User login
Telemedicine in primary care
How to effectively utilize this tool
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
How to effectively utilize this tool
How to effectively utilize this tool
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
Health disparities training falls short for internal medicine residents
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
FROM JAMA NETWORK OPEN
Shielding ‘had little effect on rates of COVID-19 in rheumatology patients’
Researchers from the Royal Wolverhampton (England) Hospitals National Health Service Trust say shielding – or taking extra steps to protect oneself against COVID-19 if at high risk – has had little effect on the incidence of COVID-19 in rheumatology patients.
In Annals of the Rheumatic Diseases, the team present data from a large rheumatology cohort in the United Kingdom between Feb. 1, 2020, and May 1, 2020. Patients’ health-related quality of life (HRQoL) was assessed on April 24, 2020, using the Short Form–12 to assess Physical Component Score (PCS) and Mental Component Score (MCS) on a 0-100 scale (0 being the lowest score).
Of 1,693 participants, at the time, there were 61 (3.6%) reported COVID-19 infections (eight had confirmatory swab results; three had clinical diagnoses with “false-negative” swab; 50 had clinical diagnosis but were not swabbed in line with U.K. policy at that time).
Seven of the 61 (11.5%) patients were hospitalized, two requiring intensive care. Of this group, 24 were shielding, a similar proportion to the non-COVID cohort (24/61 vs. 768/1,632; P = .24). There was no significant effect of treatment on self-reported COVID-19 incidence.
There were significantly lower MCSs in the infected group, compared with control participants (38.9 vs. 42.2; mean difference: −3.3; 95% CI, −5.2 to 1.4; P < .001). There was no difference in PCS (−0.4; 95% CI, −2.1 to 1.3).
In patients without COVID-19, the ‘shielding’ group had significantly lower MCS (−2.1; 95% CI, −2.9 to 1.4; P < .001) and PCS (−2.2; 95% CI, −3.8 to 2.5; P < .001) than those not shielding.
There were no differences in MCSs between patients on non–biologic disease-modifying antirheumatic drugs and biologic DMARDs (0.6; 95% CI, 0.1-2.4).
The findings suggest that overall strict social isolation had little effect on the incidence of COVID-19 infection. Patients who had suffered from the virus had reduced mental but not physical HRQoL scores.
There was an adverse effect on both MCS and PCS reported by patients undergoing shielding,n compared with those not. This has also been shown in previous work from India.
This article originally appeared on Univadis, part of the Medscape Professional Network.
Researchers from the Royal Wolverhampton (England) Hospitals National Health Service Trust say shielding – or taking extra steps to protect oneself against COVID-19 if at high risk – has had little effect on the incidence of COVID-19 in rheumatology patients.
In Annals of the Rheumatic Diseases, the team present data from a large rheumatology cohort in the United Kingdom between Feb. 1, 2020, and May 1, 2020. Patients’ health-related quality of life (HRQoL) was assessed on April 24, 2020, using the Short Form–12 to assess Physical Component Score (PCS) and Mental Component Score (MCS) on a 0-100 scale (0 being the lowest score).
Of 1,693 participants, at the time, there were 61 (3.6%) reported COVID-19 infections (eight had confirmatory swab results; three had clinical diagnoses with “false-negative” swab; 50 had clinical diagnosis but were not swabbed in line with U.K. policy at that time).
Seven of the 61 (11.5%) patients were hospitalized, two requiring intensive care. Of this group, 24 were shielding, a similar proportion to the non-COVID cohort (24/61 vs. 768/1,632; P = .24). There was no significant effect of treatment on self-reported COVID-19 incidence.
There were significantly lower MCSs in the infected group, compared with control participants (38.9 vs. 42.2; mean difference: −3.3; 95% CI, −5.2 to 1.4; P < .001). There was no difference in PCS (−0.4; 95% CI, −2.1 to 1.3).
In patients without COVID-19, the ‘shielding’ group had significantly lower MCS (−2.1; 95% CI, −2.9 to 1.4; P < .001) and PCS (−2.2; 95% CI, −3.8 to 2.5; P < .001) than those not shielding.
There were no differences in MCSs between patients on non–biologic disease-modifying antirheumatic drugs and biologic DMARDs (0.6; 95% CI, 0.1-2.4).
The findings suggest that overall strict social isolation had little effect on the incidence of COVID-19 infection. Patients who had suffered from the virus had reduced mental but not physical HRQoL scores.
There was an adverse effect on both MCS and PCS reported by patients undergoing shielding,n compared with those not. This has also been shown in previous work from India.
This article originally appeared on Univadis, part of the Medscape Professional Network.
Researchers from the Royal Wolverhampton (England) Hospitals National Health Service Trust say shielding – or taking extra steps to protect oneself against COVID-19 if at high risk – has had little effect on the incidence of COVID-19 in rheumatology patients.
In Annals of the Rheumatic Diseases, the team present data from a large rheumatology cohort in the United Kingdom between Feb. 1, 2020, and May 1, 2020. Patients’ health-related quality of life (HRQoL) was assessed on April 24, 2020, using the Short Form–12 to assess Physical Component Score (PCS) and Mental Component Score (MCS) on a 0-100 scale (0 being the lowest score).
Of 1,693 participants, at the time, there were 61 (3.6%) reported COVID-19 infections (eight had confirmatory swab results; three had clinical diagnoses with “false-negative” swab; 50 had clinical diagnosis but were not swabbed in line with U.K. policy at that time).
Seven of the 61 (11.5%) patients were hospitalized, two requiring intensive care. Of this group, 24 were shielding, a similar proportion to the non-COVID cohort (24/61 vs. 768/1,632; P = .24). There was no significant effect of treatment on self-reported COVID-19 incidence.
There were significantly lower MCSs in the infected group, compared with control participants (38.9 vs. 42.2; mean difference: −3.3; 95% CI, −5.2 to 1.4; P < .001). There was no difference in PCS (−0.4; 95% CI, −2.1 to 1.3).
In patients without COVID-19, the ‘shielding’ group had significantly lower MCS (−2.1; 95% CI, −2.9 to 1.4; P < .001) and PCS (−2.2; 95% CI, −3.8 to 2.5; P < .001) than those not shielding.
There were no differences in MCSs between patients on non–biologic disease-modifying antirheumatic drugs and biologic DMARDs (0.6; 95% CI, 0.1-2.4).
The findings suggest that overall strict social isolation had little effect on the incidence of COVID-19 infection. Patients who had suffered from the virus had reduced mental but not physical HRQoL scores.
There was an adverse effect on both MCS and PCS reported by patients undergoing shielding,n compared with those not. This has also been shown in previous work from India.
This article originally appeared on Univadis, part of the Medscape Professional Network.
Misconduct, Failures, and Miscommunication Contributed to Patient Suicide at Washington VAMC
The US Department of Veterans Affairs (VA) Office of Inspector General (OIG) recently completed a highly critical investigation into allegations concerning the care of a suicidal patient in the Washington, DC, VA Medical Center Emergency Department (ED). The patient committed suicide by gunshot 6 days after an ED visit in which a VA provider reportedly commented, “[The patient] can go shoot [themself]. I do not care.”
In early 2019, the patient, who was in his 60s and had a history of panic attacks, painkiller addiction, and various injuries, came to the ED complaining of alprazolam and oxycodone withdrawal and insomnia. He asked to be admitted for detoxification. The ED resident physician documented that request and recommended outpatient psychiatry follow-up. The attending physician documented agreement with the assessment, and an ED social worker scheduled the patient for a same-day outpatient psychiatry evaluation. However, the patient, along with a family member, told a Veteran Experience Specialist he was dissatisfied with care, and again requested admission for inpatient detoxification. The specialist accompanied the patient and family member to the ED and informed a staff member of the patient’s preference for admission.
Following this, the patient presented to the outpatient psychiatry appointment, where a psychiatrist assessed his suicide risk as “moderate” and recommended admission. He was escorted back to the ED, where the psychiatrist reportedly handed him off both verbally and with an alert in the electronic health record to the attending physician. The family member told the OIG that the outpatient psychiatrist had indicated that the patient was going to be admitted to the detoxification of the psychiatry unit. The family member left, thinking the patient was being admitted.
A physician assistant documented the patient’s chief complaint as anxiety, documented the patient’s suicidal ideation, and placed a psychiatry consult to evaluate the patient for inpatient admission. The consulting psychiatry resident and attending psychiatrist deemed him at mild risk of suicide and didn’t meet the criterial for inpatient admission. They recommended outpatient care, and that the patient be discharged and sent home. The patient, though, refused to leave. A second ED attending physician documented that the patient was “clearly malingering” and “ranting.” Police were called to escort him out. At least 3 hospital staff members said they heard the physician say “I do not care,” if the patient committed suicide. A family member later called the facility’s medical advice line and told the on-call nurse that the patient had died at home 6 days after the ED visit.
The OIG found numerous preventable mix-ups, oversights, and outright misconduct throughout this patient’s health care experience. Notably, the patient navigated 2 transitions between the ED and outpatient Mental Health Clinic and saw 7 providers over the course of 12 hours. The lack of collaboration between the various health care providers, deficiencies in the hand-off process, and ED and inpatient mental health providers’ failure to read the outpatient psychiatrist’s notes led to a “compromised understanding” of the patient’s treatment needs and a failure to enact the outpatient psychiatrist’s recommended treatment plan.
For instance, 2 days after the patient presented to the ED, the outpatient psychiatrist entered a consult for the outpatient substance use treatment program indicating that the patient was informed of the appointment date and time (5 days after the ED visit); however, the OIG found no evidence that staff informed the patient of the appointment date and time. An outpatient nurse closed the consult and added a comment that the patient was to report to the treatment program 5 days after the ED visit. Contrary to Veterans Health Administration (VHA) policy, the OIG report says, the nurse explained that an appointment was not scheduled because it was not program procedure at the time. The nurse mistakenly thought the patient already was receiving outpatient treatment, and because the patient had no scheduled appointment, staff did not follow up when he missed it.
The OIG also found that the facility’s Suicide Prevention Coordinator had failed to complete the suicide behavior report following notification of the patient’s death by suicide, as required by VHA. In fact, the coordinator was unable to locate a suicide behavior report. Moreover, the OIG says, the ED failed to meet VHA’s requirements for a safe and secure evaluation area for patients seeking mental health services. A renovation project begun in 2009 to include 3 mental health examination rooms had been on hold.
Regarding the doctor who was heard making the callous statement, the OIG found that, despite the facility leaders’ awareness of the comment and of the doctor’s “prior pattern of misconduct,” they did not conduct a formal fact-finding or administrative investigation as required by the VA. Instead, they seemed to focus on the physician’s “overall positive clinical outcomes.”
