User login
Safety after Surgery
An 86-year-old female with Alzheimer’s dementia, hypertension, type 2 diabetes, and chronic obstructive pulmonary disease was admitted with lethargy, fever, and vomiting. After she was diagnosed with necrotizing cholecystitis, she underwent an emergent cholecystectomy. Three days later the patient was short of breath, confused, and hadn’t urinated since the indwelling catheter was removed.
Sound familiar? If this scenario doesn’t ring a bell now, then it soon will. The 65-and-up age group is the fastest growing section of the United States population. A recent poll found that elderly patients now account for more than 60% of most general surgeons’ practices. Additionally, the use of minimally invasive surgical techniques and advanced perioperative monitoring has permitted elderly patients who were previously considered too debilitated to now become surgical candidates.
Though patients and their families most often worry about events in the operating room, the vast majority of complications occur in the postoperative period. Morbidity and mortality rates double during the first 24 hours after surgery and are tenfold higher over the remainder of the first postoperative week. In a recent study of more than 500 elderly general surgery patients, 21% experienced complications during this period.
The most common postoperative complications in the geriatric population include delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. The goal in managing any elderly patient is to preserve cognitive and physical function. Maintaining this goal in the postoperative setting requires the early implementation of preventive measures, as well as an understanding of when age-appropriate intervention is necessary.
Hospitalists are often the first line of defense for postoperative situations in medically ill patients, and an amplification of issues unique to the geriatric patient follows.
Delirium
Postoperative delirium occurs in 10%-15% of older general surgery patients and in 30%-60% of older patients who undergo orthopedic procedures. The most common presentation of delirium in the elderly postoperative patient is a “quiet confusion” that is more pronounced in the evening—otherwise known as sundowning. An acute change in mental status, manifested as a fluctuating level of consciousness or a cognitive deficit, is also common. Though delirium may result solely from the acute stress of the operation, other medically relevant causes include metabolic abnormalities, abnormal respiratory parameters, infections, and medications, and these causes should be aggressively investigated and treated.
After potential medical etiologies have been addressed, focus the treatment of delirium in the elderly postoperative patient on interventions to restore mental and physical function as well as pharmacotherapy. Measures to restore function, such as early mobilization and ambulation, sleep hygiene, volume repletion, and restoration of vision and hearing with appropriate devices, have been shown to decrease the duration of the delirium episode. Other non-pharmacologic interventions, including placing a patient near the nurses’ station, encouraging social visits with caregivers, and avoiding the use of physical restraints (which can aggravate agitation) may also prove helpful.
Avoid the use of psychoactive medications (e.g., antiarrhythmic agents, tricyclic antidepressants, neuroleptics, gastrointestinal medications, antihistamines, ciprofloxacin, nonsteroidal anti-inflammatory drugs, meperidine, and cimetidine) as much as possible during the acute confusional state.
Pharmacologic treatment of delirium may be warranted in patients experiencing symptoms of psychosis or in those exhibiting signs of physical aggression or severe personal distress. Haloperidol and risperidol are the medications of choice, though the FDA has approved neither drug specifically for this indication. High doses of these medications are associated with extrapyramidal effects, dystonic reactions, and torsade de pointe. Once the delirium begins to resolve, doses should be tapered gradually over several days.
Ileus
Postsurgical ileus can cause profound clinical consequences in elderly patients. This complication is associated with delayed enteral feeding and malnutrition, increased length of hospital stay, and increased risk of pulmonary complications. Patients present with abdominal distension, nausea and vomiting, limited flatus, and a decreased presence of bowel sounds on auscultation. In cases of prolonged postsurgical ileus, consider pseudo-obstruction (Ogilvie’s syndrome) and mechanical obstruction.
Intravenous hydration and nutrition (in prolonged cases), assisted ambulation, and the avoidance of opiates remain the mainstays of treatment. Nasogastric tubes may provide symptomatic relief in patients with nausea and vomiting, but studies don’t support the use of this intervention to enhance resolution of the ileus. Many prokinetic agents have been examined for this use, including neostigmine and cisapride, but the results have been mixed, and the side effect profiles are generally unacceptable for elderly patients. Delay oral feeding until satisfactory bowel function has been restored.
Nutritional Care
An estimated 12%-50% of geriatric patients are found to be malnourished in the acute hospital setting. The adverse effects of malnutrition include delayed wound healing, greater risk of sepsis and wound infections, deterioration of functional status secondary to muscle wasting, and increased mortality.
Early identification of the patient’s feeding limitations is the key to preventing adverse outcomes. If a patient is restricted from oral or enteral feeding, parenteral nutrition should be started within 48 hours. When volitional food intake is permitted, the addition of canned nutritional supplements, fortified meals, and between-meal snacks may improve elderly patients’ energy and protein intake.
Initiate enteral feeding in patients for whom voluntary food intake is decreased. Parenteral nutrition may still be required until enteral feeding is established, however, and prescribed nutrients can be administered enterally. Because glucose tolerance diminishes with normal aging and may be further reduced in a state of acute illness, initiation of insulin therapy may be necessary in patients receiving either enteral or parenteral supplementation. Additionally, supplementation with a zinc-containing daily multivitamin has been shown to enhance immune function and prevent infections.
Respiratory Care
Respiratory function may be diminished in elderly patients due to age-related changes in the upper and lower respiratory tracts. Factors that contribute to an increased rate of pulmonary postoperative complications include diminished protective mechanisms like coughing and swallowing, decreased compliance of the chest wall and lung tissue, inadequate mucociliary transport, and a blunted ventilatory response to hypoxia and hypercapnia. Postoperative respiratory complications, including pneumonia, hypoxemia, hypoventilation, and atelectasis, occur in 2.1%-10.2% of elderly patients. These complications are associated with increased length of stay and a higher risk of long-term mortality.
Respiratory function may be preserved in the postoperative geriatric patient using a variety of measures. Effective pain control is essential in maintaining adequate lung volumes, and regional analgesia is associated with less-severe postoperative decreases in vital capacity and functional residual capacity (FRC). Once postoperative pain has been controlled, encourage the early resumption of physical activity (with appropriate assistance). Positioning patients in a seated position increases FRC and improves gas exchange in those recovering from abdominal procedures. Additionally, incentive spirometers, breathing exercises, and intermittent positive-pressure breathing may reduce the incidence of pulmonary complications after upper-abdominal operations, shortening the length of hospital stay.
Thromboembolic Disease
Fatal pulmonary embolism accounts for a large proportion of postoperative deaths in the elderly population. Between 20%-30% of patients undergoing general surgery without prophylaxis develop deep vein thrombosis, and the incidence is as high as 40% in those undergoing orthopedic surgeries, gynecologic cancer operations, and major neurosurgical procedures.
The Fifth American College of Chest Physicians Consensus Conference on Antithrombotic Therapy recommends the following postoperative interventions for older surgical patients:
- General surgery without clinical risk factors for thrombosis: Give low-dose unfractionated heparin two hours before and every 12 hours after the operation;
- General surgery with any clinical risk factors such as prolonged immobilization or paralysis, obesity, varicose veins, congestive heart failure, or pelvic or leg fractures: Administer low molecular weight heparin (LMWH) or low-dose unfractionated heparin every eight hours. If the patient is also prone to bleeding or infection, intermittent pneumatic compression (IPC) can be used instead;
- General surgery with multiple clinical risk factors or with a history of previous deep vein thrombosis, malignancy, stroke, spinal cord injury, or hip fracture: Use low dose unfractionated heparin or LMWH combined with intermittent pneumatic compression; for very high risk patients, perioperative warfarin is an alternative;
- Total hip replacement: Give postoperative LMWH every 12 hours; initiate low-intensity warfarin therapy—to keep International Normalized Ratio of 2-3—preoperatively or immediately postoperatively;
- Total knee replacement: Administer postoperative LMWH every 12 hours. IPC is the most effective non-pharmacologic regimen and is comparable to LMWH. Low-intensity warfarin can also be used; and
- Hip fracture repair: Start preoperative fixed-dose LMWH or low-intensity warfarin.
Urinary Retention
The incidence of postoperative urinary retention in elderly patients has been reported to be as high as 87%. Factors contributing to the development of this complication include immobility, analgesics and opiates, intravenous hydration, and general anesthesia. Urinary retention can lead to overflow incontinence and urinary tract infection and is associated with a decline in function and nursing home placement. The first indication of urinary retention may be a diminished urinary output after removal of an indwelling catheter, overflow incontinence, or the frequent voiding of small amounts of urine.
Urinary retention is treated with catheterization. This prevents bladder distension, which leads to reduced detrusor contractile function, and helps restore preoperative bladder function.
Recent studies have found that normal voiding resumes earlier with the use of intermittent catheterization (if begun at the onset of urinary retention and repeated every six to eight hours) than with the use of an indwelling catheter. Additionally, the use of indwelling catheters in the elderly after the immediate perioperative period is associated with an increased risk of urosepsis and a more dependent postoperative functional status.
Conclusion
The 65-and-up age group is the fastest growing section of the United States population. The vast majority of complications for this age group occur in the postoperative period. It’s important for hospitalists to remain involved in key areas of postoperative complications in the geriatric population—specifically, delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. TH
Jill Landis is a frequent contributor to The Hospitalist.
References
- Souders JE, Rooke GA. Perioperative care for geriatric patients. Ann Long Term Care. 2005;13(6):17-29.
- Williams SL, Jones PB, Pofahl WE. Preoperative management of the older patient—a surgeon’s perspective: part I. Ann Long Term Care. 2006;14(6):24-30.
- Palmer RM. Management of common clinical disorders in geriatric patients: delirium. ACP Medicine Online. June 7, 2006. Available at: www.medscape.com/viewarticle/534766. Last accessed January 11, 2007.
- Manku K, Bacchetti P, Leung JM. Prognostic significance of postoperative in-hospital complications in elderly patients. I. Long-term survival. Anesth Analg. 2003 Feb;96(2):583-589.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient: introduction. ACS Surgery Online. June 7, 2006. Available at: www.medscape.com/viewarticle/535461?rss. Last accessed January 11, 2006.
- Skelly JM, Guyatt GH, Kalbfleisch R, et al. Management of urinary retention after surgical repair of hip fracture. CMAJ. 1992 Apr 1;146(7):1185-1189.
- Wittbrodt E. The impact of postoperative ileus and emerging therapies. Pharm Treatment. 2006 Jan;31(1):39-59.
An 86-year-old female with Alzheimer’s dementia, hypertension, type 2 diabetes, and chronic obstructive pulmonary disease was admitted with lethargy, fever, and vomiting. After she was diagnosed with necrotizing cholecystitis, she underwent an emergent cholecystectomy. Three days later the patient was short of breath, confused, and hadn’t urinated since the indwelling catheter was removed.
Sound familiar? If this scenario doesn’t ring a bell now, then it soon will. The 65-and-up age group is the fastest growing section of the United States population. A recent poll found that elderly patients now account for more than 60% of most general surgeons’ practices. Additionally, the use of minimally invasive surgical techniques and advanced perioperative monitoring has permitted elderly patients who were previously considered too debilitated to now become surgical candidates.
Though patients and their families most often worry about events in the operating room, the vast majority of complications occur in the postoperative period. Morbidity and mortality rates double during the first 24 hours after surgery and are tenfold higher over the remainder of the first postoperative week. In a recent study of more than 500 elderly general surgery patients, 21% experienced complications during this period.
The most common postoperative complications in the geriatric population include delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. The goal in managing any elderly patient is to preserve cognitive and physical function. Maintaining this goal in the postoperative setting requires the early implementation of preventive measures, as well as an understanding of when age-appropriate intervention is necessary.
Hospitalists are often the first line of defense for postoperative situations in medically ill patients, and an amplification of issues unique to the geriatric patient follows.
Delirium
Postoperative delirium occurs in 10%-15% of older general surgery patients and in 30%-60% of older patients who undergo orthopedic procedures. The most common presentation of delirium in the elderly postoperative patient is a “quiet confusion” that is more pronounced in the evening—otherwise known as sundowning. An acute change in mental status, manifested as a fluctuating level of consciousness or a cognitive deficit, is also common. Though delirium may result solely from the acute stress of the operation, other medically relevant causes include metabolic abnormalities, abnormal respiratory parameters, infections, and medications, and these causes should be aggressively investigated and treated.
After potential medical etiologies have been addressed, focus the treatment of delirium in the elderly postoperative patient on interventions to restore mental and physical function as well as pharmacotherapy. Measures to restore function, such as early mobilization and ambulation, sleep hygiene, volume repletion, and restoration of vision and hearing with appropriate devices, have been shown to decrease the duration of the delirium episode. Other non-pharmacologic interventions, including placing a patient near the nurses’ station, encouraging social visits with caregivers, and avoiding the use of physical restraints (which can aggravate agitation) may also prove helpful.
Avoid the use of psychoactive medications (e.g., antiarrhythmic agents, tricyclic antidepressants, neuroleptics, gastrointestinal medications, antihistamines, ciprofloxacin, nonsteroidal anti-inflammatory drugs, meperidine, and cimetidine) as much as possible during the acute confusional state.
Pharmacologic treatment of delirium may be warranted in patients experiencing symptoms of psychosis or in those exhibiting signs of physical aggression or severe personal distress. Haloperidol and risperidol are the medications of choice, though the FDA has approved neither drug specifically for this indication. High doses of these medications are associated with extrapyramidal effects, dystonic reactions, and torsade de pointe. Once the delirium begins to resolve, doses should be tapered gradually over several days.
Ileus
Postsurgical ileus can cause profound clinical consequences in elderly patients. This complication is associated with delayed enteral feeding and malnutrition, increased length of hospital stay, and increased risk of pulmonary complications. Patients present with abdominal distension, nausea and vomiting, limited flatus, and a decreased presence of bowel sounds on auscultation. In cases of prolonged postsurgical ileus, consider pseudo-obstruction (Ogilvie’s syndrome) and mechanical obstruction.
Intravenous hydration and nutrition (in prolonged cases), assisted ambulation, and the avoidance of opiates remain the mainstays of treatment. Nasogastric tubes may provide symptomatic relief in patients with nausea and vomiting, but studies don’t support the use of this intervention to enhance resolution of the ileus. Many prokinetic agents have been examined for this use, including neostigmine and cisapride, but the results have been mixed, and the side effect profiles are generally unacceptable for elderly patients. Delay oral feeding until satisfactory bowel function has been restored.
Nutritional Care
An estimated 12%-50% of geriatric patients are found to be malnourished in the acute hospital setting. The adverse effects of malnutrition include delayed wound healing, greater risk of sepsis and wound infections, deterioration of functional status secondary to muscle wasting, and increased mortality.
Early identification of the patient’s feeding limitations is the key to preventing adverse outcomes. If a patient is restricted from oral or enteral feeding, parenteral nutrition should be started within 48 hours. When volitional food intake is permitted, the addition of canned nutritional supplements, fortified meals, and between-meal snacks may improve elderly patients’ energy and protein intake.
Initiate enteral feeding in patients for whom voluntary food intake is decreased. Parenteral nutrition may still be required until enteral feeding is established, however, and prescribed nutrients can be administered enterally. Because glucose tolerance diminishes with normal aging and may be further reduced in a state of acute illness, initiation of insulin therapy may be necessary in patients receiving either enteral or parenteral supplementation. Additionally, supplementation with a zinc-containing daily multivitamin has been shown to enhance immune function and prevent infections.
Respiratory Care
Respiratory function may be diminished in elderly patients due to age-related changes in the upper and lower respiratory tracts. Factors that contribute to an increased rate of pulmonary postoperative complications include diminished protective mechanisms like coughing and swallowing, decreased compliance of the chest wall and lung tissue, inadequate mucociliary transport, and a blunted ventilatory response to hypoxia and hypercapnia. Postoperative respiratory complications, including pneumonia, hypoxemia, hypoventilation, and atelectasis, occur in 2.1%-10.2% of elderly patients. These complications are associated with increased length of stay and a higher risk of long-term mortality.
