User login
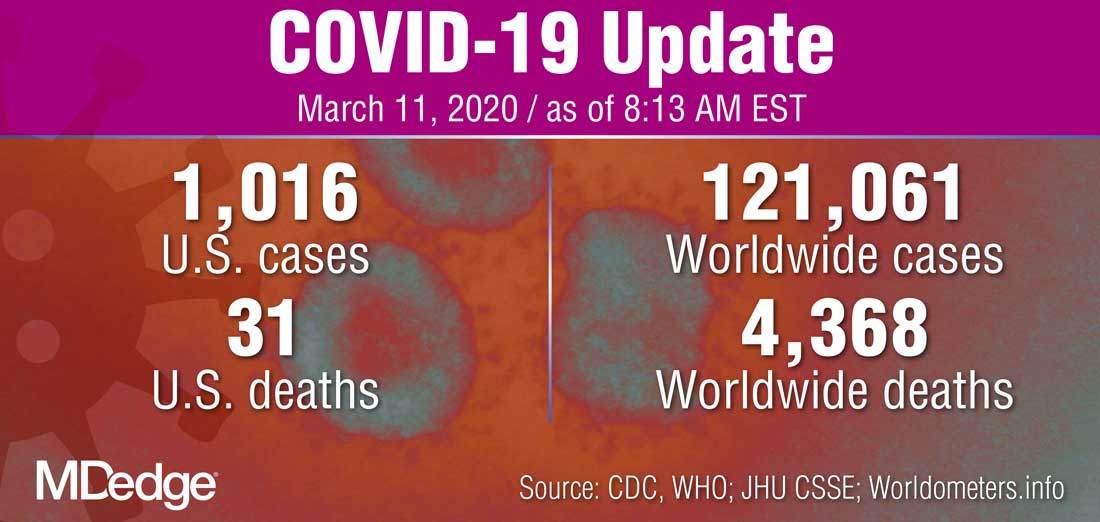
WHO declares COVID-19 outbreak a pandemic
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
FDA broadens nintedanib interstitial lung disease indication
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
Pancreatic enzyme replacement flunked randomized trial
Pancreatic enzyme replacement therapy (PERT) did not significantly alter body weight after pancreatoduodenectomy in the intention-to-treat analysis of a randomized, placebo-controlled trial.
After 3 months of treatment, the PERT group lost an average of 0.68 kg, and the placebo group lost an average of 1.19 kg (P = .302). Low adherence might explain this missed primary endpoint – the 31% of patients who did not adhere to PERT were about four times more likely to lose weight, compared with patients who adhered to PERT (hazard ratio, 4.1, 95% confidence interval, 2.1-7.6), even after possible confounders were controlled for.
In the per-protocol analysis, PERT was associated with an average gain of 1.09 kg in body weight, whereas placebo was associated with an average loss of 2.28 kg (P < .001 for difference between groups). Therefore, clinicians should consider “active education and monitoring” to increase adherence to PERT among patients with pancreatic enzyme insufficiency after pancreatoduodenectomy, wrote Hongbeom Kim of Seoul (South Korea) National University College of Medicine. The findings were published in Clinical Gastroenterology and Hepatology.
Nutritional deficiencies, steatorrhea, bowel issues, and flatulence undermine health and quality of life among these patients, the researchers noted. Although guidelines recommend PERT, doses and indications are not standardized because of insufficient data. To date, most studies have focused on PERT for patients with pancreatic enzyme insufficiency attributable to chronic pancreatitis, not surgery.
This double-blind trial enrolled 304 patients who underwent pancreatoduodenectomy for benign or malignant indications at seven tertiary referral hospitals in South Korea. All patients had a preoperative or postoperative fecal elastase level of 200 mg/g or less. They were randomly assigned to receive thrice-daily capsules with meals consisting of PERT (40,000 FIP lipase, 25,000 FIP amylase, and 1,500 FIP protease) or placebo.
To assess adherence, patients filled out medication diaries and the investigators counted the number of capsules left at 3-month follow-up. “Patients who took more than two-thirds of the total [PERT or placebo] dose without taking other digestive enzymes were considered to have completed the protocol,” the researchers wrote.
In all, 67 patients were excluded from the intention-to-treat analysis because they withdrew consent or were lost to follow-up. Among the remaining 237 patients, PERT did not significantly outperform placebo for the primary endpoint of body weight or for secondary endpoints, including nutritional status and quality of life. The study was powered to assess the intention-to-treat population and hence missed its primary endpoint.
