User login
Indurated Plaque on the Shoulder
Herpes zoster (HZ) is a painful skin condition caused by reactivation of latent varicella-zoster virus (VZV) in dorsal root ganglion cells.1 Upon reactivation, VZV replicates in the dorsal root ganglion, which ultimately results in inflammation and necrosis of the neuron and intense neuralgia. Reactivation of latent VZV may occur spontaneously or may be induced by various factors including immunosuppression, stress, illness, and trauma. Prior to the development of skin lesions, many patients experience a prodrome of tingling, pain, or pruritus. Herpes zoster classically presents with grouped vesicles on an erythematous base in a unilateral dermatomal distribution; however, more than one adjacent dermatome may be involved, and the lesions can cross the midline. Furthermore, the development of vesicles may be preceded by the development of edematous papules or plaques.1
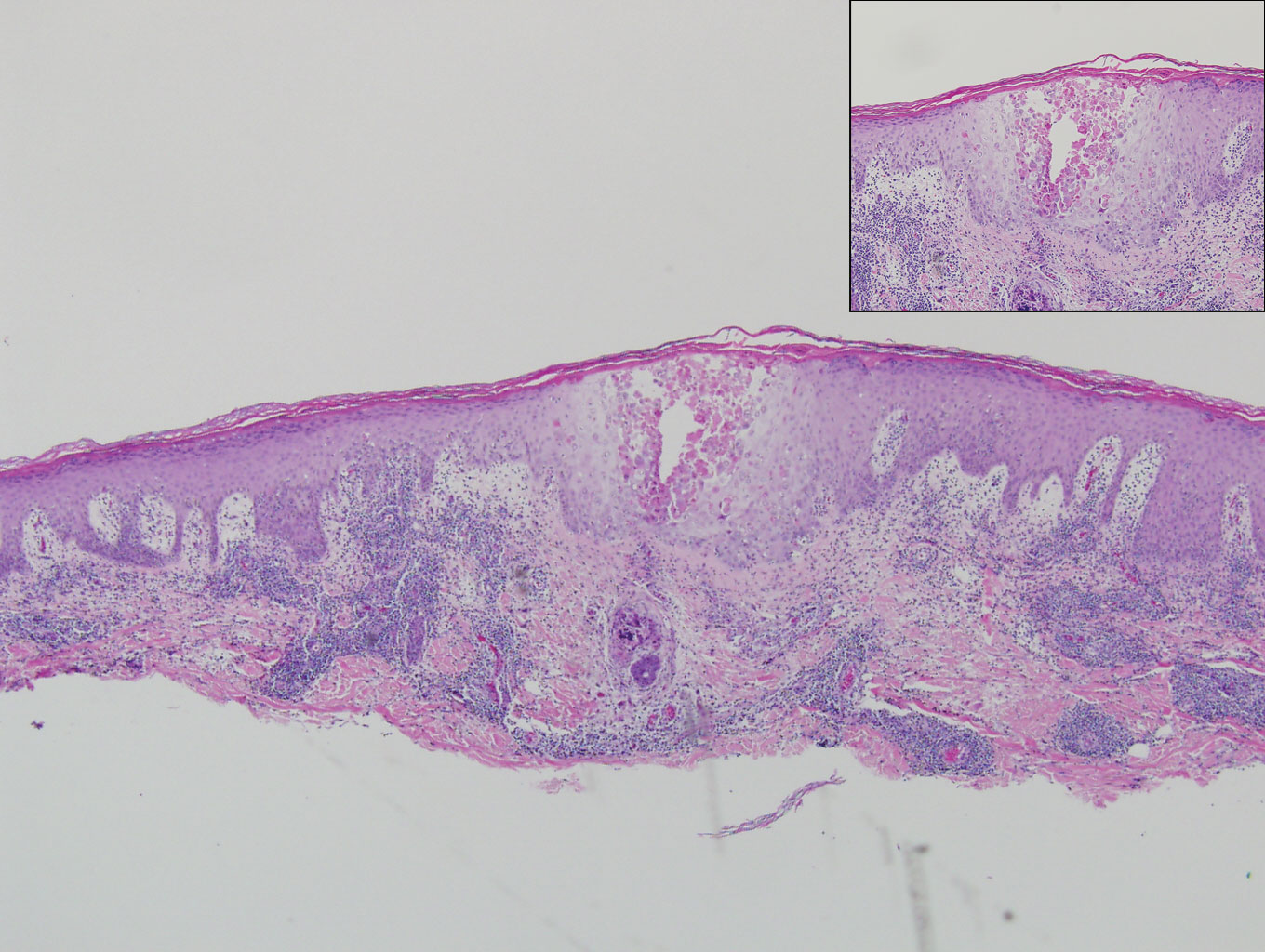
On histology, VZV closely resembles herpes simplex virus type 1 and herpes simplex virus type 2 infections.2 Classic histologic findings include ballooning degeneration of keratinocytes, acantholysis, nuclear molding, ground-glass nuclear inclusions, marginated chromatin, and multinucleated keratinocytes, as well as necrosis of follicles and sebaceous glands.2 Varicella-zoster virus polymerase chain reaction or immunostaining can be used to confirm the diagnosis.2
Classic mycosis fungoides (MF) presents with well-circumscribed erythematous patches in non–sun-exposed areas and eventually may progress to plaques and tumors.3 Patients with cutaneous T-cell lymphomas, such as MF, are at a higher risk for skin infections including HZ4,5; however, immunocompromised patients, such as those with cutaneous lymphomas, can have atypical clinical presentations of HZ that may be concerning for cutaneous lymphoma.6 Furthermore, cutaneous malignancies can occur in dermatomal distributions that may mimic HZ.7 Therefore, the threshold for biopsy should be lowered in those patients with dermatomal lesions and history concerning for possible malignancy.
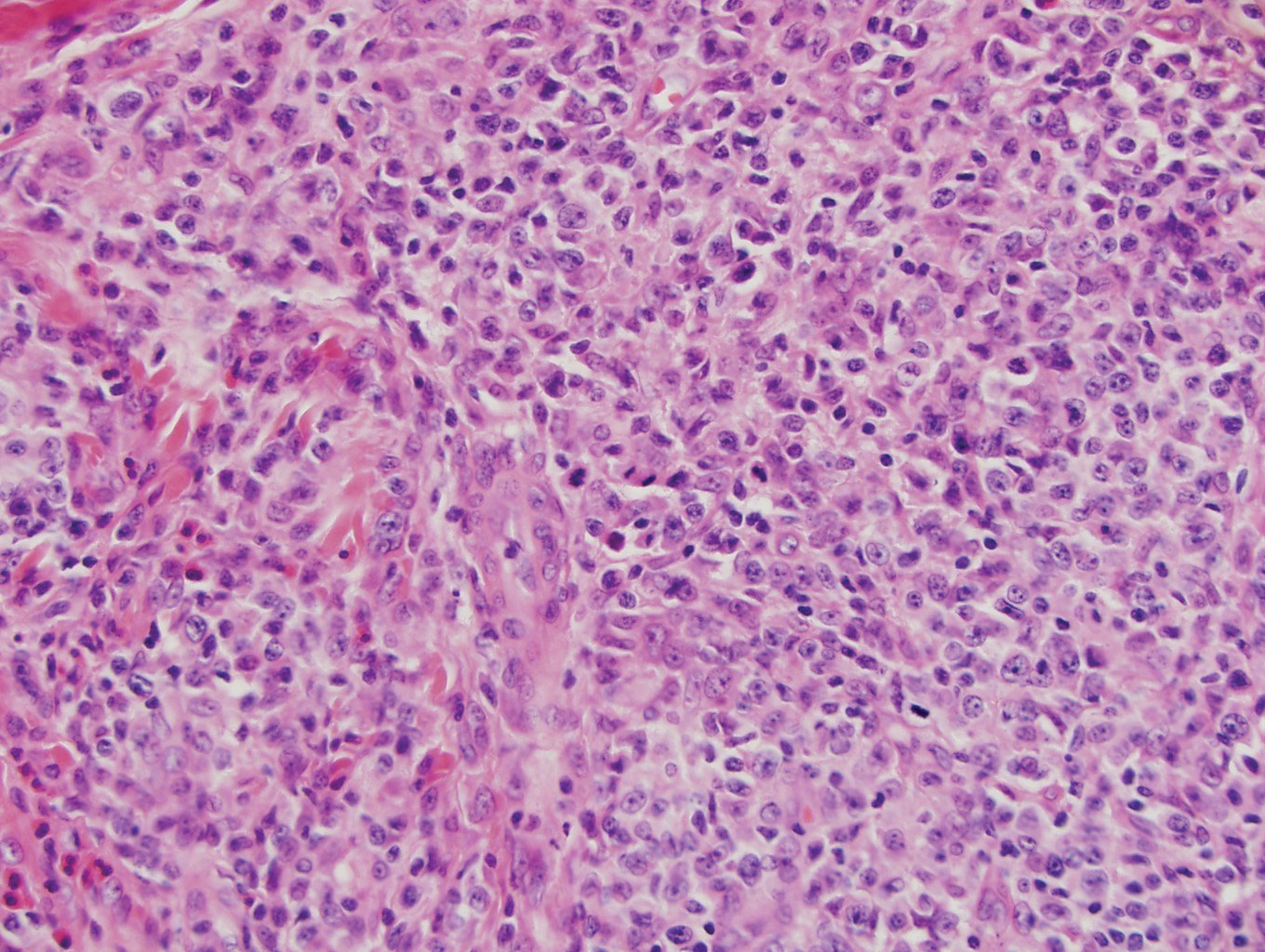
Classically, histologic examination of MF demonstrates an infiltrate of haloed cells at the dermoepidermal junction, which are atypical T cells with hyperchromatic cerebriform nuclei that are larger, darker, and more angulated than the benign recruited lymphocytes in the perivascular infiltrate seen in VZV infection (Figure 1).3 Papillary dermal fibrosis typically is present, and the perivascular infiltrate is denser above the postcapillary venule rather than being symmetrical around the vessel (bare underbelly sign). Clusters of these cells may form within the epidermis, which are called Pautrier microabscesses.3 Mycosis fungoides also can exhibit large cell transformation in which small lymphocytes transform into larger cells, thereby associated with a poorer prognosis.8
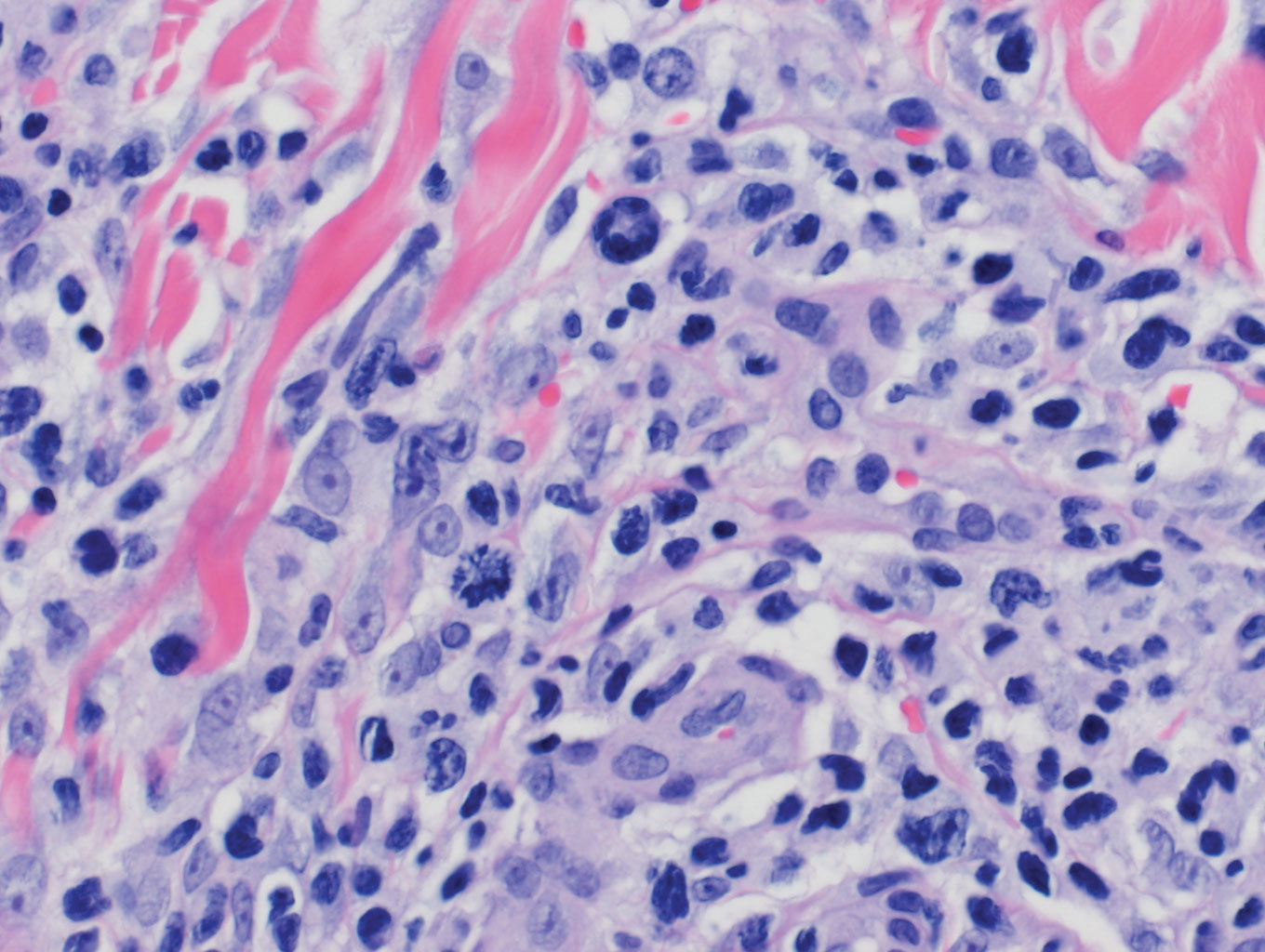
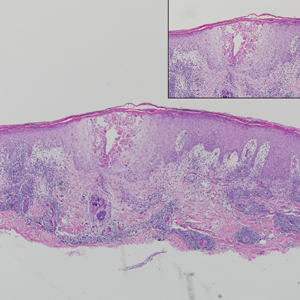
Lymphomatoid papulosis is a CD30+-predominant form of cutaneous T-cell lymphoma characterized by papules and nodules that spontaneously involute.9 This condition is most commonly associated with MF but can be associated with other lymphomas. This condition may be mistaken for HZ clinically, but histology classically demonstrates large atypical lymphocytes resembling Reed-Sternberg cells in small clusters rather than follicular necrosis (Figure 2).9
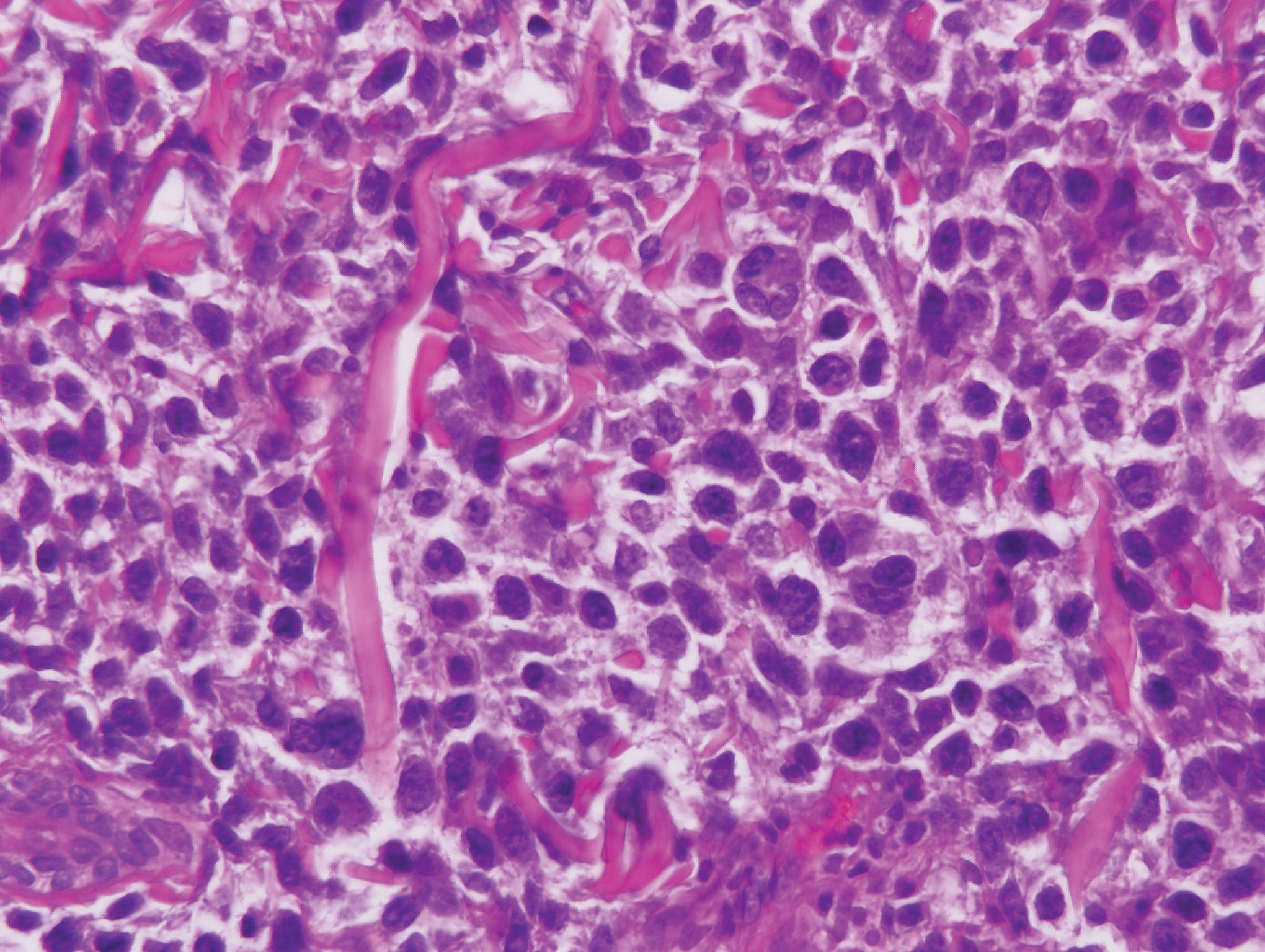
Patients with lymphoma may sequentially develop a secondary lymphoma. There have been reports of secondary B-cell lymphomas associated with MF, but this phenomenon is rare.10 The histology depends on the type of B-cell lymphoma present, but follicular necrosis would not be expected (Figure 3).
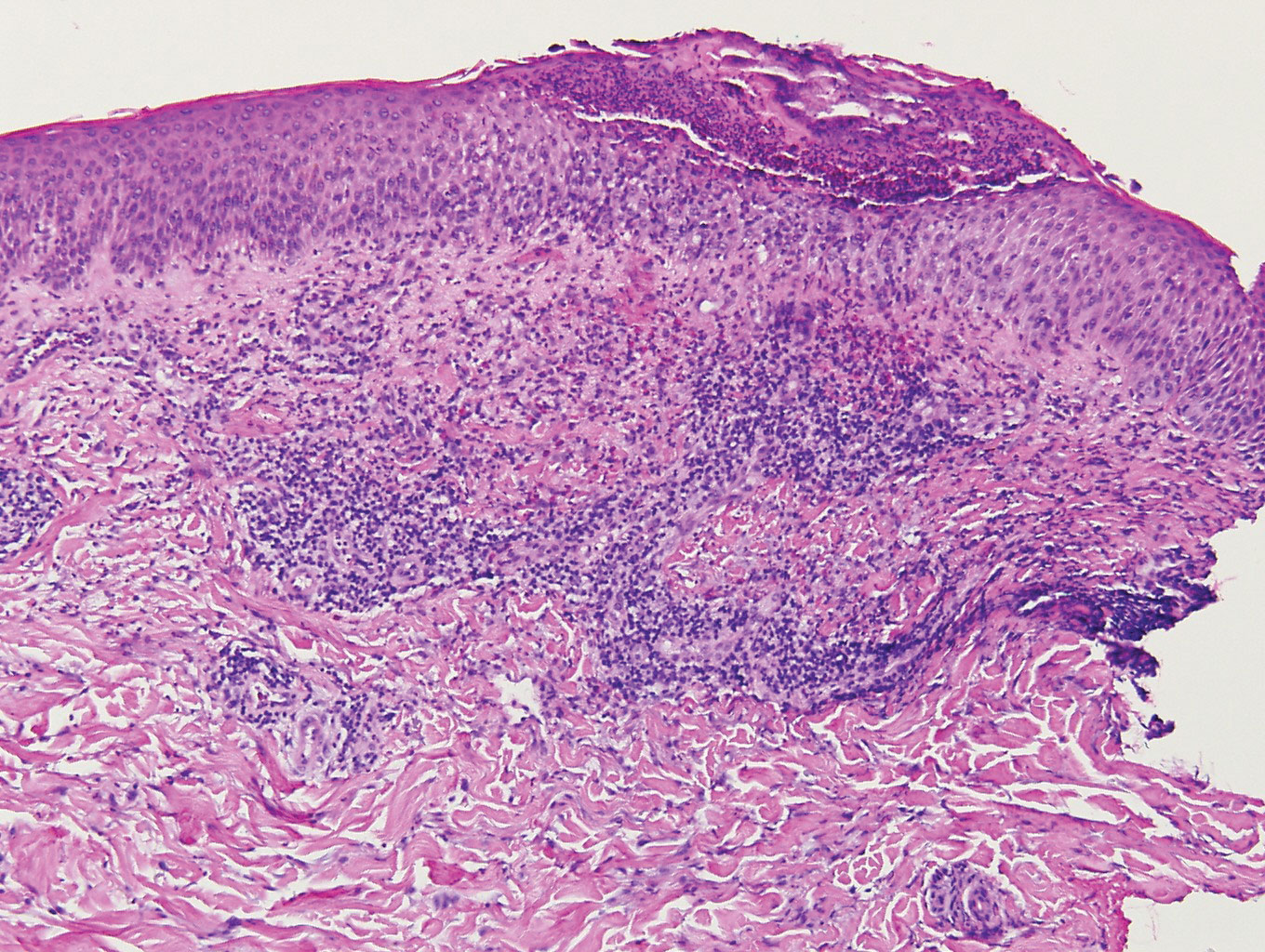
