User login
Sleep hygiene helps patients catch some ZZZs
Proper sleep hygiene can help your patients fall and stay asleep consistently. Patients with insomnia are at a higher risk of developing or experiencing a recurrence of a mood disorder, and poor sleep can worsen psychiatric symptoms such as depression or mania.1 Data about combining behavioral approaches and hypnotic medications to treat insomnia are inconclusive;2 however, using the 2 together may help patients who do not respond to a single approach.
First rule out other causes of insomnia, such as sleep apnea, other medical conditions, or medications. Patients may improve after these factors are addressed.
Teaching sleep hygiene principles (Box) does not mean patients will adopt these habits, but employing the following suggestions could improve adherence:
Obtain a detailed sleep history to identify specific behaviors to be changed. For example, a patient might only have to stop watching television in bed to get a good night’s sleep, although some may find a brief exposure to television or radio facilitates relaxation.
Explain the rationale for changing a behavior. For example, when telling patients to limit caffeine or alcohol at night, list these substances’ negative effects on sleep. Similarly, when instructing patients to avoid watching television in bed, tell them that using the bedroom only for sleep or sex will help condition them for sleep at bedtime.
- Establish a regular sleep-wake schedule
- Limit caffeine and alcohol consumption
- Avoid naps
- Eliminate noise and light from the sleep environment
- Use the bed only for sleep or sex
- Avoid looking at a clock when trying to sleep
Discuss sleep regularly. A patient might not disclose poor sleeping habits during the first session.
Give your patient handouts on sleep hygiene principles and highlight the most pertinent information. Ask the patient to place the handout where he or she will see it regularly.
Involve the family to help identify a patient’s poor sleep habits and find ways to implement sleep hygiene principles.
Encourage patients to keep a sleep diary. Ask the patient to note how many hours and at what time he or she slept for at least 2 weeks, then bring this information to the next appointment. This record allows you to examine patients’ sleep patterns and recommend appropriate changes.
Ask patients for creative ideas to improve their sleep. This dialogue will facilitate the therapeutic alliance and encourage positive changes in patients’ lives.
1. Peterson MJ, Benca RM. Sleep in mood disorders. Psychiatr Clin North Am 2006;29:1009-32.
2. Mendelson WB. Combining pharmacological and non-pharmacological therapies for insomnia. J Clin Psychiatry 2007;68(suppl 5):19-23.
Dr. Khawaja is staff psychiatrist, VA Medical Center, Minneapolis, MN; Dr. Hurwitz is a psychiatrist and sleep medicine physician, VA Medical Center, Minneapolis, MN; Dr. Ebrahim is an endocrinologist, Minnesota Center for Obesity, Metabolism, and Endocrinology, Eagan, MN.
Proper sleep hygiene can help your patients fall and stay asleep consistently. Patients with insomnia are at a higher risk of developing or experiencing a recurrence of a mood disorder, and poor sleep can worsen psychiatric symptoms such as depression or mania.1 Data about combining behavioral approaches and hypnotic medications to treat insomnia are inconclusive;2 however, using the 2 together may help patients who do not respond to a single approach.
First rule out other causes of insomnia, such as sleep apnea, other medical conditions, or medications. Patients may improve after these factors are addressed.
Teaching sleep hygiene principles (Box) does not mean patients will adopt these habits, but employing the following suggestions could improve adherence:
Obtain a detailed sleep history to identify specific behaviors to be changed. For example, a patient might only have to stop watching television in bed to get a good night’s sleep, although some may find a brief exposure to television or radio facilitates relaxation.
Explain the rationale for changing a behavior. For example, when telling patients to limit caffeine or alcohol at night, list these substances’ negative effects on sleep. Similarly, when instructing patients to avoid watching television in bed, tell them that using the bedroom only for sleep or sex will help condition them for sleep at bedtime.
- Establish a regular sleep-wake schedule
- Limit caffeine and alcohol consumption
- Avoid naps
- Eliminate noise and light from the sleep environment
- Use the bed only for sleep or sex
- Avoid looking at a clock when trying to sleep
Discuss sleep regularly. A patient might not disclose poor sleeping habits during the first session.
Give your patient handouts on sleep hygiene principles and highlight the most pertinent information. Ask the patient to place the handout where he or she will see it regularly.
Involve the family to help identify a patient’s poor sleep habits and find ways to implement sleep hygiene principles.
Encourage patients to keep a sleep diary. Ask the patient to note how many hours and at what time he or she slept for at least 2 weeks, then bring this information to the next appointment. This record allows you to examine patients’ sleep patterns and recommend appropriate changes.
Ask patients for creative ideas to improve their sleep. This dialogue will facilitate the therapeutic alliance and encourage positive changes in patients’ lives.
Proper sleep hygiene can help your patients fall and stay asleep consistently. Patients with insomnia are at a higher risk of developing or experiencing a recurrence of a mood disorder, and poor sleep can worsen psychiatric symptoms such as depression or mania.1 Data about combining behavioral approaches and hypnotic medications to treat insomnia are inconclusive;2 however, using the 2 together may help patients who do not respond to a single approach.
First rule out other causes of insomnia, such as sleep apnea, other medical conditions, or medications. Patients may improve after these factors are addressed.
Teaching sleep hygiene principles (Box) does not mean patients will adopt these habits, but employing the following suggestions could improve adherence:
Obtain a detailed sleep history to identify specific behaviors to be changed. For example, a patient might only have to stop watching television in bed to get a good night’s sleep, although some may find a brief exposure to television or radio facilitates relaxation.
Explain the rationale for changing a behavior. For example, when telling patients to limit caffeine or alcohol at night, list these substances’ negative effects on sleep. Similarly, when instructing patients to avoid watching television in bed, tell them that using the bedroom only for sleep or sex will help condition them for sleep at bedtime.
- Establish a regular sleep-wake schedule
- Limit caffeine and alcohol consumption
- Avoid naps
- Eliminate noise and light from the sleep environment
- Use the bed only for sleep or sex
- Avoid looking at a clock when trying to sleep
Discuss sleep regularly. A patient might not disclose poor sleeping habits during the first session.
Give your patient handouts on sleep hygiene principles and highlight the most pertinent information. Ask the patient to place the handout where he or she will see it regularly.
Involve the family to help identify a patient’s poor sleep habits and find ways to implement sleep hygiene principles.
Encourage patients to keep a sleep diary. Ask the patient to note how many hours and at what time he or she slept for at least 2 weeks, then bring this information to the next appointment. This record allows you to examine patients’ sleep patterns and recommend appropriate changes.
Ask patients for creative ideas to improve their sleep. This dialogue will facilitate the therapeutic alliance and encourage positive changes in patients’ lives.
1. Peterson MJ, Benca RM. Sleep in mood disorders. Psychiatr Clin North Am 2006;29:1009-32.
2. Mendelson WB. Combining pharmacological and non-pharmacological therapies for insomnia. J Clin Psychiatry 2007;68(suppl 5):19-23.
Dr. Khawaja is staff psychiatrist, VA Medical Center, Minneapolis, MN; Dr. Hurwitz is a psychiatrist and sleep medicine physician, VA Medical Center, Minneapolis, MN; Dr. Ebrahim is an endocrinologist, Minnesota Center for Obesity, Metabolism, and Endocrinology, Eagan, MN.
1. Peterson MJ, Benca RM. Sleep in mood disorders. Psychiatr Clin North Am 2006;29:1009-32.
2. Mendelson WB. Combining pharmacological and non-pharmacological therapies for insomnia. J Clin Psychiatry 2007;68(suppl 5):19-23.
Dr. Khawaja is staff psychiatrist, VA Medical Center, Minneapolis, MN; Dr. Hurwitz is a psychiatrist and sleep medicine physician, VA Medical Center, Minneapolis, MN; Dr. Ebrahim is an endocrinologist, Minnesota Center for Obesity, Metabolism, and Endocrinology, Eagan, MN.
Can medications prevent PTSD in trauma victims?
Posttraumatic stress disorder (PTSD) is a preventable mental illness—without trauma, the illness does not occur. Primary prevention (such as eliminating war, rape, physical assaults, child abuse, or motor vehicle accidents) would be effective but is an unrealistic goal. Secondary prevention (such as preventing PTSD after individuals have been exposed to trauma) may be attainable.
No medication is FDA-approved to prevent PTSD, but patients recently exposed to trauma might benefit from drugs approved for other indications. Possibilities include noradrenergics such as propranolol, corticosteroids that affect the hypothalamic-pituitary-adrenal (HPA) axis, opioids, benzodiazepines, and antidepressants. Some investigational agents also might block the process that turns a traumatic experience into PTSD.
This article discusses these intriguing ideas and suggests which trauma victims might benefit now from acute pharmacologic PTSD prevention.
Who might be treated?
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life (Box 1).1,2 A person’s risk of developing PTSD after a traumatic event depends on the type of trauma. For example, 10% of motor vehicle accident survivors develop PTSD, compared with 60% of rape survivors.1
Targeting anyone who has experienced trauma for secondary PTSD prevention would expose large groups of people to medications they do not need. Targeting selected persons who are at the highest risk would be more efficient and cost-effective. In a group of acute trauma-exposed persons, 2 selection criteria could be considered simultaneously:
- Which patients may be most predisposed to PTSD?
- Which patients are showing early symptoms that may predict PTSD?
More than half of all American adults have been exposed to at least one traumatic event at some point in their lives.1 In most persons, the posttraumatic stress reaction causes short-term distress, with hyperarousal, agitation, intrusive memories, and exaggerated startle. Although these symptoms usually subside relatively quickly, they persist and evolve into posttraumatic stress disorder (PTSD) in a substantial number of trauma victims.
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life.2 Emotional distress, social and occupational disability, and persistent decrements in quality of life make PTSD a major public health problem.
Risk factors and resiliency. Certain factors have been shown to increase a person’s vulnerability for PTSD (Table 1).3 Other proposed risk factors include:
- personality types4
- psychophysiologic factors such as reactivity, conditionability, and resistance to extinction/habituation.5
Strong evidence also indicates that acute trauma-related symptoms—including excessive arousal and fear,6 peritraumatic dissociation, and depression—predict the later development of PTSD.
Once identified, individuals predisposed to developing PTSD could be given treatment to increase their resiliency after they have been exposed to trauma. Early evidence suggests that you also could consider giving these patients medications as secondary prevention (Table 2).
Table 1
Who develops PTSD? Risk and resiliency factors
Risk factors that may increase vulnerability for PTSD
|
Resiliency factors that may protect against PTSD
|
| Source: Reference 3 |
Table 2
Medications being studied for PTSD prevention
| Mechanism of action | Medication | FDA-approved indications | ||
|---|---|---|---|---|
| Psychiatric | Nonpsychiatric | |||
| Noradrenergic | Clonidine | No | Yes | |
| Guanfacine | No | Yes | ||
| Prazosin | No | Yes | ||
| Propranolol | No | Yes | ||
| Hypothalamic-pituitary-adrenal axis | Hydrocortisone | No | Yes | |
| Opioid | Morphine | No | Yes | |
| Antidepressant | Dual action | Duloxetine | Yes | Yes |
| Venlafaxine | Yes | No | ||
| SSRIs | Citalopram | Yes | No | |
| Fluoxetine | Yes | No | ||
| Paroxetine | Yes | No | ||
| Sertraline | Yes | No | ||
| TCAs | Amitriptyline | Yes | No | |
| Imipramine | Yes | No | ||
| GABA-benzodiazepine | Alprazolam | Yes | No | |
| Temazepam | Yes | No | ||
| Corticotropin-releasing hormone (CRH) | CRH antagonist | Investigational | ||
| Substance P | Substance P antagonist | Investigational | ||
| Neuropeptide Y | Neuropeptide Y agonist | Investigational | ||
| SSRIs: selective serotonin reuptake inhibitors | ||||
| TCAs: tricyclic antidepressants | ||||
Targeting noradrenergic activity
Increased noradrenergic activity has been associated with persistent memories and PTSD. Therefore, medications that reduce noradrenergic tone by blocking receptors or reduce norepinephrine release are being explored for PTSD prevention.
Propranolol. Three small studies have examined whether the beta-noradrenergic receptor blocker propranolol can prevent PTSD.
In a randomized, double-blind, placebo-controlled trial,7 41 emergency department patients who had a heart rate of ≥ 80 bpm within 6 hours of a traumatic accident received propranolol, 40 mg qid, or placebo for 10 days. After 1 month, the 11 patients who completed propranolol treatment showed a nonsignificant trend toward lower scores on the Clinician-Administered PTSD Scale (CAPS), compared with 20 patients taking placebo. At 3 months, the propranolol group had less physiologic reactivity (as measured by heart rate and skin conductance) to trauma-related cues than the placebo group.
In a nonrandomized study,8 PTSD developed within 2 months in 1 of 11 trauma victims who agreed to take propranolol, 40 mg tid, immediately after the trauma, compared with 3 of 8 victims who refused the medication.
In an unpublished randomized, double-blind trial,9 48 patients admitted to a level I trauma center received propranolol, 40 mg tid; gabapentin, 400 mg tid; or placebo for PTSD prevention. Gabapentin was chosen because it has few side effects or metabolic interactions and preliminary evidence of anxiolytic efficacy.
Neither propranolol nor gabapentin showed statistically significant benefit in preventing PTSD compared with placebo. Effect sizes with the 2 treatments were too small to suggest that larger samples would produce a statistically significant result.
Prazosin—an alpha-1 adrenergic receptor antagonist—has been evaluated in 3 controlled studies and found to reduce intrusive nightmares typical of chronic PTSD.
Ten combat veterans with chronic PTSD showed significantly improved sleep, fewer severe nightmares, and improved global clinical status after receiving prazosin (mean dose 9.5 mg at bedtime) in a 20-week, placebo-controlled, double-blind, crossover study.10
In a larger randomized, parallel group trial,11 the same authors compared prazosin with placebo in 40 combat veterans (mean age 56) with chronic PTSD. After 8 weeks, veterans taking prazosin (mean 13.3 ± 3 mg) had significantly fewer trauma nightmares, improved sleep (including return of normal dreams), and improved global clinical status vs placebo. Overall CAP scores did not decline significantly, however.
In a third placebo-controlled study,12 a midmorning dose of prazosin was added to the regimens of 11 civilian trauma patients already taking the drug at bedtime to suppress trauma-related nightmares. Their daytime PTSD symptoms improved, as shown by reduced psychological distress in response to verbal trauma cues.
Prazosin can reduce chronic PTSD manifestations of nightmares and disturbed sleep, but it has not been shown to ameliorate the full PTSD syndrome. Prazosin has not been studied as an early PTSD intervention.
Other antiadrenergics that reduce the release of norepinephrine—including clonidine and guanfacine—have been studied in open trials as treatment for PTSD. The only controlled study13 showed no benefit from guanfacine for PTSD prevention.
De-stressing the HPA axis
Hydrocortisone has been proposed to prevent PTSD by reducing HPA axis activation, acting as a countermeasure to elevated corticotropin-releasing factor found in patients with chronic PTSD.
IV hydrocortisone’s effect on the development of PTSD was compared with placebo in 20 septic shock survivors after discharge from intensive care.14 One of 9 patients (11%) in the hydrocortisone group was diagnosed with PTSD at follow-up (mean 31 months), compared with 7 of 11 (64%) in the placebo group.
In a similar study, the same researchers gave patients hydrocortisone before, during, and after cardiac surgery. Follow-up interviews revealed significantly lower PTSD and chronic stress symptom scores in the treatment group vs the placebo group.15
These studies—although provocative—are limited by the narrow range of trauma related to severe medical illness or extensive medical procedures.
Norepinephrine-blocking opioids
When the noradrenergic system is activated, one physiologic response is the activation of endogenous opioid systems, which may promote recovery by inhibiting the HPA axis. Opioid systems might be involved in PTSD, as suggested by:
- preclinical evidence that opioids modulate memory16
- studies showing low pain thresholds17 and abnormal beta-endorphin (an opioid peptide neurotransmitter)18 and methionine enkephalin (an opioid peptide)19 levels in PTSD patients.
In theory, opioid administration immediately after trauma may attenuate norepinephrine release, thus thwarting arousal-charged memory consolidation, hyperarousal, and re-experiencing.
One uncontrolled report of pediatric burn victims found a significant association between the morphine dose given for pain during hospitalization and reduced PTSD symptoms 6 months later.20 Decreased pain did not explain the reduction in PTSD, as no significant correlation was seen between pain symptoms and PTSD outcome measures. Similarly, a longitudinal study of substance use among Vietnam War veterans with PTSD found decreased hyperarousal symptoms in heroin users.21
Using opioids to prevent PTSD would be feasible and efficient in acute care settings because 80% to 90% of traumatically-injured patients are discharged on opioid analgesics (compared with <10% on beta blockers or corticosteroids).22 However, 20% to 40% of physically injured inpatients are diagnosed with a substance use disorder at some point in life, making the use of opioid analgesics a practical concern.23
GABA-benzodiazepine paradox
The GABA-benzodiazepine system plays an important role in mediating anxiety, which is consistent with the potent anxiolytic effects of benzodiazepines. Even so, trials of benzodiazepines have found these drugs surprisingly unhelpful—and perhaps harmful—in patients with acute trauma.
Alprazolam did not reduce PTSD symptoms in a small randomized, double-blind study.24 Another trial found that receiving benzodiazepines shortly after trauma exposure was associated with increased PTSD risk in trauma survivors. Nine of 13 patients (69%) who received alprazolam or clonazepam met PTSD diagnostic criteria 6 months after the trauma, compared with 3 of 13 controls (15%).25
Similarly, in a randomized controlled trial, 22 patients were given temazepam for 7 nights, starting approximately 14 days after exposure to a traumatic event. Six weeks later, 55% of those receiving temazepam and 27% of those receiving placebo met criteria for PTSD.26
In summary, benzodiazepines might be helpful when given for a few days after traumatization to control overwhelming anxiety but could be harmful over a longer term.
Other agents for PTSD
Antidepressants. Early trauma-related symptoms of depression predict later development of PTSD.27 Thus, antidepressants have been proposed for early intervention in addition to their well-established role as first-line treatment of PTSD.28
One study supports this idea: a 7-day randomized double-blind trial that compared the tricyclic antidepressant imipramine with chloral hydrate in pediatric burn patients with acute stress disorder (ASD). Imipramine was more effective (83% response) than chloral hydrate (38% response) in reducing ASD symptoms.29
Drugs in development. Three new medications being explored for treating anxiety and depression also might be useful for PTSD prevention. Neuropeptide Y (NPY) agonists,30 substance P antagonists,31 and CRH-antagonists32 are thought to hold promise because of their more proximate roles—compared with monoamine neurotransmitters such as dopamine, norepinephrine and serotonin—in mediating the stress response.
Manage the post-trauma environment:
- Move the victim to safety.
- Treat pain effectively.
- Avoid stress from interrogations, separation from loved ones, or unstable housing.
Avoid crisis incident stress debriefing (CISD), which could enhance physiologic hyperarousal and is not recommended as first-line treatment for most trauma victims. CISD was designed for and is best received by emergency personnel.