The per-protocol analysis included 71 patients who adhered to PERT and 93 who adhered to placebo. Among these patients, adherence to PERT versus placebo was associated with a 3.37-kg absolute mean increase in body weight (P < .001). [The use] of PERT [also significantly] increased prealbumin and transferrin levels, reflecting short-term nutritional status,” the researchers wrote. “However, no difference in quality of life was observed.”
Subgroup analyses also favored PERT in the per-protocol analysis but not the intention-to-treat analysis, the researchers said. The use of PERT did not significantly affect the frequency of defecation in either the intention-to-treat or the per-protocol analysis.
Korea Pharmbio and the Ministry of Science and ICT provided funding. The researchers reported having no conflicts of interest.
SOURCE: Kim H et al. Clin Gastroenterol Hepatol. 2019 Sep 12. doi: 10.1016/j.cgh.2019.08.061.
Pancreatic enzyme replacement therapy (PERT) did not significantly alter body weight after pancreatoduodenectomy in the intention-to-treat analysis of a randomized, placebo-controlled trial.
After 3 months of treatment, the PERT group lost an average of 0.68 kg, and the placebo group lost an average of 1.19 kg (P = .302). Low adherence might explain this missed primary endpoint – the 31% of patients who did not adhere to PERT were about four times more likely to lose weight, compared with patients who adhered to PERT (hazard ratio, 4.1, 95% confidence interval, 2.1-7.6), even after possible confounders were controlled for.
In the per-protocol analysis, PERT was associated with an average gain of 1.09 kg in body weight, whereas placebo was associated with an average loss of 2.28 kg (P < .001 for difference between groups). Therefore, clinicians should consider “active education and monitoring” to increase adherence to PERT among patients with pancreatic enzyme insufficiency after pancreatoduodenectomy, wrote Hongbeom Kim of Seoul (South Korea) National University College of Medicine. The findings were published in Clinical Gastroenterology and Hepatology.
Nutritional deficiencies, steatorrhea, bowel issues, and flatulence undermine health and quality of life among these patients, the researchers noted. Although guidelines recommend PERT, doses and indications are not standardized because of insufficient data. To date, most studies have focused on PERT for patients with pancreatic enzyme insufficiency attributable to chronic pancreatitis, not surgery.
This double-blind trial enrolled 304 patients who underwent pancreatoduodenectomy for benign or malignant indications at seven tertiary referral hospitals in South Korea. All patients had a preoperative or postoperative fecal elastase level of 200 mg/g or less. They were randomly assigned to receive thrice-daily capsules with meals consisting of PERT (40,000 FIP lipase, 25,000 FIP amylase, and 1,500 FIP protease) or placebo.
To assess adherence, patients filled out medication diaries and the investigators counted the number of capsules left at 3-month follow-up. “Patients who took more than two-thirds of the total [PERT or placebo] dose without taking other digestive enzymes were considered to have completed the protocol,” the researchers wrote.
In all, 67 patients were excluded from the intention-to-treat analysis because they withdrew consent or were lost to follow-up. Among the remaining 237 patients, PERT did not significantly outperform placebo for the primary endpoint of body weight or for secondary endpoints, including nutritional status and quality of life. The study was powered to assess the intention-to-treat population and hence missed its primary endpoint.
The per-protocol analysis included 71 patients who adhered to PERT and 93 who adhered to placebo. Among these patients, adherence to PERT versus placebo was associated with a 3.37-kg absolute mean increase in body weight (P < .001). [The use] of PERT [also significantly] increased prealbumin and transferrin levels, reflecting short-term nutritional status,” the researchers wrote. “However, no difference in quality of life was observed.”
Subgroup analyses also favored PERT in the per-protocol analysis but not the intention-to-treat analysis, the researchers said. The use of PERT did not significantly affect the frequency of defecation in either the intention-to-treat or the per-protocol analysis.
Korea Pharmbio and the Ministry of Science and ICT provided funding. The researchers reported having no conflicts of interest.
SOURCE: Kim H et al. Clin Gastroenterol Hepatol. 2019 Sep 12. doi: 10.1016/j.cgh.2019.08.061.
Pancreatic enzyme replacement therapy (PERT) did not significantly alter body weight after pancreatoduodenectomy in the intention-to-treat analysis of a randomized, placebo-controlled trial.
