User login
Physician PAC dollars support candidates against gun regulation
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
FROM JAMA NETWORK OPEN
What is the ‘microbiome’ and how may it influence gynecologic cancers?
Bacteria are everywhere, good and bad alike! It is well known in the scientific community that microbes significantly outnumber the cells in the human body by at least 10 times. Joshua Lederberg, PhD, gave meaning to the term “microbiome” in 2001 as the “ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space.”1 This community of microorganisms comprises bacteria, fungi, viruses, archaea, and protists.
In 2007, the National Institutes of Health Human Microbiome Project was established to study the human microbiome starting with five specific sites – the gastrointestinal tract, the mouth, the vagina, the skin, and nasal cavity. The goal was not only to identify the microbes inhabiting a specific body site but also to establish a range of “normal” for resident microbes as well as sequence the genomes of these microbes.2 Much of the research predating this era focused on microorganisms in terms of disease potential rather than a focus on the benefits of resident microorganisms.
The richness – the number of microorganisms in an area – and diversity – the relative proportion of microorganisms in an environment – can vary regionally. The microbiota that contribute to the class of resident microorganisms in a specific body habitat can be described broadly as commensals or mutualistic. With commensal microorganisms, one partner benefits and the other is unaffected. On the other hand, mutualistic microorganisms allow both parties to derive benefit. For example, resident microorganisms in the gut aid in the absorption of nutrients and in the production of vitamin K. On mucosal surfaces and the skin, it is possible that these resident microorganisms prevent colonization of pathogenic microbes, which could aid in prevention of disease.3
The microbiota composition can be influenced by multiple factors such as age, diet, medications, environment, early microbial exposure, and host genetics. The gut microbiota, for example, can be significantly altered by dietary intake or antibiotic use. Alterations in the diversity of microbes in certain body habitats has been linked to several human diseases such as obesity, inflammatory bowel disease, and bacterial vaginosis.4
In women, there are differences noted in the composition of resident microorganisms soon after birth as well as at prepubertal, postpubertal, and postmenopausal transitions. At puberty, anaerobic and aerobic lactobacilli aid in maintaining vaginal pH. If the normal microbiota is suppressed, it allows for yeast and other bacteria to grow causing vaginitis, and dramatic shifts in the makeup of the vaginal microbiota can lead to bacterial vaginosis. Interestingly, research has shown that the pH and microbiome of the vagina differs by ethnicity. These differences in composition of the vaginal microbiome likely contribute to known differences in the acquisition of sexually transmitted infections and development of bacterial vaginosis. The microbiome is believed to have a complex role in regulating human health and disease, including cancer.
There is growing evidence to suggest the gut microbiome may play an important role in the pathogenesis of both obesity and cancer. Two divisions of bacteria predominate in the gut in humans and mice, Bacteroidetes and Firmicutes, and the relative ratio of these two divisions is dramatically affected by obesity, such that Bacteroidetes levels decrease and Firmicutes levels increase.5 The change in the microbial environment leads to a greater ability to harvest dietary energy, which would be conducive to cancer development.
The microbiome and gynecologic cancers
The presence and relative abundance of bacterial species in the vagina are affected by unique factors such as hormonal contraception, pregnancy, and menopause. There are researchers investigating alterations in the microbiome of the vagina and implications in persistence of high-risk human papillomavirus infections and HPV-induced carcinogenesis. There were significant differences found in the composition of the vaginal microbiota in healthy women, compared with women with low-grade squamous intraepithelial neoplasm and high-grade squamous intraepithelial neoplasm.6
Conceivably, the subsequent clinical questions are: Can we apply this data to diagnose women at risk for dysplasia or can we alter the vaginal microbiome to impact the clearance rate of the HPV virus in susceptible or infected women to decrease the long-term risk of cervical dysplasia or malignancy?
The upper reproductive tract in women – the uterus, fallopian tubes, and ovaries – had been presumed to be a sterile environment. However, we know that bacteria have been isolated in the pre- and postmenopausal uterus of healthy women. Therefore, there also are investigators seeking to establish the microbiome of normal uteri to accurately compare it with malignant uteri. Notably, there also is interest in how treatments for cancer – chemotherapy and radiation – ultimately can affect a woman’s vaginal and gut microbiome.
Currently, microbiome research has an expansive range. Women will greatly benefit from research seeking to define improved prevention, diagnosis, and treatment based on alterations of the microbiome for common gynecologic premalignant and malignant conditions.
Dr. Hawkins is a fellow of gynecologic oncology and Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. They had no conflicts of interest to disclose.
References
1. “ ’Ome Sweet ’Omics – a genealogical treasury of words,” by Joshua Lederberg, The Scientist, Apr 2, 2001.
2. Genome Res. 2009 Dec;19(12):2317-23.
3. “Normal Human Microbiota,” Jawetz, Melnick & Adelberg’s Medical Microbiology, 27th edition (New York, NY: McGraw-Hill, 2016).
4. Nature. 2012 Jun 13;486(7402):207-14.
5. Nature. 2006 Dec 21;444(7122):1027-31.
6. Oncol Lett. 2018 Dec; 16(6): 7035-47.
Bacteria are everywhere, good and bad alike! It is well known in the scientific community that microbes significantly outnumber the cells in the human body by at least 10 times. Joshua Lederberg, PhD, gave meaning to the term “microbiome” in 2001 as the “ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space.”1 This community of microorganisms comprises bacteria, fungi, viruses, archaea, and protists.
In 2007, the National Institutes of Health Human Microbiome Project was established to study the human microbiome starting with five specific sites – the gastrointestinal tract, the mouth, the vagina, the skin, and nasal cavity. The goal was not only to identify the microbes inhabiting a specific body site but also to establish a range of “normal” for resident microbes as well as sequence the genomes of these microbes.2 Much of the research predating this era focused on microorganisms in terms of disease potential rather than a focus on the benefits of resident microorganisms.
The richness – the number of microorganisms in an area – and diversity – the relative proportion of microorganisms in an environment – can vary regionally. The microbiota that contribute to the class of resident microorganisms in a specific body habitat can be described broadly as commensals or mutualistic. With commensal microorganisms, one partner benefits and the other is unaffected. On the other hand, mutualistic microorganisms allow both parties to derive benefit. For example, resident microorganisms in the gut aid in the absorption of nutrients and in the production of vitamin K. On mucosal surfaces and the skin, it is possible that these resident microorganisms prevent colonization of pathogenic microbes, which could aid in prevention of disease.3
The microbiota composition can be influenced by multiple factors such as age, diet, medications, environment, early microbial exposure, and host genetics. The gut microbiota, for example, can be significantly altered by dietary intake or antibiotic use. Alterations in the diversity of microbes in certain body habitats has been linked to several human diseases such as obesity, inflammatory bowel disease, and bacterial vaginosis.4
In women, there are differences noted in the composition of resident microorganisms soon after birth as well as at prepubertal, postpubertal, and postmenopausal transitions. At puberty, anaerobic and aerobic lactobacilli aid in maintaining vaginal pH. If the normal microbiota is suppressed, it allows for yeast and other bacteria to grow causing vaginitis, and dramatic shifts in the makeup of the vaginal microbiota can lead to bacterial vaginosis. Interestingly, research has shown that the pH and microbiome of the vagina differs by ethnicity. These differences in composition of the vaginal microbiome likely contribute to known differences in the acquisition of sexually transmitted infections and development of bacterial vaginosis. The microbiome is believed to have a complex role in regulating human health and disease, including cancer.
