User login
Neutrophils may decline in patients on fingolimod
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
REPORTING FROM CMSC 2019
Being a leader in medicine doesn’t have to mean changing careers
About once a week, along with all the other junk mail, I get a glossy brochure for some university’s online courses to “become a leader in medicine.”
They extol the virtues of their programs: How they equip me to “change the health care system,” “harness market forces to improve medical care,” “empower the next generation of physicians,” and other statements that were almost certainly not written by a doctor.
I’m sure some people are interested in this sort of thing. Maybe they’re ready for a career change from the exam room to the boardroom. But me? I have, pretty much, zero desire to do that. I don’t want to be a corporate leader in medicine. I didn’t come here to sit at a table and watch PowerPoint slides. I didn’t work to get into, and through, medical school, residency, and fellowship to debate earnings ratios and procedure costs with accountants.
I’m here for the patients. I’m sure there are some who became attending physicians, realized this wasn’t for them, and went off to do something else. That’s fine. I have nothing against it.
But, after 20 years in practice, I’m happy where I am. Like most others, I wish I made more money, or that my overhead was less, but I’m overall content with my little world. I have a great staff, a relaxed office, and the majority of my patients are good people.
I have no interest in trading that to be a leader in medicine. In the game of trying to make the world a better place, I’ve found my calling. I can do good for others far more effectively at my second-floor office than in a corporate tower.
And if doing my best for patients day in and day out doesn’t make me a leader in medicine, I don’t know what does.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
About once a week, along with all the other junk mail, I get a glossy brochure for some university’s online courses to “become a leader in medicine.”
They extol the virtues of their programs: How they equip me to “change the health care system,” “harness market forces to improve medical care,” “empower the next generation of physicians,” and other statements that were almost certainly not written by a doctor.
I’m sure some people are interested in this sort of thing. Maybe they’re ready for a career change from the exam room to the boardroom. But me? I have, pretty much, zero desire to do that. I don’t want to be a corporate leader in medicine. I didn’t come here to sit at a table and watch PowerPoint slides. I didn’t work to get into, and through, medical school, residency, and fellowship to debate earnings ratios and procedure costs with accountants.
I’m here for the patients. I’m sure there are some who became attending physicians, realized this wasn’t for them, and went off to do something else. That’s fine. I have nothing against it.
But, after 20 years in practice, I’m happy where I am. Like most others, I wish I made more money, or that my overhead was less, but I’m overall content with my little world. I have a great staff, a relaxed office, and the majority of my patients are good people.
I have no interest in trading that to be a leader in medicine. In the game of trying to make the world a better place, I’ve found my calling. I can do good for others far more effectively at my second-floor office than in a corporate tower.
And if doing my best for patients day in and day out doesn’t make me a leader in medicine, I don’t know what does.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
About once a week, along with all the other junk mail, I get a glossy brochure for some university’s online courses to “become a leader in medicine.”
They extol the virtues of their programs: How they equip me to “change the health care system,” “harness market forces to improve medical care,” “empower the next generation of physicians,” and other statements that were almost certainly not written by a doctor.
I’m sure some people are interested in this sort of thing. Maybe they’re ready for a career change from the exam room to the boardroom. But me? I have, pretty much, zero desire to do that. I don’t want to be a corporate leader in medicine. I didn’t come here to sit at a table and watch PowerPoint slides. I didn’t work to get into, and through, medical school, residency, and fellowship to debate earnings ratios and procedure costs with accountants.
I’m here for the patients. I’m sure there are some who became attending physicians, realized this wasn’t for them, and went off to do something else. That’s fine. I have nothing against it.
But, after 20 years in practice, I’m happy where I am. Like most others, I wish I made more money, or that my overhead was less, but I’m overall content with my little world. I have a great staff, a relaxed office, and the majority of my patients are good people.
I have no interest in trading that to be a leader in medicine. In the game of trying to make the world a better place, I’ve found my calling. I can do good for others far more effectively at my second-floor office than in a corporate tower.
And if doing my best for patients day in and day out doesn’t make me a leader in medicine, I don’t know what does.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
rFVIII product shows better PK profile than rFVIIIFc
The recombinant factor VIII (rFVIII) product BAY 94‐9027 had a better pharmacokinetic (PK) profile than a recombinant factor VIII-Fc fusion protein (rFVIIIFc) in patients with hemophilia A, according to a recent report.
“The objective of the current study was to directly compare the PK profiles of BAY 94-9027 and rFVIIIFc,” wrote Anita Shah, lead author and an employee of Bayer, and colleagues. The findings were published in the Annals of Hematology.
In a two-way PK crossover study, adults (aged 18-65 years) with severe hemophilia A were randomized to receive a single intravenous dose (60 IU/kg) of BAY 94-9027 or rFVIIIFc. These infusions were followed by a crossover to a single infusion of the other product.
The maximum wash-out period between infusions was 28 days, with a greater than or equal to 7-day wash-out between doses. FVIII activity was analyzed using a single one-stage clotting assay.
After population PK modeling, the median time to achieve FVIII threshold levels (1 IU/dL) was found to be 13 hours longer for BAY 94-9027 than it was for rFVIIIFc following a single intravenous dose of 60 IU/kg.
In addition, the team reported that the geometric mean area under the curve from baseline to the last data point was significantly greater for BAY 94-9027 than it was for rFVIIIFc (coefficient of variation, 2,940 vs. 2,360 IU h/dL; P = .0001)
“This increase in the time above threshold may thereby provide improved bleeding protection,” the authors explained.
With respect to safety, no adverse events were reported among study participants.
The researchers acknowledged a key limitation of the study was the nonexistence of a two-stage chromogenic assay to measure FVIII activity of both products. As a result, a one-stage clotting assay was used to analyze FVIII activity for both treatments.
“Real-world data may provide an insight into whether these PK advantages provide additional bleeding protection,” they concluded.
The study was funded by Bayer AG. The authors reported financial affiliations with Bayer, LFB, Octapharma, Pfizer, Roche, Shire, and several others.
SOURCE: Shah A et al. Ann Hematol. 2019 Jun 24. doi: 10.1007/s00277-019-03747-2.
The recombinant factor VIII (rFVIII) product BAY 94‐9027 had a better pharmacokinetic (PK) profile than a recombinant factor VIII-Fc fusion protein (rFVIIIFc) in patients with hemophilia A, according to a recent report.
“The objective of the current study was to directly compare the PK profiles of BAY 94-9027 and rFVIIIFc,” wrote Anita Shah, lead author and an employee of Bayer, and colleagues. The findings were published in the Annals of Hematology.
In a two-way PK crossover study, adults (aged 18-65 years) with severe hemophilia A were randomized to receive a single intravenous dose (60 IU/kg) of BAY 94-9027 or rFVIIIFc. These infusions were followed by a crossover to a single infusion of the other product.
The maximum wash-out period between infusions was 28 days, with a greater than or equal to 7-day wash-out between doses. FVIII activity was analyzed using a single one-stage clotting assay.
After population PK modeling, the median time to achieve FVIII threshold levels (1 IU/dL) was found to be 13 hours longer for BAY 94-9027 than it was for rFVIIIFc following a single intravenous dose of 60 IU/kg.
In addition, the team reported that the geometric mean area under the curve from baseline to the last data point was significantly greater for BAY 94-9027 than it was for rFVIIIFc (coefficient of variation, 2,940 vs. 2,360 IU h/dL; P = .0001)
“This increase in the time above threshold may thereby provide improved bleeding protection,” the authors explained.
With respect to safety, no adverse events were reported among study participants.
The researchers acknowledged a key limitation of the study was the nonexistence of a two-stage chromogenic assay to measure FVIII activity of both products. As a result, a one-stage clotting assay was used to analyze FVIII activity for both treatments.
“Real-world data may provide an insight into whether these PK advantages provide additional bleeding protection,” they concluded.
The study was funded by Bayer AG. The authors reported financial affiliations with Bayer, LFB, Octapharma, Pfizer, Roche, Shire, and several others.
SOURCE: Shah A et al. Ann Hematol. 2019 Jun 24. doi: 10.1007/s00277-019-03747-2.
The recombinant factor VIII (rFVIII) product BAY 94‐9027 had a better pharmacokinetic (PK) profile than a recombinant factor VIII-Fc fusion protein (rFVIIIFc) in patients with hemophilia A, according to a recent report.
“The objective of the current study was to directly compare the PK profiles of BAY 94-9027 and rFVIIIFc,” wrote Anita Shah, lead author and an employee of Bayer, and colleagues. The findings were published in the Annals of Hematology.
In a two-way PK crossover study, adults (aged 18-65 years) with severe hemophilia A were randomized to receive a single intravenous dose (60 IU/kg) of BAY 94-9027 or rFVIIIFc. These infusions were followed by a crossover to a single infusion of the other product.
The maximum wash-out period between infusions was 28 days, with a greater than or equal to 7-day wash-out between doses. FVIII activity was analyzed using a single one-stage clotting assay.
After population PK modeling, the median time to achieve FVIII threshold levels (1 IU/dL) was found to be 13 hours longer for BAY 94-9027 than it was for rFVIIIFc following a single intravenous dose of 60 IU/kg.
In addition, the team reported that the geometric mean area under the curve from baseline to the last data point was significantly greater for BAY 94-9027 than it was for rFVIIIFc (coefficient of variation, 2,940 vs. 2,360 IU h/dL; P = .0001)
“This increase in the time above threshold may thereby provide improved bleeding protection,” the authors explained.
With respect to safety, no adverse events were reported among study participants.
The researchers acknowledged a key limitation of the study was the nonexistence of a two-stage chromogenic assay to measure FVIII activity of both products. As a result, a one-stage clotting assay was used to analyze FVIII activity for both treatments.
“Real-world data may provide an insight into whether these PK advantages provide additional bleeding protection,” they concluded.
The study was funded by Bayer AG. The authors reported financial affiliations with Bayer, LFB, Octapharma, Pfizer, Roche, Shire, and several others.