Consider prescribing antidepressants for patients thought to be particularly vulnerable to develop posttraumatic stress disorder (PTSD). Risk factors include:
- history of PTSD, depression, or anxiety disorder
- severe trauma (such as from sexual assault or torture)
- physical injury, when antidepressants with analgesic properties might be useful.
Analyzing the evidence
Insufficient evidence exists to determine which strategies might be most effective to prevent PTSD, what optimal dosing might be, and which traumatized individuals might be best targeted with these approaches.
- Beta-blockers and corticosteroids—the most theoretically compelling strategies—are the most difficult agents to use for PTSD prevention because they have the most medical contraindications. In addition, evidence supporting their ability to prevent PTSD is meager at best.
- Prazosin is intriguing but has contra-indications similar to those of beta blockers, no studies of secondary prevention, and no clear indication that it works for the overall PTSD syndrome.
- Opioids are restricted agents with substantial contraindications.
- Evidence is limited but points most strongly toward earlier use of antidepressants. Early trauma-related symptoms of depression predict later development of PTSD,27 and a number of selective serotonin reuptake inhibitors—such as citalopram, fluoxetine, paroxetine, and sertraline—are FDA-approved or used off-label for treating PTSD.33
Prescribing recommendations. Consider practicality, ease of use, and safety of the proposed medication when choosing a drug for PTSD prevention (Table 3).22 Based on the evidence, the most reasonable posttrauma approach (Box 2) might be to consider starting an approved antidepressant for individuals thought to be particularly vulnerable to PTSD because of:
- past history of PTSD, depression, or anxiety disorder
- severity of the trauma (such as in cases of sexual assault or torture)
- pain (antidepressants with analgesic properties—such as venlafaxine or duloxetine—might be useful in patients whose trauma is associated with physical injury, although neither is FDA-approved to treat PTSD).
Table 3
4 considerations when choosing a drug for PTSD prevention
| Potential benefits | Practicality, ease of use, and safety of the proposed medication |
| Potential drug-drug or drug-disease interactions | Asthma, diabetes, and trauma are relative contraindications to the use of antiadrenergics and corticosteroids |
| Psychiatric comorbidities | A patient’s history of substance use disorder makes opioid analgesics a concern |
| Clinical experience | Agents already prescribed safely and broadly in clinical practice are easiest to test and to use |
Related resources
- Mental health and mass violence: Evidence-based early psychological intervention for victims/survivors of mass violence. A workshop to reach consensus on best practices. Rockland, MD: National Institute of Mental Health; 2002. www.nimh.nih.gov.
- Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care (clinical guideline 26). London, UK: National Institute for Clinical Excellence; 2005. www.nice.org.uk.
- Ursano RJ, Bell C, Eth S, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry 2004;161(suppl 11):3-31.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clonidine • Catapres
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Guanfacine • Tenex
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Paroxetine • Paxil
- Prazosin • Minipress
- Propranolol • Inderal
- Sertraline • Zoloft
- Temazepam • Restoril
- Venlafaxine • Effexor
Disclosure
Dr. Bennett and Dr. Zatzick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Roy-Byrne is a consultant to Jazz Pharmaceuticals and Solvay and has received speaker honoraria from Wyeth and Forrest Pharmaceuticals.
1. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52(12):1048-60.
2. Zatzick D. Posttraumatic stress, functional impairment, and service utilization after injury: a public health approach. Semin Clin Neuropsychiatry 2003;8(3):149-57.
3. Yehuda R, Flory JD, Southwick S, Charney DS. Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Ann NY Acad Sci 2006;1071:379-96.
4. Schnurr P, Vielhauer M. Personality as a risk factor for PTSD. In: Yehuda R, ed. Risk factors for post-traumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1999:191-222.
5. Shalev A. Psychophysiological expression of risk factors for PTSD. In: Yehuda R, ed. Risk factors for posttraumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1995.
6. Bryant RA, Harvey AG, Guthrie RM, Moulds ML. A prospective study of psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol 2000;109(2):341-4.
7. Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol Psychiatry 2002;51(2):189-92.
8. Vaiva G, Ducrocq F, Jezequel K, et al. Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma. Biol Psychiatry 2003;54(9):947-9.
9. Stein M. Pharmacoprevention of adverse psychiatric sequelae of physical injury. Paper presented at: 21st Annual Meeting of the International Society for Traumatic Stress Studies; November 2-5, 2005; Toronto, Ontario, Canada.
10. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
11. Raskind MA, Peskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry 2007;61(8):928-34.
12. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry 2006;59(7):577-81.
13. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry 2006;163(12):2186-8.
14. Schelling G, Briegel J, Roozendaal B, et al. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biol Psychiatry 2001;50(12):978-85.
15. Weis F, Kilger E, Roozendaal B, et al. Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: a randomized study. J Thorac Cardiovasc Surg 2006;131(2):277-82.
16. McGaugh JL, Introini-Collison IB, Nagahara AH, et al. Involvement of the amygdaloid complex in neuromodulatory influences on memory storage. Neurosci Biobehav Rev 1990;14(4):425-31.
17. Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996;153(2):219-25.
18. Baker DG, West SA, Orth DN, et al. Cerebrospinal fluid and plasma beta-endorphin in combat veterans with post-traumatic stress disorder. Psychoneuroendocrinol 1997;22(7):517-29.
19. Wolf ME, Mosnaim AD, Puente J, Ignacio R. Plasma methionine-enkephalin in PTSD. Biol Psychiatry 1991;29(3):305-7.
20. Saxe G, Stoddard F, Courtney D, et al. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001;40(8):915-21.
21. Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry 1996;153(3):369-75.
22. Zatzick D, Roy-Byrne PP. From bedside to bench: how the epidemiology of clinical practice can inform the secondary prevention of PTSD. Psychiatr Serv 2006;57(12):1726-30.
23. Zatzick D, Jurkovich G, Russo J, et al. Posttraumatic distress, alcohol disorders, and recurrent trauma across level 1 trauma centers. J Trauma 2004;57(2):360-6.
24. Braun P, Greenberg D, Dasberg H, Lerer B. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry 1990;51(6):236-8.
25. Gelpin E, Bonne O, Peri T, et al. Treatment of recent trauma survivors with benzodiazepines: a prospective study. J Clin Psychiatry 1996;57(9):390-4.
26. Mellman TA, Bustamante V, David D, et al. Hypnotic medication in the aftermath of trauma. J Clin Psychiatry 2002;63(12):1183-4.
27. Freedman SA, Brandes D, Peri T, Shalev A. Predictors of chronic post-traumatic stress disorder. A prospective study. Br J Psychiatry 1999;174:353-9.
28. Davidson JR. Pharmacologic treatment of acute and chronic stress following trauma. J Clin Psychiatry 2006;67(suppl 2):34-9.
29. Robert R, Blakeney PE, Villarreal C, et al. Imipramine treatment in pediatric burn patients with symptoms of acute stress disorder: a pilot study. J Am Acad Child Adolesc Psychiatry 1999;38(7):873-82.
30. Morgan CA, Wang S, Southwick SM, et al. Plasma neuropeptide-Y concentrations in humans exposed to military survival training. Biol Psychiatry 2000;47(10):902-9.
31. Geracioti TD, Carpenter LL, Owens MJ, et al. Elevated cerebrospinal fluid substance P concentrations in posttraumatic stress disorder and major depression. Am J Psychiatry 2006;163(4):637-43.
32. Zobel AW, Nickel T, Künzel HE, et al. Effects of the highaffinity corticotropin-releasing hormone receptor 1 antagonist R121919 in major depression: the first 20 patients treated. J Psychiatr Res 2000;34(3):171-81.
33. Davidson JR. Treatment of posttraumatic stress disorder: the impact of paroxetine. Psychopharmacol Bull 2003;37(suppl 1):76-88.
Posttraumatic stress disorder (PTSD) is a preventable mental illness—without trauma, the illness does not occur. Primary prevention (such as eliminating war, rape, physical assaults, child abuse, or motor vehicle accidents) would be effective but is an unrealistic goal. Secondary prevention (such as preventing PTSD after individuals have been exposed to trauma) may be attainable.
No medication is FDA-approved to prevent PTSD, but patients recently exposed to trauma might benefit from drugs approved for other indications. Possibilities include noradrenergics such as propranolol, corticosteroids that affect the hypothalamic-pituitary-adrenal (HPA) axis, opioids, benzodiazepines, and antidepressants. Some investigational agents also might block the process that turns a traumatic experience into PTSD.
This article discusses these intriguing ideas and suggests which trauma victims might benefit now from acute pharmacologic PTSD prevention.
Who might be treated?
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life (Box 1).1,2 A person’s risk of developing PTSD after a traumatic event depends on the type of trauma. For example, 10% of motor vehicle accident survivors develop PTSD, compared with 60% of rape survivors.1
Targeting anyone who has experienced trauma for secondary PTSD prevention would expose large groups of people to medications they do not need. Targeting selected persons who are at the highest risk would be more efficient and cost-effective. In a group of acute trauma-exposed persons, 2 selection criteria could be considered simultaneously:
- Which patients may be most predisposed to PTSD?
- Which patients are showing early symptoms that may predict PTSD?
More than half of all American adults have been exposed to at least one traumatic event at some point in their lives.1 In most persons, the posttraumatic stress reaction causes short-term distress, with hyperarousal, agitation, intrusive memories, and exaggerated startle. Although these symptoms usually subside relatively quickly, they persist and evolve into posttraumatic stress disorder (PTSD) in a substantial number of trauma victims.
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life.2 Emotional distress, social and occupational disability, and persistent decrements in quality of life make PTSD a major public health problem.
Risk factors and resiliency. Certain factors have been shown to increase a person’s vulnerability for PTSD (Table 1).3 Other proposed risk factors include:
- personality types4
- psychophysiologic factors such as reactivity, conditionability, and resistance to extinction/habituation.5
Strong evidence also indicates that acute trauma-related symptoms—including excessive arousal and fear,6 peritraumatic dissociation, and depression—predict the later development of PTSD.
Once identified, individuals predisposed to developing PTSD could be given treatment to increase their resiliency after they have been exposed to trauma. Early evidence suggests that you also could consider giving these patients medications as secondary prevention (Table 2).
Table 1
Who develops PTSD? Risk and resiliency factors
Risk factors that may increase vulnerability for PTSD
|
Resiliency factors that may protect against PTSD
|
| Source: Reference 3 |
Table 2
Medications being studied for PTSD prevention
| Mechanism of action | Medication | FDA-approved indications | ||
|---|---|---|---|---|
| Psychiatric | Nonpsychiatric | |||
| Noradrenergic | Clonidine | No | Yes | |
| Guanfacine | No | Yes | ||
| Prazosin | No | Yes | ||
| Propranolol | No | Yes | ||
| Hypothalamic-pituitary-adrenal axis | Hydrocortisone | No | Yes | |
| Opioid | Morphine | No | Yes | |
| Antidepressant | Dual action | Duloxetine | Yes | Yes |
| Venlafaxine | Yes | No | ||
| SSRIs | Citalopram | Yes | No | |
| Fluoxetine | Yes | No | ||
| Paroxetine | Yes | No | ||
| Sertraline | Yes | No | ||
| TCAs | Amitriptyline | Yes | No | |
| Imipramine | Yes | No | ||
| GABA-benzodiazepine | Alprazolam | Yes | No | |
| Temazepam | Yes | No | ||
| Corticotropin-releasing hormone (CRH) | CRH antagonist | Investigational | ||
| Substance P | Substance P antagonist | Investigational | ||
| Neuropeptide Y | Neuropeptide Y agonist | Investigational | ||
| SSRIs: selective serotonin reuptake inhibitors | ||||
| TCAs: tricyclic antidepressants | ||||
Targeting noradrenergic activity
Increased noradrenergic activity has been associated with persistent memories and PTSD. Therefore, medications that reduce noradrenergic tone by blocking receptors or reduce norepinephrine release are being explored for PTSD prevention.
Propranolol. Three small studies have examined whether the beta-noradrenergic receptor blocker propranolol can prevent PTSD.
In a randomized, double-blind, placebo-controlled trial,7 41 emergency department patients who had a heart rate of ≥ 80 bpm within 6 hours of a traumatic accident received propranolol, 40 mg qid, or placebo for 10 days. After 1 month, the 11 patients who completed propranolol treatment showed a nonsignificant trend toward lower scores on the Clinician-Administered PTSD Scale (CAPS), compared with 20 patients taking placebo. At 3 months, the propranolol group had less physiologic reactivity (as measured by heart rate and skin conductance) to trauma-related cues than the placebo group.
In a nonrandomized study,8 PTSD developed within 2 months in 1 of 11 trauma victims who agreed to take propranolol, 40 mg tid, immediately after the trauma, compared with 3 of 8 victims who refused the medication.
In an unpublished randomized, double-blind trial,9 48 patients admitted to a level I trauma center received propranolol, 40 mg tid; gabapentin, 400 mg tid; or placebo for PTSD prevention. Gabapentin was chosen because it has few side effects or metabolic interactions and preliminary evidence of anxiolytic efficacy.
Neither propranolol nor gabapentin showed statistically significant benefit in preventing PTSD compared with placebo. Effect sizes with the 2 treatments were too small to suggest that larger samples would produce a statistically significant result.
Prazosin—an alpha-1 adrenergic receptor antagonist—has been evaluated in 3 controlled studies and found to reduce intrusive nightmares typical of chronic PTSD.
Ten combat veterans with chronic PTSD showed significantly improved sleep, fewer severe nightmares, and improved global clinical status after receiving prazosin (mean dose 9.5 mg at bedtime) in a 20-week, placebo-controlled, double-blind, crossover study.10
In a larger randomized, parallel group trial,11 the same authors compared prazosin with placebo in 40 combat veterans (mean age 56) with chronic PTSD. After 8 weeks, veterans taking prazosin (mean 13.3 ± 3 mg) had significantly fewer trauma nightmares, improved sleep (including return of normal dreams), and improved global clinical status vs placebo. Overall CAP scores did not decline significantly, however.
In a third placebo-controlled study,12 a midmorning dose of prazosin was added to the regimens of 11 civilian trauma patients already taking the drug at bedtime to suppress trauma-related nightmares. Their daytime PTSD symptoms improved, as shown by reduced psychological distress in response to verbal trauma cues.
Prazosin can reduce chronic PTSD manifestations of nightmares and disturbed sleep, but it has not been shown to ameliorate the full PTSD syndrome. Prazosin has not been studied as an early PTSD intervention.
Other antiadrenergics that reduce the release of norepinephrine—including clonidine and guanfacine—have been studied in open trials as treatment for PTSD. The only controlled study13 showed no benefit from guanfacine for PTSD prevention.
De-stressing the HPA axis
Hydrocortisone has been proposed to prevent PTSD by reducing HPA axis activation, acting as a countermeasure to elevated corticotropin-releasing factor found in patients with chronic PTSD.
IV hydrocortisone’s effect on the development of PTSD was compared with placebo in 20 septic shock survivors after discharge from intensive care.14 One of 9 patients (11%) in the hydrocortisone group was diagnosed with PTSD at follow-up (mean 31 months), compared with 7 of 11 (64%) in the placebo group.
In a similar study, the same researchers gave patients hydrocortisone before, during, and after cardiac surgery. Follow-up interviews revealed significantly lower PTSD and chronic stress symptom scores in the treatment group vs the placebo group.15
These studies—although provocative—are limited by the narrow range of trauma related to severe medical illness or extensive medical procedures.
Norepinephrine-blocking opioids
When the noradrenergic system is activated, one physiologic response is the activation of endogenous opioid systems, which may promote recovery by inhibiting the HPA axis. Opioid systems might be involved in PTSD, as suggested by:
- preclinical evidence that opioids modulate memory16
- studies showing low pain thresholds17 and abnormal beta-endorphin (an opioid peptide neurotransmitter)18 and methionine enkephalin (an opioid peptide)19 levels in PTSD patients.
In theory, opioid administration immediately after trauma may attenuate norepinephrine release, thus thwarting arousal-charged memory consolidation, hyperarousal, and re-experiencing.
One uncontrolled report of pediatric burn victims found a significant association between the morphine dose given for pain during hospitalization and reduced PTSD symptoms 6 months later.20 Decreased pain did not explain the reduction in PTSD, as no significant correlation was seen between pain symptoms and PTSD outcome measures. Similarly, a longitudinal study of substance use among Vietnam War veterans with PTSD found decreased hyperarousal symptoms in heroin users.21
Using opioids to prevent PTSD would be feasible and efficient in acute care settings because 80% to 90% of traumatically-injured patients are discharged on opioid analgesics (compared with <10% on beta blockers or corticosteroids).22 However, 20% to 40% of physically injured inpatients are diagnosed with a substance use disorder at some point in life, making the use of opioid analgesics a practical concern.23
GABA-benzodiazepine paradox
The GABA-benzodiazepine system plays an important role in mediating anxiety, which is consistent with the potent anxiolytic effects of benzodiazepines. Even so, trials of benzodiazepines have found these drugs surprisingly unhelpful—and perhaps harmful—in patients with acute trauma.
Alprazolam did not reduce PTSD symptoms in a small randomized, double-blind study.24 Another trial found that receiving benzodiazepines shortly after trauma exposure was associated with increased PTSD risk in trauma survivors. Nine of 13 patients (69%) who received alprazolam or clonazepam met PTSD diagnostic criteria 6 months after the trauma, compared with 3 of 13 controls (15%).25
Similarly, in a randomized controlled trial, 22 patients were given temazepam for 7 nights, starting approximately 14 days after exposure to a traumatic event. Six weeks later, 55% of those receiving temazepam and 27% of those receiving placebo met criteria for PTSD.26
In summary, benzodiazepines might be helpful when given for a few days after traumatization to control overwhelming anxiety but could be harmful over a longer term.
Other agents for PTSD
Antidepressants. Early trauma-related symptoms of depression predict later development of PTSD.27 Thus, antidepressants have been proposed for early intervention in addition to their well-established role as first-line treatment of PTSD.28
One study supports this idea: a 7-day randomized double-blind trial that compared the tricyclic antidepressant imipramine with chloral hydrate in pediatric burn patients with acute stress disorder (ASD). Imipramine was more effective (83% response) than chloral hydrate (38% response) in reducing ASD symptoms.29
Drugs in development. Three new medications being explored for treating anxiety and depression also might be useful for PTSD prevention. Neuropeptide Y (NPY) agonists,30 substance P antagonists,31 and CRH-antagonists32 are thought to hold promise because of their more proximate roles—compared with monoamine neurotransmitters such as dopamine, norepinephrine and serotonin—in mediating the stress response.
Manage the post-trauma environment:
- Move the victim to safety.
- Treat pain effectively.
- Avoid stress from interrogations, separation from loved ones, or unstable housing.
Avoid crisis incident stress debriefing (CISD), which could enhance physiologic hyperarousal and is not recommended as first-line treatment for most trauma victims. CISD was designed for and is best received by emergency personnel.
Consider prescribing antidepressants for patients thought to be particularly vulnerable to develop posttraumatic stress disorder (PTSD). Risk factors include:
- history of PTSD, depression, or anxiety disorder
- severe trauma (such as from sexual assault or torture)
- physical injury, when antidepressants with analgesic properties might be useful.
