User login
FDA approves hyaluronic acid filler for lip augmentation, perioral rhytids
, the manufacturer has announced.
Approval was supported by results of a phase 3 clinical trial in which a lower amount of Restylane Kysse was needed to see an improvement in lip fullness (1.82 mL) vs. a comparator (2.24 mL), according to the press release issued by Galderma. After 1 year, 78% of those who received the Restylane product were satisfied, and it was also shown to be safe and well tolerated, the release said.
In the statement, the company said that it is “working to determine the appropriate launch timing and availability” of this new product.
lfranki@mdedge.com
, the manufacturer has announced.
Approval was supported by results of a phase 3 clinical trial in which a lower amount of Restylane Kysse was needed to see an improvement in lip fullness (1.82 mL) vs. a comparator (2.24 mL), according to the press release issued by Galderma. After 1 year, 78% of those who received the Restylane product were satisfied, and it was also shown to be safe and well tolerated, the release said.
In the statement, the company said that it is “working to determine the appropriate launch timing and availability” of this new product.
lfranki@mdedge.com
, the manufacturer has announced.
Approval was supported by results of a phase 3 clinical trial in which a lower amount of Restylane Kysse was needed to see an improvement in lip fullness (1.82 mL) vs. a comparator (2.24 mL), according to the press release issued by Galderma. After 1 year, 78% of those who received the Restylane product were satisfied, and it was also shown to be safe and well tolerated, the release said.
In the statement, the company said that it is “working to determine the appropriate launch timing and availability” of this new product.
lfranki@mdedge.com
Moving beyond the hospital ward
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
GI symptoms in Parkinson’s disease correlate with less microbial diversity
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
FROM AAN 2020
AHA emphasizes the need for cardio-obstetrics teams
according to a statement from the American Heart Association.
Cardiovascular disease (CVD) remains the leading cause of pregnancy-related mortality in the United States, and accounted for approximately 17 deaths per 100,000 live births in 2015, wrote Laxmi S. Mehta, MD, of The Ohio State University, Columbus, and colleagues.
Ideally, a woman with CVD at the time of pregnancy should be managed by a multidisciplinary cardio-obstetrics team that can assess cardiovascular risk, obstetric risk, and fetal risk throughout pregnancy, delivery, and up to a year post partum. The team should develop a shared strategy to promote best outcomes, according to the statement. The cardio-obstetrics team may include obstetricians, cardiologists, anesthesiologists, maternal-fetal medicine specialists, geneticists, neurologists, nurses, and pharmacists, according to the statement.
Women with preexisting CVD should receive counseling about maternal and fetal risks before conception, if possible, to involve the women in shared decision-making and to develop strategies for each stage of pregnancy and delivery, Dr. Mehta and associates said. Such counseling should include a review of all medications and assessment of risk factors.
However, some women present already in the early stages of pregnancy even with severe conditions such as pulmonary arterial hypertension, severe ventricular dysfunction, severe left-sided heart obstruction, and significant aortic dilatation with underlying connective tissue disease. Women with these conditions often are counseled to avoid pregnancy, but if they already are pregnant, a high-risk cardio-obstetrics team will need to work together to discover the best strategies going forward to mitigate risk, Dr. Mehta and associates said.
Common CVD conditions that affect pregnancy include hypertensive disorders, notably preeclampsia, defined as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg in women after 20 weeks of gestation whose blood pressure was normal prior to pregnancy. A management strategy to reduce the risk of pregnancy-related complications from hypertension includes healthy lifestyle behaviors such as exercise, nutrition, and smoking cessation, according to the statement. However, patients with severe hypertension may require intravenous labetalol or hydralazine. The statement gives more information about handling preeclampsia with pulmonary edema, and prevention of eclampsia and treatment of seizures.
It is important to recognize that severe hypertension or superimposed preeclampsia may occur for the first time post partum. Early ambulatory visits in the first 1-2 weeks are sensible. Medications may be needed to keep a systolic blood pressure not higher than 150 mm Hg and a diastolic blood pressure not higher than 100 mm Hg, Dr. Mehta and associates said.
According to the statement, severe hypertriglyceridemia and familial hypercholesterolemia are the two most common conditions in which lipids should be addressed during pregnancy, with consideration of the fetal risks associated with certain medications.
“Statins are contraindicated during pregnancy, and all women who are on any lipid-lowering agents should review with their physician the safety of treatment during pregnancy and whether to discontinue treatment before pregnancy,” according to the statement. A heart-healthy lifestyle can help improve lipid profiles in all pregnant patients, Dr. Mehta and associates said. Patients with extremely high triglycerides above 500 mg/dL are at risk of pancreatitis and “may benefit from pharmacological agents (omega-3 fatty acids with or without fenofibrate or gemfibrozil) during the second trimester,” they noted. Pregnant women with familial hypercholesterolemia might take bile acid sequestrants, or as a last resort, low-density lipoprotein apheresis.
Other conditions calling for a multidisciplinary cardio-obstetric approach include preexisting coronary artery disease, cardiomyopathies, arrhythmias, valvular heart disease, cerebrovascular disease, and deep venous thrombosis, according to the statement, which provides information about the risks, diagnosis, and management.
When it is time for delivery, spontaneous labor and vaginal birth are preferable for most women with heart disease, as cesarean delivery is associated with increased risk of infection, thrombotic complications, and blood loss, according to the statement.
Women with CVD and associated complications will require “specialized long-term cardiovascular follow-up,” Dr. Mehta and associates said. “In women with a high-risk pregnancy, a cardio-obstetrics team is essential to prevent maternal morbidity and mortality during the length of the pregnancy and post partum.”
“The release of this document demonstrates the AHA’s recognition of the importance of CVD in pregnancy-related death and their commitment to education and ensuring best practices in this field,” said Lisa M. Hollier, MD, past president of the American College of Obstetricians and Gynecologists and chief medical officer at Texas Children’s Health Plan, Bellaire.
“I think one of the most important outcomes from the release of this scientific statement from AHA will be increased implementation of cardio-obstetrics teams,” she said in an interview.
“In the United States, cardiovascular disease and cardiomyopathy together are now the leading cause of death in pregnancy and the postpartum period, and constitute 26.5% of pregnancy-related deaths, with higher rates of mortality among women of color and women with lower incomes,” she said. “The rising trend in cardiovascular-related maternal deaths appears to be due to acquired, not congenital, heart disease.”
During her tenure as president of ACOG, Dr. Hollier convened a task force on cardiovascular disease in pregnancy that developed guidance that outlines screening, diagnosis, and management of CVD for women from prepregnancy through post partum.
Dr. Hollier noted that COVID-19 emphasizes racial disparities for maternal mortality.
“Pregnant patients with comorbidities, like heart conditions, may be at increased risk for severe illness from COVID-19 – consistent with the general population with similar comorbidities,” she said. “And as we know, black women’s risk of dying from CVD-related pregnancy complications is 3.4 times higher than that of white women. During the COVID-19 pandemic, we are seeing these racial health disparities exacerbated.”
However, any pregnant patients should not hesitate to communicate with their health care providers despite the pandemic situation, Dr. Hollier emphasized. “Communication between a patient and her ob.gyn., cardiologist, or other clinician is even more critical now during the COVID-19 pandemic. We’re hearing reports that patients who are experiencing symptoms or those with known cardiac conditions are avoiding the hospital and delaying or not seeking necessary treatment. This has the very real possibility of worsening the devastating maternal mortality crisis that we’re already experiencing in this country.”
To help overcome barriers to treatment, “collaboration between ob.gyns. and cardiologists, such as the cardio-obstetrics team or pregnancy heart team, is critical,” said Dr. Hollier. “These collaborative teams with a multidisciplinary approach can prospectively reduce the communication gaps across specialties when patients are seen separately. They can also improve the communication during care transitions such as between outpatient and inpatient care.
“In reviews of maternal deaths, we have found that there are often delays in diagnosis of heart conditions during and after pregnancy,” Dr. Hollier added. “Most maternal deaths from CVD are due to either undiagnosed cardiovascular disease or new-onset cardiomyopathy. ACOG recommends that all women be assessed for cardiovascular disease in the antepartum and postpartum periods using a recently developed algorithm,” she said. “Women who have known CVD and women who have concerning symptoms should have a consultation with this team. With increased awareness and screening, women can receive the additional care that they need.
“Because management of cardiac conditions in pregnancy is so complex, it is important to ensure that women receive care with teams and in facilities that have appropriate resources,” explained Dr. Hollier. “Women with known heart disease should see a cardiologist prior to pregnancy and receive prepregnancy counseling,” as noted in the AHA statement. “Patients determined to have moderate and high-risk CVD should be managed during pregnancy, delivery, and post partum in a medical center that is able to provide a higher level of care, including a cardio-obstetrics team.”
Early recognition of cardiovascular conditions is essential to help manage care and reduce risks to mother and baby, said Dr. Hollier. “Identification before a woman becomes pregnant means the patient’s care can be properly managed throughout the pregnancy and a detailed delivery plan can be developed through shared decision making between the patient and provider. We must think of heart disease as a possibility in every pregnant or postpartum patient we see to detect and treat at-risk mothers,” she said.
Additional research should focus on identifying risk factors prior to pregnancy, said Dr. Hollier. “There are often delays in recognizing symptoms during pregnancy and post partum, particularly for black women. We need data to understand which protocols are best to identify heart disease,”
Dr. Hollier had no financial conflicts to disclose. The authors of the AHA statement had no financial conflicts to disclose. The scientific statement was produced on behalf of the American Heart Association Council on Clinical Cardiology; Council on Atherosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
SOURCE: Mehta LS et al. Circulation. 2020 May 4. doi: 10.1161/CIR.0000000000000772.
according to a statement from the American Heart Association.
Cardiovascular disease (CVD) remains the leading cause of pregnancy-related mortality in the United States, and accounted for approximately 17 deaths per 100,000 live births in 2015, wrote Laxmi S. Mehta, MD, of The Ohio State University, Columbus, and colleagues.
Ideally, a woman with CVD at the time of pregnancy should be managed by a multidisciplinary cardio-obstetrics team that can assess cardiovascular risk, obstetric risk, and fetal risk throughout pregnancy, delivery, and up to a year post partum. The team should develop a shared strategy to promote best outcomes, according to the statement. The cardio-obstetrics team may include obstetricians, cardiologists, anesthesiologists, maternal-fetal medicine specialists, geneticists, neurologists, nurses, and pharmacists, according to the statement.
Women with preexisting CVD should receive counseling about maternal and fetal risks before conception, if possible, to involve the women in shared decision-making and to develop strategies for each stage of pregnancy and delivery, Dr. Mehta and associates said. Such counseling should include a review of all medications and assessment of risk factors.
However, some women present already in the early stages of pregnancy even with severe conditions such as pulmonary arterial hypertension, severe ventricular dysfunction, severe left-sided heart obstruction, and significant aortic dilatation with underlying connective tissue disease. Women with these conditions often are counseled to avoid pregnancy, but if they already are pregnant, a high-risk cardio-obstetrics team will need to work together to discover the best strategies going forward to mitigate risk, Dr. Mehta and associates said.
Common CVD conditions that affect pregnancy include hypertensive disorders, notably preeclampsia, defined as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg in women after 20 weeks of gestation whose blood pressure was normal prior to pregnancy. A management strategy to reduce the risk of pregnancy-related complications from hypertension includes healthy lifestyle behaviors such as exercise, nutrition, and smoking cessation, according to the statement. However, patients with severe hypertension may require intravenous labetalol or hydralazine. The statement gives more information about handling preeclampsia with pulmonary edema, and prevention of eclampsia and treatment of seizures.
It is important to recognize that severe hypertension or superimposed preeclampsia may occur for the first time post partum. Early ambulatory visits in the first 1-2 weeks are sensible. Medications may be needed to keep a systolic blood pressure not higher than 150 mm Hg and a diastolic blood pressure not higher than 100 mm Hg, Dr. Mehta and associates said.
According to the statement, severe hypertriglyceridemia and familial hypercholesterolemia are the two most common conditions in which lipids should be addressed during pregnancy, with consideration of the fetal risks associated with certain medications.
“Statins are contraindicated during pregnancy, and all women who are on any lipid-lowering agents should review with their physician the safety of treatment during pregnancy and whether to discontinue treatment before pregnancy,” according to the statement. A heart-healthy lifestyle can help improve lipid profiles in all pregnant patients, Dr. Mehta and associates said. Patients with extremely high triglycerides above 500 mg/dL are at risk of pancreatitis and “may benefit from pharmacological agents (omega-3 fatty acids with or without fenofibrate or gemfibrozil) during the second trimester,” they noted. Pregnant women with familial hypercholesterolemia might take bile acid sequestrants, or as a last resort, low-density lipoprotein apheresis.
Other conditions calling for a multidisciplinary cardio-obstetric approach include preexisting coronary artery disease, cardiomyopathies, arrhythmias, valvular heart disease, cerebrovascular disease, and deep venous thrombosis, according to the statement, which provides information about the risks, diagnosis, and management.
When it is time for delivery, spontaneous labor and vaginal birth are preferable for most women with heart disease, as cesarean delivery is associated with increased risk of infection, thrombotic complications, and blood loss, according to the statement.
Women with CVD and associated complications will require “specialized long-term cardiovascular follow-up,” Dr. Mehta and associates said. “In women with a high-risk pregnancy, a cardio-obstetrics team is essential to prevent maternal morbidity and mortality during the length of the pregnancy and post partum.”