There is growing evidence to suggest the gut microbiome may play an important role in the pathogenesis of both obesity and cancer. Two divisions of bacteria predominate in the gut in humans and mice, Bacteroidetes and Firmicutes, and the relative ratio of these two divisions is dramatically affected by obesity, such that Bacteroidetes levels decrease and Firmicutes levels increase.5 The change in the microbial environment leads to a greater ability to harvest dietary energy, which would be conducive to cancer development.
The microbiome and gynecologic cancers
The presence and relative abundance of bacterial species in the vagina are affected by unique factors such as hormonal contraception, pregnancy, and menopause. There are researchers investigating alterations in the microbiome of the vagina and implications in persistence of high-risk human papillomavirus infections and HPV-induced carcinogenesis. There were significant differences found in the composition of the vaginal microbiota in healthy women, compared with women with low-grade squamous intraepithelial neoplasm and high-grade squamous intraepithelial neoplasm.6
Conceivably, the subsequent clinical questions are: Can we apply this data to diagnose women at risk for dysplasia or can we alter the vaginal microbiome to impact the clearance rate of the HPV virus in susceptible or infected women to decrease the long-term risk of cervical dysplasia or malignancy?
The upper reproductive tract in women – the uterus, fallopian tubes, and ovaries – had been presumed to be a sterile environment. However, we know that bacteria have been isolated in the pre- and postmenopausal uterus of healthy women. Therefore, there also are investigators seeking to establish the microbiome of normal uteri to accurately compare it with malignant uteri. Notably, there also is interest in how treatments for cancer – chemotherapy and radiation – ultimately can affect a woman’s vaginal and gut microbiome.
Currently, microbiome research has an expansive range. Women will greatly benefit from research seeking to define improved prevention, diagnosis, and treatment based on alterations of the microbiome for common gynecologic premalignant and malignant conditions.
Dr. Hawkins is a fellow of gynecologic oncology and Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. They had no conflicts of interest to disclose.
References
1. “ ’Ome Sweet ’Omics – a genealogical treasury of words,” by Joshua Lederberg, The Scientist, Apr 2, 2001.
2. Genome Res. 2009 Dec;19(12):2317-23.
3. “Normal Human Microbiota,” Jawetz, Melnick & Adelberg’s Medical Microbiology, 27th edition (New York, NY: McGraw-Hill, 2016).
4. Nature. 2012 Jun 13;486(7402):207-14.
5. Nature. 2006 Dec 21;444(7122):1027-31.
6. Oncol Lett. 2018 Dec; 16(6): 7035-47.
Bacteria are everywhere, good and bad alike! It is well known in the scientific community that microbes significantly outnumber the cells in the human body by at least 10 times. Joshua Lederberg, PhD, gave meaning to the term “microbiome” in 2001 as the “ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space.”1 This community of microorganisms comprises bacteria, fungi, viruses, archaea, and protists.
In 2007, the National Institutes of Health Human Microbiome Project was established to study the human microbiome starting with five specific sites – the gastrointestinal tract, the mouth, the vagina, the skin, and nasal cavity. The goal was not only to identify the microbes inhabiting a specific body site but also to establish a range of “normal” for resident microbes as well as sequence the genomes of these microbes.2 Much of the research predating this era focused on microorganisms in terms of disease potential rather than a focus on the benefits of resident microorganisms.
The richness – the number of microorganisms in an area – and diversity – the relative proportion of microorganisms in an environment – can vary regionally. The microbiota that contribute to the class of resident microorganisms in a specific body habitat can be described broadly as commensals or mutualistic. With commensal microorganisms, one partner benefits and the other is unaffected. On the other hand, mutualistic microorganisms allow both parties to derive benefit. For example, resident microorganisms in the gut aid in the absorption of nutrients and in the production of vitamin K. On mucosal surfaces and the skin, it is possible that these resident microorganisms prevent colonization of pathogenic microbes, which could aid in prevention of disease.3
The microbiota composition can be influenced by multiple factors such as age, diet, medications, environment, early microbial exposure, and host genetics. The gut microbiota, for example, can be significantly altered by dietary intake or antibiotic use. Alterations in the diversity of microbes in certain body habitats has been linked to several human diseases such as obesity, inflammatory bowel disease, and bacterial vaginosis.4
In women, there are differences noted in the composition of resident microorganisms soon after birth as well as at prepubertal, postpubertal, and postmenopausal transitions. At puberty, anaerobic and aerobic lactobacilli aid in maintaining vaginal pH. If the normal microbiota is suppressed, it allows for yeast and other bacteria to grow causing vaginitis, and dramatic shifts in the makeup of the vaginal microbiota can lead to bacterial vaginosis. Interestingly, research has shown that the pH and microbiome of the vagina differs by ethnicity. These differences in composition of the vaginal microbiome likely contribute to known differences in the acquisition of sexually transmitted infections and development of bacterial vaginosis. The microbiome is believed to have a complex role in regulating human health and disease, including cancer.
There is growing evidence to suggest the gut microbiome may play an important role in the pathogenesis of both obesity and cancer. Two divisions of bacteria predominate in the gut in humans and mice, Bacteroidetes and Firmicutes, and the relative ratio of these two divisions is dramatically affected by obesity, such that Bacteroidetes levels decrease and Firmicutes levels increase.5 The change in the microbial environment leads to a greater ability to harvest dietary energy, which would be conducive to cancer development.
The microbiome and gynecologic cancers
The presence and relative abundance of bacterial species in the vagina are affected by unique factors such as hormonal contraception, pregnancy, and menopause. There are researchers investigating alterations in the microbiome of the vagina and implications in persistence of high-risk human papillomavirus infections and HPV-induced carcinogenesis. There were significant differences found in the composition of the vaginal microbiota in healthy women, compared with women with low-grade squamous intraepithelial neoplasm and high-grade squamous intraepithelial neoplasm.6
Conceivably, the subsequent clinical questions are: Can we apply this data to diagnose women at risk for dysplasia or can we alter the vaginal microbiome to impact the clearance rate of the HPV virus in susceptible or infected women to decrease the long-term risk of cervical dysplasia or malignancy?