Analyzing the evidence
Insufficient evidence exists to determine which strategies might be most effective to prevent PTSD, what optimal dosing might be, and which traumatized individuals might be best targeted with these approaches.
- Beta-blockers and corticosteroids—the most theoretically compelling strategies—are the most difficult agents to use for PTSD prevention because they have the most medical contraindications. In addition, evidence supporting their ability to prevent PTSD is meager at best.
- Prazosin is intriguing but has contra-indications similar to those of beta blockers, no studies of secondary prevention, and no clear indication that it works for the overall PTSD syndrome.
- Opioids are restricted agents with substantial contraindications.
- Evidence is limited but points most strongly toward earlier use of antidepressants. Early trauma-related symptoms of depression predict later development of PTSD,27 and a number of selective serotonin reuptake inhibitors—such as citalopram, fluoxetine, paroxetine, and sertraline—are FDA-approved or used off-label for treating PTSD.33
Prescribing recommendations. Consider practicality, ease of use, and safety of the proposed medication when choosing a drug for PTSD prevention (Table 3).22 Based on the evidence, the most reasonable posttrauma approach (Box 2) might be to consider starting an approved antidepressant for individuals thought to be particularly vulnerable to PTSD because of:
- past history of PTSD, depression, or anxiety disorder
- severity of the trauma (such as in cases of sexual assault or torture)
- pain (antidepressants with analgesic properties—such as venlafaxine or duloxetine—might be useful in patients whose trauma is associated with physical injury, although neither is FDA-approved to treat PTSD).
Table 3
4 considerations when choosing a drug for PTSD prevention
| Potential benefits | Practicality, ease of use, and safety of the proposed medication |
| Potential drug-drug or drug-disease interactions | Asthma, diabetes, and trauma are relative contraindications to the use of antiadrenergics and corticosteroids |
| Psychiatric comorbidities | A patient’s history of substance use disorder makes opioid analgesics a concern |
| Clinical experience | Agents already prescribed safely and broadly in clinical practice are easiest to test and to use |
Related resources
- Mental health and mass violence: Evidence-based early psychological intervention for victims/survivors of mass violence. A workshop to reach consensus on best practices. Rockland, MD: National Institute of Mental Health; 2002. www.nimh.nih.gov.
- Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care (clinical guideline 26). London, UK: National Institute for Clinical Excellence; 2005. www.nice.org.uk.
- Ursano RJ, Bell C, Eth S, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry 2004;161(suppl 11):3-31.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clonidine • Catapres
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Guanfacine • Tenex
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Paroxetine • Paxil
- Prazosin • Minipress
- Propranolol • Inderal
- Sertraline • Zoloft
- Temazepam • Restoril
- Venlafaxine • Effexor
Disclosure
Dr. Bennett and Dr. Zatzick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Roy-Byrne is a consultant to Jazz Pharmaceuticals and Solvay and has received speaker honoraria from Wyeth and Forrest Pharmaceuticals.
Posttraumatic stress disorder (PTSD) is a preventable mental illness—without trauma, the illness does not occur. Primary prevention (such as eliminating war, rape, physical assaults, child abuse, or motor vehicle accidents) would be effective but is an unrealistic goal. Secondary prevention (such as preventing PTSD after individuals have been exposed to trauma) may be attainable.
No medication is FDA-approved to prevent PTSD, but patients recently exposed to trauma might benefit from drugs approved for other indications. Possibilities include noradrenergics such as propranolol, corticosteroids that affect the hypothalamic-pituitary-adrenal (HPA) axis, opioids, benzodiazepines, and antidepressants. Some investigational agents also might block the process that turns a traumatic experience into PTSD.
This article discusses these intriguing ideas and suggests which trauma victims might benefit now from acute pharmacologic PTSD prevention.
Who might be treated?
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life (Box 1).1,2 A person’s risk of developing PTSD after a traumatic event depends on the type of trauma. For example, 10% of motor vehicle accident survivors develop PTSD, compared with 60% of rape survivors.1
Targeting anyone who has experienced trauma for secondary PTSD prevention would expose large groups of people to medications they do not need. Targeting selected persons who are at the highest risk would be more efficient and cost-effective. In a group of acute trauma-exposed persons, 2 selection criteria could be considered simultaneously:
- Which patients may be most predisposed to PTSD?
- Which patients are showing early symptoms that may predict PTSD?
More than half of all American adults have been exposed to at least one traumatic event at some point in their lives.1 In most persons, the posttraumatic stress reaction causes short-term distress, with hyperarousal, agitation, intrusive memories, and exaggerated startle. Although these symptoms usually subside relatively quickly, they persist and evolve into posttraumatic stress disorder (PTSD) in a substantial number of trauma victims.
An estimated 8% to 10% of the U.S. population experiences PTSD at some point in life.2 Emotional distress, social and occupational disability, and persistent decrements in quality of life make PTSD a major public health problem.
Risk factors and resiliency. Certain factors have been shown to increase a person’s vulnerability for PTSD (Table 1).3 Other proposed risk factors include:
- personality types4
- psychophysiologic factors such as reactivity, conditionability, and resistance to extinction/habituation.5
Strong evidence also indicates that acute trauma-related symptoms—including excessive arousal and fear,6 peritraumatic dissociation, and depression—predict the later development of PTSD.
Once identified, individuals predisposed to developing PTSD could be given treatment to increase their resiliency after they have been exposed to trauma. Early evidence suggests that you also could consider giving these patients medications as secondary prevention (Table 2).
Table 1
Who develops PTSD? Risk and resiliency factors
Risk factors that may increase vulnerability for PTSD
|
Resiliency factors that may protect against PTSD
|
| Source: Reference 3 |
Table 2
Medications being studied for PTSD prevention
| Mechanism of action | Medication | FDA-approved indications | ||
|---|---|---|---|---|
| Psychiatric | Nonpsychiatric | |||
| Noradrenergic | Clonidine | No | Yes | |
| Guanfacine | No | Yes | ||
| Prazosin | No | Yes | ||
| Propranolol | No | Yes | ||
| Hypothalamic-pituitary-adrenal axis | Hydrocortisone | No | Yes | |
| Opioid | Morphine | No | Yes | |
| Antidepressant | Dual action | Duloxetine | Yes | Yes |
| Venlafaxine | Yes | No | ||
| SSRIs | Citalopram | Yes | No | |
| Fluoxetine | Yes | No | ||
| Paroxetine | Yes | No | ||
| Sertraline | Yes | No | ||
| TCAs | Amitriptyline | Yes | No | |
| Imipramine | Yes | No | ||
| GABA-benzodiazepine | Alprazolam | Yes | No | |
| Temazepam | Yes | No | ||
| Corticotropin-releasing hormone (CRH) | CRH antagonist | Investigational | ||
| Substance P | Substance P antagonist | Investigational | ||
| Neuropeptide Y | Neuropeptide Y agonist | Investigational | ||
| SSRIs: selective serotonin reuptake inhibitors | ||||
| TCAs: tricyclic antidepressants | ||||
Targeting noradrenergic activity
Increased noradrenergic activity has been associated with persistent memories and PTSD. Therefore, medications that reduce noradrenergic tone by blocking receptors or reduce norepinephrine release are being explored for PTSD prevention.
Propranolol. Three small studies have examined whether the beta-noradrenergic receptor blocker propranolol can prevent PTSD.
In a randomized, double-blind, placebo-controlled trial,7 41 emergency department patients who had a heart rate of ≥ 80 bpm within 6 hours of a traumatic accident received propranolol, 40 mg qid, or placebo for 10 days. After 1 month, the 11 patients who completed propranolol treatment showed a nonsignificant trend toward lower scores on the Clinician-Administered PTSD Scale (CAPS), compared with 20 patients taking placebo. At 3 months, the propranolol group had less physiologic reactivity (as measured by heart rate and skin conductance) to trauma-related cues than the placebo group.
In a nonrandomized study,8 PTSD developed within 2 months in 1 of 11 trauma victims who agreed to take propranolol, 40 mg tid, immediately after the trauma, compared with 3 of 8 victims who refused the medication.
In an unpublished randomized, double-blind trial,9 48 patients admitted to a level I trauma center received propranolol, 40 mg tid; gabapentin, 400 mg tid; or placebo for PTSD prevention. Gabapentin was chosen because it has few side effects or metabolic interactions and preliminary evidence of anxiolytic efficacy.
Neither propranolol nor gabapentin showed statistically significant benefit in preventing PTSD compared with placebo. Effect sizes with the 2 treatments were too small to suggest that larger samples would produce a statistically significant result.
Prazosin—an alpha-1 adrenergic receptor antagonist—has been evaluated in 3 controlled studies and found to reduce intrusive nightmares typical of chronic PTSD.
Ten combat veterans with chronic PTSD showed significantly improved sleep, fewer severe nightmares, and improved global clinical status after receiving prazosin (mean dose 9.5 mg at bedtime) in a 20-week, placebo-controlled, double-blind, crossover study.10
In a larger randomized, parallel group trial,11 the same authors compared prazosin with placebo in 40 combat veterans (mean age 56) with chronic PTSD. After 8 weeks, veterans taking prazosin (mean 13.3 ± 3 mg) had significantly fewer trauma nightmares, improved sleep (including return of normal dreams), and improved global clinical status vs placebo. Overall CAP scores did not decline significantly, however.
In a third placebo-controlled study,12 a midmorning dose of prazosin was added to the regimens of 11 civilian trauma patients already taking the drug at bedtime to suppress trauma-related nightmares. Their daytime PTSD symptoms improved, as shown by reduced psychological distress in response to verbal trauma cues.
Prazosin can reduce chronic PTSD manifestations of nightmares and disturbed sleep, but it has not been shown to ameliorate the full PTSD syndrome. Prazosin has not been studied as an early PTSD intervention.
Other antiadrenergics that reduce the release of norepinephrine—including clonidine and guanfacine—have been studied in open trials as treatment for PTSD. The only controlled study13 showed no benefit from guanfacine for PTSD prevention.
De-stressing the HPA axis
Hydrocortisone has been proposed to prevent PTSD by reducing HPA axis activation, acting as a countermeasure to elevated corticotropin-releasing factor found in patients with chronic PTSD.
IV hydrocortisone’s effect on the development of PTSD was compared with placebo in 20 septic shock survivors after discharge from intensive care.14 One of 9 patients (11%) in the hydrocortisone group was diagnosed with PTSD at follow-up (mean 31 months), compared with 7 of 11 (64%) in the placebo group.
In a similar study, the same researchers gave patients hydrocortisone before, during, and after cardiac surgery. Follow-up interviews revealed significantly lower PTSD and chronic stress symptom scores in the treatment group vs the placebo group.15
These studies—although provocative—are limited by the narrow range of trauma related to severe medical illness or extensive medical procedures.
Norepinephrine-blocking opioids
When the noradrenergic system is activated, one physiologic response is the activation of endogenous opioid systems, which may promote recovery by inhibiting the HPA axis. Opioid systems might be involved in PTSD, as suggested by:
- preclinical evidence that opioids modulate memory16
- studies showing low pain thresholds17 and abnormal beta-endorphin (an opioid peptide neurotransmitter)18 and methionine enkephalin (an opioid peptide)19 levels in PTSD patients.
In theory, opioid administration immediately after trauma may attenuate norepinephrine release, thus thwarting arousal-charged memory consolidation, hyperarousal, and re-experiencing.
One uncontrolled report of pediatric burn victims found a significant association between the morphine dose given for pain during hospitalization and reduced PTSD symptoms 6 months later.20 Decreased pain did not explain the reduction in PTSD, as no significant correlation was seen between pain symptoms and PTSD outcome measures. Similarly, a longitudinal study of substance use among Vietnam War veterans with PTSD found decreased hyperarousal symptoms in heroin users.21
Using opioids to prevent PTSD would be feasible and efficient in acute care settings because 80% to 90% of traumatically-injured patients are discharged on opioid analgesics (compared with <10% on beta blockers or corticosteroids).22 However, 20% to 40% of physically injured inpatients are diagnosed with a substance use disorder at some point in life, making the use of opioid analgesics a practical concern.23
GABA-benzodiazepine paradox
The GABA-benzodiazepine system plays an important role in mediating anxiety, which is consistent with the potent anxiolytic effects of benzodiazepines. Even so, trials of benzodiazepines have found these drugs surprisingly unhelpful—and perhaps harmful—in patients with acute trauma.
Alprazolam did not reduce PTSD symptoms in a small randomized, double-blind study.24 Another trial found that receiving benzodiazepines shortly after trauma exposure was associated with increased PTSD risk in trauma survivors. Nine of 13 patients (69%) who received alprazolam or clonazepam met PTSD diagnostic criteria 6 months after the trauma, compared with 3 of 13 controls (15%).25
Similarly, in a randomized controlled trial, 22 patients were given temazepam for 7 nights, starting approximately 14 days after exposure to a traumatic event. Six weeks later, 55% of those receiving temazepam and 27% of those receiving placebo met criteria for PTSD.26
In summary, benzodiazepines might be helpful when given for a few days after traumatization to control overwhelming anxiety but could be harmful over a longer term.
Other agents for PTSD
Antidepressants. Early trauma-related symptoms of depression predict later development of PTSD.27 Thus, antidepressants have been proposed for early intervention in addition to their well-established role as first-line treatment of PTSD.28
One study supports this idea: a 7-day randomized double-blind trial that compared the tricyclic antidepressant imipramine with chloral hydrate in pediatric burn patients with acute stress disorder (ASD). Imipramine was more effective (83% response) than chloral hydrate (38% response) in reducing ASD symptoms.29
Drugs in development. Three new medications being explored for treating anxiety and depression also might be useful for PTSD prevention. Neuropeptide Y (NPY) agonists,30 substance P antagonists,31 and CRH-antagonists32 are thought to hold promise because of their more proximate roles—compared with monoamine neurotransmitters such as dopamine, norepinephrine and serotonin—in mediating the stress response.
Manage the post-trauma environment:
- Move the victim to safety.
- Treat pain effectively.
- Avoid stress from interrogations, separation from loved ones, or unstable housing.
Avoid crisis incident stress debriefing (CISD), which could enhance physiologic hyperarousal and is not recommended as first-line treatment for most trauma victims. CISD was designed for and is best received by emergency personnel.
Consider prescribing antidepressants for patients thought to be particularly vulnerable to develop posttraumatic stress disorder (PTSD). Risk factors include:
- history of PTSD, depression, or anxiety disorder
- severe trauma (such as from sexual assault or torture)
- physical injury, when antidepressants with analgesic properties might be useful.
Analyzing the evidence
Insufficient evidence exists to determine which strategies might be most effective to prevent PTSD, what optimal dosing might be, and which traumatized individuals might be best targeted with these approaches.
- Beta-blockers and corticosteroids—the most theoretically compelling strategies—are the most difficult agents to use for PTSD prevention because they have the most medical contraindications. In addition, evidence supporting their ability to prevent PTSD is meager at best.
- Prazosin is intriguing but has contra-indications similar to those of beta blockers, no studies of secondary prevention, and no clear indication that it works for the overall PTSD syndrome.
- Opioids are restricted agents with substantial contraindications.
- Evidence is limited but points most strongly toward earlier use of antidepressants. Early trauma-related symptoms of depression predict later development of PTSD,27 and a number of selective serotonin reuptake inhibitors—such as citalopram, fluoxetine, paroxetine, and sertraline—are FDA-approved or used off-label for treating PTSD.33
Prescribing recommendations. Consider practicality, ease of use, and safety of the proposed medication when choosing a drug for PTSD prevention (Table 3).22 Based on the evidence, the most reasonable posttrauma approach (Box 2) might be to consider starting an approved antidepressant for individuals thought to be particularly vulnerable to PTSD because of:
- past history of PTSD, depression, or anxiety disorder
- severity of the trauma (such as in cases of sexual assault or torture)
- pain (antidepressants with analgesic properties—such as venlafaxine or duloxetine—might be useful in patients whose trauma is associated with physical injury, although neither is FDA-approved to treat PTSD).
Table 3
4 considerations when choosing a drug for PTSD prevention
| Potential benefits | Practicality, ease of use, and safety of the proposed medication |
| Potential drug-drug or drug-disease interactions | Asthma, diabetes, and trauma are relative contraindications to the use of antiadrenergics and corticosteroids |
| Psychiatric comorbidities | A patient’s history of substance use disorder makes opioid analgesics a concern |
| Clinical experience | Agents already prescribed safely and broadly in clinical practice are easiest to test and to use |
Related resources
- Mental health and mass violence: Evidence-based early psychological intervention for victims/survivors of mass violence. A workshop to reach consensus on best practices. Rockland, MD: National Institute of Mental Health; 2002. www.nimh.nih.gov.
- Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care (clinical guideline 26). London, UK: National Institute for Clinical Excellence; 2005. www.nice.org.uk.
- Ursano RJ, Bell C, Eth S, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry 2004;161(suppl 11):3-31.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clonidine • Catapres
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Guanfacine • Tenex
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Paroxetine • Paxil
- Prazosin • Minipress
- Propranolol • Inderal
- Sertraline • Zoloft
- Temazepam • Restoril
- Venlafaxine • Effexor
Disclosure
Dr. Bennett and Dr. Zatzick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Roy-Byrne is a consultant to Jazz Pharmaceuticals and Solvay and has received speaker honoraria from Wyeth and Forrest Pharmaceuticals.
1. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52(12):1048-60.
2. Zatzick D. Posttraumatic stress, functional impairment, and service utilization after injury: a public health approach. Semin Clin Neuropsychiatry 2003;8(3):149-57.
3. Yehuda R, Flory JD, Southwick S, Charney DS. Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Ann NY Acad Sci 2006;1071:379-96.
4. Schnurr P, Vielhauer M. Personality as a risk factor for PTSD. In: Yehuda R, ed. Risk factors for post-traumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1999:191-222.
5. Shalev A. Psychophysiological expression of risk factors for PTSD. In: Yehuda R, ed. Risk factors for posttraumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1995.
6. Bryant RA, Harvey AG, Guthrie RM, Moulds ML. A prospective study of psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol 2000;109(2):341-4.
7. Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol Psychiatry 2002;51(2):189-92.
8. Vaiva G, Ducrocq F, Jezequel K, et al. Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma. Biol Psychiatry 2003;54(9):947-9.
9. Stein M. Pharmacoprevention of adverse psychiatric sequelae of physical injury. Paper presented at: 21st Annual Meeting of the International Society for Traumatic Stress Studies; November 2-5, 2005; Toronto, Ontario, Canada.
10. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
11. Raskind MA, Peskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry 2007;61(8):928-34.
12. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry 2006;59(7):577-81.
13. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry 2006;163(12):2186-8.
14. Schelling G, Briegel J, Roozendaal B, et al. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biol Psychiatry 2001;50(12):978-85.
15. Weis F, Kilger E, Roozendaal B, et al. Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: a randomized study. J Thorac Cardiovasc Surg 2006;131(2):277-82.