After 3 months of treatment, the PERT group lost an average of 0.68 kg, and the placebo group lost an average of 1.19 kg (P = .302). Low adherence might explain this missed primary endpoint – the 31% of patients who did not adhere to PERT were about four times more likely to lose weight, compared with patients who adhered to PERT (hazard ratio, 4.1, 95% confidence interval, 2.1-7.6), even after possible confounders were controlled for.
In the per-protocol analysis, PERT was associated with an average gain of 1.09 kg in body weight, whereas placebo was associated with an average loss of 2.28 kg (P < .001 for difference between groups). Therefore, clinicians should consider “active education and monitoring” to increase adherence to PERT among patients with pancreatic enzyme insufficiency after pancreatoduodenectomy, wrote Hongbeom Kim of Seoul (South Korea) National University College of Medicine. The findings were published in Clinical Gastroenterology and Hepatology.
Nutritional deficiencies, steatorrhea, bowel issues, and flatulence undermine health and quality of life among these patients, the researchers noted. Although guidelines recommend PERT, doses and indications are not standardized because of insufficient data. To date, most studies have focused on PERT for patients with pancreatic enzyme insufficiency attributable to chronic pancreatitis, not surgery.
This double-blind trial enrolled 304 patients who underwent pancreatoduodenectomy for benign or malignant indications at seven tertiary referral hospitals in South Korea. All patients had a preoperative or postoperative fecal elastase level of 200 mg/g or less. They were randomly assigned to receive thrice-daily capsules with meals consisting of PERT (40,000 FIP lipase, 25,000 FIP amylase, and 1,500 FIP protease) or placebo.
To assess adherence, patients filled out medication diaries and the investigators counted the number of capsules left at 3-month follow-up. “Patients who took more than two-thirds of the total [PERT or placebo] dose without taking other digestive enzymes were considered to have completed the protocol,” the researchers wrote.
In all, 67 patients were excluded from the intention-to-treat analysis because they withdrew consent or were lost to follow-up. Among the remaining 237 patients, PERT did not significantly outperform placebo for the primary endpoint of body weight or for secondary endpoints, including nutritional status and quality of life. The study was powered to assess the intention-to-treat population and hence missed its primary endpoint.
The per-protocol analysis included 71 patients who adhered to PERT and 93 who adhered to placebo. Among these patients, adherence to PERT versus placebo was associated with a 3.37-kg absolute mean increase in body weight (P < .001). [The use] of PERT [also significantly] increased prealbumin and transferrin levels, reflecting short-term nutritional status,” the researchers wrote. “However, no difference in quality of life was observed.”
Subgroup analyses also favored PERT in the per-protocol analysis but not the intention-to-treat analysis, the researchers said. The use of PERT did not significantly affect the frequency of defecation in either the intention-to-treat or the per-protocol analysis.
Korea Pharmbio and the Ministry of Science and ICT provided funding. The researchers reported having no conflicts of interest.
SOURCE: Kim H et al. Clin Gastroenterol Hepatol. 2019 Sep 12. doi: 10.1016/j.cgh.2019.08.061.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Young women with insomnia at higher risk for car accidents
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
FROM SLEEP
Patients accept artificial intelligence in skin cancer screening
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
FROM JAMA DERMATOLOGY
Australian apocalypse essentials and bacterial evolution stoppers
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
Largest meeting on cancer research canceled: AACR
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.
Manual dexterity may decline more rapidly in pediatric-onset MS
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
REPORTING FROM ACTRIMS FORUM 2020
Managing children’s fear, anxiety in the age of COVID-19
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
AAD-NPF releases first guidelines for nonbiologic treatments of psoriasis
It’s been 11 years since monotherapy and suggest a framework for a number of off-label treatments.
The guidelines, issued jointly with the National Psoriasis Foundation (NPF), were published in the Journal of the American Academy of Dermatology.
“I think we are way behind,” Alan Menter, MD, chairman of the division of dermatology at Baylor University Medical Center, Dallas, and cochair of the guideline writing committee, said in an interview. “Most other countries update their guidelines every 1 or 2 years; we were 10 years behind.” The guidelines for systemic nonbiologic drugs follow up psoriasis guidelines issued by the AAD and the NPF on pediatric patients issued earlier this year, and on phototherapy, biologic treatments, and management of comorbidities issued last year.
