User login
COVID-19–associated coagulopathy
Coronavirus disease 2019 (COVID-19) is a viral illness caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), currently causing a pandemic affecting many countries around the world, beginning in December 2019 and spreading rapidly on a global scale since. Globally, its burden has been increasing rapidly, with more than 1.2 million people testing positive for the illness and 123,000 people losing their lives, as per April 15th’s WHO COVID-19 Situation Report.1 These numbers are increasing with each passing day. Clinically, SARS-CoV-2 has a highly variable course, ranging from mild disease manifested as a self-limited illness (seen in younger and healthier patients) to severe pneumonia/ARDS and multiorgan failure with intravascular coagulopathy.2
In this article, we intend to investigate and establish a comprehensive review of COVID-19–associated coagulopathy mechanisms, laboratory findings, and current management guidelines put forth by various societies globally.
Mechanism of coagulopathy
COVID-19–associated coagulopathy has been shown to predispose to both arterial and venous thrombosis through excessive inflammation and hypoxia, leading to activation of the coagulation cascade and consumption of coagulation factors, resulting in microvascular thrombosis.3 Though the exact pathophysiology for the activation of this cascade is not known, the proposed mechanism has been: endothelial damage triggering platelet activation within the lung, leading to aggregation, thrombosis, and consumption of platelets in the lung.2,5,6
Fox et al. noted similar coagulopathy findings of four deceased COVID-19 patients. Autopsy results concluded that the dominant process was diffuse alveolar damage, notable CD4+ aggregates around thrombosed small vessels, significant associated hemorrhage, and thrombotic microangiopathy restricted to the lungs. The proposed mechanism was the activation of megakaryocytes, possibly native to the lung, with platelet aggregation, formation of platelet-rich clots, and fibrin deposition playing a major role.4
It has been noted that diabetic patients are at an increased risk of vascular events and hypercoagulability with COVID-19.7 COVID-19 can also cause livedo reticularis and acrocyanosis because of the microthrombosis in the cutaneous vasculature secondary to underlying coagulopathy, as reported in a case report of two U.S. patients with COVID-19.8
Clinical and laboratory abnormalities
A recent study reported from Netherlands by Klok et al. analyzed 184 ICU patients with COVID-19 pneumonia and concluded that the cumulative incidence of acute pulmonary embolism (PE), deep vein thrombosis (DVT), ischemic stroke, MI, or systemic arterial embolism was 31% (95% confidence interval, 20%-41%). PE was the most frequent thrombotic complication and was noted in 81% of patients. Coagulopathy, defined as spontaneous prolongation of prothrombin time (PT) > 3s or activated partial thromboplastin time (aPTT) > 5s, was reported as an independent predictor of thrombotic complications.3
Hematologic abnormalities that were noted in COVID-19 coagulopathy include: decreased platelet counts, decreased fibrinogen levels, elevated PT/INR, elevated partial thromboplastin time (PTT), and elevated d-dimer.9,10 In a retrospective analysis9 by Tang et al., 71.4% of nonsurvivors and 0.6% of survivors had met the criteria of disseminated intravascular coagulation (DIC) during their hospital stay. Nonsurvivors of COVID-19 had statistically significant elevation of d-dimer levels, FDP levels, PT, and aPTT, when compared to survivors (P < .05). The overall mortality in this study was reported as 11.5%.9 In addition, elevated d-dimer, fibrin and fibrinogen degradation product (FDP) levels and longer PT and aPTT were associated with poor prognosis.
Thus, d-dimer, PT, and platelet count should be measured in all patients who present with COVID-19 infection. We can also suggest that in patients with markedly elevated d-dimer (three- to fourfold increase), admission to hospital should be considered even in the absence of severe clinical symptoms.11
COVID-19 coagulopathy management
In a retrospective study9 of 449 patients with severe COVID-19 from Wuhan, China, by Tang et al., 99 patients mainly received low-weight molecular heparin (LMWH) for 7 days or longer. No difference in 28-day mortality was noted between heparin users and nonusers (30.3% vs. 29.7%; P = .910). A lower 28-day mortality rate was noted in heparin patients with sepsis-induced coagulopathy score of ≥4.0 (40.0% vs. 64.2%; P = .029) or a d-dimer level greater than sixfold of upper limit of normal, compared with nonusers of heparin.12
Another small study of seven COVID-19 patients with acroischemia in China demonstrated that administering LMWH was successful at decreasing the d-dimer and fibrinogen degradation product levels but noted no significant improvement in clinical symptoms.13
Recently, the International Society of Thrombosis and Hemostasis and American Society of Hematology published recommendations and guidelines regarding the recognition and management of coagulopathy in COVID-19.11 Prophylactic anticoagulation therapy with LMWH was recommended in all hospitalized patients with COVID-19, provided there was an absence of any contraindications (active bleeding, platelet count less than 25 x 109/L and fibrinogen less than 0.5 g/dL). Anticoagulation with LMWH was associated with better prognosis in severe COVID-19 patients and in COVID-19 patients with markedly elevated d-dimer, as it also has anti-inflammatory effects.12 This anti-inflammatory property of heparin has been documented in previous studies but the underlying mechanism is unknown and more research is required.14,15
Despite coagulopathy being noticed with cases of COVID-19, bleeding has been a rare finding in COVID-19 infections. If bleeding is noted, recommendations were made to keep platelet levels greater than 50 x109/L, fibrinogen less than 2.0 g/L, and INR [international normalized ratio] greater than 1.5.11 Mechanical thromboprophylaxis should be used when pharmacologic thromboprophylaxis is contraindicated.16
COVID-19 patients with new diagnoses of venous thromboembolism (VTE) or atrial fibrillation should be prescribed therapeutic anticoagulation. Patients who are already on anticoagulation for VTE or atrial fibrillation should continue their therapy unless the platelet count is less than 30-50x109/L or if the fibrinogen is less than 1.0 g/L.16
Conclusion
Coagulopathies associated with COVID-19 infections have been documented in several studies around the world, and it has been shown to be fatal in some cases. Despite documentation, the mechanism behind this coagulopathy is not well understood. Because of the potentially lethal complications associated with coagulopathies, early recognition and anticoagulation is imperative to improve clinical outcomes. These results are very preliminary: More studies are required to understand the role of anticoagulation and its effect on the morbidity and mortality associated with COVID-19–associated coagulopathy.
Dr. Yeruva is a board-certified hematologist/medical oncologist with WellSpan Health and clinical assistant professor of internal medicine, Penn State University, Hershey. Mr. Henderson is a third-year graduate-entry medical student at the Royal College of Surgeons in Ireland with interests in family medicine, dermatology, and tropical diseases. Dr. Al-Tawfiq is a consultant of internal medicine & infectious diseases, and the director of quality at Johns Hopkins Aramco Healthcare in Dhahran, Saudi Arabia, an adjunct associate professor of infectious diseases, molecular medicine and clinical pharmacology at Johns Hopkins University School of Medicine, and adjunct associate professor at Indiana University School of Medicine, Indianapolis. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals.
References
1. World Health Organization. Coronavirus disease (COVID-2019) situation reports.
2. Lippi G et al. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020 Mar 13. 506:145-8. doi: 10.1016/j.cca.2020.03.022.
3. Klok FA et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Throm Res. 2020;18(4):844-7. doi: 10.1016/j.thromres.2020.04.013.
4. Fox S et al. Pulmonary and cardiac pathology in Covid-19: The first autopsy series from New Orleans. MedRxiv. 2020 Apr 10. doi: 10.1101/2020.04.06.20050575.
5. Yang M et al. Thrombocytopenia in patients with severe acute respiratory syndrome (review). Hematology 2013 Sep 4. doi: 10.1080/1024533040002617.
6. Giannis D et al. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020 June. doi: 10.1016/j.jcv.2020.104362.
7. Guo W et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
8. Manalo IF et al. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J Am Acad Dermat. 2020 Apr. doi: 10.1016/j.jaad.2020.04.018.
9. Tang N et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020 Feb 19. doi: 10.1111/jth.14768, 18: 844-847.
10. Huang C et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Jan 24. doi: 10.1016/S0140-6736(20)30183-5.
11. Thachil J et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020 Mar 25. doi: 10.1111/JTH.14810.
12. Tang N et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 Mar 27. doi: 10.1111/JTH.14817.
13. Zhang Y et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020 Mar 28. doi: 10.3760/cma.j.issn.0253-2727.2020.0006.
14. Poterucha TJ et al. More than an anticoagulant: Do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017. doi: 10.1160/TH16-08-0620.
15. Mousavi S et al. Anti-inflammatory effects of heparin and its derivatives: A systematic review. Adv Pharmacol Pharm Sci. 2015 May 12. doi: 10.1155/2015/507151.
16. Kreuziger L et al. COVID-19 and VTE/anticoagulation: Frequently asked questions. American Society of Hematology. 2020 Apr 17.
Coronavirus disease 2019 (COVID-19) is a viral illness caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), currently causing a pandemic affecting many countries around the world, beginning in December 2019 and spreading rapidly on a global scale since. Globally, its burden has been increasing rapidly, with more than 1.2 million people testing positive for the illness and 123,000 people losing their lives, as per April 15th’s WHO COVID-19 Situation Report.1 These numbers are increasing with each passing day. Clinically, SARS-CoV-2 has a highly variable course, ranging from mild disease manifested as a self-limited illness (seen in younger and healthier patients) to severe pneumonia/ARDS and multiorgan failure with intravascular coagulopathy.2
In this article, we intend to investigate and establish a comprehensive review of COVID-19–associated coagulopathy mechanisms, laboratory findings, and current management guidelines put forth by various societies globally.