“The release of this document demonstrates the AHA’s recognition of the importance of CVD in pregnancy-related death and their commitment to education and ensuring best practices in this field,” said Lisa M. Hollier, MD, past president of the American College of Obstetricians and Gynecologists and chief medical officer at Texas Children’s Health Plan, Bellaire.
“I think one of the most important outcomes from the release of this scientific statement from AHA will be increased implementation of cardio-obstetrics teams,” she said in an interview.
“In the United States, cardiovascular disease and cardiomyopathy together are now the leading cause of death in pregnancy and the postpartum period, and constitute 26.5% of pregnancy-related deaths, with higher rates of mortality among women of color and women with lower incomes,” she said. “The rising trend in cardiovascular-related maternal deaths appears to be due to acquired, not congenital, heart disease.”
During her tenure as president of ACOG, Dr. Hollier convened a task force on cardiovascular disease in pregnancy that developed guidance that outlines screening, diagnosis, and management of CVD for women from prepregnancy through post partum.
Dr. Hollier noted that COVID-19 emphasizes racial disparities for maternal mortality.
“Pregnant patients with comorbidities, like heart conditions, may be at increased risk for severe illness from COVID-19 – consistent with the general population with similar comorbidities,” she said. “And as we know, black women’s risk of dying from CVD-related pregnancy complications is 3.4 times higher than that of white women. During the COVID-19 pandemic, we are seeing these racial health disparities exacerbated.”
However, any pregnant patients should not hesitate to communicate with their health care providers despite the pandemic situation, Dr. Hollier emphasized. “Communication between a patient and her ob.gyn., cardiologist, or other clinician is even more critical now during the COVID-19 pandemic. We’re hearing reports that patients who are experiencing symptoms or those with known cardiac conditions are avoiding the hospital and delaying or not seeking necessary treatment. This has the very real possibility of worsening the devastating maternal mortality crisis that we’re already experiencing in this country.”
To help overcome barriers to treatment, “collaboration between ob.gyns. and cardiologists, such as the cardio-obstetrics team or pregnancy heart team, is critical,” said Dr. Hollier. “These collaborative teams with a multidisciplinary approach can prospectively reduce the communication gaps across specialties when patients are seen separately. They can also improve the communication during care transitions such as between outpatient and inpatient care.
“In reviews of maternal deaths, we have found that there are often delays in diagnosis of heart conditions during and after pregnancy,” Dr. Hollier added. “Most maternal deaths from CVD are due to either undiagnosed cardiovascular disease or new-onset cardiomyopathy. ACOG recommends that all women be assessed for cardiovascular disease in the antepartum and postpartum periods using a recently developed algorithm,” she said. “Women who have known CVD and women who have concerning symptoms should have a consultation with this team. With increased awareness and screening, women can receive the additional care that they need.
“Because management of cardiac conditions in pregnancy is so complex, it is important to ensure that women receive care with teams and in facilities that have appropriate resources,” explained Dr. Hollier. “Women with known heart disease should see a cardiologist prior to pregnancy and receive prepregnancy counseling,” as noted in the AHA statement. “Patients determined to have moderate and high-risk CVD should be managed during pregnancy, delivery, and post partum in a medical center that is able to provide a higher level of care, including a cardio-obstetrics team.”
Early recognition of cardiovascular conditions is essential to help manage care and reduce risks to mother and baby, said Dr. Hollier. “Identification before a woman becomes pregnant means the patient’s care can be properly managed throughout the pregnancy and a detailed delivery plan can be developed through shared decision making between the patient and provider. We must think of heart disease as a possibility in every pregnant or postpartum patient we see to detect and treat at-risk mothers,” she said.
Additional research should focus on identifying risk factors prior to pregnancy, said Dr. Hollier. “There are often delays in recognizing symptoms during pregnancy and post partum, particularly for black women. We need data to understand which protocols are best to identify heart disease,”
Dr. Hollier had no financial conflicts to disclose. The authors of the AHA statement had no financial conflicts to disclose. The scientific statement was produced on behalf of the American Heart Association Council on Clinical Cardiology; Council on Atherosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
SOURCE: Mehta LS et al. Circulation. 2020 May 4. doi: 10.1161/CIR.0000000000000772.
according to a statement from the American Heart Association.
Cardiovascular disease (CVD) remains the leading cause of pregnancy-related mortality in the United States, and accounted for approximately 17 deaths per 100,000 live births in 2015, wrote Laxmi S. Mehta, MD, of The Ohio State University, Columbus, and colleagues.
Ideally, a woman with CVD at the time of pregnancy should be managed by a multidisciplinary cardio-obstetrics team that can assess cardiovascular risk, obstetric risk, and fetal risk throughout pregnancy, delivery, and up to a year post partum. The team should develop a shared strategy to promote best outcomes, according to the statement. The cardio-obstetrics team may include obstetricians, cardiologists, anesthesiologists, maternal-fetal medicine specialists, geneticists, neurologists, nurses, and pharmacists, according to the statement.
Women with preexisting CVD should receive counseling about maternal and fetal risks before conception, if possible, to involve the women in shared decision-making and to develop strategies for each stage of pregnancy and delivery, Dr. Mehta and associates said. Such counseling should include a review of all medications and assessment of risk factors.
However, some women present already in the early stages of pregnancy even with severe conditions such as pulmonary arterial hypertension, severe ventricular dysfunction, severe left-sided heart obstruction, and significant aortic dilatation with underlying connective tissue disease. Women with these conditions often are counseled to avoid pregnancy, but if they already are pregnant, a high-risk cardio-obstetrics team will need to work together to discover the best strategies going forward to mitigate risk, Dr. Mehta and associates said.
Common CVD conditions that affect pregnancy include hypertensive disorders, notably preeclampsia, defined as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg in women after 20 weeks of gestation whose blood pressure was normal prior to pregnancy. A management strategy to reduce the risk of pregnancy-related complications from hypertension includes healthy lifestyle behaviors such as exercise, nutrition, and smoking cessation, according to the statement. However, patients with severe hypertension may require intravenous labetalol or hydralazine. The statement gives more information about handling preeclampsia with pulmonary edema, and prevention of eclampsia and treatment of seizures.
It is important to recognize that severe hypertension or superimposed preeclampsia may occur for the first time post partum. Early ambulatory visits in the first 1-2 weeks are sensible. Medications may be needed to keep a systolic blood pressure not higher than 150 mm Hg and a diastolic blood pressure not higher than 100 mm Hg, Dr. Mehta and associates said.
According to the statement, severe hypertriglyceridemia and familial hypercholesterolemia are the two most common conditions in which lipids should be addressed during pregnancy, with consideration of the fetal risks associated with certain medications.
“Statins are contraindicated during pregnancy, and all women who are on any lipid-lowering agents should review with their physician the safety of treatment during pregnancy and whether to discontinue treatment before pregnancy,” according to the statement. A heart-healthy lifestyle can help improve lipid profiles in all pregnant patients, Dr. Mehta and associates said. Patients with extremely high triglycerides above 500 mg/dL are at risk of pancreatitis and “may benefit from pharmacological agents (omega-3 fatty acids with or without fenofibrate or gemfibrozil) during the second trimester,” they noted. Pregnant women with familial hypercholesterolemia might take bile acid sequestrants, or as a last resort, low-density lipoprotein apheresis.
Other conditions calling for a multidisciplinary cardio-obstetric approach include preexisting coronary artery disease, cardiomyopathies, arrhythmias, valvular heart disease, cerebrovascular disease, and deep venous thrombosis, according to the statement, which provides information about the risks, diagnosis, and management.
When it is time for delivery, spontaneous labor and vaginal birth are preferable for most women with heart disease, as cesarean delivery is associated with increased risk of infection, thrombotic complications, and blood loss, according to the statement.
Women with CVD and associated complications will require “specialized long-term cardiovascular follow-up,” Dr. Mehta and associates said. “In women with a high-risk pregnancy, a cardio-obstetrics team is essential to prevent maternal morbidity and mortality during the length of the pregnancy and post partum.”
“The release of this document demonstrates the AHA’s recognition of the importance of CVD in pregnancy-related death and their commitment to education and ensuring best practices in this field,” said Lisa M. Hollier, MD, past president of the American College of Obstetricians and Gynecologists and chief medical officer at Texas Children’s Health Plan, Bellaire.
“I think one of the most important outcomes from the release of this scientific statement from AHA will be increased implementation of cardio-obstetrics teams,” she said in an interview.
“In the United States, cardiovascular disease and cardiomyopathy together are now the leading cause of death in pregnancy and the postpartum period, and constitute 26.5% of pregnancy-related deaths, with higher rates of mortality among women of color and women with lower incomes,” she said. “The rising trend in cardiovascular-related maternal deaths appears to be due to acquired, not congenital, heart disease.”
During her tenure as president of ACOG, Dr. Hollier convened a task force on cardiovascular disease in pregnancy that developed guidance that outlines screening, diagnosis, and management of CVD for women from prepregnancy through post partum.
Dr. Hollier noted that COVID-19 emphasizes racial disparities for maternal mortality.
“Pregnant patients with comorbidities, like heart conditions, may be at increased risk for severe illness from COVID-19 – consistent with the general population with similar comorbidities,” she said. “And as we know, black women’s risk of dying from CVD-related pregnancy complications is 3.4 times higher than that of white women. During the COVID-19 pandemic, we are seeing these racial health disparities exacerbated.”
However, any pregnant patients should not hesitate to communicate with their health care providers despite the pandemic situation, Dr. Hollier emphasized. “Communication between a patient and her ob.gyn., cardiologist, or other clinician is even more critical now during the COVID-19 pandemic. We’re hearing reports that patients who are experiencing symptoms or those with known cardiac conditions are avoiding the hospital and delaying or not seeking necessary treatment. This has the very real possibility of worsening the devastating maternal mortality crisis that we’re already experiencing in this country.”
To help overcome barriers to treatment, “collaboration between ob.gyns. and cardiologists, such as the cardio-obstetrics team or pregnancy heart team, is critical,” said Dr. Hollier. “These collaborative teams with a multidisciplinary approach can prospectively reduce the communication gaps across specialties when patients are seen separately. They can also improve the communication during care transitions such as between outpatient and inpatient care.
“In reviews of maternal deaths, we have found that there are often delays in diagnosis of heart conditions during and after pregnancy,” Dr. Hollier added. “Most maternal deaths from CVD are due to either undiagnosed cardiovascular disease or new-onset cardiomyopathy. ACOG recommends that all women be assessed for cardiovascular disease in the antepartum and postpartum periods using a recently developed algorithm,” she said. “Women who have known CVD and women who have concerning symptoms should have a consultation with this team. With increased awareness and screening, women can receive the additional care that they need.
“Because management of cardiac conditions in pregnancy is so complex, it is important to ensure that women receive care with teams and in facilities that have appropriate resources,” explained Dr. Hollier. “Women with known heart disease should see a cardiologist prior to pregnancy and receive prepregnancy counseling,” as noted in the AHA statement. “Patients determined to have moderate and high-risk CVD should be managed during pregnancy, delivery, and post partum in a medical center that is able to provide a higher level of care, including a cardio-obstetrics team.”
Early recognition of cardiovascular conditions is essential to help manage care and reduce risks to mother and baby, said Dr. Hollier. “Identification before a woman becomes pregnant means the patient’s care can be properly managed throughout the pregnancy and a detailed delivery plan can be developed through shared decision making between the patient and provider. We must think of heart disease as a possibility in every pregnant or postpartum patient we see to detect and treat at-risk mothers,” she said.
Additional research should focus on identifying risk factors prior to pregnancy, said Dr. Hollier. “There are often delays in recognizing symptoms during pregnancy and post partum, particularly for black women. We need data to understand which protocols are best to identify heart disease,”
Dr. Hollier had no financial conflicts to disclose. The authors of the AHA statement had no financial conflicts to disclose. The scientific statement was produced on behalf of the American Heart Association Council on Clinical Cardiology; Council on Atherosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
SOURCE: Mehta LS et al. Circulation. 2020 May 4. doi: 10.1161/CIR.0000000000000772.
FROM CIRCULATION
Hand Hygiene in Preventing COVID-19 Transmission
Handwashing with antimicrobial soaps or alcohol-based sanitizers is an effective measure in preventing microbial disease transmission. In the context of coronavirus disease 2019 (COVID-19) prevention, the World Health Organization and Centers for Disease Control and Prevention have recommended handwashing with soap and water after coughing/sneezing, visiting a public place, touching surfaces outside the home, and taking care of a sick person(s), as well as before and after eating. When soap and water are not available, alcohol-based sanitizers may be used.1,2
Irritant contact dermatitis (ICD) is most commonly associated with wet work and is frequently seen in health care workers in relation to hand hygiene, with survey-based studies reporting 25% to 55% of nurses affected.3-5 In a prospective study (N=102), health care workers who washed their hands more than 10 times per day were55% more likely to develop hand dermatitis.6 Frequent ICD of the hands has been reported in Chinese health care workers in association with COVID-19.7 Handwashing and/or glove wearing may be newly prioritized by workers who handle frequently touched goods and surfaces, such as flight attendants (Figure). Patients with obsessive-compulsive disorder may be another vulnerable population.8

Alcohol-based sanitizers and detergents or antimicrobials in soaps may cause ICD of the hands by denaturation of stratum corneum proteins, depletion of intercellular lipids, and decreased corneocyte cohesion. These agents alter the skin flora, with increased colonization by staphylococci and gram-negative bacilli.9 Clinical findings include xerosis, scaling, fissuring, and bleeding. Physicians may evaluate severity of ICD of the hands using the
Cleansing the hands with alcohol-based sanitizers has consistently shown equivalent or greater efficacy than antimicrobial soaps for eradication of most microbes, with exception of bacterial spores and protozoan oocysts.11 In an in vivo experiment, 70% ethanol solution was more effective in eradicating rotavirus from the fingerpads of adults than 10% povidone-iodine solution, nonmedicated soaps, and soaps containing chloroxylenol 4.8% or chlorhexidine gluconate 4%.12 Coronavirus disease 2019 is a lipophilic enveloped virus. The lipid-dissolving effects of alcohol-based sanitizers is especially effective against these kinds of viruses. An in vitro experiment showed that alcohol solutions are effective against enveloped viruses including severe acute respiratory syndrome coronavirus, Ebola virus, and Zika virus.13 There are limited data for the virucidal efficacy of non–alcohol-based sanitizers containing quaternary ammonium compounds (most commonly benzalkonium chloride) and therefore they are not recommended for protection against COVID-19. Handwashing is preferred over alcohol-based solutions when hands are visibly dirty.