The doctor “was never a VA employee, only worked on a contract basis and is no longer welcome at the facility,” said Dr. Michael Heimall, the center’s director, in a statement to The New York Times.
He added that the episode has prompted the hospital to change its policies. Among the changes: a “comprehensive education program” on employee misconduct and patient abuse has been instituted. Further, now only the Chief of Staff can reverse the outpatient mental health provider’s recommendation for a patient’s admission.
The US Department of Veterans Affairs (VA) Office of Inspector General (OIG) recently completed a highly critical investigation into allegations concerning the care of a suicidal patient in the Washington, DC, VA Medical Center Emergency Department (ED). The patient committed suicide by gunshot 6 days after an ED visit in which a VA provider reportedly commented, “[The patient] can go shoot [themself]. I do not care.”
In early 2019, the patient, who was in his 60s and had a history of panic attacks, painkiller addiction, and various injuries, came to the ED complaining of alprazolam and oxycodone withdrawal and insomnia. He asked to be admitted for detoxification. The ED resident physician documented that request and recommended outpatient psychiatry follow-up. The attending physician documented agreement with the assessment, and an ED social worker scheduled the patient for a same-day outpatient psychiatry evaluation. However, the patient, along with a family member, told a Veteran Experience Specialist he was dissatisfied with care, and again requested admission for inpatient detoxification. The specialist accompanied the patient and family member to the ED and informed a staff member of the patient’s preference for admission.
Following this, the patient presented to the outpatient psychiatry appointment, where a psychiatrist assessed his suicide risk as “moderate” and recommended admission. He was escorted back to the ED, where the psychiatrist reportedly handed him off both verbally and with an alert in the electronic health record to the attending physician. The family member told the OIG that the outpatient psychiatrist had indicated that the patient was going to be admitted to the detoxification of the psychiatry unit. The family member left, thinking the patient was being admitted.
A physician assistant documented the patient’s chief complaint as anxiety, documented the patient’s suicidal ideation, and placed a psychiatry consult to evaluate the patient for inpatient admission. The consulting psychiatry resident and attending psychiatrist deemed him at mild risk of suicide and didn’t meet the criterial for inpatient admission. They recommended outpatient care, and that the patient be discharged and sent home. The patient, though, refused to leave. A second ED attending physician documented that the patient was “clearly malingering” and “ranting.” Police were called to escort him out. At least 3 hospital staff members said they heard the physician say “I do not care,” if the patient committed suicide. A family member later called the facility’s medical advice line and told the on-call nurse that the patient had died at home 6 days after the ED visit.
The OIG found numerous preventable mix-ups, oversights, and outright misconduct throughout this patient’s health care experience. Notably, the patient navigated 2 transitions between the ED and outpatient Mental Health Clinic and saw 7 providers over the course of 12 hours. The lack of collaboration between the various health care providers, deficiencies in the hand-off process, and ED and inpatient mental health providers’ failure to read the outpatient psychiatrist’s notes led to a “compromised understanding” of the patient’s treatment needs and a failure to enact the outpatient psychiatrist’s recommended treatment plan.
For instance, 2 days after the patient presented to the ED, the outpatient psychiatrist entered a consult for the outpatient substance use treatment program indicating that the patient was informed of the appointment date and time (5 days after the ED visit); however, the OIG found no evidence that staff informed the patient of the appointment date and time. An outpatient nurse closed the consult and added a comment that the patient was to report to the treatment program 5 days after the ED visit. Contrary to Veterans Health Administration (VHA) policy, the OIG report says, the nurse explained that an appointment was not scheduled because it was not program procedure at the time. The nurse mistakenly thought the patient already was receiving outpatient treatment, and because the patient had no scheduled appointment, staff did not follow up when he missed it.
The OIG also found that the facility’s Suicide Prevention Coordinator had failed to complete the suicide behavior report following notification of the patient’s death by suicide, as required by VHA. In fact, the coordinator was unable to locate a suicide behavior report. Moreover, the OIG says, the ED failed to meet VHA’s requirements for a safe and secure evaluation area for patients seeking mental health services. A renovation project begun in 2009 to include 3 mental health examination rooms had been on hold.
Regarding the doctor who was heard making the callous statement, the OIG found that, despite the facility leaders’ awareness of the comment and of the doctor’s “prior pattern of misconduct,” they did not conduct a formal fact-finding or administrative investigation as required by the VA. Instead, they seemed to focus on the physician’s “overall positive clinical outcomes.”
The doctor “was never a VA employee, only worked on a contract basis and is no longer welcome at the facility,” said Dr. Michael Heimall, the center’s director, in a statement to The New York Times.
He added that the episode has prompted the hospital to change its policies. Among the changes: a “comprehensive education program” on employee misconduct and patient abuse has been instituted. Further, now only the Chief of Staff can reverse the outpatient mental health provider’s recommendation for a patient’s admission.
The US Department of Veterans Affairs (VA) Office of Inspector General (OIG) recently completed a highly critical investigation into allegations concerning the care of a suicidal patient in the Washington, DC, VA Medical Center Emergency Department (ED). The patient committed suicide by gunshot 6 days after an ED visit in which a VA provider reportedly commented, “[The patient] can go shoot [themself]. I do not care.”
In early 2019, the patient, who was in his 60s and had a history of panic attacks, painkiller addiction, and various injuries, came to the ED complaining of alprazolam and oxycodone withdrawal and insomnia. He asked to be admitted for detoxification. The ED resident physician documented that request and recommended outpatient psychiatry follow-up. The attending physician documented agreement with the assessment, and an ED social worker scheduled the patient for a same-day outpatient psychiatry evaluation. However, the patient, along with a family member, told a Veteran Experience Specialist he was dissatisfied with care, and again requested admission for inpatient detoxification. The specialist accompanied the patient and family member to the ED and informed a staff member of the patient’s preference for admission.
Following this, the patient presented to the outpatient psychiatry appointment, where a psychiatrist assessed his suicide risk as “moderate” and recommended admission. He was escorted back to the ED, where the psychiatrist reportedly handed him off both verbally and with an alert in the electronic health record to the attending physician. The family member told the OIG that the outpatient psychiatrist had indicated that the patient was going to be admitted to the detoxification of the psychiatry unit. The family member left, thinking the patient was being admitted.
A physician assistant documented the patient’s chief complaint as anxiety, documented the patient’s suicidal ideation, and placed a psychiatry consult to evaluate the patient for inpatient admission. The consulting psychiatry resident and attending psychiatrist deemed him at mild risk of suicide and didn’t meet the criterial for inpatient admission. They recommended outpatient care, and that the patient be discharged and sent home. The patient, though, refused to leave. A second ED attending physician documented that the patient was “clearly malingering” and “ranting.” Police were called to escort him out. At least 3 hospital staff members said they heard the physician say “I do not care,” if the patient committed suicide. A family member later called the facility’s medical advice line and told the on-call nurse that the patient had died at home 6 days after the ED visit.
The OIG found numerous preventable mix-ups, oversights, and outright misconduct throughout this patient’s health care experience. Notably, the patient navigated 2 transitions between the ED and outpatient Mental Health Clinic and saw 7 providers over the course of 12 hours. The lack of collaboration between the various health care providers, deficiencies in the hand-off process, and ED and inpatient mental health providers’ failure to read the outpatient psychiatrist’s notes led to a “compromised understanding” of the patient’s treatment needs and a failure to enact the outpatient psychiatrist’s recommended treatment plan.
For instance, 2 days after the patient presented to the ED, the outpatient psychiatrist entered a consult for the outpatient substance use treatment program indicating that the patient was informed of the appointment date and time (5 days after the ED visit); however, the OIG found no evidence that staff informed the patient of the appointment date and time. An outpatient nurse closed the consult and added a comment that the patient was to report to the treatment program 5 days after the ED visit. Contrary to Veterans Health Administration (VHA) policy, the OIG report says, the nurse explained that an appointment was not scheduled because it was not program procedure at the time. The nurse mistakenly thought the patient already was receiving outpatient treatment, and because the patient had no scheduled appointment, staff did not follow up when he missed it.
The OIG also found that the facility’s Suicide Prevention Coordinator had failed to complete the suicide behavior report following notification of the patient’s death by suicide, as required by VHA. In fact, the coordinator was unable to locate a suicide behavior report. Moreover, the OIG says, the ED failed to meet VHA’s requirements for a safe and secure evaluation area for patients seeking mental health services. A renovation project begun in 2009 to include 3 mental health examination rooms had been on hold.
Regarding the doctor who was heard making the callous statement, the OIG found that, despite the facility leaders’ awareness of the comment and of the doctor’s “prior pattern of misconduct,” they did not conduct a formal fact-finding or administrative investigation as required by the VA. Instead, they seemed to focus on the physician’s “overall positive clinical outcomes.”
The doctor “was never a VA employee, only worked on a contract basis and is no longer welcome at the facility,” said Dr. Michael Heimall, the center’s director, in a statement to The New York Times.
He added that the episode has prompted the hospital to change its policies. Among the changes: a “comprehensive education program” on employee misconduct and patient abuse has been instituted. Further, now only the Chief of Staff can reverse the outpatient mental health provider’s recommendation for a patient’s admission.
Study highlights potential advantages of tape strips over biopsy
for monitoring these and potentially other dermatologic diseases, according to the latest advances with this approach.
“Tape strips are not going to fully replace biopsies, but we think they will have an important role in diagnosing and monitoring response to therapy by avoiding the potential scarring and pain of biopsy,” reported Emma Guttman-Yassky, MD, PhD, professor of dermatology and director of the laboratory inflammatory skin diseases at the Icahn School of Medicine at Mount Sinai Medical Center, New York.
The concept of using adhesive strips to remove surface skin cells for clinical study has been around for more than 20 years, but there has been recent progress. A newly published study, which compared skin from patients with atopic dermatitis (AD) or psoriasis with that of controls, was characterized as “the most comprehensive tape strip molecular profiling in any inflammatory skin disease to date and the first to fully characterize and compare AD to psoriasis,” wrote Dr. Guttman-Yassky, the senior author, and coauthors.
It also appears to be a leap forward. RNA sequencing detected thousands of differentially expressed genes reflecting immune and barrier biomarkers characteristic of the molecular phenotypes of atopic dermatitis and psoriasis. These were not only found to be consistent with biopsy studies but identified additional unique genes and pathways relevant to their pathological signature.