Mechanism of coagulopathy
COVID-19–associated coagulopathy has been shown to predispose to both arterial and venous thrombosis through excessive inflammation and hypoxia, leading to activation of the coagulation cascade and consumption of coagulation factors, resulting in microvascular thrombosis.3 Though the exact pathophysiology for the activation of this cascade is not known, the proposed mechanism has been: endothelial damage triggering platelet activation within the lung, leading to aggregation, thrombosis, and consumption of platelets in the lung.2,5,6
Fox et al. noted similar coagulopathy findings of four deceased COVID-19 patients. Autopsy results concluded that the dominant process was diffuse alveolar damage, notable CD4+ aggregates around thrombosed small vessels, significant associated hemorrhage, and thrombotic microangiopathy restricted to the lungs. The proposed mechanism was the activation of megakaryocytes, possibly native to the lung, with platelet aggregation, formation of platelet-rich clots, and fibrin deposition playing a major role.4
It has been noted that diabetic patients are at an increased risk of vascular events and hypercoagulability with COVID-19.7 COVID-19 can also cause livedo reticularis and acrocyanosis because of the microthrombosis in the cutaneous vasculature secondary to underlying coagulopathy, as reported in a case report of two U.S. patients with COVID-19.8
Clinical and laboratory abnormalities
A recent study reported from Netherlands by Klok et al. analyzed 184 ICU patients with COVID-19 pneumonia and concluded that the cumulative incidence of acute pulmonary embolism (PE), deep vein thrombosis (DVT), ischemic stroke, MI, or systemic arterial embolism was 31% (95% confidence interval, 20%-41%). PE was the most frequent thrombotic complication and was noted in 81% of patients. Coagulopathy, defined as spontaneous prolongation of prothrombin time (PT) > 3s or activated partial thromboplastin time (aPTT) > 5s, was reported as an independent predictor of thrombotic complications.3
Hematologic abnormalities that were noted in COVID-19 coagulopathy include: decreased platelet counts, decreased fibrinogen levels, elevated PT/INR, elevated partial thromboplastin time (PTT), and elevated d-dimer.9,10 In a retrospective analysis9 by Tang et al., 71.4% of nonsurvivors and 0.6% of survivors had met the criteria of disseminated intravascular coagulation (DIC) during their hospital stay. Nonsurvivors of COVID-19 had statistically significant elevation of d-dimer levels, FDP levels, PT, and aPTT, when compared to survivors (P < .05). The overall mortality in this study was reported as 11.5%.9 In addition, elevated d-dimer, fibrin and fibrinogen degradation product (FDP) levels and longer PT and aPTT were associated with poor prognosis.
Thus, d-dimer, PT, and platelet count should be measured in all patients who present with COVID-19 infection. We can also suggest that in patients with markedly elevated d-dimer (three- to fourfold increase), admission to hospital should be considered even in the absence of severe clinical symptoms.11
COVID-19 coagulopathy management
In a retrospective study9 of 449 patients with severe COVID-19 from Wuhan, China, by Tang et al., 99 patients mainly received low-weight molecular heparin (LMWH) for 7 days or longer. No difference in 28-day mortality was noted between heparin users and nonusers (30.3% vs. 29.7%; P = .910). A lower 28-day mortality rate was noted in heparin patients with sepsis-induced coagulopathy score of ≥4.0 (40.0% vs. 64.2%; P = .029) or a d-dimer level greater than sixfold of upper limit of normal, compared with nonusers of heparin.12
Another small study of seven COVID-19 patients with acroischemia in China demonstrated that administering LMWH was successful at decreasing the d-dimer and fibrinogen degradation product levels but noted no significant improvement in clinical symptoms.13
Recently, the International Society of Thrombosis and Hemostasis and American Society of Hematology published recommendations and guidelines regarding the recognition and management of coagulopathy in COVID-19.11 Prophylactic anticoagulation therapy with LMWH was recommended in all hospitalized patients with COVID-19, provided there was an absence of any contraindications (active bleeding, platelet count less than 25 x 109/L and fibrinogen less than 0.5 g/dL). Anticoagulation with LMWH was associated with better prognosis in severe COVID-19 patients and in COVID-19 patients with markedly elevated d-dimer, as it also has anti-inflammatory effects.12 This anti-inflammatory property of heparin has been documented in previous studies but the underlying mechanism is unknown and more research is required.14,15
Despite coagulopathy being noticed with cases of COVID-19, bleeding has been a rare finding in COVID-19 infections. If bleeding is noted, recommendations were made to keep platelet levels greater than 50 x109/L, fibrinogen less than 2.0 g/L, and INR [international normalized ratio] greater than 1.5.11 Mechanical thromboprophylaxis should be used when pharmacologic thromboprophylaxis is contraindicated.16
COVID-19 patients with new diagnoses of venous thromboembolism (VTE) or atrial fibrillation should be prescribed therapeutic anticoagulation. Patients who are already on anticoagulation for VTE or atrial fibrillation should continue their therapy unless the platelet count is less than 30-50x109/L or if the fibrinogen is less than 1.0 g/L.16
Conclusion
Coagulopathies associated with COVID-19 infections have been documented in several studies around the world, and it has been shown to be fatal in some cases. Despite documentation, the mechanism behind this coagulopathy is not well understood. Because of the potentially lethal complications associated with coagulopathies, early recognition and anticoagulation is imperative to improve clinical outcomes. These results are very preliminary: More studies are required to understand the role of anticoagulation and its effect on the morbidity and mortality associated with COVID-19–associated coagulopathy.
Dr. Yeruva is a board-certified hematologist/medical oncologist with WellSpan Health and clinical assistant professor of internal medicine, Penn State University, Hershey. Mr. Henderson is a third-year graduate-entry medical student at the Royal College of Surgeons in Ireland with interests in family medicine, dermatology, and tropical diseases. Dr. Al-Tawfiq is a consultant of internal medicine & infectious diseases, and the director of quality at Johns Hopkins Aramco Healthcare in Dhahran, Saudi Arabia, an adjunct associate professor of infectious diseases, molecular medicine and clinical pharmacology at Johns Hopkins University School of Medicine, and adjunct associate professor at Indiana University School of Medicine, Indianapolis. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals.
References
1. World Health Organization. Coronavirus disease (COVID-2019) situation reports.
2. Lippi G et al. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020 Mar 13. 506:145-8. doi: 10.1016/j.cca.2020.03.022.
3. Klok FA et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Throm Res. 2020;18(4):844-7. doi: 10.1016/j.thromres.2020.04.013.
4. Fox S et al. Pulmonary and cardiac pathology in Covid-19: The first autopsy series from New Orleans. MedRxiv. 2020 Apr 10. doi: 10.1101/2020.04.06.20050575.
5. Yang M et al. Thrombocytopenia in patients with severe acute respiratory syndrome (review). Hematology 2013 Sep 4. doi: 10.1080/1024533040002617.
6. Giannis D et al. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020 June. doi: 10.1016/j.jcv.2020.104362.
7. Guo W et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
8. Manalo IF et al. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J Am Acad Dermat. 2020 Apr. doi: 10.1016/j.jaad.2020.04.018.
9. Tang N et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020 Feb 19. doi: 10.1111/jth.14768, 18: 844-847.
10. Huang C et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Jan 24. doi: 10.1016/S0140-6736(20)30183-5.
11. Thachil J et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020 Mar 25. doi: 10.1111/JTH.14810.
12. Tang N et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 Mar 27. doi: 10.1111/JTH.14817.
13. Zhang Y et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020 Mar 28. doi: 10.3760/cma.j.issn.0253-2727.2020.0006.
14. Poterucha TJ et al. More than an anticoagulant: Do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017. doi: 10.1160/TH16-08-0620.
15. Mousavi S et al. Anti-inflammatory effects of heparin and its derivatives: A systematic review. Adv Pharmacol Pharm Sci. 2015 May 12. doi: 10.1155/2015/507151.
16. Kreuziger L et al. COVID-19 and VTE/anticoagulation: Frequently asked questions. American Society of Hematology. 2020 Apr 17.
Coronavirus disease 2019 (COVID-19) is a viral illness caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), currently causing a pandemic affecting many countries around the world, beginning in December 2019 and spreading rapidly on a global scale since. Globally, its burden has been increasing rapidly, with more than 1.2 million people testing positive for the illness and 123,000 people losing their lives, as per April 15th’s WHO COVID-19 Situation Report.1 These numbers are increasing with each passing day. Clinically, SARS-CoV-2 has a highly variable course, ranging from mild disease manifested as a self-limited illness (seen in younger and healthier patients) to severe pneumonia/ARDS and multiorgan failure with intravascular coagulopathy.2
In this article, we intend to investigate and establish a comprehensive review of COVID-19–associated coagulopathy mechanisms, laboratory findings, and current management guidelines put forth by various societies globally.
