User login
Obstructive sleep apnea and cardiovascular disease: Implications for clinical practice
What's Eating You? Pigeon Mite (Dermanyssus gallinae)
CPT codes diversify for hysterectomy and repair of paravaginal defects
There’s more: If you’ve been spending time on telephone or on-line counseling, codes that may get you paid for that service are about to make their debut.
Key additions and revisions to CPT for the new year are detailed in this article and in next issue’s Reimbursement Adviser.
Specify repair of paravaginal defect
57284 Paravaginal defect repair (including repair of cystocele, if performed); open abdominal approach
57285 Paravaginal defect repair (including repair of cystocele, if performed); vaginal approach
57423 Paravaginal defect repair (including repair of cystocele, if performed); laparoscopic approach
You’ll now have to carefully document your surgical approach to repairing a paravaginal defect, thanks to creation of two new codes and revision of the existing 57284.
Several bundles are still attached to the new codes, however. CPT did remove references to “stress urinary incontinence, and/or incomplete vaginal prolapse” from the revised and new codes, but repair of a cystocele, by any method, is still included.
CPT 2008 is, therefore, listing codes that cannot be reported additionally. In general, urethropexy codes 51840, 51841, 51990, 58152, and 58267 and cystocele repair codes 57240, 57260, and 57265 should not be reported when a paravaginal defect repair is performed.
Also, be alert for any National Correct Coding Initiatives (NCCI) bundles assigned by Medicare to these new codes if they are different from the ones that will be listed by CPT. In particular, 57288 [sling operation for stress incontinence (e.g., fascia or synthetic)] was permanently bundled into 57284. (If that bundle isn’t removed in 2008, I encourage you to contact ACOG and urge the College to discuss this inappropriate bundle with Medicare administrators.)
Total lap hysterectomy
58570 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less
58571 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of tube(s) and/or ovary(ies)
58572 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g
58573 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(ies)
For some time, surgeons have been able to perform a hysterectomy by completely detaching both the uterine cervix and the body of the uterus from their surrounding support structures laparoscopically, then closing the vaginal cuff via this approach as well. Before 2008, the only coding choices were laparoscopic-assisted hysterectomy codes (58550–58554) or the unlisted laparoscopic code 58578. The new codes—as with codes for any vaginal or laparoscopic approach—are selected based on 1) the documented weight of the uterus and 2) whether the fallopian tubes or ovaries have been removed.
Intraperitoneal tumors, coded by size
49203 Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors; largest tumor 5 cm diameter or less
49204 …largest tumor 5.1–10.0 cm diameter
49205 …largest tumor greater than 10.0 cm diameter
In 2007, documenting the removal of intraperitoneal or retroperitoneal tumors, cysts, and endometriomas via abdominal incision was fairly simple: There were two codes and you had only to decide if removal was extensive or not.
In 2008, codes 49200 and 49201 are deleted and replaced by three new codes—each of which requires you to document the size of the largest tumor or lesion removed.
The new codes will come in handy during surgery in which the originating organ has been removed but the patient is found to have additional tumors. For example: A patient had ovarian cancer and now there are additional tumors in the abdominal cavity, but an omentectomy is not being performed. Of course, the new codes can still be used for excision or destruction of cysts or endometriomas, as well. But CPT has also listed codes that cannot be billed with the new codes: Among them are 38770 [pelvic lymphadenectomy] and 58900–58960 [surgeries performed on the ovaries]. If the new codes don’t fit the surgery, the other option for tumor debulking after the organ has been removed is to report 58957 or 58958; note, however, that these codes include omentectomy and optional pelvic lymph node sampling.
Bladder aspiration is renumbered
51100 Aspiration of bladder; by needle
51101 …by trocar or intracatheter
51102 …with insertion of suprapubic catheter
If you have the old codes for bladder aspiration memorized, relearn them. Once again, CPT tinkered with placement of codes and decided that bladder aspiration codes are placed more appropriately under “Bladder, Removal” than “Bladder, Incision.” The uses of those codes are unchanged.
Giving flu, HPV vaccines
90661 Influenza virus vaccine, derived from cell cultures, subunit, preservative and antibiotic free, for intramuscular use
90662 Influenza virus vaccine, split virus, preservative free, enhanced immunogenicity via increased antigen content, for intramuscular use
90663 Influenza virus vaccine, pandemic formulation
90650 Human papillomavirus (HPV) vaccine, types 16 and 18, bivalent, 3-dose schedule, for intramuscular use
Four new codes for vaccines can be reported beginning January 1, but only those for the influenza vaccine appear in the CPT 2008 book. The code for the new bivalent HPV vaccine is a valid code for 2008 but will not appear in print until CPT 2009.
Changes made to “modifier -51” exemptions
CPT 2008 also reassessed codes that have been designated as “modifier - 51 exempt.” Typically, these are codes that do not involve significant preoperative or postoperative work. 36660 [catheterization, umbilical artery, newborn, for diagnosis or therapy] now requires a modifier when performed with other procedures, whereas 51797 [voiding pressure studies (VP); intra-abdominal voiding pressure (AP) (rectal, gastric, intraperitoneal)] becomes an add-on code that does not take a modifier -51. Beginning January 1, 51797 can be billed only if 51795 [voiding pressure studies (VP); bladder voiding pressure, any technique] has also been reported.
Fecal blood testing
If you bill 82272 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, single specimen (e.g., from digital rectal exam)] for the annual fecal occult blood screening test, CPT has revised the code to make it clear that this code is not to be reported for a screening test.
The only two CPT codes that can be reported for the screening fecal occult blood test are 82270 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, consecutive collected specimens with single determination, for colorectal neoplasm screening] (that is, the patient was provided three cards or a single triple card for consecutive collection) or 82274 [blood, occult, by fecal hemoglobin determination by immunoassay, qualitative, feces, 1–3 simultaneous determinations].
Note: The physician may collect the specimen for an immunoassay (except on a Medicare patient), but a guaiac test specimen must be collected by the patient.
Cervical biopsy
The descriptor for 57500 will now specifically refer to the cervix as the location for biopsy or excision of a lesion. Before this change, only the subheading title gave any indication of anatomic location.
Hysterectomy
If you perform a laparoscopic-assisted (58550–58554), total (58570–58573), or supracervical (58541–58544) hysterectomy, CPT has added a list of codes that you may not report as well. These include:
- 49320 [diagnostic laparoscopy]
- 57000 [colpotomy]
- 57180 [hemostatic vaginal packing]
- 57410 [EUA]
- 58140–58146, 58545–58546, 58561 [myomectomy]
- 58661 [removal of tubes and/or ovaries]
- 58670, 58671 [tubal ligations]
Vascular ultrasound
Last, CPT has clarified that, to bill 93975 or 93976 [duplex scan of arterial inflow and venous outflow of abdominal, pelvic, scrotal contents and/or retroperitoneal organs], the purpose of the exam must be to evaluate vascular structures. If color Doppler ultrasound is used to identify anatomic structures at the time of US scan, neither of those two codes may be billed additionally.
There’s more: If you’ve been spending time on telephone or on-line counseling, codes that may get you paid for that service are about to make their debut.
Key additions and revisions to CPT for the new year are detailed in this article and in next issue’s Reimbursement Adviser.
Specify repair of paravaginal defect
57284 Paravaginal defect repair (including repair of cystocele, if performed); open abdominal approach
57285 Paravaginal defect repair (including repair of cystocele, if performed); vaginal approach
57423 Paravaginal defect repair (including repair of cystocele, if performed); laparoscopic approach
You’ll now have to carefully document your surgical approach to repairing a paravaginal defect, thanks to creation of two new codes and revision of the existing 57284.
Several bundles are still attached to the new codes, however. CPT did remove references to “stress urinary incontinence, and/or incomplete vaginal prolapse” from the revised and new codes, but repair of a cystocele, by any method, is still included.
CPT 2008 is, therefore, listing codes that cannot be reported additionally. In general, urethropexy codes 51840, 51841, 51990, 58152, and 58267 and cystocele repair codes 57240, 57260, and 57265 should not be reported when a paravaginal defect repair is performed.
Also, be alert for any National Correct Coding Initiatives (NCCI) bundles assigned by Medicare to these new codes if they are different from the ones that will be listed by CPT. In particular, 57288 [sling operation for stress incontinence (e.g., fascia or synthetic)] was permanently bundled into 57284. (If that bundle isn’t removed in 2008, I encourage you to contact ACOG and urge the College to discuss this inappropriate bundle with Medicare administrators.)
Total lap hysterectomy
58570 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less
58571 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of tube(s) and/or ovary(ies)
58572 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g
58573 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(ies)
For some time, surgeons have been able to perform a hysterectomy by completely detaching both the uterine cervix and the body of the uterus from their surrounding support structures laparoscopically, then closing the vaginal cuff via this approach as well. Before 2008, the only coding choices were laparoscopic-assisted hysterectomy codes (58550–58554) or the unlisted laparoscopic code 58578. The new codes—as with codes for any vaginal or laparoscopic approach—are selected based on 1) the documented weight of the uterus and 2) whether the fallopian tubes or ovaries have been removed.
Intraperitoneal tumors, coded by size
49203 Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors; largest tumor 5 cm diameter or less
49204 …largest tumor 5.1–10.0 cm diameter
49205 …largest tumor greater than 10.0 cm diameter
In 2007, documenting the removal of intraperitoneal or retroperitoneal tumors, cysts, and endometriomas via abdominal incision was fairly simple: There were two codes and you had only to decide if removal was extensive or not.
In 2008, codes 49200 and 49201 are deleted and replaced by three new codes—each of which requires you to document the size of the largest tumor or lesion removed.
The new codes will come in handy during surgery in which the originating organ has been removed but the patient is found to have additional tumors. For example: A patient had ovarian cancer and now there are additional tumors in the abdominal cavity, but an omentectomy is not being performed. Of course, the new codes can still be used for excision or destruction of cysts or endometriomas, as well. But CPT has also listed codes that cannot be billed with the new codes: Among them are 38770 [pelvic lymphadenectomy] and 58900–58960 [surgeries performed on the ovaries]. If the new codes don’t fit the surgery, the other option for tumor debulking after the organ has been removed is to report 58957 or 58958; note, however, that these codes include omentectomy and optional pelvic lymph node sampling.
Bladder aspiration is renumbered
51100 Aspiration of bladder; by needle
51101 …by trocar or intracatheter
51102 …with insertion of suprapubic catheter
If you have the old codes for bladder aspiration memorized, relearn them. Once again, CPT tinkered with placement of codes and decided that bladder aspiration codes are placed more appropriately under “Bladder, Removal” than “Bladder, Incision.” The uses of those codes are unchanged.
Giving flu, HPV vaccines
90661 Influenza virus vaccine, derived from cell cultures, subunit, preservative and antibiotic free, for intramuscular use
90662 Influenza virus vaccine, split virus, preservative free, enhanced immunogenicity via increased antigen content, for intramuscular use
90663 Influenza virus vaccine, pandemic formulation
90650 Human papillomavirus (HPV) vaccine, types 16 and 18, bivalent, 3-dose schedule, for intramuscular use
Four new codes for vaccines can be reported beginning January 1, but only those for the influenza vaccine appear in the CPT 2008 book. The code for the new bivalent HPV vaccine is a valid code for 2008 but will not appear in print until CPT 2009.
Changes made to “modifier -51” exemptions
CPT 2008 also reassessed codes that have been designated as “modifier - 51 exempt.” Typically, these are codes that do not involve significant preoperative or postoperative work. 36660 [catheterization, umbilical artery, newborn, for diagnosis or therapy] now requires a modifier when performed with other procedures, whereas 51797 [voiding pressure studies (VP); intra-abdominal voiding pressure (AP) (rectal, gastric, intraperitoneal)] becomes an add-on code that does not take a modifier -51. Beginning January 1, 51797 can be billed only if 51795 [voiding pressure studies (VP); bladder voiding pressure, any technique] has also been reported.
Fecal blood testing
If you bill 82272 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, single specimen (e.g., from digital rectal exam)] for the annual fecal occult blood screening test, CPT has revised the code to make it clear that this code is not to be reported for a screening test.
The only two CPT codes that can be reported for the screening fecal occult blood test are 82270 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, consecutive collected specimens with single determination, for colorectal neoplasm screening] (that is, the patient was provided three cards or a single triple card for consecutive collection) or 82274 [blood, occult, by fecal hemoglobin determination by immunoassay, qualitative, feces, 1–3 simultaneous determinations].
Note: The physician may collect the specimen for an immunoassay (except on a Medicare patient), but a guaiac test specimen must be collected by the patient.
Cervical biopsy
The descriptor for 57500 will now specifically refer to the cervix as the location for biopsy or excision of a lesion. Before this change, only the subheading title gave any indication of anatomic location.
Hysterectomy
If you perform a laparoscopic-assisted (58550–58554), total (58570–58573), or supracervical (58541–58544) hysterectomy, CPT has added a list of codes that you may not report as well. These include:
- 49320 [diagnostic laparoscopy]
- 57000 [colpotomy]
- 57180 [hemostatic vaginal packing]
- 57410 [EUA]
- 58140–58146, 58545–58546, 58561 [myomectomy]
- 58661 [removal of tubes and/or ovaries]
- 58670, 58671 [tubal ligations]
Vascular ultrasound
Last, CPT has clarified that, to bill 93975 or 93976 [duplex scan of arterial inflow and venous outflow of abdominal, pelvic, scrotal contents and/or retroperitoneal organs], the purpose of the exam must be to evaluate vascular structures. If color Doppler ultrasound is used to identify anatomic structures at the time of US scan, neither of those two codes may be billed additionally.
There’s more: If you’ve been spending time on telephone or on-line counseling, codes that may get you paid for that service are about to make their debut.
Key additions and revisions to CPT for the new year are detailed in this article and in next issue’s Reimbursement Adviser.
Specify repair of paravaginal defect
57284 Paravaginal defect repair (including repair of cystocele, if performed); open abdominal approach
57285 Paravaginal defect repair (including repair of cystocele, if performed); vaginal approach
57423 Paravaginal defect repair (including repair of cystocele, if performed); laparoscopic approach
You’ll now have to carefully document your surgical approach to repairing a paravaginal defect, thanks to creation of two new codes and revision of the existing 57284.
Several bundles are still attached to the new codes, however. CPT did remove references to “stress urinary incontinence, and/or incomplete vaginal prolapse” from the revised and new codes, but repair of a cystocele, by any method, is still included.
CPT 2008 is, therefore, listing codes that cannot be reported additionally. In general, urethropexy codes 51840, 51841, 51990, 58152, and 58267 and cystocele repair codes 57240, 57260, and 57265 should not be reported when a paravaginal defect repair is performed.
Also, be alert for any National Correct Coding Initiatives (NCCI) bundles assigned by Medicare to these new codes if they are different from the ones that will be listed by CPT. In particular, 57288 [sling operation for stress incontinence (e.g., fascia or synthetic)] was permanently bundled into 57284. (If that bundle isn’t removed in 2008, I encourage you to contact ACOG and urge the College to discuss this inappropriate bundle with Medicare administrators.)
Total lap hysterectomy
58570 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less
58571 Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of tube(s) and/or ovary(ies)
58572 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g
58573 Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(ies)
For some time, surgeons have been able to perform a hysterectomy by completely detaching both the uterine cervix and the body of the uterus from their surrounding support structures laparoscopically, then closing the vaginal cuff via this approach as well. Before 2008, the only coding choices were laparoscopic-assisted hysterectomy codes (58550–58554) or the unlisted laparoscopic code 58578. The new codes—as with codes for any vaginal or laparoscopic approach—are selected based on 1) the documented weight of the uterus and 2) whether the fallopian tubes or ovaries have been removed.
Intraperitoneal tumors, coded by size
49203 Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors; largest tumor 5 cm diameter or less
49204 …largest tumor 5.1–10.0 cm diameter
49205 …largest tumor greater than 10.0 cm diameter
In 2007, documenting the removal of intraperitoneal or retroperitoneal tumors, cysts, and endometriomas via abdominal incision was fairly simple: There were two codes and you had only to decide if removal was extensive or not.
In 2008, codes 49200 and 49201 are deleted and replaced by three new codes—each of which requires you to document the size of the largest tumor or lesion removed.
The new codes will come in handy during surgery in which the originating organ has been removed but the patient is found to have additional tumors. For example: A patient had ovarian cancer and now there are additional tumors in the abdominal cavity, but an omentectomy is not being performed. Of course, the new codes can still be used for excision or destruction of cysts or endometriomas, as well. But CPT has also listed codes that cannot be billed with the new codes: Among them are 38770 [pelvic lymphadenectomy] and 58900–58960 [surgeries performed on the ovaries]. If the new codes don’t fit the surgery, the other option for tumor debulking after the organ has been removed is to report 58957 or 58958; note, however, that these codes include omentectomy and optional pelvic lymph node sampling.
Bladder aspiration is renumbered
51100 Aspiration of bladder; by needle
51101 …by trocar or intracatheter
51102 …with insertion of suprapubic catheter
If you have the old codes for bladder aspiration memorized, relearn them. Once again, CPT tinkered with placement of codes and decided that bladder aspiration codes are placed more appropriately under “Bladder, Removal” than “Bladder, Incision.” The uses of those codes are unchanged.
Giving flu, HPV vaccines
90661 Influenza virus vaccine, derived from cell cultures, subunit, preservative and antibiotic free, for intramuscular use
90662 Influenza virus vaccine, split virus, preservative free, enhanced immunogenicity via increased antigen content, for intramuscular use
90663 Influenza virus vaccine, pandemic formulation
90650 Human papillomavirus (HPV) vaccine, types 16 and 18, bivalent, 3-dose schedule, for intramuscular use
Four new codes for vaccines can be reported beginning January 1, but only those for the influenza vaccine appear in the CPT 2008 book. The code for the new bivalent HPV vaccine is a valid code for 2008 but will not appear in print until CPT 2009.
Changes made to “modifier -51” exemptions
CPT 2008 also reassessed codes that have been designated as “modifier - 51 exempt.” Typically, these are codes that do not involve significant preoperative or postoperative work. 36660 [catheterization, umbilical artery, newborn, for diagnosis or therapy] now requires a modifier when performed with other procedures, whereas 51797 [voiding pressure studies (VP); intra-abdominal voiding pressure (AP) (rectal, gastric, intraperitoneal)] becomes an add-on code that does not take a modifier -51. Beginning January 1, 51797 can be billed only if 51795 [voiding pressure studies (VP); bladder voiding pressure, any technique] has also been reported.