Respiratory function may be preserved in the postoperative geriatric patient using a variety of measures. Effective pain control is essential in maintaining adequate lung volumes, and regional analgesia is associated with less-severe postoperative decreases in vital capacity and functional residual capacity (FRC). Once postoperative pain has been controlled, encourage the early resumption of physical activity (with appropriate assistance). Positioning patients in a seated position increases FRC and improves gas exchange in those recovering from abdominal procedures. Additionally, incentive spirometers, breathing exercises, and intermittent positive-pressure breathing may reduce the incidence of pulmonary complications after upper-abdominal operations, shortening the length of hospital stay.
Thromboembolic Disease
Fatal pulmonary embolism accounts for a large proportion of postoperative deaths in the elderly population. Between 20%-30% of patients undergoing general surgery without prophylaxis develop deep vein thrombosis, and the incidence is as high as 40% in those undergoing orthopedic surgeries, gynecologic cancer operations, and major neurosurgical procedures.
The Fifth American College of Chest Physicians Consensus Conference on Antithrombotic Therapy recommends the following postoperative interventions for older surgical patients:
- General surgery without clinical risk factors for thrombosis: Give low-dose unfractionated heparin two hours before and every 12 hours after the operation;
- General surgery with any clinical risk factors such as prolonged immobilization or paralysis, obesity, varicose veins, congestive heart failure, or pelvic or leg fractures: Administer low molecular weight heparin (LMWH) or low-dose unfractionated heparin every eight hours. If the patient is also prone to bleeding or infection, intermittent pneumatic compression (IPC) can be used instead;
- General surgery with multiple clinical risk factors or with a history of previous deep vein thrombosis, malignancy, stroke, spinal cord injury, or hip fracture: Use low dose unfractionated heparin or LMWH combined with intermittent pneumatic compression; for very high risk patients, perioperative warfarin is an alternative;
- Total hip replacement: Give postoperative LMWH every 12 hours; initiate low-intensity warfarin therapy—to keep International Normalized Ratio of 2-3—preoperatively or immediately postoperatively;
- Total knee replacement: Administer postoperative LMWH every 12 hours. IPC is the most effective non-pharmacologic regimen and is comparable to LMWH. Low-intensity warfarin can also be used; and
- Hip fracture repair: Start preoperative fixed-dose LMWH or low-intensity warfarin.
Urinary Retention
The incidence of postoperative urinary retention in elderly patients has been reported to be as high as 87%. Factors contributing to the development of this complication include immobility, analgesics and opiates, intravenous hydration, and general anesthesia. Urinary retention can lead to overflow incontinence and urinary tract infection and is associated with a decline in function and nursing home placement. The first indication of urinary retention may be a diminished urinary output after removal of an indwelling catheter, overflow incontinence, or the frequent voiding of small amounts of urine.
Urinary retention is treated with catheterization. This prevents bladder distension, which leads to reduced detrusor contractile function, and helps restore preoperative bladder function.
Recent studies have found that normal voiding resumes earlier with the use of intermittent catheterization (if begun at the onset of urinary retention and repeated every six to eight hours) than with the use of an indwelling catheter. Additionally, the use of indwelling catheters in the elderly after the immediate perioperative period is associated with an increased risk of urosepsis and a more dependent postoperative functional status.
Conclusion
The 65-and-up age group is the fastest growing section of the United States population. The vast majority of complications for this age group occur in the postoperative period. It’s important for hospitalists to remain involved in key areas of postoperative complications in the geriatric population—specifically, delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. TH
Jill Landis is a frequent contributor to The Hospitalist.
References
- Souders JE, Rooke GA. Perioperative care for geriatric patients. Ann Long Term Care. 2005;13(6):17-29.
- Williams SL, Jones PB, Pofahl WE. Preoperative management of the older patient—a surgeon’s perspective: part I. Ann Long Term Care. 2006;14(6):24-30.
- Palmer RM. Management of common clinical disorders in geriatric patients: delirium. ACP Medicine Online. June 7, 2006. Available at: www.medscape.com/viewarticle/534766. Last accessed January 11, 2007.
- Manku K, Bacchetti P, Leung JM. Prognostic significance of postoperative in-hospital complications in elderly patients. I. Long-term survival. Anesth Analg. 2003 Feb;96(2):583-589.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient: introduction. ACS Surgery Online. June 7, 2006. Available at: www.medscape.com/viewarticle/535461?rss. Last accessed January 11, 2006.
- Skelly JM, Guyatt GH, Kalbfleisch R, et al. Management of urinary retention after surgical repair of hip fracture. CMAJ. 1992 Apr 1;146(7):1185-1189.
- Wittbrodt E. The impact of postoperative ileus and emerging therapies. Pharm Treatment. 2006 Jan;31(1):39-59.
An 86-year-old female with Alzheimer’s dementia, hypertension, type 2 diabetes, and chronic obstructive pulmonary disease was admitted with lethargy, fever, and vomiting. After she was diagnosed with necrotizing cholecystitis, she underwent an emergent cholecystectomy. Three days later the patient was short of breath, confused, and hadn’t urinated since the indwelling catheter was removed.
Sound familiar? If this scenario doesn’t ring a bell now, then it soon will. The 65-and-up age group is the fastest growing section of the United States population. A recent poll found that elderly patients now account for more than 60% of most general surgeons’ practices. Additionally, the use of minimally invasive surgical techniques and advanced perioperative monitoring has permitted elderly patients who were previously considered too debilitated to now become surgical candidates.
Though patients and their families most often worry about events in the operating room, the vast majority of complications occur in the postoperative period. Morbidity and mortality rates double during the first 24 hours after surgery and are tenfold higher over the remainder of the first postoperative week. In a recent study of more than 500 elderly general surgery patients, 21% experienced complications during this period.
The most common postoperative complications in the geriatric population include delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. The goal in managing any elderly patient is to preserve cognitive and physical function. Maintaining this goal in the postoperative setting requires the early implementation of preventive measures, as well as an understanding of when age-appropriate intervention is necessary.
Hospitalists are often the first line of defense for postoperative situations in medically ill patients, and an amplification of issues unique to the geriatric patient follows.
Delirium
Postoperative delirium occurs in 10%-15% of older general surgery patients and in 30%-60% of older patients who undergo orthopedic procedures. The most common presentation of delirium in the elderly postoperative patient is a “quiet confusion” that is more pronounced in the evening—otherwise known as sundowning. An acute change in mental status, manifested as a fluctuating level of consciousness or a cognitive deficit, is also common. Though delirium may result solely from the acute stress of the operation, other medically relevant causes include metabolic abnormalities, abnormal respiratory parameters, infections, and medications, and these causes should be aggressively investigated and treated.
After potential medical etiologies have been addressed, focus the treatment of delirium in the elderly postoperative patient on interventions to restore mental and physical function as well as pharmacotherapy. Measures to restore function, such as early mobilization and ambulation, sleep hygiene, volume repletion, and restoration of vision and hearing with appropriate devices, have been shown to decrease the duration of the delirium episode. Other non-pharmacologic interventions, including placing a patient near the nurses’ station, encouraging social visits with caregivers, and avoiding the use of physical restraints (which can aggravate agitation) may also prove helpful.
Avoid the use of psychoactive medications (e.g., antiarrhythmic agents, tricyclic antidepressants, neuroleptics, gastrointestinal medications, antihistamines, ciprofloxacin, nonsteroidal anti-inflammatory drugs, meperidine, and cimetidine) as much as possible during the acute confusional state.
Pharmacologic treatment of delirium may be warranted in patients experiencing symptoms of psychosis or in those exhibiting signs of physical aggression or severe personal distress. Haloperidol and risperidol are the medications of choice, though the FDA has approved neither drug specifically for this indication. High doses of these medications are associated with extrapyramidal effects, dystonic reactions, and torsade de pointe. Once the delirium begins to resolve, doses should be tapered gradually over several days.
Ileus
Postsurgical ileus can cause profound clinical consequences in elderly patients. This complication is associated with delayed enteral feeding and malnutrition, increased length of hospital stay, and increased risk of pulmonary complications. Patients present with abdominal distension, nausea and vomiting, limited flatus, and a decreased presence of bowel sounds on auscultation. In cases of prolonged postsurgical ileus, consider pseudo-obstruction (Ogilvie’s syndrome) and mechanical obstruction.
Intravenous hydration and nutrition (in prolonged cases), assisted ambulation, and the avoidance of opiates remain the mainstays of treatment. Nasogastric tubes may provide symptomatic relief in patients with nausea and vomiting, but studies don’t support the use of this intervention to enhance resolution of the ileus. Many prokinetic agents have been examined for this use, including neostigmine and cisapride, but the results have been mixed, and the side effect profiles are generally unacceptable for elderly patients. Delay oral feeding until satisfactory bowel function has been restored.
Nutritional Care
An estimated 12%-50% of geriatric patients are found to be malnourished in the acute hospital setting. The adverse effects of malnutrition include delayed wound healing, greater risk of sepsis and wound infections, deterioration of functional status secondary to muscle wasting, and increased mortality.
Early identification of the patient’s feeding limitations is the key to preventing adverse outcomes. If a patient is restricted from oral or enteral feeding, parenteral nutrition should be started within 48 hours. When volitional food intake is permitted, the addition of canned nutritional supplements, fortified meals, and between-meal snacks may improve elderly patients’ energy and protein intake.
Initiate enteral feeding in patients for whom voluntary food intake is decreased. Parenteral nutrition may still be required until enteral feeding is established, however, and prescribed nutrients can be administered enterally. Because glucose tolerance diminishes with normal aging and may be further reduced in a state of acute illness, initiation of insulin therapy may be necessary in patients receiving either enteral or parenteral supplementation. Additionally, supplementation with a zinc-containing daily multivitamin has been shown to enhance immune function and prevent infections.
Respiratory Care
Respiratory function may be diminished in elderly patients due to age-related changes in the upper and lower respiratory tracts. Factors that contribute to an increased rate of pulmonary postoperative complications include diminished protective mechanisms like coughing and swallowing, decreased compliance of the chest wall and lung tissue, inadequate mucociliary transport, and a blunted ventilatory response to hypoxia and hypercapnia. Postoperative respiratory complications, including pneumonia, hypoxemia, hypoventilation, and atelectasis, occur in 2.1%-10.2% of elderly patients. These complications are associated with increased length of stay and a higher risk of long-term mortality.
Respiratory function may be preserved in the postoperative geriatric patient using a variety of measures. Effective pain control is essential in maintaining adequate lung volumes, and regional analgesia is associated with less-severe postoperative decreases in vital capacity and functional residual capacity (FRC). Once postoperative pain has been controlled, encourage the early resumption of physical activity (with appropriate assistance). Positioning patients in a seated position increases FRC and improves gas exchange in those recovering from abdominal procedures. Additionally, incentive spirometers, breathing exercises, and intermittent positive-pressure breathing may reduce the incidence of pulmonary complications after upper-abdominal operations, shortening the length of hospital stay.
Thromboembolic Disease
Fatal pulmonary embolism accounts for a large proportion of postoperative deaths in the elderly population. Between 20%-30% of patients undergoing general surgery without prophylaxis develop deep vein thrombosis, and the incidence is as high as 40% in those undergoing orthopedic surgeries, gynecologic cancer operations, and major neurosurgical procedures.
The Fifth American College of Chest Physicians Consensus Conference on Antithrombotic Therapy recommends the following postoperative interventions for older surgical patients:
- General surgery without clinical risk factors for thrombosis: Give low-dose unfractionated heparin two hours before and every 12 hours after the operation;
- General surgery with any clinical risk factors such as prolonged immobilization or paralysis, obesity, varicose veins, congestive heart failure, or pelvic or leg fractures: Administer low molecular weight heparin (LMWH) or low-dose unfractionated heparin every eight hours. If the patient is also prone to bleeding or infection, intermittent pneumatic compression (IPC) can be used instead;
- General surgery with multiple clinical risk factors or with a history of previous deep vein thrombosis, malignancy, stroke, spinal cord injury, or hip fracture: Use low dose unfractionated heparin or LMWH combined with intermittent pneumatic compression; for very high risk patients, perioperative warfarin is an alternative;
- Total hip replacement: Give postoperative LMWH every 12 hours; initiate low-intensity warfarin therapy—to keep International Normalized Ratio of 2-3—preoperatively or immediately postoperatively;
- Total knee replacement: Administer postoperative LMWH every 12 hours. IPC is the most effective non-pharmacologic regimen and is comparable to LMWH. Low-intensity warfarin can also be used; and
- Hip fracture repair: Start preoperative fixed-dose LMWH or low-intensity warfarin.
Urinary Retention
The incidence of postoperative urinary retention in elderly patients has been reported to be as high as 87%. Factors contributing to the development of this complication include immobility, analgesics and opiates, intravenous hydration, and general anesthesia. Urinary retention can lead to overflow incontinence and urinary tract infection and is associated with a decline in function and nursing home placement. The first indication of urinary retention may be a diminished urinary output after removal of an indwelling catheter, overflow incontinence, or the frequent voiding of small amounts of urine.
Urinary retention is treated with catheterization. This prevents bladder distension, which leads to reduced detrusor contractile function, and helps restore preoperative bladder function.
Recent studies have found that normal voiding resumes earlier with the use of intermittent catheterization (if begun at the onset of urinary retention and repeated every six to eight hours) than with the use of an indwelling catheter. Additionally, the use of indwelling catheters in the elderly after the immediate perioperative period is associated with an increased risk of urosepsis and a more dependent postoperative functional status.
Conclusion
The 65-and-up age group is the fastest growing section of the United States population. The vast majority of complications for this age group occur in the postoperative period. It’s important for hospitalists to remain involved in key areas of postoperative complications in the geriatric population—specifically, delirium, ileus, nutritional deficiencies, respiratory complications—including pulmonary embolism—and urinary retention. TH
Jill Landis is a frequent contributor to The Hospitalist.
References
- Souders JE, Rooke GA. Perioperative care for geriatric patients. Ann Long Term Care. 2005;13(6):17-29.
- Williams SL, Jones PB, Pofahl WE. Preoperative management of the older patient—a surgeon’s perspective: part I. Ann Long Term Care. 2006;14(6):24-30.
- Palmer RM. Management of common clinical disorders in geriatric patients: delirium. ACP Medicine Online. June 7, 2006. Available at: www.medscape.com/viewarticle/534766. Last accessed January 11, 2007.
- Manku K, Bacchetti P, Leung JM. Prognostic significance of postoperative in-hospital complications in elderly patients. I. Long-term survival. Anesth Analg. 2003 Feb;96(2):583-589.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient: introduction. ACS Surgery Online. June 7, 2006. Available at: www.medscape.com/viewarticle/535461?rss. Last accessed January 11, 2006.
- Skelly JM, Guyatt GH, Kalbfleisch R, et al. Management of urinary retention after surgical repair of hip fracture. CMAJ. 1992 Apr 1;146(7):1185-1189.
- Wittbrodt E. The impact of postoperative ileus and emerging therapies. Pharm Treatment. 2006 Jan;31(1):39-59.
Constructive Criticism
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
Fibromuscular Dysplasia
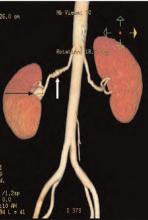
Brief history: 52-year-old female with uncontrolled hypertension.
