User login
Hours to Expertise
Glass of wine in one hand and the Sept. 30 copy of Wine Spectator in the other, I intended to relax a bit—the future of hospital medicine not necessarily uppermost in my mind. But then I was struck by an article by Matt Kramer titled “10,000 hours.” In it he discusses the implications Daniel Levitin’s new book This Is Your Brain on Music: The Science of a Human Obsession (Dutton) may have for the field of wine tasting.
Levitin notes that “ten thousand hours of practice is required to achieve the level of mastery associated with being a world-class expert—in anything.” It turns out it doesn’t matter what you are trying to master.
“In study after study of composers, basketball players, fiction writers, ice skaters, concert pianists, chess players, master criminals, and what have you, this number comes up again and again,” he says. “No one has yet found a case in which true world-class expertise was accomplished in less time.” This is consistent with how we learn. “Learning requires the assimilation and consolidation of information in neural tissue,” writes Levitin. “The more experiences we have with something the stronger the memory/learning trace for the experience becomes.”
Ten thousand hours. Are you an expert in hospital medicine? Have you compiled the requisite 10,000 hours? The average hospitalist working approximately 200 shifts a year of 10 to 12 hours each would take four to five years to master the practice of hospital medicine. On the other hand, a provider spending 10 hours a week in the hospital would require 20 years to achieve the numeric equivalent of expert status.
While Levitin was discussing the impact of this calculation on music and Kramer on wine expertise, it struck me as applicable to one of the great debates surrounding hospital medicine. Early in the days of the hospitalist movement, many inside and outside the field opined as to whether hospitals should be the domain of hospitalists and clinics the domain of primary care doctors, without overlap. SHM and I proclaimed hospitals should be open to all providers, regardless of primary practice site.
Over time the argument has died down as the threat of a hospitalist takeover has given way to the realization that many primary care doctors prefer a practice without inpatient obligations.
Recently the American Board of Internal Medicine (ABIM) has decided to move forward with a Recognition of Focused Practice in hospital medicine (RFP-HM) certification. This designation will utilize the structure of the ABIM Maintenance of Certification (MOC) program. It will be available to those who have practiced hospital medicine at least three years, meet inpatient volume requirements, and successfully complete hospital medicine-specific Self-Evaluation Process (SEP) modules, Practice Improvement Modules (PIM) and a secure exam.
This has again raised concerns about the growth and direction of hospital medicine and the implications for internal medicine. Would this confer specialty status to hospitalists while leaving primary care doctors as the remaining generalists? Would this further fracture the field of internal medicine? Would this allow hospital-credentialing boards to preferentially allow only those with RFP-HM to practice within their walls, effectively outlawing the primary care doctor?
Having been a member of the task force that worked on RFP-HM, I can say emphatically that it is not intended to confer specialty status to hospitalists or exalt them above other general internists. Rather, it is meant to recognize that a practitioner has focused his or her practice in a manner that demonstrates greater proficiency in the practice of hospital medicine. While this denotes a presumably higher level of proficiency by RFP-HM providers, it does not mean those without it are not capable providers.
How then should we define who is a capable provider in the hospital setting? According to the Dreyfus Model of Skills Acquisition, as learners develop along the continuum from novice to beginner to competent to proficient to expert, their skills become more developed, letting them tackle more complex issues and tasks more efficiently.
For example, the novice knows that a patient with dyspnea might have pneumonia and orders a chest X-ray but little more. The competent provider realizes many other disease states can cause dyspnea and would assess for those as well, often getting bogged down in extraneous details. The proficient provider immediately focuses on the important details and determines pneumonia as the cause of the dyspnea, applying the proper treatment algorithms with a level of efficiency beyond that of the competent peer.
The expert intuitively diagnoses the pneumonia and prescribes the proper diagnostic and therapeutic evaluation. He does so while considering the patient’s immune status, the impact of the hospital’s antimicrobial resistance patterns, and the potential risks and benefits of short-course antimicrobial therapy—all through the prism of quality core measures, cost, and throughput.
In a healthcare system at best strained and by most evidence severely fractured, we can no longer accept competence as the determinant of a capable provider. Rather, we should use proficiency moving toward expertise as the measuring stick for caring for increasingly more complex patients.
The designation “hospitalist” or even RFP-HM should not determine if one is proficient to practice hospital medicine, just as the designation of primary care provider should not exclude one from practicing in the hospital. Certainly, there are practitioners able to seamlessly cross the inpatient/outpatient boundary without losing a step. However, I suspect the more likely scenario is expertise in one and at best proficiency in the other.
Levitin’s 10,000-hour threshold supports this assumption, as it would take at least 10 years to amass 10,000 hours in each practice setting. Most likely, development of expertise in one arena means mere competence in another. As exhibit A, I tremble at the thought of the mischief I would cause if I took my stethoscope to the primary care clinic.
Instead, the ethical standards of our profession should dictate that each provider determines if they meet this pursuit-of-expertise standard. Employers and credentialing boards need to raise the bar toward expertise, ensuring these thresholds are met.
In the end, hospital or clinic sites should be the domain of capable providers, regardless of their primary practice site. However, we need to recalibrate how we define a capable provider who is moving away from competence toward proficiency verging on expertise. Experience as a surrogate for expertise, more than primary practice setting or RFP-HM status, should be the major determinant for who cares for hospitalized patients. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Glass of wine in one hand and the Sept. 30 copy of Wine Spectator in the other, I intended to relax a bit—the future of hospital medicine not necessarily uppermost in my mind. But then I was struck by an article by Matt Kramer titled “10,000 hours.” In it he discusses the implications Daniel Levitin’s new book This Is Your Brain on Music: The Science of a Human Obsession (Dutton) may have for the field of wine tasting.
Levitin notes that “ten thousand hours of practice is required to achieve the level of mastery associated with being a world-class expert—in anything.” It turns out it doesn’t matter what you are trying to master.
“In study after study of composers, basketball players, fiction writers, ice skaters, concert pianists, chess players, master criminals, and what have you, this number comes up again and again,” he says. “No one has yet found a case in which true world-class expertise was accomplished in less time.” This is consistent with how we learn. “Learning requires the assimilation and consolidation of information in neural tissue,” writes Levitin. “The more experiences we have with something the stronger the memory/learning trace for the experience becomes.”
Ten thousand hours. Are you an expert in hospital medicine? Have you compiled the requisite 10,000 hours? The average hospitalist working approximately 200 shifts a year of 10 to 12 hours each would take four to five years to master the practice of hospital medicine. On the other hand, a provider spending 10 hours a week in the hospital would require 20 years to achieve the numeric equivalent of expert status.
While Levitin was discussing the impact of this calculation on music and Kramer on wine expertise, it struck me as applicable to one of the great debates surrounding hospital medicine. Early in the days of the hospitalist movement, many inside and outside the field opined as to whether hospitals should be the domain of hospitalists and clinics the domain of primary care doctors, without overlap. SHM and I proclaimed hospitals should be open to all providers, regardless of primary practice site.
Over time the argument has died down as the threat of a hospitalist takeover has given way to the realization that many primary care doctors prefer a practice without inpatient obligations.
Recently the American Board of Internal Medicine (ABIM) has decided to move forward with a Recognition of Focused Practice in hospital medicine (RFP-HM) certification. This designation will utilize the structure of the ABIM Maintenance of Certification (MOC) program. It will be available to those who have practiced hospital medicine at least three years, meet inpatient volume requirements, and successfully complete hospital medicine-specific Self-Evaluation Process (SEP) modules, Practice Improvement Modules (PIM) and a secure exam.
This has again raised concerns about the growth and direction of hospital medicine and the implications for internal medicine. Would this confer specialty status to hospitalists while leaving primary care doctors as the remaining generalists? Would this further fracture the field of internal medicine? Would this allow hospital-credentialing boards to preferentially allow only those with RFP-HM to practice within their walls, effectively outlawing the primary care doctor?
Having been a member of the task force that worked on RFP-HM, I can say emphatically that it is not intended to confer specialty status to hospitalists or exalt them above other general internists. Rather, it is meant to recognize that a practitioner has focused his or her practice in a manner that demonstrates greater proficiency in the practice of hospital medicine. While this denotes a presumably higher level of proficiency by RFP-HM providers, it does not mean those without it are not capable providers.
How then should we define who is a capable provider in the hospital setting? According to the Dreyfus Model of Skills Acquisition, as learners develop along the continuum from novice to beginner to competent to proficient to expert, their skills become more developed, letting them tackle more complex issues and tasks more efficiently.
For example, the novice knows that a patient with dyspnea might have pneumonia and orders a chest X-ray but little more. The competent provider realizes many other disease states can cause dyspnea and would assess for those as well, often getting bogged down in extraneous details. The proficient provider immediately focuses on the important details and determines pneumonia as the cause of the dyspnea, applying the proper treatment algorithms with a level of efficiency beyond that of the competent peer.
The expert intuitively diagnoses the pneumonia and prescribes the proper diagnostic and therapeutic evaluation. He does so while considering the patient’s immune status, the impact of the hospital’s antimicrobial resistance patterns, and the potential risks and benefits of short-course antimicrobial therapy—all through the prism of quality core measures, cost, and throughput.
In a healthcare system at best strained and by most evidence severely fractured, we can no longer accept competence as the determinant of a capable provider. Rather, we should use proficiency moving toward expertise as the measuring stick for caring for increasingly more complex patients.
The designation “hospitalist” or even RFP-HM should not determine if one is proficient to practice hospital medicine, just as the designation of primary care provider should not exclude one from practicing in the hospital. Certainly, there are practitioners able to seamlessly cross the inpatient/outpatient boundary without losing a step. However, I suspect the more likely scenario is expertise in one and at best proficiency in the other.
Levitin’s 10,000-hour threshold supports this assumption, as it would take at least 10 years to amass 10,000 hours in each practice setting. Most likely, development of expertise in one arena means mere competence in another. As exhibit A, I tremble at the thought of the mischief I would cause if I took my stethoscope to the primary care clinic.