Unusual hypersensitivity reactions to arthropod attacks have been described in patients with lymphoproliferative disorders and could be mistaken for HZ. Histology may demonstrate a wedge-shaped perivascular and/or interstitial infiltrate containing eosinophils with endothelial swelling (Figure 4), but these findings may vary depending on the type of arthropod involved.11
Our case provided a unique example of HZ in a patient with a known history of MF. Clinically, there was concern for progression of the patient’s underlying disease; however, histology demonstrated ballooning keratinocytes and follicular necrosis, which are classically seen in HZ infection.
- Downing C, Medoza N, Sra K, et al. Human herpesviruses. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:1400-1424.
- Chisholm C, Lopez L. Cutaneous infections caused by Herpesviridae: a review. Arch Pathol Lab Med. 2011;135:1357-1362.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70: 205.e1-205.e16.
- Vonderheid EC, van Voorst Vader PC. Herpes zoster-varicella in cutaneous T-cell lymphomas. Arch Dermatol. 1980;116:408-412.
- Lebas E, Arrese JE, Nikkels AF. Risk factors for skin infections in mycosis fungoides. Dermatology. 2016;232:731-737.
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Niiyama S, Satoh K, Kaneko S, et al. Zosteriform skin involvement of nodal T-cell lymphoma: a review of the published work of cutaneous malignancies mimicking herpes zoster. J Dermatol. 2007;34:68-73.
- Pulitzer M, Myskowski PL, Horwitz SM, et al. Mycosis fungoides with large cell transformation:clinicopathological features and prognostic factors. Pathology. 2014;46:610-616.
- Zackheim HS, Jones C, Leboit PE, et al. Lymphomatoid papulosis associated with mycosis fungoides: a study of 21 patients including analyses for clonality. J Am Acad Dermatol. 2003;49:620-623.
- Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155:379-386.
- Vassallo C, Passamonti F, Cananzi R, et al. Exaggerated insect bite-like reaction in patients affected by oncohaematological diseases. Acta Derm Venereol. 2005;85:76-77.
Herpes zoster (HZ) is a painful skin condition caused by reactivation of latent varicella-zoster virus (VZV) in dorsal root ganglion cells.1 Upon reactivation, VZV replicates in the dorsal root ganglion, which ultimately results in inflammation and necrosis of the neuron and intense neuralgia. Reactivation of latent VZV may occur spontaneously or may be induced by various factors including immunosuppression, stress, illness, and trauma. Prior to the development of skin lesions, many patients experience a prodrome of tingling, pain, or pruritus. Herpes zoster classically presents with grouped vesicles on an erythematous base in a unilateral dermatomal distribution; however, more than one adjacent dermatome may be involved, and the lesions can cross the midline. Furthermore, the development of vesicles may be preceded by the development of edematous papules or plaques.1
On histology, VZV closely resembles herpes simplex virus type 1 and herpes simplex virus type 2 infections.2 Classic histologic findings include ballooning degeneration of keratinocytes, acantholysis, nuclear molding, ground-glass nuclear inclusions, marginated chromatin, and multinucleated keratinocytes, as well as necrosis of follicles and sebaceous glands.2 Varicella-zoster virus polymerase chain reaction or immunostaining can be used to confirm the diagnosis.2
Classic mycosis fungoides (MF) presents with well-circumscribed erythematous patches in non–sun-exposed areas and eventually may progress to plaques and tumors.3 Patients with cutaneous T-cell lymphomas, such as MF, are at a higher risk for skin infections including HZ4,5; however, immunocompromised patients, such as those with cutaneous lymphomas, can have atypical clinical presentations of HZ that may be concerning for cutaneous lymphoma.6 Furthermore, cutaneous malignancies can occur in dermatomal distributions that may mimic HZ.7 Therefore, the threshold for biopsy should be lowered in those patients with dermatomal lesions and history concerning for possible malignancy.