“A lot has happened in the last 10 years,” said cochair Craig Elmets, MD, professor of dermatology at the University of Alabama at Birmingham. “While much of the interest is on biologic agents, nonbiologics are still used quite frequently, and the guidelines for their appropriate use have changed. Use of the guidelines provides people in the health profession with the most up to date evidence-based information so they can give their patients the best care.”
The guidelines acknowledge that the medications it covers are still widely used, either by themselves or in combination with biologic agents; readily available; easy to use; and, in the case of older therapies, relatively cheap.
Methotrexate has been available since the 1970s. Given as an injection or taken orally, the guidelines recommend supplementation with folic acid to counteract methotrexate’s side effects, particularly GI upset. The guidelines note that folic acid is less expensive than folinic acid. Combination therapy with methotrexate and tumor necrosis factor (TNF) inhibitors is more effective than methotrexate monotherapy, with a similar side effect profile, the guidelines state.
Methotrexate is more widely used outside the United States, “but it is a very good, quick fix and it’s much safer in children and young people than it is in people with cardiovascular disease,” Dr. Menter noted. “It’s still the most commonly used drug worldwide because it’s cheap, and you do have to worry about the long-term toxicity which is related the liver issues.”
The guidelines say that subcutaneous administration of methotrexate “may be particularly useful” for patients on higher doses, which when taken orally, are associated with a higher risk of GI effects.
Dr. Menter referred to a 2017 study, which reported 41% of patients treated with subcutaneous methotrexate once a week achieved a Psoriasis Area and Severity Index 75 score of 41% after a year of treatment, compared with 10% of those on placebo (Lancet. 2017 Feb 4;389[10068]:528-37).
The guidelines rate strength of recommendation as class A for methotrexate for moderate to severe psoriasis in adults, recommend supplementation with folic or folinic acid to counteract GI complications and liver problems, and note that adalimumab and infliximab are more effective than methotrexate for cutaneous psoriasis. Class B recommendations for methotrexate and psoriasis include statements that patients should begin with a test dose, especially if they have impaired kidney function; methotrexate is effective for peripheral, but not axial, psoriatic arthritis (PsA); and TNF inhibitors are more effective than methotrexate for PsA.
Approved by the FDA in 2014 for psoriasis, apremilast, which inhibits phosphodiesterase-4, is the newest drug in the recommendations. The guidelines recommend its use for moderate to severe psoriasis in adults, with a class A recommendation. Patients should start on a low dose and then build up to the 30-mg, twice-daily dose over 6 days and should be counseled about the risk of depression before starting treatment. Routine laboratory testing can be considered on an individual basis.
The guidelines also lay out three recommendations (and strength of recommendation) for cyclosporine, a drug that’s been around since the 1990s: for severe, recalcitrant cases (class A); for erythrodermic, general pustular, and palmoplantar psoriasis (class B); and as short-term therapy for psoriasis flare in patients already on another drug (class C).
Acitretin is another longstanding therapy used mostly for palmar-plantar psoriasis, but it can also be used as monotherapy for plaque psoriasis as well as erythrodermic and pustular disease. It can also be used in combination with psoralens with UVA for psoriasis and combined with broadband UVB phototherapy for plaque psoriasis. The acitretin recommendations are class B.
The oral Janus kinase (JAK) inhibitor tofacitinib isn’t specifically approved for psoriasis, but it is approved for RA, PsA, and ulcerative colitis. The drug targets the JAK-STAT signaling pathway that causes inflammation. The guidelines state that tofacitinib can be considered for moderate to severe psoriasis, but lists no strength of recommendation. The recommended dose is either 5 or 10 mg orally twice a day, with a caveat that the higher dose carries a higher risk of adverse events. Patients should be evaluated for getting a zoster vaccine before they begin therapy.
“We thought that, because there was probably a small chance that it might get approved for psoriasis, that we would discuss it briefly,” Dr. Menter said of tofacitinib.
Another off-label use the guidelines address is for fumaric and acid esters, also known as fumarates, which are used to in Europe to treat moderate to severe psoriasis. Dimethyl fumarate is approved for relapsing forms of multiple sclerosis in the United States. The guidelines state that fumarates can be used for psoriasis, but offer no strength of recommendation. Side effects include gastrointestinal disturbance and flushing.
