User login
New road map for CRC screening: Use more stool tests, says AGA
where the default screening modality to date has been colonoscopy.
Instead, the American Gastroenterological Association is proposing new approaches that combine better risk assessment, more use of noninvasive testing (such as fecal occult blood tests), and more targeted referrals for colonoscopy. Such changes could increase patient compliance and “save countless lives.”
“We need to improve our strategies to curb the cancer that ranks second for deaths in the U.S.,” commented Srinadh Komanduri, MD, chair of the AGA Center for GI Innovation and Technology, in a statement.
“Approximately 67% of eligible Americans are screened for colorectal cancer,” he said, which means that a third (33%) are not.
During the COVID-19 pandemic, the proportion of individuals not being screened has increased. One report of medical claims data showed that colonoscopies dropped by 90% during April.
The proposed changes are outlined in an AGA white paper: “Roadmap for the Future of Colorectal Cancer Screening in the United States.”
The report, written following consultation with 60 gastroenterology and research experts, was published online in Clinical Gastroenterology and Hepatology.
It proposed that alternative testing modalities to colonoscopy will need to be integrated into organized screening programs.
Rather than offering colonoscopy as the default screening method for all patients at risk, the AGA advised that it be offered initially only to patients at high risk, which would increase access for those who need it most. For patients at lower risk, noninvasive screening methods, such as fecal occult blood testing, could be offered initially and then integrated with colonoscopy.
“If we offered tests that were convenient, accurate, and of lower cost, and we could help people choose the best option based on their individual cancer risks, we would save more lives,” Joshua E. Melson, MD, MPH, lead author of the AGA white paper and professor at Rush University Medical Center, Chicago, said in an interview.
Screening can reduce CRC mortality by more than 50%, he added.
“Screening should be thought of as a process over time, not a single test isolated in time,” Dr. Melson commented. A clinical practice that has historically used only colonoscopy will need an organized, structured program to incorporate noninvasive testing, he said.
To date, efforts to increase CRC screening uptake have met with limited success, the AGA says. In 2014, the National Colorectal Cancer Round Table set the bar high with a 2018 screening goal of 80% for adults 50 years of age and older. As of 2020, some states had almost reached this goal, but most had not.
“In the opportunistic screening environment in the U.S., where colonoscopy is the most prevalent method, CRC screening has not reached aspirational goals in terms of uptake, reduction in CRC incidence, and disease burden,” the AGA said. “It is questionable if 80% uptake is achievable in a primarily opportunistic screening environment.”
In the proposed revamping of the current CRC screening infrastructure, patients whose physicians recommend CRC screening would no longer be left to their own devices to follow up. Clinicians would initiate CRC screening and oversee follow-up testing at defined intervals and would employ ongoing surveillance.
Ensuring that appropriate screening is readily available to at-risk individuals with no social, racial, or economic disparities is crucial, the AGA says. Racial disparities in access to screening disproportionately burden Blacks and Latin Americans as well as people living in rural areas. Screening differences account for 42% of the disparity in CRC incidence between Black and White Americans and 19% of the disparity in CRC mortality.
Compared with colonoscopy, which requires bowel preparation, time off from work, and a hospital or clinic procedure, the fecal immunochemical test (FIT), for which a patient provides stool samples that are examined for the presence of blood, is much less stressful: it is noninvasive, and the patients collect the samples themselves in their own home. Studies show that, in diverse environments, patients prefer FIT over colonoscopy.
In a controlled trial that involved more than 55,000 patients who were randomly assigned to undergo either FIT or colonoscopy, the participation rate in the first cycle was greater for FIT than for colonoscopy (34.2% vs. 24.6%). This partially offset the lower single-application sensitivity for CRC of FIT, the researchers said.
Results from a study with a cluster randomized design showed that offering up-front stool testing as an option in addition to colonoscopy increased screening uptake. Of patients offered fecal occult blood testing or colonoscopy, 69% completed the noninvasive screening, compared with 38% of those offered colonoscopy alone. Notably, non-White participants were more adherent to stool testing.
The success of the AGA’s new initiative hinges largely upon the development of affordable, highly accurate, easy-to-use, noninvasive tests. In this regard, the organization has challenged scientists and industry partners with an aspirational target that is “far superior to current methodologies in terms of sensitivity and specificity,” said Dr. Melson, who is associate professor at Rush Medical College, Chicago, and a member of the AGA Center for GI Innovation and Technology.
The AGA wants new CRC screening tests that are capable of detecting advanced adenomas and advanced serrated lesions with a one-time sensitivity and specificity of 90% or higher, which is comparable with colonoscopy.
The FIT test has a sensitivity of less than 50% for detecting an advanced polyp of 10 mm or larger, said Dr. Melson.
The multitarget stool DNA (MT-sDNA) test may offer some improvement.
In a 2014 pivotal trial that compared FIT with the MT-sDNA in patients at average risk, the MT-sDNA test had higher sensitivity for detecting nonadvanced CRC lesions than FIT (92% vs. 74%) but less specificity (87% vs. 95%). The rate of detection of polyps with high-grade dysplasia was 69.2% with DNA testing and 46.2% with FIT.
However, the MT-sDNA test costs more than $500, compared with $25 for the FIT test, Dr. Melson pointed out.
To help identify the most appropriate screening for individual patients, better understanding and more thorough identification of risk factors are needed. “Risk assessment is definitely not where it could be,” Dr. Melson said.
The accuracy of risk assessment can be improved by sharing information from electronic health records on past colonoscopy polyp data, the presence of molecular markers, and family history, the AGA said. “With clearer risk assessment, shared decision-making on the most appropriate test becomes more clear and screening rates would benefit from patient buy-in and from easier access.”
The AGA recommended that research focus on the cost-effectiveness of screening younger patients, because the proportion of CRC cases in adults aged younger than 50 years has doubled since 1990.
This has raised the question as to whether the age for initial CRC screening should be lowered to 45 years (it already has been by the American Cancer Society), but there is much debate over this move.
Dr. Melson has received consulting fees from Clinical Genomics and research support from Boston Scientific Corporation and holds stocks in Virgo Imaging. A number of AGA white paper coauthors have disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
where the default screening modality to date has been colonoscopy.
Instead, the American Gastroenterological Association is proposing new approaches that combine better risk assessment, more use of noninvasive testing (such as fecal occult blood tests), and more targeted referrals for colonoscopy. Such changes could increase patient compliance and “save countless lives.”
“We need to improve our strategies to curb the cancer that ranks second for deaths in the U.S.,” commented Srinadh Komanduri, MD, chair of the AGA Center for GI Innovation and Technology, in a statement.
“Approximately 67% of eligible Americans are screened for colorectal cancer,” he said, which means that a third (33%) are not.
During the COVID-19 pandemic, the proportion of individuals not being screened has increased. One report of medical claims data showed that colonoscopies dropped by 90% during April.
The proposed changes are outlined in an AGA white paper: “Roadmap for the Future of Colorectal Cancer Screening in the United States.”
The report, written following consultation with 60 gastroenterology and research experts, was published online in Clinical Gastroenterology and Hepatology.
It proposed that alternative testing modalities to colonoscopy will need to be integrated into organized screening programs.
Rather than offering colonoscopy as the default screening method for all patients at risk, the AGA advised that it be offered initially only to patients at high risk, which would increase access for those who need it most. For patients at lower risk, noninvasive screening methods, such as fecal occult blood testing, could be offered initially and then integrated with colonoscopy.
“If we offered tests that were convenient, accurate, and of lower cost, and we could help people choose the best option based on their individual cancer risks, we would save more lives,” Joshua E. Melson, MD, MPH, lead author of the AGA white paper and professor at Rush University Medical Center, Chicago, said in an interview.
Screening can reduce CRC mortality by more than 50%, he added.
“Screening should be thought of as a process over time, not a single test isolated in time,” Dr. Melson commented. A clinical practice that has historically used only colonoscopy will need an organized, structured program to incorporate noninvasive testing, he said.
To date, efforts to increase CRC screening uptake have met with limited success, the AGA says. In 2014, the National Colorectal Cancer Round Table set the bar high with a 2018 screening goal of 80% for adults 50 years of age and older. As of 2020, some states had almost reached this goal, but most had not.
“In the opportunistic screening environment in the U.S., where colonoscopy is the most prevalent method, CRC screening has not reached aspirational goals in terms of uptake, reduction in CRC incidence, and disease burden,” the AGA said. “It is questionable if 80% uptake is achievable in a primarily opportunistic screening environment.”
In the proposed revamping of the current CRC screening infrastructure, patients whose physicians recommend CRC screening would no longer be left to their own devices to follow up. Clinicians would initiate CRC screening and oversee follow-up testing at defined intervals and would employ ongoing surveillance.
Ensuring that appropriate screening is readily available to at-risk individuals with no social, racial, or economic disparities is crucial, the AGA says. Racial disparities in access to screening disproportionately burden Blacks and Latin Americans as well as people living in rural areas. Screening differences account for 42% of the disparity in CRC incidence between Black and White Americans and 19% of the disparity in CRC mortality.
Compared with colonoscopy, which requires bowel preparation, time off from work, and a hospital or clinic procedure, the fecal immunochemical test (FIT), for which a patient provides stool samples that are examined for the presence of blood, is much less stressful: it is noninvasive, and the patients collect the samples themselves in their own home. Studies show that, in diverse environments, patients prefer FIT over colonoscopy.
In a controlled trial that involved more than 55,000 patients who were randomly assigned to undergo either FIT or colonoscopy, the participation rate in the first cycle was greater for FIT than for colonoscopy (34.2% vs. 24.6%). This partially offset the lower single-application sensitivity for CRC of FIT, the researchers said.
Results from a study with a cluster randomized design showed that offering up-front stool testing as an option in addition to colonoscopy increased screening uptake. Of patients offered fecal occult blood testing or colonoscopy, 69% completed the noninvasive screening, compared with 38% of those offered colonoscopy alone. Notably, non-White participants were more adherent to stool testing.
The success of the AGA’s new initiative hinges largely upon the development of affordable, highly accurate, easy-to-use, noninvasive tests. In this regard, the organization has challenged scientists and industry partners with an aspirational target that is “far superior to current methodologies in terms of sensitivity and specificity,” said Dr. Melson, who is associate professor at Rush Medical College, Chicago, and a member of the AGA Center for GI Innovation and Technology.
The AGA wants new CRC screening tests that are capable of detecting advanced adenomas and advanced serrated lesions with a one-time sensitivity and specificity of 90% or higher, which is comparable with colonoscopy.
The FIT test has a sensitivity of less than 50% for detecting an advanced polyp of 10 mm or larger, said Dr. Melson.
The multitarget stool DNA (MT-sDNA) test may offer some improvement.
In a 2014 pivotal trial that compared FIT with the MT-sDNA in patients at average risk, the MT-sDNA test had higher sensitivity for detecting nonadvanced CRC lesions than FIT (92% vs. 74%) but less specificity (87% vs. 95%). The rate of detection of polyps with high-grade dysplasia was 69.2% with DNA testing and 46.2% with FIT.
However, the MT-sDNA test costs more than $500, compared with $25 for the FIT test, Dr. Melson pointed out.
To help identify the most appropriate screening for individual patients, better understanding and more thorough identification of risk factors are needed. “Risk assessment is definitely not where it could be,” Dr. Melson said.
The accuracy of risk assessment can be improved by sharing information from electronic health records on past colonoscopy polyp data, the presence of molecular markers, and family history, the AGA said. “With clearer risk assessment, shared decision-making on the most appropriate test becomes more clear and screening rates would benefit from patient buy-in and from easier access.”
The AGA recommended that research focus on the cost-effectiveness of screening younger patients, because the proportion of CRC cases in adults aged younger than 50 years has doubled since 1990.
This has raised the question as to whether the age for initial CRC screening should be lowered to 45 years (it already has been by the American Cancer Society), but there is much debate over this move.
Dr. Melson has received consulting fees from Clinical Genomics and research support from Boston Scientific Corporation and holds stocks in Virgo Imaging. A number of AGA white paper coauthors have disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
where the default screening modality to date has been colonoscopy.
Instead, the American Gastroenterological Association is proposing new approaches that combine better risk assessment, more use of noninvasive testing (such as fecal occult blood tests), and more targeted referrals for colonoscopy. Such changes could increase patient compliance and “save countless lives.”
“We need to improve our strategies to curb the cancer that ranks second for deaths in the U.S.,” commented Srinadh Komanduri, MD, chair of the AGA Center for GI Innovation and Technology, in a statement.
“Approximately 67% of eligible Americans are screened for colorectal cancer,” he said, which means that a third (33%) are not.
During the COVID-19 pandemic, the proportion of individuals not being screened has increased. One report of medical claims data showed that colonoscopies dropped by 90% during April.
The proposed changes are outlined in an AGA white paper: “Roadmap for the Future of Colorectal Cancer Screening in the United States.”
The report, written following consultation with 60 gastroenterology and research experts, was published online in Clinical Gastroenterology and Hepatology.
It proposed that alternative testing modalities to colonoscopy will need to be integrated into organized screening programs.
Rather than offering colonoscopy as the default screening method for all patients at risk, the AGA advised that it be offered initially only to patients at high risk, which would increase access for those who need it most. For patients at lower risk, noninvasive screening methods, such as fecal occult blood testing, could be offered initially and then integrated with colonoscopy.
“If we offered tests that were convenient, accurate, and of lower cost, and we could help people choose the best option based on their individual cancer risks, we would save more lives,” Joshua E. Melson, MD, MPH, lead author of the AGA white paper and professor at Rush University Medical Center, Chicago, said in an interview.
Screening can reduce CRC mortality by more than 50%, he added.
“Screening should be thought of as a process over time, not a single test isolated in time,” Dr. Melson commented. A clinical practice that has historically used only colonoscopy will need an organized, structured program to incorporate noninvasive testing, he said.
To date, efforts to increase CRC screening uptake have met with limited success, the AGA says. In 2014, the National Colorectal Cancer Round Table set the bar high with a 2018 screening goal of 80% for adults 50 years of age and older. As of 2020, some states had almost reached this goal, but most had not.
“In the opportunistic screening environment in the U.S., where colonoscopy is the most prevalent method, CRC screening has not reached aspirational goals in terms of uptake, reduction in CRC incidence, and disease burden,” the AGA said. “It is questionable if 80% uptake is achievable in a primarily opportunistic screening environment.”
In the proposed revamping of the current CRC screening infrastructure, patients whose physicians recommend CRC screening would no longer be left to their own devices to follow up. Clinicians would initiate CRC screening and oversee follow-up testing at defined intervals and would employ ongoing surveillance.
Ensuring that appropriate screening is readily available to at-risk individuals with no social, racial, or economic disparities is crucial, the AGA says. Racial disparities in access to screening disproportionately burden Blacks and Latin Americans as well as people living in rural areas. Screening differences account for 42% of the disparity in CRC incidence between Black and White Americans and 19% of the disparity in CRC mortality.