“In the past, the success rate for transcriptome sequencing even for a more limited panel of proteins was approaching 50% when considering both lesional, nonlesional skin, and healthy skin, but we are now approaching 100% for sample recovery and for analysis of RNA and genes,” Dr. Guttman-Yassky said in an interview.
Tissue samples were obtained with tape strips from lesional and nonlesional skin from 20 patients with AD and 20 patients with psoriasis. Compared with 20 tape strips from controls, they were evaluated with RNA sequencing followed by quantitative real-time polymerase chain reaction of immune and barrier biomarkers.
The sample recovery rate was 96% overall and 95% or better regardless of whether the skin was lesional or nonlesional.
With RNA sequencing of more than 20,000 transcripts, including multiple cellular, immune, and barrier biomarkers, an enormous amount of data was generated, but the key finding is that these diseases are readily distinguished with profiling based on tape strips.
Although numerous biomarkers were shared, “tape strips completely discriminate between atopic dermatitis and psoriasis with a degree of reliability that is comparable to skin biopsy,” Dr. Guttman-Yassky said.
One of the biomarkers, expression of nitric oxide synthase 2/inducible nitric oxide synthase, distinguished AD from psoriasis with 100% accuracy. As previously reported in biopsy studies, other biomarkers collectively associated AD with a profile related to a Th2-type inflammatory response and psoriasis with a Th17-type inflammatory response.
Tape strips also confirmed significant pathology in the nonlesional as well as the lesional skin of patients with AD or psoriasis. This included an increase in Th2-type products, such as interleukin-4 and IL-13, in nonlesional skin of atopic dermatitis and Th17-type products, such as IL-17, in nonlesional skin of psoriasis.
Some biomarkers of AD and psoriasis had an even greater differentiation in tape strips than previously reported from biopsy studies, according to Dr. Guttman-Yassky. In this study, tape strips also captured more differentially expressed genes than previously reported with biopsies.
One potential limitation of tape strips is that the RNA isolation process is time consuming, but this might be less of an issue in routine clinical use if there is a more refined number of biomarkers that are targeted or if technological improvements simplify processing, Dr. Guttman-Yassky pointed out.
To develop clinical utility for tape strips beyond AD and psoriasis, more work is needed to standardize the depth of sampling, which is variable with tape strips, she noted. Depth is relevant to the analysis of gene expression and mRNA activity of each dermatologic disease.
“Tape strips remain a research tool for now, but we do think that this technique can be refined and employed for clinical purposes, including diagnosis and monitoring response to treatment,” she said.
Relative to biopsy, the advantages are not difficult to envision. Dr. Guttman-Yassky, who recently published a study of tape strips for evaluating AD in children emphasized that tape strips are generally painless.
“Patients really do not mind tape strips,” she said. Although she believes that tape strips are providing unique insight into the pathology of inflammatory diseases not necessarily available with biopsy, she emphasized the practical value. Not least, “these could really help when the goal is to evaluate response to therapy over time.”
Another investigator who has conducted studies with tape strips, Maja-Lisa Clausen, MD, PhD, also thinks tape strips are likely to become routine clinical tools.
“Once the basis research, validation, and data are out, I think numerous companies will be ready to develop machines for more quick and easy processing, compared to the more labor intensive process that is used today for research,” explained Dr. Clausen, who is in the department of dermatology, Bispebjerb Hospital, University of Copenhagen.
She considers tape strips particularly promising for children, but she thinks the biomarker profiling made possible by these strips might be leading to personalized treatment programs for dermatologic diseases.
“What we need is further validation; which tape to use, how deep, and the importance of storage, which is a big issue in the clinic,” Dr. Clausen said in an interview.
Dr. Guttman-Yassky has financial relationships with multiple pharmaceutical companies, including those with therapies for psoriasis.
SOURCE: Guttman-Yassky E et al. J Allergy Clin Immunol. 2020 Jul 9. doi: 10.1016/j.jaci.2020.05.048.
for monitoring these and potentially other dermatologic diseases, according to the latest advances with this approach.
“Tape strips are not going to fully replace biopsies, but we think they will have an important role in diagnosing and monitoring response to therapy by avoiding the potential scarring and pain of biopsy,” reported Emma Guttman-Yassky, MD, PhD, professor of dermatology and director of the laboratory inflammatory skin diseases at the Icahn School of Medicine at Mount Sinai Medical Center, New York.
The concept of using adhesive strips to remove surface skin cells for clinical study has been around for more than 20 years, but there has been recent progress. A newly published study, which compared skin from patients with atopic dermatitis (AD) or psoriasis with that of controls, was characterized as “the most comprehensive tape strip molecular profiling in any inflammatory skin disease to date and the first to fully characterize and compare AD to psoriasis,” wrote Dr. Guttman-Yassky, the senior author, and coauthors.
It also appears to be a leap forward. RNA sequencing detected thousands of differentially expressed genes reflecting immune and barrier biomarkers characteristic of the molecular phenotypes of atopic dermatitis and psoriasis. These were not only found to be consistent with biopsy studies but identified additional unique genes and pathways relevant to their pathological signature.
“In the past, the success rate for transcriptome sequencing even for a more limited panel of proteins was approaching 50% when considering both lesional, nonlesional skin, and healthy skin, but we are now approaching 100% for sample recovery and for analysis of RNA and genes,” Dr. Guttman-Yassky said in an interview.
Tissue samples were obtained with tape strips from lesional and nonlesional skin from 20 patients with AD and 20 patients with psoriasis. Compared with 20 tape strips from controls, they were evaluated with RNA sequencing followed by quantitative real-time polymerase chain reaction of immune and barrier biomarkers.
The sample recovery rate was 96% overall and 95% or better regardless of whether the skin was lesional or nonlesional.
With RNA sequencing of more than 20,000 transcripts, including multiple cellular, immune, and barrier biomarkers, an enormous amount of data was generated, but the key finding is that these diseases are readily distinguished with profiling based on tape strips.
Although numerous biomarkers were shared, “tape strips completely discriminate between atopic dermatitis and psoriasis with a degree of reliability that is comparable to skin biopsy,” Dr. Guttman-Yassky said.
One of the biomarkers, expression of nitric oxide synthase 2/inducible nitric oxide synthase, distinguished AD from psoriasis with 100% accuracy. As previously reported in biopsy studies, other biomarkers collectively associated AD with a profile related to a Th2-type inflammatory response and psoriasis with a Th17-type inflammatory response.
Tape strips also confirmed significant pathology in the nonlesional as well as the lesional skin of patients with AD or psoriasis. This included an increase in Th2-type products, such as interleukin-4 and IL-13, in nonlesional skin of atopic dermatitis and Th17-type products, such as IL-17, in nonlesional skin of psoriasis.
Some biomarkers of AD and psoriasis had an even greater differentiation in tape strips than previously reported from biopsy studies, according to Dr. Guttman-Yassky. In this study, tape strips also captured more differentially expressed genes than previously reported with biopsies.
One potential limitation of tape strips is that the RNA isolation process is time consuming, but this might be less of an issue in routine clinical use if there is a more refined number of biomarkers that are targeted or if technological improvements simplify processing, Dr. Guttman-Yassky pointed out.
To develop clinical utility for tape strips beyond AD and psoriasis, more work is needed to standardize the depth of sampling, which is variable with tape strips, she noted. Depth is relevant to the analysis of gene expression and mRNA activity of each dermatologic disease.
“Tape strips remain a research tool for now, but we do think that this technique can be refined and employed for clinical purposes, including diagnosis and monitoring response to treatment,” she said.
Relative to biopsy, the advantages are not difficult to envision. Dr. Guttman-Yassky, who recently published a study of tape strips for evaluating AD in children emphasized that tape strips are generally painless.
“Patients really do not mind tape strips,” she said. Although she believes that tape strips are providing unique insight into the pathology of inflammatory diseases not necessarily available with biopsy, she emphasized the practical value. Not least, “these could really help when the goal is to evaluate response to therapy over time.”
Another investigator who has conducted studies with tape strips, Maja-Lisa Clausen, MD, PhD, also thinks tape strips are likely to become routine clinical tools.
“Once the basis research, validation, and data are out, I think numerous companies will be ready to develop machines for more quick and easy processing, compared to the more labor intensive process that is used today for research,” explained Dr. Clausen, who is in the department of dermatology, Bispebjerb Hospital, University of Copenhagen.
She considers tape strips particularly promising for children, but she thinks the biomarker profiling made possible by these strips might be leading to personalized treatment programs for dermatologic diseases.
“What we need is further validation; which tape to use, how deep, and the importance of storage, which is a big issue in the clinic,” Dr. Clausen said in an interview.
Dr. Guttman-Yassky has financial relationships with multiple pharmaceutical companies, including those with therapies for psoriasis.
SOURCE: Guttman-Yassky E et al. J Allergy Clin Immunol. 2020 Jul 9. doi: 10.1016/j.jaci.2020.05.048.
for monitoring these and potentially other dermatologic diseases, according to the latest advances with this approach.
“Tape strips are not going to fully replace biopsies, but we think they will have an important role in diagnosing and monitoring response to therapy by avoiding the potential scarring and pain of biopsy,” reported Emma Guttman-Yassky, MD, PhD, professor of dermatology and director of the laboratory inflammatory skin diseases at the Icahn School of Medicine at Mount Sinai Medical Center, New York.
The concept of using adhesive strips to remove surface skin cells for clinical study has been around for more than 20 years, but there has been recent progress. A newly published study, which compared skin from patients with atopic dermatitis (AD) or psoriasis with that of controls, was characterized as “the most comprehensive tape strip molecular profiling in any inflammatory skin disease to date and the first to fully characterize and compare AD to psoriasis,” wrote Dr. Guttman-Yassky, the senior author, and coauthors.
It also appears to be a leap forward. RNA sequencing detected thousands of differentially expressed genes reflecting immune and barrier biomarkers characteristic of the molecular phenotypes of atopic dermatitis and psoriasis. These were not only found to be consistent with biopsy studies but identified additional unique genes and pathways relevant to their pathological signature.
“In the past, the success rate for transcriptome sequencing even for a more limited panel of proteins was approaching 50% when considering both lesional, nonlesional skin, and healthy skin, but we are now approaching 100% for sample recovery and for analysis of RNA and genes,” Dr. Guttman-Yassky said in an interview.
Tissue samples were obtained with tape strips from lesional and nonlesional skin from 20 patients with AD and 20 patients with psoriasis. Compared with 20 tape strips from controls, they were evaluated with RNA sequencing followed by quantitative real-time polymerase chain reaction of immune and barrier biomarkers.