SOURCE: Shah A et al. Ann Hematol. 2019 Jun 24. doi: 10.1007/s00277-019-03747-2.
FROM ANNALS OF HEMATOLOGY
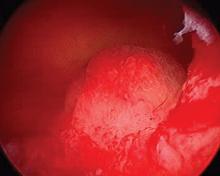
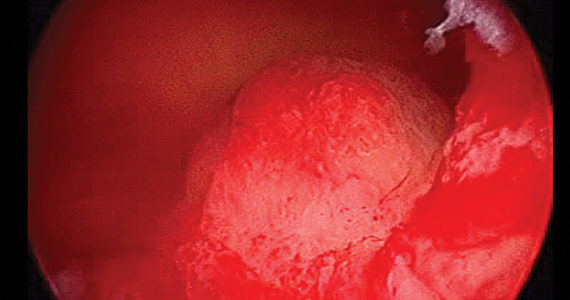
Underwater endoscopic mucosal resection may be an option for colorectal lesions
without increasing procedure time or risk of adverse events, based on a recent head-to-head trial conducted in Japan.
UEMR was associated with higher R0 and en bloc resection rates than was conventional EMR (CEMR) when used for intermediate-size colorectal lesions, reported lead author Takeshi Yamashina, MD, of Osaka (Japan) International Cancer Institute, and colleagues. The study was the first multicenter, randomized trial to demonstrate the superiority of UEMR over CEMR, they noted.
Although CEMR is a well-established method of removing sessile colorectal lesions, those larger than 10 mm can be difficult to resect en bloc, which contributes to a local recurrence rate exceeding 15% when alternative, piecemeal resection is performed, the investigators explained in Gastroenterology
Recently, UEMR has emerged as “an alternative to CEMR and is reported to be effective for removing flat or large colorectal polyps,” the investigators wrote. “With UEMR, the bowel lumen is filled with water instead of air/CO2, and the lesion is captured and resected with a snare without submucosal injection of normal saline.”
To find out if UEMR offers better results than CEMR, the investigators recruited 211 patients with 214 colorectal lesions at five centers in Japan. Patients were aged at least 20 years and had mucosal lesions of 10-20 mm in diameter. Based on macroscopic appearance, pit pattern classification with magnifying chromoendoscopy, or narrow-band imaging, lesions were classified as adenoma, sessile serrated adenoma/polyp, or intramucosal adenocarcinoma. Patients were randomly assigned in a 1:1 ratio to the UEMR or CEMR group, and just prior to the procedure, operators were informed of the allocated treatment. Ten expert operators were involved, each with at least 10 years of experience, in addition to 18 nonexpert operators with less than 10 years of experience. The primary endpoint was the difference in R0 resection rate between the two groups, with R0 defined as en bloc resection with histologically negative margins. Secondary endpoints were en bloc resection rate, adverse events, and procedure time.
The results showed a clear win for UEMR, with an R0 rate of 69%, compared with 50% for CEMR (P = .011), and an en bloc resection rate that followed the same trend (89% vs. 75%; P = .007). Neither median procedure times nor number of adverse events were significantly different between groups.
Subset analysis showed that UEMR was best suited for lesions at least 15 mm in diameter, although the investigators pointed out the superior R0 resection rate with UEMR held steady regardless of lesion morphology, size, location, or operator experience level.
The investigators suggested that the findings give reason to amend some existing recommendations. “Although the European Society of Gastrointestinal Endoscopy Clinical Guidelines suggest hot-snare polypectomy with submucosal injection for removing sessile polyps 10-19 mm in size, we found that UEMR was more effective than CEMR, in terms of better R0 and en bloc resection rates,” they wrote. “Hence, we think that UEMR will become an alternative to CEMR. It could fill the gap for removing polyps 9 mm [or larger] (indication for removal by cold-snare polypectomy) and [smaller than] 20 mm (indication for ESD removal).”
During the discussion, the investigators explained that UEMR achieves better outcomes primarily by improving access to lesions. Water immersion causes lesions to float upright into the lumen, while keeping the muscularis propria circular behind the submucosa, which allows for easier snaring and decreases risk of perforation. Furthermore, the investigators noted, water immersion limits flexure angulation, luminal distension, and loop formation, all of which improve maneuverability and visibility.
Still, UEMR may take some operator adjustment, the investigators added, going on to provide some pointers. “In practice, we think it is important to fill the entire lumen only with fluid, so we always deflate the lumen completely and then fill it with fluid,” they wrote. “[When the lumen is filled], it is not necessary to change the patient’s position during the UEMR procedure.”
“Also, in cases with unclear endoscopic vision, endoscopists are familiar with air insufflation but, during UEMR, it is better to infuse the fluid to expand the lumen and maintain a good endoscopic view. Therefore, for the beginner, we recommend that the air insufflation button of the endoscopy machine be switched off.”
Additional tips included using saline instead of distilled water, and employing thin, soft snares.
The investigators reported no external funding or conflicts of interest.
SOURCE: Yamashina T et al. Gastro. 2018 Apr 11. doi: 10.1053/j.gastro.2019.04.005.
without increasing procedure time or risk of adverse events, based on a recent head-to-head trial conducted in Japan.
UEMR was associated with higher R0 and en bloc resection rates than was conventional EMR (CEMR) when used for intermediate-size colorectal lesions, reported lead author Takeshi Yamashina, MD, of Osaka (Japan) International Cancer Institute, and colleagues. The study was the first multicenter, randomized trial to demonstrate the superiority of UEMR over CEMR, they noted.
Although CEMR is a well-established method of removing sessile colorectal lesions, those larger than 10 mm can be difficult to resect en bloc, which contributes to a local recurrence rate exceeding 15% when alternative, piecemeal resection is performed, the investigators explained in Gastroenterology
Recently, UEMR has emerged as “an alternative to CEMR and is reported to be effective for removing flat or large colorectal polyps,” the investigators wrote. “With UEMR, the bowel lumen is filled with water instead of air/CO2, and the lesion is captured and resected with a snare without submucosal injection of normal saline.”
To find out if UEMR offers better results than CEMR, the investigators recruited 211 patients with 214 colorectal lesions at five centers in Japan. Patients were aged at least 20 years and had mucosal lesions of 10-20 mm in diameter. Based on macroscopic appearance, pit pattern classification with magnifying chromoendoscopy, or narrow-band imaging, lesions were classified as adenoma, sessile serrated adenoma/polyp, or intramucosal adenocarcinoma. Patients were randomly assigned in a 1:1 ratio to the UEMR or CEMR group, and just prior to the procedure, operators were informed of the allocated treatment. Ten expert operators were involved, each with at least 10 years of experience, in addition to 18 nonexpert operators with less than 10 years of experience. The primary endpoint was the difference in R0 resection rate between the two groups, with R0 defined as en bloc resection with histologically negative margins. Secondary endpoints were en bloc resection rate, adverse events, and procedure time.
The results showed a clear win for UEMR, with an R0 rate of 69%, compared with 50% for CEMR (P = .011), and an en bloc resection rate that followed the same trend (89% vs. 75%; P = .007). Neither median procedure times nor number of adverse events were significantly different between groups.
Subset analysis showed that UEMR was best suited for lesions at least 15 mm in diameter, although the investigators pointed out the superior R0 resection rate with UEMR held steady regardless of lesion morphology, size, location, or operator experience level.
The investigators suggested that the findings give reason to amend some existing recommendations. “Although the European Society of Gastrointestinal Endoscopy Clinical Guidelines suggest hot-snare polypectomy with submucosal injection for removing sessile polyps 10-19 mm in size, we found that UEMR was more effective than CEMR, in terms of better R0 and en bloc resection rates,” they wrote. “Hence, we think that UEMR will become an alternative to CEMR. It could fill the gap for removing polyps 9 mm [or larger] (indication for removal by cold-snare polypectomy) and [smaller than] 20 mm (indication for ESD removal).”
During the discussion, the investigators explained that UEMR achieves better outcomes primarily by improving access to lesions. Water immersion causes lesions to float upright into the lumen, while keeping the muscularis propria circular behind the submucosa, which allows for easier snaring and decreases risk of perforation. Furthermore, the investigators noted, water immersion limits flexure angulation, luminal distension, and loop formation, all of which improve maneuverability and visibility.
Still, UEMR may take some operator adjustment, the investigators added, going on to provide some pointers. “In practice, we think it is important to fill the entire lumen only with fluid, so we always deflate the lumen completely and then fill it with fluid,” they wrote. “[When the lumen is filled], it is not necessary to change the patient’s position during the UEMR procedure.”
“Also, in cases with unclear endoscopic vision, endoscopists are familiar with air insufflation but, during UEMR, it is better to infuse the fluid to expand the lumen and maintain a good endoscopic view. Therefore, for the beginner, we recommend that the air insufflation button of the endoscopy machine be switched off.”
Additional tips included using saline instead of distilled water, and employing thin, soft snares.
The investigators reported no external funding or conflicts of interest.
SOURCE: Yamashina T et al. Gastro. 2018 Apr 11. doi: 10.1053/j.gastro.2019.04.005.
without increasing procedure time or risk of adverse events, based on a recent head-to-head trial conducted in Japan.
UEMR was associated with higher R0 and en bloc resection rates than was conventional EMR (CEMR) when used for intermediate-size colorectal lesions, reported lead author Takeshi Yamashina, MD, of Osaka (Japan) International Cancer Institute, and colleagues. The study was the first multicenter, randomized trial to demonstrate the superiority of UEMR over CEMR, they noted.
Although CEMR is a well-established method of removing sessile colorectal lesions, those larger than 10 mm can be difficult to resect en bloc, which contributes to a local recurrence rate exceeding 15% when alternative, piecemeal resection is performed, the investigators explained in Gastroenterology
Recently, UEMR has emerged as “an alternative to CEMR and is reported to be effective for removing flat or large colorectal polyps,” the investigators wrote. “With UEMR, the bowel lumen is filled with water instead of air/CO2, and the lesion is captured and resected with a snare without submucosal injection of normal saline.”