Compared with colonoscopy, which requires bowel preparation, time off from work, and a hospital or clinic procedure, the fecal immunochemical test (FIT), for which a patient provides stool samples that are examined for the presence of blood, is much less stressful: it is noninvasive, and the patients collect the samples themselves in their own home. Studies show that, in diverse environments, patients prefer FIT over colonoscopy.
In a controlled trial that involved more than 55,000 patients who were randomly assigned to undergo either FIT or colonoscopy, the participation rate in the first cycle was greater for FIT than for colonoscopy (34.2% vs. 24.6%). This partially offset the lower single-application sensitivity for CRC of FIT, the researchers said.
Results from a study with a cluster randomized design showed that offering up-front stool testing as an option in addition to colonoscopy increased screening uptake. Of patients offered fecal occult blood testing or colonoscopy, 69% completed the noninvasive screening, compared with 38% of those offered colonoscopy alone. Notably, non-White participants were more adherent to stool testing.
The success of the AGA’s new initiative hinges largely upon the development of affordable, highly accurate, easy-to-use, noninvasive tests. In this regard, the organization has challenged scientists and industry partners with an aspirational target that is “far superior to current methodologies in terms of sensitivity and specificity,” said Dr. Melson, who is associate professor at Rush Medical College, Chicago, and a member of the AGA Center for GI Innovation and Technology.
The AGA wants new CRC screening tests that are capable of detecting advanced adenomas and advanced serrated lesions with a one-time sensitivity and specificity of 90% or higher, which is comparable with colonoscopy.
The FIT test has a sensitivity of less than 50% for detecting an advanced polyp of 10 mm or larger, said Dr. Melson.
The multitarget stool DNA (MT-sDNA) test may offer some improvement.
In a 2014 pivotal trial that compared FIT with the MT-sDNA in patients at average risk, the MT-sDNA test had higher sensitivity for detecting nonadvanced CRC lesions than FIT (92% vs. 74%) but less specificity (87% vs. 95%). The rate of detection of polyps with high-grade dysplasia was 69.2% with DNA testing and 46.2% with FIT.
However, the MT-sDNA test costs more than $500, compared with $25 for the FIT test, Dr. Melson pointed out.
To help identify the most appropriate screening for individual patients, better understanding and more thorough identification of risk factors are needed. “Risk assessment is definitely not where it could be,” Dr. Melson said.
The accuracy of risk assessment can be improved by sharing information from electronic health records on past colonoscopy polyp data, the presence of molecular markers, and family history, the AGA said. “With clearer risk assessment, shared decision-making on the most appropriate test becomes more clear and screening rates would benefit from patient buy-in and from easier access.”
The AGA recommended that research focus on the cost-effectiveness of screening younger patients, because the proportion of CRC cases in adults aged younger than 50 years has doubled since 1990.
This has raised the question as to whether the age for initial CRC screening should be lowered to 45 years (it already has been by the American Cancer Society), but there is much debate over this move.
Dr. Melson has received consulting fees from Clinical Genomics and research support from Boston Scientific Corporation and holds stocks in Virgo Imaging. A number of AGA white paper coauthors have disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
PVR reassessed as predictor of heart failure
A study of patients with pulmonary hypertension suggests a reconsideration of the accepted benchmark for pulmonary vascular hypertension as a predictor of heart failure may be warranted.
An elevated pulmonary vascular resistance of 3.0 Wood units or greater has been used as a prognostic marker for death and heart failure in pulmonary hypertension subgroups. But a large, multiyear study of a veterans population suggests that shifting that threshold to 2.2 Wood units in patients with right-heart catheterization may be justified.
Bradley A. Maron, MD, of the Veterans Affairs Boston Healthcare System and Brigham and Women’s Hospital and Harvard Medical School, Boston, and colleagues evaluated 40,082 veterans in the VA Clinical Assessment, Reporting and Tracking (CART) program who had right-heart catheterization (RHC) in the VA system from Oct. 1, 2007, to Sept. 30, 2016.
“To our knowledge, these data provide the first evidence-based information on the continuum of clinical risk related to PVR in patients with elevated pulmonary artery pressure,” the researchers wrote. Their report was published online in Lancet Respiratory Medicine (2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9).
The retrospective cohort study found that all-cause mortality hazard ratio (HR), when adjusted for clinical variables, and mean pulmonary artery pressure (mPAP) increased progressively beginning at around 2.0 Wood units (WU). Clinically significant mortality HR emerged at 2.2 WU, with an adjusted risk 9% greater than a PVR of 2.1 Wood units (P < .0034), which the study considered the upper limit of normal PVR in health adults of a similar age range (61.5 to 73.5 years) as the study cohort. The researchers noted that a PVR of 3.0 WU has been the standard for forecasting outcomes in pulmonary hypertension (PH) (Eur Heart J. 2010;31:2915-57).
“Overall, these results suggest that reconsidering the hemodynamic parameters that define pulmonary hypertension in patients with cardiopulmonary disease is warranted, and they identify a need for early detection strategies to capture this large and vulnerable population,” the researchers wrote.
A subsequent analysis focused on patients with an mPAP of >19 mm HG (n = 32,725) and found that all-cause death when adjusted over a wide range of clinical variables that included PVR of 2.2 WU increased to a 25% HR. “However,” the researchers added, “a median cardiac output of < 4.0 L/min, which has been shown to be independently associated with adverse outcome, was present only when PVR was more than 4.0 Wood units.”
For a PVR of 2.2-3.0 WU, the median cardiac output was 4.87 L/min; for > 3.0 WU, it was 4.13 L/min. Among the patients with PVR > 2.2 WU (n = 15,780), 13.6% (n = 2,147) had an mPAP of 19-24 mm Hg.
In all patients with mPAP > 19 mm HG, pulmonary artery wedge pressure (PAWP) became a determining risk factor, with 15 mm HG the demarcation between low and high PAWP. At PVR of 2.2 WU, low-PAWP patients had a 52% greater adjusted risk of death and high-PAWP a 23% greater risk. At 4.0 WU, those adjusted risks rose dramatically – to 272% and 58%, for the low- and high-PAWP subgroups, respectively (P < .0001).
“Stratification of patients by PAWP had a major effect on outcome estimates in our study, illustrating the limitations of using the same PVR level to define clinical risk between precapillary and postcapillary pulmonary hypertension,” the researchers wrote.
They called for further study into how these findings impact people with PH but lower levels of cardiopulmonary disease than the cohort. “Overall, these findings support reconsidering the combination of hemodynamic variables used to identify patients with pulmonary hypertension,” the researchers stated.
The analyses of the VA CART database makes this “an interesting study,” said G. Hossein Almassi, MD, FCCP, of the Medical College of Wisconsin and Zablocki VA Medical Center in Milwaukee. “Within its limitation as a retrospective cohort study, the findings of a lower PVR and a lower mean PAP of > 19 mm being associated with increased risk of all-cause mortality and HF hospitalization are significant.”
He added: “Time will tell whether this will be an impetus for the clinicians to consider earlier therapeutic interventions in addition to lifestyle modification such as smoking cessation in this group of patients.”
Dr. Maron disclosed a financial relationship with Actelion.
SOURCE: Maron BA et al. Lancet Respir Med. 2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9.
A study of patients with pulmonary hypertension suggests a reconsideration of the accepted benchmark for pulmonary vascular hypertension as a predictor of heart failure may be warranted.
An elevated pulmonary vascular resistance of 3.0 Wood units or greater has been used as a prognostic marker for death and heart failure in pulmonary hypertension subgroups. But a large, multiyear study of a veterans population suggests that shifting that threshold to 2.2 Wood units in patients with right-heart catheterization may be justified.
Bradley A. Maron, MD, of the Veterans Affairs Boston Healthcare System and Brigham and Women’s Hospital and Harvard Medical School, Boston, and colleagues evaluated 40,082 veterans in the VA Clinical Assessment, Reporting and Tracking (CART) program who had right-heart catheterization (RHC) in the VA system from Oct. 1, 2007, to Sept. 30, 2016.
“To our knowledge, these data provide the first evidence-based information on the continuum of clinical risk related to PVR in patients with elevated pulmonary artery pressure,” the researchers wrote. Their report was published online in Lancet Respiratory Medicine (2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9).
The retrospective cohort study found that all-cause mortality hazard ratio (HR), when adjusted for clinical variables, and mean pulmonary artery pressure (mPAP) increased progressively beginning at around 2.0 Wood units (WU). Clinically significant mortality HR emerged at 2.2 WU, with an adjusted risk 9% greater than a PVR of 2.1 Wood units (P < .0034), which the study considered the upper limit of normal PVR in health adults of a similar age range (61.5 to 73.5 years) as the study cohort. The researchers noted that a PVR of 3.0 WU has been the standard for forecasting outcomes in pulmonary hypertension (PH) (Eur Heart J. 2010;31:2915-57).
“Overall, these results suggest that reconsidering the hemodynamic parameters that define pulmonary hypertension in patients with cardiopulmonary disease is warranted, and they identify a need for early detection strategies to capture this large and vulnerable population,” the researchers wrote.
A subsequent analysis focused on patients with an mPAP of >19 mm HG (n = 32,725) and found that all-cause death when adjusted over a wide range of clinical variables that included PVR of 2.2 WU increased to a 25% HR. “However,” the researchers added, “a median cardiac output of < 4.0 L/min, which has been shown to be independently associated with adverse outcome, was present only when PVR was more than 4.0 Wood units.”
For a PVR of 2.2-3.0 WU, the median cardiac output was 4.87 L/min; for > 3.0 WU, it was 4.13 L/min. Among the patients with PVR > 2.2 WU (n = 15,780), 13.6% (n = 2,147) had an mPAP of 19-24 mm Hg.
In all patients with mPAP > 19 mm HG, pulmonary artery wedge pressure (PAWP) became a determining risk factor, with 15 mm HG the demarcation between low and high PAWP. At PVR of 2.2 WU, low-PAWP patients had a 52% greater adjusted risk of death and high-PAWP a 23% greater risk. At 4.0 WU, those adjusted risks rose dramatically – to 272% and 58%, for the low- and high-PAWP subgroups, respectively (P < .0001).
“Stratification of patients by PAWP had a major effect on outcome estimates in our study, illustrating the limitations of using the same PVR level to define clinical risk between precapillary and postcapillary pulmonary hypertension,” the researchers wrote.
They called for further study into how these findings impact people with PH but lower levels of cardiopulmonary disease than the cohort. “Overall, these findings support reconsidering the combination of hemodynamic variables used to identify patients with pulmonary hypertension,” the researchers stated.
The analyses of the VA CART database makes this “an interesting study,” said G. Hossein Almassi, MD, FCCP, of the Medical College of Wisconsin and Zablocki VA Medical Center in Milwaukee. “Within its limitation as a retrospective cohort study, the findings of a lower PVR and a lower mean PAP of > 19 mm being associated with increased risk of all-cause mortality and HF hospitalization are significant.”
He added: “Time will tell whether this will be an impetus for the clinicians to consider earlier therapeutic interventions in addition to lifestyle modification such as smoking cessation in this group of patients.”
Dr. Maron disclosed a financial relationship with Actelion.
SOURCE: Maron BA et al. Lancet Respir Med. 2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9.
A study of patients with pulmonary hypertension suggests a reconsideration of the accepted benchmark for pulmonary vascular hypertension as a predictor of heart failure may be warranted.
An elevated pulmonary vascular resistance of 3.0 Wood units or greater has been used as a prognostic marker for death and heart failure in pulmonary hypertension subgroups. But a large, multiyear study of a veterans population suggests that shifting that threshold to 2.2 Wood units in patients with right-heart catheterization may be justified.
Bradley A. Maron, MD, of the Veterans Affairs Boston Healthcare System and Brigham and Women’s Hospital and Harvard Medical School, Boston, and colleagues evaluated 40,082 veterans in the VA Clinical Assessment, Reporting and Tracking (CART) program who had right-heart catheterization (RHC) in the VA system from Oct. 1, 2007, to Sept. 30, 2016.
“To our knowledge, these data provide the first evidence-based information on the continuum of clinical risk related to PVR in patients with elevated pulmonary artery pressure,” the researchers wrote. Their report was published online in Lancet Respiratory Medicine (2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9).
The retrospective cohort study found that all-cause mortality hazard ratio (HR), when adjusted for clinical variables, and mean pulmonary artery pressure (mPAP) increased progressively beginning at around 2.0 Wood units (WU). Clinically significant mortality HR emerged at 2.2 WU, with an adjusted risk 9% greater than a PVR of 2.1 Wood units (P < .0034), which the study considered the upper limit of normal PVR in health adults of a similar age range (61.5 to 73.5 years) as the study cohort. The researchers noted that a PVR of 3.0 WU has been the standard for forecasting outcomes in pulmonary hypertension (PH) (Eur Heart J. 2010;31:2915-57).
“Overall, these results suggest that reconsidering the hemodynamic parameters that define pulmonary hypertension in patients with cardiopulmonary disease is warranted, and they identify a need for early detection strategies to capture this large and vulnerable population,” the researchers wrote.
A subsequent analysis focused on patients with an mPAP of >19 mm HG (n = 32,725) and found that all-cause death when adjusted over a wide range of clinical variables that included PVR of 2.2 WU increased to a 25% HR. “However,” the researchers added, “a median cardiac output of < 4.0 L/min, which has been shown to be independently associated with adverse outcome, was present only when PVR was more than 4.0 Wood units.”
For a PVR of 2.2-3.0 WU, the median cardiac output was 4.87 L/min; for > 3.0 WU, it was 4.13 L/min. Among the patients with PVR > 2.2 WU (n = 15,780), 13.6% (n = 2,147) had an mPAP of 19-24 mm Hg.
In all patients with mPAP > 19 mm HG, pulmonary artery wedge pressure (PAWP) became a determining risk factor, with 15 mm HG the demarcation between low and high PAWP. At PVR of 2.2 WU, low-PAWP patients had a 52% greater adjusted risk of death and high-PAWP a 23% greater risk. At 4.0 WU, those adjusted risks rose dramatically – to 272% and 58%, for the low- and high-PAWP subgroups, respectively (P < .0001).
“Stratification of patients by PAWP had a major effect on outcome estimates in our study, illustrating the limitations of using the same PVR level to define clinical risk between precapillary and postcapillary pulmonary hypertension,” the researchers wrote.
They called for further study into how these findings impact people with PH but lower levels of cardiopulmonary disease than the cohort. “Overall, these findings support reconsidering the combination of hemodynamic variables used to identify patients with pulmonary hypertension,” the researchers stated.
The analyses of the VA CART database makes this “an interesting study,” said G. Hossein Almassi, MD, FCCP, of the Medical College of Wisconsin and Zablocki VA Medical Center in Milwaukee. “Within its limitation as a retrospective cohort study, the findings of a lower PVR and a lower mean PAP of > 19 mm being associated with increased risk of all-cause mortality and HF hospitalization are significant.”