Mechanism of coagulopathy
COVID-19–associated coagulopathy has been shown to predispose to both arterial and venous thrombosis through excessive inflammation and hypoxia, leading to activation of the coagulation cascade and consumption of coagulation factors, resulting in microvascular thrombosis.3 Though the exact pathophysiology for the activation of this cascade is not known, the proposed mechanism has been: endothelial damage triggering platelet activation within the lung, leading to aggregation, thrombosis, and consumption of platelets in the lung.2,5,6
Fox et al. noted similar coagulopathy findings of four deceased COVID-19 patients. Autopsy results concluded that the dominant process was diffuse alveolar damage, notable CD4+ aggregates around thrombosed small vessels, significant associated hemorrhage, and thrombotic microangiopathy restricted to the lungs. The proposed mechanism was the activation of megakaryocytes, possibly native to the lung, with platelet aggregation, formation of platelet-rich clots, and fibrin deposition playing a major role.4
It has been noted that diabetic patients are at an increased risk of vascular events and hypercoagulability with COVID-19.7 COVID-19 can also cause livedo reticularis and acrocyanosis because of the microthrombosis in the cutaneous vasculature secondary to underlying coagulopathy, as reported in a case report of two U.S. patients with COVID-19.8
Clinical and laboratory abnormalities
A recent study reported from Netherlands by Klok et al. analyzed 184 ICU patients with COVID-19 pneumonia and concluded that the cumulative incidence of acute pulmonary embolism (PE), deep vein thrombosis (DVT), ischemic stroke, MI, or systemic arterial embolism was 31% (95% confidence interval, 20%-41%). PE was the most frequent thrombotic complication and was noted in 81% of patients. Coagulopathy, defined as spontaneous prolongation of prothrombin time (PT) > 3s or activated partial thromboplastin time (aPTT) > 5s, was reported as an independent predictor of thrombotic complications.3
Hematologic abnormalities that were noted in COVID-19 coagulopathy include: decreased platelet counts, decreased fibrinogen levels, elevated PT/INR, elevated partial thromboplastin time (PTT), and elevated d-dimer.9,10 In a retrospective analysis9 by Tang et al., 71.4% of nonsurvivors and 0.6% of survivors had met the criteria of disseminated intravascular coagulation (DIC) during their hospital stay. Nonsurvivors of COVID-19 had statistically significant elevation of d-dimer levels, FDP levels, PT, and aPTT, when compared to survivors (P < .05). The overall mortality in this study was reported as 11.5%.9 In addition, elevated d-dimer, fibrin and fibrinogen degradation product (FDP) levels and longer PT and aPTT were associated with poor prognosis.
Thus, d-dimer, PT, and platelet count should be measured in all patients who present with COVID-19 infection. We can also suggest that in patients with markedly elevated d-dimer (three- to fourfold increase), admission to hospital should be considered even in the absence of severe clinical symptoms.11
COVID-19 coagulopathy management
In a retrospective study9 of 449 patients with severe COVID-19 from Wuhan, China, by Tang et al., 99 patients mainly received low-weight molecular heparin (LMWH) for 7 days or longer. No difference in 28-day mortality was noted between heparin users and nonusers (30.3% vs. 29.7%; P = .910). A lower 28-day mortality rate was noted in heparin patients with sepsis-induced coagulopathy score of ≥4.0 (40.0% vs. 64.2%; P = .029) or a d-dimer level greater than sixfold of upper limit of normal, compared with nonusers of heparin.12
Another small study of seven COVID-19 patients with acroischemia in China demonstrated that administering LMWH was successful at decreasing the d-dimer and fibrinogen degradation product levels but noted no significant improvement in clinical symptoms.13
Recently, the International Society of Thrombosis and Hemostasis and American Society of Hematology published recommendations and guidelines regarding the recognition and management of coagulopathy in COVID-19.11 Prophylactic anticoagulation therapy with LMWH was recommended in all hospitalized patients with COVID-19, provided there was an absence of any contraindications (active bleeding, platelet count less than 25 x 109/L and fibrinogen less than 0.5 g/dL). Anticoagulation with LMWH was associated with better prognosis in severe COVID-19 patients and in COVID-19 patients with markedly elevated d-dimer, as it also has anti-inflammatory effects.12 This anti-inflammatory property of heparin has been documented in previous studies but the underlying mechanism is unknown and more research is required.14,15
Despite coagulopathy being noticed with cases of COVID-19, bleeding has been a rare finding in COVID-19 infections. If bleeding is noted, recommendations were made to keep platelet levels greater than 50 x109/L, fibrinogen less than 2.0 g/L, and INR [international normalized ratio] greater than 1.5.11 Mechanical thromboprophylaxis should be used when pharmacologic thromboprophylaxis is contraindicated.16
COVID-19 patients with new diagnoses of venous thromboembolism (VTE) or atrial fibrillation should be prescribed therapeutic anticoagulation. Patients who are already on anticoagulation for VTE or atrial fibrillation should continue their therapy unless the platelet count is less than 30-50x109/L or if the fibrinogen is less than 1.0 g/L.16
Conclusion
Coagulopathies associated with COVID-19 infections have been documented in several studies around the world, and it has been shown to be fatal in some cases. Despite documentation, the mechanism behind this coagulopathy is not well understood. Because of the potentially lethal complications associated with coagulopathies, early recognition and anticoagulation is imperative to improve clinical outcomes. These results are very preliminary: More studies are required to understand the role of anticoagulation and its effect on the morbidity and mortality associated with COVID-19–associated coagulopathy.
Dr. Yeruva is a board-certified hematologist/medical oncologist with WellSpan Health and clinical assistant professor of internal medicine, Penn State University, Hershey. Mr. Henderson is a third-year graduate-entry medical student at the Royal College of Surgeons in Ireland with interests in family medicine, dermatology, and tropical diseases. Dr. Al-Tawfiq is a consultant of internal medicine & infectious diseases, and the director of quality at Johns Hopkins Aramco Healthcare in Dhahran, Saudi Arabia, an adjunct associate professor of infectious diseases, molecular medicine and clinical pharmacology at Johns Hopkins University School of Medicine, and adjunct associate professor at Indiana University School of Medicine, Indianapolis. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals.
References
1. World Health Organization. Coronavirus disease (COVID-2019) situation reports.
2. Lippi G et al. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020 Mar 13. 506:145-8. doi: 10.1016/j.cca.2020.03.022.
3. Klok FA et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Throm Res. 2020;18(4):844-7. doi: 10.1016/j.thromres.2020.04.013.
4. Fox S et al. Pulmonary and cardiac pathology in Covid-19: The first autopsy series from New Orleans. MedRxiv. 2020 Apr 10. doi: 10.1101/2020.04.06.20050575.
5. Yang M et al. Thrombocytopenia in patients with severe acute respiratory syndrome (review). Hematology 2013 Sep 4. doi: 10.1080/1024533040002617.
6. Giannis D et al. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020 June. doi: 10.1016/j.jcv.2020.104362.
7. Guo W et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
8. Manalo IF et al. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J Am Acad Dermat. 2020 Apr. doi: 10.1016/j.jaad.2020.04.018.
9. Tang N et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020 Feb 19. doi: 10.1111/jth.14768, 18: 844-847.
10. Huang C et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Jan 24. doi: 10.1016/S0140-6736(20)30183-5.
11. Thachil J et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020 Mar 25. doi: 10.1111/JTH.14810.
12. Tang N et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 Mar 27. doi: 10.1111/JTH.14817.
13. Zhang Y et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020 Mar 28. doi: 10.3760/cma.j.issn.0253-2727.2020.0006.
14. Poterucha TJ et al. More than an anticoagulant: Do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017. doi: 10.1160/TH16-08-0620.
15. Mousavi S et al. Anti-inflammatory effects of heparin and its derivatives: A systematic review. Adv Pharmacol Pharm Sci. 2015 May 12. doi: 10.1155/2015/507151.
16. Kreuziger L et al. COVID-19 and VTE/anticoagulation: Frequently asked questions. American Society of Hematology. 2020 Apr 17.
IV-to-oral antibiotics can benefit patients with MRSA bloodstream infection
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
FDA approves dapagliflozin for low-EF heart failure
The Food and Drug Administration has come through with the widely anticipated approval of dapagliflozin (Farxiga, AstraZeneca) for heart failure and reduced ejection fraction (HFrEF), adding to the rich array of medications lately available for this indication.
The approval follows the agency’s priority review of the sodium-glucose cotransporter 2 (SGLT2) inhibitor for reducing the risk of cardiovascular death and heart-failure hospitalization in adults with HFrEF following last year’s seminal results of the DAPA-HF trial.
In that study, treatment with dapagliflozin led to about a one-fourth reduction in risk of a primary endpoint consisting primarily of CV death or heart failure hospitalization in patients with chronic HFrEF, in both those with and without diabetes. The randomized, placebo-controlled trial had entered more than 4,700 patients.
Soon after, the FDA approved dapagliflozin for reducing the risk of heart failure hospitalization in adults with type 2 diabetes and other CV risk factors.
And of course, dapagliflozin – traditionally viewed only as an antidiabetic agent – has long been indicated for improvement of glycemic control in adults with type 2 diabetes.
The latest approval for patients with New York Heart Association functional class III-IV HFrEF makes dapagliflozin the only SGLT2 inhibitor to be indicated for heart failure in the absence of diabetes.
Soon after the DAPA-HF results had been unveiled at a major meeting, heart failure expert Christopher O’Connor, MD, expressed concern that dapagliflozin’s uptake for patients with HFrEF would be slow once it gained approval for patients without diabetes.
“We have to think of this as a drug that you would prescribe like an ACE inhibitor, or a beta-blocker, or a mineralocorticoid receptor antagonist, or sacubitril/valsartan [Entresto, Novartis],” Dr. O’Connor, of the Inova Heart and Vascular Institute, Falls Church, Va., said in an interview.
Dr. O’Connor was not associated with DAPA-HF and had previously disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has come through with the widely anticipated approval of dapagliflozin (Farxiga, AstraZeneca) for heart failure and reduced ejection fraction (HFrEF), adding to the rich array of medications lately available for this indication.
The approval follows the agency’s priority review of the sodium-glucose cotransporter 2 (SGLT2) inhibitor for reducing the risk of cardiovascular death and heart-failure hospitalization in adults with HFrEF following last year’s seminal results of the DAPA-HF trial.
In that study, treatment with dapagliflozin led to about a one-fourth reduction in risk of a primary endpoint consisting primarily of CV death or heart failure hospitalization in patients with chronic HFrEF, in both those with and without diabetes. The randomized, placebo-controlled trial had entered more than 4,700 patients.
Soon after, the FDA approved dapagliflozin for reducing the risk of heart failure hospitalization in adults with type 2 diabetes and other CV risk factors.
And of course, dapagliflozin – traditionally viewed only as an antidiabetic agent – has long been indicated for improvement of glycemic control in adults with type 2 diabetes.
The latest approval for patients with New York Heart Association functional class III-IV HFrEF makes dapagliflozin the only SGLT2 inhibitor to be indicated for heart failure in the absence of diabetes.
