User login
Addressing CVD’s role in U.S. maternal mortality: Multispecialty collaboration is needed
Nearly 700 women died from pregnancy-related complications in the United States in 2018, and almost a third of those deaths were associated with cardiovascular disease, according to the latest data from the Centers for Disease Control and Prevention.
Strikingly, studies suggest that up to half of cardiovascular disease–related maternal deaths are preventable, yet CVD remains the leading cause of maternal morbidity and mortality – and the incidence has been rising steadily for 2 decades.
The American College of Obstetricians and Gynecologists says that acquired heart disease is the likely culprit in the rise in incidence of maternal mortality as women enter pregnancy with an increasingly heavy burden of CVD risk factors, including older age, obesity, diabetes, and hypertension.
“They are entering pregnancy while already at risk, and that has led to an increase in morbidity and mortality during pregnancy,” Renee Patrice Bullock-Palmer, MD, a cardiologist and director of the Women’s Heart Center at Deborah Heart and Lung Center in Browns Mills, N.J., explained in an interview. “Unfortunately, among developed countries, the U.S. has the highest rates of maternal morbidity and mortality, and that’s shocking.”
It’s a problem that requires collaboration between obstetricians, cardiologists, and others involved in the care of pregnant women, she said.
The data and the depth of the crisis
The maternal mortality rate in 1987 – the year the CDC’s Pregnancy Mortality Surveillance System was implemented – was 7.2 per 100,000 live births. The rate in 2016 was more than double that at 16.9, and the rate in 2018, the most recent year for which data are available, was 17.4 – and significant racial and ethnic disparities in those rates have persisted over time.
In an August 2019 article published on the American Heart Association website, Dr. Bullock-Palmer addressed the cardiovascular state of health for pregnant women and the role of the cardiologists in their care, noting that there is a “role for increased collaboration between the cardiologist and the obstetrician with regards to a pregnancy heart team.”
“It is vital that mothers who are at increased risk for CVD or have established CVD be referred to a cardiologist for cardiovascular assessment and management,” she wrote, adding it is important to raise awareness among ob.gyns. and to improve cardiologists’ recognition of women at risk when they present for care for the first time.
These referrals should be made in the antepartum and early postpartum period, she said in an interview. More attention also must be paid to racial and ethnic disparities, and the role of cardiologists in addressing these disparities.
The CDC has emphasized racial and ethnic disparities in maternal mortality, noting in a 2019 Morbidity and Mortality Weekly report that, compared with white women, black and American Indian/Alaskan Native women aged over 30 years have a 300%-400% higher rate of pregnancy-related deaths (Morb Mortal Wkly Rep. 2019 Sep 6;68[35]:762-5).
With regard to disparities, Dr. Bullock-Palmer said the causes are multifold and may be related to a higher prevalence of CVD risk factors like obesity and hypertension in non-Hispanic black women.
“There may also be limited access to adequate postpartum care in this patient population,” she wrote, adding that some attention has been paid to addressing disparities, but that “there is a lot of work left to be done in resolving these inequities in maternal health care.”
Partnerships across specialties will help in addressing most of the factors associated with CVD and maternal death, she said.
The urgent need for these partnerships is underscored by the latest findings on CVD-related complications in pregnancy. A study published in March 2020 in the Journal of the American College of Cardiology, for example, looked specifically at the incidence of serious cardiac events (SCEs) in pregnant women with heart disease, and whether the events were preventable.
In a prospective cohort of 1,315 pregnancies among women with heart disease, Birgit Pfaller, MD, of the University of Toronto Pregnancy and Heart Disease Research Program, and colleagues found that SCEs occurred in 3.6% of cases (47 women) – most often during the antepartum period – that 49% were preventable, and that 74% were related to provider management factors.
The most common SCEs were cardiac death or arrest, heart failure, arrhythmias, and urgent intervention, and they were more likely to occur in women with acquired heart disease, severe aortic or mitral stenosis, mechanical valves, and systemic ventricular dysfunction. Adverse fetal and neonatal outcomes more than doubled in cases involving SCEs, compared with those without (62% vs. 29%), and adverse obstetric events occurred most often in women with severe preeclampsia.
“The majority of the preventable events occurred due to provider management factors, including: failure to identify the patient condition prior to pregnancy, failure to identify the patient as high risk, late recognition in cardiac deterioration, delay in treatment/intervention, inappropriate treatment, and lack of preconception counseling,” Melinda Davis, MD, of the University of Michigan, Ann Arbor, wrote in a summary and editorial published in the Journal of the American College of Cardiology.
Some preventable events were attributable to patient failure to seek care, noncompliance with care recommendations, and lack of access to care, Dr. Davis noted.
“These findings suggest that provider training, patient education, and health care advocacy are all important interventions to improve outcomes among pregnant women,” she wrote, adding that “the development of multidisciplinary cardio-obstetric clinics at tertiary care centers may also be helpful.”
Dr. Bullock-Palmer added the need for greater risk-prediction tools to the list, explaining that these are needed to assess CVD risk in the prenatal, antenatal, and postnatal period.
“The recently concluded Cardiac Disease in Pregnancy [CARPREG II] study indicated that there were 10 predictors that could be utilized to asses maternal CVD risk,” she noted.
The CARPREG II authors identified five general predictors (prior cardiac events or arrhythmias, poor functional class or cyanosis, high-risk valve disease/left ventricular outflow tract obstruction, systemic ventricular dysfunction, no prior cardiac interventions), four lesion-specific predictors (mechanical valves, high-risk aortopathies, pulmonary hypertension, coronary artery disease), and one delivery-of-care predictor (late pregnancy assessment), and incorporated them into a risk index.
“It is hopeful that these new initiatives will assist providers in improving their ability to appropriately risk stratify women,” Dr. Bullock-Palmer said.
Ongoing efforts
Efforts also are ongoing to develop the types of cardio-obstetric clinics mentioned by Dr. Davis and to establish collaborations and “pregnancy heart teams” as attention is increasingly focused on the U.S. maternal mortality crisis.
In fact, such teams are a cornerstone of ACOG’s guidance on pregnancy and heart disease. In May 2019 the college released a Practice Bulletin with 27 specific recommendations and conclusions relating to screening, diagnosis, and management of CVD for women during the prepregnancy period through the postpartum period.
Pregnant women and postpartum women with known or suspected CVD should undergo evaluation by a “pregnancy heart team that includes a cardiologist and maternal-fetal medicine subspecialist, or both, and other subspecialists as necessary,” according to the bulletin.
In a recent interview, Lisa Hollier, MD, immediate past president of ACOG and an instrumental figure in the push to better address maternal mortality – and in particular the cardiovascular contributors to the crisis – said she is “seeing a strengthening of that” with numerous organizations establishing pregnancy health teams.
Dr. Bullock-Palmer said she also is seeing progress, and added that collaboration should be prioritized even in the absence of dedicated pregnancy heart teams and clinics.
“Heart disease in pregnancy requires a multidisciplinary approach. You can’t just see the patient from the cardiac perspective – you also have to interact and team up with the obstetrician who is handling the pregnancy,” she said, adding that, without a dedicated team, coordination takes more effort, but is imperative for improving outcomes. “You have to collaborate at times when it is beyond the expertise of the institution or the physician; you have to know when to refer these higher-risk patients, particularly women with adult congenital heart disease.”
This referral should occur early – preferably in the antenatal period, she added.
The most important thing, however, is “recognizing these women ... even before the pregnancy,” Dr. Bullock-Palmer said, explaining that this can facilitate the necessary management – and in some cases, postponement – of pregnancy for women whose cardiac issues need to be addressed first.
Among other efforts to address maternal mortality are several programs developed by ACOG, and the Heart Outcomes in Pregnancy: Expectations for Mom and Baby Registry (HOPE) project of the Saint Luke’s Health System in Kansas.