Classically, histologic examination of MF demonstrates an infiltrate of haloed cells at the dermoepidermal junction, which are atypical T cells with hyperchromatic cerebriform nuclei that are larger, darker, and more angulated than the benign recruited lymphocytes in the perivascular infiltrate seen in VZV infection (Figure 1).3 Papillary dermal fibrosis typically is present, and the perivascular infiltrate is denser above the postcapillary venule rather than being symmetrical around the vessel (bare underbelly sign). Clusters of these cells may form within the epidermis, which are called Pautrier microabscesses.3 Mycosis fungoides also can exhibit large cell transformation in which small lymphocytes transform into larger cells, thereby associated with a poorer prognosis.8
Lymphomatoid papulosis is a CD30+-predominant form of cutaneous T-cell lymphoma characterized by papules and nodules that spontaneously involute.9 This condition is most commonly associated with MF but can be associated with other lymphomas. This condition may be mistaken for HZ clinically, but histology classically demonstrates large atypical lymphocytes resembling Reed-Sternberg cells in small clusters rather than follicular necrosis (Figure 2).9
Patients with lymphoma may sequentially develop a secondary lymphoma. There have been reports of secondary B-cell lymphomas associated with MF, but this phenomenon is rare.10 The histology depends on the type of B-cell lymphoma present, but follicular necrosis would not be expected (Figure 3).
Unusual hypersensitivity reactions to arthropod attacks have been described in patients with lymphoproliferative disorders and could be mistaken for HZ. Histology may demonstrate a wedge-shaped perivascular and/or interstitial infiltrate containing eosinophils with endothelial swelling (Figure 4), but these findings may vary depending on the type of arthropod involved.11
Our case provided a unique example of HZ in a patient with a known history of MF. Clinically, there was concern for progression of the patient’s underlying disease; however, histology demonstrated ballooning keratinocytes and follicular necrosis, which are classically seen in HZ infection.
Herpes zoster (HZ) is a painful skin condition caused by reactivation of latent varicella-zoster virus (VZV) in dorsal root ganglion cells.1 Upon reactivation, VZV replicates in the dorsal root ganglion, which ultimately results in inflammation and necrosis of the neuron and intense neuralgia. Reactivation of latent VZV may occur spontaneously or may be induced by various factors including immunosuppression, stress, illness, and trauma. Prior to the development of skin lesions, many patients experience a prodrome of tingling, pain, or pruritus. Herpes zoster classically presents with grouped vesicles on an erythematous base in a unilateral dermatomal distribution; however, more than one adjacent dermatome may be involved, and the lesions can cross the midline. Furthermore, the development of vesicles may be preceded by the development of edematous papules or plaques.1
On histology, VZV closely resembles herpes simplex virus type 1 and herpes simplex virus type 2 infections.2 Classic histologic findings include ballooning degeneration of keratinocytes, acantholysis, nuclear molding, ground-glass nuclear inclusions, marginated chromatin, and multinucleated keratinocytes, as well as necrosis of follicles and sebaceous glands.2 Varicella-zoster virus polymerase chain reaction or immunostaining can be used to confirm the diagnosis.2
Classic mycosis fungoides (MF) presents with well-circumscribed erythematous patches in non–sun-exposed areas and eventually may progress to plaques and tumors.3 Patients with cutaneous T-cell lymphomas, such as MF, are at a higher risk for skin infections including HZ4,5; however, immunocompromised patients, such as those with cutaneous lymphomas, can have atypical clinical presentations of HZ that may be concerning for cutaneous lymphoma.6 Furthermore, cutaneous malignancies can occur in dermatomal distributions that may mimic HZ.7 Therefore, the threshold for biopsy should be lowered in those patients with dermatomal lesions and history concerning for possible malignancy.
Classically, histologic examination of MF demonstrates an infiltrate of haloed cells at the dermoepidermal junction, which are atypical T cells with hyperchromatic cerebriform nuclei that are larger, darker, and more angulated than the benign recruited lymphocytes in the perivascular infiltrate seen in VZV infection (Figure 1).3 Papillary dermal fibrosis typically is present, and the perivascular infiltrate is denser above the postcapillary venule rather than being symmetrical around the vessel (bare underbelly sign). Clusters of these cells may form within the epidermis, which are called Pautrier microabscesses.3 Mycosis fungoides also can exhibit large cell transformation in which small lymphocytes transform into larger cells, thereby associated with a poorer prognosis.8
Lymphomatoid papulosis is a CD30+-predominant form of cutaneous T-cell lymphoma characterized by papules and nodules that spontaneously involute.9 This condition is most commonly associated with MF but can be associated with other lymphomas. This condition may be mistaken for HZ clinically, but histology classically demonstrates large atypical lymphocytes resembling Reed-Sternberg cells in small clusters rather than follicular necrosis (Figure 2).9
Patients with lymphoma may sequentially develop a secondary lymphoma. There have been reports of secondary B-cell lymphomas associated with MF, but this phenomenon is rare.10 The histology depends on the type of B-cell lymphoma present, but follicular necrosis would not be expected (Figure 3).
Unusual hypersensitivity reactions to arthropod attacks have been described in patients with lymphoproliferative disorders and could be mistaken for HZ. Histology may demonstrate a wedge-shaped perivascular and/or interstitial infiltrate containing eosinophils with endothelial swelling (Figure 4), but these findings may vary depending on the type of arthropod involved.11
Our case provided a unique example of HZ in a patient with a known history of MF. Clinically, there was concern for progression of the patient’s underlying disease; however, histology demonstrated ballooning keratinocytes and follicular necrosis, which are classically seen in HZ infection.
- Downing C, Medoza N, Sra K, et al. Human herpesviruses. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:1400-1424.
- Chisholm C, Lopez L. Cutaneous infections caused by Herpesviridae: a review. Arch Pathol Lab Med. 2011;135:1357-1362.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70: 205.e1-205.e16.
- Vonderheid EC, van Voorst Vader PC. Herpes zoster-varicella in cutaneous T-cell lymphomas. Arch Dermatol. 1980;116:408-412.
- Lebas E, Arrese JE, Nikkels AF. Risk factors for skin infections in mycosis fungoides. Dermatology. 2016;232:731-737.
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Niiyama S, Satoh K, Kaneko S, et al. Zosteriform skin involvement of nodal T-cell lymphoma: a review of the published work of cutaneous malignancies mimicking herpes zoster. J Dermatol. 2007;34:68-73.
- Pulitzer M, Myskowski PL, Horwitz SM, et al. Mycosis fungoides with large cell transformation:clinicopathological features and prognostic factors. Pathology. 2014;46:610-616.
- Zackheim HS, Jones C, Leboit PE, et al. Lymphomatoid papulosis associated with mycosis fungoides: a study of 21 patients including analyses for clonality. J Am Acad Dermatol. 2003;49:620-623.
- Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155:379-386.
- Vassallo C, Passamonti F, Cananzi R, et al. Exaggerated insect bite-like reaction in patients affected by oncohaematological diseases. Acta Derm Venereol. 2005;85:76-77.
- Downing C, Medoza N, Sra K, et al. Human herpesviruses. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:1400-1424.
- Chisholm C, Lopez L. Cutaneous infections caused by Herpesviridae: a review. Arch Pathol Lab Med. 2011;135:1357-1362.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70: 205.e1-205.e16.
- Vonderheid EC, van Voorst Vader PC. Herpes zoster-varicella in cutaneous T-cell lymphomas. Arch Dermatol. 1980;116:408-412.
- Lebas E, Arrese JE, Nikkels AF. Risk factors for skin infections in mycosis fungoides. Dermatology. 2016;232:731-737.
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Niiyama S, Satoh K, Kaneko S, et al. Zosteriform skin involvement of nodal T-cell lymphoma: a review of the published work of cutaneous malignancies mimicking herpes zoster. J Dermatol. 2007;34:68-73.
- Pulitzer M, Myskowski PL, Horwitz SM, et al. Mycosis fungoides with large cell transformation:clinicopathological features and prognostic factors. Pathology. 2014;46:610-616.
- Zackheim HS, Jones C, Leboit PE, et al. Lymphomatoid papulosis associated with mycosis fungoides: a study of 21 patients including analyses for clonality. J Am Acad Dermatol. 2003;49:620-623.
- Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155:379-386.
- Vassallo C, Passamonti F, Cananzi R, et al. Exaggerated insect bite-like reaction in patients affected by oncohaematological diseases. Acta Derm Venereol. 2005;85:76-77.
A 66-year-old man with mycosis fungoides presented with a new indurated plaque on the left shoulder. Biopsies of the left shoulder and back lesions were obtained.
Novel transplant regimen improves survival in primary immunodeficiency
HOUSTON – Allogeneic hematopoietic stem cell transplantation (allo-HCT) following a novel reduced-intensity conditioning regimen was largely successful in a heterogeneous cohort of 29 adults and children with primary immunodeficiency in a prospective clinical trial.
At 1 year after transplant, overall survival was 98% and the estimated graft failure–free and graft-versus-host disease (GVHD)–free survival was 82% among the participants, who had various underlying primary immunodeficiencies (PIDs), Dimana Dimitrova, MD, reported at the Transplantation and Cellular Therapy Meetings.
GVHD-free survival was defined in this National Institutes of Health study as the absence of steroid-refractory grade 3-4 acute GVHD and chronic GVHD, noted Dr. Dimitrova of the NIH.
All patients, including 19 adults and 10 children (median age, 25 years), received a serotherapy-free, radiation-free, reduced-intensity conditioning regimen designed to optimize immune reconstitution, minimize toxicity and GVHD, reduce the risk of infectious complications, and enable successful use of alternative donors.
The conditioning platform included pentostatin on day –11 and day –7 at 4 mg/m2 along with 8 days of low-dose cyclophosphamide and 2 days of pharmacokinetically dosed busulfan at 4,600 mmol/min. GVHD prophylaxis included posttransplantation cyclophosphamide, mycophenolate mofetil (MMF), and sirolimus.
All patients received T cell–replete bone marrow or peripheral blood stem cell allografts; 72% received alternative donor grafts, Dr. Dimitrova said.
Two patients died, including one with bacterial sepsis and invasive aspergillosis who died on day +44 and one with presumed viral encephalitis who died on day +110. The patients were high risk overall (median HCT–comorbidity index score of 3, with a range of 0-11), and the two who died had HCT-CI scores of 6 and 8, respectively.
An additional accidental death occurred at 18 months after transplant “in the setting of continued remission, good graft function, and no transplant-related complications,” she said.
Neutrophil recovery occurred at a median of 17 days after transplant; three patients experienced graft failure, including one primary failure with autologous recovery on day +14 and two secondary graft failures.
“Two patients with known underlying difficult-to-engraft diseases required second transplants using different nonmyeloabalative platforms, and nevertheless required donor lymphocyte infusions to avoid threatened secondary graft failure,” she said. “The third patient actually had sufficiently improved infectious disease control and has not needed a second transplant to date.”
Overall GVHD incidence using the novel platform has been extremely low, she said, noting that 14% of patients had grade 2-4 GVHD and 3% had grade 3-4 acute GVHD. There was no steroid-refractory GVHD or chronic GVHD.
Among the infectious complications, other than those that led to the two deaths, were cytomegalovirus reactivation in 7 of 16 patients at risk, BK virus–associated hemorrhagic cystitis in 19 of 22 patients at risk, and a suspected case of viral cardiomyopathy that ultimately resolved.
“Importantly, although many patients had Epstein-Barr virus [EBV] control issues prior to transplant, no patients received preemptive EBV-directed therapy, and no patients had EBV-PTLD [posttransplant lymphoproliferative disorder],” she said.
Additionally, blood stream infections were detected in five patients, there were two cases of confirmed aspergillosis, and one child developed cutaneous candidiasis. Other complications and toxicities appeared to relate to underlying pretransplant issues in the affected organ or exuberant immune responses to existing infection.
“Phenotype reversal was evident to some degree in all evaluable patients, even in those with mixed chimerism or unknown underlying genetic defect,” Dr. Dimitrova said.
All 10 patients with malignancy or lymphoproliferative disease as an additional indication for allo-HCT remain in remission, and most patients who required immunoglobulin replacement therapy prior to transplant have been able to discontinue it, she noted.
