User login
Presurgery Discontinuation of Antiplatelet Therapy in Patients
There are currently limited data to guide perioperative management of antiplatelet therapy after drug‐eluting stent (DES) implantation. The clinician must balance the risk of excessive bleeding if antiplatelet agents are continued perioperatively with the risk of stent thrombosis if antiplatelet agents are discontinued for surgerya risk that may be amplified in the perioperative period because of the prothrombotic state that accompanies the stress of surgery.
Paclitaxel‐ and sirolimus‐eluting stents have supplanted bare‐metal stents as first‐line treatment for coronary stenosis because of their efficacy in preventing in‐stent restenosis by inhibiting neointimal proliferation. However, the antiproliferative effects of DESs may also delay endothelialization, rendering them vulnerable to stent thrombosis when antiplatelet therapy is prematurely discontinued.15 Some patients with DESs may be vulnerable to stent thrombosis when antiplatelet therapy is discontinued even after a year or more of treatment.6 Although stent thrombosis is uncommon, it is deadly, with a mortality rate approaching 50%.1 Generally, antiplatelet therapy is discontinued prior to surgery. This presents a clinical dilemma for patients with DES because guidelines recommend lifelong aspirin therapy and at least 36 months of clopidogrel for patients who have undergone DES placement.79
In the bare‐metal stent era, studies demonstrated an alarming risk of stent thrombosis in the setting of noncardiac surgery within 26 weeks of stent placement.10, 11 However, the appropriate interval before elective noncardiac surgery following DES placement has not been defined and may be longer. Case reports and case series have highlighted this risk12 and have even suggested that a DES may be susceptible to stent thrombosis as long as a year after its placement.6 More recently, pooled data from controlled trials have suggested that although the overall rate of DES thrombosis may not be consistently higher than that of bare‐metal stents, the risk appears to persist far longer (probably from delayed endothelialization of the target vessel) and may be more pronounced following discontinuation of antiplatelet agents.9, 1316 This has led to recent recommendations to continue dual antiplatelet therapy (with aspirin and clopidogrel) for at least a year following DES placement and possibly indefinitely, provided that the therapy is tolerated.9 Whether this risk is accentuated in the perioperative setting independent of discontinuation of antiplatelet therapy remains unknown. In 1 registry, the strongest predictor of DES thrombosis was premature discontinuation of antiplatelet therapy (hazard ratio 90, 95% confidence interval 30270, P < .001), and noncardiac surgery was the most frequent reason for discontinuation of antiplatelet therapy.1 However, the actual incidence of stent thrombosis in patients undergoing surgery was unavailable because the denominator was unknown (ie, number of patients with stents who underwent surgery). Although it is certainly plausible that the prothrombotic and proinflammatory postoperative state augments the risk of stent thrombosis independent of discontinuation of antiplatelet therapy alone, this remains unproven.
At the time of the present study, protocol‐based clinical practice at the Cleveland Clinic Foundation's Internal Medicine Preoperative Assessment Consultation and Treatment (IMPACT) Center included routine discontinuation of all antiplatelet agents (including aspirin and clopidogrel) at least 7 days prior to noncardiac surgery, including in patients with coronary stents. Exceptions to this policy were generally made only for very minor procedures. The purpose of this study was to systematically quantify the risk of adverse cardiovascular events in patients who had DES placement and subsequently underwent elective or semielective noncardiac surgery, most of whom had discontinued all antiplatelet agents at least 7 days before surgery.
Methods
We identified all patients who had DES placement at the Cleveland Clinic who subsequently underwent preoperative evaluation for noncardiac surgery at the IMPACT Center between July 2003 and July 2005. About half the patients undergoing surgery at the Cleveland Clinic were seen in the IMPACT Center prior to surgery during the study period. Preoperative evaluation at the IMPACT Center included a standardized assessment by a hospitalist with expertise in preoperative medicine. Clinical data for each patient were contemporaneously entered into an electronic medical record. Written preoperative medication instructions were provided to each patient and documented in the electronic record, indicating specific instructions to discontinue any antiplatelet agents 710 days preoperatively.
The IMPACT Center database was crosslinked to the Cleveland Clinic Foundation Heart Center Database, which contains records of all patients who have undergone coronary stenting at the Cleveland Clinic. Computerized and written medical records of all patients in both databases were reviewed using a standardized data collection instrument. All medical data generated up to 30 days postoperatively at the Cleveland Clinic were reviewed. Social Security numbers were linked with the Social Security Death Index to verify that no patients died within 30 days of surgery.
Predefined outcomes included catheterization‐confirmed DES thrombosis, any myocardial infarction, and major bleeding within 30 days of the surgical procedure. Myocardial infarction was defined as elevation of troponin T to more than twice the upper limit of normal (0.2 mg/mL) with or without associated electrocardiographic changes or symptoms. This biochemically based definition was used with the understanding that cardiac enzyme tests are consistently ordered for patients at the Cleveland Clinic with suspected coronary events and that postoperative myocardial infarction may be atypical in presentation (eg, delirium or hypotension without chest pain). Stent thrombosis was considered present if confirmed by catheterization or autopsy and considered possible if a patient suffered from a myocardial infarction but did not have a definitive diagnostic procedure performed. DES thrombosis was considered absent if a patient underwent postoperative catheterization and the DES appeared patent. Major bleeding was defined as any bleeding requiring unplanned reoperation or bleeding in a critical location (intracranial or retroperitoneal). Invasiveness of surgery was defined prospectively according to a Cleveland Clinic bleeding classification scheme based on that of Pasternak17, 18:
Category 1. Minimal risk to patient; little or no anticipated blood loss (eg, breast biopsy, cystoscopy).
Category 2. Mild risk to patient; minimal to moderately invasive procedure; estimated blood loss < 500 cc (eg, laparoscopy, arthroscopy, hernia repair).
Category 3. Moderate risk to patient and moderate to significantly invasive; blood loss potential 5001000 cc (eg, laminectomy, total hip or knee replacement).
Category 4. Major risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc (eg, major spinal reconstruction, major reconstruction of GI tract, major vascular repair without intensive care unit stay).
Category 5. Critical risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc with anticipated postoperative intensive care unit stay (eg, cardiac procedure, major vascular repair with anticipated intensive care unit stay).
Statistical analyses were descriptive. We determined the rate of adverse outcomes with 95% confidence intervals (CIs) in the entire patient cohort and among prespecified patient subsets, based on timing of discontinuation of antiplatelet therapy. Predefined subsets included those who had clopidogrel and aspirin discontinued less than 3 months and less than 6 months following DES implantation. The 2 test was used to test the hypothesis that discontinuation of antiplatelet therapy was a function of the type of surgery or timing of stent placement.
The study was approved by the Cleveland Clinic Foundation's institutional review board. The requirement for informed consent was waived.
RESULTS
In total, 114 patients were evaluated in the IMPACT Center following DES placement. Baseline patient characteristics are shown in Table 1. The median age was 71 years (interquartile range 6476 years), and 66% were male. Patients had a moderate degree of comorbidity: 41% had diabetes, 12% had an ejection fraction < 45%, 34% had undergone coronary bypass, 17% had atrial fibrillation or flutter, and 20% had chronic renal insufficiency (creatinine 2.0 or end‐stage renal disease). Most patients received ‐adrenergic blockers (97%), statins (95%), and either angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (77%) preoperatively. Patients underwent a variety of surgeries (Table 1).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Demographics | |
| Age (years), median (IQR) | 71 (6476) |
| Male | 75 (65.7%) |
| White | 88 (77.2%) |
| Comorbid illnesses | |
| Diabetes mellitus | 47 (41.2%) |
| History of prior myocardial infarction | 48 (42.1%) |
| Hypertension | 108 (94.7%) |
| History of stroke or transient cerebral ischemia | 15 (13.2%) |
| Dyslipidemia or treatment with lipid‐lowering drugs | 106 (93.0%) |
| Ejection fraction < 45% | 14 (12.3%) |
| History of coronary artery bypass | 39 (34.2%) |
| Atrial fibrillation or flutter | 19 (16.7%) |
| End‐stage renal disease on dialysis | 13 (11.4%) |
| Chronic renal impairment (creatinine 2.0) without dialysis | 10 (8.8%) |
| Other medical treatments | |
| Angiotensin converting enzyme inhibitor or angiotensin receptor blocker | 88 (77.2%) |
| ‐blocker | 111 (97.3%) |
| Statin | 108 (94.7%) |
| Invasiveness of surgery* | |
| Category 1 (lowest risk) | 37 (32.5%) |
| Category 2 | 22 (19.3%) |
| Category 3 | 48 (42.1%) |
| Category 4 | 7 (6.1%) |
| Category 5 (highest risk) | 0 (0%) |
| Outpatient or short‐stay surgery | 50 (47.2%) |
| Type of surgery | |
| Major orthopedic | 39 (34.2%) |
| Minor orthopedic | 5 (4.4%) |
| Ophthalmologic | 30 (26.3%) |
| General abdominal | 8 (7.0%) |
| Gynecological | 5 (4.4%) |
| Urological | 11 (9.6%) |
| Head and neck | 5 (4.4%) |
| Vascular | 1 (0.9%) |
| Other | 10 (8.8%) |
Patients had received both paclitaxel and sirolimus stents (28% and 73% of patients, respectively); 33% of patients had had more than 1 DES (Table 2). Most patients underwent surgery within 1 year of stent placement (77%), but only 40% had surgery within 180 days of stenting and only 13% within 90 days of stenting. Most patients (77%) had antiplatelet therapy completely discontinued a median of 10 days before surgery and remained off antiplatelet therapy for a median of 14 days total. Ten of the 15 patients (67%) who underwent surgery within 90 days of stenting had all antiplatelet agents discontinued preoperatively, 24 of the 30 patients (80%) who had surgery between 91 and 180 days after stenting had antiplatelet therapy completely discontinued, and 54 of the 69 patients (78%) who had surgery more than 180 days after stenting had antiplatelet therapy completely discontinued. There was no significant relationship between timing of stent placement relative to surgery (<90, 91180, or >180 days) and decision about whether to discontinue antiplatelet therapy (P = .59). However, invasiveness of the surgery was associated with antiplatelet management: 85% of those who continued antiplatelet therapy (aspirin or aspirin and clopidogrel) during the perioperative period were patients who underwent minimally invasive surgery (P < .0001).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Timing of surgery and antiplatelet agent discontinuation relative to Percutaneous coronary intervention | |
| Duration of most recent intervention relative to surgery (days), median (IQR) | 236 (125354) |
| Surgery within 90 days of DES placement | 15 (13.2%) |
| Surgery within 180 days of DES placement | 45 (39.5%) |
| Surgery within 1 year of DES placement | 88 (77.2%) |
| Percutaneous Coronary Intervention History | |
| Number of drug‐eluting stents | |
| 1 | 76 (66.7%) |
| 2 | 26 (22.8%) |
| 3+ | 12 (10.5%) |
| Paclitaxel stent 1 | 32 (28.1%) |
| Sirolimus stent 1 | 83 (72.8%) |
| Bare‐metal stent 1 | 10 (8.8%) |
| Perioperative antiplatelet treatment | |
| Clopidogrel and aspirin continued through surgery | 24 (21.1%) |
| Aspirin alone continued through surgery | 2 (1.8%) |
| Clopidogrel alone continued through surgery | 0 (0%) |
| No antiplatelet treatment at time of surgery | 88 (77.2%) |
| Among the 15 patients who had surgery within 90 days of stenting | 10 (66.7%) |
| Among the 45 patients who had surgery within 180 days of stenting | 34 (75.6%) |
| Duration of discontinuance of aspirin | |
| Median number of days discontinued preoperatively (IQR) | 10 (812) |
| Median total duration of discontinuance [days, IQR) | 14 (1019) |
| Duration of discontinuance of clopidogrel | |
| Median number of days discontinued preoperatively [days, IQR] | 10 (813) |
| Median number of days discontinued in total (IQR) | 14 (1020) |
The outcome events are presented in Table 3. Two patients (1.8%, 95% CI 0.5%6.2%) suffered a non‐ST‐elevation myocardial infarction (NSTEMI) postoperatively, and another patient (0.9%, 95% CI 0.2%4.8%) developed major bleeding, a retroperitoneal hemorrhage following kidney transplantation. This patient had been taking both aspirin and clopidogrel until 7 days prior to surgery and began to hemorrhage the day after surgery; antiplatelet agents were resumed 12 days postoperatively. No patients died (0%, 95% CI 0%3.3%). One of the 2 patients who suffered an MI was a 72‐year‐old man who had had placement of a single sirolimus‐eluting stent in the posterior descending artery 284 days prior to elective hip arthroplasty. He had no history of myocardial infarction but had undergone coronary bypass surgery 4 years earlier. Echocardiography showed he had aortic stenosis, with a calculated valve area of 0.9 cm2. He had a baseline left ventricular ejection fraction of 45%. His preoperative cardiac medications included lovastatin, lisinopril, and atenolol; he discontinued both aspirin and clopidogrel 7 days before the surgery. His NSTEMI occurred on the day of his operation, presenting with hypotension and anterolateral ST depressions. His troponin T peaked at 0.48 mg/mL, with a peak creatinine kinase of 795 U/L (MB fraction 6%). His left ventricular ejection fraction was 45% on postoperative day 2 (unchanged from baseline). He was discharged on postoperative day 8 and returned for catheterization 3 weeks later, at which time he was found to have a 70% ostial lesion in a saphenous vein graft to an obtuse marginal, which was stented. The previously placed DES was widely patent. The other patient who suffered a postoperative NSTEMI was a 68‐year‐old man with a history of carotid artery stenting and renal artery stenosis who had undergone placement of 3 sirolimus‐eluting stents in the right coronary artery 50 days prior to cervical laminectomy. He had had elective placement of the stents following a positive pharmacologic stress test. He was taking 50 mg of atenolol daily and had been taking aspirin and clopidogrel until 17 days before surgery. On postoperative day 3 he developed dyspnea, and leads V4 and V5 showed ST depressions. His troponin T peaked at 1.24 mg/mL, with a peak creatinine kinase of 879 U/L (MB fraction 6%). The patient underwent left‐heart catheterization on hospital day 10. All 3 DESs were widely patent. His left ventricular ejection fraction was estimated at 65%. He was discharged on postoperative day 15. Because neither of the patients who had a postoperative NSTEMI showed evidence of stent thrombosis on catheterization, the overall rate of stent thrombosis was 0% (95% CI 0%3.3%).
| Outcome | Entire cohort (n = 114) [all antiplatelet therapy stopped in 88 patients (77%)] | Surgery < 90 days after DES (n = 15) [all antiplatelet therapy stopped in 10 patients (67%)] | Surgery < 180 days after DES (n = 45) [all antiplatelet therapy stopped in 34 patients (76%)] |
|---|---|---|---|
| |||
| Death | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Any myocardial infarction | 2 (1.8%, 0.5%6.2%) | 1 (6.7%, 1.2%29.8%) | 1 (2.2%, 0.4%11.6%) |
| DES thrombosis | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Major bleeding | 1 (0.9%, 0.2%4.8%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
DISCUSSION
Although 2 patients in our study cohort suffered a postoperative myocardial infarction and underwent postoperative catheterization, neither was found to have stent thrombosis, and the MIs of both patients were NSTEMIs with modest cardiac enzyme elevations only. No patients died. A rate of myocardial infarction of less than 2% is well within that expected for patients with established coronary disease undergoing noncardiac surgery.19 That most of our patients discontinued both aspirin and clopidogrel and did not receive antiplatelet agents for a median of 14 days suggests that transient termination of antiplatelet agents in the perioperative setting is not associated with high morbidity or mortality in patients with DES, even when patients have had their stents implanted in the preceding 36 months.
Our study builds on the limited data on this topic. One small case series examined outcomes in 38 patients who had had DES placement and subsequently underwent noncardiac surgery a median of 297 days after stenting.20 None of the patients in this series suffered from stent thrombosis or myocardial infarction, but most underwent surgery without discontinuing aspirin, and 41% underwent surgery without discontinuing clopidogrel. Another recent study demonstrated a high rate of adverse cardiovascular events in patients with coronary stents who underwent noncardiac surgery up to a year after stenting, but the authors of this study did not differentiate between drug‐eluting and bare‐metal stents, and all patients were continued on antiplatelet agents and received parenteral antithrombotic treatment.21
The major strength of our study was its systematic approach. Using a computerized and comprehensive search strategy, we identified all patients who had undergone DES placement at the Cleveland Clinic who subsequently had a preoperative evaluation at the IMPACT Center. Therefore, we are confident that the number of patients in our cohort truly reflects a well‐defined at‐risk population, allowing for an accurate calculation of event rates. This approach contrasts sharply with prior case reports and case series, in which the number of patients at risk was unknown. Nevertheless, these previous reports demonstrate that DES thromboses do occur and can be devastating, so even a small risk of DES thrombosis should be taken seriously. The upper bound of the 95% confidence interval of our estimate of the rate of DES thrombosis was 3.3%, so it is entirely plausible that sampling error contributed to the low rate of thrombosis that we observed.
One major limitation of our study is its sample size. Although our cohort was more than 3 times larger than the only other published cohort of DES patients undergoing noncardiac surgery,20 we had only limited precision to quantify the risk of DES thrombosis. This limitation is particularly relevant for patients who have undergone stent implantation within 36 months of surgery, as they are the patients most likely to have incomplete reendothelialization of the stented artery. We believe that when possible it remains prudent to delay noncardiac surgery for at least 36 months and perhaps up to 12 months following DES implantation, in keeping with recent guidelines.7, 8 However, for patients with conditions such as cancer whose surgery is semielective or patients with nonsurgical bleeding problems (such as gastrointestinal bleeding), our study provides at least some reassurance that short‐term discontinuation of antiplatelet agents may not be as dangerous as some authors have suggested,1 even within 36 months of DES placement. Another important limitation of our study is potential referral bias. At the Cleveland Clinic, most patients undergoing vascular and thoracic procedures are not evaluated at the IMPACT Center. Similarly, some of the patients with severe cardiovascular disease may also have bypassed the IMPACT Center and gone to a cardiologist for preoperative evaluation. As such, we believe our findings should not be generalized to high‐risk cardiac patients or to those undergoing high‐risk procedures.
A noteworthy distinction between our cohort and the cohort reported by Compton and colleagues is that in the perioperative period, most of our patients underwent complete discontinuation of antiplatelet therapy and remained off both aspirin and clopidogrel for an average of 2 weeks, whereas most patients in the other cohort were continued on antiplatelet therapy.20 This highlights the continued controversy surrounding management of antiplatelet therapy in perioperative patients with established coronary disease, who are at substantial risk for both bleeding and myocardial infarction because of the surgery.22 Our data offer little guidance on the optimal management of antiplatelet agents perioperatively because the incidence of both bleeding and thrombosis was low and whether or not patients were continued on antiplatelet agents was not random. We advocate individualized management strategies of perioperative patients with DES. Patients undergoing procedures that carry a high risk of outcome‐affecting bleeding (such as brain surgery) should probably have their antiplatelet agents discontinued preoperatively, whereas those undergoing minor surgery may have their antiplatelet agents continued, provided the surgeon and the anesthesiologist are in agreement with this approach. The timing of DES placement should also be factored into this decision because recently placed stents carry a higher risk of thrombosis.
In summary, our findings clarify the risks of stent thrombosis and postoperative myocardial infarction in clinically stable patients with DES who undergo low‐ and intermediate‐risk noncardiac surgery. Because it is unlikely to ever be ethically appropriate or logistically feasible to conduct a randomized study of patients with DES having early versus delayed noncardiac surgery, observational cohorts will have to suffice. Additional similar studies will help to validate (or refute) our findings and to more precisely quantify the risk of adverse cardiac events when patients with DES undergo surgery, which is real, feared, and potentially catastrophic but may be overestimated.
- ,,, et al.Incidence, predictors, and outcome of thrombosis after successful implantation of drug‐eluting stents.JAMA.2005;293:2126–230.
- ,,, et al.Pathology of drug‐eluting stents in humans: delayed healing and late thrombotic risk.J Am Coll Cardiol.2006;48:193–202.
- ,,, et al.Correlates and long‐term outcomes of angiographically proven stent thrombosis with sirolimus‐ and paclitaxel‐eluting stents.Circulation.2006;113:1108–1113.
- ,,, et al.Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug‐eluting stent placement: results from the PREMIER registry.Circulation.2006;113:2803–2809.
- .Trading restenosis for thrombosis? New questions about drug‐eluting stents.N Engl J Med.2006;355:1949–1952.
- ,,, et al.Late thrombosis in drug‐eluting coronary stents after discontinuation of antiplatelet therapy.Lancet2004;364:1519–1521.
- ,,, et al.ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention).Circulation.2006;113:e166–e286.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction).Circulation.2004;110:588–636.
- ,,, et al.Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians.Circulation.2007;115:813–818.
- ,,, et al.Clinical outcome of patients undergoing non‐cardiac surgery in the two months following coronary stenting.J Am Coll Cardiol.2003;42:234–240.
- ,,,,.Catastrophic outcomes of noncardiac surgery soon after coronary stenting.J Am Coll Cardiol.2000;35:1288–1294.
- ,.Thrombosis of sirolimus‐eluting coronary stent in the postanesthesia care unit.Anesth Analg.2005;101:971–973.
- ,,,,,.Late thrombosis of drug‐eluting stents: a meta‐analysis of randomized clinical trials.Am J Med.2006;119:1056–1061.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med.2007;356:1009–1019.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med.2007;356:998–1008.
- ,,,,.A pooled analysis of data comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med.2007;356:989–997.
- .Preoperative assessment: guidelines and challenges.Acta Anaesthesiol ScandSuppl.1997;111:318–320.
- .Preoperative assessment of the ambulatory and same day admission patient.Wellcome Trends Anesthesiol.1991;9:3–11.
- ,,, et al.Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery.Circulation.1999;100:1043–1049.
- ,,,,.Risk of noncardiac surgery after coronary drug‐eluting stent implantation.Am J Cardiol.2006;98:1212–1213.
- ,,,,,.Coronary artery stenting and non‐cardiac surgery—a prospective outcome study.Br J Anaesth.2006;96:686–693.
- ,,.Double jeopardy: balance between bleeding and stent thrombosis with prolonged dual antiplatelet therapy after drug‐eluting stent implantation.Cardiovasc Revasc Med.2006;7:155–158.
There are currently limited data to guide perioperative management of antiplatelet therapy after drug‐eluting stent (DES) implantation. The clinician must balance the risk of excessive bleeding if antiplatelet agents are continued perioperatively with the risk of stent thrombosis if antiplatelet agents are discontinued for surgerya risk that may be amplified in the perioperative period because of the prothrombotic state that accompanies the stress of surgery.
Paclitaxel‐ and sirolimus‐eluting stents have supplanted bare‐metal stents as first‐line treatment for coronary stenosis because of their efficacy in preventing in‐stent restenosis by inhibiting neointimal proliferation. However, the antiproliferative effects of DESs may also delay endothelialization, rendering them vulnerable to stent thrombosis when antiplatelet therapy is prematurely discontinued.15 Some patients with DESs may be vulnerable to stent thrombosis when antiplatelet therapy is discontinued even after a year or more of treatment.6 Although stent thrombosis is uncommon, it is deadly, with a mortality rate approaching 50%.1 Generally, antiplatelet therapy is discontinued prior to surgery. This presents a clinical dilemma for patients with DES because guidelines recommend lifelong aspirin therapy and at least 36 months of clopidogrel for patients who have undergone DES placement.79
In the bare‐metal stent era, studies demonstrated an alarming risk of stent thrombosis in the setting of noncardiac surgery within 26 weeks of stent placement.10, 11 However, the appropriate interval before elective noncardiac surgery following DES placement has not been defined and may be longer. Case reports and case series have highlighted this risk12 and have even suggested that a DES may be susceptible to stent thrombosis as long as a year after its placement.6 More recently, pooled data from controlled trials have suggested that although the overall rate of DES thrombosis may not be consistently higher than that of bare‐metal stents, the risk appears to persist far longer (probably from delayed endothelialization of the target vessel) and may be more pronounced following discontinuation of antiplatelet agents.9, 1316 This has led to recent recommendations to continue dual antiplatelet therapy (with aspirin and clopidogrel) for at least a year following DES placement and possibly indefinitely, provided that the therapy is tolerated.9 Whether this risk is accentuated in the perioperative setting independent of discontinuation of antiplatelet therapy remains unknown. In 1 registry, the strongest predictor of DES thrombosis was premature discontinuation of antiplatelet therapy (hazard ratio 90, 95% confidence interval 30270, P < .001), and noncardiac surgery was the most frequent reason for discontinuation of antiplatelet therapy.1 However, the actual incidence of stent thrombosis in patients undergoing surgery was unavailable because the denominator was unknown (ie, number of patients with stents who underwent surgery). Although it is certainly plausible that the prothrombotic and proinflammatory postoperative state augments the risk of stent thrombosis independent of discontinuation of antiplatelet therapy alone, this remains unproven.
At the time of the present study, protocol‐based clinical practice at the Cleveland Clinic Foundation's Internal Medicine Preoperative Assessment Consultation and Treatment (IMPACT) Center included routine discontinuation of all antiplatelet agents (including aspirin and clopidogrel) at least 7 days prior to noncardiac surgery, including in patients with coronary stents. Exceptions to this policy were generally made only for very minor procedures. The purpose of this study was to systematically quantify the risk of adverse cardiovascular events in patients who had DES placement and subsequently underwent elective or semielective noncardiac surgery, most of whom had discontinued all antiplatelet agents at least 7 days before surgery.
Methods
We identified all patients who had DES placement at the Cleveland Clinic who subsequently underwent preoperative evaluation for noncardiac surgery at the IMPACT Center between July 2003 and July 2005. About half the patients undergoing surgery at the Cleveland Clinic were seen in the IMPACT Center prior to surgery during the study period. Preoperative evaluation at the IMPACT Center included a standardized assessment by a hospitalist with expertise in preoperative medicine. Clinical data for each patient were contemporaneously entered into an electronic medical record. Written preoperative medication instructions were provided to each patient and documented in the electronic record, indicating specific instructions to discontinue any antiplatelet agents 710 days preoperatively.
The IMPACT Center database was crosslinked to the Cleveland Clinic Foundation Heart Center Database, which contains records of all patients who have undergone coronary stenting at the Cleveland Clinic. Computerized and written medical records of all patients in both databases were reviewed using a standardized data collection instrument. All medical data generated up to 30 days postoperatively at the Cleveland Clinic were reviewed. Social Security numbers were linked with the Social Security Death Index to verify that no patients died within 30 days of surgery.
Predefined outcomes included catheterization‐confirmed DES thrombosis, any myocardial infarction, and major bleeding within 30 days of the surgical procedure. Myocardial infarction was defined as elevation of troponin T to more than twice the upper limit of normal (0.2 mg/mL) with or without associated electrocardiographic changes or symptoms. This biochemically based definition was used with the understanding that cardiac enzyme tests are consistently ordered for patients at the Cleveland Clinic with suspected coronary events and that postoperative myocardial infarction may be atypical in presentation (eg, delirium or hypotension without chest pain). Stent thrombosis was considered present if confirmed by catheterization or autopsy and considered possible if a patient suffered from a myocardial infarction but did not have a definitive diagnostic procedure performed. DES thrombosis was considered absent if a patient underwent postoperative catheterization and the DES appeared patent. Major bleeding was defined as any bleeding requiring unplanned reoperation or bleeding in a critical location (intracranial or retroperitoneal). Invasiveness of surgery was defined prospectively according to a Cleveland Clinic bleeding classification scheme based on that of Pasternak17, 18:
Category 1. Minimal risk to patient; little or no anticipated blood loss (eg, breast biopsy, cystoscopy).
Category 2. Mild risk to patient; minimal to moderately invasive procedure; estimated blood loss < 500 cc (eg, laparoscopy, arthroscopy, hernia repair).
Category 3. Moderate risk to patient and moderate to significantly invasive; blood loss potential 5001000 cc (eg, laminectomy, total hip or knee replacement).
Category 4. Major risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc (eg, major spinal reconstruction, major reconstruction of GI tract, major vascular repair without intensive care unit stay).
Category 5. Critical risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc with anticipated postoperative intensive care unit stay (eg, cardiac procedure, major vascular repair with anticipated intensive care unit stay).
Statistical analyses were descriptive. We determined the rate of adverse outcomes with 95% confidence intervals (CIs) in the entire patient cohort and among prespecified patient subsets, based on timing of discontinuation of antiplatelet therapy. Predefined subsets included those who had clopidogrel and aspirin discontinued less than 3 months and less than 6 months following DES implantation. The 2 test was used to test the hypothesis that discontinuation of antiplatelet therapy was a function of the type of surgery or timing of stent placement.
The study was approved by the Cleveland Clinic Foundation's institutional review board. The requirement for informed consent was waived.
RESULTS
In total, 114 patients were evaluated in the IMPACT Center following DES placement. Baseline patient characteristics are shown in Table 1. The median age was 71 years (interquartile range 6476 years), and 66% were male. Patients had a moderate degree of comorbidity: 41% had diabetes, 12% had an ejection fraction < 45%, 34% had undergone coronary bypass, 17% had atrial fibrillation or flutter, and 20% had chronic renal insufficiency (creatinine 2.0 or end‐stage renal disease). Most patients received ‐adrenergic blockers (97%), statins (95%), and either angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (77%) preoperatively. Patients underwent a variety of surgeries (Table 1).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Demographics | |
| Age (years), median (IQR) | 71 (6476) |
| Male | 75 (65.7%) |
| White | 88 (77.2%) |
| Comorbid illnesses | |
| Diabetes mellitus | 47 (41.2%) |
| History of prior myocardial infarction | 48 (42.1%) |
| Hypertension | 108 (94.7%) |
| History of stroke or transient cerebral ischemia | 15 (13.2%) |
| Dyslipidemia or treatment with lipid‐lowering drugs | 106 (93.0%) |
| Ejection fraction < 45% | 14 (12.3%) |
| History of coronary artery bypass | 39 (34.2%) |
| Atrial fibrillation or flutter | 19 (16.7%) |
| End‐stage renal disease on dialysis | 13 (11.4%) |
| Chronic renal impairment (creatinine 2.0) without dialysis | 10 (8.8%) |
| Other medical treatments | |
| Angiotensin converting enzyme inhibitor or angiotensin receptor blocker | 88 (77.2%) |
| ‐blocker | 111 (97.3%) |
| Statin | 108 (94.7%) |
| Invasiveness of surgery* | |
| Category 1 (lowest risk) | 37 (32.5%) |
| Category 2 | 22 (19.3%) |
| Category 3 | 48 (42.1%) |
| Category 4 | 7 (6.1%) |
| Category 5 (highest risk) | 0 (0%) |
| Outpatient or short‐stay surgery | 50 (47.2%) |
| Type of surgery | |
| Major orthopedic | 39 (34.2%) |
| Minor orthopedic | 5 (4.4%) |
| Ophthalmologic | 30 (26.3%) |
| General abdominal | 8 (7.0%) |
| Gynecological | 5 (4.4%) |
| Urological | 11 (9.6%) |
| Head and neck | 5 (4.4%) |
| Vascular | 1 (0.9%) |
| Other | 10 (8.8%) |
Patients had received both paclitaxel and sirolimus stents (28% and 73% of patients, respectively); 33% of patients had had more than 1 DES (Table 2). Most patients underwent surgery within 1 year of stent placement (77%), but only 40% had surgery within 180 days of stenting and only 13% within 90 days of stenting. Most patients (77%) had antiplatelet therapy completely discontinued a median of 10 days before surgery and remained off antiplatelet therapy for a median of 14 days total. Ten of the 15 patients (67%) who underwent surgery within 90 days of stenting had all antiplatelet agents discontinued preoperatively, 24 of the 30 patients (80%) who had surgery between 91 and 180 days after stenting had antiplatelet therapy completely discontinued, and 54 of the 69 patients (78%) who had surgery more than 180 days after stenting had antiplatelet therapy completely discontinued. There was no significant relationship between timing of stent placement relative to surgery (<90, 91180, or >180 days) and decision about whether to discontinue antiplatelet therapy (P = .59). However, invasiveness of the surgery was associated with antiplatelet management: 85% of those who continued antiplatelet therapy (aspirin or aspirin and clopidogrel) during the perioperative period were patients who underwent minimally invasive surgery (P < .0001).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Timing of surgery and antiplatelet agent discontinuation relative to Percutaneous coronary intervention | |
| Duration of most recent intervention relative to surgery (days), median (IQR) | 236 (125354) |
| Surgery within 90 days of DES placement | 15 (13.2%) |
| Surgery within 180 days of DES placement | 45 (39.5%) |
| Surgery within 1 year of DES placement | 88 (77.2%) |
| Percutaneous Coronary Intervention History | |
| Number of drug‐eluting stents | |
| 1 | 76 (66.7%) |
| 2 | 26 (22.8%) |
| 3+ | 12 (10.5%) |
| Paclitaxel stent 1 | 32 (28.1%) |
| Sirolimus stent 1 | 83 (72.8%) |
| Bare‐metal stent 1 | 10 (8.8%) |
| Perioperative antiplatelet treatment | |
| Clopidogrel and aspirin continued through surgery | 24 (21.1%) |
| Aspirin alone continued through surgery | 2 (1.8%) |
| Clopidogrel alone continued through surgery | 0 (0%) |
| No antiplatelet treatment at time of surgery | 88 (77.2%) |
| Among the 15 patients who had surgery within 90 days of stenting | 10 (66.7%) |
| Among the 45 patients who had surgery within 180 days of stenting | 34 (75.6%) |
| Duration of discontinuance of aspirin | |
| Median number of days discontinued preoperatively (IQR) | 10 (812) |
| Median total duration of discontinuance [days, IQR) | 14 (1019) |
| Duration of discontinuance of clopidogrel | |
| Median number of days discontinued preoperatively [days, IQR] | 10 (813) |
| Median number of days discontinued in total (IQR) | 14 (1020) |
The outcome events are presented in Table 3. Two patients (1.8%, 95% CI 0.5%6.2%) suffered a non‐ST‐elevation myocardial infarction (NSTEMI) postoperatively, and another patient (0.9%, 95% CI 0.2%4.8%) developed major bleeding, a retroperitoneal hemorrhage following kidney transplantation. This patient had been taking both aspirin and clopidogrel until 7 days prior to surgery and began to hemorrhage the day after surgery; antiplatelet agents were resumed 12 days postoperatively. No patients died (0%, 95% CI 0%3.3%). One of the 2 patients who suffered an MI was a 72‐year‐old man who had had placement of a single sirolimus‐eluting stent in the posterior descending artery 284 days prior to elective hip arthroplasty. He had no history of myocardial infarction but had undergone coronary bypass surgery 4 years earlier. Echocardiography showed he had aortic stenosis, with a calculated valve area of 0.9 cm2. He had a baseline left ventricular ejection fraction of 45%. His preoperative cardiac medications included lovastatin, lisinopril, and atenolol; he discontinued both aspirin and clopidogrel 7 days before the surgery. His NSTEMI occurred on the day of his operation, presenting with hypotension and anterolateral ST depressions. His troponin T peaked at 0.48 mg/mL, with a peak creatinine kinase of 795 U/L (MB fraction 6%). His left ventricular ejection fraction was 45% on postoperative day 2 (unchanged from baseline). He was discharged on postoperative day 8 and returned for catheterization 3 weeks later, at which time he was found to have a 70% ostial lesion in a saphenous vein graft to an obtuse marginal, which was stented. The previously placed DES was widely patent. The other patient who suffered a postoperative NSTEMI was a 68‐year‐old man with a history of carotid artery stenting and renal artery stenosis who had undergone placement of 3 sirolimus‐eluting stents in the right coronary artery 50 days prior to cervical laminectomy. He had had elective placement of the stents following a positive pharmacologic stress test. He was taking 50 mg of atenolol daily and had been taking aspirin and clopidogrel until 17 days before surgery. On postoperative day 3 he developed dyspnea, and leads V4 and V5 showed ST depressions. His troponin T peaked at 1.24 mg/mL, with a peak creatinine kinase of 879 U/L (MB fraction 6%). The patient underwent left‐heart catheterization on hospital day 10. All 3 DESs were widely patent. His left ventricular ejection fraction was estimated at 65%. He was discharged on postoperative day 15. Because neither of the patients who had a postoperative NSTEMI showed evidence of stent thrombosis on catheterization, the overall rate of stent thrombosis was 0% (95% CI 0%3.3%).
| Outcome | Entire cohort (n = 114) [all antiplatelet therapy stopped in 88 patients (77%)] | Surgery < 90 days after DES (n = 15) [all antiplatelet therapy stopped in 10 patients (67%)] | Surgery < 180 days after DES (n = 45) [all antiplatelet therapy stopped in 34 patients (76%)] |
|---|---|---|---|
| |||
| Death | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Any myocardial infarction | 2 (1.8%, 0.5%6.2%) | 1 (6.7%, 1.2%29.8%) | 1 (2.2%, 0.4%11.6%) |
| DES thrombosis | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Major bleeding | 1 (0.9%, 0.2%4.8%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
DISCUSSION
Although 2 patients in our study cohort suffered a postoperative myocardial infarction and underwent postoperative catheterization, neither was found to have stent thrombosis, and the MIs of both patients were NSTEMIs with modest cardiac enzyme elevations only. No patients died. A rate of myocardial infarction of less than 2% is well within that expected for patients with established coronary disease undergoing noncardiac surgery.19 That most of our patients discontinued both aspirin and clopidogrel and did not receive antiplatelet agents for a median of 14 days suggests that transient termination of antiplatelet agents in the perioperative setting is not associated with high morbidity or mortality in patients with DES, even when patients have had their stents implanted in the preceding 36 months.
Our study builds on the limited data on this topic. One small case series examined outcomes in 38 patients who had had DES placement and subsequently underwent noncardiac surgery a median of 297 days after stenting.20 None of the patients in this series suffered from stent thrombosis or myocardial infarction, but most underwent surgery without discontinuing aspirin, and 41% underwent surgery without discontinuing clopidogrel. Another recent study demonstrated a high rate of adverse cardiovascular events in patients with coronary stents who underwent noncardiac surgery up to a year after stenting, but the authors of this study did not differentiate between drug‐eluting and bare‐metal stents, and all patients were continued on antiplatelet agents and received parenteral antithrombotic treatment.21
The major strength of our study was its systematic approach. Using a computerized and comprehensive search strategy, we identified all patients who had undergone DES placement at the Cleveland Clinic who subsequently had a preoperative evaluation at the IMPACT Center. Therefore, we are confident that the number of patients in our cohort truly reflects a well‐defined at‐risk population, allowing for an accurate calculation of event rates. This approach contrasts sharply with prior case reports and case series, in which the number of patients at risk was unknown. Nevertheless, these previous reports demonstrate that DES thromboses do occur and can be devastating, so even a small risk of DES thrombosis should be taken seriously. The upper bound of the 95% confidence interval of our estimate of the rate of DES thrombosis was 3.3%, so it is entirely plausible that sampling error contributed to the low rate of thrombosis that we observed.
One major limitation of our study is its sample size. Although our cohort was more than 3 times larger than the only other published cohort of DES patients undergoing noncardiac surgery,20 we had only limited precision to quantify the risk of DES thrombosis. This limitation is particularly relevant for patients who have undergone stent implantation within 36 months of surgery, as they are the patients most likely to have incomplete reendothelialization of the stented artery. We believe that when possible it remains prudent to delay noncardiac surgery for at least 36 months and perhaps up to 12 months following DES implantation, in keeping with recent guidelines.7, 8 However, for patients with conditions such as cancer whose surgery is semielective or patients with nonsurgical bleeding problems (such as gastrointestinal bleeding), our study provides at least some reassurance that short‐term discontinuation of antiplatelet agents may not be as dangerous as some authors have suggested,1 even within 36 months of DES placement. Another important limitation of our study is potential referral bias. At the Cleveland Clinic, most patients undergoing vascular and thoracic procedures are not evaluated at the IMPACT Center. Similarly, some of the patients with severe cardiovascular disease may also have bypassed the IMPACT Center and gone to a cardiologist for preoperative evaluation. As such, we believe our findings should not be generalized to high‐risk cardiac patients or to those undergoing high‐risk procedures.
A noteworthy distinction between our cohort and the cohort reported by Compton and colleagues is that in the perioperative period, most of our patients underwent complete discontinuation of antiplatelet therapy and remained off both aspirin and clopidogrel for an average of 2 weeks, whereas most patients in the other cohort were continued on antiplatelet therapy.20 This highlights the continued controversy surrounding management of antiplatelet therapy in perioperative patients with established coronary disease, who are at substantial risk for both bleeding and myocardial infarction because of the surgery.22 Our data offer little guidance on the optimal management of antiplatelet agents perioperatively because the incidence of both bleeding and thrombosis was low and whether or not patients were continued on antiplatelet agents was not random. We advocate individualized management strategies of perioperative patients with DES. Patients undergoing procedures that carry a high risk of outcome‐affecting bleeding (such as brain surgery) should probably have their antiplatelet agents discontinued preoperatively, whereas those undergoing minor surgery may have their antiplatelet agents continued, provided the surgeon and the anesthesiologist are in agreement with this approach. The timing of DES placement should also be factored into this decision because recently placed stents carry a higher risk of thrombosis.
In summary, our findings clarify the risks of stent thrombosis and postoperative myocardial infarction in clinically stable patients with DES who undergo low‐ and intermediate‐risk noncardiac surgery. Because it is unlikely to ever be ethically appropriate or logistically feasible to conduct a randomized study of patients with DES having early versus delayed noncardiac surgery, observational cohorts will have to suffice. Additional similar studies will help to validate (or refute) our findings and to more precisely quantify the risk of adverse cardiac events when patients with DES undergo surgery, which is real, feared, and potentially catastrophic but may be overestimated.
There are currently limited data to guide perioperative management of antiplatelet therapy after drug‐eluting stent (DES) implantation. The clinician must balance the risk of excessive bleeding if antiplatelet agents are continued perioperatively with the risk of stent thrombosis if antiplatelet agents are discontinued for surgerya risk that may be amplified in the perioperative period because of the prothrombotic state that accompanies the stress of surgery.
Paclitaxel‐ and sirolimus‐eluting stents have supplanted bare‐metal stents as first‐line treatment for coronary stenosis because of their efficacy in preventing in‐stent restenosis by inhibiting neointimal proliferation. However, the antiproliferative effects of DESs may also delay endothelialization, rendering them vulnerable to stent thrombosis when antiplatelet therapy is prematurely discontinued.15 Some patients with DESs may be vulnerable to stent thrombosis when antiplatelet therapy is discontinued even after a year or more of treatment.6 Although stent thrombosis is uncommon, it is deadly, with a mortality rate approaching 50%.1 Generally, antiplatelet therapy is discontinued prior to surgery. This presents a clinical dilemma for patients with DES because guidelines recommend lifelong aspirin therapy and at least 36 months of clopidogrel for patients who have undergone DES placement.79
In the bare‐metal stent era, studies demonstrated an alarming risk of stent thrombosis in the setting of noncardiac surgery within 26 weeks of stent placement.10, 11 However, the appropriate interval before elective noncardiac surgery following DES placement has not been defined and may be longer. Case reports and case series have highlighted this risk12 and have even suggested that a DES may be susceptible to stent thrombosis as long as a year after its placement.6 More recently, pooled data from controlled trials have suggested that although the overall rate of DES thrombosis may not be consistently higher than that of bare‐metal stents, the risk appears to persist far longer (probably from delayed endothelialization of the target vessel) and may be more pronounced following discontinuation of antiplatelet agents.9, 1316 This has led to recent recommendations to continue dual antiplatelet therapy (with aspirin and clopidogrel) for at least a year following DES placement and possibly indefinitely, provided that the therapy is tolerated.9 Whether this risk is accentuated in the perioperative setting independent of discontinuation of antiplatelet therapy remains unknown. In 1 registry, the strongest predictor of DES thrombosis was premature discontinuation of antiplatelet therapy (hazard ratio 90, 95% confidence interval 30270, P < .001), and noncardiac surgery was the most frequent reason for discontinuation of antiplatelet therapy.1 However, the actual incidence of stent thrombosis in patients undergoing surgery was unavailable because the denominator was unknown (ie, number of patients with stents who underwent surgery). Although it is certainly plausible that the prothrombotic and proinflammatory postoperative state augments the risk of stent thrombosis independent of discontinuation of antiplatelet therapy alone, this remains unproven.