Fecal blood testing
If you bill 82272 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, single specimen (e.g., from digital rectal exam)] for the annual fecal occult blood screening test, CPT has revised the code to make it clear that this code is not to be reported for a screening test.
The only two CPT codes that can be reported for the screening fecal occult blood test are 82270 [blood, occult, by peroxidase activity (e.g., guaiac), qualitative, feces, consecutive collected specimens with single determination, for colorectal neoplasm screening] (that is, the patient was provided three cards or a single triple card for consecutive collection) or 82274 [blood, occult, by fecal hemoglobin determination by immunoassay, qualitative, feces, 1–3 simultaneous determinations].
Note: The physician may collect the specimen for an immunoassay (except on a Medicare patient), but a guaiac test specimen must be collected by the patient.
Cervical biopsy
The descriptor for 57500 will now specifically refer to the cervix as the location for biopsy or excision of a lesion. Before this change, only the subheading title gave any indication of anatomic location.
Hysterectomy
If you perform a laparoscopic-assisted (58550–58554), total (58570–58573), or supracervical (58541–58544) hysterectomy, CPT has added a list of codes that you may not report as well. These include:
- 49320 [diagnostic laparoscopy]
- 57000 [colpotomy]
- 57180 [hemostatic vaginal packing]
- 57410 [EUA]
- 58140–58146, 58545–58546, 58561 [myomectomy]
- 58661 [removal of tubes and/or ovaries]
- 58670, 58671 [tubal ligations]
Vascular ultrasound
Last, CPT has clarified that, to bill 93975 or 93976 [duplex scan of arterial inflow and venous outflow of abdominal, pelvic, scrotal contents and/or retroperitoneal organs], the purpose of the exam must be to evaluate vascular structures. If color Doppler ultrasound is used to identify anatomic structures at the time of US scan, neither of those two codes may be billed additionally.
Empathy goes a long way in weight loss discussions
- A physician’s empathy, collaborative approach, and words of support can have a positive effect on overweight and obese women’s weight loss efforts.
Purpose This study explores how weight-related topics are discussed between physicians and their overweight and obese female patients.
Methods We surveyed and audio-recorded preventive health and chronic care visits with 25 overweight and obese female patients. We coded both for quantity (content and time) of weight-related discussions and quality (adherence to Motivational Interviewing [MI] techniques). We then tested correlations of these measures with patients’ reported attempts to lose weight, change diet, and change exercise patterns 1 month after the visit.
Results Weight was routinely addressed (19 of 25 encounters). Patients usually initiated the topic (67% of time). Physicians’ use of MI techniques resulted in patients attempting to lose weight and changing their exercise patterns.
Conclusion Physicians may benefit from MI training to help patients lose weight.
Research has shown that when physicians advise overweight patients to lose weight, improve their diet, or increase their physical activity, patients are more likely to report attempting to do so.1-3 In a study of 433 primary care patients, 46% reported trying to lose weight after their physician counseled them about nutrition, compared with 37% who were not counseled.1
The reality, though, is that physicians are not very likely to address weight loss. Data from the Behavioral Risk Factor Surveillance System indicate that patients report their providers address weight loss in fewer than 20% of their examinations.4 These low rates are concerning; when physicians do not advise patients to lose weight, patients may believe their weight is not a problem.5 Even more worrisome: Physicians are rarely trained on how to counsel patients about weight loss. So, when physicians do counsel patients, it may not be effective.
Using Motivational Interviewing
One effective style of counseling is Motivational Interviewing (MI). MI is a patient-centered, directive counseling style used to help patients explore and resolve their ambivalence related to a particular behavior change (see What is Motivational Interviewing?).6,7 Researchers have studied the use of MI by counselors and case managers (in handling smoking cessation),8-11 but not by physicians. Further, no one has examined whether physicians instinctively use MI techniques when discussing weight loss with their patients, or whether MI counseling results in patients trying to lose weight.
The primary aim of this study was to assess how overweight and obese female patients discuss weight loss with their physicians. We also wanted to explore the role that physicians’ way of discussing weight loss—and the use of MI in particular—might play in their patients’ motivation to lose weight.
Motivational Interviewing is a counseling style intended to create changes in behavior by helping patients to explore and resolve their ambivalence.7 In a patient-physician encounter guided by MI:
- The motivation to change comes from the patient.
- It is the patient’s job to articulate and resolve his or her ambivalence.
- Direct persuasion is not used; the physician is quiet and eliciting, but directive in helping the patient examine his or her ambivalence.
- Readiness for change is recognized not as a patient trait, but as a part of the interaction between physician and patient.
- The patient-physician relationship is regarded more like a partnership.
Methods
Setting and recruitment
All data were collected in a family practice clinic within Duke University Medical Center. We approached 9 physicians in the practice to participate, and all consented. Only 7 physicians had visits with overweight or obese patients and were included in this report. We reviewed their electronic patient appointment schedules twice a week to identify female patients meeting the following criteria: English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), 40 years of age or older, and with health maintenance or chronic care appointments scheduled at least 7 days later. We sent these patients a letter describing the study, and allowed them 7 days to call a toll-free number if they didn’t want to participate.
We took several steps to avoid priming physicians and patients about the purpose of the study. First, both physicians and patients were told the study was about how doctors and patients discuss preventive health topics—they were not told the study was about examining discussions of weight. Second, we surveyed physicians 1 month prior to audio-recording visits, and patients 1 week prior to their visit. Third, we included measures for other preventive health topics (eg, smoking and alcohol) to detract attention from weight.
Gathering data
1. Phone survey before patient visit. We telephoned those patients who did not refuse participation and conducted a baseline survey. We asked about date of birth, race, marital status, level of education, income, weight, height, history of weight loss attempts, and whether this was their first visit with that physician. We categorized women with a BMI ≥25 but <30 as overweight, and those with a BMI ≥30 as obese.12
We also assessed each patient’s
- self-efficacy—that is, confidence in their ability to lose weight. We asked: “How confident are you that you can lose weight?” (1=not at all confident, 5=extremely confident).
- readiness to lose weight. We asked: “Are you seriously considering trying to losing weight within the next 6 months?” and, if yes, “Are you planning to try to lose weight in the next 30 days?”13 Those not considering trying to lose weight were staged as precontemplation; those who were considering trying but not planning to try in the next 30 days were staged as contemplation; and those who were planning to try to lose weight in the next 30 days were staged as preparation.
2. Office visit. When patients came in for their appointments, the research assistant gave them consent forms to sign. The assistant then escorted the patient to the examination rooms and started the digital audio recorder. The exams typically took 27 minutes.
Immediately following the exam, the research assistant surveyed the patients. The assistant asked 2 questions we’d asked at baseline: “How confident are you that you can lose weight?” and “Are you seriously considering trying to losing weight within the next 6 months?” (If yes, “Are you planning to try to lose weight in the next 30 days?”) She also made an appointment to conduct a 1-month follow-up telephone survey.
3. One-month follow-up survey. During a follow-up phone survey, we asked patients whether they had attempted to lose weight by changing their diet, exercise patterns, or both. Subsequent to this call, we sent the study participants a $25 check.
Analyzing the patient-physician discussion
Content. Two authors coded 9 topics that physicians and patients discussed that were “weight-related.” Topics included: physical activity, diet, BMI, psychosocial issues, referral to a nutritionist, weight loss surgery, goal setting, weight loss medications, and health care avoidance. We also coded who first brought up the topic.
Time spent. We calculated time spent discussing weight-related topics and also the total time of the patient’s visit.
Motivational Interviewing. Two coders assessed MI. To assess fidelity to MI principles, we used sections of the Motivational Interviewing Treatment Integrity scale (MITI)14 to rate patient interactions on a scale of 1 (low) to 7 (high) in 2 categories: empathy and MI spirit.
- Empathy is when physicians convey understanding of patients’ perspective.
- MI spirit includes evocation, collaboration, and autonomy. Evocation is when physicians draw out patients’ own reasons for change. Collaboration is when physicians act as partners, supporting and exploring patients’ concerns. Autonomy is when physicians convey that decisions to change lie completely with patients. Inter-rater reliability for the Empathy and MI Spirit was adequate (ICC=.94 and .97, respectively).
- MI-adherent behaviors were those where the physician asked permission to do things, affirmed statements, offered words of support, and emphasized patient control. For instance, the physician might say, “It’s great that you have stopped drinking sweetened tea” or “Whether you lose weight is up to you.”
- MI-nonadherent behaviors were those where the physician advised without asking permission. For example, the physician might say, “Let me tell you what you need to do to make this work…” or “Well, if you want to continue on the way you are, you know your diabetes is only going to get worse.”
These were combined to create a ratio of percentage MI-adherent behaviors by dividing MI-adherent by MI-nonadherent. There was an excellent level of agreement between coders for MI-nonadherent (kappa=.80) and a moderate level of agreement for MI-adherent (kappa=.52) behaviors.
Data analysis
We used Spearman correlations to assess the relationship between our predictors, quantity (time spent and whether weight was addressed) and quality (MI techniques), and mediators of behavior change (readiness to lose weight and self-efficacy to lose weight) and behavior change (attempts to lose weight, change in diet, and change in exercise patterns). We used SAS 9.1 (SAS Institute, Inc, Cary, NC) for all analyses. The study was approved by the Duke University Medical Center Institutional Review Board.
Results
We identified 202 eligible female patients. Of those, 96 had appointments that passed before we could contact them; 11 called the 800 number to refuse. Of the remaining 95 women, we reached 94 by phone. Of those, 19 refused to participate, 46 were ineligible because we had reached the targeted number of women in their weight category, and 4 skipped their appointments. Thus, we audio-recorded 25 encounters (for 14 obese and 11 overweight patients). Of these 25 patients, 24 completed the 1-month follow-up.
Patient demographics. Patients had a mean age of 59 years (standard deviation [SD]=11). Half were white; 42% were college-educated. Forty-two percent reported being in poor to fair health (TABLE 1).
The typical participant was moderately confident and ready to lose weight both before and after their visit. One month after their visit, 63% reported attempting to lose weight. More than half attempted to change their diet (67%); slightly more than half changed their exercise patterns (58%) (TABLE 2).
Physician demographics. Physicians had a mean age of 43 years (SD=10). About half were white; about half were female. No physicians were overweight.
TABLE 1
Characteristics of patients and physicians
| CHARACTERISTIC | PATIENT (N=25) | PHYSICIAN (N=7) |
|---|---|---|
| Age (M, SD) | 59 (11) | 43 (10) |
| Race (%)* | ||
| White | 50 | 57 |
| Black | 50 | 29 |
| Indian | 14 | |
| Female (%) | 100 | 57 |
| Married (%) | 46 | — |
| Employed (%) | 54 | 100 |
| College graduate (%) | 42 | 100 |
| Health status, self-reported (%) | ||
| Poor to fair | 42 | — |
| Good | 37 | — |
| Very good to excellent | 21 | — |
| Times lost at least 10 lbs (mean, SD) | 5.8 (4.0) | — |
| New patient with physician (%) | 12 | — |
| Body mass index (mean, SD) | 37 (11) | 22 (3) |
| * One participant did not provide his/her race. | ||
TABLE 2
Feeling about weight loss before and after the visit
| BASELINE | POST-VISIT | 1 MONTH | |
|---|---|---|---|
| Mediators of behavior change | |||
| Confidence in losing weight (M, SD)* | 3.8 (1.4) | 3.8 (1.1) | – |
| Stage of readiness to lose weight (%) | |||
| Precontemplation | 25% | 28% | – |
| Contemplation | 8% | 8% | – |
| Preparation | 67% | 64% | – |
| Behavior change variables | |||
| Attempted to lose weight (%) | – | – | 63% |
| Attempted to change diet (%) | – | – | 67% |
| Changed exercise patterns (%) | – | – | 58% |
| * Scale ranged from 1=not at all confident to 5=extremely confident. | |||
Patients were more likely to raise the weight issue
Weight-related topics were addressed in 19 of the 25 encounters (11 out of 12 preventive health visits, 8 out of 13 chronic care visits). The mean time spent discussing weight-related topics was 6.9 minutes out of an mean total of 27.0 minutes, or 26% of the total patient-physician time. Weight was more likely to be addressed with obese patients (86%) than with overweight patients (63%).
Patients were more likely than physicians to initiate discussions on weight. Physicians raised weight-related topics 37% of the time. Obese patients were slightly more likely to raise weight-related topics (8 out of 12 times [67%]) than overweight patients (4 out of 7 times [57%]).
The weight-related topics addressed were, in order from most to least frequent: physical activity, diet, BMI, psychosocial issues (eg, motivation to lose weight, triggers for unhealthful eating [such as family cookouts], negative talk [such as telling oneself that losing weight is too hard]), referral to a nutritionist, weight loss surgery, goal setting, health care avoidance, and weight loss medication. When comparing those who attempted to lose weight (n=15) with those who did not (n=9), there was no significant difference in whether or how often a topic was addressed.
Physicians’ empathy scores are moderate
Physicians had a moderate score for Empathy (mean=3.8, standard deviation [SD]=1.5, on 7-point scale), a low score for MI Spirit (mean=2.4, standard deviation [SD]=1.4, on 7-point scale), and displayed fewer MI-adherent behaviors than MI-nonadherent behaviors (mean=0.4, SD=0.3). These means did not differ significantly based on the patients’ weight.
Weight loss conversations linked to patients’ readiness
The discussion of weight-related topics, and the time spent doing so, were related to patients’ readiness to lose weight after their initial examination, when patients’ baseline readiness to lose weight was controlled. The more ready patients were to lose weight after their visit, the more likely they had discussed weight (Spearman’s rank correlation coefficient [r]=.52, P=.01) and spent more time discussing weight (r=.42, P=.05). No other associations were statistically significant (TABLE W1).
Several of the Motivational Interviewing scores predicted patients’ outcomes. When physicians showed more empathy, patients were more likely to report changing their exercise patterns 1 month after the visit (r=.50, P=.02). When physicians displayed more of an MI Spirit, patients were more likely to be ready to lose weight (r=.63, P=.005) and change their exercise patterns (r=.47, P=.04). Further, when physicians used more MI-adherent techniques, patients were more likely to attempt to lose weight (r=.42, P=.08).
Discussion: Good quality discussions lead to change
While more discussion about weight loss led to a greater readiness to lose weight, it was the quality of the discussions that actually led to behavior changes. Most patients had virtually the same levels of readiness to lose weight before and after the visit. It is likely that patients who were ready to lose weight discussed their weight with their physicians—and spent more time discussing it than those patients who were not ready to lose weight.
How patients and physicians discussed weight influenced behavior change. When physicians were more empathic and used techniques consistent with Motivational Interviewing, patients were more likely to report changing their exercise routine and attempting to lose weight.
To date, no one has examined the effect of physicians’ MI techniques on weight-related behavior change in a large study. The low adherence to MI techniques suggests that physicians can improve their counseling skills.
Patients aren’t afraid to talk about their weight
Unexpectedly, patients were more likely than physicians to initiate weight-related discussions. Only one third of the time did physicians raise the topic. Patients appear to be “empowered” to initiate discussions about weight loss. We expected physicians and patients to both be somewhat apprehensive about raising this sensitive topic. However, these findings suggest that overweight and obese patients will initiate the discussion most of the time.
Limitations and strengths of this study
The small sample size limited the analyses. Nonetheless, we found strong correlations in this sample that suggest true relationships that were unlikely to have occurred by chance. Also, we were unable to conduct nested analyses to account for the clustering of patients seen by the same physicians. The results may not generalize to settings outside of academic medical centers and practices in which physicians have less time to spend with patients.
The physicians in this study were not overweight, which could limit the generalizability of the results. Patients may be less likely to raise the topic of weight with physicians who were themselves overweight. In addition, while we assessed single-item outcomes, more objective and extensive standard measures of diet, physical activity, and weight loss would have been optimal.
Some notable strengths of this study were that we used a comprehensive multimodal measurement in assessing both content and style of conversations in addition to patient self-report. We also examined Motivational Interviewing techniques among physicians with little or no MI training; most studies have examined MI among trained counselors only.
How to talk about weight loss: More study is needed
The most commonly addressed weight-related topics were diet and physical activity. However, when looking at the topics that were discussed, we found no patterns between those who attempted to lose weight and those who didn’t. This may mean that because weight loss is such a complex behavior, mention of any aspect of it—be it physical activity, diet, psychosocial issues, and so on—helps patients in their efforts. It also could be that the physician and patient discussed some other aspects in a previous visit; therefore, it was the cumulative effect of many conversations that influenced the patient to change.
These results need to be explored in a larger study to understand whether discussing certain topics is more influential than discussing others in promoting weight loss.
Acknowledgments
We thank Miranda West, Laura Fish, and Mary Sochaki for their work on this project. We are also grateful to the physicians and patients who agreed to have their encounters audio recorded.
Funding
This work was supported by National Cancer Institute grant 2P50 CA68438-06A2. The authors were supported in part by National Cancer Institute grants R01CA089053, R01CA100387, and National Institute of Diabetes and Digestive and Kidney Disorders grant R01DK64986.
CorrespondenceKathryn I. Pollak, PhD, Duke Comprehensive Cancer Center, Cancer Prevention, Detection and Control Research Program, 2424 Erwin Road, Room 6029, Hock Plaza I, Suite 602, Durham, NC 27705; kathryn.pollak@duke.edu.
1. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med 2000;31:652-657.
2. Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med 2000;160:2334-2339.
3. Mehrotra C, Naimi TS, Serdula M, Bolen J, Pearson K. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med 2004;27:16-21.
4. National Center for Chronic Disease Prevention and Health Promotion. 2001 BRFSS Summary Prevalence Report. Bethesda, Md: CDC; 2001.
5. Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med 2000;132:697-704.
6. Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med 2001;20:68-74.
7. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
8. Glasgow RE, Whitlock EP, Eakin EG, Lichtenstein E. A brief smoking cessation intervention for women in low-income planned parenthood clinics. Am J Pub Health 2000;90:786-789.
9. Valanis B, Lichtenstein E, Mullooly JP, et al. Maternal smoking cessation and relapse prevention during health care visits. Am J Prev Med 2001;20:1-8.
10. Stotts AL, Diclemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav 2002;27:275-292.
11. Stotts AL, DeLaune KA, Schmitz JM, Grabowski J. Impact of a motivational intervention on mechanisms of change in low-income pregnant smokers. Addict Behav 2004;29:1649-1657.
12. National Heart Lung and Blood Institute. Obesity Education Initiative Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH publication no. 98-4083. Bethesda, MD: National Institutes of Health; 1998.