Instead, the ethical standards of our profession should dictate that each provider determines if they meet this pursuit-of-expertise standard. Employers and credentialing boards need to raise the bar toward expertise, ensuring these thresholds are met.
In the end, hospital or clinic sites should be the domain of capable providers, regardless of their primary practice site. However, we need to recalibrate how we define a capable provider who is moving away from competence toward proficiency verging on expertise. Experience as a surrogate for expertise, more than primary practice setting or RFP-HM status, should be the major determinant for who cares for hospitalized patients. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Glass of wine in one hand and the Sept. 30 copy of Wine Spectator in the other, I intended to relax a bit—the future of hospital medicine not necessarily uppermost in my mind. But then I was struck by an article by Matt Kramer titled “10,000 hours.” In it he discusses the implications Daniel Levitin’s new book This Is Your Brain on Music: The Science of a Human Obsession (Dutton) may have for the field of wine tasting.
Levitin notes that “ten thousand hours of practice is required to achieve the level of mastery associated with being a world-class expert—in anything.” It turns out it doesn’t matter what you are trying to master.
“In study after study of composers, basketball players, fiction writers, ice skaters, concert pianists, chess players, master criminals, and what have you, this number comes up again and again,” he says. “No one has yet found a case in which true world-class expertise was accomplished in less time.” This is consistent with how we learn. “Learning requires the assimilation and consolidation of information in neural tissue,” writes Levitin. “The more experiences we have with something the stronger the memory/learning trace for the experience becomes.”
Ten thousand hours. Are you an expert in hospital medicine? Have you compiled the requisite 10,000 hours? The average hospitalist working approximately 200 shifts a year of 10 to 12 hours each would take four to five years to master the practice of hospital medicine. On the other hand, a provider spending 10 hours a week in the hospital would require 20 years to achieve the numeric equivalent of expert status.
While Levitin was discussing the impact of this calculation on music and Kramer on wine expertise, it struck me as applicable to one of the great debates surrounding hospital medicine. Early in the days of the hospitalist movement, many inside and outside the field opined as to whether hospitals should be the domain of hospitalists and clinics the domain of primary care doctors, without overlap. SHM and I proclaimed hospitals should be open to all providers, regardless of primary practice site.
Over time the argument has died down as the threat of a hospitalist takeover has given way to the realization that many primary care doctors prefer a practice without inpatient obligations.
Recently the American Board of Internal Medicine (ABIM) has decided to move forward with a Recognition of Focused Practice in hospital medicine (RFP-HM) certification. This designation will utilize the structure of the ABIM Maintenance of Certification (MOC) program. It will be available to those who have practiced hospital medicine at least three years, meet inpatient volume requirements, and successfully complete hospital medicine-specific Self-Evaluation Process (SEP) modules, Practice Improvement Modules (PIM) and a secure exam.
This has again raised concerns about the growth and direction of hospital medicine and the implications for internal medicine. Would this confer specialty status to hospitalists while leaving primary care doctors as the remaining generalists? Would this further fracture the field of internal medicine? Would this allow hospital-credentialing boards to preferentially allow only those with RFP-HM to practice within their walls, effectively outlawing the primary care doctor?
Having been a member of the task force that worked on RFP-HM, I can say emphatically that it is not intended to confer specialty status to hospitalists or exalt them above other general internists. Rather, it is meant to recognize that a practitioner has focused his or her practice in a manner that demonstrates greater proficiency in the practice of hospital medicine. While this denotes a presumably higher level of proficiency by RFP-HM providers, it does not mean those without it are not capable providers.
How then should we define who is a capable provider in the hospital setting? According to the Dreyfus Model of Skills Acquisition, as learners develop along the continuum from novice to beginner to competent to proficient to expert, their skills become more developed, letting them tackle more complex issues and tasks more efficiently.
For example, the novice knows that a patient with dyspnea might have pneumonia and orders a chest X-ray but little more. The competent provider realizes many other disease states can cause dyspnea and would assess for those as well, often getting bogged down in extraneous details. The proficient provider immediately focuses on the important details and determines pneumonia as the cause of the dyspnea, applying the proper treatment algorithms with a level of efficiency beyond that of the competent peer.
The expert intuitively diagnoses the pneumonia and prescribes the proper diagnostic and therapeutic evaluation. He does so while considering the patient’s immune status, the impact of the hospital’s antimicrobial resistance patterns, and the potential risks and benefits of short-course antimicrobial therapy—all through the prism of quality core measures, cost, and throughput.
In a healthcare system at best strained and by most evidence severely fractured, we can no longer accept competence as the determinant of a capable provider. Rather, we should use proficiency moving toward expertise as the measuring stick for caring for increasingly more complex patients.
The designation “hospitalist” or even RFP-HM should not determine if one is proficient to practice hospital medicine, just as the designation of primary care provider should not exclude one from practicing in the hospital. Certainly, there are practitioners able to seamlessly cross the inpatient/outpatient boundary without losing a step. However, I suspect the more likely scenario is expertise in one and at best proficiency in the other.
Levitin’s 10,000-hour threshold supports this assumption, as it would take at least 10 years to amass 10,000 hours in each practice setting. Most likely, development of expertise in one arena means mere competence in another. As exhibit A, I tremble at the thought of the mischief I would cause if I took my stethoscope to the primary care clinic.
Instead, the ethical standards of our profession should dictate that each provider determines if they meet this pursuit-of-expertise standard. Employers and credentialing boards need to raise the bar toward expertise, ensuring these thresholds are met.
In the end, hospital or clinic sites should be the domain of capable providers, regardless of their primary practice site. However, we need to recalibrate how we define a capable provider who is moving away from competence toward proficiency verging on expertise. Experience as a surrogate for expertise, more than primary practice setting or RFP-HM status, should be the major determinant for who cares for hospitalized patients. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
A Year of Progress
It’s hard to believe eight years have gone by since I came to SHM. More than that, it is strange to think of a world without hospitalists. Hospital medicine is part of the fabric of healthcare; there’s no longer a debate over whether hospitalists are good or bad. Now, the talk is about how hospitalists can help solve so many of the ills that vex our healthcare system.
This year has been an extraordinary year even by SHM standards. Witness our progress in the following areas.
ABIM Progress
In a landmark and revolutionary decision, the American Board of Internal Medicine (ABIM) recommended proceeding with a recognition of focused practice (RFP) in hospital medicine as an option in its maintenance of certification (MOC).
This is the culmination of a strategy SHM laid out three years ago. SHM is working with ABIM to continue to make the MOC process meaningful to hospitalists as the ABIM recommendations wend their way through the American Board of Medical Specialties. SHM continues to reach out to the pediatric and family medicine boards so the RFP can be available to all hospitalists.
JHM Listed
In its first year of publication, the Journal of Hospital Medicine (JHM) has been included in PubMed, the National Institutes of Health online archive of life science journals. JHM now resides among other established journals, fielding a marked increased in submissions for publication.
Quality
SHM received its third consecutive grant from the John A. Hartford Foundation, this one for $1.4 million over three years to develop interventions to improve care transitions for older adults at discharge.
As part of our work to improve quality for our nation’s seniors, SHM is developing discharge-planning tools and implementation strategies to limit the voltage drop in care at discharge. Hartford’s support means funders see that hospitalists, with SHM support, improve quality at their hospitals. SHM has become a leader in discharge planning tools and is helping set standards for transitions of care.
To help give hospitalists tools and resources to effect change on the front lines, SHM continues to develop online resource rooms and unique strategies such as mentored implementation.
We also have several hospitalist leaders on key panels at the National Quality Forum (NQF). The American Medical Association’s Physician Consortium on Practice Improvement has asked SHM to take the lead in forming a coalition for setting transitions-of-care measurements.
When the Institute for Healthcare Improvement needed a physician group to join the announcement of its 5 Million Lives Campaign, it reached out to SHM. President Rusty Holman took the stage to support the initiative, which intends to protect 5 million patients from incidents of medical harm over the next two years.
Further, the Joint Commission on Accreditation of Healthcare Organizations asked SHM to co-sponsor its medication reconciliation workgroup. Lastly, SHM continues to get significant visibility for hospitalists with our leadership of the deep-vein thrombosis awareness coalition of more than 35 organizations.
Annual Meeting
In May, SHM took over the Gaylord Texan in Dallas with professional meeting staging that rivaled older, larger organizations. With banners, Jumbotrons, and devices projecting the SHM logo, we transformed the Gaylord into a “hospitalist city.” We treated the nearly 1,200 attendees to three superlative speakers:
- David Brailer, MD, national coordinator for health information technology, United States Department of Health and Human Services;
- Jonathan Perlin, MD, former undersecretary for health at the Veterans Health Administration and now chief medical officer and senior vice president of quality for Hospital Corporation of America in Nashville; and
- Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California, San Francisco.
And, we had our largest poster session ever, with more than 200 submissions, and our largest exhibit hall. We plan to take it up a notch in San Diego in April.
Advocacy and Policy
Our presence in Washington, D.C., allows us to be active in Medicare payment reform. SHM leadership has met with senior staff at MedPAC, the organization that makes recommendations to the Centers for Medicare and Medicaid Services and Congress. MedPAC is interested in working with SHM as Medicare attempts to move away from paying for just visits and procedures and toward reimbursement strategies that drive performance and efficiency.
Current, Future Initiatives
In June, SHM forged a partnership with the Society of General Internal Medicine (SGIM) and the Association of Chiefs of General Internal Medicine to hold an academic summit to develop strategies for academic hospitalists to have a strong and sustainable career in teaching, training, and research in hospital medicine. When the Alliance for Academic Internal Medicine developed its proposal to redesign internal medicine training, SHM took the lead in crafting the hospitalist response.
In July, we joined the SGIM and American College of Physicians to hold a consensus conference on transitions of care. This coalition of more than 25 organizations produced a statement as the basis for future standards and measurements. Also in July, SHM worked with key leaders in emergency medicine and others to redefine the management and opportunities in observation units.
We held a multidisciplinary workforce summit in November to examine the challenges and solutions in growing hospital medicine from 20,000 to 40,000 or more physicians.
