User login
Evaluate liability risks in prescribing
Dear Dr. Mossman,
I prescribed topiramate for Mr. B, a patient with no history of kidney stones. Many months later he developed back pain. During the medical workup for a possible kidney stone, Mr. B and I revisited the risk of kidney stones with topiramate, which we had discussed at the beginning of therapy. Mr. B was adamantly opposed to stopping topiramate, even if he had a kidney stone. Testing revealed that Mr. B did not have a stone, but I wasn’t sure how to proceed. I worried that I might be found liable if Mr. B stayed on topiramate and did develop a kidney stone.—Submitted by Dr. A
When a patient develops a medical problem from a drug you prescribed, it is natural to feel responsible—after all, your treatment caused the adverse event. But did you commit malpractice? To answer this, let’s review the concept of “medical negligence.”
Malpractice law applies legal principles of negligence to professional conduct.1 The elements of a negligence case (Table 1) can be summarized as “breach of duty causing damages.” Therefore, when you wonder whether possible harm to a patient might be considered malpractice, ask yourself, “Did I breach my professional duty?”
Physicians have a duty to practice within their specialty’s standard of care, and if they do this, they should not be held liable even if their treatments cause adverse effects. Each jurisdiction defines the standard of care differently, but the general expectation is “that physicians acting within the ambit of their professional work will exercise the skill, knowledge, and care normally possessed and exercised by other members of their profession…in the relevant medical community.”1
It’s impossible to describe all the skills, knowledge, and care a psychiatrist normally employs when prescribing a drug, but elements of good practice include reasonable efforts to:
- make an appropriate diagnosis
- offer appropriate treatment
- monitor effects of treatment.
Further, treatment should occur only when a patient gives informed consent. Let’s examine each of these elements as they apply to Dr. A and Mr. B.
- Submit your malpractice-related questions to Dr. Mossman at douglas.mossman@dowdenhealth.com.
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Table 1
Elements of a successful negligence case
|
| Source: Reference 1 |
Appropriate assessment
Despite the availability of guidelines for psychiatric evaluation,2,3 it is tough to summarize everything psychiatrists do when assessing patients. But—focusing on Dr. A’s question—it is reasonable to ask: Did the psychiatric evaluation provide reasonably good evidence that Mr. B had a condition that topiramate might alleviate? Mr. B’s strong desire to keep taking the drug suggests that the answer is “yes.”
Dr. A also should consider potential interactions between topiramate and any other medications that Mr. B is taking. A prudent clinician must judge whether the potential benefit of topiramate for Mr. B outweighs the risk of adverse effects. If Mr. B actually had developed a kidney stone, Dr. A might seek a nephrologist’s advice about how to minimize the risk of recurrence.
Appropriate treatment
Topiramate is FDA-approved only for treating seizures and for prophylaxis against migraine headaches. However, FDA approval limits only how pharmaceutical companies can promote a medication.4 Physicians may prescribe drugs for unapproved “off-label” uses, and doing so is accepted medical practice. Peer-reviewed publications support using topiramate to treat agitation,5 alcohol dependence,6 binge-eating disorder,7 and other conditions that psychiatrists often manage. A tendency to promote weight loss has made topiramate an attractive add-on medication for patients whose weight problems are causing other health difficulties.8
Assuming that Mr. B is taking topiramate for an off-label purpose, an appropriate question to ask is, “Does professional literature support use of topiramate in Mr. B’s circumstances?” Also, given everything known about Mr. B up to this point, is topiramate a good treatment choice?
Appropriate monitoring
As every clinician knows, medications can cause problems. Monitoring topiramate therapy involves periodic lab testing and assessment of effectiveness. Dr. A should feel reasonably sure that Mr. B—assisted by a family member or close friend, if necessary—can and will cooperate with monitoring requirements. Dr. A also should verify that Mr. B can grasp and follow instructions designed to avert complications—such as ample hydration to reduce risk of nephrolithiasis—and will promptly address problems if they occur.
Informed consent
Informed consent is especially important when a patient receives a treatment that has a known risk. Although the Physician’s Desk Reference does not list previous kidney stones as a contraindication to topiramate therapy, it urges caution under these circumstances.4 Therefore, if Dr. A wishes to prescribe topiramate for a patient with a history of kidney stone, the patient should meaningfully collaborate in the treatment decision.