16. McGaugh JL, Introini-Collison IB, Nagahara AH, et al. Involvement of the amygdaloid complex in neuromodulatory influences on memory storage. Neurosci Biobehav Rev 1990;14(4):425-31.
17. Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996;153(2):219-25.
18. Baker DG, West SA, Orth DN, et al. Cerebrospinal fluid and plasma beta-endorphin in combat veterans with post-traumatic stress disorder. Psychoneuroendocrinol 1997;22(7):517-29.
19. Wolf ME, Mosnaim AD, Puente J, Ignacio R. Plasma methionine-enkephalin in PTSD. Biol Psychiatry 1991;29(3):305-7.
20. Saxe G, Stoddard F, Courtney D, et al. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001;40(8):915-21.
21. Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry 1996;153(3):369-75.
22. Zatzick D, Roy-Byrne PP. From bedside to bench: how the epidemiology of clinical practice can inform the secondary prevention of PTSD. Psychiatr Serv 2006;57(12):1726-30.
23. Zatzick D, Jurkovich G, Russo J, et al. Posttraumatic distress, alcohol disorders, and recurrent trauma across level 1 trauma centers. J Trauma 2004;57(2):360-6.
24. Braun P, Greenberg D, Dasberg H, Lerer B. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry 1990;51(6):236-8.
25. Gelpin E, Bonne O, Peri T, et al. Treatment of recent trauma survivors with benzodiazepines: a prospective study. J Clin Psychiatry 1996;57(9):390-4.
26. Mellman TA, Bustamante V, David D, et al. Hypnotic medication in the aftermath of trauma. J Clin Psychiatry 2002;63(12):1183-4.
27. Freedman SA, Brandes D, Peri T, Shalev A. Predictors of chronic post-traumatic stress disorder. A prospective study. Br J Psychiatry 1999;174:353-9.
28. Davidson JR. Pharmacologic treatment of acute and chronic stress following trauma. J Clin Psychiatry 2006;67(suppl 2):34-9.
29. Robert R, Blakeney PE, Villarreal C, et al. Imipramine treatment in pediatric burn patients with symptoms of acute stress disorder: a pilot study. J Am Acad Child Adolesc Psychiatry 1999;38(7):873-82.
30. Morgan CA, Wang S, Southwick SM, et al. Plasma neuropeptide-Y concentrations in humans exposed to military survival training. Biol Psychiatry 2000;47(10):902-9.
31. Geracioti TD, Carpenter LL, Owens MJ, et al. Elevated cerebrospinal fluid substance P concentrations in posttraumatic stress disorder and major depression. Am J Psychiatry 2006;163(4):637-43.
32. Zobel AW, Nickel T, Künzel HE, et al. Effects of the highaffinity corticotropin-releasing hormone receptor 1 antagonist R121919 in major depression: the first 20 patients treated. J Psychiatr Res 2000;34(3):171-81.
33. Davidson JR. Treatment of posttraumatic stress disorder: the impact of paroxetine. Psychopharmacol Bull 2003;37(suppl 1):76-88.
1. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52(12):1048-60.
2. Zatzick D. Posttraumatic stress, functional impairment, and service utilization after injury: a public health approach. Semin Clin Neuropsychiatry 2003;8(3):149-57.
3. Yehuda R, Flory JD, Southwick S, Charney DS. Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Ann NY Acad Sci 2006;1071:379-96.
4. Schnurr P, Vielhauer M. Personality as a risk factor for PTSD. In: Yehuda R, ed. Risk factors for post-traumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1999:191-222.
5. Shalev A. Psychophysiological expression of risk factors for PTSD. In: Yehuda R, ed. Risk factors for posttraumatic stress disorder. Washington, DC: American Psychiatric Publishing; 1995.
6. Bryant RA, Harvey AG, Guthrie RM, Moulds ML. A prospective study of psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol 2000;109(2):341-4.
7. Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol Psychiatry 2002;51(2):189-92.
8. Vaiva G, Ducrocq F, Jezequel K, et al. Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma. Biol Psychiatry 2003;54(9):947-9.
9. Stein M. Pharmacoprevention of adverse psychiatric sequelae of physical injury. Paper presented at: 21st Annual Meeting of the International Society for Traumatic Stress Studies; November 2-5, 2005; Toronto, Ontario, Canada.
10. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
11. Raskind MA, Peskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry 2007;61(8):928-34.
12. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry 2006;59(7):577-81.
13. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry 2006;163(12):2186-8.
14. Schelling G, Briegel J, Roozendaal B, et al. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biol Psychiatry 2001;50(12):978-85.
15. Weis F, Kilger E, Roozendaal B, et al. Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: a randomized study. J Thorac Cardiovasc Surg 2006;131(2):277-82.
16. McGaugh JL, Introini-Collison IB, Nagahara AH, et al. Involvement of the amygdaloid complex in neuromodulatory influences on memory storage. Neurosci Biobehav Rev 1990;14(4):425-31.
17. Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996;153(2):219-25.
18. Baker DG, West SA, Orth DN, et al. Cerebrospinal fluid and plasma beta-endorphin in combat veterans with post-traumatic stress disorder. Psychoneuroendocrinol 1997;22(7):517-29.
19. Wolf ME, Mosnaim AD, Puente J, Ignacio R. Plasma methionine-enkephalin in PTSD. Biol Psychiatry 1991;29(3):305-7.
20. Saxe G, Stoddard F, Courtney D, et al. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001;40(8):915-21.
21. Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry 1996;153(3):369-75.
22. Zatzick D, Roy-Byrne PP. From bedside to bench: how the epidemiology of clinical practice can inform the secondary prevention of PTSD. Psychiatr Serv 2006;57(12):1726-30.
23. Zatzick D, Jurkovich G, Russo J, et al. Posttraumatic distress, alcohol disorders, and recurrent trauma across level 1 trauma centers. J Trauma 2004;57(2):360-6.
24. Braun P, Greenberg D, Dasberg H, Lerer B. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry 1990;51(6):236-8.
25. Gelpin E, Bonne O, Peri T, et al. Treatment of recent trauma survivors with benzodiazepines: a prospective study. J Clin Psychiatry 1996;57(9):390-4.
26. Mellman TA, Bustamante V, David D, et al. Hypnotic medication in the aftermath of trauma. J Clin Psychiatry 2002;63(12):1183-4.
27. Freedman SA, Brandes D, Peri T, Shalev A. Predictors of chronic post-traumatic stress disorder. A prospective study. Br J Psychiatry 1999;174:353-9.
28. Davidson JR. Pharmacologic treatment of acute and chronic stress following trauma. J Clin Psychiatry 2006;67(suppl 2):34-9.
29. Robert R, Blakeney PE, Villarreal C, et al. Imipramine treatment in pediatric burn patients with symptoms of acute stress disorder: a pilot study. J Am Acad Child Adolesc Psychiatry 1999;38(7):873-82.
30. Morgan CA, Wang S, Southwick SM, et al. Plasma neuropeptide-Y concentrations in humans exposed to military survival training. Biol Psychiatry 2000;47(10):902-9.
31. Geracioti TD, Carpenter LL, Owens MJ, et al. Elevated cerebrospinal fluid substance P concentrations in posttraumatic stress disorder and major depression. Am J Psychiatry 2006;163(4):637-43.
32. Zobel AW, Nickel T, Künzel HE, et al. Effects of the highaffinity corticotropin-releasing hormone receptor 1 antagonist R121919 in major depression: the first 20 patients treated. J Psychiatr Res 2000;34(3):171-81.
33. Davidson JR. Treatment of posttraumatic stress disorder: the impact of paroxetine. Psychopharmacol Bull 2003;37(suppl 1):76-88.
2008 codes include means to specify severity of dysplasia
Vaginal, vulvar conditions: Simpler reporting
This year’s additions include codes for vaginal intraepithelial neoplasia (VAIN) and expansion of the vulvar intraepithelial neoplasia (VIN) category to match.
| 624.01 | Vulvar intraepithelial neoplasia I [VIN I] |
| Mild dysplasia of vulva | |
| 624.02 | Vulvar intraepithelial neoplasia II [VIN II] |
| Moderate dysplasia of vulva | |
| 624.09 | Other dystrophy of vulva |
| Kraurosis of vulva | |
| Leukoplakia of vulva | |
| 233.30 | Unspecified female genital organ |
| 233.31 | Vagina |
| Severe dysplasia of vagina | |
| Vaginal intraepithelial neoplasia III [VAIN III] | |
| 233.32 | Vulva |
| Severe dysplasia of vulva | |
| Vulvar intraepithelial neoplasia III [VIN III] | |
| 233.39 | Other female genital organ |
An “excludes” note has also been added to 622.1 [dysplasia of cervix (uteri)] to clarify that a diagnosis of carcinoma in situ I or II may not be reported unless this diagnosis is assigned based on a biopsy finding—not on an abnormal finding on a Pap smear.
New code for trauma during delivery
Anal sphincter tears can occur during delivery without an accompanying third-degree perineal laceration, so a new code [664.6X, anal sphincter tear complicating delivery, not associated with third-degree perineal laceration] has been added to capture this information. Keep in mind these important points:
- Report the new code when an anal tear is noted at or after delivery. The only acceptable fifth digits for this code are 0 [unspecified as to episode of care or not applicable], 1 [delivered, with or without mention of antepartum condition], or 4 [postpartum condition or complication].
- Report the established code, 664.2X [third-degree perineal laceration] if an anal tear is noted in addition to a third-degree perineal tear. The fifth digit will be 0, 1, or 4, as it is with the code for an anal sphincter tear.
- Report the established code 654.8X [congenital or acquired abnormality of vulva] if the patient had an anal tear from a prior pregnancy, before the current delivery.
- Last, report the new code 569.43 [anal sphincter tear (healed) (old)] if you observe that the patient has an old anal tear but isn’t pregnant. Report an additional code for any associated fecal incontinence (787.6).
Report dysplasia follow-up as “medical necessity”
Once a patient has been treated for cervical dysplasia, long-term follow-up care is required to test for recurrence. The only code available to report that history last year was V13.29, a general code that reported all types of genital systems and obstetric disorders. This year, you can specify and report V13.22 [personal history of cervical dysplasia].
The role of human papillomavirus (HPV) as the cause of cervical cancer is well known, and routine screening tests for this infection are generally as accurate as a routine Pap smear. Because of this, a new code, V73.81 [human papillomavirus (HPV)], has been added to document encounters for HPV screening. The new code can be reported in conjunction with the routine gyn exam code, V72.31, or V76.2 [special screening for malignant neoplasm of cervix] to signal that additional screening is planned.
Better documentation of malignant ascites
789.51 Malignant ascites
789.59 Other ascites
Malignant ascites is seen most often in ovarian, endometrial, breast, colon, gastric, and pancreatic cancer. Management of this condition may include systemic chemotherapy, instillation of radioisotopes or chemotherapy drugs into peritoneal fluid, and peritoneal–venous shunting procedures.
Before October 1, under ICD-9 rules, malignant ascites could be reported only using the code 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].The problem is that this condition can also be caused by a primary ovarian malignancy, for which there has been no reporting mechanism. With expansion of the code 789.5 [ascites], you can specify the type of malignant ascites.
Note: Instructions in ICD-9 indicate that you should list a code for the site of the current malignancy first, such as 183.0 [malignant neoplasm of ovary] or 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].
Assisted reproductive fertility procedure status
Every endocrinologist is aware that assisted reproductive fertility procedures are a multistage undertaking. A number of pretreatment diagnostic tests are independent of the procedure itself, and payers might cover such tests if there were a way to identify patients who were undergoing a procedure from those who were still undergoing pretreatment testing.
Before October 1, only one code, V26.8 [other specified procreative management], was available. Starting this month, to identify a patient undergoing treatment, use V26.81 [encounter for assisted reproductive fertility procedure cycle], with an additional code to identify the type of infertility. With this expansion, a second code was added to capture “other specified procreative management” [V26.89].
Natural family planning comes of age
Natural family planning helps a couple determine when sexual intercourse is likely to (and not likely to) result in pregnancy. It encompasses provider counseling and education on either of two acceptable methods: tracking ovulation by examining cervical mucus or temperature charting. ICD-9 has expanded the existing code, V26.4, to capture this means of family planning more accurately:
V26.41 Procreative counseling and advice using natural family planning
In addition, a code was added to the contraceptive counseling codes to capture this approach as well:
V25.04 Counseling and instruction in natural family planning to avoid pregnancy
Last, a new code also covers other types of procreative management counseling and advice:
V26.49 Other procreative management counseling and advice
Disability certificates, made easy(ier) to report
Do patients come to you to have medical forms and certificates completed? Now you can be more specific, when coding, about the type of document you’re asked to fill out.
V68.01 Disability examination
V68.09 Other issue of medical certificates
The old code, V68.0, was a catch-all of medical certificates, including cause of death, fitness, and disability. The new codes distinguish a certificate for a disability examination from the rest of the pack. That’s a useful change because insurers and state disability programs often reimburse for a disability exam.
Remember: You still need to identify the specific exam, screening, or testing performed by using a code from the series V72.0–V82.9 as a secondary diagnosis. Examples: V72.31 for a gyn exam and V81.6 [screening for other and unspecified genitourinary conditions].
Diversified codes for iatrogenic ID complications
Patients sometimes develop infection in the presence of a central venous catheter or after injection or vaccination. Previously, you used code 999.3 to report such a complication, but that code lumped into one all reasons for infection.
This year, a new code, 993.31, exclusively covers infection caused by a central venous catheter. The code lists several catheter types—Hickman, peripherally inserted central catheter (PICC), triplelumen catheter—and makes clear that it should not be used to report infection caused by a urinary (996.64), arterial (996.62), venous (996.62), or unspecified type of catheter (996.69).
An additional code, 999.39, has been added to report all infections after intravenous infusion, injection, transfusion, or vaccination.
Vaginal, vulvar conditions: Simpler reporting
This year’s additions include codes for vaginal intraepithelial neoplasia (VAIN) and expansion of the vulvar intraepithelial neoplasia (VIN) category to match.
| 624.01 | Vulvar intraepithelial neoplasia I [VIN I] |
| Mild dysplasia of vulva | |
| 624.02 | Vulvar intraepithelial neoplasia II [VIN II] |
| Moderate dysplasia of vulva | |
| 624.09 | Other dystrophy of vulva |
| Kraurosis of vulva | |
| Leukoplakia of vulva | |
| 233.30 | Unspecified female genital organ |
| 233.31 | Vagina |
| Severe dysplasia of vagina | |
| Vaginal intraepithelial neoplasia III [VAIN III] | |
| 233.32 | Vulva |
| Severe dysplasia of vulva | |
| Vulvar intraepithelial neoplasia III [VIN III] | |
| 233.39 | Other female genital organ |
An “excludes” note has also been added to 622.1 [dysplasia of cervix (uteri)] to clarify that a diagnosis of carcinoma in situ I or II may not be reported unless this diagnosis is assigned based on a biopsy finding—not on an abnormal finding on a Pap smear.
New code for trauma during delivery
Anal sphincter tears can occur during delivery without an accompanying third-degree perineal laceration, so a new code [664.6X, anal sphincter tear complicating delivery, not associated with third-degree perineal laceration] has been added to capture this information. Keep in mind these important points:
- Report the new code when an anal tear is noted at or after delivery. The only acceptable fifth digits for this code are 0 [unspecified as to episode of care or not applicable], 1 [delivered, with or without mention of antepartum condition], or 4 [postpartum condition or complication].
- Report the established code, 664.2X [third-degree perineal laceration] if an anal tear is noted in addition to a third-degree perineal tear. The fifth digit will be 0, 1, or 4, as it is with the code for an anal sphincter tear.
- Report the established code 654.8X [congenital or acquired abnormality of vulva] if the patient had an anal tear from a prior pregnancy, before the current delivery.
- Last, report the new code 569.43 [anal sphincter tear (healed) (old)] if you observe that the patient has an old anal tear but isn’t pregnant. Report an additional code for any associated fecal incontinence (787.6).
Report dysplasia follow-up as “medical necessity”
Once a patient has been treated for cervical dysplasia, long-term follow-up care is required to test for recurrence. The only code available to report that history last year was V13.29, a general code that reported all types of genital systems and obstetric disorders. This year, you can specify and report V13.22 [personal history of cervical dysplasia].
The role of human papillomavirus (HPV) as the cause of cervical cancer is well known, and routine screening tests for this infection are generally as accurate as a routine Pap smear. Because of this, a new code, V73.81 [human papillomavirus (HPV)], has been added to document encounters for HPV screening. The new code can be reported in conjunction with the routine gyn exam code, V72.31, or V76.2 [special screening for malignant neoplasm of cervix] to signal that additional screening is planned.
Better documentation of malignant ascites
789.51 Malignant ascites
789.59 Other ascites
Malignant ascites is seen most often in ovarian, endometrial, breast, colon, gastric, and pancreatic cancer. Management of this condition may include systemic chemotherapy, instillation of radioisotopes or chemotherapy drugs into peritoneal fluid, and peritoneal–venous shunting procedures.
Before October 1, under ICD-9 rules, malignant ascites could be reported only using the code 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].The problem is that this condition can also be caused by a primary ovarian malignancy, for which there has been no reporting mechanism. With expansion of the code 789.5 [ascites], you can specify the type of malignant ascites.
Note: Instructions in ICD-9 indicate that you should list a code for the site of the current malignancy first, such as 183.0 [malignant neoplasm of ovary] or 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].
Assisted reproductive fertility procedure status
Every endocrinologist is aware that assisted reproductive fertility procedures are a multistage undertaking. A number of pretreatment diagnostic tests are independent of the procedure itself, and payers might cover such tests if there were a way to identify patients who were undergoing a procedure from those who were still undergoing pretreatment testing.
Before October 1, only one code, V26.8 [other specified procreative management], was available. Starting this month, to identify a patient undergoing treatment, use V26.81 [encounter for assisted reproductive fertility procedure cycle], with an additional code to identify the type of infertility. With this expansion, a second code was added to capture “other specified procreative management” [V26.89].
Natural family planning comes of age
Natural family planning helps a couple determine when sexual intercourse is likely to (and not likely to) result in pregnancy. It encompasses provider counseling and education on either of two acceptable methods: tracking ovulation by examining cervical mucus or temperature charting. ICD-9 has expanded the existing code, V26.4, to capture this means of family planning more accurately:
V26.41 Procreative counseling and advice using natural family planning
In addition, a code was added to the contraceptive counseling codes to capture this approach as well:
V25.04 Counseling and instruction in natural family planning to avoid pregnancy
Last, a new code also covers other types of procreative management counseling and advice:
V26.49 Other procreative management counseling and advice
Disability certificates, made easy(ier) to report
Do patients come to you to have medical forms and certificates completed? Now you can be more specific, when coding, about the type of document you’re asked to fill out.
V68.01 Disability examination
V68.09 Other issue of medical certificates
The old code, V68.0, was a catch-all of medical certificates, including cause of death, fitness, and disability. The new codes distinguish a certificate for a disability examination from the rest of the pack. That’s a useful change because insurers and state disability programs often reimburse for a disability exam.
