each patient’s condition. Now, 745 severity-adjusted DRGs have replaced the previous 538. This means hospitals that serve more severely ill patients will receive increased payments in an effort to prevent rewards for cherry-picking the healthiest patients.
“At least conceptually, this is a better way of doing things,” says Dr. Siegal. “Hospitals have been effectively penalized for taking care of really sick patients, because the DRGs weren’t really differentiating degrees of serious illness. Now that hospital comparison is becoming a big deal, people look at a statistic like mortality rates,” and the figures don’t specify which patients were mortally ill upon admission.
What’s Not Covered?
One interesting aspect to IPPS is that it specifies that Medicare will not cover additional costs of eight preventable, hospital-acquired conditions. These conditions include an object mistakenly left in a patient during surgery, air embolism, blood incompatibility, falls, mediastinitis, catheter-associated urinary tract infections (UTIs), pressure ulcers, and vascular catheter associated infections. For 2009, CMS will also propose excluding ventilator associated pneumonia, staphylococcus aureus septicemia, and deep-vein thrombosis/pulmonary embolism.
“Some of this stuff will be easy. Some cases, like ‘object left in patient during surgery’ are so obvious as to be laughable,” says Dr. Siegal. “Others are a tougher call, such as a catheter-associated UTI. These are not always as clear-cut as [CMS] says they will be. Philosophically, I think this is the right thing to do—it’s not right to pay a hospital for treating something they caused.”
Hospitalists and hospital staff are likely to see added paperwork as a result of this rule. “I can guarantee that there will be an added checklist for these conditions on admission,” says Dr. Siegal. “We’ll have to check for pressure ulcer, UTI, etc.—and that’s not necessarily a bad thing.”
Key Role for Hospitalists
When hospital payment based on reporting is involved, hospitalists are quickly drawn in. “This puts more money for hospitals at risk,” explains Dr. Siegal. “There’s a clear imperative to document better, and to identify who’s really sick. This will all land squarely on the shoulders of hospitalists—and, in fact, it already [has].”
On average, hospitals that comply with all provisions of the rule will earn an additional 3.5% in Medicare payments. This is really a result of the 3.3% market basket increase.
“The difference between doing this well and doing it poorly can add up to the margin for some hospitals,” stresses Dr. Siegal. “There’s absolutely no question that if I’m a hospital and I’m shelling out for a hospital medicine program, the single thing I want them to do and do well is report properly on these measures.”
Careful documentation includes the DRGs. Dr. Siegal points out that there’s a $4,000 swing between the DRG for low-acuity heart failure (a $3,900 payment) and high-acuity heart failure (a $7,900 payment). “Clearly, there will be a shift in reimbursement to those hospitals with sicker patients—or those that do a better job of documenting those patients,” he says. “You can bet that hospitals will make this a priority. They’re going to get much more finicky about how we document.”
Here’s an example: If presented with a patient with sepsis and a UTI, different physicians will have different diagnoses—or rather, use different terms, whether it’s sepsis, severe sepsis, urosepsis, SIRS, or something else. “Hospitals will try to force all physicians to get more crisp in their definitions,” says Dr. Siegal. “This could be good, because we’ll all be using the same language. But some aspects of this will just be a pain … like any other broadly applied rule. If you admit someone with chest pains, you will no longer be able to note ‘chest pains’; you’ll have to describe the pains.”
Starting now, the new IPPS will force hospitalists to perform more—and more careful—documentation for each patient. “It feels like one more hoop to jump through,” says Dr. Siegal. “But there should be no doubt that this is the future of healthcare, like it or not.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
Tips from the Top
Whether your goal is to build your management skills, stay on top of industry trends, or simply continue your education, self-study should be part of your career plans.
There are many resources for ambitious physicians. How does one choose? Here, four hospitalists who have advanced their careers share their favorite resources—the Web sites, books, and periodicals that have helped them and that they recommend to other hospitalists.
Fred A. McCurdy, MD, PhD, MBA, associate dean for faculty development, Texas Tech University Health Sciences Center at Amarillo
Dr. McCurdy has an extensive list of resources he regularly recommends to colleagues. The following are a sample from his continually growing list:
- “I’m a member of the American College of Physician Executives and find that membership, along with their journal Physician Executive, pretty valuable,” he says.
- Other journals he recommends include Academic Medicine. (www.academicmedicine.org) and Leader to Leader. (www.leadertoleader.org/knowledgecenter/journal.aspx).
- Any booklet published by the Walk The Talk Company (www.walkthetalk.com).
- The Health Leaders Web site: www.healthleadersmedia.com.
- “Jim Clemmer has some really good, practical books that [can be generalized] to almost any context,” says Dr. McCurdy. “And he has free information via a newsletter and e-mail bulletins at www.clemmer.net.”
Dr. McCurdy also recommends these books:
- Leading Others, Managing Yourself by Peter McGunn;
- Leadership in Healthcare by Carson Dye;
- Leading Physicians through Change by Jack Silversin and Mary Jane Kornacki; and
- John P. Kotter’s works on change and change management (e.g., Leading Change and The Heart of Change).
Eric E. Howell MD, director of Collaborative Inpatient Medicine Service, Department of Medicine, Johns Hopkins Bayview Medical Center, Baltimore
Dr. Howell chairs SHM’s Leadership Committee and says: “I have personal favorites [for reading recommendations]. However, the Leadership Committee is coming up with a list of recommended books.” That list can be found online this month on the SHM Web site (www.hospitalmedicine.org).
Here are Dr. Howell’s top six books for hospitalists:
- Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher, Bruce M. Patton, and William L. Ury. “This is a first, easier book for hospitalists starting out. It doesn’t matter if you’re working on the wards or running a 50-person department. Everyone needs negotiation skills—they’re crucial to being happy and successful.”
- Good to Great: Why Some Companies Make the Leap ... and Others Don’t by Jim Collins. “This book is important to hospitalists because many of us have small groups that are good and need to be great. This book has actually helped our practice a good deal.”
- 21 Irrefutable Laws of Leadership by John C. Maxwell. “Simple and basic, this is a very good book that gives concrete steps for building leadership skills.”
- 7 Habits of Highly Effective People by Stephen Covey. “This isn’t a great book, but it’s got important information for people who want to get ahead in life.”
- Team of Rivals: The Political Genius of Abraham Lincoln by Doris Kearns Goodwin. “My chairman recommended this to each of us. It’s a really good, higher level leadership book for someone in middle or upper management who wants to get to the next level.”
- Moneyball: The Art of Winning an Unfair Game by Michael Lewis. “This talks about baseball. Lewis compares the Oakland A’s to the New York Yankees. Both teams have been to the World Series … but the Yankees spend loads of cash while Oakland does it by being smarter. They’ve found a way to use little-known statistics to choose players. This book is about measuring your organization—something that hospitalists already do more than any other physician group.”
Bob Wachter, MD professor and associate chairman of the Department of Medicine at the University of California, San Francisco Resources Dr. Wachter recommends or checks regularly include:
- Wachter’s World blog: Dr. Wachter suggests reading his new blog, now available at www.wachtersworld.org, to keep up with relevant issues in the industry and opinions you’re not likely to find anywhere else.
- AHRQ Patient Safety Network (which he edits), at http://psnet.ahrq.gov: “This is a weekly round up of key articles, Web sites, and tools in patient safety. It’s also the world’s most extensive, searchable patient safety library. It’s an essential tool for those trying to keep up on safety, quality, and IT.”
- Modern Healthcare’s Daily Dose: An electronic newsletter delivered daily. Subscriptions are available for $49/year at www.modernhealthcare.com. “An excellent news aggregator that keeps you up to date on the key policy issues affecting hospital care.”
- California Healthline: A free daily e-newsletter, available at www.californiahealthline.org. “Particularly for Californians, this newsletter includes news and policy changes, as well as some interesting blogs and links to California Healthcare Foundation reports, which are usually very well done and helpful.”
- ihealthbeat: The California Healthcare Foundation’s free daily healthcare IT e-newsletter is available at www.ihealthbeat.org.
- HITS: Modern Healthcare’s daily healthcare IT enewsletter is available free at www.modernhealthcare.com. These resources obviously focus on information technology news. “I’m not an informationist, but anyone interested in hospital care, quality, and safety needs to keep a finger on the pulse of the IT movement.”
Mary Jo Gorman, MD, MBA, chief executive officer, Advanced ICU Care, St. Louis, Mo., and former SHM president
“My recommendations are all books,” says Dr. Gorman. “I consider them timeless in their application to leadership growth.” Her reading list includes:
- How to Win Friends & Influence People by Dale Carnegie. “Anyone who has to work with others—all of us, I think—can pick up some gems here.”
- Who Moved My Cheese? by Spencer Johnson and Kenneth Blanchard. “A growing field like hospital medicine calls for constantly changing strategy and being open to new things. Whining that things have changed is not a strategy. This book can be an eye-opener in the midst of upheaval.”
- Books by Deborah Tannen. “She is a linguist, and some of her books are more focused on work or family. Two examples are Talking from 9 to 5: Women and Men at Work and That’s Not What I Meant! All of us are conversing with other those of other genders; these books give good insight into what others might mean and how to overcome misunderstandings.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
Whether your goal is to build your management skills, stay on top of industry trends, or simply continue your education, self-study should be part of your career plans.
There are many resources for ambitious physicians. How does one choose? Here, four hospitalists who have advanced their careers share their favorite resources—the Web sites, books, and periodicals that have helped them and that they recommend to other hospitalists.
Fred A. McCurdy, MD, PhD, MBA, associate dean for faculty development, Texas Tech University Health Sciences Center at Amarillo
Dr. McCurdy has an extensive list of resources he regularly recommends to colleagues. The following are a sample from his continually growing list:
- “I’m a member of the American College of Physician Executives and find that membership, along with their journal Physician Executive, pretty valuable,” he says.
- Other journals he recommends include Academic Medicine. (www.academicmedicine.org) and Leader to Leader. (www.leadertoleader.org/knowledgecenter/journal.aspx).
- Any booklet published by the Walk The Talk Company (www.walkthetalk.com).
- The Health Leaders Web site: www.healthleadersmedia.com.
- “Jim Clemmer has some really good, practical books that [can be generalized] to almost any context,” says Dr. McCurdy. “And he has free information via a newsletter and e-mail bulletins at www.clemmer.net.”
Dr. McCurdy also recommends these books:
- Leading Others, Managing Yourself by Peter McGunn;
- Leadership in Healthcare by Carson Dye;
- Leading Physicians through Change by Jack Silversin and Mary Jane Kornacki; and
- John P. Kotter’s works on change and change management (e.g., Leading Change and The Heart of Change).
Eric E. Howell MD, director of Collaborative Inpatient Medicine Service, Department of Medicine, Johns Hopkins Bayview Medical Center, Baltimore
Dr. Howell chairs SHM’s Leadership Committee and says: “I have personal favorites [for reading recommendations]. However, the Leadership Committee is coming up with a list of recommended books.” That list can be found online this month on the SHM Web site (www.hospitalmedicine.org).
Here are Dr. Howell’s top six books for hospitalists:
- Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher, Bruce M. Patton, and William L. Ury. “This is a first, easier book for hospitalists starting out. It doesn’t matter if you’re working on the wards or running a 50-person department. Everyone needs negotiation skills—they’re crucial to being happy and successful.”
- Good to Great: Why Some Companies Make the Leap ... and Others Don’t by Jim Collins. “This book is important to hospitalists because many of us have small groups that are good and need to be great. This book has actually helped our practice a good deal.”
- 21 Irrefutable Laws of Leadership by John C. Maxwell. “Simple and basic, this is a very good book that gives concrete steps for building leadership skills.”
- 7 Habits of Highly Effective People by Stephen Covey. “This isn’t a great book, but it’s got important information for people who want to get ahead in life.”
- Team of Rivals: The Political Genius of Abraham Lincoln by Doris Kearns Goodwin. “My chairman recommended this to each of us. It’s a really good, higher level leadership book for someone in middle or upper management who wants to get to the next level.”
- Moneyball: The Art of Winning an Unfair Game by Michael Lewis. “This talks about baseball. Lewis compares the Oakland A’s to the New York Yankees. Both teams have been to the World Series … but the Yankees spend loads of cash while Oakland does it by being smarter. They’ve found a way to use little-known statistics to choose players. This book is about measuring your organization—something that hospitalists already do more than any other physician group.”
Bob Wachter, MD professor and associate chairman of the Department of Medicine at the University of California, San Francisco Resources Dr. Wachter recommends or checks regularly include:
- Wachter’s World blog: Dr. Wachter suggests reading his new blog, now available at www.wachtersworld.org, to keep up with relevant issues in the industry and opinions you’re not likely to find anywhere else.
- AHRQ Patient Safety Network (which he edits), at http://psnet.ahrq.gov: “This is a weekly round up of key articles, Web sites, and tools in patient safety. It’s also the world’s most extensive, searchable patient safety library. It’s an essential tool for those trying to keep up on safety, quality, and IT.”
- Modern Healthcare’s Daily Dose: An electronic newsletter delivered daily. Subscriptions are available for $49/year at www.modernhealthcare.com. “An excellent news aggregator that keeps you up to date on the key policy issues affecting hospital care.”
- California Healthline: A free daily e-newsletter, available at www.californiahealthline.org. “Particularly for Californians, this newsletter includes news and policy changes, as well as some interesting blogs and links to California Healthcare Foundation reports, which are usually very well done and helpful.”
- ihealthbeat: The California Healthcare Foundation’s free daily healthcare IT e-newsletter is available at www.ihealthbeat.org.
