User login
Medical Communities Go Virtual
Throughout history, physicians have formed communities to aid in the dissemination of knowledge, skills, and professional norms. From local physician groups to international societies and conferences, this drive to connect with members of our profession across the globe is timeless. We do so to learn from each other and continue to move the field of medicine forward.
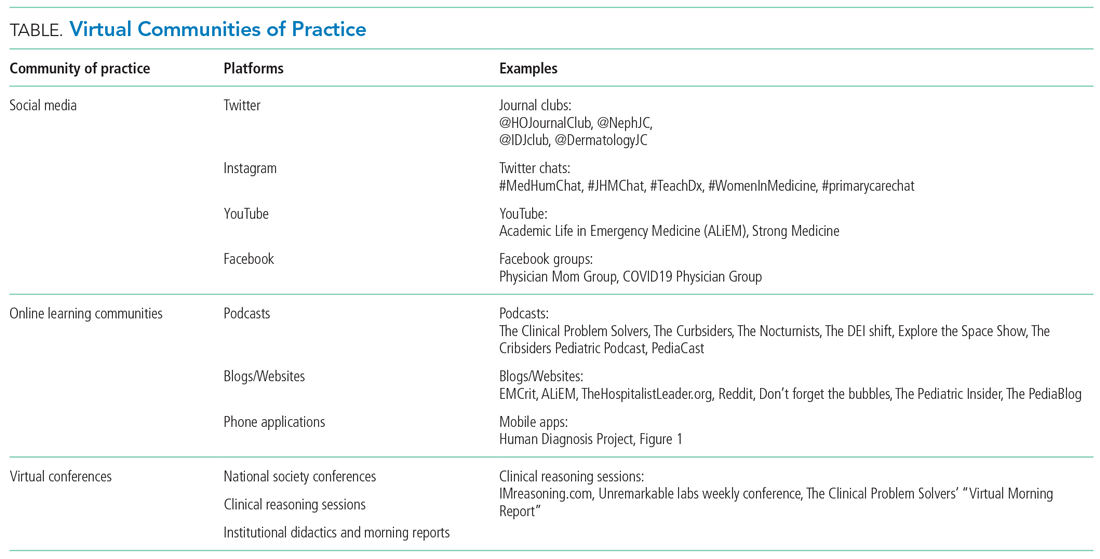
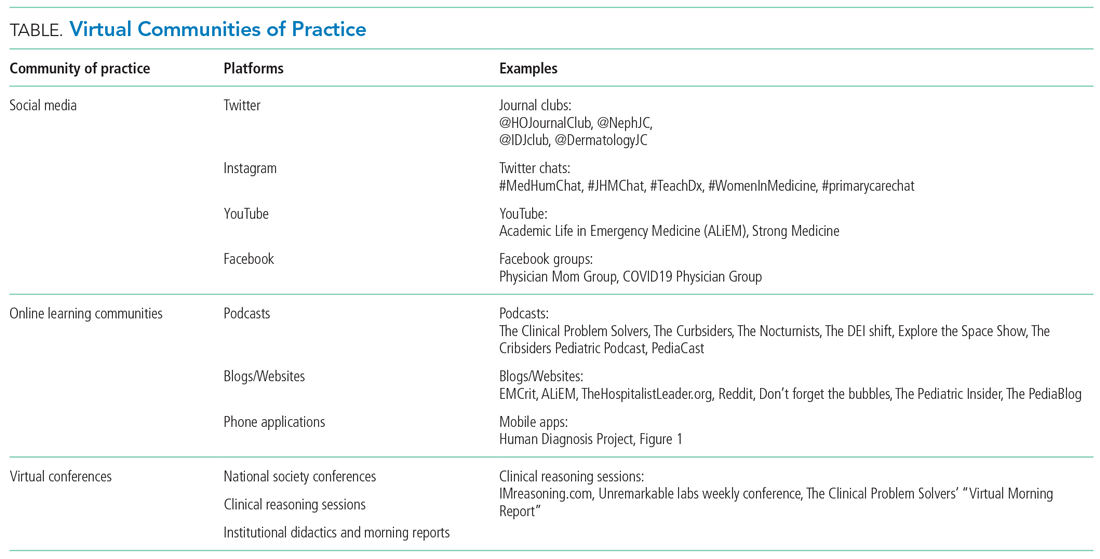
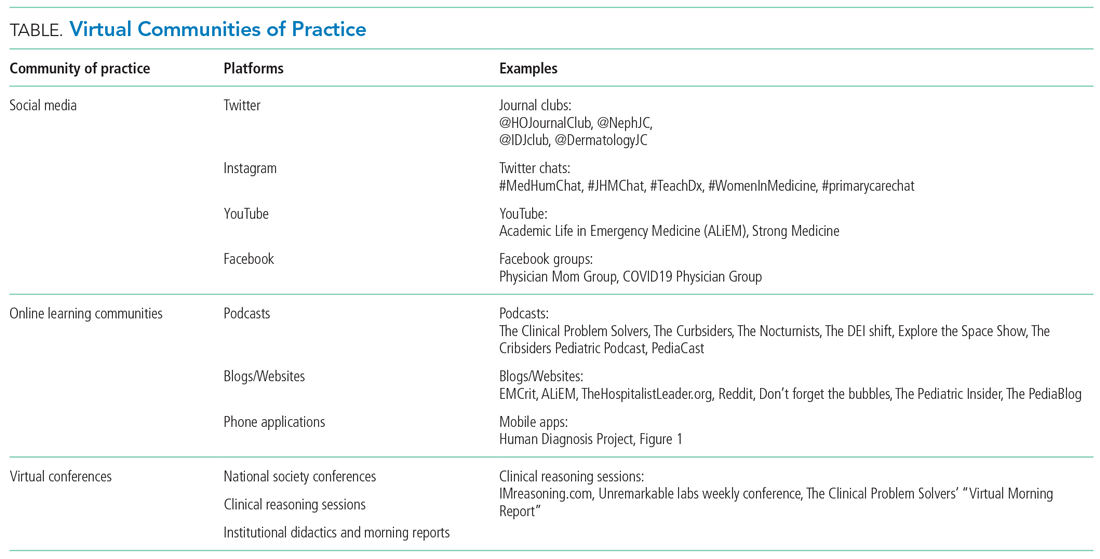
Yet, these communities are being strained by necessary physical distancing required during the COVID-19 pandemic. Many physicians accustomed to a sense of community are now finding themselves surprisingly isolated and alone. Into this distanced landscape, however, new digital groups—specifically social media (SoMe), online learning communities, and virtual conferences—have emerged. We are all active members in virtual communities; all of the authors are team members of The Clinical Problem Solvers podcast and one author of this paper, A.P., has previously served as the medical education lead for the Human Diagnosis Project. Both entities are described later in this article. Here, we provide an overview of these virtual communities and discuss how they have the potential to more equitably and effectively disseminate medical knowledge and education both during and after the COVID-19 pandemic (Table).
SOCIAL MEDIA
Even prior to the COVID-19 pandemic, SoMe—especially Twitter—had become a virtual gathering place where digital colleagues exchange Twitter handles like business cards.1,2 They celebrate each other’s achievements and provide support during difficult times.
Importantly, the format of Twitter tends toward a flattened hierarchy. It is this egalitarian nature that has served SoMe well in its position as a modern learning community. Users from across the experience spectrum engage with and create novel educational content. This often occurs in the form of Tweetorials, or short lessons conveyed over a series of linked tweets. These have gained immense popularity on the platform and are becoming increasingly recognized forms of scholarship.3 Further, case-based lessons have become ubiquitous and are valuable opportunities for users to learn from other members of their digital communities. During the current pandemic, SoMe has become extremely important in the early dissemination and critique of the slew of research on the COVID-19 crisis.4
Beyond its role as an educational platform, SoMe functions as a virtual gathering place for members of the medical community to discuss topics relevant to the field. Subspecialists and researchers have gathered in digital journal clubs (eg, #NephJC, #IDJClub, #BloodandBone) and a number of journals have hosted live Twitter chats covering topics like controversies in clinical practice or professional development (eg, #JHMChat). More recently, social issues affecting the medical field, such as gender equity and the growing antiracism movement, have led to robust discussion on this medium.
Beyond Twitter, many medical professionals gather and exchange ideas on other platforms. Virtual networking and educational groups have arisen using Slack and Facebook.5-7 Trainees and faculty members alike consume and produce content on YouTube, which often serve to teach technical skills.8 Given widespread use of SoMe, we anticipate that the range of platforms utilized by medical professionals will continue to expand in the future.
ONLINE LEARNING COMMUNITIES
There have long existed multiple print and online forums dedicated to the development of clinical skills. These include clinical challenges in medical journals, interactive online cases, and more formal diagnostic education curricula at academic centers.9-11 With the COVID-19 pandemic, it has become more difficult to ensure that trainees have an in-person learning community to discuss and receive feedback. This has led to a wider adoption of application-based clinical exercises, educational podcasts, and curricular innovations to support these virtual efforts.
The Human Diagnosis Project (Human Dx) is a smart-phone application that provides a platform for individuals to submit clinical cases that can be rapidly peer-reviewed and disseminated to the larger user pool. Human Dx is notable for fostering a strong sense of community amongst its users.12,13 Case consumers and case creators are able to engage in further discussion after solving a case, and opportunities for feedback and growth are ample.
Medical education podcasts have taken on greater importance during the pandemic.14,15 Many educators have begun referring their learners towards certain podcasts as in-person learning communities have been put on hold. Medical professionals may appreciate the up-to-date and candid conversations held on many podcasts, which can provide both educationally useful and emotionally sympathetic connections to their distanced peers. Similarly, while academic clinicians previously benefitted from invited grand rounds speakers, they may now find that such expert discussants are most easily accessible through their appearances on podcasts.
As institutions suspended clerkships during the pandemic, many created virtual communities for trainees to engage in diagnostic reasoning and education. They built novel curricula that meld asynchronous learning with online community-based learning.14 Gamified learning tools and quizzes have also been incorporated into these hybrid curricula to help ensure participation of learners within their virtual communities.16,17
VIRTUAL CONFERENCES
Perhaps the most notable advance in digital communities catalyzed by the COVID-19 pandemic has been the increasing reliance on and comfort with video-based software. While many of our clinical, administrative, and social activities have migrated toward these virtual environments, they have also been used for a variety of activities related to education and professional development.
As institutions struggled to adapt to physical distancing, many medical schools and residency programs have moved their regular meetings and conferences to virtual platforms. Similar free and open-access conferences have also emerged, including the “Virtual Morning Report” (VMR) series from The Clinical Problem Solvers podcast, wherein a few individuals are invited to discuss a case on the video conference, with the remainder of the audience contributing via the chat feature.
Beyond the growing popularity of video conferencing for education, these virtual sessions have become their own community. On The Clinical Problem Solvers VMR, many participants, ranging from preclinical students to seasoned attendings, show up on a daily basis and interact with each other as close friends, as do members of more insular institutional sessions (eg, residency run reports). In these strangely isolating times, many of us have experienced comfort in seeing the faces of our friends and colleagues joining us to listen and discuss cases.
Separately, many professional societies have struggled with how to replace their large yearly in-person conferences, which would pose substantial infectious risks were they to be held in person. While many of those scheduled to occur during the early days of the pandemic were canceled or held limited online sessions, the trend towards virtual conference platforms seems to be accelerating. Organizers of the 2020 Conference on Retroviruses and Opportunistic Infections (March 8-11, 2020) decided to convert from an in-person to entirely virtual conference 48 hours before it started. With the benefit of more forewarning, other conferences are planning and exploring best practices to promote networking and advancement of research goals at future academic meetings.18,19
BENEFITS OF VIRTUAL COMMUNITIES
The growing importance of these new digital communities could be viewed as a necessary evolution in the way that we gather and learn from each other. Traditional physician communities were inherently restricted by location, specialty, and hierarchy, thereby limiting the dissemination of knowledge and changes to professional norms. These restrictions could conceivably insulate and promote elite institutions in a fashion that perpetuates the inequalities within global medical systems. Unrestricted and open-access virtual communities, in contrast, have the potential to remove historical barriers and connect first-class mentors with trainees they would never have met otherwise.
Beyond promoting a more equitable distribution of knowledge and resources, these virtual communities are well suited to harness the benefits of group learning. The concept of communities of practice (CoP) refers to groupings of individuals involved in a personal or professional endeavor, with the community facilitating advancement of their own knowledge and skill set. Members of the CoP learn from each other, with more established members passing down essential knowledge and cultural norms. The three main components of CoP are maintaining a social network, a mutual enterprise (eg, a common goal), and a shared repertoire (eg, experiences, languages, etc).
Designing virtual learning spaces with these aspects in mind may allow these communities to function as CoPs. Some strategies include use of chat functions in videoconferences (to promote further dialogue) and development of dedicated sessions for specific subgroups or aims (eg, professional mentorship). The anticipated benefits of integrating virtual CoPs into medical education are notable, as a number of studies have already suggested that they are effective for disseminating knowledge, enhancing social learning, and aiding with professional development.7,20-23 These virtual CoPs continue to evolve, however, and further research is warranted to clarify how best to utilize them in medical education and professional societies.
CONCLUSION
Amidst the tragic loss of lives and financial calamity, the COVID-19 pandemic has also spurred innovation and change in the way health professionals learn and communicate. Going forward, the medical establishment should capitalize on these recent innovations and work to further build, recognize, and foster such digital gathering spaces in order to more equitably and effectively disseminate knowledge and educational resources.
Despite physical distancing, health professionals have grown closer during these past few months. Innovations spurred by the pandemic have made us stronger and more united. Our experience with social media, online learning communities, and virtual conferences suggests the opportunity to grow and evolve from this experience. As Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said in March 2020, “...life is not going to be how it used to be [after the pandemic]…” Let’s hope he’s right.
ACKNOWLEDGMENTS
We thank Reza Manesh, MD, Rabih Geha, MD, and Jack Penner, MD, for their careful review of the manuscript.
1. Markham MJ, Gentile D, Graham DL. Social media for networking, professional development, and patient engagement. Am Soc Clin Oncol Educ Book. 2017;37:782-787. https://doi.org/10.1200/EDBK_180077
2. Melvin L, Chan T. Using Twitter in clinical education and practice. J Grad Med Educ. 2014;6(3):581-582. https://doi.org/10.4300/JGME-D-14-00342.1
3. Breu AC. Why is a cow? Curiosity, Tweetorials, and the return to why. N Engl J Med. 2019;381(12):1097-1098. https://doi.org/10.1056/NEJMp1906790
4. Chan AKM, Nickson CP, Rudolph JW, Lee A, Joynt GM. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020:10.1111/anae.15057. https://doi.org/10.1111/anae.15057
5. Pander T, Pinilla S, Dimitriadis K, Fischer MR. The use of Facebook in medical education--a literature review. GMS Z Med Ausbild. 2014;31(3):Doc33. https://doi.org/10.3205/zma000925
6. Cree-Green M, Carreau AM, Davis SM, et al. Peer mentoring for professional and personal growth in academic medicine. J Investig Med. 2020;68(6):1128-1134. https://doi.org/10.1136/jim-2020-001391
7. Yarris LM, Chan TM, Gottlieb M, Juve AM. Finding your people in the digital age: virtual communities of practice to promote education scholarship. J Grad Med Educ. 2019;11(1):1-5. https://doi.org/10.4300/JGME-D-18-01093.1
8. Sterling M, Leung P, Wright D, Bishop TF. The use of social media in graduate medical education: a systematic review. Acad Med. 2017;92(7):1043-1056. https://doi.org/10.1097/ACM.0000000000001617
9. Manesh R, Dhaliwal G. Digital tools to enhance clinical reasoning. Med Clin North Am. 2018;102(3):559-565. https://doi.org/10.1016/j.mcna.2017.12.015
10. Subramanian A, Connor DM, Berger G, et al. A curriculum for diagnostic reasoning: JGIM’s exercises in clinical reasoning. J Gen Intern Med. 2019;34(3):344-345. https://doi.org/10.1007/s11606-018-4689-y
11. Olson APJ, Singhal G, Dhaliwal G. Diagnosis education - an emerging field. Diagnosis (Berl). 2019;6(2):75-77. https://doi.org/10.1515/dx-2019-0029
12. Chatterjee S, Desai S, Manesh R, Sun J, Nundy S, Wright SM. Assessment of a simulated case-based measurement of physician diagnostic performance. JAMA Netw Open. 2019;2(1):e187006. https://doi.org/10.1001/jamanetworkopen.2018.7006
13. Russell SW, Desai SV, O’Rourke P, et al. The genealogy of teaching clinical reasoning and diagnostic skill: the GEL Study. Diagnosis (Berl). 2020;7(3):197-203. https://doi.org/10.1515/dx-2019-0107
14. Geha R, Dhaliwal G. Pilot virtual clerkship curriculum during the COVID-19 pandemic: podcasts, peers, and problem-solving. Med Educ. 2020;54(9):855-856. https://doi.org/10.1111/medu.14246
15. AlGaeed M, Grewal M, Richardson PK, Leon Guerrero CR. COVID-19: Neurology residents’ perspective. J Clin Neurosci. 2020;78:452-453. https://doi.org/10.1016/j.jocn.2020.05.032
16. Moro C, Stromberga Z. Enhancing variety through gamified, interactive learning experiences. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14251
17. Morawo A, Sun C, Lowden M. Enhancing engagement during live virtual learning using interactive quizzes. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14253
18. Rubinger L, Gazendam A, Ekhtiari S, et al. Maximizing virtual meetings and conferences: a review of best practices. Int Orthop. 2020;44(8):1461-1466. https://doi.org/10.1007/s00264-020-04615-9
19. Woolston C. Learning to love virtual conferences in the coronavirus era. Nature. 2020;582(7810):135-136. https://doi.org/10.1038/d41586-020-01489-0
20. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
21. McLoughlin C, Patel KD, O’Callaghan T, Reeves S. The use of virtual communities of practice to improve interprofessional collaboration and education: findings from an integrated review. J Interprof Care. 2018;32(2):136-142. https://doi.org/10.1080/13561820.2017.1377692
22. Barnett S, Jones SC, Caton T, Iverson D, Bennett S, Robinson L. Implementing a virtual community of practice for family physician training: a mixed-methods case study. J Med Internet Res. 2014;16(3):e83. https://doi.org/10.2196/jmir.3083
23. Healy MG, Traeger LN, Axelsson CGS, et al. NEJM Knowledge+ Question of the Week: a novel virtual learning community effectively utilizing an online discussion forum. Med Teach. 2019;41(11):1270-1276. https://doi.org/10.1080/0142159X.2019.1635685
Throughout history, physicians have formed communities to aid in the dissemination of knowledge, skills, and professional norms. From local physician groups to international societies and conferences, this drive to connect with members of our profession across the globe is timeless. We do so to learn from each other and continue to move the field of medicine forward.
Yet, these communities are being strained by necessary physical distancing required during the COVID-19 pandemic. Many physicians accustomed to a sense of community are now finding themselves surprisingly isolated and alone. Into this distanced landscape, however, new digital groups—specifically social media (SoMe), online learning communities, and virtual conferences—have emerged. We are all active members in virtual communities; all of the authors are team members of The Clinical Problem Solvers podcast and one author of this paper, A.P., has previously served as the medical education lead for the Human Diagnosis Project. Both entities are described later in this article. Here, we provide an overview of these virtual communities and discuss how they have the potential to more equitably and effectively disseminate medical knowledge and education both during and after the COVID-19 pandemic (Table).
SOCIAL MEDIA
Even prior to the COVID-19 pandemic, SoMe—especially Twitter—had become a virtual gathering place where digital colleagues exchange Twitter handles like business cards.1,2 They celebrate each other’s achievements and provide support during difficult times.
Importantly, the format of Twitter tends toward a flattened hierarchy. It is this egalitarian nature that has served SoMe well in its position as a modern learning community. Users from across the experience spectrum engage with and create novel educational content. This often occurs in the form of Tweetorials, or short lessons conveyed over a series of linked tweets. These have gained immense popularity on the platform and are becoming increasingly recognized forms of scholarship.3 Further, case-based lessons have become ubiquitous and are valuable opportunities for users to learn from other members of their digital communities. During the current pandemic, SoMe has become extremely important in the early dissemination and critique of the slew of research on the COVID-19 crisis.4
Beyond its role as an educational platform, SoMe functions as a virtual gathering place for members of the medical community to discuss topics relevant to the field. Subspecialists and researchers have gathered in digital journal clubs (eg, #NephJC, #IDJClub, #BloodandBone) and a number of journals have hosted live Twitter chats covering topics like controversies in clinical practice or professional development (eg, #JHMChat). More recently, social issues affecting the medical field, such as gender equity and the growing antiracism movement, have led to robust discussion on this medium.
Beyond Twitter, many medical professionals gather and exchange ideas on other platforms. Virtual networking and educational groups have arisen using Slack and Facebook.5-7 Trainees and faculty members alike consume and produce content on YouTube, which often serve to teach technical skills.8 Given widespread use of SoMe, we anticipate that the range of platforms utilized by medical professionals will continue to expand in the future.
ONLINE LEARNING COMMUNITIES
There have long existed multiple print and online forums dedicated to the development of clinical skills. These include clinical challenges in medical journals, interactive online cases, and more formal diagnostic education curricula at academic centers.9-11 With the COVID-19 pandemic, it has become more difficult to ensure that trainees have an in-person learning community to discuss and receive feedback. This has led to a wider adoption of application-based clinical exercises, educational podcasts, and curricular innovations to support these virtual efforts.
The Human Diagnosis Project (Human Dx) is a smart-phone application that provides a platform for individuals to submit clinical cases that can be rapidly peer-reviewed and disseminated to the larger user pool. Human Dx is notable for fostering a strong sense of community amongst its users.12,13 Case consumers and case creators are able to engage in further discussion after solving a case, and opportunities for feedback and growth are ample.
Medical education podcasts have taken on greater importance during the pandemic.14,15 Many educators have begun referring their learners towards certain podcasts as in-person learning communities have been put on hold. Medical professionals may appreciate the up-to-date and candid conversations held on many podcasts, which can provide both educationally useful and emotionally sympathetic connections to their distanced peers. Similarly, while academic clinicians previously benefitted from invited grand rounds speakers, they may now find that such expert discussants are most easily accessible through their appearances on podcasts.
As institutions suspended clerkships during the pandemic, many created virtual communities for trainees to engage in diagnostic reasoning and education. They built novel curricula that meld asynchronous learning with online community-based learning.14 Gamified learning tools and quizzes have also been incorporated into these hybrid curricula to help ensure participation of learners within their virtual communities.16,17
VIRTUAL CONFERENCES
Perhaps the most notable advance in digital communities catalyzed by the COVID-19 pandemic has been the increasing reliance on and comfort with video-based software. While many of our clinical, administrative, and social activities have migrated toward these virtual environments, they have also been used for a variety of activities related to education and professional development.
As institutions struggled to adapt to physical distancing, many medical schools and residency programs have moved their regular meetings and conferences to virtual platforms. Similar free and open-access conferences have also emerged, including the “Virtual Morning Report” (VMR) series from The Clinical Problem Solvers podcast, wherein a few individuals are invited to discuss a case on the video conference, with the remainder of the audience contributing via the chat feature.
Beyond the growing popularity of video conferencing for education, these virtual sessions have become their own community. On The Clinical Problem Solvers VMR, many participants, ranging from preclinical students to seasoned attendings, show up on a daily basis and interact with each other as close friends, as do members of more insular institutional sessions (eg, residency run reports). In these strangely isolating times, many of us have experienced comfort in seeing the faces of our friends and colleagues joining us to listen and discuss cases.
Separately, many professional societies have struggled with how to replace their large yearly in-person conferences, which would pose substantial infectious risks were they to be held in person. While many of those scheduled to occur during the early days of the pandemic were canceled or held limited online sessions, the trend towards virtual conference platforms seems to be accelerating. Organizers of the 2020 Conference on Retroviruses and Opportunistic Infections (March 8-11, 2020) decided to convert from an in-person to entirely virtual conference 48 hours before it started. With the benefit of more forewarning, other conferences are planning and exploring best practices to promote networking and advancement of research goals at future academic meetings.18,19
BENEFITS OF VIRTUAL COMMUNITIES
The growing importance of these new digital communities could be viewed as a necessary evolution in the way that we gather and learn from each other. Traditional physician communities were inherently restricted by location, specialty, and hierarchy, thereby limiting the dissemination of knowledge and changes to professional norms. These restrictions could conceivably insulate and promote elite institutions in a fashion that perpetuates the inequalities within global medical systems. Unrestricted and open-access virtual communities, in contrast, have the potential to remove historical barriers and connect first-class mentors with trainees they would never have met otherwise.
Beyond promoting a more equitable distribution of knowledge and resources, these virtual communities are well suited to harness the benefits of group learning. The concept of communities of practice (CoP) refers to groupings of individuals involved in a personal or professional endeavor, with the community facilitating advancement of their own knowledge and skill set. Members of the CoP learn from each other, with more established members passing down essential knowledge and cultural norms. The three main components of CoP are maintaining a social network, a mutual enterprise (eg, a common goal), and a shared repertoire (eg, experiences, languages, etc).
Designing virtual learning spaces with these aspects in mind may allow these communities to function as CoPs. Some strategies include use of chat functions in videoconferences (to promote further dialogue) and development of dedicated sessions for specific subgroups or aims (eg, professional mentorship). The anticipated benefits of integrating virtual CoPs into medical education are notable, as a number of studies have already suggested that they are effective for disseminating knowledge, enhancing social learning, and aiding with professional development.7,20-23 These virtual CoPs continue to evolve, however, and further research is warranted to clarify how best to utilize them in medical education and professional societies.
CONCLUSION
Amidst the tragic loss of lives and financial calamity, the COVID-19 pandemic has also spurred innovation and change in the way health professionals learn and communicate. Going forward, the medical establishment should capitalize on these recent innovations and work to further build, recognize, and foster such digital gathering spaces in order to more equitably and effectively disseminate knowledge and educational resources.
Despite physical distancing, health professionals have grown closer during these past few months. Innovations spurred by the pandemic have made us stronger and more united. Our experience with social media, online learning communities, and virtual conferences suggests the opportunity to grow and evolve from this experience. As Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said in March 2020, “...life is not going to be how it used to be [after the pandemic]…” Let’s hope he’s right.
ACKNOWLEDGMENTS
We thank Reza Manesh, MD, Rabih Geha, MD, and Jack Penner, MD, for their careful review of the manuscript.
Throughout history, physicians have formed communities to aid in the dissemination of knowledge, skills, and professional norms. From local physician groups to international societies and conferences, this drive to connect with members of our profession across the globe is timeless. We do so to learn from each other and continue to move the field of medicine forward.
Yet, these communities are being strained by necessary physical distancing required during the COVID-19 pandemic. Many physicians accustomed to a sense of community are now finding themselves surprisingly isolated and alone. Into this distanced landscape, however, new digital groups—specifically social media (SoMe), online learning communities, and virtual conferences—have emerged. We are all active members in virtual communities; all of the authors are team members of The Clinical Problem Solvers podcast and one author of this paper, A.P., has previously served as the medical education lead for the Human Diagnosis Project. Both entities are described later in this article. Here, we provide an overview of these virtual communities and discuss how they have the potential to more equitably and effectively disseminate medical knowledge and education both during and after the COVID-19 pandemic (Table).
SOCIAL MEDIA
Even prior to the COVID-19 pandemic, SoMe—especially Twitter—had become a virtual gathering place where digital colleagues exchange Twitter handles like business cards.1,2 They celebrate each other’s achievements and provide support during difficult times.
Importantly, the format of Twitter tends toward a flattened hierarchy. It is this egalitarian nature that has served SoMe well in its position as a modern learning community. Users from across the experience spectrum engage with and create novel educational content. This often occurs in the form of Tweetorials, or short lessons conveyed over a series of linked tweets. These have gained immense popularity on the platform and are becoming increasingly recognized forms of scholarship.3 Further, case-based lessons have become ubiquitous and are valuable opportunities for users to learn from other members of their digital communities. During the current pandemic, SoMe has become extremely important in the early dissemination and critique of the slew of research on the COVID-19 crisis.4
Beyond its role as an educational platform, SoMe functions as a virtual gathering place for members of the medical community to discuss topics relevant to the field. Subspecialists and researchers have gathered in digital journal clubs (eg, #NephJC, #IDJClub, #BloodandBone) and a number of journals have hosted live Twitter chats covering topics like controversies in clinical practice or professional development (eg, #JHMChat). More recently, social issues affecting the medical field, such as gender equity and the growing antiracism movement, have led to robust discussion on this medium.
Beyond Twitter, many medical professionals gather and exchange ideas on other platforms. Virtual networking and educational groups have arisen using Slack and Facebook.5-7 Trainees and faculty members alike consume and produce content on YouTube, which often serve to teach technical skills.8 Given widespread use of SoMe, we anticipate that the range of platforms utilized by medical professionals will continue to expand in the future.
ONLINE LEARNING COMMUNITIES
There have long existed multiple print and online forums dedicated to the development of clinical skills. These include clinical challenges in medical journals, interactive online cases, and more formal diagnostic education curricula at academic centers.9-11 With the COVID-19 pandemic, it has become more difficult to ensure that trainees have an in-person learning community to discuss and receive feedback. This has led to a wider adoption of application-based clinical exercises, educational podcasts, and curricular innovations to support these virtual efforts.
The Human Diagnosis Project (Human Dx) is a smart-phone application that provides a platform for individuals to submit clinical cases that can be rapidly peer-reviewed and disseminated to the larger user pool. Human Dx is notable for fostering a strong sense of community amongst its users.12,13 Case consumers and case creators are able to engage in further discussion after solving a case, and opportunities for feedback and growth are ample.
Medical education podcasts have taken on greater importance during the pandemic.14,15 Many educators have begun referring their learners towards certain podcasts as in-person learning communities have been put on hold. Medical professionals may appreciate the up-to-date and candid conversations held on many podcasts, which can provide both educationally useful and emotionally sympathetic connections to their distanced peers. Similarly, while academic clinicians previously benefitted from invited grand rounds speakers, they may now find that such expert discussants are most easily accessible through their appearances on podcasts.
As institutions suspended clerkships during the pandemic, many created virtual communities for trainees to engage in diagnostic reasoning and education. They built novel curricula that meld asynchronous learning with online community-based learning.14 Gamified learning tools and quizzes have also been incorporated into these hybrid curricula to help ensure participation of learners within their virtual communities.16,17
VIRTUAL CONFERENCES
Perhaps the most notable advance in digital communities catalyzed by the COVID-19 pandemic has been the increasing reliance on and comfort with video-based software. While many of our clinical, administrative, and social activities have migrated toward these virtual environments, they have also been used for a variety of activities related to education and professional development.
As institutions struggled to adapt to physical distancing, many medical schools and residency programs have moved their regular meetings and conferences to virtual platforms. Similar free and open-access conferences have also emerged, including the “Virtual Morning Report” (VMR) series from The Clinical Problem Solvers podcast, wherein a few individuals are invited to discuss a case on the video conference, with the remainder of the audience contributing via the chat feature.
Beyond the growing popularity of video conferencing for education, these virtual sessions have become their own community. On The Clinical Problem Solvers VMR, many participants, ranging from preclinical students to seasoned attendings, show up on a daily basis and interact with each other as close friends, as do members of more insular institutional sessions (eg, residency run reports). In these strangely isolating times, many of us have experienced comfort in seeing the faces of our friends and colleagues joining us to listen and discuss cases.
Separately, many professional societies have struggled with how to replace their large yearly in-person conferences, which would pose substantial infectious risks were they to be held in person. While many of those scheduled to occur during the early days of the pandemic were canceled or held limited online sessions, the trend towards virtual conference platforms seems to be accelerating. Organizers of the 2020 Conference on Retroviruses and Opportunistic Infections (March 8-11, 2020) decided to convert from an in-person to entirely virtual conference 48 hours before it started. With the benefit of more forewarning, other conferences are planning and exploring best practices to promote networking and advancement of research goals at future academic meetings.18,19
BENEFITS OF VIRTUAL COMMUNITIES
The growing importance of these new digital communities could be viewed as a necessary evolution in the way that we gather and learn from each other. Traditional physician communities were inherently restricted by location, specialty, and hierarchy, thereby limiting the dissemination of knowledge and changes to professional norms. These restrictions could conceivably insulate and promote elite institutions in a fashion that perpetuates the inequalities within global medical systems. Unrestricted and open-access virtual communities, in contrast, have the potential to remove historical barriers and connect first-class mentors with trainees they would never have met otherwise.