Alcohol-based sanitizers typically are less likely to cause ICD than handwashing with detergent-based or antimicrobial soaps. Antimicrobial ingredients in soaps such as chlorhexidine, chloroxylenol, and triclosan are frequent culprits.11 Detergents in soap such as sodium laureth sulfate cause more skin irritation and transepidermal water loss than alcohol14; however, among health care workers, alcohol-based sanitizers often are perceived as more damaging to the skin.15 During the 2014 Ebola outbreak, use of alcohol-based sanitizers vs handwashing resulted in lower hand eczema severity index scores (n=108).16
Propensity for ICD is a limiting factor in hand hygiene adherence.17 In a double-blind randomized trial (N=54), scheduled use of an oil-containing lotion was shown to increase compliance with hand hygiene protocols in health care workers by preventing cracks, scaling, and pain.18 Using sanitizers containing humectants (eg, aloe vera gel) or moisturizers with petrolatum, liquid paraffin, glycerin, or mineral oil have all been shown to decrease the incidence of ICD in frequent handwashers.19,20 Thorough hand drying also is important in preventing dermatitis. Drying with disposable paper towels is preferred over automated air dryers to prevent aerosolization of microbes.21 Because latex has been implicated in development of ICD, use of latex-free gloves is recommended.22
Alcohol-based sanitizer is not only an effective virucidal agent but also is less likely to cause ICD, therefore promoting hand hygiene adherence. Handwashing with soap still is necessary when hands are visibly dirty but should be performed less frequently if feasible. Hand hygiene and emollient usage education is important for physicians and patients alike, particularly during the COVID-19 crisis.
- Centers for Disease Control and Prevention. Coronavirus disease 2019. how to protect yourself & others. https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html. Updated April 13, 2020. Accessed April 21, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Updated March 31, 2020. Accessed April 21, 2020.
- Carøe TK, Ebbehøj NE, Bonde JPE, et al. Hand eczema and wet work: dose-response relationship and effect of leaving the profession. Contact Dermatitis. 2018;78:341-347.
- Larson E, Friedman C, Cohran J, et al. Prevalence and correlates of skin damage on the hands of nurses. Heart Lung. 1997;26:404-412.
- Lampel HP, Patel N, Boyse K, et al. Prevalence of hand dermatitis in inpatient nurses at a United States hospital. Dermatitis. 2007;18:140-142.
- Callahan A, Baron E, Fekedulegn D, et al. Winter season, frequent hand washing, and irritant patch test reactions to detergents are associated with hand dermatitis in health care workers. Dermatitis. 2013;24:170-175.
- Lan J, Song Z, Miao X, et al. Skin damage among healthcare workers managing coronavirus disease-2019 [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1215-1216.
- Katz RJ, Landau P, DeVeaugh-Geiss J, et al. Pharmacological responsiveness of dermatitis secondary to compulsive washing. Psychiatry Res. 1990;34:223-226.
- Larson EL, Hughes CA, Pyrek JD, et al. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am J Infect Control. 1998;26:513-521.
- Held E, Skoet R, Johansen JD, et al. The hand eczema severity index (HECSI): a scoring system for clinical assessment of hand eczema. a study of inter- and intraobserver reliability. Br J Dermatol. 2005;152:302-307.
- Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee, et al. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am J Infect Control. 2002;30:S1-S46.
- Ansari SA, Sattar SA, Springthorpe VS, et al. Invivo protocol for testing efficacy of hand-washing agents against viruses and bacteria—experiments with rotavirus and Escherichi coli. Appl Environ Microbiol. 1989;55:3113-3118.
- Siddharta A, Pfaender S, Vielle NJ, et al. virucidal activity of world health organization-recommended formulations against enveloped viruses, including Zika, Ebola, and emerging coronaviruses. J Infect Dis. 2017;215:902-906.
- Pedersen LK, Held E, Johansen JD, et al. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol. 2005;153:1142-1146.
- Stutz N, Becker D, Jappe U, et al. Nurses’ perceptions of the benefits and adverse effects of hand disinfection: alcohol-based hand rubs vs. hygienic handwashing: a multicentre questionnaire study with additional patch testing by the German Contact Dermatitis Research Group. Br J Dermatol. 2009;160:565-572.
- Wolfe MK, Wells E, Mitro B, et al. Seeking clearer recommendations for hand hygiene in communities facing Ebola: a randomized trial investigating the impact of six handwashing methods on skin irritation and dermatitis. PLoS One. 2016;11:e0167378.
- Pittet D, Allegranzi B, Storr J. The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health. 2008;1:4-10.
- McCormick RD, Buchman TL, Maki DG. Double-blind, randomized trial of scheduled use of a novel barrier cream and an oil-containing lotion for protecting the hands of health care workers. Am J Infect Control. 2000;28:302-310.
- Berndt U, Wigger-Alberti W, Gabard B, et al. Efficacy of a barrier cream and its vehicle as protective measures against occupational irritant contact dermatitis. Contact Dermatitis. 2000;42:77-80.
- Kampf G, Ennen J. Regular use of a hand cream can attenuate skin dryness and roughness caused by frequent hand washing. BMC Dermatol. 2006;6:1.
- Gammon J, Hunt J. The neglected element of hand hygiene - significance of hand drying, efficiency of different methods, and clinical implication: a review. J Infect Prev. 2019;20:66-74.
- Elston DM. Letter from the editor: occupational skin disease among healthcare workers during the coronavirus (COVID-19) epidemic [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1085-1086.
Handwashing with antimicrobial soaps or alcohol-based sanitizers is an effective measure in preventing microbial disease transmission. In the context of coronavirus disease 2019 (COVID-19) prevention, the World Health Organization and Centers for Disease Control and Prevention have recommended handwashing with soap and water after coughing/sneezing, visiting a public place, touching surfaces outside the home, and taking care of a sick person(s), as well as before and after eating. When soap and water are not available, alcohol-based sanitizers may be used.1,2
Irritant contact dermatitis (ICD) is most commonly associated with wet work and is frequently seen in health care workers in relation to hand hygiene, with survey-based studies reporting 25% to 55% of nurses affected.3-5 In a prospective study (N=102), health care workers who washed their hands more than 10 times per day were55% more likely to develop hand dermatitis.6 Frequent ICD of the hands has been reported in Chinese health care workers in association with COVID-19.7 Handwashing and/or glove wearing may be newly prioritized by workers who handle frequently touched goods and surfaces, such as flight attendants (Figure). Patients with obsessive-compulsive disorder may be another vulnerable population.8

Alcohol-based sanitizers and detergents or antimicrobials in soaps may cause ICD of the hands by denaturation of stratum corneum proteins, depletion of intercellular lipids, and decreased corneocyte cohesion. These agents alter the skin flora, with increased colonization by staphylococci and gram-negative bacilli.9 Clinical findings include xerosis, scaling, fissuring, and bleeding. Physicians may evaluate severity of ICD of the hands using the
Cleansing the hands with alcohol-based sanitizers has consistently shown equivalent or greater efficacy than antimicrobial soaps for eradication of most microbes, with exception of bacterial spores and protozoan oocysts.11 In an in vivo experiment, 70% ethanol solution was more effective in eradicating rotavirus from the fingerpads of adults than 10% povidone-iodine solution, nonmedicated soaps, and soaps containing chloroxylenol 4.8% or chlorhexidine gluconate 4%.12 Coronavirus disease 2019 is a lipophilic enveloped virus. The lipid-dissolving effects of alcohol-based sanitizers is especially effective against these kinds of viruses. An in vitro experiment showed that alcohol solutions are effective against enveloped viruses including severe acute respiratory syndrome coronavirus, Ebola virus, and Zika virus.13 There are limited data for the virucidal efficacy of non–alcohol-based sanitizers containing quaternary ammonium compounds (most commonly benzalkonium chloride) and therefore they are not recommended for protection against COVID-19. Handwashing is preferred over alcohol-based solutions when hands are visibly dirty.
Alcohol-based sanitizers typically are less likely to cause ICD than handwashing with detergent-based or antimicrobial soaps. Antimicrobial ingredients in soaps such as chlorhexidine, chloroxylenol, and triclosan are frequent culprits.11 Detergents in soap such as sodium laureth sulfate cause more skin irritation and transepidermal water loss than alcohol14; however, among health care workers, alcohol-based sanitizers often are perceived as more damaging to the skin.15 During the 2014 Ebola outbreak, use of alcohol-based sanitizers vs handwashing resulted in lower hand eczema severity index scores (n=108).16
Propensity for ICD is a limiting factor in hand hygiene adherence.17 In a double-blind randomized trial (N=54), scheduled use of an oil-containing lotion was shown to increase compliance with hand hygiene protocols in health care workers by preventing cracks, scaling, and pain.18 Using sanitizers containing humectants (eg, aloe vera gel) or moisturizers with petrolatum, liquid paraffin, glycerin, or mineral oil have all been shown to decrease the incidence of ICD in frequent handwashers.19,20 Thorough hand drying also is important in preventing dermatitis. Drying with disposable paper towels is preferred over automated air dryers to prevent aerosolization of microbes.21 Because latex has been implicated in development of ICD, use of latex-free gloves is recommended.22
Alcohol-based sanitizer is not only an effective virucidal agent but also is less likely to cause ICD, therefore promoting hand hygiene adherence. Handwashing with soap still is necessary when hands are visibly dirty but should be performed less frequently if feasible. Hand hygiene and emollient usage education is important for physicians and patients alike, particularly during the COVID-19 crisis.
Handwashing with antimicrobial soaps or alcohol-based sanitizers is an effective measure in preventing microbial disease transmission. In the context of coronavirus disease 2019 (COVID-19) prevention, the World Health Organization and Centers for Disease Control and Prevention have recommended handwashing with soap and water after coughing/sneezing, visiting a public place, touching surfaces outside the home, and taking care of a sick person(s), as well as before and after eating. When soap and water are not available, alcohol-based sanitizers may be used.1,2
Irritant contact dermatitis (ICD) is most commonly associated with wet work and is frequently seen in health care workers in relation to hand hygiene, with survey-based studies reporting 25% to 55% of nurses affected.3-5 In a prospective study (N=102), health care workers who washed their hands more than 10 times per day were55% more likely to develop hand dermatitis.6 Frequent ICD of the hands has been reported in Chinese health care workers in association with COVID-19.7 Handwashing and/or glove wearing may be newly prioritized by workers who handle frequently touched goods and surfaces, such as flight attendants (Figure). Patients with obsessive-compulsive disorder may be another vulnerable population.8

Alcohol-based sanitizers and detergents or antimicrobials in soaps may cause ICD of the hands by denaturation of stratum corneum proteins, depletion of intercellular lipids, and decreased corneocyte cohesion. These agents alter the skin flora, with increased colonization by staphylococci and gram-negative bacilli.9 Clinical findings include xerosis, scaling, fissuring, and bleeding. Physicians may evaluate severity of ICD of the hands using the
Cleansing the hands with alcohol-based sanitizers has consistently shown equivalent or greater efficacy than antimicrobial soaps for eradication of most microbes, with exception of bacterial spores and protozoan oocysts.11 In an in vivo experiment, 70% ethanol solution was more effective in eradicating rotavirus from the fingerpads of adults than 10% povidone-iodine solution, nonmedicated soaps, and soaps containing chloroxylenol 4.8% or chlorhexidine gluconate 4%.12 Coronavirus disease 2019 is a lipophilic enveloped virus. The lipid-dissolving effects of alcohol-based sanitizers is especially effective against these kinds of viruses. An in vitro experiment showed that alcohol solutions are effective against enveloped viruses including severe acute respiratory syndrome coronavirus, Ebola virus, and Zika virus.13 There are limited data for the virucidal efficacy of non–alcohol-based sanitizers containing quaternary ammonium compounds (most commonly benzalkonium chloride) and therefore they are not recommended for protection against COVID-19. Handwashing is preferred over alcohol-based solutions when hands are visibly dirty.
