User login
Discharge Appointments
Dicharge of a patient from the hospital is a complicated, interprofessional endeavor.1, 2 Several institutions report that discharge is one of the least satisfying elements of the patient's hospital experience.35 Recent evidence suggests that a poorly planned or disorganized discharge may compromise patient safety in the period soon after dismissal.6 Several initiatives have been aimed at improving patient satisfaction and safety related to discharge.710
In 2000 the Mayo Clinic (Rochester, Minnesota) Department of Internal Medicine leadership established a goal to improve patient satisfaction with the hospital dismissal process. Patient focus group data suggested that uncertainty about the anticipated date and time of discharge causes frustration to some patients and families.
We hypothesized that an appointment to leave the hospital might be practicable. We joined an Institute for Healthcare Improvement collaborative (Improving Flow Through Acute Care Settings, 1 of 6 Improvement Action Network [IMPACT] Learning and Innovation Communities) aimed at scheduling discharge appointments (DAs). The collaborating members deemed that, although the ideal DA is set at least a day in advance, a same‐day DA is also desirable for both patient satisfaction and staff task organization in pursuit of a high‐quality discharge.
METHODS
This project was approved by the Mayo Foundation Institutional Review Board. We tested the following hypotheses:
It is possible to make and display DAs in various care units.
Most DAs can be scheduled a day before dismissal.
Most DA patients depart on time.
Setting
Mayo Clinic in Rochester, Minnesota, is a tertiary academic medical center with 2 hospitals (Saint Marys and Rochester Methodist) that house a total of 1951 licensed beds in 76 care units.
The preliminary study displaying DAs was carried out in the Innovation and Quality (IQ) Unit of Saint Marys Hospital, a 23‐bed general medical care unit that supports both resident and nonresident services. Traditionally, primary services usually consist of an attending physician and house officer physicians (junior and senior residents). Less commonly, primary services consist of an attending physician and either a nurse‐practitioner or a physician assistant.
The design pilot took place between August 2 and December 24, 2003. The subsequent, larger study of applicability took place across 8 care units (including the IQ Unit) between December 28, 2003, and April 25, 2004.
Preliminary Work: Design Pilot
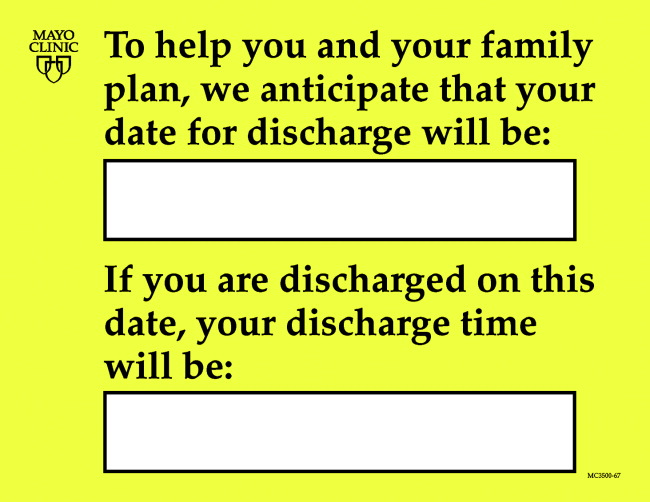
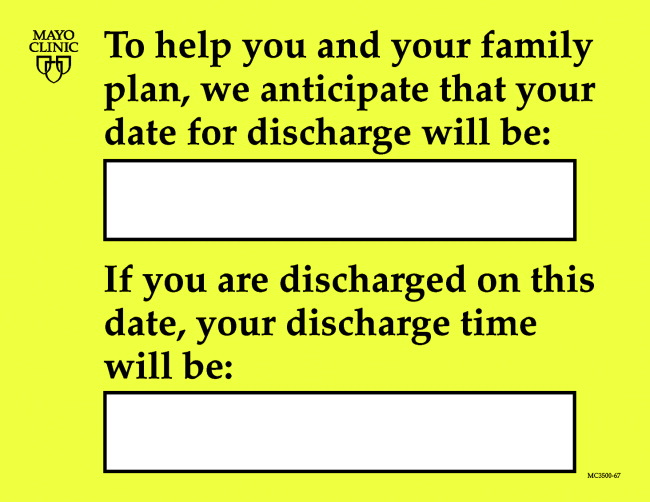
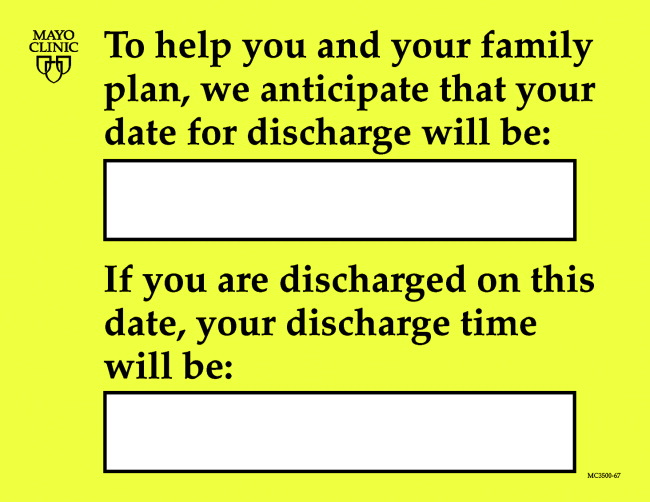
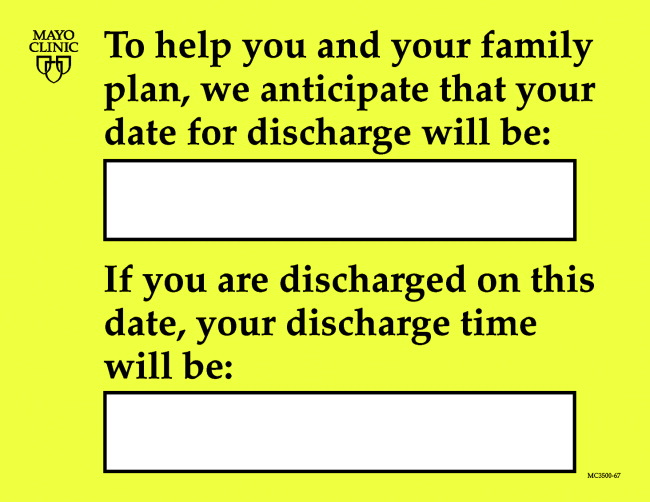
We designed bedside dry‐erase wall displays and mounted them in the rooms in plain view of patients and their families and caregivers. Pilot testing of DA scheduling was done on a general medical care unit from August 2 to December 24, 2003. To optimize the process for scheduling a DA, our team developed 21 small tests to change the dismissal process through plan, do, study, and act cycles.11
The recommended process was that as soon as an organized discharge could be reasonably envisioned, the primary service provider would discuss with the patient, family, and primary nurse (and a social service worker, if involved) the anticipated discharge day. A member of the primary service was to handwrite (with a marker) the anticipated day on the specially designed bedside dry‐erase board (Fig. 1) in view of the patient. The same primary service prescribers could amend this anticipated day (or time) by repeating the process of consultation and discussion as needed. The time of the DA could be written on the DA board (or amended) by either a member of the primary service or the primary care nurse.
Each morning, the primary care nurse transmitted the DA board data to the admission, discharge, and transfer log kept at the unit secretary desk (in which the actual discharge time has always been routinely recorded by the unit secretary).
Adoption of DA Scheduling in Other Care Units
Several meetings were held with 7 other patient care unit leaders about adopting the protocol. These units, both medical and surgical, were selected according to 3 criteria: (1) prior participation in unit‐level continuous improvement work, (2) current or recent work in any aspect of the discharge process, and (3) a reputation for having innovative nursing leadership and staff.
Data Acquisition and Analysis
Data were collected daily from each participating unit's admission, discharge, and transfer log: both the actual time of departure and the DA, if one had been scheduled. For each DA patient, the DA time was compared with the actual departure time.
RESULTS
During the 4‐month study of discharges across 8 care units, 1256 of 2046 patients (61%) received a DA; 576 of the DAs (46%) were scheduled at least 1 day in advance (Table 1). Among patients with a DA, 752 were discharged on time (60%), and only 240 (19%) were tardy.
| Unit | DAs | Departure time of patients compared with DA | |||||
|---|---|---|---|---|---|---|---|
| No. | Type of unit | No. of patients | Patients with DAs, n (%) | DAs scheduled ϵ 1 day ahead, n (%) | On time, n (%)a | Early, n (%) | Late, n (%) |
| |||||||
| 1 | Neurology/neurosurgery | 525 | 270 (51) | 0 (0) | 175 (65) | 44 (16) | 51 (19) |
| 2 | Surgery (mixed) | 481 | 325 (68) | 289 (89) | 166 (51) | 101 (31) | 58 (18) |
| 3 | General internal medicine (IQ Unit) | 466 | 243 (52) | 35 (14) | 132 (54) | 50 (21) | 61 (25) |
| 4 | Neurology/neurosurgery | 267 | 189 (71) | 40 (21) | 119 (63) | 41 (22) | 29 (15) |
| 5 | Vascular surgery | 201 | 127 (63) | 127 (100) | 90 (71) | 12 (9) | 25 (20) |
| 6 | Psychiatry | 46 | 42 (91) | 42 (100) | 28 (67) | 9 (21) | 5 (12) |
| 7 | Orthopedic surgeryelective | 38 | 38 (100) | 22 (58) | 24 (63) | 3 (8) | 11 (29) |
| 8 | Orthopedic surgerytrauma | 22 | 22 (100) | 21 (95) | 18 (82) | 4 (18) | 0 (0) |
| Total | 2046 | 1256 (61) | 576 (46) | 752 (60) | 264 (21) | 240 (19) | |
DISCUSSION
In response to patient focus group feedback, we designed a tool and a process by which a DA could be made and posted at bedside. Among 2046 patients discharged from 8 care units over 4 months, 61% (1256) had a posted, in‐room DA. Almost half the patients with DAs (46%) had a DA scheduled at least 1 calendar day ahead. Remarkably, among patients with a DA, fewer than 20% were discharged tardily. In‐room posting of DAs across a spectrum of care units appears to be practicable, even in the face of extant diagnostic or therapeutic uncertainty.
This was an initial test‐of‐concept project and an exploratory trial. The limitations are: (1) satisfaction (patient, family, nurse, and physician) was not tested with any validated survey instrument, (2) length of stay was not studied, (3) reasons for variable DA success among care units were not ascertained, and (4) resource use was not measured.
Anecdotal information from a postdischarge phone survey indicated that patients seemed appreciative of a DA. The survey data were not included in this article because the survey tool was not a validated instrument and the interviewer (a coauthor) was not blinded to the hypothesis and was therefore subject to bias. No negative comments were received through informal real‐time feedback from patients and family during the making and posting of DAs, and encouraging comments were common.
Physician participation in posting the DA appeared to be key, and the unavoidable dialogue about the clinical rationale for a chosen date seemed welcome. A telling anecdote came from a patient who did not have a DA board: I didn't get the same treatment as my roommate with the [DA] board. The other doctors talked with [him] more about discharge. I wish my team would have done this more with me.
We cannot be certain of the reasons for the care unit disparity in setting and meeting DAs. We speculate that the level of staff enthusiasm for DAs explains the variation rather than patient population characteristics. Further, we cannot explain why 39% of the patients did not receive a DA. Physician feedback was generally, but not uniformly, positive. Negative comments that might explain DA omissions include: (1) patients already are informed and awarethe tool is superfluous; (2) the day of discharge is unknowable in advance; and (3) patients or family members will hold us to it or be upset if the DA is changed.
We expected that diagnostic uncertainty might pose challenges to providing DAs. When primary service providers were reassured that DAs could be amended, this concern was reduced (but not eliminated). It seemed useful for providers to envision the earliest day of discharge by assuming that the results of a pending key test or consultation would be favorable. Frequency of DA modification was not studied. DAs were amended, however, and patients (to our knowledge) seemed unperturbedperhaps because of an almost unavoidable discussion of the clinical rationale because the act of posting the DA occurred in full view of (and in partnership with) the patient.
A trend toward discharge earlier in the day was observed (data not shown). Theoretically, such a trend offers the potential to improve inpatient flow, in part by discharging patients before morning surgical cases are completed.
Although we had many favorable comments about DAs from patients, family members, and nurses, satisfaction of patients, families, and staff members deserves formal study. Further, it is not known whether unused DA boards might contribute to patient dissatisfaction. Any effect that the display of DAs may have on the length of stay also may be a topic worthy of future study.
CONCLUSIONS
Patients and their families sometimes desire more communication about the anticipated day and time of hospital discharge. We designed a process for making a tentative DA and a tool by which the DA could be posted at the bedside. The results of this study suggest that (1) despite some uncertainty it is possible to schedule and post DAs in‐room in various care units and in various settings, (2) DAs were made at least a day ahead of time in almost half the DA discharges, and (3) most DA discharges were characterized by on‐time departure. In addition, patient, family, and nursing satisfaction (in relation to the DA) warrants further investigation.
Acknowledgements
We acknowledge the valuable insights and collaboration of our colleagues Deborah R. Fischer, Steven L. Bahnemann, Matthew Skelton, MD, Lauri J. Dahl, Pamela O. Johnson, MSN, Debra A. Hernke, MSN, Susan L. Stirn, MSN, Barbara R. Spurrier, Ryan R. Armbruster, Todd J. Bille, and Donna K. Lawson of the Mayo Clinic and Mayo Foundation.
- ,,, et al.Learning from patients: a discharge planning improvement project.Jt Comm J Qual Improv.1996;22:311–22.
- ,,,,,, et al.Payer‐hospital collaboration to improve patient satisfaction with hospital discharge.Jt Comm J Qual Improv.1996;22:336–344.
- ,,,,,.How was your hospital stay? Patients' reports about their care in Canadian hospitals.CMAJ.1994;150:1813–1822.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14:76–87.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Patient callback program: a quality improvement, customer service, and marketing tool.J Health Care Mark.1993;13:60–65.
- ,,,.Effects of a medical team coordinator on length of hospital stay.CMAJ.1992;146:511–515.
- ,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2000;4:CD000313.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- Institute for Healthcare Improvement. Cambridge, UK: Institute for Healthcare Improvement. Available from: http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/HowToImprove/testingchanges.htm. Accessed July 28,2006.
Dicharge of a patient from the hospital is a complicated, interprofessional endeavor.1, 2 Several institutions report that discharge is one of the least satisfying elements of the patient's hospital experience.35 Recent evidence suggests that a poorly planned or disorganized discharge may compromise patient safety in the period soon after dismissal.6 Several initiatives have been aimed at improving patient satisfaction and safety related to discharge.710
In 2000 the Mayo Clinic (Rochester, Minnesota) Department of Internal Medicine leadership established a goal to improve patient satisfaction with the hospital dismissal process. Patient focus group data suggested that uncertainty about the anticipated date and time of discharge causes frustration to some patients and families.
We hypothesized that an appointment to leave the hospital might be practicable. We joined an Institute for Healthcare Improvement collaborative (Improving Flow Through Acute Care Settings, 1 of 6 Improvement Action Network [IMPACT] Learning and Innovation Communities) aimed at scheduling discharge appointments (DAs). The collaborating members deemed that, although the ideal DA is set at least a day in advance, a same‐day DA is also desirable for both patient satisfaction and staff task organization in pursuit of a high‐quality discharge.
METHODS
This project was approved by the Mayo Foundation Institutional Review Board. We tested the following hypotheses:
It is possible to make and display DAs in various care units.
Most DAs can be scheduled a day before dismissal.
Most DA patients depart on time.
Setting
Mayo Clinic in Rochester, Minnesota, is a tertiary academic medical center with 2 hospitals (Saint Marys and Rochester Methodist) that house a total of 1951 licensed beds in 76 care units.
The preliminary study displaying DAs was carried out in the Innovation and Quality (IQ) Unit of Saint Marys Hospital, a 23‐bed general medical care unit that supports both resident and nonresident services. Traditionally, primary services usually consist of an attending physician and house officer physicians (junior and senior residents). Less commonly, primary services consist of an attending physician and either a nurse‐practitioner or a physician assistant.
The design pilot took place between August 2 and December 24, 2003. The subsequent, larger study of applicability took place across 8 care units (including the IQ Unit) between December 28, 2003, and April 25, 2004.
Preliminary Work: Design Pilot
We designed bedside dry‐erase wall displays and mounted them in the rooms in plain view of patients and their families and caregivers. Pilot testing of DA scheduling was done on a general medical care unit from August 2 to December 24, 2003. To optimize the process for scheduling a DA, our team developed 21 small tests to change the dismissal process through plan, do, study, and act cycles.11
The recommended process was that as soon as an organized discharge could be reasonably envisioned, the primary service provider would discuss with the patient, family, and primary nurse (and a social service worker, if involved) the anticipated discharge day. A member of the primary service was to handwrite (with a marker) the anticipated day on the specially designed bedside dry‐erase board (Fig. 1) in view of the patient. The same primary service prescribers could amend this anticipated day (or time) by repeating the process of consultation and discussion as needed. The time of the DA could be written on the DA board (or amended) by either a member of the primary service or the primary care nurse.
Each morning, the primary care nurse transmitted the DA board data to the admission, discharge, and transfer log kept at the unit secretary desk (in which the actual discharge time has always been routinely recorded by the unit secretary).
Adoption of DA Scheduling in Other Care Units
Several meetings were held with 7 other patient care unit leaders about adopting the protocol. These units, both medical and surgical, were selected according to 3 criteria: (1) prior participation in unit‐level continuous improvement work, (2) current or recent work in any aspect of the discharge process, and (3) a reputation for having innovative nursing leadership and staff.
Data Acquisition and Analysis
Data were collected daily from each participating unit's admission, discharge, and transfer log: both the actual time of departure and the DA, if one had been scheduled. For each DA patient, the DA time was compared with the actual departure time.
RESULTS
During the 4‐month study of discharges across 8 care units, 1256 of 2046 patients (61%) received a DA; 576 of the DAs (46%) were scheduled at least 1 day in advance (Table 1). Among patients with a DA, 752 were discharged on time (60%), and only 240 (19%) were tardy.
| Unit | DAs | Departure time of patients compared with DA | |||||
|---|---|---|---|---|---|---|---|
| No. | Type of unit | No. of patients | Patients with DAs, n (%) | DAs scheduled ϵ 1 day ahead, n (%) | On time, n (%)a | Early, n (%) | Late, n (%) |
| |||||||
| 1 | Neurology/neurosurgery | 525 | 270 (51) | 0 (0) | 175 (65) | 44 (16) | 51 (19) |
| 2 | Surgery (mixed) | 481 | 325 (68) | 289 (89) | 166 (51) | 101 (31) | 58 (18) |
| 3 | General internal medicine (IQ Unit) | 466 | 243 (52) | 35 (14) | 132 (54) | 50 (21) | 61 (25) |
| 4 | Neurology/neurosurgery | 267 | 189 (71) | 40 (21) | 119 (63) | 41 (22) | 29 (15) |
| 5 | Vascular surgery | 201 | 127 (63) | 127 (100) | 90 (71) | 12 (9) | 25 (20) |
| 6 | Psychiatry | 46 | 42 (91) | 42 (100) | 28 (67) | 9 (21) | 5 (12) |
| 7 | Orthopedic surgeryelective | 38 | 38 (100) | 22 (58) | 24 (63) | 3 (8) | 11 (29) |
| 8 | Orthopedic surgerytrauma | 22 | 22 (100) | 21 (95) | 18 (82) | 4 (18) | 0 (0) |
| Total | 2046 | 1256 (61) | 576 (46) | 752 (60) | 264 (21) | 240 (19) | |
DISCUSSION
In response to patient focus group feedback, we designed a tool and a process by which a DA could be made and posted at bedside. Among 2046 patients discharged from 8 care units over 4 months, 61% (1256) had a posted, in‐room DA. Almost half the patients with DAs (46%) had a DA scheduled at least 1 calendar day ahead. Remarkably, among patients with a DA, fewer than 20% were discharged tardily. In‐room posting of DAs across a spectrum of care units appears to be practicable, even in the face of extant diagnostic or therapeutic uncertainty.
This was an initial test‐of‐concept project and an exploratory trial. The limitations are: (1) satisfaction (patient, family, nurse, and physician) was not tested with any validated survey instrument, (2) length of stay was not studied, (3) reasons for variable DA success among care units were not ascertained, and (4) resource use was not measured.
Anecdotal information from a postdischarge phone survey indicated that patients seemed appreciative of a DA. The survey data were not included in this article because the survey tool was not a validated instrument and the interviewer (a coauthor) was not blinded to the hypothesis and was therefore subject to bias. No negative comments were received through informal real‐time feedback from patients and family during the making and posting of DAs, and encouraging comments were common.
Physician participation in posting the DA appeared to be key, and the unavoidable dialogue about the clinical rationale for a chosen date seemed welcome. A telling anecdote came from a patient who did not have a DA board: I didn't get the same treatment as my roommate with the [DA] board. The other doctors talked with [him] more about discharge. I wish my team would have done this more with me.
We cannot be certain of the reasons for the care unit disparity in setting and meeting DAs. We speculate that the level of staff enthusiasm for DAs explains the variation rather than patient population characteristics. Further, we cannot explain why 39% of the patients did not receive a DA. Physician feedback was generally, but not uniformly, positive. Negative comments that might explain DA omissions include: (1) patients already are informed and awarethe tool is superfluous; (2) the day of discharge is unknowable in advance; and (3) patients or family members will hold us to it or be upset if the DA is changed.
We expected that diagnostic uncertainty might pose challenges to providing DAs. When primary service providers were reassured that DAs could be amended, this concern was reduced (but not eliminated). It seemed useful for providers to envision the earliest day of discharge by assuming that the results of a pending key test or consultation would be favorable. Frequency of DA modification was not studied. DAs were amended, however, and patients (to our knowledge) seemed unperturbedperhaps because of an almost unavoidable discussion of the clinical rationale because the act of posting the DA occurred in full view of (and in partnership with) the patient.
A trend toward discharge earlier in the day was observed (data not shown). Theoretically, such a trend offers the potential to improve inpatient flow, in part by discharging patients before morning surgical cases are completed.
Although we had many favorable comments about DAs from patients, family members, and nurses, satisfaction of patients, families, and staff members deserves formal study. Further, it is not known whether unused DA boards might contribute to patient dissatisfaction. Any effect that the display of DAs may have on the length of stay also may be a topic worthy of future study.
CONCLUSIONS
Patients and their families sometimes desire more communication about the anticipated day and time of hospital discharge. We designed a process for making a tentative DA and a tool by which the DA could be posted at the bedside. The results of this study suggest that (1) despite some uncertainty it is possible to schedule and post DAs in‐room in various care units and in various settings, (2) DAs were made at least a day ahead of time in almost half the DA discharges, and (3) most DA discharges were characterized by on‐time departure. In addition, patient, family, and nursing satisfaction (in relation to the DA) warrants further investigation.
Acknowledgements
We acknowledge the valuable insights and collaboration of our colleagues Deborah R. Fischer, Steven L. Bahnemann, Matthew Skelton, MD, Lauri J. Dahl, Pamela O. Johnson, MSN, Debra A. Hernke, MSN, Susan L. Stirn, MSN, Barbara R. Spurrier, Ryan R. Armbruster, Todd J. Bille, and Donna K. Lawson of the Mayo Clinic and Mayo Foundation.
Dicharge of a patient from the hospital is a complicated, interprofessional endeavor.1, 2 Several institutions report that discharge is one of the least satisfying elements of the patient's hospital experience.35 Recent evidence suggests that a poorly planned or disorganized discharge may compromise patient safety in the period soon after dismissal.6 Several initiatives have been aimed at improving patient satisfaction and safety related to discharge.710
In 2000 the Mayo Clinic (Rochester, Minnesota) Department of Internal Medicine leadership established a goal to improve patient satisfaction with the hospital dismissal process. Patient focus group data suggested that uncertainty about the anticipated date and time of discharge causes frustration to some patients and families.
We hypothesized that an appointment to leave the hospital might be practicable. We joined an Institute for Healthcare Improvement collaborative (Improving Flow Through Acute Care Settings, 1 of 6 Improvement Action Network [IMPACT] Learning and Innovation Communities) aimed at scheduling discharge appointments (DAs). The collaborating members deemed that, although the ideal DA is set at least a day in advance, a same‐day DA is also desirable for both patient satisfaction and staff task organization in pursuit of a high‐quality discharge.
METHODS
This project was approved by the Mayo Foundation Institutional Review Board. We tested the following hypotheses:
It is possible to make and display DAs in various care units.
Most DAs can be scheduled a day before dismissal.
Most DA patients depart on time.
Setting
Mayo Clinic in Rochester, Minnesota, is a tertiary academic medical center with 2 hospitals (Saint Marys and Rochester Methodist) that house a total of 1951 licensed beds in 76 care units.
The preliminary study displaying DAs was carried out in the Innovation and Quality (IQ) Unit of Saint Marys Hospital, a 23‐bed general medical care unit that supports both resident and nonresident services. Traditionally, primary services usually consist of an attending physician and house officer physicians (junior and senior residents). Less commonly, primary services consist of an attending physician and either a nurse‐practitioner or a physician assistant.
The design pilot took place between August 2 and December 24, 2003. The subsequent, larger study of applicability took place across 8 care units (including the IQ Unit) between December 28, 2003, and April 25, 2004.
Preliminary Work: Design Pilot
We designed bedside dry‐erase wall displays and mounted them in the rooms in plain view of patients and their families and caregivers. Pilot testing of DA scheduling was done on a general medical care unit from August 2 to December 24, 2003. To optimize the process for scheduling a DA, our team developed 21 small tests to change the dismissal process through plan, do, study, and act cycles.11
The recommended process was that as soon as an organized discharge could be reasonably envisioned, the primary service provider would discuss with the patient, family, and primary nurse (and a social service worker, if involved) the anticipated discharge day. A member of the primary service was to handwrite (with a marker) the anticipated day on the specially designed bedside dry‐erase board (Fig. 1) in view of the patient. The same primary service prescribers could amend this anticipated day (or time) by repeating the process of consultation and discussion as needed. The time of the DA could be written on the DA board (or amended) by either a member of the primary service or the primary care nurse.
Each morning, the primary care nurse transmitted the DA board data to the admission, discharge, and transfer log kept at the unit secretary desk (in which the actual discharge time has always been routinely recorded by the unit secretary).
Adoption of DA Scheduling in Other Care Units
Several meetings were held with 7 other patient care unit leaders about adopting the protocol. These units, both medical and surgical, were selected according to 3 criteria: (1) prior participation in unit‐level continuous improvement work, (2) current or recent work in any aspect of the discharge process, and (3) a reputation for having innovative nursing leadership and staff.
Data Acquisition and Analysis
Data were collected daily from each participating unit's admission, discharge, and transfer log: both the actual time of departure and the DA, if one had been scheduled. For each DA patient, the DA time was compared with the actual departure time.
RESULTS
During the 4‐month study of discharges across 8 care units, 1256 of 2046 patients (61%) received a DA; 576 of the DAs (46%) were scheduled at least 1 day in advance (Table 1). Among patients with a DA, 752 were discharged on time (60%), and only 240 (19%) were tardy.
| Unit | DAs | Departure time of patients compared with DA | |||||
|---|---|---|---|---|---|---|---|
| No. | Type of unit | No. of patients | Patients with DAs, n (%) | DAs scheduled ϵ 1 day ahead, n (%) | On time, n (%)a | Early, n (%) | Late, n (%) |
| |||||||
| 1 | Neurology/neurosurgery | 525 | 270 (51) | 0 (0) | 175 (65) | 44 (16) | 51 (19) |
| 2 | Surgery (mixed) | 481 | 325 (68) | 289 (89) | 166 (51) | 101 (31) | 58 (18) |
| 3 | General internal medicine (IQ Unit) | 466 | 243 (52) | 35 (14) | 132 (54) | 50 (21) | 61 (25) |
| 4 | Neurology/neurosurgery | 267 | 189 (71) | 40 (21) | 119 (63) | 41 (22) | 29 (15) |
| 5 | Vascular surgery | 201 | 127 (63) | 127 (100) | 90 (71) | 12 (9) | 25 (20) |
| 6 | Psychiatry | 46 | 42 (91) | 42 (100) | 28 (67) | 9 (21) | 5 (12) |
| 7 | Orthopedic surgeryelective | 38 | 38 (100) | 22 (58) | 24 (63) | 3 (8) | 11 (29) |
| 8 | Orthopedic surgerytrauma | 22 | 22 (100) | 21 (95) | 18 (82) | 4 (18) | 0 (0) |
| Total | 2046 | 1256 (61) | 576 (46) | 752 (60) | 264 (21) | 240 (19) | |
DISCUSSION
In response to patient focus group feedback, we designed a tool and a process by which a DA could be made and posted at bedside. Among 2046 patients discharged from 8 care units over 4 months, 61% (1256) had a posted, in‐room DA. Almost half the patients with DAs (46%) had a DA scheduled at least 1 calendar day ahead. Remarkably, among patients with a DA, fewer than 20% were discharged tardily. In‐room posting of DAs across a spectrum of care units appears to be practicable, even in the face of extant diagnostic or therapeutic uncertainty.
This was an initial test‐of‐concept project and an exploratory trial. The limitations are: (1) satisfaction (patient, family, nurse, and physician) was not tested with any validated survey instrument, (2) length of stay was not studied, (3) reasons for variable DA success among care units were not ascertained, and (4) resource use was not measured.
Anecdotal information from a postdischarge phone survey indicated that patients seemed appreciative of a DA. The survey data were not included in this article because the survey tool was not a validated instrument and the interviewer (a coauthor) was not blinded to the hypothesis and was therefore subject to bias. No negative comments were received through informal real‐time feedback from patients and family during the making and posting of DAs, and encouraging comments were common.
Physician participation in posting the DA appeared to be key, and the unavoidable dialogue about the clinical rationale for a chosen date seemed welcome. A telling anecdote came from a patient who did not have a DA board: I didn't get the same treatment as my roommate with the [DA] board. The other doctors talked with [him] more about discharge. I wish my team would have done this more with me.
We cannot be certain of the reasons for the care unit disparity in setting and meeting DAs. We speculate that the level of staff enthusiasm for DAs explains the variation rather than patient population characteristics. Further, we cannot explain why 39% of the patients did not receive a DA. Physician feedback was generally, but not uniformly, positive. Negative comments that might explain DA omissions include: (1) patients already are informed and awarethe tool is superfluous; (2) the day of discharge is unknowable in advance; and (3) patients or family members will hold us to it or be upset if the DA is changed.
We expected that diagnostic uncertainty might pose challenges to providing DAs. When primary service providers were reassured that DAs could be amended, this concern was reduced (but not eliminated). It seemed useful for providers to envision the earliest day of discharge by assuming that the results of a pending key test or consultation would be favorable. Frequency of DA modification was not studied. DAs were amended, however, and patients (to our knowledge) seemed unperturbedperhaps because of an almost unavoidable discussion of the clinical rationale because the act of posting the DA occurred in full view of (and in partnership with) the patient.
A trend toward discharge earlier in the day was observed (data not shown). Theoretically, such a trend offers the potential to improve inpatient flow, in part by discharging patients before morning surgical cases are completed.
Although we had many favorable comments about DAs from patients, family members, and nurses, satisfaction of patients, families, and staff members deserves formal study. Further, it is not known whether unused DA boards might contribute to patient dissatisfaction. Any effect that the display of DAs may have on the length of stay also may be a topic worthy of future study.
CONCLUSIONS
Patients and their families sometimes desire more communication about the anticipated day and time of hospital discharge. We designed a process for making a tentative DA and a tool by which the DA could be posted at the bedside. The results of this study suggest that (1) despite some uncertainty it is possible to schedule and post DAs in‐room in various care units and in various settings, (2) DAs were made at least a day ahead of time in almost half the DA discharges, and (3) most DA discharges were characterized by on‐time departure. In addition, patient, family, and nursing satisfaction (in relation to the DA) warrants further investigation.
Acknowledgements
We acknowledge the valuable insights and collaboration of our colleagues Deborah R. Fischer, Steven L. Bahnemann, Matthew Skelton, MD, Lauri J. Dahl, Pamela O. Johnson, MSN, Debra A. Hernke, MSN, Susan L. Stirn, MSN, Barbara R. Spurrier, Ryan R. Armbruster, Todd J. Bille, and Donna K. Lawson of the Mayo Clinic and Mayo Foundation.
- ,,, et al.Learning from patients: a discharge planning improvement project.Jt Comm J Qual Improv.1996;22:311–22.
