User login
Poor COPD management might increase MI risk in HIV
SEATTLE – Chronic obstructive pulmonary disease is independently associated with an increased risk of myocardial infarction in people with HIV, according to a report at the Conference on Retroviruses and Opportunistic Infections.
Chronic obstructive pulmonary disease (COPD) is known to increase the risk of myocardial infarction (MI) in the general population, but hadn’t been shown until now to do the same in HIV. The study raises the question of whether COPD is being managed adequately in patients with the virus, according to study lead Kristina Crothers, MD, associate professor in the division of pulmonary, critical care & sleep medicine at the University of Washington, Seattle.
The investigators reviewed 25,509 HIV patients in the Center for AIDS Research Network of Integrated Clinical Systems cohort, a large electronic database of HIV-infected people. They defined COPD by diagnostic codes and inhaler prescriptions. MIs were adjudicated by review.
The team identified 423 subjects with moderate to severe COPD, and 698 who had MIs, including 339 type 1 MIs (T1MI) from a ruptured plaque (54%), and 294 (46%) type 2 heart attacks (T2MI) from a supply-demand mismatch due to sepsis or some other problem. In general, T2MIs are far more common in people with HIV.
COPD was associated with a greater than twofold increased risk of MI after adjustment for age, sex, viral load, nadir CD4 count, hypertension, and other confounders. The risk dropped slightly when smoking – both current smoking and pack years – was added to the model (adjusted hazard ratio 1.88, 95% confidence interval, 1.34-2.63).
The association was particularly strong for T2MI, especially in the setting of bacteremia and sepsis, and unlike T1MI, it remained significant after adjustment for smoking.
The study establishes a link between COPD and MI in HIV, but it could not answer what’s going on. Chronic inflammation from the virus could be at play, but the team also found hints of inadequate COPD management.
“About 60% of patients were on inhalers ... but only about 25% of them were on long-acting inhalers. 75% were only on short-acting.” That’s a problem because long-acting inhalers are needed to control exacerbations, Dr. Crothers said.
The study didn’t capture exacerbation rates, but increased rates could help explain the MI risk. Increased rates of pneumonia could as well, since pneumonia is a common cause of sepsis.
“We need to better manage complications of COPD in this population. I think optimizing long-term COPD management could have many beneficial effects,” Dr. Crothers said.
The National Institutes of Health funded the work. Dr. Crothers had no disclosures.
SOURCE: Crothers K et al. CROI 2019, Abstract 31.
SEATTLE – Chronic obstructive pulmonary disease is independently associated with an increased risk of myocardial infarction in people with HIV, according to a report at the Conference on Retroviruses and Opportunistic Infections.
Chronic obstructive pulmonary disease (COPD) is known to increase the risk of myocardial infarction (MI) in the general population, but hadn’t been shown until now to do the same in HIV. The study raises the question of whether COPD is being managed adequately in patients with the virus, according to study lead Kristina Crothers, MD, associate professor in the division of pulmonary, critical care & sleep medicine at the University of Washington, Seattle.
The investigators reviewed 25,509 HIV patients in the Center for AIDS Research Network of Integrated Clinical Systems cohort, a large electronic database of HIV-infected people. They defined COPD by diagnostic codes and inhaler prescriptions. MIs were adjudicated by review.
The team identified 423 subjects with moderate to severe COPD, and 698 who had MIs, including 339 type 1 MIs (T1MI) from a ruptured plaque (54%), and 294 (46%) type 2 heart attacks (T2MI) from a supply-demand mismatch due to sepsis or some other problem. In general, T2MIs are far more common in people with HIV.
COPD was associated with a greater than twofold increased risk of MI after adjustment for age, sex, viral load, nadir CD4 count, hypertension, and other confounders. The risk dropped slightly when smoking – both current smoking and pack years – was added to the model (adjusted hazard ratio 1.88, 95% confidence interval, 1.34-2.63).
The association was particularly strong for T2MI, especially in the setting of bacteremia and sepsis, and unlike T1MI, it remained significant after adjustment for smoking.
The study establishes a link between COPD and MI in HIV, but it could not answer what’s going on. Chronic inflammation from the virus could be at play, but the team also found hints of inadequate COPD management.
“About 60% of patients were on inhalers ... but only about 25% of them were on long-acting inhalers. 75% were only on short-acting.” That’s a problem because long-acting inhalers are needed to control exacerbations, Dr. Crothers said.
The study didn’t capture exacerbation rates, but increased rates could help explain the MI risk. Increased rates of pneumonia could as well, since pneumonia is a common cause of sepsis.
“We need to better manage complications of COPD in this population. I think optimizing long-term COPD management could have many beneficial effects,” Dr. Crothers said.
The National Institutes of Health funded the work. Dr. Crothers had no disclosures.
SOURCE: Crothers K et al. CROI 2019, Abstract 31.
SEATTLE – Chronic obstructive pulmonary disease is independently associated with an increased risk of myocardial infarction in people with HIV, according to a report at the Conference on Retroviruses and Opportunistic Infections.
Chronic obstructive pulmonary disease (COPD) is known to increase the risk of myocardial infarction (MI) in the general population, but hadn’t been shown until now to do the same in HIV. The study raises the question of whether COPD is being managed adequately in patients with the virus, according to study lead Kristina Crothers, MD, associate professor in the division of pulmonary, critical care & sleep medicine at the University of Washington, Seattle.
The investigators reviewed 25,509 HIV patients in the Center for AIDS Research Network of Integrated Clinical Systems cohort, a large electronic database of HIV-infected people. They defined COPD by diagnostic codes and inhaler prescriptions. MIs were adjudicated by review.
The team identified 423 subjects with moderate to severe COPD, and 698 who had MIs, including 339 type 1 MIs (T1MI) from a ruptured plaque (54%), and 294 (46%) type 2 heart attacks (T2MI) from a supply-demand mismatch due to sepsis or some other problem. In general, T2MIs are far more common in people with HIV.
COPD was associated with a greater than twofold increased risk of MI after adjustment for age, sex, viral load, nadir CD4 count, hypertension, and other confounders. The risk dropped slightly when smoking – both current smoking and pack years – was added to the model (adjusted hazard ratio 1.88, 95% confidence interval, 1.34-2.63).
The association was particularly strong for T2MI, especially in the setting of bacteremia and sepsis, and unlike T1MI, it remained significant after adjustment for smoking.
The study establishes a link between COPD and MI in HIV, but it could not answer what’s going on. Chronic inflammation from the virus could be at play, but the team also found hints of inadequate COPD management.
“About 60% of patients were on inhalers ... but only about 25% of them were on long-acting inhalers. 75% were only on short-acting.” That’s a problem because long-acting inhalers are needed to control exacerbations, Dr. Crothers said.
The study didn’t capture exacerbation rates, but increased rates could help explain the MI risk. Increased rates of pneumonia could as well, since pneumonia is a common cause of sepsis.
“We need to better manage complications of COPD in this population. I think optimizing long-term COPD management could have many beneficial effects,” Dr. Crothers said.
The National Institutes of Health funded the work. Dr. Crothers had no disclosures.
SOURCE: Crothers K et al. CROI 2019, Abstract 31.
REPORTING FROM CROI 2019
Higher dose of checkpoint inhibitor every 4 weeks feasible in NSCLC
SAN FRANCISCO – For patients with advanced non–small cell lung cancer (NSCLC) who previously had disease control with the checkpoint inhibitor nivolumab (Opdivo), second-line nivolumab at a higher dose every 4 weeks appeared to be comparable in efficacy and safety with standard-dose nivolumab every 2 weeks.
The key word in that last sentence is “appeared,” because the Checkmate 384 trial that was designed to show noninferiority of the every-4-weeks regimen lacked the statistical muscle to get the job done, reported Edward B. Garon, MD, from the University of California, Los Angeles.
“In many respects, extending the dosing frequency of nivolumab fulfills some of the promise of immunotherapy: The idea that we would be able to decrease the medicalization of the lives of our patients. For some people this would lead to them being able to resume a more normal work schedule, and for other people it would allow them to do things for fun, like travel on trips that would take longer than a couple of weeks,” he said at the American Society of Clinical Oncology (ASCO) – Society for Immunotherapy of Cancer (SITC): Clinical Immuno-Oncology Symposium.
However, because of difficulties in recruitment, the investigators had to stop enrollment early and settle for a sample size of 363 patients, instead of the 600 planned that would be necessary to meet a 10% noninferiority margin and one-sided 95% confidence interval. Thus, the trial analysis can only be reported as descriptive rather than definitive, Dr. Garon acknowledged.
Nivolumab is approved at a fixed dose of 240 mg every 2 weeks for the treatment of multiple tumor types in several different nations, and in the United States and Canada it is approved at a dose of 480 mg every 4 weeks for the treatment of NSCLC.