Alcohol-based sanitizers typically are less likely to cause ICD than handwashing with detergent-based or antimicrobial soaps. Antimicrobial ingredients in soaps such as chlorhexidine, chloroxylenol, and triclosan are frequent culprits.11 Detergents in soap such as sodium laureth sulfate cause more skin irritation and transepidermal water loss than alcohol14; however, among health care workers, alcohol-based sanitizers often are perceived as more damaging to the skin.15 During the 2014 Ebola outbreak, use of alcohol-based sanitizers vs handwashing resulted in lower hand eczema severity index scores (n=108).16
Propensity for ICD is a limiting factor in hand hygiene adherence.17 In a double-blind randomized trial (N=54), scheduled use of an oil-containing lotion was shown to increase compliance with hand hygiene protocols in health care workers by preventing cracks, scaling, and pain.18 Using sanitizers containing humectants (eg, aloe vera gel) or moisturizers with petrolatum, liquid paraffin, glycerin, or mineral oil have all been shown to decrease the incidence of ICD in frequent handwashers.19,20 Thorough hand drying also is important in preventing dermatitis. Drying with disposable paper towels is preferred over automated air dryers to prevent aerosolization of microbes.21 Because latex has been implicated in development of ICD, use of latex-free gloves is recommended.22
Alcohol-based sanitizer is not only an effective virucidal agent but also is less likely to cause ICD, therefore promoting hand hygiene adherence. Handwashing with soap still is necessary when hands are visibly dirty but should be performed less frequently if feasible. Hand hygiene and emollient usage education is important for physicians and patients alike, particularly during the COVID-19 crisis.
- Centers for Disease Control and Prevention. Coronavirus disease 2019. how to protect yourself & others. https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html. Updated April 13, 2020. Accessed April 21, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Updated March 31, 2020. Accessed April 21, 2020.
- Carøe TK, Ebbehøj NE, Bonde JPE, et al. Hand eczema and wet work: dose-response relationship and effect of leaving the profession. Contact Dermatitis. 2018;78:341-347.
- Larson E, Friedman C, Cohran J, et al. Prevalence and correlates of skin damage on the hands of nurses. Heart Lung. 1997;26:404-412.
- Lampel HP, Patel N, Boyse K, et al. Prevalence of hand dermatitis in inpatient nurses at a United States hospital. Dermatitis. 2007;18:140-142.
- Callahan A, Baron E, Fekedulegn D, et al. Winter season, frequent hand washing, and irritant patch test reactions to detergents are associated with hand dermatitis in health care workers. Dermatitis. 2013;24:170-175.
- Lan J, Song Z, Miao X, et al. Skin damage among healthcare workers managing coronavirus disease-2019 [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1215-1216.
- Katz RJ, Landau P, DeVeaugh-Geiss J, et al. Pharmacological responsiveness of dermatitis secondary to compulsive washing. Psychiatry Res. 1990;34:223-226.
- Larson EL, Hughes CA, Pyrek JD, et al. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am J Infect Control. 1998;26:513-521.
- Held E, Skoet R, Johansen JD, et al. The hand eczema severity index (HECSI): a scoring system for clinical assessment of hand eczema. a study of inter- and intraobserver reliability. Br J Dermatol. 2005;152:302-307.
- Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee, et al. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am J Infect Control. 2002;30:S1-S46.
- Ansari SA, Sattar SA, Springthorpe VS, et al. Invivo protocol for testing efficacy of hand-washing agents against viruses and bacteria—experiments with rotavirus and Escherichi coli. Appl Environ Microbiol. 1989;55:3113-3118.
- Siddharta A, Pfaender S, Vielle NJ, et al. virucidal activity of world health organization-recommended formulations against enveloped viruses, including Zika, Ebola, and emerging coronaviruses. J Infect Dis. 2017;215:902-906.
- Pedersen LK, Held E, Johansen JD, et al. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol. 2005;153:1142-1146.
- Stutz N, Becker D, Jappe U, et al. Nurses’ perceptions of the benefits and adverse effects of hand disinfection: alcohol-based hand rubs vs. hygienic handwashing: a multicentre questionnaire study with additional patch testing by the German Contact Dermatitis Research Group. Br J Dermatol. 2009;160:565-572.
- Wolfe MK, Wells E, Mitro B, et al. Seeking clearer recommendations for hand hygiene in communities facing Ebola: a randomized trial investigating the impact of six handwashing methods on skin irritation and dermatitis. PLoS One. 2016;11:e0167378.
- Pittet D, Allegranzi B, Storr J. The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health. 2008;1:4-10.
- McCormick RD, Buchman TL, Maki DG. Double-blind, randomized trial of scheduled use of a novel barrier cream and an oil-containing lotion for protecting the hands of health care workers. Am J Infect Control. 2000;28:302-310.
- Berndt U, Wigger-Alberti W, Gabard B, et al. Efficacy of a barrier cream and its vehicle as protective measures against occupational irritant contact dermatitis. Contact Dermatitis. 2000;42:77-80.
- Kampf G, Ennen J. Regular use of a hand cream can attenuate skin dryness and roughness caused by frequent hand washing. BMC Dermatol. 2006;6:1.
- Gammon J, Hunt J. The neglected element of hand hygiene - significance of hand drying, efficiency of different methods, and clinical implication: a review. J Infect Prev. 2019;20:66-74.
- Elston DM. Letter from the editor: occupational skin disease among healthcare workers during the coronavirus (COVID-19) epidemic [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1085-1086.
- Centers for Disease Control and Prevention. Coronavirus disease 2019. how to protect yourself & others. https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html. Updated April 13, 2020. Accessed April 21, 2020.
- World Health Organization. Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Updated March 31, 2020. Accessed April 21, 2020.
- Carøe TK, Ebbehøj NE, Bonde JPE, et al. Hand eczema and wet work: dose-response relationship and effect of leaving the profession. Contact Dermatitis. 2018;78:341-347.
- Larson E, Friedman C, Cohran J, et al. Prevalence and correlates of skin damage on the hands of nurses. Heart Lung. 1997;26:404-412.
- Lampel HP, Patel N, Boyse K, et al. Prevalence of hand dermatitis in inpatient nurses at a United States hospital. Dermatitis. 2007;18:140-142.
- Callahan A, Baron E, Fekedulegn D, et al. Winter season, frequent hand washing, and irritant patch test reactions to detergents are associated with hand dermatitis in health care workers. Dermatitis. 2013;24:170-175.
- Lan J, Song Z, Miao X, et al. Skin damage among healthcare workers managing coronavirus disease-2019 [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1215-1216.
- Katz RJ, Landau P, DeVeaugh-Geiss J, et al. Pharmacological responsiveness of dermatitis secondary to compulsive washing. Psychiatry Res. 1990;34:223-226.
- Larson EL, Hughes CA, Pyrek JD, et al. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am J Infect Control. 1998;26:513-521.
- Held E, Skoet R, Johansen JD, et al. The hand eczema severity index (HECSI): a scoring system for clinical assessment of hand eczema. a study of inter- and intraobserver reliability. Br J Dermatol. 2005;152:302-307.
- Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee, et al. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am J Infect Control. 2002;30:S1-S46.
- Ansari SA, Sattar SA, Springthorpe VS, et al. Invivo protocol for testing efficacy of hand-washing agents against viruses and bacteria—experiments with rotavirus and Escherichi coli. Appl Environ Microbiol. 1989;55:3113-3118.
- Siddharta A, Pfaender S, Vielle NJ, et al. virucidal activity of world health organization-recommended formulations against enveloped viruses, including Zika, Ebola, and emerging coronaviruses. J Infect Dis. 2017;215:902-906.
- Pedersen LK, Held E, Johansen JD, et al. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol. 2005;153:1142-1146.
- Stutz N, Becker D, Jappe U, et al. Nurses’ perceptions of the benefits and adverse effects of hand disinfection: alcohol-based hand rubs vs. hygienic handwashing: a multicentre questionnaire study with additional patch testing by the German Contact Dermatitis Research Group. Br J Dermatol. 2009;160:565-572.
- Wolfe MK, Wells E, Mitro B, et al. Seeking clearer recommendations for hand hygiene in communities facing Ebola: a randomized trial investigating the impact of six handwashing methods on skin irritation and dermatitis. PLoS One. 2016;11:e0167378.
- Pittet D, Allegranzi B, Storr J. The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health. 2008;1:4-10.
- McCormick RD, Buchman TL, Maki DG. Double-blind, randomized trial of scheduled use of a novel barrier cream and an oil-containing lotion for protecting the hands of health care workers. Am J Infect Control. 2000;28:302-310.
- Berndt U, Wigger-Alberti W, Gabard B, et al. Efficacy of a barrier cream and its vehicle as protective measures against occupational irritant contact dermatitis. Contact Dermatitis. 2000;42:77-80.
- Kampf G, Ennen J. Regular use of a hand cream can attenuate skin dryness and roughness caused by frequent hand washing. BMC Dermatol. 2006;6:1.
- Gammon J, Hunt J. The neglected element of hand hygiene - significance of hand drying, efficiency of different methods, and clinical implication: a review. J Infect Prev. 2019;20:66-74.
- Elston DM. Letter from the editor: occupational skin disease among healthcare workers during the coronavirus (COVID-19) epidemic [published online March 18, 2020]. J Am Acad Dermatol. 2020;82:1085-1086.
Practice Points
- Alcohol-based sanitizers are as or even more effective as handwashing with soap and water for preventing disease transmission of enveloped viruses such as severe acute respiratory syndrome coronavirus.
- Although perceived as more irritating, alcohol-based sanitizers are less likely to cause irritant contact dermatitis of the hands than handwashing with soap and water.
- Use of humectants, moisturizers, and/or emollients in combination with alcohol-based sanitizers allows for effective hand hygiene without irritating the skin.
Analysis of Education on Nail Conditions at the American Academy of Dermatology Annual Meetings
To the Editor:
The diagnosis and treatment of nail conditions are necessary competencies for board-certified dermatologists, but appropriate education often is lacking.1 The American Academy of Dermatology (AAD) annual meeting is one of the largest and most highly attended dermatology educational conferences worldwide. We sought to determine the number of hours dedicated to nail-related topics at the AAD annual meetings from 2013 to 2019.
We accessed programs from the AAD annual meetings archive online (https://www.aad.org/meetings/previous-meetings-archive), and we used hair and psoriasis content for comparison. Event titles and descriptions were searched for nail-related content (using search terms nail, onychia, and onycho), hair-related content (hair, alopecia, trichosis, hirsutism), and psoriasis content (psoriasis). Data acquired for each event included the date, hours, title, and event type (eg, forum, course, focus session, symposium, discussion group, workshop, plenary session).
The number of hours dedicated to nail education consistently lagged behind those related to hair and psoriasis content during the study period (Figure 1). According to the AAD, the conference runs Friday to Tuesday with higher attendance Friday to Sunday (Tim Moses, personal communication, July 9, 2019). Lectures during the weekend are likely to have a broader reach than lectures on Monday and Tuesday. The proportion of nail content during weekend prime time slots was similar to that of hair and psoriasis (Figure 2). Plenary sessions often are presented by renowned experts on hot topics in dermatology. Notably, hair (2014-2015) and psoriasis (2015-2017) content were represented in the plenary sessions during the study period, while nail content was not featured.