“Hopefully the [HOPE] research collaborative ... which aims to address key clinical questions surrounding the preconception period, antenatal care, delivery planning and outcomes, and long-term postpartum care and outcomes of women will help to address the knowledge gaps and disparities in the care of women with heart disease in pregnancy,” Dr. Bullock-Palmer wrote in her article.
CVD-related risks in the post partum
Dr. Bullock-Palmer has particular concern for postpartum follow-up, given the increased risk for future heart disease among women with CVD-related pregnancy complications and the heightened risk of certain CVD-related events in the postpartum period.
That’s a component of the crisis that also was addressed during a press briefing at the 2019 ACOG annual meeting when the Pregnancy and Heart Disease Practice Bulletin was released.
James Martin, MD, chair of ACOG’s Pregnancy and Heart Disease Task Force and a past ACOG president, explained during the briefing that CVD-related risks may accelerate and persist in the days and weeks after delivery, underscoring the need for follow-up and postpartum care.
Cardiomyopathy is a particular concern during this time – it’s the major cause of maternal mortality after 42 days, he noted. An emphasis on postpartum care also is especially important given that some data suggest up to 40% of women don’t return for that care.
“That is a very sad statistic and perhaps it reflects on our need to change payment models so that physicians and patients realize the importance of coming back for continuing care, because this really may be the end of pregnancy, but it is the beginning of the rest of their life,” he said. “And if they have cardiovascular disease or the risk factors ... they are going to possibly become worse over the course of their lifetime.”
Nearly 700 women died from pregnancy-related complications in the United States in 2018, and almost a third of those deaths were associated with cardiovascular disease, according to the latest data from the Centers for Disease Control and Prevention.
Strikingly, studies suggest that up to half of cardiovascular disease–related maternal deaths are preventable, yet CVD remains the leading cause of maternal morbidity and mortality – and the incidence has been rising steadily for 2 decades.
The American College of Obstetricians and Gynecologists says that acquired heart disease is the likely culprit in the rise in incidence of maternal mortality as women enter pregnancy with an increasingly heavy burden of CVD risk factors, including older age, obesity, diabetes, and hypertension.
“They are entering pregnancy while already at risk, and that has led to an increase in morbidity and mortality during pregnancy,” Renee Patrice Bullock-Palmer, MD, a cardiologist and director of the Women’s Heart Center at Deborah Heart and Lung Center in Browns Mills, N.J., explained in an interview. “Unfortunately, among developed countries, the U.S. has the highest rates of maternal morbidity and mortality, and that’s shocking.”
It’s a problem that requires collaboration between obstetricians, cardiologists, and others involved in the care of pregnant women, she said.
The data and the depth of the crisis
The maternal mortality rate in 1987 – the year the CDC’s Pregnancy Mortality Surveillance System was implemented – was 7.2 per 100,000 live births. The rate in 2016 was more than double that at 16.9, and the rate in 2018, the most recent year for which data are available, was 17.4 – and significant racial and ethnic disparities in those rates have persisted over time.
In an August 2019 article published on the American Heart Association website, Dr. Bullock-Palmer addressed the cardiovascular state of health for pregnant women and the role of the cardiologists in their care, noting that there is a “role for increased collaboration between the cardiologist and the obstetrician with regards to a pregnancy heart team.”
“It is vital that mothers who are at increased risk for CVD or have established CVD be referred to a cardiologist for cardiovascular assessment and management,” she wrote, adding it is important to raise awareness among ob.gyns. and to improve cardiologists’ recognition of women at risk when they present for care for the first time.
These referrals should be made in the antepartum and early postpartum period, she said in an interview. More attention also must be paid to racial and ethnic disparities, and the role of cardiologists in addressing these disparities.
The CDC has emphasized racial and ethnic disparities in maternal mortality, noting in a 2019 Morbidity and Mortality Weekly report that, compared with white women, black and American Indian/Alaskan Native women aged over 30 years have a 300%-400% higher rate of pregnancy-related deaths (Morb Mortal Wkly Rep. 2019 Sep 6;68[35]:762-5).
With regard to disparities, Dr. Bullock-Palmer said the causes are multifold and may be related to a higher prevalence of CVD risk factors like obesity and hypertension in non-Hispanic black women.
“There may also be limited access to adequate postpartum care in this patient population,” she wrote, adding that some attention has been paid to addressing disparities, but that “there is a lot of work left to be done in resolving these inequities in maternal health care.”
Partnerships across specialties will help in addressing most of the factors associated with CVD and maternal death, she said.
The urgent need for these partnerships is underscored by the latest findings on CVD-related complications in pregnancy. A study published in March 2020 in the Journal of the American College of Cardiology, for example, looked specifically at the incidence of serious cardiac events (SCEs) in pregnant women with heart disease, and whether the events were preventable.
In a prospective cohort of 1,315 pregnancies among women with heart disease, Birgit Pfaller, MD, of the University of Toronto Pregnancy and Heart Disease Research Program, and colleagues found that SCEs occurred in 3.6% of cases (47 women) – most often during the antepartum period – that 49% were preventable, and that 74% were related to provider management factors.
The most common SCEs were cardiac death or arrest, heart failure, arrhythmias, and urgent intervention, and they were more likely to occur in women with acquired heart disease, severe aortic or mitral stenosis, mechanical valves, and systemic ventricular dysfunction. Adverse fetal and neonatal outcomes more than doubled in cases involving SCEs, compared with those without (62% vs. 29%), and adverse obstetric events occurred most often in women with severe preeclampsia.
“The majority of the preventable events occurred due to provider management factors, including: failure to identify the patient condition prior to pregnancy, failure to identify the patient as high risk, late recognition in cardiac deterioration, delay in treatment/intervention, inappropriate treatment, and lack of preconception counseling,” Melinda Davis, MD, of the University of Michigan, Ann Arbor, wrote in a summary and editorial published in the Journal of the American College of Cardiology.
Some preventable events were attributable to patient failure to seek care, noncompliance with care recommendations, and lack of access to care, Dr. Davis noted.
“These findings suggest that provider training, patient education, and health care advocacy are all important interventions to improve outcomes among pregnant women,” she wrote, adding that “the development of multidisciplinary cardio-obstetric clinics at tertiary care centers may also be helpful.”
Dr. Bullock-Palmer added the need for greater risk-prediction tools to the list, explaining that these are needed to assess CVD risk in the prenatal, antenatal, and postnatal period.
“The recently concluded Cardiac Disease in Pregnancy [CARPREG II] study indicated that there were 10 predictors that could be utilized to asses maternal CVD risk,” she noted.
The CARPREG II authors identified five general predictors (prior cardiac events or arrhythmias, poor functional class or cyanosis, high-risk valve disease/left ventricular outflow tract obstruction, systemic ventricular dysfunction, no prior cardiac interventions), four lesion-specific predictors (mechanical valves, high-risk aortopathies, pulmonary hypertension, coronary artery disease), and one delivery-of-care predictor (late pregnancy assessment), and incorporated them into a risk index.
“It is hopeful that these new initiatives will assist providers in improving their ability to appropriately risk stratify women,” Dr. Bullock-Palmer said.
Ongoing efforts
Efforts also are ongoing to develop the types of cardio-obstetric clinics mentioned by Dr. Davis and to establish collaborations and “pregnancy heart teams” as attention is increasingly focused on the U.S. maternal mortality crisis.
In fact, such teams are a cornerstone of ACOG’s guidance on pregnancy and heart disease. In May 2019 the college released a Practice Bulletin with 27 specific recommendations and conclusions relating to screening, diagnosis, and management of CVD for women during the prepregnancy period through the postpartum period.
Pregnant women and postpartum women with known or suspected CVD should undergo evaluation by a “pregnancy heart team that includes a cardiologist and maternal-fetal medicine subspecialist, or both, and other subspecialists as necessary,” according to the bulletin.