13. O’Connell D, Velicer WF. A decision balance measure and the stages of change model of weight loss. Int J Addict 1988;23:729-750.
14. Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Substance Abuse Treat 2005;28:19-26.
- A physician’s empathy, collaborative approach, and words of support can have a positive effect on overweight and obese women’s weight loss efforts.
Purpose This study explores how weight-related topics are discussed between physicians and their overweight and obese female patients.
Methods We surveyed and audio-recorded preventive health and chronic care visits with 25 overweight and obese female patients. We coded both for quantity (content and time) of weight-related discussions and quality (adherence to Motivational Interviewing [MI] techniques). We then tested correlations of these measures with patients’ reported attempts to lose weight, change diet, and change exercise patterns 1 month after the visit.
Results Weight was routinely addressed (19 of 25 encounters). Patients usually initiated the topic (67% of time). Physicians’ use of MI techniques resulted in patients attempting to lose weight and changing their exercise patterns.
Conclusion Physicians may benefit from MI training to help patients lose weight.
Research has shown that when physicians advise overweight patients to lose weight, improve their diet, or increase their physical activity, patients are more likely to report attempting to do so.1-3 In a study of 433 primary care patients, 46% reported trying to lose weight after their physician counseled them about nutrition, compared with 37% who were not counseled.1
The reality, though, is that physicians are not very likely to address weight loss. Data from the Behavioral Risk Factor Surveillance System indicate that patients report their providers address weight loss in fewer than 20% of their examinations.4 These low rates are concerning; when physicians do not advise patients to lose weight, patients may believe their weight is not a problem.5 Even more worrisome: Physicians are rarely trained on how to counsel patients about weight loss. So, when physicians do counsel patients, it may not be effective.
Using Motivational Interviewing
One effective style of counseling is Motivational Interviewing (MI). MI is a patient-centered, directive counseling style used to help patients explore and resolve their ambivalence related to a particular behavior change (see What is Motivational Interviewing?).6,7 Researchers have studied the use of MI by counselors and case managers (in handling smoking cessation),8-11 but not by physicians. Further, no one has examined whether physicians instinctively use MI techniques when discussing weight loss with their patients, or whether MI counseling results in patients trying to lose weight.
The primary aim of this study was to assess how overweight and obese female patients discuss weight loss with their physicians. We also wanted to explore the role that physicians’ way of discussing weight loss—and the use of MI in particular—might play in their patients’ motivation to lose weight.
Motivational Interviewing is a counseling style intended to create changes in behavior by helping patients to explore and resolve their ambivalence.7 In a patient-physician encounter guided by MI:
- The motivation to change comes from the patient.
- It is the patient’s job to articulate and resolve his or her ambivalence.
- Direct persuasion is not used; the physician is quiet and eliciting, but directive in helping the patient examine his or her ambivalence.
- Readiness for change is recognized not as a patient trait, but as a part of the interaction between physician and patient.
- The patient-physician relationship is regarded more like a partnership.
Methods
Setting and recruitment
All data were collected in a family practice clinic within Duke University Medical Center. We approached 9 physicians in the practice to participate, and all consented. Only 7 physicians had visits with overweight or obese patients and were included in this report. We reviewed their electronic patient appointment schedules twice a week to identify female patients meeting the following criteria: English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), 40 years of age or older, and with health maintenance or chronic care appointments scheduled at least 7 days later. We sent these patients a letter describing the study, and allowed them 7 days to call a toll-free number if they didn’t want to participate.
We took several steps to avoid priming physicians and patients about the purpose of the study. First, both physicians and patients were told the study was about how doctors and patients discuss preventive health topics—they were not told the study was about examining discussions of weight. Second, we surveyed physicians 1 month prior to audio-recording visits, and patients 1 week prior to their visit. Third, we included measures for other preventive health topics (eg, smoking and alcohol) to detract attention from weight.
Gathering data
1. Phone survey before patient visit. We telephoned those patients who did not refuse participation and conducted a baseline survey. We asked about date of birth, race, marital status, level of education, income, weight, height, history of weight loss attempts, and whether this was their first visit with that physician. We categorized women with a BMI ≥25 but <30 as overweight, and those with a BMI ≥30 as obese.12
We also assessed each patient’s
- self-efficacy—that is, confidence in their ability to lose weight. We asked: “How confident are you that you can lose weight?” (1=not at all confident, 5=extremely confident).
- readiness to lose weight. We asked: “Are you seriously considering trying to losing weight within the next 6 months?” and, if yes, “Are you planning to try to lose weight in the next 30 days?”13 Those not considering trying to lose weight were staged as precontemplation; those who were considering trying but not planning to try in the next 30 days were staged as contemplation; and those who were planning to try to lose weight in the next 30 days were staged as preparation.
2. Office visit. When patients came in for their appointments, the research assistant gave them consent forms to sign. The assistant then escorted the patient to the examination rooms and started the digital audio recorder. The exams typically took 27 minutes.
Immediately following the exam, the research assistant surveyed the patients. The assistant asked 2 questions we’d asked at baseline: “How confident are you that you can lose weight?” and “Are you seriously considering trying to losing weight within the next 6 months?” (If yes, “Are you planning to try to lose weight in the next 30 days?”) She also made an appointment to conduct a 1-month follow-up telephone survey.
3. One-month follow-up survey. During a follow-up phone survey, we asked patients whether they had attempted to lose weight by changing their diet, exercise patterns, or both. Subsequent to this call, we sent the study participants a $25 check.
Analyzing the patient-physician discussion
Content. Two authors coded 9 topics that physicians and patients discussed that were “weight-related.” Topics included: physical activity, diet, BMI, psychosocial issues, referral to a nutritionist, weight loss surgery, goal setting, weight loss medications, and health care avoidance. We also coded who first brought up the topic.
Time spent. We calculated time spent discussing weight-related topics and also the total time of the patient’s visit.
Motivational Interviewing. Two coders assessed MI. To assess fidelity to MI principles, we used sections of the Motivational Interviewing Treatment Integrity scale (MITI)14 to rate patient interactions on a scale of 1 (low) to 7 (high) in 2 categories: empathy and MI spirit.
- Empathy is when physicians convey understanding of patients’ perspective.
- MI spirit includes evocation, collaboration, and autonomy. Evocation is when physicians draw out patients’ own reasons for change. Collaboration is when physicians act as partners, supporting and exploring patients’ concerns. Autonomy is when physicians convey that decisions to change lie completely with patients. Inter-rater reliability for the Empathy and MI Spirit was adequate (ICC=.94 and .97, respectively).
- MI-adherent behaviors were those where the physician asked permission to do things, affirmed statements, offered words of support, and emphasized patient control. For instance, the physician might say, “It’s great that you have stopped drinking sweetened tea” or “Whether you lose weight is up to you.”
- MI-nonadherent behaviors were those where the physician advised without asking permission. For example, the physician might say, “Let me tell you what you need to do to make this work…” or “Well, if you want to continue on the way you are, you know your diabetes is only going to get worse.”
These were combined to create a ratio of percentage MI-adherent behaviors by dividing MI-adherent by MI-nonadherent. There was an excellent level of agreement between coders for MI-nonadherent (kappa=.80) and a moderate level of agreement for MI-adherent (kappa=.52) behaviors.
Data analysis
We used Spearman correlations to assess the relationship between our predictors, quantity (time spent and whether weight was addressed) and quality (MI techniques), and mediators of behavior change (readiness to lose weight and self-efficacy to lose weight) and behavior change (attempts to lose weight, change in diet, and change in exercise patterns). We used SAS 9.1 (SAS Institute, Inc, Cary, NC) for all analyses. The study was approved by the Duke University Medical Center Institutional Review Board.
Results
We identified 202 eligible female patients. Of those, 96 had appointments that passed before we could contact them; 11 called the 800 number to refuse. Of the remaining 95 women, we reached 94 by phone. Of those, 19 refused to participate, 46 were ineligible because we had reached the targeted number of women in their weight category, and 4 skipped their appointments. Thus, we audio-recorded 25 encounters (for 14 obese and 11 overweight patients). Of these 25 patients, 24 completed the 1-month follow-up.
Patient demographics. Patients had a mean age of 59 years (standard deviation [SD]=11). Half were white; 42% were college-educated. Forty-two percent reported being in poor to fair health (TABLE 1).
The typical participant was moderately confident and ready to lose weight both before and after their visit. One month after their visit, 63% reported attempting to lose weight. More than half attempted to change their diet (67%); slightly more than half changed their exercise patterns (58%) (TABLE 2).
Physician demographics. Physicians had a mean age of 43 years (SD=10). About half were white; about half were female. No physicians were overweight.
TABLE 1
Characteristics of patients and physicians
| CHARACTERISTIC | PATIENT (N=25) | PHYSICIAN (N=7) |
|---|---|---|
| Age (M, SD) | 59 (11) | 43 (10) |
| Race (%)* | ||
| White | 50 | 57 |
| Black | 50 | 29 |
| Indian | 14 | |
| Female (%) | 100 | 57 |
| Married (%) | 46 | — |
| Employed (%) | 54 | 100 |
| College graduate (%) | 42 | 100 |
| Health status, self-reported (%) | ||
| Poor to fair | 42 | — |
| Good | 37 | — |
| Very good to excellent | 21 | — |
| Times lost at least 10 lbs (mean, SD) | 5.8 (4.0) | — |
| New patient with physician (%) | 12 | — |
| Body mass index (mean, SD) | 37 (11) | 22 (3) |
| * One participant did not provide his/her race. | ||
TABLE 2
Feeling about weight loss before and after the visit
| BASELINE | POST-VISIT | 1 MONTH | |
|---|---|---|---|
| Mediators of behavior change | |||
| Confidence in losing weight (M, SD)* | 3.8 (1.4) | 3.8 (1.1) | – |
| Stage of readiness to lose weight (%) | |||
| Precontemplation | 25% | 28% | – |
| Contemplation | 8% | 8% | – |
| Preparation | 67% | 64% | – |
| Behavior change variables | |||
| Attempted to lose weight (%) | – | – | 63% |
| Attempted to change diet (%) | – | – | 67% |
| Changed exercise patterns (%) | – | – | 58% |
| * Scale ranged from 1=not at all confident to 5=extremely confident. | |||
Patients were more likely to raise the weight issue
Weight-related topics were addressed in 19 of the 25 encounters (11 out of 12 preventive health visits, 8 out of 13 chronic care visits). The mean time spent discussing weight-related topics was 6.9 minutes out of an mean total of 27.0 minutes, or 26% of the total patient-physician time. Weight was more likely to be addressed with obese patients (86%) than with overweight patients (63%).
Patients were more likely than physicians to initiate discussions on weight. Physicians raised weight-related topics 37% of the time. Obese patients were slightly more likely to raise weight-related topics (8 out of 12 times [67%]) than overweight patients (4 out of 7 times [57%]).
The weight-related topics addressed were, in order from most to least frequent: physical activity, diet, BMI, psychosocial issues (eg, motivation to lose weight, triggers for unhealthful eating [such as family cookouts], negative talk [such as telling oneself that losing weight is too hard]), referral to a nutritionist, weight loss surgery, goal setting, health care avoidance, and weight loss medication. When comparing those who attempted to lose weight (n=15) with those who did not (n=9), there was no significant difference in whether or how often a topic was addressed.
Physicians’ empathy scores are moderate
Physicians had a moderate score for Empathy (mean=3.8, standard deviation [SD]=1.5, on 7-point scale), a low score for MI Spirit (mean=2.4, standard deviation [SD]=1.4, on 7-point scale), and displayed fewer MI-adherent behaviors than MI-nonadherent behaviors (mean=0.4, SD=0.3). These means did not differ significantly based on the patients’ weight.
Weight loss conversations linked to patients’ readiness
The discussion of weight-related topics, and the time spent doing so, were related to patients’ readiness to lose weight after their initial examination, when patients’ baseline readiness to lose weight was controlled. The more ready patients were to lose weight after their visit, the more likely they had discussed weight (Spearman’s rank correlation coefficient [r]=.52, P=.01) and spent more time discussing weight (r=.42, P=.05). No other associations were statistically significant (TABLE W1).
Several of the Motivational Interviewing scores predicted patients’ outcomes. When physicians showed more empathy, patients were more likely to report changing their exercise patterns 1 month after the visit (r=.50, P=.02). When physicians displayed more of an MI Spirit, patients were more likely to be ready to lose weight (r=.63, P=.005) and change their exercise patterns (r=.47, P=.04). Further, when physicians used more MI-adherent techniques, patients were more likely to attempt to lose weight (r=.42, P=.08).
Discussion: Good quality discussions lead to change
While more discussion about weight loss led to a greater readiness to lose weight, it was the quality of the discussions that actually led to behavior changes. Most patients had virtually the same levels of readiness to lose weight before and after the visit. It is likely that patients who were ready to lose weight discussed their weight with their physicians—and spent more time discussing it than those patients who were not ready to lose weight.
How patients and physicians discussed weight influenced behavior change. When physicians were more empathic and used techniques consistent with Motivational Interviewing, patients were more likely to report changing their exercise routine and attempting to lose weight.
To date, no one has examined the effect of physicians’ MI techniques on weight-related behavior change in a large study. The low adherence to MI techniques suggests that physicians can improve their counseling skills.
Patients aren’t afraid to talk about their weight
Unexpectedly, patients were more likely than physicians to initiate weight-related discussions. Only one third of the time did physicians raise the topic. Patients appear to be “empowered” to initiate discussions about weight loss. We expected physicians and patients to both be somewhat apprehensive about raising this sensitive topic. However, these findings suggest that overweight and obese patients will initiate the discussion most of the time.
Limitations and strengths of this study
The small sample size limited the analyses. Nonetheless, we found strong correlations in this sample that suggest true relationships that were unlikely to have occurred by chance. Also, we were unable to conduct nested analyses to account for the clustering of patients seen by the same physicians. The results may not generalize to settings outside of academic medical centers and practices in which physicians have less time to spend with patients.
The physicians in this study were not overweight, which could limit the generalizability of the results. Patients may be less likely to raise the topic of weight with physicians who were themselves overweight. In addition, while we assessed single-item outcomes, more objective and extensive standard measures of diet, physical activity, and weight loss would have been optimal.
Some notable strengths of this study were that we used a comprehensive multimodal measurement in assessing both content and style of conversations in addition to patient self-report. We also examined Motivational Interviewing techniques among physicians with little or no MI training; most studies have examined MI among trained counselors only.
How to talk about weight loss: More study is needed
The most commonly addressed weight-related topics were diet and physical activity. However, when looking at the topics that were discussed, we found no patterns between those who attempted to lose weight and those who didn’t. This may mean that because weight loss is such a complex behavior, mention of any aspect of it—be it physical activity, diet, psychosocial issues, and so on—helps patients in their efforts. It also could be that the physician and patient discussed some other aspects in a previous visit; therefore, it was the cumulative effect of many conversations that influenced the patient to change.
These results need to be explored in a larger study to understand whether discussing certain topics is more influential than discussing others in promoting weight loss.
Acknowledgments
We thank Miranda West, Laura Fish, and Mary Sochaki for their work on this project. We are also grateful to the physicians and patients who agreed to have their encounters audio recorded.
Funding
This work was supported by National Cancer Institute grant 2P50 CA68438-06A2. The authors were supported in part by National Cancer Institute grants R01CA089053, R01CA100387, and National Institute of Diabetes and Digestive and Kidney Disorders grant R01DK64986.
CorrespondenceKathryn I. Pollak, PhD, Duke Comprehensive Cancer Center, Cancer Prevention, Detection and Control Research Program, 2424 Erwin Road, Room 6029, Hock Plaza I, Suite 602, Durham, NC 27705; kathryn.pollak@duke.edu.
- A physician’s empathy, collaborative approach, and words of support can have a positive effect on overweight and obese women’s weight loss efforts.
Purpose This study explores how weight-related topics are discussed between physicians and their overweight and obese female patients.
Methods We surveyed and audio-recorded preventive health and chronic care visits with 25 overweight and obese female patients. We coded both for quantity (content and time) of weight-related discussions and quality (adherence to Motivational Interviewing [MI] techniques). We then tested correlations of these measures with patients’ reported attempts to lose weight, change diet, and change exercise patterns 1 month after the visit.
Results Weight was routinely addressed (19 of 25 encounters). Patients usually initiated the topic (67% of time). Physicians’ use of MI techniques resulted in patients attempting to lose weight and changing their exercise patterns.
Conclusion Physicians may benefit from MI training to help patients lose weight.
Research has shown that when physicians advise overweight patients to lose weight, improve their diet, or increase their physical activity, patients are more likely to report attempting to do so.1-3 In a study of 433 primary care patients, 46% reported trying to lose weight after their physician counseled them about nutrition, compared with 37% who were not counseled.1
The reality, though, is that physicians are not very likely to address weight loss. Data from the Behavioral Risk Factor Surveillance System indicate that patients report their providers address weight loss in fewer than 20% of their examinations.4 These low rates are concerning; when physicians do not advise patients to lose weight, patients may believe their weight is not a problem.5 Even more worrisome: Physicians are rarely trained on how to counsel patients about weight loss. So, when physicians do counsel patients, it may not be effective.
Using Motivational Interviewing
One effective style of counseling is Motivational Interviewing (MI). MI is a patient-centered, directive counseling style used to help patients explore and resolve their ambivalence related to a particular behavior change (see What is Motivational Interviewing?).6,7 Researchers have studied the use of MI by counselors and case managers (in handling smoking cessation),8-11 but not by physicians. Further, no one has examined whether physicians instinctively use MI techniques when discussing weight loss with their patients, or whether MI counseling results in patients trying to lose weight.
The primary aim of this study was to assess how overweight and obese female patients discuss weight loss with their physicians. We also wanted to explore the role that physicians’ way of discussing weight loss—and the use of MI in particular—might play in their patients’ motivation to lose weight.
Motivational Interviewing is a counseling style intended to create changes in behavior by helping patients to explore and resolve their ambivalence.7 In a patient-physician encounter guided by MI:
- The motivation to change comes from the patient.
- It is the patient’s job to articulate and resolve his or her ambivalence.
- Direct persuasion is not used; the physician is quiet and eliciting, but directive in helping the patient examine his or her ambivalence.
- Readiness for change is recognized not as a patient trait, but as a part of the interaction between physician and patient.
- The patient-physician relationship is regarded more like a partnership.