Diversity
While at times we may seem to focus more on internal-medicine-trained hospitalists, who make up more than 80% of the field, SHM continues to include hospitalists in family medicine and pediatrics, among other specialties. We also are home to nonphysician providers and physician assistants. We are working to support academic hospitalists, small groups, and multistate companies. In our toughest tightrope walk, SHM continues to be relevant and supportive of labor and management in hospital medicine.
Looking to 2008
The growth and influence of hospital medicine is relentless. Maybe 2008 is the year we will see hospitalists practicing in more than 3,000 hospitals or see the specialty grow to more than 25,000 hospitalists. One thing is for sure: SHM, with your suggestions, ideas, and energy, will be on the front lines with you, supporting and advocating a better healthcare system. TH
Dr. Wellikson is CEO of SHM.
It’s hard to believe eight years have gone by since I came to SHM. More than that, it is strange to think of a world without hospitalists. Hospital medicine is part of the fabric of healthcare; there’s no longer a debate over whether hospitalists are good or bad. Now, the talk is about how hospitalists can help solve so many of the ills that vex our healthcare system.
This year has been an extraordinary year even by SHM standards. Witness our progress in the following areas.
ABIM Progress
In a landmark and revolutionary decision, the American Board of Internal Medicine (ABIM) recommended proceeding with a recognition of focused practice (RFP) in hospital medicine as an option in its maintenance of certification (MOC).
This is the culmination of a strategy SHM laid out three years ago. SHM is working with ABIM to continue to make the MOC process meaningful to hospitalists as the ABIM recommendations wend their way through the American Board of Medical Specialties. SHM continues to reach out to the pediatric and family medicine boards so the RFP can be available to all hospitalists.
JHM Listed
In its first year of publication, the Journal of Hospital Medicine (JHM) has been included in PubMed, the National Institutes of Health online archive of life science journals. JHM now resides among other established journals, fielding a marked increased in submissions for publication.
Quality
SHM received its third consecutive grant from the John A. Hartford Foundation, this one for $1.4 million over three years to develop interventions to improve care transitions for older adults at discharge.
As part of our work to improve quality for our nation’s seniors, SHM is developing discharge-planning tools and implementation strategies to limit the voltage drop in care at discharge. Hartford’s support means funders see that hospitalists, with SHM support, improve quality at their hospitals. SHM has become a leader in discharge planning tools and is helping set standards for transitions of care.
To help give hospitalists tools and resources to effect change on the front lines, SHM continues to develop online resource rooms and unique strategies such as mentored implementation.
We also have several hospitalist leaders on key panels at the National Quality Forum (NQF). The American Medical Association’s Physician Consortium on Practice Improvement has asked SHM to take the lead in forming a coalition for setting transitions-of-care measurements.
When the Institute for Healthcare Improvement needed a physician group to join the announcement of its 5 Million Lives Campaign, it reached out to SHM. President Rusty Holman took the stage to support the initiative, which intends to protect 5 million patients from incidents of medical harm over the next two years.
Further, the Joint Commission on Accreditation of Healthcare Organizations asked SHM to co-sponsor its medication reconciliation workgroup. Lastly, SHM continues to get significant visibility for hospitalists with our leadership of the deep-vein thrombosis awareness coalition of more than 35 organizations.
Annual Meeting
In May, SHM took over the Gaylord Texan in Dallas with professional meeting staging that rivaled older, larger organizations. With banners, Jumbotrons, and devices projecting the SHM logo, we transformed the Gaylord into a “hospitalist city.” We treated the nearly 1,200 attendees to three superlative speakers:
- David Brailer, MD, national coordinator for health information technology, United States Department of Health and Human Services;
- Jonathan Perlin, MD, former undersecretary for health at the Veterans Health Administration and now chief medical officer and senior vice president of quality for Hospital Corporation of America in Nashville; and
- Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California, San Francisco.
And, we had our largest poster session ever, with more than 200 submissions, and our largest exhibit hall. We plan to take it up a notch in San Diego in April.
Advocacy and Policy
Our presence in Washington, D.C., allows us to be active in Medicare payment reform. SHM leadership has met with senior staff at MedPAC, the organization that makes recommendations to the Centers for Medicare and Medicaid Services and Congress. MedPAC is interested in working with SHM as Medicare attempts to move away from paying for just visits and procedures and toward reimbursement strategies that drive performance and efficiency.
Current, Future Initiatives
In June, SHM forged a partnership with the Society of General Internal Medicine (SGIM) and the Association of Chiefs of General Internal Medicine to hold an academic summit to develop strategies for academic hospitalists to have a strong and sustainable career in teaching, training, and research in hospital medicine. When the Alliance for Academic Internal Medicine developed its proposal to redesign internal medicine training, SHM took the lead in crafting the hospitalist response.
In July, we joined the SGIM and American College of Physicians to hold a consensus conference on transitions of care. This coalition of more than 25 organizations produced a statement as the basis for future standards and measurements. Also in July, SHM worked with key leaders in emergency medicine and others to redefine the management and opportunities in observation units.
We held a multidisciplinary workforce summit in November to examine the challenges and solutions in growing hospital medicine from 20,000 to 40,000 or more physicians.
Diversity
While at times we may seem to focus more on internal-medicine-trained hospitalists, who make up more than 80% of the field, SHM continues to include hospitalists in family medicine and pediatrics, among other specialties. We also are home to nonphysician providers and physician assistants. We are working to support academic hospitalists, small groups, and multistate companies. In our toughest tightrope walk, SHM continues to be relevant and supportive of labor and management in hospital medicine.
Looking to 2008
The growth and influence of hospital medicine is relentless. Maybe 2008 is the year we will see hospitalists practicing in more than 3,000 hospitals or see the specialty grow to more than 25,000 hospitalists. One thing is for sure: SHM, with your suggestions, ideas, and energy, will be on the front lines with you, supporting and advocating a better healthcare system. TH
Dr. Wellikson is CEO of SHM.
It’s hard to believe eight years have gone by since I came to SHM. More than that, it is strange to think of a world without hospitalists. Hospital medicine is part of the fabric of healthcare; there’s no longer a debate over whether hospitalists are good or bad. Now, the talk is about how hospitalists can help solve so many of the ills that vex our healthcare system.
This year has been an extraordinary year even by SHM standards. Witness our progress in the following areas.
ABIM Progress
In a landmark and revolutionary decision, the American Board of Internal Medicine (ABIM) recommended proceeding with a recognition of focused practice (RFP) in hospital medicine as an option in its maintenance of certification (MOC).
This is the culmination of a strategy SHM laid out three years ago. SHM is working with ABIM to continue to make the MOC process meaningful to hospitalists as the ABIM recommendations wend their way through the American Board of Medical Specialties. SHM continues to reach out to the pediatric and family medicine boards so the RFP can be available to all hospitalists.
JHM Listed
In its first year of publication, the Journal of Hospital Medicine (JHM) has been included in PubMed, the National Institutes of Health online archive of life science journals. JHM now resides among other established journals, fielding a marked increased in submissions for publication.
Quality
SHM received its third consecutive grant from the John A. Hartford Foundation, this one for $1.4 million over three years to develop interventions to improve care transitions for older adults at discharge.
As part of our work to improve quality for our nation’s seniors, SHM is developing discharge-planning tools and implementation strategies to limit the voltage drop in care at discharge. Hartford’s support means funders see that hospitalists, with SHM support, improve quality at their hospitals. SHM has become a leader in discharge planning tools and is helping set standards for transitions of care.
To help give hospitalists tools and resources to effect change on the front lines, SHM continues to develop online resource rooms and unique strategies such as mentored implementation.
We also have several hospitalist leaders on key panels at the National Quality Forum (NQF). The American Medical Association’s Physician Consortium on Practice Improvement has asked SHM to take the lead in forming a coalition for setting transitions-of-care measurements.
When the Institute for Healthcare Improvement needed a physician group to join the announcement of its 5 Million Lives Campaign, it reached out to SHM. President Rusty Holman took the stage to support the initiative, which intends to protect 5 million patients from incidents of medical harm over the next two years.
Further, the Joint Commission on Accreditation of Healthcare Organizations asked SHM to co-sponsor its medication reconciliation workgroup. Lastly, SHM continues to get significant visibility for hospitalists with our leadership of the deep-vein thrombosis awareness coalition of more than 35 organizations.
Annual Meeting
In May, SHM took over the Gaylord Texan in Dallas with professional meeting staging that rivaled older, larger organizations. With banners, Jumbotrons, and devices projecting the SHM logo, we transformed the Gaylord into a “hospitalist city.” We treated the nearly 1,200 attendees to three superlative speakers:
- David Brailer, MD, national coordinator for health information technology, United States Department of Health and Human Services;
- Jonathan Perlin, MD, former undersecretary for health at the Veterans Health Administration and now chief medical officer and senior vice president of quality for Hospital Corporation of America in Nashville; and
- Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California, San Francisco.
And, we had our largest poster session ever, with more than 200 submissions, and our largest exhibit hall. We plan to take it up a notch in San Diego in April.
Advocacy and Policy
Our presence in Washington, D.C., allows us to be active in Medicare payment reform. SHM leadership has met with senior staff at MedPAC, the organization that makes recommendations to the Centers for Medicare and Medicaid Services and Congress. MedPAC is interested in working with SHM as Medicare attempts to move away from paying for just visits and procedures and toward reimbursement strategies that drive performance and efficiency.
Current, Future Initiatives
In June, SHM forged a partnership with the Society of General Internal Medicine (SGIM) and the Association of Chiefs of General Internal Medicine to hold an academic summit to develop strategies for academic hospitalists to have a strong and sustainable career in teaching, training, and research in hospital medicine. When the Alliance for Academic Internal Medicine developed its proposal to redesign internal medicine training, SHM took the lead in crafting the hospitalist response.
In July, we joined the SGIM and American College of Physicians to hold a consensus conference on transitions of care. This coalition of more than 25 organizations produced a statement as the basis for future standards and measurements. Also in July, SHM worked with key leaders in emergency medicine and others to redefine the management and opportunities in observation units.
We held a multidisciplinary workforce summit in November to examine the challenges and solutions in growing hospital medicine from 20,000 to 40,000 or more physicians.