Informed consent for treatment requires that patients not feel coerced by the doctor or setting and have the mental capacity or competence to give consent. Under the conceptualization developed by Appelbaum and Grisso,9 competent patients can:
- express a consistent choice
- understand medical information provided to them
- appreciate how this information applies to them and their condition
- reason logically about treatment.
What information should patients receive before giving consent? The legal standard varies, but in most U.S. jurisdictions, patients “are entitled to material information about the nature of any proposed medical procedure. For example, patients are entitled to information about the risks of the procedure, its necessity, and alternate procedures that might be preferable.”1 Topiramate’s manufacturer instructs physicians to question and warn patients about the risk of kidney stones—which Dr. A did in Mr. B’s case. When you prescribe a drug off-label, you may want to tell patients this, but explain why the drug is appropriate nonetheless.
Table 2
Evaluating a patient’s capacity to consent to treatment
| Is this patient able to? | Questions to ask |
|---|---|
| Express a clear treatment preference | What treatment have you chosen? |
| Understand basic information communicated by caregivers | Can you tell me in your own words about your condition and the treatment options I have told you about? |
| Appreciate his or her medical condition and how information about treatment applies | What do you think is wrong with your health now? Do you think you need some kind of treatment? What do you think treatment will do for you? |
| Reason logically when choosing treatment options | Why did you choose this treatment? Why is it better than your other treatment options? |
| Source: Adapted and reprinted with permission from Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40 | |
1. Dobbs DB. The law of torts. St. Paul, MN: West Group; 2000:269.
2. King RA. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
3. American Psychiatric Association. Practice guideline for psychiatric evaluation of adults. Am J Psychiatry 1995;152(11 suppl):63-80.
4. Physicians’ Desk Reference. 62 ed. Montvale, NJ: Thomson Healthcare Inc.; 2007.
5. Guay DR. Newer antiepileptic drugs in the management of agitation/aggression in patients with dementia or developmental disability. Consult Pharm 2007;22:1004-34.
6. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-51.
7. McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry 2003;160:255-61.
8. Kirov G, Tredget J. Add-on topiramate reduces weight in overweight patients with affective disorders: a clinical case series. BMC Psychiatry 2005;5(1):19.-
9. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med 1988;319:1635-8.
10. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40.
Dear Dr. Mossman,
I prescribed topiramate for Mr. B, a patient with no history of kidney stones. Many months later he developed back pain. During the medical workup for a possible kidney stone, Mr. B and I revisited the risk of kidney stones with topiramate, which we had discussed at the beginning of therapy. Mr. B was adamantly opposed to stopping topiramate, even if he had a kidney stone. Testing revealed that Mr. B did not have a stone, but I wasn’t sure how to proceed. I worried that I might be found liable if Mr. B stayed on topiramate and did develop a kidney stone.—Submitted by Dr. A
When a patient develops a medical problem from a drug you prescribed, it is natural to feel responsible—after all, your treatment caused the adverse event. But did you commit malpractice? To answer this, let’s review the concept of “medical negligence.”
Malpractice law applies legal principles of negligence to professional conduct.1 The elements of a negligence case (Table 1) can be summarized as “breach of duty causing damages.” Therefore, when you wonder whether possible harm to a patient might be considered malpractice, ask yourself, “Did I breach my professional duty?”
Physicians have a duty to practice within their specialty’s standard of care, and if they do this, they should not be held liable even if their treatments cause adverse effects. Each jurisdiction defines the standard of care differently, but the general expectation is “that physicians acting within the ambit of their professional work will exercise the skill, knowledge, and care normally possessed and exercised by other members of their profession…in the relevant medical community.”1
It’s impossible to describe all the skills, knowledge, and care a psychiatrist normally employs when prescribing a drug, but elements of good practice include reasonable efforts to:
- make an appropriate diagnosis
- offer appropriate treatment
- monitor effects of treatment.
Further, treatment should occur only when a patient gives informed consent. Let’s examine each of these elements as they apply to Dr. A and Mr. B.
- Submit your malpractice-related questions to Dr. Mossman at douglas.mossman@dowdenhealth.com.