He added: “Time will tell whether this will be an impetus for the clinicians to consider earlier therapeutic interventions in addition to lifestyle modification such as smoking cessation in this group of patients.”
Dr. Maron disclosed a financial relationship with Actelion.
SOURCE: Maron BA et al. Lancet Respir Med. 2020 Jul 27. doi: 10.1016/S2213-2600(20)30317-9.
FROM LANCET RESPIRATORY MEDICINE
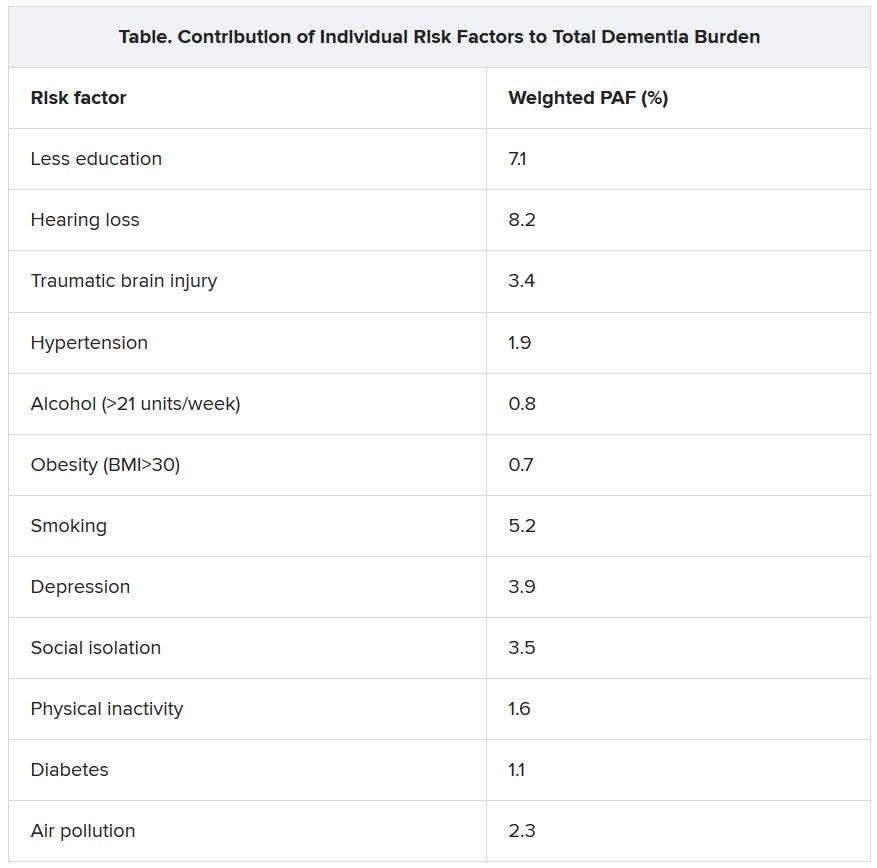
Health disparity: Race, mortality, and infants of teenage mothers
according to a new analysis from the National Center for Health Statistics.
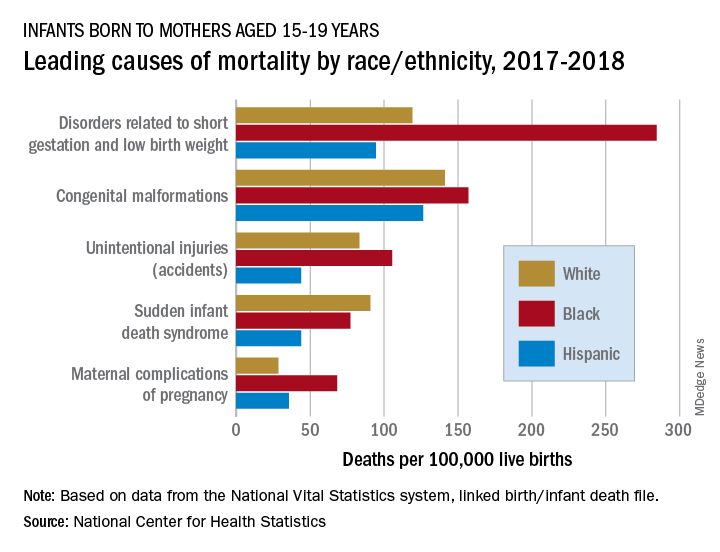
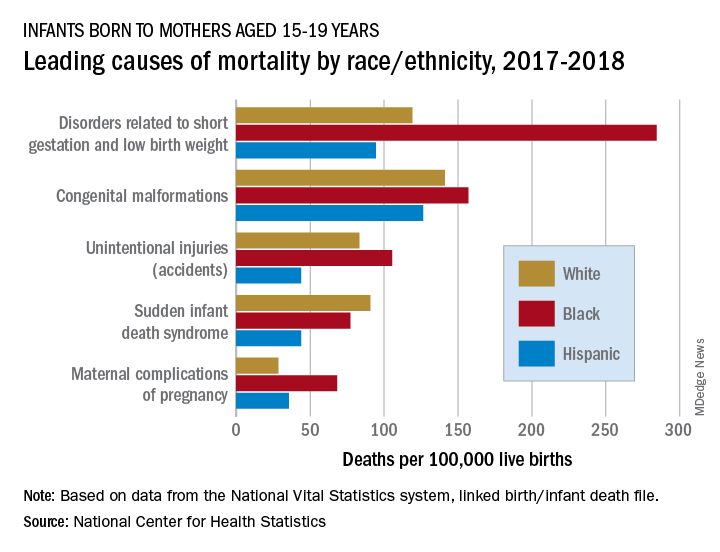
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
according to a new analysis from the National Center for Health Statistics.
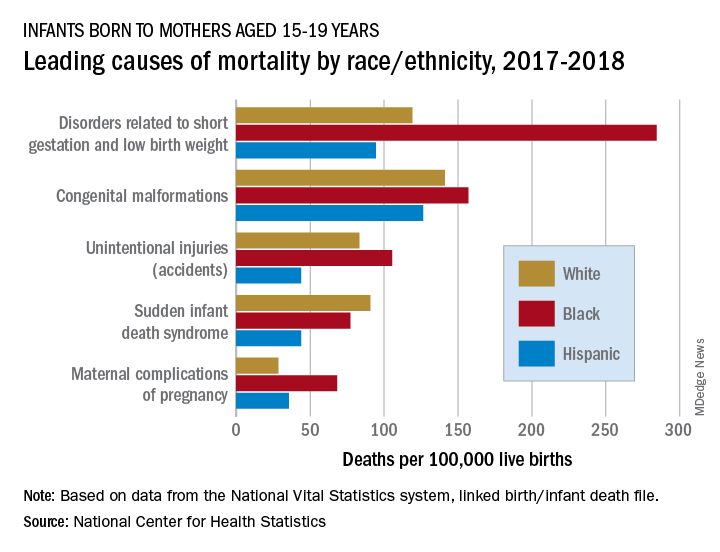
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
according to a new analysis from the National Center for Health Statistics.
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
Children’s doctors in the world of adults
Pediatric hospitalists venture into COVID-19 adult care
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.
Pediatric hospitalists venture into COVID-19 adult care
Pediatric hospitalists venture into COVID-19 adult care
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.
Beyond PSA: New prostate cancer screening options
Two noninvasive tests — an assessment of spermine levels in urine and a blood test that combines free and total PSA and the (-2) pro-PSA isoform (p2PSA) — are much safer than historically risky biopsy and what is now considered to have been unnecessary surgery.
“We’ve ‘cured’ a lot of men,” Franklin Gaylis, MD, from the University of California, San Diego, told Medscape Medical News. “Even some who didn’t need to be cured.” Now, we are working to solve this dilemma, he said. “It’s time we determine who do you screen, [who do you] not screen, and how aggressively?”
Urine Spermine Test More Accurate Than PSA
Data from a highly predictive test that assesses spermine levels in urine were presented by Peter Ka-Fung Chiu, MD, from the University of Hong Kong, at the virtual annual congress of the European Association of Urology. Normal spermine levels are inversely associated with both prostate cancer (PCa) and high-grade prostate cancer (HGPCa).
To investigate the predictive value of spermine for any PCa or HGPCa (Gleason 7 or above), the researchers recruited 556 men from two centers and collected 30 mL of urine prior to prostate biopsy.
They analyzed data from 390 men and used decision-curve analyses for PCa and for HGPCa. The multivariate spermine score — which takes into account age, prostate volume, PSA level, and spermine level — provided net clinical benefit over PSA alone and over spermine score alone.
“At 90% sensitivity, this risk score actually had a negative predictive value of 96.7% and avoided about 50% of unnecessary biopsies,” Chiu explained. “This test predicts prostate cancer and high-grade prostate cancer well, without the need for prior prostate massage, offering improved predictive performance.”
PHI Reduces Need for MRI Screening
Another test, the PHI prostate cancer biomarker, is as predictive as multiparametric (mp)MRI, both with and without PSA scoring.
PHI scores from 554 men from five centers added to either PSA density or mpMRI improved the prediction of risk for ≥GG2 cancers to more than 0.81 and for ≥CPG3 cancers to more than 0.85, according to data from the multicenter PRIM (PHI to Refine MRI) study group recently published in BMC Medicine and presented at EAU.
With a PHI cut-off of 30, mpMRI referrals could be cut by 25%, and unnecessary biopsies could be cut by 40%, the PRIM group reports. PHI misses 8% of ≥GG2 cancers, whereas mpMRI misses 9%.
The PHI strategy reduces “mpMRI and biopsies without compromising detection of significant prostate cancers,” and also reduces costs, Nicholas Boxall, MB ChB, from Cambridge University Hospitals NHS Foundation Trust in the United Kingdom, explained during his presentation
“Instead of screening everyone, we’re risk-adapting who needs to be screened, identifying the right population and defaulting to MRI as an alternative to invasive biopsy, and doing secondary tests to look at biomarkers,” said Gerald Andriole, MD, from the Washington University School of Medicine in St. Louis, Missouri.
“We don’t have to auto-toggle to aggressive treatment,” he told Medscape Medical News. “We’re getting better than we were 10 years ago, but we need slightly better tests, and we also need better biopsies; urologists must be more careful.”
Chiu and Boxall report no relevant financial relationships. Gaylis is a scientific advisor for Stratify Genomics. Andriole is on the advisory board of Stratify Genomics.
This article first appeared on Medscape.com.
Two noninvasive tests — an assessment of spermine levels in urine and a blood test that combines free and total PSA and the (-2) pro-PSA isoform (p2PSA) — are much safer than historically risky biopsy and what is now considered to have been unnecessary surgery.
“We’ve ‘cured’ a lot of men,” Franklin Gaylis, MD, from the University of California, San Diego, told Medscape Medical News. “Even some who didn’t need to be cured.” Now, we are working to solve this dilemma, he said. “It’s time we determine who do you screen, [who do you] not screen, and how aggressively?”
Urine Spermine Test More Accurate Than PSA
Data from a highly predictive test that assesses spermine levels in urine were presented by Peter Ka-Fung Chiu, MD, from the University of Hong Kong, at the virtual annual congress of the European Association of Urology. Normal spermine levels are inversely associated with both prostate cancer (PCa) and high-grade prostate cancer (HGPCa).
To investigate the predictive value of spermine for any PCa or HGPCa (Gleason 7 or above), the researchers recruited 556 men from two centers and collected 30 mL of urine prior to prostate biopsy.
They analyzed data from 390 men and used decision-curve analyses for PCa and for HGPCa. The multivariate spermine score — which takes into account age, prostate volume, PSA level, and spermine level — provided net clinical benefit over PSA alone and over spermine score alone.
“At 90% sensitivity, this risk score actually had a negative predictive value of 96.7% and avoided about 50% of unnecessary biopsies,” Chiu explained. “This test predicts prostate cancer and high-grade prostate cancer well, without the need for prior prostate massage, offering improved predictive performance.”
PHI Reduces Need for MRI Screening
Another test, the PHI prostate cancer biomarker, is as predictive as multiparametric (mp)MRI, both with and without PSA scoring.
PHI scores from 554 men from five centers added to either PSA density or mpMRI improved the prediction of risk for ≥GG2 cancers to more than 0.81 and for ≥CPG3 cancers to more than 0.85, according to data from the multicenter PRIM (PHI to Refine MRI) study group recently published in BMC Medicine and presented at EAU.
With a PHI cut-off of 30, mpMRI referrals could be cut by 25%, and unnecessary biopsies could be cut by 40%, the PRIM group reports. PHI misses 8% of ≥GG2 cancers, whereas mpMRI misses 9%.
The PHI strategy reduces “mpMRI and biopsies without compromising detection of significant prostate cancers,” and also reduces costs, Nicholas Boxall, MB ChB, from Cambridge University Hospitals NHS Foundation Trust in the United Kingdom, explained during his presentation
“Instead of screening everyone, we’re risk-adapting who needs to be screened, identifying the right population and defaulting to MRI as an alternative to invasive biopsy, and doing secondary tests to look at biomarkers,” said Gerald Andriole, MD, from the Washington University School of Medicine in St. Louis, Missouri.
“We don’t have to auto-toggle to aggressive treatment,” he told Medscape Medical News. “We’re getting better than we were 10 years ago, but we need slightly better tests, and we also need better biopsies; urologists must be more careful.”
Chiu and Boxall report no relevant financial relationships. Gaylis is a scientific advisor for Stratify Genomics. Andriole is on the advisory board of Stratify Genomics.
This article first appeared on Medscape.com.
Two noninvasive tests — an assessment of spermine levels in urine and a blood test that combines free and total PSA and the (-2) pro-PSA isoform (p2PSA) — are much safer than historically risky biopsy and what is now considered to have been unnecessary surgery.
“We’ve ‘cured’ a lot of men,” Franklin Gaylis, MD, from the University of California, San Diego, told Medscape Medical News. “Even some who didn’t need to be cured.” Now, we are working to solve this dilemma, he said. “It’s time we determine who do you screen, [who do you] not screen, and how aggressively?”
Urine Spermine Test More Accurate Than PSA
Data from a highly predictive test that assesses spermine levels in urine were presented by Peter Ka-Fung Chiu, MD, from the University of Hong Kong, at the virtual annual congress of the European Association of Urology. Normal spermine levels are inversely associated with both prostate cancer (PCa) and high-grade prostate cancer (HGPCa).
To investigate the predictive value of spermine for any PCa or HGPCa (Gleason 7 or above), the researchers recruited 556 men from two centers and collected 30 mL of urine prior to prostate biopsy.
They analyzed data from 390 men and used decision-curve analyses for PCa and for HGPCa. The multivariate spermine score — which takes into account age, prostate volume, PSA level, and spermine level — provided net clinical benefit over PSA alone and over spermine score alone.