Beyond promoting a more equitable distribution of knowledge and resources, these virtual communities are well suited to harness the benefits of group learning. The concept of communities of practice (CoP) refers to groupings of individuals involved in a personal or professional endeavor, with the community facilitating advancement of their own knowledge and skill set. Members of the CoP learn from each other, with more established members passing down essential knowledge and cultural norms. The three main components of CoP are maintaining a social network, a mutual enterprise (eg, a common goal), and a shared repertoire (eg, experiences, languages, etc).
Designing virtual learning spaces with these aspects in mind may allow these communities to function as CoPs. Some strategies include use of chat functions in videoconferences (to promote further dialogue) and development of dedicated sessions for specific subgroups or aims (eg, professional mentorship). The anticipated benefits of integrating virtual CoPs into medical education are notable, as a number of studies have already suggested that they are effective for disseminating knowledge, enhancing social learning, and aiding with professional development.7,20-23 These virtual CoPs continue to evolve, however, and further research is warranted to clarify how best to utilize them in medical education and professional societies.
CONCLUSION
Amidst the tragic loss of lives and financial calamity, the COVID-19 pandemic has also spurred innovation and change in the way health professionals learn and communicate. Going forward, the medical establishment should capitalize on these recent innovations and work to further build, recognize, and foster such digital gathering spaces in order to more equitably and effectively disseminate knowledge and educational resources.
Despite physical distancing, health professionals have grown closer during these past few months. Innovations spurred by the pandemic have made us stronger and more united. Our experience with social media, online learning communities, and virtual conferences suggests the opportunity to grow and evolve from this experience. As Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said in March 2020, “...life is not going to be how it used to be [after the pandemic]…” Let’s hope he’s right.
ACKNOWLEDGMENTS
We thank Reza Manesh, MD, Rabih Geha, MD, and Jack Penner, MD, for their careful review of the manuscript.
1. Markham MJ, Gentile D, Graham DL. Social media for networking, professional development, and patient engagement. Am Soc Clin Oncol Educ Book. 2017;37:782-787. https://doi.org/10.1200/EDBK_180077
2. Melvin L, Chan T. Using Twitter in clinical education and practice. J Grad Med Educ. 2014;6(3):581-582. https://doi.org/10.4300/JGME-D-14-00342.1
3. Breu AC. Why is a cow? Curiosity, Tweetorials, and the return to why. N Engl J Med. 2019;381(12):1097-1098. https://doi.org/10.1056/NEJMp1906790
4. Chan AKM, Nickson CP, Rudolph JW, Lee A, Joynt GM. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020:10.1111/anae.15057. https://doi.org/10.1111/anae.15057
5. Pander T, Pinilla S, Dimitriadis K, Fischer MR. The use of Facebook in medical education--a literature review. GMS Z Med Ausbild. 2014;31(3):Doc33. https://doi.org/10.3205/zma000925
6. Cree-Green M, Carreau AM, Davis SM, et al. Peer mentoring for professional and personal growth in academic medicine. J Investig Med. 2020;68(6):1128-1134. https://doi.org/10.1136/jim-2020-001391
7. Yarris LM, Chan TM, Gottlieb M, Juve AM. Finding your people in the digital age: virtual communities of practice to promote education scholarship. J Grad Med Educ. 2019;11(1):1-5. https://doi.org/10.4300/JGME-D-18-01093.1
8. Sterling M, Leung P, Wright D, Bishop TF. The use of social media in graduate medical education: a systematic review. Acad Med. 2017;92(7):1043-1056. https://doi.org/10.1097/ACM.0000000000001617
9. Manesh R, Dhaliwal G. Digital tools to enhance clinical reasoning. Med Clin North Am. 2018;102(3):559-565. https://doi.org/10.1016/j.mcna.2017.12.015
10. Subramanian A, Connor DM, Berger G, et al. A curriculum for diagnostic reasoning: JGIM’s exercises in clinical reasoning. J Gen Intern Med. 2019;34(3):344-345. https://doi.org/10.1007/s11606-018-4689-y
11. Olson APJ, Singhal G, Dhaliwal G. Diagnosis education - an emerging field. Diagnosis (Berl). 2019;6(2):75-77. https://doi.org/10.1515/dx-2019-0029
12. Chatterjee S, Desai S, Manesh R, Sun J, Nundy S, Wright SM. Assessment of a simulated case-based measurement of physician diagnostic performance. JAMA Netw Open. 2019;2(1):e187006. https://doi.org/10.1001/jamanetworkopen.2018.7006
13. Russell SW, Desai SV, O’Rourke P, et al. The genealogy of teaching clinical reasoning and diagnostic skill: the GEL Study. Diagnosis (Berl). 2020;7(3):197-203. https://doi.org/10.1515/dx-2019-0107
14. Geha R, Dhaliwal G. Pilot virtual clerkship curriculum during the COVID-19 pandemic: podcasts, peers, and problem-solving. Med Educ. 2020;54(9):855-856. https://doi.org/10.1111/medu.14246
15. AlGaeed M, Grewal M, Richardson PK, Leon Guerrero CR. COVID-19: Neurology residents’ perspective. J Clin Neurosci. 2020;78:452-453. https://doi.org/10.1016/j.jocn.2020.05.032
16. Moro C, Stromberga Z. Enhancing variety through gamified, interactive learning experiences. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14251
17. Morawo A, Sun C, Lowden M. Enhancing engagement during live virtual learning using interactive quizzes. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14253
18. Rubinger L, Gazendam A, Ekhtiari S, et al. Maximizing virtual meetings and conferences: a review of best practices. Int Orthop. 2020;44(8):1461-1466. https://doi.org/10.1007/s00264-020-04615-9
19. Woolston C. Learning to love virtual conferences in the coronavirus era. Nature. 2020;582(7810):135-136. https://doi.org/10.1038/d41586-020-01489-0
20. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
21. McLoughlin C, Patel KD, O’Callaghan T, Reeves S. The use of virtual communities of practice to improve interprofessional collaboration and education: findings from an integrated review. J Interprof Care. 2018;32(2):136-142. https://doi.org/10.1080/13561820.2017.1377692
22. Barnett S, Jones SC, Caton T, Iverson D, Bennett S, Robinson L. Implementing a virtual community of practice for family physician training: a mixed-methods case study. J Med Internet Res. 2014;16(3):e83. https://doi.org/10.2196/jmir.3083
23. Healy MG, Traeger LN, Axelsson CGS, et al. NEJM Knowledge+ Question of the Week: a novel virtual learning community effectively utilizing an online discussion forum. Med Teach. 2019;41(11):1270-1276. https://doi.org/10.1080/0142159X.2019.1635685
1. Markham MJ, Gentile D, Graham DL. Social media for networking, professional development, and patient engagement. Am Soc Clin Oncol Educ Book. 2017;37:782-787. https://doi.org/10.1200/EDBK_180077
2. Melvin L, Chan T. Using Twitter in clinical education and practice. J Grad Med Educ. 2014;6(3):581-582. https://doi.org/10.4300/JGME-D-14-00342.1
3. Breu AC. Why is a cow? Curiosity, Tweetorials, and the return to why. N Engl J Med. 2019;381(12):1097-1098. https://doi.org/10.1056/NEJMp1906790
4. Chan AKM, Nickson CP, Rudolph JW, Lee A, Joynt GM. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020:10.1111/anae.15057. https://doi.org/10.1111/anae.15057
5. Pander T, Pinilla S, Dimitriadis K, Fischer MR. The use of Facebook in medical education--a literature review. GMS Z Med Ausbild. 2014;31(3):Doc33. https://doi.org/10.3205/zma000925
6. Cree-Green M, Carreau AM, Davis SM, et al. Peer mentoring for professional and personal growth in academic medicine. J Investig Med. 2020;68(6):1128-1134. https://doi.org/10.1136/jim-2020-001391
7. Yarris LM, Chan TM, Gottlieb M, Juve AM. Finding your people in the digital age: virtual communities of practice to promote education scholarship. J Grad Med Educ. 2019;11(1):1-5. https://doi.org/10.4300/JGME-D-18-01093.1
8. Sterling M, Leung P, Wright D, Bishop TF. The use of social media in graduate medical education: a systematic review. Acad Med. 2017;92(7):1043-1056. https://doi.org/10.1097/ACM.0000000000001617
9. Manesh R, Dhaliwal G. Digital tools to enhance clinical reasoning. Med Clin North Am. 2018;102(3):559-565. https://doi.org/10.1016/j.mcna.2017.12.015
10. Subramanian A, Connor DM, Berger G, et al. A curriculum for diagnostic reasoning: JGIM’s exercises in clinical reasoning. J Gen Intern Med. 2019;34(3):344-345. https://doi.org/10.1007/s11606-018-4689-y
11. Olson APJ, Singhal G, Dhaliwal G. Diagnosis education - an emerging field. Diagnosis (Berl). 2019;6(2):75-77. https://doi.org/10.1515/dx-2019-0029
12. Chatterjee S, Desai S, Manesh R, Sun J, Nundy S, Wright SM. Assessment of a simulated case-based measurement of physician diagnostic performance. JAMA Netw Open. 2019;2(1):e187006. https://doi.org/10.1001/jamanetworkopen.2018.7006
13. Russell SW, Desai SV, O’Rourke P, et al. The genealogy of teaching clinical reasoning and diagnostic skill: the GEL Study. Diagnosis (Berl). 2020;7(3):197-203. https://doi.org/10.1515/dx-2019-0107
14. Geha R, Dhaliwal G. Pilot virtual clerkship curriculum during the COVID-19 pandemic: podcasts, peers, and problem-solving. Med Educ. 2020;54(9):855-856. https://doi.org/10.1111/medu.14246
15. AlGaeed M, Grewal M, Richardson PK, Leon Guerrero CR. COVID-19: Neurology residents’ perspective. J Clin Neurosci. 2020;78:452-453. https://doi.org/10.1016/j.jocn.2020.05.032
16. Moro C, Stromberga Z. Enhancing variety through gamified, interactive learning experiences. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14251
17. Morawo A, Sun C, Lowden M. Enhancing engagement during live virtual learning using interactive quizzes. Med Educ. 2020. Online ahead of print. https://doi.org/10.1111/medu.14253
18. Rubinger L, Gazendam A, Ekhtiari S, et al. Maximizing virtual meetings and conferences: a review of best practices. Int Orthop. 2020;44(8):1461-1466. https://doi.org/10.1007/s00264-020-04615-9
19. Woolston C. Learning to love virtual conferences in the coronavirus era. Nature. 2020;582(7810):135-136. https://doi.org/10.1038/d41586-020-01489-0
20. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
21. McLoughlin C, Patel KD, O’Callaghan T, Reeves S. The use of virtual communities of practice to improve interprofessional collaboration and education: findings from an integrated review. J Interprof Care. 2018;32(2):136-142. https://doi.org/10.1080/13561820.2017.1377692
22. Barnett S, Jones SC, Caton T, Iverson D, Bennett S, Robinson L. Implementing a virtual community of practice for family physician training: a mixed-methods case study. J Med Internet Res. 2014;16(3):e83. https://doi.org/10.2196/jmir.3083
23. Healy MG, Traeger LN, Axelsson CGS, et al. NEJM Knowledge+ Question of the Week: a novel virtual learning community effectively utilizing an online discussion forum. Med Teach. 2019;41(11):1270-1276. https://doi.org/10.1080/0142159X.2019.1635685
© 2020 Society of Hospital Medicine
Converging Crises: Caring for Hospitalized Adults With Substance Use Disorder in the Time of COVID-19
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
© 2020 Society of Hospital Medicine
Shifting Duties of Children’s Hospitals During the COVID-19 Pandemic
Public health emergencies may require shifting from conventional to contingency and ultimately to crisis standards of care, which prompts consideration of needs and resources across hospital systems.1,2 Within conventional care contexts, institutions have their usual resources including supplies, staff, and space and are able to provide a usual standard of care to patients. As institutions anticipate shortages in an emergency, they may enter a contingency state. In this state, the institution begins to plan for shortages, often by finding alternative uses of supplies, staff, and space that are functionally equivalent but still aiming to conserve resources such as rescheduling elective procedures and using alternative but functionally equivalent personal protective equipment. Still, during this state, institutions are able to provide the usual standard of care.
Under crisis standards of care, resources have reached a level of scarcity or circumstances are such that they do not permit normal operations. In this state, institutions may not be able to meet the usual standard of care. Instead, institutions are expected to provide care that is sufficient given available resources and circumstances. How to utilize scarce resources, however, invokes consideration of the ethical duties of institutions. Despite the likelihood of entering crisis standards of care (CSCs) in the current COVID-19 pandemic, limited ethical guidance exists regarding how institutions should relate to each other in a crisis. Relevant moral duties during conventional, contingency, and CSCs include duties of rescue, fidelity, solidarity, and justice. As CSCs develop, these duties require limiting elective procedures and instituting triage in certain circumstances, but how this relates to coordination among hospitals is unclear.
We argue that the primary role of pediatric institutions during the COVID-19 pandemic under CSCs is increasing system capacity by regionalization of pediatric care. Under regionalization of care, children’s hospitals that serve as local/regional referral centers would preferentially take all pediatric patients in the region, including those who might normally be admitted to a primarily adult hospital, thereby increasing availability of beds and resources at primarily adult facilities. This maximizes the expertise and resources of pediatric institutions and avoids unnecessary harm to all patients by mitigating shortages before any hospital faces conditions in which they need to invoke triage procedures. General hospitals should transfer pediatric patients to pediatric institutions and should consider transfer of patients and/or resources between regional institutions, which helps avoid triage conditions until all accessible resources are in use.
GENERAL DUTIES
Institutions are prominent moral actors with duties to patients extending beyond those of providers.3
The duty to treat includes two subsidiary duties. First, the duty of rescue has a special role in emergencies, requiring providers to intervene with those helpless without assistance.4-6 For children’s hospitals, this means providing care for children in the region who cannot receive needed care elsewhere. Second, the duty of fidelity requires promoting patients’ good, including giving precedence to patients with established treatment relationships.7
Institutions also have a duty of solidarity.8 Institutions must recognize they are bound together to care for the broader community and should work in tandem.9 Solidarity encompasses the duty of stewardship—responsibly using resources to mitigate shortages; this duty sometimes requires subsuming patient, provider, or institutional needs for overall community benefit.
Finally, institutions have duties of justice,2 to provide fair and equitable care with transparency and trustworthiness. Justice requires that institutions ensure shifting to CSCs does not disfavor already disadvantaged groups.10
APPLICATION AND ALTERATION OF DUTIES
Public health emergencies strain health care resources in ways that hinder providing usual standards of care. Public health ethics guide healthcare systems during contingency or CSCs in ethically grounded approaches to mitigate shortages and allocate resources.1,2 We consider how duties evolve from conventional care to CSCs, with a focus on actions to meet institutional duties under changing circumstances.
Conventional Care
Ordinarily, institutions provide usual standards of care, which follow typical operations. Interactions between institutions and providers rely on basic ethical principles, including primacy of patient welfare, autonomy, and social justice. A degree of redundancy allows institutions to meet duties of rescue, fidelity, solidarity, and justice even with increased demand. The duty to treat is primary but requires balancing duties to rescue with fiduciary duties. Thus, if the institution were near capacity and a decision is needed about which patient to accept in transfer, avoiding irreversible harm to a previously unknown patient who could not receive adequate care in the community should take precedence over accepting an established patient who could receive adequate care elsewhere. If neither patient could receive adequate care elsewhere, the patient known to the children’s hospital should be accepted, under the duty of fidelity. Fidelity also requires that patients currently admitted continue to receive treatment. Justice requires fair and equitable treatment of patients, without consideration of morally irrelevant features (eg, race or immigration status).
Contingency Care
Contingency care begins when a public health emergency introduces strains on hospital resources.1,2,11 As long as typical or alternative resources last, adaptations in care have minimal effects on quality, and the duties of rescue, fidelity, and justice mirror conventional care; however, operations begin to shift to recognize greater duties of solidarity. In the COVID-19 pandemic, given their missions to provide specialized care for children, pediatric hospitals can meet their duty to treat by accepting patients who might otherwise receive care elsewhere. Children’s hospitals should consider accepting any child for which they have capacity to help decompress other systems (eg, liberating beds for more adults at other institutions). Children’s hospitals should also continue to preferentially admit children requiring tertiary care (eg, neonates requiring subspecialty surgery), which respects the duty of rescue.
The duty of solidarity supports strategic sharing and stewarding of resources, including personal protective equipment, ventilators, and staff. Strategies might include postponing elective procedures, repurposing facilities, or limiting staff entering isolation rooms; such alterations to standard care require careful discussions with providers to anticipate negative consequences, ensure safe practices, and plan for reassessment.
The duty of rescue requires maintaining ability to care for patients who cannot receive adequate care elsewhere. Institutions can meet this duty by reserving a small number of intensive care and general beds to care for patients needing emergent specialty care.
Crisis Standards of Care
Under CSCs, resources are insufficient to maintain usual standards of care and mitigation attempts no longer suffice. Scarcity demands greater duties of solidarity, reducing attention to some individuals to promote the community good. To meet duties of solidarity, institutions should prepare for triage after exhausting efforts to preserve system resources.
During a pandemic such as COVID-19 that primarily affects adults, pediatric resources should be consolidated by transferring children to regional pediatric facilities. Without transfer, children who present to primarily adult facilities, where resources are more strained given the higher burden of disease in adults, may otherwise be subject to triaging of scarce resources at the adult facility. But, no child should have care determined by any hospital’s triage system if any pediatric bed is available within a region, and if pediatric resources are regionalized, children will be less likely to face triage at primarily adult facilities unless the entire system has reached capacity. In addition to regionalization, children’s hospitals may also face requests to accept adult patients or share equipment and/or staff with adult facilities; when these actions do not compromise the capacity of the pediatric institution to provide care to children, institutions should consider them.12 However, pediatric institutions can best meet the duty of solidarity by expanding regional capacity through freeing up resources in general hospitals, including beds, ventilators, and staffing usable for adults, preventing all hospitals from needing to triage. If triage is necessary because the entire system has reached capacity, triage should also take place at children’s hospitals, in respect of solidarity, to optimize this community resource.
Under CSCs, significant practice variation in triage policies may occur. Regional institutions may individually employ triage policies during crisis standards of care and deny critical care resources to some individuals who might receive them in noncrisis times, when there isn’t such scarcity. Minimizing denials across a region requires collaboration between centers to ensure solidarity. Processes should be fair and equitable. Justice entails ensuring consistency in allocation criteria, with differences prioritizing those least well off. Triage teams in a region should use consistent, aligned processes so that similarly situated patients have equitable access to resources and care across centers. However, triaging pediatric and adult patients together could disadvantage children (eg, priority given to health workers); moreover, illness severity measures for infants/children differ from those applicable to adults, which makes equivalent scoring for allocation challenging.13 Some resources are specific to pediatric or adult care. Therefore, it may be necessary to separate pediatric and adult allocation processes.
Triage criteria must not discriminate based on morally irrelevant criteria, such as sex, race/ethnicity, or disability.1 Institutions using “objective” scoring systems for morbidity and mortality should acknowledge that these systems could disadvantage marginalized populations with higher rates of chronic conditions resulting from systemic inequities.
A commitment to justice mandates that no patient should be triaged if the required resources (eg, ventilators) are available at a regional hospital and transfer is feasible. Transfer should occur across all regional hospitals, not just partners within hospital networks. Facilitating transfers requires institutions to engage in close communication. If no centralized external system exists, a group of individuals with knowledge of inpatient resources—but without direct care duties—should provide coordination.
Because CSCs are so different from conventional standards, institutions should collect data on regionalization and triage protocols. Recognition of inequitable outcomes may necessitate changing scoring criteria or reveal disproportionate burdens on vulnerable populations.
To maintain public trust and promote justice, institutions must be transparent regarding triage policies and procedures for CSCs. These should be available for public review, revised with public input, and readily available once finalized.
POTENTIAL BARRIERS TO IMPLEMENTATION
Despite the ethical justification for regional coordination of care and resources, there are multiple barriers to implementation. Providers and families may hesitate to disturb continuity of care at medical homes. Organizations may have financial disincentives to transfer long-term patients to new institutions. Openness with patients and families regarding the temporary nature of transfers and plans to return to their usual care may help. Granting temporary privileges at recipient institutions for providers to continue seeing their patients may lessen discontinuity. Solidarity in public health emergencies requires all institutions to compromise their own interests to some degree.
Similarly, barriers in achieving consistency across institutional triage policies may arise. Allocation strategies embody multiple values, for example, regarding quality of life or contributions of essential workers. Resolution of these value differences may prove difficult.
CONCLUSION
In the current COVID-19 pandemic, an ethical approach to CSCs necessitates coordination to align available resources at the regional, rather than institutional, level to avoid triage at individual institutions. Pediatric regionalization of care is the first step in freeing up system capacity for adults. Solidarity rises in importance, but must be balanced by duties of rescue, fidelity, and justice so that pediatric institutions continue to care for children with urgent needs requiring pediatric expertise.
Disclosures
Dr Paquette reported funding under the Pediatric Critical Care and Trauma Scientist Development Program, NICHD K12HDO47349 and NICHD Loan Repayment Program L40 HD089260. Dr Derrington is a director at large for the American Society of Bioethics and Medical Humanities and had travel expenses reimbursed for the annual conference in 2019. Dr Michelson has received funding from the National Palliative Care Research Center and is a consultant on a National Institutes of Health study that are unrelated to this work. Dr Michelson is also involved in unrelated work supported by the National Alliance for Grieving Children. All other authors declared they have nothing to disclose.
1. Institute of Medicine; Board on Health Sciences Policy; Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. Hanfling D, Altevogt BM, Viswanathan K, Gostin LO, eds. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. National Academies Press; 2012.
2. Berlinger N, Wynia M, Powell T, et al. Ethical Framework for Health Care Institutions & Guidelines for Institutional Ethics Services Responding to the Coronavirus Pandemic: Managing Uncertainty, Safeguarding Communities, Guiding Practice. The Hastings Center; March 16, 2020. Accessed June 22, 2020. https://www.thehastingscenter.org/ethicalframeworkcovid19/
3. Goold SD. Trust and the ethics of health care institutions. Hastings Cent Rep. 2001;31(6):26-33.
4. Garrett JR. Collectivizing rescue obligations in bioethics. Am J Bioeth. 2015;15(2):3-11. https://doi.org/10.1080/15265161.2014.990163
5. Furrow BR. Forcing rescue: the landscape of health care provider obligations to treat patients. Health Matrix Clevel. 1993;3(1):31-87.
6. Goodin RE. Protecting the Vulnerable: A Reanalysis of Our Social Responsibilities. University of Chicago Press; 1985.
7. Jecker N. Fidelity to Patients and Resource Constraints. In: Campbell CS, Lustig BA, eds. Duties to Others. Theology and Medicine, vol 4. Springer, Dordrecht; 1994. 293-308. https://doi.org/10.1007/978-94-015-8244-5_18
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Dawson A, Jennings B. The place of solidarity in public health ethics. Public Health Rev. 2012;34:65-79.
10. Rawls J. A Theory of Justice. Belknap Press of Harvard University Press; 1971.
11. Jennings B, Arras J. Ethical Guidance for Public Health Emergency Preparedness and Response: Highlighting Ethics and Values in a Vital Public Health Service. Centers for Disease Control and Prevention. October 30, 2008. Accessed April 16, 2020. https://www.cdc.gov/os/integrity/phethics/docs/white_paper_final_for_website_2012_4_6_12_final_for_web_508_compliant.pdf
12. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Medicine. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
13. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr. 2017;171(10):e172352. https://doi.org/10.1001/jamapediatrics.2017.2352
Public health emergencies may require shifting from conventional to contingency and ultimately to crisis standards of care, which prompts consideration of needs and resources across hospital systems.1,2 Within conventional care contexts, institutions have their usual resources including supplies, staff, and space and are able to provide a usual standard of care to patients. As institutions anticipate shortages in an emergency, they may enter a contingency state. In this state, the institution begins to plan for shortages, often by finding alternative uses of supplies, staff, and space that are functionally equivalent but still aiming to conserve resources such as rescheduling elective procedures and using alternative but functionally equivalent personal protective equipment. Still, during this state, institutions are able to provide the usual standard of care.
Under crisis standards of care, resources have reached a level of scarcity or circumstances are such that they do not permit normal operations. In this state, institutions may not be able to meet the usual standard of care. Instead, institutions are expected to provide care that is sufficient given available resources and circumstances. How to utilize scarce resources, however, invokes consideration of the ethical duties of institutions. Despite the likelihood of entering crisis standards of care (CSCs) in the current COVID-19 pandemic, limited ethical guidance exists regarding how institutions should relate to each other in a crisis. Relevant moral duties during conventional, contingency, and CSCs include duties of rescue, fidelity, solidarity, and justice. As CSCs develop, these duties require limiting elective procedures and instituting triage in certain circumstances, but how this relates to coordination among hospitals is unclear.
We argue that the primary role of pediatric institutions during the COVID-19 pandemic under CSCs is increasing system capacity by regionalization of pediatric care. Under regionalization of care, children’s hospitals that serve as local/regional referral centers would preferentially take all pediatric patients in the region, including those who might normally be admitted to a primarily adult hospital, thereby increasing availability of beds and resources at primarily adult facilities. This maximizes the expertise and resources of pediatric institutions and avoids unnecessary harm to all patients by mitigating shortages before any hospital faces conditions in which they need to invoke triage procedures. General hospitals should transfer pediatric patients to pediatric institutions and should consider transfer of patients and/or resources between regional institutions, which helps avoid triage conditions until all accessible resources are in use.
GENERAL DUTIES
Institutions are prominent moral actors with duties to patients extending beyond those of providers.3
The duty to treat includes two subsidiary duties. First, the duty of rescue has a special role in emergencies, requiring providers to intervene with those helpless without assistance.4-6 For children’s hospitals, this means providing care for children in the region who cannot receive needed care elsewhere. Second, the duty of fidelity requires promoting patients’ good, including giving precedence to patients with established treatment relationships.7
Institutions also have a duty of solidarity.8 Institutions must recognize they are bound together to care for the broader community and should work in tandem.9 Solidarity encompasses the duty of stewardship—responsibly using resources to mitigate shortages; this duty sometimes requires subsuming patient, provider, or institutional needs for overall community benefit.
Finally, institutions have duties of justice,2 to provide fair and equitable care with transparency and trustworthiness. Justice requires that institutions ensure shifting to CSCs does not disfavor already disadvantaged groups.10
APPLICATION AND ALTERATION OF DUTIES
Public health emergencies strain health care resources in ways that hinder providing usual standards of care. Public health ethics guide healthcare systems during contingency or CSCs in ethically grounded approaches to mitigate shortages and allocate resources.1,2 We consider how duties evolve from conventional care to CSCs, with a focus on actions to meet institutional duties under changing circumstances.
Conventional Care
Ordinarily, institutions provide usual standards of care, which follow typical operations. Interactions between institutions and providers rely on basic ethical principles, including primacy of patient welfare, autonomy, and social justice. A degree of redundancy allows institutions to meet duties of rescue, fidelity, solidarity, and justice even with increased demand. The duty to treat is primary but requires balancing duties to rescue with fiduciary duties. Thus, if the institution were near capacity and a decision is needed about which patient to accept in transfer, avoiding irreversible harm to a previously unknown patient who could not receive adequate care in the community should take precedence over accepting an established patient who could receive adequate care elsewhere. If neither patient could receive adequate care elsewhere, the patient known to the children’s hospital should be accepted, under the duty of fidelity. Fidelity also requires that patients currently admitted continue to receive treatment. Justice requires fair and equitable treatment of patients, without consideration of morally irrelevant features (eg, race or immigration status).
Contingency Care
Contingency care begins when a public health emergency introduces strains on hospital resources.1,2,11 As long as typical or alternative resources last, adaptations in care have minimal effects on quality, and the duties of rescue, fidelity, and justice mirror conventional care; however, operations begin to shift to recognize greater duties of solidarity. In the COVID-19 pandemic, given their missions to provide specialized care for children, pediatric hospitals can meet their duty to treat by accepting patients who might otherwise receive care elsewhere. Children’s hospitals should consider accepting any child for which they have capacity to help decompress other systems (eg, liberating beds for more adults at other institutions). Children’s hospitals should also continue to preferentially admit children requiring tertiary care (eg, neonates requiring subspecialty surgery), which respects the duty of rescue.
The duty of solidarity supports strategic sharing and stewarding of resources, including personal protective equipment, ventilators, and staff. Strategies might include postponing elective procedures, repurposing facilities, or limiting staff entering isolation rooms; such alterations to standard care require careful discussions with providers to anticipate negative consequences, ensure safe practices, and plan for reassessment.
The duty of rescue requires maintaining ability to care for patients who cannot receive adequate care elsewhere. Institutions can meet this duty by reserving a small number of intensive care and general beds to care for patients needing emergent specialty care.
Crisis Standards of Care
Under CSCs, resources are insufficient to maintain usual standards of care and mitigation attempts no longer suffice. Scarcity demands greater duties of solidarity, reducing attention to some individuals to promote the community good. To meet duties of solidarity, institutions should prepare for triage after exhausting efforts to preserve system resources.
During a pandemic such as COVID-19 that primarily affects adults, pediatric resources should be consolidated by transferring children to regional pediatric facilities. Without transfer, children who present to primarily adult facilities, where resources are more strained given the higher burden of disease in adults, may otherwise be subject to triaging of scarce resources at the adult facility. But, no child should have care determined by any hospital’s triage system if any pediatric bed is available within a region, and if pediatric resources are regionalized, children will be less likely to face triage at primarily adult facilities unless the entire system has reached capacity. In addition to regionalization, children’s hospitals may also face requests to accept adult patients or share equipment and/or staff with adult facilities; when these actions do not compromise the capacity of the pediatric institution to provide care to children, institutions should consider them.12 However, pediatric institutions can best meet the duty of solidarity by expanding regional capacity through freeing up resources in general hospitals, including beds, ventilators, and staffing usable for adults, preventing all hospitals from needing to triage. If triage is necessary because the entire system has reached capacity, triage should also take place at children’s hospitals, in respect of solidarity, to optimize this community resource.
Under CSCs, significant practice variation in triage policies may occur. Regional institutions may individually employ triage policies during crisis standards of care and deny critical care resources to some individuals who might receive them in noncrisis times, when there isn’t such scarcity. Minimizing denials across a region requires collaboration between centers to ensure solidarity. Processes should be fair and equitable. Justice entails ensuring consistency in allocation criteria, with differences prioritizing those least well off. Triage teams in a region should use consistent, aligned processes so that similarly situated patients have equitable access to resources and care across centers. However, triaging pediatric and adult patients together could disadvantage children (eg, priority given to health workers); moreover, illness severity measures for infants/children differ from those applicable to adults, which makes equivalent scoring for allocation challenging.13 Some resources are specific to pediatric or adult care. Therefore, it may be necessary to separate pediatric and adult allocation processes.
Triage criteria must not discriminate based on morally irrelevant criteria, such as sex, race/ethnicity, or disability.1 Institutions using “objective” scoring systems for morbidity and mortality should acknowledge that these systems could disadvantage marginalized populations with higher rates of chronic conditions resulting from systemic inequities.
A commitment to justice mandates that no patient should be triaged if the required resources (eg, ventilators) are available at a regional hospital and transfer is feasible. Transfer should occur across all regional hospitals, not just partners within hospital networks. Facilitating transfers requires institutions to engage in close communication. If no centralized external system exists, a group of individuals with knowledge of inpatient resources—but without direct care duties—should provide coordination.
Because CSCs are so different from conventional standards, institutions should collect data on regionalization and triage protocols. Recognition of inequitable outcomes may necessitate changing scoring criteria or reveal disproportionate burdens on vulnerable populations.
To maintain public trust and promote justice, institutions must be transparent regarding triage policies and procedures for CSCs. These should be available for public review, revised with public input, and readily available once finalized.
POTENTIAL BARRIERS TO IMPLEMENTATION
Despite the ethical justification for regional coordination of care and resources, there are multiple barriers to implementation. Providers and families may hesitate to disturb continuity of care at medical homes. Organizations may have financial disincentives to transfer long-term patients to new institutions. Openness with patients and families regarding the temporary nature of transfers and plans to return to their usual care may help. Granting temporary privileges at recipient institutions for providers to continue seeing their patients may lessen discontinuity. Solidarity in public health emergencies requires all institutions to compromise their own interests to some degree.
Similarly, barriers in achieving consistency across institutional triage policies may arise. Allocation strategies embody multiple values, for example, regarding quality of life or contributions of essential workers. Resolution of these value differences may prove difficult.