Other treatments that are also addressed in the guidelines include a host of systemic immunosuppressants and antimetabolites: azathioprine, hydroxyurea, leflunomide, mycophenolate mofetil, thioguanine, and tacrolimus, none of which are FDA approved for psoriasis. They’re rarely used for psoriasis, but may have value in selected cases, the guidelines state.
Dr. Menter said that apremilast is the only oral drug in the guidelines, but they are the wave of the future for treating psoriasis. “I think there’s a tremendous potential for new oral drugs – TK2 [thymidine kinase], the JAK inhibitors, and other drugs coming down the pipelines. The majority of patients, if you ask them their preference, would like to take an oral drug rather than an injectable drug. And it would be much easier for dermatologists, they wouldn’t have to train patients on how to do the injections.”
Dr. Menter and Dr. Elmets disclosed financial relationships with numerous pharmaceutical companies. Other authors/work group members also had disclosures related to pharmaceutical manufacturers, and several had no disclosures.
SOURCE: Menter A et al. J Am Acad Dermatol. 2020 Feb 28. doi: 10.1016/j.jaad.2020.02.044.
It’s been 11 years since monotherapy and suggest a framework for a number of off-label treatments.
The guidelines, issued jointly with the National Psoriasis Foundation (NPF), were published in the Journal of the American Academy of Dermatology.
“I think we are way behind,” Alan Menter, MD, chairman of the division of dermatology at Baylor University Medical Center, Dallas, and cochair of the guideline writing committee, said in an interview. “Most other countries update their guidelines every 1 or 2 years; we were 10 years behind.” The guidelines for systemic nonbiologic drugs follow up psoriasis guidelines issued by the AAD and the NPF on pediatric patients issued earlier this year, and on phototherapy, biologic treatments, and management of comorbidities issued last year.
“A lot has happened in the last 10 years,” said cochair Craig Elmets, MD, professor of dermatology at the University of Alabama at Birmingham. “While much of the interest is on biologic agents, nonbiologics are still used quite frequently, and the guidelines for their appropriate use have changed. Use of the guidelines provides people in the health profession with the most up to date evidence-based information so they can give their patients the best care.”
The guidelines acknowledge that the medications it covers are still widely used, either by themselves or in combination with biologic agents; readily available; easy to use; and, in the case of older therapies, relatively cheap.
Methotrexate has been available since the 1970s. Given as an injection or taken orally, the guidelines recommend supplementation with folic acid to counteract methotrexate’s side effects, particularly GI upset. The guidelines note that folic acid is less expensive than folinic acid. Combination therapy with methotrexate and tumor necrosis factor (TNF) inhibitors is more effective than methotrexate monotherapy, with a similar side effect profile, the guidelines state.
Methotrexate is more widely used outside the United States, “but it is a very good, quick fix and it’s much safer in children and young people than it is in people with cardiovascular disease,” Dr. Menter noted. “It’s still the most commonly used drug worldwide because it’s cheap, and you do have to worry about the long-term toxicity which is related the liver issues.”
The guidelines say that subcutaneous administration of methotrexate “may be particularly useful” for patients on higher doses, which when taken orally, are associated with a higher risk of GI effects.
Dr. Menter referred to a 2017 study, which reported 41% of patients treated with subcutaneous methotrexate once a week achieved a Psoriasis Area and Severity Index 75 score of 41% after a year of treatment, compared with 10% of those on placebo (Lancet. 2017 Feb 4;389[10068]:528-37).
The guidelines rate strength of recommendation as class A for methotrexate for moderate to severe psoriasis in adults, recommend supplementation with folic or folinic acid to counteract GI complications and liver problems, and note that adalimumab and infliximab are more effective than methotrexate for cutaneous psoriasis. Class B recommendations for methotrexate and psoriasis include statements that patients should begin with a test dose, especially if they have impaired kidney function; methotrexate is effective for peripheral, but not axial, psoriatic arthritis (PsA); and TNF inhibitors are more effective than methotrexate for PsA.
Approved by the FDA in 2014 for psoriasis, apremilast, which inhibits phosphodiesterase-4, is the newest drug in the recommendations. The guidelines recommend its use for moderate to severe psoriasis in adults, with a class A recommendation. Patients should start on a low dose and then build up to the 30-mg, twice-daily dose over 6 days and should be counseled about the risk of depression before starting treatment. Routine laboratory testing can be considered on an individual basis.