Methods
Setting and recruitment
All data were collected in a family practice clinic within Duke University Medical Center. We approached 9 physicians in the practice to participate, and all consented. Only 7 physicians had visits with overweight or obese patients and were included in this report. We reviewed their electronic patient appointment schedules twice a week to identify female patients meeting the following criteria: English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), 40 years of age or older, and with health maintenance or chronic care appointments scheduled at least 7 days later. We sent these patients a letter describing the study, and allowed them 7 days to call a toll-free number if they didn’t want to participate.
We took several steps to avoid priming physicians and patients about the purpose of the study. First, both physicians and patients were told the study was about how doctors and patients discuss preventive health topics—they were not told the study was about examining discussions of weight. Second, we surveyed physicians 1 month prior to audio-recording visits, and patients 1 week prior to their visit. Third, we included measures for other preventive health topics (eg, smoking and alcohol) to detract attention from weight.
Gathering data
1. Phone survey before patient visit. We telephoned those patients who did not refuse participation and conducted a baseline survey. We asked about date of birth, race, marital status, level of education, income, weight, height, history of weight loss attempts, and whether this was their first visit with that physician. We categorized women with a BMI ≥25 but <30 as overweight, and those with a BMI ≥30 as obese.12
We also assessed each patient’s
- self-efficacy—that is, confidence in their ability to lose weight. We asked: “How confident are you that you can lose weight?” (1=not at all confident, 5=extremely confident).
- readiness to lose weight. We asked: “Are you seriously considering trying to losing weight within the next 6 months?” and, if yes, “Are you planning to try to lose weight in the next 30 days?”13 Those not considering trying to lose weight were staged as precontemplation; those who were considering trying but not planning to try in the next 30 days were staged as contemplation; and those who were planning to try to lose weight in the next 30 days were staged as preparation.
2. Office visit. When patients came in for their appointments, the research assistant gave them consent forms to sign. The assistant then escorted the patient to the examination rooms and started the digital audio recorder. The exams typically took 27 minutes.
Immediately following the exam, the research assistant surveyed the patients. The assistant asked 2 questions we’d asked at baseline: “How confident are you that you can lose weight?” and “Are you seriously considering trying to losing weight within the next 6 months?” (If yes, “Are you planning to try to lose weight in the next 30 days?”) She also made an appointment to conduct a 1-month follow-up telephone survey.
3. One-month follow-up survey. During a follow-up phone survey, we asked patients whether they had attempted to lose weight by changing their diet, exercise patterns, or both. Subsequent to this call, we sent the study participants a $25 check.
Analyzing the patient-physician discussion
Content. Two authors coded 9 topics that physicians and patients discussed that were “weight-related.” Topics included: physical activity, diet, BMI, psychosocial issues, referral to a nutritionist, weight loss surgery, goal setting, weight loss medications, and health care avoidance. We also coded who first brought up the topic.
Time spent. We calculated time spent discussing weight-related topics and also the total time of the patient’s visit.
Motivational Interviewing. Two coders assessed MI. To assess fidelity to MI principles, we used sections of the Motivational Interviewing Treatment Integrity scale (MITI)14 to rate patient interactions on a scale of 1 (low) to 7 (high) in 2 categories: empathy and MI spirit.
- Empathy is when physicians convey understanding of patients’ perspective.
- MI spirit includes evocation, collaboration, and autonomy. Evocation is when physicians draw out patients’ own reasons for change. Collaboration is when physicians act as partners, supporting and exploring patients’ concerns. Autonomy is when physicians convey that decisions to change lie completely with patients. Inter-rater reliability for the Empathy and MI Spirit was adequate (ICC=.94 and .97, respectively).
- MI-adherent behaviors were those where the physician asked permission to do things, affirmed statements, offered words of support, and emphasized patient control. For instance, the physician might say, “It’s great that you have stopped drinking sweetened tea” or “Whether you lose weight is up to you.”
- MI-nonadherent behaviors were those where the physician advised without asking permission. For example, the physician might say, “Let me tell you what you need to do to make this work…” or “Well, if you want to continue on the way you are, you know your diabetes is only going to get worse.”
These were combined to create a ratio of percentage MI-adherent behaviors by dividing MI-adherent by MI-nonadherent. There was an excellent level of agreement between coders for MI-nonadherent (kappa=.80) and a moderate level of agreement for MI-adherent (kappa=.52) behaviors.
Data analysis
We used Spearman correlations to assess the relationship between our predictors, quantity (time spent and whether weight was addressed) and quality (MI techniques), and mediators of behavior change (readiness to lose weight and self-efficacy to lose weight) and behavior change (attempts to lose weight, change in diet, and change in exercise patterns). We used SAS 9.1 (SAS Institute, Inc, Cary, NC) for all analyses. The study was approved by the Duke University Medical Center Institutional Review Board.
Results
We identified 202 eligible female patients. Of those, 96 had appointments that passed before we could contact them; 11 called the 800 number to refuse. Of the remaining 95 women, we reached 94 by phone. Of those, 19 refused to participate, 46 were ineligible because we had reached the targeted number of women in their weight category, and 4 skipped their appointments. Thus, we audio-recorded 25 encounters (for 14 obese and 11 overweight patients). Of these 25 patients, 24 completed the 1-month follow-up.
Patient demographics. Patients had a mean age of 59 years (standard deviation [SD]=11). Half were white; 42% were college-educated. Forty-two percent reported being in poor to fair health (TABLE 1).
The typical participant was moderately confident and ready to lose weight both before and after their visit. One month after their visit, 63% reported attempting to lose weight. More than half attempted to change their diet (67%); slightly more than half changed their exercise patterns (58%) (TABLE 2).
Physician demographics. Physicians had a mean age of 43 years (SD=10). About half were white; about half were female. No physicians were overweight.
TABLE 1
Characteristics of patients and physicians
| CHARACTERISTIC | PATIENT (N=25) | PHYSICIAN (N=7) |
|---|---|---|
| Age (M, SD) | 59 (11) | 43 (10) |
| Race (%)* | ||
| White | 50 | 57 |
| Black | 50 | 29 |
| Indian | 14 | |
| Female (%) | 100 | 57 |
| Married (%) | 46 | — |
| Employed (%) | 54 | 100 |
| College graduate (%) | 42 | 100 |
| Health status, self-reported (%) | ||
| Poor to fair | 42 | — |
| Good | 37 | — |
| Very good to excellent | 21 | — |
| Times lost at least 10 lbs (mean, SD) | 5.8 (4.0) | — |
| New patient with physician (%) | 12 | — |
| Body mass index (mean, SD) | 37 (11) | 22 (3) |
| * One participant did not provide his/her race. | ||
TABLE 2
Feeling about weight loss before and after the visit
| BASELINE | POST-VISIT | 1 MONTH | |
|---|---|---|---|
| Mediators of behavior change | |||
| Confidence in losing weight (M, SD)* | 3.8 (1.4) | 3.8 (1.1) | – |
| Stage of readiness to lose weight (%) | |||
| Precontemplation | 25% | 28% | – |
| Contemplation | 8% | 8% | – |
| Preparation | 67% | 64% | – |
| Behavior change variables | |||
| Attempted to lose weight (%) | – | – | 63% |
| Attempted to change diet (%) | – | – | 67% |
| Changed exercise patterns (%) | – | – | 58% |
| * Scale ranged from 1=not at all confident to 5=extremely confident. | |||
Patients were more likely to raise the weight issue
Weight-related topics were addressed in 19 of the 25 encounters (11 out of 12 preventive health visits, 8 out of 13 chronic care visits). The mean time spent discussing weight-related topics was 6.9 minutes out of an mean total of 27.0 minutes, or 26% of the total patient-physician time. Weight was more likely to be addressed with obese patients (86%) than with overweight patients (63%).
Patients were more likely than physicians to initiate discussions on weight. Physicians raised weight-related topics 37% of the time. Obese patients were slightly more likely to raise weight-related topics (8 out of 12 times [67%]) than overweight patients (4 out of 7 times [57%]).
The weight-related topics addressed were, in order from most to least frequent: physical activity, diet, BMI, psychosocial issues (eg, motivation to lose weight, triggers for unhealthful eating [such as family cookouts], negative talk [such as telling oneself that losing weight is too hard]), referral to a nutritionist, weight loss surgery, goal setting, health care avoidance, and weight loss medication. When comparing those who attempted to lose weight (n=15) with those who did not (n=9), there was no significant difference in whether or how often a topic was addressed.
Physicians’ empathy scores are moderate
Physicians had a moderate score for Empathy (mean=3.8, standard deviation [SD]=1.5, on 7-point scale), a low score for MI Spirit (mean=2.4, standard deviation [SD]=1.4, on 7-point scale), and displayed fewer MI-adherent behaviors than MI-nonadherent behaviors (mean=0.4, SD=0.3). These means did not differ significantly based on the patients’ weight.
Weight loss conversations linked to patients’ readiness
The discussion of weight-related topics, and the time spent doing so, were related to patients’ readiness to lose weight after their initial examination, when patients’ baseline readiness to lose weight was controlled. The more ready patients were to lose weight after their visit, the more likely they had discussed weight (Spearman’s rank correlation coefficient [r]=.52, P=.01) and spent more time discussing weight (r=.42, P=.05). No other associations were statistically significant (TABLE W1).
Several of the Motivational Interviewing scores predicted patients’ outcomes. When physicians showed more empathy, patients were more likely to report changing their exercise patterns 1 month after the visit (r=.50, P=.02). When physicians displayed more of an MI Spirit, patients were more likely to be ready to lose weight (r=.63, P=.005) and change their exercise patterns (r=.47, P=.04). Further, when physicians used more MI-adherent techniques, patients were more likely to attempt to lose weight (r=.42, P=.08).
Discussion: Good quality discussions lead to change
While more discussion about weight loss led to a greater readiness to lose weight, it was the quality of the discussions that actually led to behavior changes. Most patients had virtually the same levels of readiness to lose weight before and after the visit. It is likely that patients who were ready to lose weight discussed their weight with their physicians—and spent more time discussing it than those patients who were not ready to lose weight.
How patients and physicians discussed weight influenced behavior change. When physicians were more empathic and used techniques consistent with Motivational Interviewing, patients were more likely to report changing their exercise routine and attempting to lose weight.
To date, no one has examined the effect of physicians’ MI techniques on weight-related behavior change in a large study. The low adherence to MI techniques suggests that physicians can improve their counseling skills.
Patients aren’t afraid to talk about their weight
Unexpectedly, patients were more likely than physicians to initiate weight-related discussions. Only one third of the time did physicians raise the topic. Patients appear to be “empowered” to initiate discussions about weight loss. We expected physicians and patients to both be somewhat apprehensive about raising this sensitive topic. However, these findings suggest that overweight and obese patients will initiate the discussion most of the time.
Limitations and strengths of this study
The small sample size limited the analyses. Nonetheless, we found strong correlations in this sample that suggest true relationships that were unlikely to have occurred by chance. Also, we were unable to conduct nested analyses to account for the clustering of patients seen by the same physicians. The results may not generalize to settings outside of academic medical centers and practices in which physicians have less time to spend with patients.
The physicians in this study were not overweight, which could limit the generalizability of the results. Patients may be less likely to raise the topic of weight with physicians who were themselves overweight. In addition, while we assessed single-item outcomes, more objective and extensive standard measures of diet, physical activity, and weight loss would have been optimal.
Some notable strengths of this study were that we used a comprehensive multimodal measurement in assessing both content and style of conversations in addition to patient self-report. We also examined Motivational Interviewing techniques among physicians with little or no MI training; most studies have examined MI among trained counselors only.
How to talk about weight loss: More study is needed
The most commonly addressed weight-related topics were diet and physical activity. However, when looking at the topics that were discussed, we found no patterns between those who attempted to lose weight and those who didn’t. This may mean that because weight loss is such a complex behavior, mention of any aspect of it—be it physical activity, diet, psychosocial issues, and so on—helps patients in their efforts. It also could be that the physician and patient discussed some other aspects in a previous visit; therefore, it was the cumulative effect of many conversations that influenced the patient to change.
These results need to be explored in a larger study to understand whether discussing certain topics is more influential than discussing others in promoting weight loss.
Acknowledgments
We thank Miranda West, Laura Fish, and Mary Sochaki for their work on this project. We are also grateful to the physicians and patients who agreed to have their encounters audio recorded.
Funding
This work was supported by National Cancer Institute grant 2P50 CA68438-06A2. The authors were supported in part by National Cancer Institute grants R01CA089053, R01CA100387, and National Institute of Diabetes and Digestive and Kidney Disorders grant R01DK64986.
CorrespondenceKathryn I. Pollak, PhD, Duke Comprehensive Cancer Center, Cancer Prevention, Detection and Control Research Program, 2424 Erwin Road, Room 6029, Hock Plaza I, Suite 602, Durham, NC 27705; kathryn.pollak@duke.edu.
1. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med 2000;31:652-657.
2. Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med 2000;160:2334-2339.
3. Mehrotra C, Naimi TS, Serdula M, Bolen J, Pearson K. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med 2004;27:16-21.
4. National Center for Chronic Disease Prevention and Health Promotion. 2001 BRFSS Summary Prevalence Report. Bethesda, Md: CDC; 2001.
5. Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med 2000;132:697-704.
6. Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med 2001;20:68-74.
7. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
8. Glasgow RE, Whitlock EP, Eakin EG, Lichtenstein E. A brief smoking cessation intervention for women in low-income planned parenthood clinics. Am J Pub Health 2000;90:786-789.
9. Valanis B, Lichtenstein E, Mullooly JP, et al. Maternal smoking cessation and relapse prevention during health care visits. Am J Prev Med 2001;20:1-8.
10. Stotts AL, Diclemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav 2002;27:275-292.
11. Stotts AL, DeLaune KA, Schmitz JM, Grabowski J. Impact of a motivational intervention on mechanisms of change in low-income pregnant smokers. Addict Behav 2004;29:1649-1657.
12. National Heart Lung and Blood Institute. Obesity Education Initiative Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH publication no. 98-4083. Bethesda, MD: National Institutes of Health; 1998.
13. O’Connell D, Velicer WF. A decision balance measure and the stages of change model of weight loss. Int J Addict 1988;23:729-750.
14. Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Substance Abuse Treat 2005;28:19-26.
1. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med 2000;31:652-657.
2. Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med 2000;160:2334-2339.
3. Mehrotra C, Naimi TS, Serdula M, Bolen J, Pearson K. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med 2004;27:16-21.
4. National Center for Chronic Disease Prevention and Health Promotion. 2001 BRFSS Summary Prevalence Report. Bethesda, Md: CDC; 2001.
5. Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med 2000;132:697-704.
6. Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med 2001;20:68-74.
7. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
8. Glasgow RE, Whitlock EP, Eakin EG, Lichtenstein E. A brief smoking cessation intervention for women in low-income planned parenthood clinics. Am J Pub Health 2000;90:786-789.
9. Valanis B, Lichtenstein E, Mullooly JP, et al. Maternal smoking cessation and relapse prevention during health care visits. Am J Prev Med 2001;20:1-8.
10. Stotts AL, Diclemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav 2002;27:275-292.
11. Stotts AL, DeLaune KA, Schmitz JM, Grabowski J. Impact of a motivational intervention on mechanisms of change in low-income pregnant smokers. Addict Behav 2004;29:1649-1657.
12. National Heart Lung and Blood Institute. Obesity Education Initiative Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH publication no. 98-4083. Bethesda, MD: National Institutes of Health; 1998.
13. O’Connell D, Velicer WF. A decision balance measure and the stages of change model of weight loss. Int J Addict 1988;23:729-750.
14. Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Substance Abuse Treat 2005;28:19-26.
Transdermal rivastigmine for dementia
The rivastigmine patch is the first transdermal treatment for symptoms of mild to moderate Alzheimer’s disease (AD) and mild to moderate Parkinson’s disease dementia (Table). Rivastigmine, a cholinesterase inhibitor, is the only therapy approved for both indications.
Table
Rivastigmine transdermal patch: Fast facts
| Brand name: Exelon Patch |
| Class: Cholinesterase inhibitor |
| Indication: Symptomatic treatment of mild to moderate Alzheimer’s-type dementia and mild to moderate dementia associated with Parkinson’s disease |
| Manufacturer: Novartis Pharmaceuticals, Inc. |
| Dosing forms: 4.6 and 9.5 mg/24 hours transdermal patches (5 cm2 and 10 cm2, respectively) |
| Recommended dosage: Start with 4.6 mg/24 hours patch for ≥4 weeks, followed by a one-step increase to the target dose 9.5 mg/24 hours patch* |
| *Unless the patient is taking oral rivastigmine (see ‘Transitioning to rivastigmine patch,’) |
Clinical implications
The rivastigmine patch offers continuous drug delivery through the skin into the bloodstream over 24 hours.1 This may reduce the incidence of side effects compared with oral rivastigmine,2 making optimal therapeutic doses easier to attain.3 The target dose 9.5 mg/24 hours patch provides efficacy similar to the highest recommended rivastigmine capsule dose (6 mg bid for a total of 12 mg/d).2
How it works
The rivastigmine patch uses matrix technology, which enables delivery of a large amount of drug from a small surface area.4 The patch is available in 2 dosage forms:
- a 5-cm2 size containing 9 mg of rivastigmine that delivers 4.6 mg/24 hours
- a 10-cm2 size containing 18 mg of rivastigmine that delivers 9.5 mg/24 hours.
Each patch consists of 4 layers: the backing layer, an acrylic drug matrix, a silicone adhesive matrix, and an overlapping release liner that is removed and discarded before the patch is applied.1
Cholinesterase inhibitors are believed to exert their effects by increasing available levels of the neurotransmitter acetylcholine in the brain. Two studies have demonstrated that cognitive improvements associated with rivastigmine treatment correlate significantly with cholinesterase inhibition.5,6 In 1 study, rivastigmine’s inhibitory effects on cholinesterase were sustained for 12 months.6
Pharmacokinetics
Rivastigmine is metabolized by its target cholinesterase enzymes to the decarbamylated metabolite NAP 226-90, which has minimal acetylcholinesterase inhibition and is excreted through the urine.1 As a result of its low accumulation potential and cytochrome P 450-independent metabolism, rivastigmine has low potential for pharmacokinetic drug–drug interactions. This lack of interaction has been confirmed for many drugs commonly taken by elderly patients, such as digoxin, nonsteroidal anti-inflammatory drugs, and estrogens.7
Rivastigmine has a half-life of 1 to 2 hours, so it is rapidly cleared.8 In the event of a serious reaction, significant clearance of rivastigmine from the body would occur within 3 hours of patch removal.