The upper reproductive tract in women – the uterus, fallopian tubes, and ovaries – had been presumed to be a sterile environment. However, we know that bacteria have been isolated in the pre- and postmenopausal uterus of healthy women. Therefore, there also are investigators seeking to establish the microbiome of normal uteri to accurately compare it with malignant uteri. Notably, there also is interest in how treatments for cancer – chemotherapy and radiation – ultimately can affect a woman’s vaginal and gut microbiome.
Currently, microbiome research has an expansive range. Women will greatly benefit from research seeking to define improved prevention, diagnosis, and treatment based on alterations of the microbiome for common gynecologic premalignant and malignant conditions.
Dr. Hawkins is a fellow of gynecologic oncology and Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. They had no conflicts of interest to disclose.
References
1. “ ’Ome Sweet ’Omics – a genealogical treasury of words,” by Joshua Lederberg, The Scientist, Apr 2, 2001.
2. Genome Res. 2009 Dec;19(12):2317-23.
3. “Normal Human Microbiota,” Jawetz, Melnick & Adelberg’s Medical Microbiology, 27th edition (New York, NY: McGraw-Hill, 2016).
4. Nature. 2012 Jun 13;486(7402):207-14.
5. Nature. 2006 Dec 21;444(7122):1027-31.
6. Oncol Lett. 2018 Dec; 16(6): 7035-47.
Final ‘Vision’ report addresses MOC woes
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Palliative care has improved for critically ill children, but challenges remain
SAN DIEGO – and is more common among older children, female children, and those with government insurance or at a high risk of mortality. The findings come from a retrospective analysis of data from 52 hospitals, which included ICU admissions (except neonatal ICU) during 2007-2018.
The good news is that palliative care consultations have increased, with consultations in less than 1% of cases at the start of the study and rising quickly to more than 7% in 2018.
“In the adult world, palliative care has expanded in recent decades, and I think now that it’s coming to the pediatric world, it’ll just continue to go up,” said Siobhan O’Keefe, MD, in an interview. Dr. O’Keefe is with Children’s Hospital Colorado, Aurora. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
More work needs to be done, she said. “We are not uniformly using palliative care for critically ill children in the U.S., and it varies across institutions. That’s probably not the ideal situation,” said Dr. O’Keefe. The study did not track palliative care versus the presence of board-certified palliative care physicians or palliative care fellowships, but she suspects they would correlate.
Dr. O’Keefe called for physicians to think beyond the patient, to family members and caregivers. “We need to focus on family outcomes, how they are taking care of children with moderate disability, and incorporate that into our outcomes,” she said. Previous research has shown family members to be at risk of anxiety, depression, unemployment, and financial distress.
The researchers analyzed data from 740,890 patients with 1,024,666 hospitalizations (82% had one hospitalization). They divided subjects into three cohorts, one of which was a category of patients with criteria for palliative care based on previous research (PC-ICU). The PC-ICU cohort included patients with an expected length of stay more than 2 weeks, patients receiving extracorporeal membrane oxygenation (ECMO), severe brain injuries, acute respiratory failure with serious comorbidity, hematologic or oncologic disease, metabolic disease, renal failure that required continuous renal replacement therapy, hepatic failure, or serious chromosomal abnormality. A second cohort included chronic complex conditions not found in the PC-ICU cohort (additional criteria), and a third cohort had no criteria for palliative care.
Thirty percent of hospitalizations met the PC-ICU cohort criteria, 40% met the additional cohort criteria, and 30% fell in the no criteria cohort. The PC-ICU group had the highest mortality, at 8.03%, compared with 1.08% in the additional criteria group and 0.34% in the no criteria group (P less than .00001).
Palliative care consultations occurred more frequently in 5-12 year olds (odds ratio 1.06; 95% confidence interval, 1.01-1.13) and in those aged 13 years or older (OR, 1.38; 95% CI, 1.3-1.46), in females (OR, 1.13; 95% CI, 1.06-1.15), and in patients with government insurance (OR, 1.23; 95% CI, 1.17-1.29). Compared with those in the no criteria cohort, PC-ICU patients were more likely to receive a palliative care consult (OR, 75.5; 95% CI, 60.4-94.3), as were those in the additional criteria group (OR, 19.1; 95% CI, 15.3-23.9).
Cross-institutional palliative care frequency varied widely among patients in the PC-ICU group, ranging from 0% to 44%. The frequency ranged from 0% to 12% across institutions for patients in the additional criteria group.
SOURCE: O’Keefe S et al. Critical Care Congress 2019, Abstract 418.
SAN DIEGO – and is more common among older children, female children, and those with government insurance or at a high risk of mortality. The findings come from a retrospective analysis of data from 52 hospitals, which included ICU admissions (except neonatal ICU) during 2007-2018.
The good news is that palliative care consultations have increased, with consultations in less than 1% of cases at the start of the study and rising quickly to more than 7% in 2018.
“In the adult world, palliative care has expanded in recent decades, and I think now that it’s coming to the pediatric world, it’ll just continue to go up,” said Siobhan O’Keefe, MD, in an interview. Dr. O’Keefe is with Children’s Hospital Colorado, Aurora. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
More work needs to be done, she said. “We are not uniformly using palliative care for critically ill children in the U.S., and it varies across institutions. That’s probably not the ideal situation,” said Dr. O’Keefe. The study did not track palliative care versus the presence of board-certified palliative care physicians or palliative care fellowships, but she suspects they would correlate.
Dr. O’Keefe called for physicians to think beyond the patient, to family members and caregivers. “We need to focus on family outcomes, how they are taking care of children with moderate disability, and incorporate that into our outcomes,” she said. Previous research has shown family members to be at risk of anxiety, depression, unemployment, and financial distress.
The researchers analyzed data from 740,890 patients with 1,024,666 hospitalizations (82% had one hospitalization). They divided subjects into three cohorts, one of which was a category of patients with criteria for palliative care based on previous research (PC-ICU). The PC-ICU cohort included patients with an expected length of stay more than 2 weeks, patients receiving extracorporeal membrane oxygenation (ECMO), severe brain injuries, acute respiratory failure with serious comorbidity, hematologic or oncologic disease, metabolic disease, renal failure that required continuous renal replacement therapy, hepatic failure, or serious chromosomal abnormality. A second cohort included chronic complex conditions not found in the PC-ICU cohort (additional criteria), and a third cohort had no criteria for palliative care.
Thirty percent of hospitalizations met the PC-ICU cohort criteria, 40% met the additional cohort criteria, and 30% fell in the no criteria cohort. The PC-ICU group had the highest mortality, at 8.03%, compared with 1.08% in the additional criteria group and 0.34% in the no criteria group (P less than .00001).