To find out if UEMR offers better results than CEMR, the investigators recruited 211 patients with 214 colorectal lesions at five centers in Japan. Patients were aged at least 20 years and had mucosal lesions of 10-20 mm in diameter. Based on macroscopic appearance, pit pattern classification with magnifying chromoendoscopy, or narrow-band imaging, lesions were classified as adenoma, sessile serrated adenoma/polyp, or intramucosal adenocarcinoma. Patients were randomly assigned in a 1:1 ratio to the UEMR or CEMR group, and just prior to the procedure, operators were informed of the allocated treatment. Ten expert operators were involved, each with at least 10 years of experience, in addition to 18 nonexpert operators with less than 10 years of experience. The primary endpoint was the difference in R0 resection rate between the two groups, with R0 defined as en bloc resection with histologically negative margins. Secondary endpoints were en bloc resection rate, adverse events, and procedure time.
The results showed a clear win for UEMR, with an R0 rate of 69%, compared with 50% for CEMR (P = .011), and an en bloc resection rate that followed the same trend (89% vs. 75%; P = .007). Neither median procedure times nor number of adverse events were significantly different between groups.
Subset analysis showed that UEMR was best suited for lesions at least 15 mm in diameter, although the investigators pointed out the superior R0 resection rate with UEMR held steady regardless of lesion morphology, size, location, or operator experience level.
The investigators suggested that the findings give reason to amend some existing recommendations. “Although the European Society of Gastrointestinal Endoscopy Clinical Guidelines suggest hot-snare polypectomy with submucosal injection for removing sessile polyps 10-19 mm in size, we found that UEMR was more effective than CEMR, in terms of better R0 and en bloc resection rates,” they wrote. “Hence, we think that UEMR will become an alternative to CEMR. It could fill the gap for removing polyps 9 mm [or larger] (indication for removal by cold-snare polypectomy) and [smaller than] 20 mm (indication for ESD removal).”
During the discussion, the investigators explained that UEMR achieves better outcomes primarily by improving access to lesions. Water immersion causes lesions to float upright into the lumen, while keeping the muscularis propria circular behind the submucosa, which allows for easier snaring and decreases risk of perforation. Furthermore, the investigators noted, water immersion limits flexure angulation, luminal distension, and loop formation, all of which improve maneuverability and visibility.
Still, UEMR may take some operator adjustment, the investigators added, going on to provide some pointers. “In practice, we think it is important to fill the entire lumen only with fluid, so we always deflate the lumen completely and then fill it with fluid,” they wrote. “[When the lumen is filled], it is not necessary to change the patient’s position during the UEMR procedure.”
“Also, in cases with unclear endoscopic vision, endoscopists are familiar with air insufflation but, during UEMR, it is better to infuse the fluid to expand the lumen and maintain a good endoscopic view. Therefore, for the beginner, we recommend that the air insufflation button of the endoscopy machine be switched off.”
Additional tips included using saline instead of distilled water, and employing thin, soft snares.
The investigators reported no external funding or conflicts of interest.
SOURCE: Yamashina T et al. Gastro. 2018 Apr 11. doi: 10.1053/j.gastro.2019.04.005.
FROM GASTROENTEROLOGY
Unacceptable pain despite inflammation control commonly occurs in PsA patients
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
REPORTING FROM EULAR 2019 CONGRESS
Legislative, educational interventions influenced vaccine status of California kindergartners
After California lawmakers implemented policies to limit and eventually eliminate nonmedical exemptions for childhood vaccinations, the proportion of kindergartners who were not up to date for recommended vaccinations fell from 10% in 2013 to 5% in 2017.
At the same time, the
The findings come from an observational study that used cross-sectional school-entry data from 2000 to 2017 to calculate the rates of kindergartners attending California schools who were not up to date on required vaccinations.
“Large-scale vaccination programs that included school-entry mandates have been essential to maintaining high levels of immunization coverage and low rates of vaccine-preventable diseases,” researchers led by S. Cassandra Pingali, MPH, MS, wrote in JAMA. “However, an increasing number of parents are not vaccinating their children over concerns about potential adverse effects. These parental actions threaten the herd immunity established by decades of high vaccine uptake and increase the potential for disease outbreaks.”
Ms. Pingali, of the department of epidemiology at Emory University, Atlanta, and colleagues conducted an observational analysis of California kindergartners who were not up to date on one or more of the required vaccinations during the course of three interventions implemented in the state. The first was Assembly Bill 2109 (AB 2109), which was passed in 2014. It required parents to show proof they had discussed the risks of not vaccinating their children with a health care practitioner before they obtained a personal belief exemption. The second intervention was a campaign carried out in 2015 by the California Department of Public Health and local health departments, designed to educate school staff on the proper application of the conditional admission criteria, which allowed students additional time to catch up on vaccination. The third intervention was the implementation of Senate bill 277 (SB 277), which banned all personal belief exemptions.
Between 2000 and 2017, the researchers reported that the yearly mean kindergarten enrollment in California was 517,962 and the mean number of schools was 7,278. Over this time, the yearly rate of students without up-to-date vaccination status rose from 8% during 2000 to 10% during 2013, before decreasing to 5% during 2017. Ms. Pingali and associates also found that average percentage chance of any within-school contact for a student without up-to-date vaccination status with another student with the same status was 19% during 2000, and increased steadily to 26% during 2014, the first year of AB 2109. The values decreased to 3% (the first year of SB 277), before increasing slightly to 5% during 2017.
“Across the interventions, the percentage of kindergartners attending schools with an up-to-date vaccination status percentage that was greater than the herd immunity threshold also increased for various vaccine-preventable diseases,” the researchers wrote. “Overall, the results suggest that the risk of disease outbreak via potential contact among susceptible children decreased over the course of the interventions.”
The way Matthew M. Davis, MD and Seema K. Shah, JD, see it, the current outbreak of measles in the United States is rooted in the failure of parents to vaccinate their children against the disease based on their beliefs rather than medical contraindications.
“The public health implications of such decisions are amplified because parents who share belief systems about childhood vaccinations tend to congregate socially and residentially, thereby forming clusters of unvaccinated children who are at elevated health risks when exposed to vaccine-preventable diseases,” the authors wrote in an accompanying editorial.
While the study reported by Pingali et al. did not measure actual outbreaks of disease, “reductions in children’s risk of contracting measles are a promising outcome in California resulting from policy changes,” wrote Dr. Davis and Ms. Shah, both of Northwestern University, Chicago (JAMA. 2019;322[1]:33-4). “Yet, because of the ease of domestic and international travel, the mobile nature of young families, and the inability of all states to implement this approach, changes made in each state for nonmedical exemptions may not ensure sufficiently high protection against measles for children across all jurisdictions in the United States. Although states have historically made their own decisions about vaccination exemptions linked to day care or school entry because states exercise primary authority over educational matters, childhood vaccination is a national matter in many respects.”
The best way to remedy the current system failure regarding measles vaccination, they continued, may be to adopt a unified national approach to prohibit nonmedical exemptions. They pointed to the fact that the United States previously achieved virtual eradication of measles as recently as 2000. “Following that achievement, state-level policy changes relaxed immunization requirements and set the stage for progressively larger outbreaks in the United States in recent years. Such system failures result when the products, processes, and people (including the public) that comprise systems do not function or behave in ways that protect health optimally.”
The study was supported by a grant from the National Institutes of Health. One coauthor reported having received consulting fees from Merck and grants from Pfizer and Walgreens. Another reported receiving grants from Pfizer, Merck, GlaxoSmithKline, Sanofi Pasteur, Protein Science, Dynavax, and MedImmune. The remaining coauthors reported no relevant financial disclosures.
The editorialists reported having no financial disclosures.
SOURCE: Pingali SC et al. JAMA. 2019 Jul 2. doi: 10.1001/jama.2019.7924.
After California lawmakers implemented policies to limit and eventually eliminate nonmedical exemptions for childhood vaccinations, the proportion of kindergartners who were not up to date for recommended vaccinations fell from 10% in 2013 to 5% in 2017.
At the same time, the
The findings come from an observational study that used cross-sectional school-entry data from 2000 to 2017 to calculate the rates of kindergartners attending California schools who were not up to date on required vaccinations.
“Large-scale vaccination programs that included school-entry mandates have been essential to maintaining high levels of immunization coverage and low rates of vaccine-preventable diseases,” researchers led by S. Cassandra Pingali, MPH, MS, wrote in JAMA. “However, an increasing number of parents are not vaccinating their children over concerns about potential adverse effects. These parental actions threaten the herd immunity established by decades of high vaccine uptake and increase the potential for disease outbreaks.”
Ms. Pingali, of the department of epidemiology at Emory University, Atlanta, and colleagues conducted an observational analysis of California kindergartners who were not up to date on one or more of the required vaccinations during the course of three interventions implemented in the state. The first was Assembly Bill 2109 (AB 2109), which was passed in 2014. It required parents to show proof they had discussed the risks of not vaccinating their children with a health care practitioner before they obtained a personal belief exemption. The second intervention was a campaign carried out in 2015 by the California Department of Public Health and local health departments, designed to educate school staff on the proper application of the conditional admission criteria, which allowed students additional time to catch up on vaccination. The third intervention was the implementation of Senate bill 277 (SB 277), which banned all personal belief exemptions.
Between 2000 and 2017, the researchers reported that the yearly mean kindergarten enrollment in California was 517,962 and the mean number of schools was 7,278. Over this time, the yearly rate of students without up-to-date vaccination status rose from 8% during 2000 to 10% during 2013, before decreasing to 5% during 2017. Ms. Pingali and associates also found that average percentage chance of any within-school contact for a student without up-to-date vaccination status with another student with the same status was 19% during 2000, and increased steadily to 26% during 2014, the first year of AB 2109. The values decreased to 3% (the first year of SB 277), before increasing slightly to 5% during 2017.