Diversity
While at times we may seem to focus more on internal-medicine-trained hospitalists, who make up more than 80% of the field, SHM continues to include hospitalists in family medicine and pediatrics, among other specialties. We also are home to nonphysician providers and physician assistants. We are working to support academic hospitalists, small groups, and multistate companies. In our toughest tightrope walk, SHM continues to be relevant and supportive of labor and management in hospital medicine.
Looking to 2008
The growth and influence of hospital medicine is relentless. Maybe 2008 is the year we will see hospitalists practicing in more than 3,000 hospitals or see the specialty grow to more than 25,000 hospitalists. One thing is for sure: SHM, with your suggestions, ideas, and energy, will be on the front lines with you, supporting and advocating a better healthcare system. TH
Dr. Wellikson is CEO of SHM.
Care & Prayer
Charles Petit, MD, like many healthcare professionals, spends a good deal of time addressing the needs of the underprivileged. Since 2004, he has taken up the cause of the indigenous Miskito Indians of Puerto Lempira, Honduras. He is putting his own money into developing a modern clinic and international medicine program there.
But medicine isn’t his only mission. Dr. Petit, 56, a hospitalist at Palmetto Health Care’s Richland Memorial Hospital in Columbia, S.C., is also an Episcopal priest.
He joined Palmetto Health Senior Care as its first medical director in 1988 and reconnected with the group in 2004—not in his previous role as an office-based physician but as a hospitalist. In between those stints he pursued his ordination and medical missionary work in Africa and Latin America.
As a physician, Dr. Petit says he feels God’s presence at each patient’s bedside. Years ago he wondered how to handle that.
To deepen his connection between medicine and spirituality, he lived in a Christian intentional community in Indiana, Pa., from 1981 to 1988. Gradually, his views on medicine and spirituality crystallized.
“How does God do what he does?” Dr. Petit wondered. “Can medicine put Him to the test? I have seen that prayer works, including a patient miraculously healed of metastatic ovarian cancer. But God isn’t a vending machine. You don’t drop in a prayer and get a healing back.”
The Second Calling
Recognizing he needed something more to integrate medicine and spirituality, Dr. Petit sought a firmer grounding in religious studies.
He moved to Simpsonville, S.C., in 1995 and entered the Episcopal seminary, working as an emergency department doctor to pay the bills. Later, he earned a master’s of divinity from the University of the South in Sewanee, Tenn., in 2003.
His spiritual “internship” was a transitional deaconship from 2003 to 2005, under the Rev. Michael Flanagan, rector at Simpsonville’s Holy Cross Episcopal Church. Both had dual vocations—Flanagan was an engineer who sold electrical equipment for 10 years before ordination. Prior to meeting Dr. Petit, Flanagan was leery of the doctor’s ability to balance pastoral and medical duties.
“Would he be a doctor/priest?” Flanagan wondered. “A priest/doctor? His desire was to meld both and he did. Medicine and spirituality are both in his blood. He sees both as calls from God and connects medicine with spirituality into a holistic view of each person.” He says Dr. Petit “seems to know everything and sucks up knowledge, which he wants to share. He loves being the doctor and having the knowledge to fix the patient’s problem.”
While Dr. Petit keeps his hospitalist and priest roles mostly separate, working with elderly patients sometimes requires the skills of both disciplines. At Richland he wears a clerical collar on pastoral rounds. If a family or patient asks him to pray with them or discuss life’s ending, he does. He has conducted funerals for his own and colleagues’ patients.
“It’s a very powerful experience being both a priest and a doctor,” he says. “I grow so close to the patients and their families that it is natural for me to serve in both roles.”
Honduras Mission
As a seminarian, Dr. Petit took medical mission trips and briefly supported an African orphanage, looking for a cause to call his own. Until his first trip to Puerto Lempira, a village on the Miskito Coast of the Atlantic Ocean.
The abject poverty and medical needs of the Miskito Indians there pulled at him. Early on he enlisted the help of Ennis Whiddon, a builder and Holy Cross parishioner. Whiddon, who usually accompanies Dr. Petit to Puerto Lempira, says of his friend: “I knew him as [an emergency department] doctor first. Then I realized his extraordinary spiritual commitment. I went to Puerto Lempira on his first mission trip and I asked myself why anyone would want to be there, but I knew Chuck couldn’t bear not to be there. I also knew he wasn’t just going to give people two aspirins, come home and pray for them.”
Dr. Petit returns to Puerto Lempira three or four times a year with a team of doctors, seeing several hundred patients a day. During one two-week stint he dispensed $200,000 worth of medication he cadged from drug companies for $600 out of his pocket to rid the town’s youngsters of debilitating parasites.
Dr. Petit works with a Miskito nurse who runs their rudimentary clinic in his absence. He also uses hyperbaric medicine to treat divers whose crippling injuries result from diving deeply using pressurized oxygen tanks and rising too quickly to the surface.
“You wouldn’t believe the indescribably poor facilities we found there,” Whiddon says of the town’s clinic. “You wouldn’t have your dog treated there if you loved your dog.”
Last year Dr. Petit ratcheted up his commitment to Puerto Lempira, dreaming of building a permanent clinic there.
He decided to use his money to buy land to build a clinic, but got stonewalled by a stubborn local bureaucracy.
Then Andres Leone, a like-minded younger doctor who was part of the mission trip, stepped in with handy language and cultural skills. Leone who had attended medical school in Ecuador, is a Lutheran seminarian, and is completing a geriatric hospitalist fellowship at Palmetto Healthcare.
“We were in Puerto Lempira for two weeks and visited the mayor several times to buy land,” Dr. Leone explains. “He said the price was $600,000, which was ridiculous. In the town I overheard some conversations, which led to us meeting the 77-year-old daughter of missionaries. She sold us some of her land and even donated money to help build the clinic, which will be dedicated in her name.”
Thinking big, Dr. Petit is adding an apartment complete with air conditioning and a modern bathroom to the clinic’s blueprint, to attract residents in a to-be-formed international medicine program. As an assistant professor of family medicine at the University of South Carolina’s (USC) School of Medicine, he intends to oversee those residents.
Just back from Puerto Lempira, Dr. Petit finalized the clinic’s design, lined up local workers to figure out how to make concrete building blocks with native materials, and met with Anglican bishop the Right Rev. Lloyd E. Allen, bolstering support for the new clinic and the possibility of HIV outreach. Side by side with Honduran and Cuban doctors, Dr. Petit treated hundreds of Puerto Lempira’s villagers every day.
Back in the Hospital
Dr. Petit always wanted to be a doctor. Although his father suggested he become a hospital orderly, Dr. Petit knew being a physician was his calling, graduating from the University of West Virginia School of Medicine (Morgantown) family medicine program in 1978.
He enjoys hospital medicine as a holistic approach to caring for patients, consistent with his work early in his career.
An earlier 10-year stint as a hospitalist at HealthSouth Rehabilitation Hospital, also at USC, involved teaching residents and students rotating through the hospital, as well as a consultative service for neurosurgical patients at Richland. At Wheeling Hospital early in his career he became comfortable as a generalist, covering intensive care, assisting in surgery, and delivering many babies.
Being a hospitalist keeps that spirit alive. “It gives me the gift of time to spend with patients,” he says. “I try not to tie frail elderly patients down with IVs, Foley catheters, EKG monitors, worries that eating a leafy green vegetable will react badly with their Coumadin [warfarin], and polypharmacy.”
He discusses advanced directives, palliative care, and how the elderly in fragile condition can maintain as much freedom as possible. The hospital medicine group’s accommodating scheduling allows time for his parish duties and medical mission trips.
The group’s medical director, Victor Hirth, MD, describes Dr. Petit as a borderline workaholic who’s always looking for ways to make things better for the practice and patients. “The patients absolutely love him because he takes time to sit and talk to them,” says Dr. Hirth.
Dr. Petit also embraces new technologies. “Our [electronic medical record] makes working with my outpatient colleagues smooth and straightforward.” He relies on a personal digital device assistant for updates on clinical guidelines and optimal drug doses for elderly patients. Integrating a healer’s touch with new technology he says: “While medicine is a science, it’s still an art, a ministry, and a gift.”
What’s Next?
Back in South Carolina, Dr. Petit has picked up his hospitalist and pastoral responsibilities without missing a beat. He looks forward to building the palliative care consulting service and intends to launch a nonprofit corporation to receive donations to support the Puerto Lempira clinic’s construction.
He is planning more mission trips. He thrives on the work. Infused with boundless energy, he’s always looking for more to do.
“I love what I do,” he concludes. “If I felt much better they’d charge me an amusement tax.” TH
Marlene Piturro is a medical writer based in New York.
Charles Petit, MD, like many healthcare professionals, spends a good deal of time addressing the needs of the underprivileged. Since 2004, he has taken up the cause of the indigenous Miskito Indians of Puerto Lempira, Honduras. He is putting his own money into developing a modern clinic and international medicine program there.
But medicine isn’t his only mission. Dr. Petit, 56, a hospitalist at Palmetto Health Care’s Richland Memorial Hospital in Columbia, S.C., is also an Episcopal priest.
He joined Palmetto Health Senior Care as its first medical director in 1988 and reconnected with the group in 2004—not in his previous role as an office-based physician but as a hospitalist. In between those stints he pursued his ordination and medical missionary work in Africa and Latin America.
As a physician, Dr. Petit says he feels God’s presence at each patient’s bedside. Years ago he wondered how to handle that.
To deepen his connection between medicine and spirituality, he lived in a Christian intentional community in Indiana, Pa., from 1981 to 1988. Gradually, his views on medicine and spirituality crystallized.
“How does God do what he does?” Dr. Petit wondered. “Can medicine put Him to the test? I have seen that prayer works, including a patient miraculously healed of metastatic ovarian cancer. But God isn’t a vending machine. You don’t drop in a prayer and get a healing back.”
The Second Calling
Recognizing he needed something more to integrate medicine and spirituality, Dr. Petit sought a firmer grounding in religious studies.