- HITS: Modern Healthcare’s daily healthcare IT enewsletter is available free at www.modernhealthcare.com. These resources obviously focus on information technology news. “I’m not an informationist, but anyone interested in hospital care, quality, and safety needs to keep a finger on the pulse of the IT movement.”
Mary Jo Gorman, MD, MBA, chief executive officer, Advanced ICU Care, St. Louis, Mo., and former SHM president
“My recommendations are all books,” says Dr. Gorman. “I consider them timeless in their application to leadership growth.” Her reading list includes:
- How to Win Friends & Influence People by Dale Carnegie. “Anyone who has to work with others—all of us, I think—can pick up some gems here.”
- Who Moved My Cheese? by Spencer Johnson and Kenneth Blanchard. “A growing field like hospital medicine calls for constantly changing strategy and being open to new things. Whining that things have changed is not a strategy. This book can be an eye-opener in the midst of upheaval.”
- Books by Deborah Tannen. “She is a linguist, and some of her books are more focused on work or family. Two examples are Talking from 9 to 5: Women and Men at Work and That’s Not What I Meant! All of us are conversing with other those of other genders; these books give good insight into what others might mean and how to overcome misunderstandings.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
Whether your goal is to build your management skills, stay on top of industry trends, or simply continue your education, self-study should be part of your career plans.
There are many resources for ambitious physicians. How does one choose? Here, four hospitalists who have advanced their careers share their favorite resources—the Web sites, books, and periodicals that have helped them and that they recommend to other hospitalists.
Fred A. McCurdy, MD, PhD, MBA, associate dean for faculty development, Texas Tech University Health Sciences Center at Amarillo
Dr. McCurdy has an extensive list of resources he regularly recommends to colleagues. The following are a sample from his continually growing list:
- “I’m a member of the American College of Physician Executives and find that membership, along with their journal Physician Executive, pretty valuable,” he says.
- Other journals he recommends include Academic Medicine. (www.academicmedicine.org) and Leader to Leader. (www.leadertoleader.org/knowledgecenter/journal.aspx).
- Any booklet published by the Walk The Talk Company (www.walkthetalk.com).
- The Health Leaders Web site: www.healthleadersmedia.com.
- “Jim Clemmer has some really good, practical books that [can be generalized] to almost any context,” says Dr. McCurdy. “And he has free information via a newsletter and e-mail bulletins at www.clemmer.net.”
Dr. McCurdy also recommends these books:
- Leading Others, Managing Yourself by Peter McGunn;
- Leadership in Healthcare by Carson Dye;
- Leading Physicians through Change by Jack Silversin and Mary Jane Kornacki; and
- John P. Kotter’s works on change and change management (e.g., Leading Change and The Heart of Change).
Eric E. Howell MD, director of Collaborative Inpatient Medicine Service, Department of Medicine, Johns Hopkins Bayview Medical Center, Baltimore
Dr. Howell chairs SHM’s Leadership Committee and says: “I have personal favorites [for reading recommendations]. However, the Leadership Committee is coming up with a list of recommended books.” That list can be found online this month on the SHM Web site (www.hospitalmedicine.org).
Here are Dr. Howell’s top six books for hospitalists:
- Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher, Bruce M. Patton, and William L. Ury. “This is a first, easier book for hospitalists starting out. It doesn’t matter if you’re working on the wards or running a 50-person department. Everyone needs negotiation skills—they’re crucial to being happy and successful.”
- Good to Great: Why Some Companies Make the Leap ... and Others Don’t by Jim Collins. “This book is important to hospitalists because many of us have small groups that are good and need to be great. This book has actually helped our practice a good deal.”
- 21 Irrefutable Laws of Leadership by John C. Maxwell. “Simple and basic, this is a very good book that gives concrete steps for building leadership skills.”
- 7 Habits of Highly Effective People by Stephen Covey. “This isn’t a great book, but it’s got important information for people who want to get ahead in life.”
- Team of Rivals: The Political Genius of Abraham Lincoln by Doris Kearns Goodwin. “My chairman recommended this to each of us. It’s a really good, higher level leadership book for someone in middle or upper management who wants to get to the next level.”
- Moneyball: The Art of Winning an Unfair Game by Michael Lewis. “This talks about baseball. Lewis compares the Oakland A’s to the New York Yankees. Both teams have been to the World Series … but the Yankees spend loads of cash while Oakland does it by being smarter. They’ve found a way to use little-known statistics to choose players. This book is about measuring your organization—something that hospitalists already do more than any other physician group.”
Bob Wachter, MD professor and associate chairman of the Department of Medicine at the University of California, San Francisco Resources Dr. Wachter recommends or checks regularly include:
- Wachter’s World blog: Dr. Wachter suggests reading his new blog, now available at www.wachtersworld.org, to keep up with relevant issues in the industry and opinions you’re not likely to find anywhere else.
- AHRQ Patient Safety Network (which he edits), at http://psnet.ahrq.gov: “This is a weekly round up of key articles, Web sites, and tools in patient safety. It’s also the world’s most extensive, searchable patient safety library. It’s an essential tool for those trying to keep up on safety, quality, and IT.”
- Modern Healthcare’s Daily Dose: An electronic newsletter delivered daily. Subscriptions are available for $49/year at www.modernhealthcare.com. “An excellent news aggregator that keeps you up to date on the key policy issues affecting hospital care.”
- California Healthline: A free daily e-newsletter, available at www.californiahealthline.org. “Particularly for Californians, this newsletter includes news and policy changes, as well as some interesting blogs and links to California Healthcare Foundation reports, which are usually very well done and helpful.”
- ihealthbeat: The California Healthcare Foundation’s free daily healthcare IT e-newsletter is available at www.ihealthbeat.org.
- HITS: Modern Healthcare’s daily healthcare IT enewsletter is available free at www.modernhealthcare.com. These resources obviously focus on information technology news. “I’m not an informationist, but anyone interested in hospital care, quality, and safety needs to keep a finger on the pulse of the IT movement.”
Mary Jo Gorman, MD, MBA, chief executive officer, Advanced ICU Care, St. Louis, Mo., and former SHM president
“My recommendations are all books,” says Dr. Gorman. “I consider them timeless in their application to leadership growth.” Her reading list includes:
- How to Win Friends & Influence People by Dale Carnegie. “Anyone who has to work with others—all of us, I think—can pick up some gems here.”
- Who Moved My Cheese? by Spencer Johnson and Kenneth Blanchard. “A growing field like hospital medicine calls for constantly changing strategy and being open to new things. Whining that things have changed is not a strategy. This book can be an eye-opener in the midst of upheaval.”
- Books by Deborah Tannen. “She is a linguist, and some of her books are more focused on work or family. Two examples are Talking from 9 to 5: Women and Men at Work and That’s Not What I Meant! All of us are conversing with other those of other genders; these books give good insight into what others might mean and how to overcome misunderstandings.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
Patients In the Know
Patient autonomy is one of the core principles of medicine in the U.S. All adult patients of sound mind are entitled to know the risks and benefits of the procedures they undergo—especially when surgery or transfusions are involved.
However, sometimes principles collide with practicalities. Hospitals would grind nearly to a halt if clinicians had to stop and inform patients of the remotest risks associated with even the most benign therapies like potassium supplementation or furosemide.
As a result, the vast majority of medical treatments are administered to hospitalized patients with no discussion of risks, benefits, and alternatives. Besides, most patients wouldn’t want to be informed of every single risk associated with those medications if the likelihood of an adverse event were relatively small. Or would they?
A team of investigators at Yale and Bridgeport Hospital in Bridgeport, Conn., led by medical resident Shweta Upadhyay, MD, examined patients’ preferences when it comes to providing informed consent for routine hospital procedures associated with varying degrees of risk.
These researchers submitted questionnaires to 210 patients admitted to the hospital between June and August 2006. The questionnaires described four hypothetical situations of escalating risk:
- Administration of a diuretic to relieve pulmonary congestion resulting from heart failure;
- Supplementation to replace mineral loss associated with diuretic use; and
- Administration of tissue plasminogen activator (TPA) to treat pulmonary emboli, with a 5% or 20% risk of cerebral hemorrhage and stroke.
In each case, patients were asked if they would want their physicians to begin treatment without asking their permission, ask their permission before beginning treatment no matter what, or obtain permission only if time and clinical circumstances permitted.
—Constantine Manthous, MD, associate clinical professor of medicine, Yale and Bridgeport Hospital, Bridgeport, Conn.
“We designed the questionnaire to step up from minimal risk to life-threatening intervention,” says Constantine Manthous, MD, associate clinical professor of medicine at the hospital and senior author of the study.
Surprisingly, the vast majority of patients—85%—wanted to participate in making even the most trivial decisions about their care. Of those answering the question about potassium supplementation, 92% wanted to be informed before receiving a diuretic.
Less surprisingly, 93% and 95% of patients, respectively, wanted their doctors to obtain their permission before administering TPA when the risk of hemorrhage was 5% and 20%. “We did not expect the patients to be interested at all in the mundane things,” Dr. Manthous says.
In general, patients younger than 65 were more likely to want to discuss the risks, but more of the older patients wanted to be informed if time allowed.
“Older patients (>65 years old) were more likely in some questions than younger (<65 years old) patients to allow their physicians to make unilateral decisions regarding their healthcare. This could be explained by the fact that those age 65 and older grew up at a time when physician paternalism was more prevalent in American medicine,” the authors write.
The findings “demonstrate a big change in what it means to be a patient from 30 to 40 years ago,” Dr. Manthous points out. “These data demonstrate that patients’ expectations are high: They want to be fully involved in even the most mundane aspects of their care. I doubt that most physicians realize just how involved their patients want to be.”
Often, the decision to disclose a treatment’s risks boils down to a judgment call, especially when the frequency and severity of those risks are low, John Banja, MD, and Jason Schneider, MD, both of Emory University in Atlanta, wrote in an editorial accompanying the study (“Ethical Challenges in Disclosing Risk”).
The ethical obligation to discuss risks increases when risk severity increases, even if the frequency of those risks remains low. However, hospitals have inconsistent policies for obtaining informed consent.
“Many hospitals, for example, would have staff simply tell patients that they needed diuretics or thrombolytics, even though in certain instances—and especially with thrombolytic agents—the risk of a significant adverse event could well exceed some reasonable disclosure threshold (which is often set at 1%),” Drs. Banja and Schneider write. If a patient is about to undergo a procedure like thrombolysis, in which the risk of cerebral hemorrhage may be as high as 20%, formal informed consent would “most certainly” be required. Failure to get it could be construed as a serious ethical breach.
Like Dr. Manthous, Dr. Schneider, assistant professor of general medicine at Emory University School of Medicine, was startled by the number of patients who took such an interest in even relatively innocuous treatments. “What was most eye-opening for me was the number of people who had so much interest in the intricacies of their medical care,” he says.
Good communication can help doctors strike a balance between fulfilling patients’ wishes for information and working efficiently, Dr. Schneider adds. “Quality can compensate for quantity; with well-tuned communication, you can make up for limited time,” he explains. Unfortunately, although communication has recently been added to the list of core competencies residents should master, “physicians don’t have the interpersonal communication skills they should have. It’s definitely an area where improvement is needed.”
Indeed, doctors could use their newfound expertise in communication to describe to patients the practical implications of listing every risk of every procedure. Right now, “patients probably don’t understand how bothersome and logistically problematic it would be” to make that disclosure, says Dr. Manthous. “I suspect their answers would be different if we explained that care would slow to a crawl.”
Norra MacReady is a medical writer based in California. TH
Norra MacReady is a medical writer based in California.
Patient autonomy is one of the core principles of medicine in the U.S. All adult patients of sound mind are entitled to know the risks and benefits of the procedures they undergo—especially when surgery or transfusions are involved.
However, sometimes principles collide with practicalities. Hospitals would grind nearly to a halt if clinicians had to stop and inform patients of the remotest risks associated with even the most benign therapies like potassium supplementation or furosemide.
As a result, the vast majority of medical treatments are administered to hospitalized patients with no discussion of risks, benefits, and alternatives. Besides, most patients wouldn’t want to be informed of every single risk associated with those medications if the likelihood of an adverse event were relatively small. Or would they?
A team of investigators at Yale and Bridgeport Hospital in Bridgeport, Conn., led by medical resident Shweta Upadhyay, MD, examined patients’ preferences when it comes to providing informed consent for routine hospital procedures associated with varying degrees of risk.
These researchers submitted questionnaires to 210 patients admitted to the hospital between June and August 2006. The questionnaires described four hypothetical situations of escalating risk:
- Administration of a diuretic to relieve pulmonary congestion resulting from heart failure;
- Supplementation to replace mineral loss associated with diuretic use; and
- Administration of tissue plasminogen activator (TPA) to treat pulmonary emboli, with a 5% or 20% risk of cerebral hemorrhage and stroke.
In each case, patients were asked if they would want their physicians to begin treatment without asking their permission, ask their permission before beginning treatment no matter what, or obtain permission only if time and clinical circumstances permitted.
—Constantine Manthous, MD, associate clinical professor of medicine, Yale and Bridgeport Hospital, Bridgeport, Conn.
“We designed the questionnaire to step up from minimal risk to life-threatening intervention,” says Constantine Manthous, MD, associate clinical professor of medicine at the hospital and senior author of the study.
Surprisingly, the vast majority of patients—85%—wanted to participate in making even the most trivial decisions about their care. Of those answering the question about potassium supplementation, 92% wanted to be informed before receiving a diuretic.