- ,,,,,, et al.Payer‐hospital collaboration to improve patient satisfaction with hospital discharge.Jt Comm J Qual Improv.1996;22:336–344.
- ,,,,,.How was your hospital stay? Patients' reports about their care in Canadian hospitals.CMAJ.1994;150:1813–1822.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14:76–87.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Patient callback program: a quality improvement, customer service, and marketing tool.J Health Care Mark.1993;13:60–65.
- ,,,.Effects of a medical team coordinator on length of hospital stay.CMAJ.1992;146:511–515.
- ,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2000;4:CD000313.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- Institute for Healthcare Improvement. Cambridge, UK: Institute for Healthcare Improvement. Available from: http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/HowToImprove/testingchanges.htm. Accessed July 28,2006.
- ,,, et al.Learning from patients: a discharge planning improvement project.Jt Comm J Qual Improv.1996;22:311–22.
- ,,,,,, et al.Payer‐hospital collaboration to improve patient satisfaction with hospital discharge.Jt Comm J Qual Improv.1996;22:336–344.
- ,,,,,.How was your hospital stay? Patients' reports about their care in Canadian hospitals.CMAJ.1994;150:1813–1822.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14:76–87.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Patient callback program: a quality improvement, customer service, and marketing tool.J Health Care Mark.1993;13:60–65.
- ,,,.Effects of a medical team coordinator on length of hospital stay.CMAJ.1992;146:511–515.
- ,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2000;4:CD000313.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- Institute for Healthcare Improvement. Cambridge, UK: Institute for Healthcare Improvement. Available from: http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/HowToImprove/testingchanges.htm. Accessed July 28,2006.
Copyright © 2007 Society of Hospital Medicine
Medical Student Evaluation of Hospitalist and Nonhospitalist Faculty
In 1996 Wachter and Goldman anticipated the emergence of hospitalists,1 physicians who are responsible for the care of hospitalized patients in place of their primary care physicians. The number of physicians who identify themselves as hospitalists has grown rapidly since 1996 and is currently estimated to be 10,00012,000, with the potential to reach as high as 30,000 in the next decade.2 This growth includes academic medical centers. In surveys of chairs of internal medicine and pediatric departments, 50% have hospitalists employed at their institutions.3, 4
Hospitalists in academic institutions are playing an increasingly prominent role in the medical education of both residents and medical students. The implications of adopting a hospitalist model on medical education has been discussed.57 Despite such concerns as fragmented continuity of care; decreased exposure to primary care physicians, subspecialists and physician‐scientists; reduced autonomy; and fewer educational opportunities to observe the natural histories of illnesses because of improved efficiency,57 the overall impact of hospitalists on medical and resident education has generally been favorable.818 Internal medicine residents have rated the teaching skills of hospitalists comparable to traditional academic physicians,8, 9 and believe the addition of hospitalists has contributed to an improved educational experience.10, 11, 14 In addition, a survey of third‐year medical students at a single academic teaching hospital concluded that hospitalists were able to provide at least as positive an educational experience during their inpatient medicine rotations as highly rated nonhospitalist teaching faculty.13
The role of hospitalists as educators in pediatrics has been studied much less. Pediatric resident satisfaction has improved in institutions that have used a hospitalist model.1618 In another study, hospitalists were rated by pediatric residents as more effective teachers than nonhospitalists.15 Because we are unaware of any study that has evaluated hospitalists in the education of medical students during their inpatient pediatric rotation, the purpose of our study was to compare hospitalist and nonhospitalist faculty on the educational experience of third‐year medical students during the inpatient portion of their pediatric clerkships at a single university children's hospital.
METHODS
Study Design
We conducted a retrospective study using evaluations of third‐year medical students comparing hospitalist and nonhospitalist faculty during the inpatient portions of their pediatrics clerkships at a single academic children's hospital over a 15‐month period (July 1999September 2000).
Setting and Sample
We conducted our study at Penn State Children's Hospital (PSCH), a 120‐bed tertiary‐care facility within the 504‐bed Hershey Medical Center, the main teaching hospital affiliated with the Penn State College of Medicine, Hershey, Pennsylvania. The pediatric hospitalist program commenced on July 1, 1999, and during the 15‐month study period the hospitalist staff consisted of 2 physicians who attended a total of 8 months, whereas the nonhospitalist staff consisted of 4 academic general pediatricians and 4 academic pediatric subspecialists who attended the remaining 7 months.
The inpatient clinical responsibilities of both groups of physicians during each month were similar. Both groups of physicians conducted daily rounds with a team that included a senior resident (postgraduate year 3), 2 to 4 interns (postgraduate year 1), 1 acting intern (fourth‐year medical student), and 2 to 4 third‐year medical students. This team was responsible for all admissions to the general pediatrics service, which averages 100 admissions per month. Both the hospitalists and nonhospitalists had outpatient responsibilities during the time they served as inpatient attendings.
During the 15‐month study period, 131 students completed their third‐year pediatrics clerkships. Students at the Penn State College of Medicine may complete their pediatrics clerkship at PSCH or at one of several alternative sites. Because of variability in the structure of the rotation from site to site, it was considered valid only to analyze evaluations completed by students who rotated at PSCH. Sixty‐seven students rotated at PSCH during the study period. Students spent 3 weeks of the 6‐week rotation on the inpatient general pediatrics service. The remaining 3 weeks occurred in multiple outpatient pediatric practice settings and in the newborn nursery. During the 3 weeks the students spent on the inpatient service they did not have outpatient clinic responsibilities, so they did not interact with either the hospitalists or nonhospitalists in the outpatient setting. At the end of the rotation, students were asked to rate the effectiveness of the faculty as teachers, pediatricians, and student advocates and overall on a 4‐point scale (1 = inadequate; 2 = adequate; 3 = very good; 4 = excellent). Students were also asked to evaluate 7 components of the clerkship on the same 4‐point scale (Table 1). Finally, students were asked to provide additional written comments in an unstructured format.
| Evaluation item | Hospitalist mean score (32 evaluations) | Nonhospitalist mean score (35 evaluations) | P value | No. of evaluations rated adequate or inadequate (%)b | |
|---|---|---|---|---|---|
| Hospitalist | Nonhospitalist | ||||
| |||||
| Effectiveness as teacherc | 3.87 | 2.91 | < .001a | 1 (2.9) | 13 (40.6) |
| Effectiveness as pediatriciand | 3.94 | 3.25 | < .001a | 0 (0.0) | 5 (15.6) |
| Effectiveness as student advocatee | 3.76 | 2.97 | < .001a | 2 (5.7) | 13 (40.6) |
| Overall evaluation | 3.93 | 3.06 | < .001a | 0 (0.0) | 10 (31.3) |
| Ward rounds | 3.15 | 2.58 | < .006a | 5 (15.6) | 12 (37.5) |
| Morning report | 3.16 | 3.14 | 0.923 | ||
| Sick newborn | 2.79 | 2.60 | 0.518 | ||
| Well newborn | 2.89 | 3.13 | 0.211 | ||
| Outpatient department clinics | 2.96 | 3.06 | 0.425 | ||
| Private physician's office | 2.97 | 3.01 | 0.794 | ||
| Noon conference | 3.03 | 3.13 | 0.512 | ||
After reviewing the literature concerning faculty evaluation forms and their components, an evaluation form was created for students to indicate their reactions to clerkship components. All the medical students' faculty evaluations were anonymous, and the faculty was not able to review student evaluations prior to assigning grades. Students were required to turn in an evaluation at the end of their rotations. The study was limited to 15 months, as the format of the evaluation form was changed after September 2000 and the general pediatrics service was in the process of transitioning to an exclusively hospitalist‐run service, thereby limiting the number of nonhospitalists available as a comparison group. Demographic characteristics of the hospitalist and nonhospitalist faculty were collected from a faculty database. The study was approved by the Penn State Milton S. Hershey Medical Center's Institutional Review Board.
Statistics and Analysis
For all questions, a Wilcoxon rank sum test was used to evaluate whether the responses for nonhospitalists were different than those for hospitalists. Differences in response by group whose 2‐tailed P values were less than .05 were considered statistically significant. All analyses were performed using the SAS statistical software, version 8.2 (SAS Institute Inc., Cary, NC).
RESULTS
All 67 of the students who completed a pediatrics clerkship at PSCH returned evaluation forms, which were the data for further analysis. Thirty‐five students rotated with the hospitalist faculty, and 32 students rotated with the nonhospitalist faculty. There were no significant demographic differences between the hospitalist and nonhospitalist faculty in age, sex, academic rank, specialty, and years since completing training (Table 2). All the hospitalist faculty fulfilled the definition of a hospitalist,2 whereas none of the physicians in the nonhospitalist group did.
| Characteristic | Hospitalists (n = 2) | Nonhospitalists (n = 8) | P value |
|---|---|---|---|
| Age, mean (range) | 36.0 (3141) | 46.5 (3063) | 0.30 |
| Male/Female | 1/1 | 6/2 | 0.95 |
| Academic rank | |||
| Instructor | 0 | 1 | |
| Assistant professor | 2 | 3 | |
| Associate professor | 0 | 0 | 0.56 |
| Professor | 0 | 4 | |
| Specialty | |||
| General pediatrics | 1 | 4 | |
| Nephrology | 1 | 1 | |
| Genetics | 0 | 1 | 0.95 |
| Infectious ciseases | 0 | 1 | |
| Rheumatology | 0 | 1 | |
| Years since training, mean (range) | 4.0 (08) | 13.8 (030) | 0.43 |
The hospitalists were rated significantly higher than the nonhospitalist faculty in all 4 of the attending characteristics measured (Table 1): teaching effectiveness (3.87 vs. 2.91; P < .0001), effectiveness as a pediatrician (3.94 vs. 3.25; P < .001), student advocacy effectiveness (3.76 vs. 2.97; P < .0001), and overall evaluation (3.93 vs. 3.06; P < .001).
Analysis of specific aspects of the rotation showed the only feature that hospitalists were rated significantly higher on was quality of ward rounds (3.15 vs. 2.58, P < .006). There was no significant difference between the hospitalists and nonhospitalists on features that were not specifically part of the inpatient rotation, including various conferences, outpatient clinics, and newborn care (Table 1).
DISCUSSION
Our study demonstrates that pediatric hospitalists had a positive impact on the overall educational experience of third‐year medical students during the inpatient portions of their pediatrics clerkships. Hospitalists were rated more favorably than nonhospitalists as teachers, as pediatricians, as student advocates, and overall. Medical students also rated the value of ward rounds more favorably when hospitalists conducted them. In addition, higher percentages of nonhospitalists than hospitalists were rated as adequate or inadequate for the above items. When other aspects of the clerkship were analyzed, there were no statistically significant differences between the students who rotated with hospitalists and the students who rotated with nonhospitalists. This suggests that the higher scores for hospitalists were specifically related to their interactions with students, rather than with an overall more positive view of the rotation.
It has been suggested that forces promoting the use of hospitalists in adult medicine are even more persuasive in the pediatric population, as the difference in severity of illness between the inpatient and outpatient setting is greater, and the average pediatrician has less experience than the average internist in managing hospitalized patients.19 In a recent systematic review of the literature, Landrigan et al.20 reported that 6 of 7 studies demonstrated hospitalist systems had decreased hospital length of stay compared to systems in which a primary pediatrician served as the physician of record. This improved efficiency, if combined with the pressure to see more patients while trying to balance teaching and research demands, may have a negative impact on the quality of medical education.
Several factors may have contributed to the students' satisfaction with hospitalists. Studies have demonstrated that students rate clinical teachers more favorably with whom they have greater involvement.21 Hospitalists may be more likely to spend time on the inpatient wards given that is the primary site of their clinical activity. This increased presence may have contributed to more favorable evaluations for the hospitalist faculty, whereas the additional outpatient workload for nonhospitalist faculty may have reduced inpatient teaching opportunities, accounting for their lower teaching score. Included in the pediatrician category was the attribute of being a role model. In a study by Wright et al.,22 spending more than 25% of the time or 25 or more hours per week teaching and conducting rounds was independently associated with being considered an excellent role model. Again, the increased availability of the hospitalists on the inpatient wards may have led to more teaching opportunities, contributing to their higher score.
Our study had several limitations. First, it was a retrospective study conducted at a single institution with only 2 hospitalists. Although there were not statistical significant demographic differences between the 2 groups, this may simply reflect the small size of the sample in our study; therefore, the results may not be applicable to other academic institutions. Second, we retrospectively analyzed an evaluation form that had not been validated or specifically designed to compare 2 physician groups. Third, there were multiple statements in each category that students were asked to consider before scoring each attending on the parameters measured. Although hospitalists were rated higher in each category, there may have been individual characteristics within each category for which the nonhospitalist faculty performed better. Fourth, although hospitalists received higher average ratings than nonhospitalist faculty from third‐year medical students, it is important to emphasize this study measured students' attitudes and beliefs not specific educational outcomes. However, even though we cannot rule out the possibility that potentially confounding factors such as the personality of an attending physician influenced the results, prior studies have demonstrated that medical students make sophisticated judgments about teaching in the clinical setting.23, 24 It is unlikely that hospitalists at our institution were specifically selected to attend more months on a new inpatient service because they had a history of having more favorable teaching qualities because 1 of the 2 hospitalists had just finished residency training, and there were no significant demographic differences between the 2 groups. In a study examining trainee satisfaction in an internal medicine rotation 4 years after adoption of a hospitalist model, where nonhospitalist faculty attended based on their own interest and inpatient skill rather than as a requirement, Hauer et al.14 reported that trainees experienced more effective teaching and a more satisfying inpatient rotation when supervised by hospitalists. This suggests that hospitalists may possess or develop a specific inpatient knowledge base and teaching acumen over time that distinguishes them from nonhospitalists. There is evidence of accumulated experience leading to improved outcomes in the clinical setting for HIV infection,25 various surgical procedures,26 and hospitalist systems.27
In conclusion, this is the first study to evaluate the performance of hospitalists in the setting of a third‐year medical student pediatrics clerkship. Although third‐year medical students rate hospitalists at least as highly as nonhospitalist faculty, further studies are needed to reproduce this finding. In addition to the increased time spent on the wards with students and increased experience in caring for hospitalized patients, further studies should also examine the role that communication plays in clinical teaching. Also, the recent development of core competencies in hospital medicine28 may lead to the development of educational outcomes that can be objectively measured.
Acknowledgements
The authors thank David Mauger, PhD, from the Department of Health Evaluation Sciences at the Penn State College of Medicine for providing statistical analysis of the survey results.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Frequently asked questions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=FAQs75:S34–6.
- ,,,,,.Pediatric hospitalists in Canada and the United States: a survey of pediatric academic department chairs.Ambul Pediatr.2001;1:338–339.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- ,.The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- ,.Implications of the hospitalist model for medical students' education.Acad. Med.2001;76:324–330.
- ,,,,.Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,, et al.Hospitalists as teachers: how do they compare to subspecialty and general medicine faculty.J Gen Intern Med.2004;19:8–15.
- ,,,,.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- ,,,,,.Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112:597–601.
- ,,,,,,.The positive impact of initiation of hospitalist clinician educators: resource utilization and medical resident education.J Gen Intern Med.2004;19:293–301.
- ,,,.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156:877–883.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76:556.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr.2000;39:221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr.2001;40:653–660.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–477.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- ,,.Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1993.
- ,.Evaluation of clinical instructors by third‐year medical students.Acad Med.1989;64:159–164.
- ,,.Clinical tutor evaluation: a 5‐year study by students on an in‐patient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–53.
- ,,,,,.Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival.N Engl J Med.1996;334:701–706.
- ,,,.Hospital Volume, Physician Volume, and Patient Outcomes: Assessing the Evidence. Ann Arbor, MI: Health Administration Perspectives;1990.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,,,, eds.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(S1):1–67.
In 1996 Wachter and Goldman anticipated the emergence of hospitalists,1 physicians who are responsible for the care of hospitalized patients in place of their primary care physicians. The number of physicians who identify themselves as hospitalists has grown rapidly since 1996 and is currently estimated to be 10,00012,000, with the potential to reach as high as 30,000 in the next decade.2 This growth includes academic medical centers. In surveys of chairs of internal medicine and pediatric departments, 50% have hospitalists employed at their institutions.3, 4
Hospitalists in academic institutions are playing an increasingly prominent role in the medical education of both residents and medical students. The implications of adopting a hospitalist model on medical education has been discussed.57 Despite such concerns as fragmented continuity of care; decreased exposure to primary care physicians, subspecialists and physician‐scientists; reduced autonomy; and fewer educational opportunities to observe the natural histories of illnesses because of improved efficiency,57 the overall impact of hospitalists on medical and resident education has generally been favorable.818 Internal medicine residents have rated the teaching skills of hospitalists comparable to traditional academic physicians,8, 9 and believe the addition of hospitalists has contributed to an improved educational experience.10, 11, 14 In addition, a survey of third‐year medical students at a single academic teaching hospital concluded that hospitalists were able to provide at least as positive an educational experience during their inpatient medicine rotations as highly rated nonhospitalist teaching faculty.13
The role of hospitalists as educators in pediatrics has been studied much less. Pediatric resident satisfaction has improved in institutions that have used a hospitalist model.1618 In another study, hospitalists were rated by pediatric residents as more effective teachers than nonhospitalists.15 Because we are unaware of any study that has evaluated hospitalists in the education of medical students during their inpatient pediatric rotation, the purpose of our study was to compare hospitalist and nonhospitalist faculty on the educational experience of third‐year medical students during the inpatient portion of their pediatric clerkships at a single university children's hospital.
METHODS
Study Design
We conducted a retrospective study using evaluations of third‐year medical students comparing hospitalist and nonhospitalist faculty during the inpatient portions of their pediatrics clerkships at a single academic children's hospital over a 15‐month period (July 1999September 2000).
Setting and Sample
We conducted our study at Penn State Children's Hospital (PSCH), a 120‐bed tertiary‐care facility within the 504‐bed Hershey Medical Center, the main teaching hospital affiliated with the Penn State College of Medicine, Hershey, Pennsylvania. The pediatric hospitalist program commenced on July 1, 1999, and during the 15‐month study period the hospitalist staff consisted of 2 physicians who attended a total of 8 months, whereas the nonhospitalist staff consisted of 4 academic general pediatricians and 4 academic pediatric subspecialists who attended the remaining 7 months.
The inpatient clinical responsibilities of both groups of physicians during each month were similar. Both groups of physicians conducted daily rounds with a team that included a senior resident (postgraduate year 3), 2 to 4 interns (postgraduate year 1), 1 acting intern (fourth‐year medical student), and 2 to 4 third‐year medical students. This team was responsible for all admissions to the general pediatrics service, which averages 100 admissions per month. Both the hospitalists and nonhospitalists had outpatient responsibilities during the time they served as inpatient attendings.
During the 15‐month study period, 131 students completed their third‐year pediatrics clerkships. Students at the Penn State College of Medicine may complete their pediatrics clerkship at PSCH or at one of several alternative sites. Because of variability in the structure of the rotation from site to site, it was considered valid only to analyze evaluations completed by students who rotated at PSCH. Sixty‐seven students rotated at PSCH during the study period. Students spent 3 weeks of the 6‐week rotation on the inpatient general pediatrics service. The remaining 3 weeks occurred in multiple outpatient pediatric practice settings and in the newborn nursery. During the 3 weeks the students spent on the inpatient service they did not have outpatient clinic responsibilities, so they did not interact with either the hospitalists or nonhospitalists in the outpatient setting. At the end of the rotation, students were asked to rate the effectiveness of the faculty as teachers, pediatricians, and student advocates and overall on a 4‐point scale (1 = inadequate; 2 = adequate; 3 = very good; 4 = excellent). Students were also asked to evaluate 7 components of the clerkship on the same 4‐point scale (Table 1). Finally, students were asked to provide additional written comments in an unstructured format.
| Evaluation item | Hospitalist mean score (32 evaluations) | Nonhospitalist mean score (35 evaluations) | P value | No. of evaluations rated adequate or inadequate (%)b | |
|---|---|---|---|---|---|
| Hospitalist | Nonhospitalist | ||||
| |||||
| Effectiveness as teacherc | 3.87 | 2.91 | < .001a | 1 (2.9) | 13 (40.6) |
| Effectiveness as pediatriciand | 3.94 | 3.25 | < .001a | 0 (0.0) | 5 (15.6) |
| Effectiveness as student advocatee | 3.76 | 2.97 | < .001a | 2 (5.7) | 13 (40.6) |
| Overall evaluation | 3.93 | 3.06 | < .001a | 0 (0.0) | 10 (31.3) |
| Ward rounds | 3.15 | 2.58 | < .006a | 5 (15.6) | 12 (37.5) |
| Morning report | 3.16 | 3.14 | 0.923 | ||
| Sick newborn | 2.79 | 2.60 | 0.518 | ||
| Well newborn | 2.89 | 3.13 | 0.211 | ||
| Outpatient department clinics | 2.96 | 3.06 | 0.425 | ||
| Private physician's office | 2.97 | 3.01 | 0.794 | ||
| Noon conference | 3.03 | 3.13 | 0.512 | ||
After reviewing the literature concerning faculty evaluation forms and their components, an evaluation form was created for students to indicate their reactions to clerkship components. All the medical students' faculty evaluations were anonymous, and the faculty was not able to review student evaluations prior to assigning grades. Students were required to turn in an evaluation at the end of their rotations. The study was limited to 15 months, as the format of the evaluation form was changed after September 2000 and the general pediatrics service was in the process of transitioning to an exclusively hospitalist‐run service, thereby limiting the number of nonhospitalists available as a comparison group. Demographic characteristics of the hospitalist and nonhospitalist faculty were collected from a faculty database. The study was approved by the Penn State Milton S. Hershey Medical Center's Institutional Review Board.
Statistics and Analysis
For all questions, a Wilcoxon rank sum test was used to evaluate whether the responses for nonhospitalists were different than those for hospitalists. Differences in response by group whose 2‐tailed P values were less than .05 were considered statistically significant. All analyses were performed using the SAS statistical software, version 8.2 (SAS Institute Inc., Cary, NC).
RESULTS
All 67 of the students who completed a pediatrics clerkship at PSCH returned evaluation forms, which were the data for further analysis. Thirty‐five students rotated with the hospitalist faculty, and 32 students rotated with the nonhospitalist faculty. There were no significant demographic differences between the hospitalist and nonhospitalist faculty in age, sex, academic rank, specialty, and years since completing training (Table 2). All the hospitalist faculty fulfilled the definition of a hospitalist,2 whereas none of the physicians in the nonhospitalist group did.
| Characteristic | Hospitalists (n = 2) | Nonhospitalists (n = 8) | P value |
|---|---|---|---|
| Age, mean (range) | 36.0 (3141) | 46.5 (3063) | 0.30 |
| Male/Female | 1/1 | 6/2 | 0.95 |
| Academic rank | |||
| Instructor | 0 | 1 | |
| Assistant professor | 2 | 3 | |
| Associate professor | 0 | 0 | 0.56 |
| Professor | 0 | 4 | |
| Specialty | |||
| General pediatrics | 1 | 4 | |
| Nephrology | 1 | 1 | |
| Genetics | 0 | 1 | 0.95 |
| Infectious ciseases | 0 | 1 | |
| Rheumatology | 0 | 1 | |
| Years since training, mean (range) | 4.0 (08) | 13.8 (030) | 0.43 |
The hospitalists were rated significantly higher than the nonhospitalist faculty in all 4 of the attending characteristics measured (Table 1): teaching effectiveness (3.87 vs. 2.91; P < .0001), effectiveness as a pediatrician (3.94 vs. 3.25; P < .001), student advocacy effectiveness (3.76 vs. 2.97; P < .0001), and overall evaluation (3.93 vs. 3.06; P < .001).
Analysis of specific aspects of the rotation showed the only feature that hospitalists were rated significantly higher on was quality of ward rounds (3.15 vs. 2.58, P < .006). There was no significant difference between the hospitalists and nonhospitalists on features that were not specifically part of the inpatient rotation, including various conferences, outpatient clinics, and newborn care (Table 1).
DISCUSSION
Our study demonstrates that pediatric hospitalists had a positive impact on the overall educational experience of third‐year medical students during the inpatient portions of their pediatrics clerkships. Hospitalists were rated more favorably than nonhospitalists as teachers, as pediatricians, as student advocates, and overall. Medical students also rated the value of ward rounds more favorably when hospitalists conducted them. In addition, higher percentages of nonhospitalists than hospitalists were rated as adequate or inadequate for the above items. When other aspects of the clerkship were analyzed, there were no statistically significant differences between the students who rotated with hospitalists and the students who rotated with nonhospitalists. This suggests that the higher scores for hospitalists were specifically related to their interactions with students, rather than with an overall more positive view of the rotation.
It has been suggested that forces promoting the use of hospitalists in adult medicine are even more persuasive in the pediatric population, as the difference in severity of illness between the inpatient and outpatient setting is greater, and the average pediatrician has less experience than the average internist in managing hospitalized patients.19 In a recent systematic review of the literature, Landrigan et al.20 reported that 6 of 7 studies demonstrated hospitalist systems had decreased hospital length of stay compared to systems in which a primary pediatrician served as the physician of record. This improved efficiency, if combined with the pressure to see more patients while trying to balance teaching and research demands, may have a negative impact on the quality of medical education.
Several factors may have contributed to the students' satisfaction with hospitalists. Studies have demonstrated that students rate clinical teachers more favorably with whom they have greater involvement.21 Hospitalists may be more likely to spend time on the inpatient wards given that is the primary site of their clinical activity. This increased presence may have contributed to more favorable evaluations for the hospitalist faculty, whereas the additional outpatient workload for nonhospitalist faculty may have reduced inpatient teaching opportunities, accounting for their lower teaching score. Included in the pediatrician category was the attribute of being a role model. In a study by Wright et al.,22 spending more than 25% of the time or 25 or more hours per week teaching and conducting rounds was independently associated with being considered an excellent role model. Again, the increased availability of the hospitalists on the inpatient wards may have led to more teaching opportunities, contributing to their higher score.
Our study had several limitations. First, it was a retrospective study conducted at a single institution with only 2 hospitalists. Although there were not statistical significant demographic differences between the 2 groups, this may simply reflect the small size of the sample in our study; therefore, the results may not be applicable to other academic institutions. Second, we retrospectively analyzed an evaluation form that had not been validated or specifically designed to compare 2 physician groups. Third, there were multiple statements in each category that students were asked to consider before scoring each attending on the parameters measured. Although hospitalists were rated higher in each category, there may have been individual characteristics within each category for which the nonhospitalist faculty performed better. Fourth, although hospitalists received higher average ratings than nonhospitalist faculty from third‐year medical students, it is important to emphasize this study measured students' attitudes and beliefs not specific educational outcomes. However, even though we cannot rule out the possibility that potentially confounding factors such as the personality of an attending physician influenced the results, prior studies have demonstrated that medical students make sophisticated judgments about teaching in the clinical setting.23, 24 It is unlikely that hospitalists at our institution were specifically selected to attend more months on a new inpatient service because they had a history of having more favorable teaching qualities because 1 of the 2 hospitalists had just finished residency training, and there were no significant demographic differences between the 2 groups. In a study examining trainee satisfaction in an internal medicine rotation 4 years after adoption of a hospitalist model, where nonhospitalist faculty attended based on their own interest and inpatient skill rather than as a requirement, Hauer et al.14 reported that trainees experienced more effective teaching and a more satisfying inpatient rotation when supervised by hospitalists. This suggests that hospitalists may possess or develop a specific inpatient knowledge base and teaching acumen over time that distinguishes them from nonhospitalists. There is evidence of accumulated experience leading to improved outcomes in the clinical setting for HIV infection,25 various surgical procedures,26 and hospitalist systems.27
In conclusion, this is the first study to evaluate the performance of hospitalists in the setting of a third‐year medical student pediatrics clerkship. Although third‐year medical students rate hospitalists at least as highly as nonhospitalist faculty, further studies are needed to reproduce this finding. In addition to the increased time spent on the wards with students and increased experience in caring for hospitalized patients, further studies should also examine the role that communication plays in clinical teaching. Also, the recent development of core competencies in hospital medicine28 may lead to the development of educational outcomes that can be objectively measured.
Acknowledgements
The authors thank David Mauger, PhD, from the Department of Health Evaluation Sciences at the Penn State College of Medicine for providing statistical analysis of the survey results.
In 1996 Wachter and Goldman anticipated the emergence of hospitalists,1 physicians who are responsible for the care of hospitalized patients in place of their primary care physicians. The number of physicians who identify themselves as hospitalists has grown rapidly since 1996 and is currently estimated to be 10,00012,000, with the potential to reach as high as 30,000 in the next decade.2 This growth includes academic medical centers. In surveys of chairs of internal medicine and pediatric departments, 50% have hospitalists employed at their institutions.3, 4
Hospitalists in academic institutions are playing an increasingly prominent role in the medical education of both residents and medical students. The implications of adopting a hospitalist model on medical education has been discussed.57 Despite such concerns as fragmented continuity of care; decreased exposure to primary care physicians, subspecialists and physician‐scientists; reduced autonomy; and fewer educational opportunities to observe the natural histories of illnesses because of improved efficiency,57 the overall impact of hospitalists on medical and resident education has generally been favorable.818 Internal medicine residents have rated the teaching skills of hospitalists comparable to traditional academic physicians,8, 9 and believe the addition of hospitalists has contributed to an improved educational experience.10, 11, 14 In addition, a survey of third‐year medical students at a single academic teaching hospital concluded that hospitalists were able to provide at least as positive an educational experience during their inpatient medicine rotations as highly rated nonhospitalist teaching faculty.13
The role of hospitalists as educators in pediatrics has been studied much less. Pediatric resident satisfaction has improved in institutions that have used a hospitalist model.1618 In another study, hospitalists were rated by pediatric residents as more effective teachers than nonhospitalists.15 Because we are unaware of any study that has evaluated hospitalists in the education of medical students during their inpatient pediatric rotation, the purpose of our study was to compare hospitalist and nonhospitalist faculty on the educational experience of third‐year medical students during the inpatient portion of their pediatric clerkships at a single university children's hospital.
METHODS
Study Design
We conducted a retrospective study using evaluations of third‐year medical students comparing hospitalist and nonhospitalist faculty during the inpatient portions of their pediatrics clerkships at a single academic children's hospital over a 15‐month period (July 1999September 2000).
Setting and Sample
We conducted our study at Penn State Children's Hospital (PSCH), a 120‐bed tertiary‐care facility within the 504‐bed Hershey Medical Center, the main teaching hospital affiliated with the Penn State College of Medicine, Hershey, Pennsylvania. The pediatric hospitalist program commenced on July 1, 1999, and during the 15‐month study period the hospitalist staff consisted of 2 physicians who attended a total of 8 months, whereas the nonhospitalist staff consisted of 4 academic general pediatricians and 4 academic pediatric subspecialists who attended the remaining 7 months.
The inpatient clinical responsibilities of both groups of physicians during each month were similar. Both groups of physicians conducted daily rounds with a team that included a senior resident (postgraduate year 3), 2 to 4 interns (postgraduate year 1), 1 acting intern (fourth‐year medical student), and 2 to 4 third‐year medical students. This team was responsible for all admissions to the general pediatrics service, which averages 100 admissions per month. Both the hospitalists and nonhospitalists had outpatient responsibilities during the time they served as inpatient attendings.