The sample recovery rate was 96% overall and 95% or better regardless of whether the skin was lesional or nonlesional.
With RNA sequencing of more than 20,000 transcripts, including multiple cellular, immune, and barrier biomarkers, an enormous amount of data was generated, but the key finding is that these diseases are readily distinguished with profiling based on tape strips.
Although numerous biomarkers were shared, “tape strips completely discriminate between atopic dermatitis and psoriasis with a degree of reliability that is comparable to skin biopsy,” Dr. Guttman-Yassky said.
One of the biomarkers, expression of nitric oxide synthase 2/inducible nitric oxide synthase, distinguished AD from psoriasis with 100% accuracy. As previously reported in biopsy studies, other biomarkers collectively associated AD with a profile related to a Th2-type inflammatory response and psoriasis with a Th17-type inflammatory response.
Tape strips also confirmed significant pathology in the nonlesional as well as the lesional skin of patients with AD or psoriasis. This included an increase in Th2-type products, such as interleukin-4 and IL-13, in nonlesional skin of atopic dermatitis and Th17-type products, such as IL-17, in nonlesional skin of psoriasis.
Some biomarkers of AD and psoriasis had an even greater differentiation in tape strips than previously reported from biopsy studies, according to Dr. Guttman-Yassky. In this study, tape strips also captured more differentially expressed genes than previously reported with biopsies.
One potential limitation of tape strips is that the RNA isolation process is time consuming, but this might be less of an issue in routine clinical use if there is a more refined number of biomarkers that are targeted or if technological improvements simplify processing, Dr. Guttman-Yassky pointed out.
To develop clinical utility for tape strips beyond AD and psoriasis, more work is needed to standardize the depth of sampling, which is variable with tape strips, she noted. Depth is relevant to the analysis of gene expression and mRNA activity of each dermatologic disease.
“Tape strips remain a research tool for now, but we do think that this technique can be refined and employed for clinical purposes, including diagnosis and monitoring response to treatment,” she said.
Relative to biopsy, the advantages are not difficult to envision. Dr. Guttman-Yassky, who recently published a study of tape strips for evaluating AD in children emphasized that tape strips are generally painless.
“Patients really do not mind tape strips,” she said. Although she believes that tape strips are providing unique insight into the pathology of inflammatory diseases not necessarily available with biopsy, she emphasized the practical value. Not least, “these could really help when the goal is to evaluate response to therapy over time.”
Another investigator who has conducted studies with tape strips, Maja-Lisa Clausen, MD, PhD, also thinks tape strips are likely to become routine clinical tools.
“Once the basis research, validation, and data are out, I think numerous companies will be ready to develop machines for more quick and easy processing, compared to the more labor intensive process that is used today for research,” explained Dr. Clausen, who is in the department of dermatology, Bispebjerb Hospital, University of Copenhagen.
She considers tape strips particularly promising for children, but she thinks the biomarker profiling made possible by these strips might be leading to personalized treatment programs for dermatologic diseases.
“What we need is further validation; which tape to use, how deep, and the importance of storage, which is a big issue in the clinic,” Dr. Clausen said in an interview.
Dr. Guttman-Yassky has financial relationships with multiple pharmaceutical companies, including those with therapies for psoriasis.
SOURCE: Guttman-Yassky E et al. J Allergy Clin Immunol. 2020 Jul 9. doi: 10.1016/j.jaci.2020.05.048.
FROM THE JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY
Guidance covers glycemia in dexamethasone-treated COVID-19 patients
New guidance from the U.K. National Diabetes COVID-19 Response Group addresses glucose management in patients with COVID-19 who are receiving dexamethasone therapy.
Although there are already guidelines that address inpatient management of steroid-induced hyperglycemia, the authors of the new document wrote that this new expert opinion paper was needed “given the ‘triple insult’ of dexamethasone-induced–impaired glucose metabolism, COVID-19–induced insulin resistance, and COVID-19–impaired insulin production.”
RECOVERY trial spurs response
The document, which is the latest in a series from the Association of British Clinical Diabetologists, was published online Aug. 2 in Diabetic Medicine. The group is chaired by Gerry Rayman, MD, consultant physician at the diabetes centre and diabetes research unit, East Suffolk (England) and North East NHS Foundation Trust.
The guidance was developed in response to the recent “breakthrough” Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, which showed that dexamethasone reduced deaths in patients with COVID-19 on ventilators or receiving oxygen therapy. The advice is not intended for critical care units but can be adapted for that use.
The dose used in RECOVERY – 6 mg daily for 10 days – is 400%-500% greater than the therapeutic glucocorticoid replacement dose. High glucocorticoid doses can exacerbate hyperglycemia in people with established diabetes, unmask undiagnosed diabetes, precipitate hyperglycemia or new-onset diabetes, and can also cause hyperglycemic hyperosmolar state (HHS), the authors explained.
They recommended a target glucose of 6.0-10.0 mmol/L (108-180 mg/dL), although they say up to 12 mmol/L (216 mg/dL) is “acceptable.” They then gave advice on frequency of monitoring for people with and without known diabetes, exclusion of diabetic ketoacidosis and HHS, correction of initial hyperglycemia and maintenance of glycemic control using subcutaneous insulin, and prevention of hypoglycemia at the end of dexamethasone therapy (day 10) with insulin down-titration, discharge, and follow-up.
The detailed insulin guidance covers dose escalation for both insulin-treated and insulin-naive patients. A table suggests increasing correction doses of rapid-acting insulin based on prior total daily dose or weight.
Use of once- or twice-daily NPH insulin is recommended for patients whose glucose has risen above 12 mmol/L, in some cases with the addition of a long-acting analog. A second chart gives dose adjustments for those insulins. Additional guidance addresses patients on insulin pumps.
Guidance useful for U.S. physicians
Francisco Pasquel, MD, assistant professor of medicine in the division of endocrinology at Emory University, Atlanta, said in an interview that he believes the guidance is “acceptable” for worldwide use, and that “it’s coherent and consistent with what we typically do.”
However, Dr. Pasquel, who founded COVID-in-Diabetes, an online repository of published guidance and shared experience – to which this new document has now been added – did take issue with one piece of advice. The guidance says that patients already taking premixed insulin formulations can continue using them while increasing the dose by 20%-40%. Given the risk of hypoglycemia associated with those formulations, Dr. Pasquel said he would switch those patients to NPH during the time that they’re on dexamethasone.
He also noted that the rapid-acting insulin dose range of 2-10 units provided in the first table, for correction of initial hyperglycemia, are more conservative than those used at his hospital, where correction doses of up to 14-16 units are sometimes necessary.
But Dr. Pasquel praised the group’s overall efforts since the pandemic began, noting that “they’re very organized and constantly updating their recommendations. They have a unified system in the [National Health Service], so it’s easier to standardize. They have a unique [electronic health record] which is far superior to what we do from a public health perspective.”
Dr. Rayman reported no relevant financial relationships. Dr. Pasquel reported receiving research funding from Dexcom, Merck, and the National Institutes of Health, and consulting for AstraZeneca, Eli Lilly, Merck, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.
New guidance from the U.K. National Diabetes COVID-19 Response Group addresses glucose management in patients with COVID-19 who are receiving dexamethasone therapy.
Although there are already guidelines that address inpatient management of steroid-induced hyperglycemia, the authors of the new document wrote that this new expert opinion paper was needed “given the ‘triple insult’ of dexamethasone-induced–impaired glucose metabolism, COVID-19–induced insulin resistance, and COVID-19–impaired insulin production.”
RECOVERY trial spurs response
The document, which is the latest in a series from the Association of British Clinical Diabetologists, was published online Aug. 2 in Diabetic Medicine. The group is chaired by Gerry Rayman, MD, consultant physician at the diabetes centre and diabetes research unit, East Suffolk (England) and North East NHS Foundation Trust.
The guidance was developed in response to the recent “breakthrough” Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, which showed that dexamethasone reduced deaths in patients with COVID-19 on ventilators or receiving oxygen therapy. The advice is not intended for critical care units but can be adapted for that use.
The dose used in RECOVERY – 6 mg daily for 10 days – is 400%-500% greater than the therapeutic glucocorticoid replacement dose. High glucocorticoid doses can exacerbate hyperglycemia in people with established diabetes, unmask undiagnosed diabetes, precipitate hyperglycemia or new-onset diabetes, and can also cause hyperglycemic hyperosmolar state (HHS), the authors explained.
They recommended a target glucose of 6.0-10.0 mmol/L (108-180 mg/dL), although they say up to 12 mmol/L (216 mg/dL) is “acceptable.” They then gave advice on frequency of monitoring for people with and without known diabetes, exclusion of diabetic ketoacidosis and HHS, correction of initial hyperglycemia and maintenance of glycemic control using subcutaneous insulin, and prevention of hypoglycemia at the end of dexamethasone therapy (day 10) with insulin down-titration, discharge, and follow-up.
The detailed insulin guidance covers dose escalation for both insulin-treated and insulin-naive patients. A table suggests increasing correction doses of rapid-acting insulin based on prior total daily dose or weight.
Use of once- or twice-daily NPH insulin is recommended for patients whose glucose has risen above 12 mmol/L, in some cases with the addition of a long-acting analog. A second chart gives dose adjustments for those insulins. Additional guidance addresses patients on insulin pumps.
Guidance useful for U.S. physicians
Francisco Pasquel, MD, assistant professor of medicine in the division of endocrinology at Emory University, Atlanta, said in an interview that he believes the guidance is “acceptable” for worldwide use, and that “it’s coherent and consistent with what we typically do.”
However, Dr. Pasquel, who founded COVID-in-Diabetes, an online repository of published guidance and shared experience – to which this new document has now been added – did take issue with one piece of advice. The guidance says that patients already taking premixed insulin formulations can continue using them while increasing the dose by 20%-40%. Given the risk of hypoglycemia associated with those formulations, Dr. Pasquel said he would switch those patients to NPH during the time that they’re on dexamethasone.
He also noted that the rapid-acting insulin dose range of 2-10 units provided in the first table, for correction of initial hyperglycemia, are more conservative than those used at his hospital, where correction doses of up to 14-16 units are sometimes necessary.
But Dr. Pasquel praised the group’s overall efforts since the pandemic began, noting that “they’re very organized and constantly updating their recommendations. They have a unified system in the [National Health Service], so it’s easier to standardize. They have a unique [electronic health record] which is far superior to what we do from a public health perspective.”
Dr. Rayman reported no relevant financial relationships. Dr. Pasquel reported receiving research funding from Dexcom, Merck, and the National Institutes of Health, and consulting for AstraZeneca, Eli Lilly, Merck, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.