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Table 1
Elements of a successful negligence case
|
| Source: Reference 1 |
Appropriate assessment
Despite the availability of guidelines for psychiatric evaluation,2,3 it is tough to summarize everything psychiatrists do when assessing patients. But—focusing on Dr. A’s question—it is reasonable to ask: Did the psychiatric evaluation provide reasonably good evidence that Mr. B had a condition that topiramate might alleviate? Mr. B’s strong desire to keep taking the drug suggests that the answer is “yes.”
Dr. A also should consider potential interactions between topiramate and any other medications that Mr. B is taking. A prudent clinician must judge whether the potential benefit of topiramate for Mr. B outweighs the risk of adverse effects. If Mr. B actually had developed a kidney stone, Dr. A might seek a nephrologist’s advice about how to minimize the risk of recurrence.
Appropriate treatment
Topiramate is FDA-approved only for treating seizures and for prophylaxis against migraine headaches. However, FDA approval limits only how pharmaceutical companies can promote a medication.4 Physicians may prescribe drugs for unapproved “off-label” uses, and doing so is accepted medical practice. Peer-reviewed publications support using topiramate to treat agitation,5 alcohol dependence,6 binge-eating disorder,7 and other conditions that psychiatrists often manage. A tendency to promote weight loss has made topiramate an attractive add-on medication for patients whose weight problems are causing other health difficulties.8
Assuming that Mr. B is taking topiramate for an off-label purpose, an appropriate question to ask is, “Does professional literature support use of topiramate in Mr. B’s circumstances?” Also, given everything known about Mr. B up to this point, is topiramate a good treatment choice?
Appropriate monitoring
As every clinician knows, medications can cause problems. Monitoring topiramate therapy involves periodic lab testing and assessment of effectiveness. Dr. A should feel reasonably sure that Mr. B—assisted by a family member or close friend, if necessary—can and will cooperate with monitoring requirements. Dr. A also should verify that Mr. B can grasp and follow instructions designed to avert complications—such as ample hydration to reduce risk of nephrolithiasis—and will promptly address problems if they occur.
Informed consent
Informed consent is especially important when a patient receives a treatment that has a known risk. Although the Physician’s Desk Reference does not list previous kidney stones as a contraindication to topiramate therapy, it urges caution under these circumstances.4 Therefore, if Dr. A wishes to prescribe topiramate for a patient with a history of kidney stone, the patient should meaningfully collaborate in the treatment decision.
Informed consent for treatment requires that patients not feel coerced by the doctor or setting and have the mental capacity or competence to give consent. Under the conceptualization developed by Appelbaum and Grisso,9 competent patients can:
- express a consistent choice
- understand medical information provided to them
- appreciate how this information applies to them and their condition
- reason logically about treatment.
What information should patients receive before giving consent? The legal standard varies, but in most U.S. jurisdictions, patients “are entitled to material information about the nature of any proposed medical procedure. For example, patients are entitled to information about the risks of the procedure, its necessity, and alternate procedures that might be preferable.”1 Topiramate’s manufacturer instructs physicians to question and warn patients about the risk of kidney stones—which Dr. A did in Mr. B’s case. When you prescribe a drug off-label, you may want to tell patients this, but explain why the drug is appropriate nonetheless.
Table 2
Evaluating a patient’s capacity to consent to treatment
| Is this patient able to? | Questions to ask |
|---|---|
| Express a clear treatment preference | What treatment have you chosen? |
| Understand basic information communicated by caregivers | Can you tell me in your own words about your condition and the treatment options I have told you about? |
| Appreciate his or her medical condition and how information about treatment applies | What do you think is wrong with your health now? Do you think you need some kind of treatment? What do you think treatment will do for you? |
| Reason logically when choosing treatment options | Why did you choose this treatment? Why is it better than your other treatment options? |
| Source: Adapted and reprinted with permission from Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40 | |
Dear Dr. Mossman,
I prescribed topiramate for Mr. B, a patient with no history of kidney stones. Many months later he developed back pain. During the medical workup for a possible kidney stone, Mr. B and I revisited the risk of kidney stones with topiramate, which we had discussed at the beginning of therapy. Mr. B was adamantly opposed to stopping topiramate, even if he had a kidney stone. Testing revealed that Mr. B did not have a stone, but I wasn’t sure how to proceed. I worried that I might be found liable if Mr. B stayed on topiramate and did develop a kidney stone.—Submitted by Dr. A
When a patient develops a medical problem from a drug you prescribed, it is natural to feel responsible—after all, your treatment caused the adverse event. But did you commit malpractice? To answer this, let’s review the concept of “medical negligence.”