Salient findings: The middle third of the arteries are involved with a “string of pearls” appearance of alternating webs and stenoses. This appearance is classic for fibromuscular dysplasia (FMD) (white arrow, above). The patient also has a 1.8-cm right renal artery aneurysm at the trifurcation of her first order renal artery branches (black arrow, above).
Patient population and natural history of disease: FMD is most common in young adult females, and its etiology is unknown. An association with alpha-1 antitrypsin deficiency has been reported in the literature. FMD is a leading cause of curable hypertension. Clinical manifestations of FMD include distal embolization of thrombus formed in small aneurysms, hypertension/ischemia due to obstruction by webs, and occlusion/infarct via spontaneous dissection. The natural prevalence of renal artery aneurysms is low—0.1% in all angiography patients—and its natural course is not well established. Renal artery aneurysms are most common in FMD, vasculitides, neoplasm, trauma, and Ehlers-Danlos Syndrome; they may be iatrogenic or idiopathic.
Management: Symptomatic medial fibroplasia-type FMD responds well to balloon angioplasty. Renal artery aneurysms may be managed medically or surgically, depending on risk factors. Indications for repair of renal artery aneurysms include a size of 2 cm or greater, pregnancy, expansion, renovascular hypertension, distal embolization, and rupture. Mortality from ruptured renal artery aneurysms is 10% in nonpregnant patients and 55% during pregnancy.
This patient had a good response to balloon angioplasty of the left renal artery. The right renal artery could not be angioplastied secondary to increased risk of aneurysm rupture with restoration of arterial blood flow due to increased pressure on the walls of the aneurysm. Hence, physicians surgically resected the right renal artery aneurysm and performed a bypass to the aorta.
Take Home Points
- FMD is most common in young or middle-age women;
- FMD is a type of curable hypertension, treated by renal artery angioplasty;
- FMD is diagnosed by an angiographic study—in classic cases, the involved artery has a string of pearls appearance; and
- FMD is associated with renal artery aneurysms. Consider surgical intervention in aneurysms greater than 2 cm. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
- Kaufman JA, Lee MJ. Vascular and Interventional Radiology: The Requisites. Philadelphia: Mosby; 2004.
- Bisschops RH, Popma JJ, Meyerovitz MF. Treatment of fibromuscular dysplasia and renal artery aneurysm with use of a stent-graft. J Vasc Interv Radiol. 2001 Jun;12(6):757-760.
- Luscher TF, Lie JT, Stanson AW, et al. Arterial fibromuscular dysplasia. Mayo Clin Proc. 1987;62:931-952.
Brief history: 52-year-old female with uncontrolled hypertension.
Salient findings: The middle third of the arteries are involved with a “string of pearls” appearance of alternating webs and stenoses. This appearance is classic for fibromuscular dysplasia (FMD) (white arrow, above). The patient also has a 1.8-cm right renal artery aneurysm at the trifurcation of her first order renal artery branches (black arrow, above).
Patient population and natural history of disease: FMD is most common in young adult females, and its etiology is unknown. An association with alpha-1 antitrypsin deficiency has been reported in the literature. FMD is a leading cause of curable hypertension. Clinical manifestations of FMD include distal embolization of thrombus formed in small aneurysms, hypertension/ischemia due to obstruction by webs, and occlusion/infarct via spontaneous dissection. The natural prevalence of renal artery aneurysms is low—0.1% in all angiography patients—and its natural course is not well established. Renal artery aneurysms are most common in FMD, vasculitides, neoplasm, trauma, and Ehlers-Danlos Syndrome; they may be iatrogenic or idiopathic.
Management: Symptomatic medial fibroplasia-type FMD responds well to balloon angioplasty. Renal artery aneurysms may be managed medically or surgically, depending on risk factors. Indications for repair of renal artery aneurysms include a size of 2 cm or greater, pregnancy, expansion, renovascular hypertension, distal embolization, and rupture. Mortality from ruptured renal artery aneurysms is 10% in nonpregnant patients and 55% during pregnancy.
This patient had a good response to balloon angioplasty of the left renal artery. The right renal artery could not be angioplastied secondary to increased risk of aneurysm rupture with restoration of arterial blood flow due to increased pressure on the walls of the aneurysm. Hence, physicians surgically resected the right renal artery aneurysm and performed a bypass to the aorta.
Take Home Points
- FMD is most common in young or middle-age women;
- FMD is a type of curable hypertension, treated by renal artery angioplasty;
- FMD is diagnosed by an angiographic study—in classic cases, the involved artery has a string of pearls appearance; and
- FMD is associated with renal artery aneurysms. Consider surgical intervention in aneurysms greater than 2 cm. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
- Kaufman JA, Lee MJ. Vascular and Interventional Radiology: The Requisites. Philadelphia: Mosby; 2004.
- Bisschops RH, Popma JJ, Meyerovitz MF. Treatment of fibromuscular dysplasia and renal artery aneurysm with use of a stent-graft. J Vasc Interv Radiol. 2001 Jun;12(6):757-760.
- Luscher TF, Lie JT, Stanson AW, et al. Arterial fibromuscular dysplasia. Mayo Clin Proc. 1987;62:931-952.
Brief history: 52-year-old female with uncontrolled hypertension.
Salient findings: The middle third of the arteries are involved with a “string of pearls” appearance of alternating webs and stenoses. This appearance is classic for fibromuscular dysplasia (FMD) (white arrow, above). The patient also has a 1.8-cm right renal artery aneurysm at the trifurcation of her first order renal artery branches (black arrow, above).
Patient population and natural history of disease: FMD is most common in young adult females, and its etiology is unknown. An association with alpha-1 antitrypsin deficiency has been reported in the literature. FMD is a leading cause of curable hypertension. Clinical manifestations of FMD include distal embolization of thrombus formed in small aneurysms, hypertension/ischemia due to obstruction by webs, and occlusion/infarct via spontaneous dissection. The natural prevalence of renal artery aneurysms is low—0.1% in all angiography patients—and its natural course is not well established. Renal artery aneurysms are most common in FMD, vasculitides, neoplasm, trauma, and Ehlers-Danlos Syndrome; they may be iatrogenic or idiopathic.
Management: Symptomatic medial fibroplasia-type FMD responds well to balloon angioplasty. Renal artery aneurysms may be managed medically or surgically, depending on risk factors. Indications for repair of renal artery aneurysms include a size of 2 cm or greater, pregnancy, expansion, renovascular hypertension, distal embolization, and rupture. Mortality from ruptured renal artery aneurysms is 10% in nonpregnant patients and 55% during pregnancy.
This patient had a good response to balloon angioplasty of the left renal artery. The right renal artery could not be angioplastied secondary to increased risk of aneurysm rupture with restoration of arterial blood flow due to increased pressure on the walls of the aneurysm. Hence, physicians surgically resected the right renal artery aneurysm and performed a bypass to the aorta.
Take Home Points
- FMD is most common in young or middle-age women;
- FMD is a type of curable hypertension, treated by renal artery angioplasty;
- FMD is diagnosed by an angiographic study—in classic cases, the involved artery has a string of pearls appearance; and
- FMD is associated with renal artery aneurysms. Consider surgical intervention in aneurysms greater than 2 cm. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
- Kaufman JA, Lee MJ. Vascular and Interventional Radiology: The Requisites. Philadelphia: Mosby; 2004.
- Bisschops RH, Popma JJ, Meyerovitz MF. Treatment of fibromuscular dysplasia and renal artery aneurysm with use of a stent-graft. J Vasc Interv Radiol. 2001 Jun;12(6):757-760.
- Luscher TF, Lie JT, Stanson AW, et al. Arterial fibromuscular dysplasia. Mayo Clin Proc. 1987;62:931-952.
New Party in Power
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Hospital Medicine 2007
This year marks the 10-year anniversary of Robert Wachter’s coining of the term “hospitalist,” as well as the celebration of the decade-old SHM. The celebration culminates in a stellar annual meeting that epitomizes the growth of hospital medicine.
The SHM Annual Meeting attendance has grown from just a handful of participants to more than 1,200 expected at the 2007 Annual Meeting. More importantly, as the role of hospitalists has changed from primarily focusing on providing care to the hospitalized patient to serving as the leader of quality improvement, a key staff educator, and a facilitator of care transitions, so have their educational needs. Thus, the annual meeting has evolved in order to provide an educational experience that has relevance on a practical level.
The SHM 2007 Annual Meeting Committee (AMC), led by Course Director Chad Whelan, MD, challenged itself to develop a program that will meet the needs of a diverse audience that includes community-based and academic-based hospitalists; research-oriented and clinician-focused seasoned veteran physicians and early career hospitalists; as well as pediatric, geriatric, and family practice hospitalists. Such an effort begins with the big picture: What is happening in the environment that will impact healthcare today and in the future?
The answer is found in the role of information technology, and SHM will welcome two renowned speakers to provide current and future perspectives. David Brailer, MD, PhD, the first National Coordinator for Health Information Technology (2004-2006), will examine the forces driving health information technology and how technology affects pressures on the quality and cost of care. Jonathan Perlin, MD, PhD, chief medical officer and senior vice president for Quality for Hospital Corporation of America, will look to healthcare’s challenges and opportunities in the decade ahead, with a focus on health IT and performance and the role of hospital medicine as it relates to care improvement.
The 2007 Annual Meeting will again feature Robert Wachter, MD, as the keynote speaker in the closing plenary session. Dr. Wachter is sure to entertain as he examines “The Hospitalist Movement a Decade Later: Life as a Swiss Army Knife.”
The goal of a broad-based program will be achieved through separate breakout sessions and workshops, divided into seven tracks. Though the format is similar to other years, the 2007 program has some new twists. One clinical track focuses on “Things You Didn’t Learn in Medical School,” and a palliative care track has been added. Relevant sessions have been selected using the Core Competencies in Hospital Medicine and collaborating with SHM’s committees, which serve the interests of all of the groups.
The connection between the program and SHM’s committees will be strong. The committees will focus their efforts on topics and goals that are important to our members. The AMC solicits ideas for breakout sessions from the committees; it also profiles the output of a committee that has significance to attendees in their daily responsibilities.
Suggestions from the committees have resulted in a combination of pertinent and innovative sessions. Here are just a few to whet your appetite for the complete program:
- A workshop jointly planned by the Hospital Quality and Patient Safety (HQPS) and Education Committees, designed to obtain input and consensus on SHM-developed communication and hand-off standards;
- An Academic Track, intended to appeal to those hospitalists focused on teaching, quality improvement, research, and growing a hospital medicine program;
- A workshop, proposed by the Career Satisfaction Task Force, that addresses relevant career issues from the leaders’ and hospitalists’ perspectives;
- A Quality Track defined by the HQPS Committee that, in addition to the consensus-building workshop, features medication reconciliation and Toyota Methods sessions;
- A Pediatric Track, designed to address the needs of our fastest growing member segment, features a range of clinical and leadership topics, including electronic health records, the prevention of the transmission of infectious agents, and the utilization of dashboards to improve care;
- The work of the Benchmarks Committee will be profiled in a session that will demonstrate how to use key performance metrics to improve hospital medicine and the care of the hospitalized patient;
- The Public Policy Committee has recommended a pay-for-performance (P4P) breakout session, because P4P has been identified as an important issue in hospital medicine;
- A Palliative Care Track, proposed and developed by the Palliative Care Task Force, includes relevant topics such as pain management, the ethical and legal considerations of palliative care, and communications skills; and
- A visiting professor, Stephan Fihn, MD, MPH, will conduct poster rounds, lead a workshop, and participate in “Breakfast with Leaders in Hospital Medicine.”
The Annual Meeting Committee focused on identifying faculty members who can share their experience and expertise in an entertaining and elucidating way. We anticipate that you will enjoy presentations by experts new to the SHM Annual Meeting, as well as return engagements by past faculty.
The SHM Annual Meeting traditionally offers networking opportunities with more than 1,100 hospitalists. Special Interest Forums provide each attendee not only with a unique occasion to meet with hospitalists who share similar interests but also with the venue to express their opinions on a national level. SHM utilizes the input to change and grow the organization and hospital medicine. Planned Special Interest Forums include:
- Research;
- Community-based hospitalists;
- Pediatric hospitalists;
- Medical directors and leadership;
- Family practice hospitalists;
- Geriatric hospitalists;
- Nurse practitioners and physician assistants;
- Women in hospital medicine;
- Early career hospitalists;
- Education;
- Curriculum/fellowship;
- Public policy; and
- History of medicine.
Other networking mainstays of the Annual Meeting, including the Research, Innovations, and Clinical Vignettes Competition; Exhibits; President’s Lunch; and Town Meeting, will again be featured. Satellite symposia are planned, as well as the following pre-courses:
- Inpatient Coding and Documentation: Getting Paid What You Deserve;
- Best Practices in Managing a Hospital Medicine Program;
- Critical Care Medicine for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- High Impact Quality Improvement: How to Ensure a Successful Project.
Additionally, a PICC Line Placement for Pediatric and Adult Hospitalists pre-course is being proposed by the Pediatrics Committee.
As you can see, 2007 Annual Meeting will present variety and choice; there is something for everyone. Don’t miss this premier educational event for hospitalists and the opportunity to be a part of the hospital medicine movement. The SHM 2007 Annual Meeting will be held at the Gaylord Texan Resort and Convention Center outside Dallas on May 24 and 25, with pre-courses held on May 23. Visit the SHM Web site at www.hospitalmedicine.org/hospitalmedicine2007 for complete program details or to register online. You may also register by calling SHM at (800) 843-3360. Come to Texas and help us celebrate 10 years of improving the quality of healthcare!
SHM: BEHIND THE SCENES
Resolutions
By Tina Budnitz, MPH
This is the time of year when many New Year’s resolutions dissolve. In some cases, people set unrealistic goals. Others lack the tools to succeed or live in an environment that makes change too difficult. In 2006 I resolved to start running each morning before work. I have the determination and the physical ability to meet this goal. Disarming the house alarm at 5 a.m., however, awakens my two toddlers. And detaching two toddlers from my legs proves to be quite a challenge. It also turns out that my tolerance for cold weather is low, while my ability to forgive a missed run is high.
Sustaining quality improvement initiatives at the hospital is lot like sustaining New Year’s resolutions. The best of intentions are often thwarted by a lack of time, resources, or energy to change the system, as well as by those within the system who resist change. For example, SHM members tell me that attempting to introduce a new discharge planning process feels a lot like trying to run through the hospital with two toddlers hanging on to your legs. SHM strives to support hospitalists in their resolutions to implement positive change in the hospital.
My role at SHM is to lead the development of programs, tool kits, and support mechanisms that will enable you, our members, to implement and sustain local quality improvement efforts.
SHM currently supports members in their efforts to improve outcomes for patients with heart failure, stroke, or diabetes; we work to prevent venous thromboembolism (VTE) and hospital-acquired blood-stream infections. We also support members in their efforts to improve the discharge process for older adults, thereby reducing readmission rates and adverse drug events while improving communications with receiving physicians.
We support members in their efforts to implement, evaluate, and sustain QI initiatives using a variety of methodologies. We offer symposia, workshops, and a full-day Annual Meeting Pre-Course on quality improvement; we also provide Leadership Academy Level I and Level II and networking opportunities for members and their mentors. We’ve designed Web-based clinical tool kits around specific disease states and special patient populations. We offer Web-based resource rooms to guide members from start to finish through a new local QI initiative. We have funded demonstration projects to pilot new approaches and tools for use in discharge planning, along with innovative research to improve care for heart failure patients. And we’ve only just begun.
Researching the Approach
For each QI area we address, an advisory board is recruited to represent the best available experts, organizations, and multidisciplinary professionals. For example, the Discharge Planning for Older Adults Advisory Board includes representatives from the American Geriatrics Society (AGS), the Institute for Healthcare Improvement (IHI), the Agency for Healthcare Research and Quality (AHRQ), the Society of General Internal Medicine (SGIM), the Case Management Society of America (CMSA), the National Quality Forum (NQF), and the Association for Health-System Pharmacists (AHSP), in addition to nationally renowned leaders in care transitions, geriatrics, nursing, patient literacy, and pharmacy.