Palliative care consultations occurred more frequently in 5-12 year olds (odds ratio 1.06; 95% confidence interval, 1.01-1.13) and in those aged 13 years or older (OR, 1.38; 95% CI, 1.3-1.46), in females (OR, 1.13; 95% CI, 1.06-1.15), and in patients with government insurance (OR, 1.23; 95% CI, 1.17-1.29). Compared with those in the no criteria cohort, PC-ICU patients were more likely to receive a palliative care consult (OR, 75.5; 95% CI, 60.4-94.3), as were those in the additional criteria group (OR, 19.1; 95% CI, 15.3-23.9).
Cross-institutional palliative care frequency varied widely among patients in the PC-ICU group, ranging from 0% to 44%. The frequency ranged from 0% to 12% across institutions for patients in the additional criteria group.
SOURCE: O’Keefe S et al. Critical Care Congress 2019, Abstract 418.
SAN DIEGO – and is more common among older children, female children, and those with government insurance or at a high risk of mortality. The findings come from a retrospective analysis of data from 52 hospitals, which included ICU admissions (except neonatal ICU) during 2007-2018.
The good news is that palliative care consultations have increased, with consultations in less than 1% of cases at the start of the study and rising quickly to more than 7% in 2018.
“In the adult world, palliative care has expanded in recent decades, and I think now that it’s coming to the pediatric world, it’ll just continue to go up,” said Siobhan O’Keefe, MD, in an interview. Dr. O’Keefe is with Children’s Hospital Colorado, Aurora. She presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
More work needs to be done, she said. “We are not uniformly using palliative care for critically ill children in the U.S., and it varies across institutions. That’s probably not the ideal situation,” said Dr. O’Keefe. The study did not track palliative care versus the presence of board-certified palliative care physicians or palliative care fellowships, but she suspects they would correlate.
Dr. O’Keefe called for physicians to think beyond the patient, to family members and caregivers. “We need to focus on family outcomes, how they are taking care of children with moderate disability, and incorporate that into our outcomes,” she said. Previous research has shown family members to be at risk of anxiety, depression, unemployment, and financial distress.
The researchers analyzed data from 740,890 patients with 1,024,666 hospitalizations (82% had one hospitalization). They divided subjects into three cohorts, one of which was a category of patients with criteria for palliative care based on previous research (PC-ICU). The PC-ICU cohort included patients with an expected length of stay more than 2 weeks, patients receiving extracorporeal membrane oxygenation (ECMO), severe brain injuries, acute respiratory failure with serious comorbidity, hematologic or oncologic disease, metabolic disease, renal failure that required continuous renal replacement therapy, hepatic failure, or serious chromosomal abnormality. A second cohort included chronic complex conditions not found in the PC-ICU cohort (additional criteria), and a third cohort had no criteria for palliative care.
Thirty percent of hospitalizations met the PC-ICU cohort criteria, 40% met the additional cohort criteria, and 30% fell in the no criteria cohort. The PC-ICU group had the highest mortality, at 8.03%, compared with 1.08% in the additional criteria group and 0.34% in the no criteria group (P less than .00001).
Palliative care consultations occurred more frequently in 5-12 year olds (odds ratio 1.06; 95% confidence interval, 1.01-1.13) and in those aged 13 years or older (OR, 1.38; 95% CI, 1.3-1.46), in females (OR, 1.13; 95% CI, 1.06-1.15), and in patients with government insurance (OR, 1.23; 95% CI, 1.17-1.29). Compared with those in the no criteria cohort, PC-ICU patients were more likely to receive a palliative care consult (OR, 75.5; 95% CI, 60.4-94.3), as were those in the additional criteria group (OR, 19.1; 95% CI, 15.3-23.9).
Cross-institutional palliative care frequency varied widely among patients in the PC-ICU group, ranging from 0% to 44%. The frequency ranged from 0% to 12% across institutions for patients in the additional criteria group.
SOURCE: O’Keefe S et al. Critical Care Congress 2019, Abstract 418.
REPORTING FROM CCC48
Alisertib response rate in PTCL patients was 33%
An open-label randomized phase 3 trial of oral alisertib for relapsed/refractory peripheral T-cell lymphoma (rrPTCL) was terminated in 2015 after it became clear that it was not going to prove significantly superior to options already on the market.
A new report explains what happened. Oral Alisertib was compared to two agents approved for rrPTCL: intravenous pralatrexate (Folotyn) and romidepsin (Istodax), as well as a common off-label option, intravenous gemcitabine (Gemzar). In all, 138 adults were randomized to alisertib 50 mg two times per day on days 1-7, with a median of four 21-day cycles; 133 were randomized to a comparator, the majority to gemcitabine, and again with repeated cycles as tolerated (J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899).
Overall response rate (ORR) was 33% for alisertib versus 45% for the comparator arm (odds ratio, 0.60; 95% confidence interval, 0.33-1.08). Median progression-free survival was 115 days for alisertib versus 104 days for the comparators, a non–statistically significant difference (hazard ratio, 0.87; 95% CI, 0.637-1.178). Median overall survival was 415 days in the alisertib arm versus 367 days in the comparator arm, also not statistically significant (HR, 0.98; 95% CI, 0.707-1.369).
In patients with rrPTCL, alisertib “did not demonstrate superior efficacy over comparators,” concluded investigators led by oncologist Owen A. O’Connor, MD, PhD, of the Columbia University Medical Center, New York.
Another downside to this drug is that it was associated with adverse events in more than half of patients who took it. While 53% of alisertib patients developed anemia and 47% became neutropenic, in the comparator arm, only 34% and 31% developed anemia and neutropenia, respectively. Further, three deaths in the trial were judged to have be related to alisertib. An additional two deaths occurred in this trial; those were judged to have been related to the rival treatments.
Despite alisertib’s less than great results, the story of this drug’s use for rrPTCL may not be over.
There were hints of benefits for rrPCLT, which might play out in a more focused trial, maybe “in a subgroup of patients with PTCL who responded poorly to comparator agents,” perhaps as a last ditch option. There’s also “potential for treatment combinations of alisertib with novel agents,” the investigators said.
The ORR differences were driven mostly by better performance with the approved agents: ORR was 61% with romidepsin and 43% with pralatrexate; however, alisertib’s ORR (33%) was similar to that for gemcitabine (35%) with “the potential benefits of ... oral administration,” the researchers said.
Also, the number of patients who discontinued treatment because of adverse events was higher in the comparator arm (14%) than in the alisertib group (9%), and more comparator patients required dose reductions (33% versus 28%) because of drug side effects.
Alisertib binds to and inhibits Aurora A kinase (AAK), which is essential for mitosis; studies have demonstrated overexpression in PTCL, which supports AAK inhibition as a novel therapeutic strategy. Research on alisertib for other cancer indications continues, including breast and lung cancer and leukemia.