“At 90% sensitivity, this risk score actually had a negative predictive value of 96.7% and avoided about 50% of unnecessary biopsies,” Chiu explained. “This test predicts prostate cancer and high-grade prostate cancer well, without the need for prior prostate massage, offering improved predictive performance.”
PHI Reduces Need for MRI Screening
Another test, the PHI prostate cancer biomarker, is as predictive as multiparametric (mp)MRI, both with and without PSA scoring.
PHI scores from 554 men from five centers added to either PSA density or mpMRI improved the prediction of risk for ≥GG2 cancers to more than 0.81 and for ≥CPG3 cancers to more than 0.85, according to data from the multicenter PRIM (PHI to Refine MRI) study group recently published in BMC Medicine and presented at EAU.
With a PHI cut-off of 30, mpMRI referrals could be cut by 25%, and unnecessary biopsies could be cut by 40%, the PRIM group reports. PHI misses 8% of ≥GG2 cancers, whereas mpMRI misses 9%.
The PHI strategy reduces “mpMRI and biopsies without compromising detection of significant prostate cancers,” and also reduces costs, Nicholas Boxall, MB ChB, from Cambridge University Hospitals NHS Foundation Trust in the United Kingdom, explained during his presentation
“Instead of screening everyone, we’re risk-adapting who needs to be screened, identifying the right population and defaulting to MRI as an alternative to invasive biopsy, and doing secondary tests to look at biomarkers,” said Gerald Andriole, MD, from the Washington University School of Medicine in St. Louis, Missouri.
“We don’t have to auto-toggle to aggressive treatment,” he told Medscape Medical News. “We’re getting better than we were 10 years ago, but we need slightly better tests, and we also need better biopsies; urologists must be more careful.”
Chiu and Boxall report no relevant financial relationships. Gaylis is a scientific advisor for Stratify Genomics. Andriole is on the advisory board of Stratify Genomics.
This article first appeared on Medscape.com.
Many children with COVID-19 present without classic symptoms
Most children who tested positive for SARS-CoV-2 had no respiratory illness, according to data from a retrospective study of 22 patients at a single center.
To date, children account for less than 5% of COVID-19 cases in the United States, but details of the clinical presentations in children are limited, wrote Rabia Agha, MD, and colleagues of Maimonides Children’s Hospital, Brooklyn, N.Y.
In a study published in Hospital Pediatrics, the researchers reviewed data from 22 children aged 0-18 years who tested positive for SARS-CoV-2 by polymerase chain reaction (PCR) and were admitted to a single hospital over a 4-week period from March 18, 2020, to April 15, 2020.
Of four patients requiring mechanical ventilation, two had underlying pulmonary disease. The other two patients who required intubation were one with cerebral palsy and status epilepticus and one who presented in a state of cardiac arrest.
The study population ranged from 11 days to 18 years of age, but 45% were infants younger than 1 year. None of the children had a travel history that might increase their risk for SARS-CoV-2 infection; 27% had confirmed exposure to the virus.
Most of the children (82%) were hospitalized within 3 days of the onset of symptoms, and no deaths occurred during the study period. The most common symptom was fever without a source in five (23%) otherwise healthy infants aged 11-35 days. All five of these children underwent a sepsis evaluation, received empiric antibiotics, and were discharged home with negative bacterial cultures within 48-72 hours. Another 10 children had fever in combination with other symptoms.
Other presenting symptoms were respiratory (9), fatigue (6), seizures (2), and headache (1).
Most children with respiratory illness were treated with supportive therapy and antibiotics, but three of those on mechanical ventilation also were treated with remdesivir; all three were ultimately extubated.
Neurological abnormalities occurred in two patients: an 11-year-old otherwise healthy boy who presented with fever, headache, confusion, and seizure but ultimately improved without short-term sequelae; and a 12-year-old girl with cerebral palsy who developed new onset seizures and required mechanical ventilation, but ultimately improved to baseline.
Positive PCR results were identified in seven patients (32%) during the second half of the study period who were initially hospitalized for non-COVID related symptoms; four with bacterial infections, two with illnesses of unknown etiology, and one with cardiac arrest. Another two children were completely asymptomatic at the time of admission but then tested positive by PCR; one child had been admitted for routine chemotherapy and the other for social reasons, Dr. Agha and associates said.
The study findings contrast with early data from China in which respiratory illness of varying severity was the major presentation in children with COVID-19, but support a more recent meta-analysis of 551 cases, the researchers noted. The findings also highlight the value of universal testing for children.
“Our initial testing strategy was according to the federal and local guidelines that recommended PCR testing for the symptoms of fever, cough and shortness of breath, or travel to certain countries or close contact with a confirmed case,” Dr. Agha and colleagues said.
“With the implementation of our universal screening strategy of all admitted pediatric patients, we identified 9 (41%) patients with COVID-19 that would have been missed, as they did not meet the then-recommended criteria for testing,” they wrote.
The results suggest the need for broader guidelines to test pediatric patients because children presenting with other illnesses may be positive for SARS-CoV-2 as well, the researchers said.
“Testing of all hospitalized patients will not only identify cases early in the course of their admission process, but will also help prevent inadvertent exposure of other patients and health care workers, assist in cohorting infected patients, and aid in conservation of personal protective equipment,” Dr. Agha and associates concluded.
The current study is important as clinicians continue to learn about how infection with SARS-CoV-2 presents in different populations, Diana Lee, MD, of the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Understanding how it can present in the pediatric population is important in identifying children who may have the infection and developing strategies for testing,” she said.
“I was not surprised by the finding that most children did not present with the classic symptoms of COVID-19 in adults based on other published studies and my personal clinical experience taking care of hospitalized children in New York City,” said Dr. Lee. “Studies from the U.S. and other countries have reported that fewer children experience fever, cough, and shortness of breath [compared with] adults, and that most children have a milder clinical course, though there is a small percentage of children who can have severe or critical illness,” she said.
“A multisystem inflammatory syndrome in children associated with COVID-19 has also emerged and appears to be a postinfectious process with a presentation that often differs from classic COVID-19 infection in adults,” she added.
The take-home message for clinicians is the reminder that SARS-CoV-2 infection often presents differently in children than in adults, said Dr. Lee.
“Children who present to the hospital with non-classic COVID-19 symptoms or with other diagnoses may be positive for SARS-CoV-2 on testing. Broadly testing hospitalized children for SARS-CoV-2 and instituting appropriate isolation precautions may help to protect other individuals from being exposed to the virus,” she said.
“Further research is needed to understand which individuals are contagious and how to accurately distinguish those who are infectious versus those who are not,” said Dr. Lee. “There have been individuals who persistently test positive for SARS-CoV-2 RNA (the genetic material of the virus), but were not found to have virus in their bodies that can replicate and thereby infect others,” she emphasized. “Further study is needed regarding the likelihood of household exposures in children with SARS-CoV-2 infection given that this study was done early in the epidemic in New York City when testing and contact tracing was less established,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Lee had no financial conflicts to disclose.
SOURCE: Agha R et al. Hosp Pediatr. 2020 July. doi: 10.1542/hpeds.2020-000257.
Most children who tested positive for SARS-CoV-2 had no respiratory illness, according to data from a retrospective study of 22 patients at a single center.
To date, children account for less than 5% of COVID-19 cases in the United States, but details of the clinical presentations in children are limited, wrote Rabia Agha, MD, and colleagues of Maimonides Children’s Hospital, Brooklyn, N.Y.
In a study published in Hospital Pediatrics, the researchers reviewed data from 22 children aged 0-18 years who tested positive for SARS-CoV-2 by polymerase chain reaction (PCR) and were admitted to a single hospital over a 4-week period from March 18, 2020, to April 15, 2020.
Of four patients requiring mechanical ventilation, two had underlying pulmonary disease. The other two patients who required intubation were one with cerebral palsy and status epilepticus and one who presented in a state of cardiac arrest.
The study population ranged from 11 days to 18 years of age, but 45% were infants younger than 1 year. None of the children had a travel history that might increase their risk for SARS-CoV-2 infection; 27% had confirmed exposure to the virus.
Most of the children (82%) were hospitalized within 3 days of the onset of symptoms, and no deaths occurred during the study period. The most common symptom was fever without a source in five (23%) otherwise healthy infants aged 11-35 days. All five of these children underwent a sepsis evaluation, received empiric antibiotics, and were discharged home with negative bacterial cultures within 48-72 hours. Another 10 children had fever in combination with other symptoms.
Other presenting symptoms were respiratory (9), fatigue (6), seizures (2), and headache (1).
Most children with respiratory illness were treated with supportive therapy and antibiotics, but three of those on mechanical ventilation also were treated with remdesivir; all three were ultimately extubated.
Neurological abnormalities occurred in two patients: an 11-year-old otherwise healthy boy who presented with fever, headache, confusion, and seizure but ultimately improved without short-term sequelae; and a 12-year-old girl with cerebral palsy who developed new onset seizures and required mechanical ventilation, but ultimately improved to baseline.
Positive PCR results were identified in seven patients (32%) during the second half of the study period who were initially hospitalized for non-COVID related symptoms; four with bacterial infections, two with illnesses of unknown etiology, and one with cardiac arrest. Another two children were completely asymptomatic at the time of admission but then tested positive by PCR; one child had been admitted for routine chemotherapy and the other for social reasons, Dr. Agha and associates said.
The study findings contrast with early data from China in which respiratory illness of varying severity was the major presentation in children with COVID-19, but support a more recent meta-analysis of 551 cases, the researchers noted. The findings also highlight the value of universal testing for children.
“Our initial testing strategy was according to the federal and local guidelines that recommended PCR testing for the symptoms of fever, cough and shortness of breath, or travel to certain countries or close contact with a confirmed case,” Dr. Agha and colleagues said.
“With the implementation of our universal screening strategy of all admitted pediatric patients, we identified 9 (41%) patients with COVID-19 that would have been missed, as they did not meet the then-recommended criteria for testing,” they wrote.
The results suggest the need for broader guidelines to test pediatric patients because children presenting with other illnesses may be positive for SARS-CoV-2 as well, the researchers said.
“Testing of all hospitalized patients will not only identify cases early in the course of their admission process, but will also help prevent inadvertent exposure of other patients and health care workers, assist in cohorting infected patients, and aid in conservation of personal protective equipment,” Dr. Agha and associates concluded.
The current study is important as clinicians continue to learn about how infection with SARS-CoV-2 presents in different populations, Diana Lee, MD, of the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Understanding how it can present in the pediatric population is important in identifying children who may have the infection and developing strategies for testing,” she said.
“I was not surprised by the finding that most children did not present with the classic symptoms of COVID-19 in adults based on other published studies and my personal clinical experience taking care of hospitalized children in New York City,” said Dr. Lee. “Studies from the U.S. and other countries have reported that fewer children experience fever, cough, and shortness of breath [compared with] adults, and that most children have a milder clinical course, though there is a small percentage of children who can have severe or critical illness,” she said.
“A multisystem inflammatory syndrome in children associated with COVID-19 has also emerged and appears to be a postinfectious process with a presentation that often differs from classic COVID-19 infection in adults,” she added.
The take-home message for clinicians is the reminder that SARS-CoV-2 infection often presents differently in children than in adults, said Dr. Lee.
“Children who present to the hospital with non-classic COVID-19 symptoms or with other diagnoses may be positive for SARS-CoV-2 on testing. Broadly testing hospitalized children for SARS-CoV-2 and instituting appropriate isolation precautions may help to protect other individuals from being exposed to the virus,” she said.
“Further research is needed to understand which individuals are contagious and how to accurately distinguish those who are infectious versus those who are not,” said Dr. Lee. “There have been individuals who persistently test positive for SARS-CoV-2 RNA (the genetic material of the virus), but were not found to have virus in their bodies that can replicate and thereby infect others,” she emphasized. “Further study is needed regarding the likelihood of household exposures in children with SARS-CoV-2 infection given that this study was done early in the epidemic in New York City when testing and contact tracing was less established,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Lee had no financial conflicts to disclose.
SOURCE: Agha R et al. Hosp Pediatr. 2020 July. doi: 10.1542/hpeds.2020-000257.
Most children who tested positive for SARS-CoV-2 had no respiratory illness, according to data from a retrospective study of 22 patients at a single center.
To date, children account for less than 5% of COVID-19 cases in the United States, but details of the clinical presentations in children are limited, wrote Rabia Agha, MD, and colleagues of Maimonides Children’s Hospital, Brooklyn, N.Y.
In a study published in Hospital Pediatrics, the researchers reviewed data from 22 children aged 0-18 years who tested positive for SARS-CoV-2 by polymerase chain reaction (PCR) and were admitted to a single hospital over a 4-week period from March 18, 2020, to April 15, 2020.
Of four patients requiring mechanical ventilation, two had underlying pulmonary disease. The other two patients who required intubation were one with cerebral palsy and status epilepticus and one who presented in a state of cardiac arrest.
The study population ranged from 11 days to 18 years of age, but 45% were infants younger than 1 year. None of the children had a travel history that might increase their risk for SARS-CoV-2 infection; 27% had confirmed exposure to the virus.
Most of the children (82%) were hospitalized within 3 days of the onset of symptoms, and no deaths occurred during the study period. The most common symptom was fever without a source in five (23%) otherwise healthy infants aged 11-35 days. All five of these children underwent a sepsis evaluation, received empiric antibiotics, and were discharged home with negative bacterial cultures within 48-72 hours. Another 10 children had fever in combination with other symptoms.
Other presenting symptoms were respiratory (9), fatigue (6), seizures (2), and headache (1).
Most children with respiratory illness were treated with supportive therapy and antibiotics, but three of those on mechanical ventilation also were treated with remdesivir; all three were ultimately extubated.
Neurological abnormalities occurred in two patients: an 11-year-old otherwise healthy boy who presented with fever, headache, confusion, and seizure but ultimately improved without short-term sequelae; and a 12-year-old girl with cerebral palsy who developed new onset seizures and required mechanical ventilation, but ultimately improved to baseline.
Positive PCR results were identified in seven patients (32%) during the second half of the study period who were initially hospitalized for non-COVID related symptoms; four with bacterial infections, two with illnesses of unknown etiology, and one with cardiac arrest. Another two children were completely asymptomatic at the time of admission but then tested positive by PCR; one child had been admitted for routine chemotherapy and the other for social reasons, Dr. Agha and associates said.
The study findings contrast with early data from China in which respiratory illness of varying severity was the major presentation in children with COVID-19, but support a more recent meta-analysis of 551 cases, the researchers noted. The findings also highlight the value of universal testing for children.
“Our initial testing strategy was according to the federal and local guidelines that recommended PCR testing for the symptoms of fever, cough and shortness of breath, or travel to certain countries or close contact with a confirmed case,” Dr. Agha and colleagues said.
“With the implementation of our universal screening strategy of all admitted pediatric patients, we identified 9 (41%) patients with COVID-19 that would have been missed, as they did not meet the then-recommended criteria for testing,” they wrote.