Soon after the DAPA-HF results had been unveiled at a major meeting, heart failure expert Christopher O’Connor, MD, expressed concern that dapagliflozin’s uptake for patients with HFrEF would be slow once it gained approval for patients without diabetes.
“We have to think of this as a drug that you would prescribe like an ACE inhibitor, or a beta-blocker, or a mineralocorticoid receptor antagonist, or sacubitril/valsartan [Entresto, Novartis],” Dr. O’Connor, of the Inova Heart and Vascular Institute, Falls Church, Va., said in an interview.
Dr. O’Connor was not associated with DAPA-HF and had previously disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has come through with the widely anticipated approval of dapagliflozin (Farxiga, AstraZeneca) for heart failure and reduced ejection fraction (HFrEF), adding to the rich array of medications lately available for this indication.
The approval follows the agency’s priority review of the sodium-glucose cotransporter 2 (SGLT2) inhibitor for reducing the risk of cardiovascular death and heart-failure hospitalization in adults with HFrEF following last year’s seminal results of the DAPA-HF trial.
In that study, treatment with dapagliflozin led to about a one-fourth reduction in risk of a primary endpoint consisting primarily of CV death or heart failure hospitalization in patients with chronic HFrEF, in both those with and without diabetes. The randomized, placebo-controlled trial had entered more than 4,700 patients.
Soon after, the FDA approved dapagliflozin for reducing the risk of heart failure hospitalization in adults with type 2 diabetes and other CV risk factors.
And of course, dapagliflozin – traditionally viewed only as an antidiabetic agent – has long been indicated for improvement of glycemic control in adults with type 2 diabetes.
The latest approval for patients with New York Heart Association functional class III-IV HFrEF makes dapagliflozin the only SGLT2 inhibitor to be indicated for heart failure in the absence of diabetes.
Soon after the DAPA-HF results had been unveiled at a major meeting, heart failure expert Christopher O’Connor, MD, expressed concern that dapagliflozin’s uptake for patients with HFrEF would be slow once it gained approval for patients without diabetes.
“We have to think of this as a drug that you would prescribe like an ACE inhibitor, or a beta-blocker, or a mineralocorticoid receptor antagonist, or sacubitril/valsartan [Entresto, Novartis],” Dr. O’Connor, of the Inova Heart and Vascular Institute, Falls Church, Va., said in an interview.
Dr. O’Connor was not associated with DAPA-HF and had previously disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
‘Milestone’ study shows promise for pedophilic disorder
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
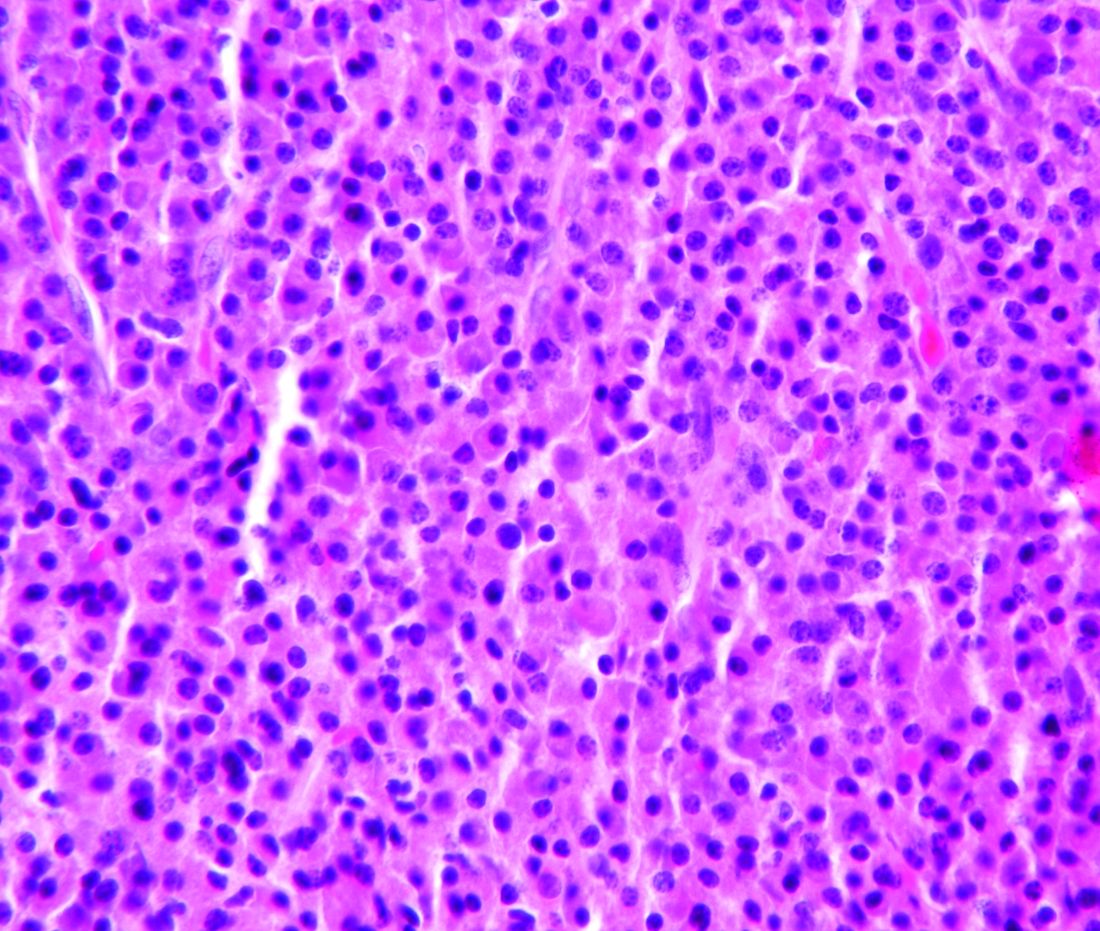
Transplant beats bortezomib-based therapy for MM, but questions remain
While upfront autologous transplantation has bested bortezomib-based intensification therapy in a large, randomized multiple myeloma (MM) trial, investigators and observers say more research will be needed to determine the optimal treatment strategy in the era of novel agents.
Autologous hematopoietic stem cell transplantation (HSCT) extended progression-free survival by almost 15 months compared with bortezomib, melphalan, and prednisone (VMP) intensification therapy for the treatment of newly diagnosed multiple myeloma, according to results of the randomized, phase 3 trial of 1,503 patients enrolled at 172 centers in the European Myeloma Network.
That finding could provide more fodder for the ongoing debate over the role of upfront autologous HSCT as a gold-standard intensification treatment for patients who can tolerate myeloablative doses of chemotherapy in light of the proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies that are now available.
However, the study is not without limitations, including the use of bortezomib, cyclophosphamide, and dexamethasone (VCD) as induction therapy, according to the investigators, led by Michele Cavo, MD, with the Seràgnoli Institute of Hematology at Bologna (Italy) University.
The VCD regimen was one of the most frequently used induction regimens back when the trial was designed, but now it’s considered “less optimal” versus regimens such as bortezomib, lenalidomide, and dexamethasone (VRD), according to Dr. Cavo and coinvestigators.
Besides, the field is moving forward based on clinical trials of “highly active” daratumumab-based four-drug regimens, which appear to enhance rates of response and minimal residual disease (MRD) negativity when given as induction before autologous HSCT and as consolidation afterward, they said.
“Final results from these studies should be awaited before a shift from routine use of upfront autologous HSCT to delayed HSCT or alternative treatment strategies driven by MRD status can be offered to patients with newly diagnosed multiple myeloma who are fit for high-dose chemotherapy,” Dr. Cavo and colleagues noted in their report, available in The Lancet Hematology.
The multicenter, randomized, open-label, phase 3 study by Dr. Cavo and coinvestigators, known as EMN02/HO95, included patients up to 65 years of age with symptomatic multiple myeloma, measurable disease, and WHO performance of 0 to 2. Patients were treated with VCD induction therapy, followed by randomization to either VMP or autologous HSCT after high-dose melphalan. In a second randomization, patients were assigned to either VRD consolidation therapy or no consolidation. All patients then received lenalidomide maintenance therapy until progression.
Median progression-free survival was 56.7 months in patients initially randomized to HSCT, compared with 41.9 months for MP (hazard ratio, 0.73; 95% confidence interval, 0.62-0.85; P = .0001), according to the investigators, who said that finding supports the value of HSCT “even in the era of highly active novel agents.”
Turning to results of the second randomization, Dr. Cavo and colleagues said the VRD consolidation strategy resulted in median progression-free survival that was significantly improved versus no consolidation, at 58.9 months and 45.5 months, respectively (P = .014).
While this is an important study, the added benefit of HSCT intensification therapy is in question given the high rates of MRD being reported for potent, daratumumab-based four-drug combination regimens, according to a related commentary by Omar Nadeem, MD, and Irene M. Ghobrial, MD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston.
“We are entering an era in which novel combinations have shown unprecedented efficacy and future studies with or without HSCT will be needed to answer these key questions,” wrote Dr. Nadeem and Dr. Ghobrial.
Dr. Cavo and colleagues said the estimated 5-year rate of overall survival in EMN02/HO95 was “comparable” between arms, at 75% for the HSCT strategy and 72% for VMP.
“Although this suggests that delaying HSCT to a later time is not harmful, a substantial proportion of patients may become ineligible for high-dose melphalan at first relapse,” they said, noting that 63% of VMP-treated patients went on to receive salvage HSCT.
Further follow-up could demonstrate a survival advantage, as seen in other studies, they added.
Dr. Cavo reported that he has received honoraria from multiple pharmaceutical companies, and is a member of speakers bureaus for Janssen and Celgene. Dr. Nadeem and Dr. Ghobrial reported serving on the advisory boards of multiple pharmaceutical companies.