CONCLUSION
In the current COVID-19 pandemic, an ethical approach to CSCs necessitates coordination to align available resources at the regional, rather than institutional, level to avoid triage at individual institutions. Pediatric regionalization of care is the first step in freeing up system capacity for adults. Solidarity rises in importance, but must be balanced by duties of rescue, fidelity, and justice so that pediatric institutions continue to care for children with urgent needs requiring pediatric expertise.
Disclosures
Dr Paquette reported funding under the Pediatric Critical Care and Trauma Scientist Development Program, NICHD K12HDO47349 and NICHD Loan Repayment Program L40 HD089260. Dr Derrington is a director at large for the American Society of Bioethics and Medical Humanities and had travel expenses reimbursed for the annual conference in 2019. Dr Michelson has received funding from the National Palliative Care Research Center and is a consultant on a National Institutes of Health study that are unrelated to this work. Dr Michelson is also involved in unrelated work supported by the National Alliance for Grieving Children. All other authors declared they have nothing to disclose.
Public health emergencies may require shifting from conventional to contingency and ultimately to crisis standards of care, which prompts consideration of needs and resources across hospital systems.1,2 Within conventional care contexts, institutions have their usual resources including supplies, staff, and space and are able to provide a usual standard of care to patients. As institutions anticipate shortages in an emergency, they may enter a contingency state. In this state, the institution begins to plan for shortages, often by finding alternative uses of supplies, staff, and space that are functionally equivalent but still aiming to conserve resources such as rescheduling elective procedures and using alternative but functionally equivalent personal protective equipment. Still, during this state, institutions are able to provide the usual standard of care.
Under crisis standards of care, resources have reached a level of scarcity or circumstances are such that they do not permit normal operations. In this state, institutions may not be able to meet the usual standard of care. Instead, institutions are expected to provide care that is sufficient given available resources and circumstances. How to utilize scarce resources, however, invokes consideration of the ethical duties of institutions. Despite the likelihood of entering crisis standards of care (CSCs) in the current COVID-19 pandemic, limited ethical guidance exists regarding how institutions should relate to each other in a crisis. Relevant moral duties during conventional, contingency, and CSCs include duties of rescue, fidelity, solidarity, and justice. As CSCs develop, these duties require limiting elective procedures and instituting triage in certain circumstances, but how this relates to coordination among hospitals is unclear.
We argue that the primary role of pediatric institutions during the COVID-19 pandemic under CSCs is increasing system capacity by regionalization of pediatric care. Under regionalization of care, children’s hospitals that serve as local/regional referral centers would preferentially take all pediatric patients in the region, including those who might normally be admitted to a primarily adult hospital, thereby increasing availability of beds and resources at primarily adult facilities. This maximizes the expertise and resources of pediatric institutions and avoids unnecessary harm to all patients by mitigating shortages before any hospital faces conditions in which they need to invoke triage procedures. General hospitals should transfer pediatric patients to pediatric institutions and should consider transfer of patients and/or resources between regional institutions, which helps avoid triage conditions until all accessible resources are in use.
GENERAL DUTIES
Institutions are prominent moral actors with duties to patients extending beyond those of providers.3
The duty to treat includes two subsidiary duties. First, the duty of rescue has a special role in emergencies, requiring providers to intervene with those helpless without assistance.4-6 For children’s hospitals, this means providing care for children in the region who cannot receive needed care elsewhere. Second, the duty of fidelity requires promoting patients’ good, including giving precedence to patients with established treatment relationships.7
Institutions also have a duty of solidarity.8 Institutions must recognize they are bound together to care for the broader community and should work in tandem.9 Solidarity encompasses the duty of stewardship—responsibly using resources to mitigate shortages; this duty sometimes requires subsuming patient, provider, or institutional needs for overall community benefit.
Finally, institutions have duties of justice,2 to provide fair and equitable care with transparency and trustworthiness. Justice requires that institutions ensure shifting to CSCs does not disfavor already disadvantaged groups.10
APPLICATION AND ALTERATION OF DUTIES
Public health emergencies strain health care resources in ways that hinder providing usual standards of care. Public health ethics guide healthcare systems during contingency or CSCs in ethically grounded approaches to mitigate shortages and allocate resources.1,2 We consider how duties evolve from conventional care to CSCs, with a focus on actions to meet institutional duties under changing circumstances.
Conventional Care
Ordinarily, institutions provide usual standards of care, which follow typical operations. Interactions between institutions and providers rely on basic ethical principles, including primacy of patient welfare, autonomy, and social justice. A degree of redundancy allows institutions to meet duties of rescue, fidelity, solidarity, and justice even with increased demand. The duty to treat is primary but requires balancing duties to rescue with fiduciary duties. Thus, if the institution were near capacity and a decision is needed about which patient to accept in transfer, avoiding irreversible harm to a previously unknown patient who could not receive adequate care in the community should take precedence over accepting an established patient who could receive adequate care elsewhere. If neither patient could receive adequate care elsewhere, the patient known to the children’s hospital should be accepted, under the duty of fidelity. Fidelity also requires that patients currently admitted continue to receive treatment. Justice requires fair and equitable treatment of patients, without consideration of morally irrelevant features (eg, race or immigration status).
Contingency Care
Contingency care begins when a public health emergency introduces strains on hospital resources.1,2,11 As long as typical or alternative resources last, adaptations in care have minimal effects on quality, and the duties of rescue, fidelity, and justice mirror conventional care; however, operations begin to shift to recognize greater duties of solidarity. In the COVID-19 pandemic, given their missions to provide specialized care for children, pediatric hospitals can meet their duty to treat by accepting patients who might otherwise receive care elsewhere. Children’s hospitals should consider accepting any child for which they have capacity to help decompress other systems (eg, liberating beds for more adults at other institutions). Children’s hospitals should also continue to preferentially admit children requiring tertiary care (eg, neonates requiring subspecialty surgery), which respects the duty of rescue.
The duty of solidarity supports strategic sharing and stewarding of resources, including personal protective equipment, ventilators, and staff. Strategies might include postponing elective procedures, repurposing facilities, or limiting staff entering isolation rooms; such alterations to standard care require careful discussions with providers to anticipate negative consequences, ensure safe practices, and plan for reassessment.
The duty of rescue requires maintaining ability to care for patients who cannot receive adequate care elsewhere. Institutions can meet this duty by reserving a small number of intensive care and general beds to care for patients needing emergent specialty care.
Crisis Standards of Care
Under CSCs, resources are insufficient to maintain usual standards of care and mitigation attempts no longer suffice. Scarcity demands greater duties of solidarity, reducing attention to some individuals to promote the community good. To meet duties of solidarity, institutions should prepare for triage after exhausting efforts to preserve system resources.
During a pandemic such as COVID-19 that primarily affects adults, pediatric resources should be consolidated by transferring children to regional pediatric facilities. Without transfer, children who present to primarily adult facilities, where resources are more strained given the higher burden of disease in adults, may otherwise be subject to triaging of scarce resources at the adult facility. But, no child should have care determined by any hospital’s triage system if any pediatric bed is available within a region, and if pediatric resources are regionalized, children will be less likely to face triage at primarily adult facilities unless the entire system has reached capacity. In addition to regionalization, children’s hospitals may also face requests to accept adult patients or share equipment and/or staff with adult facilities; when these actions do not compromise the capacity of the pediatric institution to provide care to children, institutions should consider them.12 However, pediatric institutions can best meet the duty of solidarity by expanding regional capacity through freeing up resources in general hospitals, including beds, ventilators, and staffing usable for adults, preventing all hospitals from needing to triage. If triage is necessary because the entire system has reached capacity, triage should also take place at children’s hospitals, in respect of solidarity, to optimize this community resource.
Under CSCs, significant practice variation in triage policies may occur. Regional institutions may individually employ triage policies during crisis standards of care and deny critical care resources to some individuals who might receive them in noncrisis times, when there isn’t such scarcity. Minimizing denials across a region requires collaboration between centers to ensure solidarity. Processes should be fair and equitable. Justice entails ensuring consistency in allocation criteria, with differences prioritizing those least well off. Triage teams in a region should use consistent, aligned processes so that similarly situated patients have equitable access to resources and care across centers. However, triaging pediatric and adult patients together could disadvantage children (eg, priority given to health workers); moreover, illness severity measures for infants/children differ from those applicable to adults, which makes equivalent scoring for allocation challenging.13 Some resources are specific to pediatric or adult care. Therefore, it may be necessary to separate pediatric and adult allocation processes.
Triage criteria must not discriminate based on morally irrelevant criteria, such as sex, race/ethnicity, or disability.1 Institutions using “objective” scoring systems for morbidity and mortality should acknowledge that these systems could disadvantage marginalized populations with higher rates of chronic conditions resulting from systemic inequities.
A commitment to justice mandates that no patient should be triaged if the required resources (eg, ventilators) are available at a regional hospital and transfer is feasible. Transfer should occur across all regional hospitals, not just partners within hospital networks. Facilitating transfers requires institutions to engage in close communication. If no centralized external system exists, a group of individuals with knowledge of inpatient resources—but without direct care duties—should provide coordination.
Because CSCs are so different from conventional standards, institutions should collect data on regionalization and triage protocols. Recognition of inequitable outcomes may necessitate changing scoring criteria or reveal disproportionate burdens on vulnerable populations.
To maintain public trust and promote justice, institutions must be transparent regarding triage policies and procedures for CSCs. These should be available for public review, revised with public input, and readily available once finalized.
POTENTIAL BARRIERS TO IMPLEMENTATION
Despite the ethical justification for regional coordination of care and resources, there are multiple barriers to implementation. Providers and families may hesitate to disturb continuity of care at medical homes. Organizations may have financial disincentives to transfer long-term patients to new institutions. Openness with patients and families regarding the temporary nature of transfers and plans to return to their usual care may help. Granting temporary privileges at recipient institutions for providers to continue seeing their patients may lessen discontinuity. Solidarity in public health emergencies requires all institutions to compromise their own interests to some degree.
Similarly, barriers in achieving consistency across institutional triage policies may arise. Allocation strategies embody multiple values, for example, regarding quality of life or contributions of essential workers. Resolution of these value differences may prove difficult.
CONCLUSION
In the current COVID-19 pandemic, an ethical approach to CSCs necessitates coordination to align available resources at the regional, rather than institutional, level to avoid triage at individual institutions. Pediatric regionalization of care is the first step in freeing up system capacity for adults. Solidarity rises in importance, but must be balanced by duties of rescue, fidelity, and justice so that pediatric institutions continue to care for children with urgent needs requiring pediatric expertise.
Disclosures
Dr Paquette reported funding under the Pediatric Critical Care and Trauma Scientist Development Program, NICHD K12HDO47349 and NICHD Loan Repayment Program L40 HD089260. Dr Derrington is a director at large for the American Society of Bioethics and Medical Humanities and had travel expenses reimbursed for the annual conference in 2019. Dr Michelson has received funding from the National Palliative Care Research Center and is a consultant on a National Institutes of Health study that are unrelated to this work. Dr Michelson is also involved in unrelated work supported by the National Alliance for Grieving Children. All other authors declared they have nothing to disclose.
1. Institute of Medicine; Board on Health Sciences Policy; Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. Hanfling D, Altevogt BM, Viswanathan K, Gostin LO, eds. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. National Academies Press; 2012.
2. Berlinger N, Wynia M, Powell T, et al. Ethical Framework for Health Care Institutions & Guidelines for Institutional Ethics Services Responding to the Coronavirus Pandemic: Managing Uncertainty, Safeguarding Communities, Guiding Practice. The Hastings Center; March 16, 2020. Accessed June 22, 2020. https://www.thehastingscenter.org/ethicalframeworkcovid19/
3. Goold SD. Trust and the ethics of health care institutions. Hastings Cent Rep. 2001;31(6):26-33.
4. Garrett JR. Collectivizing rescue obligations in bioethics. Am J Bioeth. 2015;15(2):3-11. https://doi.org/10.1080/15265161.2014.990163
5. Furrow BR. Forcing rescue: the landscape of health care provider obligations to treat patients. Health Matrix Clevel. 1993;3(1):31-87.
6. Goodin RE. Protecting the Vulnerable: A Reanalysis of Our Social Responsibilities. University of Chicago Press; 1985.
7. Jecker N. Fidelity to Patients and Resource Constraints. In: Campbell CS, Lustig BA, eds. Duties to Others. Theology and Medicine, vol 4. Springer, Dordrecht; 1994. 293-308. https://doi.org/10.1007/978-94-015-8244-5_18
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Dawson A, Jennings B. The place of solidarity in public health ethics. Public Health Rev. 2012;34:65-79.
10. Rawls J. A Theory of Justice. Belknap Press of Harvard University Press; 1971.
11. Jennings B, Arras J. Ethical Guidance for Public Health Emergency Preparedness and Response: Highlighting Ethics and Values in a Vital Public Health Service. Centers for Disease Control and Prevention. October 30, 2008. Accessed April 16, 2020. https://www.cdc.gov/os/integrity/phethics/docs/white_paper_final_for_website_2012_4_6_12_final_for_web_508_compliant.pdf
12. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Medicine. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
13. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr. 2017;171(10):e172352. https://doi.org/10.1001/jamapediatrics.2017.2352
1. Institute of Medicine; Board on Health Sciences Policy; Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. Hanfling D, Altevogt BM, Viswanathan K, Gostin LO, eds. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. National Academies Press; 2012.
2. Berlinger N, Wynia M, Powell T, et al. Ethical Framework for Health Care Institutions & Guidelines for Institutional Ethics Services Responding to the Coronavirus Pandemic: Managing Uncertainty, Safeguarding Communities, Guiding Practice. The Hastings Center; March 16, 2020. Accessed June 22, 2020. https://www.thehastingscenter.org/ethicalframeworkcovid19/
3. Goold SD. Trust and the ethics of health care institutions. Hastings Cent Rep. 2001;31(6):26-33.
4. Garrett JR. Collectivizing rescue obligations in bioethics. Am J Bioeth. 2015;15(2):3-11. https://doi.org/10.1080/15265161.2014.990163
5. Furrow BR. Forcing rescue: the landscape of health care provider obligations to treat patients. Health Matrix Clevel. 1993;3(1):31-87.
6. Goodin RE. Protecting the Vulnerable: A Reanalysis of Our Social Responsibilities. University of Chicago Press; 1985.
7. Jecker N. Fidelity to Patients and Resource Constraints. In: Campbell CS, Lustig BA, eds. Duties to Others. Theology and Medicine, vol 4. Springer, Dordrecht; 1994. 293-308. https://doi.org/10.1007/978-94-015-8244-5_18
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Dawson A, Jennings B. The place of solidarity in public health ethics. Public Health Rev. 2012;34:65-79.
10. Rawls J. A Theory of Justice. Belknap Press of Harvard University Press; 1971.
11. Jennings B, Arras J. Ethical Guidance for Public Health Emergency Preparedness and Response: Highlighting Ethics and Values in a Vital Public Health Service. Centers for Disease Control and Prevention. October 30, 2008. Accessed April 16, 2020. https://www.cdc.gov/os/integrity/phethics/docs/white_paper_final_for_website_2012_4_6_12_final_for_web_508_compliant.pdf
12. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Medicine. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
13. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr. 2017;171(10):e172352. https://doi.org/10.1001/jamapediatrics.2017.2352
© 2020 Society of Hospital Medicine
#ConsentObtained – Patient Privacy in the Age of Social Media
“I have a rare dermatologic disorder. In medical school, I read a case report about treatment for my disorder. I was surprised to read my history and shocked to see my childhood face staring back at me in the figures section. The case report was written when I was a child and my parents had signed a consent form that stated my case and images could be used for ‘educational purposes.’ My parents were not notified that my images and case were published. While surprised and shocked to read my history and see images of myself in a medical journal, I trusted my privacy was protected because the journal would only be read by medical professionals. Fast-forward to today, I do not know how comfortable I would feel if my images were shared on social media, with the potential to reach viewers outside of the medical community. If I were a parent, I would feel even more uncomfortable with reading my child’s case on social media, let alone viewing an image of my child.”
—A.K.
Social media has become ingrained in our society, including many facets of our professional life. According to a 2019 report from the Pew Research Center, 73% of Americans use social media.1 The PricewaterhouseCoopers Health Institute found 90% of physicians use social media personally, and 65% use it professionally.2
As the Pediatric Hospital Medicine Conference Social Media Cochairs (2015-2019), we managed official profiles on Twitter, Facebook, and Instagram. We also crafted and executed the conference’s social media strategy. During that time, we witnessed a substantial increase in the presence of physicians on social media with little available guidance on best practices. Here, we discuss patient privacy challenges with social media as well as solutions to address them.
PATIENT PRIVACY CHALLENGES ON SOCIAL MEDIA
In 2011, Greyson et al surveyed executive directors of all medical and osteopathic boards in the United States for online professionalism violations.3 Online violations of patient confidentiality were reported by over 55% of the 48 boards that responded. Of those, 10% reported more than three violations of patient confidentiality, and no actions were initially taken in 25% of violations. While these violations were not specific to social media, they highlight online patient confidentiality breaches are occurring, even if they are not being disciplined.
Several organizations, including the American Medical Association (AMA), the American Academy of Pediatrics (AAP), and the American College of Physicians (ACP) have developed social media guidelines.4-6 However, these guidelines are not always followed. Fanti Silva and Colleoni studied surgeons and surgical trainees at a university hospital and found that social media guidelines were unknown to 100% of medical students, 85% of residents, and 78% of attendings.7 They also found that 53% of medical students, 86% of residents, and 32% of attendings were sharing patient information on social media despite hospitals’ privacy policies.
Social media provides forums for physicians to discuss cases and share experiences in hopes of educating others. These posts may include images or videos. Unfortunately, sharing specific clinical information or improperly deidentifying images may lead to the unintentional identification of patients.8 Some information may not be protected by the US Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, and may lead to patient identification when shared.9 Despite disguising or omitting demographics, encounter information, or unique characteristics of the presentation, some physicians—not the posting physician—believe patients may still be able to identify their cases.8
Physicians who try to be mindful of patient privacy concerns face challenges with social media platforms themselves. For example, Facebook allows users to create Closed Groups (CGs) in which the group’s “administrators” can grant “admission” to users wishing to join the conversation (eg, Physician Moms Group). These groups are left to govern themselves and comply only with Facebook’s safety standards. The Society of Gastrointestinal and Endoscopic Surgeons used Facebook’s CGs to create a forum for education, consultation, and collaboration for society members. Group administrators grant admittance only after group members have agreed to HIPAA compliance. Group members may then share deidentified images and videos when discussing cases.10 However, Facebook’s Terms of Service states the company has “a non-exclusive, transferable, sub-licensable, royalty-free, worldwide license to host, use, distribute, modify, run, copy, publicly perform or display, translate, and create derivative works” of the content based on the privacy settings of the individual posting the content.11 Therefore, these CGs may create a false sense of security because many members may assume the content of the CGs are private. Twitter’s Terms of Service are similar to Facebook’s, but state that users should have “obtained, all rights, licenses, consents, permissions, power and/or authority necessary to grant the rights . . . for any Content that is posted.”12 If a patient’s deidentified story is posted on Twitter, the posting physician may be violating Twitter’s Terms of Service by not obtaining the patient’s consent/permission or explicitly stating so in their tweet.
SOLUTIONS
In light of the challenges faced when posting medical cases on social media, we propose several solutions that the medical community should adopt to mitigate and limit any potential breaches to patient privacy. These are summarized in the Table.
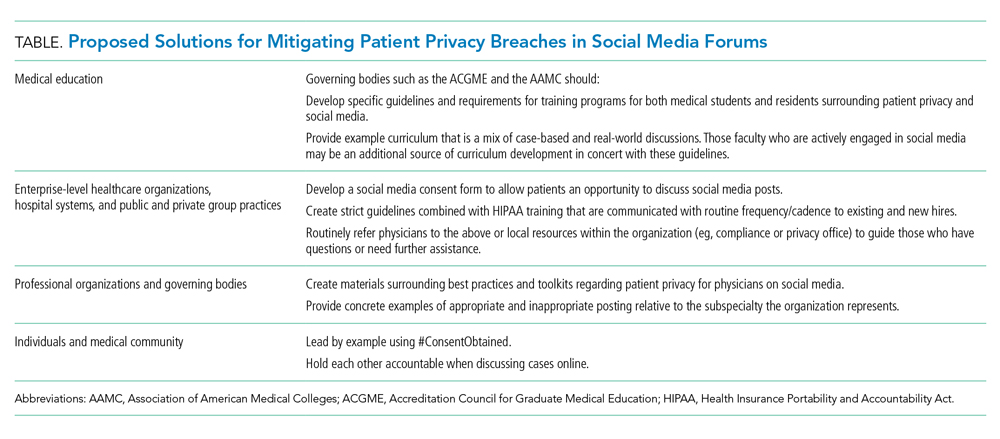
Medical Education
Many medical students and residents are active on social media. However, not all are formally educated on appropriate engagement online and social media etiquette. A recent article from the Association of American Medical Colleges (AAMC) highlights how this “curriculum” is missing from many medical schools and residency programs.13 There are plenty of resources outlining how to maintain professionalism on social media in a general sense, but maintaining patient privacy usually is not concretely explored. Consequently, many programs are left to individually provide this education without firm guidance on best practices. We propose that governing organizations for medical education such as the AAMC and Accreditation Council for Graduate Medical Education have formal requirements, guidelines, and example curriculum on educating trainees on best practices for social media activity.
Health Organization Consent Forms
Healthcare organizations have a responsibility to protect patient privacy. We propose that healthcare organizations should develop independent social media consent forms that address sharing of images, videos, and cases. This separate social media consent form would allow patients/guardians to discuss whether they want their information shared. Some organizations have taken this step and developed consent forms for sharing deidentified posts on HIPAA-compliant CGs.10 However, it is still far from standard of practice for a healthcare organization to develop a separate consent form addressing the educational uses of sharing cases on social media. The Federation of State Medical Board’s (FSMB) Social Media and Electronic Communications policy endorses obtaining “express written consent” from patients.14 The policy states that “the physician must adequately explain the risks . . . for consent to be fully informed.” The FSMB policy also reminds readers that any social media post is permanent, even after it has been deleted.
Professional Organizations
Many professional organizations have acknowledged the growing role of social media in the professional lives of medical providers and have adopted policy statements and guidelines to address social media use. However, these guidelines are quite variable. All professional organizations should take the time to clarify and discuss the nuances of patient privacy on social media in their guidelines. For example, the American College of Obstetrics and Gynecology statement warns members that “any public communication about work-related clinical events may violate . . . privacy” and posting of deidentified general events “may be traced, through public vital statistics data, to a specific patient or hospital” directly violating HIPAA.15 In comparison, the AAP and ACP’s social media guidelines and toolkits fall short when discussing how to maintain patient privacy specifically. Within these toolkits and guidelines, there is no explicit guidance or discussion about maintaining patient privacy with the use of case examples or best practices.5,6 As physicians on social media, we should be aware of these variable policy statements and guidelines from our professional organizations. Even further, as active members of our professional organizations, we should call on them to update their guidelines to increase details regarding the nuances of patient privacy.
#ConsentObtained
When a case is posted on social media, it should be the posting physician’s responsibility to clearly state in the initial post that consent was obtained. To simplify the process, we propose the use of the hashtag, #ConsentObtained, to easily identify that assurances were made to protect the patient. Moreover, we encourage our physician colleagues to remind others to explicitly state if consent was obtained if it is not mentioned. The AMA’s code of ethics states that if physicians read posts that they feel are unprofessional, then those physicians “have a responsibility to bring that content to the attention of the individual, so that he or she can remove it and/or take other appropriate actions.”4 Therefore, we encourage all readers of social media posts to ensure that posts include #ConsentObtained or otherwise clearly state that patient permission was obtained. If the hashtag or verbiage is not seen, then it is the reader’s responsibility to contact the posting physician. The AMA’s code of ethics also recommends physicians to “report the matter to appropriate authorities” if the individual posting “does not take appropriate actions.”4 While we realize that verification of consent being obtained may be virtually impossible online, we hope that, as physicians, we hold patient privacy to the highest regard and would never use this hashtag inappropriately. Lastly, it’s important to remember that removing/deleting a post may delete it from the platform, but that post and its contents are not deleted from the internet and may be accessed through another site.
CONCLUSION
Social media has allowed the healthcare community to develop a voice for individuals and communities; it has allowed for collaboration, open discussion, and education. However, it also asks us to reevaluate the professional ethics and rules we have abided for decades with regard to keeping patient health information safe. We must be proactive to develop solutions regarding patient privacy as our social media presence continues to grow.
Disclosure
The authors have no conflicts of interest to report.
1. Perrin A, Anderson M. Share of U.S. adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Center. April 10, 2019. Accessed September 9, 2019. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018
2. Modahl M, Tompsett L, Moorhead T. Doctors, Patients, and Social Media.QuantiaMD. September 2011. Accessed September 9, 2019. http://www.quantiamd.com/q-qcp/social_media.pdf
3. Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142. https://.org/10.1001/jama.2012.330
4. Code of Medical Ethics Opinion 2.3.2. American Medical Associaiton. November 14, 2016. Accessed August 18, 2019. https://www.ama-assn.org/delivering-care/ethics/professionalism-use-social-media
5. Social Media Toolkit. American Academy of Pediatrics. Accessed January 14, 2020. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Media-and-Children.aspx
6. Farnan JM, Snyder Sulmasy L, Worster BK, et al. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Annal Intern Med. 2013;158:620-627. https://doi.org/10.7326/0003-4819-158-8-201304160-00100
7. Fanti Silva DA, Colleoni R. Patient’s privacy violation on social media in the surgical area. Am Surg. 2018;84(12):1900-1905.
8. Cifu AS, Vandross AL, Prasad V. Case reports in the age of Twitter. Am J Med. 2019;132(10):e725-e726. https://doi.org/10.1016/j.amjmed.2019.03.044
9. OCR Privacy Brief: Summary of the HIPAA Privacy Rule. Department of Health & Human Services; 2003. Accessed August 18, 2019. https://www.hhs.gov/sites/default/files/privacysummary.pdf
10. Bittner JG 4th, Logghe HJ, Kane ED, et al. A Society of Gastrointestinal and Endoscopic Surgeons (SAGES) statement on closed social media (Facebook) groups for clinical education and consultation: issues of informed consent, patient privacy, and surgeon protection. Surg Endosc. 2019;33(1):1-7. https://doi.org/10.1007/s00464-018-6569-2
11. Terms of Service. Facebook. 2019. Accessed August 18, 2019. https://www.facebook.com/terms.php
12. Terms of Service. Twitter. 2020. Accessed January 3, 2020. https://twitter.com/en/tos
13. Kalter L. The social media dilemma. Special to AAMC News. Mar 4, 2019. Accessed January 2, 2020. https://www.aamc.org/news-insights/social-media-dilemma
14. Social Media and Electronic Communications; Report and Recommendations of the FSMB Ethics and Professionalism Committee; Adopted as policy by the Federation of State Medical Boards April 2019. Federation of State Medical Boards. Accessed August 18, 2019. http://www.fsmb.org/siteassets/advocacy/policies/social-media-and-electronic-communications.pdf
15. Professional use of digital and social media: ACOG Committee Opinion, Number 791. Obstet Gynecol. 2019;134(4):e117-e121. https://doi.org/10.1097/AOG.0000000000003451
“I have a rare dermatologic disorder. In medical school, I read a case report about treatment for my disorder. I was surprised to read my history and shocked to see my childhood face staring back at me in the figures section. The case report was written when I was a child and my parents had signed a consent form that stated my case and images could be used for ‘educational purposes.’ My parents were not notified that my images and case were published. While surprised and shocked to read my history and see images of myself in a medical journal, I trusted my privacy was protected because the journal would only be read by medical professionals. Fast-forward to today, I do not know how comfortable I would feel if my images were shared on social media, with the potential to reach viewers outside of the medical community. If I were a parent, I would feel even more uncomfortable with reading my child’s case on social media, let alone viewing an image of my child.”
—A.K.
Social media has become ingrained in our society, including many facets of our professional life. According to a 2019 report from the Pew Research Center, 73% of Americans use social media.1 The PricewaterhouseCoopers Health Institute found 90% of physicians use social media personally, and 65% use it professionally.2
As the Pediatric Hospital Medicine Conference Social Media Cochairs (2015-2019), we managed official profiles on Twitter, Facebook, and Instagram. We also crafted and executed the conference’s social media strategy. During that time, we witnessed a substantial increase in the presence of physicians on social media with little available guidance on best practices. Here, we discuss patient privacy challenges with social media as well as solutions to address them.
PATIENT PRIVACY CHALLENGES ON SOCIAL MEDIA
In 2011, Greyson et al surveyed executive directors of all medical and osteopathic boards in the United States for online professionalism violations.3 Online violations of patient confidentiality were reported by over 55% of the 48 boards that responded. Of those, 10% reported more than three violations of patient confidentiality, and no actions were initially taken in 25% of violations. While these violations were not specific to social media, they highlight online patient confidentiality breaches are occurring, even if they are not being disciplined.
Several organizations, including the American Medical Association (AMA), the American Academy of Pediatrics (AAP), and the American College of Physicians (ACP) have developed social media guidelines.4-6 However, these guidelines are not always followed. Fanti Silva and Colleoni studied surgeons and surgical trainees at a university hospital and found that social media guidelines were unknown to 100% of medical students, 85% of residents, and 78% of attendings.7 They also found that 53% of medical students, 86% of residents, and 32% of attendings were sharing patient information on social media despite hospitals’ privacy policies.
Social media provides forums for physicians to discuss cases and share experiences in hopes of educating others. These posts may include images or videos. Unfortunately, sharing specific clinical information or improperly deidentifying images may lead to the unintentional identification of patients.8 Some information may not be protected by the US Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, and may lead to patient identification when shared.9 Despite disguising or omitting demographics, encounter information, or unique characteristics of the presentation, some physicians—not the posting physician—believe patients may still be able to identify their cases.8
Physicians who try to be mindful of patient privacy concerns face challenges with social media platforms themselves. For example, Facebook allows users to create Closed Groups (CGs) in which the group’s “administrators” can grant “admission” to users wishing to join the conversation (eg, Physician Moms Group). These groups are left to govern themselves and comply only with Facebook’s safety standards. The Society of Gastrointestinal and Endoscopic Surgeons used Facebook’s CGs to create a forum for education, consultation, and collaboration for society members. Group administrators grant admittance only after group members have agreed to HIPAA compliance. Group members may then share deidentified images and videos when discussing cases.10 However, Facebook’s Terms of Service states the company has “a non-exclusive, transferable, sub-licensable, royalty-free, worldwide license to host, use, distribute, modify, run, copy, publicly perform or display, translate, and create derivative works” of the content based on the privacy settings of the individual posting the content.11 Therefore, these CGs may create a false sense of security because many members may assume the content of the CGs are private. Twitter’s Terms of Service are similar to Facebook’s, but state that users should have “obtained, all rights, licenses, consents, permissions, power and/or authority necessary to grant the rights . . . for any Content that is posted.”12 If a patient’s deidentified story is posted on Twitter, the posting physician may be violating Twitter’s Terms of Service by not obtaining the patient’s consent/permission or explicitly stating so in their tweet.
SOLUTIONS
In light of the challenges faced when posting medical cases on social media, we propose several solutions that the medical community should adopt to mitigate and limit any potential breaches to patient privacy. These are summarized in the Table.
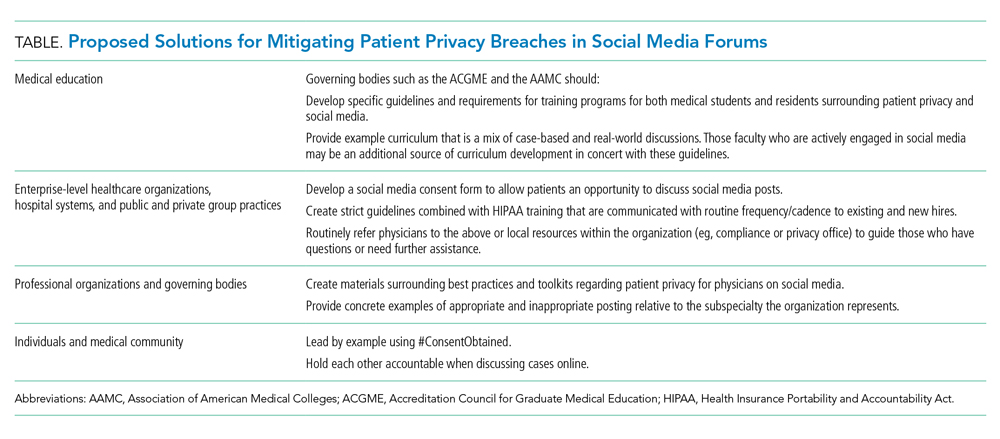
Medical Education
Many medical students and residents are active on social media. However, not all are formally educated on appropriate engagement online and social media etiquette. A recent article from the Association of American Medical Colleges (AAMC) highlights how this “curriculum” is missing from many medical schools and residency programs.13 There are plenty of resources outlining how to maintain professionalism on social media in a general sense, but maintaining patient privacy usually is not concretely explored. Consequently, many programs are left to individually provide this education without firm guidance on best practices. We propose that governing organizations for medical education such as the AAMC and Accreditation Council for Graduate Medical Education have formal requirements, guidelines, and example curriculum on educating trainees on best practices for social media activity.
Health Organization Consent Forms
Healthcare organizations have a responsibility to protect patient privacy. We propose that healthcare organizations should develop independent social media consent forms that address sharing of images, videos, and cases. This separate social media consent form would allow patients/guardians to discuss whether they want their information shared. Some organizations have taken this step and developed consent forms for sharing deidentified posts on HIPAA-compliant CGs.10 However, it is still far from standard of practice for a healthcare organization to develop a separate consent form addressing the educational uses of sharing cases on social media. The Federation of State Medical Board’s (FSMB) Social Media and Electronic Communications policy endorses obtaining “express written consent” from patients.14 The policy states that “the physician must adequately explain the risks . . . for consent to be fully informed.” The FSMB policy also reminds readers that any social media post is permanent, even after it has been deleted.
Professional Organizations
Many professional organizations have acknowledged the growing role of social media in the professional lives of medical providers and have adopted policy statements and guidelines to address social media use. However, these guidelines are quite variable. All professional organizations should take the time to clarify and discuss the nuances of patient privacy on social media in their guidelines. For example, the American College of Obstetrics and Gynecology statement warns members that “any public communication about work-related clinical events may violate . . . privacy” and posting of deidentified general events “may be traced, through public vital statistics data, to a specific patient or hospital” directly violating HIPAA.15 In comparison, the AAP and ACP’s social media guidelines and toolkits fall short when discussing how to maintain patient privacy specifically. Within these toolkits and guidelines, there is no explicit guidance or discussion about maintaining patient privacy with the use of case examples or best practices.5,6 As physicians on social media, we should be aware of these variable policy statements and guidelines from our professional organizations. Even further, as active members of our professional organizations, we should call on them to update their guidelines to increase details regarding the nuances of patient privacy.
#ConsentObtained
When a case is posted on social media, it should be the posting physician’s responsibility to clearly state in the initial post that consent was obtained. To simplify the process, we propose the use of the hashtag, #ConsentObtained, to easily identify that assurances were made to protect the patient. Moreover, we encourage our physician colleagues to remind others to explicitly state if consent was obtained if it is not mentioned. The AMA’s code of ethics states that if physicians read posts that they feel are unprofessional, then those physicians “have a responsibility to bring that content to the attention of the individual, so that he or she can remove it and/or take other appropriate actions.”4 Therefore, we encourage all readers of social media posts to ensure that posts include #ConsentObtained or otherwise clearly state that patient permission was obtained. If the hashtag or verbiage is not seen, then it is the reader’s responsibility to contact the posting physician. The AMA’s code of ethics also recommends physicians to “report the matter to appropriate authorities” if the individual posting “does not take appropriate actions.”4 While we realize that verification of consent being obtained may be virtually impossible online, we hope that, as physicians, we hold patient privacy to the highest regard and would never use this hashtag inappropriately. Lastly, it’s important to remember that removing/deleting a post may delete it from the platform, but that post and its contents are not deleted from the internet and may be accessed through another site.
CONCLUSION
Social media has allowed the healthcare community to develop a voice for individuals and communities; it has allowed for collaboration, open discussion, and education. However, it also asks us to reevaluate the professional ethics and rules we have abided for decades with regard to keeping patient health information safe. We must be proactive to develop solutions regarding patient privacy as our social media presence continues to grow.
Disclosure
The authors have no conflicts of interest to report.
“I have a rare dermatologic disorder. In medical school, I read a case report about treatment for my disorder. I was surprised to read my history and shocked to see my childhood face staring back at me in the figures section. The case report was written when I was a child and my parents had signed a consent form that stated my case and images could be used for ‘educational purposes.’ My parents were not notified that my images and case were published. While surprised and shocked to read my history and see images of myself in a medical journal, I trusted my privacy was protected because the journal would only be read by medical professionals. Fast-forward to today, I do not know how comfortable I would feel if my images were shared on social media, with the potential to reach viewers outside of the medical community. If I were a parent, I would feel even more uncomfortable with reading my child’s case on social media, let alone viewing an image of my child.”
—A.K.
Social media has become ingrained in our society, including many facets of our professional life. According to a 2019 report from the Pew Research Center, 73% of Americans use social media.1 The PricewaterhouseCoopers Health Institute found 90% of physicians use social media personally, and 65% use it professionally.2
As the Pediatric Hospital Medicine Conference Social Media Cochairs (2015-2019), we managed official profiles on Twitter, Facebook, and Instagram. We also crafted and executed the conference’s social media strategy. During that time, we witnessed a substantial increase in the presence of physicians on social media with little available guidance on best practices. Here, we discuss patient privacy challenges with social media as well as solutions to address them.
PATIENT PRIVACY CHALLENGES ON SOCIAL MEDIA
In 2011, Greyson et al surveyed executive directors of all medical and osteopathic boards in the United States for online professionalism violations.3 Online violations of patient confidentiality were reported by over 55% of the 48 boards that responded. Of those, 10% reported more than three violations of patient confidentiality, and no actions were initially taken in 25% of violations. While these violations were not specific to social media, they highlight online patient confidentiality breaches are occurring, even if they are not being disciplined.
Several organizations, including the American Medical Association (AMA), the American Academy of Pediatrics (AAP), and the American College of Physicians (ACP) have developed social media guidelines.4-6 However, these guidelines are not always followed. Fanti Silva and Colleoni studied surgeons and surgical trainees at a university hospital and found that social media guidelines were unknown to 100% of medical students, 85% of residents, and 78% of attendings.7 They also found that 53% of medical students, 86% of residents, and 32% of attendings were sharing patient information on social media despite hospitals’ privacy policies.
Social media provides forums for physicians to discuss cases and share experiences in hopes of educating others. These posts may include images or videos. Unfortunately, sharing specific clinical information or improperly deidentifying images may lead to the unintentional identification of patients.8 Some information may not be protected by the US Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, and may lead to patient identification when shared.9 Despite disguising or omitting demographics, encounter information, or unique characteristics of the presentation, some physicians—not the posting physician—believe patients may still be able to identify their cases.8
Physicians who try to be mindful of patient privacy concerns face challenges with social media platforms themselves. For example, Facebook allows users to create Closed Groups (CGs) in which the group’s “administrators” can grant “admission” to users wishing to join the conversation (eg, Physician Moms Group). These groups are left to govern themselves and comply only with Facebook’s safety standards. The Society of Gastrointestinal and Endoscopic Surgeons used Facebook’s CGs to create a forum for education, consultation, and collaboration for society members. Group administrators grant admittance only after group members have agreed to HIPAA compliance. Group members may then share deidentified images and videos when discussing cases.10 However, Facebook’s Terms of Service states the company has “a non-exclusive, transferable, sub-licensable, royalty-free, worldwide license to host, use, distribute, modify, run, copy, publicly perform or display, translate, and create derivative works” of the content based on the privacy settings of the individual posting the content.11 Therefore, these CGs may create a false sense of security because many members may assume the content of the CGs are private. Twitter’s Terms of Service are similar to Facebook’s, but state that users should have “obtained, all rights, licenses, consents, permissions, power and/or authority necessary to grant the rights . . . for any Content that is posted.”12 If a patient’s deidentified story is posted on Twitter, the posting physician may be violating Twitter’s Terms of Service by not obtaining the patient’s consent/permission or explicitly stating so in their tweet.
SOLUTIONS
In light of the challenges faced when posting medical cases on social media, we propose several solutions that the medical community should adopt to mitigate and limit any potential breaches to patient privacy. These are summarized in the Table.
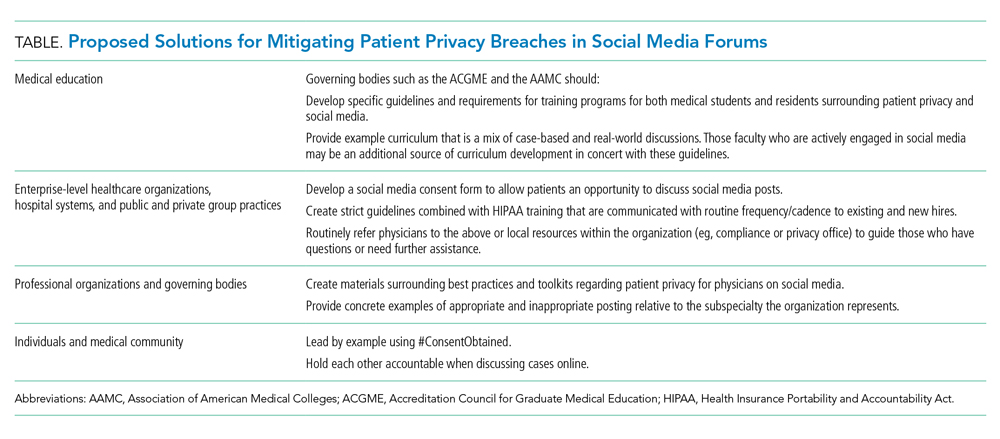
Medical Education
Many medical students and residents are active on social media. However, not all are formally educated on appropriate engagement online and social media etiquette. A recent article from the Association of American Medical Colleges (AAMC) highlights how this “curriculum” is missing from many medical schools and residency programs.13 There are plenty of resources outlining how to maintain professionalism on social media in a general sense, but maintaining patient privacy usually is not concretely explored. Consequently, many programs are left to individually provide this education without firm guidance on best practices. We propose that governing organizations for medical education such as the AAMC and Accreditation Council for Graduate Medical Education have formal requirements, guidelines, and example curriculum on educating trainees on best practices for social media activity.
Health Organization Consent Forms
Healthcare organizations have a responsibility to protect patient privacy. We propose that healthcare organizations should develop independent social media consent forms that address sharing of images, videos, and cases. This separate social media consent form would allow patients/guardians to discuss whether they want their information shared. Some organizations have taken this step and developed consent forms for sharing deidentified posts on HIPAA-compliant CGs.10 However, it is still far from standard of practice for a healthcare organization to develop a separate consent form addressing the educational uses of sharing cases on social media. The Federation of State Medical Board’s (FSMB) Social Media and Electronic Communications policy endorses obtaining “express written consent” from patients.14 The policy states that “the physician must adequately explain the risks . . . for consent to be fully informed.” The FSMB policy also reminds readers that any social media post is permanent, even after it has been deleted.
Professional Organizations
Many professional organizations have acknowledged the growing role of social media in the professional lives of medical providers and have adopted policy statements and guidelines to address social media use. However, these guidelines are quite variable. All professional organizations should take the time to clarify and discuss the nuances of patient privacy on social media in their guidelines. For example, the American College of Obstetrics and Gynecology statement warns members that “any public communication about work-related clinical events may violate . . . privacy” and posting of deidentified general events “may be traced, through public vital statistics data, to a specific patient or hospital” directly violating HIPAA.15 In comparison, the AAP and ACP’s social media guidelines and toolkits fall short when discussing how to maintain patient privacy specifically. Within these toolkits and guidelines, there is no explicit guidance or discussion about maintaining patient privacy with the use of case examples or best practices.5,6 As physicians on social media, we should be aware of these variable policy statements and guidelines from our professional organizations. Even further, as active members of our professional organizations, we should call on them to update their guidelines to increase details regarding the nuances of patient privacy.
#ConsentObtained
When a case is posted on social media, it should be the posting physician’s responsibility to clearly state in the initial post that consent was obtained. To simplify the process, we propose the use of the hashtag, #ConsentObtained, to easily identify that assurances were made to protect the patient. Moreover, we encourage our physician colleagues to remind others to explicitly state if consent was obtained if it is not mentioned. The AMA’s code of ethics states that if physicians read posts that they feel are unprofessional, then those physicians “have a responsibility to bring that content to the attention of the individual, so that he or she can remove it and/or take other appropriate actions.”4 Therefore, we encourage all readers of social media posts to ensure that posts include #ConsentObtained or otherwise clearly state that patient permission was obtained. If the hashtag or verbiage is not seen, then it is the reader’s responsibility to contact the posting physician. The AMA’s code of ethics also recommends physicians to “report the matter to appropriate authorities” if the individual posting “does not take appropriate actions.”4 While we realize that verification of consent being obtained may be virtually impossible online, we hope that, as physicians, we hold patient privacy to the highest regard and would never use this hashtag inappropriately. Lastly, it’s important to remember that removing/deleting a post may delete it from the platform, but that post and its contents are not deleted from the internet and may be accessed through another site.
CONCLUSION
Social media has allowed the healthcare community to develop a voice for individuals and communities; it has allowed for collaboration, open discussion, and education. However, it also asks us to reevaluate the professional ethics and rules we have abided for decades with regard to keeping patient health information safe. We must be proactive to develop solutions regarding patient privacy as our social media presence continues to grow.
Disclosure
The authors have no conflicts of interest to report.
1. Perrin A, Anderson M. Share of U.S. adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Center. April 10, 2019. Accessed September 9, 2019. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018
2. Modahl M, Tompsett L, Moorhead T. Doctors, Patients, and Social Media.QuantiaMD. September 2011. Accessed September 9, 2019. http://www.quantiamd.com/q-qcp/social_media.pdf
3. Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142. https://.org/10.1001/jama.2012.330
4. Code of Medical Ethics Opinion 2.3.2. American Medical Associaiton. November 14, 2016. Accessed August 18, 2019. https://www.ama-assn.org/delivering-care/ethics/professionalism-use-social-media
5. Social Media Toolkit. American Academy of Pediatrics. Accessed January 14, 2020. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Media-and-Children.aspx
6. Farnan JM, Snyder Sulmasy L, Worster BK, et al. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Annal Intern Med. 2013;158:620-627. https://doi.org/10.7326/0003-4819-158-8-201304160-00100
7. Fanti Silva DA, Colleoni R. Patient’s privacy violation on social media in the surgical area. Am Surg. 2018;84(12):1900-1905.
8. Cifu AS, Vandross AL, Prasad V. Case reports in the age of Twitter. Am J Med. 2019;132(10):e725-e726. https://doi.org/10.1016/j.amjmed.2019.03.044
9. OCR Privacy Brief: Summary of the HIPAA Privacy Rule. Department of Health & Human Services; 2003. Accessed August 18, 2019. https://www.hhs.gov/sites/default/files/privacysummary.pdf
10. Bittner JG 4th, Logghe HJ, Kane ED, et al. A Society of Gastrointestinal and Endoscopic Surgeons (SAGES) statement on closed social media (Facebook) groups for clinical education and consultation: issues of informed consent, patient privacy, and surgeon protection. Surg Endosc. 2019;33(1):1-7. https://doi.org/10.1007/s00464-018-6569-2
11. Terms of Service. Facebook. 2019. Accessed August 18, 2019. https://www.facebook.com/terms.php
12. Terms of Service. Twitter. 2020. Accessed January 3, 2020. https://twitter.com/en/tos
13. Kalter L. The social media dilemma. Special to AAMC News. Mar 4, 2019. Accessed January 2, 2020. https://www.aamc.org/news-insights/social-media-dilemma
14. Social Media and Electronic Communications; Report and Recommendations of the FSMB Ethics and Professionalism Committee; Adopted as policy by the Federation of State Medical Boards April 2019. Federation of State Medical Boards. Accessed August 18, 2019. http://www.fsmb.org/siteassets/advocacy/policies/social-media-and-electronic-communications.pdf
15. Professional use of digital and social media: ACOG Committee Opinion, Number 791. Obstet Gynecol. 2019;134(4):e117-e121. https://doi.org/10.1097/AOG.0000000000003451
1. Perrin A, Anderson M. Share of U.S. adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Center. April 10, 2019. Accessed September 9, 2019. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018
2. Modahl M, Tompsett L, Moorhead T. Doctors, Patients, and Social Media.QuantiaMD. September 2011. Accessed September 9, 2019. http://www.quantiamd.com/q-qcp/social_media.pdf
3. Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142. https://.org/10.1001/jama.2012.330
4. Code of Medical Ethics Opinion 2.3.2. American Medical Associaiton. November 14, 2016. Accessed August 18, 2019. https://www.ama-assn.org/delivering-care/ethics/professionalism-use-social-media
5. Social Media Toolkit. American Academy of Pediatrics. Accessed January 14, 2020. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Media-and-Children.aspx
6. Farnan JM, Snyder Sulmasy L, Worster BK, et al. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Annal Intern Med. 2013;158:620-627. https://doi.org/10.7326/0003-4819-158-8-201304160-00100
7. Fanti Silva DA, Colleoni R. Patient’s privacy violation on social media in the surgical area. Am Surg. 2018;84(12):1900-1905.
8. Cifu AS, Vandross AL, Prasad V. Case reports in the age of Twitter. Am J Med. 2019;132(10):e725-e726. https://doi.org/10.1016/j.amjmed.2019.03.044
9. OCR Privacy Brief: Summary of the HIPAA Privacy Rule. Department of Health & Human Services; 2003. Accessed August 18, 2019. https://www.hhs.gov/sites/default/files/privacysummary.pdf
10. Bittner JG 4th, Logghe HJ, Kane ED, et al. A Society of Gastrointestinal and Endoscopic Surgeons (SAGES) statement on closed social media (Facebook) groups for clinical education and consultation: issues of informed consent, patient privacy, and surgeon protection. Surg Endosc. 2019;33(1):1-7. https://doi.org/10.1007/s00464-018-6569-2
11. Terms of Service. Facebook. 2019. Accessed August 18, 2019. https://www.facebook.com/terms.php
12. Terms of Service. Twitter. 2020. Accessed January 3, 2020. https://twitter.com/en/tos
13. Kalter L. The social media dilemma. Special to AAMC News. Mar 4, 2019. Accessed January 2, 2020. https://www.aamc.org/news-insights/social-media-dilemma
14. Social Media and Electronic Communications; Report and Recommendations of the FSMB Ethics and Professionalism Committee; Adopted as policy by the Federation of State Medical Boards April 2019. Federation of State Medical Boards. Accessed August 18, 2019. http://www.fsmb.org/siteassets/advocacy/policies/social-media-and-electronic-communications.pdf
15. Professional use of digital and social media: ACOG Committee Opinion, Number 791. Obstet Gynecol. 2019;134(4):e117-e121. https://doi.org/10.1097/AOG.0000000000003451
© 2020 Society of Hospital Medicine
Recognizing Moral Distress in the COVID-19 Pandemic: Lessons From Global Disaster Response
Many US health care systems experienced a surge of critically ill corona virus disease 2019 (COVID-19) patients while lacking adequate resources to provide optimal care. Nurses, doctors, and other providers in the United States were confronted with having to implement crisis standards of care for the first time. The refrain “these are unprecedented times” was repeated to colleagues and patients. The demands and shortages of supplies are unique in recent history. As a result, many frontline responders have wrestled with moral distress, the feelings of distress experienced when forced to act—because of institutional or resource constraints—in a manner contrary to their beliefs.1 However, for those medical professionals whose work includes being deployed on global disaster response teams or providing healthcare in chronically low-resourced settings, navigating limitations of medicines, equipment, and personnel is a daily reality. We offer a framework for recognizing one’s own moral distress and that of one’s colleagues based on our experiences in global disaster response that may be helpful for clinicians during the COVID-19 pandemic.
A FRAMEWORK FOR MORAL DISTRESS
The intense and debilitating feelings of unexpected loss and helplessness faced by clinicians who are making challenging choices about medical interventions can be better understood by applying a theoretical framework that has the following three main stages in the evolution and response to moral distress: indignation, resignation, and acclimation. This framework can provide guidance to individuals experiencing distress during the COVID-19 pandemic and may also be beneficial in contextualizing interactions when working in teams or with referring providers.
Indignation
When working in a disaster setting, an initial period of indignation is common. The clinician is shocked and horrified by the conditions encountered, the severity of suffering, and a lack of resources with which they are unaccustomed. As we bear witness to the many healthcare providers who have fallen ill and died, we fear for our own safety in choosing to care for patients sick with COVID: “I’m risking my life caring for patients on the front lines, and it’s unacceptable that I’m not even being provided with adequate PPE!” Patients and families are suffering in ways we had previously thought our health system was capable of addressing: “How can I be a compassionate clinician when my patients are forced to die alone?!” It feels surreal and unacceptable that so many patients can die so quickly despite our heroic interventions and that we have very little control over their fate. We are unaccustomed to caring for so many dying patients at once. For example, during the peak of the pandemic in New York City, patients were dying at four times the city’s normal death rate.2 Indignation may be compounded in settings where providers are not even equipped to deal with the aftermath of deaths, such as piling bodies into makeshift morgues2: “I feel powerless to prevent my patients’ deaths and horrified that many are dying alone and scared, and now I can’t even guarantee that their bodies will be cared for after death!” Additionally, during this pandemic, many of us are now facing issues of resource allocation that we had never imagined dealing with. “I took an oath to care for and protect my patients. How could I possibly tell a patient we have no more ventilators to put them on? Who makes the decision of which patients deserve to live or die?” With the realization that COVID-19 has been disproportionately affecting racial and ethnic minorities, concerns for systemic discrimination within our healthcare system may rightly lead to a deep indignation.3
Resignation
After the initial indignation stage, resignation often follows. “I guess I can’t fix healthcare in this new setting, and I was foolish for even trying.” Clinicians go through the motions and continue to care for patients but feel disillusioned. Part of the ongoing stress involves the concern that they aren’t making a difference. Lack of viral testing may breed further resignation: Clinicians are on the front lines caring for patients that they are not even sure are positive for COVID-19, they have no way of accessing antibody testing for themselves to be able to gauge their own personal risks, and when there is not enough testing being done on a larger scale, there may be a sense that, by continuing to work on the front lines, they are sticking their finger in the dike, without actually having data to inform when it is safe to reopen states and ease restrictions. The suffering of patients and families may feel overwhelming and insurmountable. “I know I have to comply with my hospital’s visitor restriction policies, but it’s hard to see my patients suffering alone and know there’s nothing I can do to help them.”
Acclimation
Acclimation follows the indignation and resignation stages. Even amid disasters, a productive rhythm develops as teams coalesce and are galvanized by a shared sense of purpose. Clinicians make meaning out of their role in the crisis and in the care of the patients they can help, despite often deep and significant obstacles. “There’s a lot of suffering and a lot that I may not be able to fix, but some that I can.” Clinicians that have been deployed to unfamiliar roles may start to habituate and even enjoy having responsibilities and challenges that are different from those they typically face. Innovation during a pandemic may feel empowering. “I’m committed to making sure my dying patients and their families can say goodbye however possible. Although it’s not ideal, I’ve been using technology for virtual communication and advocating for families to visit in person when possible.”
RECOGNIZING THE STAGES OF MORAL DISTRESS
One’s path of moral distress through a disaster may not be linear; one does not necessarily progress through the stages of indignation, resignation, and acclimation in a certain order or at a certain pace. Additionally, the stages can recur throughout the disaster. Being able to recognize these stages may prove useful for the duration of this pandemic while waves of providers are redeployed in new settings and experience fresh indignation, whereas others who have been in the trenches for some time may be more likely experiencing resignation or, hopefully, acclimation. The trajectory and duration of this pandemic in the United States remains unclear. While hot spots such as Seattle, New York, and Boston may be moving past their peak phase and acclimating to a “new normal,” there remain concerns that surges may recur in the fall and winter, which will undoubtedly lead battle-weary clinicians to experience the stages of moral distress anew and potentially compounding their distress.
MANAGING MORAL DISTRESS
An added complexity in this pandemic is that we, as clinicians, are both the victims and the healers. From the literature on disaster mental health, we know that emotional suffering is universal in affected populations.4,5 Unlike many disaster scenarios in which teams leave the safety and security of well-established and well-resourced practices to deploy and care for disaster victims in new, austere environments, we are also part of that affected population in this pandemic. Each day or night, we return to homes that, too, are infiltrated by this pandemic. Our ability to move through the indignation, resignation, and acclimation stages may be hindered and blocked by our home responsibilities, stressors, and supports. Having to reconcile working in COVID-affected hospitals (particularly if caring for critically ill colleagues) only to return home to young or immunocompromised family members at night may place us in a state of indignation with its continued risk of burnout for the duration of this pandemic. Naming and acknowledging these painful challenges may allow self-compassion, self-forgiveness, and acceptance.
Though the primary focus of this article is to provide a framework to assist with the recognition of moral distress, it is important to address next steps once one recognizes someone is experiencing moral distress in this pandemic. Even outside of a disaster scenario, many clinicians feel obligated to put our patients’ needs before our own, and this sentiment is only heightened in a disaster scenario. It may feel unthinkable to call out sick or request a leave or reassignment during the pandemic. However, we are reminded that “the duty to serve is not endless.”6 Recognizing one’s own limits and reaching out to supervisors and mental health support before reaching one’s own limit is essential when experiencing moral distress.7,8
Cultivating resilience is also recognized as a tool for managing moral distress.6,9 For harried frontline clinicians, this may be as simple as taking a few minutes each night to journal three good things that occurred during the day.10 Mindfulness-based stress reduction has also been found to decrease perceptions of moral distress,9 and many mindfulness programs (such as Headspace®, a mindfulness and meditation app11) currently offer free membership to frontline providers during the pandemic. Mindfulness may be a particularly useful tool to leverage when one is stuck in the resignation phase and experiencing moral residue, described as a buildup of unresolved conflicts within the clinician that may crescendo with unresolved or inadequately resolved moral distress.6,12 Lastly, the American Association of Critical Care Nurses Ethics Workgroup developed the 4 A’s to Rise Above Moral Distress, which provides a framework of 4 concrete steps: ask appropriate questions, affirm your distress and your commitment to take care of yourself, assess or identify sources of your distress, and act or take action.13
Providers may experience moral distress in times of disaster. In applying this framework, we can gain self-insight and compassion, understand the types of moral distress our colleagues may be experiencing, and explore concrete tools for managing moral distress. Just as we confront the suffering of our COVID-positive patients, so too may we benefit from sitting with and naming our own suffering and moral distress.
Disclosures
The authors have nothing to disclose.
1. Morely G, Ives J, Bradbury-Jones C. Moral distress and austerity: an avoidable ethical challenge in healthcare. Health Care Anal. 2019;27(3):185-201. https://doi.org/10.1007/s10728-019-00376-8
2. Feuer A, Rashbaum W. ‘We ran out of space’: bodies pile up as N.Y. struggles to bury its dead. New York Times. April 30, 2020. Accessed June 20, 2020. https://www.nytimes.com/2020/04/30/nyregion/coronavirus-nyc-funeral-home-morgue-bodies.html
3. Coronavirus Disease 2019 (COVID-19): Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Accessed June 21, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
4. Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716-722. https://doi.org/10.1192/bjp.2018.210
5. Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510-512. https://doi.org/10.1056/nejmp2008017
6. Dunham AM, Rieder TN, Humbyrd CJ. A bioethical perspective for navigating moral dilemmas amidst the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):471-476. https://doi.org/10.5435/jaaos-d-20-00371
7. Interim Briefing Note: Addressing Mental Health and Psychosocial Aspects of COVID-19 Outbreak, Version 1.5. Reference Group on Mental Health and Psychosocial Support in Emergency Settings, Inter-Agency Standing Committee, United Nations; 2020. Accessed June 18, 2020. https://interagencystandingcommittee.org/system/files/2020-03/IASC%20Interim%20Briefing%20Note%20on%20COVID-19%20Outbreak%20Readiness%20and%20Response%20Operations%20-%20MHPSS_0.pdf
8. Cacchione PZ. Moral distress in the midst of the COVID-19 pandemic. Clin Nurs Res. 2020;29(4):215-216. https://doi.org/10.1177/1054773820920385
9. Vaclavik EA, Staffileno BA, Carlson E. Moral distress: using mindfulness-based stress reduction interventions to decrease nurse perceptions of distress. Clin J Oncol Nurs. 2018;22(3):326-332. https://doi.org/10.1188/18.cjon.326-332
10. Rippstein-Leuenberger K, Mauthner O, Bryan Sexton J, Schwendimann R. A qualitative analysis of the Three Good Things intervention in healthcare workers. BMJ Open. 2017;7(5):e015826. https://doi.org/10.1136/bmjopen-2017-015826
11. How is Headspace helping those impacted by COVID-19? Headspace. Accessed June 21, 2020. https://help.headspace.com/hc/en-us/articles/360045857254-How-is-Headspace-helping-those-impacted-by-COVID-19
12. Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330-342.
13. McCue C. Using the AACN framework to alleviate moral distress. OJIN: Online J Issues Nurs. 2010;16(1):9. https://doi.org/10.3912/ojin.vol16no01ppt02
Many US health care systems experienced a surge of critically ill corona virus disease 2019 (COVID-19) patients while lacking adequate resources to provide optimal care. Nurses, doctors, and other providers in the United States were confronted with having to implement crisis standards of care for the first time. The refrain “these are unprecedented times” was repeated to colleagues and patients. The demands and shortages of supplies are unique in recent history. As a result, many frontline responders have wrestled with moral distress, the feelings of distress experienced when forced to act—because of institutional or resource constraints—in a manner contrary to their beliefs.1 However, for those medical professionals whose work includes being deployed on global disaster response teams or providing healthcare in chronically low-resourced settings, navigating limitations of medicines, equipment, and personnel is a daily reality. We offer a framework for recognizing one’s own moral distress and that of one’s colleagues based on our experiences in global disaster response that may be helpful for clinicians during the COVID-19 pandemic.
A FRAMEWORK FOR MORAL DISTRESS
The intense and debilitating feelings of unexpected loss and helplessness faced by clinicians who are making challenging choices about medical interventions can be better understood by applying a theoretical framework that has the following three main stages in the evolution and response to moral distress: indignation, resignation, and acclimation. This framework can provide guidance to individuals experiencing distress during the COVID-19 pandemic and may also be beneficial in contextualizing interactions when working in teams or with referring providers.
Indignation
When working in a disaster setting, an initial period of indignation is common. The clinician is shocked and horrified by the conditions encountered, the severity of suffering, and a lack of resources with which they are unaccustomed. As we bear witness to the many healthcare providers who have fallen ill and died, we fear for our own safety in choosing to care for patients sick with COVID: “I’m risking my life caring for patients on the front lines, and it’s unacceptable that I’m not even being provided with adequate PPE!” Patients and families are suffering in ways we had previously thought our health system was capable of addressing: “How can I be a compassionate clinician when my patients are forced to die alone?!” It feels surreal and unacceptable that so many patients can die so quickly despite our heroic interventions and that we have very little control over their fate. We are unaccustomed to caring for so many dying patients at once. For example, during the peak of the pandemic in New York City, patients were dying at four times the city’s normal death rate.2 Indignation may be compounded in settings where providers are not even equipped to deal with the aftermath of deaths, such as piling bodies into makeshift morgues2: “I feel powerless to prevent my patients’ deaths and horrified that many are dying alone and scared, and now I can’t even guarantee that their bodies will be cared for after death!” Additionally, during this pandemic, many of us are now facing issues of resource allocation that we had never imagined dealing with. “I took an oath to care for and protect my patients. How could I possibly tell a patient we have no more ventilators to put them on? Who makes the decision of which patients deserve to live or die?” With the realization that COVID-19 has been disproportionately affecting racial and ethnic minorities, concerns for systemic discrimination within our healthcare system may rightly lead to a deep indignation.3
Resignation
After the initial indignation stage, resignation often follows. “I guess I can’t fix healthcare in this new setting, and I was foolish for even trying.” Clinicians go through the motions and continue to care for patients but feel disillusioned. Part of the ongoing stress involves the concern that they aren’t making a difference. Lack of viral testing may breed further resignation: Clinicians are on the front lines caring for patients that they are not even sure are positive for COVID-19, they have no way of accessing antibody testing for themselves to be able to gauge their own personal risks, and when there is not enough testing being done on a larger scale, there may be a sense that, by continuing to work on the front lines, they are sticking their finger in the dike, without actually having data to inform when it is safe to reopen states and ease restrictions. The suffering of patients and families may feel overwhelming and insurmountable. “I know I have to comply with my hospital’s visitor restriction policies, but it’s hard to see my patients suffering alone and know there’s nothing I can do to help them.”
Acclimation
Acclimation follows the indignation and resignation stages. Even amid disasters, a productive rhythm develops as teams coalesce and are galvanized by a shared sense of purpose. Clinicians make meaning out of their role in the crisis and in the care of the patients they can help, despite often deep and significant obstacles. “There’s a lot of suffering and a lot that I may not be able to fix, but some that I can.” Clinicians that have been deployed to unfamiliar roles may start to habituate and even enjoy having responsibilities and challenges that are different from those they typically face. Innovation during a pandemic may feel empowering. “I’m committed to making sure my dying patients and their families can say goodbye however possible. Although it’s not ideal, I’ve been using technology for virtual communication and advocating for families to visit in person when possible.”
RECOGNIZING THE STAGES OF MORAL DISTRESS
One’s path of moral distress through a disaster may not be linear; one does not necessarily progress through the stages of indignation, resignation, and acclimation in a certain order or at a certain pace. Additionally, the stages can recur throughout the disaster. Being able to recognize these stages may prove useful for the duration of this pandemic while waves of providers are redeployed in new settings and experience fresh indignation, whereas others who have been in the trenches for some time may be more likely experiencing resignation or, hopefully, acclimation. The trajectory and duration of this pandemic in the United States remains unclear. While hot spots such as Seattle, New York, and Boston may be moving past their peak phase and acclimating to a “new normal,” there remain concerns that surges may recur in the fall and winter, which will undoubtedly lead battle-weary clinicians to experience the stages of moral distress anew and potentially compounding their distress.
MANAGING MORAL DISTRESS
An added complexity in this pandemic is that we, as clinicians, are both the victims and the healers. From the literature on disaster mental health, we know that emotional suffering is universal in affected populations.4,5 Unlike many disaster scenarios in which teams leave the safety and security of well-established and well-resourced practices to deploy and care for disaster victims in new, austere environments, we are also part of that affected population in this pandemic. Each day or night, we return to homes that, too, are infiltrated by this pandemic. Our ability to move through the indignation, resignation, and acclimation stages may be hindered and blocked by our home responsibilities, stressors, and supports. Having to reconcile working in COVID-affected hospitals (particularly if caring for critically ill colleagues) only to return home to young or immunocompromised family members at night may place us in a state of indignation with its continued risk of burnout for the duration of this pandemic. Naming and acknowledging these painful challenges may allow self-compassion, self-forgiveness, and acceptance.
Though the primary focus of this article is to provide a framework to assist with the recognition of moral distress, it is important to address next steps once one recognizes someone is experiencing moral distress in this pandemic. Even outside of a disaster scenario, many clinicians feel obligated to put our patients’ needs before our own, and this sentiment is only heightened in a disaster scenario. It may feel unthinkable to call out sick or request a leave or reassignment during the pandemic. However, we are reminded that “the duty to serve is not endless.”6 Recognizing one’s own limits and reaching out to supervisors and mental health support before reaching one’s own limit is essential when experiencing moral distress.7,8
Cultivating resilience is also recognized as a tool for managing moral distress.6,9 For harried frontline clinicians, this may be as simple as taking a few minutes each night to journal three good things that occurred during the day.10 Mindfulness-based stress reduction has also been found to decrease perceptions of moral distress,9 and many mindfulness programs (such as Headspace®, a mindfulness and meditation app11) currently offer free membership to frontline providers during the pandemic. Mindfulness may be a particularly useful tool to leverage when one is stuck in the resignation phase and experiencing moral residue, described as a buildup of unresolved conflicts within the clinician that may crescendo with unresolved or inadequately resolved moral distress.6,12 Lastly, the American Association of Critical Care Nurses Ethics Workgroup developed the 4 A’s to Rise Above Moral Distress, which provides a framework of 4 concrete steps: ask appropriate questions, affirm your distress and your commitment to take care of yourself, assess or identify sources of your distress, and act or take action.13
Providers may experience moral distress in times of disaster. In applying this framework, we can gain self-insight and compassion, understand the types of moral distress our colleagues may be experiencing, and explore concrete tools for managing moral distress. Just as we confront the suffering of our COVID-positive patients, so too may we benefit from sitting with and naming our own suffering and moral distress.
Disclosures
The authors have nothing to disclose.
Many US health care systems experienced a surge of critically ill corona virus disease 2019 (COVID-19) patients while lacking adequate resources to provide optimal care. Nurses, doctors, and other providers in the United States were confronted with having to implement crisis standards of care for the first time. The refrain “these are unprecedented times” was repeated to colleagues and patients. The demands and shortages of supplies are unique in recent history. As a result, many frontline responders have wrestled with moral distress, the feelings of distress experienced when forced to act—because of institutional or resource constraints—in a manner contrary to their beliefs.1 However, for those medical professionals whose work includes being deployed on global disaster response teams or providing healthcare in chronically low-resourced settings, navigating limitations of medicines, equipment, and personnel is a daily reality. We offer a framework for recognizing one’s own moral distress and that of one’s colleagues based on our experiences in global disaster response that may be helpful for clinicians during the COVID-19 pandemic.
A FRAMEWORK FOR MORAL DISTRESS
The intense and debilitating feelings of unexpected loss and helplessness faced by clinicians who are making challenging choices about medical interventions can be better understood by applying a theoretical framework that has the following three main stages in the evolution and response to moral distress: indignation, resignation, and acclimation. This framework can provide guidance to individuals experiencing distress during the COVID-19 pandemic and may also be beneficial in contextualizing interactions when working in teams or with referring providers.
Indignation
When working in a disaster setting, an initial period of indignation is common. The clinician is shocked and horrified by the conditions encountered, the severity of suffering, and a lack of resources with which they are unaccustomed. As we bear witness to the many healthcare providers who have fallen ill and died, we fear for our own safety in choosing to care for patients sick with COVID: “I’m risking my life caring for patients on the front lines, and it’s unacceptable that I’m not even being provided with adequate PPE!” Patients and families are suffering in ways we had previously thought our health system was capable of addressing: “How can I be a compassionate clinician when my patients are forced to die alone?!” It feels surreal and unacceptable that so many patients can die so quickly despite our heroic interventions and that we have very little control over their fate. We are unaccustomed to caring for so many dying patients at once. For example, during the peak of the pandemic in New York City, patients were dying at four times the city’s normal death rate.2 Indignation may be compounded in settings where providers are not even equipped to deal with the aftermath of deaths, such as piling bodies into makeshift morgues2: “I feel powerless to prevent my patients’ deaths and horrified that many are dying alone and scared, and now I can’t even guarantee that their bodies will be cared for after death!” Additionally, during this pandemic, many of us are now facing issues of resource allocation that we had never imagined dealing with. “I took an oath to care for and protect my patients. How could I possibly tell a patient we have no more ventilators to put them on? Who makes the decision of which patients deserve to live or die?” With the realization that COVID-19 has been disproportionately affecting racial and ethnic minorities, concerns for systemic discrimination within our healthcare system may rightly lead to a deep indignation.3
Resignation
After the initial indignation stage, resignation often follows. “I guess I can’t fix healthcare in this new setting, and I was foolish for even trying.” Clinicians go through the motions and continue to care for patients but feel disillusioned. Part of the ongoing stress involves the concern that they aren’t making a difference. Lack of viral testing may breed further resignation: Clinicians are on the front lines caring for patients that they are not even sure are positive for COVID-19, they have no way of accessing antibody testing for themselves to be able to gauge their own personal risks, and when there is not enough testing being done on a larger scale, there may be a sense that, by continuing to work on the front lines, they are sticking their finger in the dike, without actually having data to inform when it is safe to reopen states and ease restrictions. The suffering of patients and families may feel overwhelming and insurmountable. “I know I have to comply with my hospital’s visitor restriction policies, but it’s hard to see my patients suffering alone and know there’s nothing I can do to help them.”
Acclimation
Acclimation follows the indignation and resignation stages. Even amid disasters, a productive rhythm develops as teams coalesce and are galvanized by a shared sense of purpose. Clinicians make meaning out of their role in the crisis and in the care of the patients they can help, despite often deep and significant obstacles. “There’s a lot of suffering and a lot that I may not be able to fix, but some that I can.” Clinicians that have been deployed to unfamiliar roles may start to habituate and even enjoy having responsibilities and challenges that are different from those they typically face. Innovation during a pandemic may feel empowering. “I’m committed to making sure my dying patients and their families can say goodbye however possible. Although it’s not ideal, I’ve been using technology for virtual communication and advocating for families to visit in person when possible.”
RECOGNIZING THE STAGES OF MORAL DISTRESS
One’s path of moral distress through a disaster may not be linear; one does not necessarily progress through the stages of indignation, resignation, and acclimation in a certain order or at a certain pace. Additionally, the stages can recur throughout the disaster. Being able to recognize these stages may prove useful for the duration of this pandemic while waves of providers are redeployed in new settings and experience fresh indignation, whereas others who have been in the trenches for some time may be more likely experiencing resignation or, hopefully, acclimation. The trajectory and duration of this pandemic in the United States remains unclear. While hot spots such as Seattle, New York, and Boston may be moving past their peak phase and acclimating to a “new normal,” there remain concerns that surges may recur in the fall and winter, which will undoubtedly lead battle-weary clinicians to experience the stages of moral distress anew and potentially compounding their distress.
MANAGING MORAL DISTRESS
An added complexity in this pandemic is that we, as clinicians, are both the victims and the healers. From the literature on disaster mental health, we know that emotional suffering is universal in affected populations.4,5 Unlike many disaster scenarios in which teams leave the safety and security of well-established and well-resourced practices to deploy and care for disaster victims in new, austere environments, we are also part of that affected population in this pandemic. Each day or night, we return to homes that, too, are infiltrated by this pandemic. Our ability to move through the indignation, resignation, and acclimation stages may be hindered and blocked by our home responsibilities, stressors, and supports. Having to reconcile working in COVID-affected hospitals (particularly if caring for critically ill colleagues) only to return home to young or immunocompromised family members at night may place us in a state of indignation with its continued risk of burnout for the duration of this pandemic. Naming and acknowledging these painful challenges may allow self-compassion, self-forgiveness, and acceptance.
Though the primary focus of this article is to provide a framework to assist with the recognition of moral distress, it is important to address next steps once one recognizes someone is experiencing moral distress in this pandemic. Even outside of a disaster scenario, many clinicians feel obligated to put our patients’ needs before our own, and this sentiment is only heightened in a disaster scenario. It may feel unthinkable to call out sick or request a leave or reassignment during the pandemic. However, we are reminded that “the duty to serve is not endless.”6 Recognizing one’s own limits and reaching out to supervisors and mental health support before reaching one’s own limit is essential when experiencing moral distress.7,8
Cultivating resilience is also recognized as a tool for managing moral distress.6,9 For harried frontline clinicians, this may be as simple as taking a few minutes each night to journal three good things that occurred during the day.10 Mindfulness-based stress reduction has also been found to decrease perceptions of moral distress,9 and many mindfulness programs (such as Headspace®, a mindfulness and meditation app11) currently offer free membership to frontline providers during the pandemic. Mindfulness may be a particularly useful tool to leverage when one is stuck in the resignation phase and experiencing moral residue, described as a buildup of unresolved conflicts within the clinician that may crescendo with unresolved or inadequately resolved moral distress.6,12 Lastly, the American Association of Critical Care Nurses Ethics Workgroup developed the 4 A’s to Rise Above Moral Distress, which provides a framework of 4 concrete steps: ask appropriate questions, affirm your distress and your commitment to take care of yourself, assess or identify sources of your distress, and act or take action.13
Providers may experience moral distress in times of disaster. In applying this framework, we can gain self-insight and compassion, understand the types of moral distress our colleagues may be experiencing, and explore concrete tools for managing moral distress. Just as we confront the suffering of our COVID-positive patients, so too may we benefit from sitting with and naming our own suffering and moral distress.
Disclosures
The authors have nothing to disclose.
1. Morely G, Ives J, Bradbury-Jones C. Moral distress and austerity: an avoidable ethical challenge in healthcare. Health Care Anal. 2019;27(3):185-201. https://doi.org/10.1007/s10728-019-00376-8
2. Feuer A, Rashbaum W. ‘We ran out of space’: bodies pile up as N.Y. struggles to bury its dead. New York Times. April 30, 2020. Accessed June 20, 2020. https://www.nytimes.com/2020/04/30/nyregion/coronavirus-nyc-funeral-home-morgue-bodies.html
3. Coronavirus Disease 2019 (COVID-19): Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Accessed June 21, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
4. Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716-722. https://doi.org/10.1192/bjp.2018.210
5. Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510-512. https://doi.org/10.1056/nejmp2008017
6. Dunham AM, Rieder TN, Humbyrd CJ. A bioethical perspective for navigating moral dilemmas amidst the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):471-476. https://doi.org/10.5435/jaaos-d-20-00371
7. Interim Briefing Note: Addressing Mental Health and Psychosocial Aspects of COVID-19 Outbreak, Version 1.5. Reference Group on Mental Health and Psychosocial Support in Emergency Settings, Inter-Agency Standing Committee, United Nations; 2020. Accessed June 18, 2020. https://interagencystandingcommittee.org/system/files/2020-03/IASC%20Interim%20Briefing%20Note%20on%20COVID-19%20Outbreak%20Readiness%20and%20Response%20Operations%20-%20MHPSS_0.pdf
8. Cacchione PZ. Moral distress in the midst of the COVID-19 pandemic. Clin Nurs Res. 2020;29(4):215-216. https://doi.org/10.1177/1054773820920385
9. Vaclavik EA, Staffileno BA, Carlson E. Moral distress: using mindfulness-based stress reduction interventions to decrease nurse perceptions of distress. Clin J Oncol Nurs. 2018;22(3):326-332. https://doi.org/10.1188/18.cjon.326-332
10. Rippstein-Leuenberger K, Mauthner O, Bryan Sexton J, Schwendimann R. A qualitative analysis of the Three Good Things intervention in healthcare workers. BMJ Open. 2017;7(5):e015826. https://doi.org/10.1136/bmjopen-2017-015826
11. How is Headspace helping those impacted by COVID-19? Headspace. Accessed June 21, 2020. https://help.headspace.com/hc/en-us/articles/360045857254-How-is-Headspace-helping-those-impacted-by-COVID-19
12. Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330-342.
13. McCue C. Using the AACN framework to alleviate moral distress. OJIN: Online J Issues Nurs. 2010;16(1):9. https://doi.org/10.3912/ojin.vol16no01ppt02
1. Morely G, Ives J, Bradbury-Jones C. Moral distress and austerity: an avoidable ethical challenge in healthcare. Health Care Anal. 2019;27(3):185-201. https://doi.org/10.1007/s10728-019-00376-8
2. Feuer A, Rashbaum W. ‘We ran out of space’: bodies pile up as N.Y. struggles to bury its dead. New York Times. April 30, 2020. Accessed June 20, 2020. https://www.nytimes.com/2020/04/30/nyregion/coronavirus-nyc-funeral-home-morgue-bodies.html
3. Coronavirus Disease 2019 (COVID-19): Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Accessed June 21, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
4. Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716-722. https://doi.org/10.1192/bjp.2018.210
5. Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510-512. https://doi.org/10.1056/nejmp2008017
6. Dunham AM, Rieder TN, Humbyrd CJ. A bioethical perspective for navigating moral dilemmas amidst the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):471-476. https://doi.org/10.5435/jaaos-d-20-00371
7. Interim Briefing Note: Addressing Mental Health and Psychosocial Aspects of COVID-19 Outbreak, Version 1.5. Reference Group on Mental Health and Psychosocial Support in Emergency Settings, Inter-Agency Standing Committee, United Nations; 2020. Accessed June 18, 2020. https://interagencystandingcommittee.org/system/files/2020-03/IASC%20Interim%20Briefing%20Note%20on%20COVID-19%20Outbreak%20Readiness%20and%20Response%20Operations%20-%20MHPSS_0.pdf
8. Cacchione PZ. Moral distress in the midst of the COVID-19 pandemic. Clin Nurs Res. 2020;29(4):215-216. https://doi.org/10.1177/1054773820920385
9. Vaclavik EA, Staffileno BA, Carlson E. Moral distress: using mindfulness-based stress reduction interventions to decrease nurse perceptions of distress. Clin J Oncol Nurs. 2018;22(3):326-332. https://doi.org/10.1188/18.cjon.326-332
10. Rippstein-Leuenberger K, Mauthner O, Bryan Sexton J, Schwendimann R. A qualitative analysis of the Three Good Things intervention in healthcare workers. BMJ Open. 2017;7(5):e015826. https://doi.org/10.1136/bmjopen-2017-015826
11. How is Headspace helping those impacted by COVID-19? Headspace. Accessed June 21, 2020. https://help.headspace.com/hc/en-us/articles/360045857254-How-is-Headspace-helping-those-impacted-by-COVID-19
12. Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330-342.
13. McCue C. Using the AACN framework to alleviate moral distress. OJIN: Online J Issues Nurs. 2010;16(1):9. https://doi.org/10.3912/ojin.vol16no01ppt02
© 2020 Society of Hospital Medicine
Preprints During the COVID-19 Pandemic: Public Health Emergencies and Medical Literature
Basic science and clinical research are the hallmarks of progress in biomedicine. Scientists rely on timely access to research findings to accelerate and strengthen their work, and clinicians depend on the latest data to ensure that the highest level of care reaches each patient’s bedside. Historically, academic journals have served as the gatekeepers of this knowledge, using expert peer review to cull the bad science from the good and ensure a meticulous standard of reporting before sharing information with the public. While robust and effective, the peer review process can, at times, be slow and cumbersome. During widespread emergencies, such as the current COVID-19 pandemic, delays in publication may handicap our ability to meet the urgent demands of the global scientific and medical communities. Indeed, academic journals initially struggled to manage the deluge of COVID-19–related submissions, with potential reviewers similarly occupied on the clinical front lines and unable to promptly evaluate pending submissions. This impasse necessarily hindered the dissemination of relevant clinical data, which left physicians operatingwith limited evidence in some settings and, in turn, may have led to potentially avoidable harm.1 Although many journals have since expedited their review processes in light of current pressing circumstances, these measures are not necessarily sustainable or scalable in the face of an increasingly expansive biomedical enterprise that will continue to face challenges of increasing urgency.2 Moreover, it remains unclear to what extent quality has been sacrificed in exchange for this temporary expedience.
ADVANTAGES OF THE PREPRINT SERVER SYSTEM
Scientific progress demands access to the rapid dissemination of robust data, and preprint servers are uniquely positioned to meet this need. Preprints are manuscripts released to the public before formal peer review and publication in an “official” indexed journal. Long used in mathematics and the physical sciences, preprint servers for the biomedical community such as medRxiv and bioRxiv have previously had limited traction because many have cited the risks of circulating information that may later be disputed or, worse, invalidated.3-6 The risk-benefit calculus, however, must be carefully considered. Preprints provide a fast and wide-reaching means for sharing new discoveries. Submissions often undergo a brief screening process to ensure appropriateness, but otherwise largely forego scientific review before being posted online where the data become freely and widely available to the public.
The enthusiasm for preprints in the current era has demonstrated both the promise and peril of a free and wide distribution strategy.5 Early in the COVID-19 pandemic, Western hospitals were flooded with critically ill patients and relied on reports from providers in China, where the disease had struck first, to define the basic pathophysiology. Guan et al shared the clinical symptoms, laboratory abnormalities, and radiologic findings of 1,099 patients with COVID-19 through preprint servers in early February 2020, well before many American clinicians had gained direct experience with SARS-CoV-2.7 Their findings were published in the New England Journal of Medicine 1 month later,8 but the initial preprint provided an early window into the largest threats that COVID-19 would pose for patients and the health system and corroborated that the increasing number of patients with acute respiratory distress syndrome was on pace to dwarf the number of available ventilators around the world. Physicians responded in kind and used preprints as a mechanism to share their early experience with awake prone positioning and shared ventilation, which were critical components of the global strategy to contend with the limited ventilator supply during the height of the pandemic.9-12
DISADVANTAGES OF THE PREPRINT SERVER SYSTEM
Despite these undisputed triumphs, hazards abound. Rapidly disseminating new findings via preprint servers neither implies shoddy science nor absolves investigators of the need for critical review, yet it provides opportunities for both. As an example, Gautret et al first shared their open-label study examining the efficacy of hydroxychloroquine and azithromycin for COVID-19 by using preprint publication.13 The study did not meet a priori sample size requirements, it incorporated a trial arm that was not prespecified, and it was promptly contradicted by a second trial, which raised concern about the validity of the findings.14 While the study was ultimately published in a journal, preprint allowed these often-misquoted data to circulate far longer than would have been possible were expert peer review to have requested strengthening of the findings.15 Under ideal circumstances, peer review serves to capture and address these types of methodologic errors in order to avoid the publication of misleading or incomplete results. By foregoing the peer review process when posting a preprint manuscript, investigators have an equal opportunity to share good and bad science with a community that may lack the expertise to distinguish between the two. Indeed, the results posted by Gautret et al were immediately amplified by media and policy makers alike, who touted hydroxychloroquine as a “game-changing” panacea despite the preliminary nature of the findings.16 Irrational exuberance then prompted drug hoarding and supply issues before more robust studies alerted providers to the potential adverse effects of this regimen and the limited evidence of any efficacy.17,18
Ultimately, both preprints and perfunctory peer review afford minimal safeguards to prevent the adoption of incomplete or misinterpreted results. While envisioned as a tool for scientific collaboration, preprints do have a broader readership that may be unaware of fundamental differences between a preprint manuscript and one reviewed by a rigorous academic journal. Considering the reliability of findings from these different domains as equivalent could ultimately cause public harm.
IMPROVING THE PREPRINT SERVER SYSTEM
To be sure, there are ways to enhance the current system and limit opportunities for misguided enthusiasm. Firstly, preprint servers can be difficult to navigate. Limited indexing in disparate silos that are distinct from the rest of the literature (ie, the U.S. National Library of Medicine’s PubMed) make relevant articles challenging to identify and, in some instances, relegate the curation of new papers to social media platforms. Resources to aggregate and query the growing database of submissions would improve our ability to identify appropriate articles and use this preliminary evidence base.
Secondly, once an article has been unearthed, few tools exist to help nonexpert readers evaluate the quality of the research. Many consumers, inclusive of other scientists, may not share the investigators’ expertise. Preprint platforms might aid readers by compiling metrics to indicate study quality. For example, a voting and commenting function to permit a form of crowd-sourced peer review, while imperfect, would allow subject matter experts to communicate the value of a submission and point out errors. Weighting of votes by the h-index or institution of each “reviewer” might further enhance the value of this crowd-sourced evaluation. Additionally, the site could indicate when there is broad agreement on a particular critique by alerting readers to an established limitation of the study in question. Ultimately, numerous such mechanisms might be considered, but all share the overarching goal of guiding readers to exercise appropriate caution in interpreting a study in order to avoid unfettered acceptance of flawed research.
Thirdly, preprint servers can minimize the circulation of outdated research by highlighting manuscripts whose findings have subsequently been disproven. There are certainly complexities in distinguishing between a scientific difference of opinion and an invalidated research finding, but rather than avoid these challenging topics, systems must acknowledge this critical nuance and address it transparently. Indeed, the more prominent preprint servers have already begun to limit the dissemination of clearly misleading research in acknowledgment of this responsibility.1,19 The biomedical community must continue to engage in open dialogue to determine where the filter is set between blocking harmful pseudoscience and honest efforts to evaluate research validity.
Lastly, while prominent preprint platforms continue to limit the dissemination of opinion pieces, clinical recommendations, and review articles, these submissions are among the most urgently useful content during a pandemic, as evidenced by the ongoing stream of published consensus statements and clinical guidelines. Moreover, these pieces are often invited unilaterally by journal editors and are less likely to undergo peer review before formal publication. Clinicians hunger for practical insights during this pandemic, and allowing guidelines and reviews to be posted rapidly—and to be flagged accordingly as “nonoriginal” research—could spark timely dialogue that might ultimately accelerate science.
Preprint servers do not obviate the need for critical scientific appraisal of their content; however, their risks are not an excuse to limit their adoption as an effective and practical data sharing platform. By embracing the rapid and transparent dissemination of data afforded by preprints, and thoughtfully navigating the caveats of applying new research (non–peer-reviewed manuscripts or otherwise), we will have added a powerful instrument to the biomedical armamentarium with lasting implications beyond the current crisis.
Disclosures
Dr Guterman reported receipt of grants from the National Institute of Neurological Disorders and Stroke (1K23NS116128-01), the National Institute on Aging (5R01AG056715), the American Academy of Neurology, as well as consulting fees from Marinus, Inc, that are outside the submitted work. Dr Braunstein reported no potential conflicts of interest.
1. Kwon D. How swamped preprint servers are blocking bad coronavirus research. Nature. 2020;581(7807):130-131. https://doi.org/10.1038/d41586-020-01394-6
2. Horbach SPJM. Pandemic publishing: medical journals drastically speed up their publication process for Covid-19. bioRxiv. Preprint posted online April 18, 2020. https://doi.org/10.1101/2020.04.18.045963
3. Serghiou S, Ioannidis JPA. Altmetric scores, citations, and publication of studies posted as preprints. JAMA. 2018;319(4):402. https://doi.org/10.1001/jama.2017.21168
4. Annesley T, Scott M, Bastian H, et al. Biomedical journals and preprint services: friends or foes? Clin Chem. 2017;63(2):453-458. https://doi.org/10.1373/clinchem.2016.268227
5. medRxiv: The Preprint Server for Health Sciences. 2020. Accessed March 26 2020. https://www.medrxiv.org
6. bioRxiv: The Preprint Server for Biology. 2020. Accessed June 15, 2020. https://www.biorxiv.org/
7. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. Preprint posted online February 9, 2020. https://doi.org/10.1101/2020.02.06.20020974
8. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. https://doi.org/10.1056/nejmoa2002032
9. Levin M, Chen MD, Shah A, et al. Differential ventilation using flow control valves as a potential bridge to full ventilatory support during the COVID-19 crisis. medRxiv. Preprint posted online April 21, 2020. https://doi.org/10.1101/2020.04.14.20053587
10. Dong W, Gong Y, Feng J, et al. Early awake prone and lateral position in non-intubated severe and critical patients with COVID-19 in Wuhan: a respective [sic] cohort study. medRxiv. Preprint posted online May 13, 2020. https://doi.org/10.1101/2020.05.09.20091454
11. Elharrar X, Trigui Y, Dols AM, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323(22):2336-2338. https://doi.org/10.1001/jama.2020.8255
12. Rosenthal BM, Pinkowski J, Goldstein J. ‘The other option is death’: New York starts sharing of ventilators. New York Times. March 26, 2020. Accessed June 15, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-ventilator-sharing.html
13. Gautret P, Lagier J, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: preliminary results of an open-label non-randomized clinical trial. medRxiv. Preprint posted online March 20, 2020. https://doi.org/10.1101/2020.03.16.20037135
14. Jun C, Danping L, Li L, et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19). J Zhejiang University. 2020;49(2):215-219. https://doi.org/10.3785/j.issn.1008-9292.2020.03.03
15. Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. Published online March 20, 2020. https://doi.org/10.1016/j.ijantimicag.2020.105949
16. Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Briefing. Whitehouse: Healthcare. March 20, 2020. Accessed March 27, 2020. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-vice-president-pence-members-c-oronavirus-task-force-press-briefing/
17. Torres S. Stop hoarding hydroxychloroquine. Many Americans, including me, need it. Washington Post. March 3, 2020. Accessed June 15, 2020. https://www.washingtonpost.com/opinions/2020/03/24/stop-hoarding-hydroxychloroquine-many-americans-including-me-need-it/
18. Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. Published online May 7, 2020. https://doi.org/10.1056/nejmoa2012410
19. Else H. How to bring preprints to the charged field of medicine. Nature. June 6, 2019. https://doi.org/10.1038/d41586-019-01806-2
Basic science and clinical research are the hallmarks of progress in biomedicine. Scientists rely on timely access to research findings to accelerate and strengthen their work, and clinicians depend on the latest data to ensure that the highest level of care reaches each patient’s bedside. Historically, academic journals have served as the gatekeepers of this knowledge, using expert peer review to cull the bad science from the good and ensure a meticulous standard of reporting before sharing information with the public. While robust and effective, the peer review process can, at times, be slow and cumbersome. During widespread emergencies, such as the current COVID-19 pandemic, delays in publication may handicap our ability to meet the urgent demands of the global scientific and medical communities. Indeed, academic journals initially struggled to manage the deluge of COVID-19–related submissions, with potential reviewers similarly occupied on the clinical front lines and unable to promptly evaluate pending submissions. This impasse necessarily hindered the dissemination of relevant clinical data, which left physicians operatingwith limited evidence in some settings and, in turn, may have led to potentially avoidable harm.1 Although many journals have since expedited their review processes in light of current pressing circumstances, these measures are not necessarily sustainable or scalable in the face of an increasingly expansive biomedical enterprise that will continue to face challenges of increasing urgency.2 Moreover, it remains unclear to what extent quality has been sacrificed in exchange for this temporary expedience.
ADVANTAGES OF THE PREPRINT SERVER SYSTEM
Scientific progress demands access to the rapid dissemination of robust data, and preprint servers are uniquely positioned to meet this need. Preprints are manuscripts released to the public before formal peer review and publication in an “official” indexed journal. Long used in mathematics and the physical sciences, preprint servers for the biomedical community such as medRxiv and bioRxiv have previously had limited traction because many have cited the risks of circulating information that may later be disputed or, worse, invalidated.3-6 The risk-benefit calculus, however, must be carefully considered. Preprints provide a fast and wide-reaching means for sharing new discoveries. Submissions often undergo a brief screening process to ensure appropriateness, but otherwise largely forego scientific review before being posted online where the data become freely and widely available to the public.
The enthusiasm for preprints in the current era has demonstrated both the promise and peril of a free and wide distribution strategy.5 Early in the COVID-19 pandemic, Western hospitals were flooded with critically ill patients and relied on reports from providers in China, where the disease had struck first, to define the basic pathophysiology. Guan et al shared the clinical symptoms, laboratory abnormalities, and radiologic findings of 1,099 patients with COVID-19 through preprint servers in early February 2020, well before many American clinicians had gained direct experience with SARS-CoV-2.7 Their findings were published in the New England Journal of Medicine 1 month later,8 but the initial preprint provided an early window into the largest threats that COVID-19 would pose for patients and the health system and corroborated that the increasing number of patients with acute respiratory distress syndrome was on pace to dwarf the number of available ventilators around the world. Physicians responded in kind and used preprints as a mechanism to share their early experience with awake prone positioning and shared ventilation, which were critical components of the global strategy to contend with the limited ventilator supply during the height of the pandemic.9-12
DISADVANTAGES OF THE PREPRINT SERVER SYSTEM
Despite these undisputed triumphs, hazards abound. Rapidly disseminating new findings via preprint servers neither implies shoddy science nor absolves investigators of the need for critical review, yet it provides opportunities for both. As an example, Gautret et al first shared their open-label study examining the efficacy of hydroxychloroquine and azithromycin for COVID-19 by using preprint publication.13 The study did not meet a priori sample size requirements, it incorporated a trial arm that was not prespecified, and it was promptly contradicted by a second trial, which raised concern about the validity of the findings.14 While the study was ultimately published in a journal, preprint allowed these often-misquoted data to circulate far longer than would have been possible were expert peer review to have requested strengthening of the findings.15 Under ideal circumstances, peer review serves to capture and address these types of methodologic errors in order to avoid the publication of misleading or incomplete results. By foregoing the peer review process when posting a preprint manuscript, investigators have an equal opportunity to share good and bad science with a community that may lack the expertise to distinguish between the two. Indeed, the results posted by Gautret et al were immediately amplified by media and policy makers alike, who touted hydroxychloroquine as a “game-changing” panacea despite the preliminary nature of the findings.16 Irrational exuberance then prompted drug hoarding and supply issues before more robust studies alerted providers to the potential adverse effects of this regimen and the limited evidence of any efficacy.17,18
Ultimately, both preprints and perfunctory peer review afford minimal safeguards to prevent the adoption of incomplete or misinterpreted results. While envisioned as a tool for scientific collaboration, preprints do have a broader readership that may be unaware of fundamental differences between a preprint manuscript and one reviewed by a rigorous academic journal. Considering the reliability of findings from these different domains as equivalent could ultimately cause public harm.