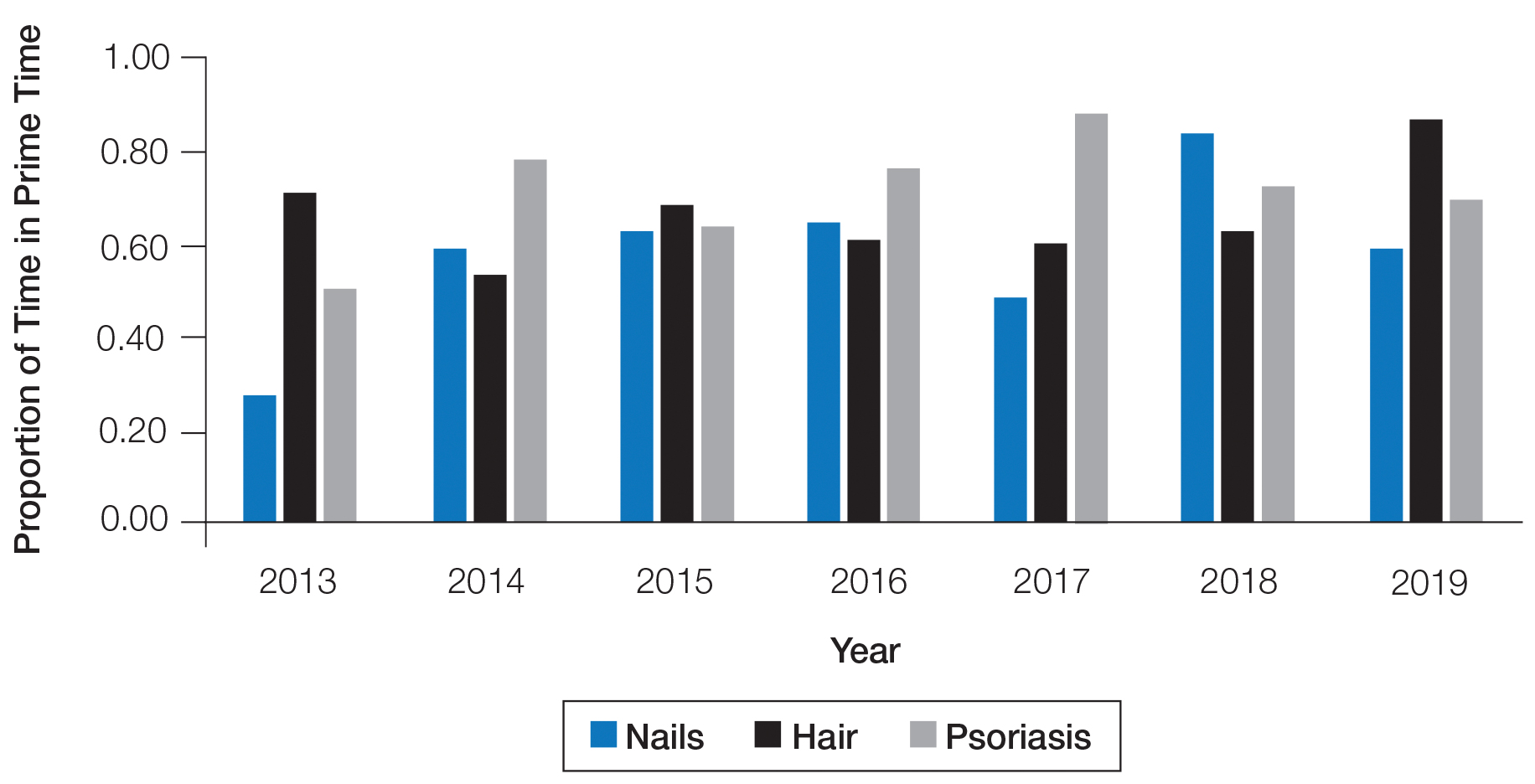
Our study shows that nail-related education was underrepresented at the AAD annual meetings from 2013 to 2019 compared to hair- and psoriasis-related content. Educational gaps in the diagnosis of fignail conditions previously have been delineated, and prioritization of instruction on nail disease pathology and diagnostic procedures has been recommended to improve patient care.1 The majority of nail unit melanomas are diagnosed at late stages, which has been attributed to deficiencies in clinical knowledge and failure to perform or inadequate biopsy techniques.2 Notably, a survey of third-year dermatology residents (N=240) assessing experience in procedural dermatology showed that 58% performed 10 or fewer nail procedures and 30% did not feel competent in performing nail surgery.3 Furthermore, a survey examining the management of longitudinal melanonychia among attending and resident dermatologists (N=402) found that 62% of residents and 28% of total respondents were not confident in managing melanonychia.4
A limitation of this study was the lack of online data available for AAD annual meetings before 2013, so we were unable to characterize any long-term trends. Furthermore, we were unable to assess the educational reach of these sessions, as data on attendance are lacking.
This study demonstrates a paucity of nail-related content at the AAD annual meetings. The introduction of the “Hands-on: Nail Surgery” in 2015 is an important step forward to diminish the knowledge gap in the diagnosis of various nail diseases and malignancies. We recommend increasing the number of hours and overall content of didactic nail sessions at the AAD annual meeting to further the knowledge and procedural skills of dermatologists in caring for patients with nail disorders.
- Hare AQ, R ich P. Clinical and educational gaps in diagnosis of nail disorders. Dermatol Clin. 2016;34:269-273.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol. 2007;31:1902-1912.
- Lee EH, Nehal KS, Dusza SW, et al. Procedural dermatology training during dermatology residency: a survey of third-year dermatology residents. J Am Acad Dermatol. 2011;64:475-483.
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996.
To the Editor:
The diagnosis and treatment of nail conditions are necessary competencies for board-certified dermatologists, but appropriate education often is lacking.1 The American Academy of Dermatology (AAD) annual meeting is one of the largest and most highly attended dermatology educational conferences worldwide. We sought to determine the number of hours dedicated to nail-related topics at the AAD annual meetings from 2013 to 2019.
We accessed programs from the AAD annual meetings archive online (https://www.aad.org/meetings/previous-meetings-archive), and we used hair and psoriasis content for comparison. Event titles and descriptions were searched for nail-related content (using search terms nail, onychia, and onycho), hair-related content (hair, alopecia, trichosis, hirsutism), and psoriasis content (psoriasis). Data acquired for each event included the date, hours, title, and event type (eg, forum, course, focus session, symposium, discussion group, workshop, plenary session).
The number of hours dedicated to nail education consistently lagged behind those related to hair and psoriasis content during the study period (Figure 1). According to the AAD, the conference runs Friday to Tuesday with higher attendance Friday to Sunday (Tim Moses, personal communication, July 9, 2019). Lectures during the weekend are likely to have a broader reach than lectures on Monday and Tuesday. The proportion of nail content during weekend prime time slots was similar to that of hair and psoriasis (Figure 2). Plenary sessions often are presented by renowned experts on hot topics in dermatology. Notably, hair (2014-2015) and psoriasis (2015-2017) content were represented in the plenary sessions during the study period, while nail content was not featured.

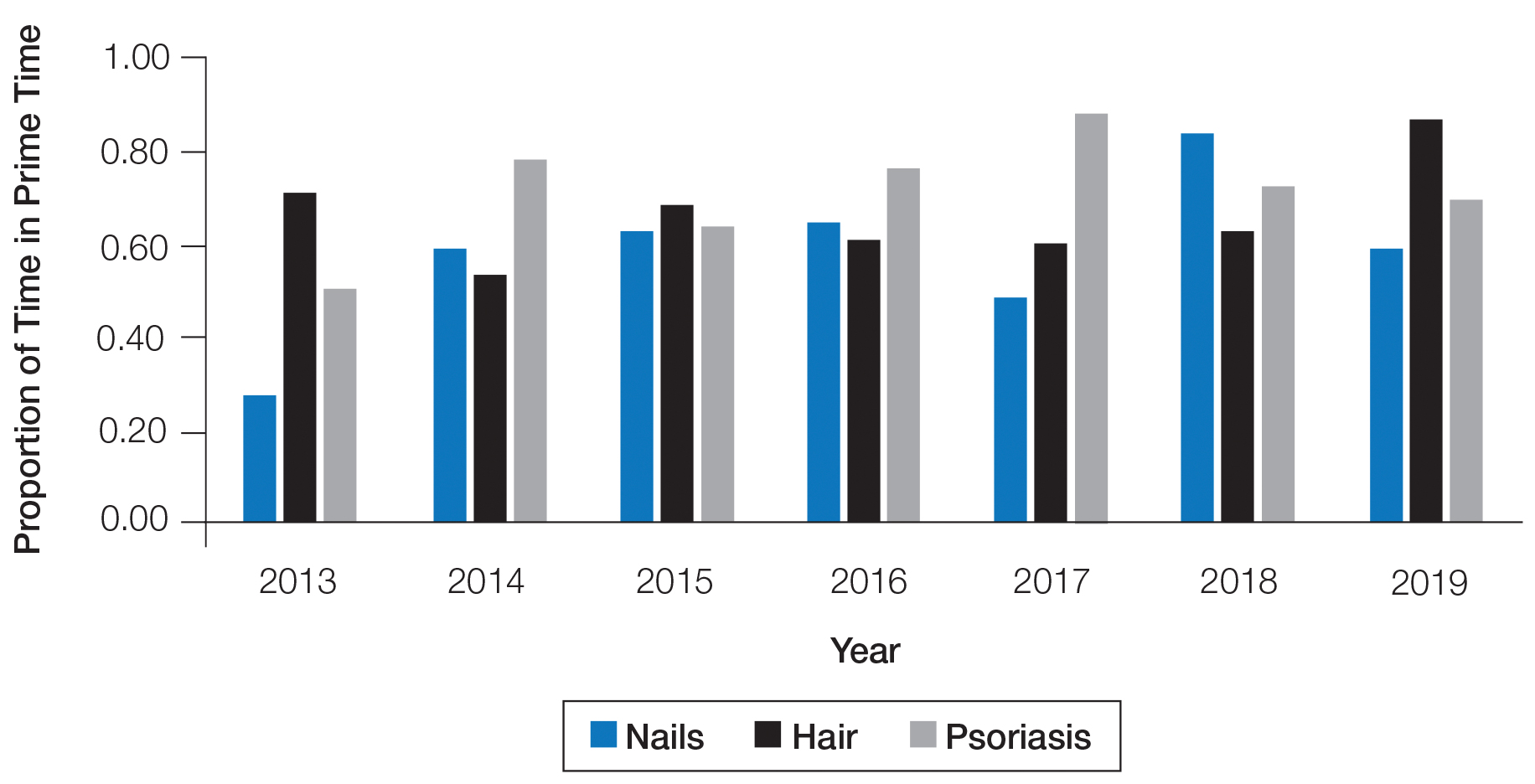
Our study shows that nail-related education was underrepresented at the AAD annual meetings from 2013 to 2019 compared to hair- and psoriasis-related content. Educational gaps in the diagnosis of fignail conditions previously have been delineated, and prioritization of instruction on nail disease pathology and diagnostic procedures has been recommended to improve patient care.1 The majority of nail unit melanomas are diagnosed at late stages, which has been attributed to deficiencies in clinical knowledge and failure to perform or inadequate biopsy techniques.2 Notably, a survey of third-year dermatology residents (N=240) assessing experience in procedural dermatology showed that 58% performed 10 or fewer nail procedures and 30% did not feel competent in performing nail surgery.3 Furthermore, a survey examining the management of longitudinal melanonychia among attending and resident dermatologists (N=402) found that 62% of residents and 28% of total respondents were not confident in managing melanonychia.4
A limitation of this study was the lack of online data available for AAD annual meetings before 2013, so we were unable to characterize any long-term trends. Furthermore, we were unable to assess the educational reach of these sessions, as data on attendance are lacking.
This study demonstrates a paucity of nail-related content at the AAD annual meetings. The introduction of the “Hands-on: Nail Surgery” in 2015 is an important step forward to diminish the knowledge gap in the diagnosis of various nail diseases and malignancies. We recommend increasing the number of hours and overall content of didactic nail sessions at the AAD annual meeting to further the knowledge and procedural skills of dermatologists in caring for patients with nail disorders.
To the Editor:
The diagnosis and treatment of nail conditions are necessary competencies for board-certified dermatologists, but appropriate education often is lacking.1 The American Academy of Dermatology (AAD) annual meeting is one of the largest and most highly attended dermatology educational conferences worldwide. We sought to determine the number of hours dedicated to nail-related topics at the AAD annual meetings from 2013 to 2019.
We accessed programs from the AAD annual meetings archive online (https://www.aad.org/meetings/previous-meetings-archive), and we used hair and psoriasis content for comparison. Event titles and descriptions were searched for nail-related content (using search terms nail, onychia, and onycho), hair-related content (hair, alopecia, trichosis, hirsutism), and psoriasis content (psoriasis). Data acquired for each event included the date, hours, title, and event type (eg, forum, course, focus session, symposium, discussion group, workshop, plenary session).
The number of hours dedicated to nail education consistently lagged behind those related to hair and psoriasis content during the study period (Figure 1). According to the AAD, the conference runs Friday to Tuesday with higher attendance Friday to Sunday (Tim Moses, personal communication, July 9, 2019). Lectures during the weekend are likely to have a broader reach than lectures on Monday and Tuesday. The proportion of nail content during weekend prime time slots was similar to that of hair and psoriasis (Figure 2). Plenary sessions often are presented by renowned experts on hot topics in dermatology. Notably, hair (2014-2015) and psoriasis (2015-2017) content were represented in the plenary sessions during the study period, while nail content was not featured.