Less surprisingly, 93% and 95% of patients, respectively, wanted their doctors to obtain their permission before administering TPA when the risk of hemorrhage was 5% and 20%. “We did not expect the patients to be interested at all in the mundane things,” Dr. Manthous says.
In general, patients younger than 65 were more likely to want to discuss the risks, but more of the older patients wanted to be informed if time allowed.
“Older patients (>65 years old) were more likely in some questions than younger (<65 years old) patients to allow their physicians to make unilateral decisions regarding their healthcare. This could be explained by the fact that those age 65 and older grew up at a time when physician paternalism was more prevalent in American medicine,” the authors write.
The findings “demonstrate a big change in what it means to be a patient from 30 to 40 years ago,” Dr. Manthous points out. “These data demonstrate that patients’ expectations are high: They want to be fully involved in even the most mundane aspects of their care. I doubt that most physicians realize just how involved their patients want to be.”
Often, the decision to disclose a treatment’s risks boils down to a judgment call, especially when the frequency and severity of those risks are low, John Banja, MD, and Jason Schneider, MD, both of Emory University in Atlanta, wrote in an editorial accompanying the study (“Ethical Challenges in Disclosing Risk”).
The ethical obligation to discuss risks increases when risk severity increases, even if the frequency of those risks remains low. However, hospitals have inconsistent policies for obtaining informed consent.
“Many hospitals, for example, would have staff simply tell patients that they needed diuretics or thrombolytics, even though in certain instances—and especially with thrombolytic agents—the risk of a significant adverse event could well exceed some reasonable disclosure threshold (which is often set at 1%),” Drs. Banja and Schneider write. If a patient is about to undergo a procedure like thrombolysis, in which the risk of cerebral hemorrhage may be as high as 20%, formal informed consent would “most certainly” be required. Failure to get it could be construed as a serious ethical breach.
Like Dr. Manthous, Dr. Schneider, assistant professor of general medicine at Emory University School of Medicine, was startled by the number of patients who took such an interest in even relatively innocuous treatments. “What was most eye-opening for me was the number of people who had so much interest in the intricacies of their medical care,” he says.
Good communication can help doctors strike a balance between fulfilling patients’ wishes for information and working efficiently, Dr. Schneider adds. “Quality can compensate for quantity; with well-tuned communication, you can make up for limited time,” he explains. Unfortunately, although communication has recently been added to the list of core competencies residents should master, “physicians don’t have the interpersonal communication skills they should have. It’s definitely an area where improvement is needed.”
Indeed, doctors could use their newfound expertise in communication to describe to patients the practical implications of listing every risk of every procedure. Right now, “patients probably don’t understand how bothersome and logistically problematic it would be” to make that disclosure, says Dr. Manthous. “I suspect their answers would be different if we explained that care would slow to a crawl.”
Norra MacReady is a medical writer based in California. TH
Norra MacReady is a medical writer based in California.
Patient autonomy is one of the core principles of medicine in the U.S. All adult patients of sound mind are entitled to know the risks and benefits of the procedures they undergo—especially when surgery or transfusions are involved.
However, sometimes principles collide with practicalities. Hospitals would grind nearly to a halt if clinicians had to stop and inform patients of the remotest risks associated with even the most benign therapies like potassium supplementation or furosemide.
As a result, the vast majority of medical treatments are administered to hospitalized patients with no discussion of risks, benefits, and alternatives. Besides, most patients wouldn’t want to be informed of every single risk associated with those medications if the likelihood of an adverse event were relatively small. Or would they?
A team of investigators at Yale and Bridgeport Hospital in Bridgeport, Conn., led by medical resident Shweta Upadhyay, MD, examined patients’ preferences when it comes to providing informed consent for routine hospital procedures associated with varying degrees of risk.
These researchers submitted questionnaires to 210 patients admitted to the hospital between June and August 2006. The questionnaires described four hypothetical situations of escalating risk:
- Administration of a diuretic to relieve pulmonary congestion resulting from heart failure;
- Supplementation to replace mineral loss associated with diuretic use; and
- Administration of tissue plasminogen activator (TPA) to treat pulmonary emboli, with a 5% or 20% risk of cerebral hemorrhage and stroke.
In each case, patients were asked if they would want their physicians to begin treatment without asking their permission, ask their permission before beginning treatment no matter what, or obtain permission only if time and clinical circumstances permitted.
—Constantine Manthous, MD, associate clinical professor of medicine, Yale and Bridgeport Hospital, Bridgeport, Conn.
“We designed the questionnaire to step up from minimal risk to life-threatening intervention,” says Constantine Manthous, MD, associate clinical professor of medicine at the hospital and senior author of the study.
Surprisingly, the vast majority of patients—85%—wanted to participate in making even the most trivial decisions about their care. Of those answering the question about potassium supplementation, 92% wanted to be informed before receiving a diuretic.
Less surprisingly, 93% and 95% of patients, respectively, wanted their doctors to obtain their permission before administering TPA when the risk of hemorrhage was 5% and 20%. “We did not expect the patients to be interested at all in the mundane things,” Dr. Manthous says.
In general, patients younger than 65 were more likely to want to discuss the risks, but more of the older patients wanted to be informed if time allowed.
“Older patients (>65 years old) were more likely in some questions than younger (<65 years old) patients to allow their physicians to make unilateral decisions regarding their healthcare. This could be explained by the fact that those age 65 and older grew up at a time when physician paternalism was more prevalent in American medicine,” the authors write.
The findings “demonstrate a big change in what it means to be a patient from 30 to 40 years ago,” Dr. Manthous points out. “These data demonstrate that patients’ expectations are high: They want to be fully involved in even the most mundane aspects of their care. I doubt that most physicians realize just how involved their patients want to be.”
Often, the decision to disclose a treatment’s risks boils down to a judgment call, especially when the frequency and severity of those risks are low, John Banja, MD, and Jason Schneider, MD, both of Emory University in Atlanta, wrote in an editorial accompanying the study (“Ethical Challenges in Disclosing Risk”).
The ethical obligation to discuss risks increases when risk severity increases, even if the frequency of those risks remains low. However, hospitals have inconsistent policies for obtaining informed consent.
“Many hospitals, for example, would have staff simply tell patients that they needed diuretics or thrombolytics, even though in certain instances—and especially with thrombolytic agents—the risk of a significant adverse event could well exceed some reasonable disclosure threshold (which is often set at 1%),” Drs. Banja and Schneider write. If a patient is about to undergo a procedure like thrombolysis, in which the risk of cerebral hemorrhage may be as high as 20%, formal informed consent would “most certainly” be required. Failure to get it could be construed as a serious ethical breach.
Like Dr. Manthous, Dr. Schneider, assistant professor of general medicine at Emory University School of Medicine, was startled by the number of patients who took such an interest in even relatively innocuous treatments. “What was most eye-opening for me was the number of people who had so much interest in the intricacies of their medical care,” he says.
Good communication can help doctors strike a balance between fulfilling patients’ wishes for information and working efficiently, Dr. Schneider adds. “Quality can compensate for quantity; with well-tuned communication, you can make up for limited time,” he explains. Unfortunately, although communication has recently been added to the list of core competencies residents should master, “physicians don’t have the interpersonal communication skills they should have. It’s definitely an area where improvement is needed.”
Indeed, doctors could use their newfound expertise in communication to describe to patients the practical implications of listing every risk of every procedure. Right now, “patients probably don’t understand how bothersome and logistically problematic it would be” to make that disclosure, says Dr. Manthous. “I suspect their answers would be different if we explained that care would slow to a crawl.”
Norra MacReady is a medical writer based in California. TH
Norra MacReady is a medical writer based in California.
Renal Function Caveats
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
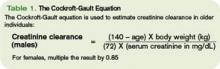
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
Nutrition Mission
Despite a general understanding among hospitalists that malnutrition has severe negative effects on hospitalized patients, preventive or corrective measures often aren’t taken.
The ill effects of nutritional deficiency are particularly profound in elderly inpatients. Estimates of protein-energy malnutrition vary between 20%-78% of elderly medical patients, who are uniquely disposed to the cognitive, metabolic, and immune-mediating consequences of malnutrition.1
Most hospitalists know when to request a nutritionist consultation or order extra mealtime cans of Ensure. But many do not realize these efforts often do little to alter patients’ descent into nutritional deficiency.
Define the Problem
Four patterns of problematic eating have been described in elderly inpatients.
The first and most common is the patient who is permitted nothing by mouth and is not provided an alternate route of nutrition. Data show 44% of elderly malnourished inpatients fall into this category.2
Other abnormal feeding subgroups include patients who need to be fed but have no other eating problem, patients who refuse food but can swallow with difficulty, and those who aspirate liquid or solid food. In a study of 73 institutionalized patients with Alzheimer’s dementia, the latter subgroup accounted for 34% of the patients assessed.
Poor diet is the main source of protein-energy deficiency in elderly inpatients. Occult malabsorption secondary to bacterial overgrowth in the small intestine may also be an important factor, as is the increased catabolic state associated with acute illness.
Though the most at-risk patients have severe mental and physical incapacities, other problems including respiratory disease, gastrointestinal disease, and stroke are associated with a malnourished state.3
Though hospitalists generally acknowledge the potential seriousness of a patient developing nutritional deficits, the attending healthcare team may be slow to diagnose or manage this problem because:
- Elderly patients can be malnourished on admission, but classic signs of protein-energy deficiency are mistaken for normal signs of aging;
- Nutritional problems are observed by the medical staff, but aggressive treatment is deferred in light of seemingly more pressing medical issues;
- Many physicians take action to prevent nutritional deficiencies, but these interventions are often insufficient or ineffective in preventing the spiral into malnutrition; and
- Physicians may assume a nutritionist is working to prevent and treat nutritional deficiencies, while the nutritionist is waiting for the medical staff to address the problem with a feeding tube.
Clinical Outcomes
Most physicians have observed the declining physical and cognitive capabilities of a nutritionally deprived elderly inpatient.
Although a causal relationship between malnutrition and adverse events has not been established, this is most likely because an older person’s clinical course affects and is affected by his nutritional status. Further, frequently compromised homeostatic mechanisms make the risk of complications related to malnutrition potentially more severe.
Though researchers are studying how inadequate nutritional intake contributes to the risk of adverse outcomes in elderly inpatients, numerous studies have identified strong correlations between the severity of the nutritional deficit and the risk of subsequent morbid events.
Sullivan, et al., found in their 1999 study of protein-energy undernutrition among elderly hospitalized patients that those maintained on nutrient intakes far less than their estimated energy requirements were at more risk of in-hospital mortality.
Other studies have shown that the risk of in-hospital starvation correlates strongly with polypharmacy and long stay. The severity of the nutritional deficiency correlates not only with weight loss and secretory protein loss, but also the risk of in-hospital and long-term complications.
Who Needs Help
Basic nutritional requirements vary much less than might be expected among younger and older patients. However, while a malnourished 20-year-old can be easily identified, the classic signs of malnutrition (wasting, brittle hair, dry skin, fissured mucus membranes) are less easily detected in elderly patients. They are often mistaken for signs of normal aging. Questions that can elicit evidence of a protein-energy deficiency include:
- Has food intake decreased recently?
- Are there physical difficulties with eating?
- Is the patient confused or depressed?
- Has there been diarrhea or vomiting?
- Has the patient been able to shop and manage food preparation?
- Has the patient or family noticed weight loss?
- What does the patient regard as a normal weight?
However, because the clinical signs of malnutrition-weight loss, muscle wasting, and fatigue can be difficult to detect from history alone, use of an assessment tool is often necessary.
There is no simple diagnostic test for undernutrition. Measurements of albumin, prealbumin, body-mass index (BMI), and weight loss have been used, albeit problematically, for this purpose. More useful for the quantification of nutritional status in elderly outpatients, these measurements are difficult to use in the hospital because albumin levels are frequently affected by disease processes involving the liver, kidney, and immune system, and correct baseline weights and heights are notoriously difficult to obtain from elderly patients.4
The Nutritional Risk Index was developed in response to these difficulties, but it was originally calibrated for young, post-surgical patients. Because of the problematic nature of obtaining the accurate heights and weights needed for the NRI in elderly patients, Bouillanne, et al,. developed the Geriatric Nutritional Risk Index (GNRI) in 2005 based on albumin levels, hospital recorded weights, and weight loss (see Table 1, above).
The GNRI’s creators classified patients according to their level of malnutrition and calculated their risk of related comorbidities. They found that 44% of their study population had major or moderate nutrition-related risk and recommended nutritional supplementation.
Path to Recovery
Refeeding regimens for elderly patients diagnosed as undernourished are best started with meals of personally chosen foods, timed for when patients are hungry.
Many elderly patients do not eat on a strict schedule at home and have difficulty complying with such a schedule. If oral intake remains inadequate, offer nutritional supplements. Because low-energy diets are usually low in vitamins and minerals, supplementation with a multivitamin, thiamine, folic acid, and zinc can be beneficial.
A common approach to problems with nutritional intake in elderly patients, particularly those with altered cognition or fluctuating consciousness, is insertion of a feeding tube.5 According to Medicare data from the 1990s, in individuals older than 85, one in 131 whites, and one in 58 African-Americans had a gastrostomy.
Despite the large numbers of feeding-tube placements in elderly patients, proof of their effectiveness is scant. No randomized trials have been performed to determine whether this practice improves survival, and observational data reveal that the one-year survival for these patients is less than 40%.
Feeding tubes are often placed to reverse the clinical sequelae of malnutrition—to heal pressure ulcers, prevent infection, and improve the patient’s functional status. But prospective observational studies do not support this methodology, and some contradictory evidence in the form of worsening pressure ulcers has been observed.