Centrally mediated cholinergic gastrointestinal (GI) side effects associated with oral rivastigmine are related to high maximum plasma concentrations (Cmax) and short time interval to Cmax (Tmax).9 In an open-label, parallel-group study of 51 AD patients that compared rivastigmine patches with rivastigmine capsules, transdermal administration was associated with slower increases to lower peak plasma concentrations (prolonged Tmax and reduced Cmax), and less fluctuation in plasma concentration.1 Despite these effects, the rivastigmine 9.5 mg/24 hours patch provided drug exposure comparable to the highest dose of capsules (6 mg bid for a total of 12 mg/d), with improved GI tolerability.3
Efficacy
Rivastigmine patch efficacy was evaluated in a single, 24-week, international, randomized, double-blind trial of 1,195 patients with AD.2 The study group represented typical patients with mild to moderate AD—age 50 to 85 years with Mini-Mental State Examination scores of 10 to 20 at baseline. Patients were randomly assigned to receive:
- 17.4 mg/24 hours rivastigmine patch (20-cm2 patch; n=303)
- 9.5 mg/24 hours rivastigmine patch (10-cm2 patch; n=293)
- 6 mg bid rivastigmine capsules (n=297)
- or placebo (n=302).
Data for the 17.4 mg/24 hours patch are not discussed here because this dose exceeds the FDA-approved maximum dosage (9.5 mg/24 hours) and is not available.
Patients in the 9.5 mg/24 hours patch group received a 4.6 mg/24 hours patch (5 cm2) for weeks 1 through 4, and then the 9.5 mg/24 hours patch for the remainder of the study. Patients in the capsule group started on 3 mg/d (1.5 mg bid) and were titrated every 4 weeks in steps of 3 mg/d to a maximum of 12 mg/d administered as 6 mg bid.
Primary outcomes were measured as mean change in score from baseline to endpoint on the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) and Alzheimer’s Disease Co-operative Study–Clinical Global Impression of Change (ADCS-CGIC). By study endpoint, the 9.5 mg/24 hours patch and capsules, 12 mg/d, showed comparable efficacy (Figure).2 Compared with those receiving placebo, patients in the 9.5 mg/24 hours patch and capsule groups showed significant improvements in dementia symptoms, including:
- cognition
- global performance
- attention
- activities of daily living.2
Based on my clinical experience, these improvements reflect small but clinically meaningful changes that are noted by patients and caregivers.
Figure
Efficacy of transdermal rivastigmine for Alzheimer’s symptoms
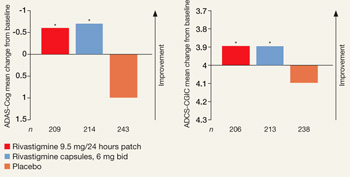
*P<0.05 vs placebo
ADAS-Cog: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; ADCS-CGIC: Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change
Source: Adapted from reference 2
In a 24-week study, transdermal rivastigmine, 9.5 mg/24 hours, and the highest recommended dose of oral rivastigmine (6 mg bid) showed comparable efficacy as measured by mean change in score on scales commonly used in Alzheimer’s disease clinical trials. ADAS-Cog assesses orientation, memory, language, praxis, and visuospatial functions. ADCS-CGIC provides a single global rating of change from baseline based on interviews with the patient and caregiver.
Safety and tolerability
Adverse events associated with rivastigmine are predominantly cholinergic; GI side effects—nausea, vomiting, and diarrhea—are observed most frequently.2 These events occur less frequently with the patch than with capsules. In the efficacy trial, patients in the 9.5 mg/24 hours rivastigmine patch group had one-third as many reports of nausea (7.2% vs 23.1%) and vomiting (6.2% vs 17.0%) compared with the 6 mg bid capsule group.2
Diarrhea was reported by 6% of subjects receiving the 9.5 mg/24 hours patch, 5% of those taking 6-mg capsule bid, and 3% receiving placebo. Fewer subjects in the 9.5 mg/24 hours patch group (3%) experienced decreased weight compared with those in the capsule group (5%). The rate of decreased weight with placebo was 1%.
Dizziness affected 2% of those in the 9.5 mg/24 hours patch and placebo groups; incidence in the capsule group was significantly higher at 8%. Headache was similar with the 9.5 mg/24 hours patch (3%) and placebo (2%), with the capsule significantly higher at 6%.2
The proportion of patients who experienced no, slight, or mild skin irritation ranged from 90% to 98%.2 The most commonly reported moderate or severe skin irritations were erythema (8% rivastigmine patch vs 4% placebo) and pruritus (7% rivastigmine patch vs 3% placebo). Two percent of patients using active patch discontinued the trial because of skin irritation.
Rivastigmine appears not to produce adverse effects on cardiac function as assessed by ECG. In clinical trials of 2,791 patients, pooled 12-lead ECG data comparing oral rivastigmine and placebo groups did not differ significantly in heart rate or PR, QRS, and QTc intervals.10
Dosing
The rivastigmine patch is administered once daily, and the recommended maintenance dose is the 9.5 mg/24 hours patch. Start patients on a 4.6 mg/24 hours patch for at least 4 weeks and then increase to the 9.5 mg/24 hours target dose if the lower dose is well tolerated.
Dosage adjustment of rivastigmine is not necessary in patients with hepatic or renal disease because of minimal liver metabolism and the acetylcholinesterase-mediated hydrolysis of rivastigmine to the inactive decarbamylated metabolite NAP 226-90, which is excreted in the urine.11
Instruct patients or caregivers to apply the patch to clean, dry, hairless skin that is free of cuts, rashes, or irritation on the upper or lower back or upper arm or chest.1 The patch has shown good adhesive properties over 24 hours, remaining attached in a range of situations, including bathing and hot weather.2 In the 9.5 mg/24 hours group of the efficacy study, 96% of patches remained attached or had slight lifting of the edges (1,336 total patch evaluations).
Transitioning to rivastigmine patch
The efficacy study included an open-label extension, during which blinding was maintained. This provided information on patients beginning rivastigmine patch therapy directly from placebo2 or transitioning from rivastigmine capsules to the target dose 9.5 mg/24 hours patch.12 Based on these results, transition patients as follows:
- Patients taking oral rivastigmine, <6 mg/d: Switch to a 4.6 mg/24 hours patch for ≥4 weeks before increasing to a 9.5 mg/24 hours patch.
- Patients taking oral rivastigmine, 6 to 12 mg/d: Switch directly to a 9.5 mg/24 hours patch.
Apply the first patch the day after the last oral dose.
Related resource
- Rivastigmine transdermal system prescribing information. www.pharma.us.novartis.com/product/pi/pdf/exelonpatch.pdf.
Drug brand names
- Digoxin • Lanoxin
- Rivastigmine • Exelon
- Rivastigmine transdermal
- system • Exelon Patch
Disclosure
Dr. Sadowsky is a consultant to and speaker for Forest Pharmaceuticals and Novartis Pharmaceuticals.
Acknowledgment
The author thanks Christina Mackins, PhD, a medical writer for Alpha-Plus Medical Communications Ltd, for her editorial assistance with this article. Funding for her work was provided by Novartis Pharmaceuticals.
1. Lefèvre G, Sedek G, Jhee S, et al. Pharmacokinetics and pharmacodynamics of the novel daily rivastigmine transdermal patch compared with twice-daily capsules in Alzheimer’s disease patients. J Clin Pharmacol 2007;47:471-8.
2. Winblad B, Cummings J, Andreasen N, et al. A six-month, double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer’s disease—rivastigmine patch versus capsule. Int J Geriatr Psychiatry 2007;22:456-67.
3. Oertel W, Ross JS, Eggert K, Adler G. Rationale for transdermal drug administration in Alzheimer disease. Neurology 2007;69(suppl 1):S4-S9.
4. Petersen TA. Transdermal drug formulations and process development. Pharmaceut Technol 2003;(suppl):18-21.
5. Giacobini E, Spiegel R, Enz A, et al. Inhibition of acetyl- and butyryl-cholinesterase in the cerebrospinal fluid of patients with Alzheimer’s disease by rivastigmine: correlation with cognitive benefit. J Neural Transm 2002;109:1053-65.
6. Darreh-Shori T, Almkvist O, Guan ZZ, et al. Sustained cholinesterase inhibition in AD patients receiving rivastigmine for 12 months. Neurology 2002;59:563-72.
7. Grossberg GT, Stahelin HB, Messina JC, et al. Lack of adverse pharmacodynamic drug interactions with rivastigmine and twenty-two classes of medications. Int J Geriatr Psychiatry 2000;15(3):242-7.
8. Polinsky RJ. Clinical pharmacology of rivastigmine: a new-generation acetylcholinesterase inhibitor for the treatment of Alzheimer’s disease. Clin Ther 1998;20:634-47.
9. Jann MW, Shirley KL, Small GW. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin Pharmacokinet 2002;41:719-39.
10. Morganroth J, Graham S, Hartman R, et al. Electrocardiographic effects of rivastigmine. J Clin Pharmacol 2002;42:558-68.
11. Exelon patch [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2007.
12. Frölich L, Barone P, Förstl H, et al. IDEAL: A 28-week open-label extension of a 24-week double-blind study of the first transdermal patch in Alzheimer’s disease. Poster presented at: 11th Congress of the European Federation of Neurological Societies; August 25-28, 2007; Brussels, Belgium.
Dr. Sadowsky is associate clinical professor of neurology, Nova Southeastern University, Fort Lauderdale, FL, and director, Premier Research Institute, Palm Beach Neurology, West Palm Beach, FL.
The rivastigmine patch is the first transdermal treatment for symptoms of mild to moderate Alzheimer’s disease (AD) and mild to moderate Parkinson’s disease dementia (Table). Rivastigmine, a cholinesterase inhibitor, is the only therapy approved for both indications.
Table
Rivastigmine transdermal patch: Fast facts
| Brand name: Exelon Patch |
| Class: Cholinesterase inhibitor |
| Indication: Symptomatic treatment of mild to moderate Alzheimer’s-type dementia and mild to moderate dementia associated with Parkinson’s disease |
| Manufacturer: Novartis Pharmaceuticals, Inc. |
| Dosing forms: 4.6 and 9.5 mg/24 hours transdermal patches (5 cm2 and 10 cm2, respectively) |
| Recommended dosage: Start with 4.6 mg/24 hours patch for ≥4 weeks, followed by a one-step increase to the target dose 9.5 mg/24 hours patch* |
| *Unless the patient is taking oral rivastigmine (see ‘Transitioning to rivastigmine patch,’) |
Clinical implications
The rivastigmine patch offers continuous drug delivery through the skin into the bloodstream over 24 hours.1 This may reduce the incidence of side effects compared with oral rivastigmine,2 making optimal therapeutic doses easier to attain.3 The target dose 9.5 mg/24 hours patch provides efficacy similar to the highest recommended rivastigmine capsule dose (6 mg bid for a total of 12 mg/d).2
How it works
The rivastigmine patch uses matrix technology, which enables delivery of a large amount of drug from a small surface area.4 The patch is available in 2 dosage forms:
- a 5-cm2 size containing 9 mg of rivastigmine that delivers 4.6 mg/24 hours
- a 10-cm2 size containing 18 mg of rivastigmine that delivers 9.5 mg/24 hours.
Each patch consists of 4 layers: the backing layer, an acrylic drug matrix, a silicone adhesive matrix, and an overlapping release liner that is removed and discarded before the patch is applied.1
Cholinesterase inhibitors are believed to exert their effects by increasing available levels of the neurotransmitter acetylcholine in the brain. Two studies have demonstrated that cognitive improvements associated with rivastigmine treatment correlate significantly with cholinesterase inhibition.5,6 In 1 study, rivastigmine’s inhibitory effects on cholinesterase were sustained for 12 months.6
Pharmacokinetics
Rivastigmine is metabolized by its target cholinesterase enzymes to the decarbamylated metabolite NAP 226-90, which has minimal acetylcholinesterase inhibition and is excreted through the urine.1 As a result of its low accumulation potential and cytochrome P 450-independent metabolism, rivastigmine has low potential for pharmacokinetic drug–drug interactions. This lack of interaction has been confirmed for many drugs commonly taken by elderly patients, such as digoxin, nonsteroidal anti-inflammatory drugs, and estrogens.7
Rivastigmine has a half-life of 1 to 2 hours, so it is rapidly cleared.8 In the event of a serious reaction, significant clearance of rivastigmine from the body would occur within 3 hours of patch removal.
Centrally mediated cholinergic gastrointestinal (GI) side effects associated with oral rivastigmine are related to high maximum plasma concentrations (Cmax) and short time interval to Cmax (Tmax).9 In an open-label, parallel-group study of 51 AD patients that compared rivastigmine patches with rivastigmine capsules, transdermal administration was associated with slower increases to lower peak plasma concentrations (prolonged Tmax and reduced Cmax), and less fluctuation in plasma concentration.1 Despite these effects, the rivastigmine 9.5 mg/24 hours patch provided drug exposure comparable to the highest dose of capsules (6 mg bid for a total of 12 mg/d), with improved GI tolerability.3
Efficacy
Rivastigmine patch efficacy was evaluated in a single, 24-week, international, randomized, double-blind trial of 1,195 patients with AD.2 The study group represented typical patients with mild to moderate AD—age 50 to 85 years with Mini-Mental State Examination scores of 10 to 20 at baseline. Patients were randomly assigned to receive:
- 17.4 mg/24 hours rivastigmine patch (20-cm2 patch; n=303)
- 9.5 mg/24 hours rivastigmine patch (10-cm2 patch; n=293)
- 6 mg bid rivastigmine capsules (n=297)
- or placebo (n=302).
Data for the 17.4 mg/24 hours patch are not discussed here because this dose exceeds the FDA-approved maximum dosage (9.5 mg/24 hours) and is not available.
Patients in the 9.5 mg/24 hours patch group received a 4.6 mg/24 hours patch (5 cm2) for weeks 1 through 4, and then the 9.5 mg/24 hours patch for the remainder of the study. Patients in the capsule group started on 3 mg/d (1.5 mg bid) and were titrated every 4 weeks in steps of 3 mg/d to a maximum of 12 mg/d administered as 6 mg bid.
Primary outcomes were measured as mean change in score from baseline to endpoint on the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) and Alzheimer’s Disease Co-operative Study–Clinical Global Impression of Change (ADCS-CGIC). By study endpoint, the 9.5 mg/24 hours patch and capsules, 12 mg/d, showed comparable efficacy (Figure).2 Compared with those receiving placebo, patients in the 9.5 mg/24 hours patch and capsule groups showed significant improvements in dementia symptoms, including:
- cognition
- global performance
- attention
- activities of daily living.2
Based on my clinical experience, these improvements reflect small but clinically meaningful changes that are noted by patients and caregivers.
Figure
Efficacy of transdermal rivastigmine for Alzheimer’s symptoms
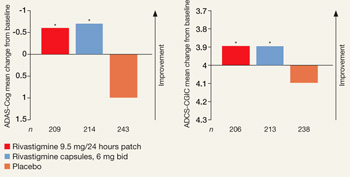
*P<0.05 vs placebo
ADAS-Cog: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; ADCS-CGIC: Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change
Source: Adapted from reference 2
In a 24-week study, transdermal rivastigmine, 9.5 mg/24 hours, and the highest recommended dose of oral rivastigmine (6 mg bid) showed comparable efficacy as measured by mean change in score on scales commonly used in Alzheimer’s disease clinical trials. ADAS-Cog assesses orientation, memory, language, praxis, and visuospatial functions. ADCS-CGIC provides a single global rating of change from baseline based on interviews with the patient and caregiver.
Safety and tolerability
Adverse events associated with rivastigmine are predominantly cholinergic; GI side effects—nausea, vomiting, and diarrhea—are observed most frequently.2 These events occur less frequently with the patch than with capsules. In the efficacy trial, patients in the 9.5 mg/24 hours rivastigmine patch group had one-third as many reports of nausea (7.2% vs 23.1%) and vomiting (6.2% vs 17.0%) compared with the 6 mg bid capsule group.2
Diarrhea was reported by 6% of subjects receiving the 9.5 mg/24 hours patch, 5% of those taking 6-mg capsule bid, and 3% receiving placebo. Fewer subjects in the 9.5 mg/24 hours patch group (3%) experienced decreased weight compared with those in the capsule group (5%). The rate of decreased weight with placebo was 1%.
Dizziness affected 2% of those in the 9.5 mg/24 hours patch and placebo groups; incidence in the capsule group was significantly higher at 8%. Headache was similar with the 9.5 mg/24 hours patch (3%) and placebo (2%), with the capsule significantly higher at 6%.2
The proportion of patients who experienced no, slight, or mild skin irritation ranged from 90% to 98%.2 The most commonly reported moderate or severe skin irritations were erythema (8% rivastigmine patch vs 4% placebo) and pruritus (7% rivastigmine patch vs 3% placebo). Two percent of patients using active patch discontinued the trial because of skin irritation.
Rivastigmine appears not to produce adverse effects on cardiac function as assessed by ECG. In clinical trials of 2,791 patients, pooled 12-lead ECG data comparing oral rivastigmine and placebo groups did not differ significantly in heart rate or PR, QRS, and QTc intervals.10
Dosing
The rivastigmine patch is administered once daily, and the recommended maintenance dose is the 9.5 mg/24 hours patch. Start patients on a 4.6 mg/24 hours patch for at least 4 weeks and then increase to the 9.5 mg/24 hours target dose if the lower dose is well tolerated.
Dosage adjustment of rivastigmine is not necessary in patients with hepatic or renal disease because of minimal liver metabolism and the acetylcholinesterase-mediated hydrolysis of rivastigmine to the inactive decarbamylated metabolite NAP 226-90, which is excreted in the urine.11
Instruct patients or caregivers to apply the patch to clean, dry, hairless skin that is free of cuts, rashes, or irritation on the upper or lower back or upper arm or chest.1 The patch has shown good adhesive properties over 24 hours, remaining attached in a range of situations, including bathing and hot weather.2 In the 9.5 mg/24 hours group of the efficacy study, 96% of patches remained attached or had slight lifting of the edges (1,336 total patch evaluations).
Transitioning to rivastigmine patch
The efficacy study included an open-label extension, during which blinding was maintained. This provided information on patients beginning rivastigmine patch therapy directly from placebo2 or transitioning from rivastigmine capsules to the target dose 9.5 mg/24 hours patch.12 Based on these results, transition patients as follows:
- Patients taking oral rivastigmine, <6 mg/d: Switch to a 4.6 mg/24 hours patch for ≥4 weeks before increasing to a 9.5 mg/24 hours patch.
- Patients taking oral rivastigmine, 6 to 12 mg/d: Switch directly to a 9.5 mg/24 hours patch.