He moved to Simpsonville, S.C., in 1995 and entered the Episcopal seminary, working as an emergency department doctor to pay the bills. Later, he earned a master’s of divinity from the University of the South in Sewanee, Tenn., in 2003.
His spiritual “internship” was a transitional deaconship from 2003 to 2005, under the Rev. Michael Flanagan, rector at Simpsonville’s Holy Cross Episcopal Church. Both had dual vocations—Flanagan was an engineer who sold electrical equipment for 10 years before ordination. Prior to meeting Dr. Petit, Flanagan was leery of the doctor’s ability to balance pastoral and medical duties.
“Would he be a doctor/priest?” Flanagan wondered. “A priest/doctor? His desire was to meld both and he did. Medicine and spirituality are both in his blood. He sees both as calls from God and connects medicine with spirituality into a holistic view of each person.” He says Dr. Petit “seems to know everything and sucks up knowledge, which he wants to share. He loves being the doctor and having the knowledge to fix the patient’s problem.”
While Dr. Petit keeps his hospitalist and priest roles mostly separate, working with elderly patients sometimes requires the skills of both disciplines. At Richland he wears a clerical collar on pastoral rounds. If a family or patient asks him to pray with them or discuss life’s ending, he does. He has conducted funerals for his own and colleagues’ patients.
“It’s a very powerful experience being both a priest and a doctor,” he says. “I grow so close to the patients and their families that it is natural for me to serve in both roles.”
Honduras Mission
As a seminarian, Dr. Petit took medical mission trips and briefly supported an African orphanage, looking for a cause to call his own. Until his first trip to Puerto Lempira, a village on the Miskito Coast of the Atlantic Ocean.
The abject poverty and medical needs of the Miskito Indians there pulled at him. Early on he enlisted the help of Ennis Whiddon, a builder and Holy Cross parishioner. Whiddon, who usually accompanies Dr. Petit to Puerto Lempira, says of his friend: “I knew him as [an emergency department] doctor first. Then I realized his extraordinary spiritual commitment. I went to Puerto Lempira on his first mission trip and I asked myself why anyone would want to be there, but I knew Chuck couldn’t bear not to be there. I also knew he wasn’t just going to give people two aspirins, come home and pray for them.”
Dr. Petit returns to Puerto Lempira three or four times a year with a team of doctors, seeing several hundred patients a day. During one two-week stint he dispensed $200,000 worth of medication he cadged from drug companies for $600 out of his pocket to rid the town’s youngsters of debilitating parasites.
Dr. Petit works with a Miskito nurse who runs their rudimentary clinic in his absence. He also uses hyperbaric medicine to treat divers whose crippling injuries result from diving deeply using pressurized oxygen tanks and rising too quickly to the surface.
“You wouldn’t believe the indescribably poor facilities we found there,” Whiddon says of the town’s clinic. “You wouldn’t have your dog treated there if you loved your dog.”
Last year Dr. Petit ratcheted up his commitment to Puerto Lempira, dreaming of building a permanent clinic there.
He decided to use his money to buy land to build a clinic, but got stonewalled by a stubborn local bureaucracy.
Then Andres Leone, a like-minded younger doctor who was part of the mission trip, stepped in with handy language and cultural skills. Leone who had attended medical school in Ecuador, is a Lutheran seminarian, and is completing a geriatric hospitalist fellowship at Palmetto Healthcare.
“We were in Puerto Lempira for two weeks and visited the mayor several times to buy land,” Dr. Leone explains. “He said the price was $600,000, which was ridiculous. In the town I overheard some conversations, which led to us meeting the 77-year-old daughter of missionaries. She sold us some of her land and even donated money to help build the clinic, which will be dedicated in her name.”
Thinking big, Dr. Petit is adding an apartment complete with air conditioning and a modern bathroom to the clinic’s blueprint, to attract residents in a to-be-formed international medicine program. As an assistant professor of family medicine at the University of South Carolina’s (USC) School of Medicine, he intends to oversee those residents.
Just back from Puerto Lempira, Dr. Petit finalized the clinic’s design, lined up local workers to figure out how to make concrete building blocks with native materials, and met with Anglican bishop the Right Rev. Lloyd E. Allen, bolstering support for the new clinic and the possibility of HIV outreach. Side by side with Honduran and Cuban doctors, Dr. Petit treated hundreds of Puerto Lempira’s villagers every day.
Back in the Hospital
Dr. Petit always wanted to be a doctor. Although his father suggested he become a hospital orderly, Dr. Petit knew being a physician was his calling, graduating from the University of West Virginia School of Medicine (Morgantown) family medicine program in 1978.
He enjoys hospital medicine as a holistic approach to caring for patients, consistent with his work early in his career.
An earlier 10-year stint as a hospitalist at HealthSouth Rehabilitation Hospital, also at USC, involved teaching residents and students rotating through the hospital, as well as a consultative service for neurosurgical patients at Richland. At Wheeling Hospital early in his career he became comfortable as a generalist, covering intensive care, assisting in surgery, and delivering many babies.
Being a hospitalist keeps that spirit alive. “It gives me the gift of time to spend with patients,” he says. “I try not to tie frail elderly patients down with IVs, Foley catheters, EKG monitors, worries that eating a leafy green vegetable will react badly with their Coumadin [warfarin], and polypharmacy.”
He discusses advanced directives, palliative care, and how the elderly in fragile condition can maintain as much freedom as possible. The hospital medicine group’s accommodating scheduling allows time for his parish duties and medical mission trips.
The group’s medical director, Victor Hirth, MD, describes Dr. Petit as a borderline workaholic who’s always looking for ways to make things better for the practice and patients. “The patients absolutely love him because he takes time to sit and talk to them,” says Dr. Hirth.
Dr. Petit also embraces new technologies. “Our [electronic medical record] makes working with my outpatient colleagues smooth and straightforward.” He relies on a personal digital device assistant for updates on clinical guidelines and optimal drug doses for elderly patients. Integrating a healer’s touch with new technology he says: “While medicine is a science, it’s still an art, a ministry, and a gift.”
What’s Next?
Back in South Carolina, Dr. Petit has picked up his hospitalist and pastoral responsibilities without missing a beat. He looks forward to building the palliative care consulting service and intends to launch a nonprofit corporation to receive donations to support the Puerto Lempira clinic’s construction.
He is planning more mission trips. He thrives on the work. Infused with boundless energy, he’s always looking for more to do.
“I love what I do,” he concludes. “If I felt much better they’d charge me an amusement tax.” TH
Marlene Piturro is a medical writer based in New York.
Charles Petit, MD, like many healthcare professionals, spends a good deal of time addressing the needs of the underprivileged. Since 2004, he has taken up the cause of the indigenous Miskito Indians of Puerto Lempira, Honduras. He is putting his own money into developing a modern clinic and international medicine program there.
But medicine isn’t his only mission. Dr. Petit, 56, a hospitalist at Palmetto Health Care’s Richland Memorial Hospital in Columbia, S.C., is also an Episcopal priest.
He joined Palmetto Health Senior Care as its first medical director in 1988 and reconnected with the group in 2004—not in his previous role as an office-based physician but as a hospitalist. In between those stints he pursued his ordination and medical missionary work in Africa and Latin America.
As a physician, Dr. Petit says he feels God’s presence at each patient’s bedside. Years ago he wondered how to handle that.
To deepen his connection between medicine and spirituality, he lived in a Christian intentional community in Indiana, Pa., from 1981 to 1988. Gradually, his views on medicine and spirituality crystallized.
“How does God do what he does?” Dr. Petit wondered. “Can medicine put Him to the test? I have seen that prayer works, including a patient miraculously healed of metastatic ovarian cancer. But God isn’t a vending machine. You don’t drop in a prayer and get a healing back.”
The Second Calling
Recognizing he needed something more to integrate medicine and spirituality, Dr. Petit sought a firmer grounding in religious studies.
He moved to Simpsonville, S.C., in 1995 and entered the Episcopal seminary, working as an emergency department doctor to pay the bills. Later, he earned a master’s of divinity from the University of the South in Sewanee, Tenn., in 2003.
His spiritual “internship” was a transitional deaconship from 2003 to 2005, under the Rev. Michael Flanagan, rector at Simpsonville’s Holy Cross Episcopal Church. Both had dual vocations—Flanagan was an engineer who sold electrical equipment for 10 years before ordination. Prior to meeting Dr. Petit, Flanagan was leery of the doctor’s ability to balance pastoral and medical duties.
“Would he be a doctor/priest?” Flanagan wondered. “A priest/doctor? His desire was to meld both and he did. Medicine and spirituality are both in his blood. He sees both as calls from God and connects medicine with spirituality into a holistic view of each person.” He says Dr. Petit “seems to know everything and sucks up knowledge, which he wants to share. He loves being the doctor and having the knowledge to fix the patient’s problem.”
While Dr. Petit keeps his hospitalist and priest roles mostly separate, working with elderly patients sometimes requires the skills of both disciplines. At Richland he wears a clerical collar on pastoral rounds. If a family or patient asks him to pray with them or discuss life’s ending, he does. He has conducted funerals for his own and colleagues’ patients.
“It’s a very powerful experience being both a priest and a doctor,” he says. “I grow so close to the patients and their families that it is natural for me to serve in both roles.”
Honduras Mission
As a seminarian, Dr. Petit took medical mission trips and briefly supported an African orphanage, looking for a cause to call his own. Until his first trip to Puerto Lempira, a village on the Miskito Coast of the Atlantic Ocean.
The abject poverty and medical needs of the Miskito Indians there pulled at him. Early on he enlisted the help of Ennis Whiddon, a builder and Holy Cross parishioner. Whiddon, who usually accompanies Dr. Petit to Puerto Lempira, says of his friend: “I knew him as [an emergency department] doctor first. Then I realized his extraordinary spiritual commitment. I went to Puerto Lempira on his first mission trip and I asked myself why anyone would want to be there, but I knew Chuck couldn’t bear not to be there. I also knew he wasn’t just going to give people two aspirins, come home and pray for them.”
Dr. Petit returns to Puerto Lempira three or four times a year with a team of doctors, seeing several hundred patients a day. During one two-week stint he dispensed $200,000 worth of medication he cadged from drug companies for $600 out of his pocket to rid the town’s youngsters of debilitating parasites.