Aspiration pneumonia is the most serious infection for which tube feeding is considered a preventive measure. The condition results from the misdirection of pharyngeal contents and is believed to develop when nonpathologic oral secretions are deposited in dependent areas of the lung. The bacterial inoculum is high enough to overcome local defenses, which results in an infectious, febrile illness, usually involving mixed gram-negative rods and anaerobes.
Summaries of current data show that tube feeding may increase the risk of aspiration pneumonia. Further support for this hypothesis comes from the observation that jejunostomy feeding also does not appear to reduce the risk of aspiration pneumonia. If a patient is unable to protect his airway during mealtimes, he will also be at risk of aspiration and pneumonia between meals, regardless of how nutrition is delivered. TH
Dr. Landis is a rheumatologist and freelance writer.
References
- Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients. JAMA. 1999;281(21):2013-2019.
- Incalzi RA, Gemma A, Capparella O, et al. Energy intake and in-hospital starvation: a clinically relevant relationship. Arch Intern Med. 1996;156(4):425-429.
- Tierney A. Undernutrition and elderly patients. J Adv Nurs. 1995;23(2):228-236.
- Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: a new index for evaluating at risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777-783.
- Finucane T, Williams M. Tube feeding the demented patient: a review of the evidence. American Geriatrics Society Annual Scientific Meeting 2001.
Despite a general understanding among hospitalists that malnutrition has severe negative effects on hospitalized patients, preventive or corrective measures often aren’t taken.
The ill effects of nutritional deficiency are particularly profound in elderly inpatients. Estimates of protein-energy malnutrition vary between 20%-78% of elderly medical patients, who are uniquely disposed to the cognitive, metabolic, and immune-mediating consequences of malnutrition.1
Most hospitalists know when to request a nutritionist consultation or order extra mealtime cans of Ensure. But many do not realize these efforts often do little to alter patients’ descent into nutritional deficiency.
Define the Problem
Four patterns of problematic eating have been described in elderly inpatients.
The first and most common is the patient who is permitted nothing by mouth and is not provided an alternate route of nutrition. Data show 44% of elderly malnourished inpatients fall into this category.2
Other abnormal feeding subgroups include patients who need to be fed but have no other eating problem, patients who refuse food but can swallow with difficulty, and those who aspirate liquid or solid food. In a study of 73 institutionalized patients with Alzheimer’s dementia, the latter subgroup accounted for 34% of the patients assessed.
Poor diet is the main source of protein-energy deficiency in elderly inpatients. Occult malabsorption secondary to bacterial overgrowth in the small intestine may also be an important factor, as is the increased catabolic state associated with acute illness.
Though the most at-risk patients have severe mental and physical incapacities, other problems including respiratory disease, gastrointestinal disease, and stroke are associated with a malnourished state.3
Though hospitalists generally acknowledge the potential seriousness of a patient developing nutritional deficits, the attending healthcare team may be slow to diagnose or manage this problem because:
- Elderly patients can be malnourished on admission, but classic signs of protein-energy deficiency are mistaken for normal signs of aging;
- Nutritional problems are observed by the medical staff, but aggressive treatment is deferred in light of seemingly more pressing medical issues;
- Many physicians take action to prevent nutritional deficiencies, but these interventions are often insufficient or ineffective in preventing the spiral into malnutrition; and
- Physicians may assume a nutritionist is working to prevent and treat nutritional deficiencies, while the nutritionist is waiting for the medical staff to address the problem with a feeding tube.
Clinical Outcomes
Most physicians have observed the declining physical and cognitive capabilities of a nutritionally deprived elderly inpatient.
Although a causal relationship between malnutrition and adverse events has not been established, this is most likely because an older person’s clinical course affects and is affected by his nutritional status. Further, frequently compromised homeostatic mechanisms make the risk of complications related to malnutrition potentially more severe.
Though researchers are studying how inadequate nutritional intake contributes to the risk of adverse outcomes in elderly inpatients, numerous studies have identified strong correlations between the severity of the nutritional deficit and the risk of subsequent morbid events.
Sullivan, et al., found in their 1999 study of protein-energy undernutrition among elderly hospitalized patients that those maintained on nutrient intakes far less than their estimated energy requirements were at more risk of in-hospital mortality.
Other studies have shown that the risk of in-hospital starvation correlates strongly with polypharmacy and long stay. The severity of the nutritional deficiency correlates not only with weight loss and secretory protein loss, but also the risk of in-hospital and long-term complications.
Who Needs Help
Basic nutritional requirements vary much less than might be expected among younger and older patients. However, while a malnourished 20-year-old can be easily identified, the classic signs of malnutrition (wasting, brittle hair, dry skin, fissured mucus membranes) are less easily detected in elderly patients. They are often mistaken for signs of normal aging. Questions that can elicit evidence of a protein-energy deficiency include:
- Has food intake decreased recently?
- Are there physical difficulties with eating?
- Is the patient confused or depressed?
- Has there been diarrhea or vomiting?
- Has the patient been able to shop and manage food preparation?
- Has the patient or family noticed weight loss?
- What does the patient regard as a normal weight?
However, because the clinical signs of malnutrition-weight loss, muscle wasting, and fatigue can be difficult to detect from history alone, use of an assessment tool is often necessary.
There is no simple diagnostic test for undernutrition. Measurements of albumin, prealbumin, body-mass index (BMI), and weight loss have been used, albeit problematically, for this purpose. More useful for the quantification of nutritional status in elderly outpatients, these measurements are difficult to use in the hospital because albumin levels are frequently affected by disease processes involving the liver, kidney, and immune system, and correct baseline weights and heights are notoriously difficult to obtain from elderly patients.4
The Nutritional Risk Index was developed in response to these difficulties, but it was originally calibrated for young, post-surgical patients. Because of the problematic nature of obtaining the accurate heights and weights needed for the NRI in elderly patients, Bouillanne, et al,. developed the Geriatric Nutritional Risk Index (GNRI) in 2005 based on albumin levels, hospital recorded weights, and weight loss (see Table 1, above).
The GNRI’s creators classified patients according to their level of malnutrition and calculated their risk of related comorbidities. They found that 44% of their study population had major or moderate nutrition-related risk and recommended nutritional supplementation.
Path to Recovery
Refeeding regimens for elderly patients diagnosed as undernourished are best started with meals of personally chosen foods, timed for when patients are hungry.
Many elderly patients do not eat on a strict schedule at home and have difficulty complying with such a schedule. If oral intake remains inadequate, offer nutritional supplements. Because low-energy diets are usually low in vitamins and minerals, supplementation with a multivitamin, thiamine, folic acid, and zinc can be beneficial.
A common approach to problems with nutritional intake in elderly patients, particularly those with altered cognition or fluctuating consciousness, is insertion of a feeding tube.5 According to Medicare data from the 1990s, in individuals older than 85, one in 131 whites, and one in 58 African-Americans had a gastrostomy.
Despite the large numbers of feeding-tube placements in elderly patients, proof of their effectiveness is scant. No randomized trials have been performed to determine whether this practice improves survival, and observational data reveal that the one-year survival for these patients is less than 40%.
Feeding tubes are often placed to reverse the clinical sequelae of malnutrition—to heal pressure ulcers, prevent infection, and improve the patient’s functional status. But prospective observational studies do not support this methodology, and some contradictory evidence in the form of worsening pressure ulcers has been observed.
Aspiration pneumonia is the most serious infection for which tube feeding is considered a preventive measure. The condition results from the misdirection of pharyngeal contents and is believed to develop when nonpathologic oral secretions are deposited in dependent areas of the lung. The bacterial inoculum is high enough to overcome local defenses, which results in an infectious, febrile illness, usually involving mixed gram-negative rods and anaerobes.
Summaries of current data show that tube feeding may increase the risk of aspiration pneumonia. Further support for this hypothesis comes from the observation that jejunostomy feeding also does not appear to reduce the risk of aspiration pneumonia. If a patient is unable to protect his airway during mealtimes, he will also be at risk of aspiration and pneumonia between meals, regardless of how nutrition is delivered. TH
Dr. Landis is a rheumatologist and freelance writer.
References
- Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients. JAMA. 1999;281(21):2013-2019.
- Incalzi RA, Gemma A, Capparella O, et al. Energy intake and in-hospital starvation: a clinically relevant relationship. Arch Intern Med. 1996;156(4):425-429.
- Tierney A. Undernutrition and elderly patients. J Adv Nurs. 1995;23(2):228-236.
- Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: a new index for evaluating at risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777-783.
- Finucane T, Williams M. Tube feeding the demented patient: a review of the evidence. American Geriatrics Society Annual Scientific Meeting 2001.
Despite a general understanding among hospitalists that malnutrition has severe negative effects on hospitalized patients, preventive or corrective measures often aren’t taken.
The ill effects of nutritional deficiency are particularly profound in elderly inpatients. Estimates of protein-energy malnutrition vary between 20%-78% of elderly medical patients, who are uniquely disposed to the cognitive, metabolic, and immune-mediating consequences of malnutrition.1
Most hospitalists know when to request a nutritionist consultation or order extra mealtime cans of Ensure. But many do not realize these efforts often do little to alter patients’ descent into nutritional deficiency.
Define the Problem
Four patterns of problematic eating have been described in elderly inpatients.
The first and most common is the patient who is permitted nothing by mouth and is not provided an alternate route of nutrition. Data show 44% of elderly malnourished inpatients fall into this category.2
Other abnormal feeding subgroups include patients who need to be fed but have no other eating problem, patients who refuse food but can swallow with difficulty, and those who aspirate liquid or solid food. In a study of 73 institutionalized patients with Alzheimer’s dementia, the latter subgroup accounted for 34% of the patients assessed.
Poor diet is the main source of protein-energy deficiency in elderly inpatients. Occult malabsorption secondary to bacterial overgrowth in the small intestine may also be an important factor, as is the increased catabolic state associated with acute illness.
Though the most at-risk patients have severe mental and physical incapacities, other problems including respiratory disease, gastrointestinal disease, and stroke are associated with a malnourished state.3
Though hospitalists generally acknowledge the potential seriousness of a patient developing nutritional deficits, the attending healthcare team may be slow to diagnose or manage this problem because:
- Elderly patients can be malnourished on admission, but classic signs of protein-energy deficiency are mistaken for normal signs of aging;
- Nutritional problems are observed by the medical staff, but aggressive treatment is deferred in light of seemingly more pressing medical issues;
- Many physicians take action to prevent nutritional deficiencies, but these interventions are often insufficient or ineffective in preventing the spiral into malnutrition; and
- Physicians may assume a nutritionist is working to prevent and treat nutritional deficiencies, while the nutritionist is waiting for the medical staff to address the problem with a feeding tube.
Clinical Outcomes
Most physicians have observed the declining physical and cognitive capabilities of a nutritionally deprived elderly inpatient.
Although a causal relationship between malnutrition and adverse events has not been established, this is most likely because an older person’s clinical course affects and is affected by his nutritional status. Further, frequently compromised homeostatic mechanisms make the risk of complications related to malnutrition potentially more severe.
Though researchers are studying how inadequate nutritional intake contributes to the risk of adverse outcomes in elderly inpatients, numerous studies have identified strong correlations between the severity of the nutritional deficit and the risk of subsequent morbid events.
Sullivan, et al., found in their 1999 study of protein-energy undernutrition among elderly hospitalized patients that those maintained on nutrient intakes far less than their estimated energy requirements were at more risk of in-hospital mortality.
Other studies have shown that the risk of in-hospital starvation correlates strongly with polypharmacy and long stay. The severity of the nutritional deficiency correlates not only with weight loss and secretory protein loss, but also the risk of in-hospital and long-term complications.
Who Needs Help
Basic nutritional requirements vary much less than might be expected among younger and older patients. However, while a malnourished 20-year-old can be easily identified, the classic signs of malnutrition (wasting, brittle hair, dry skin, fissured mucus membranes) are less easily detected in elderly patients. They are often mistaken for signs of normal aging. Questions that can elicit evidence of a protein-energy deficiency include:
- Has food intake decreased recently?
- Are there physical difficulties with eating?
- Is the patient confused or depressed?
- Has there been diarrhea or vomiting?
- Has the patient been able to shop and manage food preparation?
- Has the patient or family noticed weight loss?
- What does the patient regard as a normal weight?
However, because the clinical signs of malnutrition-weight loss, muscle wasting, and fatigue can be difficult to detect from history alone, use of an assessment tool is often necessary.
There is no simple diagnostic test for undernutrition. Measurements of albumin, prealbumin, body-mass index (BMI), and weight loss have been used, albeit problematically, for this purpose. More useful for the quantification of nutritional status in elderly outpatients, these measurements are difficult to use in the hospital because albumin levels are frequently affected by disease processes involving the liver, kidney, and immune system, and correct baseline weights and heights are notoriously difficult to obtain from elderly patients.4
The Nutritional Risk Index was developed in response to these difficulties, but it was originally calibrated for young, post-surgical patients. Because of the problematic nature of obtaining the accurate heights and weights needed for the NRI in elderly patients, Bouillanne, et al,. developed the Geriatric Nutritional Risk Index (GNRI) in 2005 based on albumin levels, hospital recorded weights, and weight loss (see Table 1, above).
The GNRI’s creators classified patients according to their level of malnutrition and calculated their risk of related comorbidities. They found that 44% of their study population had major or moderate nutrition-related risk and recommended nutritional supplementation.
Path to Recovery
Refeeding regimens for elderly patients diagnosed as undernourished are best started with meals of personally chosen foods, timed for when patients are hungry.