New guidance from the U.K. National Diabetes COVID-19 Response Group addresses glucose management in patients with COVID-19 who are receiving dexamethasone therapy.
Although there are already guidelines that address inpatient management of steroid-induced hyperglycemia, the authors of the new document wrote that this new expert opinion paper was needed “given the ‘triple insult’ of dexamethasone-induced–impaired glucose metabolism, COVID-19–induced insulin resistance, and COVID-19–impaired insulin production.”
RECOVERY trial spurs response
The document, which is the latest in a series from the Association of British Clinical Diabetologists, was published online Aug. 2 in Diabetic Medicine. The group is chaired by Gerry Rayman, MD, consultant physician at the diabetes centre and diabetes research unit, East Suffolk (England) and North East NHS Foundation Trust.
The guidance was developed in response to the recent “breakthrough” Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, which showed that dexamethasone reduced deaths in patients with COVID-19 on ventilators or receiving oxygen therapy. The advice is not intended for critical care units but can be adapted for that use.
The dose used in RECOVERY – 6 mg daily for 10 days – is 400%-500% greater than the therapeutic glucocorticoid replacement dose. High glucocorticoid doses can exacerbate hyperglycemia in people with established diabetes, unmask undiagnosed diabetes, precipitate hyperglycemia or new-onset diabetes, and can also cause hyperglycemic hyperosmolar state (HHS), the authors explained.
They recommended a target glucose of 6.0-10.0 mmol/L (108-180 mg/dL), although they say up to 12 mmol/L (216 mg/dL) is “acceptable.” They then gave advice on frequency of monitoring for people with and without known diabetes, exclusion of diabetic ketoacidosis and HHS, correction of initial hyperglycemia and maintenance of glycemic control using subcutaneous insulin, and prevention of hypoglycemia at the end of dexamethasone therapy (day 10) with insulin down-titration, discharge, and follow-up.
The detailed insulin guidance covers dose escalation for both insulin-treated and insulin-naive patients. A table suggests increasing correction doses of rapid-acting insulin based on prior total daily dose or weight.
Use of once- or twice-daily NPH insulin is recommended for patients whose glucose has risen above 12 mmol/L, in some cases with the addition of a long-acting analog. A second chart gives dose adjustments for those insulins. Additional guidance addresses patients on insulin pumps.
Guidance useful for U.S. physicians
Francisco Pasquel, MD, assistant professor of medicine in the division of endocrinology at Emory University, Atlanta, said in an interview that he believes the guidance is “acceptable” for worldwide use, and that “it’s coherent and consistent with what we typically do.”
However, Dr. Pasquel, who founded COVID-in-Diabetes, an online repository of published guidance and shared experience – to which this new document has now been added – did take issue with one piece of advice. The guidance says that patients already taking premixed insulin formulations can continue using them while increasing the dose by 20%-40%. Given the risk of hypoglycemia associated with those formulations, Dr. Pasquel said he would switch those patients to NPH during the time that they’re on dexamethasone.
He also noted that the rapid-acting insulin dose range of 2-10 units provided in the first table, for correction of initial hyperglycemia, are more conservative than those used at his hospital, where correction doses of up to 14-16 units are sometimes necessary.
But Dr. Pasquel praised the group’s overall efforts since the pandemic began, noting that “they’re very organized and constantly updating their recommendations. They have a unified system in the [National Health Service], so it’s easier to standardize. They have a unique [electronic health record] which is far superior to what we do from a public health perspective.”
Dr. Rayman reported no relevant financial relationships. Dr. Pasquel reported receiving research funding from Dexcom, Merck, and the National Institutes of Health, and consulting for AstraZeneca, Eli Lilly, Merck, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.
Antiaffirmative action paper blasted on Twitter now retracted
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
ED visits for mental health, substance use doubled in 1 decade
ED visits related to mental health conditions increased nearly twofold from 2007-2008 to 2015-2016, new research suggests.
Data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) showed that, over the 10-year study period, the proportion of ED visits for mental health diagnoses increased from 6.6% to 10.9%, with substance use accounting for much of the increase.
Although there have been policy efforts, such as expanding access to mental health care as part of the Affordable Care Act (ACA) of 2011, the senior author Taeho Greg Rhee, PhD, MSW, said in an interview.
“Treating mental health conditions in EDs is often considered suboptimal” because of limited time for full psychiatric assessment, lack of trained providers, and limited privacy in EDs, said Dr. Rhee of Yale University, New Haven, Conn.
The findings were published online July 28 in The Journal of Clinical Psychiatry.
“Outdated” research
Roughly one-fifth of U.S. adults experience some type of mental, behavioral, or emotional disorder annually. Moreover, the suicide rate has been steadily increasing, and there continues to be a “raging opioid epidemic,” the researchers wrote.
Despite these alarming figures, 57.4% of adults with mental illness reported in 2017 that they had not received any mental health treatment in the past year, reported the investigators.
Previous research has suggested that many adults have difficulty seeking outpatient mental health treatment and may turn to EDs instead. However, most studies of mental health ED use “are by now outdated, as they used data from years prior to the full implementation of the ACA,” the researchers noted.
“More Americans are suffering from mental illness, and given the recent policy efforts of expanding access to mental health care, we were questioning if ED visits due to mental health has changed or not,” Dr. Rhee said.
To investigate the question, the researchers conducted a cross-sectional analysis of data from the NHAMCS, a publicly available dataset provided by the National Center for Health Statistics of the Centers for Disease Control and Prevention.
They grouped psychiatric diagnoses into five categories: mood disorders, anxiety disorders, psychosis or schizophrenia, suicide attempt or ideation, or other/unspecified. Substance use diagnoses were grouped into six categories: alcohol, amphetamine, cannabis, cocaine, opioid, or other/unspecified.
These categories were used to determine the type of disorder a patient had, whether the patient had both psychiatric and substance-related diagnoses, and whether the patient received multiple mental health diagnoses at the time of the ED visit.
Sociodemographic covariates included age, sex, race/ethnicity, and insurance coverage.
Twofold and fourfold increases
Of 100.9 million outpatient ED visits that took place between 2007 and 2016, approximately 8.4 million (8.3%) were for psychiatric or substance use–related diagnoses. Also, the visits were more likely from adults who were younger than 45 years, male, non-Hispanic White, and covered by Medicaid or other public insurance types (58.5%, 52.5%, 65.2%, and 58.6%, respectively).
The overall rate of ED visits for any mental health diagnosis nearly doubled between 2007-2008 and 2015-2016. The rate of visits in which both psychiatric and substance use–related diagnoses increased fourfold during that time span. ED visits involving at least two mental health diagnoses increased twofold.
Additional changes in the number of visits are listed below (for each, P < .001).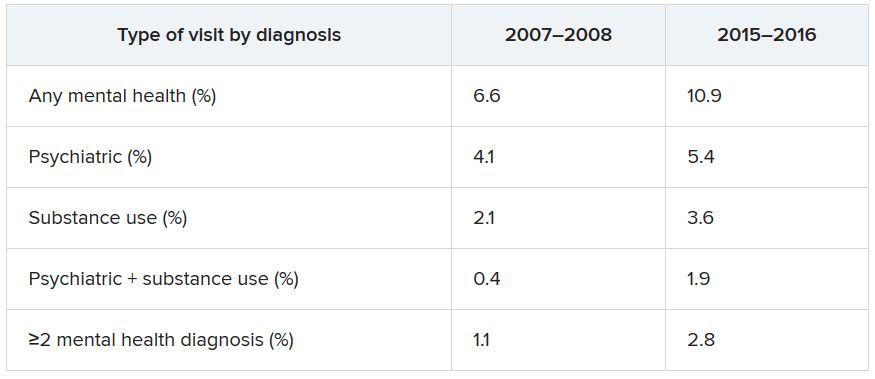
When these comparisons were adjusted for age, sex, and race/ethnicity, “linearly increasing trends of mental health–related ED visits were consistently found in all categories,” the authors reported. No trends were found regarding age, sex, or race/ethnicity. By contrast, mental health–related ED visits in which Medicaid was identified as the primary source of insurance nearly doubled between 2007–2008 and 2015–2016 (from 27.2% to 42.8%).
Other/unspecified psychiatric diagnoses, such as adjustment disorder and personality disorders, almost tripled between 2007-2008 and 2015-2016 (from 1,040 to 2,961 per 100,000 ED visits). ED visits for mood disorders and anxiety disorders also increased over time.
Alcohol-related ED visits were the most common substance use visits, increasing from 1,669 in 2007-2008 to 3,007 per 100,000 visits in 2015-2016. Amphetamine- and opioid-related ED visits more than doubled, and other/unspecified–related ED visits more than tripled during that time.
“One explanation why ED visits for mental health conditions have increased is that substance-related problems, which include overdose/self-injury issues, have increased over time,” Dr. Rhee noted, which “makes sense,” inasmuch as opioid, cannabis, and amphetamine use has increased across the country.
Another explanation is that, although mental health care access has been expanded through the ACA, “people, especially those with lower socioeconomic backgrounds, do not know how to get access to care and are still underserved,” he said.
“If mental health–related ED visits continue to increase in the future, there are several steps to be made. ED providers need to be better equipped with mental health care, and behavioral health should be better integrated as part of the care coordination,” said Dr. Rhee.
He added that reimbursement models across different insurance types, such as Medicare, Medicaid, and private insurance, “should consider expanding their coverage of mental health treatment in ED settings.”
“Canary in the coal mine”
Commenting on the study in an interview, Benjamin Druss, MD, MPH, professor and Rosalynn Carter Chair in Mental Health, Rollins School of Public Health, Emory University, Atlanta, called EDs the “canaries in the coal mine” for the broader health system.
The growing number of ED visits for behavioral problems “could represent both a rise in acute conditions such as substance use and lack of access to outpatient treatment,” said Dr. Druss, who was not involved with the research.
The findings “suggest the importance of strategies to effectively manage patients with behavioral conditions in ED settings and to effectively link them with high-quality outpatient care,” he noted.
Dr. Rhee has received funding from the National Institute on Aging and the American Foundation for Suicide Prevention. The other study authors and Dr. Druss report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
ED visits related to mental health conditions increased nearly twofold from 2007-2008 to 2015-2016, new research suggests.
Data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) showed that, over the 10-year study period, the proportion of ED visits for mental health diagnoses increased from 6.6% to 10.9%, with substance use accounting for much of the increase.