The CheckMate 384 study enrolled patients with advanced or metastatic NSCLC who had received 3 mg/kg or 240 mg of nivolumab every 2 weeks for up to 1 year. The patients had to have had relatively good performance status (Eastern Cooperative Oncology Group 0-2) and two consecutive assessments of either complete response, partial response, or stable disease.
The patients were stratified by tumor histology (squamous or nonsquamous) and response to prior nivolumab therapy at randomization, and were then randomized to receive nivolumab 240 mg every 2 weeks or 480 mg every 4 weeks until disease progression or unacceptable toxicity for up to 2 years.
Dr. Garon presented an interim analysis including data on 329 of the 363 patients; the final analysis will occur after all patients have had a minimum of 12 months of follow-up. Here, he reported on 6-month progression-free survival, a coprimary endpoint with 12-month PFS.
After a median follow-up of 9.5 months in the Q4-week group and 10.2 months in the Q2-week group, the 6-month PFS rates were identical between the two dosing strategies, at 72%. The median PFS was 12.1 months and 12.2 months, respectively.
“Although the study is no longer formally powered to show noninferiority, there’s certainly nothing in these curves that makes me concerned that this 480 mg every-4-week dose would be inferior,” Dr. Garon said.
There was a slightly higher rate of treatment-related adverse events of any grade in the lower, more frequent dose group: 48% in the Q4-week versus 61% in the Q2-week arm. The respective rates of grade 3 or 4 adverse events were 8% and 12%. Rates of serious adverse events and events leading to treatment discontinuation were similar between the group; there were no treatment-related deaths.
The investigators hypothesize that the higher rate of overall events in the lower-dose group may be attributable to more frequent visits and more opportunities to report adverse events, Dr. Garon said.
“Overall, the clinical data are in agreement with the pharmacokinetic modeling and give further evidence for this 480 mg every 4 week nivolumab dosing option,” he concluded.
The study was supported by Bristol-Myers Squibb. Dr. Garon reported receiving research support from Bristol-Myers Squibb and others and consulting fees from Dracen Pharmaceuticals.
SOURCE: Garon EB et al. ASCO-SITC, Abstract 100.
SAN FRANCISCO – For patients with advanced non–small cell lung cancer (NSCLC) who previously had disease control with the checkpoint inhibitor nivolumab (Opdivo), second-line nivolumab at a higher dose every 4 weeks appeared to be comparable in efficacy and safety with standard-dose nivolumab every 2 weeks.
The key word in that last sentence is “appeared,” because the Checkmate 384 trial that was designed to show noninferiority of the every-4-weeks regimen lacked the statistical muscle to get the job done, reported Edward B. Garon, MD, from the University of California, Los Angeles.
“In many respects, extending the dosing frequency of nivolumab fulfills some of the promise of immunotherapy: The idea that we would be able to decrease the medicalization of the lives of our patients. For some people this would lead to them being able to resume a more normal work schedule, and for other people it would allow them to do things for fun, like travel on trips that would take longer than a couple of weeks,” he said at the American Society of Clinical Oncology (ASCO) – Society for Immunotherapy of Cancer (SITC): Clinical Immuno-Oncology Symposium.
However, because of difficulties in recruitment, the investigators had to stop enrollment early and settle for a sample size of 363 patients, instead of the 600 planned that would be necessary to meet a 10% noninferiority margin and one-sided 95% confidence interval. Thus, the trial analysis can only be reported as descriptive rather than definitive, Dr. Garon acknowledged.
Nivolumab is approved at a fixed dose of 240 mg every 2 weeks for the treatment of multiple tumor types in several different nations, and in the United States and Canada it is approved at a dose of 480 mg every 4 weeks for the treatment of NSCLC.
The CheckMate 384 study enrolled patients with advanced or metastatic NSCLC who had received 3 mg/kg or 240 mg of nivolumab every 2 weeks for up to 1 year. The patients had to have had relatively good performance status (Eastern Cooperative Oncology Group 0-2) and two consecutive assessments of either complete response, partial response, or stable disease.
The patients were stratified by tumor histology (squamous or nonsquamous) and response to prior nivolumab therapy at randomization, and were then randomized to receive nivolumab 240 mg every 2 weeks or 480 mg every 4 weeks until disease progression or unacceptable toxicity for up to 2 years.
Dr. Garon presented an interim analysis including data on 329 of the 363 patients; the final analysis will occur after all patients have had a minimum of 12 months of follow-up. Here, he reported on 6-month progression-free survival, a coprimary endpoint with 12-month PFS.
After a median follow-up of 9.5 months in the Q4-week group and 10.2 months in the Q2-week group, the 6-month PFS rates were identical between the two dosing strategies, at 72%. The median PFS was 12.1 months and 12.2 months, respectively.
“Although the study is no longer formally powered to show noninferiority, there’s certainly nothing in these curves that makes me concerned that this 480 mg every-4-week dose would be inferior,” Dr. Garon said.
There was a slightly higher rate of treatment-related adverse events of any grade in the lower, more frequent dose group: 48% in the Q4-week versus 61% in the Q2-week arm. The respective rates of grade 3 or 4 adverse events were 8% and 12%. Rates of serious adverse events and events leading to treatment discontinuation were similar between the group; there were no treatment-related deaths.
The investigators hypothesize that the higher rate of overall events in the lower-dose group may be attributable to more frequent visits and more opportunities to report adverse events, Dr. Garon said.
“Overall, the clinical data are in agreement with the pharmacokinetic modeling and give further evidence for this 480 mg every 4 week nivolumab dosing option,” he concluded.
The study was supported by Bristol-Myers Squibb. Dr. Garon reported receiving research support from Bristol-Myers Squibb and others and consulting fees from Dracen Pharmaceuticals.
SOURCE: Garon EB et al. ASCO-SITC, Abstract 100.
SAN FRANCISCO – For patients with advanced non–small cell lung cancer (NSCLC) who previously had disease control with the checkpoint inhibitor nivolumab (Opdivo), second-line nivolumab at a higher dose every 4 weeks appeared to be comparable in efficacy and safety with standard-dose nivolumab every 2 weeks.
The key word in that last sentence is “appeared,” because the Checkmate 384 trial that was designed to show noninferiority of the every-4-weeks regimen lacked the statistical muscle to get the job done, reported Edward B. Garon, MD, from the University of California, Los Angeles.
“In many respects, extending the dosing frequency of nivolumab fulfills some of the promise of immunotherapy: The idea that we would be able to decrease the medicalization of the lives of our patients. For some people this would lead to them being able to resume a more normal work schedule, and for other people it would allow them to do things for fun, like travel on trips that would take longer than a couple of weeks,” he said at the American Society of Clinical Oncology (ASCO) – Society for Immunotherapy of Cancer (SITC): Clinical Immuno-Oncology Symposium.
However, because of difficulties in recruitment, the investigators had to stop enrollment early and settle for a sample size of 363 patients, instead of the 600 planned that would be necessary to meet a 10% noninferiority margin and one-sided 95% confidence interval. Thus, the trial analysis can only be reported as descriptive rather than definitive, Dr. Garon acknowledged.
Nivolumab is approved at a fixed dose of 240 mg every 2 weeks for the treatment of multiple tumor types in several different nations, and in the United States and Canada it is approved at a dose of 480 mg every 4 weeks for the treatment of NSCLC.
The CheckMate 384 study enrolled patients with advanced or metastatic NSCLC who had received 3 mg/kg or 240 mg of nivolumab every 2 weeks for up to 1 year. The patients had to have had relatively good performance status (Eastern Cooperative Oncology Group 0-2) and two consecutive assessments of either complete response, partial response, or stable disease.
The patients were stratified by tumor histology (squamous or nonsquamous) and response to prior nivolumab therapy at randomization, and were then randomized to receive nivolumab 240 mg every 2 weeks or 480 mg every 4 weeks until disease progression or unacceptable toxicity for up to 2 years.
Dr. Garon presented an interim analysis including data on 329 of the 363 patients; the final analysis will occur after all patients have had a minimum of 12 months of follow-up. Here, he reported on 6-month progression-free survival, a coprimary endpoint with 12-month PFS.
After a median follow-up of 9.5 months in the Q4-week group and 10.2 months in the Q2-week group, the 6-month PFS rates were identical between the two dosing strategies, at 72%. The median PFS was 12.1 months and 12.2 months, respectively.
“Although the study is no longer formally powered to show noninferiority, there’s certainly nothing in these curves that makes me concerned that this 480 mg every-4-week dose would be inferior,” Dr. Garon said.
There was a slightly higher rate of treatment-related adverse events of any grade in the lower, more frequent dose group: 48% in the Q4-week versus 61% in the Q2-week arm. The respective rates of grade 3 or 4 adverse events were 8% and 12%. Rates of serious adverse events and events leading to treatment discontinuation were similar between the group; there were no treatment-related deaths.
The investigators hypothesize that the higher rate of overall events in the lower-dose group may be attributable to more frequent visits and more opportunities to report adverse events, Dr. Garon said.