“Across the interventions, the percentage of kindergartners attending schools with an up-to-date vaccination status percentage that was greater than the herd immunity threshold also increased for various vaccine-preventable diseases,” the researchers wrote. “Overall, the results suggest that the risk of disease outbreak via potential contact among susceptible children decreased over the course of the interventions.”
The way Matthew M. Davis, MD and Seema K. Shah, JD, see it, the current outbreak of measles in the United States is rooted in the failure of parents to vaccinate their children against the disease based on their beliefs rather than medical contraindications.
“The public health implications of such decisions are amplified because parents who share belief systems about childhood vaccinations tend to congregate socially and residentially, thereby forming clusters of unvaccinated children who are at elevated health risks when exposed to vaccine-preventable diseases,” the authors wrote in an accompanying editorial.
While the study reported by Pingali et al. did not measure actual outbreaks of disease, “reductions in children’s risk of contracting measles are a promising outcome in California resulting from policy changes,” wrote Dr. Davis and Ms. Shah, both of Northwestern University, Chicago (JAMA. 2019;322[1]:33-4). “Yet, because of the ease of domestic and international travel, the mobile nature of young families, and the inability of all states to implement this approach, changes made in each state for nonmedical exemptions may not ensure sufficiently high protection against measles for children across all jurisdictions in the United States. Although states have historically made their own decisions about vaccination exemptions linked to day care or school entry because states exercise primary authority over educational matters, childhood vaccination is a national matter in many respects.”
The best way to remedy the current system failure regarding measles vaccination, they continued, may be to adopt a unified national approach to prohibit nonmedical exemptions. They pointed to the fact that the United States previously achieved virtual eradication of measles as recently as 2000. “Following that achievement, state-level policy changes relaxed immunization requirements and set the stage for progressively larger outbreaks in the United States in recent years. Such system failures result when the products, processes, and people (including the public) that comprise systems do not function or behave in ways that protect health optimally.”
The study was supported by a grant from the National Institutes of Health. One coauthor reported having received consulting fees from Merck and grants from Pfizer and Walgreens. Another reported receiving grants from Pfizer, Merck, GlaxoSmithKline, Sanofi Pasteur, Protein Science, Dynavax, and MedImmune. The remaining coauthors reported no relevant financial disclosures.
The editorialists reported having no financial disclosures.
SOURCE: Pingali SC et al. JAMA. 2019 Jul 2. doi: 10.1001/jama.2019.7924.
After California lawmakers implemented policies to limit and eventually eliminate nonmedical exemptions for childhood vaccinations, the proportion of kindergartners who were not up to date for recommended vaccinations fell from 10% in 2013 to 5% in 2017.
At the same time, the
The findings come from an observational study that used cross-sectional school-entry data from 2000 to 2017 to calculate the rates of kindergartners attending California schools who were not up to date on required vaccinations.
“Large-scale vaccination programs that included school-entry mandates have been essential to maintaining high levels of immunization coverage and low rates of vaccine-preventable diseases,” researchers led by S. Cassandra Pingali, MPH, MS, wrote in JAMA. “However, an increasing number of parents are not vaccinating their children over concerns about potential adverse effects. These parental actions threaten the herd immunity established by decades of high vaccine uptake and increase the potential for disease outbreaks.”
Ms. Pingali, of the department of epidemiology at Emory University, Atlanta, and colleagues conducted an observational analysis of California kindergartners who were not up to date on one or more of the required vaccinations during the course of three interventions implemented in the state. The first was Assembly Bill 2109 (AB 2109), which was passed in 2014. It required parents to show proof they had discussed the risks of not vaccinating their children with a health care practitioner before they obtained a personal belief exemption. The second intervention was a campaign carried out in 2015 by the California Department of Public Health and local health departments, designed to educate school staff on the proper application of the conditional admission criteria, which allowed students additional time to catch up on vaccination. The third intervention was the implementation of Senate bill 277 (SB 277), which banned all personal belief exemptions.
Between 2000 and 2017, the researchers reported that the yearly mean kindergarten enrollment in California was 517,962 and the mean number of schools was 7,278. Over this time, the yearly rate of students without up-to-date vaccination status rose from 8% during 2000 to 10% during 2013, before decreasing to 5% during 2017. Ms. Pingali and associates also found that average percentage chance of any within-school contact for a student without up-to-date vaccination status with another student with the same status was 19% during 2000, and increased steadily to 26% during 2014, the first year of AB 2109. The values decreased to 3% (the first year of SB 277), before increasing slightly to 5% during 2017.
“Across the interventions, the percentage of kindergartners attending schools with an up-to-date vaccination status percentage that was greater than the herd immunity threshold also increased for various vaccine-preventable diseases,” the researchers wrote. “Overall, the results suggest that the risk of disease outbreak via potential contact among susceptible children decreased over the course of the interventions.”
The way Matthew M. Davis, MD and Seema K. Shah, JD, see it, the current outbreak of measles in the United States is rooted in the failure of parents to vaccinate their children against the disease based on their beliefs rather than medical contraindications.
“The public health implications of such decisions are amplified because parents who share belief systems about childhood vaccinations tend to congregate socially and residentially, thereby forming clusters of unvaccinated children who are at elevated health risks when exposed to vaccine-preventable diseases,” the authors wrote in an accompanying editorial.
While the study reported by Pingali et al. did not measure actual outbreaks of disease, “reductions in children’s risk of contracting measles are a promising outcome in California resulting from policy changes,” wrote Dr. Davis and Ms. Shah, both of Northwestern University, Chicago (JAMA. 2019;322[1]:33-4). “Yet, because of the ease of domestic and international travel, the mobile nature of young families, and the inability of all states to implement this approach, changes made in each state for nonmedical exemptions may not ensure sufficiently high protection against measles for children across all jurisdictions in the United States. Although states have historically made their own decisions about vaccination exemptions linked to day care or school entry because states exercise primary authority over educational matters, childhood vaccination is a national matter in many respects.”
The best way to remedy the current system failure regarding measles vaccination, they continued, may be to adopt a unified national approach to prohibit nonmedical exemptions. They pointed to the fact that the United States previously achieved virtual eradication of measles as recently as 2000. “Following that achievement, state-level policy changes relaxed immunization requirements and set the stage for progressively larger outbreaks in the United States in recent years. Such system failures result when the products, processes, and people (including the public) that comprise systems do not function or behave in ways that protect health optimally.”
The study was supported by a grant from the National Institutes of Health. One coauthor reported having received consulting fees from Merck and grants from Pfizer and Walgreens. Another reported receiving grants from Pfizer, Merck, GlaxoSmithKline, Sanofi Pasteur, Protein Science, Dynavax, and MedImmune. The remaining coauthors reported no relevant financial disclosures.
The editorialists reported having no financial disclosures.
SOURCE: Pingali SC et al. JAMA. 2019 Jul 2. doi: 10.1001/jama.2019.7924.
FROM JAMA
Claims data suggest endometriosis ups risk of chronic opioid use
NASHVILLE, TENN. – Women with endometriosis are at increased risk of chronic opioid use, compared with those without endometriosis, based on an analysis of claims data.
The 2-year rate of chronic opioid use was 4.4% among 36,373 women with endometriosis, compared with 1.1% among 2,172,936 women without endometriosis (odds ratio, 3.94) – a finding with important implications for physician prescribing considerations, Stephanie E. Chiuve, ScD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
The OR was 3.76 after adjusting for age, race, and geographic region, said Dr. Chiuve of AbbVie, North Chicago.
Notably, the prevalence of other pain conditions, depression, anxiety, abuse of substances other than opioids, immunologic disorders, and use of opioids and other medications at baseline was higher in women with endometriosis versus those without. In any year, women with endometriosis were twice as likely to fill at least one opioid prescription, and were 3.5-4 times more likely to be a chronic opioid user than were women without endometriosis, she and her colleagues wrote in a poster presented at the meeting.
“Up to 60% of women with endometriosis experience significant chronic pain, including dysmenorrhea, nonmenstrual pelvic pain, and dyspareunia,” they explained, adding that opioids may be prescribed for chronic pain management or for acute pain in the context of surgical procedures for endometriosis.
“This was due in part to various comorbidities that are also risk factors for chronic opioid use,” Dr. Chiuve said.
Women included in the study were aged 18-50 years (mean, 35 years), and were identified from a U.S. commercial insurance claims database and followed for 2 years after enrolling between January 2006 and December 2017. Chronic opioid use was defined as at least 120 days covered by an opioid dispensing or at least 10 fills of an opioid over a 1-year period during the 2-year follow-up study.
“With a less restrictive definition of chronic opioid use [of at least 6 fills] in any given year, the OR for chronic use comparing women with endometriosis to [the referent group] was similar [OR, 3.77],” the investigators wrote. “The OR for chronic use was attenuated to 2.88 after further adjustment for comorbidities and other medication use.”
Women with endometriosis in this study also experienced higher rates of opioid-associated clinical sequelae, they noted. For example, the adjusted ORs were 17.71 for an opioid dependence diagnosis, 12.52 for opioid overdose, and 10.39 for opioid use disorder treatment in chronic versus nonchronic users of opioids.
Additionally, chronic users were more likely to be prescribed high dose opioids (aOR, 6.45) and to be coprescribed benzodiazepines and sedatives (aORs, 5.87 and 3.78, respectively).
In fact, the findings of this study – though limited by factors such as the use of prescription fills rather than intake to measure exposure, and possible misclassification of endometriosis because of a lack of billing claims or undiagnosed disease – raise concerns about harmful opioid-related outcomes and dangerous prescribing patterns, they said.