Dr. Petit works with a Miskito nurse who runs their rudimentary clinic in his absence. He also uses hyperbaric medicine to treat divers whose crippling injuries result from diving deeply using pressurized oxygen tanks and rising too quickly to the surface.
“You wouldn’t believe the indescribably poor facilities we found there,” Whiddon says of the town’s clinic. “You wouldn’t have your dog treated there if you loved your dog.”
Last year Dr. Petit ratcheted up his commitment to Puerto Lempira, dreaming of building a permanent clinic there.
He decided to use his money to buy land to build a clinic, but got stonewalled by a stubborn local bureaucracy.
Then Andres Leone, a like-minded younger doctor who was part of the mission trip, stepped in with handy language and cultural skills. Leone who had attended medical school in Ecuador, is a Lutheran seminarian, and is completing a geriatric hospitalist fellowship at Palmetto Healthcare.
“We were in Puerto Lempira for two weeks and visited the mayor several times to buy land,” Dr. Leone explains. “He said the price was $600,000, which was ridiculous. In the town I overheard some conversations, which led to us meeting the 77-year-old daughter of missionaries. She sold us some of her land and even donated money to help build the clinic, which will be dedicated in her name.”
Thinking big, Dr. Petit is adding an apartment complete with air conditioning and a modern bathroom to the clinic’s blueprint, to attract residents in a to-be-formed international medicine program. As an assistant professor of family medicine at the University of South Carolina’s (USC) School of Medicine, he intends to oversee those residents.
Just back from Puerto Lempira, Dr. Petit finalized the clinic’s design, lined up local workers to figure out how to make concrete building blocks with native materials, and met with Anglican bishop the Right Rev. Lloyd E. Allen, bolstering support for the new clinic and the possibility of HIV outreach. Side by side with Honduran and Cuban doctors, Dr. Petit treated hundreds of Puerto Lempira’s villagers every day.
Back in the Hospital
Dr. Petit always wanted to be a doctor. Although his father suggested he become a hospital orderly, Dr. Petit knew being a physician was his calling, graduating from the University of West Virginia School of Medicine (Morgantown) family medicine program in 1978.
He enjoys hospital medicine as a holistic approach to caring for patients, consistent with his work early in his career.
An earlier 10-year stint as a hospitalist at HealthSouth Rehabilitation Hospital, also at USC, involved teaching residents and students rotating through the hospital, as well as a consultative service for neurosurgical patients at Richland. At Wheeling Hospital early in his career he became comfortable as a generalist, covering intensive care, assisting in surgery, and delivering many babies.
Being a hospitalist keeps that spirit alive. “It gives me the gift of time to spend with patients,” he says. “I try not to tie frail elderly patients down with IVs, Foley catheters, EKG monitors, worries that eating a leafy green vegetable will react badly with their Coumadin [warfarin], and polypharmacy.”
He discusses advanced directives, palliative care, and how the elderly in fragile condition can maintain as much freedom as possible. The hospital medicine group’s accommodating scheduling allows time for his parish duties and medical mission trips.
The group’s medical director, Victor Hirth, MD, describes Dr. Petit as a borderline workaholic who’s always looking for ways to make things better for the practice and patients. “The patients absolutely love him because he takes time to sit and talk to them,” says Dr. Hirth.
Dr. Petit also embraces new technologies. “Our [electronic medical record] makes working with my outpatient colleagues smooth and straightforward.” He relies on a personal digital device assistant for updates on clinical guidelines and optimal drug doses for elderly patients. Integrating a healer’s touch with new technology he says: “While medicine is a science, it’s still an art, a ministry, and a gift.”
What’s Next?
Back in South Carolina, Dr. Petit has picked up his hospitalist and pastoral responsibilities without missing a beat. He looks forward to building the palliative care consulting service and intends to launch a nonprofit corporation to receive donations to support the Puerto Lempira clinic’s construction.
He is planning more mission trips. He thrives on the work. Infused with boundless energy, he’s always looking for more to do.
“I love what I do,” he concludes. “If I felt much better they’d charge me an amusement tax.” TH
Marlene Piturro is a medical writer based in New York.
Do feeding tubes improve outcomes in patients with dementia?
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Patient Proxies
In the best interests of the patient. In accordance with the patient’s wishes. Preserving patient autonomy. These concepts are at the core of modern medical decision-making.
Traditionally medical decisions are made by hospitalists and communicated to patients. This approach has shifted to an emphasis on patient autonomy and input in decision-making.
But what about the patient unable to make decisions or provide input to the medical caregivers? How can the comatose or incompetent patient participate in his or her own care decisions? What happens when half of a team is no longer able to share team functions?
In these instances, hospitalists rely on surrogates. A surrogate is empowered not only to speak for but also to make legal decisions for a patient. The relationship becomes a triad of hospitalist, surrogate, and patient. This triad must include:
- A hospitalist who brings the same degree of trust, respect, and open communication to the new relationship;
- A surrogate who is an active participant rather than a passive spokesperson; and
- A patient whose interests are the primary goal.
Key Issues
The aging of the population and the increased prevalence of medical conditions causing cognitive impairment point up the need to take a closer look at the hospitalist-surrogate relationship. A study this year outlined four key issues:
- There are unique challenges for both parties in creating a hospitalist-surrogate relationship;
- The hospitalist and surrogate are dealing not only with each other but also with the decision-making role each will play in regard to the patient;
- The surrogate must understand that serving as a surrogate for a loved one is completely different from making decisions for oneself; and
- There may be more than one surrogate decision maker.1
The first challenge facing hospitalist and surrogate is establishing a foundation of trust, respect, and a treatment plan. Their perspectives play a critical role: The surrogate knows the patient as a lively, engaged, and interesting individual, while the hospitalist has seen the patient only in a nonresponsive, incapacitated state. Opening an immediate line of communication is the best way to assume their respective responsibilities.
Second, even after the hospitalist and surrogate develop an initial working relationship, they may still need to outline mutually satisfying ways to share decision-making with the patient. Both must balance their concern for the patient, their understanding of the patient’s status, and their perspectives of what the patient would want. With time pressures and the capabilities of modern technology, this mutual decision-making responsibility may seem daunting.
Third, surrogates may discover a conflict between their personal values and their patient’s. They may have to make a decision that reflects their patient’s wishes yet contradicts their own beliefs. Sometimes hospitalists can help the surrogate resolve this dilemma by suggesting consultations with other family members or professionals.
The fourth issue, multiple surrogates, may magnify the challenges but can also be an advantage. In most cases families, even those with members who have differing belief systems, tend to support each other during crises to reach a consensus in the patient’s best interests.
Tom Baudendistel, MD, a hospitalist at California Pacific Medical Center in San Francisco, says that although engaging in a dialogue with the multiple surrogates may reveal a family conflict, mistrust, or other issues, the problem is usually resolved. “One surrogate comes around after we make sure the one disagreeing sees in person what the patient is going through, the low quality of life,” says Dr. Baudendistel.
Howard Epstein, MD, medical director, Care Management and Palliative Care, Regions Hospital, St. Paul, Minn., suggests a different approach. “We ask the surrogate to imagine that if the patient could stand outside his or her body, hearing everything that is being said, what would he or she say?” says Dr. Epstein.
The Process
While these issues affect all hospitalists who work with surrogates, hospitalists often encounter additional circumstances that require special attention. These are not always problems but may be situations unique to the hospital setting or the hospitalist’s job.
The hospitalist’s first contact with a patient is often the patient’s admission to the hospital. The hospitalist is most often starting with a blank page with no background information. Gathering information quickly about an unknown patient is critical.
This duty often falls to hospitalists. Donald Krause, MD, medical director for quality assurance at St. Joseph Hospital in Bangor, Maine, and a hospitalist for 11 years, points out that “hospitalists take care of 90% of medical admissions and as part of this job arrange for surrogates if needed as well as anything else to help the patient.”
Beginning with the admission of a patient, the hospitalist may take on the responsibility of finding a surrogate.
Find a surrogate: When a patient is admitted, the hospitalist questions everyone connected to the patient about the existence of a surrogate or family spokesperson. If there is no information available, many hospitalists turn to other staff experts, such as social workers or chaplains, to seek people who know the patient.
Dr. Baudendistel says his medical center resuscitates “unbefriended” patients admitted to the emergency department to allow time to find a family member or surrogate. “Social workers then search the Internet, call shelters, and contact other hospitals and institutions to learn anything they can about the patient,” he says. If the search is unsuccessful, the hospitalist usually consults the institution’s ethics committee for additional suggestions.
Don C. Postema, PhD, ethics consultant for Regions Hospital, chair of the HealthPartners Ethics Committee, and ethicist-in-residence at Gillette Children’s Specialty HealthCare in St. Paul, Minn., proposes that an ethics committee look beyond the standard candidates in searching for a surrogate. “The legal relationship of a potential surrogate to the patient is secondary to what I consider to be the primary relationship, that is, the person who knows the patient best,” says Dr. Postema. “It could be the patient’s landlord or a neighbor who sees the patient on a regular basis.”
What about the patient whose family lives too far away to see the patient on a regular basis? Look into hiring a local geriatric case manager, Dr. Epstein advises.
There is one person who should not serve as a patient’s surrogate: the attending physician, whether a hospitalist or the primary caregiver. Erin Egan, MD, JD, assistant professor of hospital medicine, University of Colorado Hospitals, warns that a hospitalist acting as a surrogate has a conflict of interest. “Most states prohibit hospitalists from acting as surrogates,” Dr. Egan warns. “In some cases a doctor can presume consent for a short time before a surrogate is appointed in order to make an immediate medical decision. As a general rule, however, a clinician should never assume the surrogate’s role.”
Look for advance directives: Ideally, every patient’s file would contain an advance directive indicating a surrogate or a note that there is no surrogate.2 In addition, there should be a healthcare advance directive, also known as a healthcare power of attorney, that appoints a surrogate. It is often accompanied by a living will, an instruction sheet stipulating what treatment the patient wants if he or she is unable to speak or communicate. Unfortunately, many hospitalists cannot find these documents when they admit a patient.