Apply the first patch the day after the last oral dose.
Related resource
- Rivastigmine transdermal system prescribing information. www.pharma.us.novartis.com/product/pi/pdf/exelonpatch.pdf.
Drug brand names
- Digoxin • Lanoxin
- Rivastigmine • Exelon
- Rivastigmine transdermal
- system • Exelon Patch
Disclosure
Dr. Sadowsky is a consultant to and speaker for Forest Pharmaceuticals and Novartis Pharmaceuticals.
Acknowledgment
The author thanks Christina Mackins, PhD, a medical writer for Alpha-Plus Medical Communications Ltd, for her editorial assistance with this article. Funding for her work was provided by Novartis Pharmaceuticals.
The rivastigmine patch is the first transdermal treatment for symptoms of mild to moderate Alzheimer’s disease (AD) and mild to moderate Parkinson’s disease dementia (Table). Rivastigmine, a cholinesterase inhibitor, is the only therapy approved for both indications.
Table
Rivastigmine transdermal patch: Fast facts
| Brand name: Exelon Patch |
| Class: Cholinesterase inhibitor |
| Indication: Symptomatic treatment of mild to moderate Alzheimer’s-type dementia and mild to moderate dementia associated with Parkinson’s disease |
| Manufacturer: Novartis Pharmaceuticals, Inc. |
| Dosing forms: 4.6 and 9.5 mg/24 hours transdermal patches (5 cm2 and 10 cm2, respectively) |
| Recommended dosage: Start with 4.6 mg/24 hours patch for ≥4 weeks, followed by a one-step increase to the target dose 9.5 mg/24 hours patch* |
| *Unless the patient is taking oral rivastigmine (see ‘Transitioning to rivastigmine patch,’) |
Clinical implications
The rivastigmine patch offers continuous drug delivery through the skin into the bloodstream over 24 hours.1 This may reduce the incidence of side effects compared with oral rivastigmine,2 making optimal therapeutic doses easier to attain.3 The target dose 9.5 mg/24 hours patch provides efficacy similar to the highest recommended rivastigmine capsule dose (6 mg bid for a total of 12 mg/d).2
How it works
The rivastigmine patch uses matrix technology, which enables delivery of a large amount of drug from a small surface area.4 The patch is available in 2 dosage forms:
- a 5-cm2 size containing 9 mg of rivastigmine that delivers 4.6 mg/24 hours
- a 10-cm2 size containing 18 mg of rivastigmine that delivers 9.5 mg/24 hours.
Each patch consists of 4 layers: the backing layer, an acrylic drug matrix, a silicone adhesive matrix, and an overlapping release liner that is removed and discarded before the patch is applied.1
Cholinesterase inhibitors are believed to exert their effects by increasing available levels of the neurotransmitter acetylcholine in the brain. Two studies have demonstrated that cognitive improvements associated with rivastigmine treatment correlate significantly with cholinesterase inhibition.5,6 In 1 study, rivastigmine’s inhibitory effects on cholinesterase were sustained for 12 months.6
Pharmacokinetics
Rivastigmine is metabolized by its target cholinesterase enzymes to the decarbamylated metabolite NAP 226-90, which has minimal acetylcholinesterase inhibition and is excreted through the urine.1 As a result of its low accumulation potential and cytochrome P 450-independent metabolism, rivastigmine has low potential for pharmacokinetic drug–drug interactions. This lack of interaction has been confirmed for many drugs commonly taken by elderly patients, such as digoxin, nonsteroidal anti-inflammatory drugs, and estrogens.7
Rivastigmine has a half-life of 1 to 2 hours, so it is rapidly cleared.8 In the event of a serious reaction, significant clearance of rivastigmine from the body would occur within 3 hours of patch removal.
Centrally mediated cholinergic gastrointestinal (GI) side effects associated with oral rivastigmine are related to high maximum plasma concentrations (Cmax) and short time interval to Cmax (Tmax).9 In an open-label, parallel-group study of 51 AD patients that compared rivastigmine patches with rivastigmine capsules, transdermal administration was associated with slower increases to lower peak plasma concentrations (prolonged Tmax and reduced Cmax), and less fluctuation in plasma concentration.1 Despite these effects, the rivastigmine 9.5 mg/24 hours patch provided drug exposure comparable to the highest dose of capsules (6 mg bid for a total of 12 mg/d), with improved GI tolerability.3
Efficacy
Rivastigmine patch efficacy was evaluated in a single, 24-week, international, randomized, double-blind trial of 1,195 patients with AD.2 The study group represented typical patients with mild to moderate AD—age 50 to 85 years with Mini-Mental State Examination scores of 10 to 20 at baseline. Patients were randomly assigned to receive:
- 17.4 mg/24 hours rivastigmine patch (20-cm2 patch; n=303)
- 9.5 mg/24 hours rivastigmine patch (10-cm2 patch; n=293)
- 6 mg bid rivastigmine capsules (n=297)
- or placebo (n=302).
Data for the 17.4 mg/24 hours patch are not discussed here because this dose exceeds the FDA-approved maximum dosage (9.5 mg/24 hours) and is not available.
Patients in the 9.5 mg/24 hours patch group received a 4.6 mg/24 hours patch (5 cm2) for weeks 1 through 4, and then the 9.5 mg/24 hours patch for the remainder of the study. Patients in the capsule group started on 3 mg/d (1.5 mg bid) and were titrated every 4 weeks in steps of 3 mg/d to a maximum of 12 mg/d administered as 6 mg bid.
Primary outcomes were measured as mean change in score from baseline to endpoint on the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) and Alzheimer’s Disease Co-operative Study–Clinical Global Impression of Change (ADCS-CGIC). By study endpoint, the 9.5 mg/24 hours patch and capsules, 12 mg/d, showed comparable efficacy (Figure).2 Compared with those receiving placebo, patients in the 9.5 mg/24 hours patch and capsule groups showed significant improvements in dementia symptoms, including:
- cognition
- global performance
- attention
- activities of daily living.2
Based on my clinical experience, these improvements reflect small but clinically meaningful changes that are noted by patients and caregivers.
Figure
Efficacy of transdermal rivastigmine for Alzheimer’s symptoms
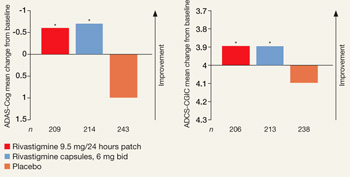
*P<0.05 vs placebo
ADAS-Cog: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; ADCS-CGIC: Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change
Source: Adapted from reference 2
In a 24-week study, transdermal rivastigmine, 9.5 mg/24 hours, and the highest recommended dose of oral rivastigmine (6 mg bid) showed comparable efficacy as measured by mean change in score on scales commonly used in Alzheimer’s disease clinical trials. ADAS-Cog assesses orientation, memory, language, praxis, and visuospatial functions. ADCS-CGIC provides a single global rating of change from baseline based on interviews with the patient and caregiver.
Safety and tolerability
Adverse events associated with rivastigmine are predominantly cholinergic; GI side effects—nausea, vomiting, and diarrhea—are observed most frequently.2 These events occur less frequently with the patch than with capsules. In the efficacy trial, patients in the 9.5 mg/24 hours rivastigmine patch group had one-third as many reports of nausea (7.2% vs 23.1%) and vomiting (6.2% vs 17.0%) compared with the 6 mg bid capsule group.2
Diarrhea was reported by 6% of subjects receiving the 9.5 mg/24 hours patch, 5% of those taking 6-mg capsule bid, and 3% receiving placebo. Fewer subjects in the 9.5 mg/24 hours patch group (3%) experienced decreased weight compared with those in the capsule group (5%). The rate of decreased weight with placebo was 1%.
Dizziness affected 2% of those in the 9.5 mg/24 hours patch and placebo groups; incidence in the capsule group was significantly higher at 8%. Headache was similar with the 9.5 mg/24 hours patch (3%) and placebo (2%), with the capsule significantly higher at 6%.2
The proportion of patients who experienced no, slight, or mild skin irritation ranged from 90% to 98%.2 The most commonly reported moderate or severe skin irritations were erythema (8% rivastigmine patch vs 4% placebo) and pruritus (7% rivastigmine patch vs 3% placebo). Two percent of patients using active patch discontinued the trial because of skin irritation.
Rivastigmine appears not to produce adverse effects on cardiac function as assessed by ECG. In clinical trials of 2,791 patients, pooled 12-lead ECG data comparing oral rivastigmine and placebo groups did not differ significantly in heart rate or PR, QRS, and QTc intervals.10
Dosing
The rivastigmine patch is administered once daily, and the recommended maintenance dose is the 9.5 mg/24 hours patch. Start patients on a 4.6 mg/24 hours patch for at least 4 weeks and then increase to the 9.5 mg/24 hours target dose if the lower dose is well tolerated.
Dosage adjustment of rivastigmine is not necessary in patients with hepatic or renal disease because of minimal liver metabolism and the acetylcholinesterase-mediated hydrolysis of rivastigmine to the inactive decarbamylated metabolite NAP 226-90, which is excreted in the urine.11
Instruct patients or caregivers to apply the patch to clean, dry, hairless skin that is free of cuts, rashes, or irritation on the upper or lower back or upper arm or chest.1 The patch has shown good adhesive properties over 24 hours, remaining attached in a range of situations, including bathing and hot weather.2 In the 9.5 mg/24 hours group of the efficacy study, 96% of patches remained attached or had slight lifting of the edges (1,336 total patch evaluations).
Transitioning to rivastigmine patch
The efficacy study included an open-label extension, during which blinding was maintained. This provided information on patients beginning rivastigmine patch therapy directly from placebo2 or transitioning from rivastigmine capsules to the target dose 9.5 mg/24 hours patch.12 Based on these results, transition patients as follows:
- Patients taking oral rivastigmine, <6 mg/d: Switch to a 4.6 mg/24 hours patch for ≥4 weeks before increasing to a 9.5 mg/24 hours patch.
- Patients taking oral rivastigmine, 6 to 12 mg/d: Switch directly to a 9.5 mg/24 hours patch.
Apply the first patch the day after the last oral dose.
Related resource
- Rivastigmine transdermal system prescribing information. www.pharma.us.novartis.com/product/pi/pdf/exelonpatch.pdf.
Drug brand names
- Digoxin • Lanoxin
- Rivastigmine • Exelon
- Rivastigmine transdermal
- system • Exelon Patch
Disclosure
Dr. Sadowsky is a consultant to and speaker for Forest Pharmaceuticals and Novartis Pharmaceuticals.
Acknowledgment
The author thanks Christina Mackins, PhD, a medical writer for Alpha-Plus Medical Communications Ltd, for her editorial assistance with this article. Funding for her work was provided by Novartis Pharmaceuticals.
1. Lefèvre G, Sedek G, Jhee S, et al. Pharmacokinetics and pharmacodynamics of the novel daily rivastigmine transdermal patch compared with twice-daily capsules in Alzheimer’s disease patients. J Clin Pharmacol 2007;47:471-8.
2. Winblad B, Cummings J, Andreasen N, et al. A six-month, double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer’s disease—rivastigmine patch versus capsule. Int J Geriatr Psychiatry 2007;22:456-67.
3. Oertel W, Ross JS, Eggert K, Adler G. Rationale for transdermal drug administration in Alzheimer disease. Neurology 2007;69(suppl 1):S4-S9.
4. Petersen TA. Transdermal drug formulations and process development. Pharmaceut Technol 2003;(suppl):18-21.
5. Giacobini E, Spiegel R, Enz A, et al. Inhibition of acetyl- and butyryl-cholinesterase in the cerebrospinal fluid of patients with Alzheimer’s disease by rivastigmine: correlation with cognitive benefit. J Neural Transm 2002;109:1053-65.
6. Darreh-Shori T, Almkvist O, Guan ZZ, et al. Sustained cholinesterase inhibition in AD patients receiving rivastigmine for 12 months. Neurology 2002;59:563-72.
7. Grossberg GT, Stahelin HB, Messina JC, et al. Lack of adverse pharmacodynamic drug interactions with rivastigmine and twenty-two classes of medications. Int J Geriatr Psychiatry 2000;15(3):242-7.
8. Polinsky RJ. Clinical pharmacology of rivastigmine: a new-generation acetylcholinesterase inhibitor for the treatment of Alzheimer’s disease. Clin Ther 1998;20:634-47.
9. Jann MW, Shirley KL, Small GW. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin Pharmacokinet 2002;41:719-39.
10. Morganroth J, Graham S, Hartman R, et al. Electrocardiographic effects of rivastigmine. J Clin Pharmacol 2002;42:558-68.
11. Exelon patch [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2007.
12. Frölich L, Barone P, Förstl H, et al. IDEAL: A 28-week open-label extension of a 24-week double-blind study of the first transdermal patch in Alzheimer’s disease. Poster presented at: 11th Congress of the European Federation of Neurological Societies; August 25-28, 2007; Brussels, Belgium.
Dr. Sadowsky is associate clinical professor of neurology, Nova Southeastern University, Fort Lauderdale, FL, and director, Premier Research Institute, Palm Beach Neurology, West Palm Beach, FL.
1. Lefèvre G, Sedek G, Jhee S, et al. Pharmacokinetics and pharmacodynamics of the novel daily rivastigmine transdermal patch compared with twice-daily capsules in Alzheimer’s disease patients. J Clin Pharmacol 2007;47:471-8.
2. Winblad B, Cummings J, Andreasen N, et al. A six-month, double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer’s disease—rivastigmine patch versus capsule. Int J Geriatr Psychiatry 2007;22:456-67.
3. Oertel W, Ross JS, Eggert K, Adler G. Rationale for transdermal drug administration in Alzheimer disease. Neurology 2007;69(suppl 1):S4-S9.
4. Petersen TA. Transdermal drug formulations and process development. Pharmaceut Technol 2003;(suppl):18-21.
5. Giacobini E, Spiegel R, Enz A, et al. Inhibition of acetyl- and butyryl-cholinesterase in the cerebrospinal fluid of patients with Alzheimer’s disease by rivastigmine: correlation with cognitive benefit. J Neural Transm 2002;109:1053-65.
6. Darreh-Shori T, Almkvist O, Guan ZZ, et al. Sustained cholinesterase inhibition in AD patients receiving rivastigmine for 12 months. Neurology 2002;59:563-72.
7. Grossberg GT, Stahelin HB, Messina JC, et al. Lack of adverse pharmacodynamic drug interactions with rivastigmine and twenty-two classes of medications. Int J Geriatr Psychiatry 2000;15(3):242-7.
8. Polinsky RJ. Clinical pharmacology of rivastigmine: a new-generation acetylcholinesterase inhibitor for the treatment of Alzheimer’s disease. Clin Ther 1998;20:634-47.
9. Jann MW, Shirley KL, Small GW. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin Pharmacokinet 2002;41:719-39.
10. Morganroth J, Graham S, Hartman R, et al. Electrocardiographic effects of rivastigmine. J Clin Pharmacol 2002;42:558-68.
11. Exelon patch [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2007.
12. Frölich L, Barone P, Förstl H, et al. IDEAL: A 28-week open-label extension of a 24-week double-blind study of the first transdermal patch in Alzheimer’s disease. Poster presented at: 11th Congress of the European Federation of Neurological Societies; August 25-28, 2007; Brussels, Belgium.
Dr. Sadowsky is associate clinical professor of neurology, Nova Southeastern University, Fort Lauderdale, FL, and director, Premier Research Institute, Palm Beach Neurology, West Palm Beach, FL.
How to protect patients’ confidentiality
Psychiatrist reveals patients’ information to another patient
Alameda County (CA) Superior Court
For several years 2 female patients were treated by the same psychiatrist. Jane Doe, age 56, read a breach of confidentiality report alleging sexual abuse filed by another patient of the psychiatrist. Jane Doe contacted the alleged victim, who informed her that the psychiatrist had disclosed information to her (the victim) regarding Jane Doe’s treatment, emotional problems, sexual preferences, and medication regimen.
Susan Doe, age 64, learned of the sexual abuse accusations against the psychiatrist in the same way and also contacted the alleged victim. She told Susan Doe that the psychiatrist had disclosed to her Susan Doe’s personal information regarding her dificult relationship with her daughter, depression, and instances when she stormed out of counseling sessions.
The patients brought separate claims, and their cases were later consolidated. The psychiatrist denied that he told the alleged sexual abuse victim details of the 2 patients’ treatments. The patients claimed that the victim could not have known their personal details unless the psychiatrist had told her.
- A jury returned a verdict in favor of the 2 patients. Jane Doe was awarded $225,000, and Susan Doe was awarded $47,000.
Dr. Grant’s observations
In the case of Jane Doe and Susan Doe, disclosing a patient’s personal information to another patient violates confidentiality. Patients must consent to the disclosure of information to third parties, and in this case these 2 patients apparently did not provide consent.
Medical practice—and particularly psychiatric practice—is based on the principle that communications between clinicians and patients are private. The Hippocratic oath states, “Whatever I see or hear in the lives of my patients, whether in connection with my professional practice or not, which ought not to be spoken of outside, I will keep secret, as considering all such things to be private.”1
According to the American Psychiatric Association’s (APA) code of ethics, “Psychiatric records, including even the identification of a person as a patient, must be protected with extreme care. Confidentiality is essential to psychiatric treatment, in part because of the special nature of psychiatric therapy. A psychiatrist may release confidential information only with the patient’s authorization or under proper legal compulsion.”2
Doctor-patient confidentiality is rooted in the belief that potential disclosure of information communicated during psychiatric diagnosis and treatment would discourage patients from seeking medical and mental health care (Table)
Table
Underlying values of confidentiality
| Proper doctor-patient confidentiality aims to: |
|
| Source: U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health, 1999. |
When to disclose
There are circumstances, however, that override the requirement to maintain confidentiality and do not need a patient’s consent. Examples include:3
Duty to protect third parties. In 1976 the California Supreme Court ruled in the landmark Tarasoff case4 that a psychiatrist has a duty to do what is reasonably necessary to protect third parties if a patient presents a serious risk of violence to another person. The specific applications of this principle are governed by other states’ laws, which have extended or limited this duty.5 Be familiar with the law in your jurisdiction before disclosing confidential information to third parties who may be at risk of violence.
The APA’s position on this exception is consistent with legal standards. Its code of ethics states, “When, in the clinical judgment of the treating psychiatrist, the risk of danger is deemed to be significant, the psychiatrist may reveal confidential information disclosed by the patient.”6
Emergency release of information. Psychiatrists can release confidential information during a medical emergency. Releasing the information must be in the patient’s best interests, and the patient’s inability to consent to the release should be the result of a potentially reversible condition that leads the clinician to question the patient’s capacity to consent.3
For example, if a patient in an emergency room is delirious because of ingesting an unknown substance and is unable to consent, a physician can call family members to ask about the patient’s medical problems. Notifying family that the patient is in the hospital could violate confidentiality, however.