At the time of the present study, protocol‐based clinical practice at the Cleveland Clinic Foundation's Internal Medicine Preoperative Assessment Consultation and Treatment (IMPACT) Center included routine discontinuation of all antiplatelet agents (including aspirin and clopidogrel) at least 7 days prior to noncardiac surgery, including in patients with coronary stents. Exceptions to this policy were generally made only for very minor procedures. The purpose of this study was to systematically quantify the risk of adverse cardiovascular events in patients who had DES placement and subsequently underwent elective or semielective noncardiac surgery, most of whom had discontinued all antiplatelet agents at least 7 days before surgery.
Methods
We identified all patients who had DES placement at the Cleveland Clinic who subsequently underwent preoperative evaluation for noncardiac surgery at the IMPACT Center between July 2003 and July 2005. About half the patients undergoing surgery at the Cleveland Clinic were seen in the IMPACT Center prior to surgery during the study period. Preoperative evaluation at the IMPACT Center included a standardized assessment by a hospitalist with expertise in preoperative medicine. Clinical data for each patient were contemporaneously entered into an electronic medical record. Written preoperative medication instructions were provided to each patient and documented in the electronic record, indicating specific instructions to discontinue any antiplatelet agents 710 days preoperatively.
The IMPACT Center database was crosslinked to the Cleveland Clinic Foundation Heart Center Database, which contains records of all patients who have undergone coronary stenting at the Cleveland Clinic. Computerized and written medical records of all patients in both databases were reviewed using a standardized data collection instrument. All medical data generated up to 30 days postoperatively at the Cleveland Clinic were reviewed. Social Security numbers were linked with the Social Security Death Index to verify that no patients died within 30 days of surgery.
Predefined outcomes included catheterization‐confirmed DES thrombosis, any myocardial infarction, and major bleeding within 30 days of the surgical procedure. Myocardial infarction was defined as elevation of troponin T to more than twice the upper limit of normal (0.2 mg/mL) with or without associated electrocardiographic changes or symptoms. This biochemically based definition was used with the understanding that cardiac enzyme tests are consistently ordered for patients at the Cleveland Clinic with suspected coronary events and that postoperative myocardial infarction may be atypical in presentation (eg, delirium or hypotension without chest pain). Stent thrombosis was considered present if confirmed by catheterization or autopsy and considered possible if a patient suffered from a myocardial infarction but did not have a definitive diagnostic procedure performed. DES thrombosis was considered absent if a patient underwent postoperative catheterization and the DES appeared patent. Major bleeding was defined as any bleeding requiring unplanned reoperation or bleeding in a critical location (intracranial or retroperitoneal). Invasiveness of surgery was defined prospectively according to a Cleveland Clinic bleeding classification scheme based on that of Pasternak17, 18:
Category 1. Minimal risk to patient; little or no anticipated blood loss (eg, breast biopsy, cystoscopy).
Category 2. Mild risk to patient; minimal to moderately invasive procedure; estimated blood loss < 500 cc (eg, laparoscopy, arthroscopy, hernia repair).
Category 3. Moderate risk to patient and moderate to significantly invasive; blood loss potential 5001000 cc (eg, laminectomy, total hip or knee replacement).
Category 4. Major risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc (eg, major spinal reconstruction, major reconstruction of GI tract, major vascular repair without intensive care unit stay).
Category 5. Critical risk to patient; highly invasive procedure; anticipated blood loss > 1500 cc with anticipated postoperative intensive care unit stay (eg, cardiac procedure, major vascular repair with anticipated intensive care unit stay).
Statistical analyses were descriptive. We determined the rate of adverse outcomes with 95% confidence intervals (CIs) in the entire patient cohort and among prespecified patient subsets, based on timing of discontinuation of antiplatelet therapy. Predefined subsets included those who had clopidogrel and aspirin discontinued less than 3 months and less than 6 months following DES implantation. The 2 test was used to test the hypothesis that discontinuation of antiplatelet therapy was a function of the type of surgery or timing of stent placement.
The study was approved by the Cleveland Clinic Foundation's institutional review board. The requirement for informed consent was waived.
RESULTS
In total, 114 patients were evaluated in the IMPACT Center following DES placement. Baseline patient characteristics are shown in Table 1. The median age was 71 years (interquartile range 6476 years), and 66% were male. Patients had a moderate degree of comorbidity: 41% had diabetes, 12% had an ejection fraction < 45%, 34% had undergone coronary bypass, 17% had atrial fibrillation or flutter, and 20% had chronic renal insufficiency (creatinine 2.0 or end‐stage renal disease). Most patients received ‐adrenergic blockers (97%), statins (95%), and either angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (77%) preoperatively. Patients underwent a variety of surgeries (Table 1).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Demographics | |
| Age (years), median (IQR) | 71 (6476) |
| Male | 75 (65.7%) |
| White | 88 (77.2%) |
| Comorbid illnesses | |
| Diabetes mellitus | 47 (41.2%) |
| History of prior myocardial infarction | 48 (42.1%) |
| Hypertension | 108 (94.7%) |
| History of stroke or transient cerebral ischemia | 15 (13.2%) |
| Dyslipidemia or treatment with lipid‐lowering drugs | 106 (93.0%) |
| Ejection fraction < 45% | 14 (12.3%) |
| History of coronary artery bypass | 39 (34.2%) |
| Atrial fibrillation or flutter | 19 (16.7%) |
| End‐stage renal disease on dialysis | 13 (11.4%) |
| Chronic renal impairment (creatinine 2.0) without dialysis | 10 (8.8%) |
| Other medical treatments | |
| Angiotensin converting enzyme inhibitor or angiotensin receptor blocker | 88 (77.2%) |
| ‐blocker | 111 (97.3%) |
| Statin | 108 (94.7%) |
| Invasiveness of surgery* | |
| Category 1 (lowest risk) | 37 (32.5%) |
| Category 2 | 22 (19.3%) |
| Category 3 | 48 (42.1%) |
| Category 4 | 7 (6.1%) |
| Category 5 (highest risk) | 0 (0%) |
| Outpatient or short‐stay surgery | 50 (47.2%) |
| Type of surgery | |
| Major orthopedic | 39 (34.2%) |
| Minor orthopedic | 5 (4.4%) |
| Ophthalmologic | 30 (26.3%) |
| General abdominal | 8 (7.0%) |
| Gynecological | 5 (4.4%) |
| Urological | 11 (9.6%) |
| Head and neck | 5 (4.4%) |
| Vascular | 1 (0.9%) |
| Other | 10 (8.8%) |
Patients had received both paclitaxel and sirolimus stents (28% and 73% of patients, respectively); 33% of patients had had more than 1 DES (Table 2). Most patients underwent surgery within 1 year of stent placement (77%), but only 40% had surgery within 180 days of stenting and only 13% within 90 days of stenting. Most patients (77%) had antiplatelet therapy completely discontinued a median of 10 days before surgery and remained off antiplatelet therapy for a median of 14 days total. Ten of the 15 patients (67%) who underwent surgery within 90 days of stenting had all antiplatelet agents discontinued preoperatively, 24 of the 30 patients (80%) who had surgery between 91 and 180 days after stenting had antiplatelet therapy completely discontinued, and 54 of the 69 patients (78%) who had surgery more than 180 days after stenting had antiplatelet therapy completely discontinued. There was no significant relationship between timing of stent placement relative to surgery (<90, 91180, or >180 days) and decision about whether to discontinue antiplatelet therapy (P = .59). However, invasiveness of the surgery was associated with antiplatelet management: 85% of those who continued antiplatelet therapy (aspirin or aspirin and clopidogrel) during the perioperative period were patients who underwent minimally invasive surgery (P < .0001).
| Characteristic | n (%) unless otherwise noted |
|---|---|
| |
| Timing of surgery and antiplatelet agent discontinuation relative to Percutaneous coronary intervention | |
| Duration of most recent intervention relative to surgery (days), median (IQR) | 236 (125354) |
| Surgery within 90 days of DES placement | 15 (13.2%) |
| Surgery within 180 days of DES placement | 45 (39.5%) |
| Surgery within 1 year of DES placement | 88 (77.2%) |
| Percutaneous Coronary Intervention History | |
| Number of drug‐eluting stents | |
| 1 | 76 (66.7%) |
| 2 | 26 (22.8%) |
| 3+ | 12 (10.5%) |
| Paclitaxel stent 1 | 32 (28.1%) |
| Sirolimus stent 1 | 83 (72.8%) |
| Bare‐metal stent 1 | 10 (8.8%) |
| Perioperative antiplatelet treatment | |
| Clopidogrel and aspirin continued through surgery | 24 (21.1%) |
| Aspirin alone continued through surgery | 2 (1.8%) |
| Clopidogrel alone continued through surgery | 0 (0%) |
| No antiplatelet treatment at time of surgery | 88 (77.2%) |
| Among the 15 patients who had surgery within 90 days of stenting | 10 (66.7%) |
| Among the 45 patients who had surgery within 180 days of stenting | 34 (75.6%) |
| Duration of discontinuance of aspirin | |
| Median number of days discontinued preoperatively (IQR) | 10 (812) |
| Median total duration of discontinuance [days, IQR) | 14 (1019) |
| Duration of discontinuance of clopidogrel | |
| Median number of days discontinued preoperatively [days, IQR] | 10 (813) |
| Median number of days discontinued in total (IQR) | 14 (1020) |
The outcome events are presented in Table 3. Two patients (1.8%, 95% CI 0.5%6.2%) suffered a non‐ST‐elevation myocardial infarction (NSTEMI) postoperatively, and another patient (0.9%, 95% CI 0.2%4.8%) developed major bleeding, a retroperitoneal hemorrhage following kidney transplantation. This patient had been taking both aspirin and clopidogrel until 7 days prior to surgery and began to hemorrhage the day after surgery; antiplatelet agents were resumed 12 days postoperatively. No patients died (0%, 95% CI 0%3.3%). One of the 2 patients who suffered an MI was a 72‐year‐old man who had had placement of a single sirolimus‐eluting stent in the posterior descending artery 284 days prior to elective hip arthroplasty. He had no history of myocardial infarction but had undergone coronary bypass surgery 4 years earlier. Echocardiography showed he had aortic stenosis, with a calculated valve area of 0.9 cm2. He had a baseline left ventricular ejection fraction of 45%. His preoperative cardiac medications included lovastatin, lisinopril, and atenolol; he discontinued both aspirin and clopidogrel 7 days before the surgery. His NSTEMI occurred on the day of his operation, presenting with hypotension and anterolateral ST depressions. His troponin T peaked at 0.48 mg/mL, with a peak creatinine kinase of 795 U/L (MB fraction 6%). His left ventricular ejection fraction was 45% on postoperative day 2 (unchanged from baseline). He was discharged on postoperative day 8 and returned for catheterization 3 weeks later, at which time he was found to have a 70% ostial lesion in a saphenous vein graft to an obtuse marginal, which was stented. The previously placed DES was widely patent. The other patient who suffered a postoperative NSTEMI was a 68‐year‐old man with a history of carotid artery stenting and renal artery stenosis who had undergone placement of 3 sirolimus‐eluting stents in the right coronary artery 50 days prior to cervical laminectomy. He had had elective placement of the stents following a positive pharmacologic stress test. He was taking 50 mg of atenolol daily and had been taking aspirin and clopidogrel until 17 days before surgery. On postoperative day 3 he developed dyspnea, and leads V4 and V5 showed ST depressions. His troponin T peaked at 1.24 mg/mL, with a peak creatinine kinase of 879 U/L (MB fraction 6%). The patient underwent left‐heart catheterization on hospital day 10. All 3 DESs were widely patent. His left ventricular ejection fraction was estimated at 65%. He was discharged on postoperative day 15. Because neither of the patients who had a postoperative NSTEMI showed evidence of stent thrombosis on catheterization, the overall rate of stent thrombosis was 0% (95% CI 0%3.3%).
| Outcome | Entire cohort (n = 114) [all antiplatelet therapy stopped in 88 patients (77%)] | Surgery < 90 days after DES (n = 15) [all antiplatelet therapy stopped in 10 patients (67%)] | Surgery < 180 days after DES (n = 45) [all antiplatelet therapy stopped in 34 patients (76%)] |
|---|---|---|---|
| |||
| Death | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Any myocardial infarction | 2 (1.8%, 0.5%6.2%) | 1 (6.7%, 1.2%29.8%) | 1 (2.2%, 0.4%11.6%) |
| DES thrombosis | 0 (0%, 0%3.3%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
| Major bleeding | 1 (0.9%, 0.2%4.8%) | 0 (0%, 0%20.4%) | 0 (0%, 0%7.9%) |
DISCUSSION
Although 2 patients in our study cohort suffered a postoperative myocardial infarction and underwent postoperative catheterization, neither was found to have stent thrombosis, and the MIs of both patients were NSTEMIs with modest cardiac enzyme elevations only. No patients died. A rate of myocardial infarction of less than 2% is well within that expected for patients with established coronary disease undergoing noncardiac surgery.19 That most of our patients discontinued both aspirin and clopidogrel and did not receive antiplatelet agents for a median of 14 days suggests that transient termination of antiplatelet agents in the perioperative setting is not associated with high morbidity or mortality in patients with DES, even when patients have had their stents implanted in the preceding 36 months.
Our study builds on the limited data on this topic. One small case series examined outcomes in 38 patients who had had DES placement and subsequently underwent noncardiac surgery a median of 297 days after stenting.20 None of the patients in this series suffered from stent thrombosis or myocardial infarction, but most underwent surgery without discontinuing aspirin, and 41% underwent surgery without discontinuing clopidogrel. Another recent study demonstrated a high rate of adverse cardiovascular events in patients with coronary stents who underwent noncardiac surgery up to a year after stenting, but the authors of this study did not differentiate between drug‐eluting and bare‐metal stents, and all patients were continued on antiplatelet agents and received parenteral antithrombotic treatment.21
The major strength of our study was its systematic approach. Using a computerized and comprehensive search strategy, we identified all patients who had undergone DES placement at the Cleveland Clinic who subsequently had a preoperative evaluation at the IMPACT Center. Therefore, we are confident that the number of patients in our cohort truly reflects a well‐defined at‐risk population, allowing for an accurate calculation of event rates. This approach contrasts sharply with prior case reports and case series, in which the number of patients at risk was unknown. Nevertheless, these previous reports demonstrate that DES thromboses do occur and can be devastating, so even a small risk of DES thrombosis should be taken seriously. The upper bound of the 95% confidence interval of our estimate of the rate of DES thrombosis was 3.3%, so it is entirely plausible that sampling error contributed to the low rate of thrombosis that we observed.
One major limitation of our study is its sample size. Although our cohort was more than 3 times larger than the only other published cohort of DES patients undergoing noncardiac surgery,20 we had only limited precision to quantify the risk of DES thrombosis. This limitation is particularly relevant for patients who have undergone stent implantation within 36 months of surgery, as they are the patients most likely to have incomplete reendothelialization of the stented artery. We believe that when possible it remains prudent to delay noncardiac surgery for at least 36 months and perhaps up to 12 months following DES implantation, in keeping with recent guidelines.7, 8 However, for patients with conditions such as cancer whose surgery is semielective or patients with nonsurgical bleeding problems (such as gastrointestinal bleeding), our study provides at least some reassurance that short‐term discontinuation of antiplatelet agents may not be as dangerous as some authors have suggested,1 even within 36 months of DES placement. Another important limitation of our study is potential referral bias. At the Cleveland Clinic, most patients undergoing vascular and thoracic procedures are not evaluated at the IMPACT Center. Similarly, some of the patients with severe cardiovascular disease may also have bypassed the IMPACT Center and gone to a cardiologist for preoperative evaluation. As such, we believe our findings should not be generalized to high‐risk cardiac patients or to those undergoing high‐risk procedures.
A noteworthy distinction between our cohort and the cohort reported by Compton and colleagues is that in the perioperative period, most of our patients underwent complete discontinuation of antiplatelet therapy and remained off both aspirin and clopidogrel for an average of 2 weeks, whereas most patients in the other cohort were continued on antiplatelet therapy.20 This highlights the continued controversy surrounding management of antiplatelet therapy in perioperative patients with established coronary disease, who are at substantial risk for both bleeding and myocardial infarction because of the surgery.22 Our data offer little guidance on the optimal management of antiplatelet agents perioperatively because the incidence of both bleeding and thrombosis was low and whether or not patients were continued on antiplatelet agents was not random. We advocate individualized management strategies of perioperative patients with DES. Patients undergoing procedures that carry a high risk of outcome‐affecting bleeding (such as brain surgery) should probably have their antiplatelet agents discontinued preoperatively, whereas those undergoing minor surgery may have their antiplatelet agents continued, provided the surgeon and the anesthesiologist are in agreement with this approach. The timing of DES placement should also be factored into this decision because recently placed stents carry a higher risk of thrombosis.
In summary, our findings clarify the risks of stent thrombosis and postoperative myocardial infarction in clinically stable patients with DES who undergo low‐ and intermediate‐risk noncardiac surgery. Because it is unlikely to ever be ethically appropriate or logistically feasible to conduct a randomized study of patients with DES having early versus delayed noncardiac surgery, observational cohorts will have to suffice. Additional similar studies will help to validate (or refute) our findings and to more precisely quantify the risk of adverse cardiac events when patients with DES undergo surgery, which is real, feared, and potentially catastrophic but may be overestimated.
- ,,, et al.Incidence, predictors, and outcome of thrombosis after successful implantation of drug‐eluting stents.JAMA.2005;293:2126–230.
- ,,, et al.Pathology of drug‐eluting stents in humans: delayed healing and late thrombotic risk.J Am Coll Cardiol.2006;48:193–202.
- ,,, et al.Correlates and long‐term outcomes of angiographically proven stent thrombosis with sirolimus‐ and paclitaxel‐eluting stents.Circulation.2006;113:1108–1113.
- ,,, et al.Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug‐eluting stent placement: results from the PREMIER registry.Circulation.2006;113:2803–2809.
- .Trading restenosis for thrombosis? New questions about drug‐eluting stents.N Engl J Med.2006;355:1949–1952.
- ,,, et al.Late thrombosis in drug‐eluting coronary stents after discontinuation of antiplatelet therapy.Lancet2004;364:1519–1521.
- ,,, et al.ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention).Circulation.2006;113:e166–e286.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction).Circulation.2004;110:588–636.
- ,,, et al.Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians.Circulation.2007;115:813–818.
- ,,, et al.Clinical outcome of patients undergoing non‐cardiac surgery in the two months following coronary stenting.J Am Coll Cardiol.2003;42:234–240.
- ,,,,.Catastrophic outcomes of noncardiac surgery soon after coronary stenting.J Am Coll Cardiol.2000;35:1288–1294.
- ,.Thrombosis of sirolimus‐eluting coronary stent in the postanesthesia care unit.Anesth Analg.2005;101:971–973.
- ,,,,,.Late thrombosis of drug‐eluting stents: a meta‐analysis of randomized clinical trials.Am J Med.2006;119:1056–1061.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med.2007;356:1009–1019.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med.2007;356:998–1008.
- ,,,,.A pooled analysis of data comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med.2007;356:989–997.
- .Preoperative assessment: guidelines and challenges.Acta Anaesthesiol ScandSuppl.1997;111:318–320.
- .Preoperative assessment of the ambulatory and same day admission patient.Wellcome Trends Anesthesiol.1991;9:3–11.
- ,,, et al.Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery.Circulation.1999;100:1043–1049.
- ,,,,.Risk of noncardiac surgery after coronary drug‐eluting stent implantation.Am J Cardiol.2006;98:1212–1213.
- ,,,,,.Coronary artery stenting and non‐cardiac surgery—a prospective outcome study.Br J Anaesth.2006;96:686–693.
- ,,.Double jeopardy: balance between bleeding and stent thrombosis with prolonged dual antiplatelet therapy after drug‐eluting stent implantation.Cardiovasc Revasc Med.2006;7:155–158.
- ,,, et al.Incidence, predictors, and outcome of thrombosis after successful implantation of drug‐eluting stents.JAMA.2005;293:2126–230.
- ,,, et al.Pathology of drug‐eluting stents in humans: delayed healing and late thrombotic risk.J Am Coll Cardiol.2006;48:193–202.
- ,,, et al.Correlates and long‐term outcomes of angiographically proven stent thrombosis with sirolimus‐ and paclitaxel‐eluting stents.Circulation.2006;113:1108–1113.
- ,,, et al.Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug‐eluting stent placement: results from the PREMIER registry.Circulation.2006;113:2803–2809.
- .Trading restenosis for thrombosis? New questions about drug‐eluting stents.N Engl J Med.2006;355:1949–1952.
- ,,, et al.Late thrombosis in drug‐eluting coronary stents after discontinuation of antiplatelet therapy.Lancet2004;364:1519–1521.
- ,,, et al.ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention).Circulation.2006;113:e166–e286.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction).Circulation.2004;110:588–636.
- ,,, et al.Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians.Circulation.2007;115:813–818.
- ,,, et al.Clinical outcome of patients undergoing non‐cardiac surgery in the two months following coronary stenting.J Am Coll Cardiol.2003;42:234–240.
- ,,,,.Catastrophic outcomes of noncardiac surgery soon after coronary stenting.J Am Coll Cardiol.2000;35:1288–1294.
- ,.Thrombosis of sirolimus‐eluting coronary stent in the postanesthesia care unit.Anesth Analg.2005;101:971–973.
- ,,,,,.Late thrombosis of drug‐eluting stents: a meta‐analysis of randomized clinical trials.Am J Med.2006;119:1056–1061.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med.2007;356:1009–1019.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med.2007;356:998–1008.
- ,,,,.A pooled analysis of data comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med.2007;356:989–997.
- .Preoperative assessment: guidelines and challenges.Acta Anaesthesiol ScandSuppl.1997;111:318–320.
- .Preoperative assessment of the ambulatory and same day admission patient.Wellcome Trends Anesthesiol.1991;9:3–11.
- ,,, et al.Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery.Circulation.1999;100:1043–1049.
- ,,,,.Risk of noncardiac surgery after coronary drug‐eluting stent implantation.Am J Cardiol.2006;98:1212–1213.
- ,,,,,.Coronary artery stenting and non‐cardiac surgery—a prospective outcome study.Br J Anaesth.2006;96:686–693.
- ,,.Double jeopardy: balance between bleeding and stent thrombosis with prolonged dual antiplatelet therapy after drug‐eluting stent implantation.Cardiovasc Revasc Med.2006;7:155–158.
Copyright © 2007 Society of Hospital Medicine
Trial of Safety Nets in Hospitalized Patients
Physical restraints, such as bed rails, Posey vests, and 2‐point and 4‐point soft or hard restraints, are commonly used in acute care hospitals to protect agitated patients from harming themselves or others.1 Yet restraints are viewed by patient advocates and health care practitioners as inhumane and overly restrictive. Furthermore, currently used physical restraints have been linked to minor injuries such as sores and abrasions, intensification of agitation, and even death.2, 3 Hospitals and nursing homes are therefore required to try alternative and less severe means of alleviating agitation and delirium among patients before resorting to physical restraints. However, despite a general dislike of restraints and stricter federal guidelines governing their use, the application of restraints is often unavoidable for some patients. It is estimated that between 4% and 25% of in‐patients will have physical restraints applied at some point during their hospital stay.4
Given these numbers, it is surprising that newer and potentially safer restraint systems have not been explored. Safe enclosures may provide health care facilities with an alternative option. This type of restraint consists of a nylon net canopy that safely surrounds both the patient and the mattress. The potential for safe enclosures to provide a safe, humane, and acceptable method of restraint for both hospital staff and patients warranted investigation. In addition, because this system does not restrict a person's ability to move within the enclosure, the many potential hazards of immobility associated with standard restraints may be reduced or eliminated. However, to our knowledge, there have been no reports published of randomized trials comparing standard restraints to newer and possibly safer restraint systems.
We report a randomized controlled trial that compared the use of safe enclosures with standard restraints among agitated, hospitalized patients. Compared with patients in standard restraints, we hypothesized that safe enclosures would: (1) be perceived as more acceptable and humane by family members, physicians, and nurses; (2) lead to improved health outcomes such as decreased duration of restraint use, decreased agitation, shorter length of stay, decreased need to administer medication to treat agitation, and fewer injuries to the patient.
METHODS
Design and Setting
This was a prospective, single‐center, randomized, controlled trial conducted at a community hospital in Connecticut.
Subjects
Male and female hospitalized patients at least 18 years old in the general medicine in‐patient services at a community hospital in Connecticut were assessed for eligibility to participate in this study if they had been put in restraints by the health care team independent of the study for one of these acute conditions: (1) delirium from any cause, including drug or alcohol withdrawal, or other medical conditions resulting in acute delirium; (2) confusional state from any cause; (3) agitation and disruptive behavior requiring restraints; (4) psychosis, hallucinations, or delusions requiring acute intervention (such as medication, restraints, or sitter); or (5) suicidality. Once in restraints, patients were screened for eligibility to participate in this study.
Exclusion criteria included: (1) need for acute respiratory or hemodynamic support or cardiac or septic shock; (2) terminal illness; (3) documented history of claustrophobia; (4) refusal by the family to give consent; (5) hospital stay < 24 hours; and (6) need for intravenous vasopressors, intubation, or ventilatory support. We also excluded patients who had been in restraints for more than 48 hours prior to potential study enrollment. Because safe enclosure would be a redundant system of restraint for patients requiring more than 1 limb in restraints, those patients were also excluded from the study. Figure 1 shows participation flow.
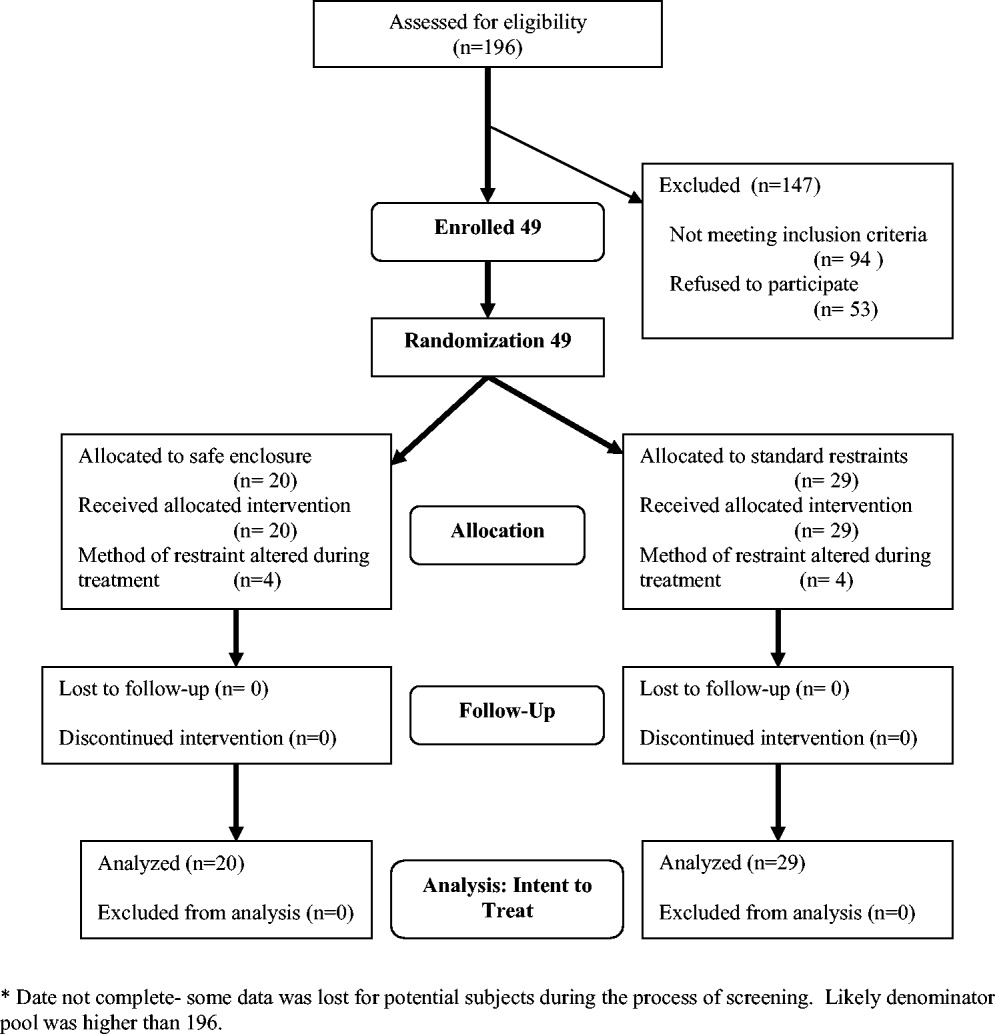
A number of screened patients were excluded for not being appropriate candidates for the safe enclosure. Of these, 20% required more than 1 limb in restraints, 13% required restraint not for agitation but for IV or catheter protection only, 10% were in critical care or on ventilators, and 13% were not appropriate for various other reasons including claustrophobia. The remaining excluded patients may have been eligible but either were preparing for discharge on screening (26%), were in restraints for more than 48 hours on screening (11%), stayed in the hospital less than 24 hours (4%), or had previously been a study participant (3%).
A stratified permuted block randomization was used to control for age (65 vs. >65 years) and sex (male vs. female) to ensure equal representation in both study arms. The study was approved by the institutional review board of the study site, and written informed consent was obtained by the study coordinator from patients' families. Because eligible patients suffered from acute delirium or agitation, most were not sufficiently cognizant to participate in the consent process. As a result, consent was largely obtained from patients' family members. Although the intent of this trial was to recruit 60 patients over an 18‐month period, the study was closed at 49 after 2 years because of slow recruitment and a lack of remaining funds.
Intervention
The safe enclosure, also known as a net bed or safety net, is an alternative to standard restraints. It consists of: (1) a metal frame that sits on the floor completely enclosing a standard hospital bed and (2) a nylon net canopy that encloses the patient and the mattress. We used the SOMA Safe Enclosure (Vivax Medical Corporation, Torrington, CT,
Procedures
Patients were enrolled in this study from April 2003 to February 2005. Once a patient had been placed in restraints by a physician, the nurse in charge alerted the study investigators by beeper of a potential subject, who was then screened based on the above eligibility criteria. We also actively screened restraint log sheets maintained by the nursing staff on most weekdays to monitor new patients who may have been put on restraints. Subjects were randomized to remain in standard restraints or be transferred to the safe enclosure. The randomization scheme was generated using software available at
Modification of the use of restraints is common in hospital settings, as patient needs fluctuate. In the 2 study groups, restraint crossover did occur at the discretion of the attending physician or nurse. Four patients in the safe enclosure group required either additional restraints or had the safe enclosure removed and alternate restraints applied. Similarly, 4 patients in the standard restraint group were either given the safe enclosure or had additional standard restraints applied. Under the principle of intent to treat, patients remained in their original randomized group for the purpose of analyses. This approach provided the most conservative analyses by keeping the sickest patients in the intervention group, thus guarding against type I error.
Measurements
Baseline data obtained at enrollment included: (1) demographic information, (2) clinical information, and (3) restraint information (ie, time of restraint application, clinical indication for use, type of restraint used, ordering physician, and alternative treatment tried before decision to start restraints).
Primary outcomes included: (1) perception survey scores of family members, physicians, and nurses regarding patient comfort, acceptability, and safety of the restraint device; and (2) patient agitation scores. A preplanned subgroup analysis separated nurses into 2 categories (primary and secondary). The admitting nurse was designated the primary nurse; all other nurses were considered secondary nurses. This analysis was performed to examine any differences in perception resulting from a nurse's level of patient involvement.
Family and provider perceptions were assessed with a self‐administered survey containing 11 items each measured on a 10‐point scale (from 1 = viewed negatively to 10 = viewed positively; maximum score 110 points). Surveyed physicians, nurses, and relatives were asked to rate: (1) patient comfort, (2) accessibility to patient, (3) ease of communication with patient, (4) how calm patient was, (5) perceived safety of patient, (6) patient's feeding convenience, (7) ease of bedpan use, (8) impact on recovery time; (9) how humane and ethical the restraint was, (10) recommendation for use on other patients, and (11) how demanding or difficult caring for the patient was.
Agitation was measured using 2 distinct methods: the Alcohol Withdrawal Assessment Form (AWAF)5 and the Agitated Behavior Scale (ABS).6, 7 Both techniques have been widely used to assess delirium of hospitalized patients. The AWAF measures agitation by analyzing key physiologic indicators such as blood pressure and heart rate on a 0‐ to 22‐point scale. The ABS is a 14‐item scale that measures specific behaviors related to agitation (eg, distractibility, uncooperativeness, and restlessness). Each behavior is rated on a 4‐point Likert scale (0‐3); total score ranges from 0 to 42. Each scale was completed once per 8‐hour shift by the nurse on duty.
Secondary outcomes consisted of total length of stay, duration of restraint use, time from application of restraints until time of discharge, and time from admission until time of application of restraints. Length of stay was calculated as the number of days from the time the patient was admitted to the time the patient was discharged. Time from admission until time of restraint application, duration of restraint use, and time from restraint application until discharge were assessed in minutes. These measurements were based on written restraint order forms and nursing progress reports. Hospital protocol regarding restraint requires hospital staff members to document the application, removal, and adjustment of restraints.
Additional outcomes measured included total amount of medications used to treat agitation and number of injuries incurred. Total amount of medication administered was determined with an equivalence system for different drugs used to treat agitation or delirium.811 Medications were separated into 4 groups: antianxiety medications, antidepressants, antipsychotics, and opioid analgesics. Total amount included both regularly administered and as‐needed dosages of medication. We identified injuries through reports of a subject's primary nurse and by review of medical records.
Data Analyses
Sample size was calculated using a 2‐sample t test formula based on the primary outcome. The study was designed to detect an absolute difference in points of 10% (total absolute score difference of 11 per survey or a total difference of 33). The 2‐sided alpha was initially set at 0.05 and the power at 80%, with an estimated standard deviation of 20. The alpha level was Bonferroni‐adjusted for up to 6 additional comparisons, with each significance level of 0.0071 (z = 2.70).
To assess differences in patient characteristics between the standard restraints and safe enclosure groups, we used the Student t test for continuous variables and Fisher's 2‐sided exact test for categorical variables. Differences in family and staff perceptions of the restraint mechanisms were measured using the Student t test with Satterthwaite's method for calculating variance. However, to account for questions marked not applicable by the responder, weighted scores, defined as the total score divided by the percentage of questions answered, were calculated.
Differences in agitation scores (ABS and AWAF) were analyzed using 2 strategies. First, the ABS and AWAF scores 24 hours after study enrollment were compared across groups using the Student t test with Satterthwaite's method for calculating variance. Then, separate comparisons of the ABS and AWAF scores 48 and 72 hours after enrollment were conducted using the Student t test with a pooled variance. Next, 2 longitudinal analyses were performed using a mixed‐effects (fixed and random) model. These analyses modeled change in the ABS or AWAF scores over (1) the first 3 days and (2) the first 6 days of hospitalization as a function of being restrained with the safe enclosure or being restrained with the hospital's standard restraint systems. For these comparisons, the model included not only the main effects of type of restraint and time, but also the interaction between type of restraint and time and the covariates sex, age, and initial ABS or AWAF score. For these models, a backward elimination procedure was undertaken using a significance level of = 0.05 in order to determine the most parsimonious model.
To determine if the total length of subject stay in the hospital was different between groups, the Student t test was used with Satterthwaite's method for calculating variance. Differences in time from admission until time of restraint application, duration of restraint use, and time from application of restraints until time of discharge were analyzed with the Student t test with pooled variances.
To compare the amount of medication used, equivalent dosage conversions were used for each of the 4 medication categories (antianxiety medications, antidepressants, antipsychotics, and opioid analgesics). To determine if the amounts of these 4 categories of medications differed between groups, the Student t test was used. Last, to determine if there was a difference in the number of patient injuries between groups, Fisher's 2‐sided exact test was used.
RESULTS
Study Population
Of the 49 subjects enrolled in the study, 20 were randomized to the safe enclosure and 29 to standard restraints. This imbalance was likely a result of the premature termination of the study, which in turn was a result of slow recruitment. Table 1 shows selected baseline characteristics of the enrolled subjects. There were no significant differences between the 2 groups in sex, age, patient diagnoses, reason for restraint, or type of medication. However, the subjects randomized to the safe enclosure were less likely to have hypertension than those randomized to standard restraints (36.8% vs. 72.4%, P = .019).
| Variable | All (n = 49) | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) |
|---|---|---|---|
| |||
| Sex (male) | 26 (53.1%) | 11 (55.0%) | 15 (51.7%) |
| Age (years) | 81.3 (13.1%) | 77.2 (15.6%) | 84.2 (10.3%) |
| Alzheimer's disease | 23 (47.9%) | 11 (57.9%) | 12 (41.4%) |
| Dementia | 3 (6.3%) | 2 (10.5%) | 1 (3.5%) |
| Coronary artery disease | 19 (39.6%) | 10 (52.6%) | 9 (31.0%) |
| Hypertension* | 28 (58.3%) | 7 (36.8%) | 21 (72.4%) |
| Congestive heart failure | 6 (12.5%) | 3 (15.8%) | 3 (10.3%) |
| Atrial fibrillation | 7 (14.6%) | 1 (5.3%) | 6 (20.7%) |
| Transient ischemic attacks/cerebral vascular accidents | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Chronic obstructive pulmonary disease | 3 (6.3%) | 1 (5.3%) | 2 (6.9%) |
| Diabetes mellitus | 11 (22.9%) | 5 (26.3%) | 6 (20.7%) |
| Alcohol abuse | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Drug abuse | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Where admitted | |||
| General medicine floor | 41 (83.7%) | 17 (85.0%) | 24 (82.8%) |
| Telemetry | 7 (14.3%) | 2 (10.0%) | 5 (17.2%) |
| ICU | 1 (2.0%) | 1 (5.0%) | 0 (0.0%) |
Primary Outcomes
The rates of response to the perception survey were: relatives/next of kin, 90%; physicians, 90%; primary nurses, 100%; and secondary nurses, 78%. Family members and physicians viewed the safe enclosure significantly more positively than they viewed standard restraints (P < .0001 and P < .0001, respectively; Table 2). There was a trend toward more positive perceptions of the safe enclosure among nurses; however, this trend did not achieve statistical significance (P = .0836). The subgroup analysis of nurses (primary vs. secondary) revealed that secondary nurses viewed the safe enclosure more positively (P = .023). Primary nurses tended to view the safe enclosure more positively than the standard restraints, but the association was not significant (P = .1313).
| Variable | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) | P value (observed power)* |
|---|---|---|---|
| |||
| 1. Perception Survey | |||
| Relative or next of kin | 86.84 | 68.47 | < .0001 (96%) |
| Physician | 83.38 | 65.76 | < .0001 (96%) |
| All nurses | 75.20 | 69.45 | .086 (40%) |
| Primary nurse | 75.45 | 69.72 | .1313 (31%) |
| Secondary nurse | 80.35 | 69.82 | .0230 (58%) |
| 2. Alcohol Withdrawal Assessment Form | |||
| 24 hours | 3.06 | 3.25 | .7972 (6%) |
| 48 hours | 3.23 | 3.40 | .8516 (5%) |
| 72 hours | 3.44 | 2.67 | .6163 (7%) |
| 3. Agitated Behavior Scale score | |||
| 24 hours | 11.93 | 8.33 | .2312 (27%) |
| 48 hours | 6.00 | 8.75 | .3743 (13%) |
| 72 hours | 7.83 | 7.11 | .7762 (6%) |
There were no statistically significant differences between the 2 randomized groups in ABS or AWAF scores 24, 48, or 72 hours after restraint application (Table 2). In addition, there were no statistically significant differences during the study between the groups in the rates of change in ABS or AWAF score . This was the case when looking at the first 3 days of hospitalization as well as the first 6 days (data not shown). All results were also calculated after adjusting for length of stay; this covariate did not affect any of the results.
Table 3 details the results for each perception survey question. Perceived comfort, calmness, and safety of patients were rated higher in the safe enclosure group by physicians, relatives, and all nurses. With the exception of perceived accessibility to patients, relatives rated the safe enclosure higher than standard restraints on all other perception measures. Table 4 illustrates the differences in the responses of primary and secondary nurse to each perception survey question. Primary and secondary nurses viewed the safety of the safe enclosure significantly more positively than they did the standard restraints.
| Variable | Relative/next of kin (n = 16, 28) | Primary and secondary nurses (n = 29, 29) | Physician (n = 29, 29) |
|---|---|---|---|
| |||
| Comfort | (8.78, 7.29).0033 | (7.98, 6.78).0194 | (8.40, 6.77).0003 |
| Accessibility | (8.28, 8.07).6486 | (7.68, 8.29).2236 | (8.35, 7.58).1056 |
| Communication | (9.11, 8.19).0214 | (8.29, 8.12).7333 | (8.40, 8.31).8469 |
| Calmness | (8.72, 6.29).0005 | (7.68, 6.53).0382 | (7.70, 5.92).0062 |
| Safety | (9.11, 6.74) < 0.001 | (8.53, 6.76).0024 | (8.60, 5.96).0002 |
| Feeding convenience | (8.50, 7.04).0164 | (7.11, 7.74).2327 | (8.25, 6.28).0047 |
| Ease of bedpan use | (7.91, 6.06).0224 | (7.36, 6.90).3977 | (6.82, 6.25).5376 |
| Impact on recovery time | (7.53, 6.07).0244 | (6.29, 5.66).3864 | (6.95, 6.43).4254 |
| Humane/ethical | (7.94, 5.50).0026 | (6.88, 6.31).4049 | (7.95, 5.96).0052 |
| Recommend for other patients | (8.71, 5.50).0002 | (7.15, 6.12).1395 | (8.05, 6.04).0037 |
| Ease of caring for patient | (8.44, 5.70) < .001 | (7.55, 6.38).0749 | (8.05, 6.25).0028 |
| Variable | Primary Nurse (n = 20, 29) (SOMA safe enclosure, control)* P value | Secondary Nurse (n = 12, 26) (SOMA safe enclosure, control)* P value |
|---|---|---|
| ||
| Comfort | (7.85, 6.62).0270 | (8.33, 6.81).0346 |
| Accessibility | (7.55, 8.21).2656 | (8.17, 8.16).9902 |
| Communication | (8.21, 8.34).8093 | (8.83, 7.88).0705 |
| Calmness | (7.70, 6.28).0153 | (7.83, 6.85).2001 |
| Safety | (8.55, 6.34).0012 | (8.67, 6.76).0435 |
| Feeding convenience | (7.37, 7.93).3861 | (7.60, 7.42).8282 |
| Ease of bedpan use | (7.53, 6.95).3945 | (7.00, 6.84).8602 |
| Impact on recovery time | (6.16, 5.39).3251 | (7.50, 6.50).2340 |
| Humane/ethical | (6.45, 6.66).7871 | (7.73, 5.96).0571 |
| Recommend for other patients | (6.70, 6.11).4553 | (8.42, 5.92).0075 |
| Ease of caring for patient | (7.65, 6.41).0860 | (7.83, 6.38).0565 |
Secondary Outcomes
There was a trend toward shorter total length of stay, time from admission until restraint application, duration of restraint use, and time from restraint application until discharge among subjects restrained by the safe enclosure compared with those restrained with standard restraints. However, these unadjusted differences were not statistically significant. We examined secondary outcomes after adjusting for 2 covariates, age and sex. Age but not sex affected the results. We found that subjects in the intervention group younger than 80 years of age had a shorter length of stay for 2 of the 4 related outcomes: time of admittance to time of discharge (P = .0199) and time of restraint to time of discharge (P = .0274). Time of admission to time of restraint application and duration of restraint did not differ between groups. The former outcome was not expected to differ between groups.
Additional Outcomes
There were no differences between groups in the amounts of 3 of the 4 types of medications used to treat agitation or delirium (ie, antianxiety medications, antipsychotic medications, opioid analgesic medications). The proportion of patients on these medications did not differ by group (P = .59). Only 5% of patients in standard restraints were on antidepressants, and about 5% were on opioids in each group. There was only 1 minor patient injury recorded during the study. This minor abrasion was to a patient assigned to the standard restraint group. No injuries were reported in the safe enclosure group.
DISCUSSION
We have demonstrated that the SOMA Safe Enclosure may be a more acceptable alternative to the restraints currently in use. Our results show that the safe enclosure was rated as more acceptable by family members, physicians, and secondary nurses in our composite perception scores. The results from the primary nurses did not show a significant difference between the 2 groups. An analysis of the individual perception variables found that family members viewed the safe enclosure as more acceptable for 10 of the 11 variables examined. Furthermore, in this small‐scale study, safe enclosures appeared to be safe, as there were no injuries reported in the intervention group. As stated above, there was 1 minor injury reported in the standard restraint groups.