Each Advisory Board conducts a needs assessment and a review of the literature to examine interventions and approaches. The board identifies existing “gaps” in clinical tools and guidelines. Finally, the Advisory Board determines specific, measurable targets for a hospitalist-led intervention and suggests the evidence-based approach(es) that should be most effective.
Implementing an Intervention: Where the Rubber Meets the Road
As I pointed out earlier, resolving what should be done and getting it done are two very different things. In most cases, few people debate the need for the intervention—reducing the incidence of inpatient VTEs, for example—or the validity of the proposed intervention. The challenge arises in changing the system of care so that the intervention becomes the new standard of care. Therefore, after the Advisory Board has determined the aims and intervention(s), SHM develops a “workbook,” a step-by-step field guide for hospitalists that walks them through the process of building a project team, establishing project aims and key metrics, obtaining institutional support, planning the intervention, launching the intervention, measuring impact, and sustaining system improvements.
The workbooks are posted in the SHM Resource Rooms along with other key resources, including slide sets, bedside teaching tools, patient education literature, CME modules, reviews of key literature, interactive “Ask the Expert” discussion boards, and improvement reports detailing the strategies, successes, and setbacks of other institutions. SHM currently offers resource rooms for Preventing VTE, Heart Failure, Stroke, Discharge Planning for the Elderly, Glycemic Control, and Antimicrobial Resistance. To access the resource rooms, visit our Web site at www.hospitalmedicine.org.
Training Leaders
SHM offers its members diverse training opportunities designed to accommodate the range of knowledge, expertise, and resources available at local institutions. The resource rooms and workbooks described above are made freely available to everyone. At the 2007 SHM Annual Meeting, we will offer a quality pre-course for hands-on training to lead a QI initiative for discharge planning, VTE prevention, or glycemic control.
For SHM members who desire additional support, SHM is developing “Mentored Implementation” and “On-Site Consulting” programs. The Mentored Implementation Program provides enrolled sites with all of the tools described above and an additional yearlong training program conducted via monthly conference calls with SHM mentors and/or one-day training programs. The On-Site Consulting Program surveys an institution’s resources and infrastructure. The SHM consultant team reviews the assessment with the site. Following this assessment, the consultant team visits the site to meet with hospital administrators, QI teams, and others to further assess the site and to help build internal support for the QI initiative. Following the visit, each site receives a customized report detailing recommendations and strategies to advance specific local QI initiatives.
SHM recently launched a Mentored Implementation and On-Site Consulting Program for VTE (known as the SHM VTE Collaborative). Similar programs are scheduled to launch for discharge planning this spring. In the coming years, we hope to add training programs in several other key patient safety areas.
Additionally, SHM is engaged in a strategic planning process to determine how best to attract the highest caliber medical students into hospital medicine and to mentor, train, and retain the next generation of leaders.
In summary, I hope the range of training opportunities and educational programs, the depth of SHM tool kits, and the scope of patient safety initiatives are meeting your needs to plan, implement, evaluate, and sustain positive change at your institution. If you are interested in learning more about SHM QI programs or have suggestions on how we might improve them to better meet your needs, please e-mail me at TBudnitz@hospitalmedicine.org.
And, in case you were wondering, I’m making progress on my resolution to run. This year my resolution has the support of my department chairs (Jacob, five; Noah, two), with better-defined outcomes (run three times a week for more than 40 minutes each time), and a better tool kit (gloves, ear muffs). In the planning stage, I addressed my biggest barrier (leave the alarm off) and built a support team (my neighbor joins me).
If you see me at the annual meeting, please let me know how your resolutions are working to prevent DVT or to improve the discharge process, glycemic control, or heart failure care. Or better yet, submit those stories to me to share with members in our “Improvement Stories” or resource rooms Web site areas or in print via The Hospitalist or Journal of Hospital Medicine.
Budnitz is senior advisor, quality initiatives, for SHM.
This year marks the 10-year anniversary of Robert Wachter’s coining of the term “hospitalist,” as well as the celebration of the decade-old SHM. The celebration culminates in a stellar annual meeting that epitomizes the growth of hospital medicine.
The SHM Annual Meeting attendance has grown from just a handful of participants to more than 1,200 expected at the 2007 Annual Meeting. More importantly, as the role of hospitalists has changed from primarily focusing on providing care to the hospitalized patient to serving as the leader of quality improvement, a key staff educator, and a facilitator of care transitions, so have their educational needs. Thus, the annual meeting has evolved in order to provide an educational experience that has relevance on a practical level.
The SHM 2007 Annual Meeting Committee (AMC), led by Course Director Chad Whelan, MD, challenged itself to develop a program that will meet the needs of a diverse audience that includes community-based and academic-based hospitalists; research-oriented and clinician-focused seasoned veteran physicians and early career hospitalists; as well as pediatric, geriatric, and family practice hospitalists. Such an effort begins with the big picture: What is happening in the environment that will impact healthcare today and in the future?
The answer is found in the role of information technology, and SHM will welcome two renowned speakers to provide current and future perspectives. David Brailer, MD, PhD, the first National Coordinator for Health Information Technology (2004-2006), will examine the forces driving health information technology and how technology affects pressures on the quality and cost of care. Jonathan Perlin, MD, PhD, chief medical officer and senior vice president for Quality for Hospital Corporation of America, will look to healthcare’s challenges and opportunities in the decade ahead, with a focus on health IT and performance and the role of hospital medicine as it relates to care improvement.
The 2007 Annual Meeting will again feature Robert Wachter, MD, as the keynote speaker in the closing plenary session. Dr. Wachter is sure to entertain as he examines “The Hospitalist Movement a Decade Later: Life as a Swiss Army Knife.”
The goal of a broad-based program will be achieved through separate breakout sessions and workshops, divided into seven tracks. Though the format is similar to other years, the 2007 program has some new twists. One clinical track focuses on “Things You Didn’t Learn in Medical School,” and a palliative care track has been added. Relevant sessions have been selected using the Core Competencies in Hospital Medicine and collaborating with SHM’s committees, which serve the interests of all of the groups.
The connection between the program and SHM’s committees will be strong. The committees will focus their efforts on topics and goals that are important to our members. The AMC solicits ideas for breakout sessions from the committees; it also profiles the output of a committee that has significance to attendees in their daily responsibilities.
Suggestions from the committees have resulted in a combination of pertinent and innovative sessions. Here are just a few to whet your appetite for the complete program:
- A workshop jointly planned by the Hospital Quality and Patient Safety (HQPS) and Education Committees, designed to obtain input and consensus on SHM-developed communication and hand-off standards;
- An Academic Track, intended to appeal to those hospitalists focused on teaching, quality improvement, research, and growing a hospital medicine program;
- A workshop, proposed by the Career Satisfaction Task Force, that addresses relevant career issues from the leaders’ and hospitalists’ perspectives;
- A Quality Track defined by the HQPS Committee that, in addition to the consensus-building workshop, features medication reconciliation and Toyota Methods sessions;
- A Pediatric Track, designed to address the needs of our fastest growing member segment, features a range of clinical and leadership topics, including electronic health records, the prevention of the transmission of infectious agents, and the utilization of dashboards to improve care;
- The work of the Benchmarks Committee will be profiled in a session that will demonstrate how to use key performance metrics to improve hospital medicine and the care of the hospitalized patient;
- The Public Policy Committee has recommended a pay-for-performance (P4P) breakout session, because P4P has been identified as an important issue in hospital medicine;
- A Palliative Care Track, proposed and developed by the Palliative Care Task Force, includes relevant topics such as pain management, the ethical and legal considerations of palliative care, and communications skills; and
- A visiting professor, Stephan Fihn, MD, MPH, will conduct poster rounds, lead a workshop, and participate in “Breakfast with Leaders in Hospital Medicine.”
The Annual Meeting Committee focused on identifying faculty members who can share their experience and expertise in an entertaining and elucidating way. We anticipate that you will enjoy presentations by experts new to the SHM Annual Meeting, as well as return engagements by past faculty.
The SHM Annual Meeting traditionally offers networking opportunities with more than 1,100 hospitalists. Special Interest Forums provide each attendee not only with a unique occasion to meet with hospitalists who share similar interests but also with the venue to express their opinions on a national level. SHM utilizes the input to change and grow the organization and hospital medicine. Planned Special Interest Forums include:
- Research;
- Community-based hospitalists;
- Pediatric hospitalists;
- Medical directors and leadership;
- Family practice hospitalists;
- Geriatric hospitalists;
- Nurse practitioners and physician assistants;
- Women in hospital medicine;
- Early career hospitalists;
- Education;
- Curriculum/fellowship;
- Public policy; and
- History of medicine.
Other networking mainstays of the Annual Meeting, including the Research, Innovations, and Clinical Vignettes Competition; Exhibits; President’s Lunch; and Town Meeting, will again be featured. Satellite symposia are planned, as well as the following pre-courses:
- Inpatient Coding and Documentation: Getting Paid What You Deserve;
- Best Practices in Managing a Hospital Medicine Program;
- Critical Care Medicine for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- High Impact Quality Improvement: How to Ensure a Successful Project.
Additionally, a PICC Line Placement for Pediatric and Adult Hospitalists pre-course is being proposed by the Pediatrics Committee.
As you can see, 2007 Annual Meeting will present variety and choice; there is something for everyone. Don’t miss this premier educational event for hospitalists and the opportunity to be a part of the hospital medicine movement. The SHM 2007 Annual Meeting will be held at the Gaylord Texan Resort and Convention Center outside Dallas on May 24 and 25, with pre-courses held on May 23. Visit the SHM Web site at www.hospitalmedicine.org/hospitalmedicine2007 for complete program details or to register online. You may also register by calling SHM at (800) 843-3360. Come to Texas and help us celebrate 10 years of improving the quality of healthcare!
SHM: BEHIND THE SCENES
Resolutions
By Tina Budnitz, MPH
This is the time of year when many New Year’s resolutions dissolve. In some cases, people set unrealistic goals. Others lack the tools to succeed or live in an environment that makes change too difficult. In 2006 I resolved to start running each morning before work. I have the determination and the physical ability to meet this goal. Disarming the house alarm at 5 a.m., however, awakens my two toddlers. And detaching two toddlers from my legs proves to be quite a challenge. It also turns out that my tolerance for cold weather is low, while my ability to forgive a missed run is high.
Sustaining quality improvement initiatives at the hospital is lot like sustaining New Year’s resolutions. The best of intentions are often thwarted by a lack of time, resources, or energy to change the system, as well as by those within the system who resist change. For example, SHM members tell me that attempting to introduce a new discharge planning process feels a lot like trying to run through the hospital with two toddlers hanging on to your legs. SHM strives to support hospitalists in their resolutions to implement positive change in the hospital.
My role at SHM is to lead the development of programs, tool kits, and support mechanisms that will enable you, our members, to implement and sustain local quality improvement efforts.
SHM currently supports members in their efforts to improve outcomes for patients with heart failure, stroke, or diabetes; we work to prevent venous thromboembolism (VTE) and hospital-acquired blood-stream infections. We also support members in their efforts to improve the discharge process for older adults, thereby reducing readmission rates and adverse drug events while improving communications with receiving physicians.
We support members in their efforts to implement, evaluate, and sustain QI initiatives using a variety of methodologies. We offer symposia, workshops, and a full-day Annual Meeting Pre-Course on quality improvement; we also provide Leadership Academy Level I and Level II and networking opportunities for members and their mentors. We’ve designed Web-based clinical tool kits around specific disease states and special patient populations. We offer Web-based resource rooms to guide members from start to finish through a new local QI initiative. We have funded demonstration projects to pilot new approaches and tools for use in discharge planning, along with innovative research to improve care for heart failure patients. And we’ve only just begun.
Researching the Approach
For each QI area we address, an advisory board is recruited to represent the best available experts, organizations, and multidisciplinary professionals. For example, the Discharge Planning for Older Adults Advisory Board includes representatives from the American Geriatrics Society (AGS), the Institute for Healthcare Improvement (IHI), the Agency for Healthcare Research and Quality (AHRQ), the Society of General Internal Medicine (SGIM), the Case Management Society of America (CMSA), the National Quality Forum (NQF), and the Association for Health-System Pharmacists (AHSP), in addition to nationally renowned leaders in care transitions, geriatrics, nursing, patient literacy, and pharmacy.
Each Advisory Board conducts a needs assessment and a review of the literature to examine interventions and approaches. The board identifies existing “gaps” in clinical tools and guidelines. Finally, the Advisory Board determines specific, measurable targets for a hospitalist-led intervention and suggests the evidence-based approach(es) that should be most effective.
Implementing an Intervention: Where the Rubber Meets the Road
As I pointed out earlier, resolving what should be done and getting it done are two very different things. In most cases, few people debate the need for the intervention—reducing the incidence of inpatient VTEs, for example—or the validity of the proposed intervention. The challenge arises in changing the system of care so that the intervention becomes the new standard of care. Therefore, after the Advisory Board has determined the aims and intervention(s), SHM develops a “workbook,” a step-by-step field guide for hospitalists that walks them through the process of building a project team, establishing project aims and key metrics, obtaining institutional support, planning the intervention, launching the intervention, measuring impact, and sustaining system improvements.
The workbooks are posted in the SHM Resource Rooms along with other key resources, including slide sets, bedside teaching tools, patient education literature, CME modules, reviews of key literature, interactive “Ask the Expert” discussion boards, and improvement reports detailing the strategies, successes, and setbacks of other institutions. SHM currently offers resource rooms for Preventing VTE, Heart Failure, Stroke, Discharge Planning for the Elderly, Glycemic Control, and Antimicrobial Resistance. To access the resource rooms, visit our Web site at www.hospitalmedicine.org.
Training Leaders
SHM offers its members diverse training opportunities designed to accommodate the range of knowledge, expertise, and resources available at local institutions. The resource rooms and workbooks described above are made freely available to everyone. At the 2007 SHM Annual Meeting, we will offer a quality pre-course for hands-on training to lead a QI initiative for discharge planning, VTE prevention, or glycemic control.
For SHM members who desire additional support, SHM is developing “Mentored Implementation” and “On-Site Consulting” programs. The Mentored Implementation Program provides enrolled sites with all of the tools described above and an additional yearlong training program conducted via monthly conference calls with SHM mentors and/or one-day training programs. The On-Site Consulting Program surveys an institution’s resources and infrastructure. The SHM consultant team reviews the assessment with the site. Following this assessment, the consultant team visits the site to meet with hospital administrators, QI teams, and others to further assess the site and to help build internal support for the QI initiative. Following the visit, each site receives a customized report detailing recommendations and strategies to advance specific local QI initiatives.
SHM recently launched a Mentored Implementation and On-Site Consulting Program for VTE (known as the SHM VTE Collaborative). Similar programs are scheduled to launch for discharge planning this spring. In the coming years, we hope to add training programs in several other key patient safety areas.
Additionally, SHM is engaged in a strategic planning process to determine how best to attract the highest caliber medical students into hospital medicine and to mentor, train, and retain the next generation of leaders.
In summary, I hope the range of training opportunities and educational programs, the depth of SHM tool kits, and the scope of patient safety initiatives are meeting your needs to plan, implement, evaluate, and sustain positive change at your institution. If you are interested in learning more about SHM QI programs or have suggestions on how we might improve them to better meet your needs, please e-mail me at TBudnitz@hospitalmedicine.org.