During the 15‐month study period, 131 students completed their third‐year pediatrics clerkships. Students at the Penn State College of Medicine may complete their pediatrics clerkship at PSCH or at one of several alternative sites. Because of variability in the structure of the rotation from site to site, it was considered valid only to analyze evaluations completed by students who rotated at PSCH. Sixty‐seven students rotated at PSCH during the study period. Students spent 3 weeks of the 6‐week rotation on the inpatient general pediatrics service. The remaining 3 weeks occurred in multiple outpatient pediatric practice settings and in the newborn nursery. During the 3 weeks the students spent on the inpatient service they did not have outpatient clinic responsibilities, so they did not interact with either the hospitalists or nonhospitalists in the outpatient setting. At the end of the rotation, students were asked to rate the effectiveness of the faculty as teachers, pediatricians, and student advocates and overall on a 4‐point scale (1 = inadequate; 2 = adequate; 3 = very good; 4 = excellent). Students were also asked to evaluate 7 components of the clerkship on the same 4‐point scale (Table 1). Finally, students were asked to provide additional written comments in an unstructured format.
| Evaluation item | Hospitalist mean score (32 evaluations) | Nonhospitalist mean score (35 evaluations) | P value | No. of evaluations rated adequate or inadequate (%)b | |
|---|---|---|---|---|---|
| Hospitalist | Nonhospitalist | ||||
| |||||
| Effectiveness as teacherc | 3.87 | 2.91 | < .001a | 1 (2.9) | 13 (40.6) |
| Effectiveness as pediatriciand | 3.94 | 3.25 | < .001a | 0 (0.0) | 5 (15.6) |
| Effectiveness as student advocatee | 3.76 | 2.97 | < .001a | 2 (5.7) | 13 (40.6) |
| Overall evaluation | 3.93 | 3.06 | < .001a | 0 (0.0) | 10 (31.3) |
| Ward rounds | 3.15 | 2.58 | < .006a | 5 (15.6) | 12 (37.5) |
| Morning report | 3.16 | 3.14 | 0.923 | ||
| Sick newborn | 2.79 | 2.60 | 0.518 | ||
| Well newborn | 2.89 | 3.13 | 0.211 | ||
| Outpatient department clinics | 2.96 | 3.06 | 0.425 | ||
| Private physician's office | 2.97 | 3.01 | 0.794 | ||
| Noon conference | 3.03 | 3.13 | 0.512 | ||
After reviewing the literature concerning faculty evaluation forms and their components, an evaluation form was created for students to indicate their reactions to clerkship components. All the medical students' faculty evaluations were anonymous, and the faculty was not able to review student evaluations prior to assigning grades. Students were required to turn in an evaluation at the end of their rotations. The study was limited to 15 months, as the format of the evaluation form was changed after September 2000 and the general pediatrics service was in the process of transitioning to an exclusively hospitalist‐run service, thereby limiting the number of nonhospitalists available as a comparison group. Demographic characteristics of the hospitalist and nonhospitalist faculty were collected from a faculty database. The study was approved by the Penn State Milton S. Hershey Medical Center's Institutional Review Board.
Statistics and Analysis
For all questions, a Wilcoxon rank sum test was used to evaluate whether the responses for nonhospitalists were different than those for hospitalists. Differences in response by group whose 2‐tailed P values were less than .05 were considered statistically significant. All analyses were performed using the SAS statistical software, version 8.2 (SAS Institute Inc., Cary, NC).
RESULTS
All 67 of the students who completed a pediatrics clerkship at PSCH returned evaluation forms, which were the data for further analysis. Thirty‐five students rotated with the hospitalist faculty, and 32 students rotated with the nonhospitalist faculty. There were no significant demographic differences between the hospitalist and nonhospitalist faculty in age, sex, academic rank, specialty, and years since completing training (Table 2). All the hospitalist faculty fulfilled the definition of a hospitalist,2 whereas none of the physicians in the nonhospitalist group did.
| Characteristic | Hospitalists (n = 2) | Nonhospitalists (n = 8) | P value |
|---|---|---|---|
| Age, mean (range) | 36.0 (3141) | 46.5 (3063) | 0.30 |
| Male/Female | 1/1 | 6/2 | 0.95 |
| Academic rank | |||
| Instructor | 0 | 1 | |
| Assistant professor | 2 | 3 | |
| Associate professor | 0 | 0 | 0.56 |
| Professor | 0 | 4 | |
| Specialty | |||
| General pediatrics | 1 | 4 | |
| Nephrology | 1 | 1 | |
| Genetics | 0 | 1 | 0.95 |
| Infectious ciseases | 0 | 1 | |
| Rheumatology | 0 | 1 | |
| Years since training, mean (range) | 4.0 (08) | 13.8 (030) | 0.43 |
The hospitalists were rated significantly higher than the nonhospitalist faculty in all 4 of the attending characteristics measured (Table 1): teaching effectiveness (3.87 vs. 2.91; P < .0001), effectiveness as a pediatrician (3.94 vs. 3.25; P < .001), student advocacy effectiveness (3.76 vs. 2.97; P < .0001), and overall evaluation (3.93 vs. 3.06; P < .001).
Analysis of specific aspects of the rotation showed the only feature that hospitalists were rated significantly higher on was quality of ward rounds (3.15 vs. 2.58, P < .006). There was no significant difference between the hospitalists and nonhospitalists on features that were not specifically part of the inpatient rotation, including various conferences, outpatient clinics, and newborn care (Table 1).
DISCUSSION
Our study demonstrates that pediatric hospitalists had a positive impact on the overall educational experience of third‐year medical students during the inpatient portions of their pediatrics clerkships. Hospitalists were rated more favorably than nonhospitalists as teachers, as pediatricians, as student advocates, and overall. Medical students also rated the value of ward rounds more favorably when hospitalists conducted them. In addition, higher percentages of nonhospitalists than hospitalists were rated as adequate or inadequate for the above items. When other aspects of the clerkship were analyzed, there were no statistically significant differences between the students who rotated with hospitalists and the students who rotated with nonhospitalists. This suggests that the higher scores for hospitalists were specifically related to their interactions with students, rather than with an overall more positive view of the rotation.
It has been suggested that forces promoting the use of hospitalists in adult medicine are even more persuasive in the pediatric population, as the difference in severity of illness between the inpatient and outpatient setting is greater, and the average pediatrician has less experience than the average internist in managing hospitalized patients.19 In a recent systematic review of the literature, Landrigan et al.20 reported that 6 of 7 studies demonstrated hospitalist systems had decreased hospital length of stay compared to systems in which a primary pediatrician served as the physician of record. This improved efficiency, if combined with the pressure to see more patients while trying to balance teaching and research demands, may have a negative impact on the quality of medical education.
Several factors may have contributed to the students' satisfaction with hospitalists. Studies have demonstrated that students rate clinical teachers more favorably with whom they have greater involvement.21 Hospitalists may be more likely to spend time on the inpatient wards given that is the primary site of their clinical activity. This increased presence may have contributed to more favorable evaluations for the hospitalist faculty, whereas the additional outpatient workload for nonhospitalist faculty may have reduced inpatient teaching opportunities, accounting for their lower teaching score. Included in the pediatrician category was the attribute of being a role model. In a study by Wright et al.,22 spending more than 25% of the time or 25 or more hours per week teaching and conducting rounds was independently associated with being considered an excellent role model. Again, the increased availability of the hospitalists on the inpatient wards may have led to more teaching opportunities, contributing to their higher score.
Our study had several limitations. First, it was a retrospective study conducted at a single institution with only 2 hospitalists. Although there were not statistical significant demographic differences between the 2 groups, this may simply reflect the small size of the sample in our study; therefore, the results may not be applicable to other academic institutions. Second, we retrospectively analyzed an evaluation form that had not been validated or specifically designed to compare 2 physician groups. Third, there were multiple statements in each category that students were asked to consider before scoring each attending on the parameters measured. Although hospitalists were rated higher in each category, there may have been individual characteristics within each category for which the nonhospitalist faculty performed better. Fourth, although hospitalists received higher average ratings than nonhospitalist faculty from third‐year medical students, it is important to emphasize this study measured students' attitudes and beliefs not specific educational outcomes. However, even though we cannot rule out the possibility that potentially confounding factors such as the personality of an attending physician influenced the results, prior studies have demonstrated that medical students make sophisticated judgments about teaching in the clinical setting.23, 24 It is unlikely that hospitalists at our institution were specifically selected to attend more months on a new inpatient service because they had a history of having more favorable teaching qualities because 1 of the 2 hospitalists had just finished residency training, and there were no significant demographic differences between the 2 groups. In a study examining trainee satisfaction in an internal medicine rotation 4 years after adoption of a hospitalist model, where nonhospitalist faculty attended based on their own interest and inpatient skill rather than as a requirement, Hauer et al.14 reported that trainees experienced more effective teaching and a more satisfying inpatient rotation when supervised by hospitalists. This suggests that hospitalists may possess or develop a specific inpatient knowledge base and teaching acumen over time that distinguishes them from nonhospitalists. There is evidence of accumulated experience leading to improved outcomes in the clinical setting for HIV infection,25 various surgical procedures,26 and hospitalist systems.27
In conclusion, this is the first study to evaluate the performance of hospitalists in the setting of a third‐year medical student pediatrics clerkship. Although third‐year medical students rate hospitalists at least as highly as nonhospitalist faculty, further studies are needed to reproduce this finding. In addition to the increased time spent on the wards with students and increased experience in caring for hospitalized patients, further studies should also examine the role that communication plays in clinical teaching. Also, the recent development of core competencies in hospital medicine28 may lead to the development of educational outcomes that can be objectively measured.
Acknowledgements
The authors thank David Mauger, PhD, from the Department of Health Evaluation Sciences at the Penn State College of Medicine for providing statistical analysis of the survey results.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Frequently asked questions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=FAQs75:S34–6.
- ,,,,,.Pediatric hospitalists in Canada and the United States: a survey of pediatric academic department chairs.Ambul Pediatr.2001;1:338–339.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- ,.The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- ,.Implications of the hospitalist model for medical students' education.Acad. Med.2001;76:324–330.
- ,,,,.Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,, et al.Hospitalists as teachers: how do they compare to subspecialty and general medicine faculty.J Gen Intern Med.2004;19:8–15.
- ,,,,.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- ,,,,,.Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112:597–601.
- ,,,,,,.The positive impact of initiation of hospitalist clinician educators: resource utilization and medical resident education.J Gen Intern Med.2004;19:293–301.
- ,,,.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156:877–883.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76:556.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr.2000;39:221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr.2001;40:653–660.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–477.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- ,,.Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1993.
- ,.Evaluation of clinical instructors by third‐year medical students.Acad Med.1989;64:159–164.
- ,,.Clinical tutor evaluation: a 5‐year study by students on an in‐patient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–53.
- ,,,,,.Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival.N Engl J Med.1996;334:701–706.
- ,,,.Hospital Volume, Physician Volume, and Patient Outcomes: Assessing the Evidence. Ann Arbor, MI: Health Administration Perspectives;1990.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,,,, eds.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(S1):1–67.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Frequently asked questions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=FAQs75:S34–6.
- ,,,,,.Pediatric hospitalists in Canada and the United States: a survey of pediatric academic department chairs.Ambul Pediatr.2001;1:338–339.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- ,.The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- ,.Implications of the hospitalist model for medical students' education.Acad. Med.2001;76:324–330.
- ,,,,.Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,, et al.Hospitalists as teachers: how do they compare to subspecialty and general medicine faculty.J Gen Intern Med.2004;19:8–15.
- ,,,,.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- ,,,,,.Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112:597–601.
- ,,,,,,.The positive impact of initiation of hospitalist clinician educators: resource utilization and medical resident education.J Gen Intern Med.2004;19:293–301.
- ,,,.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156:877–883.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76:556.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr.2000;39:221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr.2001;40:653–660.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–477.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- ,,.Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1993.
- ,.Evaluation of clinical instructors by third‐year medical students.Acad Med.1989;64:159–164.
- ,,.Clinical tutor evaluation: a 5‐year study by students on an in‐patient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–53.
- ,,,,,.Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival.N Engl J Med.1996;334:701–706.
- ,,,.Hospital Volume, Physician Volume, and Patient Outcomes: Assessing the Evidence. Ann Arbor, MI: Health Administration Perspectives;1990.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,,,, eds.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(S1):1–67.
Copyright © 2007 Society of Hospital Medicine
A new home awaits the hospitalist
In this issue of the Journal of Hospital Medicine, Simon et al.1 provide the first report of pediatric hospitalist comanagement of patients undergoing spinal fusion surgery. In this retrospective cohort study, 14 of 115 patients were comanaged by a pediatric hospitalist. The primary outcomes of the study were length of stay and variability in length of stay. Prior to the initiation of hospitalist comanagement service, all patients were managed preoperatively by a spine surgery nurse and aided by medical subspecialists and other allied health professionals (nutritionists, respiratory therapists, physical therapists, social workers). After the intervention, patients with the most complex medical disease were assigned to comanagement by a pediatric hospitalist. When compared to a historical control of patients with similar medical complexity but not comanaged by hospitalists, the length of stay was reduced by 2.4 days (8.6 vs. 6.2 days). The variability in mean length of stay was also reduced.
This study follows on the heels of 3 important studies addressing the utility of hospitalists in the comanagement of surgical patients. The HOT (Hospitalist Orthopedic Team) trial was a randomized controlled trial assessing the effect of hospitalists on the management of patients undergoing elective hip and knee arthroplasty.2 There was no effect on length of stay or patient outcomes, though the comanagement model did decrease minor postoperative medical complications and improve physician and nurse satisfaction. Macpherson et al. conducted a retrospective trial where an internist joined a cardiothoracic surgery service at a tertiary‐care center.3 They found a decrease in overall mortality and resource utilization such as labs testing and consultations. There was significant reduction in the length of stay and number of x‐rays performed. The third study, by Jaffer et al.,4 showed that an outpatient, preoperative evaluation clinic staffed by hospitalists at a large tertiary‐care center provides a practical model for managing preoperative patients and may be associated with a low rate of postoperative pulmonary complications.
The study by Simon et al. in this issue of the journal has limitations. It is a retrospective cohort trial, and like all such study designs, the validity of the results is subject to confounding. Severity of patient medical disease, intraoperative complications, and advances in surgical technique are examples. While the authors did everything possible to minimize the effect of confounding, it remains a limitation of the study. The study also enrolled only 14 patients in the comanagement group, and this limited any stratification or subgroup analysis to offset known confounders. Patients assigned to the hospitalist comanagement service were by design more medically complex than other spinal fusion patients, and generalizing the results of this trial to all spinal fusion patients may not be possible.
From the study's limitations, however, comes great insight into the role of the hospitalist in surgical comanagement. It is clear from the aforementioned studies that there is a role for the hospitalist in comanagement of surgical patients. While the evidence is conflicting, there are scenarios in which comanagement improves efficiency and quality of care. Yet it is also possible that hospitalist comanagement is not ideal for all surgical patients. The HOT trial did not show benefits in length‐of‐stay reduction or patient mortality because the patients were homogenous in their complexity and pre‐ and postoperative care was protocol driven. Length of stay was limited by accessibility of rehabilitation facilities after discharge and not the efficiency of medical care in the hospital. The study in this issue of the Journal of Hospital Medicine selectively included patients with the highest complexity of medical disease, and there was a reduction in length of stay. Both trials suggest that the greatest potential benefit for augmenting efficiency and outcomes with hospitalist comanagement may be predicated on the complexity of the patients involved and the surgical system through which they will receive care.
The next step in assessing hospitalist comanagement should not be a hunt‐and‐peck exercise to stumble on the surgical procedures that show benefit from comanagement. Rather, the prudent next step is to follow the lead of Simon et al. and others3, 4 in trying to identify those surgical patients who represent the greatest medical complexity or have the most variability in their preoperative and postoperative medical care. These are the patients for whom the hospitalist can effect the greatest benefit and the services for which the hospitalist can best augment efficiency. High‐risk procedures, patients with multiple comorbitities or elevated preoperative risks, and surgical procedures without defined pre‐ and postoperative protocols would appear to be the ideal candidates for hospitalist comanagement.
As the discussion of hospital comanagement progresses, it is important to recognize comanagement as a paradigm shift. Surgical comanagement is not merely medical consultation. To be successful, the role of the hospitalist in comanaging surgical patients must be clearly defined as advancing postoperative care as much as it is in assessing preoperative risk. As a comanager, a hospitalist must actively manage preexisting and newly developed medical issues rather than just make recommendations for the surgical team.
The hospitalist must also be more than a discharge coordinator postoperatively; investing in hospitalists merely for discharge planning is a poor use of resources both from a financial and an opportunity‐cost perspective. The paradigm of comanagement is not foreign, however, and hospitalists are likely to prosper by learning from the experience of our nephrology and hepatology colleagues, who have successfully found collaborative roles in improving patient care on renal and liver transplant services. The success of these services is due to the precisely defined roles for the internist and the surgeon and because the complexity of the patient being managed warrants continuity of expert consultation.
There is great potential for the hospitalist in surgical comanagement. In less than a decade, the focus of hospital‐based medical care has shifted from staffing a shift to improving the quality of the system through which patients traverse the hospital. The lessons hospitalists have learned in quality improvement and in augmenting systems of care are perfectly suited for application to surgical services. Hospitalist comanagement is right not only because it may offer improvement in a surgical patient's medical care, but also for the augmentation of quality improvement in surgical services that have yet to reap the benefits that have defined the excellence of hospitalist medicine. The next step is to embark on the road of prudent prospective research: identifying the patients, and the procedures, that have the greatest opportunity for improvement by hospitalist comanagement. And at the end of that road will be a new home for the hospitalist, assuming the role of the quality‐advocate for all aspects of hospital care: pediatric, medical, and surgical patients.
- ,,,,.Pediatric co‐management of spine fusion surgery patients.J Hosp Med.2007;2:23–30.
- ,,, et al.;Hospitalist‐Orthopedic Team Trial Investigators.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,,,.An internist joins the surgery service: does comanagement make a difference?J Gen Intern Med.1994;9:440–444.
- ,,, et al.Postoperative pulmonary complications: experience with an outpatient pre‐operative assessment program.J Clin Outcomes Manag.2005;12:505–510.
In this issue of the Journal of Hospital Medicine, Simon et al.1 provide the first report of pediatric hospitalist comanagement of patients undergoing spinal fusion surgery. In this retrospective cohort study, 14 of 115 patients were comanaged by a pediatric hospitalist. The primary outcomes of the study were length of stay and variability in length of stay. Prior to the initiation of hospitalist comanagement service, all patients were managed preoperatively by a spine surgery nurse and aided by medical subspecialists and other allied health professionals (nutritionists, respiratory therapists, physical therapists, social workers). After the intervention, patients with the most complex medical disease were assigned to comanagement by a pediatric hospitalist. When compared to a historical control of patients with similar medical complexity but not comanaged by hospitalists, the length of stay was reduced by 2.4 days (8.6 vs. 6.2 days). The variability in mean length of stay was also reduced.
This study follows on the heels of 3 important studies addressing the utility of hospitalists in the comanagement of surgical patients. The HOT (Hospitalist Orthopedic Team) trial was a randomized controlled trial assessing the effect of hospitalists on the management of patients undergoing elective hip and knee arthroplasty.2 There was no effect on length of stay or patient outcomes, though the comanagement model did decrease minor postoperative medical complications and improve physician and nurse satisfaction. Macpherson et al. conducted a retrospective trial where an internist joined a cardiothoracic surgery service at a tertiary‐care center.3 They found a decrease in overall mortality and resource utilization such as labs testing and consultations. There was significant reduction in the length of stay and number of x‐rays performed. The third study, by Jaffer et al.,4 showed that an outpatient, preoperative evaluation clinic staffed by hospitalists at a large tertiary‐care center provides a practical model for managing preoperative patients and may be associated with a low rate of postoperative pulmonary complications.
The study by Simon et al. in this issue of the journal has limitations. It is a retrospective cohort trial, and like all such study designs, the validity of the results is subject to confounding. Severity of patient medical disease, intraoperative complications, and advances in surgical technique are examples. While the authors did everything possible to minimize the effect of confounding, it remains a limitation of the study. The study also enrolled only 14 patients in the comanagement group, and this limited any stratification or subgroup analysis to offset known confounders. Patients assigned to the hospitalist comanagement service were by design more medically complex than other spinal fusion patients, and generalizing the results of this trial to all spinal fusion patients may not be possible.
From the study's limitations, however, comes great insight into the role of the hospitalist in surgical comanagement. It is clear from the aforementioned studies that there is a role for the hospitalist in comanagement of surgical patients. While the evidence is conflicting, there are scenarios in which comanagement improves efficiency and quality of care. Yet it is also possible that hospitalist comanagement is not ideal for all surgical patients. The HOT trial did not show benefits in length‐of‐stay reduction or patient mortality because the patients were homogenous in their complexity and pre‐ and postoperative care was protocol driven. Length of stay was limited by accessibility of rehabilitation facilities after discharge and not the efficiency of medical care in the hospital. The study in this issue of the Journal of Hospital Medicine selectively included patients with the highest complexity of medical disease, and there was a reduction in length of stay. Both trials suggest that the greatest potential benefit for augmenting efficiency and outcomes with hospitalist comanagement may be predicated on the complexity of the patients involved and the surgical system through which they will receive care.
The next step in assessing hospitalist comanagement should not be a hunt‐and‐peck exercise to stumble on the surgical procedures that show benefit from comanagement. Rather, the prudent next step is to follow the lead of Simon et al. and others3, 4 in trying to identify those surgical patients who represent the greatest medical complexity or have the most variability in their preoperative and postoperative medical care. These are the patients for whom the hospitalist can effect the greatest benefit and the services for which the hospitalist can best augment efficiency. High‐risk procedures, patients with multiple comorbitities or elevated preoperative risks, and surgical procedures without defined pre‐ and postoperative protocols would appear to be the ideal candidates for hospitalist comanagement.
As the discussion of hospital comanagement progresses, it is important to recognize comanagement as a paradigm shift. Surgical comanagement is not merely medical consultation. To be successful, the role of the hospitalist in comanaging surgical patients must be clearly defined as advancing postoperative care as much as it is in assessing preoperative risk. As a comanager, a hospitalist must actively manage preexisting and newly developed medical issues rather than just make recommendations for the surgical team.
The hospitalist must also be more than a discharge coordinator postoperatively; investing in hospitalists merely for discharge planning is a poor use of resources both from a financial and an opportunity‐cost perspective. The paradigm of comanagement is not foreign, however, and hospitalists are likely to prosper by learning from the experience of our nephrology and hepatology colleagues, who have successfully found collaborative roles in improving patient care on renal and liver transplant services. The success of these services is due to the precisely defined roles for the internist and the surgeon and because the complexity of the patient being managed warrants continuity of expert consultation.
There is great potential for the hospitalist in surgical comanagement. In less than a decade, the focus of hospital‐based medical care has shifted from staffing a shift to improving the quality of the system through which patients traverse the hospital. The lessons hospitalists have learned in quality improvement and in augmenting systems of care are perfectly suited for application to surgical services. Hospitalist comanagement is right not only because it may offer improvement in a surgical patient's medical care, but also for the augmentation of quality improvement in surgical services that have yet to reap the benefits that have defined the excellence of hospitalist medicine. The next step is to embark on the road of prudent prospective research: identifying the patients, and the procedures, that have the greatest opportunity for improvement by hospitalist comanagement. And at the end of that road will be a new home for the hospitalist, assuming the role of the quality‐advocate for all aspects of hospital care: pediatric, medical, and surgical patients.
In this issue of the Journal of Hospital Medicine, Simon et al.1 provide the first report of pediatric hospitalist comanagement of patients undergoing spinal fusion surgery. In this retrospective cohort study, 14 of 115 patients were comanaged by a pediatric hospitalist. The primary outcomes of the study were length of stay and variability in length of stay. Prior to the initiation of hospitalist comanagement service, all patients were managed preoperatively by a spine surgery nurse and aided by medical subspecialists and other allied health professionals (nutritionists, respiratory therapists, physical therapists, social workers). After the intervention, patients with the most complex medical disease were assigned to comanagement by a pediatric hospitalist. When compared to a historical control of patients with similar medical complexity but not comanaged by hospitalists, the length of stay was reduced by 2.4 days (8.6 vs. 6.2 days). The variability in mean length of stay was also reduced.
This study follows on the heels of 3 important studies addressing the utility of hospitalists in the comanagement of surgical patients. The HOT (Hospitalist Orthopedic Team) trial was a randomized controlled trial assessing the effect of hospitalists on the management of patients undergoing elective hip and knee arthroplasty.2 There was no effect on length of stay or patient outcomes, though the comanagement model did decrease minor postoperative medical complications and improve physician and nurse satisfaction. Macpherson et al. conducted a retrospective trial where an internist joined a cardiothoracic surgery service at a tertiary‐care center.3 They found a decrease in overall mortality and resource utilization such as labs testing and consultations. There was significant reduction in the length of stay and number of x‐rays performed. The third study, by Jaffer et al.,4 showed that an outpatient, preoperative evaluation clinic staffed by hospitalists at a large tertiary‐care center provides a practical model for managing preoperative patients and may be associated with a low rate of postoperative pulmonary complications.
The study by Simon et al. in this issue of the journal has limitations. It is a retrospective cohort trial, and like all such study designs, the validity of the results is subject to confounding. Severity of patient medical disease, intraoperative complications, and advances in surgical technique are examples. While the authors did everything possible to minimize the effect of confounding, it remains a limitation of the study. The study also enrolled only 14 patients in the comanagement group, and this limited any stratification or subgroup analysis to offset known confounders. Patients assigned to the hospitalist comanagement service were by design more medically complex than other spinal fusion patients, and generalizing the results of this trial to all spinal fusion patients may not be possible.
From the study's limitations, however, comes great insight into the role of the hospitalist in surgical comanagement. It is clear from the aforementioned studies that there is a role for the hospitalist in comanagement of surgical patients. While the evidence is conflicting, there are scenarios in which comanagement improves efficiency and quality of care. Yet it is also possible that hospitalist comanagement is not ideal for all surgical patients. The HOT trial did not show benefits in length‐of‐stay reduction or patient mortality because the patients were homogenous in their complexity and pre‐ and postoperative care was protocol driven. Length of stay was limited by accessibility of rehabilitation facilities after discharge and not the efficiency of medical care in the hospital. The study in this issue of the Journal of Hospital Medicine selectively included patients with the highest complexity of medical disease, and there was a reduction in length of stay. Both trials suggest that the greatest potential benefit for augmenting efficiency and outcomes with hospitalist comanagement may be predicated on the complexity of the patients involved and the surgical system through which they will receive care.
The next step in assessing hospitalist comanagement should not be a hunt‐and‐peck exercise to stumble on the surgical procedures that show benefit from comanagement. Rather, the prudent next step is to follow the lead of Simon et al. and others3, 4 in trying to identify those surgical patients who represent the greatest medical complexity or have the most variability in their preoperative and postoperative medical care. These are the patients for whom the hospitalist can effect the greatest benefit and the services for which the hospitalist can best augment efficiency. High‐risk procedures, patients with multiple comorbitities or elevated preoperative risks, and surgical procedures without defined pre‐ and postoperative protocols would appear to be the ideal candidates for hospitalist comanagement.
As the discussion of hospital comanagement progresses, it is important to recognize comanagement as a paradigm shift. Surgical comanagement is not merely medical consultation. To be successful, the role of the hospitalist in comanaging surgical patients must be clearly defined as advancing postoperative care as much as it is in assessing preoperative risk. As a comanager, a hospitalist must actively manage preexisting and newly developed medical issues rather than just make recommendations for the surgical team.
The hospitalist must also be more than a discharge coordinator postoperatively; investing in hospitalists merely for discharge planning is a poor use of resources both from a financial and an opportunity‐cost perspective. The paradigm of comanagement is not foreign, however, and hospitalists are likely to prosper by learning from the experience of our nephrology and hepatology colleagues, who have successfully found collaborative roles in improving patient care on renal and liver transplant services. The success of these services is due to the precisely defined roles for the internist and the surgeon and because the complexity of the patient being managed warrants continuity of expert consultation.
There is great potential for the hospitalist in surgical comanagement. In less than a decade, the focus of hospital‐based medical care has shifted from staffing a shift to improving the quality of the system through which patients traverse the hospital. The lessons hospitalists have learned in quality improvement and in augmenting systems of care are perfectly suited for application to surgical services. Hospitalist comanagement is right not only because it may offer improvement in a surgical patient's medical care, but also for the augmentation of quality improvement in surgical services that have yet to reap the benefits that have defined the excellence of hospitalist medicine. The next step is to embark on the road of prudent prospective research: identifying the patients, and the procedures, that have the greatest opportunity for improvement by hospitalist comanagement. And at the end of that road will be a new home for the hospitalist, assuming the role of the quality‐advocate for all aspects of hospital care: pediatric, medical, and surgical patients.
- ,,,,.Pediatric co‐management of spine fusion surgery patients.J Hosp Med.2007;2:23–30.
- ,,, et al.;Hospitalist‐Orthopedic Team Trial Investigators.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,,,.An internist joins the surgery service: does comanagement make a difference?J Gen Intern Med.1994;9:440–444.
- ,,, et al.Postoperative pulmonary complications: experience with an outpatient pre‐operative assessment program.J Clin Outcomes Manag.2005;12:505–510.
- ,,,,.Pediatric co‐management of spine fusion surgery patients.J Hosp Med.2007;2:23–30.
- ,,, et al.;Hospitalist‐Orthopedic Team Trial Investigators.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,,,.An internist joins the surgery service: does comanagement make a difference?J Gen Intern Med.1994;9:440–444.
- ,,, et al.Postoperative pulmonary complications: experience with an outpatient pre‐operative assessment program.J Clin Outcomes Manag.2005;12:505–510.
Editorial
One year of the Journal of Hospital Medicine is done, and we now embark on our second with this first issue of volume 2. Before moving on, I heartily thank all the authors who contributed their manuscripts to the Journal of Hospital Medicine (JHM), bravely investing in this new academic periodical. A remarkable 284 manuscripts have been submitted since we first opened the JHM Web site, 197 of them during 2006. This clearly reflects the robust demand by hospitalists and their colleagues for original research and relevant clinical reviews about our evolving specialty of hospital medicine. I probably should not be surprised that this demand exists among the 15,000‐plus hospitalists in America and the 6000‐plus members of the Society of Hospital Medicine. Regardless, I am ineffably humbled by the enthusiasm and energy of all the contributors.
Understandably, this volume of submissions, exceeding our projections by nearly 50%, required yeoman's work by our associate editors and reviewers. On page 55 we list the 203 reviewers who donated their time and acumen to assure the quality of our publication. Many reviewed more than 4 articles during the year. Our associate editors deserve particular appreciation and gratitude for their willingness to donate extraordinary amounts of time and effort to ensure the success of JHMVincent Chang from Boston Children's Hospital, Scott Flanders from the University of Michigan, Karen Hauer from the University of California, San Francisco, Jean Kutner from the University of Colorado, James Pile from Cleveland MetroHealth, and Kaveh Shojania from the University of Ottawa. Additionally, the energetic assistant editors have supported them and me with frequent reviews, article submissions, and creative ideas for improving the journal. Finally, our auspicious editorial board has proffered sage guidance, and many of its members have also submitted manuscripts and participated in reviewing articles.
Moving forward we expect continued growth, as both the submitted articles and demand for the journal are being recognized. At 7:29 a.m. on November 30, 2006, Vickie Thaw (Vice President and Publisher, John Wiley & Sons, Inc.) called me to report that the National Library of Medicine validated all our efforts. The Journal of Hospital Medicine had been selected for indexing and inclusion in the National Library of Medicine's MEDLINE (Medical Literature Analysis and Retrieval System Online). The primary component of PubMed, MEDLINE is a bibliographic database containing approximately 13 million references to journal articles on medicine, nursing, dentistry, veterinary medicine, health care systems, and preclinical sciences dating to the mid‐1960s. With this approval, hospital medicine has achieved another milestone in its evolution into a new specialty.
We now hope to respond to the robust interest in clinical materials as well as to continue publication of original research. To achieve our aim of increasing the amount of clinically relevant content for practicing hospitalists, authors are encouraged to submit to JHM case reports, clinical updates, and clinical images that convey novel or underappreciated teaching points. Teaching points may be purely clinical and may focus on clinical pearls or unusual presentations of well‐known diseases, although submission of straightforward presentations of rare diseases is discouraged. Alternatively, manuscripts may involve succinct case‐based descriptions of innovations, quality improvementrelated issues, or medical errors. Submitted case reports should be less than 800 words and should contain a maximum of 5 references and no more than 1 table or figure. Case reports should not include an abstract. Submission of the case report and review type should be avoided. Instead, we seek formal clinical updates of no more than 2000 words that present important aspects of a case along with new research findings and citations from the literature that change what has historically been the standard of delivery of care. Finally, we continue to seek cases most appropriate for the Hospital Images Dx section, edited by Paul Aronowitz. They should be submitted with that designation and have fewer than 150 words. These 3 categories are identified on our Manuscript Central website (
Again, thanks to all of you for making the launch of the Journal of Hospital Medicine an unqualified success. We look forward to your continued participation as we grow as the premier journal for the specialty of hospital medicine.
P.S. Sadly, one of our superstar associate editors, Kaveh Shojania, is stepping aside, and we sincerely express thanks for his terrific contributions. We welcome suggestions for an alternative to fulfill his responsibilities.
One year of the Journal of Hospital Medicine is done, and we now embark on our second with this first issue of volume 2. Before moving on, I heartily thank all the authors who contributed their manuscripts to the Journal of Hospital Medicine (JHM), bravely investing in this new academic periodical. A remarkable 284 manuscripts have been submitted since we first opened the JHM Web site, 197 of them during 2006. This clearly reflects the robust demand by hospitalists and their colleagues for original research and relevant clinical reviews about our evolving specialty of hospital medicine. I probably should not be surprised that this demand exists among the 15,000‐plus hospitalists in America and the 6000‐plus members of the Society of Hospital Medicine. Regardless, I am ineffably humbled by the enthusiasm and energy of all the contributors.