Restraints are commonly used to protect agitated hospitalized patients from harming themselves or others. Despite the significant reluctance of hospital staff members to use restraints, they continue to be necessary in certain situations. Factors such as a general nursing shortage and the expense required to allocate nursing or other ancillary health care workers as sitters contribute to the use of restraints. Therefore, it is reasonable to conclude that restraint use in some form or fashion will continue into the foreseeable future. There are no clear estimates of the prevalence of restraint use in acute care hospitals. A chart review study from Canada reported physical restraints in about 7.7% of in‐patients.12 Other studies have reported the use of restraints on patients in the range of 4%‐25%.2 Given the prevalence of restraint use in acute care hospitals, surprisingly little innovative research has been undertaken to develop more effective and humane systems of restraint. Furthermore, no research has examined how restraint use may affect important clinical outcomes such as length of stay. To our knowledge, this is the first clinical trial to compare currently used restraints to a newer method of restraint using the SOMA Safe Enclosure.
The idea that restraint use can lead to further agitation is not supported by our data. We observed a decrease in agitated behavior scale scores from 9.6 to 7.4 from the 24‐ and to the 72‐hour assessments; however, these results were not significant and appeared to be more dramatic for the safe enclosure group because of higher baseline levels. Our adjusted analyses of length of stayrelated outcomes indicated an association with age. Total length of stay and time from restraint application until discharge were significantly reduced for those subjects younger than 80 years of age in the safe enclosure group. The basis for this finding is not entirely clear. It may be a chance finding, or there may have been a complex combination of factors at work.
There was a reduction in overall length of stay by 1.5 days among those in the safe enclosure group when compared with the standard restraint group. Similarly, total duration of restraint use of the safe enclosure group was 551 minutes (9 hours) shorter. Although these findings were not significant, they warrant further investigation in a larger trial. If safe enclosure use truly reduces length of stay and duration of restraint use, it is an important finding, for it could translate into meaningful cost savings for acute care hospitals. It is possible, however, that any potential cost savings could be tempered by the additional time required to set up the enclosure. Ethically, if restraints are to be used, their use should be minimized, and in that sense, safe enclosures may help acute care hospitals achieve this goal more effectively.
Limitations of this trial include its small sample size and inadequate power to determine certain outcomes. Although we saw encouraging trends in several outcomes, they failed to reach statistical significance because of the limited power. For instance, the observed power for total length of stay difference was only 17%. It is conceivable that a larger trial powered specifically for length of stayrelated outcomes may show significant results. Because subjects in this study were patients in a single midsize community teaching hospital, the results may not be generalizable to patients in, for example, tertiary‐care centers or nursing homes. However, these results may apply to a large proportion of patients in the United States, as most are treated in community hospitals. We found that many patients required 2 wrist restraints in order to protect IV lines, and this resulted in exclusion of a large proportion of potential subjects. Therefore, safe enclosures may not be appropriate for all agitated patients. They may be an ideal method of restraining patients who are not at risk of pulling out their IV line or catheters but require restraints for other reasons. This could include patients in nursing homes or rehabilitation centers.
It is also important to discuss the issue of practitioner acceptability of a newer method of restraint in acute care hospitals. As expected, we found the nursing staff was originally reluctant to use the safe enclosure, even as part of a trial. This may have been because of fear of change and having a high level of comfort with the restraint systems already in use. The setup of safe enclosures can take 10‐15 minutes, whereas the use of 2‐point soft restraints or Posey vests can be accomplished in as little as a minute. However, we found that after initial use of the safe enclosure, resistance among nurses declined. In fact, in our hospital, nurses began using safe enclosures for confused and agitated patients not enrolled in the study in order to prevent wandering and falls at night. Another difficulty reported by the nursing staff was feeling somewhat limited in their access to patients by a safe enclosure. Nurses had to open a zipped flap to access the patient to administer medication or provide food. Health care providers must remember to close the flap to avoid potential falls.
In summary, safe enclosures seem to be a safe and more acceptable alternative to the restraints currently in use in acute care hospitals. These findings should be replicated in a larger trial.
- ,,,,.Prevalence and patterns of physical restraint use in the acute care setting.J Nurs Adm.1998;28(11):19–24.
- ,Strumpf. Myths about Elder Restraint.J Nurs Scholarsh.1990;22(2):124–128.
- , et al.Deadly restraint: a Hartford Courant investigative report.Hartford Courant1998; October 11‐15.
- ,,,,,, et al.Jt Comm J Qual Improv2001;27:605–618.
- ,,,,.Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale.Br J Addict.1989;84:1353–1357.
- ,.Development of an agitated behavior rating scale for discrete temporal observations.Nursing Meas1993;1:115–124.
- ,,,.Reliability of the Agitated Behavior Scale.J Head Trauma Rehabil.1999;14:91–96.
- University of Newcastle. The Ashton Manual. Available at: http://www.benzo.org.uk/manual/bzcha01.htm. Accessed November 15,2006.
- Postgraduate Medicine Online. Sedation and analgesia in intensive care. Available at: http://www.postgradmed.com/issues/2002/02_02/blanchard.htm. Accessed November 15,2006.
- Anti‐psychotic Comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antipsychotics%20Comparison%20Chart.pdf. Accessed November 15,2006.
- Anti‐depressant comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antidepressant%20comparison%20Chart.pdf. Accessed November 15,2006.
- ,.Use of physical and chemical restraints in medical teaching units.Can Med Assoc J.2000;162:339–340.
Physical restraints, such as bed rails, Posey vests, and 2‐point and 4‐point soft or hard restraints, are commonly used in acute care hospitals to protect agitated patients from harming themselves or others.1 Yet restraints are viewed by patient advocates and health care practitioners as inhumane and overly restrictive. Furthermore, currently used physical restraints have been linked to minor injuries such as sores and abrasions, intensification of agitation, and even death.2, 3 Hospitals and nursing homes are therefore required to try alternative and less severe means of alleviating agitation and delirium among patients before resorting to physical restraints. However, despite a general dislike of restraints and stricter federal guidelines governing their use, the application of restraints is often unavoidable for some patients. It is estimated that between 4% and 25% of in‐patients will have physical restraints applied at some point during their hospital stay.4
Given these numbers, it is surprising that newer and potentially safer restraint systems have not been explored. Safe enclosures may provide health care facilities with an alternative option. This type of restraint consists of a nylon net canopy that safely surrounds both the patient and the mattress. The potential for safe enclosures to provide a safe, humane, and acceptable method of restraint for both hospital staff and patients warranted investigation. In addition, because this system does not restrict a person's ability to move within the enclosure, the many potential hazards of immobility associated with standard restraints may be reduced or eliminated. However, to our knowledge, there have been no reports published of randomized trials comparing standard restraints to newer and possibly safer restraint systems.
We report a randomized controlled trial that compared the use of safe enclosures with standard restraints among agitated, hospitalized patients. Compared with patients in standard restraints, we hypothesized that safe enclosures would: (1) be perceived as more acceptable and humane by family members, physicians, and nurses; (2) lead to improved health outcomes such as decreased duration of restraint use, decreased agitation, shorter length of stay, decreased need to administer medication to treat agitation, and fewer injuries to the patient.
METHODS
Design and Setting
This was a prospective, single‐center, randomized, controlled trial conducted at a community hospital in Connecticut.
Subjects
Male and female hospitalized patients at least 18 years old in the general medicine in‐patient services at a community hospital in Connecticut were assessed for eligibility to participate in this study if they had been put in restraints by the health care team independent of the study for one of these acute conditions: (1) delirium from any cause, including drug or alcohol withdrawal, or other medical conditions resulting in acute delirium; (2) confusional state from any cause; (3) agitation and disruptive behavior requiring restraints; (4) psychosis, hallucinations, or delusions requiring acute intervention (such as medication, restraints, or sitter); or (5) suicidality. Once in restraints, patients were screened for eligibility to participate in this study.
Exclusion criteria included: (1) need for acute respiratory or hemodynamic support or cardiac or septic shock; (2) terminal illness; (3) documented history of claustrophobia; (4) refusal by the family to give consent; (5) hospital stay < 24 hours; and (6) need for intravenous vasopressors, intubation, or ventilatory support. We also excluded patients who had been in restraints for more than 48 hours prior to potential study enrollment. Because safe enclosure would be a redundant system of restraint for patients requiring more than 1 limb in restraints, those patients were also excluded from the study. Figure 1 shows participation flow.
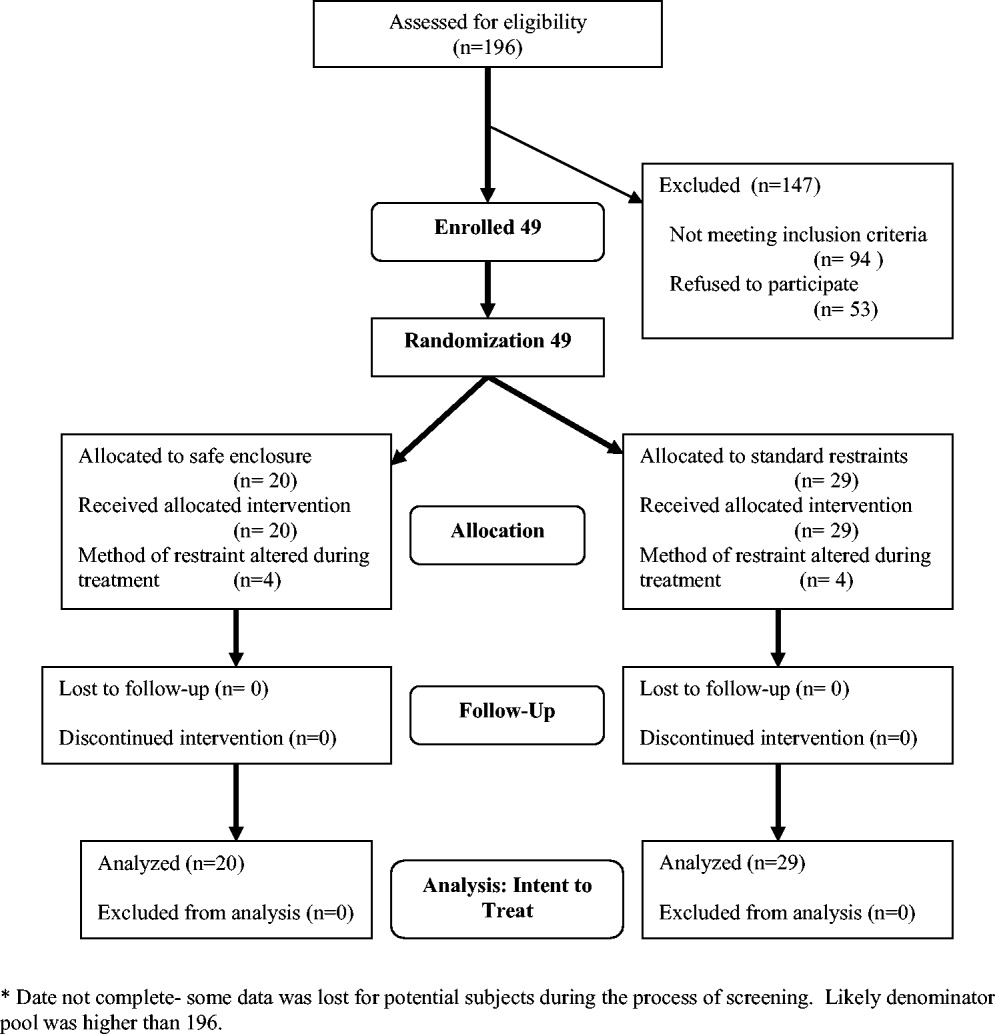
A number of screened patients were excluded for not being appropriate candidates for the safe enclosure. Of these, 20% required more than 1 limb in restraints, 13% required restraint not for agitation but for IV or catheter protection only, 10% were in critical care or on ventilators, and 13% were not appropriate for various other reasons including claustrophobia. The remaining excluded patients may have been eligible but either were preparing for discharge on screening (26%), were in restraints for more than 48 hours on screening (11%), stayed in the hospital less than 24 hours (4%), or had previously been a study participant (3%).
A stratified permuted block randomization was used to control for age (65 vs. >65 years) and sex (male vs. female) to ensure equal representation in both study arms. The study was approved by the institutional review board of the study site, and written informed consent was obtained by the study coordinator from patients' families. Because eligible patients suffered from acute delirium or agitation, most were not sufficiently cognizant to participate in the consent process. As a result, consent was largely obtained from patients' family members. Although the intent of this trial was to recruit 60 patients over an 18‐month period, the study was closed at 49 after 2 years because of slow recruitment and a lack of remaining funds.
Intervention
The safe enclosure, also known as a net bed or safety net, is an alternative to standard restraints. It consists of: (1) a metal frame that sits on the floor completely enclosing a standard hospital bed and (2) a nylon net canopy that encloses the patient and the mattress. We used the SOMA Safe Enclosure (Vivax Medical Corporation, Torrington, CT,
Procedures
Patients were enrolled in this study from April 2003 to February 2005. Once a patient had been placed in restraints by a physician, the nurse in charge alerted the study investigators by beeper of a potential subject, who was then screened based on the above eligibility criteria. We also actively screened restraint log sheets maintained by the nursing staff on most weekdays to monitor new patients who may have been put on restraints. Subjects were randomized to remain in standard restraints or be transferred to the safe enclosure. The randomization scheme was generated using software available at
Modification of the use of restraints is common in hospital settings, as patient needs fluctuate. In the 2 study groups, restraint crossover did occur at the discretion of the attending physician or nurse. Four patients in the safe enclosure group required either additional restraints or had the safe enclosure removed and alternate restraints applied. Similarly, 4 patients in the standard restraint group were either given the safe enclosure or had additional standard restraints applied. Under the principle of intent to treat, patients remained in their original randomized group for the purpose of analyses. This approach provided the most conservative analyses by keeping the sickest patients in the intervention group, thus guarding against type I error.
Measurements
Baseline data obtained at enrollment included: (1) demographic information, (2) clinical information, and (3) restraint information (ie, time of restraint application, clinical indication for use, type of restraint used, ordering physician, and alternative treatment tried before decision to start restraints).
Primary outcomes included: (1) perception survey scores of family members, physicians, and nurses regarding patient comfort, acceptability, and safety of the restraint device; and (2) patient agitation scores. A preplanned subgroup analysis separated nurses into 2 categories (primary and secondary). The admitting nurse was designated the primary nurse; all other nurses were considered secondary nurses. This analysis was performed to examine any differences in perception resulting from a nurse's level of patient involvement.
Family and provider perceptions were assessed with a self‐administered survey containing 11 items each measured on a 10‐point scale (from 1 = viewed negatively to 10 = viewed positively; maximum score 110 points). Surveyed physicians, nurses, and relatives were asked to rate: (1) patient comfort, (2) accessibility to patient, (3) ease of communication with patient, (4) how calm patient was, (5) perceived safety of patient, (6) patient's feeding convenience, (7) ease of bedpan use, (8) impact on recovery time; (9) how humane and ethical the restraint was, (10) recommendation for use on other patients, and (11) how demanding or difficult caring for the patient was.
Agitation was measured using 2 distinct methods: the Alcohol Withdrawal Assessment Form (AWAF)5 and the Agitated Behavior Scale (ABS).6, 7 Both techniques have been widely used to assess delirium of hospitalized patients. The AWAF measures agitation by analyzing key physiologic indicators such as blood pressure and heart rate on a 0‐ to 22‐point scale. The ABS is a 14‐item scale that measures specific behaviors related to agitation (eg, distractibility, uncooperativeness, and restlessness). Each behavior is rated on a 4‐point Likert scale (0‐3); total score ranges from 0 to 42. Each scale was completed once per 8‐hour shift by the nurse on duty.
Secondary outcomes consisted of total length of stay, duration of restraint use, time from application of restraints until time of discharge, and time from admission until time of application of restraints. Length of stay was calculated as the number of days from the time the patient was admitted to the time the patient was discharged. Time from admission until time of restraint application, duration of restraint use, and time from restraint application until discharge were assessed in minutes. These measurements were based on written restraint order forms and nursing progress reports. Hospital protocol regarding restraint requires hospital staff members to document the application, removal, and adjustment of restraints.
Additional outcomes measured included total amount of medications used to treat agitation and number of injuries incurred. Total amount of medication administered was determined with an equivalence system for different drugs used to treat agitation or delirium.811 Medications were separated into 4 groups: antianxiety medications, antidepressants, antipsychotics, and opioid analgesics. Total amount included both regularly administered and as‐needed dosages of medication. We identified injuries through reports of a subject's primary nurse and by review of medical records.
Data Analyses
Sample size was calculated using a 2‐sample t test formula based on the primary outcome. The study was designed to detect an absolute difference in points of 10% (total absolute score difference of 11 per survey or a total difference of 33). The 2‐sided alpha was initially set at 0.05 and the power at 80%, with an estimated standard deviation of 20. The alpha level was Bonferroni‐adjusted for up to 6 additional comparisons, with each significance level of 0.0071 (z = 2.70).
To assess differences in patient characteristics between the standard restraints and safe enclosure groups, we used the Student t test for continuous variables and Fisher's 2‐sided exact test for categorical variables. Differences in family and staff perceptions of the restraint mechanisms were measured using the Student t test with Satterthwaite's method for calculating variance. However, to account for questions marked not applicable by the responder, weighted scores, defined as the total score divided by the percentage of questions answered, were calculated.
Differences in agitation scores (ABS and AWAF) were analyzed using 2 strategies. First, the ABS and AWAF scores 24 hours after study enrollment were compared across groups using the Student t test with Satterthwaite's method for calculating variance. Then, separate comparisons of the ABS and AWAF scores 48 and 72 hours after enrollment were conducted using the Student t test with a pooled variance. Next, 2 longitudinal analyses were performed using a mixed‐effects (fixed and random) model. These analyses modeled change in the ABS or AWAF scores over (1) the first 3 days and (2) the first 6 days of hospitalization as a function of being restrained with the safe enclosure or being restrained with the hospital's standard restraint systems. For these comparisons, the model included not only the main effects of type of restraint and time, but also the interaction between type of restraint and time and the covariates sex, age, and initial ABS or AWAF score. For these models, a backward elimination procedure was undertaken using a significance level of = 0.05 in order to determine the most parsimonious model.
To determine if the total length of subject stay in the hospital was different between groups, the Student t test was used with Satterthwaite's method for calculating variance. Differences in time from admission until time of restraint application, duration of restraint use, and time from application of restraints until time of discharge were analyzed with the Student t test with pooled variances.
To compare the amount of medication used, equivalent dosage conversions were used for each of the 4 medication categories (antianxiety medications, antidepressants, antipsychotics, and opioid analgesics). To determine if the amounts of these 4 categories of medications differed between groups, the Student t test was used. Last, to determine if there was a difference in the number of patient injuries between groups, Fisher's 2‐sided exact test was used.
RESULTS
Study Population
Of the 49 subjects enrolled in the study, 20 were randomized to the safe enclosure and 29 to standard restraints. This imbalance was likely a result of the premature termination of the study, which in turn was a result of slow recruitment. Table 1 shows selected baseline characteristics of the enrolled subjects. There were no significant differences between the 2 groups in sex, age, patient diagnoses, reason for restraint, or type of medication. However, the subjects randomized to the safe enclosure were less likely to have hypertension than those randomized to standard restraints (36.8% vs. 72.4%, P = .019).
| Variable | All (n = 49) | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) |
|---|---|---|---|
| |||
| Sex (male) | 26 (53.1%) | 11 (55.0%) | 15 (51.7%) |
| Age (years) | 81.3 (13.1%) | 77.2 (15.6%) | 84.2 (10.3%) |
| Alzheimer's disease | 23 (47.9%) | 11 (57.9%) | 12 (41.4%) |
| Dementia | 3 (6.3%) | 2 (10.5%) | 1 (3.5%) |
| Coronary artery disease | 19 (39.6%) | 10 (52.6%) | 9 (31.0%) |
| Hypertension* | 28 (58.3%) | 7 (36.8%) | 21 (72.4%) |
| Congestive heart failure | 6 (12.5%) | 3 (15.8%) | 3 (10.3%) |
| Atrial fibrillation | 7 (14.6%) | 1 (5.3%) | 6 (20.7%) |
| Transient ischemic attacks/cerebral vascular accidents | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Chronic obstructive pulmonary disease | 3 (6.3%) | 1 (5.3%) | 2 (6.9%) |
| Diabetes mellitus | 11 (22.9%) | 5 (26.3%) | 6 (20.7%) |
| Alcohol abuse | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Drug abuse | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Where admitted | |||
| General medicine floor | 41 (83.7%) | 17 (85.0%) | 24 (82.8%) |
| Telemetry | 7 (14.3%) | 2 (10.0%) | 5 (17.2%) |
| ICU | 1 (2.0%) | 1 (5.0%) | 0 (0.0%) |
Primary Outcomes
The rates of response to the perception survey were: relatives/next of kin, 90%; physicians, 90%; primary nurses, 100%; and secondary nurses, 78%. Family members and physicians viewed the safe enclosure significantly more positively than they viewed standard restraints (P < .0001 and P < .0001, respectively; Table 2). There was a trend toward more positive perceptions of the safe enclosure among nurses; however, this trend did not achieve statistical significance (P = .0836). The subgroup analysis of nurses (primary vs. secondary) revealed that secondary nurses viewed the safe enclosure more positively (P = .023). Primary nurses tended to view the safe enclosure more positively than the standard restraints, but the association was not significant (P = .1313).
| Variable | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) | P value (observed power)* |
|---|---|---|---|
| |||
| 1. Perception Survey | |||
| Relative or next of kin | 86.84 | 68.47 | < .0001 (96%) |
| Physician | 83.38 | 65.76 | < .0001 (96%) |
| All nurses | 75.20 | 69.45 | .086 (40%) |
| Primary nurse | 75.45 | 69.72 | .1313 (31%) |
| Secondary nurse | 80.35 | 69.82 | .0230 (58%) |
| 2. Alcohol Withdrawal Assessment Form | |||
| 24 hours | 3.06 | 3.25 | .7972 (6%) |
| 48 hours | 3.23 | 3.40 | .8516 (5%) |
| 72 hours | 3.44 | 2.67 | .6163 (7%) |
| 3. Agitated Behavior Scale score | |||
| 24 hours | 11.93 | 8.33 | .2312 (27%) |
| 48 hours | 6.00 | 8.75 | .3743 (13%) |
| 72 hours | 7.83 | 7.11 | .7762 (6%) |
There were no statistically significant differences between the 2 randomized groups in ABS or AWAF scores 24, 48, or 72 hours after restraint application (Table 2). In addition, there were no statistically significant differences during the study between the groups in the rates of change in ABS or AWAF score . This was the case when looking at the first 3 days of hospitalization as well as the first 6 days (data not shown). All results were also calculated after adjusting for length of stay; this covariate did not affect any of the results.
Table 3 details the results for each perception survey question. Perceived comfort, calmness, and safety of patients were rated higher in the safe enclosure group by physicians, relatives, and all nurses. With the exception of perceived accessibility to patients, relatives rated the safe enclosure higher than standard restraints on all other perception measures. Table 4 illustrates the differences in the responses of primary and secondary nurse to each perception survey question. Primary and secondary nurses viewed the safety of the safe enclosure significantly more positively than they did the standard restraints.
| Variable | Relative/next of kin (n = 16, 28) | Primary and secondary nurses (n = 29, 29) | Physician (n = 29, 29) |
|---|---|---|---|
| |||
| Comfort | (8.78, 7.29).0033 | (7.98, 6.78).0194 | (8.40, 6.77).0003 |
| Accessibility | (8.28, 8.07).6486 | (7.68, 8.29).2236 | (8.35, 7.58).1056 |
| Communication | (9.11, 8.19).0214 | (8.29, 8.12).7333 | (8.40, 8.31).8469 |
| Calmness | (8.72, 6.29).0005 | (7.68, 6.53).0382 | (7.70, 5.92).0062 |
| Safety | (9.11, 6.74) < 0.001 | (8.53, 6.76).0024 | (8.60, 5.96).0002 |
| Feeding convenience | (8.50, 7.04).0164 | (7.11, 7.74).2327 | (8.25, 6.28).0047 |
| Ease of bedpan use | (7.91, 6.06).0224 | (7.36, 6.90).3977 | (6.82, 6.25).5376 |
| Impact on recovery time | (7.53, 6.07).0244 | (6.29, 5.66).3864 | (6.95, 6.43).4254 |
| Humane/ethical | (7.94, 5.50).0026 | (6.88, 6.31).4049 | (7.95, 5.96).0052 |
| Recommend for other patients | (8.71, 5.50).0002 | (7.15, 6.12).1395 | (8.05, 6.04).0037 |
| Ease of caring for patient | (8.44, 5.70) < .001 | (7.55, 6.38).0749 | (8.05, 6.25).0028 |
| Variable | Primary Nurse (n = 20, 29) (SOMA safe enclosure, control)* P value | Secondary Nurse (n = 12, 26) (SOMA safe enclosure, control)* P value |
|---|---|---|
| ||
| Comfort | (7.85, 6.62).0270 | (8.33, 6.81).0346 |
| Accessibility | (7.55, 8.21).2656 | (8.17, 8.16).9902 |
| Communication | (8.21, 8.34).8093 | (8.83, 7.88).0705 |
| Calmness | (7.70, 6.28).0153 | (7.83, 6.85).2001 |
| Safety | (8.55, 6.34).0012 | (8.67, 6.76).0435 |
| Feeding convenience | (7.37, 7.93).3861 | (7.60, 7.42).8282 |
| Ease of bedpan use | (7.53, 6.95).3945 | (7.00, 6.84).8602 |
| Impact on recovery time | (6.16, 5.39).3251 | (7.50, 6.50).2340 |
| Humane/ethical | (6.45, 6.66).7871 | (7.73, 5.96).0571 |
| Recommend for other patients | (6.70, 6.11).4553 | (8.42, 5.92).0075 |
| Ease of caring for patient | (7.65, 6.41).0860 | (7.83, 6.38).0565 |
Secondary Outcomes
There was a trend toward shorter total length of stay, time from admission until restraint application, duration of restraint use, and time from restraint application until discharge among subjects restrained by the safe enclosure compared with those restrained with standard restraints. However, these unadjusted differences were not statistically significant. We examined secondary outcomes after adjusting for 2 covariates, age and sex. Age but not sex affected the results. We found that subjects in the intervention group younger than 80 years of age had a shorter length of stay for 2 of the 4 related outcomes: time of admittance to time of discharge (P = .0199) and time of restraint to time of discharge (P = .0274). Time of admission to time of restraint application and duration of restraint did not differ between groups. The former outcome was not expected to differ between groups.
Additional Outcomes
There were no differences between groups in the amounts of 3 of the 4 types of medications used to treat agitation or delirium (ie, antianxiety medications, antipsychotic medications, opioid analgesic medications). The proportion of patients on these medications did not differ by group (P = .59). Only 5% of patients in standard restraints were on antidepressants, and about 5% were on opioids in each group. There was only 1 minor patient injury recorded during the study. This minor abrasion was to a patient assigned to the standard restraint group. No injuries were reported in the safe enclosure group.
DISCUSSION
We have demonstrated that the SOMA Safe Enclosure may be a more acceptable alternative to the restraints currently in use. Our results show that the safe enclosure was rated as more acceptable by family members, physicians, and secondary nurses in our composite perception scores. The results from the primary nurses did not show a significant difference between the 2 groups. An analysis of the individual perception variables found that family members viewed the safe enclosure as more acceptable for 10 of the 11 variables examined. Furthermore, in this small‐scale study, safe enclosures appeared to be safe, as there were no injuries reported in the intervention group. As stated above, there was 1 minor injury reported in the standard restraint groups.
Restraints are commonly used to protect agitated hospitalized patients from harming themselves or others. Despite the significant reluctance of hospital staff members to use restraints, they continue to be necessary in certain situations. Factors such as a general nursing shortage and the expense required to allocate nursing or other ancillary health care workers as sitters contribute to the use of restraints. Therefore, it is reasonable to conclude that restraint use in some form or fashion will continue into the foreseeable future. There are no clear estimates of the prevalence of restraint use in acute care hospitals. A chart review study from Canada reported physical restraints in about 7.7% of in‐patients.12 Other studies have reported the use of restraints on patients in the range of 4%‐25%.2 Given the prevalence of restraint use in acute care hospitals, surprisingly little innovative research has been undertaken to develop more effective and humane systems of restraint. Furthermore, no research has examined how restraint use may affect important clinical outcomes such as length of stay. To our knowledge, this is the first clinical trial to compare currently used restraints to a newer method of restraint using the SOMA Safe Enclosure.
The idea that restraint use can lead to further agitation is not supported by our data. We observed a decrease in agitated behavior scale scores from 9.6 to 7.4 from the 24‐ and to the 72‐hour assessments; however, these results were not significant and appeared to be more dramatic for the safe enclosure group because of higher baseline levels. Our adjusted analyses of length of stayrelated outcomes indicated an association with age. Total length of stay and time from restraint application until discharge were significantly reduced for those subjects younger than 80 years of age in the safe enclosure group. The basis for this finding is not entirely clear. It may be a chance finding, or there may have been a complex combination of factors at work.
There was a reduction in overall length of stay by 1.5 days among those in the safe enclosure group when compared with the standard restraint group. Similarly, total duration of restraint use of the safe enclosure group was 551 minutes (9 hours) shorter. Although these findings were not significant, they warrant further investigation in a larger trial. If safe enclosure use truly reduces length of stay and duration of restraint use, it is an important finding, for it could translate into meaningful cost savings for acute care hospitals. It is possible, however, that any potential cost savings could be tempered by the additional time required to set up the enclosure. Ethically, if restraints are to be used, their use should be minimized, and in that sense, safe enclosures may help acute care hospitals achieve this goal more effectively.
Limitations of this trial include its small sample size and inadequate power to determine certain outcomes. Although we saw encouraging trends in several outcomes, they failed to reach statistical significance because of the limited power. For instance, the observed power for total length of stay difference was only 17%. It is conceivable that a larger trial powered specifically for length of stayrelated outcomes may show significant results. Because subjects in this study were patients in a single midsize community teaching hospital, the results may not be generalizable to patients in, for example, tertiary‐care centers or nursing homes. However, these results may apply to a large proportion of patients in the United States, as most are treated in community hospitals. We found that many patients required 2 wrist restraints in order to protect IV lines, and this resulted in exclusion of a large proportion of potential subjects. Therefore, safe enclosures may not be appropriate for all agitated patients. They may be an ideal method of restraining patients who are not at risk of pulling out their IV line or catheters but require restraints for other reasons. This could include patients in nursing homes or rehabilitation centers.
It is also important to discuss the issue of practitioner acceptability of a newer method of restraint in acute care hospitals. As expected, we found the nursing staff was originally reluctant to use the safe enclosure, even as part of a trial. This may have been because of fear of change and having a high level of comfort with the restraint systems already in use. The setup of safe enclosures can take 10‐15 minutes, whereas the use of 2‐point soft restraints or Posey vests can be accomplished in as little as a minute. However, we found that after initial use of the safe enclosure, resistance among nurses declined. In fact, in our hospital, nurses began using safe enclosures for confused and agitated patients not enrolled in the study in order to prevent wandering and falls at night. Another difficulty reported by the nursing staff was feeling somewhat limited in their access to patients by a safe enclosure. Nurses had to open a zipped flap to access the patient to administer medication or provide food. Health care providers must remember to close the flap to avoid potential falls.
In summary, safe enclosures seem to be a safe and more acceptable alternative to the restraints currently in use in acute care hospitals. These findings should be replicated in a larger trial.
Physical restraints, such as bed rails, Posey vests, and 2‐point and 4‐point soft or hard restraints, are commonly used in acute care hospitals to protect agitated patients from harming themselves or others.1 Yet restraints are viewed by patient advocates and health care practitioners as inhumane and overly restrictive. Furthermore, currently used physical restraints have been linked to minor injuries such as sores and abrasions, intensification of agitation, and even death.2, 3 Hospitals and nursing homes are therefore required to try alternative and less severe means of alleviating agitation and delirium among patients before resorting to physical restraints. However, despite a general dislike of restraints and stricter federal guidelines governing their use, the application of restraints is often unavoidable for some patients. It is estimated that between 4% and 25% of in‐patients will have physical restraints applied at some point during their hospital stay.4
Given these numbers, it is surprising that newer and potentially safer restraint systems have not been explored. Safe enclosures may provide health care facilities with an alternative option. This type of restraint consists of a nylon net canopy that safely surrounds both the patient and the mattress. The potential for safe enclosures to provide a safe, humane, and acceptable method of restraint for both hospital staff and patients warranted investigation. In addition, because this system does not restrict a person's ability to move within the enclosure, the many potential hazards of immobility associated with standard restraints may be reduced or eliminated. However, to our knowledge, there have been no reports published of randomized trials comparing standard restraints to newer and possibly safer restraint systems.
We report a randomized controlled trial that compared the use of safe enclosures with standard restraints among agitated, hospitalized patients. Compared with patients in standard restraints, we hypothesized that safe enclosures would: (1) be perceived as more acceptable and humane by family members, physicians, and nurses; (2) lead to improved health outcomes such as decreased duration of restraint use, decreased agitation, shorter length of stay, decreased need to administer medication to treat agitation, and fewer injuries to the patient.
METHODS
Design and Setting
This was a prospective, single‐center, randomized, controlled trial conducted at a community hospital in Connecticut.
Subjects
Male and female hospitalized patients at least 18 years old in the general medicine in‐patient services at a community hospital in Connecticut were assessed for eligibility to participate in this study if they had been put in restraints by the health care team independent of the study for one of these acute conditions: (1) delirium from any cause, including drug or alcohol withdrawal, or other medical conditions resulting in acute delirium; (2) confusional state from any cause; (3) agitation and disruptive behavior requiring restraints; (4) psychosis, hallucinations, or delusions requiring acute intervention (such as medication, restraints, or sitter); or (5) suicidality. Once in restraints, patients were screened for eligibility to participate in this study.
Exclusion criteria included: (1) need for acute respiratory or hemodynamic support or cardiac or septic shock; (2) terminal illness; (3) documented history of claustrophobia; (4) refusal by the family to give consent; (5) hospital stay < 24 hours; and (6) need for intravenous vasopressors, intubation, or ventilatory support. We also excluded patients who had been in restraints for more than 48 hours prior to potential study enrollment. Because safe enclosure would be a redundant system of restraint for patients requiring more than 1 limb in restraints, those patients were also excluded from the study. Figure 1 shows participation flow.
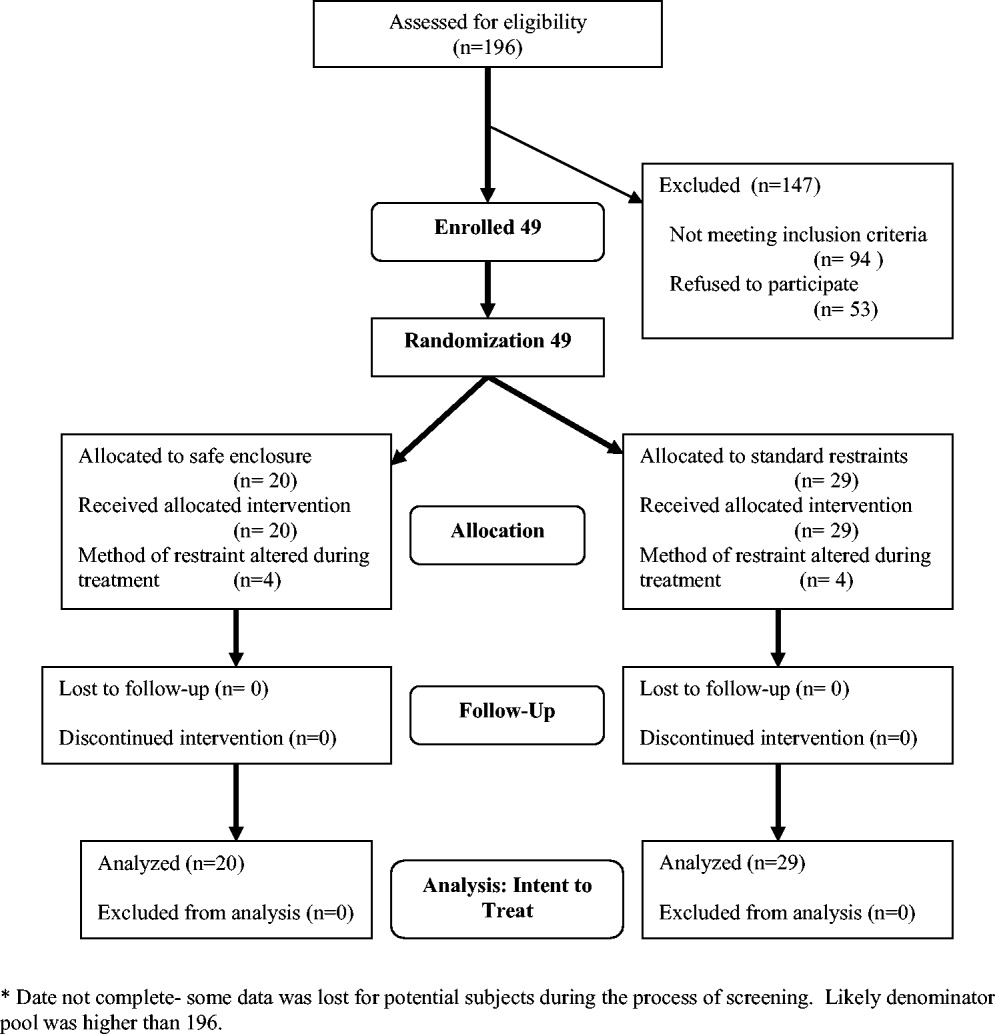
A number of screened patients were excluded for not being appropriate candidates for the safe enclosure. Of these, 20% required more than 1 limb in restraints, 13% required restraint not for agitation but for IV or catheter protection only, 10% were in critical care or on ventilators, and 13% were not appropriate for various other reasons including claustrophobia. The remaining excluded patients may have been eligible but either were preparing for discharge on screening (26%), were in restraints for more than 48 hours on screening (11%), stayed in the hospital less than 24 hours (4%), or had previously been a study participant (3%).
A stratified permuted block randomization was used to control for age (65 vs. >65 years) and sex (male vs. female) to ensure equal representation in both study arms. The study was approved by the institutional review board of the study site, and written informed consent was obtained by the study coordinator from patients' families. Because eligible patients suffered from acute delirium or agitation, most were not sufficiently cognizant to participate in the consent process. As a result, consent was largely obtained from patients' family members. Although the intent of this trial was to recruit 60 patients over an 18‐month period, the study was closed at 49 after 2 years because of slow recruitment and a lack of remaining funds.
Intervention
The safe enclosure, also known as a net bed or safety net, is an alternative to standard restraints. It consists of: (1) a metal frame that sits on the floor completely enclosing a standard hospital bed and (2) a nylon net canopy that encloses the patient and the mattress. We used the SOMA Safe Enclosure (Vivax Medical Corporation, Torrington, CT,
Procedures
Patients were enrolled in this study from April 2003 to February 2005. Once a patient had been placed in restraints by a physician, the nurse in charge alerted the study investigators by beeper of a potential subject, who was then screened based on the above eligibility criteria. We also actively screened restraint log sheets maintained by the nursing staff on most weekdays to monitor new patients who may have been put on restraints. Subjects were randomized to remain in standard restraints or be transferred to the safe enclosure. The randomization scheme was generated using software available at
Modification of the use of restraints is common in hospital settings, as patient needs fluctuate. In the 2 study groups, restraint crossover did occur at the discretion of the attending physician or nurse. Four patients in the safe enclosure group required either additional restraints or had the safe enclosure removed and alternate restraints applied. Similarly, 4 patients in the standard restraint group were either given the safe enclosure or had additional standard restraints applied. Under the principle of intent to treat, patients remained in their original randomized group for the purpose of analyses. This approach provided the most conservative analyses by keeping the sickest patients in the intervention group, thus guarding against type I error.
Measurements
Baseline data obtained at enrollment included: (1) demographic information, (2) clinical information, and (3) restraint information (ie, time of restraint application, clinical indication for use, type of restraint used, ordering physician, and alternative treatment tried before decision to start restraints).
Primary outcomes included: (1) perception survey scores of family members, physicians, and nurses regarding patient comfort, acceptability, and safety of the restraint device; and (2) patient agitation scores. A preplanned subgroup analysis separated nurses into 2 categories (primary and secondary). The admitting nurse was designated the primary nurse; all other nurses were considered secondary nurses. This analysis was performed to examine any differences in perception resulting from a nurse's level of patient involvement.
Family and provider perceptions were assessed with a self‐administered survey containing 11 items each measured on a 10‐point scale (from 1 = viewed negatively to 10 = viewed positively; maximum score 110 points). Surveyed physicians, nurses, and relatives were asked to rate: (1) patient comfort, (2) accessibility to patient, (3) ease of communication with patient, (4) how calm patient was, (5) perceived safety of patient, (6) patient's feeding convenience, (7) ease of bedpan use, (8) impact on recovery time; (9) how humane and ethical the restraint was, (10) recommendation for use on other patients, and (11) how demanding or difficult caring for the patient was.
Agitation was measured using 2 distinct methods: the Alcohol Withdrawal Assessment Form (AWAF)5 and the Agitated Behavior Scale (ABS).6, 7 Both techniques have been widely used to assess delirium of hospitalized patients. The AWAF measures agitation by analyzing key physiologic indicators such as blood pressure and heart rate on a 0‐ to 22‐point scale. The ABS is a 14‐item scale that measures specific behaviors related to agitation (eg, distractibility, uncooperativeness, and restlessness). Each behavior is rated on a 4‐point Likert scale (0‐3); total score ranges from 0 to 42. Each scale was completed once per 8‐hour shift by the nurse on duty.
Secondary outcomes consisted of total length of stay, duration of restraint use, time from application of restraints until time of discharge, and time from admission until time of application of restraints. Length of stay was calculated as the number of days from the time the patient was admitted to the time the patient was discharged. Time from admission until time of restraint application, duration of restraint use, and time from restraint application until discharge were assessed in minutes. These measurements were based on written restraint order forms and nursing progress reports. Hospital protocol regarding restraint requires hospital staff members to document the application, removal, and adjustment of restraints.
Additional outcomes measured included total amount of medications used to treat agitation and number of injuries incurred. Total amount of medication administered was determined with an equivalence system for different drugs used to treat agitation or delirium.811 Medications were separated into 4 groups: antianxiety medications, antidepressants, antipsychotics, and opioid analgesics. Total amount included both regularly administered and as‐needed dosages of medication. We identified injuries through reports of a subject's primary nurse and by review of medical records.
Data Analyses
Sample size was calculated using a 2‐sample t test formula based on the primary outcome. The study was designed to detect an absolute difference in points of 10% (total absolute score difference of 11 per survey or a total difference of 33). The 2‐sided alpha was initially set at 0.05 and the power at 80%, with an estimated standard deviation of 20. The alpha level was Bonferroni‐adjusted for up to 6 additional comparisons, with each significance level of 0.0071 (z = 2.70).
To assess differences in patient characteristics between the standard restraints and safe enclosure groups, we used the Student t test for continuous variables and Fisher's 2‐sided exact test for categorical variables. Differences in family and staff perceptions of the restraint mechanisms were measured using the Student t test with Satterthwaite's method for calculating variance. However, to account for questions marked not applicable by the responder, weighted scores, defined as the total score divided by the percentage of questions answered, were calculated.
Differences in agitation scores (ABS and AWAF) were analyzed using 2 strategies. First, the ABS and AWAF scores 24 hours after study enrollment were compared across groups using the Student t test with Satterthwaite's method for calculating variance. Then, separate comparisons of the ABS and AWAF scores 48 and 72 hours after enrollment were conducted using the Student t test with a pooled variance. Next, 2 longitudinal analyses were performed using a mixed‐effects (fixed and random) model. These analyses modeled change in the ABS or AWAF scores over (1) the first 3 days and (2) the first 6 days of hospitalization as a function of being restrained with the safe enclosure or being restrained with the hospital's standard restraint systems. For these comparisons, the model included not only the main effects of type of restraint and time, but also the interaction between type of restraint and time and the covariates sex, age, and initial ABS or AWAF score. For these models, a backward elimination procedure was undertaken using a significance level of = 0.05 in order to determine the most parsimonious model.