In a recent interview, Lisa Hollier, MD, immediate past president of ACOG and an instrumental figure in the push to better address maternal mortality – and in particular the cardiovascular contributors to the crisis – said she is “seeing a strengthening of that” with numerous organizations establishing pregnancy health teams.
Dr. Bullock-Palmer said she also is seeing progress, and added that collaboration should be prioritized even in the absence of dedicated pregnancy heart teams and clinics.
“Heart disease in pregnancy requires a multidisciplinary approach. You can’t just see the patient from the cardiac perspective – you also have to interact and team up with the obstetrician who is handling the pregnancy,” she said, adding that, without a dedicated team, coordination takes more effort, but is imperative for improving outcomes. “You have to collaborate at times when it is beyond the expertise of the institution or the physician; you have to know when to refer these higher-risk patients, particularly women with adult congenital heart disease.”
This referral should occur early – preferably in the antenatal period, she added.
The most important thing, however, is “recognizing these women ... even before the pregnancy,” Dr. Bullock-Palmer said, explaining that this can facilitate the necessary management – and in some cases, postponement – of pregnancy for women whose cardiac issues need to be addressed first.
Among other efforts to address maternal mortality are several programs developed by ACOG, and the Heart Outcomes in Pregnancy: Expectations for Mom and Baby Registry (HOPE) project of the Saint Luke’s Health System in Kansas.
“Hopefully the [HOPE] research collaborative ... which aims to address key clinical questions surrounding the preconception period, antenatal care, delivery planning and outcomes, and long-term postpartum care and outcomes of women will help to address the knowledge gaps and disparities in the care of women with heart disease in pregnancy,” Dr. Bullock-Palmer wrote in her article.
CVD-related risks in the post partum
Dr. Bullock-Palmer has particular concern for postpartum follow-up, given the increased risk for future heart disease among women with CVD-related pregnancy complications and the heightened risk of certain CVD-related events in the postpartum period.
That’s a component of the crisis that also was addressed during a press briefing at the 2019 ACOG annual meeting when the Pregnancy and Heart Disease Practice Bulletin was released.
James Martin, MD, chair of ACOG’s Pregnancy and Heart Disease Task Force and a past ACOG president, explained during the briefing that CVD-related risks may accelerate and persist in the days and weeks after delivery, underscoring the need for follow-up and postpartum care.
Cardiomyopathy is a particular concern during this time – it’s the major cause of maternal mortality after 42 days, he noted. An emphasis on postpartum care also is especially important given that some data suggest up to 40% of women don’t return for that care.
“That is a very sad statistic and perhaps it reflects on our need to change payment models so that physicians and patients realize the importance of coming back for continuing care, because this really may be the end of pregnancy, but it is the beginning of the rest of their life,” he said. “And if they have cardiovascular disease or the risk factors ... they are going to possibly become worse over the course of their lifetime.”
Nearly 700 women died from pregnancy-related complications in the United States in 2018, and almost a third of those deaths were associated with cardiovascular disease, according to the latest data from the Centers for Disease Control and Prevention.
Strikingly, studies suggest that up to half of cardiovascular disease–related maternal deaths are preventable, yet CVD remains the leading cause of maternal morbidity and mortality – and the incidence has been rising steadily for 2 decades.
The American College of Obstetricians and Gynecologists says that acquired heart disease is the likely culprit in the rise in incidence of maternal mortality as women enter pregnancy with an increasingly heavy burden of CVD risk factors, including older age, obesity, diabetes, and hypertension.
“They are entering pregnancy while already at risk, and that has led to an increase in morbidity and mortality during pregnancy,” Renee Patrice Bullock-Palmer, MD, a cardiologist and director of the Women’s Heart Center at Deborah Heart and Lung Center in Browns Mills, N.J., explained in an interview. “Unfortunately, among developed countries, the U.S. has the highest rates of maternal morbidity and mortality, and that’s shocking.”
It’s a problem that requires collaboration between obstetricians, cardiologists, and others involved in the care of pregnant women, she said.
The data and the depth of the crisis
The maternal mortality rate in 1987 – the year the CDC’s Pregnancy Mortality Surveillance System was implemented – was 7.2 per 100,000 live births. The rate in 2016 was more than double that at 16.9, and the rate in 2018, the most recent year for which data are available, was 17.4 – and significant racial and ethnic disparities in those rates have persisted over time.
In an August 2019 article published on the American Heart Association website, Dr. Bullock-Palmer addressed the cardiovascular state of health for pregnant women and the role of the cardiologists in their care, noting that there is a “role for increased collaboration between the cardiologist and the obstetrician with regards to a pregnancy heart team.”
“It is vital that mothers who are at increased risk for CVD or have established CVD be referred to a cardiologist for cardiovascular assessment and management,” she wrote, adding it is important to raise awareness among ob.gyns. and to improve cardiologists’ recognition of women at risk when they present for care for the first time.
These referrals should be made in the antepartum and early postpartum period, she said in an interview. More attention also must be paid to racial and ethnic disparities, and the role of cardiologists in addressing these disparities.
The CDC has emphasized racial and ethnic disparities in maternal mortality, noting in a 2019 Morbidity and Mortality Weekly report that, compared with white women, black and American Indian/Alaskan Native women aged over 30 years have a 300%-400% higher rate of pregnancy-related deaths (Morb Mortal Wkly Rep. 2019 Sep 6;68[35]:762-5).
With regard to disparities, Dr. Bullock-Palmer said the causes are multifold and may be related to a higher prevalence of CVD risk factors like obesity and hypertension in non-Hispanic black women.
“There may also be limited access to adequate postpartum care in this patient population,” she wrote, adding that some attention has been paid to addressing disparities, but that “there is a lot of work left to be done in resolving these inequities in maternal health care.”
Partnerships across specialties will help in addressing most of the factors associated with CVD and maternal death, she said.
The urgent need for these partnerships is underscored by the latest findings on CVD-related complications in pregnancy. A study published in March 2020 in the Journal of the American College of Cardiology, for example, looked specifically at the incidence of serious cardiac events (SCEs) in pregnant women with heart disease, and whether the events were preventable.
In a prospective cohort of 1,315 pregnancies among women with heart disease, Birgit Pfaller, MD, of the University of Toronto Pregnancy and Heart Disease Research Program, and colleagues found that SCEs occurred in 3.6% of cases (47 women) – most often during the antepartum period – that 49% were preventable, and that 74% were related to provider management factors.
The most common SCEs were cardiac death or arrest, heart failure, arrhythmias, and urgent intervention, and they were more likely to occur in women with acquired heart disease, severe aortic or mitral stenosis, mechanical valves, and systemic ventricular dysfunction. Adverse fetal and neonatal outcomes more than doubled in cases involving SCEs, compared with those without (62% vs. 29%), and adverse obstetric events occurred most often in women with severe preeclampsia.
“The majority of the preventable events occurred due to provider management factors, including: failure to identify the patient condition prior to pregnancy, failure to identify the patient as high risk, late recognition in cardiac deterioration, delay in treatment/intervention, inappropriate treatment, and lack of preconception counseling,” Melinda Davis, MD, of the University of Michigan, Ann Arbor, wrote in a summary and editorial published in the Journal of the American College of Cardiology.
Some preventable events were attributable to patient failure to seek care, noncompliance with care recommendations, and lack of access to care, Dr. Davis noted.
“These findings suggest that provider training, patient education, and health care advocacy are all important interventions to improve outcomes among pregnant women,” she wrote, adding that “the development of multidisciplinary cardio-obstetric clinics at tertiary care centers may also be helpful.”
Dr. Bullock-Palmer added the need for greater risk-prediction tools to the list, explaining that these are needed to assess CVD risk in the prenatal, antenatal, and postnatal period.