Although there have been policy efforts, such as expanding access to mental health care as part of the Affordable Care Act (ACA) of 2011, the senior author Taeho Greg Rhee, PhD, MSW, said in an interview.
“Treating mental health conditions in EDs is often considered suboptimal” because of limited time for full psychiatric assessment, lack of trained providers, and limited privacy in EDs, said Dr. Rhee of Yale University, New Haven, Conn.
The findings were published online July 28 in The Journal of Clinical Psychiatry.
“Outdated” research
Roughly one-fifth of U.S. adults experience some type of mental, behavioral, or emotional disorder annually. Moreover, the suicide rate has been steadily increasing, and there continues to be a “raging opioid epidemic,” the researchers wrote.
Despite these alarming figures, 57.4% of adults with mental illness reported in 2017 that they had not received any mental health treatment in the past year, reported the investigators.
Previous research has suggested that many adults have difficulty seeking outpatient mental health treatment and may turn to EDs instead. However, most studies of mental health ED use “are by now outdated, as they used data from years prior to the full implementation of the ACA,” the researchers noted.
“More Americans are suffering from mental illness, and given the recent policy efforts of expanding access to mental health care, we were questioning if ED visits due to mental health has changed or not,” Dr. Rhee said.
To investigate the question, the researchers conducted a cross-sectional analysis of data from the NHAMCS, a publicly available dataset provided by the National Center for Health Statistics of the Centers for Disease Control and Prevention.
They grouped psychiatric diagnoses into five categories: mood disorders, anxiety disorders, psychosis or schizophrenia, suicide attempt or ideation, or other/unspecified. Substance use diagnoses were grouped into six categories: alcohol, amphetamine, cannabis, cocaine, opioid, or other/unspecified.
These categories were used to determine the type of disorder a patient had, whether the patient had both psychiatric and substance-related diagnoses, and whether the patient received multiple mental health diagnoses at the time of the ED visit.
Sociodemographic covariates included age, sex, race/ethnicity, and insurance coverage.
Twofold and fourfold increases
Of 100.9 million outpatient ED visits that took place between 2007 and 2016, approximately 8.4 million (8.3%) were for psychiatric or substance use–related diagnoses. Also, the visits were more likely from adults who were younger than 45 years, male, non-Hispanic White, and covered by Medicaid or other public insurance types (58.5%, 52.5%, 65.2%, and 58.6%, respectively).
The overall rate of ED visits for any mental health diagnosis nearly doubled between 2007-2008 and 2015-2016. The rate of visits in which both psychiatric and substance use–related diagnoses increased fourfold during that time span. ED visits involving at least two mental health diagnoses increased twofold.
Additional changes in the number of visits are listed below (for each, P < .001).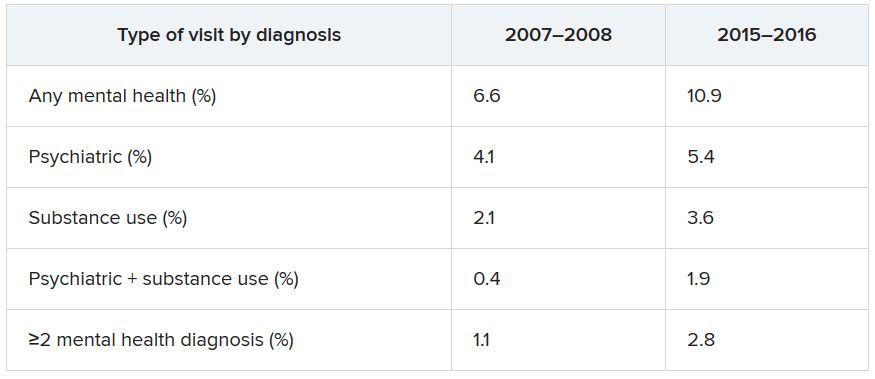
When these comparisons were adjusted for age, sex, and race/ethnicity, “linearly increasing trends of mental health–related ED visits were consistently found in all categories,” the authors reported. No trends were found regarding age, sex, or race/ethnicity. By contrast, mental health–related ED visits in which Medicaid was identified as the primary source of insurance nearly doubled between 2007–2008 and 2015–2016 (from 27.2% to 42.8%).
Other/unspecified psychiatric diagnoses, such as adjustment disorder and personality disorders, almost tripled between 2007-2008 and 2015-2016 (from 1,040 to 2,961 per 100,000 ED visits). ED visits for mood disorders and anxiety disorders also increased over time.
Alcohol-related ED visits were the most common substance use visits, increasing from 1,669 in 2007-2008 to 3,007 per 100,000 visits in 2015-2016. Amphetamine- and opioid-related ED visits more than doubled, and other/unspecified–related ED visits more than tripled during that time.
“One explanation why ED visits for mental health conditions have increased is that substance-related problems, which include overdose/self-injury issues, have increased over time,” Dr. Rhee noted, which “makes sense,” inasmuch as opioid, cannabis, and amphetamine use has increased across the country.
Another explanation is that, although mental health care access has been expanded through the ACA, “people, especially those with lower socioeconomic backgrounds, do not know how to get access to care and are still underserved,” he said.
“If mental health–related ED visits continue to increase in the future, there are several steps to be made. ED providers need to be better equipped with mental health care, and behavioral health should be better integrated as part of the care coordination,” said Dr. Rhee.
He added that reimbursement models across different insurance types, such as Medicare, Medicaid, and private insurance, “should consider expanding their coverage of mental health treatment in ED settings.”
“Canary in the coal mine”
Commenting on the study in an interview, Benjamin Druss, MD, MPH, professor and Rosalynn Carter Chair in Mental Health, Rollins School of Public Health, Emory University, Atlanta, called EDs the “canaries in the coal mine” for the broader health system.
The growing number of ED visits for behavioral problems “could represent both a rise in acute conditions such as substance use and lack of access to outpatient treatment,” said Dr. Druss, who was not involved with the research.
The findings “suggest the importance of strategies to effectively manage patients with behavioral conditions in ED settings and to effectively link them with high-quality outpatient care,” he noted.
Dr. Rhee has received funding from the National Institute on Aging and the American Foundation for Suicide Prevention. The other study authors and Dr. Druss report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
ED visits related to mental health conditions increased nearly twofold from 2007-2008 to 2015-2016, new research suggests.
Data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) showed that, over the 10-year study period, the proportion of ED visits for mental health diagnoses increased from 6.6% to 10.9%, with substance use accounting for much of the increase.
Although there have been policy efforts, such as expanding access to mental health care as part of the Affordable Care Act (ACA) of 2011, the senior author Taeho Greg Rhee, PhD, MSW, said in an interview.
“Treating mental health conditions in EDs is often considered suboptimal” because of limited time for full psychiatric assessment, lack of trained providers, and limited privacy in EDs, said Dr. Rhee of Yale University, New Haven, Conn.
The findings were published online July 28 in The Journal of Clinical Psychiatry.
“Outdated” research
Roughly one-fifth of U.S. adults experience some type of mental, behavioral, or emotional disorder annually. Moreover, the suicide rate has been steadily increasing, and there continues to be a “raging opioid epidemic,” the researchers wrote.
Despite these alarming figures, 57.4% of adults with mental illness reported in 2017 that they had not received any mental health treatment in the past year, reported the investigators.
Previous research has suggested that many adults have difficulty seeking outpatient mental health treatment and may turn to EDs instead. However, most studies of mental health ED use “are by now outdated, as they used data from years prior to the full implementation of the ACA,” the researchers noted.
“More Americans are suffering from mental illness, and given the recent policy efforts of expanding access to mental health care, we were questioning if ED visits due to mental health has changed or not,” Dr. Rhee said.
To investigate the question, the researchers conducted a cross-sectional analysis of data from the NHAMCS, a publicly available dataset provided by the National Center for Health Statistics of the Centers for Disease Control and Prevention.
They grouped psychiatric diagnoses into five categories: mood disorders, anxiety disorders, psychosis or schizophrenia, suicide attempt or ideation, or other/unspecified. Substance use diagnoses were grouped into six categories: alcohol, amphetamine, cannabis, cocaine, opioid, or other/unspecified.
These categories were used to determine the type of disorder a patient had, whether the patient had both psychiatric and substance-related diagnoses, and whether the patient received multiple mental health diagnoses at the time of the ED visit.
Sociodemographic covariates included age, sex, race/ethnicity, and insurance coverage.
Twofold and fourfold increases
Of 100.9 million outpatient ED visits that took place between 2007 and 2016, approximately 8.4 million (8.3%) were for psychiatric or substance use–related diagnoses. Also, the visits were more likely from adults who were younger than 45 years, male, non-Hispanic White, and covered by Medicaid or other public insurance types (58.5%, 52.5%, 65.2%, and 58.6%, respectively).
The overall rate of ED visits for any mental health diagnosis nearly doubled between 2007-2008 and 2015-2016. The rate of visits in which both psychiatric and substance use–related diagnoses increased fourfold during that time span. ED visits involving at least two mental health diagnoses increased twofold.
Additional changes in the number of visits are listed below (for each, P < .001).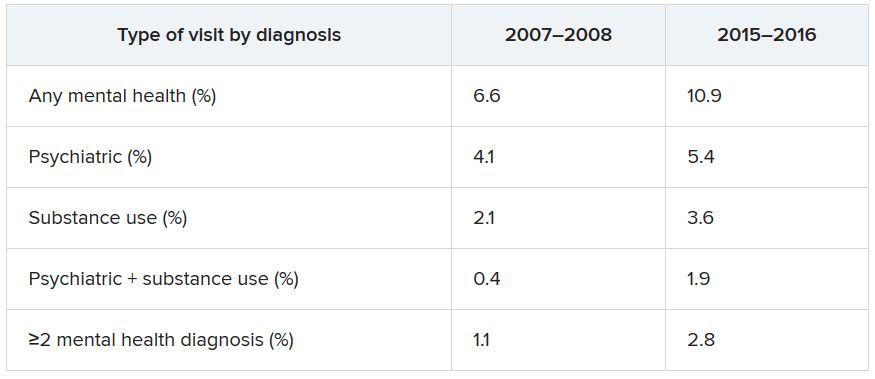
When these comparisons were adjusted for age, sex, and race/ethnicity, “linearly increasing trends of mental health–related ED visits were consistently found in all categories,” the authors reported. No trends were found regarding age, sex, or race/ethnicity. By contrast, mental health–related ED visits in which Medicaid was identified as the primary source of insurance nearly doubled between 2007–2008 and 2015–2016 (from 27.2% to 42.8%).