To determine if the total length of subject stay in the hospital was different between groups, the Student t test was used with Satterthwaite's method for calculating variance. Differences in time from admission until time of restraint application, duration of restraint use, and time from application of restraints until time of discharge were analyzed with the Student t test with pooled variances.
To compare the amount of medication used, equivalent dosage conversions were used for each of the 4 medication categories (antianxiety medications, antidepressants, antipsychotics, and opioid analgesics). To determine if the amounts of these 4 categories of medications differed between groups, the Student t test was used. Last, to determine if there was a difference in the number of patient injuries between groups, Fisher's 2‐sided exact test was used.
RESULTS
Study Population
Of the 49 subjects enrolled in the study, 20 were randomized to the safe enclosure and 29 to standard restraints. This imbalance was likely a result of the premature termination of the study, which in turn was a result of slow recruitment. Table 1 shows selected baseline characteristics of the enrolled subjects. There were no significant differences between the 2 groups in sex, age, patient diagnoses, reason for restraint, or type of medication. However, the subjects randomized to the safe enclosure were less likely to have hypertension than those randomized to standard restraints (36.8% vs. 72.4%, P = .019).
| Variable | All (n = 49) | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) |
|---|---|---|---|
| |||
| Sex (male) | 26 (53.1%) | 11 (55.0%) | 15 (51.7%) |
| Age (years) | 81.3 (13.1%) | 77.2 (15.6%) | 84.2 (10.3%) |
| Alzheimer's disease | 23 (47.9%) | 11 (57.9%) | 12 (41.4%) |
| Dementia | 3 (6.3%) | 2 (10.5%) | 1 (3.5%) |
| Coronary artery disease | 19 (39.6%) | 10 (52.6%) | 9 (31.0%) |
| Hypertension* | 28 (58.3%) | 7 (36.8%) | 21 (72.4%) |
| Congestive heart failure | 6 (12.5%) | 3 (15.8%) | 3 (10.3%) |
| Atrial fibrillation | 7 (14.6%) | 1 (5.3%) | 6 (20.7%) |
| Transient ischemic attacks/cerebral vascular accidents | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Chronic obstructive pulmonary disease | 3 (6.3%) | 1 (5.3%) | 2 (6.9%) |
| Diabetes mellitus | 11 (22.9%) | 5 (26.3%) | 6 (20.7%) |
| Alcohol abuse | 7 (14.6%) | 2 (10.5%) | 5 (17.2%) |
| Drug abuse | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Where admitted | |||
| General medicine floor | 41 (83.7%) | 17 (85.0%) | 24 (82.8%) |
| Telemetry | 7 (14.3%) | 2 (10.0%) | 5 (17.2%) |
| ICU | 1 (2.0%) | 1 (5.0%) | 0 (0.0%) |
Primary Outcomes
The rates of response to the perception survey were: relatives/next of kin, 90%; physicians, 90%; primary nurses, 100%; and secondary nurses, 78%. Family members and physicians viewed the safe enclosure significantly more positively than they viewed standard restraints (P < .0001 and P < .0001, respectively; Table 2). There was a trend toward more positive perceptions of the safe enclosure among nurses; however, this trend did not achieve statistical significance (P = .0836). The subgroup analysis of nurses (primary vs. secondary) revealed that secondary nurses viewed the safe enclosure more positively (P = .023). Primary nurses tended to view the safe enclosure more positively than the standard restraints, but the association was not significant (P = .1313).
| Variable | SOMA Safe Enclosure (n = 20) | Standard restraint system (n = 29) | P value (observed power)* |
|---|---|---|---|
| |||
| 1. Perception Survey | |||
| Relative or next of kin | 86.84 | 68.47 | < .0001 (96%) |
| Physician | 83.38 | 65.76 | < .0001 (96%) |
| All nurses | 75.20 | 69.45 | .086 (40%) |
| Primary nurse | 75.45 | 69.72 | .1313 (31%) |
| Secondary nurse | 80.35 | 69.82 | .0230 (58%) |
| 2. Alcohol Withdrawal Assessment Form | |||
| 24 hours | 3.06 | 3.25 | .7972 (6%) |
| 48 hours | 3.23 | 3.40 | .8516 (5%) |
| 72 hours | 3.44 | 2.67 | .6163 (7%) |
| 3. Agitated Behavior Scale score | |||
| 24 hours | 11.93 | 8.33 | .2312 (27%) |
| 48 hours | 6.00 | 8.75 | .3743 (13%) |
| 72 hours | 7.83 | 7.11 | .7762 (6%) |
There were no statistically significant differences between the 2 randomized groups in ABS or AWAF scores 24, 48, or 72 hours after restraint application (Table 2). In addition, there were no statistically significant differences during the study between the groups in the rates of change in ABS or AWAF score . This was the case when looking at the first 3 days of hospitalization as well as the first 6 days (data not shown). All results were also calculated after adjusting for length of stay; this covariate did not affect any of the results.
Table 3 details the results for each perception survey question. Perceived comfort, calmness, and safety of patients were rated higher in the safe enclosure group by physicians, relatives, and all nurses. With the exception of perceived accessibility to patients, relatives rated the safe enclosure higher than standard restraints on all other perception measures. Table 4 illustrates the differences in the responses of primary and secondary nurse to each perception survey question. Primary and secondary nurses viewed the safety of the safe enclosure significantly more positively than they did the standard restraints.
| Variable | Relative/next of kin (n = 16, 28) | Primary and secondary nurses (n = 29, 29) | Physician (n = 29, 29) |
|---|---|---|---|
| |||
| Comfort | (8.78, 7.29).0033 | (7.98, 6.78).0194 | (8.40, 6.77).0003 |
| Accessibility | (8.28, 8.07).6486 | (7.68, 8.29).2236 | (8.35, 7.58).1056 |
| Communication | (9.11, 8.19).0214 | (8.29, 8.12).7333 | (8.40, 8.31).8469 |
| Calmness | (8.72, 6.29).0005 | (7.68, 6.53).0382 | (7.70, 5.92).0062 |
| Safety | (9.11, 6.74) < 0.001 | (8.53, 6.76).0024 | (8.60, 5.96).0002 |
| Feeding convenience | (8.50, 7.04).0164 | (7.11, 7.74).2327 | (8.25, 6.28).0047 |
| Ease of bedpan use | (7.91, 6.06).0224 | (7.36, 6.90).3977 | (6.82, 6.25).5376 |
| Impact on recovery time | (7.53, 6.07).0244 | (6.29, 5.66).3864 | (6.95, 6.43).4254 |
| Humane/ethical | (7.94, 5.50).0026 | (6.88, 6.31).4049 | (7.95, 5.96).0052 |
| Recommend for other patients | (8.71, 5.50).0002 | (7.15, 6.12).1395 | (8.05, 6.04).0037 |
| Ease of caring for patient | (8.44, 5.70) < .001 | (7.55, 6.38).0749 | (8.05, 6.25).0028 |
| Variable | Primary Nurse (n = 20, 29) (SOMA safe enclosure, control)* P value | Secondary Nurse (n = 12, 26) (SOMA safe enclosure, control)* P value |
|---|---|---|
| ||
| Comfort | (7.85, 6.62).0270 | (8.33, 6.81).0346 |
| Accessibility | (7.55, 8.21).2656 | (8.17, 8.16).9902 |
| Communication | (8.21, 8.34).8093 | (8.83, 7.88).0705 |
| Calmness | (7.70, 6.28).0153 | (7.83, 6.85).2001 |
| Safety | (8.55, 6.34).0012 | (8.67, 6.76).0435 |
| Feeding convenience | (7.37, 7.93).3861 | (7.60, 7.42).8282 |
| Ease of bedpan use | (7.53, 6.95).3945 | (7.00, 6.84).8602 |
| Impact on recovery time | (6.16, 5.39).3251 | (7.50, 6.50).2340 |
| Humane/ethical | (6.45, 6.66).7871 | (7.73, 5.96).0571 |
| Recommend for other patients | (6.70, 6.11).4553 | (8.42, 5.92).0075 |
| Ease of caring for patient | (7.65, 6.41).0860 | (7.83, 6.38).0565 |
Secondary Outcomes
There was a trend toward shorter total length of stay, time from admission until restraint application, duration of restraint use, and time from restraint application until discharge among subjects restrained by the safe enclosure compared with those restrained with standard restraints. However, these unadjusted differences were not statistically significant. We examined secondary outcomes after adjusting for 2 covariates, age and sex. Age but not sex affected the results. We found that subjects in the intervention group younger than 80 years of age had a shorter length of stay for 2 of the 4 related outcomes: time of admittance to time of discharge (P = .0199) and time of restraint to time of discharge (P = .0274). Time of admission to time of restraint application and duration of restraint did not differ between groups. The former outcome was not expected to differ between groups.
Additional Outcomes
There were no differences between groups in the amounts of 3 of the 4 types of medications used to treat agitation or delirium (ie, antianxiety medications, antipsychotic medications, opioid analgesic medications). The proportion of patients on these medications did not differ by group (P = .59). Only 5% of patients in standard restraints were on antidepressants, and about 5% were on opioids in each group. There was only 1 minor patient injury recorded during the study. This minor abrasion was to a patient assigned to the standard restraint group. No injuries were reported in the safe enclosure group.
DISCUSSION
We have demonstrated that the SOMA Safe Enclosure may be a more acceptable alternative to the restraints currently in use. Our results show that the safe enclosure was rated as more acceptable by family members, physicians, and secondary nurses in our composite perception scores. The results from the primary nurses did not show a significant difference between the 2 groups. An analysis of the individual perception variables found that family members viewed the safe enclosure as more acceptable for 10 of the 11 variables examined. Furthermore, in this small‐scale study, safe enclosures appeared to be safe, as there were no injuries reported in the intervention group. As stated above, there was 1 minor injury reported in the standard restraint groups.
Restraints are commonly used to protect agitated hospitalized patients from harming themselves or others. Despite the significant reluctance of hospital staff members to use restraints, they continue to be necessary in certain situations. Factors such as a general nursing shortage and the expense required to allocate nursing or other ancillary health care workers as sitters contribute to the use of restraints. Therefore, it is reasonable to conclude that restraint use in some form or fashion will continue into the foreseeable future. There are no clear estimates of the prevalence of restraint use in acute care hospitals. A chart review study from Canada reported physical restraints in about 7.7% of in‐patients.12 Other studies have reported the use of restraints on patients in the range of 4%‐25%.2 Given the prevalence of restraint use in acute care hospitals, surprisingly little innovative research has been undertaken to develop more effective and humane systems of restraint. Furthermore, no research has examined how restraint use may affect important clinical outcomes such as length of stay. To our knowledge, this is the first clinical trial to compare currently used restraints to a newer method of restraint using the SOMA Safe Enclosure.
The idea that restraint use can lead to further agitation is not supported by our data. We observed a decrease in agitated behavior scale scores from 9.6 to 7.4 from the 24‐ and to the 72‐hour assessments; however, these results were not significant and appeared to be more dramatic for the safe enclosure group because of higher baseline levels. Our adjusted analyses of length of stayrelated outcomes indicated an association with age. Total length of stay and time from restraint application until discharge were significantly reduced for those subjects younger than 80 years of age in the safe enclosure group. The basis for this finding is not entirely clear. It may be a chance finding, or there may have been a complex combination of factors at work.
There was a reduction in overall length of stay by 1.5 days among those in the safe enclosure group when compared with the standard restraint group. Similarly, total duration of restraint use of the safe enclosure group was 551 minutes (9 hours) shorter. Although these findings were not significant, they warrant further investigation in a larger trial. If safe enclosure use truly reduces length of stay and duration of restraint use, it is an important finding, for it could translate into meaningful cost savings for acute care hospitals. It is possible, however, that any potential cost savings could be tempered by the additional time required to set up the enclosure. Ethically, if restraints are to be used, their use should be minimized, and in that sense, safe enclosures may help acute care hospitals achieve this goal more effectively.
Limitations of this trial include its small sample size and inadequate power to determine certain outcomes. Although we saw encouraging trends in several outcomes, they failed to reach statistical significance because of the limited power. For instance, the observed power for total length of stay difference was only 17%. It is conceivable that a larger trial powered specifically for length of stayrelated outcomes may show significant results. Because subjects in this study were patients in a single midsize community teaching hospital, the results may not be generalizable to patients in, for example, tertiary‐care centers or nursing homes. However, these results may apply to a large proportion of patients in the United States, as most are treated in community hospitals. We found that many patients required 2 wrist restraints in order to protect IV lines, and this resulted in exclusion of a large proportion of potential subjects. Therefore, safe enclosures may not be appropriate for all agitated patients. They may be an ideal method of restraining patients who are not at risk of pulling out their IV line or catheters but require restraints for other reasons. This could include patients in nursing homes or rehabilitation centers.
It is also important to discuss the issue of practitioner acceptability of a newer method of restraint in acute care hospitals. As expected, we found the nursing staff was originally reluctant to use the safe enclosure, even as part of a trial. This may have been because of fear of change and having a high level of comfort with the restraint systems already in use. The setup of safe enclosures can take 10‐15 minutes, whereas the use of 2‐point soft restraints or Posey vests can be accomplished in as little as a minute. However, we found that after initial use of the safe enclosure, resistance among nurses declined. In fact, in our hospital, nurses began using safe enclosures for confused and agitated patients not enrolled in the study in order to prevent wandering and falls at night. Another difficulty reported by the nursing staff was feeling somewhat limited in their access to patients by a safe enclosure. Nurses had to open a zipped flap to access the patient to administer medication or provide food. Health care providers must remember to close the flap to avoid potential falls.
In summary, safe enclosures seem to be a safe and more acceptable alternative to the restraints currently in use in acute care hospitals. These findings should be replicated in a larger trial.
- ,,,,.Prevalence and patterns of physical restraint use in the acute care setting.J Nurs Adm.1998;28(11):19–24.
- ,Strumpf. Myths about Elder Restraint.J Nurs Scholarsh.1990;22(2):124–128.
- , et al.Deadly restraint: a Hartford Courant investigative report.Hartford Courant1998; October 11‐15.
- ,,,,,, et al.Jt Comm J Qual Improv2001;27:605–618.
- ,,,,.Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale.Br J Addict.1989;84:1353–1357.
- ,.Development of an agitated behavior rating scale for discrete temporal observations.Nursing Meas1993;1:115–124.
- ,,,.Reliability of the Agitated Behavior Scale.J Head Trauma Rehabil.1999;14:91–96.
- University of Newcastle. The Ashton Manual. Available at: http://www.benzo.org.uk/manual/bzcha01.htm. Accessed November 15,2006.
- Postgraduate Medicine Online. Sedation and analgesia in intensive care. Available at: http://www.postgradmed.com/issues/2002/02_02/blanchard.htm. Accessed November 15,2006.
- Anti‐psychotic Comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antipsychotics%20Comparison%20Chart.pdf. Accessed November 15,2006.
- Anti‐depressant comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antidepressant%20comparison%20Chart.pdf. Accessed November 15,2006.
- ,.Use of physical and chemical restraints in medical teaching units.Can Med Assoc J.2000;162:339–340.
- ,,,,.Prevalence and patterns of physical restraint use in the acute care setting.J Nurs Adm.1998;28(11):19–24.
- ,Strumpf. Myths about Elder Restraint.J Nurs Scholarsh.1990;22(2):124–128.
- , et al.Deadly restraint: a Hartford Courant investigative report.Hartford Courant1998; October 11‐15.
- ,,,,,, et al.Jt Comm J Qual Improv2001;27:605–618.
- ,,,,.Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale.Br J Addict.1989;84:1353–1357.
- ,.Development of an agitated behavior rating scale for discrete temporal observations.Nursing Meas1993;1:115–124.
- ,,,.Reliability of the Agitated Behavior Scale.J Head Trauma Rehabil.1999;14:91–96.
- University of Newcastle. The Ashton Manual. Available at: http://www.benzo.org.uk/manual/bzcha01.htm. Accessed November 15,2006.
- Postgraduate Medicine Online. Sedation and analgesia in intensive care. Available at: http://www.postgradmed.com/issues/2002/02_02/blanchard.htm. Accessed November 15,2006.
- Anti‐psychotic Comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antipsychotics%20Comparison%20Chart.pdf. Accessed November 15,2006.
- Anti‐depressant comparison chart. Available at: http://meds.queensu.ca/∼clpsych/orientation/Antidepressant%20comparison%20Chart.pdf. Accessed November 15,2006.
- ,.Use of physical and chemical restraints in medical teaching units.Can Med Assoc J.2000;162:339–340.
Copyright © 2007 Society of Hospital Medicine
Color‐coded wristbands: Promoting safety or confusion?
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
Breaking Bad News
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
Evaluation of Clerkship Structure
The third‐year pediatric clerkship at the University of Utah School of Medicine has a relatively unique inpatient service, the Glasgow Service, which consists of an academic attending, a third‐year pediatric resident, and 4 third‐year medical students, but no interns. (This service was named in honor of Lowell Glasgow, chair of pediatrics, 1972‐82.) This structure was introduced in 1992 by the chair of pediatrics, Michael Simmons, the residency program director, Richard Molteni, and the clerkship director, Karen Hansen. These individuals desired to improve students' inpatient experience by providing greater responsibility for patient care. An additional motive was to increase the total number of patients followed by house staff without increasing the size of the residency program.
This inpatient service is a part of a 6‐week pediatric clerkship. All students perform the 3‐week inpatient portion of their clerkship at Primary Children's Medical Center, a tertiary‐care, freestanding children's hospital. (The students also spend 1 week each in a newborn nursery, an outpatient clinic, and a subspecialty setting). The academic attendings include generalists, hospitalists, and specialists who concurrently have other clinical responsibilities. The students take in‐house call every fourth night, supervised by senior residents who are not necessarily members of their service. All students share the same formal teaching activities, including morning report, a noon conference, and a student conference.
Patients are assigned to the ward services by a senior admitting resident. The admitting resident distributes patients among the services based on the complexity and acuity of the patients' conditions as well as the census on the various services. The senior resident supervising a particular service then assigns patients among the members of that service. Each third‐year medical student is expected to care for 2 or 3 patients at a time.
In addition to the intervention service, students also rotate on 2 similar traditional services. These services are traditional in the sense that they are composed of an academic attending, a community attending, a third‐year pediatric resident, 4 interns, and up to 2 fourth‐year and 2 third‐year medical students. Faculty preferences regarding service assignments were accommodated when possible. Therefore, some faculty attended only on one type of service, intervention or traditional, and others attended on both types. Because they have more members and because interns are capable of caring for more patients than are medical students, the traditional services cared for more patients than the intervention service. Although identical in composition, the 2 traditional services differ with each other in several ways. One service typically admits children 3 years old and younger, whereas the other admits children who are between 3 and 12 years old. The service that admits older children also admits most of the hematology‐oncology patients.
Although other authors have described similar inpatient clerkship structures, to our knowledge, none have evaluated them through a prospective randomized controlled trial.1, 2 The recent literature on ambulatory experiences during third‐year clerkships provided a methodological framework for this study. Collectively, such studies have evaluated outcomes with a variety of measures, including patient logs,35 evaluations,3, 4, 6, 7 examinations,37 surveys,3, 5, 7, 8 and career choices.4, 68 Additional outcomes, such as the effect of educational interventions on patient care, have been emphasized.9
In the light of this research, we conducted a prospective, randomized controlled trial to compare outcomes on the intervention service with those on the traditional services. We hypothesized that, compared with the traditional services, the intervention service would show:
improved process measures in terms of increased number of patients admitted, number of key diagnoses encountered in the patients cared for, and range of ages of the patients admitted;
similar or improved student performance, as measured by faculty and resident evaluations and a National Board of Medical Examiners (NBME) subject examination;
increased student satisfaction, as assessed by an end‐of‐rotation questionnaire;
increased interest in pediatric and, more broadly, primary care careers, as measured by subinternship and internship selections; and
comparable or improved resource utilization in terms of length of stay and total charges.
METHODS
All students enrolled in the third‐year pediatric rotation during the 2001‐2003 academic years were individually randomized by the clerkship assistant to the intervention service or 1 of the 2 traditional services without respect to career preference. A 5:3 student randomization ratio was used to fulfill the requirement that 4 students be assigned to the intervention service during every 3‐week block. This permitted the service to have call every fourth night.
To evaluate the adequacy of the randomization process, we obtained baseline student characteristics on age, sex, and United States Medical Licensing Examination (USMLE) Step 1 score from the Dean of Student Affairs. The dean also reported the discipline each student enrolled in for the required fourth‐year subinternship(s) and matched in for internship. These data were reported anonymously and linked to the service to which the student was assigned. In this study, pediatrics, internal medicine, and family practice were all considered primary care, but preliminary or transitional internships were not.
Process Measures
Students were required to submit logs at the end of their rotations, recording patients' names, ages, diagnoses, and admission dates. The accuracy and completeness of these logs were not independently verified.
As there was no authoritative list of key diagnoses third‐year medical students should encounter in the patients they care for during their inpatient rotations, we relied on expert opinion at our institution. The Council on Medical Student Education in Pediatrics' curriculum was not used because it did not differentiate between inpatient and ambulatory contexts. A preliminary list of 93 diagnoses was developed from the table of contents of Pediatric Hospital Medicine.10 This list was distributed to the 26 clinical faculty members in the Divisions of Pediatric Inpatient Medicine and General Pediatrics who were asked to select the 10 most important diagnoses. Surveys were numerically coded to permit 1 reminder.
The survey had a response rate of 92.3% (24 of 26 surveys). One survey was excluded because the respondent significantly deviated from the instructions. The 10 key diagnoses and the percentages of respondents who selected each individual diagnosis are: asthma (100%), febrile infant (95.6%), diarrhea and dehydration (91.3%), bronchiolitis (78.2%), diabetes mellitus and diabetic ketoacidemia (60.9%), failure to thrive (56.5%), urinary tract infections (52.1%), pneumonia (47.8%), upper airway infections such as croup (43.5%), and seizures and status epilepticus (43.5%).
Two of the authors independently coded the diagnoses on the students' patient logs in terms of these 93 diagnoses. The authors were blinded to the students' service assignment. As many students reported more than 1 diagnosis, the authors prioritized primary, secondary, and tertiary diagnoses to simplify the evaluation. The most likely cause of admission was listed as the primary diagnosis. If the authors could not reconcile divergent views, a third party was consulted.
Student Performance
Students were evaluated by both the attending physician(s) and senior resident(s) using a standardized evaluation form available from the corresponding author. The evaluation contained 18 items in 7 categories: data gathering, data recording/reporting, knowledge, data interpretation, clinical performance, professional attitudes, and professional demeanor. The student was rated exceptional, above expectations, meets expectations, below expectations, unacceptable, or not observed on each item. A short narrative description illustrated each rating. The ratings were converted to a 5‐point scale, with exceptional being 5. If the evaluator marked the line between 2 ratings, it was recorded as half. When multiple attendings or residents evaluated a student, the scores for a given item were collapsed into an average score.
Students also completed a NBME pediatric subject examination on the last day of their rotation.
Additionally, students were requested to complete a questionnaire during the final week of the clerkship. The items on the questionnaire were meant to access students' perceptions of the quality of their attendings' and residents' teaching, a potentially confounding variable. The survey was piloted on a group of similar subjects. Informed consent was obtained for survey completion. The survey was anonymous and required approximately 7 minutes to complete.
Resource Utilization
Last, resource utilization data, length of stay and total charges, for the 4 most common primary diagnoses were compared between the intervention and the traditional services. The 4 most common primary diagnoses and the percentage of total diagnoses (n = 2047) that each represents were bronchiolitis, 13%; febrile infant, 8.6%; pneumonia, 7.1%; and asthma, 6.5% (the diagnosis other accounted for 12% of the total diagnoses). Unique patient identifiers were used to obtain length of stay and total charges from the hospital's database. All‐Patient‐Refined Diagnosis‐Related Groups Severity of Illness (APR‐DRG‐SOI) were also obtained and used to construct multivariate models. Patients who were admitted to the pediatric intensive care unit (PICU) were excluded from the analysis.
Statistical Analysis
Statistical analyses were conducted and frequencies and percentages were calculated using Stata SE version 8.0 (College Station, TX). For all interval and ratio‐scaled variables, distributions were tested for normality using the Shapiro‐Wilks test to determine whether to use parametric or nonparametric statistical tests. For distributions meeting the normality assumption, the unpaired t test was used to compare the intervention service with traditional services. Where the normality assumption was not met, the Mann‐Whitney test was used. Categorically scaled data were compared using Pearson's chi‐square test. The standardized mean differences, reported as d values, were calculated to determine the effect size. Small, medium, and large effect sizes were defined as d values of 0.20, 0.50, and 0.80, respectively.11 Teaching quality, an effect modifier, was entered as a covariate into a linear regression model. Analyses of length of stay and total charges were conducted using multivariate linear regression controlling for patient age and severity of illness.
This study was approved by the University of Utah and Primary Children's Medical Center's Institutional Review Board.
RESULTS
Two hundred and three students enrolled in the third‐year pediatric clerkship during the study period, and all students completed the clerkship on their assigned services. One hundred and twenty‐eight were randomized to the intervention service and 75 to the traditional services. There were no statistically significant differences in median age, percentage of male students, or mean USMLE Step 1 score between the students randomized to the intervention service and those randomized to the traditional services (Table 1).
| Intervention service | Traditional services | P value | |
|---|---|---|---|
| |||
| Age (median) | 28 | 28 | .76* |
| Sex (% male) | 58.6 | 62.7 | .57 |
| USMLE Step 1 score | 217 | 217 | .94 |
Process Measures
Overall, 96.6% of students (196 of 203) submitted patient logs; 97.7% of students (125 of 128) on the intervention service and 94.7% of students (71 of 75) on the traditional services. The students on the intervention service admitted a median of 10 patients, whereas the students on the traditional services admitted a median of 11 patients (d = 0.45, P < .01). Age data were recorded on 137 patient logs (69.9% of submitted logs, 72.0% of students on the intervention service vs. 66.2% of students on the traditional services). The percentage of students who saw at least 1 newborn (birth‐23 months), child (2‐12 years), and adolescent (12‐18 years) was 34.8% on the intervention service and 33.3% on the traditional services (P = .87) (Table 2).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| Median number of patients | 10 | 11 | 0.45 | < .01* |
| Percent of students who saw 1 newborn, child, and adolescent | 34.8% | 33.3% | 0.03 | .87 |
| Top 10 diagnoses cared for (n) | 4.4 | 3.6 | 0.48 | < .01 |
| Percent of patients cared for whose diagnoses were in top 10 | 59.3% | 46.8% | 0.62# | < .01 |
| Percent of unique diagnoses (median) | 80.0% | 80.0% | 0.02 | .62 |
Students on the intervention service encountered, on average, a larger number of the 10 key diagnoses (4.4 vs. 3.6, d = 0.48, P < .01) and a higher percentage of their patients had clinical conditions among the key diagnoses (59.3 vs. 46.8, d = 0.62, P < .01). To determine if this higher percentage was the result of admitting multiple patients with the same diagnosis, we examined the percentage of unique primary diagnosesthe number of different primary diagnoses divided by the total number of patientsand found no differences (Table 2).
Student Performance
The faculty and resident evaluations of the students showed statistically significant differences between those in the intervention service and those in the traditional services in only 2 of the 18 items. These items were analysis in the data interpretation category (3.81 vs. 3.64, d = 0.35, P = .02) and patient interaction in the professional demeanor category (3.89 vs. 3.76, d = 0.31, P < .05). Both differences favored the intervention service. There were no statistical differences by service in student performance on the NBME subject examination (73.2 vs. 72.3, P = .39).
Student Satisfaction
Overall, 87.2% of students (177 of 203) completed the survey; 87.5% of students (112 of 124) on the intervention service and 86.7% of students (65 of 75) on the traditional services. The students on the intervention service both had a more positive overall attitude about their rotation and were more likely to find it a satisfying educational experience. Students on the intervention service also reported greater participation in patient care. Effect sizes ranged from small to medium (Table 3). The internal consistency of answers about participation in patient care was high (Pearson correlation coefficient r = 0.80).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| My overall attitude toward this rotation is: 1. highly negative to 5. highly positive | 4.48 | 4.26 | 0.26 | .02* |
| I found this rotation a satisfying educational experience: 1. strongly disagree to 5. strongly agree | 4.49 | 4.22 | 0.35 | < .01* |
| My role on this rotation was that of an: 1. observer, 3. participant, 5. director | 3.77 | 3.33 | 0.60# | < .01 |
| My supervising interns/residents were _____ teachers: 1. poor, 3. good, 5. exemplary | 3.91 | 3.75 | 0.17 | .26* |
| My input into patient care decisions was: 1. strongly discouraged to 5. strongly encouraged | 4.45 | 3.98 | 0.66# | < .01* |
| I was able to make a significant contribution to patient care: 1. strongly disagree to 5. strongly agree | 4.19 | 3.92 | 0.34 | .02* |
| I had direct responsibility for patient care: 1. strongly disagree to 5. strongly agree | 4.33 | 3.95 | 0.46 | .01* |
| My attendings were _____ teachers: 1. poor, 3. good, 5. exemplary | 4.09 | 3.75 | 0.40 | < .01* |
| I found the feedback I received during this rotation to be: 1. insufficient, 3. appropriate, 5. excessive | 2.84 | 2.65 | 0.22 | .17* |
| The following best describes the quality of my supervision during this rotation: 1. I was expected to do things beyond my competence unsupervised 3. The degree of supervision was appropriate for my level of training 5. I was excessively supervised on skills I had already demonstrated | 2.95 | 3.06 | 0.18 | .19 |
| During this rotation: 1. I was expected to see too many patients 3. I was expected to see an appropriate number of patients 5. I expected to see more patients | 3.46 | 3.31 | 0.18 | .33* |
| Before this rotation I _____ pediatrics as a career choice: 1. had rejected, 3. was considering, 5. had decided on | 2.37 | 2.14 | 0.22 | .11* |
| This rotation increased my interest in pursuing pediatrics as a career: 1. strongly disagree to 5. strongly agree | 3.74 | 3.60 | 0.14 | .32* |
Students on the intervention service rated the teaching of their attendings, but not of their residents, higher than did students on the traditional services. Controlling for the perceived quality of the attending, 3 of 6 satisfaction outcomes remained statistically significant: role on rotation (P < .01), input into patient care decisions (P < .01), and direct responsibility for patient care (P = .04). Students on both services believed they were appropriately supervised (P = .19). Despite the students on the traditional services on average admitting more patients, there was no significant difference by service in the students' rating of patient load (P = .33).
Career Choice
The odds ratio and 95% confidence interval for students enrolling in a pediatric subinternship was 1.94 (0.83‐4.49) and matching in a pediatric residency was 2.52 (0.99‐6.37). There were no statistically significant differences by service in the percentage of students enrolling in primary care (pediatric, internal medicine, and family practice) subinternships or residencies (Table 4).
| Intervention service | Traditional services | Odds ratio (95% CI) | |
|---|---|---|---|
| Pediatric subinternship | 19.5% | 11.1% | 1.94 (0.83‐4.49) |
| Primary care subinternship | 68.3% | 70.8% | 0.89 (0.47‐1.67) |
| Pediatric residency | 18.6% | 8.3% | 2.52 (0.99‐6.37) |
| Primary care residency | 40.7% | 31.9% | 1.46 (0.79‐2.70) |
Resource Utilization
One hundred and thirty‐five patients were excluded from the resource utilization analysis (n = 594) because their unique identifiers could not be found or they had been admitted to the PICU. Univariate analysis demonstrated statistically significant differences for patients with asthma, but not patients with bronchiolitis, febrile infants, or patients with pneumonia, favoring the intervention service. Patients with asthma admitted to the intervention service had a shorter length of stay (49.9 vs. 70.1 hours, P = .02) and lower total charges ($3600 vs. $4600, P = .02), as shown in Table 5. Of 4 multivariate models controlling for age and severity of illness, each with length of stay and total charges as the dependant variables, length of stay was significantly less for patients with asthma admitted to the intervention service only. Such patients were discharged an average of 23.3 hours earlier than patients with asthma admitted to the traditional services (P = .02).
| Diagnosis (n) | n | Length of stay (hours) | P value | Total charges | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention service | Traditional services | Intervention service | Traditional services | Intervention service | Traditional services | P value | ||
| ||||||||
| Bronchiolitis (210) | 159 | 51 | 63.7 | 70.5 | .20* | $4300 | $4800 | .20* |
| Febrile infant (152) | 105 | 47 | 58.8 | 58.9 | .50* | $4800 | $4900 | .28* |
| Pneumonia (123) | 82 | 41 | 84.3 | 116.8 | .71* | $6300 | $9200 | .63* |
| Asthma (109) | 80 | 29 | 49.9 | 70.1 | .02* | $3600 | $4600 | .02* |
DISCUSSION
This study's objective was to evaluate a third‐year pediatric clerkship structure that focuses on students, using multiple outcome parameters. Utilizing a robust design, the results of this study have demonstrated that the intervention service is more successful than the traditional services in several outcomes. Students assigned to the intervention service were more satisfied and more likely to select pediatrics as a career. These improvements were accomplished while maintaining similar process measures, student performance, and resource utilization compared with those of the traditional services.
Methods
The methods used in this study compare favorably with other evaluations of educational interventions. The present study incorporated a randomized controlled design.12 Although several studies of ambulatory clerkships used a randomized design, few randomized all eligible students.7, 8 The others used some form of selection prior to randomization. For example, in the Pangaro et al. study, students selected their clerkship site by lottery, with students selecting a certain site then offered the opportunity to participate in the intervention.6 The present study manifested several additional strengths. Multiple outcomes, including effects on patient care, were evaluated. Moreover, this study had a relatively large intervention group and total sample size compared with those in other medical education studies. Finally, because the intervention service had been in place for several years prior to its evaluation, the confounding influence of difficulties working out its implementation was minimized.
Results
Few studies of ambulatory experiences demonstrated statistically significant, let alone clinically significant, results. Most studies showed no statistically significant differences in student evaluations or examination scores. An exception is Grum et al., who showed improvements on 3 of 5 examinations.4 A few studies have found improved student satisfaction.3 None of the randomized controlled trials demonstrate increases in students matching in internal medicine or primary care residencies.4, 68 In contrast, this study produced statistically or programmatically significant results in process measures, evaluations, satisfaction, and career choices.
Several of our specific findings deserve additional comment. Although the admitting residents were instructed to assign patients to the intervention service based on their acuity and complexity, it is important to examine these residents' actual behavior. Several of our hypotheses were not validated. The students on the intervention service admitted fewer patients and were no more likely to see at least 1 patient in each age category. The admitting resident may have limited the number of patients admitted to the intervention service based on the workload of the supervising resident not that of the student. The supervising resident on the intervention service must round on all the patients, whereas the oversight of patients seen by students on the traditional services is shared with the interns. Having the attending on the intervention service share this supervising responsibility might improve this outcome.
Students on the intervention service had more positive attitudes toward the rotation. In addition, potentially negative attitudes were not manifest. For example, it might be argued that third‐year medical students are not prepared to bear this increased responsibility. However, there was not a significant difference in students' perception of the quality of supervision or the workload.
Although the goal of medical education is the production of competent physicians, it is important that the process not place undo burdens on patients and the health care system. Univariate analysis showed similar resource utilization. It might be contended that the admitting resident assigned the intervention service patients who were less acutely ill. Therefore, we performed multivariate analysis using APR‐DRG‐SOI to control for severity of illness. Of 8 comparisons, the only statistically significant difference, length of stay of patients with asthma, favored the intervention service.
Limitations
Although this study had numerous strengths, it also had several limitations. The primary limitations were lack of generalizability, difficulty in obtaining authentic assessments, the potential difference between statistical and educational significance, and inability to identify which components of the intervention service were responsible for the outcomes. This study's findings may not be generalizable to other institutions. For example, institutions without age or organ systembased teams may not observe increases in the number of key diagnoses encountered in the patients cared for. Regarding the assessments, there may be better measures of clinical competence, such as an objective structured clinical examination (OSCE),13 than those used in this study. However, there were not sufficient resources to implement an OSCE at the end of the rotation.
Some might question whether the statistically significant differences have educational significance. Although that is an important concern, this study should be compared with other educational interventions that found few statistically significant, let alone educationally significant, differences. To address this concern, we calculated effect sizes. The differences in student satisfaction were small to moderate. Although the lower limit of the 95% confidence interval of the odds ratio for matching in a pediatric residency was 0.99, the magnitude was programmatically important.
Finally, this study was an evaluation of an existing program. The authors were unable to control some potential confounders including patient allocation, average daily census, and quality of teaching. For example, Griffith and colleagues have shown that working with the best teachers improves student performance.14 We were not able to randomly assign the faculty among the services, and unequal distribution of better teachers could have biased this study's outcomes. The students on the intervention service rated their attendings, but not their residents, higher than did the students on the other services. However, the linear regression model showed that the perceived quality of the attending did not account for all the differences in student satisfaction. It was not possible to control for this factor in comparing student performance or subinternship or residency selection because the survey, which included the faculty evaluations, was anonymous and therefore could not be linked to the other data sets.
The perceived differences in the quality of teaching may not have been the result of differences in the attendings but instead of differences in the structure of the services. Accessibility is one of the characteristics of excellent clinical teachers.15 The intervention structure may permit faculty to spend more time with students, and this may increase the perceived quality of the teaching. However, it is not possible to resolve this issue with the available data.
CONCLUSIONS
The intervention service is a structure for the pediatric inpatient rotation of third‐year medical students that, instead of dividing the faculty and supervising resident's attention between interns and students, focuses their attention on the students. Although it has been difficult to demonstrate improvements as a result of the educational interventions, we have shown several improvements in the evaluations of the students. Moreover, the pattern of increased student satisfaction and a tendency toward more student selecting careers in pediatrics are remarkable. This was accomplished with similar resource utilization. Therefore, this program merits being continued at our institution and possibly adopted at other medical schools. Further research is needed to determine which aspects of the intervention are responsible for its effects. Some components, such as focused time with students, may be applicable to traditional services.
Acknowledgements
The authors thank Ronald Bloom for encouraging us to conduct this study; Kathy Bailey, Alice Dowling, and Margie Thompson for their assistance in the data collection; and Elizabeth Allen, Ronald Bloom, Flory Nkoy, Louis Pangaro, Stephanie Richardson, and Rajendu Srivastava for manuscript review.
- ,,.The role of the student ward in the medical clerkships.J Med Educ.1985;60:524–529.
- .Changing the fourth‐year medicine clerkship structure: A successful model for a teaching service without housestaff.J Gen Intern Med.1993;8:31–32.
- ,.A randomized, controlled pilot study of placing third‐year medical clerks in a continuity clinic.Acad Med.1993;68:845–847.
- ,,.Consequences of shifting medical‐student education to the outpatient setting: effects on performance and experiences.Acad Med.1996;71(suppl 1):S99–S101.
- ,.Learning outcomes of an ambulatory care rotation in internal medicine for junior medical students.J Gen Intern Med.1993;8:189–192.
- ,,,,.A prospective, randomized trial of a six‐week ambulatory medicine rotation.Acad Med.1995;70:537–541.
- ,,,,.Ambulatory versus inpatient rotations in teaching third‐year students internal medicine.J Gen Intern Med.1998;13:327–330.
- ,,,,.The effect of an ambulatory internal medicine rotation on students' career choices.Acad Med.1997;72:147–149.
- .Theme issue on medical education: Call for papers.JAMA.2005;293:742.
- Perkin RM,Swift JD,Newton DA, eds.Pediatric Hospital Medicine: Textbook of Inpatient Management.Philadelphia:Lippincott Williams 2003.
- .Call for greater emphasis on effect‐size measures in published articles in Teaching and Learning in Medicine.Teach Learn Med.2002;14:206–210.
- .Educational research and randomised trials.Med Educ.2002;36:1002–1003.
- ,.The objective structured clinical examination.Arch Pediatr Adolesc Med.2000;154:736–741.
- ,,,.Relationship of how well attending physicians teach to their student's performances and residency choices.Acad Med.1997;72(suppl 1):S118–S120.
- ,.Assessing quality and costs of education in the ambulatory setting: A review of the literature.Acad Med.2002;77:621–680.
The third‐year pediatric clerkship at the University of Utah School of Medicine has a relatively unique inpatient service, the Glasgow Service, which consists of an academic attending, a third‐year pediatric resident, and 4 third‐year medical students, but no interns. (This service was named in honor of Lowell Glasgow, chair of pediatrics, 1972‐82.) This structure was introduced in 1992 by the chair of pediatrics, Michael Simmons, the residency program director, Richard Molteni, and the clerkship director, Karen Hansen. These individuals desired to improve students' inpatient experience by providing greater responsibility for patient care. An additional motive was to increase the total number of patients followed by house staff without increasing the size of the residency program.
This inpatient service is a part of a 6‐week pediatric clerkship. All students perform the 3‐week inpatient portion of their clerkship at Primary Children's Medical Center, a tertiary‐care, freestanding children's hospital. (The students also spend 1 week each in a newborn nursery, an outpatient clinic, and a subspecialty setting). The academic attendings include generalists, hospitalists, and specialists who concurrently have other clinical responsibilities. The students take in‐house call every fourth night, supervised by senior residents who are not necessarily members of their service. All students share the same formal teaching activities, including morning report, a noon conference, and a student conference.
Patients are assigned to the ward services by a senior admitting resident. The admitting resident distributes patients among the services based on the complexity and acuity of the patients' conditions as well as the census on the various services. The senior resident supervising a particular service then assigns patients among the members of that service. Each third‐year medical student is expected to care for 2 or 3 patients at a time.
In addition to the intervention service, students also rotate on 2 similar traditional services. These services are traditional in the sense that they are composed of an academic attending, a community attending, a third‐year pediatric resident, 4 interns, and up to 2 fourth‐year and 2 third‐year medical students. Faculty preferences regarding service assignments were accommodated when possible. Therefore, some faculty attended only on one type of service, intervention or traditional, and others attended on both types. Because they have more members and because interns are capable of caring for more patients than are medical students, the traditional services cared for more patients than the intervention service. Although identical in composition, the 2 traditional services differ with each other in several ways. One service typically admits children 3 years old and younger, whereas the other admits children who are between 3 and 12 years old. The service that admits older children also admits most of the hematology‐oncology patients.
Although other authors have described similar inpatient clerkship structures, to our knowledge, none have evaluated them through a prospective randomized controlled trial.1, 2 The recent literature on ambulatory experiences during third‐year clerkships provided a methodological framework for this study. Collectively, such studies have evaluated outcomes with a variety of measures, including patient logs,35 evaluations,3, 4, 6, 7 examinations,37 surveys,3, 5, 7, 8 and career choices.4, 68 Additional outcomes, such as the effect of educational interventions on patient care, have been emphasized.9
In the light of this research, we conducted a prospective, randomized controlled trial to compare outcomes on the intervention service with those on the traditional services. We hypothesized that, compared with the traditional services, the intervention service would show:
improved process measures in terms of increased number of patients admitted, number of key diagnoses encountered in the patients cared for, and range of ages of the patients admitted;
similar or improved student performance, as measured by faculty and resident evaluations and a National Board of Medical Examiners (NBME) subject examination;
increased student satisfaction, as assessed by an end‐of‐rotation questionnaire;
increased interest in pediatric and, more broadly, primary care careers, as measured by subinternship and internship selections; and
comparable or improved resource utilization in terms of length of stay and total charges.
METHODS
All students enrolled in the third‐year pediatric rotation during the 2001‐2003 academic years were individually randomized by the clerkship assistant to the intervention service or 1 of the 2 traditional services without respect to career preference. A 5:3 student randomization ratio was used to fulfill the requirement that 4 students be assigned to the intervention service during every 3‐week block. This permitted the service to have call every fourth night.
To evaluate the adequacy of the randomization process, we obtained baseline student characteristics on age, sex, and United States Medical Licensing Examination (USMLE) Step 1 score from the Dean of Student Affairs. The dean also reported the discipline each student enrolled in for the required fourth‐year subinternship(s) and matched in for internship. These data were reported anonymously and linked to the service to which the student was assigned. In this study, pediatrics, internal medicine, and family practice were all considered primary care, but preliminary or transitional internships were not.
Process Measures
Students were required to submit logs at the end of their rotations, recording patients' names, ages, diagnoses, and admission dates. The accuracy and completeness of these logs were not independently verified.
As there was no authoritative list of key diagnoses third‐year medical students should encounter in the patients they care for during their inpatient rotations, we relied on expert opinion at our institution. The Council on Medical Student Education in Pediatrics' curriculum was not used because it did not differentiate between inpatient and ambulatory contexts. A preliminary list of 93 diagnoses was developed from the table of contents of Pediatric Hospital Medicine.10 This list was distributed to the 26 clinical faculty members in the Divisions of Pediatric Inpatient Medicine and General Pediatrics who were asked to select the 10 most important diagnoses. Surveys were numerically coded to permit 1 reminder.