In this case, the hospitalist must search. Most hospitals, nursing homes, or home healthcare agencies are required by the federal Patient Self-Determination Act (PSDA) to offer information about advance directives at the time of admission. This information states the patient’s healthcare decision-making rights under state law and the institution’s policy about adhering to advance directives. Contacting these agencies is a starting point.
Make difficult decisions: While some advance directives carry legal power, they often are not helpful to hospitalists or surrogates making end-of-life decisions. Because a medical crisis cannot always be predicted and treatment options change rapidly, a specific directive may not be as helpful as a written description of a patient’s beliefs, religious convictions, and cultural values. Equally valuable are notes about conversations among patients, family members, friends, and caregivers.3 This creates a picture of the patient’s feelings about quality of life, treatment preferences, and end-of-life outcomes.
The hospitalist’s role in this situation is to facilitate such discussions among all family and friends involved. The goal is to develop an accurate picture of the patient to make appropriate decisions. The hospitalist should explore the cultural values and religious beliefs of the patient, surrogate, family, and friends. “Different ethnic groups view medical care differently,” says Richard L. Heinrich, MD, medical director of Hospice of the Lakes, Bloomington, Minn. “Some religions believe that suffering in this life is rewarded in the next life, which makes a difference when making treatment decisions,” he says. “We must honor and work with cultural values unless in our view the individual is suffering needlessly.”
The hospitalist should be alert to the need for an interpreter and anything else that will promote a meaningful discussion. And, the hospitalist and the medical staff should be prepared to share as much medical information as is possible, including individual staff opinions, the rationale behind recommendations, and the pros and cons of each suggestion. The surrogate and family cannot make any meaningful contribution without all the pertinent information.
The goal should be a consensus about the patient’s best interests, how certain medical decisions will provide benefit or burden to the patient, and if the decision is what the patient would want. It’s especially critical to call a family conference to allow everyone the opportunity to discuss the patient’s concept of his or her death.
“Most people are afraid of getting caught in an end-of-life situation where they lose control,” says Dr. Postema. TH
Ann Kepler is a medical writer based in Chicago.
References
- Torke AM, Alexander GC, Lantos J, et al. The physician-surrogate relationship. Arch Intern Med. 2007 Jun 11;167(11):1117-1121.
- Wenger NS, Rosenfeld K. Quality indicators for end-of-life care in vulnerable elders. Ann Intern Med. 2001 Oct 16;135(8):677-685.
- Bloche MG. Managing conflict at the end of life. N Engl J Med. 2005 Jun 9;352:2371-2373.
In the best interests of the patient. In accordance with the patient’s wishes. Preserving patient autonomy. These concepts are at the core of modern medical decision-making.
Traditionally medical decisions are made by hospitalists and communicated to patients. This approach has shifted to an emphasis on patient autonomy and input in decision-making.
But what about the patient unable to make decisions or provide input to the medical caregivers? How can the comatose or incompetent patient participate in his or her own care decisions? What happens when half of a team is no longer able to share team functions?
In these instances, hospitalists rely on surrogates. A surrogate is empowered not only to speak for but also to make legal decisions for a patient. The relationship becomes a triad of hospitalist, surrogate, and patient. This triad must include:
- A hospitalist who brings the same degree of trust, respect, and open communication to the new relationship;
- A surrogate who is an active participant rather than a passive spokesperson; and
- A patient whose interests are the primary goal.
Key Issues
The aging of the population and the increased prevalence of medical conditions causing cognitive impairment point up the need to take a closer look at the hospitalist-surrogate relationship. A study this year outlined four key issues:
- There are unique challenges for both parties in creating a hospitalist-surrogate relationship;
- The hospitalist and surrogate are dealing not only with each other but also with the decision-making role each will play in regard to the patient;
- The surrogate must understand that serving as a surrogate for a loved one is completely different from making decisions for oneself; and
- There may be more than one surrogate decision maker.1
The first challenge facing hospitalist and surrogate is establishing a foundation of trust, respect, and a treatment plan. Their perspectives play a critical role: The surrogate knows the patient as a lively, engaged, and interesting individual, while the hospitalist has seen the patient only in a nonresponsive, incapacitated state. Opening an immediate line of communication is the best way to assume their respective responsibilities.
Second, even after the hospitalist and surrogate develop an initial working relationship, they may still need to outline mutually satisfying ways to share decision-making with the patient. Both must balance their concern for the patient, their understanding of the patient’s status, and their perspectives of what the patient would want. With time pressures and the capabilities of modern technology, this mutual decision-making responsibility may seem daunting.
Third, surrogates may discover a conflict between their personal values and their patient’s. They may have to make a decision that reflects their patient’s wishes yet contradicts their own beliefs. Sometimes hospitalists can help the surrogate resolve this dilemma by suggesting consultations with other family members or professionals.
The fourth issue, multiple surrogates, may magnify the challenges but can also be an advantage. In most cases families, even those with members who have differing belief systems, tend to support each other during crises to reach a consensus in the patient’s best interests.
Tom Baudendistel, MD, a hospitalist at California Pacific Medical Center in San Francisco, says that although engaging in a dialogue with the multiple surrogates may reveal a family conflict, mistrust, or other issues, the problem is usually resolved. “One surrogate comes around after we make sure the one disagreeing sees in person what the patient is going through, the low quality of life,” says Dr. Baudendistel.
Howard Epstein, MD, medical director, Care Management and Palliative Care, Regions Hospital, St. Paul, Minn., suggests a different approach. “We ask the surrogate to imagine that if the patient could stand outside his or her body, hearing everything that is being said, what would he or she say?” says Dr. Epstein.
The Process
While these issues affect all hospitalists who work with surrogates, hospitalists often encounter additional circumstances that require special attention. These are not always problems but may be situations unique to the hospital setting or the hospitalist’s job.
The hospitalist’s first contact with a patient is often the patient’s admission to the hospital. The hospitalist is most often starting with a blank page with no background information. Gathering information quickly about an unknown patient is critical.
This duty often falls to hospitalists. Donald Krause, MD, medical director for quality assurance at St. Joseph Hospital in Bangor, Maine, and a hospitalist for 11 years, points out that “hospitalists take care of 90% of medical admissions and as part of this job arrange for surrogates if needed as well as anything else to help the patient.”
Beginning with the admission of a patient, the hospitalist may take on the responsibility of finding a surrogate.
Find a surrogate: When a patient is admitted, the hospitalist questions everyone connected to the patient about the existence of a surrogate or family spokesperson. If there is no information available, many hospitalists turn to other staff experts, such as social workers or chaplains, to seek people who know the patient.
Dr. Baudendistel says his medical center resuscitates “unbefriended” patients admitted to the emergency department to allow time to find a family member or surrogate. “Social workers then search the Internet, call shelters, and contact other hospitals and institutions to learn anything they can about the patient,” he says. If the search is unsuccessful, the hospitalist usually consults the institution’s ethics committee for additional suggestions.
Don C. Postema, PhD, ethics consultant for Regions Hospital, chair of the HealthPartners Ethics Committee, and ethicist-in-residence at Gillette Children’s Specialty HealthCare in St. Paul, Minn., proposes that an ethics committee look beyond the standard candidates in searching for a surrogate. “The legal relationship of a potential surrogate to the patient is secondary to what I consider to be the primary relationship, that is, the person who knows the patient best,” says Dr. Postema. “It could be the patient’s landlord or a neighbor who sees the patient on a regular basis.”
What about the patient whose family lives too far away to see the patient on a regular basis? Look into hiring a local geriatric case manager, Dr. Epstein advises.
There is one person who should not serve as a patient’s surrogate: the attending physician, whether a hospitalist or the primary caregiver. Erin Egan, MD, JD, assistant professor of hospital medicine, University of Colorado Hospitals, warns that a hospitalist acting as a surrogate has a conflict of interest. “Most states prohibit hospitalists from acting as surrogates,” Dr. Egan warns. “In some cases a doctor can presume consent for a short time before a surrogate is appointed in order to make an immediate medical decision. As a general rule, however, a clinician should never assume the surrogate’s role.”
Look for advance directives: Ideally, every patient’s file would contain an advance directive indicating a surrogate or a note that there is no surrogate.2 In addition, there should be a healthcare advance directive, also known as a healthcare power of attorney, that appoints a surrogate. It is often accompanied by a living will, an instruction sheet stipulating what treatment the patient wants if he or she is unable to speak or communicate. Unfortunately, many hospitalists cannot find these documents when they admit a patient.
In this case, the hospitalist must search. Most hospitals, nursing homes, or home healthcare agencies are required by the federal Patient Self-Determination Act (PSDA) to offer information about advance directives at the time of admission. This information states the patient’s healthcare decision-making rights under state law and the institution’s policy about adhering to advance directives. Contacting these agencies is a starting point.
Make difficult decisions: While some advance directives carry legal power, they often are not helpful to hospitalists or surrogates making end-of-life decisions. Because a medical crisis cannot always be predicted and treatment options change rapidly, a specific directive may not be as helpful as a written description of a patient’s beliefs, religious convictions, and cultural values. Equally valuable are notes about conversations among patients, family members, friends, and caregivers.3 This creates a picture of the patient’s feelings about quality of life, treatment preferences, and end-of-life outcomes.
The hospitalist’s role in this situation is to facilitate such discussions among all family and friends involved. The goal is to develop an accurate picture of the patient to make appropriate decisions. The hospitalist should explore the cultural values and religious beliefs of the patient, surrogate, family, and friends. “Different ethnic groups view medical care differently,” says Richard L. Heinrich, MD, medical director of Hospice of the Lakes, Bloomington, Minn. “Some religions believe that suffering in this life is rewarded in the next life, which makes a difference when making treatment decisions,” he says. “We must honor and work with cultural values unless in our view the individual is suffering needlessly.”
The hospitalist should be alert to the need for an interpreter and anything else that will promote a meaningful discussion. And, the hospitalist and the medical staff should be prepared to share as much medical information as is possible, including individual staff opinions, the rationale behind recommendations, and the pros and cons of each suggestion. The surrogate and family cannot make any meaningful contribution without all the pertinent information.