Many elderly patients do not eat on a strict schedule at home and have difficulty complying with such a schedule. If oral intake remains inadequate, offer nutritional supplements. Because low-energy diets are usually low in vitamins and minerals, supplementation with a multivitamin, thiamine, folic acid, and zinc can be beneficial.
A common approach to problems with nutritional intake in elderly patients, particularly those with altered cognition or fluctuating consciousness, is insertion of a feeding tube.5 According to Medicare data from the 1990s, in individuals older than 85, one in 131 whites, and one in 58 African-Americans had a gastrostomy.
Despite the large numbers of feeding-tube placements in elderly patients, proof of their effectiveness is scant. No randomized trials have been performed to determine whether this practice improves survival, and observational data reveal that the one-year survival for these patients is less than 40%.
Feeding tubes are often placed to reverse the clinical sequelae of malnutrition—to heal pressure ulcers, prevent infection, and improve the patient’s functional status. But prospective observational studies do not support this methodology, and some contradictory evidence in the form of worsening pressure ulcers has been observed.
Aspiration pneumonia is the most serious infection for which tube feeding is considered a preventive measure. The condition results from the misdirection of pharyngeal contents and is believed to develop when nonpathologic oral secretions are deposited in dependent areas of the lung. The bacterial inoculum is high enough to overcome local defenses, which results in an infectious, febrile illness, usually involving mixed gram-negative rods and anaerobes.
Summaries of current data show that tube feeding may increase the risk of aspiration pneumonia. Further support for this hypothesis comes from the observation that jejunostomy feeding also does not appear to reduce the risk of aspiration pneumonia. If a patient is unable to protect his airway during mealtimes, he will also be at risk of aspiration and pneumonia between meals, regardless of how nutrition is delivered. TH
Dr. Landis is a rheumatologist and freelance writer.
References
- Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients. JAMA. 1999;281(21):2013-2019.
- Incalzi RA, Gemma A, Capparella O, et al. Energy intake and in-hospital starvation: a clinically relevant relationship. Arch Intern Med. 1996;156(4):425-429.
- Tierney A. Undernutrition and elderly patients. J Adv Nurs. 1995;23(2):228-236.
- Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: a new index for evaluating at risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777-783.
- Finucane T, Williams M. Tube feeding the demented patient: a review of the evidence. American Geriatrics Society Annual Scientific Meeting 2001.
In the Literature
In This Edition
- Treat with antibiotics for seven days or less in adults with community-acquired pneumonia.
- In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux (Arixtra) is safer than with enoxaparin (Lovenox).
- Multislice coronary angiography rules out suspected coronary artery disease.
- Hospitalists in teaching hospitals decrease length of stay in complex patients.
- Epoetin alfa (Procrit/Epogen) use in critically ill patients does not reduce red-cell transfusion but may reduce mortality in trauma.
- Newer antibiotics appear to be more effective for acute exacerbations of chronic bronchitis.
- Low-income patients and patients seen by specialists are less likely to use generic medications.
- Hospitalist-orthopedic comanagement of patients with hip fractures does not negatively affect long-term mortality.
- Probiotics reduce antibiotic and C. difficile-associated diarrhea.
- Healthcare-associated pneumonia closely resembles nosocomial pneumonia.
What Is the Appropriate Duration of Antibiotic Therapy for Adults with CAP?
Background: Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality, but there is little consensus on the appropriate duration of antibiotic therapy. Current guidelines recommend antibiotic regimens lasting from five to 14 days. Shorter courses of antibiotic therapy may improve patient compliance, reduce risk of medication related adverse effects, and minimize the risk of antimicrobial resistance.
Study design: Meta-analysis.
Synopsis: Authors included 15 randomized controlled trials from 1990 through 2004. They compared the efficacy of short-course (seven days or less) antibiotic monotherapy versus extended regimens (longer than seven days) in patients age 12 or older with mild to moderate CAP. They excluded trials with a significant number of patients with bronchitis, healthcare-associated pneumonias, and chronic obstructive pulmonary disease exacerbations. The primary outcome measure failed to achieve clinical improvement or cure. Secondary outcome measures included mortality, bacteriologic failure, and other adverse events.
The authors found no significant differences in the risk of clinical failure, risk of mortality, risk of bacteriologic failure, or risk of adverse events in the short-course versus extended-course antibiotic regimens. This was consistent among the four antibiotic classes in the study: beta-lactam, fluoroquinolone, ketolide, and macrolide.
Bottom line: This study found no differences between short-course and extended-course antibiotic regimens in the treatment of adults with mild to moderate CAP in regard to clinical success, mortality, bacteriologic success, and adverse events.
Citation: Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for CAP: A meta-analysis. Am J Med. 2007;120(9):783-790.
Is Fondaparinux Superior to Enoxaparin in Non-ST-Elevation Acute Coronary Syndromes?
Background: Fondaparinux is a selective factor Xa inhibitor approved by the FDA for the treatment and prevention of venous thromboembolism. The Organization to Assess Strategies for Ischemic Syndromes (OASIS)-5 was a randomized, double-blind trial that demonstrated fondaparinux is similar to enoxaparin in reducing the risk of ischemic events, but substantially reduces major bleeding, long-term mortality, and morbidity.1
Study design: Subgroup analysis of a randomized, controlled trial.
Setting: Hospitals to which patients with non-ST-segment elevation acute coronary syndrome presented.
Synopsis: In a subgroup analysis of 19,979 in the OASIS-5 trial, patients were divided into quartiles based on their estimated creatinine clearance, calculated by using the Modification of Diet in Renal Disease formula.2 Death, myocardial infarction, refractory ischemia, and major bleeding were evaluated separately, and as a composite end point at nine, 30, and 180 days.
At nine days, death, myocardial infarction, or refractory ischemia occurred in 6.7% of patients receiving fondaparinux and 7.4% of those receiving enoxaparin (hazard ratio, 0.90, 95% confidence interval [CI], 0.73 to 1.11); major bleeding occurred in 2.8% and 6.4%, respectively (hazard ratio, 0.42, CI, 0.32 to 0.56). Statistically significant differences in major bleeding persisted at 30 and 180 days.
While there was a trend toward a reduction in the composite end point among all quartiles of glomerular filtration rate (GFR), the differences were statistically significant only among patients with a GFR less than 58 mL/min per 1.73 m2. The authors concluded that the absolute differences in favor of fondaparinux (efficacy and safety) were most apparent in patients with a GFR less than 58 mL/min per 1.73 m2 and were largely the result in a reduction in bleeding events.
The subgroup analysis was not planned before the OASIS-5 data were collected, and the results have not been confirmed elsewhere. For patients managed with an early invasive strategy, catheter thrombosis occurred more often in those who received fondaparinux than enoxaparin alone. Fondaparinux is not FDA approved for this indication.
Bottom line: In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux is associated with a significant reduction in the incidence of major bleeding as compared with enoxaparin.
Citations:
- Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354(14):1464-1476.
- Fox KA, Bassand JP, Mehta SR, et al. Influence of renal function on the efficacy and safety of fondaparinux relative to enoxaparin in non ST-segment elevation acute coronary syndromes. Ann Intern Med. 2007;147(5):304-310.
What’s the Prognosis of Asymptomatic Patients with Suspected Coronary Artery Disease with Normal Multislice Angiogram?
Background: Several studies have demonstrated high sensitivity and negative predictive values for computed tomography (CT) coronary angiography.
Study design: Prospective, sequentially enrolled subjects.
Synopsis: A CT angiogram was given to 182 consecutive patients scheduled for conventional coronary angiography without acute coronary syndrome and insufficient coronary calcification to limit CT angiography. Researchers enrolled 141 because CT angiography was inconclusive or warranted actual conventional angiography.
These normal CT angiogram subjects were followed for a mean time of 14.7 months without loss to follow-up or any mortality. Five subsequently underwent conventional angiography eight to 11 months following CT, and three had clinically significant single-vessel disease. The other two had normal conventional angiograms. There was one myocardial infarction patient who, upon further review of CT, had previously unappreciated right-coronary-artery (RCA) disease. This prospective study demonstrated a 97.2% negative predictive value consistent with previous studies. Mortality, myocardial infarction, and subsequently identified coronary artery disease (CAD) are also consistent with previously published data for conventional angiography.
Bottom line: In this small, prospective study, multislice CT coronary angiography safely rules out suspected CAD.
Citation: Gilard M, Le Gal G, Cornily JC, et al. Midterm prognosis of patients with suspected coronary artery disease and normal multislice computer tomographic findings. Arch Intern Med. 2007;165(15):1687-1689.
Does Epoetin Alfa Reduce Need for Blood Transfusion Therapy in Critically Ill Patients?
Background: Two prior studies demonstrated that the use of epoetin reduced the number of red-cell transfusions in ICU patients without any other clinical benefits. There were possible subgroup differences between trauma and nontrauma patients. This study assessed a reduced dose of epoetin alfa and evaluated clinical outcomes and subgroup differences suggested by the previous studies.
Study design: Prospective, randomized, double-blind, placebo-controlled clinical trial.
Setting: 115 medical centers.
Synopsis: The study group of 1,460 patients underwent stratified randomization into trauma, surgical nontrauma, and medical nontrauma groups. There were no significant differences in transfusion requirements between the epoetin group, the placebo group, or in any subgroup. The mean pre-transfusion hemoglobin was the same in each group.
The epoetin group had a higher-than-baseline hemoglobin level at day 29 (1.6 versus 1.2 g/dL, p<0.001) and a higher absolute hemoglobin (11.2 versus 10.8 g/dL, p<0.001) than the placebo group. Mortality was lower in the epoetin group (8.5% versus 11.4%, p=0.02) and in the trauma subgroup (3.5% versus 6.6%, p=0.04). In two nontrauma groups, point estimates demonstrated similar lower mortality but were not statistically significant.
Thrombotic vascular events were higher in the epoetin group than the placebo group (16.5% versus 11.5%, p=0.008), but post-hoc analyses demonstrated that the effect was only observed in patients who had not received heparin at baseline. There were no other observed differences in length of stay or use of mechanical ventilation.
Bottom line: Epoetin alfa does not reduce red blood cell transfusions in ICU patients but may reduce mortality in trauma patients. Increased thrombotic events may be mitigated with the use of heparin.
Citation: Corwin HL, Gettinger A, Fabian TC, et al. Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med. 2007;357 (10):965-976.
What Patients Benefit Most from Hospitalist Care in an Academic Medical Center?
Background: Hospitalists increasingly serve as teaching attending physicians at many academic medical centers. Studies have shown hospitalists’ care can reduce the length of hospital stay in patients with a limited number of specific diagnoses. It has not been established whether there are other specific patient diagnoses or discharge dispositions that might benefit from hospitalist care in a teaching hospital.
Study design: Retrospective cohort.
Setting: Urban teaching hospital.
Synopsis: The authors examined the patients discharged from a hospitalist and a non-hospitalist teaching attending service at an academic medical center during a two-year period beginning July 1, 2002. The length of hospital stay for patients on the hospitalist teaching attending service was significantly lower than that of the non-hospitalist teaching attending service. This difference was most pronounced in patients with highest overall acuity as measured by diagnosis-related group (DRG) weight and patients who required discharge to nursing facilities.
Bottom line: Medically complex inpatients and inpatients with complex discharge planning needs appear to have a shorter length of hospital stay when under the care of hospitalists serving as teaching attending physicians compared with non-hospitalist teaching attending physicians.
Citation: Southern WN, Berger MA, Bellin EY, et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167(17):1869-1874.
What Influences Use of Generic, Branded Medications?
Background: Expenditures for prescription medications exceeded $250 billion in 2005. Various patient, physician, and payment factors may increase generic drug use in an attempt to reduce costs without affecting quality of care.
Study design: Observational analysis.
Synopsis: This study analyzed initial and subsequent pharmacy claims for 5,399 patients enrolled in a large health plan in the western United States, from 2001-2003. For new prescriptions, 23% were generics. Initiation of generic medications was less likely for patients in poor neighborhoods and for prescriptions written by specialists; pharmacy benefit design and pharmacy type did not have a significant influence.
After initiation of branded medications, 15% switched to generics during the study follow-up. Patients were more likely to switch to generic medications if they were older, if they used mail-order pharmacies, or if they participated in multitier (three or more) co-payment plans.
Bottom line: Low-income patients and patients who see specialists are less likely to initiate generic medications; after initiation on branded medications, patients using mail-order pharmacies or multitier co-payment systems are more likely to switch to generics.
Citation: Shrank WH, Stedman M, Ettner SL, et al. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med. 2007; 22:1298-1304.
Does Orthopedic Comanagement Increase Mortality in Elderly Hip Fracture Patients?
Background: Prior studies have demonstrated that for patients with hip fracture, a hospitalist-orthopedic comanagement management service reduced time to surgery and length of stay, with no difference in inpatient mortality. This study sought to address whether this applied to long-term mortality as well.
Study design: Retrospective cohort study.
Setting: Tertiary care center.
Synopsis: This study examined 466 patients admitted consecutively to a tertiary care center for surgical repair of a hip fracture, and followed them for one year postoperatively. It compared outcomes for patients admitted to a hospitalist-orthopedic comanagement service (2001-2002) with a standard care group of historical controls admitted to either an orthopedic or general medical teaching service (2000-2001).
One-year survival did not differ between the patients on the hospitalist-orthopedic comanagement service (70.5%) versus those in the standard care group (70.6%). The hospitalist-orthopedic comanagement model was associated with shorter time to surgery and shorter length of stay (8.4 versus 10.6 days). According to multivariate analysis, independent predictors of mortality were: American Society of Anesthesiologists (ASA) class III or IV (hazard ratio 4.2, 95% CI, 2.21, 7.99), admission from a nursing home (hazard ratio 2.24, 95% CI, 1.73, 2.90), and inpatient complications such as renal failure, myocardial infarction, or ICU admission (hazard ratio 1.85, CI 95%, 1.45, 2.35).