Remember: You still need to identify the specific exam, screening, or testing performed by using a code from the series V72.0–V82.9 as a secondary diagnosis. Examples: V72.31 for a gyn exam and V81.6 [screening for other and unspecified genitourinary conditions].
Diversified codes for iatrogenic ID complications
Patients sometimes develop infection in the presence of a central venous catheter or after injection or vaccination. Previously, you used code 999.3 to report such a complication, but that code lumped into one all reasons for infection.
This year, a new code, 993.31, exclusively covers infection caused by a central venous catheter. The code lists several catheter types—Hickman, peripherally inserted central catheter (PICC), triplelumen catheter—and makes clear that it should not be used to report infection caused by a urinary (996.64), arterial (996.62), venous (996.62), or unspecified type of catheter (996.69).
An additional code, 999.39, has been added to report all infections after intravenous infusion, injection, transfusion, or vaccination.
Vaginal, vulvar conditions: Simpler reporting
This year’s additions include codes for vaginal intraepithelial neoplasia (VAIN) and expansion of the vulvar intraepithelial neoplasia (VIN) category to match.
| 624.01 | Vulvar intraepithelial neoplasia I [VIN I] |
| Mild dysplasia of vulva | |
| 624.02 | Vulvar intraepithelial neoplasia II [VIN II] |
| Moderate dysplasia of vulva | |
| 624.09 | Other dystrophy of vulva |
| Kraurosis of vulva | |
| Leukoplakia of vulva | |
| 233.30 | Unspecified female genital organ |
| 233.31 | Vagina |
| Severe dysplasia of vagina | |
| Vaginal intraepithelial neoplasia III [VAIN III] | |
| 233.32 | Vulva |
| Severe dysplasia of vulva | |
| Vulvar intraepithelial neoplasia III [VIN III] | |
| 233.39 | Other female genital organ |
An “excludes” note has also been added to 622.1 [dysplasia of cervix (uteri)] to clarify that a diagnosis of carcinoma in situ I or II may not be reported unless this diagnosis is assigned based on a biopsy finding—not on an abnormal finding on a Pap smear.
New code for trauma during delivery
Anal sphincter tears can occur during delivery without an accompanying third-degree perineal laceration, so a new code [664.6X, anal sphincter tear complicating delivery, not associated with third-degree perineal laceration] has been added to capture this information. Keep in mind these important points:
- Report the new code when an anal tear is noted at or after delivery. The only acceptable fifth digits for this code are 0 [unspecified as to episode of care or not applicable], 1 [delivered, with or without mention of antepartum condition], or 4 [postpartum condition or complication].
- Report the established code, 664.2X [third-degree perineal laceration] if an anal tear is noted in addition to a third-degree perineal tear. The fifth digit will be 0, 1, or 4, as it is with the code for an anal sphincter tear.
- Report the established code 654.8X [congenital or acquired abnormality of vulva] if the patient had an anal tear from a prior pregnancy, before the current delivery.
- Last, report the new code 569.43 [anal sphincter tear (healed) (old)] if you observe that the patient has an old anal tear but isn’t pregnant. Report an additional code for any associated fecal incontinence (787.6).
Report dysplasia follow-up as “medical necessity”
Once a patient has been treated for cervical dysplasia, long-term follow-up care is required to test for recurrence. The only code available to report that history last year was V13.29, a general code that reported all types of genital systems and obstetric disorders. This year, you can specify and report V13.22 [personal history of cervical dysplasia].
The role of human papillomavirus (HPV) as the cause of cervical cancer is well known, and routine screening tests for this infection are generally as accurate as a routine Pap smear. Because of this, a new code, V73.81 [human papillomavirus (HPV)], has been added to document encounters for HPV screening. The new code can be reported in conjunction with the routine gyn exam code, V72.31, or V76.2 [special screening for malignant neoplasm of cervix] to signal that additional screening is planned.
Better documentation of malignant ascites
789.51 Malignant ascites
789.59 Other ascites
Malignant ascites is seen most often in ovarian, endometrial, breast, colon, gastric, and pancreatic cancer. Management of this condition may include systemic chemotherapy, instillation of radioisotopes or chemotherapy drugs into peritoneal fluid, and peritoneal–venous shunting procedures.
Before October 1, under ICD-9 rules, malignant ascites could be reported only using the code 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].The problem is that this condition can also be caused by a primary ovarian malignancy, for which there has been no reporting mechanism. With expansion of the code 789.5 [ascites], you can specify the type of malignant ascites.
Note: Instructions in ICD-9 indicate that you should list a code for the site of the current malignancy first, such as 183.0 [malignant neoplasm of ovary] or 197.6 [secondary malignant neoplasm of retroperitoneum and peritoneum].
Assisted reproductive fertility procedure status
Every endocrinologist is aware that assisted reproductive fertility procedures are a multistage undertaking. A number of pretreatment diagnostic tests are independent of the procedure itself, and payers might cover such tests if there were a way to identify patients who were undergoing a procedure from those who were still undergoing pretreatment testing.
Before October 1, only one code, V26.8 [other specified procreative management], was available. Starting this month, to identify a patient undergoing treatment, use V26.81 [encounter for assisted reproductive fertility procedure cycle], with an additional code to identify the type of infertility. With this expansion, a second code was added to capture “other specified procreative management” [V26.89].
Natural family planning comes of age
Natural family planning helps a couple determine when sexual intercourse is likely to (and not likely to) result in pregnancy. It encompasses provider counseling and education on either of two acceptable methods: tracking ovulation by examining cervical mucus or temperature charting. ICD-9 has expanded the existing code, V26.4, to capture this means of family planning more accurately:
V26.41 Procreative counseling and advice using natural family planning
In addition, a code was added to the contraceptive counseling codes to capture this approach as well:
V25.04 Counseling and instruction in natural family planning to avoid pregnancy
Last, a new code also covers other types of procreative management counseling and advice:
V26.49 Other procreative management counseling and advice
Disability certificates, made easy(ier) to report
Do patients come to you to have medical forms and certificates completed? Now you can be more specific, when coding, about the type of document you’re asked to fill out.
V68.01 Disability examination
V68.09 Other issue of medical certificates
The old code, V68.0, was a catch-all of medical certificates, including cause of death, fitness, and disability. The new codes distinguish a certificate for a disability examination from the rest of the pack. That’s a useful change because insurers and state disability programs often reimburse for a disability exam.
Remember: You still need to identify the specific exam, screening, or testing performed by using a code from the series V72.0–V82.9 as a secondary diagnosis. Examples: V72.31 for a gyn exam and V81.6 [screening for other and unspecified genitourinary conditions].
Diversified codes for iatrogenic ID complications
Patients sometimes develop infection in the presence of a central venous catheter or after injection or vaccination. Previously, you used code 999.3 to report such a complication, but that code lumped into one all reasons for infection.
This year, a new code, 993.31, exclusively covers infection caused by a central venous catheter. The code lists several catheter types—Hickman, peripherally inserted central catheter (PICC), triplelumen catheter—and makes clear that it should not be used to report infection caused by a urinary (996.64), arterial (996.62), venous (996.62), or unspecified type of catheter (996.69).
An additional code, 999.39, has been added to report all infections after intravenous infusion, injection, transfusion, or vaccination.
Should we use appetite stimulants for malnourished elderly patients?
Probably not. Only 1 appetite stimulate, megestrol acetate oral suspension (Megace) at 400 mg or 800 mg daily, has been studied in this population. The data show only limited benefit, mixed outcomes, and potential harm (strength of recommendation: B, based on small, randomized, controlled trials).
Good advice for a common problem
Kayleen P. Papin, MD
Medical College of Wisconsin, Milwaukee
This question hits home for me. I recently sat down with the husband, and main caregiver, of a woman with advanced dementia. The woman eats very little and is losing weight despite her husband’s great efforts at encouraging her to eat. Under the care of another physician, she had been given megestrol acetate and there had been some improvement. Her visit to my office was an opportunity to continue an ongoing conversation with her husband about his wife’s overall decline, her advancing dementia, and the sorrow he was feeling over her failing health.
Should we use appetite stimulants in malnourished elderly patients? “probably not.” that is a good place to start to avoid harm to our most frail, declining, elderly patients for whom we care. That leaves open flexibility to patient, family, and caregiver preferences, but reminds us that the most important part of caring for these patients and their families is clear, compassionate communication regarding goals and expectations.
Evidence summary
Although a number of studies have evaluated various appetite stimulants—megestrol, dronabinol (Marinol), cyproheptadine (Periactin), thalidomide (Thalomid), pentoxifylline (Pentoxil/Trental), nandrolone decanoate (DecaDurabolin), oxandrolone (Oxandrin), and corticosteroids—in patients with AIDS, anorexia cachexia syndrome, and advanced cancer, only megestrol has been studied in malnourished elderly patients.
Two studies, mixed results
One placebo-controlled randomized clinical trial studied 45 malnourished patients who were recently discharged from an acute care hospital to a nursing home. The patients (predominately female, with a mean age of 83) were randomized into 4 treatment arms (placebo or megestrol 200 mg, 400 mg, or 800 mg daily) and followed for 63 days.
Only those receiving megestrol (400 mg or 800 mg daily) demonstrated a statistically significant increase in patient appetite and a dose-responsive increase in prealbumin level at the 20 day interim analysis (7.5 and 9.0 mg/dL, respectfully). But at the final assessment (63 days), only the 400-mg dose maintained a statistically significant increase in prealbumin over placebo. However, there was no significant improvement in serum albumin or clinical endpoints (weight, functional status, or health-related quality of life).1
In contrast, an earlier Veterans Administration (and predominantly male) study showed 13/21 of those treated with megestrol (800 mg daily for 12 weeks) noted weight gain (≥4 lb sustained at 3 months post-treatment), compared with 5/23 of those receiving placebo (number needed to treat [NNT]=2.5).2 Of note, only 9/26 patients had sustained weight gain in the megestrol group at the 12-month endpoint post-treatment, comparable with 7/25 in the placebo group.
Some small, but statistically significant, score improvements were noted during the treatment period in appetite and enjoyment of life; however, no differences were noted in scores on the more widely accepted Geriatric Depression Scale.
Adverse effects
As in all therapeutic interventions, benefit must be balanced against risk. The Megace ES package insert notes the following potential adverse effects: diarrhea, cardiomyopathy, palpitation, hepatomegaly, leukopenia, edema, paresthesia, confusion, convulsion, depression, neuropathy, hypesthesia and abnormal thinking, thrombophlebitis, pulmonary embolism, and glucose intolerance.3
To date, the prevalence rates of these potential adverse effects have only been studied in patients with AIDS. No data reflecting potential rates in elderly patients have been published.
Recommendations from others
The American Geriatric Society4 made 3 comments on appetite stimulation:
- There are no FDA-approved drugs available for the promotion of weight gain in older adults.
- A minority of patients receiving mirtazapine report appetite stimulation and weight gain.
- All drugs used for appetite have substantial potential adverse events.
We found only 1 national guideline on this topic: Unintentional Weight Loss in the Elderly from the University of Texas School of Nursing.5 The guideline indicates that drugs should not be used as first-line intervention in the elderly, as there has been inadequate testing in this population. Benefits are restricted to small weight gains without indication of decreased morbidity or mortality, improved quality of life, or improved functional ability.
Acknowledgments
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Reuben DB, Hirsch SH, Zhou K, Greendale GA. The effects of megestrol acetate suspension for elderly patients with reduced appetite after hospitalization: a phase II randomized clinical trial. J Am Geriatr Soc 2005;53:970-975.
2. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality-of-life measures and stimulation of weight gain after treatment with megestrol acetate or suspension in geriatric cachexia: results of a double-blind, placebo controlled study. J Am Geriatr Soc 2001;48:485-492.
3. Megace Physicians’ Desk Reference 61st ed. Montvale, NJ: Thomson; 2007:2461-2463.
4. Malnutrition. Geriatrics at Your Fingertips [website]. Available at: www.geriatricsatyourfingertips.org/ebook/gayf_20.asp. Accessed August 6, 2007.
5. University of Texas, School of Nursing. Unintentional Weight Loss in the Elderly. Austin, Tex: University of Texas, School of Nursing; 2006. Available at: www.guideline.gov/summary/summary.aspx?doc_id=9435. Accessed August 6, 2007.
Probably not. Only 1 appetite stimulate, megestrol acetate oral suspension (Megace) at 400 mg or 800 mg daily, has been studied in this population. The data show only limited benefit, mixed outcomes, and potential harm (strength of recommendation: B, based on small, randomized, controlled trials).
Good advice for a common problem
Kayleen P. Papin, MD
Medical College of Wisconsin, Milwaukee
This question hits home for me. I recently sat down with the husband, and main caregiver, of a woman with advanced dementia. The woman eats very little and is losing weight despite her husband’s great efforts at encouraging her to eat. Under the care of another physician, she had been given megestrol acetate and there had been some improvement. Her visit to my office was an opportunity to continue an ongoing conversation with her husband about his wife’s overall decline, her advancing dementia, and the sorrow he was feeling over her failing health.
Should we use appetite stimulants in malnourished elderly patients? “probably not.” that is a good place to start to avoid harm to our most frail, declining, elderly patients for whom we care. That leaves open flexibility to patient, family, and caregiver preferences, but reminds us that the most important part of caring for these patients and their families is clear, compassionate communication regarding goals and expectations.
Evidence summary
Although a number of studies have evaluated various appetite stimulants—megestrol, dronabinol (Marinol), cyproheptadine (Periactin), thalidomide (Thalomid), pentoxifylline (Pentoxil/Trental), nandrolone decanoate (DecaDurabolin), oxandrolone (Oxandrin), and corticosteroids—in patients with AIDS, anorexia cachexia syndrome, and advanced cancer, only megestrol has been studied in malnourished elderly patients.
Two studies, mixed results
One placebo-controlled randomized clinical trial studied 45 malnourished patients who were recently discharged from an acute care hospital to a nursing home. The patients (predominately female, with a mean age of 83) were randomized into 4 treatment arms (placebo or megestrol 200 mg, 400 mg, or 800 mg daily) and followed for 63 days.
Only those receiving megestrol (400 mg or 800 mg daily) demonstrated a statistically significant increase in patient appetite and a dose-responsive increase in prealbumin level at the 20 day interim analysis (7.5 and 9.0 mg/dL, respectfully). But at the final assessment (63 days), only the 400-mg dose maintained a statistically significant increase in prealbumin over placebo. However, there was no significant improvement in serum albumin or clinical endpoints (weight, functional status, or health-related quality of life).1
In contrast, an earlier Veterans Administration (and predominantly male) study showed 13/21 of those treated with megestrol (800 mg daily for 12 weeks) noted weight gain (≥4 lb sustained at 3 months post-treatment), compared with 5/23 of those receiving placebo (number needed to treat [NNT]=2.5).2 Of note, only 9/26 patients had sustained weight gain in the megestrol group at the 12-month endpoint post-treatment, comparable with 7/25 in the placebo group.
Some small, but statistically significant, score improvements were noted during the treatment period in appetite and enjoyment of life; however, no differences were noted in scores on the more widely accepted Geriatric Depression Scale.
Adverse effects
As in all therapeutic interventions, benefit must be balanced against risk. The Megace ES package insert notes the following potential adverse effects: diarrhea, cardiomyopathy, palpitation, hepatomegaly, leukopenia, edema, paresthesia, confusion, convulsion, depression, neuropathy, hypesthesia and abnormal thinking, thrombophlebitis, pulmonary embolism, and glucose intolerance.3
To date, the prevalence rates of these potential adverse effects have only been studied in patients with AIDS. No data reflecting potential rates in elderly patients have been published.
Recommendations from others
The American Geriatric Society4 made 3 comments on appetite stimulation:
- There are no FDA-approved drugs available for the promotion of weight gain in older adults.
- A minority of patients receiving mirtazapine report appetite stimulation and weight gain.
- All drugs used for appetite have substantial potential adverse events.
We found only 1 national guideline on this topic: Unintentional Weight Loss in the Elderly from the University of Texas School of Nursing.5 The guideline indicates that drugs should not be used as first-line intervention in the elderly, as there has been inadequate testing in this population. Benefits are restricted to small weight gains without indication of decreased morbidity or mortality, improved quality of life, or improved functional ability.
Acknowledgments
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
Probably not. Only 1 appetite stimulate, megestrol acetate oral suspension (Megace) at 400 mg or 800 mg daily, has been studied in this population. The data show only limited benefit, mixed outcomes, and potential harm (strength of recommendation: B, based on small, randomized, controlled trials).
Good advice for a common problem
Kayleen P. Papin, MD
Medical College of Wisconsin, Milwaukee
This question hits home for me. I recently sat down with the husband, and main caregiver, of a woman with advanced dementia. The woman eats very little and is losing weight despite her husband’s great efforts at encouraging her to eat. Under the care of another physician, she had been given megestrol acetate and there had been some improvement. Her visit to my office was an opportunity to continue an ongoing conversation with her husband about his wife’s overall decline, her advancing dementia, and the sorrow he was feeling over her failing health.
Should we use appetite stimulants in malnourished elderly patients? “probably not.” that is a good place to start to avoid harm to our most frail, declining, elderly patients for whom we care. That leaves open flexibility to patient, family, and caregiver preferences, but reminds us that the most important part of caring for these patients and their families is clear, compassionate communication regarding goals and expectations.
Evidence summary
Although a number of studies have evaluated various appetite stimulants—megestrol, dronabinol (Marinol), cyproheptadine (Periactin), thalidomide (Thalomid), pentoxifylline (Pentoxil/Trental), nandrolone decanoate (DecaDurabolin), oxandrolone (Oxandrin), and corticosteroids—in patients with AIDS, anorexia cachexia syndrome, and advanced cancer, only megestrol has been studied in malnourished elderly patients.
Two studies, mixed results
One placebo-controlled randomized clinical trial studied 45 malnourished patients who were recently discharged from an acute care hospital to a nursing home. The patients (predominately female, with a mean age of 83) were randomized into 4 treatment arms (placebo or megestrol 200 mg, 400 mg, or 800 mg daily) and followed for 63 days.
Only those receiving megestrol (400 mg or 800 mg daily) demonstrated a statistically significant increase in patient appetite and a dose-responsive increase in prealbumin level at the 20 day interim analysis (7.5 and 9.0 mg/dL, respectfully). But at the final assessment (63 days), only the 400-mg dose maintained a statistically significant increase in prealbumin over placebo. However, there was no significant improvement in serum albumin or clinical endpoints (weight, functional status, or health-related quality of life).1
In contrast, an earlier Veterans Administration (and predominantly male) study showed 13/21 of those treated with megestrol (800 mg daily for 12 weeks) noted weight gain (≥4 lb sustained at 3 months post-treatment), compared with 5/23 of those receiving placebo (number needed to treat [NNT]=2.5).2 Of note, only 9/26 patients had sustained weight gain in the megestrol group at the 12-month endpoint post-treatment, comparable with 7/25 in the placebo group.
Some small, but statistically significant, score improvements were noted during the treatment period in appetite and enjoyment of life; however, no differences were noted in scores on the more widely accepted Geriatric Depression Scale.