And, in case you were wondering, I’m making progress on my resolution to run. This year my resolution has the support of my department chairs (Jacob, five; Noah, two), with better-defined outcomes (run three times a week for more than 40 minutes each time), and a better tool kit (gloves, ear muffs). In the planning stage, I addressed my biggest barrier (leave the alarm off) and built a support team (my neighbor joins me).
If you see me at the annual meeting, please let me know how your resolutions are working to prevent DVT or to improve the discharge process, glycemic control, or heart failure care. Or better yet, submit those stories to me to share with members in our “Improvement Stories” or resource rooms Web site areas or in print via The Hospitalist or Journal of Hospital Medicine.
Budnitz is senior advisor, quality initiatives, for SHM.
This year marks the 10-year anniversary of Robert Wachter’s coining of the term “hospitalist,” as well as the celebration of the decade-old SHM. The celebration culminates in a stellar annual meeting that epitomizes the growth of hospital medicine.
The SHM Annual Meeting attendance has grown from just a handful of participants to more than 1,200 expected at the 2007 Annual Meeting. More importantly, as the role of hospitalists has changed from primarily focusing on providing care to the hospitalized patient to serving as the leader of quality improvement, a key staff educator, and a facilitator of care transitions, so have their educational needs. Thus, the annual meeting has evolved in order to provide an educational experience that has relevance on a practical level.
The SHM 2007 Annual Meeting Committee (AMC), led by Course Director Chad Whelan, MD, challenged itself to develop a program that will meet the needs of a diverse audience that includes community-based and academic-based hospitalists; research-oriented and clinician-focused seasoned veteran physicians and early career hospitalists; as well as pediatric, geriatric, and family practice hospitalists. Such an effort begins with the big picture: What is happening in the environment that will impact healthcare today and in the future?
The answer is found in the role of information technology, and SHM will welcome two renowned speakers to provide current and future perspectives. David Brailer, MD, PhD, the first National Coordinator for Health Information Technology (2004-2006), will examine the forces driving health information technology and how technology affects pressures on the quality and cost of care. Jonathan Perlin, MD, PhD, chief medical officer and senior vice president for Quality for Hospital Corporation of America, will look to healthcare’s challenges and opportunities in the decade ahead, with a focus on health IT and performance and the role of hospital medicine as it relates to care improvement.
The 2007 Annual Meeting will again feature Robert Wachter, MD, as the keynote speaker in the closing plenary session. Dr. Wachter is sure to entertain as he examines “The Hospitalist Movement a Decade Later: Life as a Swiss Army Knife.”
The goal of a broad-based program will be achieved through separate breakout sessions and workshops, divided into seven tracks. Though the format is similar to other years, the 2007 program has some new twists. One clinical track focuses on “Things You Didn’t Learn in Medical School,” and a palliative care track has been added. Relevant sessions have been selected using the Core Competencies in Hospital Medicine and collaborating with SHM’s committees, which serve the interests of all of the groups.
The connection between the program and SHM’s committees will be strong. The committees will focus their efforts on topics and goals that are important to our members. The AMC solicits ideas for breakout sessions from the committees; it also profiles the output of a committee that has significance to attendees in their daily responsibilities.
Suggestions from the committees have resulted in a combination of pertinent and innovative sessions. Here are just a few to whet your appetite for the complete program:
- A workshop jointly planned by the Hospital Quality and Patient Safety (HQPS) and Education Committees, designed to obtain input and consensus on SHM-developed communication and hand-off standards;
- An Academic Track, intended to appeal to those hospitalists focused on teaching, quality improvement, research, and growing a hospital medicine program;
- A workshop, proposed by the Career Satisfaction Task Force, that addresses relevant career issues from the leaders’ and hospitalists’ perspectives;
- A Quality Track defined by the HQPS Committee that, in addition to the consensus-building workshop, features medication reconciliation and Toyota Methods sessions;
- A Pediatric Track, designed to address the needs of our fastest growing member segment, features a range of clinical and leadership topics, including electronic health records, the prevention of the transmission of infectious agents, and the utilization of dashboards to improve care;
- The work of the Benchmarks Committee will be profiled in a session that will demonstrate how to use key performance metrics to improve hospital medicine and the care of the hospitalized patient;
- The Public Policy Committee has recommended a pay-for-performance (P4P) breakout session, because P4P has been identified as an important issue in hospital medicine;
- A Palliative Care Track, proposed and developed by the Palliative Care Task Force, includes relevant topics such as pain management, the ethical and legal considerations of palliative care, and communications skills; and
- A visiting professor, Stephan Fihn, MD, MPH, will conduct poster rounds, lead a workshop, and participate in “Breakfast with Leaders in Hospital Medicine.”
The Annual Meeting Committee focused on identifying faculty members who can share their experience and expertise in an entertaining and elucidating way. We anticipate that you will enjoy presentations by experts new to the SHM Annual Meeting, as well as return engagements by past faculty.
The SHM Annual Meeting traditionally offers networking opportunities with more than 1,100 hospitalists. Special Interest Forums provide each attendee not only with a unique occasion to meet with hospitalists who share similar interests but also with the venue to express their opinions on a national level. SHM utilizes the input to change and grow the organization and hospital medicine. Planned Special Interest Forums include:
- Research;
- Community-based hospitalists;
- Pediatric hospitalists;
- Medical directors and leadership;
- Family practice hospitalists;
- Geriatric hospitalists;
- Nurse practitioners and physician assistants;
- Women in hospital medicine;
- Early career hospitalists;
- Education;
- Curriculum/fellowship;
- Public policy; and
- History of medicine.
Other networking mainstays of the Annual Meeting, including the Research, Innovations, and Clinical Vignettes Competition; Exhibits; President’s Lunch; and Town Meeting, will again be featured. Satellite symposia are planned, as well as the following pre-courses:
- Inpatient Coding and Documentation: Getting Paid What You Deserve;
- Best Practices in Managing a Hospital Medicine Program;
- Critical Care Medicine for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- High Impact Quality Improvement: How to Ensure a Successful Project.
Additionally, a PICC Line Placement for Pediatric and Adult Hospitalists pre-course is being proposed by the Pediatrics Committee.
As you can see, 2007 Annual Meeting will present variety and choice; there is something for everyone. Don’t miss this premier educational event for hospitalists and the opportunity to be a part of the hospital medicine movement. The SHM 2007 Annual Meeting will be held at the Gaylord Texan Resort and Convention Center outside Dallas on May 24 and 25, with pre-courses held on May 23. Visit the SHM Web site at www.hospitalmedicine.org/hospitalmedicine2007 for complete program details or to register online. You may also register by calling SHM at (800) 843-3360. Come to Texas and help us celebrate 10 years of improving the quality of healthcare!
SHM: BEHIND THE SCENES
Resolutions
By Tina Budnitz, MPH
This is the time of year when many New Year’s resolutions dissolve. In some cases, people set unrealistic goals. Others lack the tools to succeed or live in an environment that makes change too difficult. In 2006 I resolved to start running each morning before work. I have the determination and the physical ability to meet this goal. Disarming the house alarm at 5 a.m., however, awakens my two toddlers. And detaching two toddlers from my legs proves to be quite a challenge. It also turns out that my tolerance for cold weather is low, while my ability to forgive a missed run is high.
Sustaining quality improvement initiatives at the hospital is lot like sustaining New Year’s resolutions. The best of intentions are often thwarted by a lack of time, resources, or energy to change the system, as well as by those within the system who resist change. For example, SHM members tell me that attempting to introduce a new discharge planning process feels a lot like trying to run through the hospital with two toddlers hanging on to your legs. SHM strives to support hospitalists in their resolutions to implement positive change in the hospital.
My role at SHM is to lead the development of programs, tool kits, and support mechanisms that will enable you, our members, to implement and sustain local quality improvement efforts.
SHM currently supports members in their efforts to improve outcomes for patients with heart failure, stroke, or diabetes; we work to prevent venous thromboembolism (VTE) and hospital-acquired blood-stream infections. We also support members in their efforts to improve the discharge process for older adults, thereby reducing readmission rates and adverse drug events while improving communications with receiving physicians.
We support members in their efforts to implement, evaluate, and sustain QI initiatives using a variety of methodologies. We offer symposia, workshops, and a full-day Annual Meeting Pre-Course on quality improvement; we also provide Leadership Academy Level I and Level II and networking opportunities for members and their mentors. We’ve designed Web-based clinical tool kits around specific disease states and special patient populations. We offer Web-based resource rooms to guide members from start to finish through a new local QI initiative. We have funded demonstration projects to pilot new approaches and tools for use in discharge planning, along with innovative research to improve care for heart failure patients. And we’ve only just begun.
Researching the Approach
For each QI area we address, an advisory board is recruited to represent the best available experts, organizations, and multidisciplinary professionals. For example, the Discharge Planning for Older Adults Advisory Board includes representatives from the American Geriatrics Society (AGS), the Institute for Healthcare Improvement (IHI), the Agency for Healthcare Research and Quality (AHRQ), the Society of General Internal Medicine (SGIM), the Case Management Society of America (CMSA), the National Quality Forum (NQF), and the Association for Health-System Pharmacists (AHSP), in addition to nationally renowned leaders in care transitions, geriatrics, nursing, patient literacy, and pharmacy.
Each Advisory Board conducts a needs assessment and a review of the literature to examine interventions and approaches. The board identifies existing “gaps” in clinical tools and guidelines. Finally, the Advisory Board determines specific, measurable targets for a hospitalist-led intervention and suggests the evidence-based approach(es) that should be most effective.
Implementing an Intervention: Where the Rubber Meets the Road
As I pointed out earlier, resolving what should be done and getting it done are two very different things. In most cases, few people debate the need for the intervention—reducing the incidence of inpatient VTEs, for example—or the validity of the proposed intervention. The challenge arises in changing the system of care so that the intervention becomes the new standard of care. Therefore, after the Advisory Board has determined the aims and intervention(s), SHM develops a “workbook,” a step-by-step field guide for hospitalists that walks them through the process of building a project team, establishing project aims and key metrics, obtaining institutional support, planning the intervention, launching the intervention, measuring impact, and sustaining system improvements.
The workbooks are posted in the SHM Resource Rooms along with other key resources, including slide sets, bedside teaching tools, patient education literature, CME modules, reviews of key literature, interactive “Ask the Expert” discussion boards, and improvement reports detailing the strategies, successes, and setbacks of other institutions. SHM currently offers resource rooms for Preventing VTE, Heart Failure, Stroke, Discharge Planning for the Elderly, Glycemic Control, and Antimicrobial Resistance. To access the resource rooms, visit our Web site at www.hospitalmedicine.org.
Training Leaders
SHM offers its members diverse training opportunities designed to accommodate the range of knowledge, expertise, and resources available at local institutions. The resource rooms and workbooks described above are made freely available to everyone. At the 2007 SHM Annual Meeting, we will offer a quality pre-course for hands-on training to lead a QI initiative for discharge planning, VTE prevention, or glycemic control.
For SHM members who desire additional support, SHM is developing “Mentored Implementation” and “On-Site Consulting” programs. The Mentored Implementation Program provides enrolled sites with all of the tools described above and an additional yearlong training program conducted via monthly conference calls with SHM mentors and/or one-day training programs. The On-Site Consulting Program surveys an institution’s resources and infrastructure. The SHM consultant team reviews the assessment with the site. Following this assessment, the consultant team visits the site to meet with hospital administrators, QI teams, and others to further assess the site and to help build internal support for the QI initiative. Following the visit, each site receives a customized report detailing recommendations and strategies to advance specific local QI initiatives.
SHM recently launched a Mentored Implementation and On-Site Consulting Program for VTE (known as the SHM VTE Collaborative). Similar programs are scheduled to launch for discharge planning this spring. In the coming years, we hope to add training programs in several other key patient safety areas.
Additionally, SHM is engaged in a strategic planning process to determine how best to attract the highest caliber medical students into hospital medicine and to mentor, train, and retain the next generation of leaders.
In summary, I hope the range of training opportunities and educational programs, the depth of SHM tool kits, and the scope of patient safety initiatives are meeting your needs to plan, implement, evaluate, and sustain positive change at your institution. If you are interested in learning more about SHM QI programs or have suggestions on how we might improve them to better meet your needs, please e-mail me at TBudnitz@hospitalmedicine.org.
And, in case you were wondering, I’m making progress on my resolution to run. This year my resolution has the support of my department chairs (Jacob, five; Noah, two), with better-defined outcomes (run three times a week for more than 40 minutes each time), and a better tool kit (gloves, ear muffs). In the planning stage, I addressed my biggest barrier (leave the alarm off) and built a support team (my neighbor joins me).
If you see me at the annual meeting, please let me know how your resolutions are working to prevent DVT or to improve the discharge process, glycemic control, or heart failure care. Or better yet, submit those stories to me to share with members in our “Improvement Stories” or resource rooms Web site areas or in print via The Hospitalist or Journal of Hospital Medicine.
Budnitz is senior advisor, quality initiatives, for SHM.
Face the Future
We need not be afraid of the future, for the future will be in our own hands.
—Thomas E. Dewey
Your SHM board recently spent some time on the most comprehensive strategic planning that we have undertaken. Our last strategic planning meeting was almost three years ago. It is reassuring to review those minutes and see that we have accomplished a number of things that we set out to do. We have:
- Enhanced our chapters by making more resources and staff assistance available to them;
- Expanded our leadership training offerings;
- Established relationships with other organizations, such as the American Hospital Association, the Joint Commission on Accreditation of Healthcare Organizations, the Society of Critical Care Medicine, and many others; and
- Explored a credential for the hospitalist that distinguishes our work from other practitioners.
Planning to Plan
In these exciting times, however, we decided it was important to stop and take stock to either confirm that we are on the right track or adjust our direction. To prepare for the meeting, we hired an outside facilitator. We invited all board members and our staff from Philadelphia. Our staff has grown from several people to more than 20. They are a diverse group with a tremendous amount of talent. Their perspective and input remain crucial to our success.
We included some of our key committee chairs as well. These individuals have regular contact with other agencies, our members, and their employees. We surveyed our membership and hospitalist leaders to determine their perspective on the dilemmas that they face. We interviewed 13 “futurists” to obtain their opinions about key trends that will affect hospitalists, including:
- The current environment for hospitalists;
- The implications of future trends in patient populations;
- The regulatory and political environment;
- The competitive forces; and
- Advancements in science, technology, and pharmaceuticals.
Bang for the Buck
The SHM board, when surveyed, expressed a strong interest in better understanding SHM’s customer groups, what they value, and what we can offer to them. We conduct many activities and support many projects through our staff, our volunteer leadership, and our members. We need to know if we are spending our resources in a way that optimizes our impact on our members and our field. Each participant spent two to three hours reviewing materials in preparation for the meeting.
When we gathered for two days, our facilitator worked us hard. We began by reviewing what we are doing and checking that against the needs and directions identified by our members and others. We then attempted to prioritize new initiatives so that we could focus on “bang for the buck.”
As we continued the process of refining our findings and designing our action plans, a few things become apparent. Among them:
- There is and will continue to be a shortage of qualified hospitalists;
- The demands of an aging population, in conjunction with the expectations of healthcare givers, will be a source of pressure;
- It will take more time to deliver care to our incoming group of patients than it did for their grandparents;
- The technology and options that are available continue to expand, as does the need to stay abreast of ongoing changes; and
- There will be more medical information to absorb and more to communicate and organize.
As this pressure increases, the facilities’ search for solutions to the impact on cost will increase. In addition, the transparency of hospital results, as well as pay for performance, will drive a desire to improve quality results. The process improvement changes that will be needed cannot be accomplished without a committed medical staff. Hospitalists are uniquely positioned to take on this role. Thus, the demands on hospitalists for participation and leadership will increase.