“The recently concluded Cardiac Disease in Pregnancy [CARPREG II] study indicated that there were 10 predictors that could be utilized to asses maternal CVD risk,” she noted.
The CARPREG II authors identified five general predictors (prior cardiac events or arrhythmias, poor functional class or cyanosis, high-risk valve disease/left ventricular outflow tract obstruction, systemic ventricular dysfunction, no prior cardiac interventions), four lesion-specific predictors (mechanical valves, high-risk aortopathies, pulmonary hypertension, coronary artery disease), and one delivery-of-care predictor (late pregnancy assessment), and incorporated them into a risk index.
“It is hopeful that these new initiatives will assist providers in improving their ability to appropriately risk stratify women,” Dr. Bullock-Palmer said.
Ongoing efforts
Efforts also are ongoing to develop the types of cardio-obstetric clinics mentioned by Dr. Davis and to establish collaborations and “pregnancy heart teams” as attention is increasingly focused on the U.S. maternal mortality crisis.
In fact, such teams are a cornerstone of ACOG’s guidance on pregnancy and heart disease. In May 2019 the college released a Practice Bulletin with 27 specific recommendations and conclusions relating to screening, diagnosis, and management of CVD for women during the prepregnancy period through the postpartum period.
Pregnant women and postpartum women with known or suspected CVD should undergo evaluation by a “pregnancy heart team that includes a cardiologist and maternal-fetal medicine subspecialist, or both, and other subspecialists as necessary,” according to the bulletin.
In a recent interview, Lisa Hollier, MD, immediate past president of ACOG and an instrumental figure in the push to better address maternal mortality – and in particular the cardiovascular contributors to the crisis – said she is “seeing a strengthening of that” with numerous organizations establishing pregnancy health teams.
Dr. Bullock-Palmer said she also is seeing progress, and added that collaboration should be prioritized even in the absence of dedicated pregnancy heart teams and clinics.
“Heart disease in pregnancy requires a multidisciplinary approach. You can’t just see the patient from the cardiac perspective – you also have to interact and team up with the obstetrician who is handling the pregnancy,” she said, adding that, without a dedicated team, coordination takes more effort, but is imperative for improving outcomes. “You have to collaborate at times when it is beyond the expertise of the institution or the physician; you have to know when to refer these higher-risk patients, particularly women with adult congenital heart disease.”
This referral should occur early – preferably in the antenatal period, she added.
The most important thing, however, is “recognizing these women ... even before the pregnancy,” Dr. Bullock-Palmer said, explaining that this can facilitate the necessary management – and in some cases, postponement – of pregnancy for women whose cardiac issues need to be addressed first.
Among other efforts to address maternal mortality are several programs developed by ACOG, and the Heart Outcomes in Pregnancy: Expectations for Mom and Baby Registry (HOPE) project of the Saint Luke’s Health System in Kansas.
“Hopefully the [HOPE] research collaborative ... which aims to address key clinical questions surrounding the preconception period, antenatal care, delivery planning and outcomes, and long-term postpartum care and outcomes of women will help to address the knowledge gaps and disparities in the care of women with heart disease in pregnancy,” Dr. Bullock-Palmer wrote in her article.
CVD-related risks in the post partum
Dr. Bullock-Palmer has particular concern for postpartum follow-up, given the increased risk for future heart disease among women with CVD-related pregnancy complications and the heightened risk of certain CVD-related events in the postpartum period.
That’s a component of the crisis that also was addressed during a press briefing at the 2019 ACOG annual meeting when the Pregnancy and Heart Disease Practice Bulletin was released.
James Martin, MD, chair of ACOG’s Pregnancy and Heart Disease Task Force and a past ACOG president, explained during the briefing that CVD-related risks may accelerate and persist in the days and weeks after delivery, underscoring the need for follow-up and postpartum care.
Cardiomyopathy is a particular concern during this time – it’s the major cause of maternal mortality after 42 days, he noted. An emphasis on postpartum care also is especially important given that some data suggest up to 40% of women don’t return for that care.
“That is a very sad statistic and perhaps it reflects on our need to change payment models so that physicians and patients realize the importance of coming back for continuing care, because this really may be the end of pregnancy, but it is the beginning of the rest of their life,” he said. “And if they have cardiovascular disease or the risk factors ... they are going to possibly become worse over the course of their lifetime.”
A message from our president to the GI community
Dear colleagues,
The coronavirus pandemic has affected every facet of society, bringing almost unprecedented challenges to our world, and especially to our world of health care.
But our profession has been ignited in the way only a crisis can spark. Many of you are working on the front lines of patient care, at personal risk, lacking sufficient information and adequate resources. This is heroic work.
AGA’s priority during this time of disruption is to get practical guidance into your hands to help you treat patients, and protect yourselves and your coworkers. We’re also advocating on your behalf to get the resources you need and economic relief necessitated by the measures taken to fight the pandemic.
We are continually updating our COVID-19 website, www.gastro.org/covid. Check it for the latest clinical guidance, practice management information, and advocacy initiatives.
Our journals have started a collection of submissions related to COVID-19. Your AGA colleagues on the Clinical Guidelines Committee and Clinical Practice Updates Committee have been hard at work developing guidance for questions that you have asked us on Twitter, @AmerGastroAssn and the AGA Community. So join us there where resources and insights are being shared in real time.
Your commitment to our patients is a testament to your professionalism. Our commitment at AGA is to support you.
We’ll get through this together.
Hashem B. El-Serag, MD, MPH, AGAF
President, AGA Institute
Dear colleagues,
The coronavirus pandemic has affected every facet of society, bringing almost unprecedented challenges to our world, and especially to our world of health care.
But our profession has been ignited in the way only a crisis can spark. Many of you are working on the front lines of patient care, at personal risk, lacking sufficient information and adequate resources. This is heroic work.
AGA’s priority during this time of disruption is to get practical guidance into your hands to help you treat patients, and protect yourselves and your coworkers. We’re also advocating on your behalf to get the resources you need and economic relief necessitated by the measures taken to fight the pandemic.
We are continually updating our COVID-19 website, www.gastro.org/covid. Check it for the latest clinical guidance, practice management information, and advocacy initiatives.
Our journals have started a collection of submissions related to COVID-19. Your AGA colleagues on the Clinical Guidelines Committee and Clinical Practice Updates Committee have been hard at work developing guidance for questions that you have asked us on Twitter, @AmerGastroAssn and the AGA Community. So join us there where resources and insights are being shared in real time.
Your commitment to our patients is a testament to your professionalism. Our commitment at AGA is to support you.
We’ll get through this together.
Hashem B. El-Serag, MD, MPH, AGAF
President, AGA Institute
Dear colleagues,
The coronavirus pandemic has affected every facet of society, bringing almost unprecedented challenges to our world, and especially to our world of health care.
But our profession has been ignited in the way only a crisis can spark. Many of you are working on the front lines of patient care, at personal risk, lacking sufficient information and adequate resources. This is heroic work.
AGA’s priority during this time of disruption is to get practical guidance into your hands to help you treat patients, and protect yourselves and your coworkers. We’re also advocating on your behalf to get the resources you need and economic relief necessitated by the measures taken to fight the pandemic.
We are continually updating our COVID-19 website, www.gastro.org/covid. Check it for the latest clinical guidance, practice management information, and advocacy initiatives.
Our journals have started a collection of submissions related to COVID-19. Your AGA colleagues on the Clinical Guidelines Committee and Clinical Practice Updates Committee have been hard at work developing guidance for questions that you have asked us on Twitter, @AmerGastroAssn and the AGA Community. So join us there where resources and insights are being shared in real time.
Your commitment to our patients is a testament to your professionalism. Our commitment at AGA is to support you.
We’ll get through this together.
Hashem B. El-Serag, MD, MPH, AGAF
President, AGA Institute
AGA issues formal recommendations for PPE during gastrointestinal procedures
Based on a review of available evidence, we have published guidance for clinicians in gastroenterology: AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic. AGA recommends increasing personal protective equipment (PPE) during all GI procedures during the coronavirus pandemic, as well as triaging procedures following a decision-making framework outlined in the recommendations document.
Review this guidance, as well as the latest AGA resources and information on coronavirus, at www.gastro.org/COVID.
Masks
1. In health care workers performing upper GI procedures, regardless of COVID-19 status,* AGA recommends use of N95 (or N99 or PAPR) instead of surgical masks, as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
2. In health care workers performing lower GI procedures regardless of COVID-19 status,* AGA recommends the use of N95 (or N99 or PAPR) masks instead of surgical masks as part of appropriate personal protective equipment. (Strong recommendation, low certainty of evidence)
3. In health care workers performing upper GI procedures, in known or presumptive COVID-19 patients, AGA recommends against the use of surgical masks only, as part of adequate personal protective equipment. (Strong recommendation, low certainty of evidence)
Limited resource settings
4. In extreme resource-constrained settings involving health care workers performing any GI procedures, regardless of COVID-19 status,* AGA suggests extended use/re-use of N95 masks over surgical masks, as part of appropriate personal protective equipment. (Conditional recommendation, very low certainty evidence)
Gloves
5. In health care workers performing any GI procedure, regardless of COVID-19 status, AGA recommends the use of double gloves compared with single gloves as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
Negative pressure rooms
6. In health care workers performing any GI procedures with known or presumptive COVID-19, AGA suggests the use of negative pressure rooms over regular endoscopy rooms when available. (Conditional recommendation, very low certainty of evidence)
Endoscopic disinfection
7. For endoscopes utilized on patients regardless of COVID-status, AGA recommends continuing standard cleaning endoscopic disinfection and reprocessing protocols. (Good practice statement)
Triage
8. All procedures should be reviewed by trained medical personnel and categorized as time-sensitive or not time-sensitive as a framework for triaging procedures. (Good practice statement)
9. In an open access endoscopy system where the listed indication alone may provide insufficient information to make a determination about the time-sensitive nature of the procedure, consideration should be given for the following options (i) a telephone consultation with the referring provider or (ii) a telehealth visit with the patient or (iii) a multidisciplinary team approach to facilitate decision-making for complicated patients. (Good practice statement)
*These recommendations assume the absence of widespread reliable rapid testing for the diagnosis of COVID-19 infection or immunity
For a detailed discussion, review the full publication in Gastroenterology.
This rapid recommendation document was commissioned and approved by the AGA Institute Clinical Guidelines Committee, AGA Institute Clinical Practice Updates Committee, and the AGA Governing Board to provide timely, methodologically rigorous guidance on a topic of high clinical importance to the AGA membership and the public. Our goal is to protect health care providers and patients from coronavirus during GI procedures.
Based on a review of available evidence, we have published guidance for clinicians in gastroenterology: AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic. AGA recommends increasing personal protective equipment (PPE) during all GI procedures during the coronavirus pandemic, as well as triaging procedures following a decision-making framework outlined in the recommendations document.
Review this guidance, as well as the latest AGA resources and information on coronavirus, at www.gastro.org/COVID.
Masks
1. In health care workers performing upper GI procedures, regardless of COVID-19 status,* AGA recommends use of N95 (or N99 or PAPR) instead of surgical masks, as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
2. In health care workers performing lower GI procedures regardless of COVID-19 status,* AGA recommends the use of N95 (or N99 or PAPR) masks instead of surgical masks as part of appropriate personal protective equipment. (Strong recommendation, low certainty of evidence)
3. In health care workers performing upper GI procedures, in known or presumptive COVID-19 patients, AGA recommends against the use of surgical masks only, as part of adequate personal protective equipment. (Strong recommendation, low certainty of evidence)
Limited resource settings
4. In extreme resource-constrained settings involving health care workers performing any GI procedures, regardless of COVID-19 status,* AGA suggests extended use/re-use of N95 masks over surgical masks, as part of appropriate personal protective equipment. (Conditional recommendation, very low certainty evidence)
Gloves
5. In health care workers performing any GI procedure, regardless of COVID-19 status, AGA recommends the use of double gloves compared with single gloves as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
Negative pressure rooms
6. In health care workers performing any GI procedures with known or presumptive COVID-19, AGA suggests the use of negative pressure rooms over regular endoscopy rooms when available. (Conditional recommendation, very low certainty of evidence)
Endoscopic disinfection
7. For endoscopes utilized on patients regardless of COVID-status, AGA recommends continuing standard cleaning endoscopic disinfection and reprocessing protocols. (Good practice statement)
Triage
8. All procedures should be reviewed by trained medical personnel and categorized as time-sensitive or not time-sensitive as a framework for triaging procedures. (Good practice statement)
9. In an open access endoscopy system where the listed indication alone may provide insufficient information to make a determination about the time-sensitive nature of the procedure, consideration should be given for the following options (i) a telephone consultation with the referring provider or (ii) a telehealth visit with the patient or (iii) a multidisciplinary team approach to facilitate decision-making for complicated patients. (Good practice statement)
*These recommendations assume the absence of widespread reliable rapid testing for the diagnosis of COVID-19 infection or immunity
For a detailed discussion, review the full publication in Gastroenterology.
This rapid recommendation document was commissioned and approved by the AGA Institute Clinical Guidelines Committee, AGA Institute Clinical Practice Updates Committee, and the AGA Governing Board to provide timely, methodologically rigorous guidance on a topic of high clinical importance to the AGA membership and the public. Our goal is to protect health care providers and patients from coronavirus during GI procedures.
Based on a review of available evidence, we have published guidance for clinicians in gastroenterology: AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic. AGA recommends increasing personal protective equipment (PPE) during all GI procedures during the coronavirus pandemic, as well as triaging procedures following a decision-making framework outlined in the recommendations document.
Review this guidance, as well as the latest AGA resources and information on coronavirus, at www.gastro.org/COVID.
Masks
1. In health care workers performing upper GI procedures, regardless of COVID-19 status,* AGA recommends use of N95 (or N99 or PAPR) instead of surgical masks, as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
2. In health care workers performing lower GI procedures regardless of COVID-19 status,* AGA recommends the use of N95 (or N99 or PAPR) masks instead of surgical masks as part of appropriate personal protective equipment. (Strong recommendation, low certainty of evidence)
3. In health care workers performing upper GI procedures, in known or presumptive COVID-19 patients, AGA recommends against the use of surgical masks only, as part of adequate personal protective equipment. (Strong recommendation, low certainty of evidence)
Limited resource settings
4. In extreme resource-constrained settings involving health care workers performing any GI procedures, regardless of COVID-19 status,* AGA suggests extended use/re-use of N95 masks over surgical masks, as part of appropriate personal protective equipment. (Conditional recommendation, very low certainty evidence)
Gloves
5. In health care workers performing any GI procedure, regardless of COVID-19 status, AGA recommends the use of double gloves compared with single gloves as part of appropriate personal protective equipment. (Strong recommendation, moderate certainty of evidence)
Negative pressure rooms
6. In health care workers performing any GI procedures with known or presumptive COVID-19, AGA suggests the use of negative pressure rooms over regular endoscopy rooms when available. (Conditional recommendation, very low certainty of evidence)
Endoscopic disinfection
7. For endoscopes utilized on patients regardless of COVID-status, AGA recommends continuing standard cleaning endoscopic disinfection and reprocessing protocols. (Good practice statement)
Triage
8. All procedures should be reviewed by trained medical personnel and categorized as time-sensitive or not time-sensitive as a framework for triaging procedures. (Good practice statement)
9. In an open access endoscopy system where the listed indication alone may provide insufficient information to make a determination about the time-sensitive nature of the procedure, consideration should be given for the following options (i) a telephone consultation with the referring provider or (ii) a telehealth visit with the patient or (iii) a multidisciplinary team approach to facilitate decision-making for complicated patients. (Good practice statement)
*These recommendations assume the absence of widespread reliable rapid testing for the diagnosis of COVID-19 infection or immunity
For a detailed discussion, review the full publication in Gastroenterology.
This rapid recommendation document was commissioned and approved by the AGA Institute Clinical Guidelines Committee, AGA Institute Clinical Practice Updates Committee, and the AGA Governing Board to provide timely, methodologically rigorous guidance on a topic of high clinical importance to the AGA membership and the public. Our goal is to protect health care providers and patients from coronavirus during GI procedures.
Top AGA Community patient cases
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses.
Here are some recent discussions addressing clinical concerns and issues arising from the COVID-19 epidemic:
eQ&A on recommendations for GI procedures during the COVID-19 pandemic – Join guideline authors in discussing AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic, published in Gastroenterology.
1. IBD patients and COVID-19 – To allow for timely dissemination throughout the IBD and international gastroenterology communities, members are sharing important updates regarding COVID-19 and IBD management.
2. Medicare COVID-19 changes and telehealth reimbursement – Share your experiences and difficulties using telehealth platforms like Skype and facetime to connect with Medicare beneficiaries during the coronavirus epidemic.
3. Anesthesia options for in-patient endoscopy – Colleagues examine whether intubation is the best approach for EGDs to minimize COVID-19 transmission risk.
Access these and more discussions at https://community.gastro.org/discussions.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses.
Here are some recent discussions addressing clinical concerns and issues arising from the COVID-19 epidemic:
eQ&A on recommendations for GI procedures during the COVID-19 pandemic – Join guideline authors in discussing AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic, published in Gastroenterology.
1. IBD patients and COVID-19 – To allow for timely dissemination throughout the IBD and international gastroenterology communities, members are sharing important updates regarding COVID-19 and IBD management.
2. Medicare COVID-19 changes and telehealth reimbursement – Share your experiences and difficulties using telehealth platforms like Skype and facetime to connect with Medicare beneficiaries during the coronavirus epidemic.
3. Anesthesia options for in-patient endoscopy – Colleagues examine whether intubation is the best approach for EGDs to minimize COVID-19 transmission risk.
Access these and more discussions at https://community.gastro.org/discussions.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses.
Here are some recent discussions addressing clinical concerns and issues arising from the COVID-19 epidemic:
eQ&A on recommendations for GI procedures during the COVID-19 pandemic – Join guideline authors in discussing AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic, published in Gastroenterology.
1. IBD patients and COVID-19 – To allow for timely dissemination throughout the IBD and international gastroenterology communities, members are sharing important updates regarding COVID-19 and IBD management.
2. Medicare COVID-19 changes and telehealth reimbursement – Share your experiences and difficulties using telehealth platforms like Skype and facetime to connect with Medicare beneficiaries during the coronavirus epidemic.
3. Anesthesia options for in-patient endoscopy – Colleagues examine whether intubation is the best approach for EGDs to minimize COVID-19 transmission risk.
Access these and more discussions at https://community.gastro.org/discussions.
In praise of parents and children
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at pdnews@mdedge.com.
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at pdnews@mdedge.com.
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at pdnews@mdedge.com.
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
2019-2020 flu season ends with ‘very high’ activity in New Jersey
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
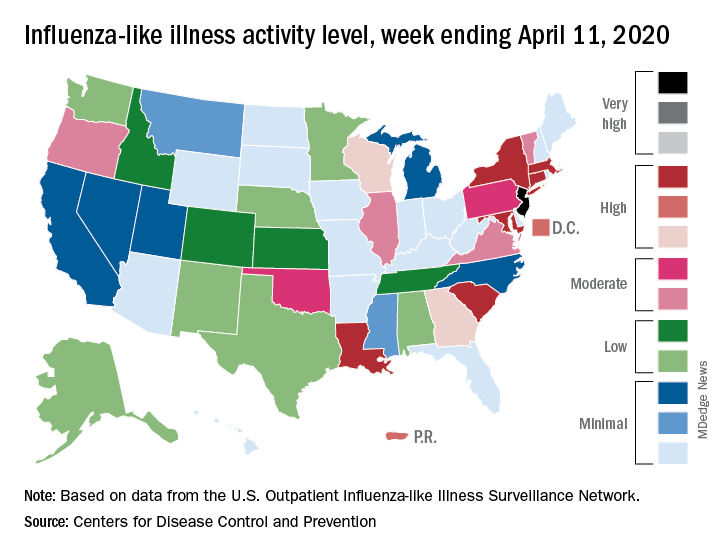
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
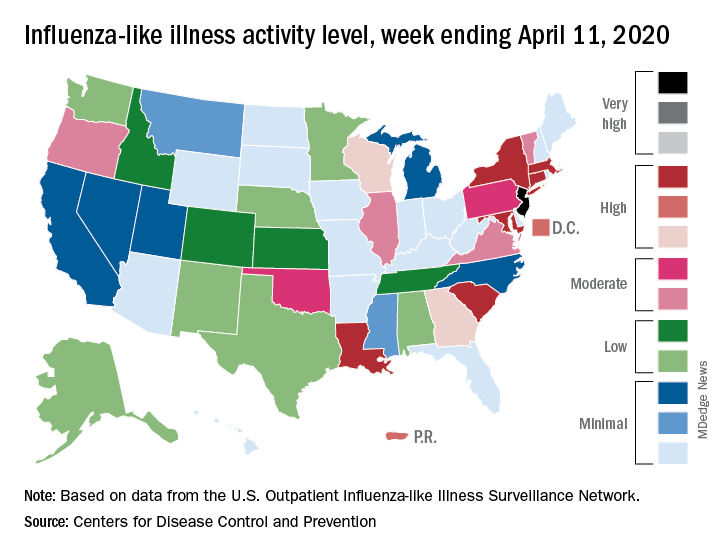
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
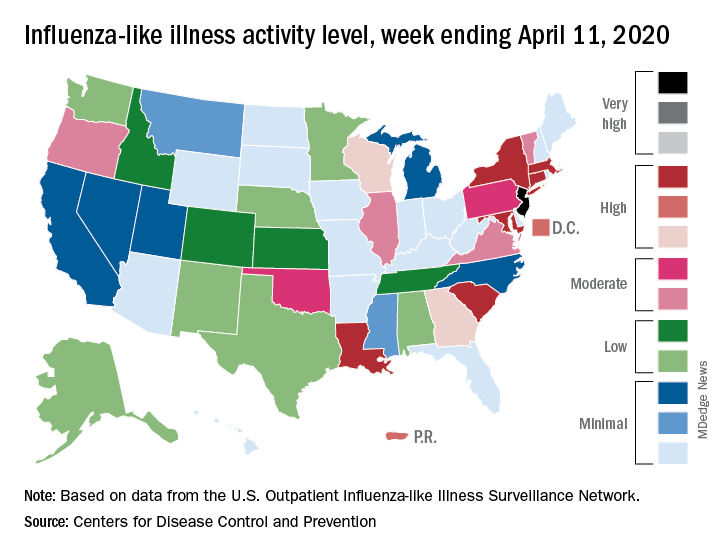
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
N.Y. universal testing: Many COVID-19+ pregnant women are asymptomatic
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Universal COVID-19 testing for pregnant women entering hospitals for delivery could better protect patients and staff.
Major finding: Approximately 88% of 33 pregnant women who tested positive for COVID-19 infection at hospital admission were asymptomatic; about 14% of the 215 women overall tested positive for the novel coronavirus.
Study details: The data come from a review of 215 pregnant women who delivered infants between March 22 and April 4, 2020, in New York City.
Disclosures: The authors had no financial conflicts to disclose.
Source: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
Infectious disease experts say testing is key to reopening
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
First-in-class schizophrenia drug safe, effective, durable
A novel first-in-class antipsychotic that has a completely different mechanism of action than other currently available agents shows long-term efficacy and a good safety profile in patients with schizophrenia.
SEP-363856 (Sunovion Pharmaceuticals) was described as a potential “game changer” for schizophrenia after initial results were presented at the American Psychiatric Association 2019 Annual Meeting. The drug has been granted breakthrough therapy designation by the Food and Drug Administration.
Additional data from this study, as well as results from a 6-month open-label extension trial were published April 15 in The New England Journal of Medicine.
“This is the first safety and effectiveness data for 6 months on therapy,” lead author Kenneth Koblan, PhD, chief scientific officer at Sunovion, said in an interview.
To be able to show “durable” benefit and that the drug is “benign with respect to weight gain, lipids, and extrapyramidal side effects really provides us with a view of what could be a whole new class of molecules with respect to safety and efficacy,” Dr. Koblan said.
Clinically meaningful improvement
Although the exact mechanism of action is unknown, It does not bind to dopamine 2 (D2) or serotonin 2A (5-HT2A) receptors, which are thought to mediate the effects of currently available antipsychotics.
The original SEP 361-201 study was a phase 2, 4-week, double-blind, placebo-controlled trial comprising 245 adults hospitalized with an acute exacerbation of schizophrenia. Patients were randomly allocated to receive SEP-363856 (50 mg or 75 mg once daily) or placebo.
Demographics of the treatment groups were similar at baseline. The SEP-363856 group included 120 patients (64% men; mean age, 30.0 years; Positive and Negative Syndrome Scale [PANSS] total score, 101.4). The placebo group included 125 patients (63% men; mean age, 30.6 years; PANSS total score, 99.7).
After 4 weeks of treatment, patients taking SEP-363856 showed statistically significant and clinically meaningful improvement in PANSS total scores (the primary outcome), compared with patients taking placebo (–17.2 vs –9.7; P = .001; effect size = 0.45).
SEP-363856 also led to significant improvement in several secondary outcomes, including overall illness severity as judged by the Clinical Global Impression of Severity score, PANSS positive subscale score, PANSS negative subscale score, and PANSS general psychopathology subscale score.
A total of 156 patients, representing 81% of those who completed the 4-week trial, were enrolled in an extension study. They received treatment with SEP-363856 for 26 weeks.
Among 77 patients who had initially been assigned to SEP-363856 in the double-blind trial and then continued to receive treatment in the open-label extension, the mean change in PANSS total score from extension-study baseline to week 26 was −17.1 points.
Among 79 patients who had initially been assigned to placebo and then switched to open-label SEP-363856, the mean change in PANSS total score was −27.9 points.
Safety and tolerability of SEP-363856 were generally similar to placebo.
The active treatment and placebo arms were similar in number of patients who reported extrapyramidal symptoms (3.3% vs. 3.2%, respectively) and who used medications to treat extrapyramidal symptoms. The findings were also similar on movement disorder scales.
In addition, the novel drug had minimal effects on the protein hormone prolactin. “These findings are consistent with the absence of D2-receptor binding for SEP-363856,” the investigators wrote.
Adverse events (AEs) occurring with an incidence of at least 2%, and with a higher incidence in SEP-363856 than placebo, were somnolence (6.7% vs. 4.8%, respectively), agitation (5% vs. 4.8%), nausea (5% vs. 3.2%), diarrhea (2.5% vs. 0.8%), and dyspepsia (2.5% vs. 0%).
Two serious AEs that occurred in the SEP-363856 arm were worsening of schizophrenia and acute cardiovascular insufficiency in a 37-year-old woman, which led to her death 1 week after taking the first 50-mg dose of treatment. However, the woman had a history of essential hypertension and, at autopsy, was found to have coronary artery disease and pulmonary embolism.
A large phase 3 program is now underway to confirm safety and efficacy of SEP-363856 for schizophrenia, Dr. Koblan said. It includes four studies that are open and enrolling.
Benefit beyond psychosis?
In an accompanying editorial , Donald C. Goff, MD, of the Nathan Kline Institute at New York University, wrote that if the findings were replicated in future trials with more patients and of longer duration, “this class of drugs may provide a valuable new therapeutic option for psychosis and the negative symptoms of schizophrenia, possibly without the adverse effects associated with direct D2-receptor antagonism.”
It is also possible that SEP-363856 will have effects “beyond D2-receptor antagonists and hence beyond the treatment of psychosis. Other potential therapeutic indications, including cognitive impairment, depression, and substance abuse, remain to be explored,” Dr. Goff wrote.
This study “not only introduces a promising therapeutic compound but also provides additional evidence, on the basis of an agnostic drug-discovery process, that TAAR1 is a promising target,” he added.
“This is very welcome news given the great need for new pharmacologic treatments for patients with schizophrenia,” Dr. Goff concluded.
The study was funded by Sunovion Pharmaceuticals. Dr. Koblan is an employee of the company. Disclosures for the other authors are listed in the original article. Dr. Goff reported having received grants and nonfinancial support from Avanir Pharmaceuticals and from Takeda.
A version of this article first appeared on Medscape.com.
A novel first-in-class antipsychotic that has a completely different mechanism of action than other currently available agents shows long-term efficacy and a good safety profile in patients with schizophrenia.
SEP-363856 (Sunovion Pharmaceuticals) was described as a potential “game changer” for schizophrenia after initial results were presented at the American Psychiatric Association 2019 Annual Meeting. The drug has been granted breakthrough therapy designation by the Food and Drug Administration.
Additional data from this study, as well as results from a 6-month open-label extension trial were published April 15 in The New England Journal of Medicine.
“This is the first safety and effectiveness data for 6 months on therapy,” lead author Kenneth Koblan, PhD, chief scientific officer at Sunovion, said in an interview.
To be able to show “durable” benefit and that the drug is “benign with respect to weight gain, lipids, and extrapyramidal side effects really provides us with a view of what could be a whole new class of molecules with respect to safety and efficacy,” Dr. Koblan said.
Clinically meaningful improvement
Although the exact mechanism of action is unknown, It does not bind to dopamine 2 (D2) or serotonin 2A (5-HT2A) receptors, which are thought to mediate the effects of currently available antipsychotics.
The original SEP 361-201 study was a phase 2, 4-week, double-blind, placebo-controlled trial comprising 245 adults hospitalized with an acute exacerbation of schizophrenia. Patients were randomly allocated to receive SEP-363856 (50 mg or 75 mg once daily) or placebo.
Demographics of the treatment groups were similar at baseline. The SEP-363856 group included 120 patients (64% men; mean age, 30.0 years; Positive and Negative Syndrome Scale [PANSS] total score, 101.4). The placebo group included 125 patients (63% men; mean age, 30.6 years; PANSS total score, 99.7).
After 4 weeks of treatment, patients taking SEP-363856 showed statistically significant and clinically meaningful improvement in PANSS total scores (the primary outcome), compared with patients taking placebo (–17.2 vs –9.7; P = .001; effect size = 0.45).
SEP-363856 also led to significant improvement in several secondary outcomes, including overall illness severity as judged by the Clinical Global Impression of Severity score, PANSS positive subscale score, PANSS negative subscale score, and PANSS general psychopathology subscale score.
A total of 156 patients, representing 81% of those who completed the 4-week trial, were enrolled in an extension study. They received treatment with SEP-363856 for 26 weeks.
Among 77 patients who had initially been assigned to SEP-363856 in the double-blind trial and then continued to receive treatment in the open-label extension, the mean change in PANSS total score from extension-study baseline to week 26 was −17.1 points.
Among 79 patients who had initially been assigned to placebo and then switched to open-label SEP-363856, the mean change in PANSS total score was −27.9 points.
Safety and tolerability of SEP-363856 were generally similar to placebo.
The active treatment and placebo arms were similar in number of patients who reported extrapyramidal symptoms (3.3% vs. 3.2%, respectively) and who used medications to treat extrapyramidal symptoms. The findings were also similar on movement disorder scales.
In addition, the novel drug had minimal effects on the protein hormone prolactin. “These findings are consistent with the absence of D2-receptor binding for SEP-363856,” the investigators wrote.
Adverse events (AEs) occurring with an incidence of at least 2%, and with a higher incidence in SEP-363856 than placebo, were somnolence (6.7% vs. 4.8%, respectively), agitation (5% vs. 4.8%), nausea (5% vs. 3.2%), diarrhea (2.5% vs. 0.8%), and dyspepsia (2.5% vs. 0%).
Two serious AEs that occurred in the SEP-363856 arm were worsening of schizophrenia and acute cardiovascular insufficiency in a 37-year-old woman, which led to her death 1 week after taking the first 50-mg dose of treatment. However, the woman had a history of essential hypertension and, at autopsy, was found to have coronary artery disease and pulmonary embolism.
A large phase 3 program is now underway to confirm safety and efficacy of SEP-363856 for schizophrenia, Dr. Koblan said. It includes four studies that are open and enrolling.
Benefit beyond psychosis?
In an accompanying editorial , Donald C. Goff, MD, of the Nathan Kline Institute at New York University, wrote that if the findings were replicated in future trials with more patients and of longer duration, “this class of drugs may provide a valuable new therapeutic option for psychosis and the negative symptoms of schizophrenia, possibly without the adverse effects associated with direct D2-receptor antagonism.”
It is also possible that SEP-363856 will have effects “beyond D2-receptor antagonists and hence beyond the treatment of psychosis. Other potential therapeutic indications, including cognitive impairment, depression, and substance abuse, remain to be explored,” Dr. Goff wrote.
This study “not only introduces a promising therapeutic compound but also provides additional evidence, on the basis of an agnostic drug-discovery process, that TAAR1 is a promising target,” he added.
“This is very welcome news given the great need for new pharmacologic treatments for patients with schizophrenia,” Dr. Goff concluded.
The study was funded by Sunovion Pharmaceuticals. Dr. Koblan is an employee of the company. Disclosures for the other authors are listed in the original article. Dr. Goff reported having received grants and nonfinancial support from Avanir Pharmaceuticals and from Takeda.
A version of this article first appeared on Medscape.com.
A novel first-in-class antipsychotic that has a completely different mechanism of action than other currently available agents shows long-term efficacy and a good safety profile in patients with schizophrenia.
SEP-363856 (Sunovion Pharmaceuticals) was described as a potential “game changer” for schizophrenia after initial results were presented at the American Psychiatric Association 2019 Annual Meeting. The drug has been granted breakthrough therapy designation by the Food and Drug Administration.
Additional data from this study, as well as results from a 6-month open-label extension trial were published April 15 in The New England Journal of Medicine.
“This is the first safety and effectiveness data for 6 months on therapy,” lead author Kenneth Koblan, PhD, chief scientific officer at Sunovion, said in an interview.
To be able to show “durable” benefit and that the drug is “benign with respect to weight gain, lipids, and extrapyramidal side effects really provides us with a view of what could be a whole new class of molecules with respect to safety and efficacy,” Dr. Koblan said.
Clinically meaningful improvement
Although the exact mechanism of action is unknown, It does not bind to dopamine 2 (D2) or serotonin 2A (5-HT2A) receptors, which are thought to mediate the effects of currently available antipsychotics.
The original SEP 361-201 study was a phase 2, 4-week, double-blind, placebo-controlled trial comprising 245 adults hospitalized with an acute exacerbation of schizophrenia. Patients were randomly allocated to receive SEP-363856 (50 mg or 75 mg once daily) or placebo.
Demographics of the treatment groups were similar at baseline. The SEP-363856 group included 120 patients (64% men; mean age, 30.0 years; Positive and Negative Syndrome Scale [PANSS] total score, 101.4). The placebo group included 125 patients (63% men; mean age, 30.6 years; PANSS total score, 99.7).
After 4 weeks of treatment, patients taking SEP-363856 showed statistically significant and clinically meaningful improvement in PANSS total scores (the primary outcome), compared with patients taking placebo (–17.2 vs –9.7; P = .001; effect size = 0.45).
SEP-363856 also led to significant improvement in several secondary outcomes, including overall illness severity as judged by the Clinical Global Impression of Severity score, PANSS positive subscale score, PANSS negative subscale score, and PANSS general psychopathology subscale score.
A total of 156 patients, representing 81% of those who completed the 4-week trial, were enrolled in an extension study. They received treatment with SEP-363856 for 26 weeks.
Among 77 patients who had initially been assigned to SEP-363856 in the double-blind trial and then continued to receive treatment in the open-label extension, the mean change in PANSS total score from extension-study baseline to week 26 was −17.1 points.
Among 79 patients who had initially been assigned to placebo and then switched to open-label SEP-363856, the mean change in PANSS total score was −27.9 points.
Safety and tolerability of SEP-363856 were generally similar to placebo.
The active treatment and placebo arms were similar in number of patients who reported extrapyramidal symptoms (3.3% vs. 3.2%, respectively) and who used medications to treat extrapyramidal symptoms. The findings were also similar on movement disorder scales.
In addition, the novel drug had minimal effects on the protein hormone prolactin. “These findings are consistent with the absence of D2-receptor binding for SEP-363856,” the investigators wrote.
Adverse events (AEs) occurring with an incidence of at least 2%, and with a higher incidence in SEP-363856 than placebo, were somnolence (6.7% vs. 4.8%, respectively), agitation (5% vs. 4.8%), nausea (5% vs. 3.2%), diarrhea (2.5% vs. 0.8%), and dyspepsia (2.5% vs. 0%).
Two serious AEs that occurred in the SEP-363856 arm were worsening of schizophrenia and acute cardiovascular insufficiency in a 37-year-old woman, which led to her death 1 week after taking the first 50-mg dose of treatment. However, the woman had a history of essential hypertension and, at autopsy, was found to have coronary artery disease and pulmonary embolism.
A large phase 3 program is now underway to confirm safety and efficacy of SEP-363856 for schizophrenia, Dr. Koblan said. It includes four studies that are open and enrolling.
Benefit beyond psychosis?
In an accompanying editorial , Donald C. Goff, MD, of the Nathan Kline Institute at New York University, wrote that if the findings were replicated in future trials with more patients and of longer duration, “this class of drugs may provide a valuable new therapeutic option for psychosis and the negative symptoms of schizophrenia, possibly without the adverse effects associated with direct D2-receptor antagonism.”
It is also possible that SEP-363856 will have effects “beyond D2-receptor antagonists and hence beyond the treatment of psychosis. Other potential therapeutic indications, including cognitive impairment, depression, and substance abuse, remain to be explored,” Dr. Goff wrote.
This study “not only introduces a promising therapeutic compound but also provides additional evidence, on the basis of an agnostic drug-discovery process, that TAAR1 is a promising target,” he added.
“This is very welcome news given the great need for new pharmacologic treatments for patients with schizophrenia,” Dr. Goff concluded.
The study was funded by Sunovion Pharmaceuticals. Dr. Koblan is an employee of the company. Disclosures for the other authors are listed in the original article. Dr. Goff reported having received grants and nonfinancial support from Avanir Pharmaceuticals and from Takeda.
A version of this article first appeared on Medscape.com.
How to sanitize N95 masks for reuse: NIH study
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.