Most of the subjects in both study arms were white, and about two-thirds were men; the median age was 63 years in both arms.
The work was funded by alisertib maker Millennium Pharmaceuticals, a subsidiary of Takeda. Dr. O’Connor and other investigators reported various ties to Millennium and Takeda, including research funding, honoraria, and consulting work. The study included employees of the companies.
SOURCE: O’Connor OA et al. J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899.
An open-label randomized phase 3 trial of oral alisertib for relapsed/refractory peripheral T-cell lymphoma (rrPTCL) was terminated in 2015 after it became clear that it was not going to prove significantly superior to options already on the market.
A new report explains what happened. Oral Alisertib was compared to two agents approved for rrPTCL: intravenous pralatrexate (Folotyn) and romidepsin (Istodax), as well as a common off-label option, intravenous gemcitabine (Gemzar). In all, 138 adults were randomized to alisertib 50 mg two times per day on days 1-7, with a median of four 21-day cycles; 133 were randomized to a comparator, the majority to gemcitabine, and again with repeated cycles as tolerated (J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899).
Overall response rate (ORR) was 33% for alisertib versus 45% for the comparator arm (odds ratio, 0.60; 95% confidence interval, 0.33-1.08). Median progression-free survival was 115 days for alisertib versus 104 days for the comparators, a non–statistically significant difference (hazard ratio, 0.87; 95% CI, 0.637-1.178). Median overall survival was 415 days in the alisertib arm versus 367 days in the comparator arm, also not statistically significant (HR, 0.98; 95% CI, 0.707-1.369).
In patients with rrPTCL, alisertib “did not demonstrate superior efficacy over comparators,” concluded investigators led by oncologist Owen A. O’Connor, MD, PhD, of the Columbia University Medical Center, New York.
Another downside to this drug is that it was associated with adverse events in more than half of patients who took it. While 53% of alisertib patients developed anemia and 47% became neutropenic, in the comparator arm, only 34% and 31% developed anemia and neutropenia, respectively. Further, three deaths in the trial were judged to have be related to alisertib. An additional two deaths occurred in this trial; those were judged to have been related to the rival treatments.
Despite alisertib’s less than great results, the story of this drug’s use for rrPTCL may not be over.
There were hints of benefits for rrPCLT, which might play out in a more focused trial, maybe “in a subgroup of patients with PTCL who responded poorly to comparator agents,” perhaps as a last ditch option. There’s also “potential for treatment combinations of alisertib with novel agents,” the investigators said.
The ORR differences were driven mostly by better performance with the approved agents: ORR was 61% with romidepsin and 43% with pralatrexate; however, alisertib’s ORR (33%) was similar to that for gemcitabine (35%) with “the potential benefits of ... oral administration,” the researchers said.
Also, the number of patients who discontinued treatment because of adverse events was higher in the comparator arm (14%) than in the alisertib group (9%), and more comparator patients required dose reductions (33% versus 28%) because of drug side effects.
Alisertib binds to and inhibits Aurora A kinase (AAK), which is essential for mitosis; studies have demonstrated overexpression in PTCL, which supports AAK inhibition as a novel therapeutic strategy. Research on alisertib for other cancer indications continues, including breast and lung cancer and leukemia.
Most of the subjects in both study arms were white, and about two-thirds were men; the median age was 63 years in both arms.
The work was funded by alisertib maker Millennium Pharmaceuticals, a subsidiary of Takeda. Dr. O’Connor and other investigators reported various ties to Millennium and Takeda, including research funding, honoraria, and consulting work. The study included employees of the companies.
SOURCE: O’Connor OA et al. J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899.
An open-label randomized phase 3 trial of oral alisertib for relapsed/refractory peripheral T-cell lymphoma (rrPTCL) was terminated in 2015 after it became clear that it was not going to prove significantly superior to options already on the market.
A new report explains what happened. Oral Alisertib was compared to two agents approved for rrPTCL: intravenous pralatrexate (Folotyn) and romidepsin (Istodax), as well as a common off-label option, intravenous gemcitabine (Gemzar). In all, 138 adults were randomized to alisertib 50 mg two times per day on days 1-7, with a median of four 21-day cycles; 133 were randomized to a comparator, the majority to gemcitabine, and again with repeated cycles as tolerated (J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899).
Overall response rate (ORR) was 33% for alisertib versus 45% for the comparator arm (odds ratio, 0.60; 95% confidence interval, 0.33-1.08). Median progression-free survival was 115 days for alisertib versus 104 days for the comparators, a non–statistically significant difference (hazard ratio, 0.87; 95% CI, 0.637-1.178). Median overall survival was 415 days in the alisertib arm versus 367 days in the comparator arm, also not statistically significant (HR, 0.98; 95% CI, 0.707-1.369).
In patients with rrPTCL, alisertib “did not demonstrate superior efficacy over comparators,” concluded investigators led by oncologist Owen A. O’Connor, MD, PhD, of the Columbia University Medical Center, New York.
Another downside to this drug is that it was associated with adverse events in more than half of patients who took it. While 53% of alisertib patients developed anemia and 47% became neutropenic, in the comparator arm, only 34% and 31% developed anemia and neutropenia, respectively. Further, three deaths in the trial were judged to have be related to alisertib. An additional two deaths occurred in this trial; those were judged to have been related to the rival treatments.
Despite alisertib’s less than great results, the story of this drug’s use for rrPTCL may not be over.
There were hints of benefits for rrPCLT, which might play out in a more focused trial, maybe “in a subgroup of patients with PTCL who responded poorly to comparator agents,” perhaps as a last ditch option. There’s also “potential for treatment combinations of alisertib with novel agents,” the investigators said.
The ORR differences were driven mostly by better performance with the approved agents: ORR was 61% with romidepsin and 43% with pralatrexate; however, alisertib’s ORR (33%) was similar to that for gemcitabine (35%) with “the potential benefits of ... oral administration,” the researchers said.
Also, the number of patients who discontinued treatment because of adverse events was higher in the comparator arm (14%) than in the alisertib group (9%), and more comparator patients required dose reductions (33% versus 28%) because of drug side effects.
Alisertib binds to and inhibits Aurora A kinase (AAK), which is essential for mitosis; studies have demonstrated overexpression in PTCL, which supports AAK inhibition as a novel therapeutic strategy. Research on alisertib for other cancer indications continues, including breast and lung cancer and leukemia.
Most of the subjects in both study arms were white, and about two-thirds were men; the median age was 63 years in both arms.
The work was funded by alisertib maker Millennium Pharmaceuticals, a subsidiary of Takeda. Dr. O’Connor and other investigators reported various ties to Millennium and Takeda, including research funding, honoraria, and consulting work. The study included employees of the companies.