In a separate poster presentation at the meeting, the researchers reported that independent risk factors for chronic opioid use in this study population were younger age (ORs, 0.90 and 0.72 for those aged 25-35 and 35-40 years, respectively, vs. those under age 25 years); concomitant chronic pain conditions, including fibromyalgia (OR, 1.49), chronic back pain (OR, 1.55), headaches/migraines (OR, 1.49), irritable bowel syndrome (OR, 1.61), and rheumatoid arthritis (OR, 2.52); the use of antipsychiatric drugs, including antidepressants (OR, 2.0), antipsychotics (OR, 1.66), and benzodiazepines (OR, 1.87); and baseline opioid use (OR, 3.95).
Hispanic ethnicity and Asian race predicted lower risk of chronic opioid use (ORs, 0.56 and 0.39, respectively), they found.
“These data contribute to the knowledge of potential risks of opioid use and may inform benefit-risk decision making of opioid use among women with endometriosis for management of endometriosis and its associated pain,” they concluded.
This study was funded by AbbVie. Dr. Chiuve is an employee of AbbVie, and she reported receiving stock/stock options.
NASHVILLE, TENN. – Women with endometriosis are at increased risk of chronic opioid use, compared with those without endometriosis, based on an analysis of claims data.
The 2-year rate of chronic opioid use was 4.4% among 36,373 women with endometriosis, compared with 1.1% among 2,172,936 women without endometriosis (odds ratio, 3.94) – a finding with important implications for physician prescribing considerations, Stephanie E. Chiuve, ScD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
The OR was 3.76 after adjusting for age, race, and geographic region, said Dr. Chiuve of AbbVie, North Chicago.
Notably, the prevalence of other pain conditions, depression, anxiety, abuse of substances other than opioids, immunologic disorders, and use of opioids and other medications at baseline was higher in women with endometriosis versus those without. In any year, women with endometriosis were twice as likely to fill at least one opioid prescription, and were 3.5-4 times more likely to be a chronic opioid user than were women without endometriosis, she and her colleagues wrote in a poster presented at the meeting.
“Up to 60% of women with endometriosis experience significant chronic pain, including dysmenorrhea, nonmenstrual pelvic pain, and dyspareunia,” they explained, adding that opioids may be prescribed for chronic pain management or for acute pain in the context of surgical procedures for endometriosis.
“This was due in part to various comorbidities that are also risk factors for chronic opioid use,” Dr. Chiuve said.
Women included in the study were aged 18-50 years (mean, 35 years), and were identified from a U.S. commercial insurance claims database and followed for 2 years after enrolling between January 2006 and December 2017. Chronic opioid use was defined as at least 120 days covered by an opioid dispensing or at least 10 fills of an opioid over a 1-year period during the 2-year follow-up study.
“With a less restrictive definition of chronic opioid use [of at least 6 fills] in any given year, the OR for chronic use comparing women with endometriosis to [the referent group] was similar [OR, 3.77],” the investigators wrote. “The OR for chronic use was attenuated to 2.88 after further adjustment for comorbidities and other medication use.”
Women with endometriosis in this study also experienced higher rates of opioid-associated clinical sequelae, they noted. For example, the adjusted ORs were 17.71 for an opioid dependence diagnosis, 12.52 for opioid overdose, and 10.39 for opioid use disorder treatment in chronic versus nonchronic users of opioids.
Additionally, chronic users were more likely to be prescribed high dose opioids (aOR, 6.45) and to be coprescribed benzodiazepines and sedatives (aORs, 5.87 and 3.78, respectively).
In fact, the findings of this study – though limited by factors such as the use of prescription fills rather than intake to measure exposure, and possible misclassification of endometriosis because of a lack of billing claims or undiagnosed disease – raise concerns about harmful opioid-related outcomes and dangerous prescribing patterns, they said.
In a separate poster presentation at the meeting, the researchers reported that independent risk factors for chronic opioid use in this study population were younger age (ORs, 0.90 and 0.72 for those aged 25-35 and 35-40 years, respectively, vs. those under age 25 years); concomitant chronic pain conditions, including fibromyalgia (OR, 1.49), chronic back pain (OR, 1.55), headaches/migraines (OR, 1.49), irritable bowel syndrome (OR, 1.61), and rheumatoid arthritis (OR, 2.52); the use of antipsychiatric drugs, including antidepressants (OR, 2.0), antipsychotics (OR, 1.66), and benzodiazepines (OR, 1.87); and baseline opioid use (OR, 3.95).
Hispanic ethnicity and Asian race predicted lower risk of chronic opioid use (ORs, 0.56 and 0.39, respectively), they found.
“These data contribute to the knowledge of potential risks of opioid use and may inform benefit-risk decision making of opioid use among women with endometriosis for management of endometriosis and its associated pain,” they concluded.
This study was funded by AbbVie. Dr. Chiuve is an employee of AbbVie, and she reported receiving stock/stock options.
NASHVILLE, TENN. – Women with endometriosis are at increased risk of chronic opioid use, compared with those without endometriosis, based on an analysis of claims data.
The 2-year rate of chronic opioid use was 4.4% among 36,373 women with endometriosis, compared with 1.1% among 2,172,936 women without endometriosis (odds ratio, 3.94) – a finding with important implications for physician prescribing considerations, Stephanie E. Chiuve, ScD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
The OR was 3.76 after adjusting for age, race, and geographic region, said Dr. Chiuve of AbbVie, North Chicago.
Notably, the prevalence of other pain conditions, depression, anxiety, abuse of substances other than opioids, immunologic disorders, and use of opioids and other medications at baseline was higher in women with endometriosis versus those without. In any year, women with endometriosis were twice as likely to fill at least one opioid prescription, and were 3.5-4 times more likely to be a chronic opioid user than were women without endometriosis, she and her colleagues wrote in a poster presented at the meeting.
“Up to 60% of women with endometriosis experience significant chronic pain, including dysmenorrhea, nonmenstrual pelvic pain, and dyspareunia,” they explained, adding that opioids may be prescribed for chronic pain management or for acute pain in the context of surgical procedures for endometriosis.
“This was due in part to various comorbidities that are also risk factors for chronic opioid use,” Dr. Chiuve said.
Women included in the study were aged 18-50 years (mean, 35 years), and were identified from a U.S. commercial insurance claims database and followed for 2 years after enrolling between January 2006 and December 2017. Chronic opioid use was defined as at least 120 days covered by an opioid dispensing or at least 10 fills of an opioid over a 1-year period during the 2-year follow-up study.
“With a less restrictive definition of chronic opioid use [of at least 6 fills] in any given year, the OR for chronic use comparing women with endometriosis to [the referent group] was similar [OR, 3.77],” the investigators wrote. “The OR for chronic use was attenuated to 2.88 after further adjustment for comorbidities and other medication use.”
Women with endometriosis in this study also experienced higher rates of opioid-associated clinical sequelae, they noted. For example, the adjusted ORs were 17.71 for an opioid dependence diagnosis, 12.52 for opioid overdose, and 10.39 for opioid use disorder treatment in chronic versus nonchronic users of opioids.
Additionally, chronic users were more likely to be prescribed high dose opioids (aOR, 6.45) and to be coprescribed benzodiazepines and sedatives (aORs, 5.87 and 3.78, respectively).
In fact, the findings of this study – though limited by factors such as the use of prescription fills rather than intake to measure exposure, and possible misclassification of endometriosis because of a lack of billing claims or undiagnosed disease – raise concerns about harmful opioid-related outcomes and dangerous prescribing patterns, they said.
In a separate poster presentation at the meeting, the researchers reported that independent risk factors for chronic opioid use in this study population were younger age (ORs, 0.90 and 0.72 for those aged 25-35 and 35-40 years, respectively, vs. those under age 25 years); concomitant chronic pain conditions, including fibromyalgia (OR, 1.49), chronic back pain (OR, 1.55), headaches/migraines (OR, 1.49), irritable bowel syndrome (OR, 1.61), and rheumatoid arthritis (OR, 2.52); the use of antipsychiatric drugs, including antidepressants (OR, 2.0), antipsychotics (OR, 1.66), and benzodiazepines (OR, 1.87); and baseline opioid use (OR, 3.95).
Hispanic ethnicity and Asian race predicted lower risk of chronic opioid use (ORs, 0.56 and 0.39, respectively), they found.
“These data contribute to the knowledge of potential risks of opioid use and may inform benefit-risk decision making of opioid use among women with endometriosis for management of endometriosis and its associated pain,” they concluded.
This study was funded by AbbVie. Dr. Chiuve is an employee of AbbVie, and she reported receiving stock/stock options.
REPORTING FROM ACOG 2019
Static and Dynamic Functional Connectivity in Migraine
Resting-state functional imaging revealed static functional connectivity and dynamic functional connectivity differences between migraine and persistent post-traumatic headache for regions involved in pain processing, a new study found. The case-control study integrated the static functional connectivity and dynamic functional connectivity patterns of 59 a priori selected regions of interest involved in pain processing. Pairwise connectivity differences between migraine (n=33) and persistent post-traumatic headache (n=44) were determined and compared to healthy controls (n=36) with ANOVA and subsequent t-tests. Researchers found:
- Significant differences in static functional connectivity between migraine and persistent post-traumatic headache were found for 17 region pairs.
- Significant differences in dynamic functional connectivity between migraine and persistent post-traumatic headache were found for 10 region pairs.
- These differences in functional connectivity may be indicative of pathophysiology associated with migraine vs persistent post-traumatic headache.
Dumkrieger G, et al. Static and dynamic functional connectivity differences between migraine and persistent post-traumatic headache: A resting-state magnetic resonance imaging study. [Published online ahead of print May 1, 2019]. Cephalalgia. doi: 10.1177/0333102419847728.
Resting-state functional imaging revealed static functional connectivity and dynamic functional connectivity differences between migraine and persistent post-traumatic headache for regions involved in pain processing, a new study found. The case-control study integrated the static functional connectivity and dynamic functional connectivity patterns of 59 a priori selected regions of interest involved in pain processing. Pairwise connectivity differences between migraine (n=33) and persistent post-traumatic headache (n=44) were determined and compared to healthy controls (n=36) with ANOVA and subsequent t-tests. Researchers found:
- Significant differences in static functional connectivity between migraine and persistent post-traumatic headache were found for 17 region pairs.