Labor Shortage a Key Issue
It appears from our membership survey that the labor shortage is a key worry. Because we have no control over demand and we expect demand to increase, we will need to be creative about impacting supply. SHM may be able to address this issue. One approach is to increase supply in the following ways:
1. Design programs that attract individuals who want to be hospitalists into the primary residencies for hospitalists: internal medicine, pediatrics, and family medicine.
An example:
- Influencing training programs and educators to develop positive experiences for residents.
2. Create a model that includes nursing and physician assistants, as well as others, who can extend physicians’ capabilities
Another approach is to improve retention, a goal that might be accomplished by:
- Educating hospitals on their roles in creating a good working environment with excellent support systems for their hospitalists;
- Training group leaders to manage their programs for success;
- Creating alternative delivery models that enhance the physician lifestyle and practice experience; and
- Training individuals to matching their career goals with the right program.
Leadership Gap
Our members and their leaders seem to feel adequately prepared for clinical decision-making to deliver high quality care, but they see a gap when it comes to how they are equipped to provide leadership in a number of areas. These areas include transitions and coordination of care, resource utilization, and collaboration with multidisciplinary teams. SHM can respond to this need with training and mentoring. Perhaps we can also influence training programs and their curriculum.
Caring for the Uninsured
As many of you experience, hospitalists are increasingly called on to provide care for those without funds. When caring for the uninsured, physicians experience special challenges that create job dissatisfaction and affect the sustainability of the practice. In many cases, hospitals are willing to pay for this care because they are required by government regulation to provide it. As they see their profit margins erode, however, they are reluctant to compensate this work. It is important for SHM to be positioned to participate in these discussions as the payment and care of the uninsured gets increasing attention. Our public policy committee will continue to try to identify our best opportunities to impact this issue. How their mission will change is unclear, but this issue continues to be identified by our members as an important one.
This article only touches briefly on the many topics that SHM continues to explore as we try to see the future and take it into our hands. TH
Dr. Gorman is the president of SHM.
We need not be afraid of the future, for the future will be in our own hands.
—Thomas E. Dewey
Your SHM board recently spent some time on the most comprehensive strategic planning that we have undertaken. Our last strategic planning meeting was almost three years ago. It is reassuring to review those minutes and see that we have accomplished a number of things that we set out to do. We have:
- Enhanced our chapters by making more resources and staff assistance available to them;
- Expanded our leadership training offerings;
- Established relationships with other organizations, such as the American Hospital Association, the Joint Commission on Accreditation of Healthcare Organizations, the Society of Critical Care Medicine, and many others; and
- Explored a credential for the hospitalist that distinguishes our work from other practitioners.
Planning to Plan
In these exciting times, however, we decided it was important to stop and take stock to either confirm that we are on the right track or adjust our direction. To prepare for the meeting, we hired an outside facilitator. We invited all board members and our staff from Philadelphia. Our staff has grown from several people to more than 20. They are a diverse group with a tremendous amount of talent. Their perspective and input remain crucial to our success.
We included some of our key committee chairs as well. These individuals have regular contact with other agencies, our members, and their employees. We surveyed our membership and hospitalist leaders to determine their perspective on the dilemmas that they face. We interviewed 13 “futurists” to obtain their opinions about key trends that will affect hospitalists, including:
- The current environment for hospitalists;
- The implications of future trends in patient populations;
- The regulatory and political environment;
- The competitive forces; and
- Advancements in science, technology, and pharmaceuticals.
Bang for the Buck
The SHM board, when surveyed, expressed a strong interest in better understanding SHM’s customer groups, what they value, and what we can offer to them. We conduct many activities and support many projects through our staff, our volunteer leadership, and our members. We need to know if we are spending our resources in a way that optimizes our impact on our members and our field. Each participant spent two to three hours reviewing materials in preparation for the meeting.
When we gathered for two days, our facilitator worked us hard. We began by reviewing what we are doing and checking that against the needs and directions identified by our members and others. We then attempted to prioritize new initiatives so that we could focus on “bang for the buck.”
As we continued the process of refining our findings and designing our action plans, a few things become apparent. Among them:
- There is and will continue to be a shortage of qualified hospitalists;
- The demands of an aging population, in conjunction with the expectations of healthcare givers, will be a source of pressure;
- It will take more time to deliver care to our incoming group of patients than it did for their grandparents;
- The technology and options that are available continue to expand, as does the need to stay abreast of ongoing changes; and
- There will be more medical information to absorb and more to communicate and organize.
As this pressure increases, the facilities’ search for solutions to the impact on cost will increase. In addition, the transparency of hospital results, as well as pay for performance, will drive a desire to improve quality results. The process improvement changes that will be needed cannot be accomplished without a committed medical staff. Hospitalists are uniquely positioned to take on this role. Thus, the demands on hospitalists for participation and leadership will increase.
Labor Shortage a Key Issue
It appears from our membership survey that the labor shortage is a key worry. Because we have no control over demand and we expect demand to increase, we will need to be creative about impacting supply. SHM may be able to address this issue. One approach is to increase supply in the following ways:
1. Design programs that attract individuals who want to be hospitalists into the primary residencies for hospitalists: internal medicine, pediatrics, and family medicine.
An example:
- Influencing training programs and educators to develop positive experiences for residents.
2. Create a model that includes nursing and physician assistants, as well as others, who can extend physicians’ capabilities
Another approach is to improve retention, a goal that might be accomplished by:
- Educating hospitals on their roles in creating a good working environment with excellent support systems for their hospitalists;
- Training group leaders to manage their programs for success;
- Creating alternative delivery models that enhance the physician lifestyle and practice experience; and
- Training individuals to matching their career goals with the right program.
Leadership Gap
Our members and their leaders seem to feel adequately prepared for clinical decision-making to deliver high quality care, but they see a gap when it comes to how they are equipped to provide leadership in a number of areas. These areas include transitions and coordination of care, resource utilization, and collaboration with multidisciplinary teams. SHM can respond to this need with training and mentoring. Perhaps we can also influence training programs and their curriculum.
Caring for the Uninsured
As many of you experience, hospitalists are increasingly called on to provide care for those without funds. When caring for the uninsured, physicians experience special challenges that create job dissatisfaction and affect the sustainability of the practice. In many cases, hospitals are willing to pay for this care because they are required by government regulation to provide it. As they see their profit margins erode, however, they are reluctant to compensate this work. It is important for SHM to be positioned to participate in these discussions as the payment and care of the uninsured gets increasing attention. Our public policy committee will continue to try to identify our best opportunities to impact this issue. How their mission will change is unclear, but this issue continues to be identified by our members as an important one.
This article only touches briefly on the many topics that SHM continues to explore as we try to see the future and take it into our hands. TH
Dr. Gorman is the president of SHM.
We need not be afraid of the future, for the future will be in our own hands.
—Thomas E. Dewey
Your SHM board recently spent some time on the most comprehensive strategic planning that we have undertaken. Our last strategic planning meeting was almost three years ago. It is reassuring to review those minutes and see that we have accomplished a number of things that we set out to do. We have:
- Enhanced our chapters by making more resources and staff assistance available to them;
- Expanded our leadership training offerings;
- Established relationships with other organizations, such as the American Hospital Association, the Joint Commission on Accreditation of Healthcare Organizations, the Society of Critical Care Medicine, and many others; and
- Explored a credential for the hospitalist that distinguishes our work from other practitioners.
Planning to Plan
In these exciting times, however, we decided it was important to stop and take stock to either confirm that we are on the right track or adjust our direction. To prepare for the meeting, we hired an outside facilitator. We invited all board members and our staff from Philadelphia. Our staff has grown from several people to more than 20. They are a diverse group with a tremendous amount of talent. Their perspective and input remain crucial to our success.
We included some of our key committee chairs as well. These individuals have regular contact with other agencies, our members, and their employees. We surveyed our membership and hospitalist leaders to determine their perspective on the dilemmas that they face. We interviewed 13 “futurists” to obtain their opinions about key trends that will affect hospitalists, including:
- The current environment for hospitalists;
- The implications of future trends in patient populations;
- The regulatory and political environment;
- The competitive forces; and
- Advancements in science, technology, and pharmaceuticals.
Bang for the Buck
The SHM board, when surveyed, expressed a strong interest in better understanding SHM’s customer groups, what they value, and what we can offer to them. We conduct many activities and support many projects through our staff, our volunteer leadership, and our members. We need to know if we are spending our resources in a way that optimizes our impact on our members and our field. Each participant spent two to three hours reviewing materials in preparation for the meeting.
When we gathered for two days, our facilitator worked us hard. We began by reviewing what we are doing and checking that against the needs and directions identified by our members and others. We then attempted to prioritize new initiatives so that we could focus on “bang for the buck.”
As we continued the process of refining our findings and designing our action plans, a few things become apparent. Among them:
- There is and will continue to be a shortage of qualified hospitalists;
- The demands of an aging population, in conjunction with the expectations of healthcare givers, will be a source of pressure;
- It will take more time to deliver care to our incoming group of patients than it did for their grandparents;
- The technology and options that are available continue to expand, as does the need to stay abreast of ongoing changes; and
- There will be more medical information to absorb and more to communicate and organize.
As this pressure increases, the facilities’ search for solutions to the impact on cost will increase. In addition, the transparency of hospital results, as well as pay for performance, will drive a desire to improve quality results. The process improvement changes that will be needed cannot be accomplished without a committed medical staff. Hospitalists are uniquely positioned to take on this role. Thus, the demands on hospitalists for participation and leadership will increase.
Labor Shortage a Key Issue
It appears from our membership survey that the labor shortage is a key worry. Because we have no control over demand and we expect demand to increase, we will need to be creative about impacting supply. SHM may be able to address this issue. One approach is to increase supply in the following ways:
1. Design programs that attract individuals who want to be hospitalists into the primary residencies for hospitalists: internal medicine, pediatrics, and family medicine.
An example:
- Influencing training programs and educators to develop positive experiences for residents.
2. Create a model that includes nursing and physician assistants, as well as others, who can extend physicians’ capabilities
Another approach is to improve retention, a goal that might be accomplished by:
- Educating hospitals on their roles in creating a good working environment with excellent support systems for their hospitalists;
- Training group leaders to manage their programs for success;
- Creating alternative delivery models that enhance the physician lifestyle and practice experience; and
- Training individuals to matching their career goals with the right program.
Leadership Gap
Our members and their leaders seem to feel adequately prepared for clinical decision-making to deliver high quality care, but they see a gap when it comes to how they are equipped to provide leadership in a number of areas. These areas include transitions and coordination of care, resource utilization, and collaboration with multidisciplinary teams. SHM can respond to this need with training and mentoring. Perhaps we can also influence training programs and their curriculum.
Caring for the Uninsured
As many of you experience, hospitalists are increasingly called on to provide care for those without funds. When caring for the uninsured, physicians experience special challenges that create job dissatisfaction and affect the sustainability of the practice. In many cases, hospitals are willing to pay for this care because they are required by government regulation to provide it. As they see their profit margins erode, however, they are reluctant to compensate this work. It is important for SHM to be positioned to participate in these discussions as the payment and care of the uninsured gets increasing attention. Our public policy committee will continue to try to identify our best opportunities to impact this issue. How their mission will change is unclear, but this issue continues to be identified by our members as an important one.
This article only touches briefly on the many topics that SHM continues to explore as we try to see the future and take it into our hands. TH
Dr. Gorman is the president of SHM.
TH NewsAlerts
Hospitalists Prone to Evidence-Based Treatments
Researchers from Harvard Medical School (Boston) and other institutions surveyed 213 pediatric hospitalists and a random sample of 352 community pediatricians. They found that, overall, the hospitalist group showed greater adherence to evidence-based therapies and tests for common pediatric illnesses in hospitalized patients, and relied less on those therapies and tests of unproven benefits.
Hourly Rounding Pays Off
According to a study by the Studer Group (Gulf Breeze, Fl.) and the Alliance for Health Care Research, having nurses round every hour results in an average 8.9-point increase in patient satisfaction, a 50% decrease in patient falls, a reduction in the use of call lights, and an undocumented improvement in clinical outcomes.
Google as Diagnostic Tool
The popular Web site Google (Mountain View, Calif.) can help physicians with diagnoses, according to researchers from Princess Alexandria Hospital in Brisbane, Australia. The team “googled” symptoms of 26 mystery cases, and a Web search resulted in a correct diagnosis for 15 of them. The researchers call Google a useful aid for physicians.
SHM Participates in IHI Campaign
When the Institute for Healthcare Improvement (IHI) introduced its “5 Million Lives” campaign recently, SHM was one of the few organizations asked to speak about their part in the campaign.
“We are ready … and could not be more enthusiastic about participating in this landmark campaign,” said Russell Holman, M.D., SHM’s president-elect.
A Winning Team Reaps Rewards
Caritas Good Samaritan Medical Center in Brockton, Mass., and hospital medicine provider Cogent Healthcare (Irvine, Calif.) collaborated to achieve quality of care goals that earned the facility pay-for-performance bonuses from major commercial payers. Cogent used best practices that also helped reduce length of stay and unnecessary re-admissions, and improve patient and physician satisfaction.
A Prevalence of Persistent Pain
The “Health United States 2006” report issued by the National Center for Health Statistics (Hyattsville, Md.) finds a prevalence of pain in the U.S. One in four adults reported a daylong bout of pain in the last month, and one in 10 say they’ve suffered pain for at least a year.
Palliative Medicine Now Official Subspecialty
The American Board of Medical Specialties (ABMS) will establish a subspecialty certificate in Hospice and Palliative Medicine. “[This certification] affirms the concept that specialized knowledge and skills must be learned to care for the increasingly complex-care needs of the dying and their families,” says David Weissman, MD, FACP, editor-in-chief of the Journal of Palliative Medicine.
Busy Shifts Put Elderly Admissions at Risk
Older patients admitted during busy hospital shifts may have a greater mortality rate, according to a study by the University of California San Francisco’s Moffitt-Long Hospital. The retrospective cohort analysis included 5,742 adults admitted to the general medicine service and intensive care unit without cardiovascular, neurologic, or cancer- related primary diagnoses. TH
Hospitalists Prone to Evidence-Based Treatments
Researchers from Harvard Medical School (Boston) and other institutions surveyed 213 pediatric hospitalists and a random sample of 352 community pediatricians. They found that, overall, the hospitalist group showed greater adherence to evidence-based therapies and tests for common pediatric illnesses in hospitalized patients, and relied less on those therapies and tests of unproven benefits.
Hourly Rounding Pays Off
According to a study by the Studer Group (Gulf Breeze, Fl.) and the Alliance for Health Care Research, having nurses round every hour results in an average 8.9-point increase in patient satisfaction, a 50% decrease in patient falls, a reduction in the use of call lights, and an undocumented improvement in clinical outcomes.
Google as Diagnostic Tool
The popular Web site Google (Mountain View, Calif.) can help physicians with diagnoses, according to researchers from Princess Alexandria Hospital in Brisbane, Australia. The team “googled” symptoms of 26 mystery cases, and a Web search resulted in a correct diagnosis for 15 of them. The researchers call Google a useful aid for physicians.
SHM Participates in IHI Campaign
When the Institute for Healthcare Improvement (IHI) introduced its “5 Million Lives” campaign recently, SHM was one of the few organizations asked to speak about their part in the campaign.
“We are ready … and could not be more enthusiastic about participating in this landmark campaign,” said Russell Holman, M.D., SHM’s president-elect.
A Winning Team Reaps Rewards
Caritas Good Samaritan Medical Center in Brockton, Mass., and hospital medicine provider Cogent Healthcare (Irvine, Calif.) collaborated to achieve quality of care goals that earned the facility pay-for-performance bonuses from major commercial payers. Cogent used best practices that also helped reduce length of stay and unnecessary re-admissions, and improve patient and physician satisfaction.