“Overall, the clinical data are in agreement with the pharmacokinetic modeling and give further evidence for this 480 mg every 4 week nivolumab dosing option,” he concluded.
The study was supported by Bristol-Myers Squibb. Dr. Garon reported receiving research support from Bristol-Myers Squibb and others and consulting fees from Dracen Pharmaceuticals.
SOURCE: Garon EB et al. ASCO-SITC, Abstract 100.
REPORTING FROM ASCO-SITC
High-calorie diet may worsen Wilson disease
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Glyceryl trinitrate does not improve outcomes of ischemic stroke
HONOLULU – , according to data presented at the International Stroke Conference sponsored by the American Heart Association. Results suggest that GTN causes adverse effects in patients with intracerebral hemorrhage (ICH), but this observation is not definitive, according to the researchers. Study results were published online ahead of print Feb. 6 in the Lancet.
Nitric oxide is a regulatory molecule that has vasoactive effects and promotes blood pressure reduction. Vascular levels of nitric oxide are low in stroke, which suggests that the molecule may be a target for stroke treatment. GTN, a nitric oxide donor, lowered blood pressure and improved functional outcome among patients with acute stroke in the phase 2 Rapid Intervention with GTN in Hypertensive Stroke Trial (RIGHT).
Philip Bath, MD, Stroke Association Professor of Stroke Medicine at the University of Nottingham (England), and colleagues conducted the RIGHT-2 study to evaluate the safety and efficacy of GTN when administered early after onset of suspected stroke. Paramedics randomized patients in equal groups to a GTN patch or a sham patch in the ambulance. Three more patches were administered in the hospital on the following days. Active and sham patches looked similar and had no writing on them, thus ensuring effective blinding upon administration. Investigators followed up patients by telephone at 90 days to assess the modified Rankin Scale score and markers of disability, mood, cognition, and quality of life.
Eligible participants were adults who had dialed emergency services, independently or with assistance, because of a possible stroke. They had a Face, Arm, Speech, Time (FAST) score of 2 or 3, were within 4 hours of onset, and had a systolic blood pressure greater than 120 mm Hg. Patients from nursing homes, those with hypoglycemia, those who were unconscious, and those with a witnessed seizure were excluded.
Dr. Bath and colleagues planned to enroll 850 patients from five ambulance services in 30 hospitals across the United Kingdom. Data were to be examined through an intention-to-treat analysis. During the trial, however, the investigators observed that the rate of stroke mimics was 26%, rather than the 12% that they had anticipated. To ensure the proper power for the study, the investigators increased the sample size to 1,149 patients. They also changed the planned data analysis from intention-to-treat to hierarchical analysis. Specifically, the researchers planned to perform the primary analysis in patients with stroke or TIA. If the results were positive, then they would perform a standard intention-to-treat analysis.
More than 99% of patients received the first patch. Approximately 57% of the population received the first two patches. One reason for this decrease in adherence was that many patients were discharged from the hospital with a TIA or a stroke mimic. Participants’ average age was 72. The median time from onset to randomization was 71 minutes, and the median time to treatment was 73 minutes. Participants’ mean systolic blood pressure was 162 mm Hg. Approximately 60% of the patients had a FAST score of 3. About 50% of participants had ischemic stroke, 13% had ICH, 10% had TIA, and 26% had stroke mimics.
At 1 hour after treatment initiation, systolic blood pressure decreased by 6.2 mm Hg and diastolic blood pressure decreased by 2.7 mm Hg among patients who received GTN, compared with controls. At one day, the differences were 5.2 mm Hg and 2.5 mm Hg, respectively, in treated patients, compared with controls. Blood pressure became similar between groups thereafter, “in part because of the tachyphylaxis that we know happens with GTN,” said Dr. Bath.
The researchers found no evidence of an effect of GTN on functional outcome at 90 days in participants with stroke or transient ischemic attack. The adjusted common odds ratio of poor outcome was 1.25 in the GTN group, compared with the control group (95 % confidence interval, 0.97-1.60; P = .083). “We were close to getting a negative trial,” said Dr. Bath.
Subgroup analyses revealed differences in outcome according to the time to randomization. GTN had a negative effect in patients treated within 1 hour of onset. Results were neutral, but tended to be negative, in patients treated between 1 and 2 hours of onset. Results were neutral, but tended to be positive, among patients treated at more than 2 hours after onset. There was no difference between groups in the rate of mortality.
One of the study’s limitations was its single-blind design. In addition, the trial was conducted in a single country, and the investigators changed the protocol after it was initiated. “We had a higher-than-expected [stroke] mimic rate, although I’m reassured by most experts that ... this is probably about right,” said Dr. Bath.
A potential reason for the neutral results is the negative effect that GTN had among patients with ICH, said Dr. Bath. “In that very early first hour, we are of course breaking a law that we learned in medical school, which is that the first part of hemostasis is spasm. We gave an antispasmodic: a vasodilator,” he added. “That is speculation.”
The trial was funded by the British Heart Foundation. Dr. Bath declared a modest ownership interest in Platelet Solutions and consultant or advisory board positions with Moleac, DiaMedica, Phagenesis, Nestle, and ReNeuron. The other investigators declared no conflicts of interest.
The RIGHT-2 trial shows the limitations of a prehospital enrollment model, wrote Karen C. Johnston, MD, professor of neurology at the University of Virginia in Charlottesville, and Valerie L. Durkalski-Mauldin, PhD, professor of medicine at Medical University of South Carolina in Charleston, in an editorial accompanying the RIGHT-2 trial results. The rate of nonstroke diagnoses was so high that it would have reduced the study’s power to assess the efficacy of glyceryl trinitrate (GTN), had the investigators not increased the sample size and changed the statistical analysis plan.
“Future prehospital trials need to consider the implications of enrolling, yet excluding, stroke mimics in the primary analysis,” said Dr. Johnston and Dr. Durkalski-Mauldin. Using telemedicine in the ambulance to facilitate direct contact between the stroke provider and the patient and emergency medical services provider could reduce the enrollment of patients with stroke mimics in clinical trials, they added. “Improved tools to exclude stroke mimics in the field have been difficult to develop and validate. The absence of imaging in most ambulances will continue to limit field personnel from definitively determining ischemic stroke from intracerebral hemorrhage, which will limit hyperacute trials to interventions presumed safe in both populations.”
In addition, the blood pressure reduction that GTN provided might not be clinically relevant, said Dr. Johnston and Dr. Durkalski-Mauldin. “The RIGHT-2 investigators report no difference in blood pressure at day 3 or day 4 of treatment, which might have been related to the very low adherence to study protocol by day 4.
“Regardless of these limitations, RIGHT-2 has provided high-level evidence that GTN given within 4 hours of onset does not significantly improve outcome in hyperacute patients presenting with possible stroke,” the authors concluded (Lancet. 2019 Feb 6. doi: 10.1016/
S0140-6736(19)30276-4). Dr. Johnston and Dr. Durkalski-Mauldin declared no conflicts of interest.
The RIGHT-2 trial shows the limitations of a prehospital enrollment model, wrote Karen C. Johnston, MD, professor of neurology at the University of Virginia in Charlottesville, and Valerie L. Durkalski-Mauldin, PhD, professor of medicine at Medical University of South Carolina in Charleston, in an editorial accompanying the RIGHT-2 trial results. The rate of nonstroke diagnoses was so high that it would have reduced the study’s power to assess the efficacy of glyceryl trinitrate (GTN), had the investigators not increased the sample size and changed the statistical analysis plan.
“Future prehospital trials need to consider the implications of enrolling, yet excluding, stroke mimics in the primary analysis,” said Dr. Johnston and Dr. Durkalski-Mauldin. Using telemedicine in the ambulance to facilitate direct contact between the stroke provider and the patient and emergency medical services provider could reduce the enrollment of patients with stroke mimics in clinical trials, they added. “Improved tools to exclude stroke mimics in the field have been difficult to develop and validate. The absence of imaging in most ambulances will continue to limit field personnel from definitively determining ischemic stroke from intracerebral hemorrhage, which will limit hyperacute trials to interventions presumed safe in both populations.”
In addition, the blood pressure reduction that GTN provided might not be clinically relevant, said Dr. Johnston and Dr. Durkalski-Mauldin. “The RIGHT-2 investigators report no difference in blood pressure at day 3 or day 4 of treatment, which might have been related to the very low adherence to study protocol by day 4.
“Regardless of these limitations, RIGHT-2 has provided high-level evidence that GTN given within 4 hours of onset does not significantly improve outcome in hyperacute patients presenting with possible stroke,” the authors concluded (Lancet. 2019 Feb 6. doi: 10.1016/
S0140-6736(19)30276-4). Dr. Johnston and Dr. Durkalski-Mauldin declared no conflicts of interest.