SOURCE: Cavo M et al. Lancet Haematol. 2020 Apr 30. doi: 10.1016/S2352-3026(20)30099-5.
While upfront autologous transplantation has bested bortezomib-based intensification therapy in a large, randomized multiple myeloma (MM) trial, investigators and observers say more research will be needed to determine the optimal treatment strategy in the era of novel agents.
Autologous hematopoietic stem cell transplantation (HSCT) extended progression-free survival by almost 15 months compared with bortezomib, melphalan, and prednisone (VMP) intensification therapy for the treatment of newly diagnosed multiple myeloma, according to results of the randomized, phase 3 trial of 1,503 patients enrolled at 172 centers in the European Myeloma Network.
That finding could provide more fodder for the ongoing debate over the role of upfront autologous HSCT as a gold-standard intensification treatment for patients who can tolerate myeloablative doses of chemotherapy in light of the proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies that are now available.
However, the study is not without limitations, including the use of bortezomib, cyclophosphamide, and dexamethasone (VCD) as induction therapy, according to the investigators, led by Michele Cavo, MD, with the Seràgnoli Institute of Hematology at Bologna (Italy) University.
The VCD regimen was one of the most frequently used induction regimens back when the trial was designed, but now it’s considered “less optimal” versus regimens such as bortezomib, lenalidomide, and dexamethasone (VRD), according to Dr. Cavo and coinvestigators.
Besides, the field is moving forward based on clinical trials of “highly active” daratumumab-based four-drug regimens, which appear to enhance rates of response and minimal residual disease (MRD) negativity when given as induction before autologous HSCT and as consolidation afterward, they said.
“Final results from these studies should be awaited before a shift from routine use of upfront autologous HSCT to delayed HSCT or alternative treatment strategies driven by MRD status can be offered to patients with newly diagnosed multiple myeloma who are fit for high-dose chemotherapy,” Dr. Cavo and colleagues noted in their report, available in The Lancet Hematology.
The multicenter, randomized, open-label, phase 3 study by Dr. Cavo and coinvestigators, known as EMN02/HO95, included patients up to 65 years of age with symptomatic multiple myeloma, measurable disease, and WHO performance of 0 to 2. Patients were treated with VCD induction therapy, followed by randomization to either VMP or autologous HSCT after high-dose melphalan. In a second randomization, patients were assigned to either VRD consolidation therapy or no consolidation. All patients then received lenalidomide maintenance therapy until progression.
Median progression-free survival was 56.7 months in patients initially randomized to HSCT, compared with 41.9 months for MP (hazard ratio, 0.73; 95% confidence interval, 0.62-0.85; P = .0001), according to the investigators, who said that finding supports the value of HSCT “even in the era of highly active novel agents.”
Turning to results of the second randomization, Dr. Cavo and colleagues said the VRD consolidation strategy resulted in median progression-free survival that was significantly improved versus no consolidation, at 58.9 months and 45.5 months, respectively (P = .014).
While this is an important study, the added benefit of HSCT intensification therapy is in question given the high rates of MRD being reported for potent, daratumumab-based four-drug combination regimens, according to a related commentary by Omar Nadeem, MD, and Irene M. Ghobrial, MD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston.
“We are entering an era in which novel combinations have shown unprecedented efficacy and future studies with or without HSCT will be needed to answer these key questions,” wrote Dr. Nadeem and Dr. Ghobrial.
Dr. Cavo and colleagues said the estimated 5-year rate of overall survival in EMN02/HO95 was “comparable” between arms, at 75% for the HSCT strategy and 72% for VMP.
“Although this suggests that delaying HSCT to a later time is not harmful, a substantial proportion of patients may become ineligible for high-dose melphalan at first relapse,” they said, noting that 63% of VMP-treated patients went on to receive salvage HSCT.
Further follow-up could demonstrate a survival advantage, as seen in other studies, they added.
Dr. Cavo reported that he has received honoraria from multiple pharmaceutical companies, and is a member of speakers bureaus for Janssen and Celgene. Dr. Nadeem and Dr. Ghobrial reported serving on the advisory boards of multiple pharmaceutical companies.
SOURCE: Cavo M et al. Lancet Haematol. 2020 Apr 30. doi: 10.1016/S2352-3026(20)30099-5.
While upfront autologous transplantation has bested bortezomib-based intensification therapy in a large, randomized multiple myeloma (MM) trial, investigators and observers say more research will be needed to determine the optimal treatment strategy in the era of novel agents.
Autologous hematopoietic stem cell transplantation (HSCT) extended progression-free survival by almost 15 months compared with bortezomib, melphalan, and prednisone (VMP) intensification therapy for the treatment of newly diagnosed multiple myeloma, according to results of the randomized, phase 3 trial of 1,503 patients enrolled at 172 centers in the European Myeloma Network.
That finding could provide more fodder for the ongoing debate over the role of upfront autologous HSCT as a gold-standard intensification treatment for patients who can tolerate myeloablative doses of chemotherapy in light of the proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies that are now available.
However, the study is not without limitations, including the use of bortezomib, cyclophosphamide, and dexamethasone (VCD) as induction therapy, according to the investigators, led by Michele Cavo, MD, with the Seràgnoli Institute of Hematology at Bologna (Italy) University.
The VCD regimen was one of the most frequently used induction regimens back when the trial was designed, but now it’s considered “less optimal” versus regimens such as bortezomib, lenalidomide, and dexamethasone (VRD), according to Dr. Cavo and coinvestigators.
Besides, the field is moving forward based on clinical trials of “highly active” daratumumab-based four-drug regimens, which appear to enhance rates of response and minimal residual disease (MRD) negativity when given as induction before autologous HSCT and as consolidation afterward, they said.
“Final results from these studies should be awaited before a shift from routine use of upfront autologous HSCT to delayed HSCT or alternative treatment strategies driven by MRD status can be offered to patients with newly diagnosed multiple myeloma who are fit for high-dose chemotherapy,” Dr. Cavo and colleagues noted in their report, available in The Lancet Hematology.
The multicenter, randomized, open-label, phase 3 study by Dr. Cavo and coinvestigators, known as EMN02/HO95, included patients up to 65 years of age with symptomatic multiple myeloma, measurable disease, and WHO performance of 0 to 2. Patients were treated with VCD induction therapy, followed by randomization to either VMP or autologous HSCT after high-dose melphalan. In a second randomization, patients were assigned to either VRD consolidation therapy or no consolidation. All patients then received lenalidomide maintenance therapy until progression.
Median progression-free survival was 56.7 months in patients initially randomized to HSCT, compared with 41.9 months for MP (hazard ratio, 0.73; 95% confidence interval, 0.62-0.85; P = .0001), according to the investigators, who said that finding supports the value of HSCT “even in the era of highly active novel agents.”
Turning to results of the second randomization, Dr. Cavo and colleagues said the VRD consolidation strategy resulted in median progression-free survival that was significantly improved versus no consolidation, at 58.9 months and 45.5 months, respectively (P = .014).
While this is an important study, the added benefit of HSCT intensification therapy is in question given the high rates of MRD being reported for potent, daratumumab-based four-drug combination regimens, according to a related commentary by Omar Nadeem, MD, and Irene M. Ghobrial, MD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston.
“We are entering an era in which novel combinations have shown unprecedented efficacy and future studies with or without HSCT will be needed to answer these key questions,” wrote Dr. Nadeem and Dr. Ghobrial.
Dr. Cavo and colleagues said the estimated 5-year rate of overall survival in EMN02/HO95 was “comparable” between arms, at 75% for the HSCT strategy and 72% for VMP.
“Although this suggests that delaying HSCT to a later time is not harmful, a substantial proportion of patients may become ineligible for high-dose melphalan at first relapse,” they said, noting that 63% of VMP-treated patients went on to receive salvage HSCT.
Further follow-up could demonstrate a survival advantage, as seen in other studies, they added.
Dr. Cavo reported that he has received honoraria from multiple pharmaceutical companies, and is a member of speakers bureaus for Janssen and Celgene. Dr. Nadeem and Dr. Ghobrial reported serving on the advisory boards of multiple pharmaceutical companies.
SOURCE: Cavo M et al. Lancet Haematol. 2020 Apr 30. doi: 10.1016/S2352-3026(20)30099-5.
FROM THE LANCET HEMATOLOGY
Starting school later in the morning improves adolescents’ sleep
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
FROM JAMA PEDIATRICS
Patients with epilepsy may underreport seizures, survey finds
according to survey results presented online as part of the 2020 American Academy of Neurology Science Highlights.
Clinicians, for their part, may underestimate the number of seizures that go unreported. This disconnect may contribute to complacency about epilepsy treatment regimens among patients, caregivers, and health care professionals (HCPs), despite continuations in seizures. “Improved reporting of all seizure occurrences and more frequent discussion of potential treatment changes, initiated by all groups, may be needed to optimize treatment outcomes,” said Patricia E. Penovich, MD, a neurologist at Minnesota Epilepsy Group in St. Paul, and colleagues.
To evaluate treatment complacency among adult patients with epilepsy, caregivers, and HCPs, Dr. Penovich and collaborators analyzed data from the STEP survey (Seize the Truth about Epilepsy Perceptions), which was conducted between February and March 2019. In all, 400 adults with epilepsy, 201 caregivers, and 258 HCPs completed the survey. The HCPs included 96 epileptologists, 112 general neurologists, and 50 nurse practitioners or physician assistants.
Patients had an average epilepsy duration of 16 years, and 58% were on at least their third antiepileptic drug (AED). In the past year, 52% of patients had 1-9 seizures, and 31% had 10 or more seizures. “Patients estimated reporting 45% of their seizures to their HCPs, and for the seizures not reported, 57% provided reasoning that they were not serious enough to mention,” reported Dr. Penovich and colleagues. “Alternatively, HCPs estimated that patients report 73% of seizures.”