Understandably, this volume of submissions, exceeding our projections by nearly 50%, required yeoman's work by our associate editors and reviewers. On page 55 we list the 203 reviewers who donated their time and acumen to assure the quality of our publication. Many reviewed more than 4 articles during the year. Our associate editors deserve particular appreciation and gratitude for their willingness to donate extraordinary amounts of time and effort to ensure the success of JHMVincent Chang from Boston Children's Hospital, Scott Flanders from the University of Michigan, Karen Hauer from the University of California, San Francisco, Jean Kutner from the University of Colorado, James Pile from Cleveland MetroHealth, and Kaveh Shojania from the University of Ottawa. Additionally, the energetic assistant editors have supported them and me with frequent reviews, article submissions, and creative ideas for improving the journal. Finally, our auspicious editorial board has proffered sage guidance, and many of its members have also submitted manuscripts and participated in reviewing articles.
Moving forward we expect continued growth, as both the submitted articles and demand for the journal are being recognized. At 7:29 a.m. on November 30, 2006, Vickie Thaw (Vice President and Publisher, John Wiley & Sons, Inc.) called me to report that the National Library of Medicine validated all our efforts. The Journal of Hospital Medicine had been selected for indexing and inclusion in the National Library of Medicine's MEDLINE (Medical Literature Analysis and Retrieval System Online). The primary component of PubMed, MEDLINE is a bibliographic database containing approximately 13 million references to journal articles on medicine, nursing, dentistry, veterinary medicine, health care systems, and preclinical sciences dating to the mid‐1960s. With this approval, hospital medicine has achieved another milestone in its evolution into a new specialty.
We now hope to respond to the robust interest in clinical materials as well as to continue publication of original research. To achieve our aim of increasing the amount of clinically relevant content for practicing hospitalists, authors are encouraged to submit to JHM case reports, clinical updates, and clinical images that convey novel or underappreciated teaching points. Teaching points may be purely clinical and may focus on clinical pearls or unusual presentations of well‐known diseases, although submission of straightforward presentations of rare diseases is discouraged. Alternatively, manuscripts may involve succinct case‐based descriptions of innovations, quality improvementrelated issues, or medical errors. Submitted case reports should be less than 800 words and should contain a maximum of 5 references and no more than 1 table or figure. Case reports should not include an abstract. Submission of the case report and review type should be avoided. Instead, we seek formal clinical updates of no more than 2000 words that present important aspects of a case along with new research findings and citations from the literature that change what has historically been the standard of delivery of care. Finally, we continue to seek cases most appropriate for the Hospital Images Dx section, edited by Paul Aronowitz. They should be submitted with that designation and have fewer than 150 words. These 3 categories are identified on our Manuscript Central website (
Again, thanks to all of you for making the launch of the Journal of Hospital Medicine an unqualified success. We look forward to your continued participation as we grow as the premier journal for the specialty of hospital medicine.
P.S. Sadly, one of our superstar associate editors, Kaveh Shojania, is stepping aside, and we sincerely express thanks for his terrific contributions. We welcome suggestions for an alternative to fulfill his responsibilities.
One year of the Journal of Hospital Medicine is done, and we now embark on our second with this first issue of volume 2. Before moving on, I heartily thank all the authors who contributed their manuscripts to the Journal of Hospital Medicine (JHM), bravely investing in this new academic periodical. A remarkable 284 manuscripts have been submitted since we first opened the JHM Web site, 197 of them during 2006. This clearly reflects the robust demand by hospitalists and their colleagues for original research and relevant clinical reviews about our evolving specialty of hospital medicine. I probably should not be surprised that this demand exists among the 15,000‐plus hospitalists in America and the 6000‐plus members of the Society of Hospital Medicine. Regardless, I am ineffably humbled by the enthusiasm and energy of all the contributors.
Understandably, this volume of submissions, exceeding our projections by nearly 50%, required yeoman's work by our associate editors and reviewers. On page 55 we list the 203 reviewers who donated their time and acumen to assure the quality of our publication. Many reviewed more than 4 articles during the year. Our associate editors deserve particular appreciation and gratitude for their willingness to donate extraordinary amounts of time and effort to ensure the success of JHMVincent Chang from Boston Children's Hospital, Scott Flanders from the University of Michigan, Karen Hauer from the University of California, San Francisco, Jean Kutner from the University of Colorado, James Pile from Cleveland MetroHealth, and Kaveh Shojania from the University of Ottawa. Additionally, the energetic assistant editors have supported them and me with frequent reviews, article submissions, and creative ideas for improving the journal. Finally, our auspicious editorial board has proffered sage guidance, and many of its members have also submitted manuscripts and participated in reviewing articles.
Moving forward we expect continued growth, as both the submitted articles and demand for the journal are being recognized. At 7:29 a.m. on November 30, 2006, Vickie Thaw (Vice President and Publisher, John Wiley & Sons, Inc.) called me to report that the National Library of Medicine validated all our efforts. The Journal of Hospital Medicine had been selected for indexing and inclusion in the National Library of Medicine's MEDLINE (Medical Literature Analysis and Retrieval System Online). The primary component of PubMed, MEDLINE is a bibliographic database containing approximately 13 million references to journal articles on medicine, nursing, dentistry, veterinary medicine, health care systems, and preclinical sciences dating to the mid‐1960s. With this approval, hospital medicine has achieved another milestone in its evolution into a new specialty.
We now hope to respond to the robust interest in clinical materials as well as to continue publication of original research. To achieve our aim of increasing the amount of clinically relevant content for practicing hospitalists, authors are encouraged to submit to JHM case reports, clinical updates, and clinical images that convey novel or underappreciated teaching points. Teaching points may be purely clinical and may focus on clinical pearls or unusual presentations of well‐known diseases, although submission of straightforward presentations of rare diseases is discouraged. Alternatively, manuscripts may involve succinct case‐based descriptions of innovations, quality improvementrelated issues, or medical errors. Submitted case reports should be less than 800 words and should contain a maximum of 5 references and no more than 1 table or figure. Case reports should not include an abstract. Submission of the case report and review type should be avoided. Instead, we seek formal clinical updates of no more than 2000 words that present important aspects of a case along with new research findings and citations from the literature that change what has historically been the standard of delivery of care. Finally, we continue to seek cases most appropriate for the Hospital Images Dx section, edited by Paul Aronowitz. They should be submitted with that designation and have fewer than 150 words. These 3 categories are identified on our Manuscript Central website (
Again, thanks to all of you for making the launch of the Journal of Hospital Medicine an unqualified success. We look forward to your continued participation as we grow as the premier journal for the specialty of hospital medicine.
P.S. Sadly, one of our superstar associate editors, Kaveh Shojania, is stepping aside, and we sincerely express thanks for his terrific contributions. We welcome suggestions for an alternative to fulfill his responsibilities.
Mortality Predictors from the CBC
The complete blood count (CBC) bundles the automated hemogram, an automated differential count of 5 types of cells, and a reflex manual differential count (when required by protocol) and is one of the most frequently ordered laboratory tests on admission to the hospital. In practice, it is a routine ingredient of all hospital admission ordersphysicians order a hemogram either alone or as part of a complete blood count for 98% of our medical/surgical admissions, and the same is true at most institutions.1 We know that the white blood cell count and hematocrit from the automated hemogram predict disease severity and mortality risk.25 For example, elevated WBC counts predict a worse prognosis in patients with cancer or coronary artery disease,6, 7 and anemia predicts increased risk of death of patients with heart failure.8, 9 Further, these two tests provide direct management guidance in common circumstances, for example, bleeding and infection.
The CBC describes the number and morphology of more than 40 cell types, from acanthocytosis to vacuolated white blood cells. Disagreement exists about the clinical significance of many of these observations.1013 And only a few components of the manual differential, for example, nucleated red blood cells (NRBCs) and lymphocytosis, have been quantitatively evaluated to determine their prognostic significance.1417 But these two observations have not been examined to determine their independent contributions to predictions of mortality when taken in conjunction with their accompanying CBC observations. Which of the numerous cell types and cell counts in the commonly ordered CBC, indicate that a patient is at high risk of death? In this article we report an inpatient study that used univariate and multivariate analyses of admission CBCs to predict 30‐day mortality in order to answer that question.
METHODS
Patients and Protocol
The institutional review board of Indiana University, Purdue University, Indianapolis, approved this study. We included in the study all adult patients (those at least 18 years old) admitted to Wishard Hospital between January 1, 1993, and December 31, 2002, except for prisoners (for IRB reasons) and obstetric patients (because their 30‐day mortality is very close to zero0.07% at our institution). Wishard Hospital is a large urban hospital that serves a diverse but predominantly inner‐city population in Indianapolis. If a patient was admitted more than once during the 10 years of observation, we included only the first admission in the analysis in order to assure statistical independence of the observations. We extracted data from the Regenstrief Medical Record System (RMRS), a comprehensive medical records system that has demographic data, vital signs, diagnoses, results of clinical tests, and pharmacy information on all inpatient, emergency department, and outpatient encounter sites.18
We obtained the admission and discharge ICD9 and DRG codes to assess the disease patterns associated with individual CBC abnormalities. We obtained these codes from routine hospital case abstractions performed by Wishard Hospital's medical records department using NCoder+ and Quadramed. Patients assigned DRG codes 370‐384 were identified as obstetric and therefore excluded. Using the ICD9 and CPT codes according to the Charlson algorithm, we calculated a Charlson Comorbidity Index value19 for each patient as a marker of coexisting conditions.
Outcomes
The primary outcome was 30‐day mortality counted from the date of admission. We used information from the hospital record (inpatient deaths) and the Indiana state death tapes to determine the dates of death of all patients. Patients were matched to the Indiana death tapes by an algorithm using name, social security number, date of birth, and sex.20
Hemogram and Differential Count Test Methods
The hemogram, differential counts, and blood smear exam results included in this study all came from Wishard Hospital's laboratory. During this study, the hospital used only 2 cell counters, the Coulter STK‐S and the Gen‐S automated blood analyzer (Beckman Coulter, Brea, California), to produce hemogram and automated blood differential counts. Both instruments provided automated differential counts of 5 cell types: neutrophils, lymphocytes, monocytes, basophils, and eosinophils. The latter machine also produced platelet counts and reticulocyte counts, but during the study period these counts were not routinely reported to physicians unless ordered specifically, so we did not include them in the analyses. The laboratory reflexively performed 100‐cell manual differential counts and blood smear exams when abnormalities as defined by College of American Pathologists (CAP) criteria were observed in the automated measures. Both automated blood analyzers used the same automated CAP criteria to decide when to add a manual differential count and blood smear analysis, and these criteria were constant throughout the study. This protocol predicts manual differential abnormalities with high sensitivity, missing less than 1% of important findings in a manual differential.21 When the CAP criteria did not require a manual differential count and blood smear exam, we assumed that those counts unique to a manual count, for example, blast cell count, were zero and that there were no abnormalities in blood smear morphology.
Laboratories may report white blood cells as absolute counts (eg, number of cells/mm3) and/or as percentages. We converted all counts reported as percentages to absolute numbers (eg, WBC count 1000 cell type percent/100). For absolute counts that have both high and low ranges, such as white blood cell (WBC) count, we constructed two binary variables. WBC‐low was 1 when the WBC was below the lower limit of normal; otherwise it was 0. WBC‐high was 1 if the WBC was above the upper limit of normal; otherwise it was 0. For continuous variables such as NRBCs or blasts where any presence on the manual differential count is abnormal, we constructed binary variables with 0 indicating absence of the cell type and 1 indicating a cell count was at least 1.
Measurements of many cell types in the manual differential count and smear assessment (eg, burr cells) are reported in qualitative terms such as occasional, few, increased, or present, if observed, or none seen, unremarkable, or no mention, if not observed. We dichotomized all such results as present or absent for analysis purposes.
Statistical Analysis
For all the original variables, we plotted cell counts against 30‐day mortality to graphically show this univariate association. To screen the effects of these 45 binary CBC variables univariately, we used each as the sole independent variable in a logistic regression model with 30‐day mortality as the dependent variable.
The simultaneous effects of the 45 CBC measures on mortality were investigated using multiple logistic regression models, always controlling for patient age (in years, as a continuous variable) and sex (as a dichotomous variable). Two approaches were taken to handle the large number of predictors in the model. First, we formed subgroups of predictors based on clinical judgment (eg, the subgroup of bands, Dohle bodies, and toxic granules associated with infections) and ran logistic regressions of each subgroup to choose the significant predictors of these subgroups to fit them into an overall prediction model of 30‐day mortality. The results were verified using a second approach that did not depend on subjective judgment. Both backward and forward stepwise variable selection procedures were used to choose the subset of significant predictors (P < .005) of 30‐day mortality in logistic regression, again controlling for age and sex. To be sure that the predictive power of the models was not decreased by converting continuous variables into categorical variables, we also ran models that included the continuous variables as potential predictors. We used the c statistic as a measure of the goodness‐of‐fit of the models. We included the Charlson Index and the 10 most common admission diagnoses in our model to control for comorbidities and prime reason for admission, respectively.
We performed the analysis using SAS software, version 8.02 (SAS Institute, Inc., Cary, NC).
Chart Review
For each independent predictor of 30‐day mortality that was both statistically significant and had a very high relative risk (>2.5), one author (A.K.) took a random sample of 100200 patients with positive values for this predictor and reviewed the dictated discharge summaries in order to asses the clinical correlates of these findings.
RESULTS
During the 10 years from January 1993 through December 2002, physicians admitted 46,522 unique eligible patients to Wishard Memorial Hospital. Each patient averaged 2 admissions during the study period, for a total of 94,582 admissions. The overall 30‐day mortality of these admissions was 3.4%. Automated hemograms (white blood cell count, hemoglobin, red cell count, and red blood cell indices) were performed on blood samples from 45,709 of these patients (98%) within one day of admission. Seventy‐seven percent (35,692) had a complete blood count that included an automated differential count plus a reflex manual count and smear when required by the CAP protocol, as well as an automated hemogram. The patients with an admission CBC with differential count had a 30‐day mortality rate of 4%, slightly higher than that of patients who had only a hemogram. The patients' mean Charlson score for the CBC with differential count was 0.83, which was lower than the national average, which is closer to 1.22 Table 1 shows the demographics of this study population.
| Characteristic | Value |
|---|---|
| Average age (years) | 46.2 17.7 |
| Average LOS (days) | 6.5 8.1 |
| Male (%) | 55.4 |
| Race | |
| White (%) | 52.9 |
| Black (%) | 43.4 |
| Other (%) | 3.7 |
| Charlson Index (mean) | 0.83 1.5 |
| Most common admission diagnoses (ICD9) | Chest pain |
| Pneumonia, organism unspecified | |
| Other symptoms involving abdomen or pelvis | |
| Unspecified heart failure | |
| Intermediate coronary syndrome | |
| Unspecified hemorrhage of GI tract | |
| Acute but ill‐defined cerebrovascular disease | |
| Diseases of pancreas | |
| Cellulitis and abscess of leg except foot | |
| Convulsions |
Predictors of 30‐Day Mortality
We examined the univariate effect of age, sex, and the 45 CBC variables (Table 2) on 30‐day mortality. Most of these variables showed a significant (P < .0001) effect on mortality. Only a few abnormalities, for example, a low WBC (< 5000/L), basophilia (>200/L), and eosinophilia (>450/L), were unrelated to 30‐day mortality. Increasing age and male sex were associated with increased mortality. Of the 45 CBC variables, 29 were strong (P < .0001) univariate predictors of mortality and had odds ratios (ORs) greater than 2.5. Eight variables had univariate ORs greater than 4: toxic granules, Dohle bodies, smudge cells, promyelocytes, myelocytes, metamyelocytes, NRBCs, and burr cells. All but 2 of these are white blood cell observations.
| Number (%) | Odds ratio | P value | |||
|---|---|---|---|---|---|
| Hemogram | Age ( 18 years) | 35,688 (100) | 1.039 | < .0001 | |
| Sex (male) | 19,788 (55.4) | 1.420 | <.0001 | ||
| WBC > 12,000 | 11,124 (31.2) | 2.049 | <.0001 | ||
| WBC < 5000 | 2176 (6.1) | 0.938 | .5765 | ||
| Hematocrit (>54) | 212 (0.6) | 2.633 | <.0001 | ||
| Hematocrit (<37) | 8687 (24.3) | 2.359 | <.0001 | ||
| MCV (>94) | 6552 (18.4) | 1.584 | <.0001 | ||
| MCV (<80) | 2815 (7.9) | 1.258 | .0121 | ||
| High RDW (>14.5) | 9478 (26.6) | 2.647 | <.0001 | ||
| High MCH (>32) | 5308 (14.9) | 1.367 | <.0001 | ||
| Low MCH (<26) | 2064 (5.8) | 1.392 | .0011 | ||
| High MCHC (>36) | 28 (0.1) | 3.964 | .0109 | ||
| Low MCHC (<32) | 738 (2.1) | 2.190 | <.0001 | ||
| Automated differential count | Neutrophilia (>7700) | 10,578 (37.8) | 1.601 | <.0001 | |
| Neutropenia (<1500) | 469 (1.3) | 2.831 | <.0001 | ||
| Basophilia (>200) | 1137 (3.2) | 1.362 | .0215 | ||
| Eosinophilia (>450) | 1529 (4.3) | 1.074 | .5788 | ||
| Monocytosis (>800) | 10,066 (28.2) | 1.262 | <.0001 | ||
| Lymphocytosis (>4000) | 3046 (8.5) | 2.495 | <.0001 | ||
| Manual differential count | Blast cells (Y/N) | 31 (0.1) | 1.638 | .5001 | |
| Myelocytes (Y/N) | 215 (0.6) | 8.231 | < .0001 | ||
| Promyelocytes (Y/N) | 25 (0.1) | 13.429 | < .0001 | ||
| Metamyeloctyes (Y/N) | 905 (2.5) | 5.798 | < .0001 | ||
| Atypical lymphocytes (Y/N) | 1303 (3.7) | 1.881 | < .0001 | ||
| Hypersegmented neutrophils (Y/N) | 141 (0.4) | 3.061 | < .0001 | ||
| Microcytes (Y/N) | 3452 (9.7) | 2.578 | < .0001 | ||
| Macrocytes (Y/N) | 3475 (9.7) | 3.282 | < .0001 | ||
| Hypochromic RBCs (Y/N) | 2252 (6.3) | 2.290 | < .0001 | ||
| Basophilic stippling (Y/N) | 273 (0.8) | 3.553 | < .0001 | ||
| Target cells (Y/N) | 1140 (3.2) | 2.866 | < .0001 | ||
| Polychromasia (Y/N) | 1675 (4.7) | 3.622 | < .0001 | ||
| Toxic granules (Y/N) | 1063 (3.0) | 4.021 | < .0001 | ||
| Dohle bodies (Y/N) | 524 (1.5) | 4.821 | < .0001 | ||
| Ovalocytes (Y/N) | 1555 (4.4) | 2.558 | < .0001 | ||
| Spherocytes (Y/N) | 465 (1.3) | 3.132 | < .0001 | ||
| Schistocytes (Y/N) | 1484 (4.2) | 3.150 | < .0001 | ||
| Sickle Cells (Y/N) | 62 (0.2) | 0.389 | .3490 | ||
| Howell‐Jolly bodies (Y/N) | 71 (0.2) | 3.025 | .0033 | ||
| Pappenheimer bodies (Y/N) | 67 (0.2) | 2.344 | .0468 | ||
| Burr cells (Y/N) | 253 (0.7) | 9.297 | <.0001 | ||
| Teardrop cells (Y/N) | 538 (1.5) | 2.150 | < .0001 | ||
| Vacuolated cells (Y/N) | 897 (2.5) | 3.667 | < .0001 | ||
| Giant platelets (Y/N) | 781 (2.2) | 3.102 | < .0001 | ||
| Smudge cells (Y/N) | 50 (0.1) | 5.237 | < .0001 | ||
| Cleaved cells (Y/N) | 8 (0.0) | 3.393 | .2533 | ||
| Band forms (Y/N) | 7594 (21.3) | 2.964 | < .0001 | ||
| NRBCs (Y/N) | 467 (1.3) | 8.756 | < .0001 |
All the statistical approaches produced essentially the same model for predicting mortality. Table 3 shows that age, sex, and 13 of the CBC variables were retained in the final model of dichotomous variables using backward and forward selection. Lymphocytosis, burr cells, and NRBCs were the greatest independent predictors of mortality, with odds ratios greater than 2.5. Only 1 variable, sickle cells, predicted reduced mortality (with an odds ratio well below 1).
| Parameter | Odds ratio | Confidence interval | P value |
|---|---|---|---|
| Age (years) | 1.040 | 1.0371.043 | < .0001 |
| Sex (male) | 1.965 | 1.7462.213 | < .0001 |
| WBC > 12,000 | 1.701 | 1.5081.919 | < .0001 |
| Hematocrit (>54) | 2.331 | 1.4383.780 | < .0006 |
| Hematocrit (<37) | 1.714 | 1.5141.941 | < .0001 |
| MCV (>94) | 1.352 | 1.1861.543 | < .0001 |
| High RDW (>14.5) | 1.463 | 1.2911.658 | < .0001 |
| Lymphocytosis (>4000) | 2.848 | 2.4353.332 | < .0001 |
| Metamyeloctye (Y/N) | 2.074 | 1.6662.581 | < .0001 |
| Macrocytes (Y/N) | 1.317 | 1.1271.539 | < .0005 |
| Toxic granules (Y/N) | 1.494 | 1.2001.859 | .0003 |
| Sickle cells (Y/N) | 0.039 | 0.0050.292 | .0016 |
| Burr cells (Y/N) | 3.254 | 2.3474.513 | < .0001 |
| Band forms (Y/N) | 1.586 | 1.3861.814 | < .0001 |
| NRBCs (Y/N) | 2.906 | 2.2403.770 | < .0001 |
The c statistic (the ratio of the area under the ROC curve to the whole area, which reflects the overall predictive power of the final model), was about 0.80 by any approach, which compared favorably with previous prediction models.3, 4 Using continuous measures of CBC in the model did not increase the predictive power. Inclusion of the Charlson Index and the top 10 admission diagnoses did not significantly change the prediction model, although 2 admission diagnoses, chest pain and acute but ill‐defined cerebrovascular disease, emerged as independent predictors of 30‐day mortality, with odds ratios of 0.314 and 2.033, respectively, at P < .0001.
Chart Review
Of the 200 cases with NRBCs, the leading probable causes for this finding were severe hypoxia (average A‐a gradient = 326 mm Hg), acute anemia (average hgb = 6.1 gm/dL), and sickle‐cell anemia. Other diseases associated with NRBCs were infection/sepsis, HIV, solid tumors (breast/lung/colon/prostate), and leukemia or multiple myeloma. Having even a single NRBC at admission correlated with a 25.5% mortality rate. Of note, 30%40% of patients with sickle‐cell disease had NRBCs and moderate anemia (hgb = 8.7 gm/dL) on admission to the hospital, but there was no excess risk of mortality. Indeed, the 49 patients with sickle‐cell disease who had NRBCs at admission had a 30‐day mortality of 0%.
Most of the patients with NRBCs reviewed exhibited overt signs of severe disease, for example, shock, respiratory failure, or severe trauma, in addition to having NRBCs. However, in 2 patients the NRBCs were the only strong signal of disease severity. Both had NRBCs on the day of discharge and were readmitted within 3 days in extremis and died. One was readmitted in fulminant septic shock, likely from a bacterial peritonitis or urinary tract infection, and the other was readmitted in shock, likely from decompensated heart failure.
In univariate analysis, burr cells at admission correlated with a mortality rate of 27.3%. A review of 100 randomly chosen patients with burr cells revealed a pattern of associated diseases, that is, acute renal failure, liver failure, and congestive heart failure, different from that of patients with NRBCs. There was little overlap in the presence of burr cells and NRBCs, but the 12% who had burr cells and NRBCs had a high mortality rate (57%).
Absolute lymphocytosis was associated with a mortality rate of 8.6%. Although univariate analysis showed that the risk with lymphocytosis was not as high as that for patients with NRBCs or burr cells at admission, lymphocytosis was much more common (8.5%), and within the logistic model its presence explained more of the chi‐square statistic than any other variable except age. Indeed, lymphocytosis was a stronger predictor of 30‐day mortality than was high WBCs or anemia. Chart review of 200 patients with lymphocytosis showed a preponderance of them had large physiologic stressors, for example, traumatic tissue injury (surgery) or cerebrovascular injury. In one subset, half the patients (50.9% of 53 patients) who underwent craniotomy for trauma and had absolute lymphocytosis at admission died, compared with 20.8% of 101 patients admitted for the same diagnosis without absolute lymphocytosis.
DISCUSSION
Some investigators have incorporated selected CBC measures, for example, white blood cell count and hemoglobin/hematocrit, into multivariable models that predict mortality or rehospitalizations.6, 7, 9, 23 However, CBC reports can include a spectrum of more than 40 distinct counts and morphologic findings. Our study was the first to take into account all the different variables in the complete blood count and differential to determine elements that independently predict a high risk of mortality.
In addition to age and sex, our multivariable analysis of the 45 CBC variables found 13 independent predictors of mortality. Five were observations about white blood cells: absolute leukocytosis, high band form cell count, the presence of metamyelocytes, the presence of toxic granules, and absolute lymphocytosis. Eight were observations about red blood cells: high hematocrit, low hematocrit, high MCV and the presence of macrocytes, high red cell distribution width, the presence of NRBCs, the presence of burr cells, and the presence of sickle cells. Because controlling for severity of illness by Charlson comorbidity scores did not significantly change the model, the CBC abnormalities among the predictors of mortality did not simply reflect how sick the patients were. Including the 10 most common admission diagnoses did not significantly attenuate our reported odds ratios, suggesting the CBC predictors did not merely reflect the primary reason for admission. Interestingly, however, admission for chest pain did correlate with a greatly reduced risk of 30‐day mortality, which may reflect the low threshold that physicians have for admitting patients with this complaint. Admission for acute but ill‐defined cerebrovascular disease independently predicted a 2‐fold increased risk of 30‐day mortality.
What is the message to physicians from this analysis? Physicians commonly order CBCs and may rely on quick heuristics to sift through the myriad findings in CBC reports. Our analysis focuses physician attention on high‐impact findings in the CBC. We assume that physicians already consider low hematocrit, high hematocrit (a sign of fluid loss and/or chronic hypoxia), high WBC count, high band cell count, and the presence of metamyeloctes (left shift) as important prognostic indicators. These abnormal findings are routinely mentioned at morning report and in a physician's notes.
Physicians, however, may not appreciate the importance of other CBC findings that our analysis found are predictive of mortality. Macrocytosis and a high RDW count (indicating an abnormally wide distribution of red blood cell size) have not previously been reported as predictors of mortality. And although other studies have suggested that bands are not predictors of mortality,11 our study found they were an important prognostic indicator, with an OR =1.59, approaching those of leukocytosis and anemia.
The most impressive predictors of mortality were burr cells, NRBCs, and absolute lymphocytosis. The multivariate ORs of these 3, ranging from 2.8 to 3.2, were the highest of any CBC finding. In univariate analysis, the first 2 were associated with mortality rates 8 to 10 times higher than that of the average admitted patient. There are anecdotal reports in the literature of burr cells being associated with ominous prognoses2426 and more robust statistical analyses showing NRBCs to be associated with increased mortality.14 Lymphocytosis has also been reported as a mortality risk in patients with trauma and emergency medical conditions.15, 16 Our analysis has shown that, indeed, all 3 of these findings are strong independent predictors of mortality.
The presence of sickle cells was also a strong predictor, but of decreased mortality. Patients with sickle cells in their smear had a risk of death one third that of patients without sickle cells. This does not indicate a protective effect. Rather, patients with sickle‐cell disease typically are young and admitted for pain control and other non‐life‐threatening conditions. The presence of NRBCs in patients with sickle‐cell disease appears to be intrinsic to the disease itself and did not have the same implications for mortality as it did for other patients in our study.
The overall logistic model including age, sex, and admission CBC variables had a respectable c statistic for predicting 30‐day mortality of 0.80. This compares well with findings in other multivariable models. For example, the APACHE II score used to predict the mortality of hospitalized critical care patients has a c statistic that ranges from 0.78 to 0.86.3, 27, 28 The APACHE score uses the worst value from the first 2 days after admission for some of its predictors so it cannot provide as early a warning as the admission CBC, and it requires collection of significantly more data. The inclusion of more CBC findings in the APACHE model might increase its predictive accuracy.
Our multivariate analysis was based on a very large number of patient samples using data collected through routine clinical care. However, our study has a number of limitations. The analysis was done at only a single institution, and the exact logistic regression model may not apply to other institutions that have different case mixes and laboratory procedures. Our institution's reported 30‐day mortality rate of 3.4% was lower than the 4.6%11.9% reported in studies of patients admitted to general ward services,2931 but this may be accounted for by the lower‐than‐average Charlson comorbidity scores in our study population. Our risk adjustment by Charlson comorbidity scores may not be as precise as a risk adjustment tailored for our particular institution.32 Our 30‐day mortality rate was calculated using state death tapes, which means we would have missed patients who died outside the state, although we believe this rarely happens. We developed predictive equations on the basis of 30‐day mortality, so we cannot comment on whether the CBC elements predict mortality beyond 30 days. We analyzed most variables as either high or low or as present or absent. Increasing degrees of abnormality may further increase the predictive power of some variables. Finally, the CBC is only one of many tests and clinical findings; it may be that some of these other variables would displace some CBC variables and/or improve the overall predictive power at the time the admission laboratory tests were performed. In this initial study, we have described the prognostic implication of the CBC across a wide range of diagnoses. Future work will focus on the predictive power of commonly gathered variables in more specific conditions (eg, low white blood cell count in sepsis).
Physicians generally have an intuitive ability to identify patients who are seriously ill and at high risk of dying33 and adjust their diagnostic and therapeutic efforts accordingly. Our analysis highlights the value that certain observations in the CBC, notably burr cells, NRBCs, and absolute lymphocytosis, add to physicians' assessments of mortality risk. Even after adjustment for age, sex, comorbidities, common admission diagnoses, and other variables in the CBC, the presence of these findings predicted a 3‐fold increase in 30‐day mortality. Identifying the red flags within this ubiquitously performed test can make the difference in premature discharge or inappropriate triage of patients. Busy physicians can choose from a wide selection of ever‐improving diagnostic tests, yet the workhorse CBC can serve as a simple and early identifier of patients with a poor prognosis.
- ,.The complete blood count and leukocyte differential count.Ann Intern Med.1987;106:65–74.
- ,.Prognostic significance of marked leukocytosis in hospitalized patients.J Gen Intern Med.1991;6:199–203.
- ,,, et al.The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults.Chest.1991;100:1619–1636.
- ,,,.APACHE II: a severity of disease classification system.Crit Care Med.1985;13:818–829.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,.Prognostic importance of the white blood cell count for coronary, cancer, and all‐cause mortality.JAMA.1985;254:1932–1937.
- ,,,.White blood cell count as a predictor of mortality: results over 18 years from the Normative Aging Study.J Clin Epidemiol.1990;43:153–157.
- ,,,,.Nucleated red blood cells in congestive heart failure.Circulation.1959;20:367–370.
- ,,.Anemia predicts mortality in severe heart failure: the prospective randomized amlodipine survival evaluation (PRAISE).J Am Coll Cardiol.2003;41:1933–1939.
- ,,.Band neutrophil counts are unnecessary for the diagnosis of infection in patients with normal total leukocyte counts.Am J Clin Pathol.1994;102:646–649.
- ,.The lack of clinical utility of white blood cell differential counts and blood morphology in elderly individuals with normal hematology profiles.Arch Pathol Lab Med.1990;114:394–398.
- ,,,.The clinical utility of the leucocyte differential in emergency medicine.Am J Clin Pathol.1986;86:298–303.
- ,,,,.Manual differential cell counts help predict bacterial infection.Am J Clin Pathol.2001;115:644–649.
- ,.Significance of nucleated red blood cells in peripheral blood; analysis of 1,496 cases.JAMA.1954;154:1339–1340.
- ,,,.Nucleated red blood cells indicate high risk of in‐hospital mortality.J Lab Clin Med.2002;140:407–412.
- ,,.Transient atypical lymphocytosis in patients with emergency medical conditions.Arch Pathol Lab Med.1987;111:712–714.
- ,,,.Acute lymphocytosis after trauma—early recognition of the high‐risk patient?J Trauma.1989;29:749–751.
- ,,, et al.The Regenstrief Medical Record System: a quarter century experience.Int J Med Inf.1999;54:225–253.
- ,,,.Validation of a combined comorbidity index.J Clin Epidemiol.1994;47:1245–1251.