A Prevalence of Persistent Pain
The “Health United States 2006” report issued by the National Center for Health Statistics (Hyattsville, Md.) finds a prevalence of pain in the U.S. One in four adults reported a daylong bout of pain in the last month, and one in 10 say they’ve suffered pain for at least a year.
Palliative Medicine Now Official Subspecialty
The American Board of Medical Specialties (ABMS) will establish a subspecialty certificate in Hospice and Palliative Medicine. “[This certification] affirms the concept that specialized knowledge and skills must be learned to care for the increasingly complex-care needs of the dying and their families,” says David Weissman, MD, FACP, editor-in-chief of the Journal of Palliative Medicine.
Busy Shifts Put Elderly Admissions at Risk
Older patients admitted during busy hospital shifts may have a greater mortality rate, according to a study by the University of California San Francisco’s Moffitt-Long Hospital. The retrospective cohort analysis included 5,742 adults admitted to the general medicine service and intensive care unit without cardiovascular, neurologic, or cancer- related primary diagnoses. TH
Hospitalists Prone to Evidence-Based Treatments
Researchers from Harvard Medical School (Boston) and other institutions surveyed 213 pediatric hospitalists and a random sample of 352 community pediatricians. They found that, overall, the hospitalist group showed greater adherence to evidence-based therapies and tests for common pediatric illnesses in hospitalized patients, and relied less on those therapies and tests of unproven benefits.
Hourly Rounding Pays Off
According to a study by the Studer Group (Gulf Breeze, Fl.) and the Alliance for Health Care Research, having nurses round every hour results in an average 8.9-point increase in patient satisfaction, a 50% decrease in patient falls, a reduction in the use of call lights, and an undocumented improvement in clinical outcomes.
Google as Diagnostic Tool
The popular Web site Google (Mountain View, Calif.) can help physicians with diagnoses, according to researchers from Princess Alexandria Hospital in Brisbane, Australia. The team “googled” symptoms of 26 mystery cases, and a Web search resulted in a correct diagnosis for 15 of them. The researchers call Google a useful aid for physicians.
SHM Participates in IHI Campaign
When the Institute for Healthcare Improvement (IHI) introduced its “5 Million Lives” campaign recently, SHM was one of the few organizations asked to speak about their part in the campaign.
“We are ready … and could not be more enthusiastic about participating in this landmark campaign,” said Russell Holman, M.D., SHM’s president-elect.
A Winning Team Reaps Rewards
Caritas Good Samaritan Medical Center in Brockton, Mass., and hospital medicine provider Cogent Healthcare (Irvine, Calif.) collaborated to achieve quality of care goals that earned the facility pay-for-performance bonuses from major commercial payers. Cogent used best practices that also helped reduce length of stay and unnecessary re-admissions, and improve patient and physician satisfaction.
A Prevalence of Persistent Pain
The “Health United States 2006” report issued by the National Center for Health Statistics (Hyattsville, Md.) finds a prevalence of pain in the U.S. One in four adults reported a daylong bout of pain in the last month, and one in 10 say they’ve suffered pain for at least a year.
Palliative Medicine Now Official Subspecialty
The American Board of Medical Specialties (ABMS) will establish a subspecialty certificate in Hospice and Palliative Medicine. “[This certification] affirms the concept that specialized knowledge and skills must be learned to care for the increasingly complex-care needs of the dying and their families,” says David Weissman, MD, FACP, editor-in-chief of the Journal of Palliative Medicine.
Busy Shifts Put Elderly Admissions at Risk
Older patients admitted during busy hospital shifts may have a greater mortality rate, according to a study by the University of California San Francisco’s Moffitt-Long Hospital. The retrospective cohort analysis included 5,742 adults admitted to the general medicine service and intensive care unit without cardiovascular, neurologic, or cancer- related primary diagnoses. TH
Proceedings of the Heart-Brain Summit
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Introduction
Heart-brain medicine: Where we go from here and why
Marc S. Penn, MD, PhD, Cleveland Clinic, Cleveland, Ohio, and Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Opening remarks
The dream behind the summit
Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Keynote address
'Voodoo' death revisited: The modern lessons of neurocardiology
Martin A. Samuels, MD, DSc (hon), Brigham and Women's Hospital, Boston, Massachusetts
The broken heart syndrome
Ilan S. Wittstein, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland
Brain imaging in cardiovascular disease: State of the art
Michael Phillips, MD, Cleveland Clinic, Cleveland, Ohio
Cortical control of the heart
Stephen Oppenheimer, MD, PhD, Sentient Medical Systems, Cockeysville, Maryland
Neurological mechanisms of chest pain and cardiac disease
Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma
Hypertension in sleep apnea: The role of the sympathetic pathway
Diana L. Kunze, PhD; David Kline, PhD; and Angelina Ramirez-Navarro, PhD, MetroHealth Medical Center and Case Western Reserve University, Cleveland, Ohio
Inflammation: Implications for understanding the heart-brain connection
Mehdi H. Shishehbor, DO; Carlos Alves, MD; and Vivek Rajagopal, MD, Cleveland Clinic, Cleveland, Ohio
The anti-ischemic effects of electrical neurostimulation in the heart
Jessica de Vries, MD, University of Groningen, The Netherlands; Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma; and Mike J.L. DeJongste, MD, PhD, University of Groningen, The Netherlands
The little brain on the heart
J. Andrew Armour, MD, PhD, Hôpital du Sacré-Coeur and Université de Montréal, Montréal, Québec, Canada
Open heart surgery and cognitive decline
Mark F. Newman, MD, Duke University Medical Center, Durham, North Carolina
The heart and the brain within the broader context of wellness
Michael O’Donnell, PhD, MBA, MPH, Cleveland Clinic, Cleveland, Ohio
The heart-brain interaction during emotionally provoked myocardial ischemia: Implications of cortical hyperactivation in CAD and gender interactions
Robert Soufer, MD, Yale University, New Haven, Connecticut, and Matthew M. Burg, PhD, Yale University, New Haven, Connecticut, and Columbia University, New York, New York
Depression and heart disease
François Lespérance, MD, Montréal Heart Institute, and Nancy Frasure-Smith, PhD, McGill University and Montréal Heart Institute, Montréal, Québec, Canada
Sick at heart: The pathophysiology of negative emotions
Laura D. Kubzansky, PhD, MPH, Harvard School of Public Health, Boston, Massachusetts
Role of the brain in ventricular fibrillation and hypertension: From animal models to early human studies
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
New paradigms in heart-brain medicine: Nonlinear physiology, state-dependent proteomics
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
Subarachnoid hemorrhage: A model for heart-brain interactions
J. Javier Provencio, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac denervation in patients with Parkinson disease
David S. Goldstein, MD, PhD, National Institutes of Health, Bethesda, Maryland
Aging and the brain renin-angiotensin system: Insights from studies in transgenic rats
Debra I. Diz, PhD; Sherry O. Kasper, PhD; Atsushi Sakima, MD; and Carlos M. Ferrario, MD, Wake Forest University School of Medicine, Winston-Salem, North Carolina
Contextual cardiology: What modern medicine can learn from ancient Hawaiian wisdom
Paul Pearsall, PhD, University of Hawaii at Manoa and Hawaii State Consortium for Integrative Medicine, Honolulu, Hawaii
Cardiocerebral resuscitation: The optimal approach to cardiac arrest
Gordon A. Ewy, MD, University of Arizona College of Medicine, Tucson, Arizona
Heart transplantation: A magnified model of heart-brain interactions
Mohamad H. Yamani, MD, and Randall C. Starling, MD, MPH, Cleveland Clinic, Cleveland, Ohio
Patent foramen ovale and migraine
Gian Paolo Anzola, MD, S. Orsola Hospital FBF, Brescia, Italy
Patent foramen ovale and stroke: To close or not to close?
Anthony J. Furlan, MD, Cleveland Clinic, Cleveland, Ohio
Sudden unexplained death in epilepsy: The role of the heart
Stephan U. Schuele, MD, Cleveland Clinic, Cleveland, Ohio, and Northwestern University, Chicago, Illinois; Peter Widdess-Walsh, MD, Adriana Bermeo, MD, and Hans O. Lüders, MD, PhD, Cleveland Clinic, Cleveland, Ohio
Hydrocephalus and the heart: Interactions of the first and third circulations
Mark Luciano, MD, PhD, and Stephen Dombrowski, PhD, Cleveland Clinic, Cleveland, Ohio
Cognitive impairment in chronic heart failure
Cathy A. Sila, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac events and brain injury: Ethical implications
Paul J. Ford, PhD, Cleveland Clinic, Cleveland, Ohio
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Introduction
Heart-brain medicine: Where we go from here and why
Marc S. Penn, MD, PhD, Cleveland Clinic, Cleveland, Ohio, and Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Opening remarks
The dream behind the summit
Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Keynote address
'Voodoo' death revisited: The modern lessons of neurocardiology
Martin A. Samuels, MD, DSc (hon), Brigham and Women's Hospital, Boston, Massachusetts
The broken heart syndrome
Ilan S. Wittstein, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland
Brain imaging in cardiovascular disease: State of the art
Michael Phillips, MD, Cleveland Clinic, Cleveland, Ohio
Cortical control of the heart
Stephen Oppenheimer, MD, PhD, Sentient Medical Systems, Cockeysville, Maryland
Neurological mechanisms of chest pain and cardiac disease
Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma
Hypertension in sleep apnea: The role of the sympathetic pathway
Diana L. Kunze, PhD; David Kline, PhD; and Angelina Ramirez-Navarro, PhD, MetroHealth Medical Center and Case Western Reserve University, Cleveland, Ohio
Inflammation: Implications for understanding the heart-brain connection
Mehdi H. Shishehbor, DO; Carlos Alves, MD; and Vivek Rajagopal, MD, Cleveland Clinic, Cleveland, Ohio
The anti-ischemic effects of electrical neurostimulation in the heart
Jessica de Vries, MD, University of Groningen, The Netherlands; Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma; and Mike J.L. DeJongste, MD, PhD, University of Groningen, The Netherlands
The little brain on the heart
J. Andrew Armour, MD, PhD, Hôpital du Sacré-Coeur and Université de Montréal, Montréal, Québec, Canada
Open heart surgery and cognitive decline
Mark F. Newman, MD, Duke University Medical Center, Durham, North Carolina
The heart and the brain within the broader context of wellness
Michael O’Donnell, PhD, MBA, MPH, Cleveland Clinic, Cleveland, Ohio
The heart-brain interaction during emotionally provoked myocardial ischemia: Implications of cortical hyperactivation in CAD and gender interactions
Robert Soufer, MD, Yale University, New Haven, Connecticut, and Matthew M. Burg, PhD, Yale University, New Haven, Connecticut, and Columbia University, New York, New York
Depression and heart disease
François Lespérance, MD, Montréal Heart Institute, and Nancy Frasure-Smith, PhD, McGill University and Montréal Heart Institute, Montréal, Québec, Canada
Sick at heart: The pathophysiology of negative emotions
Laura D. Kubzansky, PhD, MPH, Harvard School of Public Health, Boston, Massachusetts
Role of the brain in ventricular fibrillation and hypertension: From animal models to early human studies
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
New paradigms in heart-brain medicine: Nonlinear physiology, state-dependent proteomics
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
Subarachnoid hemorrhage: A model for heart-brain interactions
J. Javier Provencio, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac denervation in patients with Parkinson disease
David S. Goldstein, MD, PhD, National Institutes of Health, Bethesda, Maryland
Aging and the brain renin-angiotensin system: Insights from studies in transgenic rats
Debra I. Diz, PhD; Sherry O. Kasper, PhD; Atsushi Sakima, MD; and Carlos M. Ferrario, MD, Wake Forest University School of Medicine, Winston-Salem, North Carolina
Contextual cardiology: What modern medicine can learn from ancient Hawaiian wisdom
Paul Pearsall, PhD, University of Hawaii at Manoa and Hawaii State Consortium for Integrative Medicine, Honolulu, Hawaii
Cardiocerebral resuscitation: The optimal approach to cardiac arrest
Gordon A. Ewy, MD, University of Arizona College of Medicine, Tucson, Arizona
Heart transplantation: A magnified model of heart-brain interactions
Mohamad H. Yamani, MD, and Randall C. Starling, MD, MPH, Cleveland Clinic, Cleveland, Ohio
Patent foramen ovale and migraine
Gian Paolo Anzola, MD, S. Orsola Hospital FBF, Brescia, Italy
Patent foramen ovale and stroke: To close or not to close?
Anthony J. Furlan, MD, Cleveland Clinic, Cleveland, Ohio
Sudden unexplained death in epilepsy: The role of the heart
Stephan U. Schuele, MD, Cleveland Clinic, Cleveland, Ohio, and Northwestern University, Chicago, Illinois; Peter Widdess-Walsh, MD, Adriana Bermeo, MD, and Hans O. Lüders, MD, PhD, Cleveland Clinic, Cleveland, Ohio
Hydrocephalus and the heart: Interactions of the first and third circulations
Mark Luciano, MD, PhD, and Stephen Dombrowski, PhD, Cleveland Clinic, Cleveland, Ohio
Cognitive impairment in chronic heart failure
Cathy A. Sila, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac events and brain injury: Ethical implications
Paul J. Ford, PhD, Cleveland Clinic, Cleveland, Ohio
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Introduction
Heart-brain medicine: Where we go from here and why
Marc S. Penn, MD, PhD, Cleveland Clinic, Cleveland, Ohio, and Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Opening remarks
The dream behind the summit
Earl E. Bakken, DSc (hon), Medtronic, Inc., Minneapolis, Minnesota, and North Hawaii Community Hospital, Kamuela, Hawaii
Keynote address
'Voodoo' death revisited: The modern lessons of neurocardiology
Martin A. Samuels, MD, DSc (hon), Brigham and Women's Hospital, Boston, Massachusetts
The broken heart syndrome
Ilan S. Wittstein, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland
Brain imaging in cardiovascular disease: State of the art
Michael Phillips, MD, Cleveland Clinic, Cleveland, Ohio
Cortical control of the heart
Stephen Oppenheimer, MD, PhD, Sentient Medical Systems, Cockeysville, Maryland
Neurological mechanisms of chest pain and cardiac disease
Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma
Hypertension in sleep apnea: The role of the sympathetic pathway
Diana L. Kunze, PhD; David Kline, PhD; and Angelina Ramirez-Navarro, PhD, MetroHealth Medical Center and Case Western Reserve University, Cleveland, Ohio
Inflammation: Implications for understanding the heart-brain connection
Mehdi H. Shishehbor, DO; Carlos Alves, MD; and Vivek Rajagopal, MD, Cleveland Clinic, Cleveland, Ohio
The anti-ischemic effects of electrical neurostimulation in the heart
Jessica de Vries, MD, University of Groningen, The Netherlands; Robert D. Foreman, PhD, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma; and Mike J.L. DeJongste, MD, PhD, University of Groningen, The Netherlands
The little brain on the heart
J. Andrew Armour, MD, PhD, Hôpital du Sacré-Coeur and Université de Montréal, Montréal, Québec, Canada
Open heart surgery and cognitive decline
Mark F. Newman, MD, Duke University Medical Center, Durham, North Carolina
The heart and the brain within the broader context of wellness
Michael O’Donnell, PhD, MBA, MPH, Cleveland Clinic, Cleveland, Ohio
The heart-brain interaction during emotionally provoked myocardial ischemia: Implications of cortical hyperactivation in CAD and gender interactions
Robert Soufer, MD, Yale University, New Haven, Connecticut, and Matthew M. Burg, PhD, Yale University, New Haven, Connecticut, and Columbia University, New York, New York
Depression and heart disease
François Lespérance, MD, Montréal Heart Institute, and Nancy Frasure-Smith, PhD, McGill University and Montréal Heart Institute, Montréal, Québec, Canada
Sick at heart: The pathophysiology of negative emotions
Laura D. Kubzansky, PhD, MPH, Harvard School of Public Health, Boston, Massachusetts
Role of the brain in ventricular fibrillation and hypertension: From animal models to early human studies
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
New paradigms in heart-brain medicine: Nonlinear physiology, state-dependent proteomics
James E. Skinner, PhD, Vicor Technologies, Inc., Boca Raton, Florida
Subarachnoid hemorrhage: A model for heart-brain interactions
J. Javier Provencio, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac denervation in patients with Parkinson disease
David S. Goldstein, MD, PhD, National Institutes of Health, Bethesda, Maryland
Aging and the brain renin-angiotensin system: Insights from studies in transgenic rats
Debra I. Diz, PhD; Sherry O. Kasper, PhD; Atsushi Sakima, MD; and Carlos M. Ferrario, MD, Wake Forest University School of Medicine, Winston-Salem, North Carolina
Contextual cardiology: What modern medicine can learn from ancient Hawaiian wisdom
Paul Pearsall, PhD, University of Hawaii at Manoa and Hawaii State Consortium for Integrative Medicine, Honolulu, Hawaii
Cardiocerebral resuscitation: The optimal approach to cardiac arrest
Gordon A. Ewy, MD, University of Arizona College of Medicine, Tucson, Arizona
Heart transplantation: A magnified model of heart-brain interactions
Mohamad H. Yamani, MD, and Randall C. Starling, MD, MPH, Cleveland Clinic, Cleveland, Ohio
Patent foramen ovale and migraine
Gian Paolo Anzola, MD, S. Orsola Hospital FBF, Brescia, Italy
Patent foramen ovale and stroke: To close or not to close?