The RIGHT-2 trial shows the limitations of a prehospital enrollment model, wrote Karen C. Johnston, MD, professor of neurology at the University of Virginia in Charlottesville, and Valerie L. Durkalski-Mauldin, PhD, professor of medicine at Medical University of South Carolina in Charleston, in an editorial accompanying the RIGHT-2 trial results. The rate of nonstroke diagnoses was so high that it would have reduced the study’s power to assess the efficacy of glyceryl trinitrate (GTN), had the investigators not increased the sample size and changed the statistical analysis plan.
“Future prehospital trials need to consider the implications of enrolling, yet excluding, stroke mimics in the primary analysis,” said Dr. Johnston and Dr. Durkalski-Mauldin. Using telemedicine in the ambulance to facilitate direct contact between the stroke provider and the patient and emergency medical services provider could reduce the enrollment of patients with stroke mimics in clinical trials, they added. “Improved tools to exclude stroke mimics in the field have been difficult to develop and validate. The absence of imaging in most ambulances will continue to limit field personnel from definitively determining ischemic stroke from intracerebral hemorrhage, which will limit hyperacute trials to interventions presumed safe in both populations.”
In addition, the blood pressure reduction that GTN provided might not be clinically relevant, said Dr. Johnston and Dr. Durkalski-Mauldin. “The RIGHT-2 investigators report no difference in blood pressure at day 3 or day 4 of treatment, which might have been related to the very low adherence to study protocol by day 4.
“Regardless of these limitations, RIGHT-2 has provided high-level evidence that GTN given within 4 hours of onset does not significantly improve outcome in hyperacute patients presenting with possible stroke,” the authors concluded (Lancet. 2019 Feb 6. doi: 10.1016/
S0140-6736(19)30276-4). Dr. Johnston and Dr. Durkalski-Mauldin declared no conflicts of interest.
HONOLULU – , according to data presented at the International Stroke Conference sponsored by the American Heart Association. Results suggest that GTN causes adverse effects in patients with intracerebral hemorrhage (ICH), but this observation is not definitive, according to the researchers. Study results were published online ahead of print Feb. 6 in the Lancet.
Nitric oxide is a regulatory molecule that has vasoactive effects and promotes blood pressure reduction. Vascular levels of nitric oxide are low in stroke, which suggests that the molecule may be a target for stroke treatment. GTN, a nitric oxide donor, lowered blood pressure and improved functional outcome among patients with acute stroke in the phase 2 Rapid Intervention with GTN in Hypertensive Stroke Trial (RIGHT).
Philip Bath, MD, Stroke Association Professor of Stroke Medicine at the University of Nottingham (England), and colleagues conducted the RIGHT-2 study to evaluate the safety and efficacy of GTN when administered early after onset of suspected stroke. Paramedics randomized patients in equal groups to a GTN patch or a sham patch in the ambulance. Three more patches were administered in the hospital on the following days. Active and sham patches looked similar and had no writing on them, thus ensuring effective blinding upon administration. Investigators followed up patients by telephone at 90 days to assess the modified Rankin Scale score and markers of disability, mood, cognition, and quality of life.
Eligible participants were adults who had dialed emergency services, independently or with assistance, because of a possible stroke. They had a Face, Arm, Speech, Time (FAST) score of 2 or 3, were within 4 hours of onset, and had a systolic blood pressure greater than 120 mm Hg. Patients from nursing homes, those with hypoglycemia, those who were unconscious, and those with a witnessed seizure were excluded.
Dr. Bath and colleagues planned to enroll 850 patients from five ambulance services in 30 hospitals across the United Kingdom. Data were to be examined through an intention-to-treat analysis. During the trial, however, the investigators observed that the rate of stroke mimics was 26%, rather than the 12% that they had anticipated. To ensure the proper power for the study, the investigators increased the sample size to 1,149 patients. They also changed the planned data analysis from intention-to-treat to hierarchical analysis. Specifically, the researchers planned to perform the primary analysis in patients with stroke or TIA. If the results were positive, then they would perform a standard intention-to-treat analysis.
More than 99% of patients received the first patch. Approximately 57% of the population received the first two patches. One reason for this decrease in adherence was that many patients were discharged from the hospital with a TIA or a stroke mimic. Participants’ average age was 72. The median time from onset to randomization was 71 minutes, and the median time to treatment was 73 minutes. Participants’ mean systolic blood pressure was 162 mm Hg. Approximately 60% of the patients had a FAST score of 3. About 50% of participants had ischemic stroke, 13% had ICH, 10% had TIA, and 26% had stroke mimics.
At 1 hour after treatment initiation, systolic blood pressure decreased by 6.2 mm Hg and diastolic blood pressure decreased by 2.7 mm Hg among patients who received GTN, compared with controls. At one day, the differences were 5.2 mm Hg and 2.5 mm Hg, respectively, in treated patients, compared with controls. Blood pressure became similar between groups thereafter, “in part because of the tachyphylaxis that we know happens with GTN,” said Dr. Bath.
The researchers found no evidence of an effect of GTN on functional outcome at 90 days in participants with stroke or transient ischemic attack. The adjusted common odds ratio of poor outcome was 1.25 in the GTN group, compared with the control group (95 % confidence interval, 0.97-1.60; P = .083). “We were close to getting a negative trial,” said Dr. Bath.
Subgroup analyses revealed differences in outcome according to the time to randomization. GTN had a negative effect in patients treated within 1 hour of onset. Results were neutral, but tended to be negative, in patients treated between 1 and 2 hours of onset. Results were neutral, but tended to be positive, among patients treated at more than 2 hours after onset. There was no difference between groups in the rate of mortality.
One of the study’s limitations was its single-blind design. In addition, the trial was conducted in a single country, and the investigators changed the protocol after it was initiated. “We had a higher-than-expected [stroke] mimic rate, although I’m reassured by most experts that ... this is probably about right,” said Dr. Bath.
A potential reason for the neutral results is the negative effect that GTN had among patients with ICH, said Dr. Bath. “In that very early first hour, we are of course breaking a law that we learned in medical school, which is that the first part of hemostasis is spasm. We gave an antispasmodic: a vasodilator,” he added. “That is speculation.”
The trial was funded by the British Heart Foundation. Dr. Bath declared a modest ownership interest in Platelet Solutions and consultant or advisory board positions with Moleac, DiaMedica, Phagenesis, Nestle, and ReNeuron. The other investigators declared no conflicts of interest.
HONOLULU – , according to data presented at the International Stroke Conference sponsored by the American Heart Association. Results suggest that GTN causes adverse effects in patients with intracerebral hemorrhage (ICH), but this observation is not definitive, according to the researchers. Study results were published online ahead of print Feb. 6 in the Lancet.
Nitric oxide is a regulatory molecule that has vasoactive effects and promotes blood pressure reduction. Vascular levels of nitric oxide are low in stroke, which suggests that the molecule may be a target for stroke treatment. GTN, a nitric oxide donor, lowered blood pressure and improved functional outcome among patients with acute stroke in the phase 2 Rapid Intervention with GTN in Hypertensive Stroke Trial (RIGHT).
Philip Bath, MD, Stroke Association Professor of Stroke Medicine at the University of Nottingham (England), and colleagues conducted the RIGHT-2 study to evaluate the safety and efficacy of GTN when administered early after onset of suspected stroke. Paramedics randomized patients in equal groups to a GTN patch or a sham patch in the ambulance. Three more patches were administered in the hospital on the following days. Active and sham patches looked similar and had no writing on them, thus ensuring effective blinding upon administration. Investigators followed up patients by telephone at 90 days to assess the modified Rankin Scale score and markers of disability, mood, cognition, and quality of life.
Eligible participants were adults who had dialed emergency services, independently or with assistance, because of a possible stroke. They had a Face, Arm, Speech, Time (FAST) score of 2 or 3, were within 4 hours of onset, and had a systolic blood pressure greater than 120 mm Hg. Patients from nursing homes, those with hypoglycemia, those who were unconscious, and those with a witnessed seizure were excluded.
Dr. Bath and colleagues planned to enroll 850 patients from five ambulance services in 30 hospitals across the United Kingdom. Data were to be examined through an intention-to-treat analysis. During the trial, however, the investigators observed that the rate of stroke mimics was 26%, rather than the 12% that they had anticipated. To ensure the proper power for the study, the investigators increased the sample size to 1,149 patients. They also changed the planned data analysis from intention-to-treat to hierarchical analysis. Specifically, the researchers planned to perform the primary analysis in patients with stroke or TIA. If the results were positive, then they would perform a standard intention-to-treat analysis.
More than 99% of patients received the first patch. Approximately 57% of the population received the first two patches. One reason for this decrease in adherence was that many patients were discharged from the hospital with a TIA or a stroke mimic. Participants’ average age was 72. The median time from onset to randomization was 71 minutes, and the median time to treatment was 73 minutes. Participants’ mean systolic blood pressure was 162 mm Hg. Approximately 60% of the patients had a FAST score of 3. About 50% of participants had ischemic stroke, 13% had ICH, 10% had TIA, and 26% had stroke mimics.