The results suggest the need for broader guidelines to test pediatric patients because children presenting with other illnesses may be positive for SARS-CoV-2 as well, the researchers said.
“Testing of all hospitalized patients will not only identify cases early in the course of their admission process, but will also help prevent inadvertent exposure of other patients and health care workers, assist in cohorting infected patients, and aid in conservation of personal protective equipment,” Dr. Agha and associates concluded.
The current study is important as clinicians continue to learn about how infection with SARS-CoV-2 presents in different populations, Diana Lee, MD, of the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Understanding how it can present in the pediatric population is important in identifying children who may have the infection and developing strategies for testing,” she said.
“I was not surprised by the finding that most children did not present with the classic symptoms of COVID-19 in adults based on other published studies and my personal clinical experience taking care of hospitalized children in New York City,” said Dr. Lee. “Studies from the U.S. and other countries have reported that fewer children experience fever, cough, and shortness of breath [compared with] adults, and that most children have a milder clinical course, though there is a small percentage of children who can have severe or critical illness,” she said.
“A multisystem inflammatory syndrome in children associated with COVID-19 has also emerged and appears to be a postinfectious process with a presentation that often differs from classic COVID-19 infection in adults,” she added.
The take-home message for clinicians is the reminder that SARS-CoV-2 infection often presents differently in children than in adults, said Dr. Lee.
“Children who present to the hospital with non-classic COVID-19 symptoms or with other diagnoses may be positive for SARS-CoV-2 on testing. Broadly testing hospitalized children for SARS-CoV-2 and instituting appropriate isolation precautions may help to protect other individuals from being exposed to the virus,” she said.
“Further research is needed to understand which individuals are contagious and how to accurately distinguish those who are infectious versus those who are not,” said Dr. Lee. “There have been individuals who persistently test positive for SARS-CoV-2 RNA (the genetic material of the virus), but were not found to have virus in their bodies that can replicate and thereby infect others,” she emphasized. “Further study is needed regarding the likelihood of household exposures in children with SARS-CoV-2 infection given that this study was done early in the epidemic in New York City when testing and contact tracing was less established,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Lee had no financial conflicts to disclose.
SOURCE: Agha R et al. Hosp Pediatr. 2020 July. doi: 10.1542/hpeds.2020-000257.
FROM HOSPITAL PEDIATRICS
Diabetic amputations soared amid Italian pandemic lockdown
Amid a mandatory national lockdown, the rates of amputations skyrocketed at a hospital far from the hardest-hit region as many patients developed gangrene.
The findings offer critical lessons for the United States, said wound care specialist William H. Tettelbach, MD, of Western Peaks Specialty Hospital near Salt Lake City. “It’s become more obvious that outpatient wound care is a critical care need for the community because of the risk of ignoring these chronic wounds and letting them remain open. We cannot let these services be closed down like some were when the pandemic started.”
The study, led by Paola Caruso, MD, of the University of Campania Luigi Vanvitelli in Naples, appeared in Diabetes Care.
The researchers launched the study to understand how patients with diabetes and DFU fared during the height of the pandemic in Italy, where tens of thousands of people died, mainly in the northern region of the country. They focused on patients in the southern region who were admitted to the division of endocrinology and metabolic diseases at the Teaching Hospital at the University of Campania Luigi Vanvitelli.
The study compared 25 patients who were admitted from March 9 to May 18, 2020, with 38 patients who were admitted from a longer period between January and May 2019. The demographics of the groups are similar, with average ages in the early 60s and more men than women (21:4, respectively, in 2020 and 23:15, respectively, in 2019.)
The results reveal high numbers of emergent and serious cases in 2020. Compared with 2019, fewer were outpatients (16% vs. 45%, P = .028) and more were emergency patients (76% vs. 26%, P < .001).
Clinically, gangrene was much more common in the 2020 group, compared with the 2019 group (64% vs. 29%, P = .009), as was amputation (60% vs. 18%, P = .001).
The researchers determined that amputation was more than three times more likely in the 2020 versus the 2019 group (relative risk, 3.26; 95% confidence interval, 1.55-6.84) even though the 2019 period was longer. After adjustment for gender, the heightened risk in 2020 was 2.50 (95% CI, 1.18-5.29).
There was no statistically significant increase in the risk of revascularization.
“The COVID-19 lockdown may have had a detrimental impact on amputation risk because of the sudden interruption of DFU care and lower-limb preservation pathways, resulting in delayed diagnosis and treatment,” the researchers wrote. “DFU is often characterized by progressive clinical course, which can rapidly lead patients to critical worsening of their ulcers.”
They added that “the higher risk of amputation observed during COVID-19 lockdown confirms the need for proper and timely management of DFU patients to prevent dramatic outcomes responsible for a reduction of quality of life and increased morbidity and mortality.”
The study authors didn’t discuss why more patients seemed to have stayed home and not gotten proper care. It’s not clear if they were scared to get treatment or couldn’t obtain it because of the national shutdown.
Both have been factors affecting diabetic foot care in the United States during the pandemic, said Dr. Tettelbach. He called the study “timely and pertinent,” and said it highlights how wound care is “a critical need” that must remain available even when other medical services such as elective surgeries are shut down.
Infection-control protocols such as allowing patients to wait for appointments in their cars instead of waiting rooms will alleviate the fears of certain patients about seeking in-person care during the pandemic, he said. But some patients will be afraid to come in no matter what, he said, and home health may be the best solution for their care.
Several of the study authors reported various disclosures. Dr. Tettelbach reported no relevant disclosures.
SOURCE: Caruso P et al. Diabetes Care. 2020 Jul 23. doi:10.2337/dc20-1347.
Amid a mandatory national lockdown, the rates of amputations skyrocketed at a hospital far from the hardest-hit region as many patients developed gangrene.
The findings offer critical lessons for the United States, said wound care specialist William H. Tettelbach, MD, of Western Peaks Specialty Hospital near Salt Lake City. “It’s become more obvious that outpatient wound care is a critical care need for the community because of the risk of ignoring these chronic wounds and letting them remain open. We cannot let these services be closed down like some were when the pandemic started.”
The study, led by Paola Caruso, MD, of the University of Campania Luigi Vanvitelli in Naples, appeared in Diabetes Care.
The researchers launched the study to understand how patients with diabetes and DFU fared during the height of the pandemic in Italy, where tens of thousands of people died, mainly in the northern region of the country. They focused on patients in the southern region who were admitted to the division of endocrinology and metabolic diseases at the Teaching Hospital at the University of Campania Luigi Vanvitelli.
The study compared 25 patients who were admitted from March 9 to May 18, 2020, with 38 patients who were admitted from a longer period between January and May 2019. The demographics of the groups are similar, with average ages in the early 60s and more men than women (21:4, respectively, in 2020 and 23:15, respectively, in 2019.)
The results reveal high numbers of emergent and serious cases in 2020. Compared with 2019, fewer were outpatients (16% vs. 45%, P = .028) and more were emergency patients (76% vs. 26%, P < .001).
Clinically, gangrene was much more common in the 2020 group, compared with the 2019 group (64% vs. 29%, P = .009), as was amputation (60% vs. 18%, P = .001).
The researchers determined that amputation was more than three times more likely in the 2020 versus the 2019 group (relative risk, 3.26; 95% confidence interval, 1.55-6.84) even though the 2019 period was longer. After adjustment for gender, the heightened risk in 2020 was 2.50 (95% CI, 1.18-5.29).
There was no statistically significant increase in the risk of revascularization.
“The COVID-19 lockdown may have had a detrimental impact on amputation risk because of the sudden interruption of DFU care and lower-limb preservation pathways, resulting in delayed diagnosis and treatment,” the researchers wrote. “DFU is often characterized by progressive clinical course, which can rapidly lead patients to critical worsening of their ulcers.”
They added that “the higher risk of amputation observed during COVID-19 lockdown confirms the need for proper and timely management of DFU patients to prevent dramatic outcomes responsible for a reduction of quality of life and increased morbidity and mortality.”
The study authors didn’t discuss why more patients seemed to have stayed home and not gotten proper care. It’s not clear if they were scared to get treatment or couldn’t obtain it because of the national shutdown.
Both have been factors affecting diabetic foot care in the United States during the pandemic, said Dr. Tettelbach. He called the study “timely and pertinent,” and said it highlights how wound care is “a critical need” that must remain available even when other medical services such as elective surgeries are shut down.
Infection-control protocols such as allowing patients to wait for appointments in their cars instead of waiting rooms will alleviate the fears of certain patients about seeking in-person care during the pandemic, he said. But some patients will be afraid to come in no matter what, he said, and home health may be the best solution for their care.
Several of the study authors reported various disclosures. Dr. Tettelbach reported no relevant disclosures.
SOURCE: Caruso P et al. Diabetes Care. 2020 Jul 23. doi:10.2337/dc20-1347.
Amid a mandatory national lockdown, the rates of amputations skyrocketed at a hospital far from the hardest-hit region as many patients developed gangrene.
The findings offer critical lessons for the United States, said wound care specialist William H. Tettelbach, MD, of Western Peaks Specialty Hospital near Salt Lake City. “It’s become more obvious that outpatient wound care is a critical care need for the community because of the risk of ignoring these chronic wounds and letting them remain open. We cannot let these services be closed down like some were when the pandemic started.”
The study, led by Paola Caruso, MD, of the University of Campania Luigi Vanvitelli in Naples, appeared in Diabetes Care.
The researchers launched the study to understand how patients with diabetes and DFU fared during the height of the pandemic in Italy, where tens of thousands of people died, mainly in the northern region of the country. They focused on patients in the southern region who were admitted to the division of endocrinology and metabolic diseases at the Teaching Hospital at the University of Campania Luigi Vanvitelli.
The study compared 25 patients who were admitted from March 9 to May 18, 2020, with 38 patients who were admitted from a longer period between January and May 2019. The demographics of the groups are similar, with average ages in the early 60s and more men than women (21:4, respectively, in 2020 and 23:15, respectively, in 2019.)
The results reveal high numbers of emergent and serious cases in 2020. Compared with 2019, fewer were outpatients (16% vs. 45%, P = .028) and more were emergency patients (76% vs. 26%, P < .001).
Clinically, gangrene was much more common in the 2020 group, compared with the 2019 group (64% vs. 29%, P = .009), as was amputation (60% vs. 18%, P = .001).
The researchers determined that amputation was more than three times more likely in the 2020 versus the 2019 group (relative risk, 3.26; 95% confidence interval, 1.55-6.84) even though the 2019 period was longer. After adjustment for gender, the heightened risk in 2020 was 2.50 (95% CI, 1.18-5.29).
There was no statistically significant increase in the risk of revascularization.
“The COVID-19 lockdown may have had a detrimental impact on amputation risk because of the sudden interruption of DFU care and lower-limb preservation pathways, resulting in delayed diagnosis and treatment,” the researchers wrote. “DFU is often characterized by progressive clinical course, which can rapidly lead patients to critical worsening of their ulcers.”
They added that “the higher risk of amputation observed during COVID-19 lockdown confirms the need for proper and timely management of DFU patients to prevent dramatic outcomes responsible for a reduction of quality of life and increased morbidity and mortality.”
The study authors didn’t discuss why more patients seemed to have stayed home and not gotten proper care. It’s not clear if they were scared to get treatment or couldn’t obtain it because of the national shutdown.
Both have been factors affecting diabetic foot care in the United States during the pandemic, said Dr. Tettelbach. He called the study “timely and pertinent,” and said it highlights how wound care is “a critical need” that must remain available even when other medical services such as elective surgeries are shut down.
Infection-control protocols such as allowing patients to wait for appointments in their cars instead of waiting rooms will alleviate the fears of certain patients about seeking in-person care during the pandemic, he said. But some patients will be afraid to come in no matter what, he said, and home health may be the best solution for their care.
Several of the study authors reported various disclosures. Dr. Tettelbach reported no relevant disclosures.
SOURCE: Caruso P et al. Diabetes Care. 2020 Jul 23. doi:10.2337/dc20-1347.
FROM DIABETES CARE
Restrictive IV fluid strategy comparable to usual care for severe sepsis, septic shock
Background: Since the advent of early goal-directed therapy (EGDT), studies have challenged the notion that high-volume IV fluid resuscitation improves clinical outcomes in sepsis and septic shock. The optimal IV fluid resuscitation strategy for severe sepsis and septic shock remains unclear.
Study design: Prospective randomized controlled trial.
Setting: Two critical care units in one academic system.
Synopsis: The Restrictive IV Fluid Trial in Severe Sepsis and Septic Shock (RIFTS) randomized 109 participants ages 54-82 years to a restrictive (less than 60 mL/kg) or to usual care (no prespecified limit) IV fluid resuscitation strategy for the first 72 hours of ICU admission. The primary outcome of 30-day mortality was similar between groups (odds ratio, 1.02; 95% confidence interval, 0.41-2.53).
Limitations to RIFTS include its small sample size, single-system design, and inadequate power to detect noninferiority or superiority. While larger, multicenter trials are required for further investigation, hospitalists should note a trend toward conservative IV fluid administration in severe sepsis and septic shock.
Bottom line: Restrictive IV fluid resuscitation for severe sepsis and septic shock may result in mortality rates similar to those of usual care, but larger, multicenter studies are needed to confirm noninferiority.
Citation: Corl KA et al. The restrictive IV fluid trial in severe sepsis and septic shock (RIFTS): A randomized pilot study. Crit Care Med. 2019;47(7):951-9.
Dr. McIntyre is a hospitalist at Ochsner Health System, New Orleans.
Background: Since the advent of early goal-directed therapy (EGDT), studies have challenged the notion that high-volume IV fluid resuscitation improves clinical outcomes in sepsis and septic shock. The optimal IV fluid resuscitation strategy for severe sepsis and septic shock remains unclear.
Study design: Prospective randomized controlled trial.
Setting: Two critical care units in one academic system.
Synopsis: The Restrictive IV Fluid Trial in Severe Sepsis and Septic Shock (RIFTS) randomized 109 participants ages 54-82 years to a restrictive (less than 60 mL/kg) or to usual care (no prespecified limit) IV fluid resuscitation strategy for the first 72 hours of ICU admission. The primary outcome of 30-day mortality was similar between groups (odds ratio, 1.02; 95% confidence interval, 0.41-2.53).
Limitations to RIFTS include its small sample size, single-system design, and inadequate power to detect noninferiority or superiority. While larger, multicenter trials are required for further investigation, hospitalists should note a trend toward conservative IV fluid administration in severe sepsis and septic shock.
Bottom line: Restrictive IV fluid resuscitation for severe sepsis and septic shock may result in mortality rates similar to those of usual care, but larger, multicenter studies are needed to confirm noninferiority.
Citation: Corl KA et al. The restrictive IV fluid trial in severe sepsis and septic shock (RIFTS): A randomized pilot study. Crit Care Med. 2019;47(7):951-9.
Dr. McIntyre is a hospitalist at Ochsner Health System, New Orleans.