Other/unspecified psychiatric diagnoses, such as adjustment disorder and personality disorders, almost tripled between 2007-2008 and 2015-2016 (from 1,040 to 2,961 per 100,000 ED visits). ED visits for mood disorders and anxiety disorders also increased over time.
Alcohol-related ED visits were the most common substance use visits, increasing from 1,669 in 2007-2008 to 3,007 per 100,000 visits in 2015-2016. Amphetamine- and opioid-related ED visits more than doubled, and other/unspecified–related ED visits more than tripled during that time.
“One explanation why ED visits for mental health conditions have increased is that substance-related problems, which include overdose/self-injury issues, have increased over time,” Dr. Rhee noted, which “makes sense,” inasmuch as opioid, cannabis, and amphetamine use has increased across the country.
Another explanation is that, although mental health care access has been expanded through the ACA, “people, especially those with lower socioeconomic backgrounds, do not know how to get access to care and are still underserved,” he said.
“If mental health–related ED visits continue to increase in the future, there are several steps to be made. ED providers need to be better equipped with mental health care, and behavioral health should be better integrated as part of the care coordination,” said Dr. Rhee.
He added that reimbursement models across different insurance types, such as Medicare, Medicaid, and private insurance, “should consider expanding their coverage of mental health treatment in ED settings.”
“Canary in the coal mine”
Commenting on the study in an interview, Benjamin Druss, MD, MPH, professor and Rosalynn Carter Chair in Mental Health, Rollins School of Public Health, Emory University, Atlanta, called EDs the “canaries in the coal mine” for the broader health system.
The growing number of ED visits for behavioral problems “could represent both a rise in acute conditions such as substance use and lack of access to outpatient treatment,” said Dr. Druss, who was not involved with the research.
The findings “suggest the importance of strategies to effectively manage patients with behavioral conditions in ED settings and to effectively link them with high-quality outpatient care,” he noted.
Dr. Rhee has received funding from the National Institute on Aging and the American Foundation for Suicide Prevention. The other study authors and Dr. Druss report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Chronicles of cancer: A history of mammography, part 1
Technological imperatives
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Technological imperatives
Technological imperatives
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Educational intervention curbs use of antibiotics for respiratory infections
A clinician education program significantly reduced overall antibiotic prescribing during pediatric visits for acute respiratory tract infections, according to data from 57 clinicians who participated in an intervention.
In a study published in Pediatrics, Matthew P. Kronman, MD, of the University of Washington, Seattle, and associates randomized 57 clinicians at 19 pediatric practices to a stepped-wedge clinical trial. The study included visits for acute otitis media, bronchitis, pharyngitis, sinusitis, and upper respiratory infections (defined as ARTI visits) for children aged 6 months to less than 11 years, for a total of 72,723 ARTI visits by 29,762 patients. The primary outcome was overall antibiotic prescribing for ARTI visits.
For the intervention, known as the Dialogue Around Respiratory Illness Treatment (DART) quality improvement (QI) program, clinicians received three program modules containing online tutorials and webinars. These professionally-produced modules included a combination of evidence-based communication strategies and antibiotic prescribing, booster video vignettes, and individualized antibiotic prescribing feedback reports over 11 months.
Overall, the probability of antibiotic prescribing for ARTI visits decreased by 7% (adjusted relative risk 0.93) from baseline to a 2- to 8-month postintervention in an adjusted intent-to-treat analysis.
Analysis of secondary outcomes revealed that prescribing any antibiotics for viral ARTI decreased by 40% during the postintervention period compared to baseline (aRR 0.60).
In addition, second-line antibiotic prescribing decreased from baseline by 34% for streptococcal pharyngitis (aRR 0.66), and by 41% for sinusitis (aRR 0.59); however there was no significant change in prescribing for acute otitis media, the researchers said.
The study findings were limited by several factors including the potential for biased results because of the randomization of clinicians from multiple practices and the potential for clinicians to change their prescribing habits after the start of the study, Dr. Kronman and colleagues noted.
In addition, the study did not include complete data on rapid streptococcal antigen testing, which might eliminate some children from the study population, and the relatively short postintervention period “may not represent the true long-term intervention durability may not represent the true long-term intervention durability,” they said.
However, the results support the potential of the DART program. “The 7% reduction in antibiotic prescribing for all ARTIs, if extrapolated to all ambulatory ARTI visits to pediatricians nationally, would represent 1.5 million fewer antibiotic prescriptions for children with ARTI annually,” they wrote.
“Providing online communication training and evidence-based antibiotic prescribing education in combination with individualized antibiotic prescribing feedback reports may help achieve national goals of reducing unnecessary outpatient antibiotic prescribing for children,” Dr. Kronman and associates concluded.
Combining interventions are key to reducing unnecessary antibiotics use in pediatric ambulatory care, Rana F. Hamdy, MD, MPH, of Children’s National Hospital, Washington, , and Sophie E. Katz, MD, of Vanderbilt University, Nashville, Tenn., wrote in an accompanying editorial (Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-012922).
The researchers in the current study “seem to recognize that clinicians are adult learners, and they combine interventions to implement these adult learning theory tenets to improve appropriate antibiotic prescribing,” they wrote. The DART intervention combined best practices training, communications training, and individualized antibiotic prescribing feedback reports to improve communication between providers and families “especially when faced with a situation in which a parent or guardian might expect an antibiotic prescription but the provider does not think one is necessary,” Dr. Hamdy and Dr. Katz said.
Overall, the findings suggest that the interventions work best in combination vs. being used alone, although the study did not evaluate the separate contributions of each intervention, the editorialists wrote.
“In the current study, nonengaged physicians had an increase in second-line antibiotic prescribing, whereas the engaged physicians had a decrease in second-line antibiotic prescribing,” they noted. “This suggests that the addition of communications training could mitigate the undesirable effects that may result from solely using feedback reports.”
“Each year, U.S. children are prescribed as many as 10 million unnecessary antibiotic courses for acute respiratory tract infections,” Kristina A. Bryant, MD, of the University of Louisville, Ky., said in an interview. “Some of these prescriptions result in side effects or allergic reactions, and they contribute to growing antibiotic resistance. We need effective interventions to reduce antibiotic prescribing.”
Although the DART modules are free and available online, busy clinicians might struggle to find time to view them consistently, said Dr. Bryant.
“One advantage of the study design was that information was pushed to clinicians along with communication booster videos,” she said. “We know that education and reinforcement over time works better than a one and done approach.
“Study participants also received feedback over time about their prescribing habits, which can be a powerful motivator for change, although not all clinicians may have easy access to these reports,” she noted.
To overcome some of the barriers to using the modules, clinicians who are “interested in improving their prescribing could work with their office managers to develop antibiotic prescribing reports and schedule reminders to review them,” said Dr. Bryant.
“An individual could commit to education and review of his or her own prescribing patterns, but support from one’s partners and shared accountability is likely to be even more effective,” she said. “Sharing data within a practice and exploring differences in prescribing patterns can drive improvement.
“Spaced education and regular feedback about prescribing patterns can improve antibiotic prescribing for pharyngitis and sinusitis, and reduce antibiotic prescriptions for ARTIs,” Dr. Bryant said. The take-home from the study is that it should prompt anyone who prescribes antibiotics for children to ask themselves how they can improve their own prescribing habits.
“In this study, prescribing for viral ARTIs was reduced but not eliminated. We need additional studies to further reduce unnecessary antibiotic use,” Dr. Bryant said.
In addition, areas for future research could include longer-term follow-up. “Study participants were followed for 2 to 8 months after the intervention ended in June 2018. It would be interesting to know about their prescribing practices now, and if the changes observed in the study were durable,” she concluded.
The study was supported by the National Institutes of Health, along with additional infrastructure funding from the American Academy of Pediatrics and the Health Resources and Services Administration of the Department of Health and Human Services. The researchers had no financial conflicts to disclose.
Dr. Hamdy and Dr. Katz had no financial conflicts to disclose, but Dr. Katz disclosed grant support through the Centers for Disease Control and Prevention as a recipient of the Leadership in Epidemiology, Antimicrobial Stewardship, and Public Health fellowship, sponsored by the Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, and Pediatric Infectious Diseases Society.
Dr. Bryant disclosed serving as an investigator on multicenter clinical vaccine trials funded by Pfizer (but not in the last year). She also serves as the current president of the Pediatric Infectious Diseases Society, but the opinions expressed here are her own and do not necessarily reflect the views of PIDS.
SOURCE: Kronman MP et al. Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-0038.
A clinician education program significantly reduced overall antibiotic prescribing during pediatric visits for acute respiratory tract infections, according to data from 57 clinicians who participated in an intervention.
In a study published in Pediatrics, Matthew P. Kronman, MD, of the University of Washington, Seattle, and associates randomized 57 clinicians at 19 pediatric practices to a stepped-wedge clinical trial. The study included visits for acute otitis media, bronchitis, pharyngitis, sinusitis, and upper respiratory infections (defined as ARTI visits) for children aged 6 months to less than 11 years, for a total of 72,723 ARTI visits by 29,762 patients. The primary outcome was overall antibiotic prescribing for ARTI visits.
For the intervention, known as the Dialogue Around Respiratory Illness Treatment (DART) quality improvement (QI) program, clinicians received three program modules containing online tutorials and webinars. These professionally-produced modules included a combination of evidence-based communication strategies and antibiotic prescribing, booster video vignettes, and individualized antibiotic prescribing feedback reports over 11 months.
Overall, the probability of antibiotic prescribing for ARTI visits decreased by 7% (adjusted relative risk 0.93) from baseline to a 2- to 8-month postintervention in an adjusted intent-to-treat analysis.
Analysis of secondary outcomes revealed that prescribing any antibiotics for viral ARTI decreased by 40% during the postintervention period compared to baseline (aRR 0.60).
In addition, second-line antibiotic prescribing decreased from baseline by 34% for streptococcal pharyngitis (aRR 0.66), and by 41% for sinusitis (aRR 0.59); however there was no significant change in prescribing for acute otitis media, the researchers said.
The study findings were limited by several factors including the potential for biased results because of the randomization of clinicians from multiple practices and the potential for clinicians to change their prescribing habits after the start of the study, Dr. Kronman and colleagues noted.
In addition, the study did not include complete data on rapid streptococcal antigen testing, which might eliminate some children from the study population, and the relatively short postintervention period “may not represent the true long-term intervention durability may not represent the true long-term intervention durability,” they said.
However, the results support the potential of the DART program. “The 7% reduction in antibiotic prescribing for all ARTIs, if extrapolated to all ambulatory ARTI visits to pediatricians nationally, would represent 1.5 million fewer antibiotic prescriptions for children with ARTI annually,” they wrote.