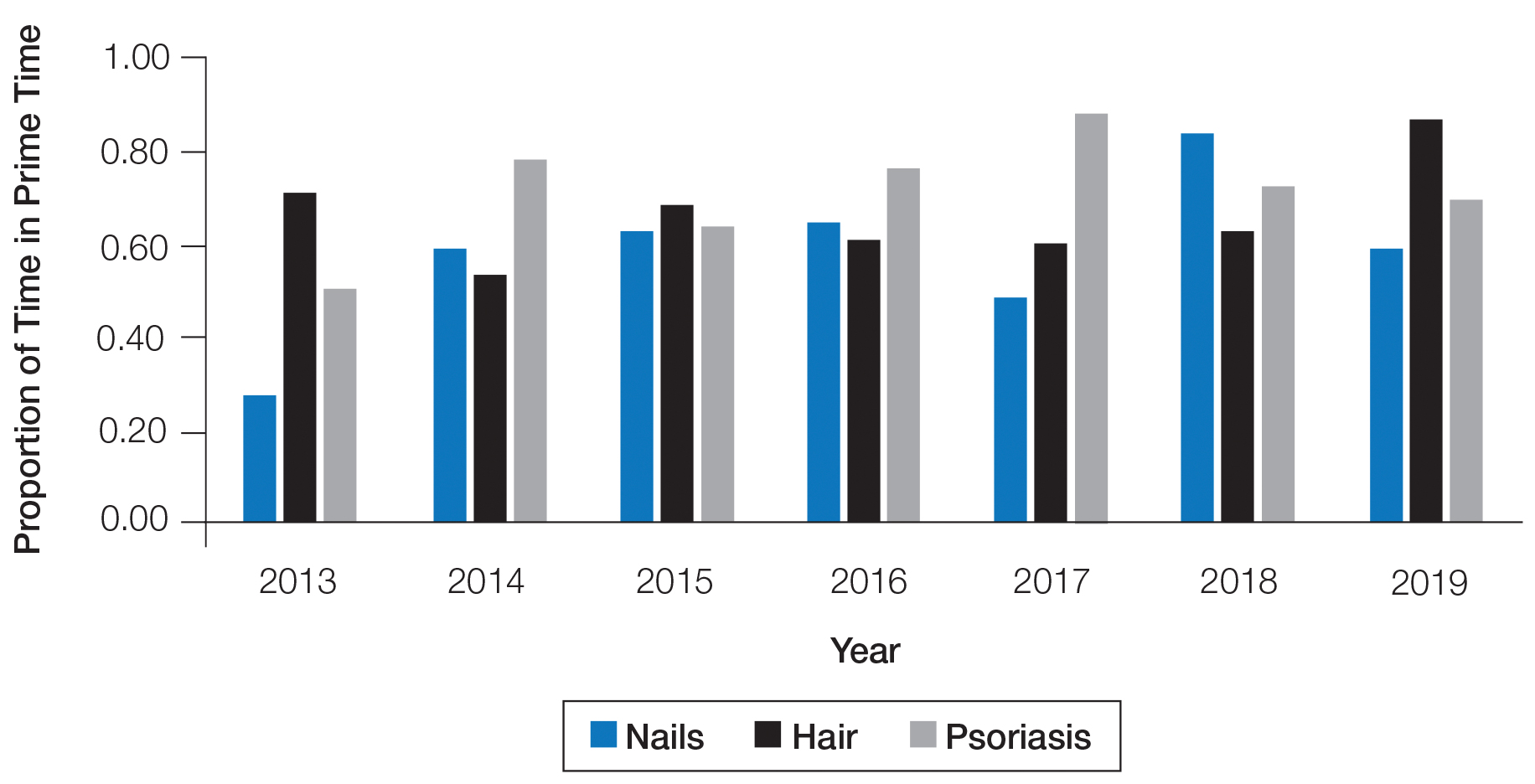
Our study shows that nail-related education was underrepresented at the AAD annual meetings from 2013 to 2019 compared to hair- and psoriasis-related content. Educational gaps in the diagnosis of fignail conditions previously have been delineated, and prioritization of instruction on nail disease pathology and diagnostic procedures has been recommended to improve patient care.1 The majority of nail unit melanomas are diagnosed at late stages, which has been attributed to deficiencies in clinical knowledge and failure to perform or inadequate biopsy techniques.2 Notably, a survey of third-year dermatology residents (N=240) assessing experience in procedural dermatology showed that 58% performed 10 or fewer nail procedures and 30% did not feel competent in performing nail surgery.3 Furthermore, a survey examining the management of longitudinal melanonychia among attending and resident dermatologists (N=402) found that 62% of residents and 28% of total respondents were not confident in managing melanonychia.4
A limitation of this study was the lack of online data available for AAD annual meetings before 2013, so we were unable to characterize any long-term trends. Furthermore, we were unable to assess the educational reach of these sessions, as data on attendance are lacking.
This study demonstrates a paucity of nail-related content at the AAD annual meetings. The introduction of the “Hands-on: Nail Surgery” in 2015 is an important step forward to diminish the knowledge gap in the diagnosis of various nail diseases and malignancies. We recommend increasing the number of hours and overall content of didactic nail sessions at the AAD annual meeting to further the knowledge and procedural skills of dermatologists in caring for patients with nail disorders.
- Hare AQ, R ich P. Clinical and educational gaps in diagnosis of nail disorders. Dermatol Clin. 2016;34:269-273.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol. 2007;31:1902-1912.
- Lee EH, Nehal KS, Dusza SW, et al. Procedural dermatology training during dermatology residency: a survey of third-year dermatology residents. J Am Acad Dermatol. 2011;64:475-483.
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996.
- Hare AQ, R ich P. Clinical and educational gaps in diagnosis of nail disorders. Dermatol Clin. 2016;34:269-273.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol. 2007;31:1902-1912.
- Lee EH, Nehal KS, Dusza SW, et al. Procedural dermatology training during dermatology residency: a survey of third-year dermatology residents. J Am Acad Dermatol. 2011;64:475-483.
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996.
Practice Points
- Diagnosis and treatment of nail conditions are necessary competencies for board-certified dermatologists, but appropriate education often is lacking.
- We recommend increasing the number of hours and overall content of didactic nail sessions at the American Academy of Dermatology annual meeting to further the knowledge and procedural skills of dermatologists caring for patients with nail disorders.
Facial Malignancies in Patients Referred for Mohs Micrographic Surgery: A Retrospective Review of the Impact of Hair Growth on Tumor and Defect Size
Male facial hair trends are continuously changing and are influenced by culture, geography, religion, and ethnicity.1 Although the natural pattern of these hairs is largely androgen dependent, the phenotypic presentation often is a result of contemporary grooming practices that reflect prevailing trends.2 Beards are common throughout adulthood, and thus, preserving this facial hair pattern is considered with reconstructive techniques.3,4 Male facial skin physiology and beard hair biology are a dynamic interplay between both internal (eg, hormonal) and external (eg, shaving) variables. The density of beard hair follicles varies within different subunits, ranging between 20 and 80 follicles/cm2. Macroscopically, hairs vary in length, diameter, color, and growth rate across individuals and ethnicities.1,5
There is a paucity of literature assessing if male facial hair offers a protective role for external insults. One study utilized dosimetry to examine the effectiveness of facial hair on mannequins with varying lengths of hair in protecting against erythemal UV radiation (UVR). The authors concluded that, although facial hair provides protection from UVR, it is not significant.6 In a study of 200 male patients with
We sought to determine if facial hair growth is implicated in the diagnosis and treatment of cutaneous malignancies. Specifically, we hypothesized that the presence of facial hair leads to a delay in diagnosis with increased subclinical growth given that tumors may be camouflaged and go undetected. Although there is a lack of literature, our anecdotal evidence suggests that male patients with facial hair have larger tumors compared to patients who do not regularly maintain any facial hair.
Methods
We performed a retrospective chart review following approval from the institutional review board at The University of North Carolina at Chapel Hill. We identified all male patients with a cutaneous malignancy located on the face who were treated from January 2015 to December 2018. Photographs were reviewed and patients with tumors located within the following facial hair-bearing anatomic subunits were included: lip, melolabial fold, chin, mandible, preauricular cheek, buccal cheek, and parotid-masseteric cheek. Tumors located within the medial cheek were excluded.
Facial hair growth was determined via image review. Because biopsy photographs were not uploaded into the health record for patients who were referred externally, we reviewed all historical photographs for patients who had undergone prior Mohs micrographic surgery at The University of North Carolina at Chapel Hill, preoperative photographs, and follow-up photographs as a proxy to determine facial hair status. Postoperative photographs taken within 2 weeks following surgery were not reviewed, as any facial hair growth was likely due to disinclination on behalf of the patient to shave near or over the incision. Age, number of days from biopsy to surgery, pathology, preoperative tumor size, number of Mohs layers, and defect size also were extrapolated from our chart review.
Statistical Analysis
Summary statistics were applied to describe demographic and clinical characteristics. An unpaired 2-tailed t test was utilized to test the null hypothesis that the mean difference was zero. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
Results
We reviewed medical records for 171 patients with facial hair and 336 patients without facial hair. The primary outcomes for this study assessed tumor and defect size in patients with facial hair compared to patients with no facial hair (Table 1). On average, patients who had facial hair were younger (67.5 years vs 74.0 years, P<.001). The median number of days from biopsy to surgery (43.0 vs 44.0 days) was comparable across both groups. The majority of patients (47%) exhibited a beard, while 30% had a mustache and 23% had a goatee. The most common tumor location was the preauricular cheek for both groups (29% and 28%, respectively). The mean preoperative tumor size in the facial hair cohort was 1.40 cm compared to 1.22 cm in the group with no facial hair (P=.03). The mean number of Mohs layers in the facial hair cohort was 1.53 compared to 1.33 in the group with no facial hair (P=.03). The facial hair cohort also had a larger mean postoperative defect size (2.18 cm) compared to the group with no facial hair (1.98 cm); however, this finding was not significant (P=.05).
We then stratified our data to analyze only lip tumors in patients with and without a mustache (Table 2). The mean preoperative tumor size in the mustache cohort was 1.10 cm compared to 0.82 cm in the group with no mustaches (P=.046). The mean number of Mohs layers in the mustache cohort was 1.57 compared to 1.42 in the group with no mustaches (P=.43). The mustache cohort also had a larger mean postoperative defect size (1.63 cm) compared to the group with no facial hair (1.33 cm), though this finding also did not reach significance (P=.13).
Comment
Our findings support anecdotal observations that tumors in men with facial hair are larger, require more Mohs layers, and result in larger defects compared with patients who are clean shaven. Similarly, in lip tumors, men with a mustache had a larger preoperative tumor size. Although these patients also required more Mohs layers to clear and a larger defect size, these parameters did not reach significance. These outcomes may, in part, be explained by a delay in diagnosis, as patients with facial hair may not notice any new suspicious lesions within the underlying skin as easily as patients with glabrous skin.
Although facial hair may shield skin from UVR, we agree with Parisi et al6 that this protection is marginal at best and that early persistent exposure to UVR plays a much more notable role in cutaneous carcinogenesis. As more men continue to grow facial hairstyles that emulate historical or contemporary trends, dermatologists should emphasize the risk for cutaneous malignancies within these sun-exposed areas of the face. Although some facial hair practices may reflect cultural or ethnic settings, the majority reflect a desired appearance that is achieved with grooming or otherwise.
Skin cancer screening in men with facial hair, particularly those with a strong history of UVR exposure and/or family history, should be discussed and encouraged to diagnose cutaneous tumors earlier. We encourage men with facial hair to be cognizant that cutaneous malignancies can arise within hair-bearing skin and to incorporate self–skin checks into grooming routines, which is particularly important in men with dense facial hair who forego regular self-care grooming or trim intermittently. Furthermore, we urge dermatologists to continue to thoroughly examine the underlying skin, especially in patients with full beards, during skin examinations. Diagnosing and treating cutaneous malignancies early is imperative to maximize ideal functional and cosmetic outcomes, particularly within perioral and lip subunits, where marginal millimeters can impact reconstructive complexity.
Conclusion
Men with facial hair who had cutaneous tumors in our study exhibited larger tumors, required more Mohs layers, and had a larger defect size compared to men without any facial hair growth. Similar findings also were noted when we stratified and compared lip tumors in patients with and without mustaches. Given these observations, patients and dermatologists should continue to have a high index of suspicion for any concerning lesion located within skin underlying facial hair. Regular screening in men with facial hair should be discussed and encouraged to diagnose and treat potential cutaneous tumors earlier.
- Wu Y, Konduru R, Deng D. Skin characteristics of Chinese men and their beard removal habits. Br J Dermatol. 2012;166:17-21.
- Janif ZJ, Brooks RC, Dixson BJ. Negative frequency-dependent preferences and variation in male facial hair. Biol Lett. 2014;10:20130958.
- Benjegerdes KE, Jamerson J, Housewright CD. Repair of a large submental defect. Dermatol Surg. 2019;45:141-143.
- Ninkovic M, Heidekruegger PI, Ehri D, et al. Beard reconstruction: a surgical algorithm. J Plast Reconstr Aesthet Surg. 2016;69:E111-E118.
- Maurer M, Rietzler M, Burghardt R, et al. The male beard hair and facial skin–challenges for shaving. Int J Cosmet Sci. 2016;38(suppl 1):3-9.
- Parisi AV, Turnbull DJ, Downs N, et al. Dosimetric investigation of the solar erythemal UV radiation protection provided by beards and moustaches. Radiat Prot Dosimetry. 2012;150:278-282.
- Liu DY, Gul MI, Wick J, et al. Long-term sheltering mustaches reduce incidence of lower lip actinic keratosis. J Am Acad Dermatol. 2019;80:1757-1758.e1.
Male facial hair trends are continuously changing and are influenced by culture, geography, religion, and ethnicity.1 Although the natural pattern of these hairs is largely androgen dependent, the phenotypic presentation often is a result of contemporary grooming practices that reflect prevailing trends.2 Beards are common throughout adulthood, and thus, preserving this facial hair pattern is considered with reconstructive techniques.3,4 Male facial skin physiology and beard hair biology are a dynamic interplay between both internal (eg, hormonal) and external (eg, shaving) variables. The density of beard hair follicles varies within different subunits, ranging between 20 and 80 follicles/cm2. Macroscopically, hairs vary in length, diameter, color, and growth rate across individuals and ethnicities.1,5
There is a paucity of literature assessing if male facial hair offers a protective role for external insults. One study utilized dosimetry to examine the effectiveness of facial hair on mannequins with varying lengths of hair in protecting against erythemal UV radiation (UVR). The authors concluded that, although facial hair provides protection from UVR, it is not significant.6 In a study of 200 male patients with
We sought to determine if facial hair growth is implicated in the diagnosis and treatment of cutaneous malignancies. Specifically, we hypothesized that the presence of facial hair leads to a delay in diagnosis with increased subclinical growth given that tumors may be camouflaged and go undetected. Although there is a lack of literature, our anecdotal evidence suggests that male patients with facial hair have larger tumors compared to patients who do not regularly maintain any facial hair.
Methods
We performed a retrospective chart review following approval from the institutional review board at The University of North Carolina at Chapel Hill. We identified all male patients with a cutaneous malignancy located on the face who were treated from January 2015 to December 2018. Photographs were reviewed and patients with tumors located within the following facial hair-bearing anatomic subunits were included: lip, melolabial fold, chin, mandible, preauricular cheek, buccal cheek, and parotid-masseteric cheek. Tumors located within the medial cheek were excluded.
Facial hair growth was determined via image review. Because biopsy photographs were not uploaded into the health record for patients who were referred externally, we reviewed all historical photographs for patients who had undergone prior Mohs micrographic surgery at The University of North Carolina at Chapel Hill, preoperative photographs, and follow-up photographs as a proxy to determine facial hair status. Postoperative photographs taken within 2 weeks following surgery were not reviewed, as any facial hair growth was likely due to disinclination on behalf of the patient to shave near or over the incision. Age, number of days from biopsy to surgery, pathology, preoperative tumor size, number of Mohs layers, and defect size also were extrapolated from our chart review.
Statistical Analysis
Summary statistics were applied to describe demographic and clinical characteristics. An unpaired 2-tailed t test was utilized to test the null hypothesis that the mean difference was zero. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
Results
We reviewed medical records for 171 patients with facial hair and 336 patients without facial hair. The primary outcomes for this study assessed tumor and defect size in patients with facial hair compared to patients with no facial hair (Table 1). On average, patients who had facial hair were younger (67.5 years vs 74.0 years, P<.001). The median number of days from biopsy to surgery (43.0 vs 44.0 days) was comparable across both groups. The majority of patients (47%) exhibited a beard, while 30% had a mustache and 23% had a goatee. The most common tumor location was the preauricular cheek for both groups (29% and 28%, respectively). The mean preoperative tumor size in the facial hair cohort was 1.40 cm compared to 1.22 cm in the group with no facial hair (P=.03). The mean number of Mohs layers in the facial hair cohort was 1.53 compared to 1.33 in the group with no facial hair (P=.03). The facial hair cohort also had a larger mean postoperative defect size (2.18 cm) compared to the group with no facial hair (1.98 cm); however, this finding was not significant (P=.05).
We then stratified our data to analyze only lip tumors in patients with and without a mustache (Table 2). The mean preoperative tumor size in the mustache cohort was 1.10 cm compared to 0.82 cm in the group with no mustaches (P=.046). The mean number of Mohs layers in the mustache cohort was 1.57 compared to 1.42 in the group with no mustaches (P=.43). The mustache cohort also had a larger mean postoperative defect size (1.63 cm) compared to the group with no facial hair (1.33 cm), though this finding also did not reach significance (P=.13).
Comment
Our findings support anecdotal observations that tumors in men with facial hair are larger, require more Mohs layers, and result in larger defects compared with patients who are clean shaven. Similarly, in lip tumors, men with a mustache had a larger preoperative tumor size. Although these patients also required more Mohs layers to clear and a larger defect size, these parameters did not reach significance. These outcomes may, in part, be explained by a delay in diagnosis, as patients with facial hair may not notice any new suspicious lesions within the underlying skin as easily as patients with glabrous skin.
Although facial hair may shield skin from UVR, we agree with Parisi et al6 that this protection is marginal at best and that early persistent exposure to UVR plays a much more notable role in cutaneous carcinogenesis. As more men continue to grow facial hairstyles that emulate historical or contemporary trends, dermatologists should emphasize the risk for cutaneous malignancies within these sun-exposed areas of the face. Although some facial hair practices may reflect cultural or ethnic settings, the majority reflect a desired appearance that is achieved with grooming or otherwise.
Skin cancer screening in men with facial hair, particularly those with a strong history of UVR exposure and/or family history, should be discussed and encouraged to diagnose cutaneous tumors earlier. We encourage men with facial hair to be cognizant that cutaneous malignancies can arise within hair-bearing skin and to incorporate self–skin checks into grooming routines, which is particularly important in men with dense facial hair who forego regular self-care grooming or trim intermittently. Furthermore, we urge dermatologists to continue to thoroughly examine the underlying skin, especially in patients with full beards, during skin examinations. Diagnosing and treating cutaneous malignancies early is imperative to maximize ideal functional and cosmetic outcomes, particularly within perioral and lip subunits, where marginal millimeters can impact reconstructive complexity.
Conclusion
Men with facial hair who had cutaneous tumors in our study exhibited larger tumors, required more Mohs layers, and had a larger defect size compared to men without any facial hair growth. Similar findings also were noted when we stratified and compared lip tumors in patients with and without mustaches. Given these observations, patients and dermatologists should continue to have a high index of suspicion for any concerning lesion located within skin underlying facial hair. Regular screening in men with facial hair should be discussed and encouraged to diagnose and treat potential cutaneous tumors earlier.
Male facial hair trends are continuously changing and are influenced by culture, geography, religion, and ethnicity.1 Although the natural pattern of these hairs is largely androgen dependent, the phenotypic presentation often is a result of contemporary grooming practices that reflect prevailing trends.2 Beards are common throughout adulthood, and thus, preserving this facial hair pattern is considered with reconstructive techniques.3,4 Male facial skin physiology and beard hair biology are a dynamic interplay between both internal (eg, hormonal) and external (eg, shaving) variables. The density of beard hair follicles varies within different subunits, ranging between 20 and 80 follicles/cm2. Macroscopically, hairs vary in length, diameter, color, and growth rate across individuals and ethnicities.1,5
There is a paucity of literature assessing if male facial hair offers a protective role for external insults. One study utilized dosimetry to examine the effectiveness of facial hair on mannequins with varying lengths of hair in protecting against erythemal UV radiation (UVR). The authors concluded that, although facial hair provides protection from UVR, it is not significant.6 In a study of 200 male patients with
We sought to determine if facial hair growth is implicated in the diagnosis and treatment of cutaneous malignancies. Specifically, we hypothesized that the presence of facial hair leads to a delay in diagnosis with increased subclinical growth given that tumors may be camouflaged and go undetected. Although there is a lack of literature, our anecdotal evidence suggests that male patients with facial hair have larger tumors compared to patients who do not regularly maintain any facial hair.
Methods
We performed a retrospective chart review following approval from the institutional review board at The University of North Carolina at Chapel Hill. We identified all male patients with a cutaneous malignancy located on the face who were treated from January 2015 to December 2018. Photographs were reviewed and patients with tumors located within the following facial hair-bearing anatomic subunits were included: lip, melolabial fold, chin, mandible, preauricular cheek, buccal cheek, and parotid-masseteric cheek. Tumors located within the medial cheek were excluded.
Facial hair growth was determined via image review. Because biopsy photographs were not uploaded into the health record for patients who were referred externally, we reviewed all historical photographs for patients who had undergone prior Mohs micrographic surgery at The University of North Carolina at Chapel Hill, preoperative photographs, and follow-up photographs as a proxy to determine facial hair status. Postoperative photographs taken within 2 weeks following surgery were not reviewed, as any facial hair growth was likely due to disinclination on behalf of the patient to shave near or over the incision. Age, number of days from biopsy to surgery, pathology, preoperative tumor size, number of Mohs layers, and defect size also were extrapolated from our chart review.
Statistical Analysis
Summary statistics were applied to describe demographic and clinical characteristics. An unpaired 2-tailed t test was utilized to test the null hypothesis that the mean difference was zero. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
Results
We reviewed medical records for 171 patients with facial hair and 336 patients without facial hair. The primary outcomes for this study assessed tumor and defect size in patients with facial hair compared to patients with no facial hair (Table 1). On average, patients who had facial hair were younger (67.5 years vs 74.0 years, P<.001). The median number of days from biopsy to surgery (43.0 vs 44.0 days) was comparable across both groups. The majority of patients (47%) exhibited a beard, while 30% had a mustache and 23% had a goatee. The most common tumor location was the preauricular cheek for both groups (29% and 28%, respectively). The mean preoperative tumor size in the facial hair cohort was 1.40 cm compared to 1.22 cm in the group with no facial hair (P=.03). The mean number of Mohs layers in the facial hair cohort was 1.53 compared to 1.33 in the group with no facial hair (P=.03). The facial hair cohort also had a larger mean postoperative defect size (2.18 cm) compared to the group with no facial hair (1.98 cm); however, this finding was not significant (P=.05).
We then stratified our data to analyze only lip tumors in patients with and without a mustache (Table 2). The mean preoperative tumor size in the mustache cohort was 1.10 cm compared to 0.82 cm in the group with no mustaches (P=.046). The mean number of Mohs layers in the mustache cohort was 1.57 compared to 1.42 in the group with no mustaches (P=.43). The mustache cohort also had a larger mean postoperative defect size (1.63 cm) compared to the group with no facial hair (1.33 cm), though this finding also did not reach significance (P=.13).
Comment
Our findings support anecdotal observations that tumors in men with facial hair are larger, require more Mohs layers, and result in larger defects compared with patients who are clean shaven. Similarly, in lip tumors, men with a mustache had a larger preoperative tumor size. Although these patients also required more Mohs layers to clear and a larger defect size, these parameters did not reach significance. These outcomes may, in part, be explained by a delay in diagnosis, as patients with facial hair may not notice any new suspicious lesions within the underlying skin as easily as patients with glabrous skin.
Although facial hair may shield skin from UVR, we agree with Parisi et al6 that this protection is marginal at best and that early persistent exposure to UVR plays a much more notable role in cutaneous carcinogenesis. As more men continue to grow facial hairstyles that emulate historical or contemporary trends, dermatologists should emphasize the risk for cutaneous malignancies within these sun-exposed areas of the face. Although some facial hair practices may reflect cultural or ethnic settings, the majority reflect a desired appearance that is achieved with grooming or otherwise.
Skin cancer screening in men with facial hair, particularly those with a strong history of UVR exposure and/or family history, should be discussed and encouraged to diagnose cutaneous tumors earlier. We encourage men with facial hair to be cognizant that cutaneous malignancies can arise within hair-bearing skin and to incorporate self–skin checks into grooming routines, which is particularly important in men with dense facial hair who forego regular self-care grooming or trim intermittently. Furthermore, we urge dermatologists to continue to thoroughly examine the underlying skin, especially in patients with full beards, during skin examinations. Diagnosing and treating cutaneous malignancies early is imperative to maximize ideal functional and cosmetic outcomes, particularly within perioral and lip subunits, where marginal millimeters can impact reconstructive complexity.
Conclusion
Men with facial hair who had cutaneous tumors in our study exhibited larger tumors, required more Mohs layers, and had a larger defect size compared to men without any facial hair growth. Similar findings also were noted when we stratified and compared lip tumors in patients with and without mustaches. Given these observations, patients and dermatologists should continue to have a high index of suspicion for any concerning lesion located within skin underlying facial hair. Regular screening in men with facial hair should be discussed and encouraged to diagnose and treat potential cutaneous tumors earlier.
- Wu Y, Konduru R, Deng D. Skin characteristics of Chinese men and their beard removal habits. Br J Dermatol. 2012;166:17-21.
- Janif ZJ, Brooks RC, Dixson BJ. Negative frequency-dependent preferences and variation in male facial hair. Biol Lett. 2014;10:20130958.
- Benjegerdes KE, Jamerson J, Housewright CD. Repair of a large submental defect. Dermatol Surg. 2019;45:141-143.
- Ninkovic M, Heidekruegger PI, Ehri D, et al. Beard reconstruction: a surgical algorithm. J Plast Reconstr Aesthet Surg. 2016;69:E111-E118.
- Maurer M, Rietzler M, Burghardt R, et al. The male beard hair and facial skin–challenges for shaving. Int J Cosmet Sci. 2016;38(suppl 1):3-9.
- Parisi AV, Turnbull DJ, Downs N, et al. Dosimetric investigation of the solar erythemal UV radiation protection provided by beards and moustaches. Radiat Prot Dosimetry. 2012;150:278-282.
- Liu DY, Gul MI, Wick J, et al. Long-term sheltering mustaches reduce incidence of lower lip actinic keratosis. J Am Acad Dermatol. 2019;80:1757-1758.e1.
- Wu Y, Konduru R, Deng D. Skin characteristics of Chinese men and their beard removal habits. Br J Dermatol. 2012;166:17-21.
- Janif ZJ, Brooks RC, Dixson BJ. Negative frequency-dependent preferences and variation in male facial hair. Biol Lett. 2014;10:20130958.
- Benjegerdes KE, Jamerson J, Housewright CD. Repair of a large submental defect. Dermatol Surg. 2019;45:141-143.
- Ninkovic M, Heidekruegger PI, Ehri D, et al. Beard reconstruction: a surgical algorithm. J Plast Reconstr Aesthet Surg. 2016;69:E111-E118.
- Maurer M, Rietzler M, Burghardt R, et al. The male beard hair and facial skin–challenges for shaving. Int J Cosmet Sci. 2016;38(suppl 1):3-9.
- Parisi AV, Turnbull DJ, Downs N, et al. Dosimetric investigation of the solar erythemal UV radiation protection provided by beards and moustaches. Radiat Prot Dosimetry. 2012;150:278-282.
- Liu DY, Gul MI, Wick J, et al. Long-term sheltering mustaches reduce incidence of lower lip actinic keratosis. J Am Acad Dermatol. 2019;80:1757-1758.e1.
Practice Points
- In our study, men with cutaneous tumors who had facial hair exhibited larger tumors, required more Mohs layers, and had a larger defect size compared to men who do not have any facial hair growth.
- Both patients and dermatologists should have a high index of suspicion for any concerning lesion contained within skin underlying facial hair to ensure prompt diagnosis and treatment of cutaneous tumors.
More on How to Decrease Dermatology Interview Costs
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP (aamir.nav.hussain@gmail.com).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP (aamir.nav.hussain@gmail.com).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP (aamir.nav.hussain@gmail.com).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
Interleukin-27 increased cytotoxic effects of bone marrow NK cells in CLL
Chronic lymphocytic leukemia is characterized by significant immune perturbation, including significant impairment of natural killer (NK) cells, which leads to disease complications and reduced effectiveness of treatment.
However, the use of , according to an in vitro study conducted by Maral Hemati, a student researcher at the Semnan (Iran) University of Medical Sciences, and colleagues.
Ms. Hemati and her colleagues obtained bone marrow aspirates (BM) and peripheral blood samples (PB) were from 12 untreated CLL patients (9 men and 3 women) with a median age of 61 years. The cells were cultured in vitro, according to their report in International Immunopharmacology.
The researchers found that the use of recombinant human interleukin-27 (IL-27) stimulated NK cells in the cultured BM and PB cells of CLL patients, based upon assessment using cell surface flow cytometry and a cytotoxicity assay.
Treatment with IL-27 also increased CD69 (a marker for NK cell activity) on NK cells both in BM and PB. In addition, , whereas it did not improve NK cell activity of PB, according to the researchers.
The research was supported by Semnan (Iran) University of Medical Sciences. The authors reported that they had no conflicts of interest.
SOURCE: Hemati M et al. Int Immunopharmacol. 2020;82:doi.org/10.1016/j.intimp.2020.106350.
Chronic lymphocytic leukemia is characterized by significant immune perturbation, including significant impairment of natural killer (NK) cells, which leads to disease complications and reduced effectiveness of treatment.
However, the use of , according to an in vitro study conducted by Maral Hemati, a student researcher at the Semnan (Iran) University of Medical Sciences, and colleagues.
Ms. Hemati and her colleagues obtained bone marrow aspirates (BM) and peripheral blood samples (PB) were from 12 untreated CLL patients (9 men and 3 women) with a median age of 61 years. The cells were cultured in vitro, according to their report in International Immunopharmacology.
The researchers found that the use of recombinant human interleukin-27 (IL-27) stimulated NK cells in the cultured BM and PB cells of CLL patients, based upon assessment using cell surface flow cytometry and a cytotoxicity assay.
Treatment with IL-27 also increased CD69 (a marker for NK cell activity) on NK cells both in BM and PB. In addition, , whereas it did not improve NK cell activity of PB, according to the researchers.
The research was supported by Semnan (Iran) University of Medical Sciences. The authors reported that they had no conflicts of interest.
SOURCE: Hemati M et al. Int Immunopharmacol. 2020;82:doi.org/10.1016/j.intimp.2020.106350.
Chronic lymphocytic leukemia is characterized by significant immune perturbation, including significant impairment of natural killer (NK) cells, which leads to disease complications and reduced effectiveness of treatment.
However, the use of , according to an in vitro study conducted by Maral Hemati, a student researcher at the Semnan (Iran) University of Medical Sciences, and colleagues.
Ms. Hemati and her colleagues obtained bone marrow aspirates (BM) and peripheral blood samples (PB) were from 12 untreated CLL patients (9 men and 3 women) with a median age of 61 years. The cells were cultured in vitro, according to their report in International Immunopharmacology.
The researchers found that the use of recombinant human interleukin-27 (IL-27) stimulated NK cells in the cultured BM and PB cells of CLL patients, based upon assessment using cell surface flow cytometry and a cytotoxicity assay.
Treatment with IL-27 also increased CD69 (a marker for NK cell activity) on NK cells both in BM and PB. In addition, , whereas it did not improve NK cell activity of PB, according to the researchers.
The research was supported by Semnan (Iran) University of Medical Sciences. The authors reported that they had no conflicts of interest.
SOURCE: Hemati M et al. Int Immunopharmacol. 2020;82:doi.org/10.1016/j.intimp.2020.106350.
FROM INTERNATIONAL IMMUNOPHARMACOLOGY
Patient Questionnaire to Reduce Anxiety Prior to Full-Body Skin Examination
To the Editor:
A thorough full-body skin examination (FBSE) is an integral component of a dermatologic encounter and helps identify potentially malignant and high-risk lesions, particularly in areas that are difficult for the patient to visualize.1 Despite these benefits, many patients experience discomfort and anxiety about this examination because it involves sensitive anatomical areas. The true psychological impact of an FBSE is not clearly understood; however, research into improving patient comfort in these circumstances can have a broad positive impact.2 The purpose of this pilot study was to establish patients’ willingness to complete a pre-encounter questionnaire that defines their FBSE preferences as well as to identify the anatomical areas that are of most concern.
This study was approved by the University of Kansas institutional review board as nonhuman subjects research. A pre-encounter questionnaire that included information about the benefits of FBSEs was administered to 34 patients, allowing them to identify anatomic locations that they wanted to exclude from the FBSE.
Following the patient visit (in which the identified anatomical locations were excluded), patients were given a brief exit survey that asked about (1) their preference for a pre-encounter FBSE questionnaire and (2) the impact of the questionnaire on their anxiety level throughout the encounter. Preference for asking was surveyed using a 10-point scale (10=strong preference for the pre-encounter survey; 1=strong preference against the pre-encounter survey). Change in anxiety was surveyed using a 10-point scale (10=strong reduction in anxiety after the pre-encounter survey; 1=strong increase in anxiety after the pre-encounter survey). Statistical analysis was performed using 2-tailed unpaired t tests, with P<.05 considered statistically significant.
Twenty female and 14 male patients were enrolled (mean age, 53 years)(Table). The most commonly excluded anatomical location on the pre-encounter survey was the genitals, followed by the buttocks, breasts/chest, legs, feet, and abdomen (Table); 10 (71%) male and 13 (65%) female respondents did not exclude any component of the FBSE.
After the provider visit, females had a higher preference for the pre-encounter survey (mean score, 9.0) compared to males (mean score, 7.2; P=.021). Similarly, females had reduced anxiety about the office visit after survey administration compared to males (mean score, 8.3 vs 6.0; P=.001)(Table).
The results of our pilot study showed that a brief pre-encounter questionnaire may reduce the distress associated with an FBSE. Our survey took less than 1 minute to complete and served as a useful guide to direct the provider during the FBSE. Moreover, recognizing that patients do not want certain anatomic locations examined can serve as an opportunity for the dermatologist to provide helpful home skin check instructions and recommendations.
The small sample size was a limitation of this study. Future studies can assess with greater precision the clear benefits of a pre-encounter survey as well as the benefits or drawbacks of a survey compared to other modalities that are aimed at reducing patient anxiety about the FBSE, such as having the physician directly ask the patient about areas to avoid during the examination.
A pre-encounter survey about the FBSE can serve as an efficient means of determining patient preference and reducing self-reported anxiety about the visit.
- Hoorens I, Vossaert K, Pil L, et al. Total-body examination vs lesion-directed skin cancer screening. JAMA Dermatol. 2016;152:27-34.
- Risica PM, Matthews NH, Dionne L, et al. Psychosocial consequences of skin cancer screening. Prev Med Rep. 2018;10:310-316.
To the Editor:
A thorough full-body skin examination (FBSE) is an integral component of a dermatologic encounter and helps identify potentially malignant and high-risk lesions, particularly in areas that are difficult for the patient to visualize.1 Despite these benefits, many patients experience discomfort and anxiety about this examination because it involves sensitive anatomical areas. The true psychological impact of an FBSE is not clearly understood; however, research into improving patient comfort in these circumstances can have a broad positive impact.2 The purpose of this pilot study was to establish patients’ willingness to complete a pre-encounter questionnaire that defines their FBSE preferences as well as to identify the anatomical areas that are of most concern.
This study was approved by the University of Kansas institutional review board as nonhuman subjects research. A pre-encounter questionnaire that included information about the benefits of FBSEs was administered to 34 patients, allowing them to identify anatomic locations that they wanted to exclude from the FBSE.
Following the patient visit (in which the identified anatomical locations were excluded), patients were given a brief exit survey that asked about (1) their preference for a pre-encounter FBSE questionnaire and (2) the impact of the questionnaire on their anxiety level throughout the encounter. Preference for asking was surveyed using a 10-point scale (10=strong preference for the pre-encounter survey; 1=strong preference against the pre-encounter survey). Change in anxiety was surveyed using a 10-point scale (10=strong reduction in anxiety after the pre-encounter survey; 1=strong increase in anxiety after the pre-encounter survey). Statistical analysis was performed using 2-tailed unpaired t tests, with P<.05 considered statistically significant.
Twenty female and 14 male patients were enrolled (mean age, 53 years)(Table). The most commonly excluded anatomical location on the pre-encounter survey was the genitals, followed by the buttocks, breasts/chest, legs, feet, and abdomen (Table); 10 (71%) male and 13 (65%) female respondents did not exclude any component of the FBSE.
After the provider visit, females had a higher preference for the pre-encounter survey (mean score, 9.0) compared to males (mean score, 7.2; P=.021). Similarly, females had reduced anxiety about the office visit after survey administration compared to males (mean score, 8.3 vs 6.0; P=.001)(Table).
The results of our pilot study showed that a brief pre-encounter questionnaire may reduce the distress associated with an FBSE. Our survey took less than 1 minute to complete and served as a useful guide to direct the provider during the FBSE. Moreover, recognizing that patients do not want certain anatomic locations examined can serve as an opportunity for the dermatologist to provide helpful home skin check instructions and recommendations.
The small sample size was a limitation of this study. Future studies can assess with greater precision the clear benefits of a pre-encounter survey as well as the benefits or drawbacks of a survey compared to other modalities that are aimed at reducing patient anxiety about the FBSE, such as having the physician directly ask the patient about areas to avoid during the examination.
A pre-encounter survey about the FBSE can serve as an efficient means of determining patient preference and reducing self-reported anxiety about the visit.
To the Editor:
A thorough full-body skin examination (FBSE) is an integral component of a dermatologic encounter and helps identify potentially malignant and high-risk lesions, particularly in areas that are difficult for the patient to visualize.1 Despite these benefits, many patients experience discomfort and anxiety about this examination because it involves sensitive anatomical areas. The true psychological impact of an FBSE is not clearly understood; however, research into improving patient comfort in these circumstances can have a broad positive impact.2 The purpose of this pilot study was to establish patients’ willingness to complete a pre-encounter questionnaire that defines their FBSE preferences as well as to identify the anatomical areas that are of most concern.
This study was approved by the University of Kansas institutional review board as nonhuman subjects research. A pre-encounter questionnaire that included information about the benefits of FBSEs was administered to 34 patients, allowing them to identify anatomic locations that they wanted to exclude from the FBSE.
Following the patient visit (in which the identified anatomical locations were excluded), patients were given a brief exit survey that asked about (1) their preference for a pre-encounter FBSE questionnaire and (2) the impact of the questionnaire on their anxiety level throughout the encounter. Preference for asking was surveyed using a 10-point scale (10=strong preference for the pre-encounter survey; 1=strong preference against the pre-encounter survey). Change in anxiety was surveyed using a 10-point scale (10=strong reduction in anxiety after the pre-encounter survey; 1=strong increase in anxiety after the pre-encounter survey). Statistical analysis was performed using 2-tailed unpaired t tests, with P<.05 considered statistically significant.
Twenty female and 14 male patients were enrolled (mean age, 53 years)(Table). The most commonly excluded anatomical location on the pre-encounter survey was the genitals, followed by the buttocks, breasts/chest, legs, feet, and abdomen (Table); 10 (71%) male and 13 (65%) female respondents did not exclude any component of the FBSE.
After the provider visit, females had a higher preference for the pre-encounter survey (mean score, 9.0) compared to males (mean score, 7.2; P=.021). Similarly, females had reduced anxiety about the office visit after survey administration compared to males (mean score, 8.3 vs 6.0; P=.001)(Table).
The results of our pilot study showed that a brief pre-encounter questionnaire may reduce the distress associated with an FBSE. Our survey took less than 1 minute to complete and served as a useful guide to direct the provider during the FBSE. Moreover, recognizing that patients do not want certain anatomic locations examined can serve as an opportunity for the dermatologist to provide helpful home skin check instructions and recommendations.
The small sample size was a limitation of this study. Future studies can assess with greater precision the clear benefits of a pre-encounter survey as well as the benefits or drawbacks of a survey compared to other modalities that are aimed at reducing patient anxiety about the FBSE, such as having the physician directly ask the patient about areas to avoid during the examination.
A pre-encounter survey about the FBSE can serve as an efficient means of determining patient preference and reducing self-reported anxiety about the visit.
- Hoorens I, Vossaert K, Pil L, et al. Total-body examination vs lesion-directed skin cancer screening. JAMA Dermatol. 2016;152:27-34.
- Risica PM, Matthews NH, Dionne L, et al. Psychosocial consequences of skin cancer screening. Prev Med Rep. 2018;10:310-316.
- Hoorens I, Vossaert K, Pil L, et al. Total-body examination vs lesion-directed skin cancer screening. JAMA Dermatol. 2016;152:27-34.
- Risica PM, Matthews NH, Dionne L, et al. Psychosocial consequences of skin cancer screening. Prev Med Rep. 2018;10:310-316.
Practice Points
- Full-body skin examination (FBSE) is an assessment that requires examination of sensitive body areas, any of which can be seen as intrusive by certain patients.
- A pre-encounter survey on the FBSE can offer an efficient means by which to determine patient preference and reduce visit-associated anxiety.