The findings of this study are of note, because while it has been known for decades that allo-HCT is a potentially curative therapy for patients with PIDs that arise from defects in cells of hematopoietic origin, it frequently fails because of complicating factors or is not an option, Dr. Dimitrova said.
“These patients will often enter transplant with multiple comorbidities and disease sequelae, particularly as diagnosis of PIDs increases in older children and adults following years of illness,” she explained, adding that related donor options may be limited if family members are also affected.
For this reason, and with the goal of improving access to allo-HCT to all who require it, the novel conditioning platform used in this study was developed.
The platform was well tolerated overall, Dr. Dimitrova said, emphasizing the “notably low” GVHD rates.
“Currently we are investigating reduced MMF with the goal of promoting earlier immune reconstitution, and a separate protocol has opened that includes several modifications to this platform aimed at patients with increased risk of graft failure who may not tolerate mixed chimerism early on,” she said, noting that both protocols are currently enrolling.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Dimitrova reported having no financial disclosures.
SOURCE: Dimitrova D et al. TCT 2019, Abstract 54.
HOUSTON – Allogeneic hematopoietic stem cell transplantation (allo-HCT) following a novel reduced-intensity conditioning regimen was largely successful in a heterogeneous cohort of 29 adults and children with primary immunodeficiency in a prospective clinical trial.
At 1 year after transplant, overall survival was 98% and the estimated graft failure–free and graft-versus-host disease (GVHD)–free survival was 82% among the participants, who had various underlying primary immunodeficiencies (PIDs), Dimana Dimitrova, MD, reported at the Transplantation and Cellular Therapy Meetings.
GVHD-free survival was defined in this National Institutes of Health study as the absence of steroid-refractory grade 3-4 acute GVHD and chronic GVHD, noted Dr. Dimitrova of the NIH.
All patients, including 19 adults and 10 children (median age, 25 years), received a serotherapy-free, radiation-free, reduced-intensity conditioning regimen designed to optimize immune reconstitution, minimize toxicity and GVHD, reduce the risk of infectious complications, and enable successful use of alternative donors.
The conditioning platform included pentostatin on day –11 and day –7 at 4 mg/m2 along with 8 days of low-dose cyclophosphamide and 2 days of pharmacokinetically dosed busulfan at 4,600 mmol/min. GVHD prophylaxis included posttransplantation cyclophosphamide, mycophenolate mofetil (MMF), and sirolimus.
All patients received T cell–replete bone marrow or peripheral blood stem cell allografts; 72% received alternative donor grafts, Dr. Dimitrova said.
Two patients died, including one with bacterial sepsis and invasive aspergillosis who died on day +44 and one with presumed viral encephalitis who died on day +110. The patients were high risk overall (median HCT–comorbidity index score of 3, with a range of 0-11), and the two who died had HCT-CI scores of 6 and 8, respectively.
An additional accidental death occurred at 18 months after transplant “in the setting of continued remission, good graft function, and no transplant-related complications,” she said.
Neutrophil recovery occurred at a median of 17 days after transplant; three patients experienced graft failure, including one primary failure with autologous recovery on day +14 and two secondary graft failures.
“Two patients with known underlying difficult-to-engraft diseases required second transplants using different nonmyeloabalative platforms, and nevertheless required donor lymphocyte infusions to avoid threatened secondary graft failure,” she said. “The third patient actually had sufficiently improved infectious disease control and has not needed a second transplant to date.”
Overall GVHD incidence using the novel platform has been extremely low, she said, noting that 14% of patients had grade 2-4 GVHD and 3% had grade 3-4 acute GVHD. There was no steroid-refractory GVHD or chronic GVHD.
Among the infectious complications, other than those that led to the two deaths, were cytomegalovirus reactivation in 7 of 16 patients at risk, BK virus–associated hemorrhagic cystitis in 19 of 22 patients at risk, and a suspected case of viral cardiomyopathy that ultimately resolved.
“Importantly, although many patients had Epstein-Barr virus [EBV] control issues prior to transplant, no patients received preemptive EBV-directed therapy, and no patients had EBV-PTLD [posttransplant lymphoproliferative disorder],” she said.
Additionally, blood stream infections were detected in five patients, there were two cases of confirmed aspergillosis, and one child developed cutaneous candidiasis. Other complications and toxicities appeared to relate to underlying pretransplant issues in the affected organ or exuberant immune responses to existing infection.
“Phenotype reversal was evident to some degree in all evaluable patients, even in those with mixed chimerism or unknown underlying genetic defect,” Dr. Dimitrova said.
All 10 patients with malignancy or lymphoproliferative disease as an additional indication for allo-HCT remain in remission, and most patients who required immunoglobulin replacement therapy prior to transplant have been able to discontinue it, she noted.
The findings of this study are of note, because while it has been known for decades that allo-HCT is a potentially curative therapy for patients with PIDs that arise from defects in cells of hematopoietic origin, it frequently fails because of complicating factors or is not an option, Dr. Dimitrova said.
“These patients will often enter transplant with multiple comorbidities and disease sequelae, particularly as diagnosis of PIDs increases in older children and adults following years of illness,” she explained, adding that related donor options may be limited if family members are also affected.
For this reason, and with the goal of improving access to allo-HCT to all who require it, the novel conditioning platform used in this study was developed.
The platform was well tolerated overall, Dr. Dimitrova said, emphasizing the “notably low” GVHD rates.
“Currently we are investigating reduced MMF with the goal of promoting earlier immune reconstitution, and a separate protocol has opened that includes several modifications to this platform aimed at patients with increased risk of graft failure who may not tolerate mixed chimerism early on,” she said, noting that both protocols are currently enrolling.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Dimitrova reported having no financial disclosures.
SOURCE: Dimitrova D et al. TCT 2019, Abstract 54.
HOUSTON – Allogeneic hematopoietic stem cell transplantation (allo-HCT) following a novel reduced-intensity conditioning regimen was largely successful in a heterogeneous cohort of 29 adults and children with primary immunodeficiency in a prospective clinical trial.
At 1 year after transplant, overall survival was 98% and the estimated graft failure–free and graft-versus-host disease (GVHD)–free survival was 82% among the participants, who had various underlying primary immunodeficiencies (PIDs), Dimana Dimitrova, MD, reported at the Transplantation and Cellular Therapy Meetings.
GVHD-free survival was defined in this National Institutes of Health study as the absence of steroid-refractory grade 3-4 acute GVHD and chronic GVHD, noted Dr. Dimitrova of the NIH.
All patients, including 19 adults and 10 children (median age, 25 years), received a serotherapy-free, radiation-free, reduced-intensity conditioning regimen designed to optimize immune reconstitution, minimize toxicity and GVHD, reduce the risk of infectious complications, and enable successful use of alternative donors.
The conditioning platform included pentostatin on day –11 and day –7 at 4 mg/m2 along with 8 days of low-dose cyclophosphamide and 2 days of pharmacokinetically dosed busulfan at 4,600 mmol/min. GVHD prophylaxis included posttransplantation cyclophosphamide, mycophenolate mofetil (MMF), and sirolimus.
All patients received T cell–replete bone marrow or peripheral blood stem cell allografts; 72% received alternative donor grafts, Dr. Dimitrova said.
Two patients died, including one with bacterial sepsis and invasive aspergillosis who died on day +44 and one with presumed viral encephalitis who died on day +110. The patients were high risk overall (median HCT–comorbidity index score of 3, with a range of 0-11), and the two who died had HCT-CI scores of 6 and 8, respectively.
An additional accidental death occurred at 18 months after transplant “in the setting of continued remission, good graft function, and no transplant-related complications,” she said.
Neutrophil recovery occurred at a median of 17 days after transplant; three patients experienced graft failure, including one primary failure with autologous recovery on day +14 and two secondary graft failures.
“Two patients with known underlying difficult-to-engraft diseases required second transplants using different nonmyeloabalative platforms, and nevertheless required donor lymphocyte infusions to avoid threatened secondary graft failure,” she said. “The third patient actually had sufficiently improved infectious disease control and has not needed a second transplant to date.”
Overall GVHD incidence using the novel platform has been extremely low, she said, noting that 14% of patients had grade 2-4 GVHD and 3% had grade 3-4 acute GVHD. There was no steroid-refractory GVHD or chronic GVHD.
Among the infectious complications, other than those that led to the two deaths, were cytomegalovirus reactivation in 7 of 16 patients at risk, BK virus–associated hemorrhagic cystitis in 19 of 22 patients at risk, and a suspected case of viral cardiomyopathy that ultimately resolved.
“Importantly, although many patients had Epstein-Barr virus [EBV] control issues prior to transplant, no patients received preemptive EBV-directed therapy, and no patients had EBV-PTLD [posttransplant lymphoproliferative disorder],” she said.
Additionally, blood stream infections were detected in five patients, there were two cases of confirmed aspergillosis, and one child developed cutaneous candidiasis. Other complications and toxicities appeared to relate to underlying pretransplant issues in the affected organ or exuberant immune responses to existing infection.
“Phenotype reversal was evident to some degree in all evaluable patients, even in those with mixed chimerism or unknown underlying genetic defect,” Dr. Dimitrova said.
All 10 patients with malignancy or lymphoproliferative disease as an additional indication for allo-HCT remain in remission, and most patients who required immunoglobulin replacement therapy prior to transplant have been able to discontinue it, she noted.
The findings of this study are of note, because while it has been known for decades that allo-HCT is a potentially curative therapy for patients with PIDs that arise from defects in cells of hematopoietic origin, it frequently fails because of complicating factors or is not an option, Dr. Dimitrova said.
“These patients will often enter transplant with multiple comorbidities and disease sequelae, particularly as diagnosis of PIDs increases in older children and adults following years of illness,” she explained, adding that related donor options may be limited if family members are also affected.
For this reason, and with the goal of improving access to allo-HCT to all who require it, the novel conditioning platform used in this study was developed.
The platform was well tolerated overall, Dr. Dimitrova said, emphasizing the “notably low” GVHD rates.
“Currently we are investigating reduced MMF with the goal of promoting earlier immune reconstitution, and a separate protocol has opened that includes several modifications to this platform aimed at patients with increased risk of graft failure who may not tolerate mixed chimerism early on,” she said, noting that both protocols are currently enrolling.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Dimitrova reported having no financial disclosures.
SOURCE: Dimitrova D et al. TCT 2019, Abstract 54.
REPORTING FROM TCT 2019
New IPF diagnosis test now covered by Medicare
The Envisia Genomic Classifier, produced by Veracyte, has received final Medicare local coverage determination for the diagnosis of idiopathic pulmonary fibrosis (IPF).
Envisia is a complement to high-resolution CT that can help differentiate IPF from other interstitial lung diseases, as more than half of patients with IPF/interstitial lung disease report being misdiagnosed at least once. The test analyzes samples obtained through transbronchial biopsy, a nonsurgical procedure commonly used in lung evaluation. Envisia has been shown to detect usual interstitial pneumonia, a signature of IPF, with high accuracy.
The new policy was issued through the Palmetto GBA MolDx program and will go into effect on April 1, 2019, making Envisia the first commercially available test of its kind, available to the 55 million people who are currently enrolled in Medicare.
“We are pleased that the evidence supporting the Envisia classifier met the MolDx program’s high standards for coverage. This important milestone will enable us to begin making the Envisia Classifier more widely available to patients with suspected IPF so that they can obtain an accurate, timely diagnosis and, in turn, appropriate treatment,” Bonnie Anderson, chairman and chief executive officer of Veracyte, said in a press release.
Find the full press release on the Veracyte website.
The Envisia Genomic Classifier, produced by Veracyte, has received final Medicare local coverage determination for the diagnosis of idiopathic pulmonary fibrosis (IPF).
Envisia is a complement to high-resolution CT that can help differentiate IPF from other interstitial lung diseases, as more than half of patients with IPF/interstitial lung disease report being misdiagnosed at least once. The test analyzes samples obtained through transbronchial biopsy, a nonsurgical procedure commonly used in lung evaluation. Envisia has been shown to detect usual interstitial pneumonia, a signature of IPF, with high accuracy.
The new policy was issued through the Palmetto GBA MolDx program and will go into effect on April 1, 2019, making Envisia the first commercially available test of its kind, available to the 55 million people who are currently enrolled in Medicare.
“We are pleased that the evidence supporting the Envisia classifier met the MolDx program’s high standards for coverage. This important milestone will enable us to begin making the Envisia Classifier more widely available to patients with suspected IPF so that they can obtain an accurate, timely diagnosis and, in turn, appropriate treatment,” Bonnie Anderson, chairman and chief executive officer of Veracyte, said in a press release.
Find the full press release on the Veracyte website.
The Envisia Genomic Classifier, produced by Veracyte, has received final Medicare local coverage determination for the diagnosis of idiopathic pulmonary fibrosis (IPF).