Survey participants most frequently selected HCPs as the ones to initiate conversations about changing AEDs or increasing dosage. “Patient-initiated discussions were reported by 39% of patients for changing AEDs and 27% of patients for increasing AED dosage; 25% of patients reported they were likely to ask their HCP about changing treatments in the next 12 months,” the authors said. Discussion of vagus nerve stimulation was reported by 21% of HCPs, and 10% reported discussion of responsive neurostimulation. HCPs also discussed surgical options such as hemispherectomy (3%), corpus callosotomy and multiple subpial transection (4%), lobe resection (8%), and lesionectomy (11%).
Among patients with 13 or more seizures per year, 27% reported referral to an epilepsy center. Most survey participants – 61% of patients and HCPs and 68% of caregivers – “reported a desire for a treatment map that tells patients to see an epileptologist/specialist as soon as they have symptoms,” the researchers said.
“What we would like to think is that we are getting the whole scoop and the honest scoop” about seizure activity, Dr. Penovich said in an interview. “What this shows us is that that’s probably not always true. Some health care providers understand that the patients do not tell them everything,” but the degree of seizure underreporting may be surprising.
Dr. Penovich has seen this phenomenon in practice. In some cases, caregivers return to the office to explain that a patient did not report all of their seizures. Other patients may omit entire days of seizures in their diaries as an oversight. In addition, patients may not report seizures to avoid having a driver’s license revoked. In some instances, clinicians may not take the time to discuss seizure activity in detail.
Having an accurate picture of seizure activity is an “important part of working with our patients, particularly when we are trying to get them to the point of being seizure free,” said Dr. Penovich.
Failing a first or second AED indicates a greater likelihood that medication will not stop a patient’s seizures, “but it does not mean that you will not be controlled,” Dr. Penovich said. More medications, surgical options, and investigative treatments have become available. Still, AED trials should not prevent a timely referral to an epilepsy center. “You don’t need to go through 10 or 15 before you get referred” to an epilepsy center, she said.
The STEP survey was conducted by Kantar Health on behalf of SK Life Science. Dr. Penovich has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities from SK Life Science, Neurelis, GW Pharmaceuticals, Engage Therapeutics, and UCB Pharma. A coauthor was employed by Kantar Health. Other coauthors disclosed compensation from SK Life Science and various pharmaceutical companies.
SOURCE: Penovich PE et al. AAN 2020, Abstract S59.007.
according to survey results presented online as part of the 2020 American Academy of Neurology Science Highlights.
Clinicians, for their part, may underestimate the number of seizures that go unreported. This disconnect may contribute to complacency about epilepsy treatment regimens among patients, caregivers, and health care professionals (HCPs), despite continuations in seizures. “Improved reporting of all seizure occurrences and more frequent discussion of potential treatment changes, initiated by all groups, may be needed to optimize treatment outcomes,” said Patricia E. Penovich, MD, a neurologist at Minnesota Epilepsy Group in St. Paul, and colleagues.
To evaluate treatment complacency among adult patients with epilepsy, caregivers, and HCPs, Dr. Penovich and collaborators analyzed data from the STEP survey (Seize the Truth about Epilepsy Perceptions), which was conducted between February and March 2019. In all, 400 adults with epilepsy, 201 caregivers, and 258 HCPs completed the survey. The HCPs included 96 epileptologists, 112 general neurologists, and 50 nurse practitioners or physician assistants.
Patients had an average epilepsy duration of 16 years, and 58% were on at least their third antiepileptic drug (AED). In the past year, 52% of patients had 1-9 seizures, and 31% had 10 or more seizures. “Patients estimated reporting 45% of their seizures to their HCPs, and for the seizures not reported, 57% provided reasoning that they were not serious enough to mention,” reported Dr. Penovich and colleagues. “Alternatively, HCPs estimated that patients report 73% of seizures.”
Survey participants most frequently selected HCPs as the ones to initiate conversations about changing AEDs or increasing dosage. “Patient-initiated discussions were reported by 39% of patients for changing AEDs and 27% of patients for increasing AED dosage; 25% of patients reported they were likely to ask their HCP about changing treatments in the next 12 months,” the authors said. Discussion of vagus nerve stimulation was reported by 21% of HCPs, and 10% reported discussion of responsive neurostimulation. HCPs also discussed surgical options such as hemispherectomy (3%), corpus callosotomy and multiple subpial transection (4%), lobe resection (8%), and lesionectomy (11%).
Among patients with 13 or more seizures per year, 27% reported referral to an epilepsy center. Most survey participants – 61% of patients and HCPs and 68% of caregivers – “reported a desire for a treatment map that tells patients to see an epileptologist/specialist as soon as they have symptoms,” the researchers said.
“What we would like to think is that we are getting the whole scoop and the honest scoop” about seizure activity, Dr. Penovich said in an interview. “What this shows us is that that’s probably not always true. Some health care providers understand that the patients do not tell them everything,” but the degree of seizure underreporting may be surprising.
Dr. Penovich has seen this phenomenon in practice. In some cases, caregivers return to the office to explain that a patient did not report all of their seizures. Other patients may omit entire days of seizures in their diaries as an oversight. In addition, patients may not report seizures to avoid having a driver’s license revoked. In some instances, clinicians may not take the time to discuss seizure activity in detail.
Having an accurate picture of seizure activity is an “important part of working with our patients, particularly when we are trying to get them to the point of being seizure free,” said Dr. Penovich.
Failing a first or second AED indicates a greater likelihood that medication will not stop a patient’s seizures, “but it does not mean that you will not be controlled,” Dr. Penovich said. More medications, surgical options, and investigative treatments have become available. Still, AED trials should not prevent a timely referral to an epilepsy center. “You don’t need to go through 10 or 15 before you get referred” to an epilepsy center, she said.
The STEP survey was conducted by Kantar Health on behalf of SK Life Science. Dr. Penovich has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities from SK Life Science, Neurelis, GW Pharmaceuticals, Engage Therapeutics, and UCB Pharma. A coauthor was employed by Kantar Health. Other coauthors disclosed compensation from SK Life Science and various pharmaceutical companies.
SOURCE: Penovich PE et al. AAN 2020, Abstract S59.007.
according to survey results presented online as part of the 2020 American Academy of Neurology Science Highlights.
Clinicians, for their part, may underestimate the number of seizures that go unreported. This disconnect may contribute to complacency about epilepsy treatment regimens among patients, caregivers, and health care professionals (HCPs), despite continuations in seizures. “Improved reporting of all seizure occurrences and more frequent discussion of potential treatment changes, initiated by all groups, may be needed to optimize treatment outcomes,” said Patricia E. Penovich, MD, a neurologist at Minnesota Epilepsy Group in St. Paul, and colleagues.
To evaluate treatment complacency among adult patients with epilepsy, caregivers, and HCPs, Dr. Penovich and collaborators analyzed data from the STEP survey (Seize the Truth about Epilepsy Perceptions), which was conducted between February and March 2019. In all, 400 adults with epilepsy, 201 caregivers, and 258 HCPs completed the survey. The HCPs included 96 epileptologists, 112 general neurologists, and 50 nurse practitioners or physician assistants.
Patients had an average epilepsy duration of 16 years, and 58% were on at least their third antiepileptic drug (AED). In the past year, 52% of patients had 1-9 seizures, and 31% had 10 or more seizures. “Patients estimated reporting 45% of their seizures to their HCPs, and for the seizures not reported, 57% provided reasoning that they were not serious enough to mention,” reported Dr. Penovich and colleagues. “Alternatively, HCPs estimated that patients report 73% of seizures.”
Survey participants most frequently selected HCPs as the ones to initiate conversations about changing AEDs or increasing dosage. “Patient-initiated discussions were reported by 39% of patients for changing AEDs and 27% of patients for increasing AED dosage; 25% of patients reported they were likely to ask their HCP about changing treatments in the next 12 months,” the authors said. Discussion of vagus nerve stimulation was reported by 21% of HCPs, and 10% reported discussion of responsive neurostimulation. HCPs also discussed surgical options such as hemispherectomy (3%), corpus callosotomy and multiple subpial transection (4%), lobe resection (8%), and lesionectomy (11%).
Among patients with 13 or more seizures per year, 27% reported referral to an epilepsy center. Most survey participants – 61% of patients and HCPs and 68% of caregivers – “reported a desire for a treatment map that tells patients to see an epileptologist/specialist as soon as they have symptoms,” the researchers said.
“What we would like to think is that we are getting the whole scoop and the honest scoop” about seizure activity, Dr. Penovich said in an interview. “What this shows us is that that’s probably not always true. Some health care providers understand that the patients do not tell them everything,” but the degree of seizure underreporting may be surprising.
Dr. Penovich has seen this phenomenon in practice. In some cases, caregivers return to the office to explain that a patient did not report all of their seizures. Other patients may omit entire days of seizures in their diaries as an oversight. In addition, patients may not report seizures to avoid having a driver’s license revoked. In some instances, clinicians may not take the time to discuss seizure activity in detail.
Having an accurate picture of seizure activity is an “important part of working with our patients, particularly when we are trying to get them to the point of being seizure free,” said Dr. Penovich.
Failing a first or second AED indicates a greater likelihood that medication will not stop a patient’s seizures, “but it does not mean that you will not be controlled,” Dr. Penovich said. More medications, surgical options, and investigative treatments have become available. Still, AED trials should not prevent a timely referral to an epilepsy center. “You don’t need to go through 10 or 15 before you get referred” to an epilepsy center, she said.
The STEP survey was conducted by Kantar Health on behalf of SK Life Science. Dr. Penovich has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities from SK Life Science, Neurelis, GW Pharmaceuticals, Engage Therapeutics, and UCB Pharma. A coauthor was employed by Kantar Health. Other coauthors disclosed compensation from SK Life Science and various pharmaceutical companies.
SOURCE: Penovich PE et al. AAN 2020, Abstract S59.007.