SOURCE: O’Connor OA et al. J Clin Oncol. 2019 Feb 1. doi: 10.1200/JCO.18.00899.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Protecting Older Women Against HIV Infection
Older women represent 56% of all women with HIV, and in a 2009 study, they had the highest rates of HIV- and AIDS-related deaths. But few HIV prevention and education programs focus on older women, says Christopher Coleman, PhD, MPH, department chair and professor, Department of Health Promotion and Disease Prevention, The University of Tennessee Health Science Center, College of Nursing. Moreover, sexual health studies mainly concentrate on younger women and reproductive health, not risk factors for HIV among older women.
Coleman says the “confluence of lack of knowledge and absent communication about HIV risk has created a significant health crisis” for this group. He reviewed 41 articles that provide some insight.
Ageism, biological factors, and lack of education all play a part. Some research has found that older women are less likely to engage in safe sex practices because they no longer use condoms to prevent pregnancy. The National AIDS Behavior Survey found that > 85% of respondents aged ≥ 50 years reported never using condoms or using them inconsistently. However, women in the postmenopausal age group are sexually active, and because they may be divorced or widowed, may not be in committed relationships. Also, age-related physical changes, such as thinning vaginal tissue and a weakened immune system, can make them more vulnerable to infection.
The problem is compounded when an older woman is unwilling to bring up the topic with health care providers—and health care providers are unwilling to believe that she is sexually active. Women aged > 50 years may also avoid seeking HIV testing due to social factors. And they may be prevented from traveling to health care or testing by poor physical health or other age-related issues.
We need new methods of reaching them, Coleman says. Existing HIV/AIDS instructional programs may not be effective tools for women with age-related comorbidities, such as cognitive, visual, or auditory deficits. Other options should be considered: For instance, small peer groups have been more successful than large groups, providing a sense of safety and belonging that encourages disclosure.
Health care providers should include education during routine office visits, Coleman advises, using non-ageist and nonstereotyping strategies and questions. Nurses are well positioned to educate women about the risks of HIV transmission; he says: discussing sexual activity with older women requires the “art of therapeutic communication without judgment.”
Older women represent 56% of all women with HIV, and in a 2009 study, they had the highest rates of HIV- and AIDS-related deaths. But few HIV prevention and education programs focus on older women, says Christopher Coleman, PhD, MPH, department chair and professor, Department of Health Promotion and Disease Prevention, The University of Tennessee Health Science Center, College of Nursing. Moreover, sexual health studies mainly concentrate on younger women and reproductive health, not risk factors for HIV among older women.
Coleman says the “confluence of lack of knowledge and absent communication about HIV risk has created a significant health crisis” for this group. He reviewed 41 articles that provide some insight.
Ageism, biological factors, and lack of education all play a part. Some research has found that older women are less likely to engage in safe sex practices because they no longer use condoms to prevent pregnancy. The National AIDS Behavior Survey found that > 85% of respondents aged ≥ 50 years reported never using condoms or using them inconsistently. However, women in the postmenopausal age group are sexually active, and because they may be divorced or widowed, may not be in committed relationships. Also, age-related physical changes, such as thinning vaginal tissue and a weakened immune system, can make them more vulnerable to infection.
The problem is compounded when an older woman is unwilling to bring up the topic with health care providers—and health care providers are unwilling to believe that she is sexually active. Women aged > 50 years may also avoid seeking HIV testing due to social factors. And they may be prevented from traveling to health care or testing by poor physical health or other age-related issues.
We need new methods of reaching them, Coleman says. Existing HIV/AIDS instructional programs may not be effective tools for women with age-related comorbidities, such as cognitive, visual, or auditory deficits. Other options should be considered: For instance, small peer groups have been more successful than large groups, providing a sense of safety and belonging that encourages disclosure.
Health care providers should include education during routine office visits, Coleman advises, using non-ageist and nonstereotyping strategies and questions. Nurses are well positioned to educate women about the risks of HIV transmission; he says: discussing sexual activity with older women requires the “art of therapeutic communication without judgment.”
Older women represent 56% of all women with HIV, and in a 2009 study, they had the highest rates of HIV- and AIDS-related deaths. But few HIV prevention and education programs focus on older women, says Christopher Coleman, PhD, MPH, department chair and professor, Department of Health Promotion and Disease Prevention, The University of Tennessee Health Science Center, College of Nursing. Moreover, sexual health studies mainly concentrate on younger women and reproductive health, not risk factors for HIV among older women.
Coleman says the “confluence of lack of knowledge and absent communication about HIV risk has created a significant health crisis” for this group. He reviewed 41 articles that provide some insight.
Ageism, biological factors, and lack of education all play a part. Some research has found that older women are less likely to engage in safe sex practices because they no longer use condoms to prevent pregnancy. The National AIDS Behavior Survey found that > 85% of respondents aged ≥ 50 years reported never using condoms or using them inconsistently. However, women in the postmenopausal age group are sexually active, and because they may be divorced or widowed, may not be in committed relationships. Also, age-related physical changes, such as thinning vaginal tissue and a weakened immune system, can make them more vulnerable to infection.
The problem is compounded when an older woman is unwilling to bring up the topic with health care providers—and health care providers are unwilling to believe that she is sexually active. Women aged > 50 years may also avoid seeking HIV testing due to social factors. And they may be prevented from traveling to health care or testing by poor physical health or other age-related issues.
We need new methods of reaching them, Coleman says. Existing HIV/AIDS instructional programs may not be effective tools for women with age-related comorbidities, such as cognitive, visual, or auditory deficits. Other options should be considered: For instance, small peer groups have been more successful than large groups, providing a sense of safety and belonging that encourages disclosure.
Health care providers should include education during routine office visits, Coleman advises, using non-ageist and nonstereotyping strategies and questions. Nurses are well positioned to educate women about the risks of HIV transmission; he says: discussing sexual activity with older women requires the “art of therapeutic communication without judgment.”
Trump bars abortion referrals from family planning program
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
Influenza activity continues to increase
The 2018-2019 flu season is showing no signs of decline as activity measures continued to increase into mid-February, according to the Centers for Disease Control and Prevention.