The authors note that prior studies demonstrated benefits from hospitalist involvement only after one year of implementation. This study was performed during the first year of the hospitalist-orthopedic comanagement team.
Bottom line: Hospitalist-orthopedic comanagement of patients with hip fracture reduces length of stay and does not negatively affect long-term mortality.
Citation: Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2:219-225.
How Effective Are First-Line, Second-Line Antibiotics for AECB?
Background: Antibiotics are frequently used for treatment of acute exacerbations of chronic bronchitis (AECB). However, in this era of increasing microbial resistance, there are insufficient data comparing the efficacy and safety of first-line antibiotics (ampicillin, amoxicillin, doxycycline, trimethoprim-sulfamethoxazole [Bactrim, Cotrima, Septra]) with second-line antibiotics (amoxicillin-clavulanic acid [Augmentin], macrolides, second- and third-generation cephalosporins, and fluoroquinolones).
Study design: Meta-analysis of randomized controlled trials (RCT).
Synopsis: Authors included 12 RCTs from 1981 to 2000, enrolling 2,261 adult patients comparing the efficacy and toxicity of first-line with second-line antibiotics for AECB in inpatient and outpatient settings. The authors measured treatment success, drug-related adverse events, all-cause mortality and pathogen eradication.
They concluded that administration of first-line antibiotics was associated with lower treatment success than administration of second-line antibiotics (odd ratio [OR] 0.51, 95% CI, 0.34 to 0.75). However, no differences were found with regard to all-cause mortality (OR 0.64, 95% CI, 0.25 to 3.35), adverse effects (OR 0.75, 95% CI, 0.39 to 1.45), or treatment success in microbiologically evaluable patients (OR 0.56, 95% CI, 0.22 to 1.43). Some limitations of this meta-analysis include:
- Inadequate data to stratify patients according to risk factors for poor outcome;
- Trials included inpatients as well as outpatients (likely with varying disease severity); and
- Trials were conducted in different time periods with changing patterns of anti-microbial resistance.
Bottom line: In patients with AECB, second-line antibiotics are more effective than first-line antibiotics with no differences in safety or mortality.
Citation: Dimopoulos G, Siempos II, Korbila IP, et al. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis. Chest. 2007;132:447-455.
Do Probiotic Drinks Reduce Antibiotic-Associated Diarrhea?
Background: Patients on antibiotics experience diarrhea as a side effect 5%-25% of the time, of which C. difficile is the cause in 15%-25% of these cases. Probiotics, such as Streptococcus thermophilus, Enterococcus species, Saccharomyces species, and Lactobacillus species are live microorganisms that can safely be used to treat diarrhea associated with antibiotic use.
Study design: Randomized, double-blind, placebo controlled
Setting: Three London hospitals
Synopsis: The study enrolled 135 hospitalized patients over age 50 who were prescribed antibiotics.
The treatment group received a probiotic yogurt drink containing Lactobacillus casei, L. bulgaricus, and S. thermophilus; the placebo group received a sterile milkshake. Subjects consumed the drinks twice daily within 48 hours of starting antibiotic therapy and continued for one week after antibiotic use.
There was a significant reduction of diarrhea in the probiotic group (p=0.007); the number needed to treat (NNT) was five. There was also a significant decrease in diarrhea caused by C. difficile (p=0.001), the secondary outcome, with an NNT of six.
These results may translate into decreased patient morbidity, mortality, healthcare costs, and length of stay. Additional studies are needed to establish the most effective probiotic and dosing for reducing diarrhea.
Bottom line: Twice-daily consumption of probiotic drinks can decrease the risk of antibiotic-induced diarrhea.
Citation: Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomized double blind placebo controlled trial. BMJ. 2007 Jul 14;335(7610):80.
What Organisms Commonly Cause Healthcare-Associated Pneumonia in Nonhospitalized Patients?
Background: Changes in practice patterns have resulted in a large number of patients who regularly interact with healthcare but aren’t admitted to the hospital (e.g., those receiving dialysis or home healthcare). These patients develop nosocomial-type infections rather than infections from traditionally community-acquired organisms.
Study design: Prospective observational for three years.
Setting: A large teaching hospital in Barcelona, Spain.
Synopsis: A total of 727 patients were stratified into community-acquired pneumonia (CAP) or healthcare-associated pneumonia (HCAP) groups based on whether they had:
- Received home intravenous therapy;
- Attended a hospital or hemodialysis clinic or had chemotherapy in the preceding 30 days;
- Were admitted to an acute care facility for at least two days in the preceding 90 days; or
- Resided in a nursing home.
The HCAP group tended to be older, have higher comorbidities (particularly cerebrovascular disease or malignancy), have previously received antibiotics, and have higher pneumonia severity indices.
The putative organisms were similar in both groups with Streptococcus pneumoniae representing the most common pathogen. HCAP patients had higher rates of penicillin, erythromycin, and levofloxacin resistance; aspiration pneumonia; longer lengths of stay; and 30-day mortality. Inappropriate therapy occurred more commonly in the HCAP group (5.6% versus 2.0%). Such therapy was defined as the absence of antibiotics targeting suspect pathogens, the use of antibiotics to which the bacteria were not susceptible, or the failure to start anaerobic coverage for aspiration pneumonia.
Bottom line: Outpatients who come in frequent contact with the healthcare system while presenting with pneumonia are more likely to have drug-resistant organisms similar to those seen in nosocomial pneumonia. Further, they tend to have inappropriate or inadequate antimicrobial therapy, longer hospital stays, and increased risk of death.
Citation: Carratalà J, Mykietiuk A, Fernández-Sabe N, et al. Health care-associated pneumonia requiring hospital admission. Arch Intern Med. 2007;167(13):1393-1399. TH
In This Edition
- Treat with antibiotics for seven days or less in adults with community-acquired pneumonia.
- In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux (Arixtra) is safer than with enoxaparin (Lovenox).
- Multislice coronary angiography rules out suspected coronary artery disease.
- Hospitalists in teaching hospitals decrease length of stay in complex patients.
- Epoetin alfa (Procrit/Epogen) use in critically ill patients does not reduce red-cell transfusion but may reduce mortality in trauma.
- Newer antibiotics appear to be more effective for acute exacerbations of chronic bronchitis.
- Low-income patients and patients seen by specialists are less likely to use generic medications.
- Hospitalist-orthopedic comanagement of patients with hip fractures does not negatively affect long-term mortality.
- Probiotics reduce antibiotic and C. difficile-associated diarrhea.
- Healthcare-associated pneumonia closely resembles nosocomial pneumonia.
What Is the Appropriate Duration of Antibiotic Therapy for Adults with CAP?
Background: Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality, but there is little consensus on the appropriate duration of antibiotic therapy. Current guidelines recommend antibiotic regimens lasting from five to 14 days. Shorter courses of antibiotic therapy may improve patient compliance, reduce risk of medication related adverse effects, and minimize the risk of antimicrobial resistance.
Study design: Meta-analysis.
Synopsis: Authors included 15 randomized controlled trials from 1990 through 2004. They compared the efficacy of short-course (seven days or less) antibiotic monotherapy versus extended regimens (longer than seven days) in patients age 12 or older with mild to moderate CAP. They excluded trials with a significant number of patients with bronchitis, healthcare-associated pneumonias, and chronic obstructive pulmonary disease exacerbations. The primary outcome measure failed to achieve clinical improvement or cure. Secondary outcome measures included mortality, bacteriologic failure, and other adverse events.
The authors found no significant differences in the risk of clinical failure, risk of mortality, risk of bacteriologic failure, or risk of adverse events in the short-course versus extended-course antibiotic regimens. This was consistent among the four antibiotic classes in the study: beta-lactam, fluoroquinolone, ketolide, and macrolide.
Bottom line: This study found no differences between short-course and extended-course antibiotic regimens in the treatment of adults with mild to moderate CAP in regard to clinical success, mortality, bacteriologic success, and adverse events.
Citation: Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for CAP: A meta-analysis. Am J Med. 2007;120(9):783-790.
Is Fondaparinux Superior to Enoxaparin in Non-ST-Elevation Acute Coronary Syndromes?
Background: Fondaparinux is a selective factor Xa inhibitor approved by the FDA for the treatment and prevention of venous thromboembolism. The Organization to Assess Strategies for Ischemic Syndromes (OASIS)-5 was a randomized, double-blind trial that demonstrated fondaparinux is similar to enoxaparin in reducing the risk of ischemic events, but substantially reduces major bleeding, long-term mortality, and morbidity.1
Study design: Subgroup analysis of a randomized, controlled trial.
Setting: Hospitals to which patients with non-ST-segment elevation acute coronary syndrome presented.
Synopsis: In a subgroup analysis of 19,979 in the OASIS-5 trial, patients were divided into quartiles based on their estimated creatinine clearance, calculated by using the Modification of Diet in Renal Disease formula.2 Death, myocardial infarction, refractory ischemia, and major bleeding were evaluated separately, and as a composite end point at nine, 30, and 180 days.
At nine days, death, myocardial infarction, or refractory ischemia occurred in 6.7% of patients receiving fondaparinux and 7.4% of those receiving enoxaparin (hazard ratio, 0.90, 95% confidence interval [CI], 0.73 to 1.11); major bleeding occurred in 2.8% and 6.4%, respectively (hazard ratio, 0.42, CI, 0.32 to 0.56). Statistically significant differences in major bleeding persisted at 30 and 180 days.
While there was a trend toward a reduction in the composite end point among all quartiles of glomerular filtration rate (GFR), the differences were statistically significant only among patients with a GFR less than 58 mL/min per 1.73 m2. The authors concluded that the absolute differences in favor of fondaparinux (efficacy and safety) were most apparent in patients with a GFR less than 58 mL/min per 1.73 m2 and were largely the result in a reduction in bleeding events.
The subgroup analysis was not planned before the OASIS-5 data were collected, and the results have not been confirmed elsewhere. For patients managed with an early invasive strategy, catheter thrombosis occurred more often in those who received fondaparinux than enoxaparin alone. Fondaparinux is not FDA approved for this indication.
Bottom line: In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux is associated with a significant reduction in the incidence of major bleeding as compared with enoxaparin.
Citations:
- Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354(14):1464-1476.
- Fox KA, Bassand JP, Mehta SR, et al. Influence of renal function on the efficacy and safety of fondaparinux relative to enoxaparin in non ST-segment elevation acute coronary syndromes. Ann Intern Med. 2007;147(5):304-310.
What’s the Prognosis of Asymptomatic Patients with Suspected Coronary Artery Disease with Normal Multislice Angiogram?
Background: Several studies have demonstrated high sensitivity and negative predictive values for computed tomography (CT) coronary angiography.
Study design: Prospective, sequentially enrolled subjects.
Synopsis: A CT angiogram was given to 182 consecutive patients scheduled for conventional coronary angiography without acute coronary syndrome and insufficient coronary calcification to limit CT angiography. Researchers enrolled 141 because CT angiography was inconclusive or warranted actual conventional angiography.
These normal CT angiogram subjects were followed for a mean time of 14.7 months without loss to follow-up or any mortality. Five subsequently underwent conventional angiography eight to 11 months following CT, and three had clinically significant single-vessel disease. The other two had normal conventional angiograms. There was one myocardial infarction patient who, upon further review of CT, had previously unappreciated right-coronary-artery (RCA) disease. This prospective study demonstrated a 97.2% negative predictive value consistent with previous studies. Mortality, myocardial infarction, and subsequently identified coronary artery disease (CAD) are also consistent with previously published data for conventional angiography.
Bottom line: In this small, prospective study, multislice CT coronary angiography safely rules out suspected CAD.
Citation: Gilard M, Le Gal G, Cornily JC, et al. Midterm prognosis of patients with suspected coronary artery disease and normal multislice computer tomographic findings. Arch Intern Med. 2007;165(15):1687-1689.
Does Epoetin Alfa Reduce Need for Blood Transfusion Therapy in Critically Ill Patients?
Background: Two prior studies demonstrated that the use of epoetin reduced the number of red-cell transfusions in ICU patients without any other clinical benefits. There were possible subgroup differences between trauma and nontrauma patients. This study assessed a reduced dose of epoetin alfa and evaluated clinical outcomes and subgroup differences suggested by the previous studies.
Study design: Prospective, randomized, double-blind, placebo-controlled clinical trial.
Setting: 115 medical centers.
Synopsis: The study group of 1,460 patients underwent stratified randomization into trauma, surgical nontrauma, and medical nontrauma groups. There were no significant differences in transfusion requirements between the epoetin group, the placebo group, or in any subgroup. The mean pre-transfusion hemoglobin was the same in each group.
The epoetin group had a higher-than-baseline hemoglobin level at day 29 (1.6 versus 1.2 g/dL, p<0.001) and a higher absolute hemoglobin (11.2 versus 10.8 g/dL, p<0.001) than the placebo group. Mortality was lower in the epoetin group (8.5% versus 11.4%, p=0.02) and in the trauma subgroup (3.5% versus 6.6%, p=0.04). In two nontrauma groups, point estimates demonstrated similar lower mortality but were not statistically significant.
Thrombotic vascular events were higher in the epoetin group than the placebo group (16.5% versus 11.5%, p=0.008), but post-hoc analyses demonstrated that the effect was only observed in patients who had not received heparin at baseline. There were no other observed differences in length of stay or use of mechanical ventilation.