At 1 hour after treatment initiation, systolic blood pressure decreased by 6.2 mm Hg and diastolic blood pressure decreased by 2.7 mm Hg among patients who received GTN, compared with controls. At one day, the differences were 5.2 mm Hg and 2.5 mm Hg, respectively, in treated patients, compared with controls. Blood pressure became similar between groups thereafter, “in part because of the tachyphylaxis that we know happens with GTN,” said Dr. Bath.
The researchers found no evidence of an effect of GTN on functional outcome at 90 days in participants with stroke or transient ischemic attack. The adjusted common odds ratio of poor outcome was 1.25 in the GTN group, compared with the control group (95 % confidence interval, 0.97-1.60; P = .083). “We were close to getting a negative trial,” said Dr. Bath.
Subgroup analyses revealed differences in outcome according to the time to randomization. GTN had a negative effect in patients treated within 1 hour of onset. Results were neutral, but tended to be negative, in patients treated between 1 and 2 hours of onset. Results were neutral, but tended to be positive, among patients treated at more than 2 hours after onset. There was no difference between groups in the rate of mortality.
One of the study’s limitations was its single-blind design. In addition, the trial was conducted in a single country, and the investigators changed the protocol after it was initiated. “We had a higher-than-expected [stroke] mimic rate, although I’m reassured by most experts that ... this is probably about right,” said Dr. Bath.
A potential reason for the neutral results is the negative effect that GTN had among patients with ICH, said Dr. Bath. “In that very early first hour, we are of course breaking a law that we learned in medical school, which is that the first part of hemostasis is spasm. We gave an antispasmodic: a vasodilator,” he added. “That is speculation.”
The trial was funded by the British Heart Foundation. Dr. Bath declared a modest ownership interest in Platelet Solutions and consultant or advisory board positions with Moleac, DiaMedica, Phagenesis, Nestle, and ReNeuron. The other investigators declared no conflicts of interest.
REPORTING FROM ISC 2019
Epicutaneous milk immunotherapy can resolve pediatric eosinophilic esophagitis
SAN FRANCISCO – Clinicians safely used epicutaneous immunotherapy to resolve eosinophilic esophagitis in children and teens secondary to milk consumption in a placebo-controlled, pilot study that included 20 patients.
Following the randomized phase of the study, all 19 patients who continued to participate began an 11-month open-label phase of epicutaneous immunotherapy to milk. At the end of this open-label phase, nine patients (47%) followed in this phase showed a substantial cut in their eosinophilic esophagitis (EoE) response to milk, with fewer than 15 eosinophils in a high-powered field, said Jonathan M. Spergel, MD, chief of the allergy section and Stuart E. Starr Chair of Pediatrics at the Children’s Hospital of Philadelphia, while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. An immunologic response of this sort would likely correlate with substantial clinical benefit.
“I’m happy with a 47% response,” Dr. Spergel said, adding that the responding patients “tolerate milk without symptoms, and there is really no risk” from this form of immunotherapy, which produced no serious adverse effects and caused 1 of 15 patients to stop treatment because of a treatment-related effect during the randomized phase. The most common adverse reaction was gastrointestinal symptoms, but these were just marginally more common among patients on active treatment than in control patients.
In contrast, oral immunotherapy with milk has been ineffective in children with an EoE milk reaction, and results from subcutaneous or sublingual immunotherapy for this form of milk allergy haven’t been reported, he said. The most common, current approaches to managing EoE from milk in children are either milk avoidance or treatment to reduce inflammation.
The epicutaneous approach “uses substantially lower dosing [micrograms vs. milligrams], avoids oral allergen ingestion, and may have a more advantageous adverse event profile and better adherence than other therapies,” according to a recent report that tested epicutaneous immunotherapy for peanut allergy in a phase 3 trial with 356 children (JAMA. 2019 Feb 22. doi: 10.1001/jama.2019.1113). The Viaskin Milk system tested in the current milk study involves placing a disc coated with 500 mcg of lyophilized milk protein on the skin for a gradually increasing number of hours daily until the disc is worn continuously, with daily changes of the disk. On the skin, the protein on the disk interacts with epidermal Langerhans cells to trigger desensitization.
The Milk Patch for Eosinophilic Esophagitis (SMILEE) study enrolled 20 patients at Children’s Hospital aged 4-17 years old and had milk-induced EoE, and randomized 15 to receive active epicutaneous immunotherapy to milk and 5 to receive placebo treatment. The protocol called for 9 month of epicutaneous immunotherapy without any milk exposure, followed by 2 months of continued treatment coupled with at least 240 mL of milk consumption daily. At the end of 2 months the researchers performed an esophageal biopsy on each patient to determine eosinophil density in the tissue. The study’s primary endpoint was the number of eosinophils in a high-powered field.
During the randomized phase, 8 of the 15 patients assigned to active treatment and 3 of 5 patients assigned to the placebo arm had violations of the treatment protocol, the diet protocol, or both. A per protocol analysis that focused on the seven actively treated and two placebo patients who adhered to the protocol showed a mean eosinophil count of 26 cells in patients on active treatment and 95 cells among the controls, a statistically significant difference. However, for the intention-to-treat analysis, which included all 20 enrolled patients, the primary endpoint showed no significant difference in eosinophil counts between the two study arms.
Although Dr. Spergel said that he was not aware of the developing company’s plans for further study of epicutaneous milk immunotherapy, from a scientific standpoint the next step should be a phase 2 or phase 2/3 trial for safety and efficacy. EoE was historically considered a rare disease, but a 2015 review of the condition called it “one of the most common conditions diagnosed during the assessment of feeding problems in children” (New Engl J Med. 2015 Oct 22;373[17]:1640-8).
The study was funded by DBV Technologies, which is developing the epicutaneous immunotherapy system. Dr. Spergel has been a consultant to and has received research funding from DBV Technologies.
SOURCE: Spergel JM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB430.
SAN FRANCISCO – Clinicians safely used epicutaneous immunotherapy to resolve eosinophilic esophagitis in children and teens secondary to milk consumption in a placebo-controlled, pilot study that included 20 patients.
Following the randomized phase of the study, all 19 patients who continued to participate began an 11-month open-label phase of epicutaneous immunotherapy to milk. At the end of this open-label phase, nine patients (47%) followed in this phase showed a substantial cut in their eosinophilic esophagitis (EoE) response to milk, with fewer than 15 eosinophils in a high-powered field, said Jonathan M. Spergel, MD, chief of the allergy section and Stuart E. Starr Chair of Pediatrics at the Children’s Hospital of Philadelphia, while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. An immunologic response of this sort would likely correlate with substantial clinical benefit.
“I’m happy with a 47% response,” Dr. Spergel said, adding that the responding patients “tolerate milk without symptoms, and there is really no risk” from this form of immunotherapy, which produced no serious adverse effects and caused 1 of 15 patients to stop treatment because of a treatment-related effect during the randomized phase. The most common adverse reaction was gastrointestinal symptoms, but these were just marginally more common among patients on active treatment than in control patients.
In contrast, oral immunotherapy with milk has been ineffective in children with an EoE milk reaction, and results from subcutaneous or sublingual immunotherapy for this form of milk allergy haven’t been reported, he said. The most common, current approaches to managing EoE from milk in children are either milk avoidance or treatment to reduce inflammation.
The epicutaneous approach “uses substantially lower dosing [micrograms vs. milligrams], avoids oral allergen ingestion, and may have a more advantageous adverse event profile and better adherence than other therapies,” according to a recent report that tested epicutaneous immunotherapy for peanut allergy in a phase 3 trial with 356 children (JAMA. 2019 Feb 22. doi: 10.1001/jama.2019.1113). The Viaskin Milk system tested in the current milk study involves placing a disc coated with 500 mcg of lyophilized milk protein on the skin for a gradually increasing number of hours daily until the disc is worn continuously, with daily changes of the disk. On the skin, the protein on the disk interacts with epidermal Langerhans cells to trigger desensitization.
The Milk Patch for Eosinophilic Esophagitis (SMILEE) study enrolled 20 patients at Children’s Hospital aged 4-17 years old and had milk-induced EoE, and randomized 15 to receive active epicutaneous immunotherapy to milk and 5 to receive placebo treatment. The protocol called for 9 month of epicutaneous immunotherapy without any milk exposure, followed by 2 months of continued treatment coupled with at least 240 mL of milk consumption daily. At the end of 2 months the researchers performed an esophageal biopsy on each patient to determine eosinophil density in the tissue. The study’s primary endpoint was the number of eosinophils in a high-powered field.
During the randomized phase, 8 of the 15 patients assigned to active treatment and 3 of 5 patients assigned to the placebo arm had violations of the treatment protocol, the diet protocol, or both. A per protocol analysis that focused on the seven actively treated and two placebo patients who adhered to the protocol showed a mean eosinophil count of 26 cells in patients on active treatment and 95 cells among the controls, a statistically significant difference. However, for the intention-to-treat analysis, which included all 20 enrolled patients, the primary endpoint showed no significant difference in eosinophil counts between the two study arms.