“Providing online communication training and evidence-based antibiotic prescribing education in combination with individualized antibiotic prescribing feedback reports may help achieve national goals of reducing unnecessary outpatient antibiotic prescribing for children,” Dr. Kronman and associates concluded.
Combining interventions are key to reducing unnecessary antibiotics use in pediatric ambulatory care, Rana F. Hamdy, MD, MPH, of Children’s National Hospital, Washington, , and Sophie E. Katz, MD, of Vanderbilt University, Nashville, Tenn., wrote in an accompanying editorial (Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-012922).
The researchers in the current study “seem to recognize that clinicians are adult learners, and they combine interventions to implement these adult learning theory tenets to improve appropriate antibiotic prescribing,” they wrote. The DART intervention combined best practices training, communications training, and individualized antibiotic prescribing feedback reports to improve communication between providers and families “especially when faced with a situation in which a parent or guardian might expect an antibiotic prescription but the provider does not think one is necessary,” Dr. Hamdy and Dr. Katz said.
Overall, the findings suggest that the interventions work best in combination vs. being used alone, although the study did not evaluate the separate contributions of each intervention, the editorialists wrote.
“In the current study, nonengaged physicians had an increase in second-line antibiotic prescribing, whereas the engaged physicians had a decrease in second-line antibiotic prescribing,” they noted. “This suggests that the addition of communications training could mitigate the undesirable effects that may result from solely using feedback reports.”
“Each year, U.S. children are prescribed as many as 10 million unnecessary antibiotic courses for acute respiratory tract infections,” Kristina A. Bryant, MD, of the University of Louisville, Ky., said in an interview. “Some of these prescriptions result in side effects or allergic reactions, and they contribute to growing antibiotic resistance. We need effective interventions to reduce antibiotic prescribing.”
Although the DART modules are free and available online, busy clinicians might struggle to find time to view them consistently, said Dr. Bryant.
“One advantage of the study design was that information was pushed to clinicians along with communication booster videos,” she said. “We know that education and reinforcement over time works better than a one and done approach.
“Study participants also received feedback over time about their prescribing habits, which can be a powerful motivator for change, although not all clinicians may have easy access to these reports,” she noted.
To overcome some of the barriers to using the modules, clinicians who are “interested in improving their prescribing could work with their office managers to develop antibiotic prescribing reports and schedule reminders to review them,” said Dr. Bryant.
“An individual could commit to education and review of his or her own prescribing patterns, but support from one’s partners and shared accountability is likely to be even more effective,” she said. “Sharing data within a practice and exploring differences in prescribing patterns can drive improvement.
“Spaced education and regular feedback about prescribing patterns can improve antibiotic prescribing for pharyngitis and sinusitis, and reduce antibiotic prescriptions for ARTIs,” Dr. Bryant said. The take-home from the study is that it should prompt anyone who prescribes antibiotics for children to ask themselves how they can improve their own prescribing habits.
“In this study, prescribing for viral ARTIs was reduced but not eliminated. We need additional studies to further reduce unnecessary antibiotic use,” Dr. Bryant said.
In addition, areas for future research could include longer-term follow-up. “Study participants were followed for 2 to 8 months after the intervention ended in June 2018. It would be interesting to know about their prescribing practices now, and if the changes observed in the study were durable,” she concluded.
The study was supported by the National Institutes of Health, along with additional infrastructure funding from the American Academy of Pediatrics and the Health Resources and Services Administration of the Department of Health and Human Services. The researchers had no financial conflicts to disclose.
Dr. Hamdy and Dr. Katz had no financial conflicts to disclose, but Dr. Katz disclosed grant support through the Centers for Disease Control and Prevention as a recipient of the Leadership in Epidemiology, Antimicrobial Stewardship, and Public Health fellowship, sponsored by the Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, and Pediatric Infectious Diseases Society.
Dr. Bryant disclosed serving as an investigator on multicenter clinical vaccine trials funded by Pfizer (but not in the last year). She also serves as the current president of the Pediatric Infectious Diseases Society, but the opinions expressed here are her own and do not necessarily reflect the views of PIDS.
SOURCE: Kronman MP et al. Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-0038.
A clinician education program significantly reduced overall antibiotic prescribing during pediatric visits for acute respiratory tract infections, according to data from 57 clinicians who participated in an intervention.
In a study published in Pediatrics, Matthew P. Kronman, MD, of the University of Washington, Seattle, and associates randomized 57 clinicians at 19 pediatric practices to a stepped-wedge clinical trial. The study included visits for acute otitis media, bronchitis, pharyngitis, sinusitis, and upper respiratory infections (defined as ARTI visits) for children aged 6 months to less than 11 years, for a total of 72,723 ARTI visits by 29,762 patients. The primary outcome was overall antibiotic prescribing for ARTI visits.
For the intervention, known as the Dialogue Around Respiratory Illness Treatment (DART) quality improvement (QI) program, clinicians received three program modules containing online tutorials and webinars. These professionally-produced modules included a combination of evidence-based communication strategies and antibiotic prescribing, booster video vignettes, and individualized antibiotic prescribing feedback reports over 11 months.
Overall, the probability of antibiotic prescribing for ARTI visits decreased by 7% (adjusted relative risk 0.93) from baseline to a 2- to 8-month postintervention in an adjusted intent-to-treat analysis.
Analysis of secondary outcomes revealed that prescribing any antibiotics for viral ARTI decreased by 40% during the postintervention period compared to baseline (aRR 0.60).
In addition, second-line antibiotic prescribing decreased from baseline by 34% for streptococcal pharyngitis (aRR 0.66), and by 41% for sinusitis (aRR 0.59); however there was no significant change in prescribing for acute otitis media, the researchers said.
The study findings were limited by several factors including the potential for biased results because of the randomization of clinicians from multiple practices and the potential for clinicians to change their prescribing habits after the start of the study, Dr. Kronman and colleagues noted.
In addition, the study did not include complete data on rapid streptococcal antigen testing, which might eliminate some children from the study population, and the relatively short postintervention period “may not represent the true long-term intervention durability may not represent the true long-term intervention durability,” they said.
However, the results support the potential of the DART program. “The 7% reduction in antibiotic prescribing for all ARTIs, if extrapolated to all ambulatory ARTI visits to pediatricians nationally, would represent 1.5 million fewer antibiotic prescriptions for children with ARTI annually,” they wrote.
“Providing online communication training and evidence-based antibiotic prescribing education in combination with individualized antibiotic prescribing feedback reports may help achieve national goals of reducing unnecessary outpatient antibiotic prescribing for children,” Dr. Kronman and associates concluded.
Combining interventions are key to reducing unnecessary antibiotics use in pediatric ambulatory care, Rana F. Hamdy, MD, MPH, of Children’s National Hospital, Washington, , and Sophie E. Katz, MD, of Vanderbilt University, Nashville, Tenn., wrote in an accompanying editorial (Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-012922).
The researchers in the current study “seem to recognize that clinicians are adult learners, and they combine interventions to implement these adult learning theory tenets to improve appropriate antibiotic prescribing,” they wrote. The DART intervention combined best practices training, communications training, and individualized antibiotic prescribing feedback reports to improve communication between providers and families “especially when faced with a situation in which a parent or guardian might expect an antibiotic prescription but the provider does not think one is necessary,” Dr. Hamdy and Dr. Katz said.
Overall, the findings suggest that the interventions work best in combination vs. being used alone, although the study did not evaluate the separate contributions of each intervention, the editorialists wrote.
“In the current study, nonengaged physicians had an increase in second-line antibiotic prescribing, whereas the engaged physicians had a decrease in second-line antibiotic prescribing,” they noted. “This suggests that the addition of communications training could mitigate the undesirable effects that may result from solely using feedback reports.”
“Each year, U.S. children are prescribed as many as 10 million unnecessary antibiotic courses for acute respiratory tract infections,” Kristina A. Bryant, MD, of the University of Louisville, Ky., said in an interview. “Some of these prescriptions result in side effects or allergic reactions, and they contribute to growing antibiotic resistance. We need effective interventions to reduce antibiotic prescribing.”
Although the DART modules are free and available online, busy clinicians might struggle to find time to view them consistently, said Dr. Bryant.
“One advantage of the study design was that information was pushed to clinicians along with communication booster videos,” she said. “We know that education and reinforcement over time works better than a one and done approach.
“Study participants also received feedback over time about their prescribing habits, which can be a powerful motivator for change, although not all clinicians may have easy access to these reports,” she noted.
To overcome some of the barriers to using the modules, clinicians who are “interested in improving their prescribing could work with their office managers to develop antibiotic prescribing reports and schedule reminders to review them,” said Dr. Bryant.
“An individual could commit to education and review of his or her own prescribing patterns, but support from one’s partners and shared accountability is likely to be even more effective,” she said. “Sharing data within a practice and exploring differences in prescribing patterns can drive improvement.
“Spaced education and regular feedback about prescribing patterns can improve antibiotic prescribing for pharyngitis and sinusitis, and reduce antibiotic prescriptions for ARTIs,” Dr. Bryant said. The take-home from the study is that it should prompt anyone who prescribes antibiotics for children to ask themselves how they can improve their own prescribing habits.
“In this study, prescribing for viral ARTIs was reduced but not eliminated. We need additional studies to further reduce unnecessary antibiotic use,” Dr. Bryant said.
In addition, areas for future research could include longer-term follow-up. “Study participants were followed for 2 to 8 months after the intervention ended in June 2018. It would be interesting to know about their prescribing practices now, and if the changes observed in the study were durable,” she concluded.
The study was supported by the National Institutes of Health, along with additional infrastructure funding from the American Academy of Pediatrics and the Health Resources and Services Administration of the Department of Health and Human Services. The researchers had no financial conflicts to disclose.
Dr. Hamdy and Dr. Katz had no financial conflicts to disclose, but Dr. Katz disclosed grant support through the Centers for Disease Control and Prevention as a recipient of the Leadership in Epidemiology, Antimicrobial Stewardship, and Public Health fellowship, sponsored by the Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, and Pediatric Infectious Diseases Society.
Dr. Bryant disclosed serving as an investigator on multicenter clinical vaccine trials funded by Pfizer (but not in the last year). She also serves as the current president of the Pediatric Infectious Diseases Society, but the opinions expressed here are her own and do not necessarily reflect the views of PIDS.
SOURCE: Kronman MP et al. Pediatrics. 2020 Aug 3. doi: 10.1542/peds.2020-0038.
FROM PEDIATRICS