The survey had a response rate of 92.3% (24 of 26 surveys). One survey was excluded because the respondent significantly deviated from the instructions. The 10 key diagnoses and the percentages of respondents who selected each individual diagnosis are: asthma (100%), febrile infant (95.6%), diarrhea and dehydration (91.3%), bronchiolitis (78.2%), diabetes mellitus and diabetic ketoacidemia (60.9%), failure to thrive (56.5%), urinary tract infections (52.1%), pneumonia (47.8%), upper airway infections such as croup (43.5%), and seizures and status epilepticus (43.5%).
Two of the authors independently coded the diagnoses on the students' patient logs in terms of these 93 diagnoses. The authors were blinded to the students' service assignment. As many students reported more than 1 diagnosis, the authors prioritized primary, secondary, and tertiary diagnoses to simplify the evaluation. The most likely cause of admission was listed as the primary diagnosis. If the authors could not reconcile divergent views, a third party was consulted.
Student Performance
Students were evaluated by both the attending physician(s) and senior resident(s) using a standardized evaluation form available from the corresponding author. The evaluation contained 18 items in 7 categories: data gathering, data recording/reporting, knowledge, data interpretation, clinical performance, professional attitudes, and professional demeanor. The student was rated exceptional, above expectations, meets expectations, below expectations, unacceptable, or not observed on each item. A short narrative description illustrated each rating. The ratings were converted to a 5‐point scale, with exceptional being 5. If the evaluator marked the line between 2 ratings, it was recorded as half. When multiple attendings or residents evaluated a student, the scores for a given item were collapsed into an average score.
Students also completed a NBME pediatric subject examination on the last day of their rotation.
Additionally, students were requested to complete a questionnaire during the final week of the clerkship. The items on the questionnaire were meant to access students' perceptions of the quality of their attendings' and residents' teaching, a potentially confounding variable. The survey was piloted on a group of similar subjects. Informed consent was obtained for survey completion. The survey was anonymous and required approximately 7 minutes to complete.
Resource Utilization
Last, resource utilization data, length of stay and total charges, for the 4 most common primary diagnoses were compared between the intervention and the traditional services. The 4 most common primary diagnoses and the percentage of total diagnoses (n = 2047) that each represents were bronchiolitis, 13%; febrile infant, 8.6%; pneumonia, 7.1%; and asthma, 6.5% (the diagnosis other accounted for 12% of the total diagnoses). Unique patient identifiers were used to obtain length of stay and total charges from the hospital's database. All‐Patient‐Refined Diagnosis‐Related Groups Severity of Illness (APR‐DRG‐SOI) were also obtained and used to construct multivariate models. Patients who were admitted to the pediatric intensive care unit (PICU) were excluded from the analysis.
Statistical Analysis
Statistical analyses were conducted and frequencies and percentages were calculated using Stata SE version 8.0 (College Station, TX). For all interval and ratio‐scaled variables, distributions were tested for normality using the Shapiro‐Wilks test to determine whether to use parametric or nonparametric statistical tests. For distributions meeting the normality assumption, the unpaired t test was used to compare the intervention service with traditional services. Where the normality assumption was not met, the Mann‐Whitney test was used. Categorically scaled data were compared using Pearson's chi‐square test. The standardized mean differences, reported as d values, were calculated to determine the effect size. Small, medium, and large effect sizes were defined as d values of 0.20, 0.50, and 0.80, respectively.11 Teaching quality, an effect modifier, was entered as a covariate into a linear regression model. Analyses of length of stay and total charges were conducted using multivariate linear regression controlling for patient age and severity of illness.
This study was approved by the University of Utah and Primary Children's Medical Center's Institutional Review Board.
RESULTS
Two hundred and three students enrolled in the third‐year pediatric clerkship during the study period, and all students completed the clerkship on their assigned services. One hundred and twenty‐eight were randomized to the intervention service and 75 to the traditional services. There were no statistically significant differences in median age, percentage of male students, or mean USMLE Step 1 score between the students randomized to the intervention service and those randomized to the traditional services (Table 1).
| Intervention service | Traditional services | P value | |
|---|---|---|---|
| |||
| Age (median) | 28 | 28 | .76* |
| Sex (% male) | 58.6 | 62.7 | .57 |
| USMLE Step 1 score | 217 | 217 | .94 |
Process Measures
Overall, 96.6% of students (196 of 203) submitted patient logs; 97.7% of students (125 of 128) on the intervention service and 94.7% of students (71 of 75) on the traditional services. The students on the intervention service admitted a median of 10 patients, whereas the students on the traditional services admitted a median of 11 patients (d = 0.45, P < .01). Age data were recorded on 137 patient logs (69.9% of submitted logs, 72.0% of students on the intervention service vs. 66.2% of students on the traditional services). The percentage of students who saw at least 1 newborn (birth‐23 months), child (2‐12 years), and adolescent (12‐18 years) was 34.8% on the intervention service and 33.3% on the traditional services (P = .87) (Table 2).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| Median number of patients | 10 | 11 | 0.45 | < .01* |
| Percent of students who saw 1 newborn, child, and adolescent | 34.8% | 33.3% | 0.03 | .87 |
| Top 10 diagnoses cared for (n) | 4.4 | 3.6 | 0.48 | < .01 |
| Percent of patients cared for whose diagnoses were in top 10 | 59.3% | 46.8% | 0.62# | < .01 |
| Percent of unique diagnoses (median) | 80.0% | 80.0% | 0.02 | .62 |
Students on the intervention service encountered, on average, a larger number of the 10 key diagnoses (4.4 vs. 3.6, d = 0.48, P < .01) and a higher percentage of their patients had clinical conditions among the key diagnoses (59.3 vs. 46.8, d = 0.62, P < .01). To determine if this higher percentage was the result of admitting multiple patients with the same diagnosis, we examined the percentage of unique primary diagnosesthe number of different primary diagnoses divided by the total number of patientsand found no differences (Table 2).
Student Performance
The faculty and resident evaluations of the students showed statistically significant differences between those in the intervention service and those in the traditional services in only 2 of the 18 items. These items were analysis in the data interpretation category (3.81 vs. 3.64, d = 0.35, P = .02) and patient interaction in the professional demeanor category (3.89 vs. 3.76, d = 0.31, P < .05). Both differences favored the intervention service. There were no statistical differences by service in student performance on the NBME subject examination (73.2 vs. 72.3, P = .39).
Student Satisfaction
Overall, 87.2% of students (177 of 203) completed the survey; 87.5% of students (112 of 124) on the intervention service and 86.7% of students (65 of 75) on the traditional services. The students on the intervention service both had a more positive overall attitude about their rotation and were more likely to find it a satisfying educational experience. Students on the intervention service also reported greater participation in patient care. Effect sizes ranged from small to medium (Table 3). The internal consistency of answers about participation in patient care was high (Pearson correlation coefficient r = 0.80).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| My overall attitude toward this rotation is: 1. highly negative to 5. highly positive | 4.48 | 4.26 | 0.26 | .02* |
| I found this rotation a satisfying educational experience: 1. strongly disagree to 5. strongly agree | 4.49 | 4.22 | 0.35 | < .01* |
| My role on this rotation was that of an: 1. observer, 3. participant, 5. director | 3.77 | 3.33 | 0.60# | < .01 |
| My supervising interns/residents were _____ teachers: 1. poor, 3. good, 5. exemplary | 3.91 | 3.75 | 0.17 | .26* |
| My input into patient care decisions was: 1. strongly discouraged to 5. strongly encouraged | 4.45 | 3.98 | 0.66# | < .01* |
| I was able to make a significant contribution to patient care: 1. strongly disagree to 5. strongly agree | 4.19 | 3.92 | 0.34 | .02* |
| I had direct responsibility for patient care: 1. strongly disagree to 5. strongly agree | 4.33 | 3.95 | 0.46 | .01* |
| My attendings were _____ teachers: 1. poor, 3. good, 5. exemplary | 4.09 | 3.75 | 0.40 | < .01* |
| I found the feedback I received during this rotation to be: 1. insufficient, 3. appropriate, 5. excessive | 2.84 | 2.65 | 0.22 | .17* |
| The following best describes the quality of my supervision during this rotation: 1. I was expected to do things beyond my competence unsupervised 3. The degree of supervision was appropriate for my level of training 5. I was excessively supervised on skills I had already demonstrated | 2.95 | 3.06 | 0.18 | .19 |
| During this rotation: 1. I was expected to see too many patients 3. I was expected to see an appropriate number of patients 5. I expected to see more patients | 3.46 | 3.31 | 0.18 | .33* |
| Before this rotation I _____ pediatrics as a career choice: 1. had rejected, 3. was considering, 5. had decided on | 2.37 | 2.14 | 0.22 | .11* |
| This rotation increased my interest in pursuing pediatrics as a career: 1. strongly disagree to 5. strongly agree | 3.74 | 3.60 | 0.14 | .32* |
Students on the intervention service rated the teaching of their attendings, but not of their residents, higher than did students on the traditional services. Controlling for the perceived quality of the attending, 3 of 6 satisfaction outcomes remained statistically significant: role on rotation (P < .01), input into patient care decisions (P < .01), and direct responsibility for patient care (P = .04). Students on both services believed they were appropriately supervised (P = .19). Despite the students on the traditional services on average admitting more patients, there was no significant difference by service in the students' rating of patient load (P = .33).
Career Choice
The odds ratio and 95% confidence interval for students enrolling in a pediatric subinternship was 1.94 (0.83‐4.49) and matching in a pediatric residency was 2.52 (0.99‐6.37). There were no statistically significant differences by service in the percentage of students enrolling in primary care (pediatric, internal medicine, and family practice) subinternships or residencies (Table 4).
| Intervention service | Traditional services | Odds ratio (95% CI) | |
|---|---|---|---|
| Pediatric subinternship | 19.5% | 11.1% | 1.94 (0.83‐4.49) |
| Primary care subinternship | 68.3% | 70.8% | 0.89 (0.47‐1.67) |
| Pediatric residency | 18.6% | 8.3% | 2.52 (0.99‐6.37) |
| Primary care residency | 40.7% | 31.9% | 1.46 (0.79‐2.70) |
Resource Utilization
One hundred and thirty‐five patients were excluded from the resource utilization analysis (n = 594) because their unique identifiers could not be found or they had been admitted to the PICU. Univariate analysis demonstrated statistically significant differences for patients with asthma, but not patients with bronchiolitis, febrile infants, or patients with pneumonia, favoring the intervention service. Patients with asthma admitted to the intervention service had a shorter length of stay (49.9 vs. 70.1 hours, P = .02) and lower total charges ($3600 vs. $4600, P = .02), as shown in Table 5. Of 4 multivariate models controlling for age and severity of illness, each with length of stay and total charges as the dependant variables, length of stay was significantly less for patients with asthma admitted to the intervention service only. Such patients were discharged an average of 23.3 hours earlier than patients with asthma admitted to the traditional services (P = .02).
| Diagnosis (n) | n | Length of stay (hours) | P value | Total charges | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention service | Traditional services | Intervention service | Traditional services | Intervention service | Traditional services | P value | ||
| ||||||||
| Bronchiolitis (210) | 159 | 51 | 63.7 | 70.5 | .20* | $4300 | $4800 | .20* |
| Febrile infant (152) | 105 | 47 | 58.8 | 58.9 | .50* | $4800 | $4900 | .28* |
| Pneumonia (123) | 82 | 41 | 84.3 | 116.8 | .71* | $6300 | $9200 | .63* |
| Asthma (109) | 80 | 29 | 49.9 | 70.1 | .02* | $3600 | $4600 | .02* |
DISCUSSION
This study's objective was to evaluate a third‐year pediatric clerkship structure that focuses on students, using multiple outcome parameters. Utilizing a robust design, the results of this study have demonstrated that the intervention service is more successful than the traditional services in several outcomes. Students assigned to the intervention service were more satisfied and more likely to select pediatrics as a career. These improvements were accomplished while maintaining similar process measures, student performance, and resource utilization compared with those of the traditional services.
Methods
The methods used in this study compare favorably with other evaluations of educational interventions. The present study incorporated a randomized controlled design.12 Although several studies of ambulatory clerkships used a randomized design, few randomized all eligible students.7, 8 The others used some form of selection prior to randomization. For example, in the Pangaro et al. study, students selected their clerkship site by lottery, with students selecting a certain site then offered the opportunity to participate in the intervention.6 The present study manifested several additional strengths. Multiple outcomes, including effects on patient care, were evaluated. Moreover, this study had a relatively large intervention group and total sample size compared with those in other medical education studies. Finally, because the intervention service had been in place for several years prior to its evaluation, the confounding influence of difficulties working out its implementation was minimized.
Results
Few studies of ambulatory experiences demonstrated statistically significant, let alone clinically significant, results. Most studies showed no statistically significant differences in student evaluations or examination scores. An exception is Grum et al., who showed improvements on 3 of 5 examinations.4 A few studies have found improved student satisfaction.3 None of the randomized controlled trials demonstrate increases in students matching in internal medicine or primary care residencies.4, 68 In contrast, this study produced statistically or programmatically significant results in process measures, evaluations, satisfaction, and career choices.
Several of our specific findings deserve additional comment. Although the admitting residents were instructed to assign patients to the intervention service based on their acuity and complexity, it is important to examine these residents' actual behavior. Several of our hypotheses were not validated. The students on the intervention service admitted fewer patients and were no more likely to see at least 1 patient in each age category. The admitting resident may have limited the number of patients admitted to the intervention service based on the workload of the supervising resident not that of the student. The supervising resident on the intervention service must round on all the patients, whereas the oversight of patients seen by students on the traditional services is shared with the interns. Having the attending on the intervention service share this supervising responsibility might improve this outcome.
Students on the intervention service had more positive attitudes toward the rotation. In addition, potentially negative attitudes were not manifest. For example, it might be argued that third‐year medical students are not prepared to bear this increased responsibility. However, there was not a significant difference in students' perception of the quality of supervision or the workload.
Although the goal of medical education is the production of competent physicians, it is important that the process not place undo burdens on patients and the health care system. Univariate analysis showed similar resource utilization. It might be contended that the admitting resident assigned the intervention service patients who were less acutely ill. Therefore, we performed multivariate analysis using APR‐DRG‐SOI to control for severity of illness. Of 8 comparisons, the only statistically significant difference, length of stay of patients with asthma, favored the intervention service.
Limitations
Although this study had numerous strengths, it also had several limitations. The primary limitations were lack of generalizability, difficulty in obtaining authentic assessments, the potential difference between statistical and educational significance, and inability to identify which components of the intervention service were responsible for the outcomes. This study's findings may not be generalizable to other institutions. For example, institutions without age or organ systembased teams may not observe increases in the number of key diagnoses encountered in the patients cared for. Regarding the assessments, there may be better measures of clinical competence, such as an objective structured clinical examination (OSCE),13 than those used in this study. However, there were not sufficient resources to implement an OSCE at the end of the rotation.
Some might question whether the statistically significant differences have educational significance. Although that is an important concern, this study should be compared with other educational interventions that found few statistically significant, let alone educationally significant, differences. To address this concern, we calculated effect sizes. The differences in student satisfaction were small to moderate. Although the lower limit of the 95% confidence interval of the odds ratio for matching in a pediatric residency was 0.99, the magnitude was programmatically important.
Finally, this study was an evaluation of an existing program. The authors were unable to control some potential confounders including patient allocation, average daily census, and quality of teaching. For example, Griffith and colleagues have shown that working with the best teachers improves student performance.14 We were not able to randomly assign the faculty among the services, and unequal distribution of better teachers could have biased this study's outcomes. The students on the intervention service rated their attendings, but not their residents, higher than did the students on the other services. However, the linear regression model showed that the perceived quality of the attending did not account for all the differences in student satisfaction. It was not possible to control for this factor in comparing student performance or subinternship or residency selection because the survey, which included the faculty evaluations, was anonymous and therefore could not be linked to the other data sets.
The perceived differences in the quality of teaching may not have been the result of differences in the attendings but instead of differences in the structure of the services. Accessibility is one of the characteristics of excellent clinical teachers.15 The intervention structure may permit faculty to spend more time with students, and this may increase the perceived quality of the teaching. However, it is not possible to resolve this issue with the available data.
CONCLUSIONS
The intervention service is a structure for the pediatric inpatient rotation of third‐year medical students that, instead of dividing the faculty and supervising resident's attention between interns and students, focuses their attention on the students. Although it has been difficult to demonstrate improvements as a result of the educational interventions, we have shown several improvements in the evaluations of the students. Moreover, the pattern of increased student satisfaction and a tendency toward more student selecting careers in pediatrics are remarkable. This was accomplished with similar resource utilization. Therefore, this program merits being continued at our institution and possibly adopted at other medical schools. Further research is needed to determine which aspects of the intervention are responsible for its effects. Some components, such as focused time with students, may be applicable to traditional services.
Acknowledgements
The authors thank Ronald Bloom for encouraging us to conduct this study; Kathy Bailey, Alice Dowling, and Margie Thompson for their assistance in the data collection; and Elizabeth Allen, Ronald Bloom, Flory Nkoy, Louis Pangaro, Stephanie Richardson, and Rajendu Srivastava for manuscript review.
The third‐year pediatric clerkship at the University of Utah School of Medicine has a relatively unique inpatient service, the Glasgow Service, which consists of an academic attending, a third‐year pediatric resident, and 4 third‐year medical students, but no interns. (This service was named in honor of Lowell Glasgow, chair of pediatrics, 1972‐82.) This structure was introduced in 1992 by the chair of pediatrics, Michael Simmons, the residency program director, Richard Molteni, and the clerkship director, Karen Hansen. These individuals desired to improve students' inpatient experience by providing greater responsibility for patient care. An additional motive was to increase the total number of patients followed by house staff without increasing the size of the residency program.
This inpatient service is a part of a 6‐week pediatric clerkship. All students perform the 3‐week inpatient portion of their clerkship at Primary Children's Medical Center, a tertiary‐care, freestanding children's hospital. (The students also spend 1 week each in a newborn nursery, an outpatient clinic, and a subspecialty setting). The academic attendings include generalists, hospitalists, and specialists who concurrently have other clinical responsibilities. The students take in‐house call every fourth night, supervised by senior residents who are not necessarily members of their service. All students share the same formal teaching activities, including morning report, a noon conference, and a student conference.
Patients are assigned to the ward services by a senior admitting resident. The admitting resident distributes patients among the services based on the complexity and acuity of the patients' conditions as well as the census on the various services. The senior resident supervising a particular service then assigns patients among the members of that service. Each third‐year medical student is expected to care for 2 or 3 patients at a time.
In addition to the intervention service, students also rotate on 2 similar traditional services. These services are traditional in the sense that they are composed of an academic attending, a community attending, a third‐year pediatric resident, 4 interns, and up to 2 fourth‐year and 2 third‐year medical students. Faculty preferences regarding service assignments were accommodated when possible. Therefore, some faculty attended only on one type of service, intervention or traditional, and others attended on both types. Because they have more members and because interns are capable of caring for more patients than are medical students, the traditional services cared for more patients than the intervention service. Although identical in composition, the 2 traditional services differ with each other in several ways. One service typically admits children 3 years old and younger, whereas the other admits children who are between 3 and 12 years old. The service that admits older children also admits most of the hematology‐oncology patients.
Although other authors have described similar inpatient clerkship structures, to our knowledge, none have evaluated them through a prospective randomized controlled trial.1, 2 The recent literature on ambulatory experiences during third‐year clerkships provided a methodological framework for this study. Collectively, such studies have evaluated outcomes with a variety of measures, including patient logs,35 evaluations,3, 4, 6, 7 examinations,37 surveys,3, 5, 7, 8 and career choices.4, 68 Additional outcomes, such as the effect of educational interventions on patient care, have been emphasized.9
In the light of this research, we conducted a prospective, randomized controlled trial to compare outcomes on the intervention service with those on the traditional services. We hypothesized that, compared with the traditional services, the intervention service would show:
improved process measures in terms of increased number of patients admitted, number of key diagnoses encountered in the patients cared for, and range of ages of the patients admitted;
similar or improved student performance, as measured by faculty and resident evaluations and a National Board of Medical Examiners (NBME) subject examination;
increased student satisfaction, as assessed by an end‐of‐rotation questionnaire;
increased interest in pediatric and, more broadly, primary care careers, as measured by subinternship and internship selections; and
comparable or improved resource utilization in terms of length of stay and total charges.
METHODS
All students enrolled in the third‐year pediatric rotation during the 2001‐2003 academic years were individually randomized by the clerkship assistant to the intervention service or 1 of the 2 traditional services without respect to career preference. A 5:3 student randomization ratio was used to fulfill the requirement that 4 students be assigned to the intervention service during every 3‐week block. This permitted the service to have call every fourth night.
To evaluate the adequacy of the randomization process, we obtained baseline student characteristics on age, sex, and United States Medical Licensing Examination (USMLE) Step 1 score from the Dean of Student Affairs. The dean also reported the discipline each student enrolled in for the required fourth‐year subinternship(s) and matched in for internship. These data were reported anonymously and linked to the service to which the student was assigned. In this study, pediatrics, internal medicine, and family practice were all considered primary care, but preliminary or transitional internships were not.
Process Measures
Students were required to submit logs at the end of their rotations, recording patients' names, ages, diagnoses, and admission dates. The accuracy and completeness of these logs were not independently verified.
As there was no authoritative list of key diagnoses third‐year medical students should encounter in the patients they care for during their inpatient rotations, we relied on expert opinion at our institution. The Council on Medical Student Education in Pediatrics' curriculum was not used because it did not differentiate between inpatient and ambulatory contexts. A preliminary list of 93 diagnoses was developed from the table of contents of Pediatric Hospital Medicine.10 This list was distributed to the 26 clinical faculty members in the Divisions of Pediatric Inpatient Medicine and General Pediatrics who were asked to select the 10 most important diagnoses. Surveys were numerically coded to permit 1 reminder.
The survey had a response rate of 92.3% (24 of 26 surveys). One survey was excluded because the respondent significantly deviated from the instructions. The 10 key diagnoses and the percentages of respondents who selected each individual diagnosis are: asthma (100%), febrile infant (95.6%), diarrhea and dehydration (91.3%), bronchiolitis (78.2%), diabetes mellitus and diabetic ketoacidemia (60.9%), failure to thrive (56.5%), urinary tract infections (52.1%), pneumonia (47.8%), upper airway infections such as croup (43.5%), and seizures and status epilepticus (43.5%).
Two of the authors independently coded the diagnoses on the students' patient logs in terms of these 93 diagnoses. The authors were blinded to the students' service assignment. As many students reported more than 1 diagnosis, the authors prioritized primary, secondary, and tertiary diagnoses to simplify the evaluation. The most likely cause of admission was listed as the primary diagnosis. If the authors could not reconcile divergent views, a third party was consulted.
Student Performance
Students were evaluated by both the attending physician(s) and senior resident(s) using a standardized evaluation form available from the corresponding author. The evaluation contained 18 items in 7 categories: data gathering, data recording/reporting, knowledge, data interpretation, clinical performance, professional attitudes, and professional demeanor. The student was rated exceptional, above expectations, meets expectations, below expectations, unacceptable, or not observed on each item. A short narrative description illustrated each rating. The ratings were converted to a 5‐point scale, with exceptional being 5. If the evaluator marked the line between 2 ratings, it was recorded as half. When multiple attendings or residents evaluated a student, the scores for a given item were collapsed into an average score.
Students also completed a NBME pediatric subject examination on the last day of their rotation.
Additionally, students were requested to complete a questionnaire during the final week of the clerkship. The items on the questionnaire were meant to access students' perceptions of the quality of their attendings' and residents' teaching, a potentially confounding variable. The survey was piloted on a group of similar subjects. Informed consent was obtained for survey completion. The survey was anonymous and required approximately 7 minutes to complete.
Resource Utilization
Last, resource utilization data, length of stay and total charges, for the 4 most common primary diagnoses were compared between the intervention and the traditional services. The 4 most common primary diagnoses and the percentage of total diagnoses (n = 2047) that each represents were bronchiolitis, 13%; febrile infant, 8.6%; pneumonia, 7.1%; and asthma, 6.5% (the diagnosis other accounted for 12% of the total diagnoses). Unique patient identifiers were used to obtain length of stay and total charges from the hospital's database. All‐Patient‐Refined Diagnosis‐Related Groups Severity of Illness (APR‐DRG‐SOI) were also obtained and used to construct multivariate models. Patients who were admitted to the pediatric intensive care unit (PICU) were excluded from the analysis.
Statistical Analysis
Statistical analyses were conducted and frequencies and percentages were calculated using Stata SE version 8.0 (College Station, TX). For all interval and ratio‐scaled variables, distributions were tested for normality using the Shapiro‐Wilks test to determine whether to use parametric or nonparametric statistical tests. For distributions meeting the normality assumption, the unpaired t test was used to compare the intervention service with traditional services. Where the normality assumption was not met, the Mann‐Whitney test was used. Categorically scaled data were compared using Pearson's chi‐square test. The standardized mean differences, reported as d values, were calculated to determine the effect size. Small, medium, and large effect sizes were defined as d values of 0.20, 0.50, and 0.80, respectively.11 Teaching quality, an effect modifier, was entered as a covariate into a linear regression model. Analyses of length of stay and total charges were conducted using multivariate linear regression controlling for patient age and severity of illness.
This study was approved by the University of Utah and Primary Children's Medical Center's Institutional Review Board.
RESULTS
Two hundred and three students enrolled in the third‐year pediatric clerkship during the study period, and all students completed the clerkship on their assigned services. One hundred and twenty‐eight were randomized to the intervention service and 75 to the traditional services. There were no statistically significant differences in median age, percentage of male students, or mean USMLE Step 1 score between the students randomized to the intervention service and those randomized to the traditional services (Table 1).
| Intervention service | Traditional services | P value | |
|---|---|---|---|
| |||
| Age (median) | 28 | 28 | .76* |
| Sex (% male) | 58.6 | 62.7 | .57 |
| USMLE Step 1 score | 217 | 217 | .94 |
Process Measures
Overall, 96.6% of students (196 of 203) submitted patient logs; 97.7% of students (125 of 128) on the intervention service and 94.7% of students (71 of 75) on the traditional services. The students on the intervention service admitted a median of 10 patients, whereas the students on the traditional services admitted a median of 11 patients (d = 0.45, P < .01). Age data were recorded on 137 patient logs (69.9% of submitted logs, 72.0% of students on the intervention service vs. 66.2% of students on the traditional services). The percentage of students who saw at least 1 newborn (birth‐23 months), child (2‐12 years), and adolescent (12‐18 years) was 34.8% on the intervention service and 33.3% on the traditional services (P = .87) (Table 2).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| Median number of patients | 10 | 11 | 0.45 | < .01* |
| Percent of students who saw 1 newborn, child, and adolescent | 34.8% | 33.3% | 0.03 | .87 |
| Top 10 diagnoses cared for (n) | 4.4 | 3.6 | 0.48 | < .01 |
| Percent of patients cared for whose diagnoses were in top 10 | 59.3% | 46.8% | 0.62# | < .01 |
| Percent of unique diagnoses (median) | 80.0% | 80.0% | 0.02 | .62 |
Students on the intervention service encountered, on average, a larger number of the 10 key diagnoses (4.4 vs. 3.6, d = 0.48, P < .01) and a higher percentage of their patients had clinical conditions among the key diagnoses (59.3 vs. 46.8, d = 0.62, P < .01). To determine if this higher percentage was the result of admitting multiple patients with the same diagnosis, we examined the percentage of unique primary diagnosesthe number of different primary diagnoses divided by the total number of patientsand found no differences (Table 2).
Student Performance
The faculty and resident evaluations of the students showed statistically significant differences between those in the intervention service and those in the traditional services in only 2 of the 18 items. These items were analysis in the data interpretation category (3.81 vs. 3.64, d = 0.35, P = .02) and patient interaction in the professional demeanor category (3.89 vs. 3.76, d = 0.31, P < .05). Both differences favored the intervention service. There were no statistical differences by service in student performance on the NBME subject examination (73.2 vs. 72.3, P = .39).
Student Satisfaction
Overall, 87.2% of students (177 of 203) completed the survey; 87.5% of students (112 of 124) on the intervention service and 86.7% of students (65 of 75) on the traditional services. The students on the intervention service both had a more positive overall attitude about their rotation and were more likely to find it a satisfying educational experience. Students on the intervention service also reported greater participation in patient care. Effect sizes ranged from small to medium (Table 3). The internal consistency of answers about participation in patient care was high (Pearson correlation coefficient r = 0.80).
| Intervention service | Traditional services | d | P value | |
|---|---|---|---|---|
| ||||
| My overall attitude toward this rotation is: 1. highly negative to 5. highly positive | 4.48 | 4.26 | 0.26 | .02* |
| I found this rotation a satisfying educational experience: 1. strongly disagree to 5. strongly agree | 4.49 | 4.22 | 0.35 | < .01* |
| My role on this rotation was that of an: 1. observer, 3. participant, 5. director | 3.77 | 3.33 | 0.60# | < .01 |
| My supervising interns/residents were _____ teachers: 1. poor, 3. good, 5. exemplary | 3.91 | 3.75 | 0.17 | .26* |
| My input into patient care decisions was: 1. strongly discouraged to 5. strongly encouraged | 4.45 | 3.98 | 0.66# | < .01* |
| I was able to make a significant contribution to patient care: 1. strongly disagree to 5. strongly agree | 4.19 | 3.92 | 0.34 | .02* |
| I had direct responsibility for patient care: 1. strongly disagree to 5. strongly agree | 4.33 | 3.95 | 0.46 | .01* |
| My attendings were _____ teachers: 1. poor, 3. good, 5. exemplary | 4.09 | 3.75 | 0.40 | < .01* |
| I found the feedback I received during this rotation to be: 1. insufficient, 3. appropriate, 5. excessive | 2.84 | 2.65 | 0.22 | .17* |
| The following best describes the quality of my supervision during this rotation: 1. I was expected to do things beyond my competence unsupervised 3. The degree of supervision was appropriate for my level of training 5. I was excessively supervised on skills I had already demonstrated | 2.95 | 3.06 | 0.18 | .19 |
| During this rotation: 1. I was expected to see too many patients 3. I was expected to see an appropriate number of patients 5. I expected to see more patients | 3.46 | 3.31 | 0.18 | .33* |
| Before this rotation I _____ pediatrics as a career choice: 1. had rejected, 3. was considering, 5. had decided on | 2.37 | 2.14 | 0.22 | .11* |
| This rotation increased my interest in pursuing pediatrics as a career: 1. strongly disagree to 5. strongly agree | 3.74 | 3.60 | 0.14 | .32* |
Students on the intervention service rated the teaching of their attendings, but not of their residents, higher than did students on the traditional services. Controlling for the perceived quality of the attending, 3 of 6 satisfaction outcomes remained statistically significant: role on rotation (P < .01), input into patient care decisions (P < .01), and direct responsibility for patient care (P = .04). Students on both services believed they were appropriately supervised (P = .19). Despite the students on the traditional services on average admitting more patients, there was no significant difference by service in the students' rating of patient load (P = .33).
Career Choice
The odds ratio and 95% confidence interval for students enrolling in a pediatric subinternship was 1.94 (0.83‐4.49) and matching in a pediatric residency was 2.52 (0.99‐6.37). There were no statistically significant differences by service in the percentage of students enrolling in primary care (pediatric, internal medicine, and family practice) subinternships or residencies (Table 4).
| Intervention service | Traditional services | Odds ratio (95% CI) | |
|---|---|---|---|
| Pediatric subinternship | 19.5% | 11.1% | 1.94 (0.83‐4.49) |
| Primary care subinternship | 68.3% | 70.8% | 0.89 (0.47‐1.67) |
| Pediatric residency | 18.6% | 8.3% | 2.52 (0.99‐6.37) |
| Primary care residency | 40.7% | 31.9% | 1.46 (0.79‐2.70) |
Resource Utilization
One hundred and thirty‐five patients were excluded from the resource utilization analysis (n = 594) because their unique identifiers could not be found or they had been admitted to the PICU. Univariate analysis demonstrated statistically significant differences for patients with asthma, but not patients with bronchiolitis, febrile infants, or patients with pneumonia, favoring the intervention service. Patients with asthma admitted to the intervention service had a shorter length of stay (49.9 vs. 70.1 hours, P = .02) and lower total charges ($3600 vs. $4600, P = .02), as shown in Table 5. Of 4 multivariate models controlling for age and severity of illness, each with length of stay and total charges as the dependant variables, length of stay was significantly less for patients with asthma admitted to the intervention service only. Such patients were discharged an average of 23.3 hours earlier than patients with asthma admitted to the traditional services (P = .02).
| Diagnosis (n) | n | Length of stay (hours) | P value | Total charges | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention service | Traditional services | Intervention service | Traditional services | Intervention service | Traditional services | P value | ||
| ||||||||
| Bronchiolitis (210) | 159 | 51 | 63.7 | 70.5 | .20* | $4300 | $4800 | .20* |
| Febrile infant (152) | 105 | 47 | 58.8 | 58.9 | .50* | $4800 | $4900 | .28* |
| Pneumonia (123) | 82 | 41 | 84.3 | 116.8 | .71* | $6300 | $9200 | .63* |
| Asthma (109) | 80 | 29 | 49.9 | 70.1 | .02* | $3600 | $4600 | .02* |
DISCUSSION
This study's objective was to evaluate a third‐year pediatric clerkship structure that focuses on students, using multiple outcome parameters. Utilizing a robust design, the results of this study have demonstrated that the intervention service is more successful than the traditional services in several outcomes. Students assigned to the intervention service were more satisfied and more likely to select pediatrics as a career. These improvements were accomplished while maintaining similar process measures, student performance, and resource utilization compared with those of the traditional services.
Methods
The methods used in this study compare favorably with other evaluations of educational interventions. The present study incorporated a randomized controlled design.12 Although several studies of ambulatory clerkships used a randomized design, few randomized all eligible students.7, 8 The others used some form of selection prior to randomization. For example, in the Pangaro et al. study, students selected their clerkship site by lottery, with students selecting a certain site then offered the opportunity to participate in the intervention.6 The present study manifested several additional strengths. Multiple outcomes, including effects on patient care, were evaluated. Moreover, this study had a relatively large intervention group and total sample size compared with those in other medical education studies. Finally, because the intervention service had been in place for several years prior to its evaluation, the confounding influence of difficulties working out its implementation was minimized.
Results
Few studies of ambulatory experiences demonstrated statistically significant, let alone clinically significant, results. Most studies showed no statistically significant differences in student evaluations or examination scores. An exception is Grum et al., who showed improvements on 3 of 5 examinations.4 A few studies have found improved student satisfaction.3 None of the randomized controlled trials demonstrate increases in students matching in internal medicine or primary care residencies.4, 68 In contrast, this study produced statistically or programmatically significant results in process measures, evaluations, satisfaction, and career choices.
Several of our specific findings deserve additional comment. Although the admitting residents were instructed to assign patients to the intervention service based on their acuity and complexity, it is important to examine these residents' actual behavior. Several of our hypotheses were not validated. The students on the intervention service admitted fewer patients and were no more likely to see at least 1 patient in each age category. The admitting resident may have limited the number of patients admitted to the intervention service based on the workload of the supervising resident not that of the student. The supervising resident on the intervention service must round on all the patients, whereas the oversight of patients seen by students on the traditional services is shared with the interns. Having the attending on the intervention service share this supervising responsibility might improve this outcome.
Students on the intervention service had more positive attitudes toward the rotation. In addition, potentially negative attitudes were not manifest. For example, it might be argued that third‐year medical students are not prepared to bear this increased responsibility. However, there was not a significant difference in students' perception of the quality of supervision or the workload.
Although the goal of medical education is the production of competent physicians, it is important that the process not place undo burdens on patients and the health care system. Univariate analysis showed similar resource utilization. It might be contended that the admitting resident assigned the intervention service patients who were less acutely ill. Therefore, we performed multivariate analysis using APR‐DRG‐SOI to control for severity of illness. Of 8 comparisons, the only statistically significant difference, length of stay of patients with asthma, favored the intervention service.
Limitations
Although this study had numerous strengths, it also had several limitations. The primary limitations were lack of generalizability, difficulty in obtaining authentic assessments, the potential difference between statistical and educational significance, and inability to identify which components of the intervention service were responsible for the outcomes. This study's findings may not be generalizable to other institutions. For example, institutions without age or organ systembased teams may not observe increases in the number of key diagnoses encountered in the patients cared for. Regarding the assessments, there may be better measures of clinical competence, such as an objective structured clinical examination (OSCE),13 than those used in this study. However, there were not sufficient resources to implement an OSCE at the end of the rotation.
Some might question whether the statistically significant differences have educational significance. Although that is an important concern, this study should be compared with other educational interventions that found few statistically significant, let alone educationally significant, differences. To address this concern, we calculated effect sizes. The differences in student satisfaction were small to moderate. Although the lower limit of the 95% confidence interval of the odds ratio for matching in a pediatric residency was 0.99, the magnitude was programmatically important.
Finally, this study was an evaluation of an existing program. The authors were unable to control some potential confounders including patient allocation, average daily census, and quality of teaching. For example, Griffith and colleagues have shown that working with the best teachers improves student performance.14 We were not able to randomly assign the faculty among the services, and unequal distribution of better teachers could have biased this study's outcomes. The students on the intervention service rated their attendings, but not their residents, higher than did the students on the other services. However, the linear regression model showed that the perceived quality of the attending did not account for all the differences in student satisfaction. It was not possible to control for this factor in comparing student performance or subinternship or residency selection because the survey, which included the faculty evaluations, was anonymous and therefore could not be linked to the other data sets.
The perceived differences in the quality of teaching may not have been the result of differences in the attendings but instead of differences in the structure of the services. Accessibility is one of the characteristics of excellent clinical teachers.15 The intervention structure may permit faculty to spend more time with students, and this may increase the perceived quality of the teaching. However, it is not possible to resolve this issue with the available data.
CONCLUSIONS
The intervention service is a structure for the pediatric inpatient rotation of third‐year medical students that, instead of dividing the faculty and supervising resident's attention between interns and students, focuses their attention on the students. Although it has been difficult to demonstrate improvements as a result of the educational interventions, we have shown several improvements in the evaluations of the students. Moreover, the pattern of increased student satisfaction and a tendency toward more student selecting careers in pediatrics are remarkable. This was accomplished with similar resource utilization. Therefore, this program merits being continued at our institution and possibly adopted at other medical schools. Further research is needed to determine which aspects of the intervention are responsible for its effects. Some components, such as focused time with students, may be applicable to traditional services.
Acknowledgements
The authors thank Ronald Bloom for encouraging us to conduct this study; Kathy Bailey, Alice Dowling, and Margie Thompson for their assistance in the data collection; and Elizabeth Allen, Ronald Bloom, Flory Nkoy, Louis Pangaro, Stephanie Richardson, and Rajendu Srivastava for manuscript review.
- ,,.The role of the student ward in the medical clerkships.J Med Educ.1985;60:524–529.
- .Changing the fourth‐year medicine clerkship structure: A successful model for a teaching service without housestaff.J Gen Intern Med.1993;8:31–32.
- ,.A randomized, controlled pilot study of placing third‐year medical clerks in a continuity clinic.Acad Med.1993;68:845–847.
- ,,.Consequences of shifting medical‐student education to the outpatient setting: effects on performance and experiences.Acad Med.1996;71(suppl 1):S99–S101.
- ,.Learning outcomes of an ambulatory care rotation in internal medicine for junior medical students.J Gen Intern Med.1993;8:189–192.
- ,,,,.A prospective, randomized trial of a six‐week ambulatory medicine rotation.Acad Med.1995;70:537–541.
- ,,,,.Ambulatory versus inpatient rotations in teaching third‐year students internal medicine.J Gen Intern Med.1998;13:327–330.
- ,,,,.The effect of an ambulatory internal medicine rotation on students' career choices.Acad Med.1997;72:147–149.
- .Theme issue on medical education: Call for papers.JAMA.2005;293:742.
- Perkin RM,Swift JD,Newton DA, eds.Pediatric Hospital Medicine: Textbook of Inpatient Management.Philadelphia:Lippincott Williams 2003.
- .Call for greater emphasis on effect‐size measures in published articles in Teaching and Learning in Medicine.Teach Learn Med.2002;14:206–210.
- .Educational research and randomised trials.Med Educ.2002;36:1002–1003.
- ,.The objective structured clinical examination.Arch Pediatr Adolesc Med.2000;154:736–741.
- ,,,.Relationship of how well attending physicians teach to their student's performances and residency choices.Acad Med.1997;72(suppl 1):S118–S120.
- ,.Assessing quality and costs of education in the ambulatory setting: A review of the literature.Acad Med.2002;77:621–680.
- ,,.The role of the student ward in the medical clerkships.J Med Educ.1985;60:524–529.
- .Changing the fourth‐year medicine clerkship structure: A successful model for a teaching service without housestaff.J Gen Intern Med.1993;8:31–32.
- ,.A randomized, controlled pilot study of placing third‐year medical clerks in a continuity clinic.Acad Med.1993;68:845–847.
- ,,.Consequences of shifting medical‐student education to the outpatient setting: effects on performance and experiences.Acad Med.1996;71(suppl 1):S99–S101.
- ,.Learning outcomes of an ambulatory care rotation in internal medicine for junior medical students.J Gen Intern Med.1993;8:189–192.
- ,,,,.A prospective, randomized trial of a six‐week ambulatory medicine rotation.Acad Med.1995;70:537–541.
- ,,,,.Ambulatory versus inpatient rotations in teaching third‐year students internal medicine.J Gen Intern Med.1998;13:327–330.
- ,,,,.The effect of an ambulatory internal medicine rotation on students' career choices.Acad Med.1997;72:147–149.
- .Theme issue on medical education: Call for papers.JAMA.2005;293:742.
- Perkin RM,Swift JD,Newton DA, eds.Pediatric Hospital Medicine: Textbook of Inpatient Management.Philadelphia:Lippincott Williams 2003.
- .Call for greater emphasis on effect‐size measures in published articles in Teaching and Learning in Medicine.Teach Learn Med.2002;14:206–210.
- .Educational research and randomised trials.Med Educ.2002;36:1002–1003.
- ,.The objective structured clinical examination.Arch Pediatr Adolesc Med.2000;154:736–741.
- ,,,.Relationship of how well attending physicians teach to their student's performances and residency choices.Acad Med.1997;72(suppl 1):S118–S120.
- ,.Assessing quality and costs of education in the ambulatory setting: A review of the literature.Acad Med.2002;77:621–680.
Copyright © 2007 Society of Hospital Medicine
Alcohol‐Dependent Patients
Alcohol dependence is commonly associated with severe medical disease1 and is common among hospitalized medical patients. A nationally representative hospital sample found current alcohol use disorders to have a prevalence of 7.4%; most of those with these disorders were alcohol dependent.2 However, depending on the communities served by specific hospitals, prevalence can be much higher among medical inpatients,25 with studies finding problem drinking in as many as 28% of such patients. Although heavy drinking and the psychosocial problems that characterize alcohol dependence cause disease and interfere with disease management, remission is often difficult to achieve. As a result, although inpatient care of such patients probably does not differ from the average,6 this population is at high risk for poor health outcomes. as illustrated by factors such as suboptimal chronic disease management,7 preventable hospitalization,8 and increased mortality.9, 10 Remission involves a major behavior change that has been conceived of as a progression of stages, including precontemplation, contemplation, preparation, action, and maintenance.11 Clinically, this process encompasses an initial lack of awareness of the problem, followed by problem recognition and ambivalence about change, an increasing desire to change and concrete attempts at behavior change, and eventually long‐lasting behavioral improvements. The work described in this article was based on the broad hypothesis that acute illness and other alcohol‐related consequences will accelerate the process of change and that it might be possible to utilize this effect of acute illness to improve treatment outcomes for medically ill, alcohol‐dependent patients. If so, then measures of the change process should be correlated with measures of health status and alcohol consequences, correlations that were estimated in this study. If such measures are correlated and future research supports a causal relationship, then the link between illness and desire to change at the time of hospitalization could be exploited to help motivate changes in drinking and involvement in alcohol dependence treatment following hospital discharge.
METHODS
Study Design and Patients
Fifty clinically suspected and subsequently confirmed medical inpatients with current alcohol dependence were surveyed. Exclusion criteria were having chronic cognitive impairment, determined clinically; being nonEnglish speaking, and living in an institutional setting prior to hospitalization. Patients with suspected alcohol dependence were consecutively identified through consultation with attending internists, senior residents, and nurse case managers staffing internal medicine inpatient services of a university‐affiliated public hospital. Patients were identified by these hospitalist teams on the basis of their usual clinical care during the admission and acute care process. Thus, they were identified by characteristics such as alcohol‐related disease, self‐reported heavy drinking, abnormalities in laboratory test results such as transaminases and MCV, intoxication and withdrawal, or known history of dependence. However, the method of identification was not specifically tracked. Research staffers approached such patients to request participation in and obtain informed consent for participation in a survey of inpatients with acute medical conditions and possible drinking problems. Those who provided informed consent were interviewed by a member of the research team for DSM‐IV current alcohol dependence12 using a brief assessment instrument that covered all 7 dependence criteria. Patients who met 3 or more criteria during the past year were considered alcohol dependent and were asked to complete additional surveys. The study protocol was approved by the appropriate university institutional review board and by the director of research at the medical center.
Process of Change Variables
The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) was developed to capture certain key elements of the process of change in persons with alcohol dependence, including recognition of the drinking problem, ambivalence about change, and planning or initiating changes to alter drinking behavior.13 The SOCRATES is a 19‐item instrument consisting of 3 scales (Recognition, Ambivalence, and Taking Steps). Each scale score is the sum of several items, with all items having 5 ordinal responses ranging from strongly disagree to strongly agree. The Recognition scale is composed of 7 items (score range 735) that estimate an individual's recognition of his or her alcohol use as an important problem, desire to change, and perception of harm related to drinking. The Ambivalence scale contains 4 items (score range 420) that ask respondents if they wonder if they are alcoholic, drink too much, are hurting others, and are in control of their drinking. Degree of wondering (as opposed to knowing) about such issues is considered a reflection of uncertainty, or ambivalence, and higher scores suggest that the patient is at a more contemplative stage of change. The Taking Steps scale has 8 items (score range 840) that assess if positive change has already been initiated and the desire for help to prevent relapse.
Perceived Overall Health Status Variables
Perceived physical and mental health status were estimated using the Medical Outcome Study Short Form‐12 physical and mental subscales, continuous measures that were standardized to the 1998 U.S. adult population.14
Perceived Alcohol‐Related Adverse Consequences
Tto assess the consequences attributed to alcohol by the patient, we administered the Short Inventory of Problems.15 This is a 15‐item instrument that assesses consequences in 5 domains (physical, interpersonal, intrapersonal, impulse control, and social responsibility). Each domain is measured by a 3‐item subscale with 4 ordinal responses ranging from never (score = 0) to daily or almost daily (score = 3), so the subscale scores range from 0 to 9. The physical subscale asks subjects if their physical health has been harmed by drinking, if their physical appearance has been harmed by drinking, and if they have not eaten properly because of drinking. Given the premise that poor health would accelerate the process of change, we were particularly interested in the physical subscale, but evaluated all adverse‐consequence domains as correlates of the change variables.
Other Descriptive Variables
The admission diagnoses of each participant were recorded. Demographic factors, determined by self‐report or from the medical record, were age, sex, ethnicity (Hispanic, non‐Hispanic black, non‐Hispanic white), years of education, and health insurance. Previous 4‐week alcohol consumption was measured using alcohol timeline follow‐back methodology.16 This method defines a standard drink and, with the help of memory cues, asks the patient to estimate how much alcohol was consumed on each day. Percent drinking days (days on which any amount of alcohol was consumed) and average number of drinks per drinking day were calculated from the resulting daily drinking record.
Analysis
Because not all scales were normally distributed, we calculated Spearman correlation coefficients to estimate the association of the change variables (SOCRATES subscales) with perceived health variables (SF‐12 subscales and SIP physical subscale) and the other adverse consequence domains of the SIP. Although the study was underpowered for subset analyses, we did explore confounding by age, sex, and ethnicity when the unadjusted association between a health or adverse consequence variable with a SOCRATES subscale was statistically significant (P < .05). We also added adjustment for alcohol consumption (ie, percent drinking days and average drinks per drinking day) when these consumption measures were associated with the process‐of‐change variables. Because the distributions of the problem Recognition and Ambivalence scores were censored at their upper limits, tobit regression, a method appropriate for censored outcomes, was used to compare adjusted and unadjusted associations. The Taking Steps scores were approximately normally distributed, and ordinary least‐squares regression was used for multivariable analyses.
RESULTS
We identified 117 potential participants, accounting for 6% of total admissions (n = 1964) during the 7‐month recruitment period (late 2004 through mid‐2005). Of this total, 20 (17%) refused or withdrew prior to completing the study questionnaires, 17 (14.5%) were not eligible because of chronic cognitive impairment, 15 (12.8%) were discharged prior to being interviewed, 14 (12%) did not meet current alcohol dependence criteria (4 of whom met abuse criteria), and 1 (<1%) did not speak English. The remaining 50 subjects were included in this analysis. Characteristics of this group are listed in Table 1. They were primarily male, and socioeconomic status (assessed on the basis of education and health insurance) was low relative to the general population.17 Persons listed as having public insurance only were mainly covered by state Medicaid plans with or without Medicare. The less common diagnoses listed as other in Table 1, pertaining to no more than 2 patients, include arrhythmia, upper gastrointestinal bleeding, gout, electrolyte imbalance, hypoglycemia, diabetic ketoacidosis, diarrhea, stroke, and congestive heart failure. Measures of alcohol consumption were consistent with the clinical diagnosis of current alcohol dependence.
| Male | 40 (80%) |
| Mean age (SD) | 50 (11) |
| Ethnicity | |
| Hispanic | 8 (16%) |
| Non‐Hispanic black | 13 (26%) |
| Non‐Hispanic white | 29 (58%) |
| Mean years of education (SD) | 11.6 (2.1) |
| Health insurance | |
| Only public | 35 (70%) |
| Private | 5 (10%) |
| None | 10 (20%) |
| Mean percent drinking days (SD) | 68 (35) |
| Mean number of drinks/drinking day (SD) | 8.4 (4.9) |
| Most common admission diagnoses | |
| Liver disease | 8 (16%) |
| Pancreatitis | 7 (14%) |
| Withdrawal seizure | 7 (14%) |
| Chest pain and/or myocardial infarction | 6 (12%) |
| Drug overdose | 5 (10%) |
| Infection | 4 (8%) |
| Other | 13 (26%) |
Of the components of the change process measured, the Recognition and Ambivalence subscales tended to have high scores. Thirty percent of subjects had the highest possible score on the Recognition scale, and 16% had the highest possible score on the Ambivalence scale. The scores for taking steps to change were more evenly distributed. A description of the study variables is included in Table 2.
| Variable* | Mean (Standard Deviation), Range |
|---|---|
| |
| Process‐of‐change variables (SOCRATES) | |
| Problem recognition | 28.9 (6.2), 1035 |
| Ambivalence | 15.3 (3.8), 420 |
| Taking steps to change | 30.6 (5.9), 1440 |
| Overall health perceptions (SF‐12) | |
| Perceived physical health status | 42.5 (8.4), 2958 |
| Perceived mental health status | 39.2 (8.3), 1855 |
| Alcohol‐related consequences (SIP) | |
| Physical | 5.7 (2.8), 09 |
| Interpersonal | 5.5 (3.1), 09 |
| Intrapersonal | 5.3 (2.8), 09 |
| Impulse control | 4.0 (2.4), 09 |
| Social responsibility | 5.1 (3.0), 09 |
The unadjusted correlations of alcohol problem recognition, ambivalence, and taking steps to change drinking with each perceived health status and alcohol‐consequence variable are shown in Table 3. Problem recognition was modestly and inversely associated with overall perception of physical health as measured by the SF‐12 but was not associated with perceived mental health. All the SIP subscales had strong univariate associations with problem recognition (P < .001 for each subscale). Problem recognition was associated with both percent drinking days (r = 0.39, P = .005) and average drinks per drinking day (r = 0.34, P = .0191). Adjustment for age, sex, and ethnicity did not modify the associations of recognition with perceived health and adverse consequences. Additional adjustment for percent drinking days eliminated the significant association with overall physical health from the SF‐12 (35% reduction in the regression coefficient, adjusted P = .100). A similar reduction in the association between problem recognition and overall physical health was observed for average drinks per drinking day (36% reduction in the regression coefficient, adjusted P = .102). All SIP subscales remained strongly associated with problem recognition despite the additional adjustment for alcohol consumption measures (all adjusted P values 0.001).
| SOCRATES process‐of‐change variables | |||
|---|---|---|---|
| Recognition | Ambivalence | Taking Steps | |
| |||
| Perceived health (SF‐12) | |||
| Physical | 0.31 (0.54, 0.03) | 0.41 (0.61, 0.14) | 0.26 (0.50, 0.03) |
| Mental | 0.06 (0.33, 0.23) | 0.10 (0.19, 0.37) | 0.09 (0.19, 0.36) |
| Alcohol consequences (SIP) | |||
| Physical | 0.72 (0.55, 0.83) | 0.44 (0.18, 0.64) | 0.42 (0.16, 0.63) |
| Interpersonal | 0.69 (0.51, 0.81) | 0.62 (0.41, 0.76) | 0.38 (0.11, 0.60) |
| Intrapersonal | 0.66 (0.46, 0.79) | 0.40 (0.13, 0.61) | 0.30 (0.02, 0.53) |
| Impulse control | 0.54 (0.31, 0.71) | 0.37 (0.10, 0.59) | 0.24 (0.04, 0.49) |
| Social responsibility | 0.57 (0.34, 0.73) | 0.48 (0.22, 0.66) | 0.19 (0.10, 0.44) |
Ambivalence was associated with overall perception of physical health (P = .003) but not perceived mental health. All SIP subscales were associated with ambivalence (all P < .010). Alcohol consumption measures were not significantly associated with ambivalence (for percent drinking days, r = 0.25, P = .083; for average drinks per drinking day, r = 0.24, P = .106). Adjustment for age, sex, and ethnicity did not alter these findings.
Taking steps to change drinking behavior was not significantly associated with overall perceptions of physical and mental health. The physical (P = .002), interpersonal (P = .006), and intrapersonal (P = .034) SIP subscales were associated with taking steps to change. Alcohol consumption measures were not significantly associated with taking steps (percent drinking days, r = 0.19, P = .196; average drinks per drinking day, r = 0.24, P = .105). Adjustment for age, sex, and ethnicity, had minimal impact on the associations between taking steps and the physical, interpersonal, and intrapersonal SIP subscales.
DISCUSSION
This study evaluated the association of recognition of problem drinking, ambivalence about change, and taking steps to change with measures of perceived health status and alcohol‐related consequences. The results suggest that most medically hospitalized patients with clinically recognized alcohol dependence are highly cognizant of their drinking problem and wonder about the consequences of their drinking, and many feel they either have taken or will take steps to change their drinking behavior. Overall physical health perceptions during hospitalization were correlated with problem recognition (possibly mediated by heavy drinking) and ambivalence, but not with taking steps to change. Conversely, specific alcohol‐related physical and other consequences were often correlated with each process of change.
The SOCRATES results for this group were similar to those found in a large group of alcohol‐dependent persons participating in a large treatment trial.18 Relative to the distribution of SOCRATES scores in that group, 42% of this hospital sample would be above the median for recognition, 66% for ambivalence, and 44% for taking steps to change.19 This finding, coupled with the correlations of problem recognition and ambivalence (but not taking steps to change) with perceived physical health, suggests that medical hospitalization presents a unique opportunity for fostering change by moving ambivalent patients toward initiating change. However, additional research is needed to establish that these change processes during hospitalization predict participation after hospitalization in available treatment programs or other objective indicators of positive behavioral change.
Several limitations should be considered in interpreting our results. The participants represent clinically recognized and subsequently confirmed alcohol‐dependent patients. Results might differ for those initially detected by systematic screening, for example, by using a heavy‐drinking‐day item, as recommended by the NIH,20 or biomarkers.21 It is possible that such patients would have fewer apparent alcohol‐related consequences and may thus be less contemplative of change. In addition, our sample was recruited from a single hospital, and was primarily male and socioeconomically disadvantaged. Results may not generalize to other groups. Although we did not find any evidence that age, sex, and ethnicity altered the relationships examined in this work, the study was not adequately powered for firm conclusions about this. Finally, although the study demonstrated an association of perceived health status with readiness to change drinking, a causal relationship may not exist. Theoretically, poorer health would increase recognition, ambivalence, and intent to change, but close measurement of these variables over time would be required to establish this.
In conclusion, clinically recognized alcohol‐dependent patients with acute medical illness typically are highly cognizant of their drinking problems and often wish to change at the time of hospitalization. This is linked to perceptions of physical health and a variety of alcohol‐related consequences. The association of recognition, ambivalence, and intention to change at the time of hospitalization with postdischarge treatment participation and outcomes should be evaluated further. If these factors do predict such outcomes, intervention studies aimed at enhancing the process of change during hospitalization will be warranted.
- .Medical and Surgical Complications of Addiction. In:Graham AW,Schultz TK,Mayo‐Smith MF, et al., eds.Principles of Addiction Medicine.3rd ed.Chevy Chase, MD:American Society of Addiction Medicine;2003:1027–1052.
- ,,.Prevalence of current DSM‐IV alcohol use disorders in short‐stay, general hospital admissions, United States, 1994.Arch Intern Med.2003;163:713–719.
- ,,,,,Point prevalence of alcoholism in hospitalized patients: continuing challenges of detection, assessment, and diagnosis.Mayo Clin Proc.2001;76:460–466.
- ,,,,.The effect of patient gender on the prevalence and recognition of alcoholism on a general medicine inpatient service.J Gen Intern Med.1992;7:38–45.
- ,,,,,.Prevalence, detection, and treatment of alcoholism in hospitalized patients.JAMA.1989;261:403–407.
- ,,,,.Quality of care for acute myocardial infarction in elderly patients with alcohol‐related diagnoses.Alcohol Clin Exp Res.2006;30:70–75.
- ,,, et al.A temporal and dose‐response association between alcohol consumption and medication adherence among veterans in care.Alcohol Clin Exp Res.2005;29:1190–1197.
- ,,, et al.The roles of low literacy and social support in predicting the preventability of hospital admission.J Gen Intern Med.2006;21:140–145.
- .Mortality risks in alcoholism and effects of abstinence and addiction treatment.Psychiatr Clin North Am.1999;22:371–383.
- ,,,,.Alcohol screening results in elderly male veterans: association with health status and mortality.J Am Geriatr Soc.2004;52:1510–1517.
- ,,.Substance Abuse Treatment and the Stages of Change.New York:Guilford Press;2001.
- American Psychiatric Association.Diagnostic and Statistical Manual4th ed. (text revision).Washington, DC:American Psychiatric Association;2000.
- ,.Assessing drinkers' motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES).Psychol Addict Behav.1996;10:81–89.
- ,,,.How to Score Version 2 of the SF‐12 Health Survey (With a Supplement Documenting Version 1).Lincoln, RI:QualityMetric Inc.;2002.
- ,,.The Drinker Inventory of Consequences (DrinC): An Instrument for Assessing Adverse Consequence of Alcohol Abuse. NIAAA Project MATCH Monograph Series.Washington, DC:U.S. Government Printing Office;1995.
- ,.Timeline Follow‐back: A technique for assessing self‐reported ethanol consumption. In:Allen J,Litten R, eds.Measuring Alcohol Consumption: Psychosocial and Biological Methods.Totowa, NJ:Humana Press;1992:41–72.
- Current Population Survey, 2005 Annual Social and Economic Supplement. U.S. Census Bureau. Available at pubdb3.census.gov/macro/032005/health/h01_000.htm. Accessed January 22,2007.
- Project MATCH Research Group.Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes.J Stud Alcohol.1997;5:7–29.
- Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute of Alcohol Abuse and Alcoholism;2003:576–582.
- Helping patients who drink too much: a clinician's guide. U.S. Dept. of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism, NIH Pub. No. 05‐3769, 2005. Available at www.niaaa.nih.gov/Publications/EducationTrainingMaterials. Accessed November, 29,2006.
- ,,,.Biomarkers of heavy drinking. In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism;2003:37–53.
Alcohol dependence is commonly associated with severe medical disease1 and is common among hospitalized medical patients. A nationally representative hospital sample found current alcohol use disorders to have a prevalence of 7.4%; most of those with these disorders were alcohol dependent.2 However, depending on the communities served by specific hospitals, prevalence can be much higher among medical inpatients,25 with studies finding problem drinking in as many as 28% of such patients. Although heavy drinking and the psychosocial problems that characterize alcohol dependence cause disease and interfere with disease management, remission is often difficult to achieve. As a result, although inpatient care of such patients probably does not differ from the average,6 this population is at high risk for poor health outcomes. as illustrated by factors such as suboptimal chronic disease management,7 preventable hospitalization,8 and increased mortality.9, 10 Remission involves a major behavior change that has been conceived of as a progression of stages, including precontemplation, contemplation, preparation, action, and maintenance.11 Clinically, this process encompasses an initial lack of awareness of the problem, followed by problem recognition and ambivalence about change, an increasing desire to change and concrete attempts at behavior change, and eventually long‐lasting behavioral improvements. The work described in this article was based on the broad hypothesis that acute illness and other alcohol‐related consequences will accelerate the process of change and that it might be possible to utilize this effect of acute illness to improve treatment outcomes for medically ill, alcohol‐dependent patients. If so, then measures of the change process should be correlated with measures of health status and alcohol consequences, correlations that were estimated in this study. If such measures are correlated and future research supports a causal relationship, then the link between illness and desire to change at the time of hospitalization could be exploited to help motivate changes in drinking and involvement in alcohol dependence treatment following hospital discharge.
METHODS
Study Design and Patients
Fifty clinically suspected and subsequently confirmed medical inpatients with current alcohol dependence were surveyed. Exclusion criteria were having chronic cognitive impairment, determined clinically; being nonEnglish speaking, and living in an institutional setting prior to hospitalization. Patients with suspected alcohol dependence were consecutively identified through consultation with attending internists, senior residents, and nurse case managers staffing internal medicine inpatient services of a university‐affiliated public hospital. Patients were identified by these hospitalist teams on the basis of their usual clinical care during the admission and acute care process. Thus, they were identified by characteristics such as alcohol‐related disease, self‐reported heavy drinking, abnormalities in laboratory test results such as transaminases and MCV, intoxication and withdrawal, or known history of dependence. However, the method of identification was not specifically tracked. Research staffers approached such patients to request participation in and obtain informed consent for participation in a survey of inpatients with acute medical conditions and possible drinking problems. Those who provided informed consent were interviewed by a member of the research team for DSM‐IV current alcohol dependence12 using a brief assessment instrument that covered all 7 dependence criteria. Patients who met 3 or more criteria during the past year were considered alcohol dependent and were asked to complete additional surveys. The study protocol was approved by the appropriate university institutional review board and by the director of research at the medical center.
Process of Change Variables
The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) was developed to capture certain key elements of the process of change in persons with alcohol dependence, including recognition of the drinking problem, ambivalence about change, and planning or initiating changes to alter drinking behavior.13 The SOCRATES is a 19‐item instrument consisting of 3 scales (Recognition, Ambivalence, and Taking Steps). Each scale score is the sum of several items, with all items having 5 ordinal responses ranging from strongly disagree to strongly agree. The Recognition scale is composed of 7 items (score range 735) that estimate an individual's recognition of his or her alcohol use as an important problem, desire to change, and perception of harm related to drinking. The Ambivalence scale contains 4 items (score range 420) that ask respondents if they wonder if they are alcoholic, drink too much, are hurting others, and are in control of their drinking. Degree of wondering (as opposed to knowing) about such issues is considered a reflection of uncertainty, or ambivalence, and higher scores suggest that the patient is at a more contemplative stage of change. The Taking Steps scale has 8 items (score range 840) that assess if positive change has already been initiated and the desire for help to prevent relapse.
Perceived Overall Health Status Variables
Perceived physical and mental health status were estimated using the Medical Outcome Study Short Form‐12 physical and mental subscales, continuous measures that were standardized to the 1998 U.S. adult population.14
Perceived Alcohol‐Related Adverse Consequences
Tto assess the consequences attributed to alcohol by the patient, we administered the Short Inventory of Problems.15 This is a 15‐item instrument that assesses consequences in 5 domains (physical, interpersonal, intrapersonal, impulse control, and social responsibility). Each domain is measured by a 3‐item subscale with 4 ordinal responses ranging from never (score = 0) to daily or almost daily (score = 3), so the subscale scores range from 0 to 9. The physical subscale asks subjects if their physical health has been harmed by drinking, if their physical appearance has been harmed by drinking, and if they have not eaten properly because of drinking. Given the premise that poor health would accelerate the process of change, we were particularly interested in the physical subscale, but evaluated all adverse‐consequence domains as correlates of the change variables.
Other Descriptive Variables
The admission diagnoses of each participant were recorded. Demographic factors, determined by self‐report or from the medical record, were age, sex, ethnicity (Hispanic, non‐Hispanic black, non‐Hispanic white), years of education, and health insurance. Previous 4‐week alcohol consumption was measured using alcohol timeline follow‐back methodology.16 This method defines a standard drink and, with the help of memory cues, asks the patient to estimate how much alcohol was consumed on each day. Percent drinking days (days on which any amount of alcohol was consumed) and average number of drinks per drinking day were calculated from the resulting daily drinking record.
Analysis
Because not all scales were normally distributed, we calculated Spearman correlation coefficients to estimate the association of the change variables (SOCRATES subscales) with perceived health variables (SF‐12 subscales and SIP physical subscale) and the other adverse consequence domains of the SIP. Although the study was underpowered for subset analyses, we did explore confounding by age, sex, and ethnicity when the unadjusted association between a health or adverse consequence variable with a SOCRATES subscale was statistically significant (P < .05). We also added adjustment for alcohol consumption (ie, percent drinking days and average drinks per drinking day) when these consumption measures were associated with the process‐of‐change variables. Because the distributions of the problem Recognition and Ambivalence scores were censored at their upper limits, tobit regression, a method appropriate for censored outcomes, was used to compare adjusted and unadjusted associations. The Taking Steps scores were approximately normally distributed, and ordinary least‐squares regression was used for multivariable analyses.
RESULTS
We identified 117 potential participants, accounting for 6% of total admissions (n = 1964) during the 7‐month recruitment period (late 2004 through mid‐2005). Of this total, 20 (17%) refused or withdrew prior to completing the study questionnaires, 17 (14.5%) were not eligible because of chronic cognitive impairment, 15 (12.8%) were discharged prior to being interviewed, 14 (12%) did not meet current alcohol dependence criteria (4 of whom met abuse criteria), and 1 (<1%) did not speak English. The remaining 50 subjects were included in this analysis. Characteristics of this group are listed in Table 1. They were primarily male, and socioeconomic status (assessed on the basis of education and health insurance) was low relative to the general population.17 Persons listed as having public insurance only were mainly covered by state Medicaid plans with or without Medicare. The less common diagnoses listed as other in Table 1, pertaining to no more than 2 patients, include arrhythmia, upper gastrointestinal bleeding, gout, electrolyte imbalance, hypoglycemia, diabetic ketoacidosis, diarrhea, stroke, and congestive heart failure. Measures of alcohol consumption were consistent with the clinical diagnosis of current alcohol dependence.
| Male | 40 (80%) |
| Mean age (SD) | 50 (11) |
| Ethnicity | |
| Hispanic | 8 (16%) |
| Non‐Hispanic black | 13 (26%) |
| Non‐Hispanic white | 29 (58%) |
| Mean years of education (SD) | 11.6 (2.1) |
| Health insurance | |
| Only public | 35 (70%) |
| Private | 5 (10%) |
| None | 10 (20%) |
| Mean percent drinking days (SD) | 68 (35) |
| Mean number of drinks/drinking day (SD) | 8.4 (4.9) |
| Most common admission diagnoses | |
| Liver disease | 8 (16%) |
| Pancreatitis | 7 (14%) |
| Withdrawal seizure | 7 (14%) |
| Chest pain and/or myocardial infarction | 6 (12%) |
| Drug overdose | 5 (10%) |
| Infection | 4 (8%) |
| Other | 13 (26%) |
Of the components of the change process measured, the Recognition and Ambivalence subscales tended to have high scores. Thirty percent of subjects had the highest possible score on the Recognition scale, and 16% had the highest possible score on the Ambivalence scale. The scores for taking steps to change were more evenly distributed. A description of the study variables is included in Table 2.
| Variable* | Mean (Standard Deviation), Range |
|---|---|
| |
| Process‐of‐change variables (SOCRATES) | |
| Problem recognition | 28.9 (6.2), 1035 |
| Ambivalence | 15.3 (3.8), 420 |
| Taking steps to change | 30.6 (5.9), 1440 |
| Overall health perceptions (SF‐12) | |
| Perceived physical health status | 42.5 (8.4), 2958 |
| Perceived mental health status | 39.2 (8.3), 1855 |
| Alcohol‐related consequences (SIP) | |
| Physical | 5.7 (2.8), 09 |
| Interpersonal | 5.5 (3.1), 09 |
| Intrapersonal | 5.3 (2.8), 09 |
| Impulse control | 4.0 (2.4), 09 |
| Social responsibility | 5.1 (3.0), 09 |
The unadjusted correlations of alcohol problem recognition, ambivalence, and taking steps to change drinking with each perceived health status and alcohol‐consequence variable are shown in Table 3. Problem recognition was modestly and inversely associated with overall perception of physical health as measured by the SF‐12 but was not associated with perceived mental health. All the SIP subscales had strong univariate associations with problem recognition (P < .001 for each subscale). Problem recognition was associated with both percent drinking days (r = 0.39, P = .005) and average drinks per drinking day (r = 0.34, P = .0191). Adjustment for age, sex, and ethnicity did not modify the associations of recognition with perceived health and adverse consequences. Additional adjustment for percent drinking days eliminated the significant association with overall physical health from the SF‐12 (35% reduction in the regression coefficient, adjusted P = .100). A similar reduction in the association between problem recognition and overall physical health was observed for average drinks per drinking day (36% reduction in the regression coefficient, adjusted P = .102). All SIP subscales remained strongly associated with problem recognition despite the additional adjustment for alcohol consumption measures (all adjusted P values 0.001).
| SOCRATES process‐of‐change variables | |||
|---|---|---|---|
| Recognition | Ambivalence | Taking Steps | |
| |||
| Perceived health (SF‐12) | |||
| Physical | 0.31 (0.54, 0.03) | 0.41 (0.61, 0.14) | 0.26 (0.50, 0.03) |
| Mental | 0.06 (0.33, 0.23) | 0.10 (0.19, 0.37) | 0.09 (0.19, 0.36) |
| Alcohol consequences (SIP) | |||
| Physical | 0.72 (0.55, 0.83) | 0.44 (0.18, 0.64) | 0.42 (0.16, 0.63) |
| Interpersonal | 0.69 (0.51, 0.81) | 0.62 (0.41, 0.76) | 0.38 (0.11, 0.60) |
| Intrapersonal | 0.66 (0.46, 0.79) | 0.40 (0.13, 0.61) | 0.30 (0.02, 0.53) |
| Impulse control | 0.54 (0.31, 0.71) | 0.37 (0.10, 0.59) | 0.24 (0.04, 0.49) |
| Social responsibility | 0.57 (0.34, 0.73) | 0.48 (0.22, 0.66) | 0.19 (0.10, 0.44) |
Ambivalence was associated with overall perception of physical health (P = .003) but not perceived mental health. All SIP subscales were associated with ambivalence (all P < .010). Alcohol consumption measures were not significantly associated with ambivalence (for percent drinking days, r = 0.25, P = .083; for average drinks per drinking day, r = 0.24, P = .106). Adjustment for age, sex, and ethnicity did not alter these findings.
Taking steps to change drinking behavior was not significantly associated with overall perceptions of physical and mental health. The physical (P = .002), interpersonal (P = .006), and intrapersonal (P = .034) SIP subscales were associated with taking steps to change. Alcohol consumption measures were not significantly associated with taking steps (percent drinking days, r = 0.19, P = .196; average drinks per drinking day, r = 0.24, P = .105). Adjustment for age, sex, and ethnicity, had minimal impact on the associations between taking steps and the physical, interpersonal, and intrapersonal SIP subscales.
DISCUSSION
This study evaluated the association of recognition of problem drinking, ambivalence about change, and taking steps to change with measures of perceived health status and alcohol‐related consequences. The results suggest that most medically hospitalized patients with clinically recognized alcohol dependence are highly cognizant of their drinking problem and wonder about the consequences of their drinking, and many feel they either have taken or will take steps to change their drinking behavior. Overall physical health perceptions during hospitalization were correlated with problem recognition (possibly mediated by heavy drinking) and ambivalence, but not with taking steps to change. Conversely, specific alcohol‐related physical and other consequences were often correlated with each process of change.
The SOCRATES results for this group were similar to those found in a large group of alcohol‐dependent persons participating in a large treatment trial.18 Relative to the distribution of SOCRATES scores in that group, 42% of this hospital sample would be above the median for recognition, 66% for ambivalence, and 44% for taking steps to change.19 This finding, coupled with the correlations of problem recognition and ambivalence (but not taking steps to change) with perceived physical health, suggests that medical hospitalization presents a unique opportunity for fostering change by moving ambivalent patients toward initiating change. However, additional research is needed to establish that these change processes during hospitalization predict participation after hospitalization in available treatment programs or other objective indicators of positive behavioral change.
Several limitations should be considered in interpreting our results. The participants represent clinically recognized and subsequently confirmed alcohol‐dependent patients. Results might differ for those initially detected by systematic screening, for example, by using a heavy‐drinking‐day item, as recommended by the NIH,20 or biomarkers.21 It is possible that such patients would have fewer apparent alcohol‐related consequences and may thus be less contemplative of change. In addition, our sample was recruited from a single hospital, and was primarily male and socioeconomically disadvantaged. Results may not generalize to other groups. Although we did not find any evidence that age, sex, and ethnicity altered the relationships examined in this work, the study was not adequately powered for firm conclusions about this. Finally, although the study demonstrated an association of perceived health status with readiness to change drinking, a causal relationship may not exist. Theoretically, poorer health would increase recognition, ambivalence, and intent to change, but close measurement of these variables over time would be required to establish this.
In conclusion, clinically recognized alcohol‐dependent patients with acute medical illness typically are highly cognizant of their drinking problems and often wish to change at the time of hospitalization. This is linked to perceptions of physical health and a variety of alcohol‐related consequences. The association of recognition, ambivalence, and intention to change at the time of hospitalization with postdischarge treatment participation and outcomes should be evaluated further. If these factors do predict such outcomes, intervention studies aimed at enhancing the process of change during hospitalization will be warranted.
Alcohol dependence is commonly associated with severe medical disease1 and is common among hospitalized medical patients. A nationally representative hospital sample found current alcohol use disorders to have a prevalence of 7.4%; most of those with these disorders were alcohol dependent.2 However, depending on the communities served by specific hospitals, prevalence can be much higher among medical inpatients,25 with studies finding problem drinking in as many as 28% of such patients. Although heavy drinking and the psychosocial problems that characterize alcohol dependence cause disease and interfere with disease management, remission is often difficult to achieve. As a result, although inpatient care of such patients probably does not differ from the average,6 this population is at high risk for poor health outcomes. as illustrated by factors such as suboptimal chronic disease management,7 preventable hospitalization,8 and increased mortality.9, 10 Remission involves a major behavior change that has been conceived of as a progression of stages, including precontemplation, contemplation, preparation, action, and maintenance.11 Clinically, this process encompasses an initial lack of awareness of the problem, followed by problem recognition and ambivalence about change, an increasing desire to change and concrete attempts at behavior change, and eventually long‐lasting behavioral improvements. The work described in this article was based on the broad hypothesis that acute illness and other alcohol‐related consequences will accelerate the process of change and that it might be possible to utilize this effect of acute illness to improve treatment outcomes for medically ill, alcohol‐dependent patients. If so, then measures of the change process should be correlated with measures of health status and alcohol consequences, correlations that were estimated in this study. If such measures are correlated and future research supports a causal relationship, then the link between illness and desire to change at the time of hospitalization could be exploited to help motivate changes in drinking and involvement in alcohol dependence treatment following hospital discharge.
METHODS
Study Design and Patients
Fifty clinically suspected and subsequently confirmed medical inpatients with current alcohol dependence were surveyed. Exclusion criteria were having chronic cognitive impairment, determined clinically; being nonEnglish speaking, and living in an institutional setting prior to hospitalization. Patients with suspected alcohol dependence were consecutively identified through consultation with attending internists, senior residents, and nurse case managers staffing internal medicine inpatient services of a university‐affiliated public hospital. Patients were identified by these hospitalist teams on the basis of their usual clinical care during the admission and acute care process. Thus, they were identified by characteristics such as alcohol‐related disease, self‐reported heavy drinking, abnormalities in laboratory test results such as transaminases and MCV, intoxication and withdrawal, or known history of dependence. However, the method of identification was not specifically tracked. Research staffers approached such patients to request participation in and obtain informed consent for participation in a survey of inpatients with acute medical conditions and possible drinking problems. Those who provided informed consent were interviewed by a member of the research team for DSM‐IV current alcohol dependence12 using a brief assessment instrument that covered all 7 dependence criteria. Patients who met 3 or more criteria during the past year were considered alcohol dependent and were asked to complete additional surveys. The study protocol was approved by the appropriate university institutional review board and by the director of research at the medical center.
Process of Change Variables
The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) was developed to capture certain key elements of the process of change in persons with alcohol dependence, including recognition of the drinking problem, ambivalence about change, and planning or initiating changes to alter drinking behavior.13 The SOCRATES is a 19‐item instrument consisting of 3 scales (Recognition, Ambivalence, and Taking Steps). Each scale score is the sum of several items, with all items having 5 ordinal responses ranging from strongly disagree to strongly agree. The Recognition scale is composed of 7 items (score range 735) that estimate an individual's recognition of his or her alcohol use as an important problem, desire to change, and perception of harm related to drinking. The Ambivalence scale contains 4 items (score range 420) that ask respondents if they wonder if they are alcoholic, drink too much, are hurting others, and are in control of their drinking. Degree of wondering (as opposed to knowing) about such issues is considered a reflection of uncertainty, or ambivalence, and higher scores suggest that the patient is at a more contemplative stage of change. The Taking Steps scale has 8 items (score range 840) that assess if positive change has already been initiated and the desire for help to prevent relapse.
Perceived Overall Health Status Variables
Perceived physical and mental health status were estimated using the Medical Outcome Study Short Form‐12 physical and mental subscales, continuous measures that were standardized to the 1998 U.S. adult population.14
Perceived Alcohol‐Related Adverse Consequences
Tto assess the consequences attributed to alcohol by the patient, we administered the Short Inventory of Problems.15 This is a 15‐item instrument that assesses consequences in 5 domains (physical, interpersonal, intrapersonal, impulse control, and social responsibility). Each domain is measured by a 3‐item subscale with 4 ordinal responses ranging from never (score = 0) to daily or almost daily (score = 3), so the subscale scores range from 0 to 9. The physical subscale asks subjects if their physical health has been harmed by drinking, if their physical appearance has been harmed by drinking, and if they have not eaten properly because of drinking. Given the premise that poor health would accelerate the process of change, we were particularly interested in the physical subscale, but evaluated all adverse‐consequence domains as correlates of the change variables.
Other Descriptive Variables
The admission diagnoses of each participant were recorded. Demographic factors, determined by self‐report or from the medical record, were age, sex, ethnicity (Hispanic, non‐Hispanic black, non‐Hispanic white), years of education, and health insurance. Previous 4‐week alcohol consumption was measured using alcohol timeline follow‐back methodology.16 This method defines a standard drink and, with the help of memory cues, asks the patient to estimate how much alcohol was consumed on each day. Percent drinking days (days on which any amount of alcohol was consumed) and average number of drinks per drinking day were calculated from the resulting daily drinking record.
Analysis
Because not all scales were normally distributed, we calculated Spearman correlation coefficients to estimate the association of the change variables (SOCRATES subscales) with perceived health variables (SF‐12 subscales and SIP physical subscale) and the other adverse consequence domains of the SIP. Although the study was underpowered for subset analyses, we did explore confounding by age, sex, and ethnicity when the unadjusted association between a health or adverse consequence variable with a SOCRATES subscale was statistically significant (P < .05). We also added adjustment for alcohol consumption (ie, percent drinking days and average drinks per drinking day) when these consumption measures were associated with the process‐of‐change variables. Because the distributions of the problem Recognition and Ambivalence scores were censored at their upper limits, tobit regression, a method appropriate for censored outcomes, was used to compare adjusted and unadjusted associations. The Taking Steps scores were approximately normally distributed, and ordinary least‐squares regression was used for multivariable analyses.
RESULTS
We identified 117 potential participants, accounting for 6% of total admissions (n = 1964) during the 7‐month recruitment period (late 2004 through mid‐2005). Of this total, 20 (17%) refused or withdrew prior to completing the study questionnaires, 17 (14.5%) were not eligible because of chronic cognitive impairment, 15 (12.8%) were discharged prior to being interviewed, 14 (12%) did not meet current alcohol dependence criteria (4 of whom met abuse criteria), and 1 (<1%) did not speak English. The remaining 50 subjects were included in this analysis. Characteristics of this group are listed in Table 1. They were primarily male, and socioeconomic status (assessed on the basis of education and health insurance) was low relative to the general population.17 Persons listed as having public insurance only were mainly covered by state Medicaid plans with or without Medicare. The less common diagnoses listed as other in Table 1, pertaining to no more than 2 patients, include arrhythmia, upper gastrointestinal bleeding, gout, electrolyte imbalance, hypoglycemia, diabetic ketoacidosis, diarrhea, stroke, and congestive heart failure. Measures of alcohol consumption were consistent with the clinical diagnosis of current alcohol dependence.
| Male | 40 (80%) |
| Mean age (SD) | 50 (11) |
| Ethnicity | |
| Hispanic | 8 (16%) |
| Non‐Hispanic black | 13 (26%) |
| Non‐Hispanic white | 29 (58%) |
| Mean years of education (SD) | 11.6 (2.1) |
| Health insurance | |
| Only public | 35 (70%) |
| Private | 5 (10%) |
| None | 10 (20%) |
| Mean percent drinking days (SD) | 68 (35) |
| Mean number of drinks/drinking day (SD) | 8.4 (4.9) |
| Most common admission diagnoses | |
| Liver disease | 8 (16%) |
| Pancreatitis | 7 (14%) |
| Withdrawal seizure | 7 (14%) |
| Chest pain and/or myocardial infarction | 6 (12%) |
| Drug overdose | 5 (10%) |
| Infection | 4 (8%) |
| Other | 13 (26%) |
Of the components of the change process measured, the Recognition and Ambivalence subscales tended to have high scores. Thirty percent of subjects had the highest possible score on the Recognition scale, and 16% had the highest possible score on the Ambivalence scale. The scores for taking steps to change were more evenly distributed. A description of the study variables is included in Table 2.
| Variable* | Mean (Standard Deviation), Range |
|---|---|
| |
| Process‐of‐change variables (SOCRATES) | |
| Problem recognition | 28.9 (6.2), 1035 |
| Ambivalence | 15.3 (3.8), 420 |
| Taking steps to change | 30.6 (5.9), 1440 |
| Overall health perceptions (SF‐12) | |
| Perceived physical health status | 42.5 (8.4), 2958 |
| Perceived mental health status | 39.2 (8.3), 1855 |
| Alcohol‐related consequences (SIP) | |
| Physical | 5.7 (2.8), 09 |
| Interpersonal | 5.5 (3.1), 09 |
| Intrapersonal | 5.3 (2.8), 09 |
| Impulse control | 4.0 (2.4), 09 |
| Social responsibility | 5.1 (3.0), 09 |
The unadjusted correlations of alcohol problem recognition, ambivalence, and taking steps to change drinking with each perceived health status and alcohol‐consequence variable are shown in Table 3. Problem recognition was modestly and inversely associated with overall perception of physical health as measured by the SF‐12 but was not associated with perceived mental health. All the SIP subscales had strong univariate associations with problem recognition (P < .001 for each subscale). Problem recognition was associated with both percent drinking days (r = 0.39, P = .005) and average drinks per drinking day (r = 0.34, P = .0191). Adjustment for age, sex, and ethnicity did not modify the associations of recognition with perceived health and adverse consequences. Additional adjustment for percent drinking days eliminated the significant association with overall physical health from the SF‐12 (35% reduction in the regression coefficient, adjusted P = .100). A similar reduction in the association between problem recognition and overall physical health was observed for average drinks per drinking day (36% reduction in the regression coefficient, adjusted P = .102). All SIP subscales remained strongly associated with problem recognition despite the additional adjustment for alcohol consumption measures (all adjusted P values 0.001).
| SOCRATES process‐of‐change variables | |||
|---|---|---|---|
| Recognition | Ambivalence | Taking Steps | |
| |||
| Perceived health (SF‐12) | |||
| Physical | 0.31 (0.54, 0.03) | 0.41 (0.61, 0.14) | 0.26 (0.50, 0.03) |
| Mental | 0.06 (0.33, 0.23) | 0.10 (0.19, 0.37) | 0.09 (0.19, 0.36) |
| Alcohol consequences (SIP) | |||
| Physical | 0.72 (0.55, 0.83) | 0.44 (0.18, 0.64) | 0.42 (0.16, 0.63) |
| Interpersonal | 0.69 (0.51, 0.81) | 0.62 (0.41, 0.76) | 0.38 (0.11, 0.60) |
| Intrapersonal | 0.66 (0.46, 0.79) | 0.40 (0.13, 0.61) | 0.30 (0.02, 0.53) |
| Impulse control | 0.54 (0.31, 0.71) | 0.37 (0.10, 0.59) | 0.24 (0.04, 0.49) |
| Social responsibility | 0.57 (0.34, 0.73) | 0.48 (0.22, 0.66) | 0.19 (0.10, 0.44) |
Ambivalence was associated with overall perception of physical health (P = .003) but not perceived mental health. All SIP subscales were associated with ambivalence (all P < .010). Alcohol consumption measures were not significantly associated with ambivalence (for percent drinking days, r = 0.25, P = .083; for average drinks per drinking day, r = 0.24, P = .106). Adjustment for age, sex, and ethnicity did not alter these findings.
Taking steps to change drinking behavior was not significantly associated with overall perceptions of physical and mental health. The physical (P = .002), interpersonal (P = .006), and intrapersonal (P = .034) SIP subscales were associated with taking steps to change. Alcohol consumption measures were not significantly associated with taking steps (percent drinking days, r = 0.19, P = .196; average drinks per drinking day, r = 0.24, P = .105). Adjustment for age, sex, and ethnicity, had minimal impact on the associations between taking steps and the physical, interpersonal, and intrapersonal SIP subscales.
DISCUSSION
This study evaluated the association of recognition of problem drinking, ambivalence about change, and taking steps to change with measures of perceived health status and alcohol‐related consequences. The results suggest that most medically hospitalized patients with clinically recognized alcohol dependence are highly cognizant of their drinking problem and wonder about the consequences of their drinking, and many feel they either have taken or will take steps to change their drinking behavior. Overall physical health perceptions during hospitalization were correlated with problem recognition (possibly mediated by heavy drinking) and ambivalence, but not with taking steps to change. Conversely, specific alcohol‐related physical and other consequences were often correlated with each process of change.
The SOCRATES results for this group were similar to those found in a large group of alcohol‐dependent persons participating in a large treatment trial.18 Relative to the distribution of SOCRATES scores in that group, 42% of this hospital sample would be above the median for recognition, 66% for ambivalence, and 44% for taking steps to change.19 This finding, coupled with the correlations of problem recognition and ambivalence (but not taking steps to change) with perceived physical health, suggests that medical hospitalization presents a unique opportunity for fostering change by moving ambivalent patients toward initiating change. However, additional research is needed to establish that these change processes during hospitalization predict participation after hospitalization in available treatment programs or other objective indicators of positive behavioral change.
Several limitations should be considered in interpreting our results. The participants represent clinically recognized and subsequently confirmed alcohol‐dependent patients. Results might differ for those initially detected by systematic screening, for example, by using a heavy‐drinking‐day item, as recommended by the NIH,20 or biomarkers.21 It is possible that such patients would have fewer apparent alcohol‐related consequences and may thus be less contemplative of change. In addition, our sample was recruited from a single hospital, and was primarily male and socioeconomically disadvantaged. Results may not generalize to other groups. Although we did not find any evidence that age, sex, and ethnicity altered the relationships examined in this work, the study was not adequately powered for firm conclusions about this. Finally, although the study demonstrated an association of perceived health status with readiness to change drinking, a causal relationship may not exist. Theoretically, poorer health would increase recognition, ambivalence, and intent to change, but close measurement of these variables over time would be required to establish this.
In conclusion, clinically recognized alcohol‐dependent patients with acute medical illness typically are highly cognizant of their drinking problems and often wish to change at the time of hospitalization. This is linked to perceptions of physical health and a variety of alcohol‐related consequences. The association of recognition, ambivalence, and intention to change at the time of hospitalization with postdischarge treatment participation and outcomes should be evaluated further. If these factors do predict such outcomes, intervention studies aimed at enhancing the process of change during hospitalization will be warranted.
- .Medical and Surgical Complications of Addiction. In:Graham AW,Schultz TK,Mayo‐Smith MF, et al., eds.Principles of Addiction Medicine.3rd ed.Chevy Chase, MD:American Society of Addiction Medicine;2003:1027–1052.
- ,,.Prevalence of current DSM‐IV alcohol use disorders in short‐stay, general hospital admissions, United States, 1994.Arch Intern Med.2003;163:713–719.
- ,,,,,Point prevalence of alcoholism in hospitalized patients: continuing challenges of detection, assessment, and diagnosis.Mayo Clin Proc.2001;76:460–466.
- ,,,,.The effect of patient gender on the prevalence and recognition of alcoholism on a general medicine inpatient service.J Gen Intern Med.1992;7:38–45.
- ,,,,,.Prevalence, detection, and treatment of alcoholism in hospitalized patients.JAMA.1989;261:403–407.
- ,,,,.Quality of care for acute myocardial infarction in elderly patients with alcohol‐related diagnoses.Alcohol Clin Exp Res.2006;30:70–75.
- ,,, et al.A temporal and dose‐response association between alcohol consumption and medication adherence among veterans in care.Alcohol Clin Exp Res.2005;29:1190–1197.
- ,,, et al.The roles of low literacy and social support in predicting the preventability of hospital admission.J Gen Intern Med.2006;21:140–145.
- .Mortality risks in alcoholism and effects of abstinence and addiction treatment.Psychiatr Clin North Am.1999;22:371–383.
- ,,,,.Alcohol screening results in elderly male veterans: association with health status and mortality.J Am Geriatr Soc.2004;52:1510–1517.
- ,,.Substance Abuse Treatment and the Stages of Change.New York:Guilford Press;2001.
- American Psychiatric Association.Diagnostic and Statistical Manual4th ed. (text revision).Washington, DC:American Psychiatric Association;2000.
- ,.Assessing drinkers' motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES).Psychol Addict Behav.1996;10:81–89.
- ,,,.How to Score Version 2 of the SF‐12 Health Survey (With a Supplement Documenting Version 1).Lincoln, RI:QualityMetric Inc.;2002.
- ,,.The Drinker Inventory of Consequences (DrinC): An Instrument for Assessing Adverse Consequence of Alcohol Abuse. NIAAA Project MATCH Monograph Series.Washington, DC:U.S. Government Printing Office;1995.
- ,.Timeline Follow‐back: A technique for assessing self‐reported ethanol consumption. In:Allen J,Litten R, eds.Measuring Alcohol Consumption: Psychosocial and Biological Methods.Totowa, NJ:Humana Press;1992:41–72.
- Current Population Survey, 2005 Annual Social and Economic Supplement. U.S. Census Bureau. Available at pubdb3.census.gov/macro/032005/health/h01_000.htm. Accessed January 22,2007.
- Project MATCH Research Group.Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes.J Stud Alcohol.1997;5:7–29.
- Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute of Alcohol Abuse and Alcoholism;2003:576–582.
- Helping patients who drink too much: a clinician's guide. U.S. Dept. of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism, NIH Pub. No. 05‐3769, 2005. Available at www.niaaa.nih.gov/Publications/EducationTrainingMaterials. Accessed November, 29,2006.
- ,,,.Biomarkers of heavy drinking. In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism;2003:37–53.
- .Medical and Surgical Complications of Addiction. In:Graham AW,Schultz TK,Mayo‐Smith MF, et al., eds.Principles of Addiction Medicine.3rd ed.Chevy Chase, MD:American Society of Addiction Medicine;2003:1027–1052.
- ,,.Prevalence of current DSM‐IV alcohol use disorders in short‐stay, general hospital admissions, United States, 1994.Arch Intern Med.2003;163:713–719.
- ,,,,,Point prevalence of alcoholism in hospitalized patients: continuing challenges of detection, assessment, and diagnosis.Mayo Clin Proc.2001;76:460–466.
- ,,,,.The effect of patient gender on the prevalence and recognition of alcoholism on a general medicine inpatient service.J Gen Intern Med.1992;7:38–45.
- ,,,,,.Prevalence, detection, and treatment of alcoholism in hospitalized patients.JAMA.1989;261:403–407.
- ,,,,.Quality of care for acute myocardial infarction in elderly patients with alcohol‐related diagnoses.Alcohol Clin Exp Res.2006;30:70–75.
- ,,, et al.A temporal and dose‐response association between alcohol consumption and medication adherence among veterans in care.Alcohol Clin Exp Res.2005;29:1190–1197.
- ,,, et al.The roles of low literacy and social support in predicting the preventability of hospital admission.J Gen Intern Med.2006;21:140–145.
- .Mortality risks in alcoholism and effects of abstinence and addiction treatment.Psychiatr Clin North Am.1999;22:371–383.
- ,,,,.Alcohol screening results in elderly male veterans: association with health status and mortality.J Am Geriatr Soc.2004;52:1510–1517.
- ,,.Substance Abuse Treatment and the Stages of Change.New York:Guilford Press;2001.
- American Psychiatric Association.Diagnostic and Statistical Manual4th ed. (text revision).Washington, DC:American Psychiatric Association;2000.
- ,.Assessing drinkers' motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES).Psychol Addict Behav.1996;10:81–89.
- ,,,.How to Score Version 2 of the SF‐12 Health Survey (With a Supplement Documenting Version 1).Lincoln, RI:QualityMetric Inc.;2002.
- ,,.The Drinker Inventory of Consequences (DrinC): An Instrument for Assessing Adverse Consequence of Alcohol Abuse. NIAAA Project MATCH Monograph Series.Washington, DC:U.S. Government Printing Office;1995.
- ,.Timeline Follow‐back: A technique for assessing self‐reported ethanol consumption. In:Allen J,Litten R, eds.Measuring Alcohol Consumption: Psychosocial and Biological Methods.Totowa, NJ:Humana Press;1992:41–72.
- Current Population Survey, 2005 Annual Social and Economic Supplement. U.S. Census Bureau. Available at pubdb3.census.gov/macro/032005/health/h01_000.htm. Accessed January 22,2007.
- Project MATCH Research Group.Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes.J Stud Alcohol.1997;5:7–29.
- Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute of Alcohol Abuse and Alcoholism;2003:576–582.
- Helping patients who drink too much: a clinician's guide. U.S. Dept. of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism, NIH Pub. No. 05‐3769, 2005. Available at www.niaaa.nih.gov/Publications/EducationTrainingMaterials. Accessed November, 29,2006.
- ,,,.Biomarkers of heavy drinking. In:Allen J,Wilson V, eds.Assessing Alcohol Problems. A Guide for Clinicians and Researchers.2nd ed.Bethesda, MD:U.S. Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism;2003:37–53.
Copyright © 2007 Society of Hospital Medicine
Identification of Inpatient DNR Status / Sehgal and Wachter
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
Copyright © 2007 Society of Hospital Medicine
Common Myths in Caring for Patients with Terminal Illness
Shortcomings in the quality of care of hospitalized patients at the end of life, especially in the final days, are well documented.1, 2 Recent studies have highlighted inadequate pain and symptom control for hospitalized terminally ill patients,24 poor communication about treatment preferences,57 and limited or delayed referral for hospice care.810 Efforts to improve the quality of end‐of‐life care have been diverse, including increased educational programs,1113 development of palliative care units in hospitals,14, 15 and greater exposure to palliative care for physicians during residency training.16 Despite these efforts, studies assessing the attitudes and knowledge of physicians about hospice and palliative care continue to show deficits in knowledge about managing pain17, 18 as well as hospice policies and services.9
Among the interventions aimed at improving hospital care, the hospitalist movement has emerged as a model of care for improving the quality and cost efficiency of hospital care.1922 Because hospitalists spend substantial time on inpatient services,23 they are often involved in the care of patients with terminal illness, with potential to improve the quality of care that these patients receive while hospitalized. However, little is known about what specific knowledge and perspectives hospitalists and residents have about the care of patients with terminal illness. Although many studies have been conducted among physicians in private practice,9, 10, 2426 they have not focused on the knowledge, reported practices, and attitudes of hospitalists and residents concerning key aspects of end‐of‐life care and hospice. Such information can help to identify potential areas for improving knowledge and addressing common barriers highlighted in linking hospital and posthospital hospice care.
METHODS
Study Design and Sample
During 2006 we surveyed hospitalists and medical residents who were on their oncology rotation at a large academic medical center that did not have a hospital‐based palliative care unit in order to examine their knowledge, attitudes, and practices regarding terminally ill patients and hospice referrals. Hospitalists (n = 23) and medical residents (n = 29) made up a convenience sample of 52 physicians. The medical residents were completing their oncology rotation during the spring of 2006. The Institutional Review Board at Yale University School of Medicine approved the research protocol and verbal consent procedures.
Survey
The brief survey instrument (see Appendix) assessed physicians' knowledge and attitudes about and practices in caring for patients with terminal illness. The survey was adapted from previously published instruments8, 24 that have been shown24 to have good test‐retest reliability and construct validity. The survey contained 5 items pertaining to clinical knowledge about palliative care practices, including common symptoms and drug indications, doses, and side effects.27 An additional 2 items pertained to respondents' knowledge about nonclinical issues concerning eligibility rules for hospice,8 such as how a patient becomes eligible for hospice and whether Medicare benefits can be revoked or reinstated after hospice is elected. The survey also included 10 statements24 assessing physician attitudes about caring for patients with terminal illness. Responses, provided using a 5‐point Likert scale, were collapsed for reporting into a 3‐point scale of agree, neutral, and disagree. The instrument also included an open‐ended question asking physicians to specify what from their perspective was needed to ensure timely referral for hospice and palliative care.
Data Analysis
We used standard frequency analysis to describe the distribution of responses to the survey items. Based on an analysis of common erroneous answers to clinical knowledge questions, we identified several common myths prevalent among hospitalists and medicine residents. We also examined whether knowledge, reported practices, and attitudes differed significantly between the hospitalist and the resident samples using ANOVA or chi‐square statistics as appropriate. We used content analysis to summarize the open‐ended responses about potential ways to overcome what respondents perceived was underutilization of hospice.
RESULTS
Overview
The response rate for the survey was 85.2%. Almost half of the respondents (44.2%) were hospitalists (Table 1). The remaining respondents included first‐year (n = 9) and second‐ or third‐year (n = 16) residents or fellows (n = 4). Approximately 54% of the 52 respondents were female, and the majority (83%) had graduated from medical school between 2000 and 2005. Several common myths were apparent and pertained to essential areas of treating patients with terminal illness: pain control, symptom control, and eligibility for hospice (Table 2). Respondents generally had strong beliefs about caring for patients with terminal illness, and most agreed that many patients who would benefit from hospice either do not receive hospice or receive it only late in the course of their illness (Table 3).
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 28 | 53.9% |
| Male | 24 | 46.1% |
| Years since graduation from medical school | ||
| 1‐2 Years | 26 | 56.5% |
| 3‐5 Years | 12 | 26.1% |
| >5 Years | 8 | 17.4% |
| Missing | 6 | |
| Physician type | ||
| Hospitalist | 23 | 44.2% |
| First‐year resident | 9 | 17.3% |
| Second‐ or third‐year resident | 16 | 30.8% |
| Fellow | 4 | 7.7% |
| Questions about hospice and palliative care practices | Response (%) |
|---|---|
| |
| The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is: | |
| Common (1 in 10 patients) | 17.3 |
| Uncommon (1 in 100 patients) | 48.1 |
| Very rare (fewer than 1 in 1000 patients) | 34.6 |
| When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates: | |
| Opioid tolerance | 69.2 |
| Increasing pathology of the cancer | 26.9 |
| Patient noncompliance | 0.0 |
| New onset of a different opioid‐resisting pain | 3.9 |
| In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to of IV morphine | |
| 1 mg | 4.0 |
| 5 mg | 40.0 |
| 10 mg | 56.0 |
| 20 mg | 0.0 |
| The 2 classes of drugs most commonly recommended for treating terminal dyspnea are: | |
| Beta‐blockers and Lasix | 7.7 |
| Opioids and benzodiazepines | 82.7 |
| Beta‐blockers and corticosteroids | 9.6 |
| Beta‐blockers and Singulair (montelukast) | 0.0 |
| A hospice patient whose agitation is primarily from anxiety should be treated with: | |
| Chlorpromazine (thorazine) | 0.0 |
| Haloperidol | 21.6 |
| Lorazepam (Ativan) | 76.4 |
| Morphine | 2.0 |
| Questions about eligibility for hospice care | Response (%) |
| Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in: | |
| 2 Weeks | 5.8 |
| 6 Weeks | 9.6 |
| 2 Months | 9.6 |
| 6 Months | 69.2 |
| Other | 1.9 |
| Don't know | 3.8 |
| To the best of your knowledge, patients become eligible for home hospice care when they are expected to die in: | |
| 2 Weeks | 0.0 |
| 6 Weeks | 5.8 |
| 2 Months | 7.7 |
| 6 Months | 73.1 |
| Other | 0.0 |
| Don't know | 13.4 |
| Beliefs | Disagree (%) | Neutral (%) | Agree (%) |
|---|---|---|---|
| Most patients want me to tell them their life‐expectancy. | 0.0 | 17.4 | 82.6 |
| Generally, family caregivers want me to tell them the patient's life expectancy. | 4.4 | 8.7 | 86.9 |
| Telling the patient and family members that the patient's illness is incurable is difficult for me. | 23.0 | 13.5 | 63.5 |
| I think it is essential to discuss the prognosis with a patient, even if it is very poor. | 0.0 | 4.4 | 95.6 |
| Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care that they would receive in the hospital. | 0.0 | 21.7 | 78.3 |
| Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. | 0.0 | 8.7 | 91.3 |
| Hospice meets the needs of the family better than conventional care does. | 0.0 | 8.7 | 91.3 |
| Many patients who should receive hospice care do not receive hospice care. | 21.8 | 13.0 | 65.2 |
| Many patients would benefit if hospice care were initiated earlier in the course of their illness. | 0.0 | 9.1 | 90.9 |
| I feel knowledgeable enough to discuss palliative and hospice care with patients and families. | 19.2 | 38.5 | 42.3 |
Common Myths in Treating Patients with Terminal Illness
Myth 1. Treating cancer pain with opioids or analgesics causes addiction in 1 in 100 patients. Most physicians thought that addiction in patients treated for cancer pain with opioids or analgesics was much more common than it is. Almost half the respondents (48.1%) thought addiction occurred in 1 in 100 patients, and an additional 17.3% of respondents thought addiction occurred in 1 in 10 patients treated for cancer pain with opioids or analgesics. In contrast, the incidence of addiction in patients treated with opioids or analgesics for cancer pain is fewer than 1 in 1000 patients.28
Myth 2. When patients with cancer already receiving opioids for pain control complain of increasing pain, it most likely indicates opioid tolerance. Nearly 70% of respondents reported that the most likely reason for complaints of increased pain was tolerance to the opioid. However, the most likely reason for increased pain is increasing pathology of the cancer.27
Myth 3. The equipotent to 30 mg of oral morphine is 5 mg intravenous. More than half of respondents were inaccurate in their conversion of oral to intravenous (IV) morphine dosing, a common task of physicians caring for terminally ill patients. Almost half the physicians (44%) erroneously reported that 30 mg of oral morphine was equipotent to 5 mg or less morphine IV. However, in fact, 30 mg of oral morphine is equipotent to 10 mg of morphine IV.27
Myth 4. The most highly recommended drug for treating terminal dyspnea is a beta‐blocker, and the most appropriate drug for agitation due to anxiety is Haldol or morphine. Most respondents were able to identify the correct drugs; however, a sizable proportion of respondents (17.3%) erroneously responded that beta‐blockers and Lasix or beta‐blockers and corticosteroids were the best drugs for treating terminal dyspnea. About one‐fifth of respondents (21.6%) responded that Haldol or morphine was the recommended medication for treating agitation. In fact, opioids and benzodiazepines are the recommended drugs for treating terminal dyspnea,27 and the proper drug for treating agitation is lorazepam (Ativan).27
Myth 5. Patient life expectancy must be 2 months or less to be eligible for hospice. One‐quarter of respondents believed this to be true for inpatient hospice, and nearly 13.5% of respondents believe this to be true for home hospice. In fact, patients are eligible for hospice benefits earlier in the course of their illness. Under Medicare and most insurance policies, patients are eligible for hospice benefits as soon as their life expectancy is 6 months or less, not 2 months or less.27
Physician Beliefs about Caring for Patients with Terminal Illness
The physicians' beliefs about hospice were generally positive; the vast majority of respondents agreed or strongly agreed with the statement that physical and emotional symptoms of patients and family needs are better addressed with hospice than with the hospital care (Table 3). Most respondents also agreed that many patients do not receive hospice as they should and that hospice should be initiated earlier in the course of the illness. In addition, more than 80% of respondents believed patients and their families want their doctors to tell them the patient's life expectancy, and 95.6% of respondents thought it was essential to discuss prognosis, even a poor one, with the patient. Nevertheless, many respondents (65.3%) reported it was difficult to tell patients and their families that an illness was incurable. Furthermore, fewer than half the respondents (42.3%) believed they were knowledgeable enough to discuss hospice and palliative care with patients and their families.
In subgroup analyses comparing responses to knowledge and attitude items reported in Tables 2 and 3, we found no significant differences between hospitalists and any subgroup of residents by year of training or fellows, or between hospitalists and the full sample of residents and fellows. Because of the sample size, the statistical power for evaluating significance was limited in these exploratory subgroup analyses.
Among physicians who provided responses to the open‐ended question (n = 42) about how to enhance hospice referral rates and improve their timeliness, the most commonly reported suggestions were: (1) involve family members, not only patients, in discussions of hospice (38.1%), (2) have discussions about hospice earlier in the course of care with patients (26.2%), and (3) be clear with patients and families about the patient's prognosis (19.0%). Table 4 has a list of all responses provided to this question.
| Response | n | %* |
|---|---|---|
| ||
| Involving family members as well as patients in discussions of hospice | 16 | 38.1 |
| Having earlier discussion with patients | 11 | 26.2 |
| Being clear with patients and families about patient prognosis | 8 | 19.0 |
| Providing education about hospice to patients and families | 6 | 14.3 |
| Discussions of goals of care with patients and families | 6 | 14.3 |
| Involving social worker in discussions | 4 | 9.5 |
| Providing literature to patients and families about hospice | 3 | 7.1 |
| Having hospice representative available to provide education to patient and families | 2 | 4.8 |
DISCUSSION
This study demonstrated that, among hospitalists and residents, there are several misconceptions about fundamental aspects of caring for terminally ill patients. Given the potential importance of the role hospitalists play in improving the quality of inpatient care,1922 it is critical to identify and address these misconceptions. Additionally, physicians in this study indicated that more and earlier communication with patients and families about prognosis and about the option of hospice would be beneficial, but they themselves did not feel knowledgeable enough to discuss hospice and palliative care with patients and their families.
The nature of the misconceptions identified in this study shed light on the well‐documented phenomena of inadequate pain control24, 29 and poor symptom management2, 4 at the end of life. Having many of the erroneous beliefs apparent in this study may be consistent with providing less pain medication than needed and appropriate. For instance, many physicians believed that developing addiction to opioids used for cancer pain is more likely to occur than it really is, according to research evidence. It is extremely rare for these patients to become addicted to opioids or other analgesics (fewer than 1 in 1000 patients).28 In addition, most physicians believed that complaints of increased pain among patients receiving opioid therapy for pain control meant tolerance to the medication, a belief consistent with physician reluctance to prescribe more medication because it would lead to tolerance.28 In reality, the increased pain experienced in these situations is typically not a result of tolerance to the pain medication but to the cancer getting worse.27 Additionally, many physicians mistakenly decreased the dose of morphine in converting the route of administration from PO to IV, as is often done in hospitals. Such an error may be a contributing factor to the unintended undertreatment of pain in hospitals. Given the variability of cancer pain4 and the difference in time to peak effect depending on the route of administration,5 it is critical for physicians to understand proper dosing in order to effectively treat cancer pain. Furthermore, many physicians were incorrect about the recommended medications for dyspnea and for agitation, 2 symptoms that are prevalent among patients at the end of life.
The hospitalists and residents reported having very positive views about hospice, as is consistent with the literature.10, 30 However, many respondents indicated that patients who would have benefited from hospice did not receive it at all or only late in their illness. Physicians indicated that better communication with patients and families about hospice, prognosis, and goals of care would enhance appropriate use of hospice. While hospitalists and residents are in a position to initiate such discussions, they reported that these discussions were difficult for them. The challenge is how to promote what is necessary and valuable conversation with patients and families despite their difficulty, so that a realistic plan of care can be designed for all involved. Providing hospitalists and residents with evidence about what approaches are most effective in such discussions would be helpful to better prepare them for their roles in caring for hospitalized patients with terminal illness.
The results of this study have substantiated the need to enhance the education of hospitalists and resident physicians, who can play a vital role in improving the transition from hospital to hospice. Such education could take place as part of the residency experience or be embedded in various continuing medical education requirements that most states now have. The results of a recent national survey of hospitalists31 indicates they consider their palliative care training inadequate and feel ill prepared to care for patients with terminal illness. Our findings are consistent with those of that survey, highlighting information that is poorly understood by both residents and hospitalists. As hospitalists continue to play key roles in linking hospital to posthospital care,21 including hospice, there is greater opportunity to improve end‐of‐life care by expanding hospitalists' understanding of these issues.
Our findings should be interpreted in light of the study's limitations. First, this was an exploratory study, and the sample was modest in size. Nevertheless, the response rate was high: 85.2%. Second, we conducted the study in a single location; results may differ in other geographical areas. Last, we were unable to link reported knowledge and attitudes to patient experiences including quality of care or adequacy of pain control. Inadequate knowledge likely limits the quality of clinical practices, but the magnitude of this effect remains unknown and worthy of future study.
Despite these limitations, this study has contributed to the literature by identifying a set of misunderstandings or myths that may be common among hospitalists and residents who frequently care for hospitalized patients with terminal illness. Many of these misunderstandings were related to pain and symptom management, although some misunderstandings related to logistical issues such as hospice eligibility rules. Previous studies have described interventions to improve physicians' knowledge about palliative and end‐of‐life care practices at the undergraduate, graduate, and postgraduate levels.13 Our findings identified specific gaps in physicians' knowledge. Interventions aimed at closing these gaps might emphasize both specific clinical information about pain management and medication recommendations, and more general information about eligibility for hospice and best practices for communicating early with patients and family is needed to promote more effective care for patients with terminal illness being cared for in acute care settings.
As the use of hospitalists has become a widely accepted model of hospital care,32 ensuring their increased training and education in the care of patients with terminal illness is an important step in improving end‐of‐life care. Larger comparison studies are needed to identify differences in the practices and perspectives of hospitalists and residents and to target educational interventions to meet their particular needs. Further, conducting these studies at additional sites including those with established palliative care programs would be useful for identifying needs among a more diverse set of physicians involved in delivering end‐of‐life care.
APPENDIX
Survey on Hospice and End‐of‐Life Care
Survey ID _________________
Date ______________
DEMOGRAPHICS
What is your gender?
□ Male
□ Female
What year did you graduate from medical school? ___________
What is your primary specialty or area of practice?
□ Hospitalist
□ Oncology fellow
□ Oncology resident
□ Physician assistant
□ Other: _____________
KNOWLEDGE OF HOSPICE AND PALLIATIVE CARE PRACTICES
The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is:
Common (1 in 10 patients)
Uncommon (1 in 100 patients)
Very rare (fewer than 1 in 1000 patients)
When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates:
Opioid tolerance
Increasing pathology of the cancer
Patient noncompliance
New onset of a different opioid‐resisting pain
In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to _______________ of IV.
1mg
5 mg
10 mg
20 mg
The 2 classes of drugs most commonly recommended for treating terminal dyspnea are:
Beta‐blockers and Lasix
Opioids and benzodiazepines
Beta‐blockers and corticosteroids
Beta‐blockers and Singulair (montelukast)
A hospice patient whose agitation is due primarily to anxiety should be treated with:
Chlorpromazine
Haloperidol
Lorazepam
Morphine
ELIGIBILITY FOR HOSPICE CARE
Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: ________________________
□ Don't know
To the best of your knowledge, patients are eligible for home hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: __________________________
□ Don't know
ATTITUDES ABOUT HOSPICE CARE 0
Following is a series of statements. Please state whether you strongly agree, agree, neither agree nor disagree, disagree, or strongly disagree with each statement. Strongly agree Strongly disagree 11) Most patients want me to tell them their life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 12) Generally, family caregivers want me to tell them the patient's life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 13) Telling the patient and family members that the patient's illness is incurable is difficult for me. 1 □ 2 □ 3 □ 4 □ 5 □ 14) I think it is essential to discuss the prognosis with a patient, even if it is very poor. 1 □ 2 □ 3 □ 4 □ 5 □ 15) Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 16) Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 17) Hospice care generally meets the needs of the family better than conventional care does. 1 □ 2 □ 3 □ 4 □ 5 □ 18) Many terminally ill patients who should receive hospice care do not receive hospice care. 1 □ 2 □ 3 □ 4 □ 5 □ 19) Many patients would benefit if hospice care were initiated earlier in the course of their illness. 1 □ 2 □ 3 □ 4 □ 5 □ 20) I feel knowledgeable enough to discuss palliative and hospice care with patients and families. 1 □ 2 □ 3 □ 4 □ 5 □ 21) What do you see as the primary ways to facilitate earlier initiation of hospice care for patients who are eligible? _____________________________________________________________________________________ ___________________________________________________________________________________________
- Institute of Medicine.Approaching Death.Washington, DC:National Academy Press;1997.
- SUPPORT Principle Investigators.A controlled trial to improve care for seriously ill hospitalized patients.JAMA.1995;274:1591–1598.
- ,,, et al.Improving the management of pain in hospitalized adults.Arch Intern Med.2006;166:1033–1039.
- .Interventions to manage symptoms at the end of life.J Palliat Med.2005;8(suppl 1):S88–S94.
- ,,, et al.Documentation of discussions about prognosis with terminally ill patients.Am J Med.2001;111:218–223.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–249.
- ,,,,,.At the crossroads: making the transition to hospice.Palliat Support Care.2004;2:351–360.
- ,,,,,.Referral of terminally ill patients for hospice: frequency and correlates.J Palliat Care.2000;16(4):20–26.
- ,,.Hospice and primary care physicians: attitudes, knowledge, and barriers.Am J Hosp Palliat Care.2003;20(1):41–51.
- ,,.Physicians and hospice care: attitudes, knowledge, and referrals.J Palliat Med.2002;5(1):85–92.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5(2):243–248.
- ,,.Improving palliative care.Ann Intern Med.1997;127(3):225–230.
- ,,,,,.Improving end‐of‐life care: internal medicine curriculum project—abstracts/progress reports.J Palliat Med.2001;4(1):75–102.
- ,,, et al.Improving processes of hospital care during the last hours of life.Arch Intern Med.2005;165:1722–1727.
- ,,, et al.How prevalent are hospital‐based palliative care programs? Status report and future directions.J Palliat Med.2001;4:315–324.
- ,,,,,.Evidence of improved knowledge and skills after an elective rotation in a hospice and palliative care program for internal medicine residents.Am J Hosp Palliat Care.2005;22(3):195–203.
- ,,,,,.Factors associated with palliative care knowledge among internal medicine house staff.J Palliat Care.2003;19:253–257.
- ,,.Unrestricted opiate administration for pain and suffering at the end of life: knowledge and attitudes as barriers to care.J Palliat Med.2006;9:873–883.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111 (9B):10S–14S.
- .The evolution of the hospitalist model in the United States.Med Clin North Am.2002;86:687–706.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,, et al.Attitudes about care at the end of life among clinicians: a quick, reliable, and valid assessment instrument.J Palliat Care.2000;16(1):6–14.
- ,,,,,.Physicians' ratings of their knowledge, attitudes, and end‐of‐life‐care practices.Acad Med.2002;77:305–311.
- .Barriers to the physician decision to offer hospice as an option for terminal care.WMJ.1999;98(3):49–53.
- Doyle D,Hanks G,Cherny N,Calman K, eds.Oxford Textbook of Palliative Medicine.3rd ed.Oxford, UK:Oxford University Press;2004.
- ,.Controversies in the long‐term management of analgesic therapy in patients with advanced cancer.J Pain Symptom Manage.1990;5:307–319.
- .Use of opioids in the treatment of severe pain in terminally ill patients—dying should not be painful.Mayo Clin Proc.2003;78:1397–1401.
- ,.Attitude and self‐reported practice regarding hospice referral in a national sample of internists.J Palliat Med.1998;1:241–248.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
Shortcomings in the quality of care of hospitalized patients at the end of life, especially in the final days, are well documented.1, 2 Recent studies have highlighted inadequate pain and symptom control for hospitalized terminally ill patients,24 poor communication about treatment preferences,57 and limited or delayed referral for hospice care.810 Efforts to improve the quality of end‐of‐life care have been diverse, including increased educational programs,1113 development of palliative care units in hospitals,14, 15 and greater exposure to palliative care for physicians during residency training.16 Despite these efforts, studies assessing the attitudes and knowledge of physicians about hospice and palliative care continue to show deficits in knowledge about managing pain17, 18 as well as hospice policies and services.9
Among the interventions aimed at improving hospital care, the hospitalist movement has emerged as a model of care for improving the quality and cost efficiency of hospital care.1922 Because hospitalists spend substantial time on inpatient services,23 they are often involved in the care of patients with terminal illness, with potential to improve the quality of care that these patients receive while hospitalized. However, little is known about what specific knowledge and perspectives hospitalists and residents have about the care of patients with terminal illness. Although many studies have been conducted among physicians in private practice,9, 10, 2426 they have not focused on the knowledge, reported practices, and attitudes of hospitalists and residents concerning key aspects of end‐of‐life care and hospice. Such information can help to identify potential areas for improving knowledge and addressing common barriers highlighted in linking hospital and posthospital hospice care.
METHODS
Study Design and Sample
During 2006 we surveyed hospitalists and medical residents who were on their oncology rotation at a large academic medical center that did not have a hospital‐based palliative care unit in order to examine their knowledge, attitudes, and practices regarding terminally ill patients and hospice referrals. Hospitalists (n = 23) and medical residents (n = 29) made up a convenience sample of 52 physicians. The medical residents were completing their oncology rotation during the spring of 2006. The Institutional Review Board at Yale University School of Medicine approved the research protocol and verbal consent procedures.
Survey
The brief survey instrument (see Appendix) assessed physicians' knowledge and attitudes about and practices in caring for patients with terminal illness. The survey was adapted from previously published instruments8, 24 that have been shown24 to have good test‐retest reliability and construct validity. The survey contained 5 items pertaining to clinical knowledge about palliative care practices, including common symptoms and drug indications, doses, and side effects.27 An additional 2 items pertained to respondents' knowledge about nonclinical issues concerning eligibility rules for hospice,8 such as how a patient becomes eligible for hospice and whether Medicare benefits can be revoked or reinstated after hospice is elected. The survey also included 10 statements24 assessing physician attitudes about caring for patients with terminal illness. Responses, provided using a 5‐point Likert scale, were collapsed for reporting into a 3‐point scale of agree, neutral, and disagree. The instrument also included an open‐ended question asking physicians to specify what from their perspective was needed to ensure timely referral for hospice and palliative care.
Data Analysis
We used standard frequency analysis to describe the distribution of responses to the survey items. Based on an analysis of common erroneous answers to clinical knowledge questions, we identified several common myths prevalent among hospitalists and medicine residents. We also examined whether knowledge, reported practices, and attitudes differed significantly between the hospitalist and the resident samples using ANOVA or chi‐square statistics as appropriate. We used content analysis to summarize the open‐ended responses about potential ways to overcome what respondents perceived was underutilization of hospice.
RESULTS
Overview
The response rate for the survey was 85.2%. Almost half of the respondents (44.2%) were hospitalists (Table 1). The remaining respondents included first‐year (n = 9) and second‐ or third‐year (n = 16) residents or fellows (n = 4). Approximately 54% of the 52 respondents were female, and the majority (83%) had graduated from medical school between 2000 and 2005. Several common myths were apparent and pertained to essential areas of treating patients with terminal illness: pain control, symptom control, and eligibility for hospice (Table 2). Respondents generally had strong beliefs about caring for patients with terminal illness, and most agreed that many patients who would benefit from hospice either do not receive hospice or receive it only late in the course of their illness (Table 3).
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 28 | 53.9% |
| Male | 24 | 46.1% |
| Years since graduation from medical school | ||
| 1‐2 Years | 26 | 56.5% |
| 3‐5 Years | 12 | 26.1% |
| >5 Years | 8 | 17.4% |
| Missing | 6 | |
| Physician type | ||
| Hospitalist | 23 | 44.2% |
| First‐year resident | 9 | 17.3% |
| Second‐ or third‐year resident | 16 | 30.8% |
| Fellow | 4 | 7.7% |
| Questions about hospice and palliative care practices | Response (%) |
|---|---|
| |
| The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is: | |
| Common (1 in 10 patients) | 17.3 |
| Uncommon (1 in 100 patients) | 48.1 |
| Very rare (fewer than 1 in 1000 patients) | 34.6 |
| When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates: | |
| Opioid tolerance | 69.2 |
| Increasing pathology of the cancer | 26.9 |
| Patient noncompliance | 0.0 |
| New onset of a different opioid‐resisting pain | 3.9 |
| In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to of IV morphine | |
| 1 mg | 4.0 |
| 5 mg | 40.0 |
| 10 mg | 56.0 |
| 20 mg | 0.0 |
| The 2 classes of drugs most commonly recommended for treating terminal dyspnea are: | |
| Beta‐blockers and Lasix | 7.7 |
| Opioids and benzodiazepines | 82.7 |
| Beta‐blockers and corticosteroids | 9.6 |
| Beta‐blockers and Singulair (montelukast) | 0.0 |
| A hospice patient whose agitation is primarily from anxiety should be treated with: | |
| Chlorpromazine (thorazine) | 0.0 |
| Haloperidol | 21.6 |
| Lorazepam (Ativan) | 76.4 |
| Morphine | 2.0 |
| Questions about eligibility for hospice care | Response (%) |
| Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in: | |
| 2 Weeks | 5.8 |
| 6 Weeks | 9.6 |
| 2 Months | 9.6 |
| 6 Months | 69.2 |
| Other | 1.9 |
| Don't know | 3.8 |
| To the best of your knowledge, patients become eligible for home hospice care when they are expected to die in: | |
| 2 Weeks | 0.0 |
| 6 Weeks | 5.8 |
| 2 Months | 7.7 |
| 6 Months | 73.1 |
| Other | 0.0 |
| Don't know | 13.4 |
| Beliefs | Disagree (%) | Neutral (%) | Agree (%) |
|---|---|---|---|
| Most patients want me to tell them their life‐expectancy. | 0.0 | 17.4 | 82.6 |
| Generally, family caregivers want me to tell them the patient's life expectancy. | 4.4 | 8.7 | 86.9 |
| Telling the patient and family members that the patient's illness is incurable is difficult for me. | 23.0 | 13.5 | 63.5 |
| I think it is essential to discuss the prognosis with a patient, even if it is very poor. | 0.0 | 4.4 | 95.6 |
| Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care that they would receive in the hospital. | 0.0 | 21.7 | 78.3 |
| Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. | 0.0 | 8.7 | 91.3 |
| Hospice meets the needs of the family better than conventional care does. | 0.0 | 8.7 | 91.3 |
| Many patients who should receive hospice care do not receive hospice care. | 21.8 | 13.0 | 65.2 |
| Many patients would benefit if hospice care were initiated earlier in the course of their illness. | 0.0 | 9.1 | 90.9 |
| I feel knowledgeable enough to discuss palliative and hospice care with patients and families. | 19.2 | 38.5 | 42.3 |
Common Myths in Treating Patients with Terminal Illness
Myth 1. Treating cancer pain with opioids or analgesics causes addiction in 1 in 100 patients. Most physicians thought that addiction in patients treated for cancer pain with opioids or analgesics was much more common than it is. Almost half the respondents (48.1%) thought addiction occurred in 1 in 100 patients, and an additional 17.3% of respondents thought addiction occurred in 1 in 10 patients treated for cancer pain with opioids or analgesics. In contrast, the incidence of addiction in patients treated with opioids or analgesics for cancer pain is fewer than 1 in 1000 patients.28
Myth 2. When patients with cancer already receiving opioids for pain control complain of increasing pain, it most likely indicates opioid tolerance. Nearly 70% of respondents reported that the most likely reason for complaints of increased pain was tolerance to the opioid. However, the most likely reason for increased pain is increasing pathology of the cancer.27
Myth 3. The equipotent to 30 mg of oral morphine is 5 mg intravenous. More than half of respondents were inaccurate in their conversion of oral to intravenous (IV) morphine dosing, a common task of physicians caring for terminally ill patients. Almost half the physicians (44%) erroneously reported that 30 mg of oral morphine was equipotent to 5 mg or less morphine IV. However, in fact, 30 mg of oral morphine is equipotent to 10 mg of morphine IV.27
Myth 4. The most highly recommended drug for treating terminal dyspnea is a beta‐blocker, and the most appropriate drug for agitation due to anxiety is Haldol or morphine. Most respondents were able to identify the correct drugs; however, a sizable proportion of respondents (17.3%) erroneously responded that beta‐blockers and Lasix or beta‐blockers and corticosteroids were the best drugs for treating terminal dyspnea. About one‐fifth of respondents (21.6%) responded that Haldol or morphine was the recommended medication for treating agitation. In fact, opioids and benzodiazepines are the recommended drugs for treating terminal dyspnea,27 and the proper drug for treating agitation is lorazepam (Ativan).27
Myth 5. Patient life expectancy must be 2 months or less to be eligible for hospice. One‐quarter of respondents believed this to be true for inpatient hospice, and nearly 13.5% of respondents believe this to be true for home hospice. In fact, patients are eligible for hospice benefits earlier in the course of their illness. Under Medicare and most insurance policies, patients are eligible for hospice benefits as soon as their life expectancy is 6 months or less, not 2 months or less.27
Physician Beliefs about Caring for Patients with Terminal Illness
The physicians' beliefs about hospice were generally positive; the vast majority of respondents agreed or strongly agreed with the statement that physical and emotional symptoms of patients and family needs are better addressed with hospice than with the hospital care (Table 3). Most respondents also agreed that many patients do not receive hospice as they should and that hospice should be initiated earlier in the course of the illness. In addition, more than 80% of respondents believed patients and their families want their doctors to tell them the patient's life expectancy, and 95.6% of respondents thought it was essential to discuss prognosis, even a poor one, with the patient. Nevertheless, many respondents (65.3%) reported it was difficult to tell patients and their families that an illness was incurable. Furthermore, fewer than half the respondents (42.3%) believed they were knowledgeable enough to discuss hospice and palliative care with patients and their families.
In subgroup analyses comparing responses to knowledge and attitude items reported in Tables 2 and 3, we found no significant differences between hospitalists and any subgroup of residents by year of training or fellows, or between hospitalists and the full sample of residents and fellows. Because of the sample size, the statistical power for evaluating significance was limited in these exploratory subgroup analyses.
Among physicians who provided responses to the open‐ended question (n = 42) about how to enhance hospice referral rates and improve their timeliness, the most commonly reported suggestions were: (1) involve family members, not only patients, in discussions of hospice (38.1%), (2) have discussions about hospice earlier in the course of care with patients (26.2%), and (3) be clear with patients and families about the patient's prognosis (19.0%). Table 4 has a list of all responses provided to this question.
| Response | n | %* |
|---|---|---|
| ||
| Involving family members as well as patients in discussions of hospice | 16 | 38.1 |
| Having earlier discussion with patients | 11 | 26.2 |
| Being clear with patients and families about patient prognosis | 8 | 19.0 |
| Providing education about hospice to patients and families | 6 | 14.3 |
| Discussions of goals of care with patients and families | 6 | 14.3 |
| Involving social worker in discussions | 4 | 9.5 |
| Providing literature to patients and families about hospice | 3 | 7.1 |
| Having hospice representative available to provide education to patient and families | 2 | 4.8 |
DISCUSSION
This study demonstrated that, among hospitalists and residents, there are several misconceptions about fundamental aspects of caring for terminally ill patients. Given the potential importance of the role hospitalists play in improving the quality of inpatient care,1922 it is critical to identify and address these misconceptions. Additionally, physicians in this study indicated that more and earlier communication with patients and families about prognosis and about the option of hospice would be beneficial, but they themselves did not feel knowledgeable enough to discuss hospice and palliative care with patients and their families.
The nature of the misconceptions identified in this study shed light on the well‐documented phenomena of inadequate pain control24, 29 and poor symptom management2, 4 at the end of life. Having many of the erroneous beliefs apparent in this study may be consistent with providing less pain medication than needed and appropriate. For instance, many physicians believed that developing addiction to opioids used for cancer pain is more likely to occur than it really is, according to research evidence. It is extremely rare for these patients to become addicted to opioids or other analgesics (fewer than 1 in 1000 patients).28 In addition, most physicians believed that complaints of increased pain among patients receiving opioid therapy for pain control meant tolerance to the medication, a belief consistent with physician reluctance to prescribe more medication because it would lead to tolerance.28 In reality, the increased pain experienced in these situations is typically not a result of tolerance to the pain medication but to the cancer getting worse.27 Additionally, many physicians mistakenly decreased the dose of morphine in converting the route of administration from PO to IV, as is often done in hospitals. Such an error may be a contributing factor to the unintended undertreatment of pain in hospitals. Given the variability of cancer pain4 and the difference in time to peak effect depending on the route of administration,5 it is critical for physicians to understand proper dosing in order to effectively treat cancer pain. Furthermore, many physicians were incorrect about the recommended medications for dyspnea and for agitation, 2 symptoms that are prevalent among patients at the end of life.
The hospitalists and residents reported having very positive views about hospice, as is consistent with the literature.10, 30 However, many respondents indicated that patients who would have benefited from hospice did not receive it at all or only late in their illness. Physicians indicated that better communication with patients and families about hospice, prognosis, and goals of care would enhance appropriate use of hospice. While hospitalists and residents are in a position to initiate such discussions, they reported that these discussions were difficult for them. The challenge is how to promote what is necessary and valuable conversation with patients and families despite their difficulty, so that a realistic plan of care can be designed for all involved. Providing hospitalists and residents with evidence about what approaches are most effective in such discussions would be helpful to better prepare them for their roles in caring for hospitalized patients with terminal illness.
The results of this study have substantiated the need to enhance the education of hospitalists and resident physicians, who can play a vital role in improving the transition from hospital to hospice. Such education could take place as part of the residency experience or be embedded in various continuing medical education requirements that most states now have. The results of a recent national survey of hospitalists31 indicates they consider their palliative care training inadequate and feel ill prepared to care for patients with terminal illness. Our findings are consistent with those of that survey, highlighting information that is poorly understood by both residents and hospitalists. As hospitalists continue to play key roles in linking hospital to posthospital care,21 including hospice, there is greater opportunity to improve end‐of‐life care by expanding hospitalists' understanding of these issues.
Our findings should be interpreted in light of the study's limitations. First, this was an exploratory study, and the sample was modest in size. Nevertheless, the response rate was high: 85.2%. Second, we conducted the study in a single location; results may differ in other geographical areas. Last, we were unable to link reported knowledge and attitudes to patient experiences including quality of care or adequacy of pain control. Inadequate knowledge likely limits the quality of clinical practices, but the magnitude of this effect remains unknown and worthy of future study.