Envisia is a complement to high-resolution CT that can help differentiate IPF from other interstitial lung diseases, as more than half of patients with IPF/interstitial lung disease report being misdiagnosed at least once. The test analyzes samples obtained through transbronchial biopsy, a nonsurgical procedure commonly used in lung evaluation. Envisia has been shown to detect usual interstitial pneumonia, a signature of IPF, with high accuracy.
The new policy was issued through the Palmetto GBA MolDx program and will go into effect on April 1, 2019, making Envisia the first commercially available test of its kind, available to the 55 million people who are currently enrolled in Medicare.
“We are pleased that the evidence supporting the Envisia classifier met the MolDx program’s high standards for coverage. This important milestone will enable us to begin making the Envisia Classifier more widely available to patients with suspected IPF so that they can obtain an accurate, timely diagnosis and, in turn, appropriate treatment,” Bonnie Anderson, chairman and chief executive officer of Veracyte, said in a press release.
Find the full press release on the Veracyte website.
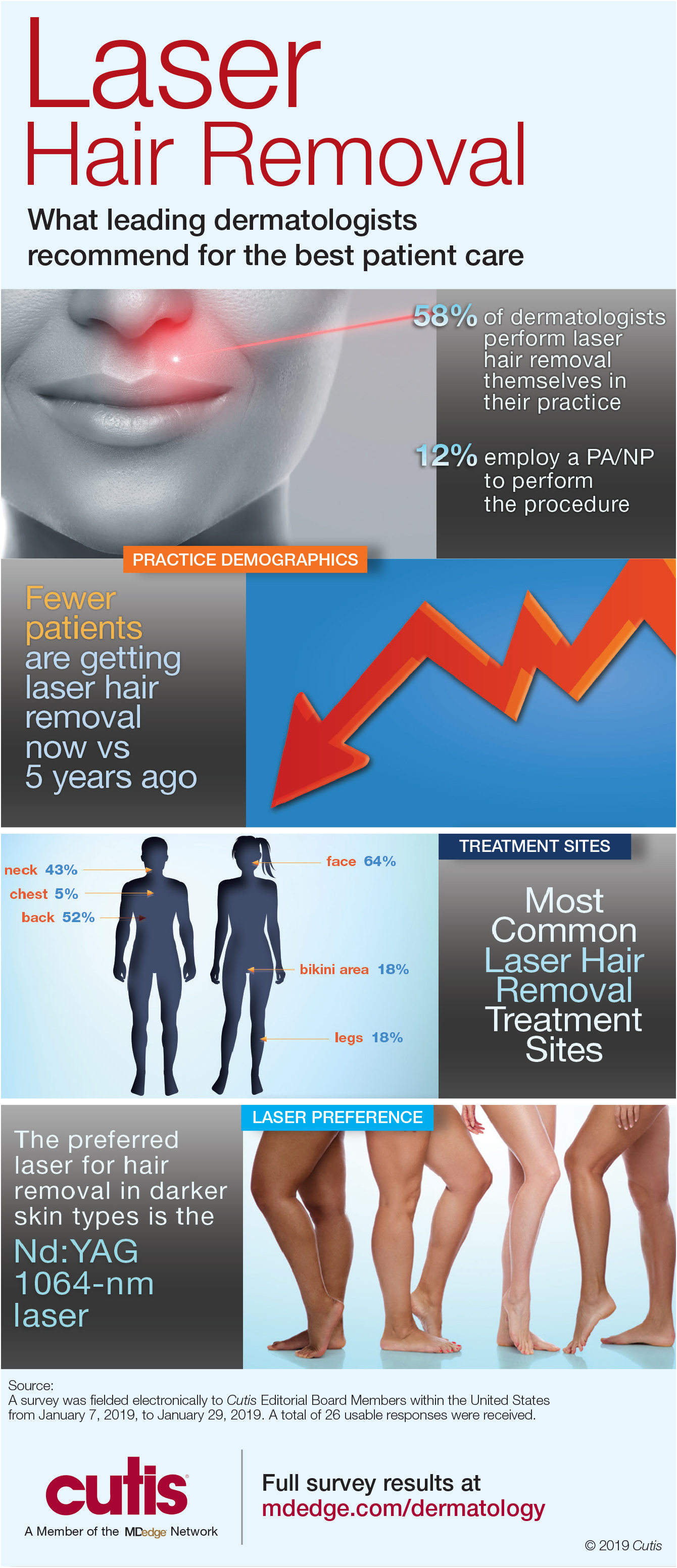
Infographic: Laser Hair Removal
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
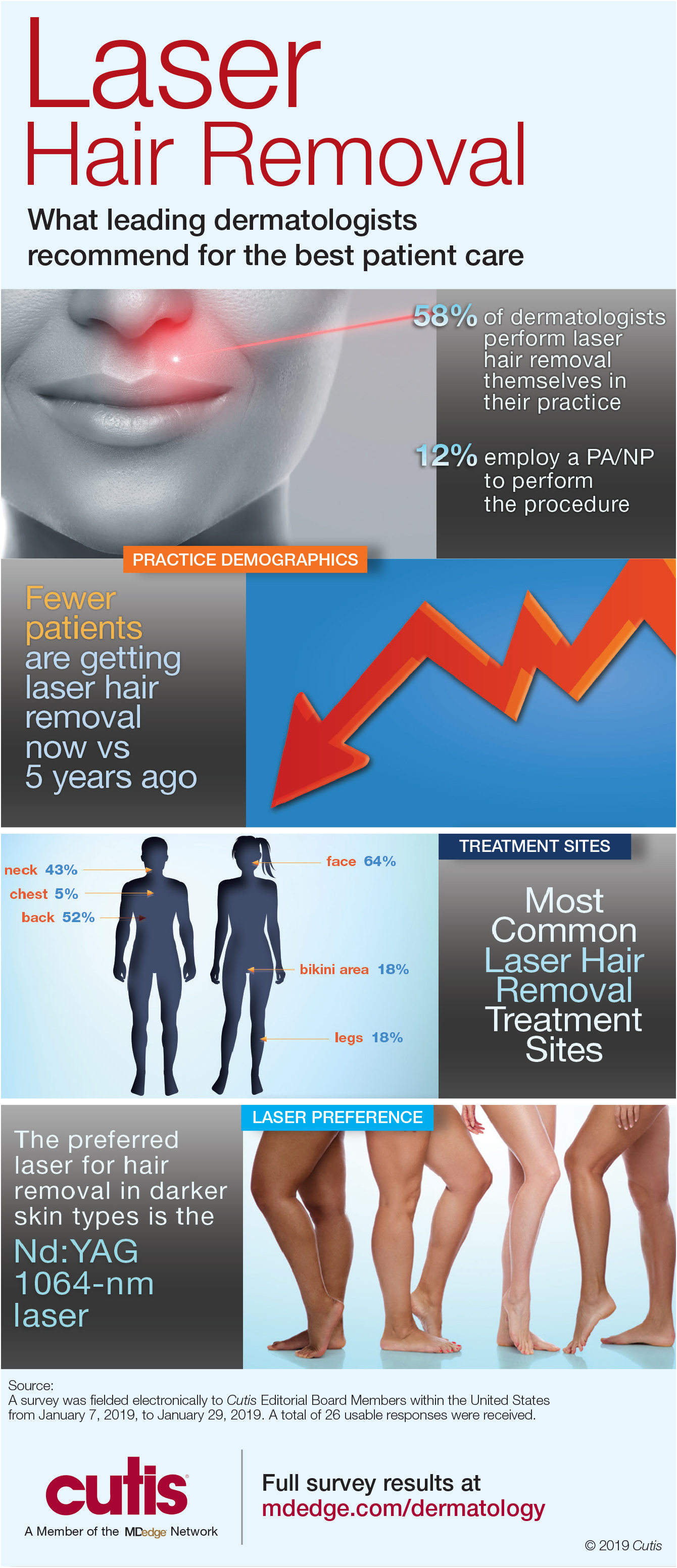
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
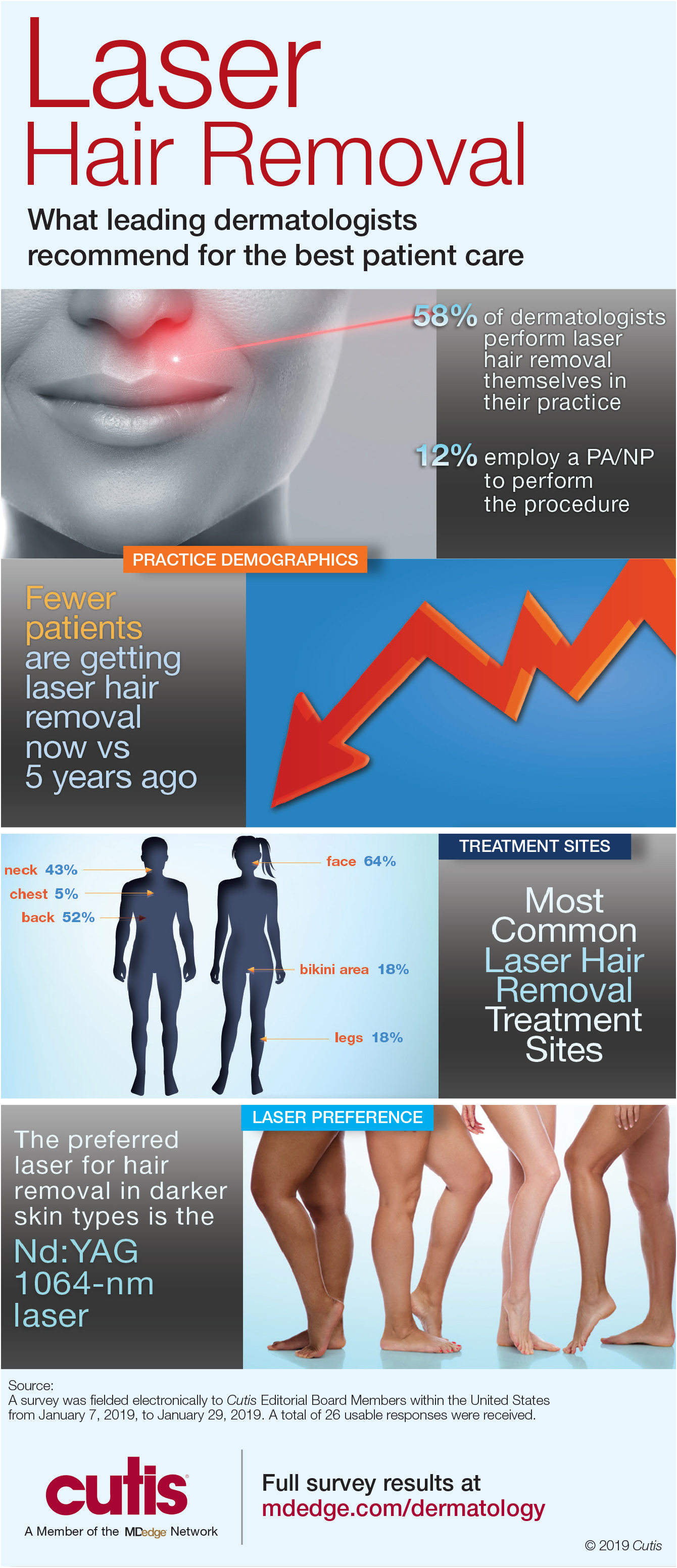
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
Women survive more often than men do when hospitalized with cirrhosis
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Atopic dermatitis at 1 year links with persistent food allergies
SAN FRANCISCO – Children diagnosed with atopic dermatitis when they were 1 year old were significantly more likely to have active food allergies and to have those allergies persist throughout childhood to age 18 years, based on findings from a prospective, longitudinal study of 287 Wisconsin children.
The link between atopic dermatitis (AD) and food allergy was especially strong in children who displayed early and recurrent AD; the link was weaker or essentially nonexistent for children with early transient AD or AD that first appeared later in childhood, Anne Marie Singh, MD, said while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The results also showed that even mild AD linked with an increased prevalence of food allergy when it appeared early and persisted, but more severe AD with this onset and recurrence pattern led to an even greater prevalence of food allergy, said Dr. Singh, a pediatric allergist and asthma specialist at the University of Wisconsin–Madison.
“The data suggest that something about early, recurrent AD increases the risk for food allergy throughout childhood,” Dr. Singh said in an interview. The findings suggest that surveillance for food allergies need to be intensified in infants who present with AD by the time they’re 1 year old and that food allergy surveillance should continue as these children age as long as their AD recurs.
The results also hint that these children might potentially benefit from steps aimed at desensitizing the allergy, although this must be proven in a future intervention study, she said.
The results suggest that a food allergy prevention regimen like the one used in the Learning Early About Peanut Allergy (LEAP) trial (New Engl J Med. 2015 Feb 26;372[9]:803-13) to prevent peanut allergy may be appropriate for selected, high-risk children with early AD, but this hypothesis needs testing, Dr. Singh said. She noted that some important differences exist between the patients enrolled in LEAP and the children studied in the current report: In LEAP, all enrolled children had severe eczema, an established egg allergy, or both. The findings reported by Dr. Singh came from children with AD, but only about 30% had moderate or severe eczema, and her analysis did not subdivide the observed food allergies by the type of food that caused a reaction.