IMPROVING THE PREPRINT SERVER SYSTEM
To be sure, there are ways to enhance the current system and limit opportunities for misguided enthusiasm. Firstly, preprint servers can be difficult to navigate. Limited indexing in disparate silos that are distinct from the rest of the literature (ie, the U.S. National Library of Medicine’s PubMed) make relevant articles challenging to identify and, in some instances, relegate the curation of new papers to social media platforms. Resources to aggregate and query the growing database of submissions would improve our ability to identify appropriate articles and use this preliminary evidence base.
Secondly, once an article has been unearthed, few tools exist to help nonexpert readers evaluate the quality of the research. Many consumers, inclusive of other scientists, may not share the investigators’ expertise. Preprint platforms might aid readers by compiling metrics to indicate study quality. For example, a voting and commenting function to permit a form of crowd-sourced peer review, while imperfect, would allow subject matter experts to communicate the value of a submission and point out errors. Weighting of votes by the h-index or institution of each “reviewer” might further enhance the value of this crowd-sourced evaluation. Additionally, the site could indicate when there is broad agreement on a particular critique by alerting readers to an established limitation of the study in question. Ultimately, numerous such mechanisms might be considered, but all share the overarching goal of guiding readers to exercise appropriate caution in interpreting a study in order to avoid unfettered acceptance of flawed research.
Thirdly, preprint servers can minimize the circulation of outdated research by highlighting manuscripts whose findings have subsequently been disproven. There are certainly complexities in distinguishing between a scientific difference of opinion and an invalidated research finding, but rather than avoid these challenging topics, systems must acknowledge this critical nuance and address it transparently. Indeed, the more prominent preprint servers have already begun to limit the dissemination of clearly misleading research in acknowledgment of this responsibility.1,19 The biomedical community must continue to engage in open dialogue to determine where the filter is set between blocking harmful pseudoscience and honest efforts to evaluate research validity.
Lastly, while prominent preprint platforms continue to limit the dissemination of opinion pieces, clinical recommendations, and review articles, these submissions are among the most urgently useful content during a pandemic, as evidenced by the ongoing stream of published consensus statements and clinical guidelines. Moreover, these pieces are often invited unilaterally by journal editors and are less likely to undergo peer review before formal publication. Clinicians hunger for practical insights during this pandemic, and allowing guidelines and reviews to be posted rapidly—and to be flagged accordingly as “nonoriginal” research—could spark timely dialogue that might ultimately accelerate science.
Preprint servers do not obviate the need for critical scientific appraisal of their content; however, their risks are not an excuse to limit their adoption as an effective and practical data sharing platform. By embracing the rapid and transparent dissemination of data afforded by preprints, and thoughtfully navigating the caveats of applying new research (non–peer-reviewed manuscripts or otherwise), we will have added a powerful instrument to the biomedical armamentarium with lasting implications beyond the current crisis.
Disclosures
Dr Guterman reported receipt of grants from the National Institute of Neurological Disorders and Stroke (1K23NS116128-01), the National Institute on Aging (5R01AG056715), the American Academy of Neurology, as well as consulting fees from Marinus, Inc, that are outside the submitted work. Dr Braunstein reported no potential conflicts of interest.
Basic science and clinical research are the hallmarks of progress in biomedicine. Scientists rely on timely access to research findings to accelerate and strengthen their work, and clinicians depend on the latest data to ensure that the highest level of care reaches each patient’s bedside. Historically, academic journals have served as the gatekeepers of this knowledge, using expert peer review to cull the bad science from the good and ensure a meticulous standard of reporting before sharing information with the public. While robust and effective, the peer review process can, at times, be slow and cumbersome. During widespread emergencies, such as the current COVID-19 pandemic, delays in publication may handicap our ability to meet the urgent demands of the global scientific and medical communities. Indeed, academic journals initially struggled to manage the deluge of COVID-19–related submissions, with potential reviewers similarly occupied on the clinical front lines and unable to promptly evaluate pending submissions. This impasse necessarily hindered the dissemination of relevant clinical data, which left physicians operatingwith limited evidence in some settings and, in turn, may have led to potentially avoidable harm.1 Although many journals have since expedited their review processes in light of current pressing circumstances, these measures are not necessarily sustainable or scalable in the face of an increasingly expansive biomedical enterprise that will continue to face challenges of increasing urgency.2 Moreover, it remains unclear to what extent quality has been sacrificed in exchange for this temporary expedience.
ADVANTAGES OF THE PREPRINT SERVER SYSTEM
Scientific progress demands access to the rapid dissemination of robust data, and preprint servers are uniquely positioned to meet this need. Preprints are manuscripts released to the public before formal peer review and publication in an “official” indexed journal. Long used in mathematics and the physical sciences, preprint servers for the biomedical community such as medRxiv and bioRxiv have previously had limited traction because many have cited the risks of circulating information that may later be disputed or, worse, invalidated.3-6 The risk-benefit calculus, however, must be carefully considered. Preprints provide a fast and wide-reaching means for sharing new discoveries. Submissions often undergo a brief screening process to ensure appropriateness, but otherwise largely forego scientific review before being posted online where the data become freely and widely available to the public.
The enthusiasm for preprints in the current era has demonstrated both the promise and peril of a free and wide distribution strategy.5 Early in the COVID-19 pandemic, Western hospitals were flooded with critically ill patients and relied on reports from providers in China, where the disease had struck first, to define the basic pathophysiology. Guan et al shared the clinical symptoms, laboratory abnormalities, and radiologic findings of 1,099 patients with COVID-19 through preprint servers in early February 2020, well before many American clinicians had gained direct experience with SARS-CoV-2.7 Their findings were published in the New England Journal of Medicine 1 month later,8 but the initial preprint provided an early window into the largest threats that COVID-19 would pose for patients and the health system and corroborated that the increasing number of patients with acute respiratory distress syndrome was on pace to dwarf the number of available ventilators around the world. Physicians responded in kind and used preprints as a mechanism to share their early experience with awake prone positioning and shared ventilation, which were critical components of the global strategy to contend with the limited ventilator supply during the height of the pandemic.9-12
DISADVANTAGES OF THE PREPRINT SERVER SYSTEM
Despite these undisputed triumphs, hazards abound. Rapidly disseminating new findings via preprint servers neither implies shoddy science nor absolves investigators of the need for critical review, yet it provides opportunities for both. As an example, Gautret et al first shared their open-label study examining the efficacy of hydroxychloroquine and azithromycin for COVID-19 by using preprint publication.13 The study did not meet a priori sample size requirements, it incorporated a trial arm that was not prespecified, and it was promptly contradicted by a second trial, which raised concern about the validity of the findings.14 While the study was ultimately published in a journal, preprint allowed these often-misquoted data to circulate far longer than would have been possible were expert peer review to have requested strengthening of the findings.15 Under ideal circumstances, peer review serves to capture and address these types of methodologic errors in order to avoid the publication of misleading or incomplete results. By foregoing the peer review process when posting a preprint manuscript, investigators have an equal opportunity to share good and bad science with a community that may lack the expertise to distinguish between the two. Indeed, the results posted by Gautret et al were immediately amplified by media and policy makers alike, who touted hydroxychloroquine as a “game-changing” panacea despite the preliminary nature of the findings.16 Irrational exuberance then prompted drug hoarding and supply issues before more robust studies alerted providers to the potential adverse effects of this regimen and the limited evidence of any efficacy.17,18
Ultimately, both preprints and perfunctory peer review afford minimal safeguards to prevent the adoption of incomplete or misinterpreted results. While envisioned as a tool for scientific collaboration, preprints do have a broader readership that may be unaware of fundamental differences between a preprint manuscript and one reviewed by a rigorous academic journal. Considering the reliability of findings from these different domains as equivalent could ultimately cause public harm.
IMPROVING THE PREPRINT SERVER SYSTEM
To be sure, there are ways to enhance the current system and limit opportunities for misguided enthusiasm. Firstly, preprint servers can be difficult to navigate. Limited indexing in disparate silos that are distinct from the rest of the literature (ie, the U.S. National Library of Medicine’s PubMed) make relevant articles challenging to identify and, in some instances, relegate the curation of new papers to social media platforms. Resources to aggregate and query the growing database of submissions would improve our ability to identify appropriate articles and use this preliminary evidence base.
Secondly, once an article has been unearthed, few tools exist to help nonexpert readers evaluate the quality of the research. Many consumers, inclusive of other scientists, may not share the investigators’ expertise. Preprint platforms might aid readers by compiling metrics to indicate study quality. For example, a voting and commenting function to permit a form of crowd-sourced peer review, while imperfect, would allow subject matter experts to communicate the value of a submission and point out errors. Weighting of votes by the h-index or institution of each “reviewer” might further enhance the value of this crowd-sourced evaluation. Additionally, the site could indicate when there is broad agreement on a particular critique by alerting readers to an established limitation of the study in question. Ultimately, numerous such mechanisms might be considered, but all share the overarching goal of guiding readers to exercise appropriate caution in interpreting a study in order to avoid unfettered acceptance of flawed research.
Thirdly, preprint servers can minimize the circulation of outdated research by highlighting manuscripts whose findings have subsequently been disproven. There are certainly complexities in distinguishing between a scientific difference of opinion and an invalidated research finding, but rather than avoid these challenging topics, systems must acknowledge this critical nuance and address it transparently. Indeed, the more prominent preprint servers have already begun to limit the dissemination of clearly misleading research in acknowledgment of this responsibility.1,19 The biomedical community must continue to engage in open dialogue to determine where the filter is set between blocking harmful pseudoscience and honest efforts to evaluate research validity.
Lastly, while prominent preprint platforms continue to limit the dissemination of opinion pieces, clinical recommendations, and review articles, these submissions are among the most urgently useful content during a pandemic, as evidenced by the ongoing stream of published consensus statements and clinical guidelines. Moreover, these pieces are often invited unilaterally by journal editors and are less likely to undergo peer review before formal publication. Clinicians hunger for practical insights during this pandemic, and allowing guidelines and reviews to be posted rapidly—and to be flagged accordingly as “nonoriginal” research—could spark timely dialogue that might ultimately accelerate science.
Preprint servers do not obviate the need for critical scientific appraisal of their content; however, their risks are not an excuse to limit their adoption as an effective and practical data sharing platform. By embracing the rapid and transparent dissemination of data afforded by preprints, and thoughtfully navigating the caveats of applying new research (non–peer-reviewed manuscripts or otherwise), we will have added a powerful instrument to the biomedical armamentarium with lasting implications beyond the current crisis.
Disclosures
Dr Guterman reported receipt of grants from the National Institute of Neurological Disorders and Stroke (1K23NS116128-01), the National Institute on Aging (5R01AG056715), the American Academy of Neurology, as well as consulting fees from Marinus, Inc, that are outside the submitted work. Dr Braunstein reported no potential conflicts of interest.
1. Kwon D. How swamped preprint servers are blocking bad coronavirus research. Nature. 2020;581(7807):130-131. https://doi.org/10.1038/d41586-020-01394-6
2. Horbach SPJM. Pandemic publishing: medical journals drastically speed up their publication process for Covid-19. bioRxiv. Preprint posted online April 18, 2020. https://doi.org/10.1101/2020.04.18.045963
3. Serghiou S, Ioannidis JPA. Altmetric scores, citations, and publication of studies posted as preprints. JAMA. 2018;319(4):402. https://doi.org/10.1001/jama.2017.21168
4. Annesley T, Scott M, Bastian H, et al. Biomedical journals and preprint services: friends or foes? Clin Chem. 2017;63(2):453-458. https://doi.org/10.1373/clinchem.2016.268227
5. medRxiv: The Preprint Server for Health Sciences. 2020. Accessed March 26 2020. https://www.medrxiv.org
6. bioRxiv: The Preprint Server for Biology. 2020. Accessed June 15, 2020. https://www.biorxiv.org/
7. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. Preprint posted online February 9, 2020. https://doi.org/10.1101/2020.02.06.20020974
8. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. https://doi.org/10.1056/nejmoa2002032
9. Levin M, Chen MD, Shah A, et al. Differential ventilation using flow control valves as a potential bridge to full ventilatory support during the COVID-19 crisis. medRxiv. Preprint posted online April 21, 2020. https://doi.org/10.1101/2020.04.14.20053587
10. Dong W, Gong Y, Feng J, et al. Early awake prone and lateral position in non-intubated severe and critical patients with COVID-19 in Wuhan: a respective [sic] cohort study. medRxiv. Preprint posted online May 13, 2020. https://doi.org/10.1101/2020.05.09.20091454
11. Elharrar X, Trigui Y, Dols AM, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323(22):2336-2338. https://doi.org/10.1001/jama.2020.8255
12. Rosenthal BM, Pinkowski J, Goldstein J. ‘The other option is death’: New York starts sharing of ventilators. New York Times. March 26, 2020. Accessed June 15, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-ventilator-sharing.html
13. Gautret P, Lagier J, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: preliminary results of an open-label non-randomized clinical trial. medRxiv. Preprint posted online March 20, 2020. https://doi.org/10.1101/2020.03.16.20037135
14. Jun C, Danping L, Li L, et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19). J Zhejiang University. 2020;49(2):215-219. https://doi.org/10.3785/j.issn.1008-9292.2020.03.03
15. Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. Published online March 20, 2020. https://doi.org/10.1016/j.ijantimicag.2020.105949
16. Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Briefing. Whitehouse: Healthcare. March 20, 2020. Accessed March 27, 2020. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-vice-president-pence-members-c-oronavirus-task-force-press-briefing/
17. Torres S. Stop hoarding hydroxychloroquine. Many Americans, including me, need it. Washington Post. March 3, 2020. Accessed June 15, 2020. https://www.washingtonpost.com/opinions/2020/03/24/stop-hoarding-hydroxychloroquine-many-americans-including-me-need-it/
18. Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. Published online May 7, 2020. https://doi.org/10.1056/nejmoa2012410
19. Else H. How to bring preprints to the charged field of medicine. Nature. June 6, 2019. https://doi.org/10.1038/d41586-019-01806-2
1. Kwon D. How swamped preprint servers are blocking bad coronavirus research. Nature. 2020;581(7807):130-131. https://doi.org/10.1038/d41586-020-01394-6
2. Horbach SPJM. Pandemic publishing: medical journals drastically speed up their publication process for Covid-19. bioRxiv. Preprint posted online April 18, 2020. https://doi.org/10.1101/2020.04.18.045963
3. Serghiou S, Ioannidis JPA. Altmetric scores, citations, and publication of studies posted as preprints. JAMA. 2018;319(4):402. https://doi.org/10.1001/jama.2017.21168
4. Annesley T, Scott M, Bastian H, et al. Biomedical journals and preprint services: friends or foes? Clin Chem. 2017;63(2):453-458. https://doi.org/10.1373/clinchem.2016.268227
5. medRxiv: The Preprint Server for Health Sciences. 2020. Accessed March 26 2020. https://www.medrxiv.org
6. bioRxiv: The Preprint Server for Biology. 2020. Accessed June 15, 2020. https://www.biorxiv.org/
7. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. Preprint posted online February 9, 2020. https://doi.org/10.1101/2020.02.06.20020974
8. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. https://doi.org/10.1056/nejmoa2002032
9. Levin M, Chen MD, Shah A, et al. Differential ventilation using flow control valves as a potential bridge to full ventilatory support during the COVID-19 crisis. medRxiv. Preprint posted online April 21, 2020. https://doi.org/10.1101/2020.04.14.20053587
10. Dong W, Gong Y, Feng J, et al. Early awake prone and lateral position in non-intubated severe and critical patients with COVID-19 in Wuhan: a respective [sic] cohort study. medRxiv. Preprint posted online May 13, 2020. https://doi.org/10.1101/2020.05.09.20091454
11. Elharrar X, Trigui Y, Dols AM, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323(22):2336-2338. https://doi.org/10.1001/jama.2020.8255
12. Rosenthal BM, Pinkowski J, Goldstein J. ‘The other option is death’: New York starts sharing of ventilators. New York Times. March 26, 2020. Accessed June 15, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-ventilator-sharing.html
13. Gautret P, Lagier J, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: preliminary results of an open-label non-randomized clinical trial. medRxiv. Preprint posted online March 20, 2020. https://doi.org/10.1101/2020.03.16.20037135
14. Jun C, Danping L, Li L, et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19). J Zhejiang University. 2020;49(2):215-219. https://doi.org/10.3785/j.issn.1008-9292.2020.03.03
15. Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. Published online March 20, 2020. https://doi.org/10.1016/j.ijantimicag.2020.105949
16. Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Briefing. Whitehouse: Healthcare. March 20, 2020. Accessed March 27, 2020. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-vice-president-pence-members-c-oronavirus-task-force-press-briefing/
17. Torres S. Stop hoarding hydroxychloroquine. Many Americans, including me, need it. Washington Post. March 3, 2020. Accessed June 15, 2020. https://www.washingtonpost.com/opinions/2020/03/24/stop-hoarding-hydroxychloroquine-many-americans-including-me-need-it/
18. Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. Published online May 7, 2020. https://doi.org/10.1056/nejmoa2012410
19. Else H. How to bring preprints to the charged field of medicine. Nature. June 6, 2019. https://doi.org/10.1038/d41586-019-01806-2
© 2020 Society of Hospital Medicine
Fool Me Twice: The Role for Hospitals and Health Systems in Fixing the Broken PPE Supply Chain
The story of the coronavirus disease 2019 (COVID-19) pandemic in the United States has been defined, in part, by a persistent shortage of medical supplies that has made it difficult and dangerous for healthcare workers to care for infected patients. States, health systems, and even individual hospitals are currently competing against one another—sometimes at auction—to obtain personal protective equipment (PPE). This “Wild West” scenario has resulted in bizarre stories involving attempts to obtain PPE. One health system recently described a James Bond–like pursuit of essential PPE, complete with a covert trip to an industrial warehouse, trucks filled with masks but labeled as food delivery vehicles, and an intervention by a United States congressman.1 Many states have experienced analogous, but still atypical, stories: masks flown in from China using the private jet of a professional sports team owner,2 widespread use of novel sterilization modalities to allow PPE reuse,3 and one attempt to purchase price-gouged PPE from the host of the show “Shark Tank.”4 In some cases, hospitals and healthcare workers have pleaded for PPE on fundraising and social media sites.5
These profound deviations from operations of contemporary health system supply chains would have seemed beyond belief just a few months ago. Instead, they now echo the collective experiences of healthcare stakeholders trying to obtain PPE to protect their frontline healthcare workers during the COVID-19 pandemic.
HEALTHCARE MARKETS DURING A PANDEMIC
How did we get into this situation? The manufacture of medical supplies like gowns and masks is a highly competitive business with very slim margins, and as a result, medical equipment manufacturers aim to match their supply with the market’s demand, with hospitals and health systems using just-in-time ordering to limit excess inventory.6 While this approach adds efficiency and reduces costs, it also renders manufacturers and customers vulnerable to supply disruptions and shortages when need surges. The COVID-19 pandemic represents perhaps the most extreme example of a massive, widespread surge in demand that occurred multifocally and in a highly compressed time frame. Unlike other industries (eg, consumer paper products), however, in which demand exceeding supply causes inconvenience, the lack of PPE has led to critical public health consequences, with lives of both healthcare workers and vulnerable patients lost because of these shortages of medical equipment.
THE SPECIAL CASE OF PPE
There are many reasons for the PPE crisis. As noted above, manufacturers have prioritized efficiency over the ability to quickly increase production. They adhere to just-in-time ordering rather than planning for a surge in demand with extra production capacity, all to avoid having warehouses filled with unsold products if surges never occur. This strategy, compounded by the fact that most PPE in the United States is imported from areas in Asia that were profoundly affected early on by COVID-19, led to the observed widespread shortages. When PPE became unavailable from usual suppliers, hospitals were unable to locate other sources of existing PPE because of a lack of transparency about where PPE could be found and how it could be obtained. The Food and Drug Administration and other federal regulatory agencies maintained strict regulations around PPE production and, despite the crisis, made few exceptions.7 The FDA did grant a few Emergency Use Authorizations (EUAs) for certain improvised, decontaminated, or alternative respirators (eg, the Chinese-made KN95), but it has only very infrequently issued EUAs to allow domestic manufacturers to ramp up production.8 These failures were accompanied by an serious increase in PPE use, leading to spikes in price, price gouging, and hoarding,9 problems that were further magnified as health systems and hospitals were forced to compete with nonhealthcare businesses for PPE.
LACK OF FEDERAL GOVERNMENT RESPONSE
The Defense Production Act (DPA) gives the federal government the power to increase production of goods needed during a crisis8 to offer purchasing guarantees, coordinate federal agencies, and regulate distribution and pricing. However, the current administration’s failure to mount a coordinated federal response has contributed to the observed market instability, medical supply shortages, and public health crisis we face. We have previously recommended that the federal government use the power of the DPA to reduce manufacturers’ risk of being uncompensated for excess supply, support temporary reductions in regulatory barriers, and create mandatory centralized reporting of PPE supply, including completed PPE and its components.10 We stand by these recommendations but also acknowledge that hospitals and health systems may be simultaneously considering how to best prepare for future crises and even surges in demand over the next 18 months as the COVID-19 pandemic continues.
RECOMMENDATIONS FOR HEALTH SYSTEMS AND HOSPITALS
1. Encourage mandates at the hospital, health system, and state level regarding minimum inventory levels for essential equipment. Stockpiles are essential for emergency preparedness. In the long term, these sorts of stockpiles are economically infeasible without government help to maintain them. In the near term, however, it is sensible that hospitals and health systems would maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases. However, a soon-to-published study suggests that over 40% of hospitals had a PPE stockpile of less than 2 weeks.11 Although this survey was conducted at the height of the shortage, it suggests that there is opportunity for improvement.
2. Coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution. The best example of this is the seven-state purchasing consortium announced by New York Governor Andrew Cuomo in early May.12 Unfortunately, since the announcement, there have been few details about whether the states were successful in their effort to reduce prices or to obtain PPE in bulk. Still, hospitals and health systems could join or emulate purchasing collaboratives to allow resources to be better allocated according to need. There are barriers to such collaboratives because the market is currently set up to encourage competition among health systems and hospitals. During the pandemic, however, cooperation has increasingly been favored over competition in science and healthcare delivery. There are also existing hospital purchasing collaboratives (eg, Premier, Inc13), which have taken steps to vet suppliers and improve access to PPE, but it is not clear how successful these efforts have been to date.
3. Advocate for strong federal leadership, including support for increased domestic manufacturing; replenishment and maintenance of state and health system stockpiles of PPE, ventilators, and medications; and development of a centrally coordinated PPE allocation and distribution process. While hospitals and health systems may favor remaining as apolitical as possible, the need for a federal response to stabilize the PPE market may be too urgent and necessary to ignore.
CONCLUSION
As hospitals and health systems prepare for continued surges in COVID-19 cases, they face challenges in providing PPE for frontline clinicians and staff. A federal plan to enhance nimbleness in responding to multifocal, geographic outbreaks and ensure awareness regarding inventory would improve our chances to successfully navigate the next pandemic and optimize the protection of our health workers, patients, and public health. In the absence of such a plan, hospitals should maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases and should continue to attempt to coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution.
1. Artenstein AW. In pursuit of PPE. N Engl J Med. 2020;382(18):e46. https://doi.org/10.1056/nejmc2010025
2. McGrane V, Ellement JR. A Patriots plane full of 1 million N95 masks from China arrived Thursday. Here’s how the plan came together. Boston Globe. Updated April 2, 2020. Accessed April 27, 2020. https://www.bostonglobe.com/2020/04/02/nation/kraft-family-used-patriots-team-plane-shuttle-protective-masks-china-boston-wsj-reports/
3. Kolodny L. California plans to decontaminate 80,000 masks a day for health workers amid the COVID-19 pandemic. CNBC. April 8, 2020. Updated April 9, 2020. Accessed April 27, 2020. https://www.cnbc.com/2020/04/08/california-plans-to-sanitize-80000-n95-masks-a-day-for-health-workers.html
4. Levenson M. Company questions deal by ‘Shark Tank’ star to sell N95 masks to Florida. New York Times. April 22, 2020. Accessed May 20, 2020. https://www.nytimes.com/2020/04/22/us/daymond-john-n95-masks-florida-3m.html
5. Padilla M. ‘It feels like a war zone’: doctors and nurses plead for masks on social media. New York Times. March 19, 2020. Updated March 22, 2020. Accessed April 27, 2020. https://www.nytimes.com/2020/03/19/us/hospitals-coronavirus-ppe-shortage.html
6. Lee HL, Billington C. Managing supply chain inventory: pitfalls and opportunities. MIT Sloan Management Review. April 15, 1992. Accessed April 27, 2020. https://sloanreview.mit.edu/article/managing-supply-chain-inventory-pitfalls-and-opportunities/
7. Emergency Situations (Medical Devices): Emergency Use Authorizations. Food and Drug Administration. Accessed May 10, 2020. https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations
8. Watney C, Stapp A. Masks for All: Using Purchase Guarantees and Targeted Deregulation to Boost Production of Essential Medical Equipment. Mercatus Center: George Mason University. April 8, 2020. Accessed June 23, 2020. https://www.mercatus.org/publications/covid-19-crisis-response/masks-all-using-purchase-guarantees-and-targeted-deregulation
9. Volkov M. DOJ hoarding and price gouging task force seizes critical medical supplies and distributes to New York and New Jersey hospitals. Corruption, Crime & Compliance blog. April 2, 2020. Accessed April 27, 2020. https://blog.volkovlaw.com/2020/04/doj-hoarding-and-price-gouging-task-force-seizes-critical-medical-supplies-and-distributes-to-new-york-and-new-jersey-hospitals/
10. Lagu T, Werner R, Artenstein AW. Why don’t hospitals have enough masks? Because coronavirus broke the market. Washington Post. May 21, 2020. Accessed May 25, 2020. https://www.washingtonpost.com/outlook/2020/05/21/why-dont-hospitals-have-enough-masks-because-coronavirus-broke-market/
11. Auerbach A, O’Leary KJ, Harrison JD, et al. Hospital ward adaptation during the COVID-19 Pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15:483-488.
12. Voytko L. NY will team up with 6 states to buy medical supplies, Cuomo says. Forbes. May 3, 2020. Accessed May 26, 2020. https://www.forbes.com/sites/lisettevoytko/2020/05/03/ny-will-team-up-with-6-states-to-buy-medical-supplies-cuomo-says/
13. Premier. Supply Chain Solutions. Accessed May 26, 2020. https://www.premierinc.com/solutions/supply-chain
The story of the coronavirus disease 2019 (COVID-19) pandemic in the United States has been defined, in part, by a persistent shortage of medical supplies that has made it difficult and dangerous for healthcare workers to care for infected patients. States, health systems, and even individual hospitals are currently competing against one another—sometimes at auction—to obtain personal protective equipment (PPE). This “Wild West” scenario has resulted in bizarre stories involving attempts to obtain PPE. One health system recently described a James Bond–like pursuit of essential PPE, complete with a covert trip to an industrial warehouse, trucks filled with masks but labeled as food delivery vehicles, and an intervention by a United States congressman.1 Many states have experienced analogous, but still atypical, stories: masks flown in from China using the private jet of a professional sports team owner,2 widespread use of novel sterilization modalities to allow PPE reuse,3 and one attempt to purchase price-gouged PPE from the host of the show “Shark Tank.”4 In some cases, hospitals and healthcare workers have pleaded for PPE on fundraising and social media sites.5
These profound deviations from operations of contemporary health system supply chains would have seemed beyond belief just a few months ago. Instead, they now echo the collective experiences of healthcare stakeholders trying to obtain PPE to protect their frontline healthcare workers during the COVID-19 pandemic.
HEALTHCARE MARKETS DURING A PANDEMIC
How did we get into this situation? The manufacture of medical supplies like gowns and masks is a highly competitive business with very slim margins, and as a result, medical equipment manufacturers aim to match their supply with the market’s demand, with hospitals and health systems using just-in-time ordering to limit excess inventory.6 While this approach adds efficiency and reduces costs, it also renders manufacturers and customers vulnerable to supply disruptions and shortages when need surges. The COVID-19 pandemic represents perhaps the most extreme example of a massive, widespread surge in demand that occurred multifocally and in a highly compressed time frame. Unlike other industries (eg, consumer paper products), however, in which demand exceeding supply causes inconvenience, the lack of PPE has led to critical public health consequences, with lives of both healthcare workers and vulnerable patients lost because of these shortages of medical equipment.
THE SPECIAL CASE OF PPE
There are many reasons for the PPE crisis. As noted above, manufacturers have prioritized efficiency over the ability to quickly increase production. They adhere to just-in-time ordering rather than planning for a surge in demand with extra production capacity, all to avoid having warehouses filled with unsold products if surges never occur. This strategy, compounded by the fact that most PPE in the United States is imported from areas in Asia that were profoundly affected early on by COVID-19, led to the observed widespread shortages. When PPE became unavailable from usual suppliers, hospitals were unable to locate other sources of existing PPE because of a lack of transparency about where PPE could be found and how it could be obtained. The Food and Drug Administration and other federal regulatory agencies maintained strict regulations around PPE production and, despite the crisis, made few exceptions.7 The FDA did grant a few Emergency Use Authorizations (EUAs) for certain improvised, decontaminated, or alternative respirators (eg, the Chinese-made KN95), but it has only very infrequently issued EUAs to allow domestic manufacturers to ramp up production.8 These failures were accompanied by an serious increase in PPE use, leading to spikes in price, price gouging, and hoarding,9 problems that were further magnified as health systems and hospitals were forced to compete with nonhealthcare businesses for PPE.
LACK OF FEDERAL GOVERNMENT RESPONSE
The Defense Production Act (DPA) gives the federal government the power to increase production of goods needed during a crisis8 to offer purchasing guarantees, coordinate federal agencies, and regulate distribution and pricing. However, the current administration’s failure to mount a coordinated federal response has contributed to the observed market instability, medical supply shortages, and public health crisis we face. We have previously recommended that the federal government use the power of the DPA to reduce manufacturers’ risk of being uncompensated for excess supply, support temporary reductions in regulatory barriers, and create mandatory centralized reporting of PPE supply, including completed PPE and its components.10 We stand by these recommendations but also acknowledge that hospitals and health systems may be simultaneously considering how to best prepare for future crises and even surges in demand over the next 18 months as the COVID-19 pandemic continues.
RECOMMENDATIONS FOR HEALTH SYSTEMS AND HOSPITALS
1. Encourage mandates at the hospital, health system, and state level regarding minimum inventory levels for essential equipment. Stockpiles are essential for emergency preparedness. In the long term, these sorts of stockpiles are economically infeasible without government help to maintain them. In the near term, however, it is sensible that hospitals and health systems would maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases. However, a soon-to-published study suggests that over 40% of hospitals had a PPE stockpile of less than 2 weeks.11 Although this survey was conducted at the height of the shortage, it suggests that there is opportunity for improvement.
2. Coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution. The best example of this is the seven-state purchasing consortium announced by New York Governor Andrew Cuomo in early May.12 Unfortunately, since the announcement, there have been few details about whether the states were successful in their effort to reduce prices or to obtain PPE in bulk. Still, hospitals and health systems could join or emulate purchasing collaboratives to allow resources to be better allocated according to need. There are barriers to such collaboratives because the market is currently set up to encourage competition among health systems and hospitals. During the pandemic, however, cooperation has increasingly been favored over competition in science and healthcare delivery. There are also existing hospital purchasing collaboratives (eg, Premier, Inc13), which have taken steps to vet suppliers and improve access to PPE, but it is not clear how successful these efforts have been to date.
3. Advocate for strong federal leadership, including support for increased domestic manufacturing; replenishment and maintenance of state and health system stockpiles of PPE, ventilators, and medications; and development of a centrally coordinated PPE allocation and distribution process. While hospitals and health systems may favor remaining as apolitical as possible, the need for a federal response to stabilize the PPE market may be too urgent and necessary to ignore.
CONCLUSION
As hospitals and health systems prepare for continued surges in COVID-19 cases, they face challenges in providing PPE for frontline clinicians and staff. A federal plan to enhance nimbleness in responding to multifocal, geographic outbreaks and ensure awareness regarding inventory would improve our chances to successfully navigate the next pandemic and optimize the protection of our health workers, patients, and public health. In the absence of such a plan, hospitals should maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases and should continue to attempt to coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution.