Although Dr. Spergel said that he was not aware of the developing company’s plans for further study of epicutaneous milk immunotherapy, from a scientific standpoint the next step should be a phase 2 or phase 2/3 trial for safety and efficacy. EoE was historically considered a rare disease, but a 2015 review of the condition called it “one of the most common conditions diagnosed during the assessment of feeding problems in children” (New Engl J Med. 2015 Oct 22;373[17]:1640-8).
The study was funded by DBV Technologies, which is developing the epicutaneous immunotherapy system. Dr. Spergel has been a consultant to and has received research funding from DBV Technologies.
SOURCE: Spergel JM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB430.
SAN FRANCISCO – Clinicians safely used epicutaneous immunotherapy to resolve eosinophilic esophagitis in children and teens secondary to milk consumption in a placebo-controlled, pilot study that included 20 patients.
Following the randomized phase of the study, all 19 patients who continued to participate began an 11-month open-label phase of epicutaneous immunotherapy to milk. At the end of this open-label phase, nine patients (47%) followed in this phase showed a substantial cut in their eosinophilic esophagitis (EoE) response to milk, with fewer than 15 eosinophils in a high-powered field, said Jonathan M. Spergel, MD, chief of the allergy section and Stuart E. Starr Chair of Pediatrics at the Children’s Hospital of Philadelphia, while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. An immunologic response of this sort would likely correlate with substantial clinical benefit.
“I’m happy with a 47% response,” Dr. Spergel said, adding that the responding patients “tolerate milk without symptoms, and there is really no risk” from this form of immunotherapy, which produced no serious adverse effects and caused 1 of 15 patients to stop treatment because of a treatment-related effect during the randomized phase. The most common adverse reaction was gastrointestinal symptoms, but these were just marginally more common among patients on active treatment than in control patients.
In contrast, oral immunotherapy with milk has been ineffective in children with an EoE milk reaction, and results from subcutaneous or sublingual immunotherapy for this form of milk allergy haven’t been reported, he said. The most common, current approaches to managing EoE from milk in children are either milk avoidance or treatment to reduce inflammation.
The epicutaneous approach “uses substantially lower dosing [micrograms vs. milligrams], avoids oral allergen ingestion, and may have a more advantageous adverse event profile and better adherence than other therapies,” according to a recent report that tested epicutaneous immunotherapy for peanut allergy in a phase 3 trial with 356 children (JAMA. 2019 Feb 22. doi: 10.1001/jama.2019.1113). The Viaskin Milk system tested in the current milk study involves placing a disc coated with 500 mcg of lyophilized milk protein on the skin for a gradually increasing number of hours daily until the disc is worn continuously, with daily changes of the disk. On the skin, the protein on the disk interacts with epidermal Langerhans cells to trigger desensitization.
The Milk Patch for Eosinophilic Esophagitis (SMILEE) study enrolled 20 patients at Children’s Hospital aged 4-17 years old and had milk-induced EoE, and randomized 15 to receive active epicutaneous immunotherapy to milk and 5 to receive placebo treatment. The protocol called for 9 month of epicutaneous immunotherapy without any milk exposure, followed by 2 months of continued treatment coupled with at least 240 mL of milk consumption daily. At the end of 2 months the researchers performed an esophageal biopsy on each patient to determine eosinophil density in the tissue. The study’s primary endpoint was the number of eosinophils in a high-powered field.
During the randomized phase, 8 of the 15 patients assigned to active treatment and 3 of 5 patients assigned to the placebo arm had violations of the treatment protocol, the diet protocol, or both. A per protocol analysis that focused on the seven actively treated and two placebo patients who adhered to the protocol showed a mean eosinophil count of 26 cells in patients on active treatment and 95 cells among the controls, a statistically significant difference. However, for the intention-to-treat analysis, which included all 20 enrolled patients, the primary endpoint showed no significant difference in eosinophil counts between the two study arms.
Although Dr. Spergel said that he was not aware of the developing company’s plans for further study of epicutaneous milk immunotherapy, from a scientific standpoint the next step should be a phase 2 or phase 2/3 trial for safety and efficacy. EoE was historically considered a rare disease, but a 2015 review of the condition called it “one of the most common conditions diagnosed during the assessment of feeding problems in children” (New Engl J Med. 2015 Oct 22;373[17]:1640-8).
The study was funded by DBV Technologies, which is developing the epicutaneous immunotherapy system. Dr. Spergel has been a consultant to and has received research funding from DBV Technologies.
SOURCE: Spergel JM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB430.
REPORTING FROM AAAAI 2019
Key clinical point:
Major finding: After 11 months of open-label treatment, 9 of 19 patients resolved their eosinophilic esophagitis reaction to milk.
Study details: A 2-year, single-center study of epicutaneous milk immunotherapy in 20 children with milk-induced eosinophilic esophagitis.
Disclosures: The study was funded by DBV Technologies, which is developing the epicutaneous immunotherapy system. Dr. Spergel has been a consultant to and has received research funding from DBV Technologies.
Source: Spergel JM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB430.
Poor asthma control during pregnancy trims live birth rate
SAN FRANCISCO – and among the live births had a significantly increased rate of both preterm delivery and neonatal intensive care admissions, according to a review of insurance claims data for more than 1 million American women during 2011-2015.
On the other hand, asthma severity, which the researchers inferred based on the type and amount of treatment patients received, showed essentially no link with the live birth rate, Jennifer Yland said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“The findings add to the body of evidence that relate poor asthma control to an increased risk for pregnancy complications.” explained Michael X. Schatz, MD, an allergist at Kaiser Permanente of Southern California, in San Diego, and a coauthor of the study.
Results from several prior studies had shown links between asthma and an increased rate of preterm birth, “but the larger, more generalizable population is a strength of the current findings. Results from prior studies have less frequently shown a link between asthma during pregnancy and neonatal ICU admissions,” he added.“The findings strengthen the case for good asthma control during pregnancy.”
For their review, Ms. Yland and her coauthors used insurance claims data from privately-insured American women aged 12-55 years who were pregnant and had drug prescription records during the study period. The database included 996,861 women without an asthma diagnosis and 29,882 women diagnosed with asthma. The analysis excluded women diagnosed with chronic obstructive pulmonary disease at least twice during pregnancy.
To analyze the pregnancy outcomes by asthma severity Ms. Yland and her associates divided the asthma patients into five subgroups based on the drug regimens they were on during pregnancy as a surrogate marker of disease severity. This analysis showed no relationship between disease severity and live birth rate.
The researchers also ran an analysis that divided patients into the quality of their management during pregnancy – either good or poor – based on either of two markers of poor control: filling five or more prescriptions for a short-acting beta-antagonist, or at least one exacerbation episode defined as an asthma-related emergency department visit, hospitalization, or need for oral corticosteroid treatment. By these criteria 7,135 (24%) of the pregnant women with asthma were poorly controlled. The live birth rate was 74% among women without asthma, 71% among those with well-controlled asthma, and 68% among women with poorly-controlled asthma, reported Ms. Yland, a researcher at the Harvard T.H. Chan School of Public Health in Boston.
In a multivariate analysis that adjusted for demographic differences and comorbidities, women with poorly-controlled asthma had preterm delivery a statistically significant 30% more often than did women with well-controlled asthma, and the rate of neonatal ICU admissions was a significant 24% higher in women with poorly-controlled asthma, compared with women who had well-controlled asthma. However, the rates of small-for-gestational-age infants and infants with congenital malformations was not significantly different between the well-controlled and poorly-controlled subgroups.
The finding that almost a quarter of the pregnant women in the study were poorly controlled wasn’t surprising, Dr. Schatz said in an interview. In some studies as many as half the asthma patients have poor control.
The 24% rate of poor asthma control during pregnancy in the studied women is “most likely an underestimate of poor control in the general population” because the study used data from women with commercial health insurance, noted Sonia Hernandez-Diaz, MD, lead investigator for the study and professor of epidemiology at Harvard T.H. Chan School of Public Health. “More disadvantaged populations, such as pregnant women on Medicaid, tend to have worse control.”
Barriers to good asthma control during pregnancy include smoking, weight gain, undertreatment, poor adherence, and viral infection. The overall approach to managing asthma during pregnancy is the same as when women are not pregnant, although certain asthma medications have a better safety record during pregnancy. “The most reassuring data exist for albuterol and inhaled steroids, particularly budesonide and fluticasone. Reassuring data also exist for the long-acting beta agonists salmeterol and formoterol, which are combined with inhaled steroids, and for montelukast,” Dr. Schatz said.
This is the first study to assess the impact of asthma management on pregnancy outcome in such a large population. The large number of women included provided a lot of statistical power and allowed the analyses to control for several potential confounders, Ms. Yland noted in an interview. She plans to expand the analysis with Medicaid data to try to further increase the generalizability and precision of the findings.
The study was funded by GlaxoSmithKline, and a coauthor of the study is a company employee. Ms. Yland had no disclosures. Dr. Schatz has received research funding from ALK, AstraZeneca, Medimmune, GlaxoSmithKline, and Merck. Dr. Hernandez-Diaz has been a consultant to Boehringer Ingelheim, Roche, and UCB, and has received research funding from GlaxoSmithKline, Lilly, and Pfizer.
SOURCE: Yland J et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB422.
SAN FRANCISCO – and among the live births had a significantly increased rate of both preterm delivery and neonatal intensive care admissions, according to a review of insurance claims data for more than 1 million American women during 2011-2015.
On the other hand, asthma severity, which the researchers inferred based on the type and amount of treatment patients received, showed essentially no link with the live birth rate, Jennifer Yland said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“The findings add to the body of evidence that relate poor asthma control to an increased risk for pregnancy complications.” explained Michael X. Schatz, MD, an allergist at Kaiser Permanente of Southern California, in San Diego, and a coauthor of the study.
Results from several prior studies had shown links between asthma and an increased rate of preterm birth, “but the larger, more generalizable population is a strength of the current findings. Results from prior studies have less frequently shown a link between asthma during pregnancy and neonatal ICU admissions,” he added.“The findings strengthen the case for good asthma control during pregnancy.”
For their review, Ms. Yland and her coauthors used insurance claims data from privately-insured American women aged 12-55 years who were pregnant and had drug prescription records during the study period. The database included 996,861 women without an asthma diagnosis and 29,882 women diagnosed with asthma. The analysis excluded women diagnosed with chronic obstructive pulmonary disease at least twice during pregnancy.
To analyze the pregnancy outcomes by asthma severity Ms. Yland and her associates divided the asthma patients into five subgroups based on the drug regimens they were on during pregnancy as a surrogate marker of disease severity. This analysis showed no relationship between disease severity and live birth rate.
The researchers also ran an analysis that divided patients into the quality of their management during pregnancy – either good or poor – based on either of two markers of poor control: filling five or more prescriptions for a short-acting beta-antagonist, or at least one exacerbation episode defined as an asthma-related emergency department visit, hospitalization, or need for oral corticosteroid treatment. By these criteria 7,135 (24%) of the pregnant women with asthma were poorly controlled. The live birth rate was 74% among women without asthma, 71% among those with well-controlled asthma, and 68% among women with poorly-controlled asthma, reported Ms. Yland, a researcher at the Harvard T.H. Chan School of Public Health in Boston.
In a multivariate analysis that adjusted for demographic differences and comorbidities, women with poorly-controlled asthma had preterm delivery a statistically significant 30% more often than did women with well-controlled asthma, and the rate of neonatal ICU admissions was a significant 24% higher in women with poorly-controlled asthma, compared with women who had well-controlled asthma. However, the rates of small-for-gestational-age infants and infants with congenital malformations was not significantly different between the well-controlled and poorly-controlled subgroups.
The finding that almost a quarter of the pregnant women in the study were poorly controlled wasn’t surprising, Dr. Schatz said in an interview. In some studies as many as half the asthma patients have poor control.
The 24% rate of poor asthma control during pregnancy in the studied women is “most likely an underestimate of poor control in the general population” because the study used data from women with commercial health insurance, noted Sonia Hernandez-Diaz, MD, lead investigator for the study and professor of epidemiology at Harvard T.H. Chan School of Public Health. “More disadvantaged populations, such as pregnant women on Medicaid, tend to have worse control.”
Barriers to good asthma control during pregnancy include smoking, weight gain, undertreatment, poor adherence, and viral infection. The overall approach to managing asthma during pregnancy is the same as when women are not pregnant, although certain asthma medications have a better safety record during pregnancy. “The most reassuring data exist for albuterol and inhaled steroids, particularly budesonide and fluticasone. Reassuring data also exist for the long-acting beta agonists salmeterol and formoterol, which are combined with inhaled steroids, and for montelukast,” Dr. Schatz said.
This is the first study to assess the impact of asthma management on pregnancy outcome in such a large population. The large number of women included provided a lot of statistical power and allowed the analyses to control for several potential confounders, Ms. Yland noted in an interview. She plans to expand the analysis with Medicaid data to try to further increase the generalizability and precision of the findings.
The study was funded by GlaxoSmithKline, and a coauthor of the study is a company employee. Ms. Yland had no disclosures. Dr. Schatz has received research funding from ALK, AstraZeneca, Medimmune, GlaxoSmithKline, and Merck. Dr. Hernandez-Diaz has been a consultant to Boehringer Ingelheim, Roche, and UCB, and has received research funding from GlaxoSmithKline, Lilly, and Pfizer.
SOURCE: Yland J et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB422.
SAN FRANCISCO – and among the live births had a significantly increased rate of both preterm delivery and neonatal intensive care admissions, according to a review of insurance claims data for more than 1 million American women during 2011-2015.
On the other hand, asthma severity, which the researchers inferred based on the type and amount of treatment patients received, showed essentially no link with the live birth rate, Jennifer Yland said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“The findings add to the body of evidence that relate poor asthma control to an increased risk for pregnancy complications.” explained Michael X. Schatz, MD, an allergist at Kaiser Permanente of Southern California, in San Diego, and a coauthor of the study.
Results from several prior studies had shown links between asthma and an increased rate of preterm birth, “but the larger, more generalizable population is a strength of the current findings. Results from prior studies have less frequently shown a link between asthma during pregnancy and neonatal ICU admissions,” he added.“The findings strengthen the case for good asthma control during pregnancy.”
For their review, Ms. Yland and her coauthors used insurance claims data from privately-insured American women aged 12-55 years who were pregnant and had drug prescription records during the study period. The database included 996,861 women without an asthma diagnosis and 29,882 women diagnosed with asthma. The analysis excluded women diagnosed with chronic obstructive pulmonary disease at least twice during pregnancy.
To analyze the pregnancy outcomes by asthma severity Ms. Yland and her associates divided the asthma patients into five subgroups based on the drug regimens they were on during pregnancy as a surrogate marker of disease severity. This analysis showed no relationship between disease severity and live birth rate.
The researchers also ran an analysis that divided patients into the quality of their management during pregnancy – either good or poor – based on either of two markers of poor control: filling five or more prescriptions for a short-acting beta-antagonist, or at least one exacerbation episode defined as an asthma-related emergency department visit, hospitalization, or need for oral corticosteroid treatment. By these criteria 7,135 (24%) of the pregnant women with asthma were poorly controlled. The live birth rate was 74% among women without asthma, 71% among those with well-controlled asthma, and 68% among women with poorly-controlled asthma, reported Ms. Yland, a researcher at the Harvard T.H. Chan School of Public Health in Boston.
In a multivariate analysis that adjusted for demographic differences and comorbidities, women with poorly-controlled asthma had preterm delivery a statistically significant 30% more often than did women with well-controlled asthma, and the rate of neonatal ICU admissions was a significant 24% higher in women with poorly-controlled asthma, compared with women who had well-controlled asthma. However, the rates of small-for-gestational-age infants and infants with congenital malformations was not significantly different between the well-controlled and poorly-controlled subgroups.
The finding that almost a quarter of the pregnant women in the study were poorly controlled wasn’t surprising, Dr. Schatz said in an interview. In some studies as many as half the asthma patients have poor control.
The 24% rate of poor asthma control during pregnancy in the studied women is “most likely an underestimate of poor control in the general population” because the study used data from women with commercial health insurance, noted Sonia Hernandez-Diaz, MD, lead investigator for the study and professor of epidemiology at Harvard T.H. Chan School of Public Health. “More disadvantaged populations, such as pregnant women on Medicaid, tend to have worse control.”
Barriers to good asthma control during pregnancy include smoking, weight gain, undertreatment, poor adherence, and viral infection. The overall approach to managing asthma during pregnancy is the same as when women are not pregnant, although certain asthma medications have a better safety record during pregnancy. “The most reassuring data exist for albuterol and inhaled steroids, particularly budesonide and fluticasone. Reassuring data also exist for the long-acting beta agonists salmeterol and formoterol, which are combined with inhaled steroids, and for montelukast,” Dr. Schatz said.
This is the first study to assess the impact of asthma management on pregnancy outcome in such a large population. The large number of women included provided a lot of statistical power and allowed the analyses to control for several potential confounders, Ms. Yland noted in an interview. She plans to expand the analysis with Medicaid data to try to further increase the generalizability and precision of the findings.
The study was funded by GlaxoSmithKline, and a coauthor of the study is a company employee. Ms. Yland had no disclosures. Dr. Schatz has received research funding from ALK, AstraZeneca, Medimmune, GlaxoSmithKline, and Merck. Dr. Hernandez-Diaz has been a consultant to Boehringer Ingelheim, Roche, and UCB, and has received research funding from GlaxoSmithKline, Lilly, and Pfizer.
SOURCE: Yland J et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB422.