- Significant differences in dynamic functional connectivity between migraine and persistent post-traumatic headache were found for 10 region pairs.
- These differences in functional connectivity may be indicative of pathophysiology associated with migraine vs persistent post-traumatic headache.
Dumkrieger G, et al. Static and dynamic functional connectivity differences between migraine and persistent post-traumatic headache: A resting-state magnetic resonance imaging study. [Published online ahead of print May 1, 2019]. Cephalalgia. doi: 10.1177/0333102419847728.
Resting-state functional imaging revealed static functional connectivity and dynamic functional connectivity differences between migraine and persistent post-traumatic headache for regions involved in pain processing, a new study found. The case-control study integrated the static functional connectivity and dynamic functional connectivity patterns of 59 a priori selected regions of interest involved in pain processing. Pairwise connectivity differences between migraine (n=33) and persistent post-traumatic headache (n=44) were determined and compared to healthy controls (n=36) with ANOVA and subsequent t-tests. Researchers found:
- Significant differences in static functional connectivity between migraine and persistent post-traumatic headache were found for 17 region pairs.
- Significant differences in dynamic functional connectivity between migraine and persistent post-traumatic headache were found for 10 region pairs.
- These differences in functional connectivity may be indicative of pathophysiology associated with migraine vs persistent post-traumatic headache.
Dumkrieger G, et al. Static and dynamic functional connectivity differences between migraine and persistent post-traumatic headache: A resting-state magnetic resonance imaging study. [Published online ahead of print May 1, 2019]. Cephalalgia. doi: 10.1177/0333102419847728.
Characteristics of Adolescents with Prolonged Headache
High levels of disability and low quality of life (QOL) were reported among children and adolescents with migraine utilizing infusion treatment, a new study found. Patients aged 6-19 years treated in an outpatient headache infusion center were included. A subset of these patients completed a behavioral health evaluation (treatment group) and were compared with a control group of similar age and gender to patients not seeking infusion treatment. Among the findings:
- 284 patients were included in the study (n=227 treatment group; n=57 controls).
- There was a promising difference in the Pediatric Pain Coping Inventory (PPCI) Distraction subscale, with a mean rank score of 61.90 for the treatment group vs 50.21 for the control group.
- There was a statistically significant difference on the Social Support subscale, with a mean rank score of 65.92 for the treatment group vs 46.26 for the control group.
- Patient-reported data also revealed a significantly higher level of disability among those seeking infusion treatment compared to the non-infusion group.
Woods K, et al. Psychosocial and demographic characteristics of children and adolescents with headache presenting for treatment in a headache infusion center. Headache. 2019;59(6):858-868. doi: 10.1111/head.13537.
High levels of disability and low quality of life (QOL) were reported among children and adolescents with migraine utilizing infusion treatment, a new study found. Patients aged 6-19 years treated in an outpatient headache infusion center were included. A subset of these patients completed a behavioral health evaluation (treatment group) and were compared with a control group of similar age and gender to patients not seeking infusion treatment. Among the findings:
- 284 patients were included in the study (n=227 treatment group; n=57 controls).
- There was a promising difference in the Pediatric Pain Coping Inventory (PPCI) Distraction subscale, with a mean rank score of 61.90 for the treatment group vs 50.21 for the control group.
- There was a statistically significant difference on the Social Support subscale, with a mean rank score of 65.92 for the treatment group vs 46.26 for the control group.
- Patient-reported data also revealed a significantly higher level of disability among those seeking infusion treatment compared to the non-infusion group.
Woods K, et al. Psychosocial and demographic characteristics of children and adolescents with headache presenting for treatment in a headache infusion center. Headache. 2019;59(6):858-868. doi: 10.1111/head.13537.
High levels of disability and low quality of life (QOL) were reported among children and adolescents with migraine utilizing infusion treatment, a new study found. Patients aged 6-19 years treated in an outpatient headache infusion center were included. A subset of these patients completed a behavioral health evaluation (treatment group) and were compared with a control group of similar age and gender to patients not seeking infusion treatment. Among the findings:
- 284 patients were included in the study (n=227 treatment group; n=57 controls).
- There was a promising difference in the Pediatric Pain Coping Inventory (PPCI) Distraction subscale, with a mean rank score of 61.90 for the treatment group vs 50.21 for the control group.
- There was a statistically significant difference on the Social Support subscale, with a mean rank score of 65.92 for the treatment group vs 46.26 for the control group.
- Patient-reported data also revealed a significantly higher level of disability among those seeking infusion treatment compared to the non-infusion group.
Woods K, et al. Psychosocial and demographic characteristics of children and adolescents with headache presenting for treatment in a headache infusion center. Headache. 2019;59(6):858-868. doi: 10.1111/head.13537.
2019 Update on abnormal uterine bleeding
Keeping current with causes of and treatments for abnormal uterine bleeding (AUB) is important. AUB can have a major impact on women’s lives in terms of health care expenses, productivity, and quality of life. The focus of this Update is on information that has been published over the past year that is helpful for clinicians who counsel and treat women with AUB. First, we focus on new data on endometrial polyps, which are a common cause of AUB. For the first time, a meta-analysis has examined polyp-associated cancer risk. In addition, does a causal relationship exist between endometrial polyps and chronic endometritis? We also address the first published report of successful treatment of endometrial intraepithelial neoplasia (EIN, formerly complex endometrial hyperplasia with atypia) using the etonogestrel subdermal implant. Last, we discuss efficacy data for a new device for endometrial ablation, which has new features to consider.
What is the risk of malignancy with endometrial polyps?
Sasaki LM, Andrade KR, Figeuiredo AC, et al. Factors associated with malignancy in hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25:777-785.
In the past year, 2 studies have contributed to our understanding of endometrial polyps, with one published as the first ever meta-analysis on polyp risk of malignancy.
What can information from more than 21,000 patients with polyps teach us about the risk factors associated with endometrial malignancy? For instance, with concern over balancing health care costs with potential surgical risks, should all patients with endometrial polyps undergo routine surgical removal, or should we stratify risks and offer surgery to only selected patients? This is the first meta-analysis to evaluate the risk factors for endometrial cancer (such as obesity, parity, tamoxifen use, and hormonal therapy use) in patients with endometrial polyps.
Risk factors for and prevalence of malignancy
Sasaki and colleagues found that about 3 of every 100 patients with recognized polyps will harbor a premalignant or malignant lesion (3.4%; 716 of 21,057 patients). The identified risk factors for a cancerous polyp included: menopausal status, age greater than 60 years, presence of AUB, diabetes mellitus, hypertension, obesity, and tamoxifen use. The risk for cancer was 2-fold greater in women older than 60 years compared with those younger than age 60 (prevalence ratio, 2.41). The authors found no risk association with use of combination hormone therapy, parity, breast cancer, or polyp size.
The investigators advised caution with using their conclusions, as there was high heterogeneity for some of the factors studied (including age, AUB, parity, and hypertension).
The study takeaways regarding clinical and demographic risk factors suggest that menopausal status, age greater than 60 years, the presence of AUB, diabetes, hypertension, obesity, and tamoxifen use have an increased risk for premalignant and malignant lesions.
This study is important because its findings will better enable physicians to inform and counsel patients about the risks for malignancy associated with endometrial polyps, which will better foster discussion and joint decision-making about whether or not surgery should be performed.
New evidence associates endometrial polyps with chronic endometritis
The second important study published this year on polyps was conducted by Cicinelli and colleagues and suggests that inflammation may be part of the pathophysiology behind the common problem of polyps. The authors cite a recent study that showed that abnormal expression of "local" paracrine inflammatory mediators, such as interferon-gamma, may enhance the proliferation of endometrial mucosa.1 Building on this possibility further, they hypothesized that chronic endometrial inflammation may affect the pathogenesis of endometrial polyps.
Details of the study
To investigate the possible correlation between polyps and chronic endometritis, Cicinelli and colleagues compared the endometrial biopsies of 240 women with AUB and hysteroscopically and histologically diagnosed endometrial polyps with 240 women with AUB and no polyp seen on hysteroscopy. The tissue samples were evaluated with immunohistochemistry for CD-138 for plasma cell identification.
The study authors found a significantly higher prevalence of chronic endometritis in the group with endometrial polyps than in the group without polyps (61.7% vs 24.2%, respectively; P <.0001). They suggest that this evidence supports the hypothesis that endometrial polyps may be a result of endometrial proliferation and vasculopathy triggered by chronic endometritis.
The significance of this study is that there is a possible causal relationship between endometrial polyps and chronic endometritis, which may expand the options for endometrial polyp therapy beyond surgical management in the future.
Continue to: Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Wong S, Naresh A. Etonogestrel subdermal implant-associated regression of endometrial intraepithelial neoplasia. Obstet Gynecol. 2019;133:780-782.
Recently, Wong and Naresh gave us the first case report of successful treatment of EIN using the etonogestrel subdermal implant. With so many other options available to treat EIN, some of which have been studied extensively, why should we take note of this study? First, the authors point out the risk of endometrial cancer development among patients with EIN, and they acknowledge the standard recommendation of hysterectomy in women with EIN who have finished childbearing and are appropriate candidates for a surgical approach. There is also concern about lower serum etonogestrel levels in obese patients. In this case, the patient (aged 36 with obesity) had been nonadherent with oral progestin therapy and stated that she would not adhere to daily oral therapy. She also declined hysterectomy, levonorgestrel-releasing intrauterine device therapy, and injectable progestin therapy after being counseled about the risk of malignancy development. She consented to subdermal etonogestrel as an alternative to no therapy.
EIN regressed. Endometrial biopsies at 4 and 8 months showed regression of EIN, and at 16 months after implantation (as well as a dilation and curettage at 9 months) demonstrated an inactive endometrium with no sign of hyperplasia.