- ,,.Real world performance of approximate string comparators for use in patient matching.Medinfo.2004;11(Pt1):43–47.
- ,,,,.Preliminary evaluation of the new hematology analyzer COULTER GEN‐S in a university hospital.Clin Chem Lab Med.1999;37:681–686.
- ,,.Differences in length of stay in veterans health administration and other united states hospitals: is the gap closing?Med Care.2003;41:882–894.
- ,,,,.The Prognostic importance of anemia in patients with heart failure.Am J Med.2003;114:112–119.
- ,.The diagnostic significance of “burr” red blood cells.Am J Med Sci.1949;218:563.
- .The “burr” red cell and azotemia.J Clin Pathol.1957;10:252–257.
- .The origin of ‘burr’ erythrocytes.Br J Haematol.1963;9:552–555.
- ,,,.The added value that increasing levels of diagnostic information provide in prognostic models to estimate hospital mortality for adult intensive care patients.Intern Care Med.2000;26:577–584.
- ,,,,.Evaluating the yield of medical tests.JAMA.1982;247:2543–2546.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medical service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Hospital care by hospital‐based and clinic‐based faculty. a prospective, controlled trial.Arch Intern Med.2001;161:235–241.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,,.Severity‐adjusted mortality and length of stay in teaching and nonteaching hospitals: results of a regional study.JAMA.1997;278:485–490.
- ,.How well can physicians estimate mortality in a medical intensive care unit?Med Decis Mak.1989;9:125–132.
The complete blood count (CBC) bundles the automated hemogram, an automated differential count of 5 types of cells, and a reflex manual differential count (when required by protocol) and is one of the most frequently ordered laboratory tests on admission to the hospital. In practice, it is a routine ingredient of all hospital admission ordersphysicians order a hemogram either alone or as part of a complete blood count for 98% of our medical/surgical admissions, and the same is true at most institutions.1 We know that the white blood cell count and hematocrit from the automated hemogram predict disease severity and mortality risk.25 For example, elevated WBC counts predict a worse prognosis in patients with cancer or coronary artery disease,6, 7 and anemia predicts increased risk of death of patients with heart failure.8, 9 Further, these two tests provide direct management guidance in common circumstances, for example, bleeding and infection.
The CBC describes the number and morphology of more than 40 cell types, from acanthocytosis to vacuolated white blood cells. Disagreement exists about the clinical significance of many of these observations.1013 And only a few components of the manual differential, for example, nucleated red blood cells (NRBCs) and lymphocytosis, have been quantitatively evaluated to determine their prognostic significance.1417 But these two observations have not been examined to determine their independent contributions to predictions of mortality when taken in conjunction with their accompanying CBC observations. Which of the numerous cell types and cell counts in the commonly ordered CBC, indicate that a patient is at high risk of death? In this article we report an inpatient study that used univariate and multivariate analyses of admission CBCs to predict 30‐day mortality in order to answer that question.
METHODS
Patients and Protocol
The institutional review board of Indiana University, Purdue University, Indianapolis, approved this study. We included in the study all adult patients (those at least 18 years old) admitted to Wishard Hospital between January 1, 1993, and December 31, 2002, except for prisoners (for IRB reasons) and obstetric patients (because their 30‐day mortality is very close to zero0.07% at our institution). Wishard Hospital is a large urban hospital that serves a diverse but predominantly inner‐city population in Indianapolis. If a patient was admitted more than once during the 10 years of observation, we included only the first admission in the analysis in order to assure statistical independence of the observations. We extracted data from the Regenstrief Medical Record System (RMRS), a comprehensive medical records system that has demographic data, vital signs, diagnoses, results of clinical tests, and pharmacy information on all inpatient, emergency department, and outpatient encounter sites.18
We obtained the admission and discharge ICD9 and DRG codes to assess the disease patterns associated with individual CBC abnormalities. We obtained these codes from routine hospital case abstractions performed by Wishard Hospital's medical records department using NCoder+ and Quadramed. Patients assigned DRG codes 370‐384 were identified as obstetric and therefore excluded. Using the ICD9 and CPT codes according to the Charlson algorithm, we calculated a Charlson Comorbidity Index value19 for each patient as a marker of coexisting conditions.
Outcomes
The primary outcome was 30‐day mortality counted from the date of admission. We used information from the hospital record (inpatient deaths) and the Indiana state death tapes to determine the dates of death of all patients. Patients were matched to the Indiana death tapes by an algorithm using name, social security number, date of birth, and sex.20
Hemogram and Differential Count Test Methods
The hemogram, differential counts, and blood smear exam results included in this study all came from Wishard Hospital's laboratory. During this study, the hospital used only 2 cell counters, the Coulter STK‐S and the Gen‐S automated blood analyzer (Beckman Coulter, Brea, California), to produce hemogram and automated blood differential counts. Both instruments provided automated differential counts of 5 cell types: neutrophils, lymphocytes, monocytes, basophils, and eosinophils. The latter machine also produced platelet counts and reticulocyte counts, but during the study period these counts were not routinely reported to physicians unless ordered specifically, so we did not include them in the analyses. The laboratory reflexively performed 100‐cell manual differential counts and blood smear exams when abnormalities as defined by College of American Pathologists (CAP) criteria were observed in the automated measures. Both automated blood analyzers used the same automated CAP criteria to decide when to add a manual differential count and blood smear analysis, and these criteria were constant throughout the study. This protocol predicts manual differential abnormalities with high sensitivity, missing less than 1% of important findings in a manual differential.21 When the CAP criteria did not require a manual differential count and blood smear exam, we assumed that those counts unique to a manual count, for example, blast cell count, were zero and that there were no abnormalities in blood smear morphology.
Laboratories may report white blood cells as absolute counts (eg, number of cells/mm3) and/or as percentages. We converted all counts reported as percentages to absolute numbers (eg, WBC count 1000 cell type percent/100). For absolute counts that have both high and low ranges, such as white blood cell (WBC) count, we constructed two binary variables. WBC‐low was 1 when the WBC was below the lower limit of normal; otherwise it was 0. WBC‐high was 1 if the WBC was above the upper limit of normal; otherwise it was 0. For continuous variables such as NRBCs or blasts where any presence on the manual differential count is abnormal, we constructed binary variables with 0 indicating absence of the cell type and 1 indicating a cell count was at least 1.
Measurements of many cell types in the manual differential count and smear assessment (eg, burr cells) are reported in qualitative terms such as occasional, few, increased, or present, if observed, or none seen, unremarkable, or no mention, if not observed. We dichotomized all such results as present or absent for analysis purposes.
Statistical Analysis
For all the original variables, we plotted cell counts against 30‐day mortality to graphically show this univariate association. To screen the effects of these 45 binary CBC variables univariately, we used each as the sole independent variable in a logistic regression model with 30‐day mortality as the dependent variable.
The simultaneous effects of the 45 CBC measures on mortality were investigated using multiple logistic regression models, always controlling for patient age (in years, as a continuous variable) and sex (as a dichotomous variable). Two approaches were taken to handle the large number of predictors in the model. First, we formed subgroups of predictors based on clinical judgment (eg, the subgroup of bands, Dohle bodies, and toxic granules associated with infections) and ran logistic regressions of each subgroup to choose the significant predictors of these subgroups to fit them into an overall prediction model of 30‐day mortality. The results were verified using a second approach that did not depend on subjective judgment. Both backward and forward stepwise variable selection procedures were used to choose the subset of significant predictors (P < .005) of 30‐day mortality in logistic regression, again controlling for age and sex. To be sure that the predictive power of the models was not decreased by converting continuous variables into categorical variables, we also ran models that included the continuous variables as potential predictors. We used the c statistic as a measure of the goodness‐of‐fit of the models. We included the Charlson Index and the 10 most common admission diagnoses in our model to control for comorbidities and prime reason for admission, respectively.
We performed the analysis using SAS software, version 8.02 (SAS Institute, Inc., Cary, NC).
Chart Review
For each independent predictor of 30‐day mortality that was both statistically significant and had a very high relative risk (>2.5), one author (A.K.) took a random sample of 100200 patients with positive values for this predictor and reviewed the dictated discharge summaries in order to asses the clinical correlates of these findings.
RESULTS
During the 10 years from January 1993 through December 2002, physicians admitted 46,522 unique eligible patients to Wishard Memorial Hospital. Each patient averaged 2 admissions during the study period, for a total of 94,582 admissions. The overall 30‐day mortality of these admissions was 3.4%. Automated hemograms (white blood cell count, hemoglobin, red cell count, and red blood cell indices) were performed on blood samples from 45,709 of these patients (98%) within one day of admission. Seventy‐seven percent (35,692) had a complete blood count that included an automated differential count plus a reflex manual count and smear when required by the CAP protocol, as well as an automated hemogram. The patients with an admission CBC with differential count had a 30‐day mortality rate of 4%, slightly higher than that of patients who had only a hemogram. The patients' mean Charlson score for the CBC with differential count was 0.83, which was lower than the national average, which is closer to 1.22 Table 1 shows the demographics of this study population.
| Characteristic | Value |
|---|---|
| Average age (years) | 46.2 17.7 |
| Average LOS (days) | 6.5 8.1 |
| Male (%) | 55.4 |
| Race | |
| White (%) | 52.9 |
| Black (%) | 43.4 |
| Other (%) | 3.7 |
| Charlson Index (mean) | 0.83 1.5 |
| Most common admission diagnoses (ICD9) | Chest pain |
| Pneumonia, organism unspecified | |
| Other symptoms involving abdomen or pelvis | |
| Unspecified heart failure | |
| Intermediate coronary syndrome | |
| Unspecified hemorrhage of GI tract | |
| Acute but ill‐defined cerebrovascular disease | |
| Diseases of pancreas | |
| Cellulitis and abscess of leg except foot | |
| Convulsions |
Predictors of 30‐Day Mortality
We examined the univariate effect of age, sex, and the 45 CBC variables (Table 2) on 30‐day mortality. Most of these variables showed a significant (P < .0001) effect on mortality. Only a few abnormalities, for example, a low WBC (< 5000/L), basophilia (>200/L), and eosinophilia (>450/L), were unrelated to 30‐day mortality. Increasing age and male sex were associated with increased mortality. Of the 45 CBC variables, 29 were strong (P < .0001) univariate predictors of mortality and had odds ratios (ORs) greater than 2.5. Eight variables had univariate ORs greater than 4: toxic granules, Dohle bodies, smudge cells, promyelocytes, myelocytes, metamyelocytes, NRBCs, and burr cells. All but 2 of these are white blood cell observations.
| Number (%) | Odds ratio | P value | |||
|---|---|---|---|---|---|
| Hemogram | Age ( 18 years) | 35,688 (100) | 1.039 | < .0001 | |
| Sex (male) | 19,788 (55.4) | 1.420 | <.0001 | ||
| WBC > 12,000 | 11,124 (31.2) | 2.049 | <.0001 | ||
| WBC < 5000 | 2176 (6.1) | 0.938 | .5765 | ||
| Hematocrit (>54) | 212 (0.6) | 2.633 | <.0001 | ||
| Hematocrit (<37) | 8687 (24.3) | 2.359 | <.0001 | ||
| MCV (>94) | 6552 (18.4) | 1.584 | <.0001 | ||
| MCV (<80) | 2815 (7.9) | 1.258 | .0121 | ||
| High RDW (>14.5) | 9478 (26.6) | 2.647 | <.0001 | ||
| High MCH (>32) | 5308 (14.9) | 1.367 | <.0001 | ||
| Low MCH (<26) | 2064 (5.8) | 1.392 | .0011 | ||
| High MCHC (>36) | 28 (0.1) | 3.964 | .0109 | ||
| Low MCHC (<32) | 738 (2.1) | 2.190 | <.0001 | ||
| Automated differential count | Neutrophilia (>7700) | 10,578 (37.8) | 1.601 | <.0001 | |
| Neutropenia (<1500) | 469 (1.3) | 2.831 | <.0001 | ||
| Basophilia (>200) | 1137 (3.2) | 1.362 | .0215 | ||
| Eosinophilia (>450) | 1529 (4.3) | 1.074 | .5788 | ||
| Monocytosis (>800) | 10,066 (28.2) | 1.262 | <.0001 | ||
| Lymphocytosis (>4000) | 3046 (8.5) | 2.495 | <.0001 | ||
| Manual differential count | Blast cells (Y/N) | 31 (0.1) | 1.638 | .5001 | |
| Myelocytes (Y/N) | 215 (0.6) | 8.231 | < .0001 | ||
| Promyelocytes (Y/N) | 25 (0.1) | 13.429 | < .0001 | ||
| Metamyeloctyes (Y/N) | 905 (2.5) | 5.798 | < .0001 | ||
| Atypical lymphocytes (Y/N) | 1303 (3.7) | 1.881 | < .0001 | ||
| Hypersegmented neutrophils (Y/N) | 141 (0.4) | 3.061 | < .0001 | ||
| Microcytes (Y/N) | 3452 (9.7) | 2.578 | < .0001 | ||
| Macrocytes (Y/N) | 3475 (9.7) | 3.282 | < .0001 | ||
| Hypochromic RBCs (Y/N) | 2252 (6.3) | 2.290 | < .0001 | ||
| Basophilic stippling (Y/N) | 273 (0.8) | 3.553 | < .0001 | ||
| Target cells (Y/N) | 1140 (3.2) | 2.866 | < .0001 | ||
| Polychromasia (Y/N) | 1675 (4.7) | 3.622 | < .0001 | ||
| Toxic granules (Y/N) | 1063 (3.0) | 4.021 | < .0001 | ||
| Dohle bodies (Y/N) | 524 (1.5) | 4.821 | < .0001 | ||
| Ovalocytes (Y/N) | 1555 (4.4) | 2.558 | < .0001 | ||
| Spherocytes (Y/N) | 465 (1.3) | 3.132 | < .0001 | ||
| Schistocytes (Y/N) | 1484 (4.2) | 3.150 | < .0001 | ||
| Sickle Cells (Y/N) | 62 (0.2) | 0.389 | .3490 | ||
| Howell‐Jolly bodies (Y/N) | 71 (0.2) | 3.025 | .0033 | ||
| Pappenheimer bodies (Y/N) | 67 (0.2) | 2.344 | .0468 | ||
| Burr cells (Y/N) | 253 (0.7) | 9.297 | <.0001 | ||
| Teardrop cells (Y/N) | 538 (1.5) | 2.150 | < .0001 | ||
| Vacuolated cells (Y/N) | 897 (2.5) | 3.667 | < .0001 | ||
| Giant platelets (Y/N) | 781 (2.2) | 3.102 | < .0001 | ||
| Smudge cells (Y/N) | 50 (0.1) | 5.237 | < .0001 | ||
| Cleaved cells (Y/N) | 8 (0.0) | 3.393 | .2533 | ||
| Band forms (Y/N) | 7594 (21.3) | 2.964 | < .0001 | ||
| NRBCs (Y/N) | 467 (1.3) | 8.756 | < .0001 |
All the statistical approaches produced essentially the same model for predicting mortality. Table 3 shows that age, sex, and 13 of the CBC variables were retained in the final model of dichotomous variables using backward and forward selection. Lymphocytosis, burr cells, and NRBCs were the greatest independent predictors of mortality, with odds ratios greater than 2.5. Only 1 variable, sickle cells, predicted reduced mortality (with an odds ratio well below 1).
| Parameter | Odds ratio | Confidence interval | P value |
|---|---|---|---|
| Age (years) | 1.040 | 1.0371.043 | < .0001 |
| Sex (male) | 1.965 | 1.7462.213 | < .0001 |
| WBC > 12,000 | 1.701 | 1.5081.919 | < .0001 |
| Hematocrit (>54) | 2.331 | 1.4383.780 | < .0006 |
| Hematocrit (<37) | 1.714 | 1.5141.941 | < .0001 |
| MCV (>94) | 1.352 | 1.1861.543 | < .0001 |
| High RDW (>14.5) | 1.463 | 1.2911.658 | < .0001 |
| Lymphocytosis (>4000) | 2.848 | 2.4353.332 | < .0001 |
| Metamyeloctye (Y/N) | 2.074 | 1.6662.581 | < .0001 |
| Macrocytes (Y/N) | 1.317 | 1.1271.539 | < .0005 |
| Toxic granules (Y/N) | 1.494 | 1.2001.859 | .0003 |
| Sickle cells (Y/N) | 0.039 | 0.0050.292 | .0016 |
| Burr cells (Y/N) | 3.254 | 2.3474.513 | < .0001 |
| Band forms (Y/N) | 1.586 | 1.3861.814 | < .0001 |
| NRBCs (Y/N) | 2.906 | 2.2403.770 | < .0001 |
The c statistic (the ratio of the area under the ROC curve to the whole area, which reflects the overall predictive power of the final model), was about 0.80 by any approach, which compared favorably with previous prediction models.3, 4 Using continuous measures of CBC in the model did not increase the predictive power. Inclusion of the Charlson Index and the top 10 admission diagnoses did not significantly change the prediction model, although 2 admission diagnoses, chest pain and acute but ill‐defined cerebrovascular disease, emerged as independent predictors of 30‐day mortality, with odds ratios of 0.314 and 2.033, respectively, at P < .0001.
Chart Review
Of the 200 cases with NRBCs, the leading probable causes for this finding were severe hypoxia (average A‐a gradient = 326 mm Hg), acute anemia (average hgb = 6.1 gm/dL), and sickle‐cell anemia. Other diseases associated with NRBCs were infection/sepsis, HIV, solid tumors (breast/lung/colon/prostate), and leukemia or multiple myeloma. Having even a single NRBC at admission correlated with a 25.5% mortality rate. Of note, 30%40% of patients with sickle‐cell disease had NRBCs and moderate anemia (hgb = 8.7 gm/dL) on admission to the hospital, but there was no excess risk of mortality. Indeed, the 49 patients with sickle‐cell disease who had NRBCs at admission had a 30‐day mortality of 0%.
Most of the patients with NRBCs reviewed exhibited overt signs of severe disease, for example, shock, respiratory failure, or severe trauma, in addition to having NRBCs. However, in 2 patients the NRBCs were the only strong signal of disease severity. Both had NRBCs on the day of discharge and were readmitted within 3 days in extremis and died. One was readmitted in fulminant septic shock, likely from a bacterial peritonitis or urinary tract infection, and the other was readmitted in shock, likely from decompensated heart failure.
In univariate analysis, burr cells at admission correlated with a mortality rate of 27.3%. A review of 100 randomly chosen patients with burr cells revealed a pattern of associated diseases, that is, acute renal failure, liver failure, and congestive heart failure, different from that of patients with NRBCs. There was little overlap in the presence of burr cells and NRBCs, but the 12% who had burr cells and NRBCs had a high mortality rate (57%).
Absolute lymphocytosis was associated with a mortality rate of 8.6%. Although univariate analysis showed that the risk with lymphocytosis was not as high as that for patients with NRBCs or burr cells at admission, lymphocytosis was much more common (8.5%), and within the logistic model its presence explained more of the chi‐square statistic than any other variable except age. Indeed, lymphocytosis was a stronger predictor of 30‐day mortality than was high WBCs or anemia. Chart review of 200 patients with lymphocytosis showed a preponderance of them had large physiologic stressors, for example, traumatic tissue injury (surgery) or cerebrovascular injury. In one subset, half the patients (50.9% of 53 patients) who underwent craniotomy for trauma and had absolute lymphocytosis at admission died, compared with 20.8% of 101 patients admitted for the same diagnosis without absolute lymphocytosis.
DISCUSSION
Some investigators have incorporated selected CBC measures, for example, white blood cell count and hemoglobin/hematocrit, into multivariable models that predict mortality or rehospitalizations.6, 7, 9, 23 However, CBC reports can include a spectrum of more than 40 distinct counts and morphologic findings. Our study was the first to take into account all the different variables in the complete blood count and differential to determine elements that independently predict a high risk of mortality.
In addition to age and sex, our multivariable analysis of the 45 CBC variables found 13 independent predictors of mortality. Five were observations about white blood cells: absolute leukocytosis, high band form cell count, the presence of metamyelocytes, the presence of toxic granules, and absolute lymphocytosis. Eight were observations about red blood cells: high hematocrit, low hematocrit, high MCV and the presence of macrocytes, high red cell distribution width, the presence of NRBCs, the presence of burr cells, and the presence of sickle cells. Because controlling for severity of illness by Charlson comorbidity scores did not significantly change the model, the CBC abnormalities among the predictors of mortality did not simply reflect how sick the patients were. Including the 10 most common admission diagnoses did not significantly attenuate our reported odds ratios, suggesting the CBC predictors did not merely reflect the primary reason for admission. Interestingly, however, admission for chest pain did correlate with a greatly reduced risk of 30‐day mortality, which may reflect the low threshold that physicians have for admitting patients with this complaint. Admission for acute but ill‐defined cerebrovascular disease independently predicted a 2‐fold increased risk of 30‐day mortality.
What is the message to physicians from this analysis? Physicians commonly order CBCs and may rely on quick heuristics to sift through the myriad findings in CBC reports. Our analysis focuses physician attention on high‐impact findings in the CBC. We assume that physicians already consider low hematocrit, high hematocrit (a sign of fluid loss and/or chronic hypoxia), high WBC count, high band cell count, and the presence of metamyeloctes (left shift) as important prognostic indicators. These abnormal findings are routinely mentioned at morning report and in a physician's notes.
Physicians, however, may not appreciate the importance of other CBC findings that our analysis found are predictive of mortality. Macrocytosis and a high RDW count (indicating an abnormally wide distribution of red blood cell size) have not previously been reported as predictors of mortality. And although other studies have suggested that bands are not predictors of mortality,11 our study found they were an important prognostic indicator, with an OR =1.59, approaching those of leukocytosis and anemia.
The most impressive predictors of mortality were burr cells, NRBCs, and absolute lymphocytosis. The multivariate ORs of these 3, ranging from 2.8 to 3.2, were the highest of any CBC finding. In univariate analysis, the first 2 were associated with mortality rates 8 to 10 times higher than that of the average admitted patient. There are anecdotal reports in the literature of burr cells being associated with ominous prognoses2426 and more robust statistical analyses showing NRBCs to be associated with increased mortality.14 Lymphocytosis has also been reported as a mortality risk in patients with trauma and emergency medical conditions.15, 16 Our analysis has shown that, indeed, all 3 of these findings are strong independent predictors of mortality.
The presence of sickle cells was also a strong predictor, but of decreased mortality. Patients with sickle cells in their smear had a risk of death one third that of patients without sickle cells. This does not indicate a protective effect. Rather, patients with sickle‐cell disease typically are young and admitted for pain control and other non‐life‐threatening conditions. The presence of NRBCs in patients with sickle‐cell disease appears to be intrinsic to the disease itself and did not have the same implications for mortality as it did for other patients in our study.
The overall logistic model including age, sex, and admission CBC variables had a respectable c statistic for predicting 30‐day mortality of 0.80. This compares well with findings in other multivariable models. For example, the APACHE II score used to predict the mortality of hospitalized critical care patients has a c statistic that ranges from 0.78 to 0.86.3, 27, 28 The APACHE score uses the worst value from the first 2 days after admission for some of its predictors so it cannot provide as early a warning as the admission CBC, and it requires collection of significantly more data. The inclusion of more CBC findings in the APACHE model might increase its predictive accuracy.
Our multivariate analysis was based on a very large number of patient samples using data collected through routine clinical care. However, our study has a number of limitations. The analysis was done at only a single institution, and the exact logistic regression model may not apply to other institutions that have different case mixes and laboratory procedures. Our institution's reported 30‐day mortality rate of 3.4% was lower than the 4.6%11.9% reported in studies of patients admitted to general ward services,2931 but this may be accounted for by the lower‐than‐average Charlson comorbidity scores in our study population. Our risk adjustment by Charlson comorbidity scores may not be as precise as a risk adjustment tailored for our particular institution.32 Our 30‐day mortality rate was calculated using state death tapes, which means we would have missed patients who died outside the state, although we believe this rarely happens. We developed predictive equations on the basis of 30‐day mortality, so we cannot comment on whether the CBC elements predict mortality beyond 30 days. We analyzed most variables as either high or low or as present or absent. Increasing degrees of abnormality may further increase the predictive power of some variables. Finally, the CBC is only one of many tests and clinical findings; it may be that some of these other variables would displace some CBC variables and/or improve the overall predictive power at the time the admission laboratory tests were performed. In this initial study, we have described the prognostic implication of the CBC across a wide range of diagnoses. Future work will focus on the predictive power of commonly gathered variables in more specific conditions (eg, low white blood cell count in sepsis).
Physicians generally have an intuitive ability to identify patients who are seriously ill and at high risk of dying33 and adjust their diagnostic and therapeutic efforts accordingly. Our analysis highlights the value that certain observations in the CBC, notably burr cells, NRBCs, and absolute lymphocytosis, add to physicians' assessments of mortality risk. Even after adjustment for age, sex, comorbidities, common admission diagnoses, and other variables in the CBC, the presence of these findings predicted a 3‐fold increase in 30‐day mortality. Identifying the red flags within this ubiquitously performed test can make the difference in premature discharge or inappropriate triage of patients. Busy physicians can choose from a wide selection of ever‐improving diagnostic tests, yet the workhorse CBC can serve as a simple and early identifier of patients with a poor prognosis.
The complete blood count (CBC) bundles the automated hemogram, an automated differential count of 5 types of cells, and a reflex manual differential count (when required by protocol) and is one of the most frequently ordered laboratory tests on admission to the hospital. In practice, it is a routine ingredient of all hospital admission ordersphysicians order a hemogram either alone or as part of a complete blood count for 98% of our medical/surgical admissions, and the same is true at most institutions.1 We know that the white blood cell count and hematocrit from the automated hemogram predict disease severity and mortality risk.25 For example, elevated WBC counts predict a worse prognosis in patients with cancer or coronary artery disease,6, 7 and anemia predicts increased risk of death of patients with heart failure.8, 9 Further, these two tests provide direct management guidance in common circumstances, for example, bleeding and infection.
The CBC describes the number and morphology of more than 40 cell types, from acanthocytosis to vacuolated white blood cells. Disagreement exists about the clinical significance of many of these observations.1013 And only a few components of the manual differential, for example, nucleated red blood cells (NRBCs) and lymphocytosis, have been quantitatively evaluated to determine their prognostic significance.1417 But these two observations have not been examined to determine their independent contributions to predictions of mortality when taken in conjunction with their accompanying CBC observations. Which of the numerous cell types and cell counts in the commonly ordered CBC, indicate that a patient is at high risk of death? In this article we report an inpatient study that used univariate and multivariate analyses of admission CBCs to predict 30‐day mortality in order to answer that question.
METHODS
Patients and Protocol
The institutional review board of Indiana University, Purdue University, Indianapolis, approved this study. We included in the study all adult patients (those at least 18 years old) admitted to Wishard Hospital between January 1, 1993, and December 31, 2002, except for prisoners (for IRB reasons) and obstetric patients (because their 30‐day mortality is very close to zero0.07% at our institution). Wishard Hospital is a large urban hospital that serves a diverse but predominantly inner‐city population in Indianapolis. If a patient was admitted more than once during the 10 years of observation, we included only the first admission in the analysis in order to assure statistical independence of the observations. We extracted data from the Regenstrief Medical Record System (RMRS), a comprehensive medical records system that has demographic data, vital signs, diagnoses, results of clinical tests, and pharmacy information on all inpatient, emergency department, and outpatient encounter sites.18
We obtained the admission and discharge ICD9 and DRG codes to assess the disease patterns associated with individual CBC abnormalities. We obtained these codes from routine hospital case abstractions performed by Wishard Hospital's medical records department using NCoder+ and Quadramed. Patients assigned DRG codes 370‐384 were identified as obstetric and therefore excluded. Using the ICD9 and CPT codes according to the Charlson algorithm, we calculated a Charlson Comorbidity Index value19 for each patient as a marker of coexisting conditions.
Outcomes
The primary outcome was 30‐day mortality counted from the date of admission. We used information from the hospital record (inpatient deaths) and the Indiana state death tapes to determine the dates of death of all patients. Patients were matched to the Indiana death tapes by an algorithm using name, social security number, date of birth, and sex.20
Hemogram and Differential Count Test Methods
The hemogram, differential counts, and blood smear exam results included in this study all came from Wishard Hospital's laboratory. During this study, the hospital used only 2 cell counters, the Coulter STK‐S and the Gen‐S automated blood analyzer (Beckman Coulter, Brea, California), to produce hemogram and automated blood differential counts. Both instruments provided automated differential counts of 5 cell types: neutrophils, lymphocytes, monocytes, basophils, and eosinophils. The latter machine also produced platelet counts and reticulocyte counts, but during the study period these counts were not routinely reported to physicians unless ordered specifically, so we did not include them in the analyses. The laboratory reflexively performed 100‐cell manual differential counts and blood smear exams when abnormalities as defined by College of American Pathologists (CAP) criteria were observed in the automated measures. Both automated blood analyzers used the same automated CAP criteria to decide when to add a manual differential count and blood smear analysis, and these criteria were constant throughout the study. This protocol predicts manual differential abnormalities with high sensitivity, missing less than 1% of important findings in a manual differential.21 When the CAP criteria did not require a manual differential count and blood smear exam, we assumed that those counts unique to a manual count, for example, blast cell count, were zero and that there were no abnormalities in blood smear morphology.
Laboratories may report white blood cells as absolute counts (eg, number of cells/mm3) and/or as percentages. We converted all counts reported as percentages to absolute numbers (eg, WBC count 1000 cell type percent/100). For absolute counts that have both high and low ranges, such as white blood cell (WBC) count, we constructed two binary variables. WBC‐low was 1 when the WBC was below the lower limit of normal; otherwise it was 0. WBC‐high was 1 if the WBC was above the upper limit of normal; otherwise it was 0. For continuous variables such as NRBCs or blasts where any presence on the manual differential count is abnormal, we constructed binary variables with 0 indicating absence of the cell type and 1 indicating a cell count was at least 1.
Measurements of many cell types in the manual differential count and smear assessment (eg, burr cells) are reported in qualitative terms such as occasional, few, increased, or present, if observed, or none seen, unremarkable, or no mention, if not observed. We dichotomized all such results as present or absent for analysis purposes.
Statistical Analysis
For all the original variables, we plotted cell counts against 30‐day mortality to graphically show this univariate association. To screen the effects of these 45 binary CBC variables univariately, we used each as the sole independent variable in a logistic regression model with 30‐day mortality as the dependent variable.
The simultaneous effects of the 45 CBC measures on mortality were investigated using multiple logistic regression models, always controlling for patient age (in years, as a continuous variable) and sex (as a dichotomous variable). Two approaches were taken to handle the large number of predictors in the model. First, we formed subgroups of predictors based on clinical judgment (eg, the subgroup of bands, Dohle bodies, and toxic granules associated with infections) and ran logistic regressions of each subgroup to choose the significant predictors of these subgroups to fit them into an overall prediction model of 30‐day mortality. The results were verified using a second approach that did not depend on subjective judgment. Both backward and forward stepwise variable selection procedures were used to choose the subset of significant predictors (P < .005) of 30‐day mortality in logistic regression, again controlling for age and sex. To be sure that the predictive power of the models was not decreased by converting continuous variables into categorical variables, we also ran models that included the continuous variables as potential predictors. We used the c statistic as a measure of the goodness‐of‐fit of the models. We included the Charlson Index and the 10 most common admission diagnoses in our model to control for comorbidities and prime reason for admission, respectively.
We performed the analysis using SAS software, version 8.02 (SAS Institute, Inc., Cary, NC).
Chart Review
For each independent predictor of 30‐day mortality that was both statistically significant and had a very high relative risk (>2.5), one author (A.K.) took a random sample of 100200 patients with positive values for this predictor and reviewed the dictated discharge summaries in order to asses the clinical correlates of these findings.