The guidelines also lay out three recommendations (and strength of recommendation) for cyclosporine, a drug that’s been around since the 1990s: for severe, recalcitrant cases (class A); for erythrodermic, general pustular, and palmoplantar psoriasis (class B); and as short-term therapy for psoriasis flare in patients already on another drug (class C).
Acitretin is another longstanding therapy used mostly for palmar-plantar psoriasis, but it can also be used as monotherapy for plaque psoriasis as well as erythrodermic and pustular disease. It can also be used in combination with psoralens with UVA for psoriasis and combined with broadband UVB phototherapy for plaque psoriasis. The acitretin recommendations are class B.
The oral Janus kinase (JAK) inhibitor tofacitinib isn’t specifically approved for psoriasis, but it is approved for RA, PsA, and ulcerative colitis. The drug targets the JAK-STAT signaling pathway that causes inflammation. The guidelines state that tofacitinib can be considered for moderate to severe psoriasis, but lists no strength of recommendation. The recommended dose is either 5 or 10 mg orally twice a day, with a caveat that the higher dose carries a higher risk of adverse events. Patients should be evaluated for getting a zoster vaccine before they begin therapy.
“We thought that, because there was probably a small chance that it might get approved for psoriasis, that we would discuss it briefly,” Dr. Menter said of tofacitinib.
Another off-label use the guidelines address is for fumaric and acid esters, also known as fumarates, which are used to in Europe to treat moderate to severe psoriasis. Dimethyl fumarate is approved for relapsing forms of multiple sclerosis in the United States. The guidelines state that fumarates can be used for psoriasis, but offer no strength of recommendation. Side effects include gastrointestinal disturbance and flushing.
Other treatments that are also addressed in the guidelines include a host of systemic immunosuppressants and antimetabolites: azathioprine, hydroxyurea, leflunomide, mycophenolate mofetil, thioguanine, and tacrolimus, none of which are FDA approved for psoriasis. They’re rarely used for psoriasis, but may have value in selected cases, the guidelines state.
Dr. Menter said that apremilast is the only oral drug in the guidelines, but they are the wave of the future for treating psoriasis. “I think there’s a tremendous potential for new oral drugs – TK2 [thymidine kinase], the JAK inhibitors, and other drugs coming down the pipelines. The majority of patients, if you ask them their preference, would like to take an oral drug rather than an injectable drug. And it would be much easier for dermatologists, they wouldn’t have to train patients on how to do the injections.”
Dr. Menter and Dr. Elmets disclosed financial relationships with numerous pharmaceutical companies. Other authors/work group members also had disclosures related to pharmaceutical manufacturers, and several had no disclosures.
SOURCE: Menter A et al. J Am Acad Dermatol. 2020 Feb 28. doi: 10.1016/j.jaad.2020.02.044.
It’s been 11 years since monotherapy and suggest a framework for a number of off-label treatments.
The guidelines, issued jointly with the National Psoriasis Foundation (NPF), were published in the Journal of the American Academy of Dermatology.
“I think we are way behind,” Alan Menter, MD, chairman of the division of dermatology at Baylor University Medical Center, Dallas, and cochair of the guideline writing committee, said in an interview. “Most other countries update their guidelines every 1 or 2 years; we were 10 years behind.” The guidelines for systemic nonbiologic drugs follow up psoriasis guidelines issued by the AAD and the NPF on pediatric patients issued earlier this year, and on phototherapy, biologic treatments, and management of comorbidities issued last year.
“A lot has happened in the last 10 years,” said cochair Craig Elmets, MD, professor of dermatology at the University of Alabama at Birmingham. “While much of the interest is on biologic agents, nonbiologics are still used quite frequently, and the guidelines for their appropriate use have changed. Use of the guidelines provides people in the health profession with the most up to date evidence-based information so they can give their patients the best care.”
The guidelines acknowledge that the medications it covers are still widely used, either by themselves or in combination with biologic agents; readily available; easy to use; and, in the case of older therapies, relatively cheap.
Methotrexate has been available since the 1970s. Given as an injection or taken orally, the guidelines recommend supplementation with folic acid to counteract methotrexate’s side effects, particularly GI upset. The guidelines note that folic acid is less expensive than folinic acid. Combination therapy with methotrexate and tumor necrosis factor (TNF) inhibitors is more effective than methotrexate monotherapy, with a similar side effect profile, the guidelines state.