The goal should be a consensus about the patient’s best interests, how certain medical decisions will provide benefit or burden to the patient, and if the decision is what the patient would want. It’s especially critical to call a family conference to allow everyone the opportunity to discuss the patient’s concept of his or her death.
“Most people are afraid of getting caught in an end-of-life situation where they lose control,” says Dr. Postema. TH
Ann Kepler is a medical writer based in Chicago.
References
- Torke AM, Alexander GC, Lantos J, et al. The physician-surrogate relationship. Arch Intern Med. 2007 Jun 11;167(11):1117-1121.
- Wenger NS, Rosenfeld K. Quality indicators for end-of-life care in vulnerable elders. Ann Intern Med. 2001 Oct 16;135(8):677-685.
- Bloche MG. Managing conflict at the end of life. N Engl J Med. 2005 Jun 9;352:2371-2373.
In the best interests of the patient. In accordance with the patient’s wishes. Preserving patient autonomy. These concepts are at the core of modern medical decision-making.
Traditionally medical decisions are made by hospitalists and communicated to patients. This approach has shifted to an emphasis on patient autonomy and input in decision-making.
But what about the patient unable to make decisions or provide input to the medical caregivers? How can the comatose or incompetent patient participate in his or her own care decisions? What happens when half of a team is no longer able to share team functions?
In these instances, hospitalists rely on surrogates. A surrogate is empowered not only to speak for but also to make legal decisions for a patient. The relationship becomes a triad of hospitalist, surrogate, and patient. This triad must include:
- A hospitalist who brings the same degree of trust, respect, and open communication to the new relationship;
- A surrogate who is an active participant rather than a passive spokesperson; and
- A patient whose interests are the primary goal.
Key Issues
The aging of the population and the increased prevalence of medical conditions causing cognitive impairment point up the need to take a closer look at the hospitalist-surrogate relationship. A study this year outlined four key issues:
- There are unique challenges for both parties in creating a hospitalist-surrogate relationship;
- The hospitalist and surrogate are dealing not only with each other but also with the decision-making role each will play in regard to the patient;
- The surrogate must understand that serving as a surrogate for a loved one is completely different from making decisions for oneself; and
- There may be more than one surrogate decision maker.1
The first challenge facing hospitalist and surrogate is establishing a foundation of trust, respect, and a treatment plan. Their perspectives play a critical role: The surrogate knows the patient as a lively, engaged, and interesting individual, while the hospitalist has seen the patient only in a nonresponsive, incapacitated state. Opening an immediate line of communication is the best way to assume their respective responsibilities.
Second, even after the hospitalist and surrogate develop an initial working relationship, they may still need to outline mutually satisfying ways to share decision-making with the patient. Both must balance their concern for the patient, their understanding of the patient’s status, and their perspectives of what the patient would want. With time pressures and the capabilities of modern technology, this mutual decision-making responsibility may seem daunting.
Third, surrogates may discover a conflict between their personal values and their patient’s. They may have to make a decision that reflects their patient’s wishes yet contradicts their own beliefs. Sometimes hospitalists can help the surrogate resolve this dilemma by suggesting consultations with other family members or professionals.
The fourth issue, multiple surrogates, may magnify the challenges but can also be an advantage. In most cases families, even those with members who have differing belief systems, tend to support each other during crises to reach a consensus in the patient’s best interests.
Tom Baudendistel, MD, a hospitalist at California Pacific Medical Center in San Francisco, says that although engaging in a dialogue with the multiple surrogates may reveal a family conflict, mistrust, or other issues, the problem is usually resolved. “One surrogate comes around after we make sure the one disagreeing sees in person what the patient is going through, the low quality of life,” says Dr. Baudendistel.
Howard Epstein, MD, medical director, Care Management and Palliative Care, Regions Hospital, St. Paul, Minn., suggests a different approach. “We ask the surrogate to imagine that if the patient could stand outside his or her body, hearing everything that is being said, what would he or she say?” says Dr. Epstein.
The Process
While these issues affect all hospitalists who work with surrogates, hospitalists often encounter additional circumstances that require special attention. These are not always problems but may be situations unique to the hospital setting or the hospitalist’s job.
The hospitalist’s first contact with a patient is often the patient’s admission to the hospital. The hospitalist is most often starting with a blank page with no background information. Gathering information quickly about an unknown patient is critical.
This duty often falls to hospitalists. Donald Krause, MD, medical director for quality assurance at St. Joseph Hospital in Bangor, Maine, and a hospitalist for 11 years, points out that “hospitalists take care of 90% of medical admissions and as part of this job arrange for surrogates if needed as well as anything else to help the patient.”
Beginning with the admission of a patient, the hospitalist may take on the responsibility of finding a surrogate.
Find a surrogate: When a patient is admitted, the hospitalist questions everyone connected to the patient about the existence of a surrogate or family spokesperson. If there is no information available, many hospitalists turn to other staff experts, such as social workers or chaplains, to seek people who know the patient.
Dr. Baudendistel says his medical center resuscitates “unbefriended” patients admitted to the emergency department to allow time to find a family member or surrogate. “Social workers then search the Internet, call shelters, and contact other hospitals and institutions to learn anything they can about the patient,” he says. If the search is unsuccessful, the hospitalist usually consults the institution’s ethics committee for additional suggestions.
Don C. Postema, PhD, ethics consultant for Regions Hospital, chair of the HealthPartners Ethics Committee, and ethicist-in-residence at Gillette Children’s Specialty HealthCare in St. Paul, Minn., proposes that an ethics committee look beyond the standard candidates in searching for a surrogate. “The legal relationship of a potential surrogate to the patient is secondary to what I consider to be the primary relationship, that is, the person who knows the patient best,” says Dr. Postema. “It could be the patient’s landlord or a neighbor who sees the patient on a regular basis.”
What about the patient whose family lives too far away to see the patient on a regular basis? Look into hiring a local geriatric case manager, Dr. Epstein advises.
There is one person who should not serve as a patient’s surrogate: the attending physician, whether a hospitalist or the primary caregiver. Erin Egan, MD, JD, assistant professor of hospital medicine, University of Colorado Hospitals, warns that a hospitalist acting as a surrogate has a conflict of interest. “Most states prohibit hospitalists from acting as surrogates,” Dr. Egan warns. “In some cases a doctor can presume consent for a short time before a surrogate is appointed in order to make an immediate medical decision. As a general rule, however, a clinician should never assume the surrogate’s role.”
Look for advance directives: Ideally, every patient’s file would contain an advance directive indicating a surrogate or a note that there is no surrogate.2 In addition, there should be a healthcare advance directive, also known as a healthcare power of attorney, that appoints a surrogate. It is often accompanied by a living will, an instruction sheet stipulating what treatment the patient wants if he or she is unable to speak or communicate. Unfortunately, many hospitalists cannot find these documents when they admit a patient.
In this case, the hospitalist must search. Most hospitals, nursing homes, or home healthcare agencies are required by the federal Patient Self-Determination Act (PSDA) to offer information about advance directives at the time of admission. This information states the patient’s healthcare decision-making rights under state law and the institution’s policy about adhering to advance directives. Contacting these agencies is a starting point.
Make difficult decisions: While some advance directives carry legal power, they often are not helpful to hospitalists or surrogates making end-of-life decisions. Because a medical crisis cannot always be predicted and treatment options change rapidly, a specific directive may not be as helpful as a written description of a patient’s beliefs, religious convictions, and cultural values. Equally valuable are notes about conversations among patients, family members, friends, and caregivers.3 This creates a picture of the patient’s feelings about quality of life, treatment preferences, and end-of-life outcomes.
The hospitalist’s role in this situation is to facilitate such discussions among all family and friends involved. The goal is to develop an accurate picture of the patient to make appropriate decisions. The hospitalist should explore the cultural values and religious beliefs of the patient, surrogate, family, and friends. “Different ethnic groups view medical care differently,” says Richard L. Heinrich, MD, medical director of Hospice of the Lakes, Bloomington, Minn. “Some religions believe that suffering in this life is rewarded in the next life, which makes a difference when making treatment decisions,” he says. “We must honor and work with cultural values unless in our view the individual is suffering needlessly.”
The hospitalist should be alert to the need for an interpreter and anything else that will promote a meaningful discussion. And, the hospitalist and the medical staff should be prepared to share as much medical information as is possible, including individual staff opinions, the rationale behind recommendations, and the pros and cons of each suggestion. The surrogate and family cannot make any meaningful contribution without all the pertinent information.
The goal should be a consensus about the patient’s best interests, how certain medical decisions will provide benefit or burden to the patient, and if the decision is what the patient would want. It’s especially critical to call a family conference to allow everyone the opportunity to discuss the patient’s concept of his or her death.
“Most people are afraid of getting caught in an end-of-life situation where they lose control,” says Dr. Postema. TH
Ann Kepler is a medical writer based in Chicago.
References
- Torke AM, Alexander GC, Lantos J, et al. The physician-surrogate relationship. Arch Intern Med. 2007 Jun 11;167(11):1117-1121.
- Wenger NS, Rosenfeld K. Quality indicators for end-of-life care in vulnerable elders. Ann Intern Med. 2001 Oct 16;135(8):677-685.
- Bloche MG. Managing conflict at the end of life. N Engl J Med. 2005 Jun 9;352:2371-2373.
To Serve in America
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
New Perspective
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Contract Caveats
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
The Admission Consult
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Massachusetts Effect
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.



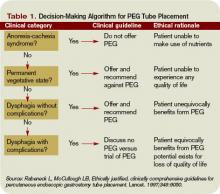
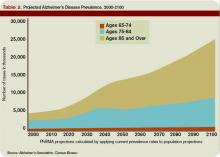
![I feel the skepticism, but I still treat the [patient or colleague] with the respect that they deserve. Ultimately, I just let my work do the talking.](https://cdn.mdedge.com/files/s3fs-public/styles/medium/public/images/2007_12_pp32_01.jpg?itok=ninhb4TU)