Background: Since the advent of early goal-directed therapy (EGDT), studies have challenged the notion that high-volume IV fluid resuscitation improves clinical outcomes in sepsis and septic shock. The optimal IV fluid resuscitation strategy for severe sepsis and septic shock remains unclear.
Study design: Prospective randomized controlled trial.
Setting: Two critical care units in one academic system.
Synopsis: The Restrictive IV Fluid Trial in Severe Sepsis and Septic Shock (RIFTS) randomized 109 participants ages 54-82 years to a restrictive (less than 60 mL/kg) or to usual care (no prespecified limit) IV fluid resuscitation strategy for the first 72 hours of ICU admission. The primary outcome of 30-day mortality was similar between groups (odds ratio, 1.02; 95% confidence interval, 0.41-2.53).
Limitations to RIFTS include its small sample size, single-system design, and inadequate power to detect noninferiority or superiority. While larger, multicenter trials are required for further investigation, hospitalists should note a trend toward conservative IV fluid administration in severe sepsis and septic shock.
Bottom line: Restrictive IV fluid resuscitation for severe sepsis and septic shock may result in mortality rates similar to those of usual care, but larger, multicenter studies are needed to confirm noninferiority.
Citation: Corl KA et al. The restrictive IV fluid trial in severe sepsis and septic shock (RIFTS): A randomized pilot study. Crit Care Med. 2019;47(7):951-9.
Dr. McIntyre is a hospitalist at Ochsner Health System, New Orleans.
Twelve risk factors linked to 40% of world’s dementia cases
according to an update of the Lancet Commission on Dementia Prevention, Intervention, and Care.
The original report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one-third of dementia cases. The commission has now added three new modifiable risk factors to the list.
“We reconvened the 2017 Lancet Commission on Dementia Prevention, Intervention, and Care to identify the evidence for advances likely to have the greatest impact since our 2017 paper,” the authors wrote.
The 2020 report was presented at the virtual annual meeting of the Alzheimer’s Association International Conference (AAIC) 2020 and also was published online July 30 in the Lancet.
Alcohol, TBI, air pollution
The three new risk factors that have been added in the latest update are excessive alcohol intake, traumatic brain injury (TBI), and air pollution. The original nine risk factors were not completing secondary education; hypertension; obesity; hearing loss; smoking; depression; physical inactivity; social isolation; and diabetes. Together, these 12 risk factors are estimated to account for 40% of the world’s dementia cases.
“We knew in 2017 when we published our first report with the nine risk factors that they would only be part of the story and that several other factors would likely be involved,” said lead author Gill Livingston, MD, professor, University College London (England). “We now have more published data giving enough evidence” to justify adding the three new factors to the list, she said.
The report includes the following nine recommendations for policymakers and individuals to prevent risk for dementia in the general population:
- Aim to maintain systolic blood pressure of 130 mm Hg or less in midlife from around age 40 years.
- Encourage use of hearing aids for hearing loss, and reduce hearing loss by protecting ears from high noise levels.
- Reduce exposure to air pollution and second-hand tobacco smoke.
- Prevent , particularly by targeting high-risk occupations and transport.
- Prevent alcohol misuse and limit drinking to less than 21 units per week.
- Stop smoking and support individuals to stop smoking, which the authors stress is beneficial at any age.
- Provide all children with primary and secondary education.
- Lead an active life into midlife and possibly later life.
- Reduce obesity and diabetes.
The report also summarizes the evidence supporting the three new risk factors for dementia.
TBI is usually caused by car, motorcycle, and bicycle injuries; military exposures; boxing, horse riding, and other recreational sports; firearms; and falls. The report notes that a single severe TBI is associated in humans and in mouse models with widespread hyperphosphorylated tau pathology. It also cites several nationwide studies that show that TBI is linked with a significantly increased risk for long-term dementia.
“We are not advising against partaking in sports, as playing sports is healthy. But we are urging people to take precautions to protect themselves properly,” Dr. Livingston said.
For excessive alcohol consumption, the report states that an “increasing body of evidence is emerging on alcohol’s complex relationship with cognition and dementia outcomes from a variety of sources including detailed cohorts and large-scale record-based studies.” One French study, which included more than 31 million individuals admitted to the hospital, showed that alcohol use disorders were associated with a threefold increased dementia risk. However, other studies have suggested that moderate drinking may be protective.
“We are not saying it is bad to drink, but we are saying it is bad to drink more than 21 units a week,” Dr. Livingston noted.
On air pollution, the report notes that in animal studies, airborne particulate pollutants have been found to accelerate neurodegenerative processes. Also, high nitrogen dioxide concentrations, fine ambient particulate matter from traffic exhaust, and residential wood burning have been shown in past research to be associated with increased dementia incidence.
“While we need international policy on reducing air pollution, individuals can take some action to reduce their risk,” Dr. Livingston said. For example, she suggested avoiding walking right next to busy roads and instead walking “a few streets back if possible.”
Hearing loss
The researchers assessed how much each risk factor contributes to dementia, expressed as the population-attributable fraction (PAF). Hearing loss had the greatest effect, accounting for an estimated 8.2% of dementia cases. This was followed by lower education levels in young people (7.1%) and smoking (5.2%).
Dr. Livingston noted that the evidence that hearing loss is one of the most important risk factors for dementia is very strong. New studies show that correcting hearing loss with hearing aids negates any increased risk.
Hearing loss “has both a high relative risk for dementia and is a common problem, so it contributes a significant amount to dementia cases. This is really something that we can reduce relatively easily by encouraging use of hearing aids. They need to be made more accessible, more comfortable, and more acceptable,” she said.
“This could make a huge difference in reducing dementia cases in the future,” Dr. Livingston added.
Other risk factors for which the evidence base has strengthened since the 2017 report include systolic blood pressure, social interaction, and early-life education.
Dr. Livingston noted that the SPRINT MIND trial showed that aiming for a target systolic blood pressure of 120 mm Hg reduced risk for future mild cognitive impairment. “Before, we thought under 140 was the target, but now are recommending under 130 to reduce risks of dementia,” she said.
Evidence on social interaction “has been very consistent, and we now have more certainty on this. It is now well established that increased social interaction in midlife reduces dementia in late life,” said Dr. Livingston.
On the benefits of education in the young, she noted that it has been known for some time that education for individuals younger than 11 years is important in reducing later-life dementia. However, it is now thought that education to the age of 20 also makes a difference.
“While keeping the brain active in later years has some positive effects, increasing brain activity in young people seems to be more important. This is probably because of the better plasticity of the brain in the young,” she said.
Sleep and diet
Two risk factors that have not made it onto the list are diet and sleep. “While there has also been a lot more data published on nutrition and sleep with regard to dementia in the last few years, we didn’t think the evidence stacked up enough to include these on the list of modifiable risk factors,” Dr. Livingston said.
The report cites studies that suggest that both more sleep and less sleep are associated with increased risk for dementia, which the authors thought did not make “biological sense.” In addition, other underlying factors involved in sleep, such as depression, apathy, and different sleep patterns, may be symptoms of early dementia.
More data have been published on diet and dementia, “but there isn’t any individual vitamin deficit that is associated with the condition. The evidence is quite clear on that,” Dr. Livingston said. “Global diets, such as the Mediterranean or Nordic diets, can probably make a difference, but there doesn’t seem to be any one particular element that is needed,” she noted.
“We just recommend to eat a healthy diet and stay a healthy weight. Diet is very connected to economic circumstances and so very difficult to separate out as a risk factor. We do think it is linked, but we are not convinced enough to put it in the model,” she added.
Among other key information that has become available since 2017, Dr. Livingston highlighted new data showing that dementia is more common in less privileged populations, including Black and minority ethnic groups and low- and middle-income countries.
Although dementia was traditionally considered a disease of high-income countries, that has now been shown not to be the case. “People in low- and middle-income countries are now living longer and so are developing dementia more, and they have higher rates of many of the risk factors, including smoking and low education levels. There is a huge potential for prevention in these countries,” said Dr. Livingston.
She also highlighted new evidence showing that patients with dementia do not do well when admitted to the hospital. “So we need to do more to keep them well at home,” she said.
COVID-19 advice
The report also has a section on COVID-19. It points out that patients with dementia are particularly vulnerable to the disease because of their age, multimorbidities, and difficulties in maintaining physical distancing. Death certificates from the United Kingdom indicate that dementia and Alzheimer’s disease were the most common underlying conditions (present in 25.6% of all deaths involving COVID-19).
The situation is particularly concerning in care homes. In one U.S. study, nursing home residents living with dementia made up 52% of COVID-19 cases, yet they accounted for 72% of all deaths (increased risk, 1.7), the commission reported.
The authors recommended rigorous public health measures, such as protective equipment and hygiene, not moving staff or residents between care homes, and not admitting new residents when their COVID-19 status is unknown. The report also recommends regular testing of staff in care homes and the provision of oxygen therapy at the home to avoid hospital admission.
It is also important to reduce isolation by providing the necessary equipment to relatives and offering them brief training on how to protect themselves and others from COVID-19 so that they can visit their relatives with dementia in nursing homes safely when it is allowed.
“Most comprehensive overview to date”
Alzheimer’s Research UK welcomed the new report. “This is the most comprehensive overview into dementia risk to date, building on previous work by this commission and moving our understanding forward,” Rosa Sancho, PhD, head of research at the charity, said.
“This report underlines the importance of acting at a personal and policy level to reduce dementia risk. With Alzheimer’s Research UK’s Dementia Attitudes Monitor showing just a third of people think it’s possible to reduce their risk of developing dementia, there’s clearly much to do here to increase people’s awareness of the steps they can take,” Dr. Sancho said.
She added that, although there is “no surefire way of preventing dementia,” the best way to keep a brain healthy as it ages is for an individual to stay physically and mentally active, eat a healthy balanced diet, not smoke, drink only within the recommended limits, and keep weight, cholesterol level, and blood pressure in check. “With no treatments yet able to slow or stop the onset of dementia, taking action to reduce these risks is an important part of our strategy for tackling the condition,” Dr. Sancho said.
The Lancet Commission is partnered by University College London, the Alzheimer’s Society UK, the Economic and Social Research Council, and Alzheimer’s Research UK, which funded fares, accommodation, and food for the commission meeting but had no role in the writing of the manuscript or the decision to submit it for publication.
A version of this article originally appeared on Medscape.com.
according to an update of the Lancet Commission on Dementia Prevention, Intervention, and Care.
The original report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one-third of dementia cases. The commission has now added three new modifiable risk factors to the list.
“We reconvened the 2017 Lancet Commission on Dementia Prevention, Intervention, and Care to identify the evidence for advances likely to have the greatest impact since our 2017 paper,” the authors wrote.
The 2020 report was presented at the virtual annual meeting of the Alzheimer’s Association International Conference (AAIC) 2020 and also was published online July 30 in the Lancet.
Alcohol, TBI, air pollution
The three new risk factors that have been added in the latest update are excessive alcohol intake, traumatic brain injury (TBI), and air pollution. The original nine risk factors were not completing secondary education; hypertension; obesity; hearing loss; smoking; depression; physical inactivity; social isolation; and diabetes. Together, these 12 risk factors are estimated to account for 40% of the world’s dementia cases.
“We knew in 2017 when we published our first report with the nine risk factors that they would only be part of the story and that several other factors would likely be involved,” said lead author Gill Livingston, MD, professor, University College London (England). “We now have more published data giving enough evidence” to justify adding the three new factors to the list, she said.
The report includes the following nine recommendations for policymakers and individuals to prevent risk for dementia in the general population:
- Aim to maintain systolic blood pressure of 130 mm Hg or less in midlife from around age 40 years.
- Encourage use of hearing aids for hearing loss, and reduce hearing loss by protecting ears from high noise levels.
- Reduce exposure to air pollution and second-hand tobacco smoke.
- Prevent , particularly by targeting high-risk occupations and transport.
- Prevent alcohol misuse and limit drinking to less than 21 units per week.
- Stop smoking and support individuals to stop smoking, which the authors stress is beneficial at any age.
- Provide all children with primary and secondary education.
- Lead an active life into midlife and possibly later life.
- Reduce obesity and diabetes.
The report also summarizes the evidence supporting the three new risk factors for dementia.
TBI is usually caused by car, motorcycle, and bicycle injuries; military exposures; boxing, horse riding, and other recreational sports; firearms; and falls. The report notes that a single severe TBI is associated in humans and in mouse models with widespread hyperphosphorylated tau pathology. It also cites several nationwide studies that show that TBI is linked with a significantly increased risk for long-term dementia.
“We are not advising against partaking in sports, as playing sports is healthy. But we are urging people to take precautions to protect themselves properly,” Dr. Livingston said.
For excessive alcohol consumption, the report states that an “increasing body of evidence is emerging on alcohol’s complex relationship with cognition and dementia outcomes from a variety of sources including detailed cohorts and large-scale record-based studies.” One French study, which included more than 31 million individuals admitted to the hospital, showed that alcohol use disorders were associated with a threefold increased dementia risk. However, other studies have suggested that moderate drinking may be protective.
“We are not saying it is bad to drink, but we are saying it is bad to drink more than 21 units a week,” Dr. Livingston noted.
On air pollution, the report notes that in animal studies, airborne particulate pollutants have been found to accelerate neurodegenerative processes. Also, high nitrogen dioxide concentrations, fine ambient particulate matter from traffic exhaust, and residential wood burning have been shown in past research to be associated with increased dementia incidence.
“While we need international policy on reducing air pollution, individuals can take some action to reduce their risk,” Dr. Livingston said. For example, she suggested avoiding walking right next to busy roads and instead walking “a few streets back if possible.”
Hearing loss
The researchers assessed how much each risk factor contributes to dementia, expressed as the population-attributable fraction (PAF). Hearing loss had the greatest effect, accounting for an estimated 8.2% of dementia cases. This was followed by lower education levels in young people (7.1%) and smoking (5.2%).
Dr. Livingston noted that the evidence that hearing loss is one of the most important risk factors for dementia is very strong. New studies show that correcting hearing loss with hearing aids negates any increased risk.
Hearing loss “has both a high relative risk for dementia and is a common problem, so it contributes a significant amount to dementia cases. This is really something that we can reduce relatively easily by encouraging use of hearing aids. They need to be made more accessible, more comfortable, and more acceptable,” she said.
“This could make a huge difference in reducing dementia cases in the future,” Dr. Livingston added.
Other risk factors for which the evidence base has strengthened since the 2017 report include systolic blood pressure, social interaction, and early-life education.
Dr. Livingston noted that the SPRINT MIND trial showed that aiming for a target systolic blood pressure of 120 mm Hg reduced risk for future mild cognitive impairment. “Before, we thought under 140 was the target, but now are recommending under 130 to reduce risks of dementia,” she said.
Evidence on social interaction “has been very consistent, and we now have more certainty on this. It is now well established that increased social interaction in midlife reduces dementia in late life,” said Dr. Livingston.