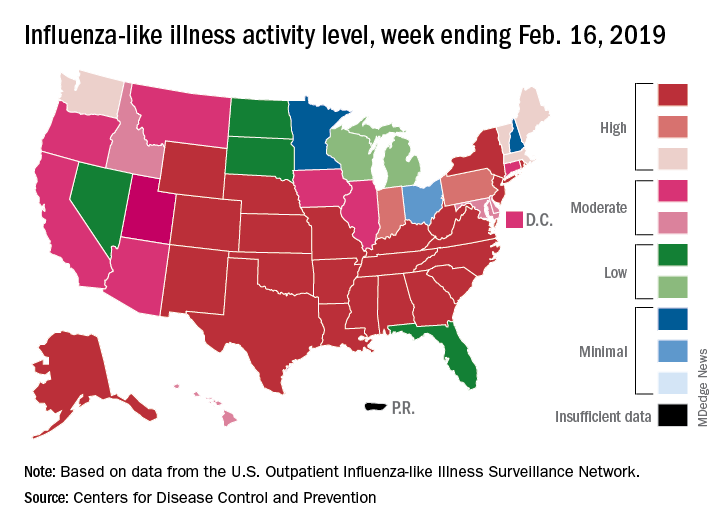
Eight of the last 10 flu seasons had already reached their peak before mid-February, but another rise brought the proportion of outpatient visits for influenza-like illness (ILI) to 5.1% for the week ending Feb. 16, compared with 4.8% the week before, the CDC’s influenza division reported Feb. 22. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
The week also brought more ILI to more states, as the number reporting an activity level of 10 on the CDC’s 1-10 scale rose from 21 to 24 and the number in the high range of 8-10 increased from 26 to 30. Another seven states – including California, which was at level 5 the previous week – and the District of Columbia were at level 7 for the current reporting week, the CDC said.
Two flu-related pediatric deaths occurred during the week ending Feb. 16 and another five were reported from previous weeks, which brings the total to 41 for the 2018-2019 season. Data for influenza deaths at all ages, which are reported a week later, show that 205 occurred in the week ending Feb. 9, with reporting 75% complete. There were 236 total deaths for the week ending Feb. 2 (94% reporting) and 218 deaths during the week ending Jan. 26 (99% reporting), the CDC said.
The 2018-2019 flu season is showing no signs of decline as activity measures continued to increase into mid-February, according to the Centers for Disease Control and Prevention.
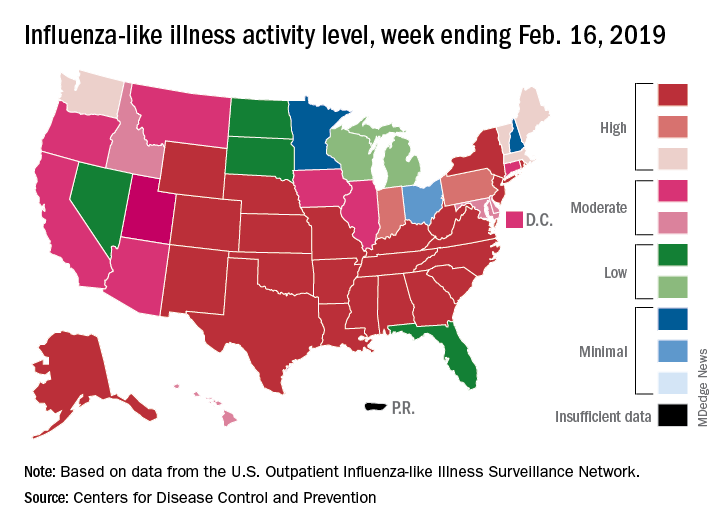
Eight of the last 10 flu seasons had already reached their peak before mid-February, but another rise brought the proportion of outpatient visits for influenza-like illness (ILI) to 5.1% for the week ending Feb. 16, compared with 4.8% the week before, the CDC’s influenza division reported Feb. 22. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
The week also brought more ILI to more states, as the number reporting an activity level of 10 on the CDC’s 1-10 scale rose from 21 to 24 and the number in the high range of 8-10 increased from 26 to 30. Another seven states – including California, which was at level 5 the previous week – and the District of Columbia were at level 7 for the current reporting week, the CDC said.
Two flu-related pediatric deaths occurred during the week ending Feb. 16 and another five were reported from previous weeks, which brings the total to 41 for the 2018-2019 season. Data for influenza deaths at all ages, which are reported a week later, show that 205 occurred in the week ending Feb. 9, with reporting 75% complete. There were 236 total deaths for the week ending Feb. 2 (94% reporting) and 218 deaths during the week ending Jan. 26 (99% reporting), the CDC said.
The 2018-2019 flu season is showing no signs of decline as activity measures continued to increase into mid-February, according to the Centers for Disease Control and Prevention.
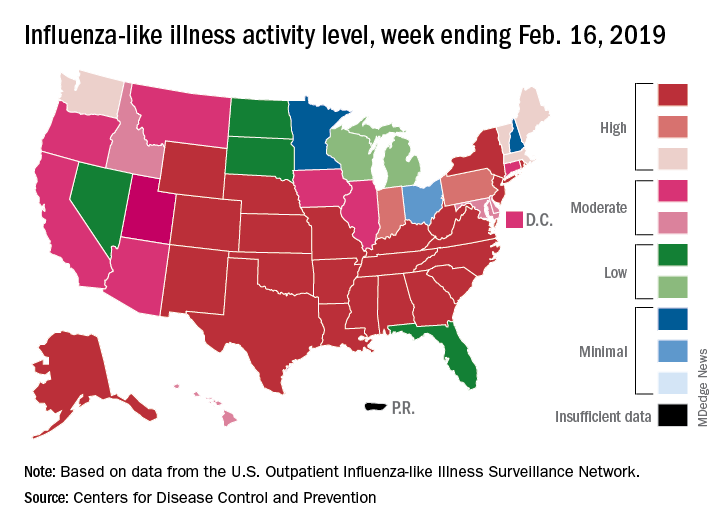
Eight of the last 10 flu seasons had already reached their peak before mid-February, but another rise brought the proportion of outpatient visits for influenza-like illness (ILI) to 5.1% for the week ending Feb. 16, compared with 4.8% the week before, the CDC’s influenza division reported Feb. 22. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
The week also brought more ILI to more states, as the number reporting an activity level of 10 on the CDC’s 1-10 scale rose from 21 to 24 and the number in the high range of 8-10 increased from 26 to 30. Another seven states – including California, which was at level 5 the previous week – and the District of Columbia were at level 7 for the current reporting week, the CDC said.
Two flu-related pediatric deaths occurred during the week ending Feb. 16 and another five were reported from previous weeks, which brings the total to 41 for the 2018-2019 season. Data for influenza deaths at all ages, which are reported a week later, show that 205 occurred in the week ending Feb. 9, with reporting 75% complete. There were 236 total deaths for the week ending Feb. 2 (94% reporting) and 218 deaths during the week ending Jan. 26 (99% reporting), the CDC said.
Smoking cessation could delay or prevent rheumatoid arthritis
Smoking is a significant risk factor for seropositive rheumatoid arthritis, and quitting may delay or even prevent the disease, a study has found.
In a paper published in Arthritis Care & Research, researchers report the analysis of data from 230,732 women – including 1,528 individuals with rheumatoid arthritis – participating in the Nurses’ Health Study (NHS) and NHS II.