FROM AAN 2020
Ear and nose plaques
Based on the clinical appearance of hyperpigmented and hypopigmented scaly plaques in sun-exposed facial areas (with associated scarring and follicular plugging in affected lesions), the patient was given a diagnosis of discoid lupus erythematosus. The diagnosis was confirmed with a punch biopsy that showed characteristic interface dermatitis with superficial and deep perivascular and peri-adnexal lymphocytes. Direct immunofluorescence showed a band of C3 at the dermo-epidermal junction, consistent with various forms of cutaneous lupus.
A review of systems was negative for signs of systemic disease, including a lack of weakness, joint pain/swelling, fever, or known blood clots. An antinuclear antibody panel was also negative, largely excluding systemic disease.
Discoid lupus erythematosus is a form of cutaneous lupus. Patients often are genetically predisposed to autoimmune disease, and disease may be triggered by sun exposure. Up to 80% of patients develop lesions that are limited to the head and neck. Up to 25% of patients develop systemic lupus erythematosus that may occur months—or even decades—after the initial diagnosis. Lesions may lead to longstanding scars; this cannot always be prevented.
Two- to 3-week trials of topical potent or superpotent steroids applied to affected plaques may lead to clearance. Additionally, lesions may be treated with intralesional triamcinolone 3 mg/mL to 10 mg/mL and repeated every 3 to 4 weeks. Systemic therapies include hydroxychloroquine, chloroquine, retinoids, steroid sparing immunomodulators, and rarely prednisone.
This patient tolerated topical therapy well and though some scars remained, he was able to control flares with 2- to 3-week courses of clobetasol 0.05% twice daily. He is followed 2 to 3 times annually and has not developed signs or serologic findings of systemic disease over several years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Jessop S, Whitelaw DA, Grainge MJ, et al. Drugs for discoid lupus erythematosus. Cochrane Database Syst Rev. 2017;5:CD002954.
Based on the clinical appearance of hyperpigmented and hypopigmented scaly plaques in sun-exposed facial areas (with associated scarring and follicular plugging in affected lesions), the patient was given a diagnosis of discoid lupus erythematosus. The diagnosis was confirmed with a punch biopsy that showed characteristic interface dermatitis with superficial and deep perivascular and peri-adnexal lymphocytes. Direct immunofluorescence showed a band of C3 at the dermo-epidermal junction, consistent with various forms of cutaneous lupus.
A review of systems was negative for signs of systemic disease, including a lack of weakness, joint pain/swelling, fever, or known blood clots. An antinuclear antibody panel was also negative, largely excluding systemic disease.
Discoid lupus erythematosus is a form of cutaneous lupus. Patients often are genetically predisposed to autoimmune disease, and disease may be triggered by sun exposure. Up to 80% of patients develop lesions that are limited to the head and neck. Up to 25% of patients develop systemic lupus erythematosus that may occur months—or even decades—after the initial diagnosis. Lesions may lead to longstanding scars; this cannot always be prevented.
Two- to 3-week trials of topical potent or superpotent steroids applied to affected plaques may lead to clearance. Additionally, lesions may be treated with intralesional triamcinolone 3 mg/mL to 10 mg/mL and repeated every 3 to 4 weeks. Systemic therapies include hydroxychloroquine, chloroquine, retinoids, steroid sparing immunomodulators, and rarely prednisone.
This patient tolerated topical therapy well and though some scars remained, he was able to control flares with 2- to 3-week courses of clobetasol 0.05% twice daily. He is followed 2 to 3 times annually and has not developed signs or serologic findings of systemic disease over several years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Based on the clinical appearance of hyperpigmented and hypopigmented scaly plaques in sun-exposed facial areas (with associated scarring and follicular plugging in affected lesions), the patient was given a diagnosis of discoid lupus erythematosus. The diagnosis was confirmed with a punch biopsy that showed characteristic interface dermatitis with superficial and deep perivascular and peri-adnexal lymphocytes. Direct immunofluorescence showed a band of C3 at the dermo-epidermal junction, consistent with various forms of cutaneous lupus.
A review of systems was negative for signs of systemic disease, including a lack of weakness, joint pain/swelling, fever, or known blood clots. An antinuclear antibody panel was also negative, largely excluding systemic disease.
Discoid lupus erythematosus is a form of cutaneous lupus. Patients often are genetically predisposed to autoimmune disease, and disease may be triggered by sun exposure. Up to 80% of patients develop lesions that are limited to the head and neck. Up to 25% of patients develop systemic lupus erythematosus that may occur months—or even decades—after the initial diagnosis. Lesions may lead to longstanding scars; this cannot always be prevented.
Two- to 3-week trials of topical potent or superpotent steroids applied to affected plaques may lead to clearance. Additionally, lesions may be treated with intralesional triamcinolone 3 mg/mL to 10 mg/mL and repeated every 3 to 4 weeks. Systemic therapies include hydroxychloroquine, chloroquine, retinoids, steroid sparing immunomodulators, and rarely prednisone.
This patient tolerated topical therapy well and though some scars remained, he was able to control flares with 2- to 3-week courses of clobetasol 0.05% twice daily. He is followed 2 to 3 times annually and has not developed signs or serologic findings of systemic disease over several years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Jessop S, Whitelaw DA, Grainge MJ, et al. Drugs for discoid lupus erythematosus. Cochrane Database Syst Rev. 2017;5:CD002954.
Jessop S, Whitelaw DA, Grainge MJ, et al. Drugs for discoid lupus erythematosus. Cochrane Database Syst Rev. 2017;5:CD002954.
NSCLC: FDA approves capmatinib and companion assay
as detected by an FDA-approved test.
The FDA also approved the FoundationOne CDx assay (F1CDx) as a companion diagnostic for capmatinib. F1CDx is a next-generation sequencing-based, in vitro diagnostic device that detects several mutations, including MET exon 14 skipping mutations.
Capmatinib is a selective, reversible inhibitor of MET tyrosine kinase and the first treatment FDA-approved for NSCLC with MET exon 14 skipping mutations.
Capmatinib was granted accelerated approval based on overall response rate and response duration in the GEOMETRY mono-1 trial, the FDA said. Results from this trial were recently presented at the AACR Virtual Annual Meeting I.
The phase 2 trial enrolled 97 patients with metastatic NSCLC and confirmed MET exon 14 skipping mutations, 69 of whom were previously treated and 28 of whom were treatment naive. The patients received capmatinib at 400 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 68% in the treatment-naive patients and 41% in the previously treated patients. The median duration of response was 12.6 months and 9.7 months, respectively, according to the FDA.
The most common adverse events (occurring in at least 20% of patients) were peripheral edema, nausea, fatigue, vomiting, dyspnea, and decreased appetite.
The full prescribing information for capmatinib is available for download from the FDA website.
The FDA granted the approval of capmatinib to Novartis Pharmaceuticals Corporation and the approval of the F1CDx companion diagnostic to Foundation Medicine.
as detected by an FDA-approved test.
The FDA also approved the FoundationOne CDx assay (F1CDx) as a companion diagnostic for capmatinib. F1CDx is a next-generation sequencing-based, in vitro diagnostic device that detects several mutations, including MET exon 14 skipping mutations.
Capmatinib is a selective, reversible inhibitor of MET tyrosine kinase and the first treatment FDA-approved for NSCLC with MET exon 14 skipping mutations.
Capmatinib was granted accelerated approval based on overall response rate and response duration in the GEOMETRY mono-1 trial, the FDA said. Results from this trial were recently presented at the AACR Virtual Annual Meeting I.
The phase 2 trial enrolled 97 patients with metastatic NSCLC and confirmed MET exon 14 skipping mutations, 69 of whom were previously treated and 28 of whom were treatment naive. The patients received capmatinib at 400 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 68% in the treatment-naive patients and 41% in the previously treated patients. The median duration of response was 12.6 months and 9.7 months, respectively, according to the FDA.
The most common adverse events (occurring in at least 20% of patients) were peripheral edema, nausea, fatigue, vomiting, dyspnea, and decreased appetite.
The full prescribing information for capmatinib is available for download from the FDA website.
The FDA granted the approval of capmatinib to Novartis Pharmaceuticals Corporation and the approval of the F1CDx companion diagnostic to Foundation Medicine.
as detected by an FDA-approved test.
The FDA also approved the FoundationOne CDx assay (F1CDx) as a companion diagnostic for capmatinib. F1CDx is a next-generation sequencing-based, in vitro diagnostic device that detects several mutations, including MET exon 14 skipping mutations.
Capmatinib is a selective, reversible inhibitor of MET tyrosine kinase and the first treatment FDA-approved for NSCLC with MET exon 14 skipping mutations.
Capmatinib was granted accelerated approval based on overall response rate and response duration in the GEOMETRY mono-1 trial, the FDA said. Results from this trial were recently presented at the AACR Virtual Annual Meeting I.
The phase 2 trial enrolled 97 patients with metastatic NSCLC and confirmed MET exon 14 skipping mutations, 69 of whom were previously treated and 28 of whom were treatment naive. The patients received capmatinib at 400 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 68% in the treatment-naive patients and 41% in the previously treated patients. The median duration of response was 12.6 months and 9.7 months, respectively, according to the FDA.
The most common adverse events (occurring in at least 20% of patients) were peripheral edema, nausea, fatigue, vomiting, dyspnea, and decreased appetite.
The full prescribing information for capmatinib is available for download from the FDA website.
The FDA granted the approval of capmatinib to Novartis Pharmaceuticals Corporation and the approval of the F1CDx companion diagnostic to Foundation Medicine.
Capmatinib shows impressive results in METex14-mutated NSCLC
according to a presentation at the AACR virtual meeting I.
The duration of response was impressive in both treatment-naive and previously treated patients, according to presenter Edward B. Garon, MD, of the University of California, Los Angeles.