On the benefits of education in the young, she noted that it has been known for some time that education for individuals younger than 11 years is important in reducing later-life dementia. However, it is now thought that education to the age of 20 also makes a difference.
“While keeping the brain active in later years has some positive effects, increasing brain activity in young people seems to be more important. This is probably because of the better plasticity of the brain in the young,” she said.
Sleep and diet
Two risk factors that have not made it onto the list are diet and sleep. “While there has also been a lot more data published on nutrition and sleep with regard to dementia in the last few years, we didn’t think the evidence stacked up enough to include these on the list of modifiable risk factors,” Dr. Livingston said.
The report cites studies that suggest that both more sleep and less sleep are associated with increased risk for dementia, which the authors thought did not make “biological sense.” In addition, other underlying factors involved in sleep, such as depression, apathy, and different sleep patterns, may be symptoms of early dementia.
More data have been published on diet and dementia, “but there isn’t any individual vitamin deficit that is associated with the condition. The evidence is quite clear on that,” Dr. Livingston said. “Global diets, such as the Mediterranean or Nordic diets, can probably make a difference, but there doesn’t seem to be any one particular element that is needed,” she noted.
“We just recommend to eat a healthy diet and stay a healthy weight. Diet is very connected to economic circumstances and so very difficult to separate out as a risk factor. We do think it is linked, but we are not convinced enough to put it in the model,” she added.
Among other key information that has become available since 2017, Dr. Livingston highlighted new data showing that dementia is more common in less privileged populations, including Black and minority ethnic groups and low- and middle-income countries.
Although dementia was traditionally considered a disease of high-income countries, that has now been shown not to be the case. “People in low- and middle-income countries are now living longer and so are developing dementia more, and they have higher rates of many of the risk factors, including smoking and low education levels. There is a huge potential for prevention in these countries,” said Dr. Livingston.
She also highlighted new evidence showing that patients with dementia do not do well when admitted to the hospital. “So we need to do more to keep them well at home,” she said.
COVID-19 advice
The report also has a section on COVID-19. It points out that patients with dementia are particularly vulnerable to the disease because of their age, multimorbidities, and difficulties in maintaining physical distancing. Death certificates from the United Kingdom indicate that dementia and Alzheimer’s disease were the most common underlying conditions (present in 25.6% of all deaths involving COVID-19).
The situation is particularly concerning in care homes. In one U.S. study, nursing home residents living with dementia made up 52% of COVID-19 cases, yet they accounted for 72% of all deaths (increased risk, 1.7), the commission reported.
The authors recommended rigorous public health measures, such as protective equipment and hygiene, not moving staff or residents between care homes, and not admitting new residents when their COVID-19 status is unknown. The report also recommends regular testing of staff in care homes and the provision of oxygen therapy at the home to avoid hospital admission.
It is also important to reduce isolation by providing the necessary equipment to relatives and offering them brief training on how to protect themselves and others from COVID-19 so that they can visit their relatives with dementia in nursing homes safely when it is allowed.
“Most comprehensive overview to date”
Alzheimer’s Research UK welcomed the new report. “This is the most comprehensive overview into dementia risk to date, building on previous work by this commission and moving our understanding forward,” Rosa Sancho, PhD, head of research at the charity, said.
“This report underlines the importance of acting at a personal and policy level to reduce dementia risk. With Alzheimer’s Research UK’s Dementia Attitudes Monitor showing just a third of people think it’s possible to reduce their risk of developing dementia, there’s clearly much to do here to increase people’s awareness of the steps they can take,” Dr. Sancho said.
She added that, although there is “no surefire way of preventing dementia,” the best way to keep a brain healthy as it ages is for an individual to stay physically and mentally active, eat a healthy balanced diet, not smoke, drink only within the recommended limits, and keep weight, cholesterol level, and blood pressure in check. “With no treatments yet able to slow or stop the onset of dementia, taking action to reduce these risks is an important part of our strategy for tackling the condition,” Dr. Sancho said.
The Lancet Commission is partnered by University College London, the Alzheimer’s Society UK, the Economic and Social Research Council, and Alzheimer’s Research UK, which funded fares, accommodation, and food for the commission meeting but had no role in the writing of the manuscript or the decision to submit it for publication.
A version of this article originally appeared on Medscape.com.
according to an update of the Lancet Commission on Dementia Prevention, Intervention, and Care.
The original report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one-third of dementia cases. The commission has now added three new modifiable risk factors to the list.
“We reconvened the 2017 Lancet Commission on Dementia Prevention, Intervention, and Care to identify the evidence for advances likely to have the greatest impact since our 2017 paper,” the authors wrote.
The 2020 report was presented at the virtual annual meeting of the Alzheimer’s Association International Conference (AAIC) 2020 and also was published online July 30 in the Lancet.
Alcohol, TBI, air pollution
The three new risk factors that have been added in the latest update are excessive alcohol intake, traumatic brain injury (TBI), and air pollution. The original nine risk factors were not completing secondary education; hypertension; obesity; hearing loss; smoking; depression; physical inactivity; social isolation; and diabetes. Together, these 12 risk factors are estimated to account for 40% of the world’s dementia cases.
“We knew in 2017 when we published our first report with the nine risk factors that they would only be part of the story and that several other factors would likely be involved,” said lead author Gill Livingston, MD, professor, University College London (England). “We now have more published data giving enough evidence” to justify adding the three new factors to the list, she said.
The report includes the following nine recommendations for policymakers and individuals to prevent risk for dementia in the general population:
- Aim to maintain systolic blood pressure of 130 mm Hg or less in midlife from around age 40 years.
- Encourage use of hearing aids for hearing loss, and reduce hearing loss by protecting ears from high noise levels.
- Reduce exposure to air pollution and second-hand tobacco smoke.
- Prevent , particularly by targeting high-risk occupations and transport.
- Prevent alcohol misuse and limit drinking to less than 21 units per week.
- Stop smoking and support individuals to stop smoking, which the authors stress is beneficial at any age.
- Provide all children with primary and secondary education.
- Lead an active life into midlife and possibly later life.
- Reduce obesity and diabetes.
The report also summarizes the evidence supporting the three new risk factors for dementia.
TBI is usually caused by car, motorcycle, and bicycle injuries; military exposures; boxing, horse riding, and other recreational sports; firearms; and falls. The report notes that a single severe TBI is associated in humans and in mouse models with widespread hyperphosphorylated tau pathology. It also cites several nationwide studies that show that TBI is linked with a significantly increased risk for long-term dementia.
“We are not advising against partaking in sports, as playing sports is healthy. But we are urging people to take precautions to protect themselves properly,” Dr. Livingston said.
For excessive alcohol consumption, the report states that an “increasing body of evidence is emerging on alcohol’s complex relationship with cognition and dementia outcomes from a variety of sources including detailed cohorts and large-scale record-based studies.” One French study, which included more than 31 million individuals admitted to the hospital, showed that alcohol use disorders were associated with a threefold increased dementia risk. However, other studies have suggested that moderate drinking may be protective.
“We are not saying it is bad to drink, but we are saying it is bad to drink more than 21 units a week,” Dr. Livingston noted.
On air pollution, the report notes that in animal studies, airborne particulate pollutants have been found to accelerate neurodegenerative processes. Also, high nitrogen dioxide concentrations, fine ambient particulate matter from traffic exhaust, and residential wood burning have been shown in past research to be associated with increased dementia incidence.
“While we need international policy on reducing air pollution, individuals can take some action to reduce their risk,” Dr. Livingston said. For example, she suggested avoiding walking right next to busy roads and instead walking “a few streets back if possible.”
Hearing loss
The researchers assessed how much each risk factor contributes to dementia, expressed as the population-attributable fraction (PAF). Hearing loss had the greatest effect, accounting for an estimated 8.2% of dementia cases. This was followed by lower education levels in young people (7.1%) and smoking (5.2%).
Dr. Livingston noted that the evidence that hearing loss is one of the most important risk factors for dementia is very strong. New studies show that correcting hearing loss with hearing aids negates any increased risk.
Hearing loss “has both a high relative risk for dementia and is a common problem, so it contributes a significant amount to dementia cases. This is really something that we can reduce relatively easily by encouraging use of hearing aids. They need to be made more accessible, more comfortable, and more acceptable,” she said.
“This could make a huge difference in reducing dementia cases in the future,” Dr. Livingston added.
Other risk factors for which the evidence base has strengthened since the 2017 report include systolic blood pressure, social interaction, and early-life education.
Dr. Livingston noted that the SPRINT MIND trial showed that aiming for a target systolic blood pressure of 120 mm Hg reduced risk for future mild cognitive impairment. “Before, we thought under 140 was the target, but now are recommending under 130 to reduce risks of dementia,” she said.
Evidence on social interaction “has been very consistent, and we now have more certainty on this. It is now well established that increased social interaction in midlife reduces dementia in late life,” said Dr. Livingston.
On the benefits of education in the young, she noted that it has been known for some time that education for individuals younger than 11 years is important in reducing later-life dementia. However, it is now thought that education to the age of 20 also makes a difference.
“While keeping the brain active in later years has some positive effects, increasing brain activity in young people seems to be more important. This is probably because of the better plasticity of the brain in the young,” she said.
Sleep and diet
Two risk factors that have not made it onto the list are diet and sleep. “While there has also been a lot more data published on nutrition and sleep with regard to dementia in the last few years, we didn’t think the evidence stacked up enough to include these on the list of modifiable risk factors,” Dr. Livingston said.
The report cites studies that suggest that both more sleep and less sleep are associated with increased risk for dementia, which the authors thought did not make “biological sense.” In addition, other underlying factors involved in sleep, such as depression, apathy, and different sleep patterns, may be symptoms of early dementia.
More data have been published on diet and dementia, “but there isn’t any individual vitamin deficit that is associated with the condition. The evidence is quite clear on that,” Dr. Livingston said. “Global diets, such as the Mediterranean or Nordic diets, can probably make a difference, but there doesn’t seem to be any one particular element that is needed,” she noted.
“We just recommend to eat a healthy diet and stay a healthy weight. Diet is very connected to economic circumstances and so very difficult to separate out as a risk factor. We do think it is linked, but we are not convinced enough to put it in the model,” she added.
Among other key information that has become available since 2017, Dr. Livingston highlighted new data showing that dementia is more common in less privileged populations, including Black and minority ethnic groups and low- and middle-income countries.
Although dementia was traditionally considered a disease of high-income countries, that has now been shown not to be the case. “People in low- and middle-income countries are now living longer and so are developing dementia more, and they have higher rates of many of the risk factors, including smoking and low education levels. There is a huge potential for prevention in these countries,” said Dr. Livingston.
She also highlighted new evidence showing that patients with dementia do not do well when admitted to the hospital. “So we need to do more to keep them well at home,” she said.
COVID-19 advice
The report also has a section on COVID-19. It points out that patients with dementia are particularly vulnerable to the disease because of their age, multimorbidities, and difficulties in maintaining physical distancing. Death certificates from the United Kingdom indicate that dementia and Alzheimer’s disease were the most common underlying conditions (present in 25.6% of all deaths involving COVID-19).
The situation is particularly concerning in care homes. In one U.S. study, nursing home residents living with dementia made up 52% of COVID-19 cases, yet they accounted for 72% of all deaths (increased risk, 1.7), the commission reported.
The authors recommended rigorous public health measures, such as protective equipment and hygiene, not moving staff or residents between care homes, and not admitting new residents when their COVID-19 status is unknown. The report also recommends regular testing of staff in care homes and the provision of oxygen therapy at the home to avoid hospital admission.
It is also important to reduce isolation by providing the necessary equipment to relatives and offering them brief training on how to protect themselves and others from COVID-19 so that they can visit their relatives with dementia in nursing homes safely when it is allowed.
“Most comprehensive overview to date”
Alzheimer’s Research UK welcomed the new report. “This is the most comprehensive overview into dementia risk to date, building on previous work by this commission and moving our understanding forward,” Rosa Sancho, PhD, head of research at the charity, said.
“This report underlines the importance of acting at a personal and policy level to reduce dementia risk. With Alzheimer’s Research UK’s Dementia Attitudes Monitor showing just a third of people think it’s possible to reduce their risk of developing dementia, there’s clearly much to do here to increase people’s awareness of the steps they can take,” Dr. Sancho said.
She added that, although there is “no surefire way of preventing dementia,” the best way to keep a brain healthy as it ages is for an individual to stay physically and mentally active, eat a healthy balanced diet, not smoke, drink only within the recommended limits, and keep weight, cholesterol level, and blood pressure in check. “With no treatments yet able to slow or stop the onset of dementia, taking action to reduce these risks is an important part of our strategy for tackling the condition,” Dr. Sancho said.
The Lancet Commission is partnered by University College London, the Alzheimer’s Society UK, the Economic and Social Research Council, and Alzheimer’s Research UK, which funded fares, accommodation, and food for the commission meeting but had no role in the writing of the manuscript or the decision to submit it for publication.
A version of this article originally appeared on Medscape.com.
From AAIC 2020
Don’t discount discharge planning during pandemic
The COVID-19 pandemic continues to disrupt all aspects of hospital care, and has altered nearly all fundamental practices, including discharge protocols. A session presented at the Society of Hospitalist Medicine’s 2020 Virtual Annual Conference will focus on discharge issues in the COVID-19 era.
“Discharge planning is an integral part of a hospitalist’s clinical care. On a daily basis, we think carefully about how to help our patients safely transition back into life outside of the hospital,” said Maralyssa Bann, MD, of the University of Washington, Seattle, a copresenter at the session.
“Patients need up-to-date information about how to keep themselves and those around them safe,” she said. “They need resources and supports to help them recover from illness.”
These supports include access to appropriate follow-up with primary care doctors or other specialists and being discharged to the right location, such as home or a skilled nursing facility, Dr. Bann noted.
In response to COVID-19, “within an exceptionally short time frame, hospitals have had to rapidly adapt their discharge planning protocols and have had to continue to adapt as new information comes out,” Dr. Bann said.
“In many ways, the COVID-19 pandemic has highlighted the importance of discharge planning for patient care and has added a new element of public health in that we have to take all possible precautions to ensure that patients are not spreading the virus after they leave the hospital,” said Ryan Greysen, MD, of the University of Pennsylvania, Philadelphia, and Dr. Bann’s copresenter.
Many elements go into creating a good discharge plan, but there are often many unknowns, Dr. Greysen said. “I think there is an opportunity to improve the process by improving follow-up as well.”
“For example, one program at our hospital focused on vulnerable older adults includes an in-home visit by a visiting nurse on the day of discharge to verify the patient has everything they need when they arrive home,” However, now with more telemedicine and social distancing, there should be creative approaches to tying up loose ends and monitoring for things that can go wrong in order to give additional guidance, he said.