Malpractice law applies legal principles of negligence to professional conduct.1 The elements of a negligence case (Table 1) can be summarized as “breach of duty causing damages.” Therefore, when you wonder whether possible harm to a patient might be considered malpractice, ask yourself, “Did I breach my professional duty?”
Physicians have a duty to practice within their specialty’s standard of care, and if they do this, they should not be held liable even if their treatments cause adverse effects. Each jurisdiction defines the standard of care differently, but the general expectation is “that physicians acting within the ambit of their professional work will exercise the skill, knowledge, and care normally possessed and exercised by other members of their profession…in the relevant medical community.”1
It’s impossible to describe all the skills, knowledge, and care a psychiatrist normally employs when prescribing a drug, but elements of good practice include reasonable efforts to:
- make an appropriate diagnosis
- offer appropriate treatment
- monitor effects of treatment.
Further, treatment should occur only when a patient gives informed consent. Let’s examine each of these elements as they apply to Dr. A and Mr. B.
- Submit your malpractice-related questions to Dr. Mossman at douglas.mossman@dowdenhealth.com.
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Table 1
Elements of a successful negligence case
|
| Source: Reference 1 |
Appropriate assessment
Despite the availability of guidelines for psychiatric evaluation,2,3 it is tough to summarize everything psychiatrists do when assessing patients. But—focusing on Dr. A’s question—it is reasonable to ask: Did the psychiatric evaluation provide reasonably good evidence that Mr. B had a condition that topiramate might alleviate? Mr. B’s strong desire to keep taking the drug suggests that the answer is “yes.”
Dr. A also should consider potential interactions between topiramate and any other medications that Mr. B is taking. A prudent clinician must judge whether the potential benefit of topiramate for Mr. B outweighs the risk of adverse effects. If Mr. B actually had developed a kidney stone, Dr. A might seek a nephrologist’s advice about how to minimize the risk of recurrence.
Appropriate treatment
Topiramate is FDA-approved only for treating seizures and for prophylaxis against migraine headaches. However, FDA approval limits only how pharmaceutical companies can promote a medication.4 Physicians may prescribe drugs for unapproved “off-label” uses, and doing so is accepted medical practice. Peer-reviewed publications support using topiramate to treat agitation,5 alcohol dependence,6 binge-eating disorder,7 and other conditions that psychiatrists often manage. A tendency to promote weight loss has made topiramate an attractive add-on medication for patients whose weight problems are causing other health difficulties.8
Assuming that Mr. B is taking topiramate for an off-label purpose, an appropriate question to ask is, “Does professional literature support use of topiramate in Mr. B’s circumstances?” Also, given everything known about Mr. B up to this point, is topiramate a good treatment choice?
Appropriate monitoring
As every clinician knows, medications can cause problems. Monitoring topiramate therapy involves periodic lab testing and assessment of effectiveness. Dr. A should feel reasonably sure that Mr. B—assisted by a family member or close friend, if necessary—can and will cooperate with monitoring requirements. Dr. A also should verify that Mr. B can grasp and follow instructions designed to avert complications—such as ample hydration to reduce risk of nephrolithiasis—and will promptly address problems if they occur.
Informed consent
Informed consent is especially important when a patient receives a treatment that has a known risk. Although the Physician’s Desk Reference does not list previous kidney stones as a contraindication to topiramate therapy, it urges caution under these circumstances.4 Therefore, if Dr. A wishes to prescribe topiramate for a patient with a history of kidney stone, the patient should meaningfully collaborate in the treatment decision.
Informed consent for treatment requires that patients not feel coerced by the doctor or setting and have the mental capacity or competence to give consent. Under the conceptualization developed by Appelbaum and Grisso,9 competent patients can:
- express a consistent choice
- understand medical information provided to them
- appreciate how this information applies to them and their condition
- reason logically about treatment.
What information should patients receive before giving consent? The legal standard varies, but in most U.S. jurisdictions, patients “are entitled to material information about the nature of any proposed medical procedure. For example, patients are entitled to information about the risks of the procedure, its necessity, and alternate procedures that might be preferable.”1 Topiramate’s manufacturer instructs physicians to question and warn patients about the risk of kidney stones—which Dr. A did in Mr. B’s case. When you prescribe a drug off-label, you may want to tell patients this, but explain why the drug is appropriate nonetheless.