In view of these responses, Dr. Garon urged early molecular testing in NSCLC.
He also noted that capmatinib produced responses in patients with brain metastases. However, because of small patient numbers, additional study is needed to validate the intracranial efficacy of capmatinib and ascertain mechanisms of resistance.
Study rationale and details
METex14 mutations are reported in up to 4% of patients with NSCLC and portend poor outcomes with chemotherapy and immune checkpoint inhibitors (PLoS One 2014; 9:e107677; Ann Oncol 2018;29:2085-91).
Capmatinib is a highly selective, reversible, and potent inhibitor of MET tyrosine kinase that crosses the blood-brain barrier.
In the phase 2 GEOMETRY mono-1 study, Dr. Garon and colleagues tested capmatinib, given at 400 mg orally twice a day, in patients with METex14-mutated, ALK and EGFR wild-type, stage IIIB/IV NSCLC. Patients with neurologically stable or asymptomatic brain metastases were eligible.
Dr. Garon presented safety data for all patients enrolled in this study and efficacy data for patients in cohorts 4 and 5b. Cohort 4 enrolled patients who received prior systemic therapy for advanced disease, and cohort 5b enrolled treatment-naive patients. Both cohorts had METex14 gene mutations but not amplification.
Efficacy
There were 97 patients evaluable for efficacy – 69 previously treated and 28 treatment naive. The median age in both cohorts was 71 years, most patients were female (58% of previously treated and 64.3% of treatment-naive patients), and most were never-smokers (58% and 64.3%, respectively). Adenocarcinoma was the predominant histology.
The overall response rate, per an independent review committee, was 40.6% in previously treated patients and 67.9% in treatment-naive patients.
Waterfall plots showed deep responses, with only four cases of disease progression in the previously treated cohort and none in the treatment-naive cohort.
Responses occurred rapidly. Many responses exceeded 1 year and were ongoing at the data cut-off. The median response duration was 9.72 months in previously treated patients and 11.14 months in treatment-naive patients.
There were 13 patients with evaluable baseline brain metastases (3.3 brain lesions per patient [range, 1-8]). Twelve patients had intracranial disease control, and seven patients (54%) had intracranial response. Four patients had complete resolution of all brain lesions.
Intracranial responses were generally seen by the first radiologic evaluation and occurred as rapidly as systemic responses.
Safety
With safety data on all 334 patients in the trial, the GEOMETRY mono-1 study is the largest reported experience with capmatinib in NSCLC patients. The median treatment exposure time was 14.9 weeks.
Overall, 35.6% of patients experienced a grade 3/4 adverse event (AE). Grade 4 AEs were observed in 4.5% of patients, and there were no treatment-related deaths.
Peripheral edema (41.6%), nausea (33.2%), increased blood creatinine (19.5%), and vomiting (18.9%) were the most frequent AEs of any grade.
In all, 21.9% of patients required dose adjustments due to treatment-related AEs, and 11.1% of patients stopped treatment because of an AE.
This study was sponsored by Novartis. Dr. Garon disclosed relationships with Novartis, AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Eli Lilly, EMD Serono, Genentech, GSK, Iovance, Merck, Mirati, and Neon.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Garon EB et al. AACR 2020, Abstract CT082.
according to a presentation at the AACR virtual meeting I.
The duration of response was impressive in both treatment-naive and previously treated patients, according to presenter Edward B. Garon, MD, of the University of California, Los Angeles.
In view of these responses, Dr. Garon urged early molecular testing in NSCLC.
He also noted that capmatinib produced responses in patients with brain metastases. However, because of small patient numbers, additional study is needed to validate the intracranial efficacy of capmatinib and ascertain mechanisms of resistance.
Study rationale and details
METex14 mutations are reported in up to 4% of patients with NSCLC and portend poor outcomes with chemotherapy and immune checkpoint inhibitors (PLoS One 2014; 9:e107677; Ann Oncol 2018;29:2085-91).
Capmatinib is a highly selective, reversible, and potent inhibitor of MET tyrosine kinase that crosses the blood-brain barrier.
In the phase 2 GEOMETRY mono-1 study, Dr. Garon and colleagues tested capmatinib, given at 400 mg orally twice a day, in patients with METex14-mutated, ALK and EGFR wild-type, stage IIIB/IV NSCLC. Patients with neurologically stable or asymptomatic brain metastases were eligible.
Dr. Garon presented safety data for all patients enrolled in this study and efficacy data for patients in cohorts 4 and 5b. Cohort 4 enrolled patients who received prior systemic therapy for advanced disease, and cohort 5b enrolled treatment-naive patients. Both cohorts had METex14 gene mutations but not amplification.
Efficacy
There were 97 patients evaluable for efficacy – 69 previously treated and 28 treatment naive. The median age in both cohorts was 71 years, most patients were female (58% of previously treated and 64.3% of treatment-naive patients), and most were never-smokers (58% and 64.3%, respectively). Adenocarcinoma was the predominant histology.
The overall response rate, per an independent review committee, was 40.6% in previously treated patients and 67.9% in treatment-naive patients.
Waterfall plots showed deep responses, with only four cases of disease progression in the previously treated cohort and none in the treatment-naive cohort.
Responses occurred rapidly. Many responses exceeded 1 year and were ongoing at the data cut-off. The median response duration was 9.72 months in previously treated patients and 11.14 months in treatment-naive patients.
There were 13 patients with evaluable baseline brain metastases (3.3 brain lesions per patient [range, 1-8]). Twelve patients had intracranial disease control, and seven patients (54%) had intracranial response. Four patients had complete resolution of all brain lesions.
Intracranial responses were generally seen by the first radiologic evaluation and occurred as rapidly as systemic responses.
Safety
With safety data on all 334 patients in the trial, the GEOMETRY mono-1 study is the largest reported experience with capmatinib in NSCLC patients. The median treatment exposure time was 14.9 weeks.
Overall, 35.6% of patients experienced a grade 3/4 adverse event (AE). Grade 4 AEs were observed in 4.5% of patients, and there were no treatment-related deaths.
Peripheral edema (41.6%), nausea (33.2%), increased blood creatinine (19.5%), and vomiting (18.9%) were the most frequent AEs of any grade.
In all, 21.9% of patients required dose adjustments due to treatment-related AEs, and 11.1% of patients stopped treatment because of an AE.
This study was sponsored by Novartis. Dr. Garon disclosed relationships with Novartis, AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Eli Lilly, EMD Serono, Genentech, GSK, Iovance, Merck, Mirati, and Neon.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Garon EB et al. AACR 2020, Abstract CT082.
according to a presentation at the AACR virtual meeting I.
The duration of response was impressive in both treatment-naive and previously treated patients, according to presenter Edward B. Garon, MD, of the University of California, Los Angeles.
In view of these responses, Dr. Garon urged early molecular testing in NSCLC.
He also noted that capmatinib produced responses in patients with brain metastases. However, because of small patient numbers, additional study is needed to validate the intracranial efficacy of capmatinib and ascertain mechanisms of resistance.
Study rationale and details
METex14 mutations are reported in up to 4% of patients with NSCLC and portend poor outcomes with chemotherapy and immune checkpoint inhibitors (PLoS One 2014; 9:e107677; Ann Oncol 2018;29:2085-91).
Capmatinib is a highly selective, reversible, and potent inhibitor of MET tyrosine kinase that crosses the blood-brain barrier.
In the phase 2 GEOMETRY mono-1 study, Dr. Garon and colleagues tested capmatinib, given at 400 mg orally twice a day, in patients with METex14-mutated, ALK and EGFR wild-type, stage IIIB/IV NSCLC. Patients with neurologically stable or asymptomatic brain metastases were eligible.
Dr. Garon presented safety data for all patients enrolled in this study and efficacy data for patients in cohorts 4 and 5b. Cohort 4 enrolled patients who received prior systemic therapy for advanced disease, and cohort 5b enrolled treatment-naive patients. Both cohorts had METex14 gene mutations but not amplification.
Efficacy
There were 97 patients evaluable for efficacy – 69 previously treated and 28 treatment naive. The median age in both cohorts was 71 years, most patients were female (58% of previously treated and 64.3% of treatment-naive patients), and most were never-smokers (58% and 64.3%, respectively). Adenocarcinoma was the predominant histology.
The overall response rate, per an independent review committee, was 40.6% in previously treated patients and 67.9% in treatment-naive patients.
Waterfall plots showed deep responses, with only four cases of disease progression in the previously treated cohort and none in the treatment-naive cohort.
Responses occurred rapidly. Many responses exceeded 1 year and were ongoing at the data cut-off. The median response duration was 9.72 months in previously treated patients and 11.14 months in treatment-naive patients.
There were 13 patients with evaluable baseline brain metastases (3.3 brain lesions per patient [range, 1-8]). Twelve patients had intracranial disease control, and seven patients (54%) had intracranial response. Four patients had complete resolution of all brain lesions.
Intracranial responses were generally seen by the first radiologic evaluation and occurred as rapidly as systemic responses.
Safety
With safety data on all 334 patients in the trial, the GEOMETRY mono-1 study is the largest reported experience with capmatinib in NSCLC patients. The median treatment exposure time was 14.9 weeks.
Overall, 35.6% of patients experienced a grade 3/4 adverse event (AE). Grade 4 AEs were observed in 4.5% of patients, and there were no treatment-related deaths.
Peripheral edema (41.6%), nausea (33.2%), increased blood creatinine (19.5%), and vomiting (18.9%) were the most frequent AEs of any grade.
In all, 21.9% of patients required dose adjustments due to treatment-related AEs, and 11.1% of patients stopped treatment because of an AE.
This study was sponsored by Novartis. Dr. Garon disclosed relationships with Novartis, AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Eli Lilly, EMD Serono, Genentech, GSK, Iovance, Merck, Mirati, and Neon.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Garon EB et al. AACR 2020, Abstract CT082.
FROM AACR 2020