RESULTS
During the 10 years from January 1993 through December 2002, physicians admitted 46,522 unique eligible patients to Wishard Memorial Hospital. Each patient averaged 2 admissions during the study period, for a total of 94,582 admissions. The overall 30‐day mortality of these admissions was 3.4%. Automated hemograms (white blood cell count, hemoglobin, red cell count, and red blood cell indices) were performed on blood samples from 45,709 of these patients (98%) within one day of admission. Seventy‐seven percent (35,692) had a complete blood count that included an automated differential count plus a reflex manual count and smear when required by the CAP protocol, as well as an automated hemogram. The patients with an admission CBC with differential count had a 30‐day mortality rate of 4%, slightly higher than that of patients who had only a hemogram. The patients' mean Charlson score for the CBC with differential count was 0.83, which was lower than the national average, which is closer to 1.22 Table 1 shows the demographics of this study population.
| Characteristic | Value |
|---|---|
| Average age (years) | 46.2 17.7 |
| Average LOS (days) | 6.5 8.1 |
| Male (%) | 55.4 |
| Race | |
| White (%) | 52.9 |
| Black (%) | 43.4 |
| Other (%) | 3.7 |
| Charlson Index (mean) | 0.83 1.5 |
| Most common admission diagnoses (ICD9) | Chest pain |
| Pneumonia, organism unspecified | |
| Other symptoms involving abdomen or pelvis | |
| Unspecified heart failure | |
| Intermediate coronary syndrome | |
| Unspecified hemorrhage of GI tract | |
| Acute but ill‐defined cerebrovascular disease | |
| Diseases of pancreas | |
| Cellulitis and abscess of leg except foot | |
| Convulsions |
Predictors of 30‐Day Mortality
We examined the univariate effect of age, sex, and the 45 CBC variables (Table 2) on 30‐day mortality. Most of these variables showed a significant (P < .0001) effect on mortality. Only a few abnormalities, for example, a low WBC (< 5000/L), basophilia (>200/L), and eosinophilia (>450/L), were unrelated to 30‐day mortality. Increasing age and male sex were associated with increased mortality. Of the 45 CBC variables, 29 were strong (P < .0001) univariate predictors of mortality and had odds ratios (ORs) greater than 2.5. Eight variables had univariate ORs greater than 4: toxic granules, Dohle bodies, smudge cells, promyelocytes, myelocytes, metamyelocytes, NRBCs, and burr cells. All but 2 of these are white blood cell observations.
| Number (%) | Odds ratio | P value | |||
|---|---|---|---|---|---|
| Hemogram | Age ( 18 years) | 35,688 (100) | 1.039 | < .0001 | |
| Sex (male) | 19,788 (55.4) | 1.420 | <.0001 | ||
| WBC > 12,000 | 11,124 (31.2) | 2.049 | <.0001 | ||
| WBC < 5000 | 2176 (6.1) | 0.938 | .5765 | ||
| Hematocrit (>54) | 212 (0.6) | 2.633 | <.0001 | ||
| Hematocrit (<37) | 8687 (24.3) | 2.359 | <.0001 | ||
| MCV (>94) | 6552 (18.4) | 1.584 | <.0001 | ||
| MCV (<80) | 2815 (7.9) | 1.258 | .0121 | ||
| High RDW (>14.5) | 9478 (26.6) | 2.647 | <.0001 | ||
| High MCH (>32) | 5308 (14.9) | 1.367 | <.0001 | ||
| Low MCH (<26) | 2064 (5.8) | 1.392 | .0011 | ||
| High MCHC (>36) | 28 (0.1) | 3.964 | .0109 | ||
| Low MCHC (<32) | 738 (2.1) | 2.190 | <.0001 | ||
| Automated differential count | Neutrophilia (>7700) | 10,578 (37.8) | 1.601 | <.0001 | |
| Neutropenia (<1500) | 469 (1.3) | 2.831 | <.0001 | ||
| Basophilia (>200) | 1137 (3.2) | 1.362 | .0215 | ||
| Eosinophilia (>450) | 1529 (4.3) | 1.074 | .5788 | ||
| Monocytosis (>800) | 10,066 (28.2) | 1.262 | <.0001 | ||
| Lymphocytosis (>4000) | 3046 (8.5) | 2.495 | <.0001 | ||
| Manual differential count | Blast cells (Y/N) | 31 (0.1) | 1.638 | .5001 | |
| Myelocytes (Y/N) | 215 (0.6) | 8.231 | < .0001 | ||
| Promyelocytes (Y/N) | 25 (0.1) | 13.429 | < .0001 | ||
| Metamyeloctyes (Y/N) | 905 (2.5) | 5.798 | < .0001 | ||
| Atypical lymphocytes (Y/N) | 1303 (3.7) | 1.881 | < .0001 | ||
| Hypersegmented neutrophils (Y/N) | 141 (0.4) | 3.061 | < .0001 | ||
| Microcytes (Y/N) | 3452 (9.7) | 2.578 | < .0001 | ||
| Macrocytes (Y/N) | 3475 (9.7) | 3.282 | < .0001 | ||
| Hypochromic RBCs (Y/N) | 2252 (6.3) | 2.290 | < .0001 | ||
| Basophilic stippling (Y/N) | 273 (0.8) | 3.553 | < .0001 | ||
| Target cells (Y/N) | 1140 (3.2) | 2.866 | < .0001 | ||
| Polychromasia (Y/N) | 1675 (4.7) | 3.622 | < .0001 | ||
| Toxic granules (Y/N) | 1063 (3.0) | 4.021 | < .0001 | ||
| Dohle bodies (Y/N) | 524 (1.5) | 4.821 | < .0001 | ||
| Ovalocytes (Y/N) | 1555 (4.4) | 2.558 | < .0001 | ||
| Spherocytes (Y/N) | 465 (1.3) | 3.132 | < .0001 | ||
| Schistocytes (Y/N) | 1484 (4.2) | 3.150 | < .0001 | ||
| Sickle Cells (Y/N) | 62 (0.2) | 0.389 | .3490 | ||
| Howell‐Jolly bodies (Y/N) | 71 (0.2) | 3.025 | .0033 | ||
| Pappenheimer bodies (Y/N) | 67 (0.2) | 2.344 | .0468 | ||
| Burr cells (Y/N) | 253 (0.7) | 9.297 | <.0001 | ||
| Teardrop cells (Y/N) | 538 (1.5) | 2.150 | < .0001 | ||
| Vacuolated cells (Y/N) | 897 (2.5) | 3.667 | < .0001 | ||
| Giant platelets (Y/N) | 781 (2.2) | 3.102 | < .0001 | ||
| Smudge cells (Y/N) | 50 (0.1) | 5.237 | < .0001 | ||
| Cleaved cells (Y/N) | 8 (0.0) | 3.393 | .2533 | ||
| Band forms (Y/N) | 7594 (21.3) | 2.964 | < .0001 | ||
| NRBCs (Y/N) | 467 (1.3) | 8.756 | < .0001 |
All the statistical approaches produced essentially the same model for predicting mortality. Table 3 shows that age, sex, and 13 of the CBC variables were retained in the final model of dichotomous variables using backward and forward selection. Lymphocytosis, burr cells, and NRBCs were the greatest independent predictors of mortality, with odds ratios greater than 2.5. Only 1 variable, sickle cells, predicted reduced mortality (with an odds ratio well below 1).
| Parameter | Odds ratio | Confidence interval | P value |
|---|---|---|---|
| Age (years) | 1.040 | 1.0371.043 | < .0001 |
| Sex (male) | 1.965 | 1.7462.213 | < .0001 |
| WBC > 12,000 | 1.701 | 1.5081.919 | < .0001 |
| Hematocrit (>54) | 2.331 | 1.4383.780 | < .0006 |
| Hematocrit (<37) | 1.714 | 1.5141.941 | < .0001 |
| MCV (>94) | 1.352 | 1.1861.543 | < .0001 |
| High RDW (>14.5) | 1.463 | 1.2911.658 | < .0001 |
| Lymphocytosis (>4000) | 2.848 | 2.4353.332 | < .0001 |
| Metamyeloctye (Y/N) | 2.074 | 1.6662.581 | < .0001 |
| Macrocytes (Y/N) | 1.317 | 1.1271.539 | < .0005 |
| Toxic granules (Y/N) | 1.494 | 1.2001.859 | .0003 |
| Sickle cells (Y/N) | 0.039 | 0.0050.292 | .0016 |
| Burr cells (Y/N) | 3.254 | 2.3474.513 | < .0001 |
| Band forms (Y/N) | 1.586 | 1.3861.814 | < .0001 |
| NRBCs (Y/N) | 2.906 | 2.2403.770 | < .0001 |
The c statistic (the ratio of the area under the ROC curve to the whole area, which reflects the overall predictive power of the final model), was about 0.80 by any approach, which compared favorably with previous prediction models.3, 4 Using continuous measures of CBC in the model did not increase the predictive power. Inclusion of the Charlson Index and the top 10 admission diagnoses did not significantly change the prediction model, although 2 admission diagnoses, chest pain and acute but ill‐defined cerebrovascular disease, emerged as independent predictors of 30‐day mortality, with odds ratios of 0.314 and 2.033, respectively, at P < .0001.
Chart Review
Of the 200 cases with NRBCs, the leading probable causes for this finding were severe hypoxia (average A‐a gradient = 326 mm Hg), acute anemia (average hgb = 6.1 gm/dL), and sickle‐cell anemia. Other diseases associated with NRBCs were infection/sepsis, HIV, solid tumors (breast/lung/colon/prostate), and leukemia or multiple myeloma. Having even a single NRBC at admission correlated with a 25.5% mortality rate. Of note, 30%40% of patients with sickle‐cell disease had NRBCs and moderate anemia (hgb = 8.7 gm/dL) on admission to the hospital, but there was no excess risk of mortality. Indeed, the 49 patients with sickle‐cell disease who had NRBCs at admission had a 30‐day mortality of 0%.
Most of the patients with NRBCs reviewed exhibited overt signs of severe disease, for example, shock, respiratory failure, or severe trauma, in addition to having NRBCs. However, in 2 patients the NRBCs were the only strong signal of disease severity. Both had NRBCs on the day of discharge and were readmitted within 3 days in extremis and died. One was readmitted in fulminant septic shock, likely from a bacterial peritonitis or urinary tract infection, and the other was readmitted in shock, likely from decompensated heart failure.
In univariate analysis, burr cells at admission correlated with a mortality rate of 27.3%. A review of 100 randomly chosen patients with burr cells revealed a pattern of associated diseases, that is, acute renal failure, liver failure, and congestive heart failure, different from that of patients with NRBCs. There was little overlap in the presence of burr cells and NRBCs, but the 12% who had burr cells and NRBCs had a high mortality rate (57%).
Absolute lymphocytosis was associated with a mortality rate of 8.6%. Although univariate analysis showed that the risk with lymphocytosis was not as high as that for patients with NRBCs or burr cells at admission, lymphocytosis was much more common (8.5%), and within the logistic model its presence explained more of the chi‐square statistic than any other variable except age. Indeed, lymphocytosis was a stronger predictor of 30‐day mortality than was high WBCs or anemia. Chart review of 200 patients with lymphocytosis showed a preponderance of them had large physiologic stressors, for example, traumatic tissue injury (surgery) or cerebrovascular injury. In one subset, half the patients (50.9% of 53 patients) who underwent craniotomy for trauma and had absolute lymphocytosis at admission died, compared with 20.8% of 101 patients admitted for the same diagnosis without absolute lymphocytosis.
DISCUSSION
Some investigators have incorporated selected CBC measures, for example, white blood cell count and hemoglobin/hematocrit, into multivariable models that predict mortality or rehospitalizations.6, 7, 9, 23 However, CBC reports can include a spectrum of more than 40 distinct counts and morphologic findings. Our study was the first to take into account all the different variables in the complete blood count and differential to determine elements that independently predict a high risk of mortality.
In addition to age and sex, our multivariable analysis of the 45 CBC variables found 13 independent predictors of mortality. Five were observations about white blood cells: absolute leukocytosis, high band form cell count, the presence of metamyelocytes, the presence of toxic granules, and absolute lymphocytosis. Eight were observations about red blood cells: high hematocrit, low hematocrit, high MCV and the presence of macrocytes, high red cell distribution width, the presence of NRBCs, the presence of burr cells, and the presence of sickle cells. Because controlling for severity of illness by Charlson comorbidity scores did not significantly change the model, the CBC abnormalities among the predictors of mortality did not simply reflect how sick the patients were. Including the 10 most common admission diagnoses did not significantly attenuate our reported odds ratios, suggesting the CBC predictors did not merely reflect the primary reason for admission. Interestingly, however, admission for chest pain did correlate with a greatly reduced risk of 30‐day mortality, which may reflect the low threshold that physicians have for admitting patients with this complaint. Admission for acute but ill‐defined cerebrovascular disease independently predicted a 2‐fold increased risk of 30‐day mortality.
What is the message to physicians from this analysis? Physicians commonly order CBCs and may rely on quick heuristics to sift through the myriad findings in CBC reports. Our analysis focuses physician attention on high‐impact findings in the CBC. We assume that physicians already consider low hematocrit, high hematocrit (a sign of fluid loss and/or chronic hypoxia), high WBC count, high band cell count, and the presence of metamyeloctes (left shift) as important prognostic indicators. These abnormal findings are routinely mentioned at morning report and in a physician's notes.
Physicians, however, may not appreciate the importance of other CBC findings that our analysis found are predictive of mortality. Macrocytosis and a high RDW count (indicating an abnormally wide distribution of red blood cell size) have not previously been reported as predictors of mortality. And although other studies have suggested that bands are not predictors of mortality,11 our study found they were an important prognostic indicator, with an OR =1.59, approaching those of leukocytosis and anemia.
The most impressive predictors of mortality were burr cells, NRBCs, and absolute lymphocytosis. The multivariate ORs of these 3, ranging from 2.8 to 3.2, were the highest of any CBC finding. In univariate analysis, the first 2 were associated with mortality rates 8 to 10 times higher than that of the average admitted patient. There are anecdotal reports in the literature of burr cells being associated with ominous prognoses2426 and more robust statistical analyses showing NRBCs to be associated with increased mortality.14 Lymphocytosis has also been reported as a mortality risk in patients with trauma and emergency medical conditions.15, 16 Our analysis has shown that, indeed, all 3 of these findings are strong independent predictors of mortality.
The presence of sickle cells was also a strong predictor, but of decreased mortality. Patients with sickle cells in their smear had a risk of death one third that of patients without sickle cells. This does not indicate a protective effect. Rather, patients with sickle‐cell disease typically are young and admitted for pain control and other non‐life‐threatening conditions. The presence of NRBCs in patients with sickle‐cell disease appears to be intrinsic to the disease itself and did not have the same implications for mortality as it did for other patients in our study.
The overall logistic model including age, sex, and admission CBC variables had a respectable c statistic for predicting 30‐day mortality of 0.80. This compares well with findings in other multivariable models. For example, the APACHE II score used to predict the mortality of hospitalized critical care patients has a c statistic that ranges from 0.78 to 0.86.3, 27, 28 The APACHE score uses the worst value from the first 2 days after admission for some of its predictors so it cannot provide as early a warning as the admission CBC, and it requires collection of significantly more data. The inclusion of more CBC findings in the APACHE model might increase its predictive accuracy.
Our multivariate analysis was based on a very large number of patient samples using data collected through routine clinical care. However, our study has a number of limitations. The analysis was done at only a single institution, and the exact logistic regression model may not apply to other institutions that have different case mixes and laboratory procedures. Our institution's reported 30‐day mortality rate of 3.4% was lower than the 4.6%11.9% reported in studies of patients admitted to general ward services,2931 but this may be accounted for by the lower‐than‐average Charlson comorbidity scores in our study population. Our risk adjustment by Charlson comorbidity scores may not be as precise as a risk adjustment tailored for our particular institution.32 Our 30‐day mortality rate was calculated using state death tapes, which means we would have missed patients who died outside the state, although we believe this rarely happens. We developed predictive equations on the basis of 30‐day mortality, so we cannot comment on whether the CBC elements predict mortality beyond 30 days. We analyzed most variables as either high or low or as present or absent. Increasing degrees of abnormality may further increase the predictive power of some variables. Finally, the CBC is only one of many tests and clinical findings; it may be that some of these other variables would displace some CBC variables and/or improve the overall predictive power at the time the admission laboratory tests were performed. In this initial study, we have described the prognostic implication of the CBC across a wide range of diagnoses. Future work will focus on the predictive power of commonly gathered variables in more specific conditions (eg, low white blood cell count in sepsis).
Physicians generally have an intuitive ability to identify patients who are seriously ill and at high risk of dying33 and adjust their diagnostic and therapeutic efforts accordingly. Our analysis highlights the value that certain observations in the CBC, notably burr cells, NRBCs, and absolute lymphocytosis, add to physicians' assessments of mortality risk. Even after adjustment for age, sex, comorbidities, common admission diagnoses, and other variables in the CBC, the presence of these findings predicted a 3‐fold increase in 30‐day mortality. Identifying the red flags within this ubiquitously performed test can make the difference in premature discharge or inappropriate triage of patients. Busy physicians can choose from a wide selection of ever‐improving diagnostic tests, yet the workhorse CBC can serve as a simple and early identifier of patients with a poor prognosis.
- ,.The complete blood count and leukocyte differential count.Ann Intern Med.1987;106:65–74.
- ,.Prognostic significance of marked leukocytosis in hospitalized patients.J Gen Intern Med.1991;6:199–203.
- ,,, et al.The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults.Chest.1991;100:1619–1636.
- ,,,.APACHE II: a severity of disease classification system.Crit Care Med.1985;13:818–829.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,.Prognostic importance of the white blood cell count for coronary, cancer, and all‐cause mortality.JAMA.1985;254:1932–1937.
- ,,,.White blood cell count as a predictor of mortality: results over 18 years from the Normative Aging Study.J Clin Epidemiol.1990;43:153–157.
- ,,,,.Nucleated red blood cells in congestive heart failure.Circulation.1959;20:367–370.
- ,,.Anemia predicts mortality in severe heart failure: the prospective randomized amlodipine survival evaluation (PRAISE).J Am Coll Cardiol.2003;41:1933–1939.
- ,,.Band neutrophil counts are unnecessary for the diagnosis of infection in patients with normal total leukocyte counts.Am J Clin Pathol.1994;102:646–649.
- ,.The lack of clinical utility of white blood cell differential counts and blood morphology in elderly individuals with normal hematology profiles.Arch Pathol Lab Med.1990;114:394–398.
- ,,,.The clinical utility of the leucocyte differential in emergency medicine.Am J Clin Pathol.1986;86:298–303.
- ,,,,.Manual differential cell counts help predict bacterial infection.Am J Clin Pathol.2001;115:644–649.
- ,.Significance of nucleated red blood cells in peripheral blood; analysis of 1,496 cases.JAMA.1954;154:1339–1340.
- ,,,.Nucleated red blood cells indicate high risk of in‐hospital mortality.J Lab Clin Med.2002;140:407–412.
- ,,.Transient atypical lymphocytosis in patients with emergency medical conditions.Arch Pathol Lab Med.1987;111:712–714.
- ,,,.Acute lymphocytosis after trauma—early recognition of the high‐risk patient?J Trauma.1989;29:749–751.
- ,,, et al.The Regenstrief Medical Record System: a quarter century experience.Int J Med Inf.1999;54:225–253.
- ,,,.Validation of a combined comorbidity index.J Clin Epidemiol.1994;47:1245–1251.
- ,,.Real world performance of approximate string comparators for use in patient matching.Medinfo.2004;11(Pt1):43–47.
- ,,,,.Preliminary evaluation of the new hematology analyzer COULTER GEN‐S in a university hospital.Clin Chem Lab Med.1999;37:681–686.
- ,,.Differences in length of stay in veterans health administration and other united states hospitals: is the gap closing?Med Care.2003;41:882–894.
- ,,,,.The Prognostic importance of anemia in patients with heart failure.Am J Med.2003;114:112–119.
- ,.The diagnostic significance of “burr” red blood cells.Am J Med Sci.1949;218:563.
- .The “burr” red cell and azotemia.J Clin Pathol.1957;10:252–257.
- .The origin of ‘burr’ erythrocytes.Br J Haematol.1963;9:552–555.
- ,,,.The added value that increasing levels of diagnostic information provide in prognostic models to estimate hospital mortality for adult intensive care patients.Intern Care Med.2000;26:577–584.
- ,,,,.Evaluating the yield of medical tests.JAMA.1982;247:2543–2546.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medical service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Hospital care by hospital‐based and clinic‐based faculty. a prospective, controlled trial.Arch Intern Med.2001;161:235–241.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,,.Severity‐adjusted mortality and length of stay in teaching and nonteaching hospitals: results of a regional study.JAMA.1997;278:485–490.
- ,.How well can physicians estimate mortality in a medical intensive care unit?Med Decis Mak.1989;9:125–132.
- ,.The complete blood count and leukocyte differential count.Ann Intern Med.1987;106:65–74.
- ,.Prognostic significance of marked leukocytosis in hospitalized patients.J Gen Intern Med.1991;6:199–203.
- ,,, et al.The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults.Chest.1991;100:1619–1636.
- ,,,.APACHE II: a severity of disease classification system.Crit Care Med.1985;13:818–829.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,.Prognostic importance of the white blood cell count for coronary, cancer, and all‐cause mortality.JAMA.1985;254:1932–1937.
- ,,,.White blood cell count as a predictor of mortality: results over 18 years from the Normative Aging Study.J Clin Epidemiol.1990;43:153–157.
- ,,,,.Nucleated red blood cells in congestive heart failure.Circulation.1959;20:367–370.
- ,,.Anemia predicts mortality in severe heart failure: the prospective randomized amlodipine survival evaluation (PRAISE).J Am Coll Cardiol.2003;41:1933–1939.
- ,,.Band neutrophil counts are unnecessary for the diagnosis of infection in patients with normal total leukocyte counts.Am J Clin Pathol.1994;102:646–649.
- ,.The lack of clinical utility of white blood cell differential counts and blood morphology in elderly individuals with normal hematology profiles.Arch Pathol Lab Med.1990;114:394–398.
- ,,,.The clinical utility of the leucocyte differential in emergency medicine.Am J Clin Pathol.1986;86:298–303.
- ,,,,.Manual differential cell counts help predict bacterial infection.Am J Clin Pathol.2001;115:644–649.
- ,.Significance of nucleated red blood cells in peripheral blood; analysis of 1,496 cases.JAMA.1954;154:1339–1340.
- ,,,.Nucleated red blood cells indicate high risk of in‐hospital mortality.J Lab Clin Med.2002;140:407–412.
- ,,.Transient atypical lymphocytosis in patients with emergency medical conditions.Arch Pathol Lab Med.1987;111:712–714.
- ,,,.Acute lymphocytosis after trauma—early recognition of the high‐risk patient?J Trauma.1989;29:749–751.
- ,,, et al.The Regenstrief Medical Record System: a quarter century experience.Int J Med Inf.1999;54:225–253.
- ,,,.Validation of a combined comorbidity index.J Clin Epidemiol.1994;47:1245–1251.
- ,,.Real world performance of approximate string comparators for use in patient matching.Medinfo.2004;11(Pt1):43–47.
- ,,,,.Preliminary evaluation of the new hematology analyzer COULTER GEN‐S in a university hospital.Clin Chem Lab Med.1999;37:681–686.
- ,,.Differences in length of stay in veterans health administration and other united states hospitals: is the gap closing?Med Care.2003;41:882–894.
- ,,,,.The Prognostic importance of anemia in patients with heart failure.Am J Med.2003;114:112–119.
- ,.The diagnostic significance of “burr” red blood cells.Am J Med Sci.1949;218:563.
- .The “burr” red cell and azotemia.J Clin Pathol.1957;10:252–257.
- .The origin of ‘burr’ erythrocytes.Br J Haematol.1963;9:552–555.
- ,,,.The added value that increasing levels of diagnostic information provide in prognostic models to estimate hospital mortality for adult intensive care patients.Intern Care Med.2000;26:577–584.
- ,,,,.Evaluating the yield of medical tests.JAMA.1982;247:2543–2546.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medical service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Hospital care by hospital‐based and clinic‐based faculty. a prospective, controlled trial.Arch Intern Med.2001;161:235–241.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,,.Severity‐adjusted mortality and length of stay in teaching and nonteaching hospitals: results of a regional study.JAMA.1997;278:485–490.
- ,.How well can physicians estimate mortality in a medical intensive care unit?Med Decis Mak.1989;9:125–132.
Copyright © 2007 Society of Hospital Medicine
The Effect of Fexofenadine Hydrochloride on Productivity and Quality of Life in Patients With Chronic Idiopathic Urticaria
Lentigo Maligna (Melanoma In Situ) Treated With Imiquimod Cream 5%: 12 Case Reports
Classic and Atypical Spitz Nevi: Review of the Literature
Spitz nevi were first described in 1948.1 Spitz1 originally called these lesions benign juvenile melanoma. She was able to identify and describe a separate class of benign melanocytic neoplasms in children that were previously diagnosed and treated as melanoma.2 Prior to this discovery, the standard of care was to remove all suspicious pigmented lesions in children prior to adulthood to prevent possible malignant transformation.2,3 Today, Spitz nevus is the more commonly used term for benign juvenile melanoma because it is encountered occasionally in adults and the term melanoma carries a negative connotation.4 Other synonyms include juvenile melanoma, Spitz tumor, nevus of large spindle and/or epithelioid cells, and spindle cell and epithelioid nevus.3,5
Classic Spitz Nevus
Spitz nevi are uncommon. The approximate incidence is 7 per 100,000 people. Spitz nevi are more frequently found in children and adolescents but can occur in adults.6,7 Spitz nevi occur predominantly in the white population and slightly more often in females.4,8
A Spitz nevus can arise de novo or in association with an existing melanocytic nevus. The lesions can be asymptomatic or have a history of rapid but limited growth. Clinical features of Spitz nevi are well-circumscribed, symmetrical, small- to medium-sized firm papules with smooth discrete borders and a uniform color (typically pink or flesh colored).9 Spitz nevi can occur in various shapes. In a study of 211 cases of Spitz nevi, 19% were described as flat or uneven, 24% as polypoid, and 57% as plateau or elevated.7 Spitz nevi usually are found on the face, neck, or lower extremities but can occur anywhere on the body.7,9 Size is typically less than 6 mm (Figures 1 and 2).
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
The classic Spitz nevus histologically consists of large spindle and/or epithelioid melanocytes arrayed as epidermal nests grouped in a vertical orientation (called "bunches of bananas" or "raining down pattern"), with clefting artifact at the perimeter (Figure 3).4,9,10 The nests are fairly uniform, nonconfluent, and evenly spaced. There is little or no pagetoid spread pattern. Epidermal changes include acanthosis, hypergranulosis, and hyperkeratosis. The intradermal pattern displays maturation, with single-file or single-unit arrays descending to the base. Eosinophilic Kamino bodies frequently are found along the dermoepidermal interface. Kamino bodies are globular clusters that represent apoptotic degenerative melanocytes (Figure 4). They stain positive with both periodic acid-Schiff and trichrome stains. At the dermal base, there is no mitosis, no pushing deep margins, and lack of significant pleomorphism. Little or no melanin is present.4,9,10 The classic Spitz nevus behaves in a benign manner.1 The differential diagnosis of the Spitz nevus includes pyogenic granuloma, mastocytoma, juvenile xanthogranuloma, and malignant melanoma.
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
Atypical Spitz Nevus
The atypical Spitz nevus is difficult to formally define. Instead, it is loosely defined. An atypical Spitz nevus shares histologic features with the classic Spitz nevus, but it may have one or more atypical features, which can be characteristic of malignancy.10-12 Gross atypical features may include irregular shape, nonuniform color, large size, or ulcerations. Histologically, there can be one or more of the following features: pleomorphism; increased cellularity; loss of cellular cohesion; epidermal pagetoid spread; minimal epidermal changes; absence of Kamino bodies; lack of maturation in the intradermal pattern; high-grade nuclear atypia; high basal mitotic rate; pushing deep margins into the dermal base or subcutis; and nests variable in size, shape, and orientation.9,10,13
The behavior of any atypical Spitz nevus is unpredictable. There are case reports of metastasizing and malignant lesions with Spitz-like characteristics causing fatal outcomes.11,13 However, there also are studies that show Spitz nevi acting in a benign manner, even with a history of metastases.11,13-15 Some researchers try to explain this phenomenon by theorizing that Spitz nevi and melanoma exist along a continuum with the classic benign Spitz nevus at one end of the spectrum and the aggressive malignant melanoma at the opposite end, with a diverse range of atypical Spitz-like lesions with features of both in between.4,10-12,14 Other researchers refute this claim and view the unequivocal Spitz nevus as benign and unrelated to melanoma. They point out that many of these case reports of melanomas with Spitz-like features do not fit the diagnosis of the Spitz nevus.16
In general, the more features an atypical Spitz nevus shares with melanoma, the greater the risk for malignant behavior. In 1999, Spatz et al12 proposed formal and specific criteria for determining the risk for malignant behavior in atypical Spitz nevi in children. In the retrospective study, atypical features were used to define atypical Spitz nevi and grade their risk for metastasis. The 5 major factors were age, size, presence of ulceration, involvement of subcutaneous fat, and mitotic activity. Positive risk factors that increased the grade included age greater than 10 years, diameter greater than 10.0 mm, lesions with fat involvement, presence of ulceration, and dermal component mitotic activity greater than 5 mitoses/mm2. The higher the grade, the higher the risk for malignancy and metastasis.12 Since its publication, this grading system for categorizing atypical Spitz nevi has been put to use in a few case reports and studies.17,18 Additional prospective studies using these criteria will be helpful in determining the true clinical nature of atypical Spitz nevi in children, the usefulness of this grading system, and the possible application of this grading system in adults.
Problems Differentiating Classic and Atypical Spitz Nevi From Melanoma
Melanoma is a major part of the differential diagnosis of Spitz nevi. The classic Spitz nevus typically has a benign nature, while the atypical Spitz nevus displays unpredictable behavior that appears to be dependent on the degree of atypia.1,3,16 In contrast, melanoma is potentially fatal. Fortunately, Spitz nevi typically occur in children and the risk for having childhood melanoma is rare.6,8,19 Though risk is minimal, rare cases of melanoma have been reported in children.8,11,14,15,19-21 Therefore, making a correct diagnosis and ruling out melanoma is important.
Unfortunately, even with clinical and histologic guidelines, sometimes it is difficult to distinguish classic and atypical Spitz nevi from melanoma. The major problem is histologic overlap with Spitz nevi and melanoma. Many researchers have emphasized that there is no single discriminating factor for Spitz nevi and melanoma because virtually every trait of Spitz nevi has been described in melanoma.2,10,13,20,22,23 Results of multiple studies show variability among researchers on the analysis of melanocytic nevi and melanoma lesions, and the final diagnosis was subjective.5,22 In one retrospective study where clinical outcome was already known, 30 melanocytic lesions were evaluated independently by a panel of 10 dermatopathologists and categorized as either a typical Spitz nevus, atypical Spitz nevus, melanoma, tumor with unknown biologic potential, or other melanocytic lesion.5 The dermatopathologists were blinded to the clinical data. Evaluation of 17 Spitzoid lesions yielded no clear diagnostic consensus and a few lethal lesions were identified by most dermatopathologists as either typical or atypical Spitz nevi. The authors maintain that these results show that current objective criteria are deficient and inadequate to permit the discrimination of Spitz nevi with atypical features from melanoma.5
Given these histologic analysis limitations, many investigators are researching other tools and techniques that may help enhance diagnostic accuracy. Promising genetic analysis techniques include comparative genomic hybridization and fluorescent in situ hybridization.24 In one study,24 researchers compared Spitz nevi with primary cutaneous melanomas using comparative genomic hybridization and fluorescent in situ hybridization and discovered differences. In the study, Spitz nevi were found to have no chromosomal aberrations or gains in chromosome 11p or 7q21qter. In comparison, primary cutaneous melanomas had frequent chromosome deletions of chromosomes 9p, 10q, 6q, and 8p, and gains of chromosomes 7, 8, 6p, and 1q.24,25 Immunohistochemistry is another potential tool for improving diagnostic accuracy. Examples of promising immunohistochemical markers include antibody MIB-1,26-28 BCL-2,29 and anti-S100A6.30 Studies have shown that most melanomas are immunoreactive to MIB-1 and BCL-2, whereas Spitz nevi are not.26-29 Recently, anti-S100A6 protein also was shown to be a potential immunohistochemical marker to differentiate a Spitz nevus from melanoma.30 Anti-S100A6 is different from anti-S100 because it is more specific to a subclass of normal cell types and certain cancer cell lines. Investigators found strong, uniform, and diffuse S100A6 protein expression in the junctional and dermal components of all 42 Spitz nevi they studied versus weak and patchy S100A6 protein expression found mainly in the dermal component of 35 of 105 melanoma specimens they studied.30 Although these techniques show exceptional potential, further research will be required to prove their reliability.
Management of Classic and Atypical Spitz Nevi
There is controversy regarding the treatment of a classic Spitz nevus. Some investigators recommend conservative treatment because a Spitz nevus is benign. They find that the Spitz nevus may be removed or left alone.3 Others agree but would add that complete excision with clinical follow-up is appropriate if there are atypical features found on the Spitz nevus.16,23,31 Other investigators are more aggressive and recommend complete excision with clear margins of all Spitz nevi, unequivocal or not, because Spitz nevi have histologic overlap with melanoma, and recurrent lesions may present with pseudomelanomatous changes, which makes differentiation more difficult later.4,32 They conclude that the benefits of complete excision outweigh the risks of partial treatment.4 Regardless of how a Spitz nevus case is managed, regular follow-up with a dermatologist is recommended to look for any changes or recurrences suggestive of malignancy.