Bottom line: Epoetin alfa does not reduce red blood cell transfusions in ICU patients but may reduce mortality in trauma patients. Increased thrombotic events may be mitigated with the use of heparin.
Citation: Corwin HL, Gettinger A, Fabian TC, et al. Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med. 2007;357 (10):965-976.
What Patients Benefit Most from Hospitalist Care in an Academic Medical Center?
Background: Hospitalists increasingly serve as teaching attending physicians at many academic medical centers. Studies have shown hospitalists’ care can reduce the length of hospital stay in patients with a limited number of specific diagnoses. It has not been established whether there are other specific patient diagnoses or discharge dispositions that might benefit from hospitalist care in a teaching hospital.
Study design: Retrospective cohort.
Setting: Urban teaching hospital.
Synopsis: The authors examined the patients discharged from a hospitalist and a non-hospitalist teaching attending service at an academic medical center during a two-year period beginning July 1, 2002. The length of hospital stay for patients on the hospitalist teaching attending service was significantly lower than that of the non-hospitalist teaching attending service. This difference was most pronounced in patients with highest overall acuity as measured by diagnosis-related group (DRG) weight and patients who required discharge to nursing facilities.
Bottom line: Medically complex inpatients and inpatients with complex discharge planning needs appear to have a shorter length of hospital stay when under the care of hospitalists serving as teaching attending physicians compared with non-hospitalist teaching attending physicians.
Citation: Southern WN, Berger MA, Bellin EY, et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167(17):1869-1874.
What Influences Use of Generic, Branded Medications?
Background: Expenditures for prescription medications exceeded $250 billion in 2005. Various patient, physician, and payment factors may increase generic drug use in an attempt to reduce costs without affecting quality of care.
Study design: Observational analysis.
Synopsis: This study analyzed initial and subsequent pharmacy claims for 5,399 patients enrolled in a large health plan in the western United States, from 2001-2003. For new prescriptions, 23% were generics. Initiation of generic medications was less likely for patients in poor neighborhoods and for prescriptions written by specialists; pharmacy benefit design and pharmacy type did not have a significant influence.
After initiation of branded medications, 15% switched to generics during the study follow-up. Patients were more likely to switch to generic medications if they were older, if they used mail-order pharmacies, or if they participated in multitier (three or more) co-payment plans.
Bottom line: Low-income patients and patients who see specialists are less likely to initiate generic medications; after initiation on branded medications, patients using mail-order pharmacies or multitier co-payment systems are more likely to switch to generics.
Citation: Shrank WH, Stedman M, Ettner SL, et al. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med. 2007; 22:1298-1304.
Does Orthopedic Comanagement Increase Mortality in Elderly Hip Fracture Patients?
Background: Prior studies have demonstrated that for patients with hip fracture, a hospitalist-orthopedic comanagement management service reduced time to surgery and length of stay, with no difference in inpatient mortality. This study sought to address whether this applied to long-term mortality as well.
Study design: Retrospective cohort study.
Setting: Tertiary care center.
Synopsis: This study examined 466 patients admitted consecutively to a tertiary care center for surgical repair of a hip fracture, and followed them for one year postoperatively. It compared outcomes for patients admitted to a hospitalist-orthopedic comanagement service (2001-2002) with a standard care group of historical controls admitted to either an orthopedic or general medical teaching service (2000-2001).
One-year survival did not differ between the patients on the hospitalist-orthopedic comanagement service (70.5%) versus those in the standard care group (70.6%). The hospitalist-orthopedic comanagement model was associated with shorter time to surgery and shorter length of stay (8.4 versus 10.6 days). According to multivariate analysis, independent predictors of mortality were: American Society of Anesthesiologists (ASA) class III or IV (hazard ratio 4.2, 95% CI, 2.21, 7.99), admission from a nursing home (hazard ratio 2.24, 95% CI, 1.73, 2.90), and inpatient complications such as renal failure, myocardial infarction, or ICU admission (hazard ratio 1.85, CI 95%, 1.45, 2.35).
The authors note that prior studies demonstrated benefits from hospitalist involvement only after one year of implementation. This study was performed during the first year of the hospitalist-orthopedic comanagement team.
Bottom line: Hospitalist-orthopedic comanagement of patients with hip fracture reduces length of stay and does not negatively affect long-term mortality.
Citation: Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2:219-225.
How Effective Are First-Line, Second-Line Antibiotics for AECB?
Background: Antibiotics are frequently used for treatment of acute exacerbations of chronic bronchitis (AECB). However, in this era of increasing microbial resistance, there are insufficient data comparing the efficacy and safety of first-line antibiotics (ampicillin, amoxicillin, doxycycline, trimethoprim-sulfamethoxazole [Bactrim, Cotrima, Septra]) with second-line antibiotics (amoxicillin-clavulanic acid [Augmentin], macrolides, second- and third-generation cephalosporins, and fluoroquinolones).
Study design: Meta-analysis of randomized controlled trials (RCT).
Synopsis: Authors included 12 RCTs from 1981 to 2000, enrolling 2,261 adult patients comparing the efficacy and toxicity of first-line with second-line antibiotics for AECB in inpatient and outpatient settings. The authors measured treatment success, drug-related adverse events, all-cause mortality and pathogen eradication.
They concluded that administration of first-line antibiotics was associated with lower treatment success than administration of second-line antibiotics (odd ratio [OR] 0.51, 95% CI, 0.34 to 0.75). However, no differences were found with regard to all-cause mortality (OR 0.64, 95% CI, 0.25 to 3.35), adverse effects (OR 0.75, 95% CI, 0.39 to 1.45), or treatment success in microbiologically evaluable patients (OR 0.56, 95% CI, 0.22 to 1.43). Some limitations of this meta-analysis include:
- Inadequate data to stratify patients according to risk factors for poor outcome;
- Trials included inpatients as well as outpatients (likely with varying disease severity); and
- Trials were conducted in different time periods with changing patterns of anti-microbial resistance.
Bottom line: In patients with AECB, second-line antibiotics are more effective than first-line antibiotics with no differences in safety or mortality.
Citation: Dimopoulos G, Siempos II, Korbila IP, et al. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis. Chest. 2007;132:447-455.
Do Probiotic Drinks Reduce Antibiotic-Associated Diarrhea?
Background: Patients on antibiotics experience diarrhea as a side effect 5%-25% of the time, of which C. difficile is the cause in 15%-25% of these cases. Probiotics, such as Streptococcus thermophilus, Enterococcus species, Saccharomyces species, and Lactobacillus species are live microorganisms that can safely be used to treat diarrhea associated with antibiotic use.
Study design: Randomized, double-blind, placebo controlled
Setting: Three London hospitals
Synopsis: The study enrolled 135 hospitalized patients over age 50 who were prescribed antibiotics.
The treatment group received a probiotic yogurt drink containing Lactobacillus casei, L. bulgaricus, and S. thermophilus; the placebo group received a sterile milkshake. Subjects consumed the drinks twice daily within 48 hours of starting antibiotic therapy and continued for one week after antibiotic use.
There was a significant reduction of diarrhea in the probiotic group (p=0.007); the number needed to treat (NNT) was five. There was also a significant decrease in diarrhea caused by C. difficile (p=0.001), the secondary outcome, with an NNT of six.
These results may translate into decreased patient morbidity, mortality, healthcare costs, and length of stay. Additional studies are needed to establish the most effective probiotic and dosing for reducing diarrhea.
Bottom line: Twice-daily consumption of probiotic drinks can decrease the risk of antibiotic-induced diarrhea.
Citation: Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomized double blind placebo controlled trial. BMJ. 2007 Jul 14;335(7610):80.
What Organisms Commonly Cause Healthcare-Associated Pneumonia in Nonhospitalized Patients?
Background: Changes in practice patterns have resulted in a large number of patients who regularly interact with healthcare but aren’t admitted to the hospital (e.g., those receiving dialysis or home healthcare). These patients develop nosocomial-type infections rather than infections from traditionally community-acquired organisms.
Study design: Prospective observational for three years.
Setting: A large teaching hospital in Barcelona, Spain.
Synopsis: A total of 727 patients were stratified into community-acquired pneumonia (CAP) or healthcare-associated pneumonia (HCAP) groups based on whether they had:
- Received home intravenous therapy;
- Attended a hospital or hemodialysis clinic or had chemotherapy in the preceding 30 days;
- Were admitted to an acute care facility for at least two days in the preceding 90 days; or
- Resided in a nursing home.
The HCAP group tended to be older, have higher comorbidities (particularly cerebrovascular disease or malignancy), have previously received antibiotics, and have higher pneumonia severity indices.
The putative organisms were similar in both groups with Streptococcus pneumoniae representing the most common pathogen. HCAP patients had higher rates of penicillin, erythromycin, and levofloxacin resistance; aspiration pneumonia; longer lengths of stay; and 30-day mortality. Inappropriate therapy occurred more commonly in the HCAP group (5.6% versus 2.0%). Such therapy was defined as the absence of antibiotics targeting suspect pathogens, the use of antibiotics to which the bacteria were not susceptible, or the failure to start anaerobic coverage for aspiration pneumonia.
Bottom line: Outpatients who come in frequent contact with the healthcare system while presenting with pneumonia are more likely to have drug-resistant organisms similar to those seen in nosocomial pneumonia. Further, they tend to have inappropriate or inadequate antimicrobial therapy, longer hospital stays, and increased risk of death.
Citation: Carratalà J, Mykietiuk A, Fernández-Sabe N, et al. Health care-associated pneumonia requiring hospital admission. Arch Intern Med. 2007;167(13):1393-1399. TH
In This Edition
- Treat with antibiotics for seven days or less in adults with community-acquired pneumonia.
- In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux (Arixtra) is safer than with enoxaparin (Lovenox).
- Multislice coronary angiography rules out suspected coronary artery disease.
- Hospitalists in teaching hospitals decrease length of stay in complex patients.
- Epoetin alfa (Procrit/Epogen) use in critically ill patients does not reduce red-cell transfusion but may reduce mortality in trauma.
- Newer antibiotics appear to be more effective for acute exacerbations of chronic bronchitis.
- Low-income patients and patients seen by specialists are less likely to use generic medications.
- Hospitalist-orthopedic comanagement of patients with hip fractures does not negatively affect long-term mortality.
- Probiotics reduce antibiotic and C. difficile-associated diarrhea.
- Healthcare-associated pneumonia closely resembles nosocomial pneumonia.
What Is the Appropriate Duration of Antibiotic Therapy for Adults with CAP?
Background: Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality, but there is little consensus on the appropriate duration of antibiotic therapy. Current guidelines recommend antibiotic regimens lasting from five to 14 days. Shorter courses of antibiotic therapy may improve patient compliance, reduce risk of medication related adverse effects, and minimize the risk of antimicrobial resistance.
Study design: Meta-analysis.
Synopsis: Authors included 15 randomized controlled trials from 1990 through 2004. They compared the efficacy of short-course (seven days or less) antibiotic monotherapy versus extended regimens (longer than seven days) in patients age 12 or older with mild to moderate CAP. They excluded trials with a significant number of patients with bronchitis, healthcare-associated pneumonias, and chronic obstructive pulmonary disease exacerbations. The primary outcome measure failed to achieve clinical improvement or cure. Secondary outcome measures included mortality, bacteriologic failure, and other adverse events.
The authors found no significant differences in the risk of clinical failure, risk of mortality, risk of bacteriologic failure, or risk of adverse events in the short-course versus extended-course antibiotic regimens. This was consistent among the four antibiotic classes in the study: beta-lactam, fluoroquinolone, ketolide, and macrolide.
Bottom line: This study found no differences between short-course and extended-course antibiotic regimens in the treatment of adults with mild to moderate CAP in regard to clinical success, mortality, bacteriologic success, and adverse events.
Citation: Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for CAP: A meta-analysis. Am J Med. 2007;120(9):783-790.
Is Fondaparinux Superior to Enoxaparin in Non-ST-Elevation Acute Coronary Syndromes?
Background: Fondaparinux is a selective factor Xa inhibitor approved by the FDA for the treatment and prevention of venous thromboembolism. The Organization to Assess Strategies for Ischemic Syndromes (OASIS)-5 was a randomized, double-blind trial that demonstrated fondaparinux is similar to enoxaparin in reducing the risk of ischemic events, but substantially reduces major bleeding, long-term mortality, and morbidity.1
Study design: Subgroup analysis of a randomized, controlled trial.
Setting: Hospitals to which patients with non-ST-segment elevation acute coronary syndrome presented.
Synopsis: In a subgroup analysis of 19,979 in the OASIS-5 trial, patients were divided into quartiles based on their estimated creatinine clearance, calculated by using the Modification of Diet in Renal Disease formula.2 Death, myocardial infarction, refractory ischemia, and major bleeding were evaluated separately, and as a composite end point at nine, 30, and 180 days.
At nine days, death, myocardial infarction, or refractory ischemia occurred in 6.7% of patients receiving fondaparinux and 7.4% of those receiving enoxaparin (hazard ratio, 0.90, 95% confidence interval [CI], 0.73 to 1.11); major bleeding occurred in 2.8% and 6.4%, respectively (hazard ratio, 0.42, CI, 0.32 to 0.56). Statistically significant differences in major bleeding persisted at 30 and 180 days.
While there was a trend toward a reduction in the composite end point among all quartiles of glomerular filtration rate (GFR), the differences were statistically significant only among patients with a GFR less than 58 mL/min per 1.73 m2. The authors concluded that the absolute differences in favor of fondaparinux (efficacy and safety) were most apparent in patients with a GFR less than 58 mL/min per 1.73 m2 and were largely the result in a reduction in bleeding events.