Despite these limitations, this study has contributed to the literature by identifying a set of misunderstandings or myths that may be common among hospitalists and residents who frequently care for hospitalized patients with terminal illness. Many of these misunderstandings were related to pain and symptom management, although some misunderstandings related to logistical issues such as hospice eligibility rules. Previous studies have described interventions to improve physicians' knowledge about palliative and end‐of‐life care practices at the undergraduate, graduate, and postgraduate levels.13 Our findings identified specific gaps in physicians' knowledge. Interventions aimed at closing these gaps might emphasize both specific clinical information about pain management and medication recommendations, and more general information about eligibility for hospice and best practices for communicating early with patients and family is needed to promote more effective care for patients with terminal illness being cared for in acute care settings.
As the use of hospitalists has become a widely accepted model of hospital care,32 ensuring their increased training and education in the care of patients with terminal illness is an important step in improving end‐of‐life care. Larger comparison studies are needed to identify differences in the practices and perspectives of hospitalists and residents and to target educational interventions to meet their particular needs. Further, conducting these studies at additional sites including those with established palliative care programs would be useful for identifying needs among a more diverse set of physicians involved in delivering end‐of‐life care.
APPENDIX
Survey on Hospice and End‐of‐Life Care
Survey ID _________________
Date ______________
DEMOGRAPHICS
What is your gender?
□ Male
□ Female
What year did you graduate from medical school? ___________
What is your primary specialty or area of practice?
□ Hospitalist
□ Oncology fellow
□ Oncology resident
□ Physician assistant
□ Other: _____________
KNOWLEDGE OF HOSPICE AND PALLIATIVE CARE PRACTICES
The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is:
Common (1 in 10 patients)
Uncommon (1 in 100 patients)
Very rare (fewer than 1 in 1000 patients)
When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates:
Opioid tolerance
Increasing pathology of the cancer
Patient noncompliance
New onset of a different opioid‐resisting pain
In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to _______________ of IV.
1mg
5 mg
10 mg
20 mg
The 2 classes of drugs most commonly recommended for treating terminal dyspnea are:
Beta‐blockers and Lasix
Opioids and benzodiazepines
Beta‐blockers and corticosteroids
Beta‐blockers and Singulair (montelukast)
A hospice patient whose agitation is due primarily to anxiety should be treated with:
Chlorpromazine
Haloperidol
Lorazepam
Morphine
ELIGIBILITY FOR HOSPICE CARE
Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: ________________________
□ Don't know
To the best of your knowledge, patients are eligible for home hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: __________________________
□ Don't know
ATTITUDES ABOUT HOSPICE CARE 0
Following is a series of statements. Please state whether you strongly agree, agree, neither agree nor disagree, disagree, or strongly disagree with each statement. Strongly agree Strongly disagree 11) Most patients want me to tell them their life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 12) Generally, family caregivers want me to tell them the patient's life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 13) Telling the patient and family members that the patient's illness is incurable is difficult for me. 1 □ 2 □ 3 □ 4 □ 5 □ 14) I think it is essential to discuss the prognosis with a patient, even if it is very poor. 1 □ 2 □ 3 □ 4 □ 5 □ 15) Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 16) Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 17) Hospice care generally meets the needs of the family better than conventional care does. 1 □ 2 □ 3 □ 4 □ 5 □ 18) Many terminally ill patients who should receive hospice care do not receive hospice care. 1 □ 2 □ 3 □ 4 □ 5 □ 19) Many patients would benefit if hospice care were initiated earlier in the course of their illness. 1 □ 2 □ 3 □ 4 □ 5 □ 20) I feel knowledgeable enough to discuss palliative and hospice care with patients and families. 1 □ 2 □ 3 □ 4 □ 5 □ 21) What do you see as the primary ways to facilitate earlier initiation of hospice care for patients who are eligible? _____________________________________________________________________________________ ___________________________________________________________________________________________
Shortcomings in the quality of care of hospitalized patients at the end of life, especially in the final days, are well documented.1, 2 Recent studies have highlighted inadequate pain and symptom control for hospitalized terminally ill patients,24 poor communication about treatment preferences,57 and limited or delayed referral for hospice care.810 Efforts to improve the quality of end‐of‐life care have been diverse, including increased educational programs,1113 development of palliative care units in hospitals,14, 15 and greater exposure to palliative care for physicians during residency training.16 Despite these efforts, studies assessing the attitudes and knowledge of physicians about hospice and palliative care continue to show deficits in knowledge about managing pain17, 18 as well as hospice policies and services.9
Among the interventions aimed at improving hospital care, the hospitalist movement has emerged as a model of care for improving the quality and cost efficiency of hospital care.1922 Because hospitalists spend substantial time on inpatient services,23 they are often involved in the care of patients with terminal illness, with potential to improve the quality of care that these patients receive while hospitalized. However, little is known about what specific knowledge and perspectives hospitalists and residents have about the care of patients with terminal illness. Although many studies have been conducted among physicians in private practice,9, 10, 2426 they have not focused on the knowledge, reported practices, and attitudes of hospitalists and residents concerning key aspects of end‐of‐life care and hospice. Such information can help to identify potential areas for improving knowledge and addressing common barriers highlighted in linking hospital and posthospital hospice care.
METHODS
Study Design and Sample
During 2006 we surveyed hospitalists and medical residents who were on their oncology rotation at a large academic medical center that did not have a hospital‐based palliative care unit in order to examine their knowledge, attitudes, and practices regarding terminally ill patients and hospice referrals. Hospitalists (n = 23) and medical residents (n = 29) made up a convenience sample of 52 physicians. The medical residents were completing their oncology rotation during the spring of 2006. The Institutional Review Board at Yale University School of Medicine approved the research protocol and verbal consent procedures.
Survey
The brief survey instrument (see Appendix) assessed physicians' knowledge and attitudes about and practices in caring for patients with terminal illness. The survey was adapted from previously published instruments8, 24 that have been shown24 to have good test‐retest reliability and construct validity. The survey contained 5 items pertaining to clinical knowledge about palliative care practices, including common symptoms and drug indications, doses, and side effects.27 An additional 2 items pertained to respondents' knowledge about nonclinical issues concerning eligibility rules for hospice,8 such as how a patient becomes eligible for hospice and whether Medicare benefits can be revoked or reinstated after hospice is elected. The survey also included 10 statements24 assessing physician attitudes about caring for patients with terminal illness. Responses, provided using a 5‐point Likert scale, were collapsed for reporting into a 3‐point scale of agree, neutral, and disagree. The instrument also included an open‐ended question asking physicians to specify what from their perspective was needed to ensure timely referral for hospice and palliative care.
Data Analysis
We used standard frequency analysis to describe the distribution of responses to the survey items. Based on an analysis of common erroneous answers to clinical knowledge questions, we identified several common myths prevalent among hospitalists and medicine residents. We also examined whether knowledge, reported practices, and attitudes differed significantly between the hospitalist and the resident samples using ANOVA or chi‐square statistics as appropriate. We used content analysis to summarize the open‐ended responses about potential ways to overcome what respondents perceived was underutilization of hospice.
RESULTS
Overview
The response rate for the survey was 85.2%. Almost half of the respondents (44.2%) were hospitalists (Table 1). The remaining respondents included first‐year (n = 9) and second‐ or third‐year (n = 16) residents or fellows (n = 4). Approximately 54% of the 52 respondents were female, and the majority (83%) had graduated from medical school between 2000 and 2005. Several common myths were apparent and pertained to essential areas of treating patients with terminal illness: pain control, symptom control, and eligibility for hospice (Table 2). Respondents generally had strong beliefs about caring for patients with terminal illness, and most agreed that many patients who would benefit from hospice either do not receive hospice or receive it only late in the course of their illness (Table 3).
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 28 | 53.9% |
| Male | 24 | 46.1% |
| Years since graduation from medical school | ||
| 1‐2 Years | 26 | 56.5% |
| 3‐5 Years | 12 | 26.1% |
| >5 Years | 8 | 17.4% |
| Missing | 6 | |
| Physician type | ||
| Hospitalist | 23 | 44.2% |
| First‐year resident | 9 | 17.3% |
| Second‐ or third‐year resident | 16 | 30.8% |
| Fellow | 4 | 7.7% |
| Questions about hospice and palliative care practices | Response (%) |
|---|---|
| |
| The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is: | |
| Common (1 in 10 patients) | 17.3 |
| Uncommon (1 in 100 patients) | 48.1 |
| Very rare (fewer than 1 in 1000 patients) | 34.6 |
| When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates: | |
| Opioid tolerance | 69.2 |
| Increasing pathology of the cancer | 26.9 |
| Patient noncompliance | 0.0 |
| New onset of a different opioid‐resisting pain | 3.9 |
| In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to of IV morphine | |
| 1 mg | 4.0 |
| 5 mg | 40.0 |
| 10 mg | 56.0 |
| 20 mg | 0.0 |
| The 2 classes of drugs most commonly recommended for treating terminal dyspnea are: | |
| Beta‐blockers and Lasix | 7.7 |
| Opioids and benzodiazepines | 82.7 |
| Beta‐blockers and corticosteroids | 9.6 |
| Beta‐blockers and Singulair (montelukast) | 0.0 |
| A hospice patient whose agitation is primarily from anxiety should be treated with: | |
| Chlorpromazine (thorazine) | 0.0 |
| Haloperidol | 21.6 |
| Lorazepam (Ativan) | 76.4 |
| Morphine | 2.0 |
| Questions about eligibility for hospice care | Response (%) |
| Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in: | |
| 2 Weeks | 5.8 |
| 6 Weeks | 9.6 |
| 2 Months | 9.6 |
| 6 Months | 69.2 |
| Other | 1.9 |
| Don't know | 3.8 |
| To the best of your knowledge, patients become eligible for home hospice care when they are expected to die in: | |
| 2 Weeks | 0.0 |
| 6 Weeks | 5.8 |
| 2 Months | 7.7 |
| 6 Months | 73.1 |
| Other | 0.0 |
| Don't know | 13.4 |
| Beliefs | Disagree (%) | Neutral (%) | Agree (%) |
|---|---|---|---|
| Most patients want me to tell them their life‐expectancy. | 0.0 | 17.4 | 82.6 |
| Generally, family caregivers want me to tell them the patient's life expectancy. | 4.4 | 8.7 | 86.9 |
| Telling the patient and family members that the patient's illness is incurable is difficult for me. | 23.0 | 13.5 | 63.5 |
| I think it is essential to discuss the prognosis with a patient, even if it is very poor. | 0.0 | 4.4 | 95.6 |
| Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care that they would receive in the hospital. | 0.0 | 21.7 | 78.3 |
| Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. | 0.0 | 8.7 | 91.3 |
| Hospice meets the needs of the family better than conventional care does. | 0.0 | 8.7 | 91.3 |
| Many patients who should receive hospice care do not receive hospice care. | 21.8 | 13.0 | 65.2 |
| Many patients would benefit if hospice care were initiated earlier in the course of their illness. | 0.0 | 9.1 | 90.9 |
| I feel knowledgeable enough to discuss palliative and hospice care with patients and families. | 19.2 | 38.5 | 42.3 |
Common Myths in Treating Patients with Terminal Illness
Myth 1. Treating cancer pain with opioids or analgesics causes addiction in 1 in 100 patients. Most physicians thought that addiction in patients treated for cancer pain with opioids or analgesics was much more common than it is. Almost half the respondents (48.1%) thought addiction occurred in 1 in 100 patients, and an additional 17.3% of respondents thought addiction occurred in 1 in 10 patients treated for cancer pain with opioids or analgesics. In contrast, the incidence of addiction in patients treated with opioids or analgesics for cancer pain is fewer than 1 in 1000 patients.28
Myth 2. When patients with cancer already receiving opioids for pain control complain of increasing pain, it most likely indicates opioid tolerance. Nearly 70% of respondents reported that the most likely reason for complaints of increased pain was tolerance to the opioid. However, the most likely reason for increased pain is increasing pathology of the cancer.27
Myth 3. The equipotent to 30 mg of oral morphine is 5 mg intravenous. More than half of respondents were inaccurate in their conversion of oral to intravenous (IV) morphine dosing, a common task of physicians caring for terminally ill patients. Almost half the physicians (44%) erroneously reported that 30 mg of oral morphine was equipotent to 5 mg or less morphine IV. However, in fact, 30 mg of oral morphine is equipotent to 10 mg of morphine IV.27
Myth 4. The most highly recommended drug for treating terminal dyspnea is a beta‐blocker, and the most appropriate drug for agitation due to anxiety is Haldol or morphine. Most respondents were able to identify the correct drugs; however, a sizable proportion of respondents (17.3%) erroneously responded that beta‐blockers and Lasix or beta‐blockers and corticosteroids were the best drugs for treating terminal dyspnea. About one‐fifth of respondents (21.6%) responded that Haldol or morphine was the recommended medication for treating agitation. In fact, opioids and benzodiazepines are the recommended drugs for treating terminal dyspnea,27 and the proper drug for treating agitation is lorazepam (Ativan).27
Myth 5. Patient life expectancy must be 2 months or less to be eligible for hospice. One‐quarter of respondents believed this to be true for inpatient hospice, and nearly 13.5% of respondents believe this to be true for home hospice. In fact, patients are eligible for hospice benefits earlier in the course of their illness. Under Medicare and most insurance policies, patients are eligible for hospice benefits as soon as their life expectancy is 6 months or less, not 2 months or less.27
Physician Beliefs about Caring for Patients with Terminal Illness
The physicians' beliefs about hospice were generally positive; the vast majority of respondents agreed or strongly agreed with the statement that physical and emotional symptoms of patients and family needs are better addressed with hospice than with the hospital care (Table 3). Most respondents also agreed that many patients do not receive hospice as they should and that hospice should be initiated earlier in the course of the illness. In addition, more than 80% of respondents believed patients and their families want their doctors to tell them the patient's life expectancy, and 95.6% of respondents thought it was essential to discuss prognosis, even a poor one, with the patient. Nevertheless, many respondents (65.3%) reported it was difficult to tell patients and their families that an illness was incurable. Furthermore, fewer than half the respondents (42.3%) believed they were knowledgeable enough to discuss hospice and palliative care with patients and their families.
In subgroup analyses comparing responses to knowledge and attitude items reported in Tables 2 and 3, we found no significant differences between hospitalists and any subgroup of residents by year of training or fellows, or between hospitalists and the full sample of residents and fellows. Because of the sample size, the statistical power for evaluating significance was limited in these exploratory subgroup analyses.
Among physicians who provided responses to the open‐ended question (n = 42) about how to enhance hospice referral rates and improve their timeliness, the most commonly reported suggestions were: (1) involve family members, not only patients, in discussions of hospice (38.1%), (2) have discussions about hospice earlier in the course of care with patients (26.2%), and (3) be clear with patients and families about the patient's prognosis (19.0%). Table 4 has a list of all responses provided to this question.
| Response | n | %* |
|---|---|---|
| ||
| Involving family members as well as patients in discussions of hospice | 16 | 38.1 |
| Having earlier discussion with patients | 11 | 26.2 |
| Being clear with patients and families about patient prognosis | 8 | 19.0 |
| Providing education about hospice to patients and families | 6 | 14.3 |
| Discussions of goals of care with patients and families | 6 | 14.3 |
| Involving social worker in discussions | 4 | 9.5 |
| Providing literature to patients and families about hospice | 3 | 7.1 |
| Having hospice representative available to provide education to patient and families | 2 | 4.8 |
DISCUSSION
This study demonstrated that, among hospitalists and residents, there are several misconceptions about fundamental aspects of caring for terminally ill patients. Given the potential importance of the role hospitalists play in improving the quality of inpatient care,1922 it is critical to identify and address these misconceptions. Additionally, physicians in this study indicated that more and earlier communication with patients and families about prognosis and about the option of hospice would be beneficial, but they themselves did not feel knowledgeable enough to discuss hospice and palliative care with patients and their families.
The nature of the misconceptions identified in this study shed light on the well‐documented phenomena of inadequate pain control24, 29 and poor symptom management2, 4 at the end of life. Having many of the erroneous beliefs apparent in this study may be consistent with providing less pain medication than needed and appropriate. For instance, many physicians believed that developing addiction to opioids used for cancer pain is more likely to occur than it really is, according to research evidence. It is extremely rare for these patients to become addicted to opioids or other analgesics (fewer than 1 in 1000 patients).28 In addition, most physicians believed that complaints of increased pain among patients receiving opioid therapy for pain control meant tolerance to the medication, a belief consistent with physician reluctance to prescribe more medication because it would lead to tolerance.28 In reality, the increased pain experienced in these situations is typically not a result of tolerance to the pain medication but to the cancer getting worse.27 Additionally, many physicians mistakenly decreased the dose of morphine in converting the route of administration from PO to IV, as is often done in hospitals. Such an error may be a contributing factor to the unintended undertreatment of pain in hospitals. Given the variability of cancer pain4 and the difference in time to peak effect depending on the route of administration,5 it is critical for physicians to understand proper dosing in order to effectively treat cancer pain. Furthermore, many physicians were incorrect about the recommended medications for dyspnea and for agitation, 2 symptoms that are prevalent among patients at the end of life.
The hospitalists and residents reported having very positive views about hospice, as is consistent with the literature.10, 30 However, many respondents indicated that patients who would have benefited from hospice did not receive it at all or only late in their illness. Physicians indicated that better communication with patients and families about hospice, prognosis, and goals of care would enhance appropriate use of hospice. While hospitalists and residents are in a position to initiate such discussions, they reported that these discussions were difficult for them. The challenge is how to promote what is necessary and valuable conversation with patients and families despite their difficulty, so that a realistic plan of care can be designed for all involved. Providing hospitalists and residents with evidence about what approaches are most effective in such discussions would be helpful to better prepare them for their roles in caring for hospitalized patients with terminal illness.
The results of this study have substantiated the need to enhance the education of hospitalists and resident physicians, who can play a vital role in improving the transition from hospital to hospice. Such education could take place as part of the residency experience or be embedded in various continuing medical education requirements that most states now have. The results of a recent national survey of hospitalists31 indicates they consider their palliative care training inadequate and feel ill prepared to care for patients with terminal illness. Our findings are consistent with those of that survey, highlighting information that is poorly understood by both residents and hospitalists. As hospitalists continue to play key roles in linking hospital to posthospital care,21 including hospice, there is greater opportunity to improve end‐of‐life care by expanding hospitalists' understanding of these issues.
Our findings should be interpreted in light of the study's limitations. First, this was an exploratory study, and the sample was modest in size. Nevertheless, the response rate was high: 85.2%. Second, we conducted the study in a single location; results may differ in other geographical areas. Last, we were unable to link reported knowledge and attitudes to patient experiences including quality of care or adequacy of pain control. Inadequate knowledge likely limits the quality of clinical practices, but the magnitude of this effect remains unknown and worthy of future study.
Despite these limitations, this study has contributed to the literature by identifying a set of misunderstandings or myths that may be common among hospitalists and residents who frequently care for hospitalized patients with terminal illness. Many of these misunderstandings were related to pain and symptom management, although some misunderstandings related to logistical issues such as hospice eligibility rules. Previous studies have described interventions to improve physicians' knowledge about palliative and end‐of‐life care practices at the undergraduate, graduate, and postgraduate levels.13 Our findings identified specific gaps in physicians' knowledge. Interventions aimed at closing these gaps might emphasize both specific clinical information about pain management and medication recommendations, and more general information about eligibility for hospice and best practices for communicating early with patients and family is needed to promote more effective care for patients with terminal illness being cared for in acute care settings.
As the use of hospitalists has become a widely accepted model of hospital care,32 ensuring their increased training and education in the care of patients with terminal illness is an important step in improving end‐of‐life care. Larger comparison studies are needed to identify differences in the practices and perspectives of hospitalists and residents and to target educational interventions to meet their particular needs. Further, conducting these studies at additional sites including those with established palliative care programs would be useful for identifying needs among a more diverse set of physicians involved in delivering end‐of‐life care.
APPENDIX
Survey on Hospice and End‐of‐Life Care
Survey ID _________________
Date ______________
DEMOGRAPHICS
What is your gender?
□ Male
□ Female
What year did you graduate from medical school? ___________
What is your primary specialty or area of practice?
□ Hospitalist
□ Oncology fellow
□ Oncology resident
□ Physician assistant
□ Other: _____________
KNOWLEDGE OF HOSPICE AND PALLIATIVE CARE PRACTICES
The incidence of psychological dependence (addiction) to opioids and analgesics when treating pain from cancer or other medical conditions is:
Common (1 in 10 patients)
Uncommon (1 in 100 patients)
Very rare (fewer than 1 in 1000 patients)
When a patient with cancer who is receiving opioids for pain complains of increasing pain, it most likely indicates:
Opioid tolerance
Increasing pathology of the cancer
Patient noncompliance
New onset of a different opioid‐resisting pain
In the pain patient receiving opioids, 30 mg of oral morphine is equipotent to _______________ of IV.
1mg
5 mg
10 mg
20 mg
The 2 classes of drugs most commonly recommended for treating terminal dyspnea are:
Beta‐blockers and Lasix
Opioids and benzodiazepines
Beta‐blockers and corticosteroids
Beta‐blockers and Singulair (montelukast)
A hospice patient whose agitation is due primarily to anxiety should be treated with:
Chlorpromazine
Haloperidol
Lorazepam
Morphine
ELIGIBILITY FOR HOSPICE CARE
Under the Medicare program, a physician must certify that the patient is expected to die within a specified time for the patients to be eligible for hospice services. To the best of your knowledge, patients become eligible for inpatient hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: ________________________
□ Don't know
To the best of your knowledge, patients are eligible for home hospice care when they are expected to die in:
□ 2 Weeks
□ 6 Weeks
□ 2 Months
□ 6 Months
□ Other: __________________________
□ Don't know
ATTITUDES ABOUT HOSPICE CARE 0
Following is a series of statements. Please state whether you strongly agree, agree, neither agree nor disagree, disagree, or strongly disagree with each statement. Strongly agree Strongly disagree 11) Most patients want me to tell them their life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 12) Generally, family caregivers want me to tell them the patient's life expectancy. 1 □ 2 □ 3 □ 4 □ 5 □ 13) Telling the patient and family members that the patient's illness is incurable is difficult for me. 1 □ 2 □ 3 □ 4 □ 5 □ 14) I think it is essential to discuss the prognosis with a patient, even if it is very poor. 1 □ 2 □ 3 □ 4 □ 5 □ 15) Most patients' physical symptoms (eg, pain, shortness of breath, and nausea) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 16) Most patients' emotional symptoms (eg, depression, anxiety) are controlled better with hospice than with the care they would receive in the hospital. 1 □ 2 □ 3 □ 4 □ 5 □ 17) Hospice care generally meets the needs of the family better than conventional care does. 1 □ 2 □ 3 □ 4 □ 5 □ 18) Many terminally ill patients who should receive hospice care do not receive hospice care. 1 □ 2 □ 3 □ 4 □ 5 □ 19) Many patients would benefit if hospice care were initiated earlier in the course of their illness. 1 □ 2 □ 3 □ 4 □ 5 □ 20) I feel knowledgeable enough to discuss palliative and hospice care with patients and families. 1 □ 2 □ 3 □ 4 □ 5 □ 21) What do you see as the primary ways to facilitate earlier initiation of hospice care for patients who are eligible? _____________________________________________________________________________________ ___________________________________________________________________________________________
- Institute of Medicine.Approaching Death.Washington, DC:National Academy Press;1997.
- SUPPORT Principle Investigators.A controlled trial to improve care for seriously ill hospitalized patients.JAMA.1995;274:1591–1598.
- ,,, et al.Improving the management of pain in hospitalized adults.Arch Intern Med.2006;166:1033–1039.
- .Interventions to manage symptoms at the end of life.J Palliat Med.2005;8(suppl 1):S88–S94.
- ,,, et al.Documentation of discussions about prognosis with terminally ill patients.Am J Med.2001;111:218–223.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–249.
- ,,,,,.At the crossroads: making the transition to hospice.Palliat Support Care.2004;2:351–360.
- ,,,,,.Referral of terminally ill patients for hospice: frequency and correlates.J Palliat Care.2000;16(4):20–26.
- ,,.Hospice and primary care physicians: attitudes, knowledge, and barriers.Am J Hosp Palliat Care.2003;20(1):41–51.
- ,,.Physicians and hospice care: attitudes, knowledge, and referrals.J Palliat Med.2002;5(1):85–92.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5(2):243–248.
- ,,.Improving palliative care.Ann Intern Med.1997;127(3):225–230.
- ,,,,,.Improving end‐of‐life care: internal medicine curriculum project—abstracts/progress reports.J Palliat Med.2001;4(1):75–102.
- ,,, et al.Improving processes of hospital care during the last hours of life.Arch Intern Med.2005;165:1722–1727.
- ,,, et al.How prevalent are hospital‐based palliative care programs? Status report and future directions.J Palliat Med.2001;4:315–324.
- ,,,,,.Evidence of improved knowledge and skills after an elective rotation in a hospice and palliative care program for internal medicine residents.Am J Hosp Palliat Care.2005;22(3):195–203.
- ,,,,,.Factors associated with palliative care knowledge among internal medicine house staff.J Palliat Care.2003;19:253–257.
- ,,.Unrestricted opiate administration for pain and suffering at the end of life: knowledge and attitudes as barriers to care.J Palliat Med.2006;9:873–883.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111 (9B):10S–14S.
- .The evolution of the hospitalist model in the United States.Med Clin North Am.2002;86:687–706.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,, et al.Attitudes about care at the end of life among clinicians: a quick, reliable, and valid assessment instrument.J Palliat Care.2000;16(1):6–14.
- ,,,,,.Physicians' ratings of their knowledge, attitudes, and end‐of‐life‐care practices.Acad Med.2002;77:305–311.
- .Barriers to the physician decision to offer hospice as an option for terminal care.WMJ.1999;98(3):49–53.
- Doyle D,Hanks G,Cherny N,Calman K, eds.Oxford Textbook of Palliative Medicine.3rd ed.Oxford, UK:Oxford University Press;2004.
- ,.Controversies in the long‐term management of analgesic therapy in patients with advanced cancer.J Pain Symptom Manage.1990;5:307–319.
- .Use of opioids in the treatment of severe pain in terminally ill patients—dying should not be painful.Mayo Clin Proc.2003;78:1397–1401.
- ,.Attitude and self‐reported practice regarding hospice referral in a national sample of internists.J Palliat Med.1998;1:241–248.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Institute of Medicine.Approaching Death.Washington, DC:National Academy Press;1997.
- SUPPORT Principle Investigators.A controlled trial to improve care for seriously ill hospitalized patients.JAMA.1995;274:1591–1598.
- ,,, et al.Improving the management of pain in hospitalized adults.Arch Intern Med.2006;166:1033–1039.
- .Interventions to manage symptoms at the end of life.J Palliat Med.2005;8(suppl 1):S88–S94.
- ,,, et al.Documentation of discussions about prognosis with terminally ill patients.Am J Med.2001;111:218–223.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–249.
- ,,,,,.At the crossroads: making the transition to hospice.Palliat Support Care.2004;2:351–360.
- ,,,,,.Referral of terminally ill patients for hospice: frequency and correlates.J Palliat Care.2000;16(4):20–26.
- ,,.Hospice and primary care physicians: attitudes, knowledge, and barriers.Am J Hosp Palliat Care.2003;20(1):41–51.
- ,,.Physicians and hospice care: attitudes, knowledge, and referrals.J Palliat Med.2002;5(1):85–92.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5(2):243–248.
- ,,.Improving palliative care.Ann Intern Med.1997;127(3):225–230.
- ,,,,,.Improving end‐of‐life care: internal medicine curriculum project—abstracts/progress reports.J Palliat Med.2001;4(1):75–102.
- ,,, et al.Improving processes of hospital care during the last hours of life.Arch Intern Med.2005;165:1722–1727.
- ,,, et al.How prevalent are hospital‐based palliative care programs? Status report and future directions.J Palliat Med.2001;4:315–324.
- ,,,,,.Evidence of improved knowledge and skills after an elective rotation in a hospice and palliative care program for internal medicine residents.Am J Hosp Palliat Care.2005;22(3):195–203.
- ,,,,,.Factors associated with palliative care knowledge among internal medicine house staff.J Palliat Care.2003;19:253–257.
- ,,.Unrestricted opiate administration for pain and suffering at the end of life: knowledge and attitudes as barriers to care.J Palliat Med.2006;9:873–883.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111 (9B):10S–14S.
- .The evolution of the hospitalist model in the United States.Med Clin North Am.2002;86:687–706.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,, et al.Attitudes about care at the end of life among clinicians: a quick, reliable, and valid assessment instrument.J Palliat Care.2000;16(1):6–14.
- ,,,,,.Physicians' ratings of their knowledge, attitudes, and end‐of‐life‐care practices.Acad Med.2002;77:305–311.
- .Barriers to the physician decision to offer hospice as an option for terminal care.WMJ.1999;98(3):49–53.
- Doyle D,Hanks G,Cherny N,Calman K, eds.Oxford Textbook of Palliative Medicine.3rd ed.Oxford, UK:Oxford University Press;2004.
- ,.Controversies in the long‐term management of analgesic therapy in patients with advanced cancer.J Pain Symptom Manage.1990;5:307–319.
- .Use of opioids in the treatment of severe pain in terminally ill patients—dying should not be painful.Mayo Clin Proc.2003;78:1397–1401.
- ,.Attitude and self‐reported practice regarding hospice referral in a national sample of internists.J Palliat Med.1998;1:241–248.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
Copyright © 2007 Society of Hospital Medicine
Editorial / Kutner
Communication, palliative care, and patient safety have been identified by the Society of Hospital Medicine as core competencies in hospital medicine. Effective communication is recognized as being central to the role of the hospitalist to promote efficient, safe, and high quality care.1 Hospitalists are increasingly recognized as having a central role in initiatives to improve palliative care for hospitalized patients and their families24 and have a vital role in leading and participating in interventions to mitigate system and process failures that affect patient safety.1 The obligation of the hospitalist to assure safe, quality care for hospitalized people with advanced illness extends from direct patient care to advocacy for systems that facilitate the provision of such care.
Four articles in this issue of the Journal of Hospital Medicine provide complementary perspectives on these crucial roles of the hospitalist. Cherlin and colleagues describe findings from a survey of hospitalists and medical residents regarding their knowledge, attitudes, and practices relative to caring for patients with terminal illness. The article identifies misperceptions related to core components of quality palliative care: pain and symptom control, hospice eligibility, and communication about prognosis and hospice and palliative care.5 Although this study was conducted at only a single academic medical center and certainly deserves to be repeated in an expanded and more representative sample, it clearly identifies deficits in core components of quality care for persons with advanced illness. The article by Minichiello and colleagues provides practical guidance and resources for addressing one of the deficits identified: communicating a poor prognosis, or bad news.6
Pain and symptom management and communication are commonly recognized aspects of quality care for persons with advanced illness. Less often appreciated are the significant threats to patient safety and medical errors that occur in the care of this vulnerable population.79 Potential errors include failure of a planned action to be completed as intended (ie, not following advance directives) and failure to treat symptoms adequately. The original research article and accompanying images discussion by Sehgal and colleagues serve as a call to action to both recognize and address the potentially significant patient safety issue related to the use of color‐coded wristbands, particularly variation in color used by different hospitals to designate do not resuscitate status.10, 11 What is exciting about this sequence of articles is that they describe opportunities for improvement and provide potential solutions. We have to be aware that there is a problem in order to initiate change. Hospitalists are in an a prime position to both identify these potential critical issues and effect the necessary changes to facilitate our ability to provide safe, effective care to our patients with advanced illness.
Palliative care is increasingly being accepted as a means for improving care for persons with advanced illness. The National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, released in 2004, was endorsed by the National Quality Forum and incorporated into its Framework for Hospice and Palliative Care in 2007.12, 13 The Joint Commission (TJC; previously known as JCAHO) is developing a Health Care Services Certification Program for palliative care services modeled on existing programs for diabetes and stroke care, to take effect in 2008.14 Newsweek featured palliative care in its August 2006 issue focused on Fixing America's Hospitals.15 US News and World Report has included hospice and palliative care indicators in its ranking of America's Best Hospitals since 2002.16 There has been significant recent growth in hospital‐based palliative care programs, with 1250 hospitals reporting palliative care programs in 2005, an increase of almost 100% over 2000. Seventy percent of U.S. hospitals with more than 250 beds report having a palliative care program.17
Although hospital‐based palliative care programs are increasing, it is the obligation of all hospitalists who care for an ill, often elderly population to assure that all hospitalized patients with advanced illness receive safe, quality care while hospitalized. This includes avoiding medical errors such as inappropriate resuscitation attempts because of miscommunication of do‐not‐resuscitate orders or advance directives, as well as minimizing distress, maximizing comfort, and addressing informational and psychosocial support needs. As evidenced by the 4 articles in this issue of the Journal of Hospital Medicine, we need to make safe, effective care for people with advanced illness a priority, then implement appropriate training and education and create systems that assure delivery of quality care.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:1–67.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- .Palliative Care in Hospitals.J Hosp Med.2006;1:21–28.
- ,,,,,.Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting.J Hosp Med.2007;2:357–365.
- ,, andBreaking bad news: a practical approach for the hospitalist.J Hosp Med.2007;2:415–421.
- ,.Patients with eventually fatal chronic illness: their importance within a national research agenda on improving patient safety and reducing medical errors.J Palliat Med.2001;4:325–332.
- ,.Advance care planning for fatal chronic illness: avoiding commonplace errors and unwarranted suffering.Ann Intern Med.2003;138:812–818.
- ,.Mortality as a measure of quality: implications for palliative and end‐of‐life care.JAMA.2007;298:802–804.
- ,.Color‐coded wristbands: promoting safety or confusion?J Hosp Med.2007;2:445.
- ,.Identification of inpatient DNR status: a safety hazard begging for standardization.J Hosp Med.2007;2:366–371.
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. Available at: http://www.nationalconsensusproject.org. Accessed August 26,2007.
- National Quality Forum. Available at: Available at: http://www.qualityforum.org. Accessed August 25,2007.
- Joint Commission for Accreditation of Health Care Organizations. Available at: http://www.jointcommission.org. Accessed August 26,2007.
- .Special Care at the End of Life.Newsweek. October 16,2006. Available at: http://www.msnbc.msn.com/id/15175919/site/newsweek/page/0/. Accessed September 22,year="2007"2007.
- U.S. News and World Report America's Best Hospitals 2007 Methodology. Available at: http://health.usnews.com/usnews/health/best‐hospitals/methodology_report.pdf. Accessed September 22,2007.
- Center to Advance Palliative Care (CAPC). Available at: http://www.capc.org. Accessed August 26,2007.
Communication, palliative care, and patient safety have been identified by the Society of Hospital Medicine as core competencies in hospital medicine. Effective communication is recognized as being central to the role of the hospitalist to promote efficient, safe, and high quality care.1 Hospitalists are increasingly recognized as having a central role in initiatives to improve palliative care for hospitalized patients and their families24 and have a vital role in leading and participating in interventions to mitigate system and process failures that affect patient safety.1 The obligation of the hospitalist to assure safe, quality care for hospitalized people with advanced illness extends from direct patient care to advocacy for systems that facilitate the provision of such care.
Four articles in this issue of the Journal of Hospital Medicine provide complementary perspectives on these crucial roles of the hospitalist. Cherlin and colleagues describe findings from a survey of hospitalists and medical residents regarding their knowledge, attitudes, and practices relative to caring for patients with terminal illness. The article identifies misperceptions related to core components of quality palliative care: pain and symptom control, hospice eligibility, and communication about prognosis and hospice and palliative care.5 Although this study was conducted at only a single academic medical center and certainly deserves to be repeated in an expanded and more representative sample, it clearly identifies deficits in core components of quality care for persons with advanced illness. The article by Minichiello and colleagues provides practical guidance and resources for addressing one of the deficits identified: communicating a poor prognosis, or bad news.6
Pain and symptom management and communication are commonly recognized aspects of quality care for persons with advanced illness. Less often appreciated are the significant threats to patient safety and medical errors that occur in the care of this vulnerable population.79 Potential errors include failure of a planned action to be completed as intended (ie, not following advance directives) and failure to treat symptoms adequately. The original research article and accompanying images discussion by Sehgal and colleagues serve as a call to action to both recognize and address the potentially significant patient safety issue related to the use of color‐coded wristbands, particularly variation in color used by different hospitals to designate do not resuscitate status.10, 11 What is exciting about this sequence of articles is that they describe opportunities for improvement and provide potential solutions. We have to be aware that there is a problem in order to initiate change. Hospitalists are in an a prime position to both identify these potential critical issues and effect the necessary changes to facilitate our ability to provide safe, effective care to our patients with advanced illness.
Palliative care is increasingly being accepted as a means for improving care for persons with advanced illness. The National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, released in 2004, was endorsed by the National Quality Forum and incorporated into its Framework for Hospice and Palliative Care in 2007.12, 13 The Joint Commission (TJC; previously known as JCAHO) is developing a Health Care Services Certification Program for palliative care services modeled on existing programs for diabetes and stroke care, to take effect in 2008.14 Newsweek featured palliative care in its August 2006 issue focused on Fixing America's Hospitals.15 US News and World Report has included hospice and palliative care indicators in its ranking of America's Best Hospitals since 2002.16 There has been significant recent growth in hospital‐based palliative care programs, with 1250 hospitals reporting palliative care programs in 2005, an increase of almost 100% over 2000. Seventy percent of U.S. hospitals with more than 250 beds report having a palliative care program.17
Although hospital‐based palliative care programs are increasing, it is the obligation of all hospitalists who care for an ill, often elderly population to assure that all hospitalized patients with advanced illness receive safe, quality care while hospitalized. This includes avoiding medical errors such as inappropriate resuscitation attempts because of miscommunication of do‐not‐resuscitate orders or advance directives, as well as minimizing distress, maximizing comfort, and addressing informational and psychosocial support needs. As evidenced by the 4 articles in this issue of the Journal of Hospital Medicine, we need to make safe, effective care for people with advanced illness a priority, then implement appropriate training and education and create systems that assure delivery of quality care.
Communication, palliative care, and patient safety have been identified by the Society of Hospital Medicine as core competencies in hospital medicine. Effective communication is recognized as being central to the role of the hospitalist to promote efficient, safe, and high quality care.1 Hospitalists are increasingly recognized as having a central role in initiatives to improve palliative care for hospitalized patients and their families24 and have a vital role in leading and participating in interventions to mitigate system and process failures that affect patient safety.1 The obligation of the hospitalist to assure safe, quality care for hospitalized people with advanced illness extends from direct patient care to advocacy for systems that facilitate the provision of such care.
Four articles in this issue of the Journal of Hospital Medicine provide complementary perspectives on these crucial roles of the hospitalist. Cherlin and colleagues describe findings from a survey of hospitalists and medical residents regarding their knowledge, attitudes, and practices relative to caring for patients with terminal illness. The article identifies misperceptions related to core components of quality palliative care: pain and symptom control, hospice eligibility, and communication about prognosis and hospice and palliative care.5 Although this study was conducted at only a single academic medical center and certainly deserves to be repeated in an expanded and more representative sample, it clearly identifies deficits in core components of quality care for persons with advanced illness. The article by Minichiello and colleagues provides practical guidance and resources for addressing one of the deficits identified: communicating a poor prognosis, or bad news.6
Pain and symptom management and communication are commonly recognized aspects of quality care for persons with advanced illness. Less often appreciated are the significant threats to patient safety and medical errors that occur in the care of this vulnerable population.79 Potential errors include failure of a planned action to be completed as intended (ie, not following advance directives) and failure to treat symptoms adequately. The original research article and accompanying images discussion by Sehgal and colleagues serve as a call to action to both recognize and address the potentially significant patient safety issue related to the use of color‐coded wristbands, particularly variation in color used by different hospitals to designate do not resuscitate status.10, 11 What is exciting about this sequence of articles is that they describe opportunities for improvement and provide potential solutions. We have to be aware that there is a problem in order to initiate change. Hospitalists are in an a prime position to both identify these potential critical issues and effect the necessary changes to facilitate our ability to provide safe, effective care to our patients with advanced illness.
Palliative care is increasingly being accepted as a means for improving care for persons with advanced illness. The National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, released in 2004, was endorsed by the National Quality Forum and incorporated into its Framework for Hospice and Palliative Care in 2007.12, 13 The Joint Commission (TJC; previously known as JCAHO) is developing a Health Care Services Certification Program for palliative care services modeled on existing programs for diabetes and stroke care, to take effect in 2008.14 Newsweek featured palliative care in its August 2006 issue focused on Fixing America's Hospitals.15 US News and World Report has included hospice and palliative care indicators in its ranking of America's Best Hospitals since 2002.16 There has been significant recent growth in hospital‐based palliative care programs, with 1250 hospitals reporting palliative care programs in 2005, an increase of almost 100% over 2000. Seventy percent of U.S. hospitals with more than 250 beds report having a palliative care program.17
Although hospital‐based palliative care programs are increasing, it is the obligation of all hospitalists who care for an ill, often elderly population to assure that all hospitalized patients with advanced illness receive safe, quality care while hospitalized. This includes avoiding medical errors such as inappropriate resuscitation attempts because of miscommunication of do‐not‐resuscitate orders or advance directives, as well as minimizing distress, maximizing comfort, and addressing informational and psychosocial support needs. As evidenced by the 4 articles in this issue of the Journal of Hospital Medicine, we need to make safe, effective care for people with advanced illness a priority, then implement appropriate training and education and create systems that assure delivery of quality care.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:1–67.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- .Palliative Care in Hospitals.J Hosp Med.2006;1:21–28.
- ,,,,,.Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting.J Hosp Med.2007;2:357–365.
- ,, andBreaking bad news: a practical approach for the hospitalist.J Hosp Med.2007;2:415–421.
- ,.Patients with eventually fatal chronic illness: their importance within a national research agenda on improving patient safety and reducing medical errors.J Palliat Med.2001;4:325–332.
- ,.Advance care planning for fatal chronic illness: avoiding commonplace errors and unwarranted suffering.Ann Intern Med.2003;138:812–818.
- ,.Mortality as a measure of quality: implications for palliative and end‐of‐life care.JAMA.2007;298:802–804.
- ,.Color‐coded wristbands: promoting safety or confusion?J Hosp Med.2007;2:445.
- ,.Identification of inpatient DNR status: a safety hazard begging for standardization.J Hosp Med.2007;2:366–371.
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. Available at: http://www.nationalconsensusproject.org. Accessed August 26,2007.
- National Quality Forum. Available at: Available at: http://www.qualityforum.org. Accessed August 25,2007.
- Joint Commission for Accreditation of Health Care Organizations. Available at: http://www.jointcommission.org. Accessed August 26,2007.
- .Special Care at the End of Life.Newsweek. October 16,2006. Available at: http://www.msnbc.msn.com/id/15175919/site/newsweek/page/0/. Accessed September 22,year="2007"2007.
- U.S. News and World Report America's Best Hospitals 2007 Methodology. Available at: http://health.usnews.com/usnews/health/best‐hospitals/methodology_report.pdf. Accessed September 22,2007.
- Center to Advance Palliative Care (CAPC). Available at: http://www.capc.org. Accessed August 26,2007.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:1–67.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- .Palliative Care in Hospitals.J Hosp Med.2006;1:21–28.
- ,,,,,.Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting.J Hosp Med.2007;2:357–365.
- ,, andBreaking bad news: a practical approach for the hospitalist.J Hosp Med.2007;2:415–421.
- ,.Patients with eventually fatal chronic illness: their importance within a national research agenda on improving patient safety and reducing medical errors.J Palliat Med.2001;4:325–332.
- ,.Advance care planning for fatal chronic illness: avoiding commonplace errors and unwarranted suffering.Ann Intern Med.2003;138:812–818.
- ,.Mortality as a measure of quality: implications for palliative and end‐of‐life care.JAMA.2007;298:802–804.
- ,.Color‐coded wristbands: promoting safety or confusion?J Hosp Med.2007;2:445.
- ,.Identification of inpatient DNR status: a safety hazard begging for standardization.J Hosp Med.2007;2:366–371.
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. Available at: http://www.nationalconsensusproject.org. Accessed August 26,2007.
- National Quality Forum. Available at: Available at: http://www.qualityforum.org. Accessed August 25,2007.
- Joint Commission for Accreditation of Health Care Organizations. Available at: http://www.jointcommission.org. Accessed August 26,2007.
- .Special Care at the End of Life.Newsweek. October 16,2006. Available at: http://www.msnbc.msn.com/id/15175919/site/newsweek/page/0/. Accessed September 22,year="2007"2007.
- U.S. News and World Report America's Best Hospitals 2007 Methodology. Available at: http://health.usnews.com/usnews/health/best‐hospitals/methodology_report.pdf. Accessed September 22,2007.
- Center to Advance Palliative Care (CAPC). Available at: http://www.capc.org. Accessed August 26,2007.
Play by the Rules
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.