REPORTING FROM AAAAI 2019
Hospitalist scheduling: A search for balance
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
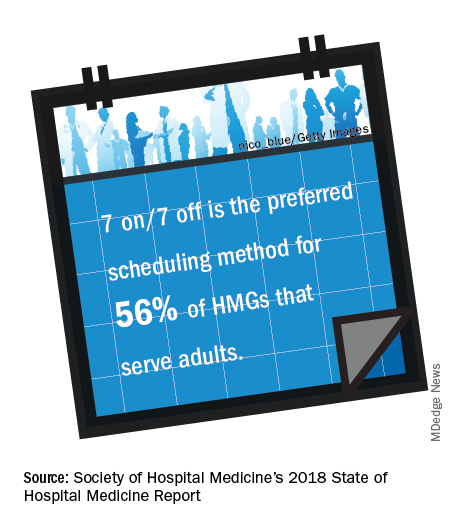
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.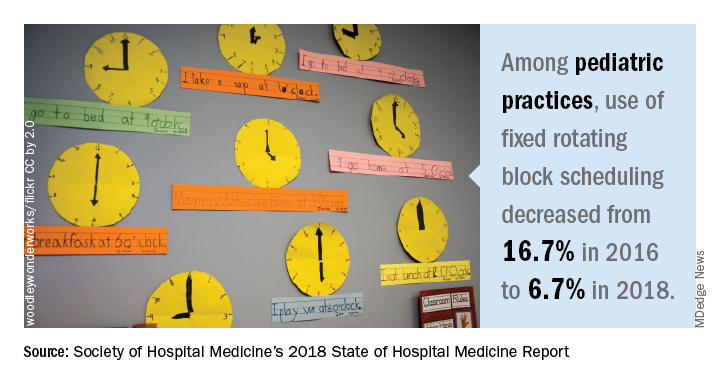
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Survey says ...
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
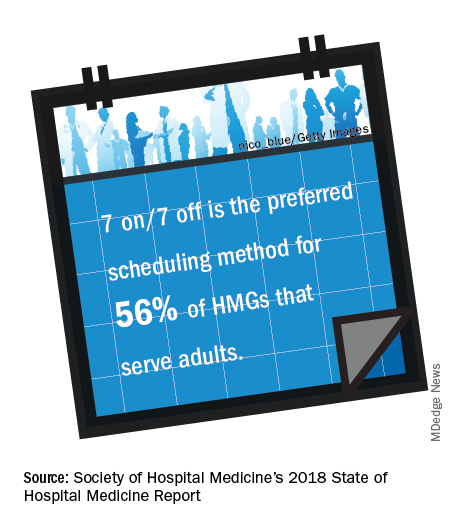
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.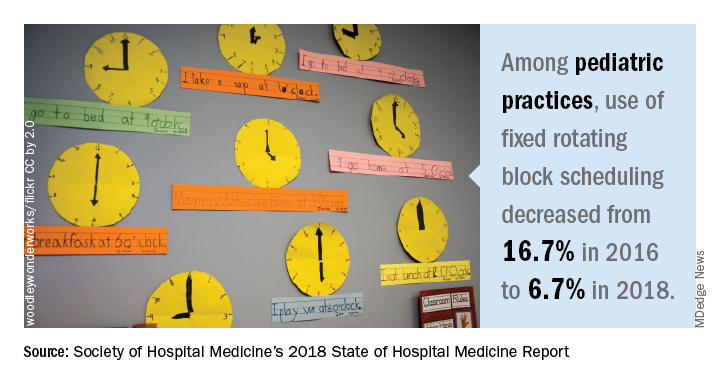
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.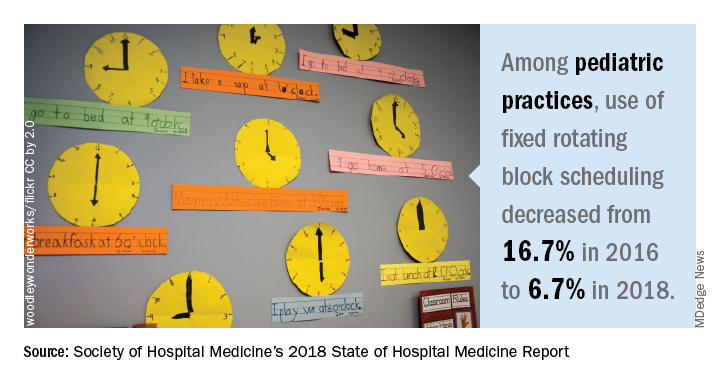
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Engraftment achieved after conditioning without radiation, alkylating agents
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
REPORTING FROM TCT 2019
Sore on head
The FP suspected that this was a skin cancer with ulceration and pigmentation. The differential diagnosis included pigmented basal cell carcinoma, melanoma, and squamous cell carcinoma. If this were a melanoma, there would appear to be areas of regression between the islands of pigmentation. The FP explained that a biopsy was needed and suggested a broad shave biopsy because this technique would provide adequate tissue to the pathologist. (See the Watch & Learn video on “Shave biopsy.”)
The FP performed the broad shave biopsy and saw some remaining pigment at the base of the initial cut. He performed a second pass with the DermaBlade and explained this in the pathology requisition. (It is acceptable to send a deeper section of tissue if it appears that there is some remaining tumor below the initial biopsy.)
The biopsy report revealed lentigo maligna melanoma, which was approximately 2 mm thick—much deeper than the clinical appearance suggested. The pathologist combined the depths from the 2 specimens to get an approximate Breslow level. In this case, the most important information was that this was >1 mm in depth, which suggested that a sentinel lymph node biopsy would be needed for prognostic information. The patient was referred to Surgical Oncology for wide excision and sentinel lymph node biopsy.
Fortunately, the nodes were negative for metastasis. The wide excision was closed with a graft that healed well over time. The patient was followed with regular skin exams and careful lymph node exams of the neck and supraclavicular areas. He now wears a hat whenever he is outdoors.
Photo courtesy of Jonathan Karnes, MD and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Squamous cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1103-1111.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP suspected that this was a skin cancer with ulceration and pigmentation. The differential diagnosis included pigmented basal cell carcinoma, melanoma, and squamous cell carcinoma. If this were a melanoma, there would appear to be areas of regression between the islands of pigmentation. The FP explained that a biopsy was needed and suggested a broad shave biopsy because this technique would provide adequate tissue to the pathologist. (See the Watch & Learn video on “Shave biopsy.”)
The FP performed the broad shave biopsy and saw some remaining pigment at the base of the initial cut. He performed a second pass with the DermaBlade and explained this in the pathology requisition. (It is acceptable to send a deeper section of tissue if it appears that there is some remaining tumor below the initial biopsy.)
The biopsy report revealed lentigo maligna melanoma, which was approximately 2 mm thick—much deeper than the clinical appearance suggested. The pathologist combined the depths from the 2 specimens to get an approximate Breslow level. In this case, the most important information was that this was >1 mm in depth, which suggested that a sentinel lymph node biopsy would be needed for prognostic information. The patient was referred to Surgical Oncology for wide excision and sentinel lymph node biopsy.
Fortunately, the nodes were negative for metastasis. The wide excision was closed with a graft that healed well over time. The patient was followed with regular skin exams and careful lymph node exams of the neck and supraclavicular areas. He now wears a hat whenever he is outdoors.
Photo courtesy of Jonathan Karnes, MD and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Squamous cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1103-1111.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP suspected that this was a skin cancer with ulceration and pigmentation. The differential diagnosis included pigmented basal cell carcinoma, melanoma, and squamous cell carcinoma. If this were a melanoma, there would appear to be areas of regression between the islands of pigmentation. The FP explained that a biopsy was needed and suggested a broad shave biopsy because this technique would provide adequate tissue to the pathologist. (See the Watch & Learn video on “Shave biopsy.”)
The FP performed the broad shave biopsy and saw some remaining pigment at the base of the initial cut. He performed a second pass with the DermaBlade and explained this in the pathology requisition. (It is acceptable to send a deeper section of tissue if it appears that there is some remaining tumor below the initial biopsy.)
The biopsy report revealed lentigo maligna melanoma, which was approximately 2 mm thick—much deeper than the clinical appearance suggested. The pathologist combined the depths from the 2 specimens to get an approximate Breslow level. In this case, the most important information was that this was >1 mm in depth, which suggested that a sentinel lymph node biopsy would be needed for prognostic information. The patient was referred to Surgical Oncology for wide excision and sentinel lymph node biopsy.
Fortunately, the nodes were negative for metastasis. The wide excision was closed with a graft that healed well over time. The patient was followed with regular skin exams and careful lymph node exams of the neck and supraclavicular areas. He now wears a hat whenever he is outdoors.
Photo courtesy of Jonathan Karnes, MD and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Squamous cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1103-1111.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
Analysis suggests ‘Burkitt-like lymphoma’ is a misnomer
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
REPORTING FROM HAEMATOLOGICA