The authors remain cautious about recommending the etonogestrel subdermal implant as a first-line therapy for EIN, but the implant was reported to be effective in this case that involved a patient with obesity. In cases in which surgery or other medical options for EIN are not feasible, the etonogestrel subdermal implant is reasonable to consider. Its routine use for EIN management warrants future study.
New endometrial ablation technology shows promising benefits
Do we need another endometrial ablation device? Are there improvements that can be made to our existing technology? There already are several endometrial ablation devices, using varying technology, that currently are approved by the US Food and Drug Administration (FDA) for treatment of AUB. The devices use bipolar radiofrequency, cryotherapy, circulating hot fluid, and combined thermal and radiofrequency modalities. Additional devices, employing heated balloon and microwaves, are no longer used. Data on a new device, approved by the FDA in 2017 (the AEGEA Vapor System, called Mara), were recently published.
Details of the study
Levie and colleagues conducted a prospective pivotal trial on Mara's safety and effectiveness. The benefits presented by the authors include that the device 1) does not require that an intrauterine array be deployed up to and abutting the fundus and cornu, 2) does not necessitate cervical dilatation, 3) is a free-flowing vapor system that can navigate differences in uterine contour and sizes (up to 12 cm in length), and 4) accomplishes ablation in 2 minutes. So there are indeed some novel features of this device.
This pivotal study was a multicenter trial using objective performance criterion (OPC), which is based on using the average success rates across the 5 FDA-approved ablation devices as historic controls. In the study an OPC of 66% correlated to the lower bound of the 95% confidence intervals. The primary outcome of the study was effectiveness in the reduction of blood loss using a pictorial blood loss assessment score (PBLAS) of less than 75. Of note, a PBLAS of 150 was a study entry criterion. FIGO types 2 through 6 fibroids were included in the trial. Secondary endpoints were quality of life and patient satisfaction as assessed by the Menorrhagia Impact Questionnaire and the Aberdeen Menorrhagia Severity Score, as well as the need to intervene medically or surgically to treat AUB in the first 12 months after ablation.
Efficacy, satisfaction, and quality of life results
At 12 months, the primary effectiveness end point was achieved in 78.7% of study participants. The satisfaction rate was 90.8% (satisfied or very satisfied), and 99% of participants showed improvement in quality of life scores. There were no reported serious adverse events.
The takeaway is that the AEGEA device appears to be effective for endometrial ablation and offers the novel features of not relying on an intrauterine array to be deployed up to and abutting the fundus and cornu, not necessitating cervical dilatation in all cases, and offering a free-flowing vapor system that can navigate differences in uterine contour and sizes quickly (approximately 2 minutes).
The fact that new devices for endometrial ablation are still being developed is encouraging, and it suggests that endometrial ablation technology can be improved. Although AEGEA's Mara system is not yet commercially available, it is anticipated that it will be available at the start of 2020. The ability to treat large uteri (up to 12-cm cavities) with FIGO type 2 to 6 fibroids with less cervical dilatation makes the device attractive and perhaps well suited for office use.
- Mollo A, Stile A, Alviggi C, et al. Endometrial polyps in infertile patients: do high concentrations of interferon-gamma play a role? Fertil Steril. 2011:96:1209-1212.
Keeping current with causes of and treatments for abnormal uterine bleeding (AUB) is important. AUB can have a major impact on women’s lives in terms of health care expenses, productivity, and quality of life. The focus of this Update is on information that has been published over the past year that is helpful for clinicians who counsel and treat women with AUB. First, we focus on new data on endometrial polyps, which are a common cause of AUB. For the first time, a meta-analysis has examined polyp-associated cancer risk. In addition, does a causal relationship exist between endometrial polyps and chronic endometritis? We also address the first published report of successful treatment of endometrial intraepithelial neoplasia (EIN, formerly complex endometrial hyperplasia with atypia) using the etonogestrel subdermal implant. Last, we discuss efficacy data for a new device for endometrial ablation, which has new features to consider.
What is the risk of malignancy with endometrial polyps?
Sasaki LM, Andrade KR, Figeuiredo AC, et al. Factors associated with malignancy in hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25:777-785.
In the past year, 2 studies have contributed to our understanding of endometrial polyps, with one published as the first ever meta-analysis on polyp risk of malignancy.
What can information from more than 21,000 patients with polyps teach us about the risk factors associated with endometrial malignancy? For instance, with concern over balancing health care costs with potential surgical risks, should all patients with endometrial polyps undergo routine surgical removal, or should we stratify risks and offer surgery to only selected patients? This is the first meta-analysis to evaluate the risk factors for endometrial cancer (such as obesity, parity, tamoxifen use, and hormonal therapy use) in patients with endometrial polyps.
Risk factors for and prevalence of malignancy
Sasaki and colleagues found that about 3 of every 100 patients with recognized polyps will harbor a premalignant or malignant lesion (3.4%; 716 of 21,057 patients). The identified risk factors for a cancerous polyp included: menopausal status, age greater than 60 years, presence of AUB, diabetes mellitus, hypertension, obesity, and tamoxifen use. The risk for cancer was 2-fold greater in women older than 60 years compared with those younger than age 60 (prevalence ratio, 2.41). The authors found no risk association with use of combination hormone therapy, parity, breast cancer, or polyp size.
The investigators advised caution with using their conclusions, as there was high heterogeneity for some of the factors studied (including age, AUB, parity, and hypertension).
The study takeaways regarding clinical and demographic risk factors suggest that menopausal status, age greater than 60 years, the presence of AUB, diabetes, hypertension, obesity, and tamoxifen use have an increased risk for premalignant and malignant lesions.
This study is important because its findings will better enable physicians to inform and counsel patients about the risks for malignancy associated with endometrial polyps, which will better foster discussion and joint decision-making about whether or not surgery should be performed.
New evidence associates endometrial polyps with chronic endometritis
The second important study published this year on polyps was conducted by Cicinelli and colleagues and suggests that inflammation may be part of the pathophysiology behind the common problem of polyps. The authors cite a recent study that showed that abnormal expression of "local" paracrine inflammatory mediators, such as interferon-gamma, may enhance the proliferation of endometrial mucosa.1 Building on this possibility further, they hypothesized that chronic endometrial inflammation may affect the pathogenesis of endometrial polyps.
Details of the study
To investigate the possible correlation between polyps and chronic endometritis, Cicinelli and colleagues compared the endometrial biopsies of 240 women with AUB and hysteroscopically and histologically diagnosed endometrial polyps with 240 women with AUB and no polyp seen on hysteroscopy. The tissue samples were evaluated with immunohistochemistry for CD-138 for plasma cell identification.
The study authors found a significantly higher prevalence of chronic endometritis in the group with endometrial polyps than in the group without polyps (61.7% vs 24.2%, respectively; P <.0001). They suggest that this evidence supports the hypothesis that endometrial polyps may be a result of endometrial proliferation and vasculopathy triggered by chronic endometritis.
The significance of this study is that there is a possible causal relationship between endometrial polyps and chronic endometritis, which may expand the options for endometrial polyp therapy beyond surgical management in the future.
Continue to: Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Wong S, Naresh A. Etonogestrel subdermal implant-associated regression of endometrial intraepithelial neoplasia. Obstet Gynecol. 2019;133:780-782.
Recently, Wong and Naresh gave us the first case report of successful treatment of EIN using the etonogestrel subdermal implant. With so many other options available to treat EIN, some of which have been studied extensively, why should we take note of this study? First, the authors point out the risk of endometrial cancer development among patients with EIN, and they acknowledge the standard recommendation of hysterectomy in women with EIN who have finished childbearing and are appropriate candidates for a surgical approach. There is also concern about lower serum etonogestrel levels in obese patients. In this case, the patient (aged 36 with obesity) had been nonadherent with oral progestin therapy and stated that she would not adhere to daily oral therapy. She also declined hysterectomy, levonorgestrel-releasing intrauterine device therapy, and injectable progestin therapy after being counseled about the risk of malignancy development. She consented to subdermal etonogestrel as an alternative to no therapy.
EIN regressed. Endometrial biopsies at 4 and 8 months showed regression of EIN, and at 16 months after implantation (as well as a dilation and curettage at 9 months) demonstrated an inactive endometrium with no sign of hyperplasia.
The authors remain cautious about recommending the etonogestrel subdermal implant as a first-line therapy for EIN, but the implant was reported to be effective in this case that involved a patient with obesity. In cases in which surgery or other medical options for EIN are not feasible, the etonogestrel subdermal implant is reasonable to consider. Its routine use for EIN management warrants future study.
New endometrial ablation technology shows promising benefits
Do we need another endometrial ablation device? Are there improvements that can be made to our existing technology? There already are several endometrial ablation devices, using varying technology, that currently are approved by the US Food and Drug Administration (FDA) for treatment of AUB. The devices use bipolar radiofrequency, cryotherapy, circulating hot fluid, and combined thermal and radiofrequency modalities. Additional devices, employing heated balloon and microwaves, are no longer used. Data on a new device, approved by the FDA in 2017 (the AEGEA Vapor System, called Mara), were recently published.
Details of the study
Levie and colleagues conducted a prospective pivotal trial on Mara's safety and effectiveness. The benefits presented by the authors include that the device 1) does not require that an intrauterine array be deployed up to and abutting the fundus and cornu, 2) does not necessitate cervical dilatation, 3) is a free-flowing vapor system that can navigate differences in uterine contour and sizes (up to 12 cm in length), and 4) accomplishes ablation in 2 minutes. So there are indeed some novel features of this device.