Methotrexate is more widely used outside the United States, “but it is a very good, quick fix and it’s much safer in children and young people than it is in people with cardiovascular disease,” Dr. Menter noted. “It’s still the most commonly used drug worldwide because it’s cheap, and you do have to worry about the long-term toxicity which is related the liver issues.”
The guidelines say that subcutaneous administration of methotrexate “may be particularly useful” for patients on higher doses, which when taken orally, are associated with a higher risk of GI effects.
Dr. Menter referred to a 2017 study, which reported 41% of patients treated with subcutaneous methotrexate once a week achieved a Psoriasis Area and Severity Index 75 score of 41% after a year of treatment, compared with 10% of those on placebo (Lancet. 2017 Feb 4;389[10068]:528-37).
The guidelines rate strength of recommendation as class A for methotrexate for moderate to severe psoriasis in adults, recommend supplementation with folic or folinic acid to counteract GI complications and liver problems, and note that adalimumab and infliximab are more effective than methotrexate for cutaneous psoriasis. Class B recommendations for methotrexate and psoriasis include statements that patients should begin with a test dose, especially if they have impaired kidney function; methotrexate is effective for peripheral, but not axial, psoriatic arthritis (PsA); and TNF inhibitors are more effective than methotrexate for PsA.
Approved by the FDA in 2014 for psoriasis, apremilast, which inhibits phosphodiesterase-4, is the newest drug in the recommendations. The guidelines recommend its use for moderate to severe psoriasis in adults, with a class A recommendation. Patients should start on a low dose and then build up to the 30-mg, twice-daily dose over 6 days and should be counseled about the risk of depression before starting treatment. Routine laboratory testing can be considered on an individual basis.
The guidelines also lay out three recommendations (and strength of recommendation) for cyclosporine, a drug that’s been around since the 1990s: for severe, recalcitrant cases (class A); for erythrodermic, general pustular, and palmoplantar psoriasis (class B); and as short-term therapy for psoriasis flare in patients already on another drug (class C).
Acitretin is another longstanding therapy used mostly for palmar-plantar psoriasis, but it can also be used as monotherapy for plaque psoriasis as well as erythrodermic and pustular disease. It can also be used in combination with psoralens with UVA for psoriasis and combined with broadband UVB phototherapy for plaque psoriasis. The acitretin recommendations are class B.
The oral Janus kinase (JAK) inhibitor tofacitinib isn’t specifically approved for psoriasis, but it is approved for RA, PsA, and ulcerative colitis. The drug targets the JAK-STAT signaling pathway that causes inflammation. The guidelines state that tofacitinib can be considered for moderate to severe psoriasis, but lists no strength of recommendation. The recommended dose is either 5 or 10 mg orally twice a day, with a caveat that the higher dose carries a higher risk of adverse events. Patients should be evaluated for getting a zoster vaccine before they begin therapy.
“We thought that, because there was probably a small chance that it might get approved for psoriasis, that we would discuss it briefly,” Dr. Menter said of tofacitinib.
Another off-label use the guidelines address is for fumaric and acid esters, also known as fumarates, which are used to in Europe to treat moderate to severe psoriasis. Dimethyl fumarate is approved for relapsing forms of multiple sclerosis in the United States. The guidelines state that fumarates can be used for psoriasis, but offer no strength of recommendation. Side effects include gastrointestinal disturbance and flushing.
Other treatments that are also addressed in the guidelines include a host of systemic immunosuppressants and antimetabolites: azathioprine, hydroxyurea, leflunomide, mycophenolate mofetil, thioguanine, and tacrolimus, none of which are FDA approved for psoriasis. They’re rarely used for psoriasis, but may have value in selected cases, the guidelines state.
Dr. Menter said that apremilast is the only oral drug in the guidelines, but they are the wave of the future for treating psoriasis. “I think there’s a tremendous potential for new oral drugs – TK2 [thymidine kinase], the JAK inhibitors, and other drugs coming down the pipelines. The majority of patients, if you ask them their preference, would like to take an oral drug rather than an injectable drug. And it would be much easier for dermatologists, they wouldn’t have to train patients on how to do the injections.”
Dr. Menter and Dr. Elmets disclosed financial relationships with numerous pharmaceutical companies. Other authors/work group members also had disclosures related to pharmaceutical manufacturers, and several had no disclosures.
SOURCE: Menter A et al. J Am Acad Dermatol. 2020 Feb 28. doi: 10.1016/j.jaad.2020.02.044.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY