User login
Wuhan virus: What clinicians need to know
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
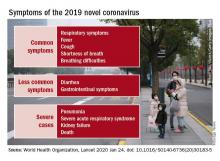
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
Catheter cryoablation effective for persistent AFib in pivotal trial
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
REPORTING FROM THE AF SYMPOSIUM 2020
Key clinical point: Catheter ablation using a cryoballoon was safe and effective for patients with persistent atrial fibrillation in a pivotal trial.
Major finding: The rate of freedom from treatment failure after 12 months was 55%, significantly exceeding the prespecified performance goal of 40%.
Study details: A multicenter, international study with 165 enrolled patients.
Disclosures: The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
New appointments at Cleveland Clinic, Fox Chase
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
EVALI update warns of chemicals in vaping products
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
FROM MMWR
Pubertal suppression reduces risk of later suicidal ideation in transgender people
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
FROM PEDIATRICS
The Lowdown on Low-Dose Naltrexone
Low-dose naltrexone (LDN) has shown efficacy in off-label treatment of a variety of inflammatory diseases ranging from Crohn disease to multiple sclerosis.1 There are limited data about the use of LDN in dermatology, but reports regarding how it works as an anti-inflammatory agent have been published.1,2
Naltrexone is an opioid receptor antagonist that originally was approved by the US Food and Drug Administration to treat addiction to alcohol, opiates, and heroin.2 The dose of naltrexone to treat addiction ranges from 50 to 100 mg/d, and at these levels the effects of opioids are blocked for 24 hours; however, the dosing for LDN is much lower, ranging from 1.5 to 4.5 mg/d.3 At this low dose, naltrexone partially binds to various opioid receptors, leading to a temporary blockade.4 One of the downstream effects of this opioid receptor blockade is a paradoxical increase in endogenous endorphins.3
In addition to opioid blockage, lower doses of naltrexone have anti-inflammatory effects by inhibiting nonopioid receptors. Naltrexone blocks toll-like receptor 4, which is found on keratinocytes and also on macrophages such as microglia.5 These macrophages also contain inflammatory compounds such as tumor necrosis factor α and IL-6. Low-dose naltrexone can suppress levels of these inflammatory markers. It is important to note that these anti-inflammatory effects have not been observed at the standard higher doses of naltrexone.1
When to Use
Low-dose naltrexone is a treatment option for inflammatory dermatologic conditions. A recent review of the literature outlined the use of LDN in a variety of inflammatory skin conditions. Improvement was noted in patients with Hailey-Hailey disease, lichen planopilaris, and various types of pruritus (ie, aquagenic, cholestatic, uremic, atopic dermatitis related).3 A case report of LDN successfully treating a patient with psoriasis also has been published.6 We often use LDN at the University of Wisconsin (Madison, Wisconsin) to treat patients with psoriasis. Ekelem et al3 also discussed patients with skin conditions that either had no response or worsened with naltrexone treatment, including various types of pruritus (ie, uremic, mycosis fungoides related, other causes of pruritus). Importantly, in the majority of cases without an improved response, the dose used was 50 mg/d.3 Higher doses of naltrexone are not known to have anti-inflammatory effects.
Low-dose naltrexone can be considered as a treatment option in patients with contraindications to other systemic anti-inflammatory treatments; for example, patients with a history of malignancy may prefer to avoid treatment with biologic agents. Low-dose naltrexone also can be considered as a treatment option in patients who are uncomfortable with the side-effect profiles of other systemic anti-inflammatory treatments, such as the risk for leukemias and lymphomas associated with biologic agents, the risk for liver toxicity with methotrexate, or the risk for hyperlipidemia with acitretin.
How to Monitor
The following monitoring information is adapted from the practice of Apple Bodemer, MD, a board-certified dermatologist at the University of Wisconsin (Madison, Wisconsin) who also is fellowship trained in integrative medicine.
There is a paucity of published data about LDN dosing for inflammatory skin diseases. However, prescribers should be aware that LDN can alter thyroid hormone levels, especially in patients with autoimmune thyroid disease. If a thyroid-stimulating hormone (TSH) level within reference range has not been noted in the last year, consider screening with a TSH test and also assessing for a personal or family history of thyroid disease. If the TSH level is within reference range, there generally is no need to monitor while treating with LDN. Consider checking TSH levels every 4 months in patients with thyroid disease while they are on LDN therapy and be sure to educate them about symptoms of hyperthyroidism.
Side Effects
Low-dose naltrexone has a minimal side-effect profile with self-limited side effects that often resolve within approximately 1 week. One of the most commonly reported side effects is sleep disturbance with vivid dreams, which has been reported in 37% of participants.1 If your patients experience this side effect, you can reassure them that it improves with time. You also can switch to morning dosing to try and alleviate sleep disturbances at night. Another possible side effect is gastrointestinal tract upset. Importantly, there is no known abuse potential for LDN.1 To stop LDN, patients should be stable for 6 to 12 months, and there is no need to wean them off it.
Cost and Availability
Because use of LDN in dermatology is considered off label and it is not approved by the US Food and Drug Administration to treat any medical conditions, it must be prescribed through a compounding pharmacy, usually without insurance coverage. The monthly cost is approximately $30 depending on the pharmacy (unpublished data), which may be cost prohibitive for patients, so it is important to counsel them about price
Final Thoughts
Low-dose naltrexone is an alternative treatment option that can be considered in patients with inflammatory skin diseases. It has a favorable side-effect profile, especially compared to other systemic anti-inflammatory agents; however, additional studies are needed to learn more about its safety and efficacy. If patients ask you about LDN, the information provided here can guide you with how it works and how to prescribe it.
- Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014;33:451-459.
- Brown N, Panksepp J. Low-dose naltrexone for disease prevention and quality of life. Med Hypotheses. 2009;72:333-337.
- Ekelem C, Juhasz M, Khera P, et al. Utility of naltrexone treatment for chronic inflammatory dermatologic conditions: a systematic review. JAMA Dermatol. 2019;155:229-236.
- Bihari B. Efficacy of low dose naltrexone as an immune stabilizing agent for the treatment of HIV/AIDS. AIDS Patient Care. 1995;9:3.
- Lee B, Elston DM. The uses of naltrexone in dermatologic conditions [published online December 21, 2018]. J Am Acad Dermatol. 2019;80:1746-1752.
- Bridgman AC, Kirchhof MG. Treatment of psoriasis vulgaris using low-dose naltrexone. JAAD Case Rep. 2018;4:827-829.
Low-dose naltrexone (LDN) has shown efficacy in off-label treatment of a variety of inflammatory diseases ranging from Crohn disease to multiple sclerosis.1 There are limited data about the use of LDN in dermatology, but reports regarding how it works as an anti-inflammatory agent have been published.1,2
Naltrexone is an opioid receptor antagonist that originally was approved by the US Food and Drug Administration to treat addiction to alcohol, opiates, and heroin.2 The dose of naltrexone to treat addiction ranges from 50 to 100 mg/d, and at these levels the effects of opioids are blocked for 24 hours; however, the dosing for LDN is much lower, ranging from 1.5 to 4.5 mg/d.3 At this low dose, naltrexone partially binds to various opioid receptors, leading to a temporary blockade.4 One of the downstream effects of this opioid receptor blockade is a paradoxical increase in endogenous endorphins.3
In addition to opioid blockage, lower doses of naltrexone have anti-inflammatory effects by inhibiting nonopioid receptors. Naltrexone blocks toll-like receptor 4, which is found on keratinocytes and also on macrophages such as microglia.5 These macrophages also contain inflammatory compounds such as tumor necrosis factor α and IL-6. Low-dose naltrexone can suppress levels of these inflammatory markers. It is important to note that these anti-inflammatory effects have not been observed at the standard higher doses of naltrexone.1
When to Use
Low-dose naltrexone is a treatment option for inflammatory dermatologic conditions. A recent review of the literature outlined the use of LDN in a variety of inflammatory skin conditions. Improvement was noted in patients with Hailey-Hailey disease, lichen planopilaris, and various types of pruritus (ie, aquagenic, cholestatic, uremic, atopic dermatitis related).3 A case report of LDN successfully treating a patient with psoriasis also has been published.6 We often use LDN at the University of Wisconsin (Madison, Wisconsin) to treat patients with psoriasis. Ekelem et al3 also discussed patients with skin conditions that either had no response or worsened with naltrexone treatment, including various types of pruritus (ie, uremic, mycosis fungoides related, other causes of pruritus). Importantly, in the majority of cases without an improved response, the dose used was 50 mg/d.3 Higher doses of naltrexone are not known to have anti-inflammatory effects.
Low-dose naltrexone can be considered as a treatment option in patients with contraindications to other systemic anti-inflammatory treatments; for example, patients with a history of malignancy may prefer to avoid treatment with biologic agents. Low-dose naltrexone also can be considered as a treatment option in patients who are uncomfortable with the side-effect profiles of other systemic anti-inflammatory treatments, such as the risk for leukemias and lymphomas associated with biologic agents, the risk for liver toxicity with methotrexate, or the risk for hyperlipidemia with acitretin.
How to Monitor
The following monitoring information is adapted from the practice of Apple Bodemer, MD, a board-certified dermatologist at the University of Wisconsin (Madison, Wisconsin) who also is fellowship trained in integrative medicine.
There is a paucity of published data about LDN dosing for inflammatory skin diseases. However, prescribers should be aware that LDN can alter thyroid hormone levels, especially in patients with autoimmune thyroid disease. If a thyroid-stimulating hormone (TSH) level within reference range has not been noted in the last year, consider screening with a TSH test and also assessing for a personal or family history of thyroid disease. If the TSH level is within reference range, there generally is no need to monitor while treating with LDN. Consider checking TSH levels every 4 months in patients with thyroid disease while they are on LDN therapy and be sure to educate them about symptoms of hyperthyroidism.
Side Effects
Low-dose naltrexone has a minimal side-effect profile with self-limited side effects that often resolve within approximately 1 week. One of the most commonly reported side effects is sleep disturbance with vivid dreams, which has been reported in 37% of participants.1 If your patients experience this side effect, you can reassure them that it improves with time. You also can switch to morning dosing to try and alleviate sleep disturbances at night. Another possible side effect is gastrointestinal tract upset. Importantly, there is no known abuse potential for LDN.1 To stop LDN, patients should be stable for 6 to 12 months, and there is no need to wean them off it.
Cost and Availability
Because use of LDN in dermatology is considered off label and it is not approved by the US Food and Drug Administration to treat any medical conditions, it must be prescribed through a compounding pharmacy, usually without insurance coverage. The monthly cost is approximately $30 depending on the pharmacy (unpublished data), which may be cost prohibitive for patients, so it is important to counsel them about price
Final Thoughts
Low-dose naltrexone is an alternative treatment option that can be considered in patients with inflammatory skin diseases. It has a favorable side-effect profile, especially compared to other systemic anti-inflammatory agents; however, additional studies are needed to learn more about its safety and efficacy. If patients ask you about LDN, the information provided here can guide you with how it works and how to prescribe it.
Low-dose naltrexone (LDN) has shown efficacy in off-label treatment of a variety of inflammatory diseases ranging from Crohn disease to multiple sclerosis.1 There are limited data about the use of LDN in dermatology, but reports regarding how it works as an anti-inflammatory agent have been published.1,2
Naltrexone is an opioid receptor antagonist that originally was approved by the US Food and Drug Administration to treat addiction to alcohol, opiates, and heroin.2 The dose of naltrexone to treat addiction ranges from 50 to 100 mg/d, and at these levels the effects of opioids are blocked for 24 hours; however, the dosing for LDN is much lower, ranging from 1.5 to 4.5 mg/d.3 At this low dose, naltrexone partially binds to various opioid receptors, leading to a temporary blockade.4 One of the downstream effects of this opioid receptor blockade is a paradoxical increase in endogenous endorphins.3
In addition to opioid blockage, lower doses of naltrexone have anti-inflammatory effects by inhibiting nonopioid receptors. Naltrexone blocks toll-like receptor 4, which is found on keratinocytes and also on macrophages such as microglia.5 These macrophages also contain inflammatory compounds such as tumor necrosis factor α and IL-6. Low-dose naltrexone can suppress levels of these inflammatory markers. It is important to note that these anti-inflammatory effects have not been observed at the standard higher doses of naltrexone.1
When to Use
Low-dose naltrexone is a treatment option for inflammatory dermatologic conditions. A recent review of the literature outlined the use of LDN in a variety of inflammatory skin conditions. Improvement was noted in patients with Hailey-Hailey disease, lichen planopilaris, and various types of pruritus (ie, aquagenic, cholestatic, uremic, atopic dermatitis related).3 A case report of LDN successfully treating a patient with psoriasis also has been published.6 We often use LDN at the University of Wisconsin (Madison, Wisconsin) to treat patients with psoriasis. Ekelem et al3 also discussed patients with skin conditions that either had no response or worsened with naltrexone treatment, including various types of pruritus (ie, uremic, mycosis fungoides related, other causes of pruritus). Importantly, in the majority of cases without an improved response, the dose used was 50 mg/d.3 Higher doses of naltrexone are not known to have anti-inflammatory effects.
Low-dose naltrexone can be considered as a treatment option in patients with contraindications to other systemic anti-inflammatory treatments; for example, patients with a history of malignancy may prefer to avoid treatment with biologic agents. Low-dose naltrexone also can be considered as a treatment option in patients who are uncomfortable with the side-effect profiles of other systemic anti-inflammatory treatments, such as the risk for leukemias and lymphomas associated with biologic agents, the risk for liver toxicity with methotrexate, or the risk for hyperlipidemia with acitretin.
How to Monitor
The following monitoring information is adapted from the practice of Apple Bodemer, MD, a board-certified dermatologist at the University of Wisconsin (Madison, Wisconsin) who also is fellowship trained in integrative medicine.
There is a paucity of published data about LDN dosing for inflammatory skin diseases. However, prescribers should be aware that LDN can alter thyroid hormone levels, especially in patients with autoimmune thyroid disease. If a thyroid-stimulating hormone (TSH) level within reference range has not been noted in the last year, consider screening with a TSH test and also assessing for a personal or family history of thyroid disease. If the TSH level is within reference range, there generally is no need to monitor while treating with LDN. Consider checking TSH levels every 4 months in patients with thyroid disease while they are on LDN therapy and be sure to educate them about symptoms of hyperthyroidism.
Side Effects
Low-dose naltrexone has a minimal side-effect profile with self-limited side effects that often resolve within approximately 1 week. One of the most commonly reported side effects is sleep disturbance with vivid dreams, which has been reported in 37% of participants.1 If your patients experience this side effect, you can reassure them that it improves with time. You also can switch to morning dosing to try and alleviate sleep disturbances at night. Another possible side effect is gastrointestinal tract upset. Importantly, there is no known abuse potential for LDN.1 To stop LDN, patients should be stable for 6 to 12 months, and there is no need to wean them off it.
Cost and Availability
Because use of LDN in dermatology is considered off label and it is not approved by the US Food and Drug Administration to treat any medical conditions, it must be prescribed through a compounding pharmacy, usually without insurance coverage. The monthly cost is approximately $30 depending on the pharmacy (unpublished data), which may be cost prohibitive for patients, so it is important to counsel them about price
Final Thoughts
Low-dose naltrexone is an alternative treatment option that can be considered in patients with inflammatory skin diseases. It has a favorable side-effect profile, especially compared to other systemic anti-inflammatory agents; however, additional studies are needed to learn more about its safety and efficacy. If patients ask you about LDN, the information provided here can guide you with how it works and how to prescribe it.
- Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014;33:451-459.
- Brown N, Panksepp J. Low-dose naltrexone for disease prevention and quality of life. Med Hypotheses. 2009;72:333-337.
- Ekelem C, Juhasz M, Khera P, et al. Utility of naltrexone treatment for chronic inflammatory dermatologic conditions: a systematic review. JAMA Dermatol. 2019;155:229-236.
- Bihari B. Efficacy of low dose naltrexone as an immune stabilizing agent for the treatment of HIV/AIDS. AIDS Patient Care. 1995;9:3.
- Lee B, Elston DM. The uses of naltrexone in dermatologic conditions [published online December 21, 2018]. J Am Acad Dermatol. 2019;80:1746-1752.
- Bridgman AC, Kirchhof MG. Treatment of psoriasis vulgaris using low-dose naltrexone. JAAD Case Rep. 2018;4:827-829.
- Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014;33:451-459.
- Brown N, Panksepp J. Low-dose naltrexone for disease prevention and quality of life. Med Hypotheses. 2009;72:333-337.
- Ekelem C, Juhasz M, Khera P, et al. Utility of naltrexone treatment for chronic inflammatory dermatologic conditions: a systematic review. JAMA Dermatol. 2019;155:229-236.
- Bihari B. Efficacy of low dose naltrexone as an immune stabilizing agent for the treatment of HIV/AIDS. AIDS Patient Care. 1995;9:3.
- Lee B, Elston DM. The uses of naltrexone in dermatologic conditions [published online December 21, 2018]. J Am Acad Dermatol. 2019;80:1746-1752.
- Bridgman AC, Kirchhof MG. Treatment of psoriasis vulgaris using low-dose naltrexone. JAAD Case Rep. 2018;4:827-829.
Resident Pearl
- Low-dose naltrexone is an alternative antiinflammatory treatment to consider in patients with inflammatory skin diseases, with a minimal side-effect profile.
Adding lymphopenia component ‘improves’ FLIPI
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
FROM BLOOD CANCER JOURNAL
Infant deaths from birth defects decline, but some disparities widen
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
FROM MMWR
AFib link with titin mutations warrants selected genetic testing
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
REPORTING FROM THE AF SYMPOSIUM 2020
Hospitalist movers and shakers – January 2020
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.