They saw that current smokers had a significant 67% increased risk for seropositive rheumatoid arthritis (RA), compared with never smokers, while those who smoked 25 or more cigarettes per day had a 92% higher risk.
There was an increasing trend of association between pack-years of smoking and seropositive RA such that 35 pack-years of exposure was associated with a 2.3-fold higher risk for seropositive RA, compared with never smokers (P less than .0001).
Xinyi Liu of the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston, and her coauthors noted that the population attributable risk of RA from smoking was 14% and that smoking could contribute up to 35% of seropositive RA risk.
“Although the biologic mechanisms linking smoking with increased risk for developing RA are still not clear, components in cigarette smoke, such as nicotine, hydrocarbons, and carbon monoxide, are known to have aberrant effects on the immune system,” the authors wrote.
The good news was that sustained smoking cessation significantly reduced the risk of RA and seropositive RA, and those benefits increased with the amount of time since the individual stopped smoking.
Women who had quit smoking at least 30 years prior showed a 22% lower risk of all RA and a 37% lower risk of seropositive RA, compared with those who had quit within the previous 5 years. However, even 30 years after quitting, there was still a 30% higher risk of seropositive rheumatoid arthritis, compared with the risk among women who had never smoked.
“While smoking cessation may not decrease RA risk to the level of a never smoker, our findings provide evidence that a behavior change of smoking cessation may delay or even prevent the onset of seropositive RA,” the authors wrote. “These results could provide rationale for a smoking intervention trial among active smokers to prevent the formation of RA-related autoantibodies or to prevent the progression to RA among those at elevated risk for seropositive RA.”
Commenting on the difference in associations with seropositive and seronegative rheumatoid arthritis and smoking behavior, the authors wrote this suggested these two types of the disease may represent separate phenotypes with different risk factors.
The National Institutes of Health supported the study. No conflicts of interest were declared.
SOURCE: Liu X et al. Arthritis Care Res. 2019 Feb 21. doi: 10.1002/acr.23837.
Smoking is a significant risk factor for seropositive rheumatoid arthritis, and quitting may delay or even prevent the disease, a study has found.
In a paper published in Arthritis Care & Research, researchers report the analysis of data from 230,732 women – including 1,528 individuals with rheumatoid arthritis – participating in the Nurses’ Health Study (NHS) and NHS II.
They saw that current smokers had a significant 67% increased risk for seropositive rheumatoid arthritis (RA), compared with never smokers, while those who smoked 25 or more cigarettes per day had a 92% higher risk.
There was an increasing trend of association between pack-years of smoking and seropositive RA such that 35 pack-years of exposure was associated with a 2.3-fold higher risk for seropositive RA, compared with never smokers (P less than .0001).
Xinyi Liu of the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston, and her coauthors noted that the population attributable risk of RA from smoking was 14% and that smoking could contribute up to 35% of seropositive RA risk.
“Although the biologic mechanisms linking smoking with increased risk for developing RA are still not clear, components in cigarette smoke, such as nicotine, hydrocarbons, and carbon monoxide, are known to have aberrant effects on the immune system,” the authors wrote.
The good news was that sustained smoking cessation significantly reduced the risk of RA and seropositive RA, and those benefits increased with the amount of time since the individual stopped smoking.
Women who had quit smoking at least 30 years prior showed a 22% lower risk of all RA and a 37% lower risk of seropositive RA, compared with those who had quit within the previous 5 years. However, even 30 years after quitting, there was still a 30% higher risk of seropositive rheumatoid arthritis, compared with the risk among women who had never smoked.
“While smoking cessation may not decrease RA risk to the level of a never smoker, our findings provide evidence that a behavior change of smoking cessation may delay or even prevent the onset of seropositive RA,” the authors wrote. “These results could provide rationale for a smoking intervention trial among active smokers to prevent the formation of RA-related autoantibodies or to prevent the progression to RA among those at elevated risk for seropositive RA.”
Commenting on the difference in associations with seropositive and seronegative rheumatoid arthritis and smoking behavior, the authors wrote this suggested these two types of the disease may represent separate phenotypes with different risk factors.
The National Institutes of Health supported the study. No conflicts of interest were declared.
SOURCE: Liu X et al. Arthritis Care Res. 2019 Feb 21. doi: 10.1002/acr.23837.
Smoking is a significant risk factor for seropositive rheumatoid arthritis, and quitting may delay or even prevent the disease, a study has found.
In a paper published in Arthritis Care & Research, researchers report the analysis of data from 230,732 women – including 1,528 individuals with rheumatoid arthritis – participating in the Nurses’ Health Study (NHS) and NHS II.
They saw that current smokers had a significant 67% increased risk for seropositive rheumatoid arthritis (RA), compared with never smokers, while those who smoked 25 or more cigarettes per day had a 92% higher risk.
There was an increasing trend of association between pack-years of smoking and seropositive RA such that 35 pack-years of exposure was associated with a 2.3-fold higher risk for seropositive RA, compared with never smokers (P less than .0001).
Xinyi Liu of the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston, and her coauthors noted that the population attributable risk of RA from smoking was 14% and that smoking could contribute up to 35% of seropositive RA risk.
“Although the biologic mechanisms linking smoking with increased risk for developing RA are still not clear, components in cigarette smoke, such as nicotine, hydrocarbons, and carbon monoxide, are known to have aberrant effects on the immune system,” the authors wrote.
The good news was that sustained smoking cessation significantly reduced the risk of RA and seropositive RA, and those benefits increased with the amount of time since the individual stopped smoking.
Women who had quit smoking at least 30 years prior showed a 22% lower risk of all RA and a 37% lower risk of seropositive RA, compared with those who had quit within the previous 5 years. However, even 30 years after quitting, there was still a 30% higher risk of seropositive rheumatoid arthritis, compared with the risk among women who had never smoked.
“While smoking cessation may not decrease RA risk to the level of a never smoker, our findings provide evidence that a behavior change of smoking cessation may delay or even prevent the onset of seropositive RA,” the authors wrote. “These results could provide rationale for a smoking intervention trial among active smokers to prevent the formation of RA-related autoantibodies or to prevent the progression to RA among those at elevated risk for seropositive RA.”
Commenting on the difference in associations with seropositive and seronegative rheumatoid arthritis and smoking behavior, the authors wrote this suggested these two types of the disease may represent separate phenotypes with different risk factors.
The National Institutes of Health supported the study. No conflicts of interest were declared.
SOURCE: Liu X et al. Arthritis Care Res. 2019 Feb 21. doi: 10.1002/acr.23837.
FROM ARTHRITIS CARE & RESEARCH
Regimen shows promise as salvage for classical HL
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
FROM BONE MARROW TRANSPLANTATION