Adverse effects
As in all therapeutic interventions, benefit must be balanced against risk. The Megace ES package insert notes the following potential adverse effects: diarrhea, cardiomyopathy, palpitation, hepatomegaly, leukopenia, edema, paresthesia, confusion, convulsion, depression, neuropathy, hypesthesia and abnormal thinking, thrombophlebitis, pulmonary embolism, and glucose intolerance.3
To date, the prevalence rates of these potential adverse effects have only been studied in patients with AIDS. No data reflecting potential rates in elderly patients have been published.
Recommendations from others
The American Geriatric Society4 made 3 comments on appetite stimulation:
- There are no FDA-approved drugs available for the promotion of weight gain in older adults.
- A minority of patients receiving mirtazapine report appetite stimulation and weight gain.
- All drugs used for appetite have substantial potential adverse events.
We found only 1 national guideline on this topic: Unintentional Weight Loss in the Elderly from the University of Texas School of Nursing.5 The guideline indicates that drugs should not be used as first-line intervention in the elderly, as there has been inadequate testing in this population. Benefits are restricted to small weight gains without indication of decreased morbidity or mortality, improved quality of life, or improved functional ability.
Acknowledgments
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Reuben DB, Hirsch SH, Zhou K, Greendale GA. The effects of megestrol acetate suspension for elderly patients with reduced appetite after hospitalization: a phase II randomized clinical trial. J Am Geriatr Soc 2005;53:970-975.
2. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality-of-life measures and stimulation of weight gain after treatment with megestrol acetate or suspension in geriatric cachexia: results of a double-blind, placebo controlled study. J Am Geriatr Soc 2001;48:485-492.
3. Megace Physicians’ Desk Reference 61st ed. Montvale, NJ: Thomson; 2007:2461-2463.
4. Malnutrition. Geriatrics at Your Fingertips [website]. Available at: www.geriatricsatyourfingertips.org/ebook/gayf_20.asp. Accessed August 6, 2007.
5. University of Texas, School of Nursing. Unintentional Weight Loss in the Elderly. Austin, Tex: University of Texas, School of Nursing; 2006. Available at: www.guideline.gov/summary/summary.aspx?doc_id=9435. Accessed August 6, 2007.
1. Reuben DB, Hirsch SH, Zhou K, Greendale GA. The effects of megestrol acetate suspension for elderly patients with reduced appetite after hospitalization: a phase II randomized clinical trial. J Am Geriatr Soc 2005;53:970-975.
2. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality-of-life measures and stimulation of weight gain after treatment with megestrol acetate or suspension in geriatric cachexia: results of a double-blind, placebo controlled study. J Am Geriatr Soc 2001;48:485-492.
3. Megace Physicians’ Desk Reference 61st ed. Montvale, NJ: Thomson; 2007:2461-2463.
4. Malnutrition. Geriatrics at Your Fingertips [website]. Available at: www.geriatricsatyourfingertips.org/ebook/gayf_20.asp. Accessed August 6, 2007.
5. University of Texas, School of Nursing. Unintentional Weight Loss in the Elderly. Austin, Tex: University of Texas, School of Nursing; 2006. Available at: www.guideline.gov/summary/summary.aspx?doc_id=9435. Accessed August 6, 2007.
Evidence-based answers from the Family Physicians Inquiries Network
U.K. Study Data Confirmed Safety of Diclofenac 3% for Actinic Keratosis
AMSTERDAM Diclofenac 3% gel was well tolerated and showed an excellent safety profile for treatment of multiple actinic keratoses in a postmarketing safety surveillance study.
The study, conducted in 140 primary care practices in the United Kingdom, showed no severe treatment-related adverse events in 450 treated patients. The most common adverse events were mild to moderate dry skin, itching, and redness, each occurring in 16%-20% of patients, Dr. Ron Higson reported at the 11th World Congress on Cancers of the Skin.
Severe versions of these side effects occurred in fewer than 4% of patients, added Dr. Higson of Clitheroe (U.K.) Health Centre.
Participants in this observational study were instructed to apply diclofenac 3% gel (Solaraze) twice daily for 12 weeks to areas of actinic keratoses (AKs). The topical nonsteroidal anti-inflammatory drug is licensed for treatment of AKs in the United States, United Kingdom, and some other European countries. Patients were assessed during office visits at baseline and at weeks 6, 12, and 16.
Although this was designed primarily as a safety study, there was a secondary efficacy end point consisting of change over time in the longest AK axis from each patient's three largest AKs. The mean reduction in the size of AKs located on the head, face, or neck was 2.8 mm at week 6 and 6.4 mm at the week 16 follow-up visit, Dr. Higson said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University, Rotterdam, the Netherlands.
The study was funded by Shire Pharmaceuticals.
Dr. Eggert Stockfleth, director of the skin cancer center at Charité University Hospital, Berlin, commented that diclofenac gel's two major advantages are its safetythe topical agent induces only very mild erythema and has no systemic effectsand the fact that it treats not only visible AK lesions but also what he calls the "field cancerization"the underlying dysplasia that gives rise to new AKs and eventually to skin cancers.
AMSTERDAM Diclofenac 3% gel was well tolerated and showed an excellent safety profile for treatment of multiple actinic keratoses in a postmarketing safety surveillance study.
The study, conducted in 140 primary care practices in the United Kingdom, showed no severe treatment-related adverse events in 450 treated patients. The most common adverse events were mild to moderate dry skin, itching, and redness, each occurring in 16%-20% of patients, Dr. Ron Higson reported at the 11th World Congress on Cancers of the Skin.
Severe versions of these side effects occurred in fewer than 4% of patients, added Dr. Higson of Clitheroe (U.K.) Health Centre.
Participants in this observational study were instructed to apply diclofenac 3% gel (Solaraze) twice daily for 12 weeks to areas of actinic keratoses (AKs). The topical nonsteroidal anti-inflammatory drug is licensed for treatment of AKs in the United States, United Kingdom, and some other European countries. Patients were assessed during office visits at baseline and at weeks 6, 12, and 16.
Although this was designed primarily as a safety study, there was a secondary efficacy end point consisting of change over time in the longest AK axis from each patient's three largest AKs. The mean reduction in the size of AKs located on the head, face, or neck was 2.8 mm at week 6 and 6.4 mm at the week 16 follow-up visit, Dr. Higson said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University, Rotterdam, the Netherlands.
The study was funded by Shire Pharmaceuticals.
Dr. Eggert Stockfleth, director of the skin cancer center at Charité University Hospital, Berlin, commented that diclofenac gel's two major advantages are its safetythe topical agent induces only very mild erythema and has no systemic effectsand the fact that it treats not only visible AK lesions but also what he calls the "field cancerization"the underlying dysplasia that gives rise to new AKs and eventually to skin cancers.
AMSTERDAM Diclofenac 3% gel was well tolerated and showed an excellent safety profile for treatment of multiple actinic keratoses in a postmarketing safety surveillance study.
The study, conducted in 140 primary care practices in the United Kingdom, showed no severe treatment-related adverse events in 450 treated patients. The most common adverse events were mild to moderate dry skin, itching, and redness, each occurring in 16%-20% of patients, Dr. Ron Higson reported at the 11th World Congress on Cancers of the Skin.
Severe versions of these side effects occurred in fewer than 4% of patients, added Dr. Higson of Clitheroe (U.K.) Health Centre.
Participants in this observational study were instructed to apply diclofenac 3% gel (Solaraze) twice daily for 12 weeks to areas of actinic keratoses (AKs). The topical nonsteroidal anti-inflammatory drug is licensed for treatment of AKs in the United States, United Kingdom, and some other European countries. Patients were assessed during office visits at baseline and at weeks 6, 12, and 16.
Although this was designed primarily as a safety study, there was a secondary efficacy end point consisting of change over time in the longest AK axis from each patient's three largest AKs. The mean reduction in the size of AKs located on the head, face, or neck was 2.8 mm at week 6 and 6.4 mm at the week 16 follow-up visit, Dr. Higson said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University, Rotterdam, the Netherlands.
The study was funded by Shire Pharmaceuticals.
Dr. Eggert Stockfleth, director of the skin cancer center at Charité University Hospital, Berlin, commented that diclofenac gel's two major advantages are its safetythe topical agent induces only very mild erythema and has no systemic effectsand the fact that it treats not only visible AK lesions but also what he calls the "field cancerization"the underlying dysplasia that gives rise to new AKs and eventually to skin cancers.
Sorafenib Results Mixed For Advanced Melanoma
CHICAGO The first two randomized trials to assess the addition of sorafenib to chemotherapy for advanced melanoma exhibited mixed results, according to presentations at the annual meeting of the American Society of Clinical Oncology.
A randomized, 17-center, phase II study of 101 chemotherapy-naive patients showed a 50% improvement in progression-free survival and a 62% improvement in time to progression when sorafenib (Nexavar) was added to dacarbazine (DTIC-Dome) compared with dacarbazine plus placebo.
Improved progression-free survival did not translate into a survival benefit, however. "At our last analysis, 65 of 101 patients had died, and there was no difference in median survival between the two study arms," said Dr. David F. McDermott, clinical director of the biologic therapy program at Beth Israel Deaconess Medical Center in Boston.
The second study, the 270-patient, phase III Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, tested paclitaxel plus carboplatin with or without sorafenib as second-line treatment. The trial produced negative results. Dr. Sanjiv S. Agarwala, chief of medical oncology at St. Luke's Cancer Center in Bethlehem, Pa., reported that sorafenib failed to improve progression-free survival, tumor response rates, or time-to-disease progression in metastatic melanoma patients, whose disease had progressed on a chemotherapy regimen containing dacarbazine or temozolomide (Temodal).
In his discussion of the two trials, Dr. Keith Flaherty said that although the trials had mixed results, the 6-month progression-free survival rate of 41% in the study by Dr. McDermott and colleagues "is truly the high water mark of what we've achieved to date … at least when focusing on this end point." These gains were achieved at a toxicity cost deemed "not unacceptable" by Dr. Flaherty of the division of hematology-oncology at the University of Pennsylvania Health System in Philadelphia.
The multicenter trial by Dr. Agarwala and colleagues did manage to produce data showing that the carboplatin-paclitaxel combination is "relatively active" in patients who have failed front-line chemotherapy containing dacarbazine or temozolomide, according to Dr. Flaherty. "The roughly 30% progression-free survival rate at 6 months is a number that many of us in the field believe is a sign of activity," he said.
"The front-line randomized phase II trial certainly suggests that sorafenib may be active in this setting, and I think the phase III study gives us enough evidence to say that carboplatin-paclitaxel control arm therapy is a perfectly reasonable therapy to offer patients," Dr. Flaherty concluded.
In the dacarbazine with or without sorafenib study, Dr. McDermott and his associates randomized 101 good performance status patients to receive either dacarbazine at 1,000 mg/m2 on day 1 in combination with oral sorafenib 400 mg twice daily, or dacarbazine at 1,000 mg/m2 on day 1 and two placebo tablets twice daily. Tumors were assessed at baseline and every 6 weeks, and treatment was continued until progression or intolerable toxicity.
Dose reductions due to adverse events (including grades 3 and 4 thrombocytopenia, neutropenia, nausea, and CNS hemorrhage) were more common in the sorafenib arm.
"All these toxicities were reversible, and there were no treatment-related deaths. Sorafenib-associated hand-foot syndrome, rash, hypertension, and elevated lipase [were] not greater than [have] been reported in earlier sorafenib trials," Dr. McDermott said.
The 270 chemotherapy-refractory patients in the PRISM trial had stage IV or unresectable stage III melanoma. Half were randomized to receive paclitaxel 225 mg/m2 and carboplatin AUC = 6 on day 1 every 3 weeks plus oral sorafenib 400 mg twice daily on days 2 to 19 every 3 weeks. The other half received the paclitaxel-carboplatin regimen plus an oral placebo. Both groups continued treatment until disease progression or intolerable toxicity.
The difference in progression-free survival between the sorafenib plus chemotherapy and sorafenib plus placebo arms was insignificant at 17.4 weeks and 17.9 weeks, respectively, and there were no tumor responses in either arm, according to Dr. Agarwala.
Neutropenia affected nearly half of patients similarly in both arms, while thrombocytopenia, diarrhea, hand-foot reactions, and rash were higher with sorafenib.
Both trials were sponsored by Bayer, which markets sorafenib. The ongoing Eastern Oncology Cooperative Group trial E2603 is evaluating the same regimen studied by Dr. Agarwala and colleagues in a larger patient population with unresectable locally advanced or stage IV melanoma.
CHICAGO The first two randomized trials to assess the addition of sorafenib to chemotherapy for advanced melanoma exhibited mixed results, according to presentations at the annual meeting of the American Society of Clinical Oncology.
A randomized, 17-center, phase II study of 101 chemotherapy-naive patients showed a 50% improvement in progression-free survival and a 62% improvement in time to progression when sorafenib (Nexavar) was added to dacarbazine (DTIC-Dome) compared with dacarbazine plus placebo.
Improved progression-free survival did not translate into a survival benefit, however. "At our last analysis, 65 of 101 patients had died, and there was no difference in median survival between the two study arms," said Dr. David F. McDermott, clinical director of the biologic therapy program at Beth Israel Deaconess Medical Center in Boston.
The second study, the 270-patient, phase III Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, tested paclitaxel plus carboplatin with or without sorafenib as second-line treatment. The trial produced negative results. Dr. Sanjiv S. Agarwala, chief of medical oncology at St. Luke's Cancer Center in Bethlehem, Pa., reported that sorafenib failed to improve progression-free survival, tumor response rates, or time-to-disease progression in metastatic melanoma patients, whose disease had progressed on a chemotherapy regimen containing dacarbazine or temozolomide (Temodal).
In his discussion of the two trials, Dr. Keith Flaherty said that although the trials had mixed results, the 6-month progression-free survival rate of 41% in the study by Dr. McDermott and colleagues "is truly the high water mark of what we've achieved to date … at least when focusing on this end point." These gains were achieved at a toxicity cost deemed "not unacceptable" by Dr. Flaherty of the division of hematology-oncology at the University of Pennsylvania Health System in Philadelphia.
The multicenter trial by Dr. Agarwala and colleagues did manage to produce data showing that the carboplatin-paclitaxel combination is "relatively active" in patients who have failed front-line chemotherapy containing dacarbazine or temozolomide, according to Dr. Flaherty. "The roughly 30% progression-free survival rate at 6 months is a number that many of us in the field believe is a sign of activity," he said.
"The front-line randomized phase II trial certainly suggests that sorafenib may be active in this setting, and I think the phase III study gives us enough evidence to say that carboplatin-paclitaxel control arm therapy is a perfectly reasonable therapy to offer patients," Dr. Flaherty concluded.
In the dacarbazine with or without sorafenib study, Dr. McDermott and his associates randomized 101 good performance status patients to receive either dacarbazine at 1,000 mg/m2 on day 1 in combination with oral sorafenib 400 mg twice daily, or dacarbazine at 1,000 mg/m2 on day 1 and two placebo tablets twice daily. Tumors were assessed at baseline and every 6 weeks, and treatment was continued until progression or intolerable toxicity.
Dose reductions due to adverse events (including grades 3 and 4 thrombocytopenia, neutropenia, nausea, and CNS hemorrhage) were more common in the sorafenib arm.
"All these toxicities were reversible, and there were no treatment-related deaths. Sorafenib-associated hand-foot syndrome, rash, hypertension, and elevated lipase [were] not greater than [have] been reported in earlier sorafenib trials," Dr. McDermott said.
The 270 chemotherapy-refractory patients in the PRISM trial had stage IV or unresectable stage III melanoma. Half were randomized to receive paclitaxel 225 mg/m2 and carboplatin AUC = 6 on day 1 every 3 weeks plus oral sorafenib 400 mg twice daily on days 2 to 19 every 3 weeks. The other half received the paclitaxel-carboplatin regimen plus an oral placebo. Both groups continued treatment until disease progression or intolerable toxicity.
The difference in progression-free survival between the sorafenib plus chemotherapy and sorafenib plus placebo arms was insignificant at 17.4 weeks and 17.9 weeks, respectively, and there were no tumor responses in either arm, according to Dr. Agarwala.
Neutropenia affected nearly half of patients similarly in both arms, while thrombocytopenia, diarrhea, hand-foot reactions, and rash were higher with sorafenib.
Both trials were sponsored by Bayer, which markets sorafenib. The ongoing Eastern Oncology Cooperative Group trial E2603 is evaluating the same regimen studied by Dr. Agarwala and colleagues in a larger patient population with unresectable locally advanced or stage IV melanoma.
CHICAGO The first two randomized trials to assess the addition of sorafenib to chemotherapy for advanced melanoma exhibited mixed results, according to presentations at the annual meeting of the American Society of Clinical Oncology.
A randomized, 17-center, phase II study of 101 chemotherapy-naive patients showed a 50% improvement in progression-free survival and a 62% improvement in time to progression when sorafenib (Nexavar) was added to dacarbazine (DTIC-Dome) compared with dacarbazine plus placebo.
Improved progression-free survival did not translate into a survival benefit, however. "At our last analysis, 65 of 101 patients had died, and there was no difference in median survival between the two study arms," said Dr. David F. McDermott, clinical director of the biologic therapy program at Beth Israel Deaconess Medical Center in Boston.
The second study, the 270-patient, phase III Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, tested paclitaxel plus carboplatin with or without sorafenib as second-line treatment. The trial produced negative results. Dr. Sanjiv S. Agarwala, chief of medical oncology at St. Luke's Cancer Center in Bethlehem, Pa., reported that sorafenib failed to improve progression-free survival, tumor response rates, or time-to-disease progression in metastatic melanoma patients, whose disease had progressed on a chemotherapy regimen containing dacarbazine or temozolomide (Temodal).
In his discussion of the two trials, Dr. Keith Flaherty said that although the trials had mixed results, the 6-month progression-free survival rate of 41% in the study by Dr. McDermott and colleagues "is truly the high water mark of what we've achieved to date … at least when focusing on this end point." These gains were achieved at a toxicity cost deemed "not unacceptable" by Dr. Flaherty of the division of hematology-oncology at the University of Pennsylvania Health System in Philadelphia.
The multicenter trial by Dr. Agarwala and colleagues did manage to produce data showing that the carboplatin-paclitaxel combination is "relatively active" in patients who have failed front-line chemotherapy containing dacarbazine or temozolomide, according to Dr. Flaherty. "The roughly 30% progression-free survival rate at 6 months is a number that many of us in the field believe is a sign of activity," he said.
"The front-line randomized phase II trial certainly suggests that sorafenib may be active in this setting, and I think the phase III study gives us enough evidence to say that carboplatin-paclitaxel control arm therapy is a perfectly reasonable therapy to offer patients," Dr. Flaherty concluded.
In the dacarbazine with or without sorafenib study, Dr. McDermott and his associates randomized 101 good performance status patients to receive either dacarbazine at 1,000 mg/m2 on day 1 in combination with oral sorafenib 400 mg twice daily, or dacarbazine at 1,000 mg/m2 on day 1 and two placebo tablets twice daily. Tumors were assessed at baseline and every 6 weeks, and treatment was continued until progression or intolerable toxicity.