She and her associates used data collected in the Childhood Origins of Asthma (COAST) study, begun in 1998, which enrolled 287 infants prior to birth who had at least one parent who was allergic, asthmatic, or both (Pediatr Allergy Immunol. 2002 Dec;13[s15]:38-43). The data showed that 62% of the infants had either no AD or transient AD, 14% had late onset AD, and 24% had early, recurrent AD. Although the data showed a statistically significant link between AD at 1 year old and food allergies throughout childhood, further analysis that broke the population into three different patterns of AD showed that the link with food allergy primarily existed among children with the early, recurrent form. Children with early, recurrent atopic dermatitis had a food allergy prevalence of 12%-27% annually through the age of 18 years.
“The data suggest that immunologic changes early in life are critical to food allergy development and that these changes have long-lasting effects throughout childhood,” Dr. Singh concluded. “The immunologic mechanisms by which early AD affects food allergy development and disease expression require further investigation.”
COAST received no commercial funding. Dr. Singh reported no relevant financial disclosures.
SOURCE: Singh AM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB125.
SAN FRANCISCO – Children diagnosed with atopic dermatitis when they were 1 year old were significantly more likely to have active food allergies and to have those allergies persist throughout childhood to age 18 years, based on findings from a prospective, longitudinal study of 287 Wisconsin children.
The link between atopic dermatitis (AD) and food allergy was especially strong in children who displayed early and recurrent AD; the link was weaker or essentially nonexistent for children with early transient AD or AD that first appeared later in childhood, Anne Marie Singh, MD, said while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The results also showed that even mild AD linked with an increased prevalence of food allergy when it appeared early and persisted, but more severe AD with this onset and recurrence pattern led to an even greater prevalence of food allergy, said Dr. Singh, a pediatric allergist and asthma specialist at the University of Wisconsin–Madison.
“The data suggest that something about early, recurrent AD increases the risk for food allergy throughout childhood,” Dr. Singh said in an interview. The findings suggest that surveillance for food allergies need to be intensified in infants who present with AD by the time they’re 1 year old and that food allergy surveillance should continue as these children age as long as their AD recurs.
The results also hint that these children might potentially benefit from steps aimed at desensitizing the allergy, although this must be proven in a future intervention study, she said.
The results suggest that a food allergy prevention regimen like the one used in the Learning Early About Peanut Allergy (LEAP) trial (New Engl J Med. 2015 Feb 26;372[9]:803-13) to prevent peanut allergy may be appropriate for selected, high-risk children with early AD, but this hypothesis needs testing, Dr. Singh said. She noted that some important differences exist between the patients enrolled in LEAP and the children studied in the current report: In LEAP, all enrolled children had severe eczema, an established egg allergy, or both. The findings reported by Dr. Singh came from children with AD, but only about 30% had moderate or severe eczema, and her analysis did not subdivide the observed food allergies by the type of food that caused a reaction.
She and her associates used data collected in the Childhood Origins of Asthma (COAST) study, begun in 1998, which enrolled 287 infants prior to birth who had at least one parent who was allergic, asthmatic, or both (Pediatr Allergy Immunol. 2002 Dec;13[s15]:38-43). The data showed that 62% of the infants had either no AD or transient AD, 14% had late onset AD, and 24% had early, recurrent AD. Although the data showed a statistically significant link between AD at 1 year old and food allergies throughout childhood, further analysis that broke the population into three different patterns of AD showed that the link with food allergy primarily existed among children with the early, recurrent form. Children with early, recurrent atopic dermatitis had a food allergy prevalence of 12%-27% annually through the age of 18 years.
“The data suggest that immunologic changes early in life are critical to food allergy development and that these changes have long-lasting effects throughout childhood,” Dr. Singh concluded. “The immunologic mechanisms by which early AD affects food allergy development and disease expression require further investigation.”
COAST received no commercial funding. Dr. Singh reported no relevant financial disclosures.
SOURCE: Singh AM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB125.
SAN FRANCISCO – Children diagnosed with atopic dermatitis when they were 1 year old were significantly more likely to have active food allergies and to have those allergies persist throughout childhood to age 18 years, based on findings from a prospective, longitudinal study of 287 Wisconsin children.
The link between atopic dermatitis (AD) and food allergy was especially strong in children who displayed early and recurrent AD; the link was weaker or essentially nonexistent for children with early transient AD or AD that first appeared later in childhood, Anne Marie Singh, MD, said while presenting a poster at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The results also showed that even mild AD linked with an increased prevalence of food allergy when it appeared early and persisted, but more severe AD with this onset and recurrence pattern led to an even greater prevalence of food allergy, said Dr. Singh, a pediatric allergist and asthma specialist at the University of Wisconsin–Madison.
“The data suggest that something about early, recurrent AD increases the risk for food allergy throughout childhood,” Dr. Singh said in an interview. The findings suggest that surveillance for food allergies need to be intensified in infants who present with AD by the time they’re 1 year old and that food allergy surveillance should continue as these children age as long as their AD recurs.
The results also hint that these children might potentially benefit from steps aimed at desensitizing the allergy, although this must be proven in a future intervention study, she said.
The results suggest that a food allergy prevention regimen like the one used in the Learning Early About Peanut Allergy (LEAP) trial (New Engl J Med. 2015 Feb 26;372[9]:803-13) to prevent peanut allergy may be appropriate for selected, high-risk children with early AD, but this hypothesis needs testing, Dr. Singh said. She noted that some important differences exist between the patients enrolled in LEAP and the children studied in the current report: In LEAP, all enrolled children had severe eczema, an established egg allergy, or both. The findings reported by Dr. Singh came from children with AD, but only about 30% had moderate or severe eczema, and her analysis did not subdivide the observed food allergies by the type of food that caused a reaction.
She and her associates used data collected in the Childhood Origins of Asthma (COAST) study, begun in 1998, which enrolled 287 infants prior to birth who had at least one parent who was allergic, asthmatic, or both (Pediatr Allergy Immunol. 2002 Dec;13[s15]:38-43). The data showed that 62% of the infants had either no AD or transient AD, 14% had late onset AD, and 24% had early, recurrent AD. Although the data showed a statistically significant link between AD at 1 year old and food allergies throughout childhood, further analysis that broke the population into three different patterns of AD showed that the link with food allergy primarily existed among children with the early, recurrent form. Children with early, recurrent atopic dermatitis had a food allergy prevalence of 12%-27% annually through the age of 18 years.
“The data suggest that immunologic changes early in life are critical to food allergy development and that these changes have long-lasting effects throughout childhood,” Dr. Singh concluded. “The immunologic mechanisms by which early AD affects food allergy development and disease expression require further investigation.”
COAST received no commercial funding. Dr. Singh reported no relevant financial disclosures.
SOURCE: Singh AM et al. J Allergy Clin Immunol. 2019 Feb;143[2]:AB125.
REPORTING FROM AAAAI 2019
Positive FIT test should prompt new colonoscopy
Patients who test positive on a fecal immunochemical test (FIT), even after a recent colonoscopy, should be offered a repeat colonoscopy. That is the conclusion following a review of 2,228 subjects who were FIT positive, which revealed a greater risk of colorectal cancer (CRC) and advanced colo-rectal neoplasia (ACRN) the longer the gap since the last colonoscopy. The findings support the recommendations of the U.S. Multi-Society Task Force on CRC Screening to offer repeat colonoscopies to FIT-positive patients, even if they recently underwent a colonoscopy.
That recommendation was based on low-quality supporting evidence, and there is currently little agreement about whether annual FIT should be performed along with colonoscopy.
The researchers set out to detect the frequency of CRC and ACRN among patients with a positive FIT test. They analyzed data from the National Cancer Screening Program in Korea, which offers an annual FIT for adults aged 50 years and older as an initial screening, followed by a colonoscopy in case of a positive result.
The researchers analyzed data from 52,376 individuals who underwent FIT at a single center in Korea during January 2013–July 2017. They excluded patients with a history of CRC or colorectal surgery, inflammatory bowel disease, or poor bowel preparation.
FIT-positive and FIT-negative patients were divided into three groups based on the length of time since their last colonoscopy: less than 3 years, 3-10 years, or more than 10 years or no colonoscopy.
Compared with FIT-negative subjects, FIT-positive individuals were more likely to be diagnosed with any colorectal neoplasia (61.3% vs. 51.8%; P less than .001), ACRN (20.0% vs. 10.3%; P less than .001), and CRC (5.0% vs. 1.9%; P less than .001).
A total of 6% of subjects had a positive FIT result, and data from 2,228 were analyzed after exclusions. They were compared with 6,135 participants who had negative FIT results but underwent a colonoscopy.
Of patients with a positive FIT result, 23.1% had a colonoscopy less than 3 years before, 19.2% had one 3-10 years prior, and 57.8% had a colonoscopy more than 10 years earlier or had never had one.
The more-than-10-year group had a higher frequency of colorectal neoplasia, ACRN, or CRC (26.0%) than did the 3 to 10-year group (12.6%), and the less-than-3-year group (10.9%; P less than .001 for all). A similar trend was seen for CRC: 7.2%, 1.6%, and 2.1%, respectively (P less than .001).
Of the 6,135 FIT-negative participants, 22.2% were in the less-than-3-years group, 28.9%, 3-10 years; and 48.8%, more-than-10 years-or-never group. The more-than-10-years group had a higher frequency of ACRN (14.7%) than did the 3 to 10-year group (0.4%) and the 0 to 3-year group (0.7%, P less than .001).
Among FIT-positive patients, the more-than-10-year group was at higher risk of ACRN diagnosis during follow-up colonoscopy than was the less-than-3-year group (adjusted OR, 3.63; 95% confidence interval, 2.48-5.31), but not compared with the 3-10-year group (aOR, 1.17; 95% CI, 0.71-1.93). The more-than-10-year group also was at greater risk of a CRC diagnosis than was the less-than-3-year group (aOR, 3.66; 95% CI, 1.74-7.73). There was no significant difference in CRC risk between the less-than-3-year group and the 3 to 10-year group (aOR, 0.58; 95% CI, 0.17-1.93).The authors suggest that CRC and ACRN found in patients who had a colonoscopy in the past 3 years are likely to be lesions that were missed in the previous exam, rather than new, fast-growing lesions. That suggests that FIT may help catch lesions that were missed during earlier screenings, though just 2.1% of the less-than-3-year group and 1.6% of the 3 to 10-year group were diagnosed with CRC, and 10.9% and 12.6% with ACRN, respectively.
The authors conclude that it may not be appropriate to offer interval FIT to all patients, since it can lead to unnecessary colonoscopies. They call for more research to determine which categories of patients are most likely to benefit from interval FIT.
The study received no funding. The authors reported no conflicts of interest.
March is Colorectal Cancer Awareness Month. AGA is here to help with patient education materials and a new video series. Visit http://crcawareness.gastro.org/ to access all the resources and share on your practice website and social media channels.
SOURCE: Kim NH et al. Gastrointest Endosc. 2019 Jan 23. doi: 10.1016/j.gie.2019.01.012.
Patients who test positive on a fecal immunochemical test (FIT), even after a recent colonoscopy, should be offered a repeat colonoscopy. That is the conclusion following a review of 2,228 subjects who were FIT positive, which revealed a greater risk of colorectal cancer (CRC) and advanced colo-rectal neoplasia (ACRN) the longer the gap since the last colonoscopy. The findings support the recommendations of the U.S. Multi-Society Task Force on CRC Screening to offer repeat colonoscopies to FIT-positive patients, even if they recently underwent a colonoscopy.
That recommendation was based on low-quality supporting evidence, and there is currently little agreement about whether annual FIT should be performed along with colonoscopy.
The researchers set out to detect the frequency of CRC and ACRN among patients with a positive FIT test. They analyzed data from the National Cancer Screening Program in Korea, which offers an annual FIT for adults aged 50 years and older as an initial screening, followed by a colonoscopy in case of a positive result.
The researchers analyzed data from 52,376 individuals who underwent FIT at a single center in Korea during January 2013–July 2017. They excluded patients with a history of CRC or colorectal surgery, inflammatory bowel disease, or poor bowel preparation.
FIT-positive and FIT-negative patients were divided into three groups based on the length of time since their last colonoscopy: less than 3 years, 3-10 years, or more than 10 years or no colonoscopy.
Compared with FIT-negative subjects, FIT-positive individuals were more likely to be diagnosed with any colorectal neoplasia (61.3% vs. 51.8%; P less than .001), ACRN (20.0% vs. 10.3%; P less than .001), and CRC (5.0% vs. 1.9%; P less than .001).
A total of 6% of subjects had a positive FIT result, and data from 2,228 were analyzed after exclusions. They were compared with 6,135 participants who had negative FIT results but underwent a colonoscopy.