This pivotal study was a multicenter trial using objective performance criterion (OPC), which is based on using the average success rates across the 5 FDA-approved ablation devices as historic controls. In the study an OPC of 66% correlated to the lower bound of the 95% confidence intervals. The primary outcome of the study was effectiveness in the reduction of blood loss using a pictorial blood loss assessment score (PBLAS) of less than 75. Of note, a PBLAS of 150 was a study entry criterion. FIGO types 2 through 6 fibroids were included in the trial. Secondary endpoints were quality of life and patient satisfaction as assessed by the Menorrhagia Impact Questionnaire and the Aberdeen Menorrhagia Severity Score, as well as the need to intervene medically or surgically to treat AUB in the first 12 months after ablation.
Efficacy, satisfaction, and quality of life results
At 12 months, the primary effectiveness end point was achieved in 78.7% of study participants. The satisfaction rate was 90.8% (satisfied or very satisfied), and 99% of participants showed improvement in quality of life scores. There were no reported serious adverse events.
The takeaway is that the AEGEA device appears to be effective for endometrial ablation and offers the novel features of not relying on an intrauterine array to be deployed up to and abutting the fundus and cornu, not necessitating cervical dilatation in all cases, and offering a free-flowing vapor system that can navigate differences in uterine contour and sizes quickly (approximately 2 minutes).
The fact that new devices for endometrial ablation are still being developed is encouraging, and it suggests that endometrial ablation technology can be improved. Although AEGEA's Mara system is not yet commercially available, it is anticipated that it will be available at the start of 2020. The ability to treat large uteri (up to 12-cm cavities) with FIGO type 2 to 6 fibroids with less cervical dilatation makes the device attractive and perhaps well suited for office use.
Keeping current with causes of and treatments for abnormal uterine bleeding (AUB) is important. AUB can have a major impact on women’s lives in terms of health care expenses, productivity, and quality of life. The focus of this Update is on information that has been published over the past year that is helpful for clinicians who counsel and treat women with AUB. First, we focus on new data on endometrial polyps, which are a common cause of AUB. For the first time, a meta-analysis has examined polyp-associated cancer risk. In addition, does a causal relationship exist between endometrial polyps and chronic endometritis? We also address the first published report of successful treatment of endometrial intraepithelial neoplasia (EIN, formerly complex endometrial hyperplasia with atypia) using the etonogestrel subdermal implant. Last, we discuss efficacy data for a new device for endometrial ablation, which has new features to consider.
What is the risk of malignancy with endometrial polyps?
Sasaki LM, Andrade KR, Figeuiredo AC, et al. Factors associated with malignancy in hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25:777-785.
In the past year, 2 studies have contributed to our understanding of endometrial polyps, with one published as the first ever meta-analysis on polyp risk of malignancy.
What can information from more than 21,000 patients with polyps teach us about the risk factors associated with endometrial malignancy? For instance, with concern over balancing health care costs with potential surgical risks, should all patients with endometrial polyps undergo routine surgical removal, or should we stratify risks and offer surgery to only selected patients? This is the first meta-analysis to evaluate the risk factors for endometrial cancer (such as obesity, parity, tamoxifen use, and hormonal therapy use) in patients with endometrial polyps.
Risk factors for and prevalence of malignancy
Sasaki and colleagues found that about 3 of every 100 patients with recognized polyps will harbor a premalignant or malignant lesion (3.4%; 716 of 21,057 patients). The identified risk factors for a cancerous polyp included: menopausal status, age greater than 60 years, presence of AUB, diabetes mellitus, hypertension, obesity, and tamoxifen use. The risk for cancer was 2-fold greater in women older than 60 years compared with those younger than age 60 (prevalence ratio, 2.41). The authors found no risk association with use of combination hormone therapy, parity, breast cancer, or polyp size.
The investigators advised caution with using their conclusions, as there was high heterogeneity for some of the factors studied (including age, AUB, parity, and hypertension).
The study takeaways regarding clinical and demographic risk factors suggest that menopausal status, age greater than 60 years, the presence of AUB, diabetes, hypertension, obesity, and tamoxifen use have an increased risk for premalignant and malignant lesions.
This study is important because its findings will better enable physicians to inform and counsel patients about the risks for malignancy associated with endometrial polyps, which will better foster discussion and joint decision-making about whether or not surgery should be performed.
New evidence associates endometrial polyps with chronic endometritis
The second important study published this year on polyps was conducted by Cicinelli and colleagues and suggests that inflammation may be part of the pathophysiology behind the common problem of polyps. The authors cite a recent study that showed that abnormal expression of "local" paracrine inflammatory mediators, such as interferon-gamma, may enhance the proliferation of endometrial mucosa.1 Building on this possibility further, they hypothesized that chronic endometrial inflammation may affect the pathogenesis of endometrial polyps.
Details of the study
To investigate the possible correlation between polyps and chronic endometritis, Cicinelli and colleagues compared the endometrial biopsies of 240 women with AUB and hysteroscopically and histologically diagnosed endometrial polyps with 240 women with AUB and no polyp seen on hysteroscopy. The tissue samples were evaluated with immunohistochemistry for CD-138 for plasma cell identification.
The study authors found a significantly higher prevalence of chronic endometritis in the group with endometrial polyps than in the group without polyps (61.7% vs 24.2%, respectively; P <.0001). They suggest that this evidence supports the hypothesis that endometrial polyps may be a result of endometrial proliferation and vasculopathy triggered by chronic endometritis.
The significance of this study is that there is a possible causal relationship between endometrial polyps and chronic endometritis, which may expand the options for endometrial polyp therapy beyond surgical management in the future.
Continue to: Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Can endometrial intraepithelial neoplasia be treated with the etonogestrel subdermal implant?
Wong S, Naresh A. Etonogestrel subdermal implant-associated regression of endometrial intraepithelial neoplasia. Obstet Gynecol. 2019;133:780-782.
Recently, Wong and Naresh gave us the first case report of successful treatment of EIN using the etonogestrel subdermal implant. With so many other options available to treat EIN, some of which have been studied extensively, why should we take note of this study? First, the authors point out the risk of endometrial cancer development among patients with EIN, and they acknowledge the standard recommendation of hysterectomy in women with EIN who have finished childbearing and are appropriate candidates for a surgical approach. There is also concern about lower serum etonogestrel levels in obese patients. In this case, the patient (aged 36 with obesity) had been nonadherent with oral progestin therapy and stated that she would not adhere to daily oral therapy. She also declined hysterectomy, levonorgestrel-releasing intrauterine device therapy, and injectable progestin therapy after being counseled about the risk of malignancy development. She consented to subdermal etonogestrel as an alternative to no therapy.
EIN regressed. Endometrial biopsies at 4 and 8 months showed regression of EIN, and at 16 months after implantation (as well as a dilation and curettage at 9 months) demonstrated an inactive endometrium with no sign of hyperplasia.
The authors remain cautious about recommending the etonogestrel subdermal implant as a first-line therapy for EIN, but the implant was reported to be effective in this case that involved a patient with obesity. In cases in which surgery or other medical options for EIN are not feasible, the etonogestrel subdermal implant is reasonable to consider. Its routine use for EIN management warrants future study.
New endometrial ablation technology shows promising benefits
Do we need another endometrial ablation device? Are there improvements that can be made to our existing technology? There already are several endometrial ablation devices, using varying technology, that currently are approved by the US Food and Drug Administration (FDA) for treatment of AUB. The devices use bipolar radiofrequency, cryotherapy, circulating hot fluid, and combined thermal and radiofrequency modalities. Additional devices, employing heated balloon and microwaves, are no longer used. Data on a new device, approved by the FDA in 2017 (the AEGEA Vapor System, called Mara), were recently published.
Details of the study
Levie and colleagues conducted a prospective pivotal trial on Mara's safety and effectiveness. The benefits presented by the authors include that the device 1) does not require that an intrauterine array be deployed up to and abutting the fundus and cornu, 2) does not necessitate cervical dilatation, 3) is a free-flowing vapor system that can navigate differences in uterine contour and sizes (up to 12 cm in length), and 4) accomplishes ablation in 2 minutes. So there are indeed some novel features of this device.
This pivotal study was a multicenter trial using objective performance criterion (OPC), which is based on using the average success rates across the 5 FDA-approved ablation devices as historic controls. In the study an OPC of 66% correlated to the lower bound of the 95% confidence intervals. The primary outcome of the study was effectiveness in the reduction of blood loss using a pictorial blood loss assessment score (PBLAS) of less than 75. Of note, a PBLAS of 150 was a study entry criterion. FIGO types 2 through 6 fibroids were included in the trial. Secondary endpoints were quality of life and patient satisfaction as assessed by the Menorrhagia Impact Questionnaire and the Aberdeen Menorrhagia Severity Score, as well as the need to intervene medically or surgically to treat AUB in the first 12 months after ablation.
Efficacy, satisfaction, and quality of life results
At 12 months, the primary effectiveness end point was achieved in 78.7% of study participants. The satisfaction rate was 90.8% (satisfied or very satisfied), and 99% of participants showed improvement in quality of life scores. There were no reported serious adverse events.
The takeaway is that the AEGEA device appears to be effective for endometrial ablation and offers the novel features of not relying on an intrauterine array to be deployed up to and abutting the fundus and cornu, not necessitating cervical dilatation in all cases, and offering a free-flowing vapor system that can navigate differences in uterine contour and sizes quickly (approximately 2 minutes).
The fact that new devices for endometrial ablation are still being developed is encouraging, and it suggests that endometrial ablation technology can be improved. Although AEGEA's Mara system is not yet commercially available, it is anticipated that it will be available at the start of 2020. The ability to treat large uteri (up to 12-cm cavities) with FIGO type 2 to 6 fibroids with less cervical dilatation makes the device attractive and perhaps well suited for office use.
- Mollo A, Stile A, Alviggi C, et al. Endometrial polyps in infertile patients: do high concentrations of interferon-gamma play a role? Fertil Steril. 2011:96:1209-1212.
- Mollo A, Stile A, Alviggi C, et al. Endometrial polyps in infertile patients: do high concentrations of interferon-gamma play a role? Fertil Steril. 2011:96:1209-1212.