Dose reductions due to adverse events (including grades 3 and 4 thrombocytopenia, neutropenia, nausea, and CNS hemorrhage) were more common in the sorafenib arm.
"All these toxicities were reversible, and there were no treatment-related deaths. Sorafenib-associated hand-foot syndrome, rash, hypertension, and elevated lipase [were] not greater than [have] been reported in earlier sorafenib trials," Dr. McDermott said.
The 270 chemotherapy-refractory patients in the PRISM trial had stage IV or unresectable stage III melanoma. Half were randomized to receive paclitaxel 225 mg/m2 and carboplatin AUC = 6 on day 1 every 3 weeks plus oral sorafenib 400 mg twice daily on days 2 to 19 every 3 weeks. The other half received the paclitaxel-carboplatin regimen plus an oral placebo. Both groups continued treatment until disease progression or intolerable toxicity.
The difference in progression-free survival between the sorafenib plus chemotherapy and sorafenib plus placebo arms was insignificant at 17.4 weeks and 17.9 weeks, respectively, and there were no tumor responses in either arm, according to Dr. Agarwala.
Neutropenia affected nearly half of patients similarly in both arms, while thrombocytopenia, diarrhea, hand-foot reactions, and rash were higher with sorafenib.
Both trials were sponsored by Bayer, which markets sorafenib. The ongoing Eastern Oncology Cooperative Group trial E2603 is evaluating the same regimen studied by Dr. Agarwala and colleagues in a larger patient population with unresectable locally advanced or stage IV melanoma.
Current Options in Stage IV Melanoma Deemed Unsatisfactory
AMSTERDAM Here's just how little progress has occurred in the systemic treatment of metastatic melanoma over the last 3 decades: Today the best therapeutic option for patients with advanced melanoma is to enroll them in a clinical trial of an investigational drug, Dr. Mark R. Middleton said at the 11th World Congress on Cancers of the Skin.
The standard treatment of advanced melanoma has for many years been single-agent dacarbazine (DTIC). None of the numerous multidrug combinations of chemotherapeutic agents or chemotherapeutic agents plus cytotoxic or biologic agents that have been tested have proved more effective than DTIC, only more toxic, he said.
Over the years, though, oncologists have come to realize that they have overestimated how good a drug DTIC is, said Dr. Middleton, a medical oncologist at Cancer Research UK and the University of Oxford (England).
Indeed, while decades-old studies suggested 20% of patients with advanced melanoma experience an objective tumor response to DTIC, more recent large multicenter studies indicate that the true figure is between 1 in 7 and 1 in 10, with no evidence DTIC offers any improvement over supportive care in terms of overall survival, he said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
This discouraging assessment isn't just one oncologist's view. Dr. Alexander M.M. Eggermont noted during his presentation that the Dutch Cancer Society recently issued an advisory that the No. 1 option in patients with advanced melanoma is to enter them into any new drug development trial, even a phase I trial.
"So phase I studies are the preferred option in stage IV melanoma patients, rather than giving them the usual stuff. I think that's a very important message because that's really what we need to move the field forward," added Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands, and president-elect of the Federation of European Cancer Societies.
AMSTERDAM Here's just how little progress has occurred in the systemic treatment of metastatic melanoma over the last 3 decades: Today the best therapeutic option for patients with advanced melanoma is to enroll them in a clinical trial of an investigational drug, Dr. Mark R. Middleton said at the 11th World Congress on Cancers of the Skin.
The standard treatment of advanced melanoma has for many years been single-agent dacarbazine (DTIC). None of the numerous multidrug combinations of chemotherapeutic agents or chemotherapeutic agents plus cytotoxic or biologic agents that have been tested have proved more effective than DTIC, only more toxic, he said.
Over the years, though, oncologists have come to realize that they have overestimated how good a drug DTIC is, said Dr. Middleton, a medical oncologist at Cancer Research UK and the University of Oxford (England).
Indeed, while decades-old studies suggested 20% of patients with advanced melanoma experience an objective tumor response to DTIC, more recent large multicenter studies indicate that the true figure is between 1 in 7 and 1 in 10, with no evidence DTIC offers any improvement over supportive care in terms of overall survival, he said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
This discouraging assessment isn't just one oncologist's view. Dr. Alexander M.M. Eggermont noted during his presentation that the Dutch Cancer Society recently issued an advisory that the No. 1 option in patients with advanced melanoma is to enter them into any new drug development trial, even a phase I trial.
"So phase I studies are the preferred option in stage IV melanoma patients, rather than giving them the usual stuff. I think that's a very important message because that's really what we need to move the field forward," added Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands, and president-elect of the Federation of European Cancer Societies.
AMSTERDAM Here's just how little progress has occurred in the systemic treatment of metastatic melanoma over the last 3 decades: Today the best therapeutic option for patients with advanced melanoma is to enroll them in a clinical trial of an investigational drug, Dr. Mark R. Middleton said at the 11th World Congress on Cancers of the Skin.
The standard treatment of advanced melanoma has for many years been single-agent dacarbazine (DTIC). None of the numerous multidrug combinations of chemotherapeutic agents or chemotherapeutic agents plus cytotoxic or biologic agents that have been tested have proved more effective than DTIC, only more toxic, he said.
Over the years, though, oncologists have come to realize that they have overestimated how good a drug DTIC is, said Dr. Middleton, a medical oncologist at Cancer Research UK and the University of Oxford (England).
Indeed, while decades-old studies suggested 20% of patients with advanced melanoma experience an objective tumor response to DTIC, more recent large multicenter studies indicate that the true figure is between 1 in 7 and 1 in 10, with no evidence DTIC offers any improvement over supportive care in terms of overall survival, he said at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
This discouraging assessment isn't just one oncologist's view. Dr. Alexander M.M. Eggermont noted during his presentation that the Dutch Cancer Society recently issued an advisory that the No. 1 option in patients with advanced melanoma is to enter them into any new drug development trial, even a phase I trial.
"So phase I studies are the preferred option in stage IV melanoma patients, rather than giving them the usual stuff. I think that's a very important message because that's really what we need to move the field forward," added Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands, and president-elect of the Federation of European Cancer Societies.
Phase III Trial Activity for Melanoma Is Robust : Biologics being studied include CTLA4 blockers, apoptosis restorers, and antiangiogenesis agents.
AMSTERDAM An unprecedented number of pivotal phase III trials of novel biologic therapies for melanoma are underway or about to start, according to speakers at the 11th World Congress on Cancers of the Skin.
"It's unbelievably busy in the field of melanoma these days," observed Dr. Alexander M.M. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands.
Among the biologic agents in phase III clinical trials for melanoma are cytotoxic T lymphocyte antigen 4 (CTLA4) blockers, apoptosis restorers, antiangiogenesis agents, and tyrosine kinase inhibitors. Numerous biologics are in earlier phase studies, including agents that interfere with melanoma's potent ability to repair chemotherapy-induced DNA damage.
"I think the CTLA4 antibodies are the most exciting agents on the horizon," Dr. Eggermont commented at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
Two such agents are in advanced development: ipilimumab, a Medarex/Bristol-Myers Squibb drug, and Pfizer's CP-675,206. Both are fully human monoclonal antibodies given by injection once every several months. CTLA4 blockade takes the brakes off T-cell proliferation, which results in an enhanced immunologic response to the tumor. These agents are in large phase III trialssome of them involving 1,000 advanced melanoma patientsas single-agent therapy, in combination with the alkylating agent dacarbazine (DTIC), as adjuvant therapy in patients with stage III or resected stage IV disease, or in conjunction with peptide vaccine therapy.
Up until now, therapeutic melanoma vaccine development programs have been "remarkably unsuccessful," with no indication of any effect on survival, Dr. Eggermont said. The early evidence suggests CTLA4 blockers may change that.
"We know we can induce immune responses. Many vaccine protocols have shown we can generate and induce T cell populations. The problem is we don't know how to maintain these T cell responses. Maintenance of the immune response is one of the critical barriers to successful development of vaccines. And here anti-CTLA4 is a crucial molecule. I predict it'll play an essential role across the board in vaccine development," he continued.
The phase II trials of CTLA4 blockers in patients with stage IV melanoma have collectively shown confirmed tumor response rates of 10%-15%, with about one-quarter of responses being complete and the remainder being long-lasting partial responses. Another 30%-40% of treated patients have experienced prolonged disease stabilization. There have been documented responses of visceral and brain metastases. The price paid for this anticancer efficacy has come in the form of immune-related adverse events affecting primarily the skin, gastrointestinal, and endocrine systems.
A particularly interesting attribute of the CTLA4 blockers is that more than 60% of confirmed responses have occurred only after more than 12 weeks of therapy. These delayed responses initially showed static or even progressive disease before later developing into partial responses, and in some cases they later evolved into complete responses.
"This is totally new kinetics," Dr. Eggermont noted. "It's different from anything you've ever seen with chemotherapy."
Dr. Céleste Lebbé, professor of dermatology and chief of dermato-oncology at Saint Louis Hospital (Paris) and the University of Paris VII, focused on the other agents in phase III: oblimersen (Genasense) and sorafenib (Nexavar).
▸ Oblimersen: This antisense oligonucleotide downregulates expression of the Bcl-2 protein. Bcl-2 overexpression inhibits apoptosis of cancer cells in response to chemotherapy or radiotherapy. Bcl-2 expression correlates negatively with treatment response and survival.
In a large phase III trial involving 771 patients with unresectable stage III or stage IV melanoma who were randomized to DTIC plus oblimersen or DTIC alone, the combination resulted in significantly better rates of overall response, complete response, durable response lasting more than 6 months, and progression-free survival (J. Clin. Oncol. 2006;24:4738-45).
Oblimersen failed to win regulatory approval in Europe or the United States based upon this study because the trend for improved overall survivalthe primary end pointdidn't achieve significance, but overall survival was significantly better with combination therapy in the 508 patients who had a normal baseline serum lactate dehydrogenase level, which was a prespecified stratification factor. Oblimersen's developer, Genta Inc., plans to conduct a repeat phase III trial, this time restricted to melanoma patients with normal lactate dehydrogenase levels, Dr. Lebbé said.
▸ Sorafenib: This Bayer drug is an antiangiogenesis agent by virtue of its inhibition of vascular endothelial growth factor 2, as well as an inhibitor of the mitogen-activated protein kinase signalling pathway with selectivity for the BRAF mutation present in 70% of melanoma patients. It quickly won regulatory approval in the United States and Europe for the treatment of renal cell carcinoma, and then for hepatocellular carcinoma, the most common malignancy worldwide. (See article on p. 18.)
Although all of this extensive research activity involving new biologic agents for advanced melanoma may look promising, a cautionary note was sounded by Dr. Mark R. Middleton of Cancer UK and the University of Oxford (England), who has witnessed a relentless succession of therapeutic disappointments on the melanoma front during his career in medical oncology.
"In melanoma we already have a wealth of therapeutic options. Untold numbers of drugs have been tested in our patients. Unfortunately, none of them work particularly well. The response rates are pretty dismal compared to those for most other solid tumors," Dr. Middleton observed.
Indeed, numerous combinations of chemotherapeutic agents or chemotherapy drugs and biologicsmainly interferons and interleukinshave been tested over the last 20 years. What these combinations have had in common was a weak therapeutic rationale and impressively high tumor response rates in mostly single-center phase II trials, which failed to translate into any overall survival advantage over DTIC alone in phase III studies.
"It's not that anybody's playing games with their phase-IIs, but naturally with combination regimens that you're trying for the first time you're going to enroll better, fitter patients and overestimate what you can get out of it, particularly if you're using historical controls," he explained.
"I think the definition of promising clinical activity has to be based on survival rather than response rates because we've clearly been caught out by the combination chemotherapy and biochemotherapy stories. It's very, very clear from that experience that the higher response rates haven't translated into survival improvements," Dr. Middleton added.
Dr. Middleton and Dr. Eggermont have received research funding from and are consultants to Schering-Plough.
In addition, Dr. Eggermont is a consultant to Bayer, Boehringer Ingelheim, GlaxoSmithKline, Sanofi Pasteur, Onyx Pharmaceuticals, Genta Inc., and Synta Pharmaceuticals. Dr. Lebbé has received research funding from Novartis.
"The definition of promising clinical activity has to be based on survival rather than response," said Dr. Mark R. Middleton. Bruce Jancin/Elsevier Global Medical News
AMSTERDAM An unprecedented number of pivotal phase III trials of novel biologic therapies for melanoma are underway or about to start, according to speakers at the 11th World Congress on Cancers of the Skin.
"It's unbelievably busy in the field of melanoma these days," observed Dr. Alexander M.M. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands.
Among the biologic agents in phase III clinical trials for melanoma are cytotoxic T lymphocyte antigen 4 (CTLA4) blockers, apoptosis restorers, antiangiogenesis agents, and tyrosine kinase inhibitors. Numerous biologics are in earlier phase studies, including agents that interfere with melanoma's potent ability to repair chemotherapy-induced DNA damage.
"I think the CTLA4 antibodies are the most exciting agents on the horizon," Dr. Eggermont commented at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
Two such agents are in advanced development: ipilimumab, a Medarex/Bristol-Myers Squibb drug, and Pfizer's CP-675,206. Both are fully human monoclonal antibodies given by injection once every several months. CTLA4 blockade takes the brakes off T-cell proliferation, which results in an enhanced immunologic response to the tumor. These agents are in large phase III trialssome of them involving 1,000 advanced melanoma patientsas single-agent therapy, in combination with the alkylating agent dacarbazine (DTIC), as adjuvant therapy in patients with stage III or resected stage IV disease, or in conjunction with peptide vaccine therapy.
Up until now, therapeutic melanoma vaccine development programs have been "remarkably unsuccessful," with no indication of any effect on survival, Dr. Eggermont said. The early evidence suggests CTLA4 blockers may change that.
"We know we can induce immune responses. Many vaccine protocols have shown we can generate and induce T cell populations. The problem is we don't know how to maintain these T cell responses. Maintenance of the immune response is one of the critical barriers to successful development of vaccines. And here anti-CTLA4 is a crucial molecule. I predict it'll play an essential role across the board in vaccine development," he continued.
The phase II trials of CTLA4 blockers in patients with stage IV melanoma have collectively shown confirmed tumor response rates of 10%-15%, with about one-quarter of responses being complete and the remainder being long-lasting partial responses. Another 30%-40% of treated patients have experienced prolonged disease stabilization. There have been documented responses of visceral and brain metastases. The price paid for this anticancer efficacy has come in the form of immune-related adverse events affecting primarily the skin, gastrointestinal, and endocrine systems.
A particularly interesting attribute of the CTLA4 blockers is that more than 60% of confirmed responses have occurred only after more than 12 weeks of therapy. These delayed responses initially showed static or even progressive disease before later developing into partial responses, and in some cases they later evolved into complete responses.
"This is totally new kinetics," Dr. Eggermont noted. "It's different from anything you've ever seen with chemotherapy."
Dr. Céleste Lebbé, professor of dermatology and chief of dermato-oncology at Saint Louis Hospital (Paris) and the University of Paris VII, focused on the other agents in phase III: oblimersen (Genasense) and sorafenib (Nexavar).
▸ Oblimersen: This antisense oligonucleotide downregulates expression of the Bcl-2 protein. Bcl-2 overexpression inhibits apoptosis of cancer cells in response to chemotherapy or radiotherapy. Bcl-2 expression correlates negatively with treatment response and survival.
In a large phase III trial involving 771 patients with unresectable stage III or stage IV melanoma who were randomized to DTIC plus oblimersen or DTIC alone, the combination resulted in significantly better rates of overall response, complete response, durable response lasting more than 6 months, and progression-free survival (J. Clin. Oncol. 2006;24:4738-45).
Oblimersen failed to win regulatory approval in Europe or the United States based upon this study because the trend for improved overall survivalthe primary end pointdidn't achieve significance, but overall survival was significantly better with combination therapy in the 508 patients who had a normal baseline serum lactate dehydrogenase level, which was a prespecified stratification factor. Oblimersen's developer, Genta Inc., plans to conduct a repeat phase III trial, this time restricted to melanoma patients with normal lactate dehydrogenase levels, Dr. Lebbé said.
▸ Sorafenib: This Bayer drug is an antiangiogenesis agent by virtue of its inhibition of vascular endothelial growth factor 2, as well as an inhibitor of the mitogen-activated protein kinase signalling pathway with selectivity for the BRAF mutation present in 70% of melanoma patients. It quickly won regulatory approval in the United States and Europe for the treatment of renal cell carcinoma, and then for hepatocellular carcinoma, the most common malignancy worldwide. (See article on p. 18.)
Although all of this extensive research activity involving new biologic agents for advanced melanoma may look promising, a cautionary note was sounded by Dr. Mark R. Middleton of Cancer UK and the University of Oxford (England), who has witnessed a relentless succession of therapeutic disappointments on the melanoma front during his career in medical oncology.
"In melanoma we already have a wealth of therapeutic options. Untold numbers of drugs have been tested in our patients. Unfortunately, none of them work particularly well. The response rates are pretty dismal compared to those for most other solid tumors," Dr. Middleton observed.
Indeed, numerous combinations of chemotherapeutic agents or chemotherapy drugs and biologicsmainly interferons and interleukinshave been tested over the last 20 years. What these combinations have had in common was a weak therapeutic rationale and impressively high tumor response rates in mostly single-center phase II trials, which failed to translate into any overall survival advantage over DTIC alone in phase III studies.
"It's not that anybody's playing games with their phase-IIs, but naturally with combination regimens that you're trying for the first time you're going to enroll better, fitter patients and overestimate what you can get out of it, particularly if you're using historical controls," he explained.
"I think the definition of promising clinical activity has to be based on survival rather than response rates because we've clearly been caught out by the combination chemotherapy and biochemotherapy stories. It's very, very clear from that experience that the higher response rates haven't translated into survival improvements," Dr. Middleton added.
Dr. Middleton and Dr. Eggermont have received research funding from and are consultants to Schering-Plough.
In addition, Dr. Eggermont is a consultant to Bayer, Boehringer Ingelheim, GlaxoSmithKline, Sanofi Pasteur, Onyx Pharmaceuticals, Genta Inc., and Synta Pharmaceuticals. Dr. Lebbé has received research funding from Novartis.
"The definition of promising clinical activity has to be based on survival rather than response," said Dr. Mark R. Middleton. Bruce Jancin/Elsevier Global Medical News
AMSTERDAM An unprecedented number of pivotal phase III trials of novel biologic therapies for melanoma are underway or about to start, according to speakers at the 11th World Congress on Cancers of the Skin.
"It's unbelievably busy in the field of melanoma these days," observed Dr. Alexander M.M. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, the Netherlands.
Among the biologic agents in phase III clinical trials for melanoma are cytotoxic T lymphocyte antigen 4 (CTLA4) blockers, apoptosis restorers, antiangiogenesis agents, and tyrosine kinase inhibitors. Numerous biologics are in earlier phase studies, including agents that interfere with melanoma's potent ability to repair chemotherapy-induced DNA damage.
"I think the CTLA4 antibodies are the most exciting agents on the horizon," Dr. Eggermont commented at the congress, which was cosponsored by the Skin Cancer Foundation and Erasmus University.