Of patients with a positive FIT result, 23.1% had a colonoscopy less than 3 years before, 19.2% had one 3-10 years prior, and 57.8% had a colonoscopy more than 10 years earlier or had never had one.
The more-than-10-year group had a higher frequency of colorectal neoplasia, ACRN, or CRC (26.0%) than did the 3 to 10-year group (12.6%), and the less-than-3-year group (10.9%; P less than .001 for all). A similar trend was seen for CRC: 7.2%, 1.6%, and 2.1%, respectively (P less than .001).
Of the 6,135 FIT-negative participants, 22.2% were in the less-than-3-years group, 28.9%, 3-10 years; and 48.8%, more-than-10 years-or-never group. The more-than-10-years group had a higher frequency of ACRN (14.7%) than did the 3 to 10-year group (0.4%) and the 0 to 3-year group (0.7%, P less than .001).
Among FIT-positive patients, the more-than-10-year group was at higher risk of ACRN diagnosis during follow-up colonoscopy than was the less-than-3-year group (adjusted OR, 3.63; 95% confidence interval, 2.48-5.31), but not compared with the 3-10-year group (aOR, 1.17; 95% CI, 0.71-1.93). The more-than-10-year group also was at greater risk of a CRC diagnosis than was the less-than-3-year group (aOR, 3.66; 95% CI, 1.74-7.73). There was no significant difference in CRC risk between the less-than-3-year group and the 3 to 10-year group (aOR, 0.58; 95% CI, 0.17-1.93).The authors suggest that CRC and ACRN found in patients who had a colonoscopy in the past 3 years are likely to be lesions that were missed in the previous exam, rather than new, fast-growing lesions. That suggests that FIT may help catch lesions that were missed during earlier screenings, though just 2.1% of the less-than-3-year group and 1.6% of the 3 to 10-year group were diagnosed with CRC, and 10.9% and 12.6% with ACRN, respectively.
The authors conclude that it may not be appropriate to offer interval FIT to all patients, since it can lead to unnecessary colonoscopies. They call for more research to determine which categories of patients are most likely to benefit from interval FIT.
The study received no funding. The authors reported no conflicts of interest.
March is Colorectal Cancer Awareness Month. AGA is here to help with patient education materials and a new video series. Visit http://crcawareness.gastro.org/ to access all the resources and share on your practice website and social media channels.
SOURCE: Kim NH et al. Gastrointest Endosc. 2019 Jan 23. doi: 10.1016/j.gie.2019.01.012.
Patients who test positive on a fecal immunochemical test (FIT), even after a recent colonoscopy, should be offered a repeat colonoscopy. That is the conclusion following a review of 2,228 subjects who were FIT positive, which revealed a greater risk of colorectal cancer (CRC) and advanced colo-rectal neoplasia (ACRN) the longer the gap since the last colonoscopy. The findings support the recommendations of the U.S. Multi-Society Task Force on CRC Screening to offer repeat colonoscopies to FIT-positive patients, even if they recently underwent a colonoscopy.
That recommendation was based on low-quality supporting evidence, and there is currently little agreement about whether annual FIT should be performed along with colonoscopy.
The researchers set out to detect the frequency of CRC and ACRN among patients with a positive FIT test. They analyzed data from the National Cancer Screening Program in Korea, which offers an annual FIT for adults aged 50 years and older as an initial screening, followed by a colonoscopy in case of a positive result.
The researchers analyzed data from 52,376 individuals who underwent FIT at a single center in Korea during January 2013–July 2017. They excluded patients with a history of CRC or colorectal surgery, inflammatory bowel disease, or poor bowel preparation.
FIT-positive and FIT-negative patients were divided into three groups based on the length of time since their last colonoscopy: less than 3 years, 3-10 years, or more than 10 years or no colonoscopy.
Compared with FIT-negative subjects, FIT-positive individuals were more likely to be diagnosed with any colorectal neoplasia (61.3% vs. 51.8%; P less than .001), ACRN (20.0% vs. 10.3%; P less than .001), and CRC (5.0% vs. 1.9%; P less than .001).
A total of 6% of subjects had a positive FIT result, and data from 2,228 were analyzed after exclusions. They were compared with 6,135 participants who had negative FIT results but underwent a colonoscopy.
Of patients with a positive FIT result, 23.1% had a colonoscopy less than 3 years before, 19.2% had one 3-10 years prior, and 57.8% had a colonoscopy more than 10 years earlier or had never had one.
The more-than-10-year group had a higher frequency of colorectal neoplasia, ACRN, or CRC (26.0%) than did the 3 to 10-year group (12.6%), and the less-than-3-year group (10.9%; P less than .001 for all). A similar trend was seen for CRC: 7.2%, 1.6%, and 2.1%, respectively (P less than .001).
Of the 6,135 FIT-negative participants, 22.2% were in the less-than-3-years group, 28.9%, 3-10 years; and 48.8%, more-than-10 years-or-never group. The more-than-10-years group had a higher frequency of ACRN (14.7%) than did the 3 to 10-year group (0.4%) and the 0 to 3-year group (0.7%, P less than .001).
Among FIT-positive patients, the more-than-10-year group was at higher risk of ACRN diagnosis during follow-up colonoscopy than was the less-than-3-year group (adjusted OR, 3.63; 95% confidence interval, 2.48-5.31), but not compared with the 3-10-year group (aOR, 1.17; 95% CI, 0.71-1.93). The more-than-10-year group also was at greater risk of a CRC diagnosis than was the less-than-3-year group (aOR, 3.66; 95% CI, 1.74-7.73). There was no significant difference in CRC risk between the less-than-3-year group and the 3 to 10-year group (aOR, 0.58; 95% CI, 0.17-1.93).The authors suggest that CRC and ACRN found in patients who had a colonoscopy in the past 3 years are likely to be lesions that were missed in the previous exam, rather than new, fast-growing lesions. That suggests that FIT may help catch lesions that were missed during earlier screenings, though just 2.1% of the less-than-3-year group and 1.6% of the 3 to 10-year group were diagnosed with CRC, and 10.9% and 12.6% with ACRN, respectively.
The authors conclude that it may not be appropriate to offer interval FIT to all patients, since it can lead to unnecessary colonoscopies. They call for more research to determine which categories of patients are most likely to benefit from interval FIT.
The study received no funding. The authors reported no conflicts of interest.
March is Colorectal Cancer Awareness Month. AGA is here to help with patient education materials and a new video series. Visit http://crcawareness.gastro.org/ to access all the resources and share on your practice website and social media channels.
SOURCE: Kim NH et al. Gastrointest Endosc. 2019 Jan 23. doi: 10.1016/j.gie.2019.01.012.
Ixazomib targets treatment failure in chronic GVHD
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
REPORTING FROM TCT 2019
Key clinical point: Ixazomib may reduce treatment failure in patients with advanced chronic graft-versus-host disease.
Major finding: The 6-month treatment failure rate was significantly lower in this trial than in historical controls – 28% and 44%, respectively (P = .01).
Study details: A phase 2 trial of 50 patients with hematologic malignancies.
Disclosures: The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute. The investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda.
Source: Pidala J et al. TCT 2019, Abstract 35.
Survey: CRC diagnosis often delayed or initially missed in patients under age 50
The incidence of colorectal cancer in patients aged 20-49 years is increasing, but the diagnosis is often delayed in this age group because of a failure by both patients and physicians to recognize the symptoms as related to CRC, a survey suggests.
Of 1,195 colorectal cancer (CRC) patients or survivors aged under 50 years who responded to the web-based survey, 63% waited between 3 and 12 months before visiting their doctor after experiencing symptoms, including bloating, constipation, rectal bleeding, blood in stool, abdominal pain, flatulence, fatigue, or nausea and vomiting, Ronit I. Yarden, PhD, reported during a press conference highlighting data to be presented at the upcoming American Association for Cancer Research (AACR) annual meeting in Atlanta.
More than half of the respondents (56%) had at least three symptoms and still waited at least 3 months before visiting a doctor.
“And almost one in four waited at least a year to visit their doctor or other provider,” said Dr. Yarden, director of medical affairs for the Colorectal Cancer Alliance in Washington, D.C., which conducted the survey.
When patients did seek medical care, they often were initially misdiagnosed. In fact, 67% of the respondents reported having seen at least two physicians, with some seeing more than four physicians, before being diagnosed correctly with CRC, she said, noting that among the most common misdiagnoses were hemorrhoids and inflammatory bowel disease.
The delays in treatment and correct diagnoses have life-threatening implications; data show that, while the overall incidence of CRC is declining, the incidence in younger adults has increased. According to the American Cancer Society, most CRC patients over the age of 50 years are diagnosed in the early stages of disease, whereas 71% of the young-onset survey respondents were diagnosed at stage III or IV, Dr. Yarden said.
This is important, because 5-year survival is only 70% for stage III disease, and is less than 50% for stage IV disease. One in four survey respondents was diagnosed at stage IV, she said.
The survey included young-onset patients and survivors and was administered over social media to track the self-reported clinical, psychosocial, financial, and quality of life experiences of “this often-overlooked group,” she said.
The majority of participants (57%) were diagnosed between the ages of 40 and 49 years, a third were diagnosed between the ages of 30 and 39, and about 10% were diagnosed before the age of 30.
The findings underscore the need for greater awareness that “colorectal cancer, which is one of the most preventable diseases, can happen in younger adults,” Dr. Yarden said, also noting that extended screening is needed “if we want to beat this disease.”
John D. Carpten, PhD, the AACR meeting program chair and press conference comoderator, agreed that the findings could have significant policy implications, as many screening recommendations for CRC call for screening beginning at age 50 years.
“So for those individuals who are diagnosed with colon cancer in their 30s or 40s, this raises a potentially significant problem,” he said. “Additional studies need to be done to actually identify the factors influencing these early onset cancers. ... Hopefully that will improve our ability to detect these cancers earlier and to identify the most appropriate and effective ways to treat these cancers – particularly given that they tend to be diagnosed at more advanced stages.”
Work is also needed to help ensure access to the most appropriate care for younger patients – a concern related to disparities in health care access, he said, noting that the AACR meeting with “have a strong emphasis on disparities.”
Disparities can be related to race/ethnicity, rural versus urban setting, and socioeconomic factors, but they can also be related to age – which might be a particular problem in the case of early-onset CRC, he said.
Adolescent and young adult patients, in particular, represent “sort of a new disparity group,” and “can sometimes get lost in the system,” said Dr. Carpten, professor and chair of translational genomics and director of the Institute of Translational Genomics at the University of Southern California, Los Angeles.
“So we need to find better ways to detect these cancers earlier so we can manage these better,” he said.
This study was funded by the Colorectal Cancer Alliance. Dr. Yarden reported having no conflicts of interest.
SOURCE: Yarden R et al. AACR 2019, Abstract preview.
The incidence of colorectal cancer in patients aged 20-49 years is increasing, but the diagnosis is often delayed in this age group because of a failure by both patients and physicians to recognize the symptoms as related to CRC, a survey suggests.
Of 1,195 colorectal cancer (CRC) patients or survivors aged under 50 years who responded to the web-based survey, 63% waited between 3 and 12 months before visiting their doctor after experiencing symptoms, including bloating, constipation, rectal bleeding, blood in stool, abdominal pain, flatulence, fatigue, or nausea and vomiting, Ronit I. Yarden, PhD, reported during a press conference highlighting data to be presented at the upcoming American Association for Cancer Research (AACR) annual meeting in Atlanta.
More than half of the respondents (56%) had at least three symptoms and still waited at least 3 months before visiting a doctor.
“And almost one in four waited at least a year to visit their doctor or other provider,” said Dr. Yarden, director of medical affairs for the Colorectal Cancer Alliance in Washington, D.C., which conducted the survey.
When patients did seek medical care, they often were initially misdiagnosed. In fact, 67% of the respondents reported having seen at least two physicians, with some seeing more than four physicians, before being diagnosed correctly with CRC, she said, noting that among the most common misdiagnoses were hemorrhoids and inflammatory bowel disease.
The delays in treatment and correct diagnoses have life-threatening implications; data show that, while the overall incidence of CRC is declining, the incidence in younger adults has increased. According to the American Cancer Society, most CRC patients over the age of 50 years are diagnosed in the early stages of disease, whereas 71% of the young-onset survey respondents were diagnosed at stage III or IV, Dr. Yarden said.
This is important, because 5-year survival is only 70% for stage III disease, and is less than 50% for stage IV disease. One in four survey respondents was diagnosed at stage IV, she said.
The survey included young-onset patients and survivors and was administered over social media to track the self-reported clinical, psychosocial, financial, and quality of life experiences of “this often-overlooked group,” she said.
The majority of participants (57%) were diagnosed between the ages of 40 and 49 years, a third were diagnosed between the ages of 30 and 39, and about 10% were diagnosed before the age of 30.