Anthony J. Furlan, MD, Cleveland Clinic, Cleveland, Ohio
Sudden unexplained death in epilepsy: The role of the heart
Stephan U. Schuele, MD, Cleveland Clinic, Cleveland, Ohio, and Northwestern University, Chicago, Illinois; Peter Widdess-Walsh, MD, Adriana Bermeo, MD, and Hans O. Lüders, MD, PhD, Cleveland Clinic, Cleveland, Ohio
Hydrocephalus and the heart: Interactions of the first and third circulations
Mark Luciano, MD, PhD, and Stephen Dombrowski, PhD, Cleveland Clinic, Cleveland, Ohio
Cognitive impairment in chronic heart failure
Cathy A. Sila, MD, Cleveland Clinic, Cleveland, Ohio
Cardiac events and brain injury: Ethical implications
Paul J. Ford, PhD, Cleveland Clinic, Cleveland, Ohio
The dream behind the summit
Pediatric Hospitalist Comanagement
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
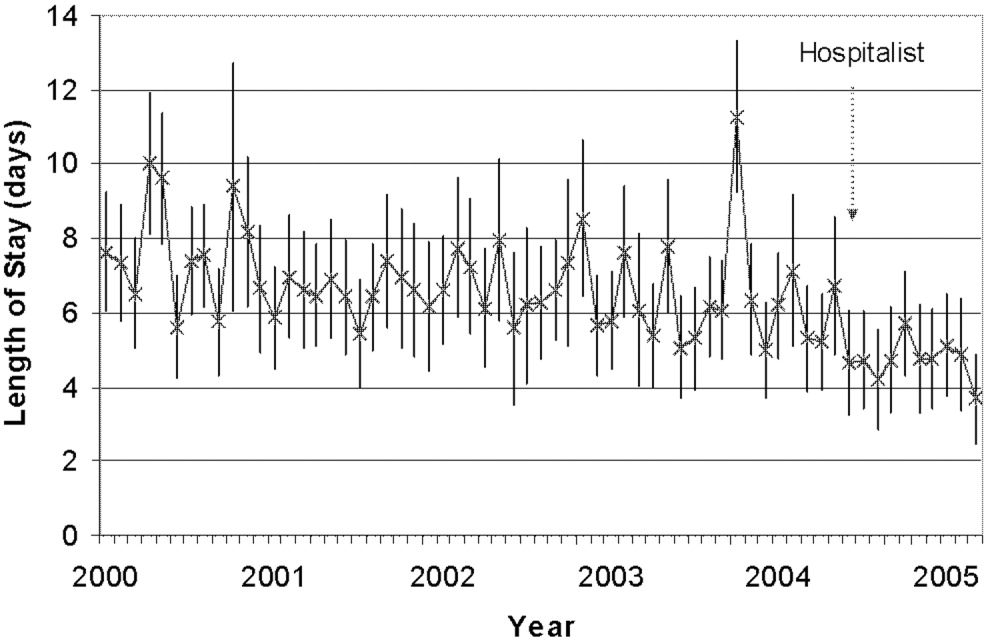
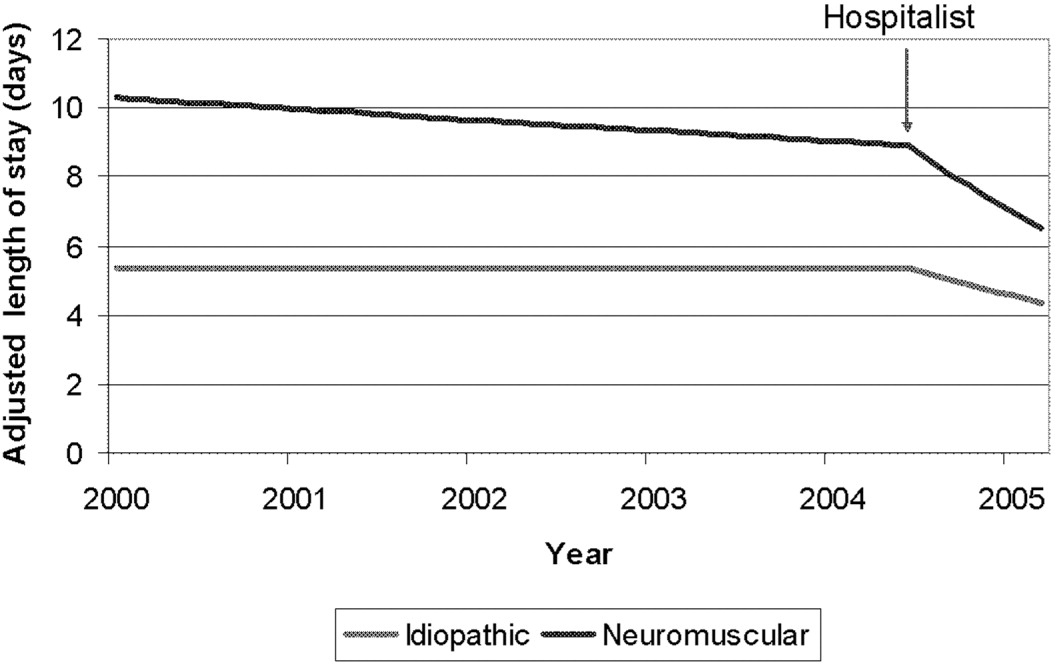
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
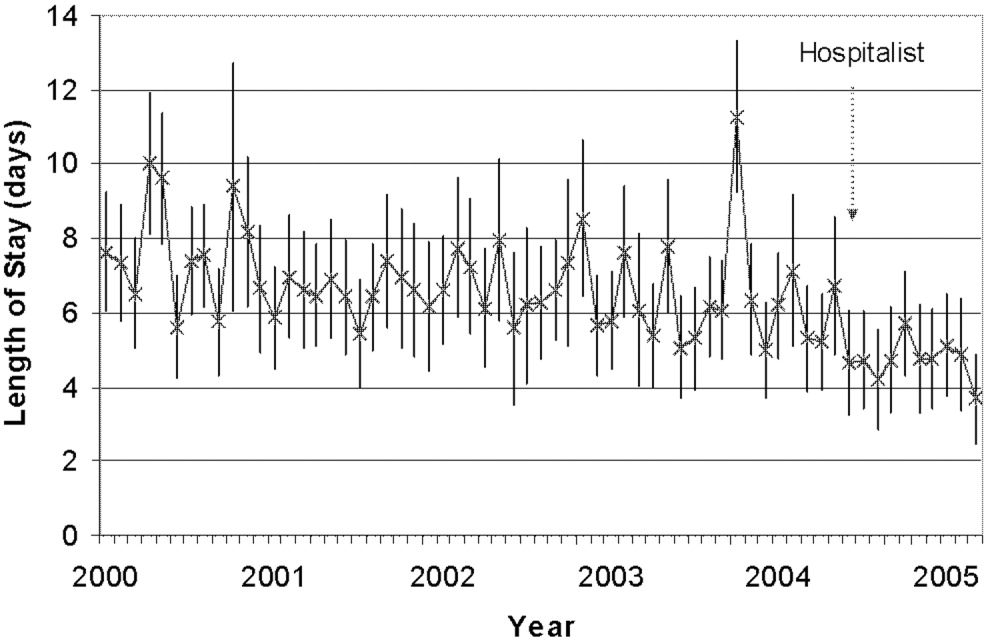
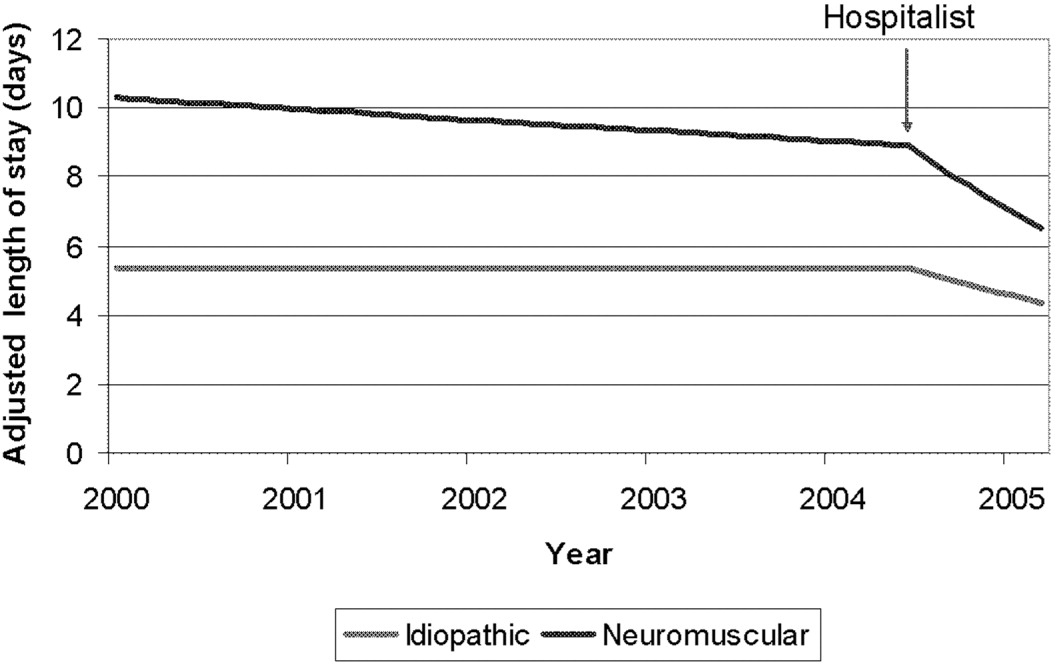
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
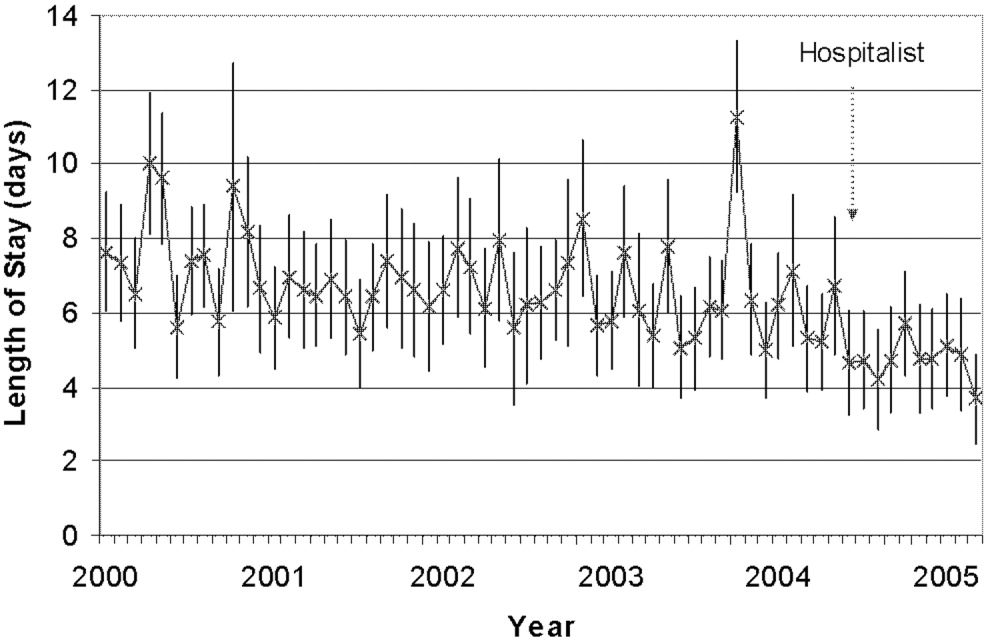
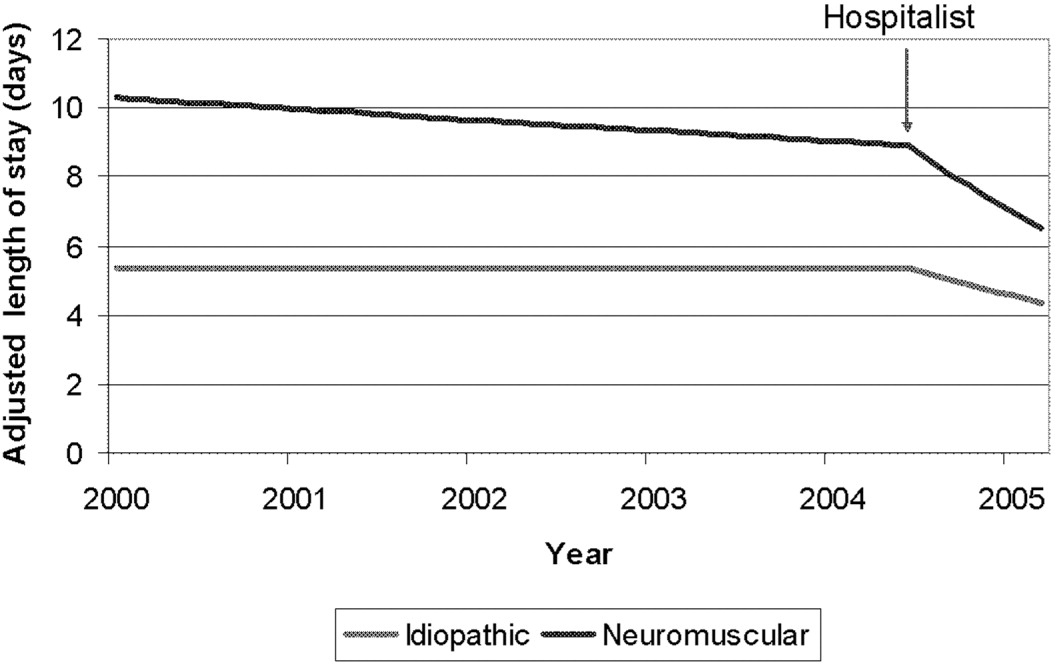
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
Copyright © 2007 Society of Hospital Medicine