Two such agents are in advanced development: ipilimumab, a Medarex/Bristol-Myers Squibb drug, and Pfizer's CP-675,206. Both are fully human monoclonal antibodies given by injection once every several months. CTLA4 blockade takes the brakes off T-cell proliferation, which results in an enhanced immunologic response to the tumor. These agents are in large phase III trialssome of them involving 1,000 advanced melanoma patientsas single-agent therapy, in combination with the alkylating agent dacarbazine (DTIC), as adjuvant therapy in patients with stage III or resected stage IV disease, or in conjunction with peptide vaccine therapy.
Up until now, therapeutic melanoma vaccine development programs have been "remarkably unsuccessful," with no indication of any effect on survival, Dr. Eggermont said. The early evidence suggests CTLA4 blockers may change that.
"We know we can induce immune responses. Many vaccine protocols have shown we can generate and induce T cell populations. The problem is we don't know how to maintain these T cell responses. Maintenance of the immune response is one of the critical barriers to successful development of vaccines. And here anti-CTLA4 is a crucial molecule. I predict it'll play an essential role across the board in vaccine development," he continued.
The phase II trials of CTLA4 blockers in patients with stage IV melanoma have collectively shown confirmed tumor response rates of 10%-15%, with about one-quarter of responses being complete and the remainder being long-lasting partial responses. Another 30%-40% of treated patients have experienced prolonged disease stabilization. There have been documented responses of visceral and brain metastases. The price paid for this anticancer efficacy has come in the form of immune-related adverse events affecting primarily the skin, gastrointestinal, and endocrine systems.
A particularly interesting attribute of the CTLA4 blockers is that more than 60% of confirmed responses have occurred only after more than 12 weeks of therapy. These delayed responses initially showed static or even progressive disease before later developing into partial responses, and in some cases they later evolved into complete responses.
"This is totally new kinetics," Dr. Eggermont noted. "It's different from anything you've ever seen with chemotherapy."
Dr. Céleste Lebbé, professor of dermatology and chief of dermato-oncology at Saint Louis Hospital (Paris) and the University of Paris VII, focused on the other agents in phase III: oblimersen (Genasense) and sorafenib (Nexavar).
▸ Oblimersen: This antisense oligonucleotide downregulates expression of the Bcl-2 protein. Bcl-2 overexpression inhibits apoptosis of cancer cells in response to chemotherapy or radiotherapy. Bcl-2 expression correlates negatively with treatment response and survival.
In a large phase III trial involving 771 patients with unresectable stage III or stage IV melanoma who were randomized to DTIC plus oblimersen or DTIC alone, the combination resulted in significantly better rates of overall response, complete response, durable response lasting more than 6 months, and progression-free survival (J. Clin. Oncol. 2006;24:4738-45).
Oblimersen failed to win regulatory approval in Europe or the United States based upon this study because the trend for improved overall survivalthe primary end pointdidn't achieve significance, but overall survival was significantly better with combination therapy in the 508 patients who had a normal baseline serum lactate dehydrogenase level, which was a prespecified stratification factor. Oblimersen's developer, Genta Inc., plans to conduct a repeat phase III trial, this time restricted to melanoma patients with normal lactate dehydrogenase levels, Dr. Lebbé said.
▸ Sorafenib: This Bayer drug is an antiangiogenesis agent by virtue of its inhibition of vascular endothelial growth factor 2, as well as an inhibitor of the mitogen-activated protein kinase signalling pathway with selectivity for the BRAF mutation present in 70% of melanoma patients. It quickly won regulatory approval in the United States and Europe for the treatment of renal cell carcinoma, and then for hepatocellular carcinoma, the most common malignancy worldwide. (See article on p. 18.)
Although all of this extensive research activity involving new biologic agents for advanced melanoma may look promising, a cautionary note was sounded by Dr. Mark R. Middleton of Cancer UK and the University of Oxford (England), who has witnessed a relentless succession of therapeutic disappointments on the melanoma front during his career in medical oncology.
"In melanoma we already have a wealth of therapeutic options. Untold numbers of drugs have been tested in our patients. Unfortunately, none of them work particularly well. The response rates are pretty dismal compared to those for most other solid tumors," Dr. Middleton observed.
Indeed, numerous combinations of chemotherapeutic agents or chemotherapy drugs and biologicsmainly interferons and interleukinshave been tested over the last 20 years. What these combinations have had in common was a weak therapeutic rationale and impressively high tumor response rates in mostly single-center phase II trials, which failed to translate into any overall survival advantage over DTIC alone in phase III studies.
"It's not that anybody's playing games with their phase-IIs, but naturally with combination regimens that you're trying for the first time you're going to enroll better, fitter patients and overestimate what you can get out of it, particularly if you're using historical controls," he explained.
"I think the definition of promising clinical activity has to be based on survival rather than response rates because we've clearly been caught out by the combination chemotherapy and biochemotherapy stories. It's very, very clear from that experience that the higher response rates haven't translated into survival improvements," Dr. Middleton added.
Dr. Middleton and Dr. Eggermont have received research funding from and are consultants to Schering-Plough.
In addition, Dr. Eggermont is a consultant to Bayer, Boehringer Ingelheim, GlaxoSmithKline, Sanofi Pasteur, Onyx Pharmaceuticals, Genta Inc., and Synta Pharmaceuticals. Dr. Lebbé has received research funding from Novartis.
"The definition of promising clinical activity has to be based on survival rather than response," said Dr. Mark R. Middleton. Bruce Jancin/Elsevier Global Medical News
New Anticancer Agents Have Distinctive Toxicities
AMSTERDAM The highly promising new class of investigational anticancer agents known at cytotoxic T-lymphocyte antigen 4 blockers has a characteristic group of side effects of special interest to dermatologists, gastroenterologists, and endocrinologists, Dr. Alexander M.M. Eggermont said at the 11th World Congress on Cancers of the Skin.
Two fully human monoclonal antibodies to CTLA4 are making major waves in oncology circles because of their efficacy in early clinical trials for the treatment of advanced melanoma, a disease which has seen discouragingly little therapeutic progress in the last 3 decades.
But it is apparent that this impressive efficacy comes at the price of what are known in the field as immune-related adverse events, or IRAEs, affecting mainly the dermatologic, gastrointestinal, and endocrinologic domains. The CTLA4 blockers have moved into an extensive program of large phase III clinical trials, so an increasing number of physicians will be confronted with IRAEs, which require prompt diagnosis and intervention, noted Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, and president-elect of the Federation of European Cancer Societies.
CTLA4 is expressed on T cells, where it functions as a fundamental negative regulator of T-cell activation. CTLA4 blockade essentially allows T-cell proliferation, enabling the patient's immune system to mount a more vigorous, prolonged, and effective anticancer responseand, in a sizable minority of cases, trigger IRAEs.
"If you have subclinical autoimmune disease, you may be propelled into clinical disease manifestations because the hand brake is off your T-cell populations," Dr. Eggermont explained at the congress, cosponsored by the Skin Cancer Foundation and Erasmus University.
Dermatologic IRAEs take the form of an array of rashes, vitiligo, and pruritic conditions involving specific T-cell infiltrates at the lesion sites. These are usually mild to moderate grade 1 or 2 side effects that resolve with corticosteroid therapy or discontinuation of the biologic agent.
Gastrointestinal IRAEs most often consist of mild to moderate enterocolitis. But occasionally, the colitis is grade 3, marked by bloody diarrhea, or grade 4, involving perforation, which is potentially fatal. Aggressive medical management, often including high doses of steroids, is sometimes required to control these toxicities.
Endocrinologic IRAEs are particularly puzzling, because they involve mainly the pituitary, a gland ordinarily very well protected against autoimmune disease. But a small number of patients with metastatic melanoma or renal cancer who are placed on anti-CTLA4 monoclonal antibody therapyless than 1% thus fardevelop autoimmune hypophysitis.
"You go into an addisonian crisis. It's not a small thing. At the sella turcica, you see a swollen pituitary gland, which will become normal again after you've stopped therapy. You need to intervene here with corticosteroids and hormone substitution," he continued.
The most intriguing thing about the IRAEs is their strong correlation with induction of tumor regression. Investigators at the National Cancer Institute reported on 198 patients with metastatic melanoma or renal cell carcinoma treated with the CTLA4 monoclonal antibody ipilimumab. Twenty-one percent of the treated patients developed grade 3 or 4 autoimmune enterocolitis. The objective tumor response rate was 36% in those melanoma patients with colitis and 11% in those without. Similarly, 35% of renal cell carcinoma patients with colitis had an objective tumor response, compared with just 2% without colitis (J. Clin. Oncol. 2006;24:2283-9).
Dr. Eggermont is a consultant to Bristol-Myers Squibb Co., which together with Medarex Inc., is developing ipilimumab. The other CTLA4 blocker in clinical development is a Pfizer drug known for now as CP-675,206.
Dermatologic adverse events take the form of rashes, vitiligo, and pruritic conditions. DR. EGGERMONT
AMSTERDAM The highly promising new class of investigational anticancer agents known at cytotoxic T-lymphocyte antigen 4 blockers has a characteristic group of side effects of special interest to dermatologists, gastroenterologists, and endocrinologists, Dr. Alexander M.M. Eggermont said at the 11th World Congress on Cancers of the Skin.
Two fully human monoclonal antibodies to CTLA4 are making major waves in oncology circles because of their efficacy in early clinical trials for the treatment of advanced melanoma, a disease which has seen discouragingly little therapeutic progress in the last 3 decades.
But it is apparent that this impressive efficacy comes at the price of what are known in the field as immune-related adverse events, or IRAEs, affecting mainly the dermatologic, gastrointestinal, and endocrinologic domains. The CTLA4 blockers have moved into an extensive program of large phase III clinical trials, so an increasing number of physicians will be confronted with IRAEs, which require prompt diagnosis and intervention, noted Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, and president-elect of the Federation of European Cancer Societies.
CTLA4 is expressed on T cells, where it functions as a fundamental negative regulator of T-cell activation. CTLA4 blockade essentially allows T-cell proliferation, enabling the patient's immune system to mount a more vigorous, prolonged, and effective anticancer responseand, in a sizable minority of cases, trigger IRAEs.
"If you have subclinical autoimmune disease, you may be propelled into clinical disease manifestations because the hand brake is off your T-cell populations," Dr. Eggermont explained at the congress, cosponsored by the Skin Cancer Foundation and Erasmus University.
Dermatologic IRAEs take the form of an array of rashes, vitiligo, and pruritic conditions involving specific T-cell infiltrates at the lesion sites. These are usually mild to moderate grade 1 or 2 side effects that resolve with corticosteroid therapy or discontinuation of the biologic agent.
Gastrointestinal IRAEs most often consist of mild to moderate enterocolitis. But occasionally, the colitis is grade 3, marked by bloody diarrhea, or grade 4, involving perforation, which is potentially fatal. Aggressive medical management, often including high doses of steroids, is sometimes required to control these toxicities.
Endocrinologic IRAEs are particularly puzzling, because they involve mainly the pituitary, a gland ordinarily very well protected against autoimmune disease. But a small number of patients with metastatic melanoma or renal cancer who are placed on anti-CTLA4 monoclonal antibody therapyless than 1% thus fardevelop autoimmune hypophysitis.
"You go into an addisonian crisis. It's not a small thing. At the sella turcica, you see a swollen pituitary gland, which will become normal again after you've stopped therapy. You need to intervene here with corticosteroids and hormone substitution," he continued.
The most intriguing thing about the IRAEs is their strong correlation with induction of tumor regression. Investigators at the National Cancer Institute reported on 198 patients with metastatic melanoma or renal cell carcinoma treated with the CTLA4 monoclonal antibody ipilimumab. Twenty-one percent of the treated patients developed grade 3 or 4 autoimmune enterocolitis. The objective tumor response rate was 36% in those melanoma patients with colitis and 11% in those without. Similarly, 35% of renal cell carcinoma patients with colitis had an objective tumor response, compared with just 2% without colitis (J. Clin. Oncol. 2006;24:2283-9).
Dr. Eggermont is a consultant to Bristol-Myers Squibb Co., which together with Medarex Inc., is developing ipilimumab. The other CTLA4 blocker in clinical development is a Pfizer drug known for now as CP-675,206.
Dermatologic adverse events take the form of rashes, vitiligo, and pruritic conditions. DR. EGGERMONT
AMSTERDAM The highly promising new class of investigational anticancer agents known at cytotoxic T-lymphocyte antigen 4 blockers has a characteristic group of side effects of special interest to dermatologists, gastroenterologists, and endocrinologists, Dr. Alexander M.M. Eggermont said at the 11th World Congress on Cancers of the Skin.
Two fully human monoclonal antibodies to CTLA4 are making major waves in oncology circles because of their efficacy in early clinical trials for the treatment of advanced melanoma, a disease which has seen discouragingly little therapeutic progress in the last 3 decades.
But it is apparent that this impressive efficacy comes at the price of what are known in the field as immune-related adverse events, or IRAEs, affecting mainly the dermatologic, gastrointestinal, and endocrinologic domains. The CTLA4 blockers have moved into an extensive program of large phase III clinical trials, so an increasing number of physicians will be confronted with IRAEs, which require prompt diagnosis and intervention, noted Dr. Eggermont, professor and head of surgical oncology at Erasmus University Medical Center, Rotterdam, and president-elect of the Federation of European Cancer Societies.
CTLA4 is expressed on T cells, where it functions as a fundamental negative regulator of T-cell activation. CTLA4 blockade essentially allows T-cell proliferation, enabling the patient's immune system to mount a more vigorous, prolonged, and effective anticancer responseand, in a sizable minority of cases, trigger IRAEs.
"If you have subclinical autoimmune disease, you may be propelled into clinical disease manifestations because the hand brake is off your T-cell populations," Dr. Eggermont explained at the congress, cosponsored by the Skin Cancer Foundation and Erasmus University.
Dermatologic IRAEs take the form of an array of rashes, vitiligo, and pruritic conditions involving specific T-cell infiltrates at the lesion sites. These are usually mild to moderate grade 1 or 2 side effects that resolve with corticosteroid therapy or discontinuation of the biologic agent.
Gastrointestinal IRAEs most often consist of mild to moderate enterocolitis. But occasionally, the colitis is grade 3, marked by bloody diarrhea, or grade 4, involving perforation, which is potentially fatal. Aggressive medical management, often including high doses of steroids, is sometimes required to control these toxicities.
Endocrinologic IRAEs are particularly puzzling, because they involve mainly the pituitary, a gland ordinarily very well protected against autoimmune disease. But a small number of patients with metastatic melanoma or renal cancer who are placed on anti-CTLA4 monoclonal antibody therapyless than 1% thus fardevelop autoimmune hypophysitis.
"You go into an addisonian crisis. It's not a small thing. At the sella turcica, you see a swollen pituitary gland, which will become normal again after you've stopped therapy. You need to intervene here with corticosteroids and hormone substitution," he continued.
The most intriguing thing about the IRAEs is their strong correlation with induction of tumor regression. Investigators at the National Cancer Institute reported on 198 patients with metastatic melanoma or renal cell carcinoma treated with the CTLA4 monoclonal antibody ipilimumab. Twenty-one percent of the treated patients developed grade 3 or 4 autoimmune enterocolitis. The objective tumor response rate was 36% in those melanoma patients with colitis and 11% in those without. Similarly, 35% of renal cell carcinoma patients with colitis had an objective tumor response, compared with just 2% without colitis (J. Clin. Oncol. 2006;24:2283-9).
Dr. Eggermont is a consultant to Bristol-Myers Squibb Co., which together with Medarex Inc., is developing ipilimumab. The other CTLA4 blocker in clinical development is a Pfizer drug known for now as CP-675,206.
Dermatologic adverse events take the form of rashes, vitiligo, and pruritic conditions. DR. EGGERMONT
Spontaneous Pneumomediastinum
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.
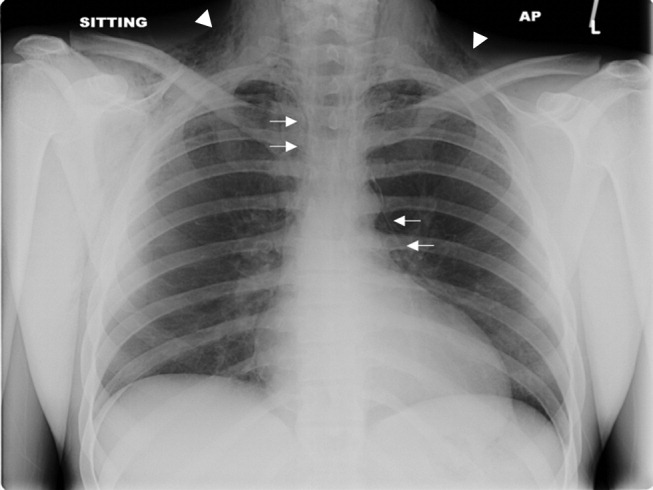

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.
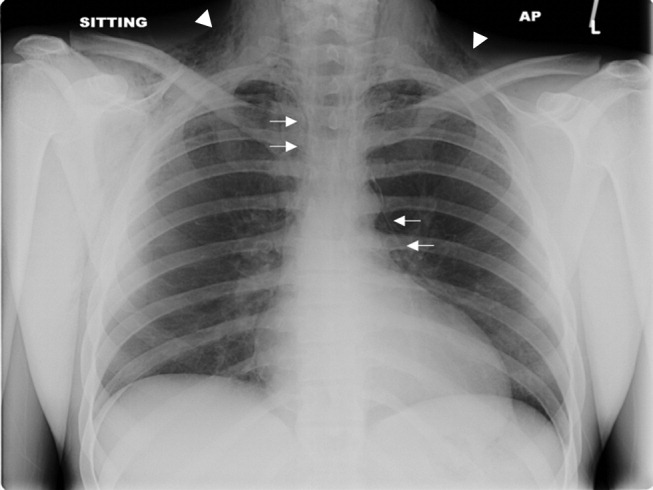

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.
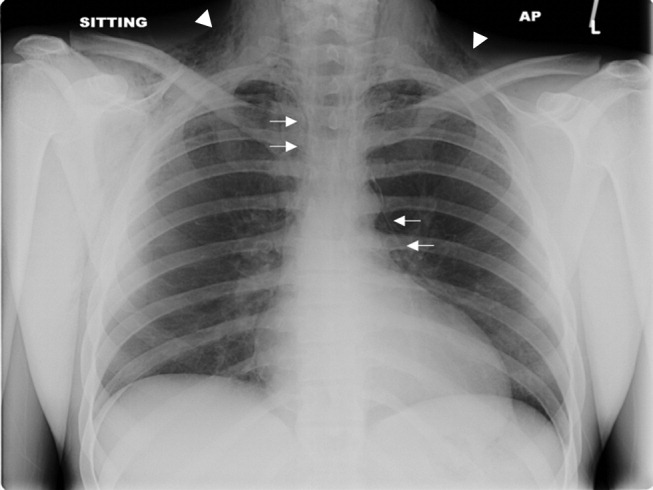

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.