“In a previous study of 12 U.S. academic medical centers, my colleagues and I interviewed over 1,000 patients who were discharged and then readmitted to ask them what they thought went wrong,” said Dr. Greysen. “Overwhelmingly, patients indicated that they understood their discharge instructions and the plan of care at the time they left the hospital, but then when there were breakdowns or unanticipated challenges in the plan, they were uncertain what to do.”
In the HM20 Virtual session, Dr. Greysen and Dr. Bann will present additional data from the same network that Dr. Greysen used in his study, the Hospital Medicine Reengineering Network or HOMERuN, but expanded to include 22 sites.
The specific areas will include clinical and nonclinical criteria for patients to be discharged home, how criteria differed for discharge destinations other than home, discharge logistics, discharge instructions for patients and caregivers, and postdischarge follow-up.
“Developing a discharge protocol during a pandemic is a major challenge. There are new barriers and challenges to finding the right discharge location, as information about illness course and outcome is incomplete or evolving,” Dr. Bann said. “The safety of patients and their loved ones, health care workers and staff, as well as the public at large is always top of mind. Decisions have to be made in a timely way and communicated clearly. This is a huge task in addition to all of the other competing work in the midst of a pandemic, which is why learning from each other and collectively creating our shared best practices is tremendously helpful. If I can take example approaches from other hospitals and update them for use at my site, this saves a lot of time and effort.”
“There is great urgency to understand when it is safe to discharge these patients from the hospital,” Dr. Greysen said. “Many COVID patients can have worsening of their symptoms after a period of initial improvement so sending them home too soon is a major concern. On the other hand, we can’t keep COVID patients in the hospital until they have fully recovered; we would increase their risk of iatrogenic events and we could risk using up capacity of the health care system to care for other patients, both COVID and non-COVID.”
Unfortunately, no evidence base yet exists to guide the creation of discharge guidelines for COVID patients, said Dr. Greysen. “Therefore, we conducted a survey of HOMERuN sites to synthesize practices across sites and provide some guidance for hospitals based on themes or concordance between these sites.
“One area of clear concordance among sites in our study was around the use of [Centers for Disease Control and Prevention] guidelines to address patient isolation procedures as well as strategies to mitigate transmission, such as providing patients with protective gear like masks or requiring the driver who picks up the patient wear a mask for transportation,” Dr. Greysen said. “We also found that many sites used certain clinical criteria – for example, temperature, oxygen saturation or supplementation, and improvement of presenting symptoms – but there was wide variation in the details for these criteria.”
In addition, “some sites required that a patient be afebrile for a certain period of time before discharge whereas others only required that patients be afebrile at the time of discharge. There was also relatively strong consensus around assessing the level of social support and ability to perform activities of daily living prior to discharge,” since social support and ability to function are often interrelated and can be difficult to assess without visiting the home, he said.
“Further development the evidence around which discharge criteria are associated with adverse outcomes such as readmission or death is urgently needed. At this moment, we really don’t know which clinical criteria such as oxygen supplementation or nonclinical criteria are associated with better outcomes in COVID patients,” Dr. Greysen said, but he and his team plan to study this using EMR data in HOMERuN.
Dr. Bann said that clinical criteria for discharge will likely provoke lively discussions during the interactive part of the virtual session. “Also, I have heard a lot of discussion and interest in learning about how different sites are handling postdischarge monitoring and follow-up, such as how we ensure that patients are recovering well after discharge, and whether there are new or different needs for this patient population,” she added.
“Attendees should come away from this session with an understanding of how hospitals across the country have augmented their discharge planning responses during the COVID-19 pandemic,” Dr. Bann said. “This session is all about learning from each other and creating shared best practices,” she said.
“I hope that those who attend our session are able to see some areas of consensus in our study that could be applied to their discharge criteria,” Dr. Greysen added.
Dr. Bann and Dr. Greysen had no relevant financial conflicts to disclose.
Discharge Planning for COVID-19: Collected Practices from Across the U.S.
The COVID-19 pandemic continues to disrupt all aspects of hospital care, and has altered nearly all fundamental practices, including discharge protocols. A session presented at the Society of Hospitalist Medicine’s 2020 Virtual Annual Conference will focus on discharge issues in the COVID-19 era.
“Discharge planning is an integral part of a hospitalist’s clinical care. On a daily basis, we think carefully about how to help our patients safely transition back into life outside of the hospital,” said Maralyssa Bann, MD, of the University of Washington, Seattle, a copresenter at the session.
“Patients need up-to-date information about how to keep themselves and those around them safe,” she said. “They need resources and supports to help them recover from illness.”
These supports include access to appropriate follow-up with primary care doctors or other specialists and being discharged to the right location, such as home or a skilled nursing facility, Dr. Bann noted.
In response to COVID-19, “within an exceptionally short time frame, hospitals have had to rapidly adapt their discharge planning protocols and have had to continue to adapt as new information comes out,” Dr. Bann said.
“In many ways, the COVID-19 pandemic has highlighted the importance of discharge planning for patient care and has added a new element of public health in that we have to take all possible precautions to ensure that patients are not spreading the virus after they leave the hospital,” said Ryan Greysen, MD, of the University of Pennsylvania, Philadelphia, and Dr. Bann’s copresenter.
Many elements go into creating a good discharge plan, but there are often many unknowns, Dr. Greysen said. “I think there is an opportunity to improve the process by improving follow-up as well.”
“For example, one program at our hospital focused on vulnerable older adults includes an in-home visit by a visiting nurse on the day of discharge to verify the patient has everything they need when they arrive home,” However, now with more telemedicine and social distancing, there should be creative approaches to tying up loose ends and monitoring for things that can go wrong in order to give additional guidance, he said.
“In a previous study of 12 U.S. academic medical centers, my colleagues and I interviewed over 1,000 patients who were discharged and then readmitted to ask them what they thought went wrong,” said Dr. Greysen. “Overwhelmingly, patients indicated that they understood their discharge instructions and the plan of care at the time they left the hospital, but then when there were breakdowns or unanticipated challenges in the plan, they were uncertain what to do.”
In the HM20 Virtual session, Dr. Greysen and Dr. Bann will present additional data from the same network that Dr. Greysen used in his study, the Hospital Medicine Reengineering Network or HOMERuN, but expanded to include 22 sites.
The specific areas will include clinical and nonclinical criteria for patients to be discharged home, how criteria differed for discharge destinations other than home, discharge logistics, discharge instructions for patients and caregivers, and postdischarge follow-up.
“Developing a discharge protocol during a pandemic is a major challenge. There are new barriers and challenges to finding the right discharge location, as information about illness course and outcome is incomplete or evolving,” Dr. Bann said. “The safety of patients and their loved ones, health care workers and staff, as well as the public at large is always top of mind. Decisions have to be made in a timely way and communicated clearly. This is a huge task in addition to all of the other competing work in the midst of a pandemic, which is why learning from each other and collectively creating our shared best practices is tremendously helpful. If I can take example approaches from other hospitals and update them for use at my site, this saves a lot of time and effort.”
“There is great urgency to understand when it is safe to discharge these patients from the hospital,” Dr. Greysen said. “Many COVID patients can have worsening of their symptoms after a period of initial improvement so sending them home too soon is a major concern. On the other hand, we can’t keep COVID patients in the hospital until they have fully recovered; we would increase their risk of iatrogenic events and we could risk using up capacity of the health care system to care for other patients, both COVID and non-COVID.”
Unfortunately, no evidence base yet exists to guide the creation of discharge guidelines for COVID patients, said Dr. Greysen. “Therefore, we conducted a survey of HOMERuN sites to synthesize practices across sites and provide some guidance for hospitals based on themes or concordance between these sites.
“One area of clear concordance among sites in our study was around the use of [Centers for Disease Control and Prevention] guidelines to address patient isolation procedures as well as strategies to mitigate transmission, such as providing patients with protective gear like masks or requiring the driver who picks up the patient wear a mask for transportation,” Dr. Greysen said. “We also found that many sites used certain clinical criteria – for example, temperature, oxygen saturation or supplementation, and improvement of presenting symptoms – but there was wide variation in the details for these criteria.”
In addition, “some sites required that a patient be afebrile for a certain period of time before discharge whereas others only required that patients be afebrile at the time of discharge. There was also relatively strong consensus around assessing the level of social support and ability to perform activities of daily living prior to discharge,” since social support and ability to function are often interrelated and can be difficult to assess without visiting the home, he said.
“Further development the evidence around which discharge criteria are associated with adverse outcomes such as readmission or death is urgently needed. At this moment, we really don’t know which clinical criteria such as oxygen supplementation or nonclinical criteria are associated with better outcomes in COVID patients,” Dr. Greysen said, but he and his team plan to study this using EMR data in HOMERuN.
Dr. Bann said that clinical criteria for discharge will likely provoke lively discussions during the interactive part of the virtual session. “Also, I have heard a lot of discussion and interest in learning about how different sites are handling postdischarge monitoring and follow-up, such as how we ensure that patients are recovering well after discharge, and whether there are new or different needs for this patient population,” she added.
“Attendees should come away from this session with an understanding of how hospitals across the country have augmented their discharge planning responses during the COVID-19 pandemic,” Dr. Bann said. “This session is all about learning from each other and creating shared best practices,” she said.
“I hope that those who attend our session are able to see some areas of consensus in our study that could be applied to their discharge criteria,” Dr. Greysen added.
Dr. Bann and Dr. Greysen had no relevant financial conflicts to disclose.
Discharge Planning for COVID-19: Collected Practices from Across the U.S.
The COVID-19 pandemic continues to disrupt all aspects of hospital care, and has altered nearly all fundamental practices, including discharge protocols. A session presented at the Society of Hospitalist Medicine’s 2020 Virtual Annual Conference will focus on discharge issues in the COVID-19 era.
“Discharge planning is an integral part of a hospitalist’s clinical care. On a daily basis, we think carefully about how to help our patients safely transition back into life outside of the hospital,” said Maralyssa Bann, MD, of the University of Washington, Seattle, a copresenter at the session.
“Patients need up-to-date information about how to keep themselves and those around them safe,” she said. “They need resources and supports to help them recover from illness.”
These supports include access to appropriate follow-up with primary care doctors or other specialists and being discharged to the right location, such as home or a skilled nursing facility, Dr. Bann noted.
In response to COVID-19, “within an exceptionally short time frame, hospitals have had to rapidly adapt their discharge planning protocols and have had to continue to adapt as new information comes out,” Dr. Bann said.
“In many ways, the COVID-19 pandemic has highlighted the importance of discharge planning for patient care and has added a new element of public health in that we have to take all possible precautions to ensure that patients are not spreading the virus after they leave the hospital,” said Ryan Greysen, MD, of the University of Pennsylvania, Philadelphia, and Dr. Bann’s copresenter.
Many elements go into creating a good discharge plan, but there are often many unknowns, Dr. Greysen said. “I think there is an opportunity to improve the process by improving follow-up as well.”
“For example, one program at our hospital focused on vulnerable older adults includes an in-home visit by a visiting nurse on the day of discharge to verify the patient has everything they need when they arrive home,” However, now with more telemedicine and social distancing, there should be creative approaches to tying up loose ends and monitoring for things that can go wrong in order to give additional guidance, he said.
“In a previous study of 12 U.S. academic medical centers, my colleagues and I interviewed over 1,000 patients who were discharged and then readmitted to ask them what they thought went wrong,” said Dr. Greysen. “Overwhelmingly, patients indicated that they understood their discharge instructions and the plan of care at the time they left the hospital, but then when there were breakdowns or unanticipated challenges in the plan, they were uncertain what to do.”
In the HM20 Virtual session, Dr. Greysen and Dr. Bann will present additional data from the same network that Dr. Greysen used in his study, the Hospital Medicine Reengineering Network or HOMERuN, but expanded to include 22 sites.
The specific areas will include clinical and nonclinical criteria for patients to be discharged home, how criteria differed for discharge destinations other than home, discharge logistics, discharge instructions for patients and caregivers, and postdischarge follow-up.
“Developing a discharge protocol during a pandemic is a major challenge. There are new barriers and challenges to finding the right discharge location, as information about illness course and outcome is incomplete or evolving,” Dr. Bann said. “The safety of patients and their loved ones, health care workers and staff, as well as the public at large is always top of mind. Decisions have to be made in a timely way and communicated clearly. This is a huge task in addition to all of the other competing work in the midst of a pandemic, which is why learning from each other and collectively creating our shared best practices is tremendously helpful. If I can take example approaches from other hospitals and update them for use at my site, this saves a lot of time and effort.”
“There is great urgency to understand when it is safe to discharge these patients from the hospital,” Dr. Greysen said. “Many COVID patients can have worsening of their symptoms after a period of initial improvement so sending them home too soon is a major concern. On the other hand, we can’t keep COVID patients in the hospital until they have fully recovered; we would increase their risk of iatrogenic events and we could risk using up capacity of the health care system to care for other patients, both COVID and non-COVID.”
Unfortunately, no evidence base yet exists to guide the creation of discharge guidelines for COVID patients, said Dr. Greysen. “Therefore, we conducted a survey of HOMERuN sites to synthesize practices across sites and provide some guidance for hospitals based on themes or concordance between these sites.
“One area of clear concordance among sites in our study was around the use of [Centers for Disease Control and Prevention] guidelines to address patient isolation procedures as well as strategies to mitigate transmission, such as providing patients with protective gear like masks or requiring the driver who picks up the patient wear a mask for transportation,” Dr. Greysen said. “We also found that many sites used certain clinical criteria – for example, temperature, oxygen saturation or supplementation, and improvement of presenting symptoms – but there was wide variation in the details for these criteria.”
In addition, “some sites required that a patient be afebrile for a certain period of time before discharge whereas others only required that patients be afebrile at the time of discharge. There was also relatively strong consensus around assessing the level of social support and ability to perform activities of daily living prior to discharge,” since social support and ability to function are often interrelated and can be difficult to assess without visiting the home, he said.
“Further development the evidence around which discharge criteria are associated with adverse outcomes such as readmission or death is urgently needed. At this moment, we really don’t know which clinical criteria such as oxygen supplementation or nonclinical criteria are associated with better outcomes in COVID patients,” Dr. Greysen said, but he and his team plan to study this using EMR data in HOMERuN.
Dr. Bann said that clinical criteria for discharge will likely provoke lively discussions during the interactive part of the virtual session. “Also, I have heard a lot of discussion and interest in learning about how different sites are handling postdischarge monitoring and follow-up, such as how we ensure that patients are recovering well after discharge, and whether there are new or different needs for this patient population,” she added.
“Attendees should come away from this session with an understanding of how hospitals across the country have augmented their discharge planning responses during the COVID-19 pandemic,” Dr. Bann said. “This session is all about learning from each other and creating shared best practices,” she said.
“I hope that those who attend our session are able to see some areas of consensus in our study that could be applied to their discharge criteria,” Dr. Greysen added.
Dr. Bann and Dr. Greysen had no relevant financial conflicts to disclose.
Discharge Planning for COVID-19: Collected Practices from Across the U.S.