Reporting abuse. All clinicians are obligated to report suspected child abuse or neglect. Some state laws also may require physicians to disclose abuse of vulnerable groups such as the elderly or the disabled and report to the local department of health diagnosis of communicable diseases such as HIV.3
Circle of confidentiality. Certain parties— including clinical staff on an inpatient unit or a psychiatrist supervising a resident— are considered to be within a circle of confidentiality.3 You do not need a patient’s consent to share clinical information with those within the circle of confidentiality. Do not release a patient’s information to parties who are not in the circle of confidentiality—such as family members, attorneys representing the patient, and law enforcement personnel—unless you’ve first obtained the patient’s consent.
Document the reasoning behind your decision to disclose your patient’s personal information without the patient’s consent. Show that you engaged in a reasonable clinical decision-making process.3 For example, record the risks and benefits of your decision and how you arrived at your conclusion.3
Other scenarios
Multidisciplinary teams. Members of a multidisciplinary treatment team—such as physicians, nurses, or social workers—should only receive confidential information that is relevant to the patient’s care. Other clinicians who are not involved in the case—although they may be seeing other patients on the same unit—should not have access to the patient’s confidential information. Discussions with these team members must be private so that others do not overhear confidential information.
Insurance companies generally are not party to the patient’s records unless the patient agrees to allow access by signing a release. If the patient’s refusal to allow disclosure results in the insurance company’s refusal to pay, then the patient is responsible for resolving the issue.7
Scientific publications and presentations. When you present a case report for a scientific publication or at a meeting, alter the patient’s biographical data so that someone who knows the patient would be unable to identify him or her based on the information in the case report. If the information is so specific that you cannot prevent patient identification, either do not publish the case or offer the patient the right to veto the manuscript’s distribution. If necessary, have the patient sign a consent form to allow publication or presentation of the case report.
Confidentiality violations
Breach of confidentiality may be intentional, such as disclosing a patient’s personal information to a third party as in this case, or unintentional, such as talking about a patient to a colleague and having someone overhear your discussion.8 Violating confidentiality may result in litigation for malpractice (negligence), invasion of privacy, or breach of contract, and ethical sanctions.8
No aspect of psychiatric practice seems to generate stronger emotions than the potential legal repercussions of our work. Keeping up with patients’ needs, billing issues, and advancements in medicine leaves little time for tracking changing state and federal laws or case precedents. For the past 4 years it has been my pleasure to provide information on the legal issues psychiatrists face and provide possible means of avoiding legal pitfalls.
Although I have decided to pursue other projects, I wish to give readers my thanks and to suggest resources—only a few among many great ones—that may be useful guides for a variety of legal issues.
Jon E. Grant, JD, MD, MPH
- Journal of the American Academy of Psychiatry and the Law.
- Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA:Harvard University Press; 1998.
- Simon RI, Shuman DW.Clinical manual of psychiatry and the law. Washington, DC: American Psychiatric Publishing, Inc. ; 2007.
Editor’s note
Current Psychiatry thanks Dr. Grant for writing the Malpractice Verdicts column since 2004. The column will continue in a new format in the February 2008 issue.
1. National Institutes of Health. The Hippocratic oath. Available at: http://www.nlm.nih.gov/hmd/greek/greek_oath.html. Accessed October 30, 2007.
2. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006: 6. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
3. Lowenthal D. Case studies in confidentiality. J Psychiatr Prac 2002;8:151-9.
4. Tarasoff vs Regents of the University of California 551P 2d 334 (Cal 1976).
5. Appelbaum PS Taras off and the clinician: problems in fulfilling the duty to protect. Am J Psychiatry 1985;142:425-9.
6. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006:7. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
7. Hilliard J. Liability issues with managed care. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:44-51.
8. Berner M. Write smarter, not longer. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:54-71.
Cases are selected by Current Psychiatry fromMedical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Psychiatrist reveals patients’ information to another patient
Alameda County (CA) Superior Court
For several years 2 female patients were treated by the same psychiatrist. Jane Doe, age 56, read a breach of confidentiality report alleging sexual abuse filed by another patient of the psychiatrist. Jane Doe contacted the alleged victim, who informed her that the psychiatrist had disclosed information to her (the victim) regarding Jane Doe’s treatment, emotional problems, sexual preferences, and medication regimen.
Susan Doe, age 64, learned of the sexual abuse accusations against the psychiatrist in the same way and also contacted the alleged victim. She told Susan Doe that the psychiatrist had disclosed to her Susan Doe’s personal information regarding her dificult relationship with her daughter, depression, and instances when she stormed out of counseling sessions.
The patients brought separate claims, and their cases were later consolidated. The psychiatrist denied that he told the alleged sexual abuse victim details of the 2 patients’ treatments. The patients claimed that the victim could not have known their personal details unless the psychiatrist had told her.
- A jury returned a verdict in favor of the 2 patients. Jane Doe was awarded $225,000, and Susan Doe was awarded $47,000.
Dr. Grant’s observations
In the case of Jane Doe and Susan Doe, disclosing a patient’s personal information to another patient violates confidentiality. Patients must consent to the disclosure of information to third parties, and in this case these 2 patients apparently did not provide consent.
Medical practice—and particularly psychiatric practice—is based on the principle that communications between clinicians and patients are private. The Hippocratic oath states, “Whatever I see or hear in the lives of my patients, whether in connection with my professional practice or not, which ought not to be spoken of outside, I will keep secret, as considering all such things to be private.”1
According to the American Psychiatric Association’s (APA) code of ethics, “Psychiatric records, including even the identification of a person as a patient, must be protected with extreme care. Confidentiality is essential to psychiatric treatment, in part because of the special nature of psychiatric therapy. A psychiatrist may release confidential information only with the patient’s authorization or under proper legal compulsion.”2
Doctor-patient confidentiality is rooted in the belief that potential disclosure of information communicated during psychiatric diagnosis and treatment would discourage patients from seeking medical and mental health care (Table)
Table
Underlying values of confidentiality
| Proper doctor-patient confidentiality aims to: |
|
| Source: U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health, 1999. |
When to disclose
There are circumstances, however, that override the requirement to maintain confidentiality and do not need a patient’s consent. Examples include:3
Duty to protect third parties. In 1976 the California Supreme Court ruled in the landmark Tarasoff case4 that a psychiatrist has a duty to do what is reasonably necessary to protect third parties if a patient presents a serious risk of violence to another person. The specific applications of this principle are governed by other states’ laws, which have extended or limited this duty.5 Be familiar with the law in your jurisdiction before disclosing confidential information to third parties who may be at risk of violence.
The APA’s position on this exception is consistent with legal standards. Its code of ethics states, “When, in the clinical judgment of the treating psychiatrist, the risk of danger is deemed to be significant, the psychiatrist may reveal confidential information disclosed by the patient.”6
Emergency release of information. Psychiatrists can release confidential information during a medical emergency. Releasing the information must be in the patient’s best interests, and the patient’s inability to consent to the release should be the result of a potentially reversible condition that leads the clinician to question the patient’s capacity to consent.3
For example, if a patient in an emergency room is delirious because of ingesting an unknown substance and is unable to consent, a physician can call family members to ask about the patient’s medical problems. Notifying family that the patient is in the hospital could violate confidentiality, however.
Reporting abuse. All clinicians are obligated to report suspected child abuse or neglect. Some state laws also may require physicians to disclose abuse of vulnerable groups such as the elderly or the disabled and report to the local department of health diagnosis of communicable diseases such as HIV.3
Circle of confidentiality. Certain parties— including clinical staff on an inpatient unit or a psychiatrist supervising a resident— are considered to be within a circle of confidentiality.3 You do not need a patient’s consent to share clinical information with those within the circle of confidentiality. Do not release a patient’s information to parties who are not in the circle of confidentiality—such as family members, attorneys representing the patient, and law enforcement personnel—unless you’ve first obtained the patient’s consent.
Document the reasoning behind your decision to disclose your patient’s personal information without the patient’s consent. Show that you engaged in a reasonable clinical decision-making process.3 For example, record the risks and benefits of your decision and how you arrived at your conclusion.3
Other scenarios
Multidisciplinary teams. Members of a multidisciplinary treatment team—such as physicians, nurses, or social workers—should only receive confidential information that is relevant to the patient’s care. Other clinicians who are not involved in the case—although they may be seeing other patients on the same unit—should not have access to the patient’s confidential information. Discussions with these team members must be private so that others do not overhear confidential information.
Insurance companies generally are not party to the patient’s records unless the patient agrees to allow access by signing a release. If the patient’s refusal to allow disclosure results in the insurance company’s refusal to pay, then the patient is responsible for resolving the issue.7
Scientific publications and presentations. When you present a case report for a scientific publication or at a meeting, alter the patient’s biographical data so that someone who knows the patient would be unable to identify him or her based on the information in the case report. If the information is so specific that you cannot prevent patient identification, either do not publish the case or offer the patient the right to veto the manuscript’s distribution. If necessary, have the patient sign a consent form to allow publication or presentation of the case report.
Confidentiality violations
Breach of confidentiality may be intentional, such as disclosing a patient’s personal information to a third party as in this case, or unintentional, such as talking about a patient to a colleague and having someone overhear your discussion.8 Violating confidentiality may result in litigation for malpractice (negligence), invasion of privacy, or breach of contract, and ethical sanctions.8
No aspect of psychiatric practice seems to generate stronger emotions than the potential legal repercussions of our work. Keeping up with patients’ needs, billing issues, and advancements in medicine leaves little time for tracking changing state and federal laws or case precedents. For the past 4 years it has been my pleasure to provide information on the legal issues psychiatrists face and provide possible means of avoiding legal pitfalls.
Although I have decided to pursue other projects, I wish to give readers my thanks and to suggest resources—only a few among many great ones—that may be useful guides for a variety of legal issues.
Jon E. Grant, JD, MD, MPH
- Journal of the American Academy of Psychiatry and the Law.
- Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA:Harvard University Press; 1998.
- Simon RI, Shuman DW.Clinical manual of psychiatry and the law. Washington, DC: American Psychiatric Publishing, Inc. ; 2007.
Editor’s note
Current Psychiatry thanks Dr. Grant for writing the Malpractice Verdicts column since 2004. The column will continue in a new format in the February 2008 issue.
Psychiatrist reveals patients’ information to another patient
Alameda County (CA) Superior Court
For several years 2 female patients were treated by the same psychiatrist. Jane Doe, age 56, read a breach of confidentiality report alleging sexual abuse filed by another patient of the psychiatrist. Jane Doe contacted the alleged victim, who informed her that the psychiatrist had disclosed information to her (the victim) regarding Jane Doe’s treatment, emotional problems, sexual preferences, and medication regimen.
Susan Doe, age 64, learned of the sexual abuse accusations against the psychiatrist in the same way and also contacted the alleged victim. She told Susan Doe that the psychiatrist had disclosed to her Susan Doe’s personal information regarding her dificult relationship with her daughter, depression, and instances when she stormed out of counseling sessions.
The patients brought separate claims, and their cases were later consolidated. The psychiatrist denied that he told the alleged sexual abuse victim details of the 2 patients’ treatments. The patients claimed that the victim could not have known their personal details unless the psychiatrist had told her.
- A jury returned a verdict in favor of the 2 patients. Jane Doe was awarded $225,000, and Susan Doe was awarded $47,000.
Dr. Grant’s observations
In the case of Jane Doe and Susan Doe, disclosing a patient’s personal information to another patient violates confidentiality. Patients must consent to the disclosure of information to third parties, and in this case these 2 patients apparently did not provide consent.
Medical practice—and particularly psychiatric practice—is based on the principle that communications between clinicians and patients are private. The Hippocratic oath states, “Whatever I see or hear in the lives of my patients, whether in connection with my professional practice or not, which ought not to be spoken of outside, I will keep secret, as considering all such things to be private.”1
According to the American Psychiatric Association’s (APA) code of ethics, “Psychiatric records, including even the identification of a person as a patient, must be protected with extreme care. Confidentiality is essential to psychiatric treatment, in part because of the special nature of psychiatric therapy. A psychiatrist may release confidential information only with the patient’s authorization or under proper legal compulsion.”2
Doctor-patient confidentiality is rooted in the belief that potential disclosure of information communicated during psychiatric diagnosis and treatment would discourage patients from seeking medical and mental health care (Table)
Table
Underlying values of confidentiality
| Proper doctor-patient confidentiality aims to: |
|
| Source: U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health, 1999. |
When to disclose
There are circumstances, however, that override the requirement to maintain confidentiality and do not need a patient’s consent. Examples include:3
Duty to protect third parties. In 1976 the California Supreme Court ruled in the landmark Tarasoff case4 that a psychiatrist has a duty to do what is reasonably necessary to protect third parties if a patient presents a serious risk of violence to another person. The specific applications of this principle are governed by other states’ laws, which have extended or limited this duty.5 Be familiar with the law in your jurisdiction before disclosing confidential information to third parties who may be at risk of violence.
The APA’s position on this exception is consistent with legal standards. Its code of ethics states, “When, in the clinical judgment of the treating psychiatrist, the risk of danger is deemed to be significant, the psychiatrist may reveal confidential information disclosed by the patient.”6
Emergency release of information. Psychiatrists can release confidential information during a medical emergency. Releasing the information must be in the patient’s best interests, and the patient’s inability to consent to the release should be the result of a potentially reversible condition that leads the clinician to question the patient’s capacity to consent.3
For example, if a patient in an emergency room is delirious because of ingesting an unknown substance and is unable to consent, a physician can call family members to ask about the patient’s medical problems. Notifying family that the patient is in the hospital could violate confidentiality, however.
Reporting abuse. All clinicians are obligated to report suspected child abuse or neglect. Some state laws also may require physicians to disclose abuse of vulnerable groups such as the elderly or the disabled and report to the local department of health diagnosis of communicable diseases such as HIV.3
Circle of confidentiality. Certain parties— including clinical staff on an inpatient unit or a psychiatrist supervising a resident— are considered to be within a circle of confidentiality.3 You do not need a patient’s consent to share clinical information with those within the circle of confidentiality. Do not release a patient’s information to parties who are not in the circle of confidentiality—such as family members, attorneys representing the patient, and law enforcement personnel—unless you’ve first obtained the patient’s consent.
Document the reasoning behind your decision to disclose your patient’s personal information without the patient’s consent. Show that you engaged in a reasonable clinical decision-making process.3 For example, record the risks and benefits of your decision and how you arrived at your conclusion.3
Other scenarios
Multidisciplinary teams. Members of a multidisciplinary treatment team—such as physicians, nurses, or social workers—should only receive confidential information that is relevant to the patient’s care. Other clinicians who are not involved in the case—although they may be seeing other patients on the same unit—should not have access to the patient’s confidential information. Discussions with these team members must be private so that others do not overhear confidential information.
Insurance companies generally are not party to the patient’s records unless the patient agrees to allow access by signing a release. If the patient’s refusal to allow disclosure results in the insurance company’s refusal to pay, then the patient is responsible for resolving the issue.7
Scientific publications and presentations. When you present a case report for a scientific publication or at a meeting, alter the patient’s biographical data so that someone who knows the patient would be unable to identify him or her based on the information in the case report. If the information is so specific that you cannot prevent patient identification, either do not publish the case or offer the patient the right to veto the manuscript’s distribution. If necessary, have the patient sign a consent form to allow publication or presentation of the case report.
Confidentiality violations
Breach of confidentiality may be intentional, such as disclosing a patient’s personal information to a third party as in this case, or unintentional, such as talking about a patient to a colleague and having someone overhear your discussion.8 Violating confidentiality may result in litigation for malpractice (negligence), invasion of privacy, or breach of contract, and ethical sanctions.8
No aspect of psychiatric practice seems to generate stronger emotions than the potential legal repercussions of our work. Keeping up with patients’ needs, billing issues, and advancements in medicine leaves little time for tracking changing state and federal laws or case precedents. For the past 4 years it has been my pleasure to provide information on the legal issues psychiatrists face and provide possible means of avoiding legal pitfalls.
Although I have decided to pursue other projects, I wish to give readers my thanks and to suggest resources—only a few among many great ones—that may be useful guides for a variety of legal issues.
Jon E. Grant, JD, MD, MPH
- Journal of the American Academy of Psychiatry and the Law.
- Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA:Harvard University Press; 1998.
- Simon RI, Shuman DW.Clinical manual of psychiatry and the law. Washington, DC: American Psychiatric Publishing, Inc. ; 2007.
Editor’s note
Current Psychiatry thanks Dr. Grant for writing the Malpractice Verdicts column since 2004. The column will continue in a new format in the February 2008 issue.
1. National Institutes of Health. The Hippocratic oath. Available at: http://www.nlm.nih.gov/hmd/greek/greek_oath.html. Accessed October 30, 2007.
2. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006: 6. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
3. Lowenthal D. Case studies in confidentiality. J Psychiatr Prac 2002;8:151-9.
4. Tarasoff vs Regents of the University of California 551P 2d 334 (Cal 1976).
5. Appelbaum PS Taras off and the clinician: problems in fulfilling the duty to protect. Am J Psychiatry 1985;142:425-9.
6. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006:7. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
7. Hilliard J. Liability issues with managed care. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:44-51.
8. Berner M. Write smarter, not longer. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:54-71.
Cases are selected by Current Psychiatry fromMedical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
1. National Institutes of Health. The Hippocratic oath. Available at: http://www.nlm.nih.gov/hmd/greek/greek_oath.html. Accessed October 30, 2007.
2. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006: 6. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
3. Lowenthal D. Case studies in confidentiality. J Psychiatr Prac 2002;8:151-9.
4. Tarasoff vs Regents of the University of California 551P 2d 334 (Cal 1976).
5. Appelbaum PS Taras off and the clinician: problems in fulfilling the duty to protect. Am J Psychiatry 1985;142:425-9.
6. Principles of medical ethics with annotations especially applicable to psychiatry. Washington, DC: American Psychiatric Association; 2006:7. Availableat: http://www.psych.org/psych_pract/ethics/ppaethics.pdf. Accessed October 30, 2007.
7. Hilliard J. Liability issues with managed care. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:44-51.
8. Berner M. Write smarter, not longer. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:54-71.
Cases are selected by Current Psychiatry fromMedical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
SHM: BEHIND THE SCENES
Enter text here
Enter text here
Enter text here
Salary Stress
Question: I am working too hard and getting paid too little. Is there any easy to figure out if I am getting paid what I am worth?