The findings underscore the need for greater awareness that “colorectal cancer, which is one of the most preventable diseases, can happen in younger adults,” Dr. Yarden said, also noting that extended screening is needed “if we want to beat this disease.”
John D. Carpten, PhD, the AACR meeting program chair and press conference comoderator, agreed that the findings could have significant policy implications, as many screening recommendations for CRC call for screening beginning at age 50 years.
“So for those individuals who are diagnosed with colon cancer in their 30s or 40s, this raises a potentially significant problem,” he said. “Additional studies need to be done to actually identify the factors influencing these early onset cancers. ... Hopefully that will improve our ability to detect these cancers earlier and to identify the most appropriate and effective ways to treat these cancers – particularly given that they tend to be diagnosed at more advanced stages.”
Work is also needed to help ensure access to the most appropriate care for younger patients – a concern related to disparities in health care access, he said, noting that the AACR meeting with “have a strong emphasis on disparities.”
Disparities can be related to race/ethnicity, rural versus urban setting, and socioeconomic factors, but they can also be related to age – which might be a particular problem in the case of early-onset CRC, he said.
Adolescent and young adult patients, in particular, represent “sort of a new disparity group,” and “can sometimes get lost in the system,” said Dr. Carpten, professor and chair of translational genomics and director of the Institute of Translational Genomics at the University of Southern California, Los Angeles.
“So we need to find better ways to detect these cancers earlier so we can manage these better,” he said.
This study was funded by the Colorectal Cancer Alliance. Dr. Yarden reported having no conflicts of interest.
SOURCE: Yarden R et al. AACR 2019, Abstract preview.
The incidence of colorectal cancer in patients aged 20-49 years is increasing, but the diagnosis is often delayed in this age group because of a failure by both patients and physicians to recognize the symptoms as related to CRC, a survey suggests.
Of 1,195 colorectal cancer (CRC) patients or survivors aged under 50 years who responded to the web-based survey, 63% waited between 3 and 12 months before visiting their doctor after experiencing symptoms, including bloating, constipation, rectal bleeding, blood in stool, abdominal pain, flatulence, fatigue, or nausea and vomiting, Ronit I. Yarden, PhD, reported during a press conference highlighting data to be presented at the upcoming American Association for Cancer Research (AACR) annual meeting in Atlanta.
More than half of the respondents (56%) had at least three symptoms and still waited at least 3 months before visiting a doctor.
“And almost one in four waited at least a year to visit their doctor or other provider,” said Dr. Yarden, director of medical affairs for the Colorectal Cancer Alliance in Washington, D.C., which conducted the survey.
When patients did seek medical care, they often were initially misdiagnosed. In fact, 67% of the respondents reported having seen at least two physicians, with some seeing more than four physicians, before being diagnosed correctly with CRC, she said, noting that among the most common misdiagnoses were hemorrhoids and inflammatory bowel disease.
The delays in treatment and correct diagnoses have life-threatening implications; data show that, while the overall incidence of CRC is declining, the incidence in younger adults has increased. According to the American Cancer Society, most CRC patients over the age of 50 years are diagnosed in the early stages of disease, whereas 71% of the young-onset survey respondents were diagnosed at stage III or IV, Dr. Yarden said.
This is important, because 5-year survival is only 70% for stage III disease, and is less than 50% for stage IV disease. One in four survey respondents was diagnosed at stage IV, she said.
The survey included young-onset patients and survivors and was administered over social media to track the self-reported clinical, psychosocial, financial, and quality of life experiences of “this often-overlooked group,” she said.
The majority of participants (57%) were diagnosed between the ages of 40 and 49 years, a third were diagnosed between the ages of 30 and 39, and about 10% were diagnosed before the age of 30.
The findings underscore the need for greater awareness that “colorectal cancer, which is one of the most preventable diseases, can happen in younger adults,” Dr. Yarden said, also noting that extended screening is needed “if we want to beat this disease.”
John D. Carpten, PhD, the AACR meeting program chair and press conference comoderator, agreed that the findings could have significant policy implications, as many screening recommendations for CRC call for screening beginning at age 50 years.
“So for those individuals who are diagnosed with colon cancer in their 30s or 40s, this raises a potentially significant problem,” he said. “Additional studies need to be done to actually identify the factors influencing these early onset cancers. ... Hopefully that will improve our ability to detect these cancers earlier and to identify the most appropriate and effective ways to treat these cancers – particularly given that they tend to be diagnosed at more advanced stages.”
Work is also needed to help ensure access to the most appropriate care for younger patients – a concern related to disparities in health care access, he said, noting that the AACR meeting with “have a strong emphasis on disparities.”
Disparities can be related to race/ethnicity, rural versus urban setting, and socioeconomic factors, but they can also be related to age – which might be a particular problem in the case of early-onset CRC, he said.
Adolescent and young adult patients, in particular, represent “sort of a new disparity group,” and “can sometimes get lost in the system,” said Dr. Carpten, professor and chair of translational genomics and director of the Institute of Translational Genomics at the University of Southern California, Los Angeles.
“So we need to find better ways to detect these cancers earlier so we can manage these better,” he said.
This study was funded by the Colorectal Cancer Alliance. Dr. Yarden reported having no conflicts of interest.
SOURCE: Yarden R et al. AACR 2019, Abstract preview.
Whole genome sequencing benefits pediatric ICU patients
SAN DIEGO – In the pediatric intensive care unit (PICU), rapid whole genome sequencing (rWGS) with targeted phenotype analysis often leads to specific changes in patient management, similar to what is seen when rWGS is applied to neonatal ICUs. The findings come from the first study to look at outcomes of rWGS in the PICU outside of infancy.
In the NICU, previous studies have shown an rWGS diagnostic rate ranging from 36% to 57%, and an estimated 49%-72% of these diagnoses result in changes to patient management; 38%-45% of those diagnoses had not been previously considered.
The researchers found similar benefits when the age of patients was extended to 18 years in the PICU. “We were happy to see we were able to make specific changes in ICU management, with three of those being medication changes based on the diagnosis, and one being in the transition to palliative care while the patient was still in the PICU,” Erica Sanford, MD, said in an interview.
Dr. Sanford is a pediatric clinical care fellow at the University of California, San Diego. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Changes as a result of rWGS included factor replacement for a factor XIII deficiency, avoidance of renal biopsy because the diagnosis was made genetically, and use of serial MRI and other imaging methods to identify disorder-related sequela. “We’re hopeful as the turnaround for genome sequencing decreases that we’ll be able to offer this as a test when appropriate when a patient is presenting with an illness that doesn’t have a clear etiologic diagnosis,” said Dr. Sanford.
Certainly not every patient in the PICU should undergo rWGS, given its expense. Although the study was too small to identify candidate patients, there were some trends – patients in cardiac arrest were more likely to be receiving a genetic diagnosis. “We weren’t able to answer the question of which patients in the pediatric ICU should get whole genome sequencing – our next step is to have a larger group of patients so we can determine specifically which patients might benefit,” said Dr. Sanford. The team also plans to do a cost analysis of rWGS in the PICU setting.
The researchers examined data from a PICU at a tertiary children’s hospital, including records from 38 patients who underwent rWGS between July 2016 and May 2018. Based on the initial sequencing results, 18 underwent diagnostic rWGS. The average age of children was 5.7 years (median 3 years), with patients ranging from 4 months to 18 years old.
The most common reasons for PICU admission were shock (16% of all patients, 17% of patients who received diagnostic rWGS), respiratory failure (18% and 17%), cardiac arrest (13% and 22%), and altered mental status (13% and 11%).
Eleven of 18 patients (61%) who received an rWGS diagnosis experienced a subacute, non-ICU change in management. Four diagnoses (22%) led to a change in ICU management, and three led to no changes in patient management.
The National Institutes of Health funded the study. Dr. Sanford had no relevant financial disclosures.
SOURCE: Sanford E et al. CCC48, Abstract 373.
SAN DIEGO – In the pediatric intensive care unit (PICU), rapid whole genome sequencing (rWGS) with targeted phenotype analysis often leads to specific changes in patient management, similar to what is seen when rWGS is applied to neonatal ICUs. The findings come from the first study to look at outcomes of rWGS in the PICU outside of infancy.
In the NICU, previous studies have shown an rWGS diagnostic rate ranging from 36% to 57%, and an estimated 49%-72% of these diagnoses result in changes to patient management; 38%-45% of those diagnoses had not been previously considered.
The researchers found similar benefits when the age of patients was extended to 18 years in the PICU. “We were happy to see we were able to make specific changes in ICU management, with three of those being medication changes based on the diagnosis, and one being in the transition to palliative care while the patient was still in the PICU,” Erica Sanford, MD, said in an interview.
Dr. Sanford is a pediatric clinical care fellow at the University of California, San Diego. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Changes as a result of rWGS included factor replacement for a factor XIII deficiency, avoidance of renal biopsy because the diagnosis was made genetically, and use of serial MRI and other imaging methods to identify disorder-related sequela. “We’re hopeful as the turnaround for genome sequencing decreases that we’ll be able to offer this as a test when appropriate when a patient is presenting with an illness that doesn’t have a clear etiologic diagnosis,” said Dr. Sanford.
Certainly not every patient in the PICU should undergo rWGS, given its expense. Although the study was too small to identify candidate patients, there were some trends – patients in cardiac arrest were more likely to be receiving a genetic diagnosis. “We weren’t able to answer the question of which patients in the pediatric ICU should get whole genome sequencing – our next step is to have a larger group of patients so we can determine specifically which patients might benefit,” said Dr. Sanford. The team also plans to do a cost analysis of rWGS in the PICU setting.
The researchers examined data from a PICU at a tertiary children’s hospital, including records from 38 patients who underwent rWGS between July 2016 and May 2018. Based on the initial sequencing results, 18 underwent diagnostic rWGS. The average age of children was 5.7 years (median 3 years), with patients ranging from 4 months to 18 years old.
The most common reasons for PICU admission were shock (16% of all patients, 17% of patients who received diagnostic rWGS), respiratory failure (18% and 17%), cardiac arrest (13% and 22%), and altered mental status (13% and 11%).
Eleven of 18 patients (61%) who received an rWGS diagnosis experienced a subacute, non-ICU change in management. Four diagnoses (22%) led to a change in ICU management, and three led to no changes in patient management.
The National Institutes of Health funded the study. Dr. Sanford had no relevant financial disclosures.
SOURCE: Sanford E et al. CCC48, Abstract 373.
SAN DIEGO – In the pediatric intensive care unit (PICU), rapid whole genome sequencing (rWGS) with targeted phenotype analysis often leads to specific changes in patient management, similar to what is seen when rWGS is applied to neonatal ICUs. The findings come from the first study to look at outcomes of rWGS in the PICU outside of infancy.
In the NICU, previous studies have shown an rWGS diagnostic rate ranging from 36% to 57%, and an estimated 49%-72% of these diagnoses result in changes to patient management; 38%-45% of those diagnoses had not been previously considered.
The researchers found similar benefits when the age of patients was extended to 18 years in the PICU. “We were happy to see we were able to make specific changes in ICU management, with three of those being medication changes based on the diagnosis, and one being in the transition to palliative care while the patient was still in the PICU,” Erica Sanford, MD, said in an interview.
Dr. Sanford is a pediatric clinical care fellow at the University of California, San Diego. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Changes as a result of rWGS included factor replacement for a factor XIII deficiency, avoidance of renal biopsy because the diagnosis was made genetically, and use of serial MRI and other imaging methods to identify disorder-related sequela. “We’re hopeful as the turnaround for genome sequencing decreases that we’ll be able to offer this as a test when appropriate when a patient is presenting with an illness that doesn’t have a clear etiologic diagnosis,” said Dr. Sanford.
Certainly not every patient in the PICU should undergo rWGS, given its expense. Although the study was too small to identify candidate patients, there were some trends – patients in cardiac arrest were more likely to be receiving a genetic diagnosis. “We weren’t able to answer the question of which patients in the pediatric ICU should get whole genome sequencing – our next step is to have a larger group of patients so we can determine specifically which patients might benefit,” said Dr. Sanford. The team also plans to do a cost analysis of rWGS in the PICU setting.
The researchers examined data from a PICU at a tertiary children’s hospital, including records from 38 patients who underwent rWGS between July 2016 and May 2018. Based on the initial sequencing results, 18 underwent diagnostic rWGS. The average age of children was 5.7 years (median 3 years), with patients ranging from 4 months to 18 years old.
The most common reasons for PICU admission were shock (16% of all patients, 17% of patients who received diagnostic rWGS), respiratory failure (18% and 17%), cardiac arrest (13% and 22%), and altered mental status (13% and 11%).
Eleven of 18 patients (61%) who received an rWGS diagnosis experienced a subacute, non-ICU change in management. Four diagnoses (22%) led to a change in ICU management, and three led to no changes in patient management.
The National Institutes of Health funded the study. Dr. Sanford had no relevant financial disclosures.
SOURCE: Sanford E et al. CCC48, Abstract 373.
REPORTING FROM CCC48