The story of the coronavirus disease 2019 (COVID-19) pandemic in the United States has been defined, in part, by a persistent shortage of medical supplies that has made it difficult and dangerous for healthcare workers to care for infected patients. States, health systems, and even individual hospitals are currently competing against one another—sometimes at auction—to obtain personal protective equipment (PPE). This “Wild West” scenario has resulted in bizarre stories involving attempts to obtain PPE. One health system recently described a James Bond–like pursuit of essential PPE, complete with a covert trip to an industrial warehouse, trucks filled with masks but labeled as food delivery vehicles, and an intervention by a United States congressman.1 Many states have experienced analogous, but still atypical, stories: masks flown in from China using the private jet of a professional sports team owner,2 widespread use of novel sterilization modalities to allow PPE reuse,3 and one attempt to purchase price-gouged PPE from the host of the show “Shark Tank.”4 In some cases, hospitals and healthcare workers have pleaded for PPE on fundraising and social media sites.5
These profound deviations from operations of contemporary health system supply chains would have seemed beyond belief just a few months ago. Instead, they now echo the collective experiences of healthcare stakeholders trying to obtain PPE to protect their frontline healthcare workers during the COVID-19 pandemic.
HEALTHCARE MARKETS DURING A PANDEMIC
How did we get into this situation? The manufacture of medical supplies like gowns and masks is a highly competitive business with very slim margins, and as a result, medical equipment manufacturers aim to match their supply with the market’s demand, with hospitals and health systems using just-in-time ordering to limit excess inventory.6 While this approach adds efficiency and reduces costs, it also renders manufacturers and customers vulnerable to supply disruptions and shortages when need surges. The COVID-19 pandemic represents perhaps the most extreme example of a massive, widespread surge in demand that occurred multifocally and in a highly compressed time frame. Unlike other industries (eg, consumer paper products), however, in which demand exceeding supply causes inconvenience, the lack of PPE has led to critical public health consequences, with lives of both healthcare workers and vulnerable patients lost because of these shortages of medical equipment.
THE SPECIAL CASE OF PPE
There are many reasons for the PPE crisis. As noted above, manufacturers have prioritized efficiency over the ability to quickly increase production. They adhere to just-in-time ordering rather than planning for a surge in demand with extra production capacity, all to avoid having warehouses filled with unsold products if surges never occur. This strategy, compounded by the fact that most PPE in the United States is imported from areas in Asia that were profoundly affected early on by COVID-19, led to the observed widespread shortages. When PPE became unavailable from usual suppliers, hospitals were unable to locate other sources of existing PPE because of a lack of transparency about where PPE could be found and how it could be obtained. The Food and Drug Administration and other federal regulatory agencies maintained strict regulations around PPE production and, despite the crisis, made few exceptions.7 The FDA did grant a few Emergency Use Authorizations (EUAs) for certain improvised, decontaminated, or alternative respirators (eg, the Chinese-made KN95), but it has only very infrequently issued EUAs to allow domestic manufacturers to ramp up production.8 These failures were accompanied by an serious increase in PPE use, leading to spikes in price, price gouging, and hoarding,9 problems that were further magnified as health systems and hospitals were forced to compete with nonhealthcare businesses for PPE.
LACK OF FEDERAL GOVERNMENT RESPONSE
The Defense Production Act (DPA) gives the federal government the power to increase production of goods needed during a crisis8 to offer purchasing guarantees, coordinate federal agencies, and regulate distribution and pricing. However, the current administration’s failure to mount a coordinated federal response has contributed to the observed market instability, medical supply shortages, and public health crisis we face. We have previously recommended that the federal government use the power of the DPA to reduce manufacturers’ risk of being uncompensated for excess supply, support temporary reductions in regulatory barriers, and create mandatory centralized reporting of PPE supply, including completed PPE and its components.10 We stand by these recommendations but also acknowledge that hospitals and health systems may be simultaneously considering how to best prepare for future crises and even surges in demand over the next 18 months as the COVID-19 pandemic continues.
RECOMMENDATIONS FOR HEALTH SYSTEMS AND HOSPITALS
1. Encourage mandates at the hospital, health system, and state level regarding minimum inventory levels for essential equipment. Stockpiles are essential for emergency preparedness. In the long term, these sorts of stockpiles are economically infeasible without government help to maintain them. In the near term, however, it is sensible that hospitals and health systems would maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases. However, a soon-to-published study suggests that over 40% of hospitals had a PPE stockpile of less than 2 weeks.11 Although this survey was conducted at the height of the shortage, it suggests that there is opportunity for improvement.
2. Coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution. The best example of this is the seven-state purchasing consortium announced by New York Governor Andrew Cuomo in early May.12 Unfortunately, since the announcement, there have been few details about whether the states were successful in their effort to reduce prices or to obtain PPE in bulk. Still, hospitals and health systems could join or emulate purchasing collaboratives to allow resources to be better allocated according to need. There are barriers to such collaboratives because the market is currently set up to encourage competition among health systems and hospitals. During the pandemic, however, cooperation has increasingly been favored over competition in science and healthcare delivery. There are also existing hospital purchasing collaboratives (eg, Premier, Inc13), which have taken steps to vet suppliers and improve access to PPE, but it is not clear how successful these efforts have been to date.
3. Advocate for strong federal leadership, including support for increased domestic manufacturing; replenishment and maintenance of state and health system stockpiles of PPE, ventilators, and medications; and development of a centrally coordinated PPE allocation and distribution process. While hospitals and health systems may favor remaining as apolitical as possible, the need for a federal response to stabilize the PPE market may be too urgent and necessary to ignore.
CONCLUSION
As hospitals and health systems prepare for continued surges in COVID-19 cases, they face challenges in providing PPE for frontline clinicians and staff. A federal plan to enhance nimbleness in responding to multifocal, geographic outbreaks and ensure awareness regarding inventory would improve our chances to successfully navigate the next pandemic and optimize the protection of our health workers, patients, and public health. In the absence of such a plan, hospitals should maintain a minimum of 2 weeks’ worth of PPE to prepare for expected regional spikes in COVID-19 cases and should continue to attempt to coordinate efforts among states and health systems to collect and report inventory, regionalize resources, and coordinate their distribution.
1. Artenstein AW. In pursuit of PPE. N Engl J Med. 2020;382(18):e46. https://doi.org/10.1056/nejmc2010025
2. McGrane V, Ellement JR. A Patriots plane full of 1 million N95 masks from China arrived Thursday. Here’s how the plan came together. Boston Globe. Updated April 2, 2020. Accessed April 27, 2020. https://www.bostonglobe.com/2020/04/02/nation/kraft-family-used-patriots-team-plane-shuttle-protective-masks-china-boston-wsj-reports/
3. Kolodny L. California plans to decontaminate 80,000 masks a day for health workers amid the COVID-19 pandemic. CNBC. April 8, 2020. Updated April 9, 2020. Accessed April 27, 2020. https://www.cnbc.com/2020/04/08/california-plans-to-sanitize-80000-n95-masks-a-day-for-health-workers.html
4. Levenson M. Company questions deal by ‘Shark Tank’ star to sell N95 masks to Florida. New York Times. April 22, 2020. Accessed May 20, 2020. https://www.nytimes.com/2020/04/22/us/daymond-john-n95-masks-florida-3m.html
5. Padilla M. ‘It feels like a war zone’: doctors and nurses plead for masks on social media. New York Times. March 19, 2020. Updated March 22, 2020. Accessed April 27, 2020. https://www.nytimes.com/2020/03/19/us/hospitals-coronavirus-ppe-shortage.html
6. Lee HL, Billington C. Managing supply chain inventory: pitfalls and opportunities. MIT Sloan Management Review. April 15, 1992. Accessed April 27, 2020. https://sloanreview.mit.edu/article/managing-supply-chain-inventory-pitfalls-and-opportunities/
7. Emergency Situations (Medical Devices): Emergency Use Authorizations. Food and Drug Administration. Accessed May 10, 2020. https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations
8. Watney C, Stapp A. Masks for All: Using Purchase Guarantees and Targeted Deregulation to Boost Production of Essential Medical Equipment. Mercatus Center: George Mason University. April 8, 2020. Accessed June 23, 2020. https://www.mercatus.org/publications/covid-19-crisis-response/masks-all-using-purchase-guarantees-and-targeted-deregulation
9. Volkov M. DOJ hoarding and price gouging task force seizes critical medical supplies and distributes to New York and New Jersey hospitals. Corruption, Crime & Compliance blog. April 2, 2020. Accessed April 27, 2020. https://blog.volkovlaw.com/2020/04/doj-hoarding-and-price-gouging-task-force-seizes-critical-medical-supplies-and-distributes-to-new-york-and-new-jersey-hospitals/
10. Lagu T, Werner R, Artenstein AW. Why don’t hospitals have enough masks? Because coronavirus broke the market. Washington Post. May 21, 2020. Accessed May 25, 2020. https://www.washingtonpost.com/outlook/2020/05/21/why-dont-hospitals-have-enough-masks-because-coronavirus-broke-market/
11. Auerbach A, O’Leary KJ, Harrison JD, et al. Hospital ward adaptation during the COVID-19 Pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15:483-488.
12. Voytko L. NY will team up with 6 states to buy medical supplies, Cuomo says. Forbes. May 3, 2020. Accessed May 26, 2020. https://www.forbes.com/sites/lisettevoytko/2020/05/03/ny-will-team-up-with-6-states-to-buy-medical-supplies-cuomo-says/
13. Premier. Supply Chain Solutions. Accessed May 26, 2020. https://www.premierinc.com/solutions/supply-chain
1. Artenstein AW. In pursuit of PPE. N Engl J Med. 2020;382(18):e46. https://doi.org/10.1056/nejmc2010025
2. McGrane V, Ellement JR. A Patriots plane full of 1 million N95 masks from China arrived Thursday. Here’s how the plan came together. Boston Globe. Updated April 2, 2020. Accessed April 27, 2020. https://www.bostonglobe.com/2020/04/02/nation/kraft-family-used-patriots-team-plane-shuttle-protective-masks-china-boston-wsj-reports/
3. Kolodny L. California plans to decontaminate 80,000 masks a day for health workers amid the COVID-19 pandemic. CNBC. April 8, 2020. Updated April 9, 2020. Accessed April 27, 2020. https://www.cnbc.com/2020/04/08/california-plans-to-sanitize-80000-n95-masks-a-day-for-health-workers.html
4. Levenson M. Company questions deal by ‘Shark Tank’ star to sell N95 masks to Florida. New York Times. April 22, 2020. Accessed May 20, 2020. https://www.nytimes.com/2020/04/22/us/daymond-john-n95-masks-florida-3m.html
5. Padilla M. ‘It feels like a war zone’: doctors and nurses plead for masks on social media. New York Times. March 19, 2020. Updated March 22, 2020. Accessed April 27, 2020. https://www.nytimes.com/2020/03/19/us/hospitals-coronavirus-ppe-shortage.html
6. Lee HL, Billington C. Managing supply chain inventory: pitfalls and opportunities. MIT Sloan Management Review. April 15, 1992. Accessed April 27, 2020. https://sloanreview.mit.edu/article/managing-supply-chain-inventory-pitfalls-and-opportunities/
7. Emergency Situations (Medical Devices): Emergency Use Authorizations. Food and Drug Administration. Accessed May 10, 2020. https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations
8. Watney C, Stapp A. Masks for All: Using Purchase Guarantees and Targeted Deregulation to Boost Production of Essential Medical Equipment. Mercatus Center: George Mason University. April 8, 2020. Accessed June 23, 2020. https://www.mercatus.org/publications/covid-19-crisis-response/masks-all-using-purchase-guarantees-and-targeted-deregulation
9. Volkov M. DOJ hoarding and price gouging task force seizes critical medical supplies and distributes to New York and New Jersey hospitals. Corruption, Crime & Compliance blog. April 2, 2020. Accessed April 27, 2020. https://blog.volkovlaw.com/2020/04/doj-hoarding-and-price-gouging-task-force-seizes-critical-medical-supplies-and-distributes-to-new-york-and-new-jersey-hospitals/
10. Lagu T, Werner R, Artenstein AW. Why don’t hospitals have enough masks? Because coronavirus broke the market. Washington Post. May 21, 2020. Accessed May 25, 2020. https://www.washingtonpost.com/outlook/2020/05/21/why-dont-hospitals-have-enough-masks-because-coronavirus-broke-market/
11. Auerbach A, O’Leary KJ, Harrison JD, et al. Hospital ward adaptation during the COVID-19 Pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15:483-488.
12. Voytko L. NY will team up with 6 states to buy medical supplies, Cuomo says. Forbes. May 3, 2020. Accessed May 26, 2020. https://www.forbes.com/sites/lisettevoytko/2020/05/03/ny-will-team-up-with-6-states-to-buy-medical-supplies-cuomo-says/
13. Premier. Supply Chain Solutions. Accessed May 26, 2020. https://www.premierinc.com/solutions/supply-chain
© 2020 Society of Hospital Medicine
To Suffer Alone: Hospital Visitation Policies During COVID-19
When my grandfather, who speaks limited English, was admitted to a hospital following a stroke amid the coronavirus disease 2019 (COVID-19) pandemic, my family was understandably worried. Sure enough, within just hours of his admission, we were told our normally very calm and beloved Nana was experiencing significant agitation and delirium. He did not understand nurses’ efforts to calm him down, became even more confused, and was eventually sedated and placed in physical restraints. Even though my family’s presence might have prevented some or all of this terrible series of events, the hospital’s visiting policies during the wave of COVID-19 admissions meant that we were forced to wait in the parking lot as they transpired. The hospital’s policy at the time only allowed visitors for pediatrics, end-of-life care, or labor, not for patients with delirium or altered mental status. We were given the option to make a video call, but my grandfather’s stroke had almost completely taken away his vision. Instead of sitting by his side, comforting him, providing explanations in voices he knew and a language he understood, we were left imagining how difficult it must be to suddenly wake up in an unfamiliar environment, with strangers speaking a different language, limited vision, and your arms and legs tied. Intellectually, I understood the hospital’s goals to minimize transmission, but spiritually and emotionally, it felt very cruel and very wrong.
The next day, we successfully petitioned administration to make an exception for one visitor. We argued that our presence would allow for removal of the sedation and restraints. The clinical team agreed that video calls were insufficient in his situation; he was allowed a visitor. We decided that it should be my mother. As soon my grandfather heard her familiar voice, there was a dramatic improvement. He immediately became calmer and restraints were no longer necessary. The team was grateful for a better physical exam and my grandfather was more cooperative with physical therapy. A few days later, unfortunately, the hospital let us know that they had reevaluated their position on my mother’s visits and that she posed an unnecessary COVID-19 risk to medical staff and other patients. And as soon as she left, my grandfather was again agitated and confused for the remaining 3 days of his hospitalization. Although we are grateful that his delirium resolved once he returned home, delirium also has the potential to lead to long-term cognitive impairment.1
The COVID-19 pandemic has required hospitals around the world to make difficult decisions about how to balance minimizing disease transmission with continuing to provide compassionate and high-quality patient care. Of these many dilemmas, developing flexible visitor policies is particularly difficult. Currently, the Centers for Disease Control and Prevention and many state health departments encourage limiting visitation in general but recognize the need for exceptions in special circumstances such as in end-of-life settings or altered mental status.2-4
At the hospital level, there is substantial variation in visitation policies among hospitals. Near our family home in San Jose, California, one hospital currently allows visitation for pediatric patients, pregnant patients, end-of-life patients, surgical patients, and patients in the emergency department, as well as those with mental disabilities or safety needs.5 A mere 10 minutes away, another hospital has implemented a very different policy that allows only one visitor for pregnant patients and in end-of-life settings; there are no exceptions for patients with cognitive or physical disabilities.6 Other hospitals in the United States have gone even further, not permitting visitors even for those at the end of life.7 These patients are forced to spend their last few moments alone.
From an infection control perspective, there are certainly valid reasons to limit visitation. Even with temperature screenings, any movement into and out of a hospital poses a risk of transmitting disease. Infected but asymptomatic persons are known to transmit the disease. Additionally, hospitals still treat non–COVID-19 patients who are most susceptible to severe illness should they develop COVID-19 infection. Early in the COVID-19 pandemic, limitations in testing capacity, personal protective equipment (PPE), and staffing made it challenging to ensure safe visitation. In many cases, it was almost impossible to mitigate the transmission risk that visitors posed. Because many hospitals did not have the capacity to test all symptomatic patients, they could not reliably limit visits to COVID-19–positive patients. Additionally, without enough PPE for healthcare workers, hospitals could not afford for visitors to use additional PPE.
Now that testing is more readily available and some aspects of the PPE shortages have been addressed, we should not forget that visitation has significant benefits for both patients’ psychological well-being and their overall outcomes.8 Putting aside the emotional support that the physical presence of loved ones can offer, a large body of research indicates that allowing visitors can also meaningfully improve other important patient outcomes. Specifically, the presence of visitors is associated with less fear,9 reduced delirium,10 and even faster recovery.8 In many cases, family members can also help improve hospital safety surveillance and catch medical errors.11
I saw firsthand how these benefits are particularly true for visitors who are also a patient’s primary caretaker. When my mother visited my grandfather, she was not simply a visitor but instead served as an active member of the care team. In addition to providing emotional comfort, my mother oriented him to his surroundings, successfully encouraged oral intake, and even caught some medication errors. Particularly for patients with cognitive impairment, caretakers know the patient better than anyone on the clinical team, and their absence can negatively affect the quality of care.
As a family member who also has familiarity with the healthcare system, I share hospitals’ concerns about wanting to minimize disease transmission. I recognize that, even with PPE and screenings, there is still a chance that visitors unknowingly spread COVID-19 to others in the hospital. On a personal level, however, it feels inhumane to maintain this policy even when it affects particularly vulnerable patients like my grandfather. As some hospitals are already doing,12 we can take steps to allow visitors for such patients while minimizing the likelihood of COVID-19 disease transmission from visitors. Arriving visitors can be screened and required to wear PPE. While these measures may not eliminate the risk of COVID-19 transmission from visitors, they will likely reduce it significantly when implemented properly and make possible a more humane experience for all.13
Fortunately, my grandfather is now recovering comfortably at home, surrounded by his loved ones. To this day, however, he has not forgotten what it was like to be confused and alone in the hospital after his stroke. Even with loved ones around, a stroke is a profoundly distressing experience. To go through such an experience alone is even worse. Because of our petitioning, my grandfather was at least allowed a visitor for part of his stay. Other patients are not even allowed that. As we plan for the pandemic’s next waves, hospitals should reevaluate their visitor policies to ensure that their most vulnerable patients do not have to suffer alone.
Acknowledgment
The author sincerely thanks Dr Allan Goroll (Massachusetts General Hospital/Harvard Medical School) for his mentorship and critical review of this manuscript.
Disclosure
The author has nothing to disclose.
1. MacLullich PAMJ, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009;21(1):30-42. https://doi.org/10.1080/09540260802675031
2. Visitor Limitations Guidance. AFL 20-38. State of California—Health and Human Services Agency. California Department of Public Health. Accessed May 29, 2020. https://www.cdph.ca.gov/Programs/CHCQ/LCP/Pages/AFL-20-38.aspx
3. Coronavirus Disease 2019 (COVID-19): Managing Visitors. Centers for Disease Control and Prevention. February 11, 2020. Accessed May 29, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html
4. Maziarz MO. Mandatory Guidelines for Visitors and Facility Staff. https://www.state.nj.us/health/legal/covid19/3-16-2020_MandatoryGuidelinesforVisitors_andFacilityStaff_%20Supersedes3-13-2020Guidelines.pdf
5. Visitor Policy. Good Samaritan Hospital. Accessed May 29, 2020. https://goodsamsanjose.com/covid-19/visitor-policy.dot
6. Visitors Information. El Camino Health. May 7, 2015. Accessed May 29, 2020. https://www.elcaminohealth.org/patients-visitors-guide/before-you-arrive/visitors-information
7. Wakam GK, Montgomery JR, Biesterveld BE, Brown CS. Not dying alone - modern compassionate care in the Covid-19 pandemic. N Engl J Med. 2020;382(24):e88. https://doi.org/10.1056/nejmp2007781
8. Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-1761. https://doi.org/10.1097/ccm.0000000000002624
9. Falk J, Wongsa S, Dang J, Comer L, LoBiondo-Wood G. Using an evidence-based practice process to change child visitation guidelines. Clin J Oncol Nurs. 2012;16(1):21-23. https://doi.org/10.1188/12.cjon.21-23
10. Granberg A, Engberg IB, Lundberg D. Acute confusion and unreal experiences in intensive care patients in relation to the ICU syndrome. part II. Intensive Crit Care Nurs. 1999;15(1):19-33. https://doi.org/10.1016/s0964-3397(99)80062-7
11. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. 2017;171(4):372-381. https://doi.org/10.1001/jamapediatrics.2016.4812
12. Patient and Visitor Guidelines. UW Health: COVID-19 Information. Accessed June 18, 2020. https://coronavirus.uwhealth.org/patient-and-visitor-guidelines/
13. Whyte J. No visitors allowed: We need humane hospital policy during COVID-19. The Hill. April 2, 2020. Accessed June 18, 2020. https://thehill.com/opinion/healthcare/490828-no-visitors-allowed-we-need-humane-hospital-policy-during-covid-19
When my grandfather, who speaks limited English, was admitted to a hospital following a stroke amid the coronavirus disease 2019 (COVID-19) pandemic, my family was understandably worried. Sure enough, within just hours of his admission, we were told our normally very calm and beloved Nana was experiencing significant agitation and delirium. He did not understand nurses’ efforts to calm him down, became even more confused, and was eventually sedated and placed in physical restraints. Even though my family’s presence might have prevented some or all of this terrible series of events, the hospital’s visiting policies during the wave of COVID-19 admissions meant that we were forced to wait in the parking lot as they transpired. The hospital’s policy at the time only allowed visitors for pediatrics, end-of-life care, or labor, not for patients with delirium or altered mental status. We were given the option to make a video call, but my grandfather’s stroke had almost completely taken away his vision. Instead of sitting by his side, comforting him, providing explanations in voices he knew and a language he understood, we were left imagining how difficult it must be to suddenly wake up in an unfamiliar environment, with strangers speaking a different language, limited vision, and your arms and legs tied. Intellectually, I understood the hospital’s goals to minimize transmission, but spiritually and emotionally, it felt very cruel and very wrong.
The next day, we successfully petitioned administration to make an exception for one visitor. We argued that our presence would allow for removal of the sedation and restraints. The clinical team agreed that video calls were insufficient in his situation; he was allowed a visitor. We decided that it should be my mother. As soon my grandfather heard her familiar voice, there was a dramatic improvement. He immediately became calmer and restraints were no longer necessary. The team was grateful for a better physical exam and my grandfather was more cooperative with physical therapy. A few days later, unfortunately, the hospital let us know that they had reevaluated their position on my mother’s visits and that she posed an unnecessary COVID-19 risk to medical staff and other patients. And as soon as she left, my grandfather was again agitated and confused for the remaining 3 days of his hospitalization. Although we are grateful that his delirium resolved once he returned home, delirium also has the potential to lead to long-term cognitive impairment.1
The COVID-19 pandemic has required hospitals around the world to make difficult decisions about how to balance minimizing disease transmission with continuing to provide compassionate and high-quality patient care. Of these many dilemmas, developing flexible visitor policies is particularly difficult. Currently, the Centers for Disease Control and Prevention and many state health departments encourage limiting visitation in general but recognize the need for exceptions in special circumstances such as in end-of-life settings or altered mental status.2-4
At the hospital level, there is substantial variation in visitation policies among hospitals. Near our family home in San Jose, California, one hospital currently allows visitation for pediatric patients, pregnant patients, end-of-life patients, surgical patients, and patients in the emergency department, as well as those with mental disabilities or safety needs.5 A mere 10 minutes away, another hospital has implemented a very different policy that allows only one visitor for pregnant patients and in end-of-life settings; there are no exceptions for patients with cognitive or physical disabilities.6 Other hospitals in the United States have gone even further, not permitting visitors even for those at the end of life.7 These patients are forced to spend their last few moments alone.
From an infection control perspective, there are certainly valid reasons to limit visitation. Even with temperature screenings, any movement into and out of a hospital poses a risk of transmitting disease. Infected but asymptomatic persons are known to transmit the disease. Additionally, hospitals still treat non–COVID-19 patients who are most susceptible to severe illness should they develop COVID-19 infection. Early in the COVID-19 pandemic, limitations in testing capacity, personal protective equipment (PPE), and staffing made it challenging to ensure safe visitation. In many cases, it was almost impossible to mitigate the transmission risk that visitors posed. Because many hospitals did not have the capacity to test all symptomatic patients, they could not reliably limit visits to COVID-19–positive patients. Additionally, without enough PPE for healthcare workers, hospitals could not afford for visitors to use additional PPE.
Now that testing is more readily available and some aspects of the PPE shortages have been addressed, we should not forget that visitation has significant benefits for both patients’ psychological well-being and their overall outcomes.8 Putting aside the emotional support that the physical presence of loved ones can offer, a large body of research indicates that allowing visitors can also meaningfully improve other important patient outcomes. Specifically, the presence of visitors is associated with less fear,9 reduced delirium,10 and even faster recovery.8 In many cases, family members can also help improve hospital safety surveillance and catch medical errors.11
I saw firsthand how these benefits are particularly true for visitors who are also a patient’s primary caretaker. When my mother visited my grandfather, she was not simply a visitor but instead served as an active member of the care team. In addition to providing emotional comfort, my mother oriented him to his surroundings, successfully encouraged oral intake, and even caught some medication errors. Particularly for patients with cognitive impairment, caretakers know the patient better than anyone on the clinical team, and their absence can negatively affect the quality of care.
As a family member who also has familiarity with the healthcare system, I share hospitals’ concerns about wanting to minimize disease transmission. I recognize that, even with PPE and screenings, there is still a chance that visitors unknowingly spread COVID-19 to others in the hospital. On a personal level, however, it feels inhumane to maintain this policy even when it affects particularly vulnerable patients like my grandfather. As some hospitals are already doing,12 we can take steps to allow visitors for such patients while minimizing the likelihood of COVID-19 disease transmission from visitors. Arriving visitors can be screened and required to wear PPE. While these measures may not eliminate the risk of COVID-19 transmission from visitors, they will likely reduce it significantly when implemented properly and make possible a more humane experience for all.13
Fortunately, my grandfather is now recovering comfortably at home, surrounded by his loved ones. To this day, however, he has not forgotten what it was like to be confused and alone in the hospital after his stroke. Even with loved ones around, a stroke is a profoundly distressing experience. To go through such an experience alone is even worse. Because of our petitioning, my grandfather was at least allowed a visitor for part of his stay. Other patients are not even allowed that. As we plan for the pandemic’s next waves, hospitals should reevaluate their visitor policies to ensure that their most vulnerable patients do not have to suffer alone.
Acknowledgment
The author sincerely thanks Dr Allan Goroll (Massachusetts General Hospital/Harvard Medical School) for his mentorship and critical review of this manuscript.
Disclosure
The author has nothing to disclose.
When my grandfather, who speaks limited English, was admitted to a hospital following a stroke amid the coronavirus disease 2019 (COVID-19) pandemic, my family was understandably worried. Sure enough, within just hours of his admission, we were told our normally very calm and beloved Nana was experiencing significant agitation and delirium. He did not understand nurses’ efforts to calm him down, became even more confused, and was eventually sedated and placed in physical restraints. Even though my family’s presence might have prevented some or all of this terrible series of events, the hospital’s visiting policies during the wave of COVID-19 admissions meant that we were forced to wait in the parking lot as they transpired. The hospital’s policy at the time only allowed visitors for pediatrics, end-of-life care, or labor, not for patients with delirium or altered mental status. We were given the option to make a video call, but my grandfather’s stroke had almost completely taken away his vision. Instead of sitting by his side, comforting him, providing explanations in voices he knew and a language he understood, we were left imagining how difficult it must be to suddenly wake up in an unfamiliar environment, with strangers speaking a different language, limited vision, and your arms and legs tied. Intellectually, I understood the hospital’s goals to minimize transmission, but spiritually and emotionally, it felt very cruel and very wrong.
The next day, we successfully petitioned administration to make an exception for one visitor. We argued that our presence would allow for removal of the sedation and restraints. The clinical team agreed that video calls were insufficient in his situation; he was allowed a visitor. We decided that it should be my mother. As soon my grandfather heard her familiar voice, there was a dramatic improvement. He immediately became calmer and restraints were no longer necessary. The team was grateful for a better physical exam and my grandfather was more cooperative with physical therapy. A few days later, unfortunately, the hospital let us know that they had reevaluated their position on my mother’s visits and that she posed an unnecessary COVID-19 risk to medical staff and other patients. And as soon as she left, my grandfather was again agitated and confused for the remaining 3 days of his hospitalization. Although we are grateful that his delirium resolved once he returned home, delirium also has the potential to lead to long-term cognitive impairment.1
The COVID-19 pandemic has required hospitals around the world to make difficult decisions about how to balance minimizing disease transmission with continuing to provide compassionate and high-quality patient care. Of these many dilemmas, developing flexible visitor policies is particularly difficult. Currently, the Centers for Disease Control and Prevention and many state health departments encourage limiting visitation in general but recognize the need for exceptions in special circumstances such as in end-of-life settings or altered mental status.2-4
At the hospital level, there is substantial variation in visitation policies among hospitals. Near our family home in San Jose, California, one hospital currently allows visitation for pediatric patients, pregnant patients, end-of-life patients, surgical patients, and patients in the emergency department, as well as those with mental disabilities or safety needs.5 A mere 10 minutes away, another hospital has implemented a very different policy that allows only one visitor for pregnant patients and in end-of-life settings; there are no exceptions for patients with cognitive or physical disabilities.6 Other hospitals in the United States have gone even further, not permitting visitors even for those at the end of life.7 These patients are forced to spend their last few moments alone.
From an infection control perspective, there are certainly valid reasons to limit visitation. Even with temperature screenings, any movement into and out of a hospital poses a risk of transmitting disease. Infected but asymptomatic persons are known to transmit the disease. Additionally, hospitals still treat non–COVID-19 patients who are most susceptible to severe illness should they develop COVID-19 infection. Early in the COVID-19 pandemic, limitations in testing capacity, personal protective equipment (PPE), and staffing made it challenging to ensure safe visitation. In many cases, it was almost impossible to mitigate the transmission risk that visitors posed. Because many hospitals did not have the capacity to test all symptomatic patients, they could not reliably limit visits to COVID-19–positive patients. Additionally, without enough PPE for healthcare workers, hospitals could not afford for visitors to use additional PPE.
Now that testing is more readily available and some aspects of the PPE shortages have been addressed, we should not forget that visitation has significant benefits for both patients’ psychological well-being and their overall outcomes.8 Putting aside the emotional support that the physical presence of loved ones can offer, a large body of research indicates that allowing visitors can also meaningfully improve other important patient outcomes. Specifically, the presence of visitors is associated with less fear,9 reduced delirium,10 and even faster recovery.8 In many cases, family members can also help improve hospital safety surveillance and catch medical errors.11
I saw firsthand how these benefits are particularly true for visitors who are also a patient’s primary caretaker. When my mother visited my grandfather, she was not simply a visitor but instead served as an active member of the care team. In addition to providing emotional comfort, my mother oriented him to his surroundings, successfully encouraged oral intake, and even caught some medication errors. Particularly for patients with cognitive impairment, caretakers know the patient better than anyone on the clinical team, and their absence can negatively affect the quality of care.
As a family member who also has familiarity with the healthcare system, I share hospitals’ concerns about wanting to minimize disease transmission. I recognize that, even with PPE and screenings, there is still a chance that visitors unknowingly spread COVID-19 to others in the hospital. On a personal level, however, it feels inhumane to maintain this policy even when it affects particularly vulnerable patients like my grandfather. As some hospitals are already doing,12 we can take steps to allow visitors for such patients while minimizing the likelihood of COVID-19 disease transmission from visitors. Arriving visitors can be screened and required to wear PPE. While these measures may not eliminate the risk of COVID-19 transmission from visitors, they will likely reduce it significantly when implemented properly and make possible a more humane experience for all.13
Fortunately, my grandfather is now recovering comfortably at home, surrounded by his loved ones. To this day, however, he has not forgotten what it was like to be confused and alone in the hospital after his stroke. Even with loved ones around, a stroke is a profoundly distressing experience. To go through such an experience alone is even worse. Because of our petitioning, my grandfather was at least allowed a visitor for part of his stay. Other patients are not even allowed that. As we plan for the pandemic’s next waves, hospitals should reevaluate their visitor policies to ensure that their most vulnerable patients do not have to suffer alone.