Currently, there are no available evidence-based recommendations with predictive value for the specific management of atypical Spitz nevi because their clinical course is mostly unknown and unpredictable. Most articles that do address the management of atypical Spitz nevi state that they should be completely excised and followed periodically.11,33 Murphy et al34 suggest that an atypical Spitz nevus should be completely excised to avoid the rare possibility of a melanoma masquerading as an atypical Spitz nevus. Furthermore, if the physician is suspicious of malignancy, it is recommended that the lesion be managed like a melanoma and be removed in accordance with current melanoma margin guidelines or with comprehensive margin control via Mohs micrographic surgery.34,35 Gurbuz et al17 stated that surgical margin excision, sentinel lymph node dissection, and clinical follow-up is recommended for atypical Spitz tumors. However, currently there are no prospective studies that have tested these various recommendations on atypical Spitz nevi management.
Within the last few years, sentinel lymph node biopsy (SLNB) has been proposed as a useful tool in the management of melanocytic neoplasms of uncertain behavior, such as the atypical Spitz nevus.36 Researchers recommend SLNB in atypical Spitz nevi greater than 1.0-mm thick.18,36,37 Supporters maintain that it increases the sensitivity of the diagnosis of melanoma (vs atypical Spitz nevus) and identifies patients who may potentially benefit from early lymph node dissection and/or adjuvant therapy. They state that a positive SLNB supports the diagnosis of malignancy and recommend that the lesion be treated aggressively. If the SLNB is negative, melanoma cannot be completely ruled out, but there is more reassurance that the lesion may be confined to the skin and can be completely removed by excision.18,36,37 Other advantages of SLNB include minimal invasiveness and morbidity. Some researchers believe melanocytic neoplasms in which melanoma cannot be ruled out should undergo complete surgical excision with wide margins in accordance with current melanoma guidelines,34,35 which can be as much as 3 cm.36,38 A negative SLNB offers the advantage of planning a complete excision of an atypical Spitz nevus that preserves surrounding margins and is cosmetically more acceptable,36 and avoiding the morbidity (ie, lymphedema, paresthesia) associated with regional or elective lymph node dissection.18
However, some researchers argue that a positive SLNB in an atypical Spitz nevus is not metastatic melanoma and point out articles that have shown classic and atypical Spitz nevi spreading to lymphatic vessels and lymph nodes but behaving in a benign manner.11,13,15,21,37 Therefore, more studies are needed to assess the prognostic significance of positive SLNB in atypical Spitz nevi.18
- Spitz S. Melanomas of childhood. Am J Pathol. 1948;24:591-609.
- Spatz A, Barnhill RL. The Spitz tumor 50 years later: revisiting a landmark contribution and unresolved controversy. J Am Acad Dermatol. 1999;40:223-228.
- Paniago-Pereira C, Maize JC, Ackerman AB. Nevus of large spindle and/or epithelioid cells (Spitz's nevus). Arch Dermatol. 1978;114:1811-1823.
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27:901-913.
- Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol. 1999;30:513-520.
- Herreid PA, Shapiro PE. Age distribution of Spitz nevus vs malignant melanoma. Arch Dermatol. 1996;132:352-353.
- Weedon D, Little JH. Spindle and epithelioid cell nevi in children and adults. a review of 211 cases of the Spitz nevus. Cancer. 1977;40:217-225.
- Bader JL, Li FP, Olmstead PM, et al. Childhood malignant melanoma. incidence and etiology. Am J Pediatr Hematol Oncol. 1985;7:341-345.
- Elder DE, Murphy GF. Melanocytic tumors of the skin. In: Elder DE, Murphy GF, eds. Atlas of Tumor Pathology. Washington, DC: Armed Forces Institute of Pathology; 1990:40-57.
- Piepkorn M. On the nature of histologic observations: the case of the Spitz nevus. J Am Acad Dermatol. 1995;32:248-254.
- Barnhill RL, Flotte TJ, Fleischli M, et al. Cutaneous melanoma and atypical Spitz tumors in childhood. Cancer. 1995;76:1833-1845.
- Spatz A, Calonje E, Handfield-Jones S, et al. Spitz tumors in children: a grading system for risk stratification. Arch Dermatol. 1999;135:282-285.
- Smith KJ, Barrett TL, Skelton HG 3rd, et al. Spindle cell and epithelioid cell nevi with atypia and metastasis (malignant Spitz nevus). Am J Surg Pathol. 1989;13:931-939.
- Barnhill RL. Childhood melanoma. Semin Diagn Pathol. 1998;15:189-194.
- Melnik MK, Urdaneta LF, Al-Jurf AS, et al. Malignant melanoma in childhood and adolescence. Am Surg. 1986;52:142-147.
- Shapiro PE. Spitz nevi. J Am Acad Dermatol. 1993;29:667-668.
- Gurbuz Y, Apaydin R, Muezzinoglu B, et al. A current dilemma in histopathology: atypical spitz tumor or Spitzoid melanoma? Pediatr Dermatol. 2002;19:99-102.
- Lohmann CM, Coit DG, Brady MS, et al. Sentinel lymph node biopsy in patients with diagnostically controversial spitzoid melanocytic tumors. Am J Surg Pathol. 2002;26:47-55.
- Handfield-Jones SE, Smith NP. Malignant melanoma in childhood. Br J Dermatol. 1996;134:607-616.
- Crotty KA, McCarthy SW, Palmer AA, et al. Malignant melanoma in childhood: a clinicopathologic study of 13 cases and comparison with Spitz nevi. World J Surg. 1992;16:179-185.
- Lerman RI, Murray D, O'Hara JM, et al. Malignant melanoma of childhood. a clinicopathologic study and a report of 12 cases. Cancer. 1970;25:436-449.
- Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melano-cytic nevi between expert pathologists. Hum Pathol.1996;27:528-531.
- Shimek CM, Golitz LE. The golden anniversary of the Spitz nevus. Arch Dermatol. 1999;135:333-335.
- Bastian BC, Wesselmann U, Pinkel D, et al. Molecular cytogenetic analysis of Spitz nevi shows clear differences to melanoma. J Invest Dermatol.1999; 113:1065-1069.
- Bastian BC, LeBoit PE, Hamm H, et al. Chromo-somal gains and losses in primary cutaneous melanomas detected by comparative genomic hybridization. Cancer Res.1998;58:2170-2175.
- Bergman R, Malkin L, Sabo E, et al. MIB-1 mono-clonal antibody to determine proliferative activity of Ki-67 antigen as an adjunct to the histopathologic dif-ferential diagnosis of Spitz nevi. J Am Acad Dermatol. 2001; 44:500-504.
- Li LX, Crotty KA, McCarthy SW, et al. A zonal com-parison of MIB1-Ki67 immunoreactivity in benign and malignant melanocytic lesions. Am J Dermatopathol. 2000;22:489-495.
- McNutt NS, Urmacher C, Hakimian J, et al. Nevoid malignant melanoma: morphologicpatterns and immu-nohistochemical reactivity. J Cutan Pathol.1995;22:502-517.
- Kanter-Lewensohn L, Hedblad MA, Wejde J, et al. Immu-nohistochemical markers for distinguishing Spitz nevi from malignant melanomas. Mod Pathol.1997;10:917-920.
- Ribé A, McNutt NS. S100A6 protein expression is different in spitz nevi and melanomas. Mod Pathol.2003;16:505-511.
- Kaye VN, Dehner LP. Spindle and epithelioid cell nevus (Spitz nevus). natural history following biopsy. Arch Dermatol.1990;126:1581-1583.
- Omura EF, Kheir SM. Recurrent Spitz’s nevus. Am J. Dermatopathol.1984;6(suppl): 207212.
- Zaenglein AL, Heintz P, Kamino H, et al. Congenital Spitz nevus clinically mimicking melanoma. J Am Acad Dermatol.2002;47:441-444.
- Murphy ME, Boyer JD, Stashower ME, et al. The surgical management of Spitz nevi. Dermatol Surg. 2002;28:1065-1069.
- Zitelli JA, Brown C, Hanusa BH. Mohs micrographic surgery for the treatment of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:236-245.
- Kelley SW, Cockerell CJ. Sentinel lymph node biopsy as an adjunct to management of histologically difficult to diagnose melanocytic lesions: a proposal. J Am Acad Dermatol. 2000;42:527-530.
- Su LD, Fullen DR, Sondak VK, et al. Sentinel lymph node biopsy for patients with problematic spitzoid melanocytic lesions: a report on 18 patients. Cancer. 2003;97:499-507.
- Martinez JC, Otley CC. The management of melanoma and nonmelanoma skin cancer: a review for the primary care physician. Mayo Clin Proc. 2001;76:1253-1265.
Spitz nevi were first described in 1948.1 Spitz1 originally called these lesions benign juvenile melanoma. She was able to identify and describe a separate class of benign melanocytic neoplasms in children that were previously diagnosed and treated as melanoma.2 Prior to this discovery, the standard of care was to remove all suspicious pigmented lesions in children prior to adulthood to prevent possible malignant transformation.2,3 Today, Spitz nevus is the more commonly used term for benign juvenile melanoma because it is encountered occasionally in adults and the term melanoma carries a negative connotation.4 Other synonyms include juvenile melanoma, Spitz tumor, nevus of large spindle and/or epithelioid cells, and spindle cell and epithelioid nevus.3,5
Classic Spitz Nevus
Spitz nevi are uncommon. The approximate incidence is 7 per 100,000 people. Spitz nevi are more frequently found in children and adolescents but can occur in adults.6,7 Spitz nevi occur predominantly in the white population and slightly more often in females.4,8
A Spitz nevus can arise de novo or in association with an existing melanocytic nevus. The lesions can be asymptomatic or have a history of rapid but limited growth. Clinical features of Spitz nevi are well-circumscribed, symmetrical, small- to medium-sized firm papules with smooth discrete borders and a uniform color (typically pink or flesh colored).9 Spitz nevi can occur in various shapes. In a study of 211 cases of Spitz nevi, 19% were described as flat or uneven, 24% as polypoid, and 57% as plateau or elevated.7 Spitz nevi usually are found on the face, neck, or lower extremities but can occur anywhere on the body.7,9 Size is typically less than 6 mm (Figures 1 and 2).
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
The classic Spitz nevus histologically consists of large spindle and/or epithelioid melanocytes arrayed as epidermal nests grouped in a vertical orientation (called "bunches of bananas" or "raining down pattern"), with clefting artifact at the perimeter (Figure 3).4,9,10 The nests are fairly uniform, nonconfluent, and evenly spaced. There is little or no pagetoid spread pattern. Epidermal changes include acanthosis, hypergranulosis, and hyperkeratosis. The intradermal pattern displays maturation, with single-file or single-unit arrays descending to the base. Eosinophilic Kamino bodies frequently are found along the dermoepidermal interface. Kamino bodies are globular clusters that represent apoptotic degenerative melanocytes (Figure 4). They stain positive with both periodic acid-Schiff and trichrome stains. At the dermal base, there is no mitosis, no pushing deep margins, and lack of significant pleomorphism. Little or no melanin is present.4,9,10 The classic Spitz nevus behaves in a benign manner.1 The differential diagnosis of the Spitz nevus includes pyogenic granuloma, mastocytoma, juvenile xanthogranuloma, and malignant melanoma.
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
Atypical Spitz Nevus
The atypical Spitz nevus is difficult to formally define. Instead, it is loosely defined. An atypical Spitz nevus shares histologic features with the classic Spitz nevus, but it may have one or more atypical features, which can be characteristic of malignancy.10-12 Gross atypical features may include irregular shape, nonuniform color, large size, or ulcerations. Histologically, there can be one or more of the following features: pleomorphism; increased cellularity; loss of cellular cohesion; epidermal pagetoid spread; minimal epidermal changes; absence of Kamino bodies; lack of maturation in the intradermal pattern; high-grade nuclear atypia; high basal mitotic rate; pushing deep margins into the dermal base or subcutis; and nests variable in size, shape, and orientation.9,10,13
The behavior of any atypical Spitz nevus is unpredictable. There are case reports of metastasizing and malignant lesions with Spitz-like characteristics causing fatal outcomes.11,13 However, there also are studies that show Spitz nevi acting in a benign manner, even with a history of metastases.11,13-15 Some researchers try to explain this phenomenon by theorizing that Spitz nevi and melanoma exist along a continuum with the classic benign Spitz nevus at one end of the spectrum and the aggressive malignant melanoma at the opposite end, with a diverse range of atypical Spitz-like lesions with features of both in between.4,10-12,14 Other researchers refute this claim and view the unequivocal Spitz nevus as benign and unrelated to melanoma. They point out that many of these case reports of melanomas with Spitz-like features do not fit the diagnosis of the Spitz nevus.16
In general, the more features an atypical Spitz nevus shares with melanoma, the greater the risk for malignant behavior. In 1999, Spatz et al12 proposed formal and specific criteria for determining the risk for malignant behavior in atypical Spitz nevi in children. In the retrospective study, atypical features were used to define atypical Spitz nevi and grade their risk for metastasis. The 5 major factors were age, size, presence of ulceration, involvement of subcutaneous fat, and mitotic activity. Positive risk factors that increased the grade included age greater than 10 years, diameter greater than 10.0 mm, lesions with fat involvement, presence of ulceration, and dermal component mitotic activity greater than 5 mitoses/mm2. The higher the grade, the higher the risk for malignancy and metastasis.12 Since its publication, this grading system for categorizing atypical Spitz nevi has been put to use in a few case reports and studies.17,18 Additional prospective studies using these criteria will be helpful in determining the true clinical nature of atypical Spitz nevi in children, the usefulness of this grading system, and the possible application of this grading system in adults.
Problems Differentiating Classic and Atypical Spitz Nevi From Melanoma
Melanoma is a major part of the differential diagnosis of Spitz nevi. The classic Spitz nevus typically has a benign nature, while the atypical Spitz nevus displays unpredictable behavior that appears to be dependent on the degree of atypia.1,3,16 In contrast, melanoma is potentially fatal. Fortunately, Spitz nevi typically occur in children and the risk for having childhood melanoma is rare.6,8,19 Though risk is minimal, rare cases of melanoma have been reported in children.8,11,14,15,19-21 Therefore, making a correct diagnosis and ruling out melanoma is important.
Unfortunately, even with clinical and histologic guidelines, sometimes it is difficult to distinguish classic and atypical Spitz nevi from melanoma. The major problem is histologic overlap with Spitz nevi and melanoma. Many researchers have emphasized that there is no single discriminating factor for Spitz nevi and melanoma because virtually every trait of Spitz nevi has been described in melanoma.2,10,13,20,22,23 Results of multiple studies show variability among researchers on the analysis of melanocytic nevi and melanoma lesions, and the final diagnosis was subjective.5,22 In one retrospective study where clinical outcome was already known, 30 melanocytic lesions were evaluated independently by a panel of 10 dermatopathologists and categorized as either a typical Spitz nevus, atypical Spitz nevus, melanoma, tumor with unknown biologic potential, or other melanocytic lesion.5 The dermatopathologists were blinded to the clinical data. Evaluation of 17 Spitzoid lesions yielded no clear diagnostic consensus and a few lethal lesions were identified by most dermatopathologists as either typical or atypical Spitz nevi. The authors maintain that these results show that current objective criteria are deficient and inadequate to permit the discrimination of Spitz nevi with atypical features from melanoma.5
Given these histologic analysis limitations, many investigators are researching other tools and techniques that may help enhance diagnostic accuracy. Promising genetic analysis techniques include comparative genomic hybridization and fluorescent in situ hybridization.24 In one study,24 researchers compared Spitz nevi with primary cutaneous melanomas using comparative genomic hybridization and fluorescent in situ hybridization and discovered differences. In the study, Spitz nevi were found to have no chromosomal aberrations or gains in chromosome 11p or 7q21qter. In comparison, primary cutaneous melanomas had frequent chromosome deletions of chromosomes 9p, 10q, 6q, and 8p, and gains of chromosomes 7, 8, 6p, and 1q.24,25 Immunohistochemistry is another potential tool for improving diagnostic accuracy. Examples of promising immunohistochemical markers include antibody MIB-1,26-28 BCL-2,29 and anti-S100A6.30 Studies have shown that most melanomas are immunoreactive to MIB-1 and BCL-2, whereas Spitz nevi are not.26-29 Recently, anti-S100A6 protein also was shown to be a potential immunohistochemical marker to differentiate a Spitz nevus from melanoma.30 Anti-S100A6 is different from anti-S100 because it is more specific to a subclass of normal cell types and certain cancer cell lines. Investigators found strong, uniform, and diffuse S100A6 protein expression in the junctional and dermal components of all 42 Spitz nevi they studied versus weak and patchy S100A6 protein expression found mainly in the dermal component of 35 of 105 melanoma specimens they studied.30 Although these techniques show exceptional potential, further research will be required to prove their reliability.
Management of Classic and Atypical Spitz Nevi
There is controversy regarding the treatment of a classic Spitz nevus. Some investigators recommend conservative treatment because a Spitz nevus is benign. They find that the Spitz nevus may be removed or left alone.3 Others agree but would add that complete excision with clinical follow-up is appropriate if there are atypical features found on the Spitz nevus.16,23,31 Other investigators are more aggressive and recommend complete excision with clear margins of all Spitz nevi, unequivocal or not, because Spitz nevi have histologic overlap with melanoma, and recurrent lesions may present with pseudomelanomatous changes, which makes differentiation more difficult later.4,32 They conclude that the benefits of complete excision outweigh the risks of partial treatment.4 Regardless of how a Spitz nevus case is managed, regular follow-up with a dermatologist is recommended to look for any changes or recurrences suggestive of malignancy.
Currently, there are no available evidence-based recommendations with predictive value for the specific management of atypical Spitz nevi because their clinical course is mostly unknown and unpredictable. Most articles that do address the management of atypical Spitz nevi state that they should be completely excised and followed periodically.11,33 Murphy et al34 suggest that an atypical Spitz nevus should be completely excised to avoid the rare possibility of a melanoma masquerading as an atypical Spitz nevus. Furthermore, if the physician is suspicious of malignancy, it is recommended that the lesion be managed like a melanoma and be removed in accordance with current melanoma margin guidelines or with comprehensive margin control via Mohs micrographic surgery.34,35 Gurbuz et al17 stated that surgical margin excision, sentinel lymph node dissection, and clinical follow-up is recommended for atypical Spitz tumors. However, currently there are no prospective studies that have tested these various recommendations on atypical Spitz nevi management.
Within the last few years, sentinel lymph node biopsy (SLNB) has been proposed as a useful tool in the management of melanocytic neoplasms of uncertain behavior, such as the atypical Spitz nevus.36 Researchers recommend SLNB in atypical Spitz nevi greater than 1.0-mm thick.18,36,37 Supporters maintain that it increases the sensitivity of the diagnosis of melanoma (vs atypical Spitz nevus) and identifies patients who may potentially benefit from early lymph node dissection and/or adjuvant therapy. They state that a positive SLNB supports the diagnosis of malignancy and recommend that the lesion be treated aggressively. If the SLNB is negative, melanoma cannot be completely ruled out, but there is more reassurance that the lesion may be confined to the skin and can be completely removed by excision.18,36,37 Other advantages of SLNB include minimal invasiveness and morbidity. Some researchers believe melanocytic neoplasms in which melanoma cannot be ruled out should undergo complete surgical excision with wide margins in accordance with current melanoma guidelines,34,35 which can be as much as 3 cm.36,38 A negative SLNB offers the advantage of planning a complete excision of an atypical Spitz nevus that preserves surrounding margins and is cosmetically more acceptable,36 and avoiding the morbidity (ie, lymphedema, paresthesia) associated with regional or elective lymph node dissection.18
However, some researchers argue that a positive SLNB in an atypical Spitz nevus is not metastatic melanoma and point out articles that have shown classic and atypical Spitz nevi spreading to lymphatic vessels and lymph nodes but behaving in a benign manner.11,13,15,21,37 Therefore, more studies are needed to assess the prognostic significance of positive SLNB in atypical Spitz nevi.18
Spitz nevi were first described in 1948.1 Spitz1 originally called these lesions benign juvenile melanoma. She was able to identify and describe a separate class of benign melanocytic neoplasms in children that were previously diagnosed and treated as melanoma.2 Prior to this discovery, the standard of care was to remove all suspicious pigmented lesions in children prior to adulthood to prevent possible malignant transformation.2,3 Today, Spitz nevus is the more commonly used term for benign juvenile melanoma because it is encountered occasionally in adults and the term melanoma carries a negative connotation.4 Other synonyms include juvenile melanoma, Spitz tumor, nevus of large spindle and/or epithelioid cells, and spindle cell and epithelioid nevus.3,5
Classic Spitz Nevus
Spitz nevi are uncommon. The approximate incidence is 7 per 100,000 people. Spitz nevi are more frequently found in children and adolescents but can occur in adults.6,7 Spitz nevi occur predominantly in the white population and slightly more often in females.4,8
A Spitz nevus can arise de novo or in association with an existing melanocytic nevus. The lesions can be asymptomatic or have a history of rapid but limited growth. Clinical features of Spitz nevi are well-circumscribed, symmetrical, small- to medium-sized firm papules with smooth discrete borders and a uniform color (typically pink or flesh colored).9 Spitz nevi can occur in various shapes. In a study of 211 cases of Spitz nevi, 19% were described as flat or uneven, 24% as polypoid, and 57% as plateau or elevated.7 Spitz nevi usually are found on the face, neck, or lower extremities but can occur anywhere on the body.7,9 Size is typically less than 6 mm (Figures 1 and 2).
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
The classic Spitz nevus histologically consists of large spindle and/or epithelioid melanocytes arrayed as epidermal nests grouped in a vertical orientation (called "bunches of bananas" or "raining down pattern"), with clefting artifact at the perimeter (Figure 3).4,9,10 The nests are fairly uniform, nonconfluent, and evenly spaced. There is little or no pagetoid spread pattern. Epidermal changes include acanthosis, hypergranulosis, and hyperkeratosis. The intradermal pattern displays maturation, with single-file or single-unit arrays descending to the base. Eosinophilic Kamino bodies frequently are found along the dermoepidermal interface. Kamino bodies are globular clusters that represent apoptotic degenerative melanocytes (Figure 4). They stain positive with both periodic acid-Schiff and trichrome stains. At the dermal base, there is no mitosis, no pushing deep margins, and lack of significant pleomorphism. Little or no melanin is present.4,9,10 The classic Spitz nevus behaves in a benign manner.1 The differential diagnosis of the Spitz nevus includes pyogenic granuloma, mastocytoma, juvenile xanthogranuloma, and malignant melanoma.
PLEASE REFER TO THE PDF TO VIEW THE FIGURES
Atypical Spitz Nevus
The atypical Spitz nevus is difficult to formally define. Instead, it is loosely defined. An atypical Spitz nevus shares histologic features with the classic Spitz nevus, but it may have one or more atypical features, which can be characteristic of malignancy.10-12 Gross atypical features may include irregular shape, nonuniform color, large size, or ulcerations. Histologically, there can be one or more of the following features: pleomorphism; increased cellularity; loss of cellular cohesion; epidermal pagetoid spread; minimal epidermal changes; absence of Kamino bodies; lack of maturation in the intradermal pattern; high-grade nuclear atypia; high basal mitotic rate; pushing deep margins into the dermal base or subcutis; and nests variable in size, shape, and orientation.9,10,13
The behavior of any atypical Spitz nevus is unpredictable. There are case reports of metastasizing and malignant lesions with Spitz-like characteristics causing fatal outcomes.11,13 However, there also are studies that show Spitz nevi acting in a benign manner, even with a history of metastases.11,13-15 Some researchers try to explain this phenomenon by theorizing that Spitz nevi and melanoma exist along a continuum with the classic benign Spitz nevus at one end of the spectrum and the aggressive malignant melanoma at the opposite end, with a diverse range of atypical Spitz-like lesions with features of both in between.4,10-12,14 Other researchers refute this claim and view the unequivocal Spitz nevus as benign and unrelated to melanoma. They point out that many of these case reports of melanomas with Spitz-like features do not fit the diagnosis of the Spitz nevus.16
In general, the more features an atypical Spitz nevus shares with melanoma, the greater the risk for malignant behavior. In 1999, Spatz et al12 proposed formal and specific criteria for determining the risk for malignant behavior in atypical Spitz nevi in children. In the retrospective study, atypical features were used to define atypical Spitz nevi and grade their risk for metastasis. The 5 major factors were age, size, presence of ulceration, involvement of subcutaneous fat, and mitotic activity. Positive risk factors that increased the grade included age greater than 10 years, diameter greater than 10.0 mm, lesions with fat involvement, presence of ulceration, and dermal component mitotic activity greater than 5 mitoses/mm2. The higher the grade, the higher the risk for malignancy and metastasis.12 Since its publication, this grading system for categorizing atypical Spitz nevi has been put to use in a few case reports and studies.17,18 Additional prospective studies using these criteria will be helpful in determining the true clinical nature of atypical Spitz nevi in children, the usefulness of this grading system, and the possible application of this grading system in adults.
Problems Differentiating Classic and Atypical Spitz Nevi From Melanoma
Melanoma is a major part of the differential diagnosis of Spitz nevi. The classic Spitz nevus typically has a benign nature, while the atypical Spitz nevus displays unpredictable behavior that appears to be dependent on the degree of atypia.1,3,16 In contrast, melanoma is potentially fatal. Fortunately, Spitz nevi typically occur in children and the risk for having childhood melanoma is rare.6,8,19 Though risk is minimal, rare cases of melanoma have been reported in children.8,11,14,15,19-21 Therefore, making a correct diagnosis and ruling out melanoma is important.
Unfortunately, even with clinical and histologic guidelines, sometimes it is difficult to distinguish classic and atypical Spitz nevi from melanoma. The major problem is histologic overlap with Spitz nevi and melanoma. Many researchers have emphasized that there is no single discriminating factor for Spitz nevi and melanoma because virtually every trait of Spitz nevi has been described in melanoma.2,10,13,20,22,23 Results of multiple studies show variability among researchers on the analysis of melanocytic nevi and melanoma lesions, and the final diagnosis was subjective.5,22 In one retrospective study where clinical outcome was already known, 30 melanocytic lesions were evaluated independently by a panel of 10 dermatopathologists and categorized as either a typical Spitz nevus, atypical Spitz nevus, melanoma, tumor with unknown biologic potential, or other melanocytic lesion.5 The dermatopathologists were blinded to the clinical data. Evaluation of 17 Spitzoid lesions yielded no clear diagnostic consensus and a few lethal lesions were identified by most dermatopathologists as either typical or atypical Spitz nevi. The authors maintain that these results show that current objective criteria are deficient and inadequate to permit the discrimination of Spitz nevi with atypical features from melanoma.5
Given these histologic analysis limitations, many investigators are researching other tools and techniques that may help enhance diagnostic accuracy. Promising genetic analysis techniques include comparative genomic hybridization and fluorescent in situ hybridization.24 In one study,24 researchers compared Spitz nevi with primary cutaneous melanomas using comparative genomic hybridization and fluorescent in situ hybridization and discovered differences. In the study, Spitz nevi were found to have no chromosomal aberrations or gains in chromosome 11p or 7q21qter. In comparison, primary cutaneous melanomas had frequent chromosome deletions of chromosomes 9p, 10q, 6q, and 8p, and gains of chromosomes 7, 8, 6p, and 1q.24,25 Immunohistochemistry is another potential tool for improving diagnostic accuracy. Examples of promising immunohistochemical markers include antibody MIB-1,26-28 BCL-2,29 and anti-S100A6.30 Studies have shown that most melanomas are immunoreactive to MIB-1 and BCL-2, whereas Spitz nevi are not.26-29 Recently, anti-S100A6 protein also was shown to be a potential immunohistochemical marker to differentiate a Spitz nevus from melanoma.30 Anti-S100A6 is different from anti-S100 because it is more specific to a subclass of normal cell types and certain cancer cell lines. Investigators found strong, uniform, and diffuse S100A6 protein expression in the junctional and dermal components of all 42 Spitz nevi they studied versus weak and patchy S100A6 protein expression found mainly in the dermal component of 35 of 105 melanoma specimens they studied.30 Although these techniques show exceptional potential, further research will be required to prove their reliability.
Management of Classic and Atypical Spitz Nevi
There is controversy regarding the treatment of a classic Spitz nevus. Some investigators recommend conservative treatment because a Spitz nevus is benign. They find that the Spitz nevus may be removed or left alone.3 Others agree but would add that complete excision with clinical follow-up is appropriate if there are atypical features found on the Spitz nevus.16,23,31 Other investigators are more aggressive and recommend complete excision with clear margins of all Spitz nevi, unequivocal or not, because Spitz nevi have histologic overlap with melanoma, and recurrent lesions may present with pseudomelanomatous changes, which makes differentiation more difficult later.4,32 They conclude that the benefits of complete excision outweigh the risks of partial treatment.4 Regardless of how a Spitz nevus case is managed, regular follow-up with a dermatologist is recommended to look for any changes or recurrences suggestive of malignancy.
Currently, there are no available evidence-based recommendations with predictive value for the specific management of atypical Spitz nevi because their clinical course is mostly unknown and unpredictable. Most articles that do address the management of atypical Spitz nevi state that they should be completely excised and followed periodically.11,33 Murphy et al34 suggest that an atypical Spitz nevus should be completely excised to avoid the rare possibility of a melanoma masquerading as an atypical Spitz nevus. Furthermore, if the physician is suspicious of malignancy, it is recommended that the lesion be managed like a melanoma and be removed in accordance with current melanoma margin guidelines or with comprehensive margin control via Mohs micrographic surgery.34,35 Gurbuz et al17 stated that surgical margin excision, sentinel lymph node dissection, and clinical follow-up is recommended for atypical Spitz tumors. However, currently there are no prospective studies that have tested these various recommendations on atypical Spitz nevi management.
Within the last few years, sentinel lymph node biopsy (SLNB) has been proposed as a useful tool in the management of melanocytic neoplasms of uncertain behavior, such as the atypical Spitz nevus.36 Researchers recommend SLNB in atypical Spitz nevi greater than 1.0-mm thick.18,36,37 Supporters maintain that it increases the sensitivity of the diagnosis of melanoma (vs atypical Spitz nevus) and identifies patients who may potentially benefit from early lymph node dissection and/or adjuvant therapy. They state that a positive SLNB supports the diagnosis of malignancy and recommend that the lesion be treated aggressively. If the SLNB is negative, melanoma cannot be completely ruled out, but there is more reassurance that the lesion may be confined to the skin and can be completely removed by excision.18,36,37 Other advantages of SLNB include minimal invasiveness and morbidity. Some researchers believe melanocytic neoplasms in which melanoma cannot be ruled out should undergo complete surgical excision with wide margins in accordance with current melanoma guidelines,34,35 which can be as much as 3 cm.36,38 A negative SLNB offers the advantage of planning a complete excision of an atypical Spitz nevus that preserves surrounding margins and is cosmetically more acceptable,36 and avoiding the morbidity (ie, lymphedema, paresthesia) associated with regional or elective lymph node dissection.18
However, some researchers argue that a positive SLNB in an atypical Spitz nevus is not metastatic melanoma and point out articles that have shown classic and atypical Spitz nevi spreading to lymphatic vessels and lymph nodes but behaving in a benign manner.11,13,15,21,37 Therefore, more studies are needed to assess the prognostic significance of positive SLNB in atypical Spitz nevi.18
- Spitz S. Melanomas of childhood. Am J Pathol. 1948;24:591-609.
- Spatz A, Barnhill RL. The Spitz tumor 50 years later: revisiting a landmark contribution and unresolved controversy. J Am Acad Dermatol. 1999;40:223-228.
- Paniago-Pereira C, Maize JC, Ackerman AB. Nevus of large spindle and/or epithelioid cells (Spitz's nevus). Arch Dermatol. 1978;114:1811-1823.
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27:901-913.
- Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol. 1999;30:513-520.
- Herreid PA, Shapiro PE. Age distribution of Spitz nevus vs malignant melanoma. Arch Dermatol. 1996;132:352-353.
- Weedon D, Little JH. Spindle and epithelioid cell nevi in children and adults. a review of 211 cases of the Spitz nevus. Cancer. 1977;40:217-225.
- Bader JL, Li FP, Olmstead PM, et al. Childhood malignant melanoma. incidence and etiology. Am J Pediatr Hematol Oncol. 1985;7:341-345.