The subgroup analysis was not planned before the OASIS-5 data were collected, and the results have not been confirmed elsewhere. For patients managed with an early invasive strategy, catheter thrombosis occurred more often in those who received fondaparinux than enoxaparin alone. Fondaparinux is not FDA approved for this indication.
Bottom line: In patients with chronic kidney disease who present with non ST-segment elevation acute coronary syndromes, anticoagulation with fondaparinux is associated with a significant reduction in the incidence of major bleeding as compared with enoxaparin.
Citations:
- Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354(14):1464-1476.
- Fox KA, Bassand JP, Mehta SR, et al. Influence of renal function on the efficacy and safety of fondaparinux relative to enoxaparin in non ST-segment elevation acute coronary syndromes. Ann Intern Med. 2007;147(5):304-310.
What’s the Prognosis of Asymptomatic Patients with Suspected Coronary Artery Disease with Normal Multislice Angiogram?
Background: Several studies have demonstrated high sensitivity and negative predictive values for computed tomography (CT) coronary angiography.
Study design: Prospective, sequentially enrolled subjects.
Synopsis: A CT angiogram was given to 182 consecutive patients scheduled for conventional coronary angiography without acute coronary syndrome and insufficient coronary calcification to limit CT angiography. Researchers enrolled 141 because CT angiography was inconclusive or warranted actual conventional angiography.
These normal CT angiogram subjects were followed for a mean time of 14.7 months without loss to follow-up or any mortality. Five subsequently underwent conventional angiography eight to 11 months following CT, and three had clinically significant single-vessel disease. The other two had normal conventional angiograms. There was one myocardial infarction patient who, upon further review of CT, had previously unappreciated right-coronary-artery (RCA) disease. This prospective study demonstrated a 97.2% negative predictive value consistent with previous studies. Mortality, myocardial infarction, and subsequently identified coronary artery disease (CAD) are also consistent with previously published data for conventional angiography.
Bottom line: In this small, prospective study, multislice CT coronary angiography safely rules out suspected CAD.
Citation: Gilard M, Le Gal G, Cornily JC, et al. Midterm prognosis of patients with suspected coronary artery disease and normal multislice computer tomographic findings. Arch Intern Med. 2007;165(15):1687-1689.
Does Epoetin Alfa Reduce Need for Blood Transfusion Therapy in Critically Ill Patients?
Background: Two prior studies demonstrated that the use of epoetin reduced the number of red-cell transfusions in ICU patients without any other clinical benefits. There were possible subgroup differences between trauma and nontrauma patients. This study assessed a reduced dose of epoetin alfa and evaluated clinical outcomes and subgroup differences suggested by the previous studies.
Study design: Prospective, randomized, double-blind, placebo-controlled clinical trial.
Setting: 115 medical centers.
Synopsis: The study group of 1,460 patients underwent stratified randomization into trauma, surgical nontrauma, and medical nontrauma groups. There were no significant differences in transfusion requirements between the epoetin group, the placebo group, or in any subgroup. The mean pre-transfusion hemoglobin was the same in each group.
The epoetin group had a higher-than-baseline hemoglobin level at day 29 (1.6 versus 1.2 g/dL, p<0.001) and a higher absolute hemoglobin (11.2 versus 10.8 g/dL, p<0.001) than the placebo group. Mortality was lower in the epoetin group (8.5% versus 11.4%, p=0.02) and in the trauma subgroup (3.5% versus 6.6%, p=0.04). In two nontrauma groups, point estimates demonstrated similar lower mortality but were not statistically significant.
Thrombotic vascular events were higher in the epoetin group than the placebo group (16.5% versus 11.5%, p=0.008), but post-hoc analyses demonstrated that the effect was only observed in patients who had not received heparin at baseline. There were no other observed differences in length of stay or use of mechanical ventilation.
Bottom line: Epoetin alfa does not reduce red blood cell transfusions in ICU patients but may reduce mortality in trauma patients. Increased thrombotic events may be mitigated with the use of heparin.
Citation: Corwin HL, Gettinger A, Fabian TC, et al. Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med. 2007;357 (10):965-976.
What Patients Benefit Most from Hospitalist Care in an Academic Medical Center?
Background: Hospitalists increasingly serve as teaching attending physicians at many academic medical centers. Studies have shown hospitalists’ care can reduce the length of hospital stay in patients with a limited number of specific diagnoses. It has not been established whether there are other specific patient diagnoses or discharge dispositions that might benefit from hospitalist care in a teaching hospital.
Study design: Retrospective cohort.
Setting: Urban teaching hospital.
Synopsis: The authors examined the patients discharged from a hospitalist and a non-hospitalist teaching attending service at an academic medical center during a two-year period beginning July 1, 2002. The length of hospital stay for patients on the hospitalist teaching attending service was significantly lower than that of the non-hospitalist teaching attending service. This difference was most pronounced in patients with highest overall acuity as measured by diagnosis-related group (DRG) weight and patients who required discharge to nursing facilities.
Bottom line: Medically complex inpatients and inpatients with complex discharge planning needs appear to have a shorter length of hospital stay when under the care of hospitalists serving as teaching attending physicians compared with non-hospitalist teaching attending physicians.
Citation: Southern WN, Berger MA, Bellin EY, et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167(17):1869-1874.
What Influences Use of Generic, Branded Medications?
Background: Expenditures for prescription medications exceeded $250 billion in 2005. Various patient, physician, and payment factors may increase generic drug use in an attempt to reduce costs without affecting quality of care.
Study design: Observational analysis.
Synopsis: This study analyzed initial and subsequent pharmacy claims for 5,399 patients enrolled in a large health plan in the western United States, from 2001-2003. For new prescriptions, 23% were generics. Initiation of generic medications was less likely for patients in poor neighborhoods and for prescriptions written by specialists; pharmacy benefit design and pharmacy type did not have a significant influence.
After initiation of branded medications, 15% switched to generics during the study follow-up. Patients were more likely to switch to generic medications if they were older, if they used mail-order pharmacies, or if they participated in multitier (three or more) co-payment plans.
Bottom line: Low-income patients and patients who see specialists are less likely to initiate generic medications; after initiation on branded medications, patients using mail-order pharmacies or multitier co-payment systems are more likely to switch to generics.
Citation: Shrank WH, Stedman M, Ettner SL, et al. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med. 2007; 22:1298-1304.
Does Orthopedic Comanagement Increase Mortality in Elderly Hip Fracture Patients?
Background: Prior studies have demonstrated that for patients with hip fracture, a hospitalist-orthopedic comanagement management service reduced time to surgery and length of stay, with no difference in inpatient mortality. This study sought to address whether this applied to long-term mortality as well.
Study design: Retrospective cohort study.
Setting: Tertiary care center.
Synopsis: This study examined 466 patients admitted consecutively to a tertiary care center for surgical repair of a hip fracture, and followed them for one year postoperatively. It compared outcomes for patients admitted to a hospitalist-orthopedic comanagement service (2001-2002) with a standard care group of historical controls admitted to either an orthopedic or general medical teaching service (2000-2001).
One-year survival did not differ between the patients on the hospitalist-orthopedic comanagement service (70.5%) versus those in the standard care group (70.6%). The hospitalist-orthopedic comanagement model was associated with shorter time to surgery and shorter length of stay (8.4 versus 10.6 days). According to multivariate analysis, independent predictors of mortality were: American Society of Anesthesiologists (ASA) class III or IV (hazard ratio 4.2, 95% CI, 2.21, 7.99), admission from a nursing home (hazard ratio 2.24, 95% CI, 1.73, 2.90), and inpatient complications such as renal failure, myocardial infarction, or ICU admission (hazard ratio 1.85, CI 95%, 1.45, 2.35).
The authors note that prior studies demonstrated benefits from hospitalist involvement only after one year of implementation. This study was performed during the first year of the hospitalist-orthopedic comanagement team.
Bottom line: Hospitalist-orthopedic comanagement of patients with hip fracture reduces length of stay and does not negatively affect long-term mortality.
Citation: Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2:219-225.
How Effective Are First-Line, Second-Line Antibiotics for AECB?
Background: Antibiotics are frequently used for treatment of acute exacerbations of chronic bronchitis (AECB). However, in this era of increasing microbial resistance, there are insufficient data comparing the efficacy and safety of first-line antibiotics (ampicillin, amoxicillin, doxycycline, trimethoprim-sulfamethoxazole [Bactrim, Cotrima, Septra]) with second-line antibiotics (amoxicillin-clavulanic acid [Augmentin], macrolides, second- and third-generation cephalosporins, and fluoroquinolones).
Study design: Meta-analysis of randomized controlled trials (RCT).
Synopsis: Authors included 12 RCTs from 1981 to 2000, enrolling 2,261 adult patients comparing the efficacy and toxicity of first-line with second-line antibiotics for AECB in inpatient and outpatient settings. The authors measured treatment success, drug-related adverse events, all-cause mortality and pathogen eradication.
They concluded that administration of first-line antibiotics was associated with lower treatment success than administration of second-line antibiotics (odd ratio [OR] 0.51, 95% CI, 0.34 to 0.75). However, no differences were found with regard to all-cause mortality (OR 0.64, 95% CI, 0.25 to 3.35), adverse effects (OR 0.75, 95% CI, 0.39 to 1.45), or treatment success in microbiologically evaluable patients (OR 0.56, 95% CI, 0.22 to 1.43). Some limitations of this meta-analysis include:
- Inadequate data to stratify patients according to risk factors for poor outcome;
- Trials included inpatients as well as outpatients (likely with varying disease severity); and
- Trials were conducted in different time periods with changing patterns of anti-microbial resistance.
Bottom line: In patients with AECB, second-line antibiotics are more effective than first-line antibiotics with no differences in safety or mortality.
Citation: Dimopoulos G, Siempos II, Korbila IP, et al. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis. Chest. 2007;132:447-455.
Do Probiotic Drinks Reduce Antibiotic-Associated Diarrhea?
Background: Patients on antibiotics experience diarrhea as a side effect 5%-25% of the time, of which C. difficile is the cause in 15%-25% of these cases. Probiotics, such as Streptococcus thermophilus, Enterococcus species, Saccharomyces species, and Lactobacillus species are live microorganisms that can safely be used to treat diarrhea associated with antibiotic use.
Study design: Randomized, double-blind, placebo controlled
Setting: Three London hospitals
Synopsis: The study enrolled 135 hospitalized patients over age 50 who were prescribed antibiotics.
The treatment group received a probiotic yogurt drink containing Lactobacillus casei, L. bulgaricus, and S. thermophilus; the placebo group received a sterile milkshake. Subjects consumed the drinks twice daily within 48 hours of starting antibiotic therapy and continued for one week after antibiotic use.
There was a significant reduction of diarrhea in the probiotic group (p=0.007); the number needed to treat (NNT) was five. There was also a significant decrease in diarrhea caused by C. difficile (p=0.001), the secondary outcome, with an NNT of six.
These results may translate into decreased patient morbidity, mortality, healthcare costs, and length of stay. Additional studies are needed to establish the most effective probiotic and dosing for reducing diarrhea.
Bottom line: Twice-daily consumption of probiotic drinks can decrease the risk of antibiotic-induced diarrhea.
Citation: Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomized double blind placebo controlled trial. BMJ. 2007 Jul 14;335(7610):80.
What Organisms Commonly Cause Healthcare-Associated Pneumonia in Nonhospitalized Patients?
Background: Changes in practice patterns have resulted in a large number of patients who regularly interact with healthcare but aren’t admitted to the hospital (e.g., those receiving dialysis or home healthcare). These patients develop nosocomial-type infections rather than infections from traditionally community-acquired organisms.
Study design: Prospective observational for three years.
Setting: A large teaching hospital in Barcelona, Spain.
Synopsis: A total of 727 patients were stratified into community-acquired pneumonia (CAP) or healthcare-associated pneumonia (HCAP) groups based on whether they had:
- Received home intravenous therapy;
- Attended a hospital or hemodialysis clinic or had chemotherapy in the preceding 30 days;
- Were admitted to an acute care facility for at least two days in the preceding 90 days; or
- Resided in a nursing home.
The HCAP group tended to be older, have higher comorbidities (particularly cerebrovascular disease or malignancy), have previously received antibiotics, and have higher pneumonia severity indices.
The putative organisms were similar in both groups with Streptococcus pneumoniae representing the most common pathogen. HCAP patients had higher rates of penicillin, erythromycin, and levofloxacin resistance; aspiration pneumonia; longer lengths of stay; and 30-day mortality. Inappropriate therapy occurred more commonly in the HCAP group (5.6% versus 2.0%). Such therapy was defined as the absence of antibiotics targeting suspect pathogens, the use of antibiotics to which the bacteria were not susceptible, or the failure to start anaerobic coverage for aspiration pneumonia.
Bottom line: Outpatients who come in frequent contact with the healthcare system while presenting with pneumonia are more likely to have drug-resistant organisms similar to those seen in nosocomial pneumonia. Further, they tend to have inappropriate or inadequate antimicrobial therapy, longer hospital stays, and increased risk of death.
Citation: Carratalà J, Mykietiuk A, Fernández-Sabe N, et al. Health care-associated pneumonia requiring hospital admission. Arch Intern Med. 2007;167(13):1393-1399. TH
SHM Behind the Scenes
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at bhansen@hospitalmedicine.org.
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at bhansen@hospitalmedicine.org.
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at bhansen@hospitalmedicine.org.
All Eyes on San Diego
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
Hospitalists Find Writing Makes Them Better Doctors
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.