Acknowledgment
The author sincerely thanks Dr Allan Goroll (Massachusetts General Hospital/Harvard Medical School) for his mentorship and critical review of this manuscript.
Disclosure
The author has nothing to disclose.
1. MacLullich PAMJ, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009;21(1):30-42. https://doi.org/10.1080/09540260802675031
2. Visitor Limitations Guidance. AFL 20-38. State of California—Health and Human Services Agency. California Department of Public Health. Accessed May 29, 2020. https://www.cdph.ca.gov/Programs/CHCQ/LCP/Pages/AFL-20-38.aspx
3. Coronavirus Disease 2019 (COVID-19): Managing Visitors. Centers for Disease Control and Prevention. February 11, 2020. Accessed May 29, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html
4. Maziarz MO. Mandatory Guidelines for Visitors and Facility Staff. https://www.state.nj.us/health/legal/covid19/3-16-2020_MandatoryGuidelinesforVisitors_andFacilityStaff_%20Supersedes3-13-2020Guidelines.pdf
5. Visitor Policy. Good Samaritan Hospital. Accessed May 29, 2020. https://goodsamsanjose.com/covid-19/visitor-policy.dot
6. Visitors Information. El Camino Health. May 7, 2015. Accessed May 29, 2020. https://www.elcaminohealth.org/patients-visitors-guide/before-you-arrive/visitors-information
7. Wakam GK, Montgomery JR, Biesterveld BE, Brown CS. Not dying alone - modern compassionate care in the Covid-19 pandemic. N Engl J Med. 2020;382(24):e88. https://doi.org/10.1056/nejmp2007781
8. Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-1761. https://doi.org/10.1097/ccm.0000000000002624
9. Falk J, Wongsa S, Dang J, Comer L, LoBiondo-Wood G. Using an evidence-based practice process to change child visitation guidelines. Clin J Oncol Nurs. 2012;16(1):21-23. https://doi.org/10.1188/12.cjon.21-23
10. Granberg A, Engberg IB, Lundberg D. Acute confusion and unreal experiences in intensive care patients in relation to the ICU syndrome. part II. Intensive Crit Care Nurs. 1999;15(1):19-33. https://doi.org/10.1016/s0964-3397(99)80062-7
11. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. 2017;171(4):372-381. https://doi.org/10.1001/jamapediatrics.2016.4812
12. Patient and Visitor Guidelines. UW Health: COVID-19 Information. Accessed June 18, 2020. https://coronavirus.uwhealth.org/patient-and-visitor-guidelines/
13. Whyte J. No visitors allowed: We need humane hospital policy during COVID-19. The Hill. April 2, 2020. Accessed June 18, 2020. https://thehill.com/opinion/healthcare/490828-no-visitors-allowed-we-need-humane-hospital-policy-during-covid-19
1. MacLullich PAMJ, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009;21(1):30-42. https://doi.org/10.1080/09540260802675031
2. Visitor Limitations Guidance. AFL 20-38. State of California—Health and Human Services Agency. California Department of Public Health. Accessed May 29, 2020. https://www.cdph.ca.gov/Programs/CHCQ/LCP/Pages/AFL-20-38.aspx
3. Coronavirus Disease 2019 (COVID-19): Managing Visitors. Centers for Disease Control and Prevention. February 11, 2020. Accessed May 29, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html
4. Maziarz MO. Mandatory Guidelines for Visitors and Facility Staff. https://www.state.nj.us/health/legal/covid19/3-16-2020_MandatoryGuidelinesforVisitors_andFacilityStaff_%20Supersedes3-13-2020Guidelines.pdf
5. Visitor Policy. Good Samaritan Hospital. Accessed May 29, 2020. https://goodsamsanjose.com/covid-19/visitor-policy.dot
6. Visitors Information. El Camino Health. May 7, 2015. Accessed May 29, 2020. https://www.elcaminohealth.org/patients-visitors-guide/before-you-arrive/visitors-information
7. Wakam GK, Montgomery JR, Biesterveld BE, Brown CS. Not dying alone - modern compassionate care in the Covid-19 pandemic. N Engl J Med. 2020;382(24):e88. https://doi.org/10.1056/nejmp2007781
8. Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-1761. https://doi.org/10.1097/ccm.0000000000002624
9. Falk J, Wongsa S, Dang J, Comer L, LoBiondo-Wood G. Using an evidence-based practice process to change child visitation guidelines. Clin J Oncol Nurs. 2012;16(1):21-23. https://doi.org/10.1188/12.cjon.21-23
10. Granberg A, Engberg IB, Lundberg D. Acute confusion and unreal experiences in intensive care patients in relation to the ICU syndrome. part II. Intensive Crit Care Nurs. 1999;15(1):19-33. https://doi.org/10.1016/s0964-3397(99)80062-7
11. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. 2017;171(4):372-381. https://doi.org/10.1001/jamapediatrics.2016.4812
12. Patient and Visitor Guidelines. UW Health: COVID-19 Information. Accessed June 18, 2020. https://coronavirus.uwhealth.org/patient-and-visitor-guidelines/
13. Whyte J. No visitors allowed: We need humane hospital policy during COVID-19. The Hill. April 2, 2020. Accessed June 18, 2020. https://thehill.com/opinion/healthcare/490828-no-visitors-allowed-we-need-humane-hospital-policy-during-covid-19
© 2020 Society of Hospital Medicine
The Importance of Emotional Intelligence When Leading in a Time of Crisis
The coronavirus disease of 2019 (COVID-19) pandemic has created innumerable challenges on scales both global and personal while straining health systems and their personnel. Hospitalists and hospital medicine groups are experiencing unique burdens as they confront the pandemic on the frontlines. Hospital medicine groups are being challenged by the rapid operational changes necessary in preparing for and caring for patients with COVID-19. These challenges include drafting new diagnostic and management algorithms, establishing and enacting policies on personal protective equipment (PPE) and patient and provider testing, modifying staffing protocols including deploying staff to new roles or integrating non-hospitalists into hospital medicine roles, and developing capacity for patient surges1—all in the setting of uncertainty about how the pandemic may affect individual hospitals or health systems and how long these repercussions may last. In this perspective, we describe key lessons we have learned in leading our hospital medicine group during the COVID-19 pandemic: how to apply emotional intelligence to proactively address the emotional effects of the crisis.
LEARNING FROM EARLY MISSTEPS
In the early days of the COVID-19 pandemic, the evolving knowledge of the disease process, changing national and local public health guidelines, and instability of the PPE supply chain necessitated rapid change. This pace no longer allowed for our typical time frame of weeks to months for implementation of large-scale operational changes; instead, it demanded adaptation in hours to days. We operated under a strategy of developing new workflows and policies that were logical and reflected the best available information at the time.
For instance, our hospital medicine service cared for some of the earliest-identified COVID-19 patients in the United States in early February 2020. Our initial operational plan for caring for patients with COVID-19 involved grouping these patients on a limited number of direct-care hospitalist teams. The advantages of this approach, which benefitted from low numbers of initial patients, were clear: consolidation of clinical and operational knowledge (including optimal PPE practices) in a few individuals, streamlining communication with infectious diseases specialists and public health departments, and requiring change on only a couple of teams while allowing others to continue their usual workflow. However, we soon learned that providers caring for COVID-19 patients were experiencing an onslaught of negative emotions: fear of contracting the virus themselves or carrying it home to infect loved ones, anxiety of not understanding the clinical disease or having treatments to offer, resentment of having been randomly assigned to the team that would care for these patients, and loneliness of being a sole provider experiencing these emotions. We found ourselves in the position of managing these emotional responses reactively.
APPLYING EMOTIONAL INTELLIGENCE TO LEADING IN A CRISIS
To reduce the distress experienced by our hospitalists and to lead more effectively, we realized the need to proactively address the emotional effects that the pandemic was having. Several authors who have written about valuable leadership lessons during this time have noted the importance of acknowledging the emotional tolls of such a crisis and creating venues for hospitalists to share their experiences.1-4 However, solely adding “wellness” as a checklist item for leaders to address fails to capture the nuances of the complex human emotions that hospitalists may endure at this time and how these emotions influence frontline hospitalists’ responses to operational changes. It is critically important for hospital medicine leaders to employ emotional intelligence, defined as “the ability to monitor one’s own and others’ feelings and emotions, to discriminate among them and to use this information to guide one’s thinking and actions.”5-7 Integrating emotional intelligence allows hospital medicine leaders to anticipate, identify, articulate, and manage the emotional responses to necessary changes and stresses that occur during a crisis such as the COVID-19 pandemic.
As we applied principles of emotional intelligence to our leadership response to the COVID crisis, we found the following seven techniques effective (Appendix Table):
1. ASK. Leaders should ask individual hospitalists “How are you feeling?” instead of “How are you doing?” or “How can I help?” This question may feel too intimate for some, or leaders may worry that the question feels patronizing; however, in our experience, hospitalists respond positively to this prompt, welcome the opportunity to communicate their feelings, and value being heard. Moreover, when hospitalists feel overwhelmed, they may not be able to determine what help they do or do not need. By understanding the emotions of frontline hospitalists, leaders may be better able to address those emotions directly, find solutions to problems, and anticipate reactions to future policies.4
2. SHARE. Leaders should model what they ask of frontline hospitalists and share their own feelings, even if they are experiencing mixed or negative emotions. For instance, a leader who is feeling saddened about the death of a patient can begin a meeting by sharing this sentiment. By allowing themselves to display vulnerability, leaders demonstrate courage and promote a culture of openness, honesty, and mutual trust.
3. INITIATE. Leaders should embrace difficult conversations and be transparent about uncertainty, although they may not have the answers and may need to take local responsibility for consequences of decisions made externally, such as those made by the health system or government. Confronting difficult discussions and being transparent about “unknowns” provides acknowledgement, reassurance, and shared experience that expresses to the hospitalist group that, while the future may be unsettled, they will face it together.
4. ANTICIPATE. Leaders should anticipate the emotional responses to operational changes while designing them and rolling them out. While negative emotions may heavily outweigh positive emotions in times of crisis, we have also found that harnessing positive emotions when designing operational initiatives can assist with successful implementation. For example, by surveying our hospitalists, we found that many felt enthusiastic about caring for patients with COVID-19, curious about new skill sets, and passionate about helping in a time of crisis. By generating a list of these hospitalists up front, we were able to preferentially staff COVID-19 teams with providers who were eager to care for those patients and, thereby, minimize anxiety among those who were more apprehensive.
5. ENCOURAGE. Leaders should provide time and space (including virtually) for hospitalists to discuss their emotions.8 We found that creating multiple layers of opportunity for expression allows for engagement with a wider range of hospitalists, some of whom may be reluctant to share feelings openly or to a group, whereas others may enjoy the opportunity to reveal their feelings publicly. These varied venues for emotional expression may range from brief individual check-ins to open “office hours” to dedicated meetings such as “Hospitalist Town Halls.” For instance, spending the first few minutes of a meeting with a smaller group by encouraging each participant to share something personal can build community and mutual understanding, as well as cue leaders in to where participants may be on the emotional landscape.
6. NURTURE. Beyond inviting the expression of emotions, leaders should ensure that hospitalists have access to more formal systems of support, especially for hospitalists who may be experiencing more intense negative emotions. Support may be provided through unit- or team-based debriefing sessions, health-system sponsored support programs, or individual counseling sessions.4,8
7. APPRECIATE. Leaders should deliberately foster gratitude by sincerely and frequently expressing their appreciation. Because expressing gratitude builds resiliency,9 cultivating a culture of gratitude may bolster resilience in the entire hospital medicine group. Opportunities for thankfulness abound as hospitalists volunteer for extra shifts, cover for ill colleagues, participate in new working groups and task forces, and sacrifice their personal safety on the front lines. We often incorporate statements of appreciation into one-on-one conversations with hospitalists, during operational and divisional meetings, and in email. We also built gratitude expressions into the daily work on the Respiratory Isolation Unit at our hospital via daily interdisciplinary huddles for frontline providers to share their experiences and emotions. During huddles, providers are asked to pair negative emotions with suggestions for improvement and to share a moment of gratitude. This helps to engender a spirit of camaraderie, shared mission, and collective optimism.
CONCLUSION
Hospitalists are experiencing a wide range of emotions related to the COVID-19 pandemic. Hospital medicine leaders must have strategies to understand the emotions providers are experiencing. Being aware of and acknowledging these emotions up front can help leaders plan and implement the operational changes necessary to manage the crisis. Because our health system and city have fortunately been spared the worst of the pandemic so far without large volumes of patients with COVID-19, we recognize that the strategies above may be challenging for leaders in overwhelmed health systems. However, we hope that leaders at all levels can apply the lessons we have learned: to ask hospitalists how they are feeling, share their own feelings, initiate difficult conversations when needed, anticipate the emotional effects of operational changes, encourage expressions of emotion in multiple venues, nurture hospitalists who need more formal support, and appreciate frontline hospitalists. While the emotional needs of hospitalists will undoubtedly change over time as the pandemic evolves, we suspect that these strategies will continue to be important over the coming weeks, months, and longer as we settle into the postpandemic world.
1. Chopra V, Toner E, Waldhorn R, Washer L. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med. 2020;172(9):621-622. https://doi.org/10.7326/m20-0907
2. Garg M, Wray CM. Hospital medicine management in the time of COVID-19: preparing for a sprint and a marathon. J Hosp Med. 2020;15(5):305-307. https://doi.org/10.12788/jhm.3427
3. Hertling M. Ten tips for a crisis : lessons from a soldier. J Hosp Med. 2020;15(5):275-276. https://doi.org/10.12788/jhm.3424
4. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. Published online April 7, 2020. https://doi.org/10.1001/jama.2020.5893
5. Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014;6(1):21-31. https://doi.org/10.4300/jgme-d-13-00012.1
6. Goleman D, Boyatzis R. Emotional intelligence has 12 elements. Which do you need to work on? Harvard Business Review. February 6, 2017. Accessed April 16, 2020. https://hbr.org/2017/02/emotional-intelligence-has-12-elements-which-do-you-need-to-work-on
7. Salovey P, Mayer JD. Emotional intelligence. Imagin Cogn Pers. 1990;9(3):185-211. https://doi.org/10.2190/DUGG-P24E-52WK-6CDG
8. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. https://doi.org/10.1136/bmj.m1642
9. Kopans D. How to evaluate, manage, and strengthen your resilience. Harvard Business Review. June 14, 2016. Accessed April 21, 2020. https://hbr.org/2016/06/how-to-evaluate-manage-and-strengthen-your-resilience
The coronavirus disease of 2019 (COVID-19) pandemic has created innumerable challenges on scales both global and personal while straining health systems and their personnel. Hospitalists and hospital medicine groups are experiencing unique burdens as they confront the pandemic on the frontlines. Hospital medicine groups are being challenged by the rapid operational changes necessary in preparing for and caring for patients with COVID-19. These challenges include drafting new diagnostic and management algorithms, establishing and enacting policies on personal protective equipment (PPE) and patient and provider testing, modifying staffing protocols including deploying staff to new roles or integrating non-hospitalists into hospital medicine roles, and developing capacity for patient surges1—all in the setting of uncertainty about how the pandemic may affect individual hospitals or health systems and how long these repercussions may last. In this perspective, we describe key lessons we have learned in leading our hospital medicine group during the COVID-19 pandemic: how to apply emotional intelligence to proactively address the emotional effects of the crisis.
LEARNING FROM EARLY MISSTEPS
In the early days of the COVID-19 pandemic, the evolving knowledge of the disease process, changing national and local public health guidelines, and instability of the PPE supply chain necessitated rapid change. This pace no longer allowed for our typical time frame of weeks to months for implementation of large-scale operational changes; instead, it demanded adaptation in hours to days. We operated under a strategy of developing new workflows and policies that were logical and reflected the best available information at the time.
For instance, our hospital medicine service cared for some of the earliest-identified COVID-19 patients in the United States in early February 2020. Our initial operational plan for caring for patients with COVID-19 involved grouping these patients on a limited number of direct-care hospitalist teams. The advantages of this approach, which benefitted from low numbers of initial patients, were clear: consolidation of clinical and operational knowledge (including optimal PPE practices) in a few individuals, streamlining communication with infectious diseases specialists and public health departments, and requiring change on only a couple of teams while allowing others to continue their usual workflow. However, we soon learned that providers caring for COVID-19 patients were experiencing an onslaught of negative emotions: fear of contracting the virus themselves or carrying it home to infect loved ones, anxiety of not understanding the clinical disease or having treatments to offer, resentment of having been randomly assigned to the team that would care for these patients, and loneliness of being a sole provider experiencing these emotions. We found ourselves in the position of managing these emotional responses reactively.
APPLYING EMOTIONAL INTELLIGENCE TO LEADING IN A CRISIS
To reduce the distress experienced by our hospitalists and to lead more effectively, we realized the need to proactively address the emotional effects that the pandemic was having. Several authors who have written about valuable leadership lessons during this time have noted the importance of acknowledging the emotional tolls of such a crisis and creating venues for hospitalists to share their experiences.1-4 However, solely adding “wellness” as a checklist item for leaders to address fails to capture the nuances of the complex human emotions that hospitalists may endure at this time and how these emotions influence frontline hospitalists’ responses to operational changes. It is critically important for hospital medicine leaders to employ emotional intelligence, defined as “the ability to monitor one’s own and others’ feelings and emotions, to discriminate among them and to use this information to guide one’s thinking and actions.”5-7 Integrating emotional intelligence allows hospital medicine leaders to anticipate, identify, articulate, and manage the emotional responses to necessary changes and stresses that occur during a crisis such as the COVID-19 pandemic.
As we applied principles of emotional intelligence to our leadership response to the COVID crisis, we found the following seven techniques effective (Appendix Table):
1. ASK. Leaders should ask individual hospitalists “How are you feeling?” instead of “How are you doing?” or “How can I help?” This question may feel too intimate for some, or leaders may worry that the question feels patronizing; however, in our experience, hospitalists respond positively to this prompt, welcome the opportunity to communicate their feelings, and value being heard. Moreover, when hospitalists feel overwhelmed, they may not be able to determine what help they do or do not need. By understanding the emotions of frontline hospitalists, leaders may be better able to address those emotions directly, find solutions to problems, and anticipate reactions to future policies.4
2. SHARE. Leaders should model what they ask of frontline hospitalists and share their own feelings, even if they are experiencing mixed or negative emotions. For instance, a leader who is feeling saddened about the death of a patient can begin a meeting by sharing this sentiment. By allowing themselves to display vulnerability, leaders demonstrate courage and promote a culture of openness, honesty, and mutual trust.
3. INITIATE. Leaders should embrace difficult conversations and be transparent about uncertainty, although they may not have the answers and may need to take local responsibility for consequences of decisions made externally, such as those made by the health system or government. Confronting difficult discussions and being transparent about “unknowns” provides acknowledgement, reassurance, and shared experience that expresses to the hospitalist group that, while the future may be unsettled, they will face it together.
4. ANTICIPATE. Leaders should anticipate the emotional responses to operational changes while designing them and rolling them out. While negative emotions may heavily outweigh positive emotions in times of crisis, we have also found that harnessing positive emotions when designing operational initiatives can assist with successful implementation. For example, by surveying our hospitalists, we found that many felt enthusiastic about caring for patients with COVID-19, curious about new skill sets, and passionate about helping in a time of crisis. By generating a list of these hospitalists up front, we were able to preferentially staff COVID-19 teams with providers who were eager to care for those patients and, thereby, minimize anxiety among those who were more apprehensive.
5. ENCOURAGE. Leaders should provide time and space (including virtually) for hospitalists to discuss their emotions.8 We found that creating multiple layers of opportunity for expression allows for engagement with a wider range of hospitalists, some of whom may be reluctant to share feelings openly or to a group, whereas others may enjoy the opportunity to reveal their feelings publicly. These varied venues for emotional expression may range from brief individual check-ins to open “office hours” to dedicated meetings such as “Hospitalist Town Halls.” For instance, spending the first few minutes of a meeting with a smaller group by encouraging each participant to share something personal can build community and mutual understanding, as well as cue leaders in to where participants may be on the emotional landscape.
6. NURTURE. Beyond inviting the expression of emotions, leaders should ensure that hospitalists have access to more formal systems of support, especially for hospitalists who may be experiencing more intense negative emotions. Support may be provided through unit- or team-based debriefing sessions, health-system sponsored support programs, or individual counseling sessions.4,8
7. APPRECIATE. Leaders should deliberately foster gratitude by sincerely and frequently expressing their appreciation. Because expressing gratitude builds resiliency,9 cultivating a culture of gratitude may bolster resilience in the entire hospital medicine group. Opportunities for thankfulness abound as hospitalists volunteer for extra shifts, cover for ill colleagues, participate in new working groups and task forces, and sacrifice their personal safety on the front lines. We often incorporate statements of appreciation into one-on-one conversations with hospitalists, during operational and divisional meetings, and in email. We also built gratitude expressions into the daily work on the Respiratory Isolation Unit at our hospital via daily interdisciplinary huddles for frontline providers to share their experiences and emotions. During huddles, providers are asked to pair negative emotions with suggestions for improvement and to share a moment of gratitude. This helps to engender a spirit of camaraderie, shared mission, and collective optimism.
CONCLUSION
Hospitalists are experiencing a wide range of emotions related to the COVID-19 pandemic. Hospital medicine leaders must have strategies to understand the emotions providers are experiencing. Being aware of and acknowledging these emotions up front can help leaders plan and implement the operational changes necessary to manage the crisis. Because our health system and city have fortunately been spared the worst of the pandemic so far without large volumes of patients with COVID-19, we recognize that the strategies above may be challenging for leaders in overwhelmed health systems. However, we hope that leaders at all levels can apply the lessons we have learned: to ask hospitalists how they are feeling, share their own feelings, initiate difficult conversations when needed, anticipate the emotional effects of operational changes, encourage expressions of emotion in multiple venues, nurture hospitalists who need more formal support, and appreciate frontline hospitalists. While the emotional needs of hospitalists will undoubtedly change over time as the pandemic evolves, we suspect that these strategies will continue to be important over the coming weeks, months, and longer as we settle into the postpandemic world.
The coronavirus disease of 2019 (COVID-19) pandemic has created innumerable challenges on scales both global and personal while straining health systems and their personnel. Hospitalists and hospital medicine groups are experiencing unique burdens as they confront the pandemic on the frontlines. Hospital medicine groups are being challenged by the rapid operational changes necessary in preparing for and caring for patients with COVID-19. These challenges include drafting new diagnostic and management algorithms, establishing and enacting policies on personal protective equipment (PPE) and patient and provider testing, modifying staffing protocols including deploying staff to new roles or integrating non-hospitalists into hospital medicine roles, and developing capacity for patient surges1—all in the setting of uncertainty about how the pandemic may affect individual hospitals or health systems and how long these repercussions may last. In this perspective, we describe key lessons we have learned in leading our hospital medicine group during the COVID-19 pandemic: how to apply emotional intelligence to proactively address the emotional effects of the crisis.
LEARNING FROM EARLY MISSTEPS
In the early days of the COVID-19 pandemic, the evolving knowledge of the disease process, changing national and local public health guidelines, and instability of the PPE supply chain necessitated rapid change. This pace no longer allowed for our typical time frame of weeks to months for implementation of large-scale operational changes; instead, it demanded adaptation in hours to days. We operated under a strategy of developing new workflows and policies that were logical and reflected the best available information at the time.
For instance, our hospital medicine service cared for some of the earliest-identified COVID-19 patients in the United States in early February 2020. Our initial operational plan for caring for patients with COVID-19 involved grouping these patients on a limited number of direct-care hospitalist teams. The advantages of this approach, which benefitted from low numbers of initial patients, were clear: consolidation of clinical and operational knowledge (including optimal PPE practices) in a few individuals, streamlining communication with infectious diseases specialists and public health departments, and requiring change on only a couple of teams while allowing others to continue their usual workflow. However, we soon learned that providers caring for COVID-19 patients were experiencing an onslaught of negative emotions: fear of contracting the virus themselves or carrying it home to infect loved ones, anxiety of not understanding the clinical disease or having treatments to offer, resentment of having been randomly assigned to the team that would care for these patients, and loneliness of being a sole provider experiencing these emotions. We found ourselves in the position of managing these emotional responses reactively.
APPLYING EMOTIONAL INTELLIGENCE TO LEADING IN A CRISIS
To reduce the distress experienced by our hospitalists and to lead more effectively, we realized the need to proactively address the emotional effects that the pandemic was having. Several authors who have written about valuable leadership lessons during this time have noted the importance of acknowledging the emotional tolls of such a crisis and creating venues for hospitalists to share their experiences.1-4 However, solely adding “wellness” as a checklist item for leaders to address fails to capture the nuances of the complex human emotions that hospitalists may endure at this time and how these emotions influence frontline hospitalists’ responses to operational changes. It is critically important for hospital medicine leaders to employ emotional intelligence, defined as “the ability to monitor one’s own and others’ feelings and emotions, to discriminate among them and to use this information to guide one’s thinking and actions.”5-7 Integrating emotional intelligence allows hospital medicine leaders to anticipate, identify, articulate, and manage the emotional responses to necessary changes and stresses that occur during a crisis such as the COVID-19 pandemic.
As we applied principles of emotional intelligence to our leadership response to the COVID crisis, we found the following seven techniques effective (Appendix Table):
1. ASK. Leaders should ask individual hospitalists “How are you feeling?” instead of “How are you doing?” or “How can I help?” This question may feel too intimate for some, or leaders may worry that the question feels patronizing; however, in our experience, hospitalists respond positively to this prompt, welcome the opportunity to communicate their feelings, and value being heard. Moreover, when hospitalists feel overwhelmed, they may not be able to determine what help they do or do not need. By understanding the emotions of frontline hospitalists, leaders may be better able to address those emotions directly, find solutions to problems, and anticipate reactions to future policies.4
2. SHARE. Leaders should model what they ask of frontline hospitalists and share their own feelings, even if they are experiencing mixed or negative emotions. For instance, a leader who is feeling saddened about the death of a patient can begin a meeting by sharing this sentiment. By allowing themselves to display vulnerability, leaders demonstrate courage and promote a culture of openness, honesty, and mutual trust.
3. INITIATE. Leaders should embrace difficult conversations and be transparent about uncertainty, although they may not have the answers and may need to take local responsibility for consequences of decisions made externally, such as those made by the health system or government. Confronting difficult discussions and being transparent about “unknowns” provides acknowledgement, reassurance, and shared experience that expresses to the hospitalist group that, while the future may be unsettled, they will face it together.
4. ANTICIPATE. Leaders should anticipate the emotional responses to operational changes while designing them and rolling them out. While negative emotions may heavily outweigh positive emotions in times of crisis, we have also found that harnessing positive emotions when designing operational initiatives can assist with successful implementation. For example, by surveying our hospitalists, we found that many felt enthusiastic about caring for patients with COVID-19, curious about new skill sets, and passionate about helping in a time of crisis. By generating a list of these hospitalists up front, we were able to preferentially staff COVID-19 teams with providers who were eager to care for those patients and, thereby, minimize anxiety among those who were more apprehensive.
5. ENCOURAGE. Leaders should provide time and space (including virtually) for hospitalists to discuss their emotions.8 We found that creating multiple layers of opportunity for expression allows for engagement with a wider range of hospitalists, some of whom may be reluctant to share feelings openly or to a group, whereas others may enjoy the opportunity to reveal their feelings publicly. These varied venues for emotional expression may range from brief individual check-ins to open “office hours” to dedicated meetings such as “Hospitalist Town Halls.” For instance, spending the first few minutes of a meeting with a smaller group by encouraging each participant to share something personal can build community and mutual understanding, as well as cue leaders in to where participants may be on the emotional landscape.
6. NURTURE. Beyond inviting the expression of emotions, leaders should ensure that hospitalists have access to more formal systems of support, especially for hospitalists who may be experiencing more intense negative emotions. Support may be provided through unit- or team-based debriefing sessions, health-system sponsored support programs, or individual counseling sessions.4,8
7. APPRECIATE. Leaders should deliberately foster gratitude by sincerely and frequently expressing their appreciation. Because expressing gratitude builds resiliency,9 cultivating a culture of gratitude may bolster resilience in the entire hospital medicine group. Opportunities for thankfulness abound as hospitalists volunteer for extra shifts, cover for ill colleagues, participate in new working groups and task forces, and sacrifice their personal safety on the front lines. We often incorporate statements of appreciation into one-on-one conversations with hospitalists, during operational and divisional meetings, and in email. We also built gratitude expressions into the daily work on the Respiratory Isolation Unit at our hospital via daily interdisciplinary huddles for frontline providers to share their experiences and emotions. During huddles, providers are asked to pair negative emotions with suggestions for improvement and to share a moment of gratitude. This helps to engender a spirit of camaraderie, shared mission, and collective optimism.
CONCLUSION
Hospitalists are experiencing a wide range of emotions related to the COVID-19 pandemic. Hospital medicine leaders must have strategies to understand the emotions providers are experiencing. Being aware of and acknowledging these emotions up front can help leaders plan and implement the operational changes necessary to manage the crisis. Because our health system and city have fortunately been spared the worst of the pandemic so far without large volumes of patients with COVID-19, we recognize that the strategies above may be challenging for leaders in overwhelmed health systems. However, we hope that leaders at all levels can apply the lessons we have learned: to ask hospitalists how they are feeling, share their own feelings, initiate difficult conversations when needed, anticipate the emotional effects of operational changes, encourage expressions of emotion in multiple venues, nurture hospitalists who need more formal support, and appreciate frontline hospitalists. While the emotional needs of hospitalists will undoubtedly change over time as the pandemic evolves, we suspect that these strategies will continue to be important over the coming weeks, months, and longer as we settle into the postpandemic world.
1. Chopra V, Toner E, Waldhorn R, Washer L. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med. 2020;172(9):621-622. https://doi.org/10.7326/m20-0907
2. Garg M, Wray CM. Hospital medicine management in the time of COVID-19: preparing for a sprint and a marathon. J Hosp Med. 2020;15(5):305-307. https://doi.org/10.12788/jhm.3427
3. Hertling M. Ten tips for a crisis : lessons from a soldier. J Hosp Med. 2020;15(5):275-276. https://doi.org/10.12788/jhm.3424
4. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. Published online April 7, 2020. https://doi.org/10.1001/jama.2020.5893
5. Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014;6(1):21-31. https://doi.org/10.4300/jgme-d-13-00012.1
6. Goleman D, Boyatzis R. Emotional intelligence has 12 elements. Which do you need to work on? Harvard Business Review. February 6, 2017. Accessed April 16, 2020. https://hbr.org/2017/02/emotional-intelligence-has-12-elements-which-do-you-need-to-work-on
7. Salovey P, Mayer JD. Emotional intelligence. Imagin Cogn Pers. 1990;9(3):185-211. https://doi.org/10.2190/DUGG-P24E-52WK-6CDG
8. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. https://doi.org/10.1136/bmj.m1642
9. Kopans D. How to evaluate, manage, and strengthen your resilience. Harvard Business Review. June 14, 2016. Accessed April 21, 2020. https://hbr.org/2016/06/how-to-evaluate-manage-and-strengthen-your-resilience
1. Chopra V, Toner E, Waldhorn R, Washer L. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med. 2020;172(9):621-622. https://doi.org/10.7326/m20-0907
2. Garg M, Wray CM. Hospital medicine management in the time of COVID-19: preparing for a sprint and a marathon. J Hosp Med. 2020;15(5):305-307. https://doi.org/10.12788/jhm.3427
3. Hertling M. Ten tips for a crisis : lessons from a soldier. J Hosp Med. 2020;15(5):275-276. https://doi.org/10.12788/jhm.3424
4. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. Published online April 7, 2020. https://doi.org/10.1001/jama.2020.5893
5. Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014;6(1):21-31. https://doi.org/10.4300/jgme-d-13-00012.1
6. Goleman D, Boyatzis R. Emotional intelligence has 12 elements. Which do you need to work on? Harvard Business Review. February 6, 2017. Accessed April 16, 2020. https://hbr.org/2017/02/emotional-intelligence-has-12-elements-which-do-you-need-to-work-on
7. Salovey P, Mayer JD. Emotional intelligence. Imagin Cogn Pers. 1990;9(3):185-211. https://doi.org/10.2190/DUGG-P24E-52WK-6CDG
8. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. https://doi.org/10.1136/bmj.m1642
9. Kopans D. How to evaluate, manage, and strengthen your resilience. Harvard Business Review. June 14, 2016. Accessed April 21, 2020. https://hbr.org/2016/06/how-to-evaluate-manage-and-strengthen-your-resilience
© 2020 Society of Hospital Medicine