- Elder DE, Murphy GF. Melanocytic tumors of the skin. In: Elder DE, Murphy GF, eds. Atlas of Tumor Pathology. Washington, DC: Armed Forces Institute of Pathology; 1990:40-57.
- Piepkorn M. On the nature of histologic observations: the case of the Spitz nevus. J Am Acad Dermatol. 1995;32:248-254.
- Barnhill RL, Flotte TJ, Fleischli M, et al. Cutaneous melanoma and atypical Spitz tumors in childhood. Cancer. 1995;76:1833-1845.
- Spatz A, Calonje E, Handfield-Jones S, et al. Spitz tumors in children: a grading system for risk stratification. Arch Dermatol. 1999;135:282-285.
- Smith KJ, Barrett TL, Skelton HG 3rd, et al. Spindle cell and epithelioid cell nevi with atypia and metastasis (malignant Spitz nevus). Am J Surg Pathol. 1989;13:931-939.
- Barnhill RL. Childhood melanoma. Semin Diagn Pathol. 1998;15:189-194.
- Melnik MK, Urdaneta LF, Al-Jurf AS, et al. Malignant melanoma in childhood and adolescence. Am Surg. 1986;52:142-147.
- Shapiro PE. Spitz nevi. J Am Acad Dermatol. 1993;29:667-668.
- Gurbuz Y, Apaydin R, Muezzinoglu B, et al. A current dilemma in histopathology: atypical spitz tumor or Spitzoid melanoma? Pediatr Dermatol. 2002;19:99-102.
- Lohmann CM, Coit DG, Brady MS, et al. Sentinel lymph node biopsy in patients with diagnostically controversial spitzoid melanocytic tumors. Am J Surg Pathol. 2002;26:47-55.
- Handfield-Jones SE, Smith NP. Malignant melanoma in childhood. Br J Dermatol. 1996;134:607-616.
- Crotty KA, McCarthy SW, Palmer AA, et al. Malignant melanoma in childhood: a clinicopathologic study of 13 cases and comparison with Spitz nevi. World J Surg. 1992;16:179-185.
- Lerman RI, Murray D, O'Hara JM, et al. Malignant melanoma of childhood. a clinicopathologic study and a report of 12 cases. Cancer. 1970;25:436-449.
- Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melano-cytic nevi between expert pathologists. Hum Pathol.1996;27:528-531.
- Shimek CM, Golitz LE. The golden anniversary of the Spitz nevus. Arch Dermatol. 1999;135:333-335.
- Bastian BC, Wesselmann U, Pinkel D, et al. Molecular cytogenetic analysis of Spitz nevi shows clear differences to melanoma. J Invest Dermatol.1999; 113:1065-1069.
- Bastian BC, LeBoit PE, Hamm H, et al. Chromo-somal gains and losses in primary cutaneous melanomas detected by comparative genomic hybridization. Cancer Res.1998;58:2170-2175.
- Bergman R, Malkin L, Sabo E, et al. MIB-1 mono-clonal antibody to determine proliferative activity of Ki-67 antigen as an adjunct to the histopathologic dif-ferential diagnosis of Spitz nevi. J Am Acad Dermatol. 2001; 44:500-504.
- Li LX, Crotty KA, McCarthy SW, et al. A zonal com-parison of MIB1-Ki67 immunoreactivity in benign and malignant melanocytic lesions. Am J Dermatopathol. 2000;22:489-495.
- McNutt NS, Urmacher C, Hakimian J, et al. Nevoid malignant melanoma: morphologicpatterns and immu-nohistochemical reactivity. J Cutan Pathol.1995;22:502-517.
- Kanter-Lewensohn L, Hedblad MA, Wejde J, et al. Immu-nohistochemical markers for distinguishing Spitz nevi from malignant melanomas. Mod Pathol.1997;10:917-920.
- Ribé A, McNutt NS. S100A6 protein expression is different in spitz nevi and melanomas. Mod Pathol.2003;16:505-511.
- Kaye VN, Dehner LP. Spindle and epithelioid cell nevus (Spitz nevus). natural history following biopsy. Arch Dermatol.1990;126:1581-1583.
- Omura EF, Kheir SM. Recurrent Spitz’s nevus. Am J. Dermatopathol.1984;6(suppl): 207212.
- Zaenglein AL, Heintz P, Kamino H, et al. Congenital Spitz nevus clinically mimicking melanoma. J Am Acad Dermatol.2002;47:441-444.
- Murphy ME, Boyer JD, Stashower ME, et al. The surgical management of Spitz nevi. Dermatol Surg. 2002;28:1065-1069.
- Zitelli JA, Brown C, Hanusa BH. Mohs micrographic surgery for the treatment of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:236-245.
- Kelley SW, Cockerell CJ. Sentinel lymph node biopsy as an adjunct to management of histologically difficult to diagnose melanocytic lesions: a proposal. J Am Acad Dermatol. 2000;42:527-530.
- Su LD, Fullen DR, Sondak VK, et al. Sentinel lymph node biopsy for patients with problematic spitzoid melanocytic lesions: a report on 18 patients. Cancer. 2003;97:499-507.
- Martinez JC, Otley CC. The management of melanoma and nonmelanoma skin cancer: a review for the primary care physician. Mayo Clin Proc. 2001;76:1253-1265.
- Spitz S. Melanomas of childhood. Am J Pathol. 1948;24:591-609.
- Spatz A, Barnhill RL. The Spitz tumor 50 years later: revisiting a landmark contribution and unresolved controversy. J Am Acad Dermatol. 1999;40:223-228.
- Paniago-Pereira C, Maize JC, Ackerman AB. Nevus of large spindle and/or epithelioid cells (Spitz's nevus). Arch Dermatol. 1978;114:1811-1823.
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27:901-913.
- Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol. 1999;30:513-520.
- Herreid PA, Shapiro PE. Age distribution of Spitz nevus vs malignant melanoma. Arch Dermatol. 1996;132:352-353.
- Weedon D, Little JH. Spindle and epithelioid cell nevi in children and adults. a review of 211 cases of the Spitz nevus. Cancer. 1977;40:217-225.
- Bader JL, Li FP, Olmstead PM, et al. Childhood malignant melanoma. incidence and etiology. Am J Pediatr Hematol Oncol. 1985;7:341-345.
- Elder DE, Murphy GF. Melanocytic tumors of the skin. In: Elder DE, Murphy GF, eds. Atlas of Tumor Pathology. Washington, DC: Armed Forces Institute of Pathology; 1990:40-57.
- Piepkorn M. On the nature of histologic observations: the case of the Spitz nevus. J Am Acad Dermatol. 1995;32:248-254.
- Barnhill RL, Flotte TJ, Fleischli M, et al. Cutaneous melanoma and atypical Spitz tumors in childhood. Cancer. 1995;76:1833-1845.
- Spatz A, Calonje E, Handfield-Jones S, et al. Spitz tumors in children: a grading system for risk stratification. Arch Dermatol. 1999;135:282-285.
- Smith KJ, Barrett TL, Skelton HG 3rd, et al. Spindle cell and epithelioid cell nevi with atypia and metastasis (malignant Spitz nevus). Am J Surg Pathol. 1989;13:931-939.
- Barnhill RL. Childhood melanoma. Semin Diagn Pathol. 1998;15:189-194.
- Melnik MK, Urdaneta LF, Al-Jurf AS, et al. Malignant melanoma in childhood and adolescence. Am Surg. 1986;52:142-147.
- Shapiro PE. Spitz nevi. J Am Acad Dermatol. 1993;29:667-668.
- Gurbuz Y, Apaydin R, Muezzinoglu B, et al. A current dilemma in histopathology: atypical spitz tumor or Spitzoid melanoma? Pediatr Dermatol. 2002;19:99-102.
- Lohmann CM, Coit DG, Brady MS, et al. Sentinel lymph node biopsy in patients with diagnostically controversial spitzoid melanocytic tumors. Am J Surg Pathol. 2002;26:47-55.
- Handfield-Jones SE, Smith NP. Malignant melanoma in childhood. Br J Dermatol. 1996;134:607-616.
- Crotty KA, McCarthy SW, Palmer AA, et al. Malignant melanoma in childhood: a clinicopathologic study of 13 cases and comparison with Spitz nevi. World J Surg. 1992;16:179-185.
- Lerman RI, Murray D, O'Hara JM, et al. Malignant melanoma of childhood. a clinicopathologic study and a report of 12 cases. Cancer. 1970;25:436-449.
- Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melano-cytic nevi between expert pathologists. Hum Pathol.1996;27:528-531.
- Shimek CM, Golitz LE. The golden anniversary of the Spitz nevus. Arch Dermatol. 1999;135:333-335.
- Bastian BC, Wesselmann U, Pinkel D, et al. Molecular cytogenetic analysis of Spitz nevi shows clear differences to melanoma. J Invest Dermatol.1999; 113:1065-1069.
- Bastian BC, LeBoit PE, Hamm H, et al. Chromo-somal gains and losses in primary cutaneous melanomas detected by comparative genomic hybridization. Cancer Res.1998;58:2170-2175.
- Bergman R, Malkin L, Sabo E, et al. MIB-1 mono-clonal antibody to determine proliferative activity of Ki-67 antigen as an adjunct to the histopathologic dif-ferential diagnosis of Spitz nevi. J Am Acad Dermatol. 2001; 44:500-504.
- Li LX, Crotty KA, McCarthy SW, et al. A zonal com-parison of MIB1-Ki67 immunoreactivity in benign and malignant melanocytic lesions. Am J Dermatopathol. 2000;22:489-495.
- McNutt NS, Urmacher C, Hakimian J, et al. Nevoid malignant melanoma: morphologicpatterns and immu-nohistochemical reactivity. J Cutan Pathol.1995;22:502-517.
- Kanter-Lewensohn L, Hedblad MA, Wejde J, et al. Immu-nohistochemical markers for distinguishing Spitz nevi from malignant melanomas. Mod Pathol.1997;10:917-920.
- Ribé A, McNutt NS. S100A6 protein expression is different in spitz nevi and melanomas. Mod Pathol.2003;16:505-511.
- Kaye VN, Dehner LP. Spindle and epithelioid cell nevus (Spitz nevus). natural history following biopsy. Arch Dermatol.1990;126:1581-1583.
- Omura EF, Kheir SM. Recurrent Spitz’s nevus. Am J. Dermatopathol.1984;6(suppl): 207212.
- Zaenglein AL, Heintz P, Kamino H, et al. Congenital Spitz nevus clinically mimicking melanoma. J Am Acad Dermatol.2002;47:441-444.
- Murphy ME, Boyer JD, Stashower ME, et al. The surgical management of Spitz nevi. Dermatol Surg. 2002;28:1065-1069.
- Zitelli JA, Brown C, Hanusa BH. Mohs micrographic surgery for the treatment of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:236-245.
- Kelley SW, Cockerell CJ. Sentinel lymph node biopsy as an adjunct to management of histologically difficult to diagnose melanocytic lesions: a proposal. J Am Acad Dermatol. 2000;42:527-530.
- Su LD, Fullen DR, Sondak VK, et al. Sentinel lymph node biopsy for patients with problematic spitzoid melanocytic lesions: a report on 18 patients. Cancer. 2003;97:499-507.
- Martinez JC, Otley CC. The management of melanoma and nonmelanoma skin cancer: a review for the primary care physician. Mayo Clin Proc. 2001;76:1253-1265.
What is the preferred treatment for a child with mild persistent asthma?
Low-dose inhaled corticosteroids are the preferred treatment for children with mild persistent asthma because they demonstrate superior reduction in severity and frequency of asthma exacerbations compared with alternatives (strength of recommendation [SOR]: A, based on multiple randomized controlled trials). As add-on therapy, nedocromil, theophylline, and cromolyn have all demonstrated a modest benefit in symptom control; leukotriene receptor antagonists are also recommended based on data from older children (SOR: B, cohort study). Unlike treatment of moderate or severe asthma, long-acting beta-agonists are not recommended (SOR: A, randomized trials).
Clear medication choices for mild asthma are supported by good evidence
John Heintzman, MD
Oregon Health and Science University, Portland
Physicians who routinely treat children with asthma are fortunate to have the body of evidence outlined in this review. Clear medication choices are supported in most instances by relatively clear comparisons with alternatives. In my practice, where many children can be classified in the “mild persistent” category, I am always surprised at how many patients’ families lack a clear understanding of the factors that trigger a child’s asthma and how to avoid them.
Another common clinical scenario among children and adolescents is exercise-induced asthma. Depending on the sport, the asthma can be classified as “mild persistent” or “mild intermittent.” for true intermittent symptoms, my clinical experience (and often parental preference) argues for pre-activity treatment with short acting beta-agonists as the most practical therapy.
Evidence summary
Mild persistent asthma is defined as forced expiratory volume over 1 second (FEV1) ≥80% predicted, with daytime symptoms more than twice per week but less than once daily, and nighttime symptoms more often than twice monthly.1
Low-dose inhaled corticosteroids
Two large randomized trials support using low-dose inhaled corticosteroids in these children. The Childhood Asthma Management Program (CAMP) study, which included 1041 children, evaluated treatment with either budesonide or nedocromil vs placebo. Patients taking budesonide had a lower rate of urgent care visits (absolute risk reduction [ARR]=10%; number needed to treat [NNT]=10; P=.02) compared with children taking nedocromil (ARR=6%; NNT=17; P=.02). The urgent care visits were reported as number of visits per 100 person-years.
In practical terms, this means that in order to decrease 1 urgent care visit, 1 patient would need to take budesonide for 10 years. However, because rates are not necessarily homogenous over time, the number of visits decreased during the first year may be different than the number of events decreased throughout the tenth year.
Children taking budesonide experienced 21.5% more episode-free days than those taking placebo (P=.01). No change was observed in the nedocromil group.2 In the inhaled Steroid Treatment As Regular Therapy (START) in early asthma study, budesonide demonstrated a 44% relative reduction in time to first severe asthma related event, compared with placebo (95% confidence interval [CI], 0.45–0.71; NNT=44; P=.0001).3
Theophylline
Theophylline is considered an alternative to inhaled corticosteroids. One study compared beclomethasone with theophylline in 195 children. This study found near-equivalent efficacy in doctor visits, hospitalizations, monthly peak expiratory flow rates, and FEV1; however, beclomethasone was superior to theophylline in maintaining symptom control and decreasing the use of inhaled bronchodilators and systemic steroids.
When compared with beclomethasone, theophylline was linked to 14% more central nervous system adverse effects (P<.001) and 17% more gastrointestinal disturbances (P<.001). Although beclomethasone induced more oral candidiasis compared with theophylline (8.9% vs 2.4%; P<.001), the incidence of this infection can be reduced by using a spacer.
Long-term systemic effects
The potential long-term adverse systemic effects of inhaled corticosteroids on growth, bone metabolism, and pituitary-adrenal function call for longer-term studies.4 A systematic review of 15 trials reported that the protective effect of leukotriene receptor antagonists is inferior to inhaled corticosteroids for adults (relative risk [RR]=1.71; 95% CI, 1.40–2.09); however, evidence is insufficient to extrapolate this to children.5
Beta-agonists
Evidence does not support use of long-acting beta-agonists as monotherapy or in combination with other medications for children with mild persistent asthma. Although 1 study showed an improvement in lung function for children taking budesonide plus formoterol compared with budesonide alone, the rate of severe exacerbations was lower for those taking budesonide alone (62% decrease vs 55.8% decrease; P=.001). Both groups had a 32% decrease in the number of rescue inhalations per day when compared with placebo (P=.0008).6
Recommendations from others
Recommendations are listed in the TABLE.1,7,8 Unlike the NAEPP and GINA asthma guidelines, the BTS/SIGN asthma guidelines define no objective measurement or staging classification to diagnose asthma among children. Diagnosis is determined by a child’s response to medication.8 Independent of any daily controller medication use, all children should have a short acting bronchodilator on hand in case of an acute attack.1,8
TABLE
Recommendations for treating mild persistent asthma
| GUIDELINE | DAILY CONTROLLER MEDICATION | ALTERNATIVE TREATMENT |
|---|---|---|
| National Asthma Education and Prevention Program (NAEPP)1 | Low-dose inhaled corticosteroids | Children <5: cromolyn, LTRAs Children >5: cromolyn, LTRAs, nedocromil, sustained release theophylline |
| Global initiative for asthma (GINA)7 | low-dose inhaled corticosteroids | All children: sustained released theophylline, Cromone, LTRAs |
| British Thoracic Society/Scottish intercollegiate Guidelines network (BTS/SIGN)8 | Inhaled steroids | All children: LTRAs, theophylline Children >5: cromones, nedocromil |
| LRTA leukotriene receptor antagonists. | ||
| Sources: NAEPP J Allergy Clin Immunol 20021; GINA Guidelines and Resources 20057 and BTS/SIGN, Thorax 2003.8 | ||
1. National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma Update on Selected Topics—2002. National Asthma Education and Prevention Program. J Allergy Clin Immunol 2002;110:S141-S219.
2. Long-term effects of budesonide or nedocromil in children with asthma. The Childhood Asthma Management Program Research Group. N Engl J Med 2000;343:1054-1063.
3. Pauwels RA, Pedersen S, Busse WW, et al. START Investigators Group. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003;361:1071-1076.
4. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild-to-moderate asthma. The American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. J Allergy Clin Immunol 1998;101:14-23.
5. Ducharme FM, Salvio F, Ducharme F. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children (Cochrane review). In: The Cochrane Library. 2006 Issue 2. Chichester, UK: John Wiley and Sons, Ltd.
6. O’byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med 2001;164:1392-1397.
7. The Global Initiative for Asthma. Guidelines and Resources: 2005 Update. Available at: www.ginasthma.com/Guidelineitem.asp??I1=2&I2=1&intId=60. Accessed January 9, 2007.
8. British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. A national clinical guideline. Thorax 2003;58:i1-i94.
Low-dose inhaled corticosteroids are the preferred treatment for children with mild persistent asthma because they demonstrate superior reduction in severity and frequency of asthma exacerbations compared with alternatives (strength of recommendation [SOR]: A, based on multiple randomized controlled trials). As add-on therapy, nedocromil, theophylline, and cromolyn have all demonstrated a modest benefit in symptom control; leukotriene receptor antagonists are also recommended based on data from older children (SOR: B, cohort study). Unlike treatment of moderate or severe asthma, long-acting beta-agonists are not recommended (SOR: A, randomized trials).
Clear medication choices for mild asthma are supported by good evidence
John Heintzman, MD
Oregon Health and Science University, Portland
Physicians who routinely treat children with asthma are fortunate to have the body of evidence outlined in this review. Clear medication choices are supported in most instances by relatively clear comparisons with alternatives. In my practice, where many children can be classified in the “mild persistent” category, I am always surprised at how many patients’ families lack a clear understanding of the factors that trigger a child’s asthma and how to avoid them.
Another common clinical scenario among children and adolescents is exercise-induced asthma. Depending on the sport, the asthma can be classified as “mild persistent” or “mild intermittent.” for true intermittent symptoms, my clinical experience (and often parental preference) argues for pre-activity treatment with short acting beta-agonists as the most practical therapy.
Evidence summary
Mild persistent asthma is defined as forced expiratory volume over 1 second (FEV1) ≥80% predicted, with daytime symptoms more than twice per week but less than once daily, and nighttime symptoms more often than twice monthly.1
Low-dose inhaled corticosteroids
Two large randomized trials support using low-dose inhaled corticosteroids in these children. The Childhood Asthma Management Program (CAMP) study, which included 1041 children, evaluated treatment with either budesonide or nedocromil vs placebo. Patients taking budesonide had a lower rate of urgent care visits (absolute risk reduction [ARR]=10%; number needed to treat [NNT]=10; P=.02) compared with children taking nedocromil (ARR=6%; NNT=17; P=.02). The urgent care visits were reported as number of visits per 100 person-years.
In practical terms, this means that in order to decrease 1 urgent care visit, 1 patient would need to take budesonide for 10 years. However, because rates are not necessarily homogenous over time, the number of visits decreased during the first year may be different than the number of events decreased throughout the tenth year.
Children taking budesonide experienced 21.5% more episode-free days than those taking placebo (P=.01). No change was observed in the nedocromil group.2 In the inhaled Steroid Treatment As Regular Therapy (START) in early asthma study, budesonide demonstrated a 44% relative reduction in time to first severe asthma related event, compared with placebo (95% confidence interval [CI], 0.45–0.71; NNT=44; P=.0001).3
Theophylline
Theophylline is considered an alternative to inhaled corticosteroids. One study compared beclomethasone with theophylline in 195 children. This study found near-equivalent efficacy in doctor visits, hospitalizations, monthly peak expiratory flow rates, and FEV1; however, beclomethasone was superior to theophylline in maintaining symptom control and decreasing the use of inhaled bronchodilators and systemic steroids.
When compared with beclomethasone, theophylline was linked to 14% more central nervous system adverse effects (P<.001) and 17% more gastrointestinal disturbances (P<.001). Although beclomethasone induced more oral candidiasis compared with theophylline (8.9% vs 2.4%; P<.001), the incidence of this infection can be reduced by using a spacer.
Long-term systemic effects
The potential long-term adverse systemic effects of inhaled corticosteroids on growth, bone metabolism, and pituitary-adrenal function call for longer-term studies.4 A systematic review of 15 trials reported that the protective effect of leukotriene receptor antagonists is inferior to inhaled corticosteroids for adults (relative risk [RR]=1.71; 95% CI, 1.40–2.09); however, evidence is insufficient to extrapolate this to children.5
Beta-agonists
Evidence does not support use of long-acting beta-agonists as monotherapy or in combination with other medications for children with mild persistent asthma. Although 1 study showed an improvement in lung function for children taking budesonide plus formoterol compared with budesonide alone, the rate of severe exacerbations was lower for those taking budesonide alone (62% decrease vs 55.8% decrease; P=.001). Both groups had a 32% decrease in the number of rescue inhalations per day when compared with placebo (P=.0008).6
Recommendations from others
Recommendations are listed in the TABLE.1,7,8 Unlike the NAEPP and GINA asthma guidelines, the BTS/SIGN asthma guidelines define no objective measurement or staging classification to diagnose asthma among children. Diagnosis is determined by a child’s response to medication.8 Independent of any daily controller medication use, all children should have a short acting bronchodilator on hand in case of an acute attack.1,8
TABLE
Recommendations for treating mild persistent asthma
| GUIDELINE | DAILY CONTROLLER MEDICATION | ALTERNATIVE TREATMENT |
|---|---|---|
| National Asthma Education and Prevention Program (NAEPP)1 | Low-dose inhaled corticosteroids | Children <5: cromolyn, LTRAs Children >5: cromolyn, LTRAs, nedocromil, sustained release theophylline |
| Global initiative for asthma (GINA)7 | low-dose inhaled corticosteroids | All children: sustained released theophylline, Cromone, LTRAs |
| British Thoracic Society/Scottish intercollegiate Guidelines network (BTS/SIGN)8 | Inhaled steroids | All children: LTRAs, theophylline Children >5: cromones, nedocromil |
| LRTA leukotriene receptor antagonists. | ||
| Sources: NAEPP J Allergy Clin Immunol 20021; GINA Guidelines and Resources 20057 and BTS/SIGN, Thorax 2003.8 | ||
Low-dose inhaled corticosteroids are the preferred treatment for children with mild persistent asthma because they demonstrate superior reduction in severity and frequency of asthma exacerbations compared with alternatives (strength of recommendation [SOR]: A, based on multiple randomized controlled trials). As add-on therapy, nedocromil, theophylline, and cromolyn have all demonstrated a modest benefit in symptom control; leukotriene receptor antagonists are also recommended based on data from older children (SOR: B, cohort study). Unlike treatment of moderate or severe asthma, long-acting beta-agonists are not recommended (SOR: A, randomized trials).
Clear medication choices for mild asthma are supported by good evidence
John Heintzman, MD
Oregon Health and Science University, Portland
Physicians who routinely treat children with asthma are fortunate to have the body of evidence outlined in this review. Clear medication choices are supported in most instances by relatively clear comparisons with alternatives. In my practice, where many children can be classified in the “mild persistent” category, I am always surprised at how many patients’ families lack a clear understanding of the factors that trigger a child’s asthma and how to avoid them.
Another common clinical scenario among children and adolescents is exercise-induced asthma. Depending on the sport, the asthma can be classified as “mild persistent” or “mild intermittent.” for true intermittent symptoms, my clinical experience (and often parental preference) argues for pre-activity treatment with short acting beta-agonists as the most practical therapy.
Evidence summary
Mild persistent asthma is defined as forced expiratory volume over 1 second (FEV1) ≥80% predicted, with daytime symptoms more than twice per week but less than once daily, and nighttime symptoms more often than twice monthly.1
Low-dose inhaled corticosteroids
Two large randomized trials support using low-dose inhaled corticosteroids in these children. The Childhood Asthma Management Program (CAMP) study, which included 1041 children, evaluated treatment with either budesonide or nedocromil vs placebo. Patients taking budesonide had a lower rate of urgent care visits (absolute risk reduction [ARR]=10%; number needed to treat [NNT]=10; P=.02) compared with children taking nedocromil (ARR=6%; NNT=17; P=.02). The urgent care visits were reported as number of visits per 100 person-years.
In practical terms, this means that in order to decrease 1 urgent care visit, 1 patient would need to take budesonide for 10 years. However, because rates are not necessarily homogenous over time, the number of visits decreased during the first year may be different than the number of events decreased throughout the tenth year.
Children taking budesonide experienced 21.5% more episode-free days than those taking placebo (P=.01). No change was observed in the nedocromil group.2 In the inhaled Steroid Treatment As Regular Therapy (START) in early asthma study, budesonide demonstrated a 44% relative reduction in time to first severe asthma related event, compared with placebo (95% confidence interval [CI], 0.45–0.71; NNT=44; P=.0001).3
Theophylline
Theophylline is considered an alternative to inhaled corticosteroids. One study compared beclomethasone with theophylline in 195 children. This study found near-equivalent efficacy in doctor visits, hospitalizations, monthly peak expiratory flow rates, and FEV1; however, beclomethasone was superior to theophylline in maintaining symptom control and decreasing the use of inhaled bronchodilators and systemic steroids.
When compared with beclomethasone, theophylline was linked to 14% more central nervous system adverse effects (P<.001) and 17% more gastrointestinal disturbances (P<.001). Although beclomethasone induced more oral candidiasis compared with theophylline (8.9% vs 2.4%; P<.001), the incidence of this infection can be reduced by using a spacer.
Long-term systemic effects
The potential long-term adverse systemic effects of inhaled corticosteroids on growth, bone metabolism, and pituitary-adrenal function call for longer-term studies.4 A systematic review of 15 trials reported that the protective effect of leukotriene receptor antagonists is inferior to inhaled corticosteroids for adults (relative risk [RR]=1.71; 95% CI, 1.40–2.09); however, evidence is insufficient to extrapolate this to children.5
Beta-agonists
Evidence does not support use of long-acting beta-agonists as monotherapy or in combination with other medications for children with mild persistent asthma. Although 1 study showed an improvement in lung function for children taking budesonide plus formoterol compared with budesonide alone, the rate of severe exacerbations was lower for those taking budesonide alone (62% decrease vs 55.8% decrease; P=.001). Both groups had a 32% decrease in the number of rescue inhalations per day when compared with placebo (P=.0008).6
Recommendations from others
Recommendations are listed in the TABLE.1,7,8 Unlike the NAEPP and GINA asthma guidelines, the BTS/SIGN asthma guidelines define no objective measurement or staging classification to diagnose asthma among children. Diagnosis is determined by a child’s response to medication.8 Independent of any daily controller medication use, all children should have a short acting bronchodilator on hand in case of an acute attack.1,8
TABLE
Recommendations for treating mild persistent asthma
| GUIDELINE | DAILY CONTROLLER MEDICATION | ALTERNATIVE TREATMENT |
|---|---|---|
| National Asthma Education and Prevention Program (NAEPP)1 | Low-dose inhaled corticosteroids | Children <5: cromolyn, LTRAs Children >5: cromolyn, LTRAs, nedocromil, sustained release theophylline |
| Global initiative for asthma (GINA)7 | low-dose inhaled corticosteroids | All children: sustained released theophylline, Cromone, LTRAs |
| British Thoracic Society/Scottish intercollegiate Guidelines network (BTS/SIGN)8 | Inhaled steroids | All children: LTRAs, theophylline Children >5: cromones, nedocromil |
| LRTA leukotriene receptor antagonists. | ||
| Sources: NAEPP J Allergy Clin Immunol 20021; GINA Guidelines and Resources 20057 and BTS/SIGN, Thorax 2003.8 | ||
1. National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma Update on Selected Topics—2002. National Asthma Education and Prevention Program. J Allergy Clin Immunol 2002;110:S141-S219.
2. Long-term effects of budesonide or nedocromil in children with asthma. The Childhood Asthma Management Program Research Group. N Engl J Med 2000;343:1054-1063.
3. Pauwels RA, Pedersen S, Busse WW, et al. START Investigators Group. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003;361:1071-1076.
4. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild-to-moderate asthma. The American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. J Allergy Clin Immunol 1998;101:14-23.
5. Ducharme FM, Salvio F, Ducharme F. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children (Cochrane review). In: The Cochrane Library. 2006 Issue 2. Chichester, UK: John Wiley and Sons, Ltd.
6. O’byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med 2001;164:1392-1397.
7. The Global Initiative for Asthma. Guidelines and Resources: 2005 Update. Available at: www.ginasthma.com/Guidelineitem.asp??I1=2&I2=1&intId=60. Accessed January 9, 2007.
8. British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. A national clinical guideline. Thorax 2003;58:i1-i94.
1. National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma Update on Selected Topics—2002. National Asthma Education and Prevention Program. J Allergy Clin Immunol 2002;110:S141-S219.
2. Long-term effects of budesonide or nedocromil in children with asthma. The Childhood Asthma Management Program Research Group. N Engl J Med 2000;343:1054-1063.
3. Pauwels RA, Pedersen S, Busse WW, et al. START Investigators Group. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003;361:1071-1076.
4. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild-to-moderate asthma. The American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. J Allergy Clin Immunol 1998;101:14-23.
5. Ducharme FM, Salvio F, Ducharme F. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children (Cochrane review). In: The Cochrane Library. 2006 Issue 2. Chichester, UK: John Wiley and Sons, Ltd.
6. O’byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med 2001;164:1392-1397.
7. The Global Initiative for Asthma. Guidelines and Resources: 2005 Update. Available at: www.ginasthma.com/Guidelineitem.asp??I1=2&I2=1&intId=60. Accessed January 9, 2007.
8. British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. A national clinical guideline. Thorax 2003;58:i1-i94.
Evidence-based answers from the Family Physicians Inquiries Network
Avoid confusion over terms when billing McCall culdoplasty ... Complete and transvaginal US scan must be specified
Your code choices are:
58263 Vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s), and/or ovary(s), with repair of enterocele
58270 Vaginal hysterectomy, for uterus 250 g or less; with repair of enterocele
58292 Vaginal hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s), with repair of enterocele
58294 Vaginal hysterectomy, for uterus greater than 250 g; with repair of enterocele
Don’t blame your billing staff if this is what occurred. The term “McCall culdoplasty” appears nowhere in the CPT book, so your billers would need to know that you actually performed an enterocele repair.
Correctly communicating what you did is an important step in getting the claim paid in a timely manner. Refile with the correct code!
Read a description of the technique of McCall culdoplasty.
Complete and transvaginal US scan must be specified
Your code choices are:
58263 Vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s), and/or ovary(s), with repair of enterocele
58270 Vaginal hysterectomy, for uterus 250 g or less; with repair of enterocele
58292 Vaginal hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s), with repair of enterocele
58294 Vaginal hysterectomy, for uterus greater than 250 g; with repair of enterocele
Don’t blame your billing staff if this is what occurred. The term “McCall culdoplasty” appears nowhere in the CPT book, so your billers would need to know that you actually performed an enterocele repair.
Correctly communicating what you did is an important step in getting the claim paid in a timely manner. Refile with the correct code!
Read a description of the technique of McCall culdoplasty.
Complete and transvaginal US scan must be specified
Your code choices are:
58263 Vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s), and/or ovary(s), with repair of enterocele
58270 Vaginal hysterectomy, for uterus 250 g or less; with repair of enterocele
58292 Vaginal hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s), with repair of enterocele
58294 Vaginal hysterectomy, for uterus greater than 250 g; with repair of enterocele
Don’t blame your billing staff if this is what occurred. The term “McCall culdoplasty” appears nowhere in the CPT book, so your billers would need to know that you actually performed an enterocele repair.
Correctly communicating what you did is an important step in getting the claim paid in a timely manner. Refile with the correct code!
Read a description of the technique of McCall culdoplasty.
Complete and transvaginal US scan must be specified