Show Me the Money, Austin, Texas
Dr. Hospitalist responds: I suspect you may have already asked hospitalists you know about how much they make and compared schedules. Although this may be sadistically fun (alas, misery loves company), there are problems with this approach.
Your perspective is limited to friends and colleagues willing to share this information. Some people are reluctant to talk money, others have a tendency to embellish their productivity. I am not saying folks would intentionally lie to you (wink, nod), but who would tell you they feel overpaid and do not work hard?
What you need are objective data. You and a couple of colleagues could develop a survey, send it to every hospitalist you know, and hope they respond. But even if you did, how often could you muster the energy to do this to keep your data up to date?
Remember, you are doing this survey to demonstrate you are compensated appropriately for how much work you produce. Lucky for you, several organizations collect physician productivity and compensation data, including SHM and the Medical Group Management Association (MGMA). But there are differences in the data.
Some believe the MGMA data set may include information from primary care groups with inpatient rounders in addition to full-time hospitalists. Meanwhile, SHM data were last collected in November 2005. SHM collects updated information from hospitalists around the country. They will make those findings available at the next SHM annual meeting in San Diego in April 2008.
This will also be the first survey done since Medicare moved to the new 2007 relative value unit (RVU) values. Hospitalists who contribute to the survey can access the data for free. I suppose critics could argue that the approach taken by these groups is subject to bias because individuals could submit false data. This is all the more reason I would encourage you to submit data to the SHM survey. The larger the sample size, the more difficult it will be for any one individual’s data to warp the survey.
Speak Up
Question: I know hospitalists should communicate with primary care physicians (PCPs) about their patients, but I find it takes a lot of time for me to call their offices. Is there an easier way to do this? I am also not completely sure of when I should communicate. Any suggestions?
No Time to Talk, Atlanta
Dr. Hospitalist responds: Let me guess. Your “communication” with the PCP goes something like this: You pick up the telephone to call a patient’s PCP. After sitting on hold for what seems like eternity (your pager rings repeatedly during this time), a voice on the other end of line tells you that the doctor is in an exam room. “Do you want me to interrupt him?”
Do you say yes and run the risk of sitting on hold another five minutes? Or do you decide whatever you had to say really isn’t that important? But don’t you need that outpatient medication list? Do you really have to tell the PCP about the ongoing end of life discussions with the patient? What’s a hospitalist to do?
This method of communication may have worked when you were a resident in training, when your workload was capped and your attending physician had to make time for your calls. But try this as a hospitalist and you’ll quickly discover you don’t have enough hours each day.
When working out a relationship with a PCP, hospitalists should engage the PCP in a discussion about how they should communicate. For example, the hospitalist and PCP may agree that each time a patient presents for admission, the hospitalist will ask the hospitalist administrative assistant to fax the PCP office. A fax with admission diagnoses will not only serve as notification of admission but also as a request for information from the PCP.
As important as it is for the hospitalist to get his staff to fax the request in a timely manner, the PCP will have to do the same with his/her office staff. In such a system, the hospitalist and the PCP communicate about admissions via their administrative staff. If the PCP or hospitalist has further questions, the expectation may be that a page will be in order. But for the majority of admissions, that won’t be necessary.
I have seen hospitalists and PCPs handle routine communication in a variety of ways: phone calls, face-to-face discussion, e-mail, voicemail, discharge summaries/letters, fax notification of admission, pages. No single method works well with all groups all the time. To succeed, communication:
- Must be timely, easy to understand, and concise;
- Must be efficient for the communicator and the recipient, not labor intensive;
- Should occur at each transition in care; and
- Should meet privacy guidelines.
Communicators must understand the rules of engagement and share common expectations. Ideally, there should be a paper trail or other record.
Hiring is Work
Question: My group is having a hard time recruiting physicians. How can we do better?
Need Help, Richmond, Va.
Dr. Hospitalist responds: If it’s any consolation, you’re not alone. Look at the number of pages devoted to job ads in this issue of The Hospitalist and you’ll understand the high demand for hospitalists. There are about 20,000 hospitalists in the country, and many believe there is room for double that number. Advertising and hiring qualified staff is not a challenge unique to hospital medicine, but most hospitalists received no training on how to do it. Most hospitalists underestimate the time and resources it takes to recruit and hire staff.
Here are some hiring hints to help you and your hospitalist program maximize your success.
The first step is to create a job description. Before you can describe the job to prospective hospitalists, you need a clear understanding yourself. I would expect applicants to ask some of the following questions:
- Do your hospitalists to work days, nights or a combination of both?
- What about weekdays versus weekends?
- How does your group handle admissions versus daily rounding?
- Do your hospitalists provide consultative services?
- Are there teaching responsibilities?
- How many patients do you expect each hospitalists to see daily?
Based on your job description, how do you expect to compensate your hospitalists? Do your homework and find out what competitors are paying for similar job descriptions. While there are many reasons prospective hospitalists might accept an offer, salary is often not the only reason. What else is part of your compensation package? It might include some of the following:
- A retirement plan, like a 401k/ 403b or a pension;
- Paid parking;
- Continuing-education stipend;
- Productivity incentive;
- Access to health, life and/or disability insurance;
- Paid malpractice insurance; and
- Ownership/equity opportunity.
Once you create an attractive job description with a competitive compensation package, it’s time to get the word out. There are many options for reaching prospective candidates:
- Advertise in journals and online;
- Advertise at meetings;
- Tell friends, colleagues and nurses;
- Work with your hospital’s recruiter;
- Send targeted mailings; and
- Be seen at local hospitalist events.
Once you have an applicant interested, it’s time to close the deal. Qualified applicants are likely going to field offers from several groups. Why should the applicant accept your offer over another? Here are several incentives:
- Signing bonus;
- Relocation package;
- Loan forgiveness;
- Title for an administrative role; and
- Opportunity for advancement.
Don’t underestimate the effect of a simple phone call or e-mail to your candidate after the interview. I can’t emphasize how often I hear people say they joined a group because they felt as though they fit in well.
Hiring is a year-round group effort. The most important resource in any hospitalist program is staff. Recruitment, hiring, and retention should be a primary goal of any hospitalist medical director. TH
Question: I am working too hard and getting paid too little. Is there any easy to figure out if I am getting paid what I am worth?
Show Me the Money, Austin, Texas
Dr. Hospitalist responds: I suspect you may have already asked hospitalists you know about how much they make and compared schedules. Although this may be sadistically fun (alas, misery loves company), there are problems with this approach.
Your perspective is limited to friends and colleagues willing to share this information. Some people are reluctant to talk money, others have a tendency to embellish their productivity. I am not saying folks would intentionally lie to you (wink, nod), but who would tell you they feel overpaid and do not work hard?
What you need are objective data. You and a couple of colleagues could develop a survey, send it to every hospitalist you know, and hope they respond. But even if you did, how often could you muster the energy to do this to keep your data up to date?
Remember, you are doing this survey to demonstrate you are compensated appropriately for how much work you produce. Lucky for you, several organizations collect physician productivity and compensation data, including SHM and the Medical Group Management Association (MGMA). But there are differences in the data.
Some believe the MGMA data set may include information from primary care groups with inpatient rounders in addition to full-time hospitalists. Meanwhile, SHM data were last collected in November 2005. SHM collects updated information from hospitalists around the country. They will make those findings available at the next SHM annual meeting in San Diego in April 2008.
This will also be the first survey done since Medicare moved to the new 2007 relative value unit (RVU) values. Hospitalists who contribute to the survey can access the data for free. I suppose critics could argue that the approach taken by these groups is subject to bias because individuals could submit false data. This is all the more reason I would encourage you to submit data to the SHM survey. The larger the sample size, the more difficult it will be for any one individual’s data to warp the survey.
Speak Up
Question: I know hospitalists should communicate with primary care physicians (PCPs) about their patients, but I find it takes a lot of time for me to call their offices. Is there an easier way to do this? I am also not completely sure of when I should communicate. Any suggestions?
No Time to Talk, Atlanta
Dr. Hospitalist responds: Let me guess. Your “communication” with the PCP goes something like this: You pick up the telephone to call a patient’s PCP. After sitting on hold for what seems like eternity (your pager rings repeatedly during this time), a voice on the other end of line tells you that the doctor is in an exam room. “Do you want me to interrupt him?”
Do you say yes and run the risk of sitting on hold another five minutes? Or do you decide whatever you had to say really isn’t that important? But don’t you need that outpatient medication list? Do you really have to tell the PCP about the ongoing end of life discussions with the patient? What’s a hospitalist to do?
This method of communication may have worked when you were a resident in training, when your workload was capped and your attending physician had to make time for your calls. But try this as a hospitalist and you’ll quickly discover you don’t have enough hours each day.
When working out a relationship with a PCP, hospitalists should engage the PCP in a discussion about how they should communicate. For example, the hospitalist and PCP may agree that each time a patient presents for admission, the hospitalist will ask the hospitalist administrative assistant to fax the PCP office. A fax with admission diagnoses will not only serve as notification of admission but also as a request for information from the PCP.
As important as it is for the hospitalist to get his staff to fax the request in a timely manner, the PCP will have to do the same with his/her office staff. In such a system, the hospitalist and the PCP communicate about admissions via their administrative staff. If the PCP or hospitalist has further questions, the expectation may be that a page will be in order. But for the majority of admissions, that won’t be necessary.
I have seen hospitalists and PCPs handle routine communication in a variety of ways: phone calls, face-to-face discussion, e-mail, voicemail, discharge summaries/letters, fax notification of admission, pages. No single method works well with all groups all the time. To succeed, communication:
- Must be timely, easy to understand, and concise;
- Must be efficient for the communicator and the recipient, not labor intensive;
- Should occur at each transition in care; and
- Should meet privacy guidelines.
Communicators must understand the rules of engagement and share common expectations. Ideally, there should be a paper trail or other record.
Hiring is Work
Question: My group is having a hard time recruiting physicians. How can we do better?
Need Help, Richmond, Va.
Dr. Hospitalist responds: If it’s any consolation, you’re not alone. Look at the number of pages devoted to job ads in this issue of The Hospitalist and you’ll understand the high demand for hospitalists. There are about 20,000 hospitalists in the country, and many believe there is room for double that number. Advertising and hiring qualified staff is not a challenge unique to hospital medicine, but most hospitalists received no training on how to do it. Most hospitalists underestimate the time and resources it takes to recruit and hire staff.
Here are some hiring hints to help you and your hospitalist program maximize your success.
The first step is to create a job description. Before you can describe the job to prospective hospitalists, you need a clear understanding yourself. I would expect applicants to ask some of the following questions:
- Do your hospitalists to work days, nights or a combination of both?
- What about weekdays versus weekends?
- How does your group handle admissions versus daily rounding?
- Do your hospitalists provide consultative services?
- Are there teaching responsibilities?
- How many patients do you expect each hospitalists to see daily?
Based on your job description, how do you expect to compensate your hospitalists? Do your homework and find out what competitors are paying for similar job descriptions. While there are many reasons prospective hospitalists might accept an offer, salary is often not the only reason. What else is part of your compensation package? It might include some of the following:
- A retirement plan, like a 401k/ 403b or a pension;
- Paid parking;
- Continuing-education stipend;
- Productivity incentive;
- Access to health, life and/or disability insurance;
- Paid malpractice insurance; and
- Ownership/equity opportunity.
Once you create an attractive job description with a competitive compensation package, it’s time to get the word out. There are many options for reaching prospective candidates:
- Advertise in journals and online;
- Advertise at meetings;
- Tell friends, colleagues and nurses;
- Work with your hospital’s recruiter;
- Send targeted mailings; and
- Be seen at local hospitalist events.
Once you have an applicant interested, it’s time to close the deal. Qualified applicants are likely going to field offers from several groups. Why should the applicant accept your offer over another? Here are several incentives:
- Signing bonus;
- Relocation package;
- Loan forgiveness;
- Title for an administrative role; and
- Opportunity for advancement.
Don’t underestimate the effect of a simple phone call or e-mail to your candidate after the interview. I can’t emphasize how often I hear people say they joined a group because they felt as though they fit in well.
Hiring is a year-round group effort. The most important resource in any hospitalist program is staff. Recruitment, hiring, and retention should be a primary goal of any hospitalist medical director. TH
Question: I am working too hard and getting paid too little. Is there any easy to figure out if I am getting paid what I am worth?
Show Me the Money, Austin, Texas
Dr. Hospitalist responds: I suspect you may have already asked hospitalists you know about how much they make and compared schedules. Although this may be sadistically fun (alas, misery loves company), there are problems with this approach.
Your perspective is limited to friends and colleagues willing to share this information. Some people are reluctant to talk money, others have a tendency to embellish their productivity. I am not saying folks would intentionally lie to you (wink, nod), but who would tell you they feel overpaid and do not work hard?
What you need are objective data. You and a couple of colleagues could develop a survey, send it to every hospitalist you know, and hope they respond. But even if you did, how often could you muster the energy to do this to keep your data up to date?
Remember, you are doing this survey to demonstrate you are compensated appropriately for how much work you produce. Lucky for you, several organizations collect physician productivity and compensation data, including SHM and the Medical Group Management Association (MGMA). But there are differences in the data.
Some believe the MGMA data set may include information from primary care groups with inpatient rounders in addition to full-time hospitalists. Meanwhile, SHM data were last collected in November 2005. SHM collects updated information from hospitalists around the country. They will make those findings available at the next SHM annual meeting in San Diego in April 2008.
This will also be the first survey done since Medicare moved to the new 2007 relative value unit (RVU) values. Hospitalists who contribute to the survey can access the data for free. I suppose critics could argue that the approach taken by these groups is subject to bias because individuals could submit false data. This is all the more reason I would encourage you to submit data to the SHM survey. The larger the sample size, the more difficult it will be for any one individual’s data to warp the survey.
Speak Up
Question: I know hospitalists should communicate with primary care physicians (PCPs) about their patients, but I find it takes a lot of time for me to call their offices. Is there an easier way to do this? I am also not completely sure of when I should communicate. Any suggestions?
No Time to Talk, Atlanta
Dr. Hospitalist responds: Let me guess. Your “communication” with the PCP goes something like this: You pick up the telephone to call a patient’s PCP. After sitting on hold for what seems like eternity (your pager rings repeatedly during this time), a voice on the other end of line tells you that the doctor is in an exam room. “Do you want me to interrupt him?”
Do you say yes and run the risk of sitting on hold another five minutes? Or do you decide whatever you had to say really isn’t that important? But don’t you need that outpatient medication list? Do you really have to tell the PCP about the ongoing end of life discussions with the patient? What’s a hospitalist to do?
This method of communication may have worked when you were a resident in training, when your workload was capped and your attending physician had to make time for your calls. But try this as a hospitalist and you’ll quickly discover you don’t have enough hours each day.
When working out a relationship with a PCP, hospitalists should engage the PCP in a discussion about how they should communicate. For example, the hospitalist and PCP may agree that each time a patient presents for admission, the hospitalist will ask the hospitalist administrative assistant to fax the PCP office. A fax with admission diagnoses will not only serve as notification of admission but also as a request for information from the PCP.
As important as it is for the hospitalist to get his staff to fax the request in a timely manner, the PCP will have to do the same with his/her office staff. In such a system, the hospitalist and the PCP communicate about admissions via their administrative staff. If the PCP or hospitalist has further questions, the expectation may be that a page will be in order. But for the majority of admissions, that won’t be necessary.
I have seen hospitalists and PCPs handle routine communication in a variety of ways: phone calls, face-to-face discussion, e-mail, voicemail, discharge summaries/letters, fax notification of admission, pages. No single method works well with all groups all the time. To succeed, communication:
- Must be timely, easy to understand, and concise;
- Must be efficient for the communicator and the recipient, not labor intensive;
- Should occur at each transition in care; and
- Should meet privacy guidelines.
Communicators must understand the rules of engagement and share common expectations. Ideally, there should be a paper trail or other record.
Hiring is Work
Question: My group is having a hard time recruiting physicians. How can we do better?
Need Help, Richmond, Va.
Dr. Hospitalist responds: If it’s any consolation, you’re not alone. Look at the number of pages devoted to job ads in this issue of The Hospitalist and you’ll understand the high demand for hospitalists. There are about 20,000 hospitalists in the country, and many believe there is room for double that number. Advertising and hiring qualified staff is not a challenge unique to hospital medicine, but most hospitalists received no training on how to do it. Most hospitalists underestimate the time and resources it takes to recruit and hire staff.
Here are some hiring hints to help you and your hospitalist program maximize your success.
The first step is to create a job description. Before you can describe the job to prospective hospitalists, you need a clear understanding yourself. I would expect applicants to ask some of the following questions:
- Do your hospitalists to work days, nights or a combination of both?
- What about weekdays versus weekends?
- How does your group handle admissions versus daily rounding?
- Do your hospitalists provide consultative services?
- Are there teaching responsibilities?
- How many patients do you expect each hospitalists to see daily?
Based on your job description, how do you expect to compensate your hospitalists? Do your homework and find out what competitors are paying for similar job descriptions. While there are many reasons prospective hospitalists might accept an offer, salary is often not the only reason. What else is part of your compensation package? It might include some of the following:
- A retirement plan, like a 401k/ 403b or a pension;
- Paid parking;
- Continuing-education stipend;
- Productivity incentive;
- Access to health, life and/or disability insurance;
- Paid malpractice insurance; and
- Ownership/equity opportunity.
Once you create an attractive job description with a competitive compensation package, it’s time to get the word out. There are many options for reaching prospective candidates:
- Advertise in journals and online;
- Advertise at meetings;
- Tell friends, colleagues and nurses;
- Work with your hospital’s recruiter;
- Send targeted mailings; and
- Be seen at local hospitalist events.
Once you have an applicant interested, it’s time to close the deal. Qualified applicants are likely going to field offers from several groups. Why should the applicant accept your offer over another? Here are several incentives:
- Signing bonus;
- Relocation package;
- Loan forgiveness;
- Title for an administrative role; and
- Opportunity for advancement.
Don’t underestimate the effect of a simple phone call or e-mail to your candidate after the interview. I can’t emphasize how often I hear people say they joined a group because they felt as though they fit in well.
Hiring is a year-round group effort. The most important resource in any hospitalist program is staff. Recruitment, hiring, and retention should be a primary goal of any hospitalist medical director. TH
A Surgical Surge
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Lesson of the Titanic
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.