Table 2
Evaluating a patient’s capacity to consent to treatment
| Is this patient able to? | Questions to ask |
|---|---|
| Express a clear treatment preference | What treatment have you chosen? |
| Understand basic information communicated by caregivers | Can you tell me in your own words about your condition and the treatment options I have told you about? |
| Appreciate his or her medical condition and how information about treatment applies | What do you think is wrong with your health now? Do you think you need some kind of treatment? What do you think treatment will do for you? |
| Reason logically when choosing treatment options | Why did you choose this treatment? Why is it better than your other treatment options? |
| Source: Adapted and reprinted with permission from Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40 | |
1. Dobbs DB. The law of torts. St. Paul, MN: West Group; 2000:269.
2. King RA. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
3. American Psychiatric Association. Practice guideline for psychiatric evaluation of adults. Am J Psychiatry 1995;152(11 suppl):63-80.
4. Physicians’ Desk Reference. 62 ed. Montvale, NJ: Thomson Healthcare Inc.; 2007.
5. Guay DR. Newer antiepileptic drugs in the management of agitation/aggression in patients with dementia or developmental disability. Consult Pharm 2007;22:1004-34.
6. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-51.
7. McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry 2003;160:255-61.
8. Kirov G, Tredget J. Add-on topiramate reduces weight in overweight patients with affective disorders: a clinical case series. BMC Psychiatry 2005;5(1):19.-
9. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med 1988;319:1635-8.
10. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40.
1. Dobbs DB. The law of torts. St. Paul, MN: West Group; 2000:269.
2. King RA. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
3. American Psychiatric Association. Practice guideline for psychiatric evaluation of adults. Am J Psychiatry 1995;152(11 suppl):63-80.
4. Physicians’ Desk Reference. 62 ed. Montvale, NJ: Thomson Healthcare Inc.; 2007.
5. Guay DR. Newer antiepileptic drugs in the management of agitation/aggression in patients with dementia or developmental disability. Consult Pharm 2007;22:1004-34.
6. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-51.
7. McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry 2003;160:255-61.
8. Kirov G, Tredget J. Add-on topiramate reduces weight in overweight patients with affective disorders: a clinical case series. BMC Psychiatry 2005;5(1):19.-
9. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med 1988;319:1635-8.
10. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med 2007;357:1834-40.
Heparin contaminant identified
The US Food and Drug Administration (FDA) has identified the structure and source of the contaminant found in lots of heparin.
The contaminant, which has been linked to severe allergic reactions and deaths, was found in crude lots of heparin at a Chinese processing plant. The substance has been identified as over-sulfated chondroitin sulfate.
Researchers initially had difficulty identifying the contaminant because it is so similar to heparin. Over-sulfated chondroitin sulfate has approximately the same molecular weight as heparin, and both materials belong to the class of molecules known as glucosaminoglycans (GAGs).
It is still unknown whether the over-sulfated chondroitin sulfate was a byproduct of the heparin production process or if it was intentionally added to the active pharmaceutical ingredient.
After learning about the source of the over-sulfated chondroitin sulfate, the FDA issued a border alert that requires all finished heparin, as well as heparin source material, to be tested before it is allowed into the US. Five heparin manufacturers, companies that supply most of the heparin used in this country, have agreed to conduct the tests.
Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said the agency would test heparin products made by companies that cannot conduct the testing themselves. Any product that is not tested or fails the tests will be destroyed.
Scientific Protein Laboratories is the company that supplied crude heparin from the Changzhou plant in China to the biopharmaceutical company Baxter. Scientific Protein Laboratories has said it is cooperating with the FDA, and the Changzhou plant is not currently producing heparin.
In addition to the new testing instituted at the US borders, the FDA said heparin testing is now being conducted worldwide. Germany and Japan are among the countries that have started testing.
Germany recalled heparin last week after a cluster of about 100 serious allergic reactions, including hypotension and anaphylaxis. Japan has also recalled heparin but has not reported any adverse events linked to heparin injections.
Both Scientific Protein Laboratories and Baxter have conducted massive voluntary recalls of heparin products. Since Baxter recalled all of its heparin vials, there have been no additional deaths.
Last week, the FDA received 785 reports of adverse events associated with heparin. Those reports included 46 deaths, but Dr Woodcock said only 19 were related to the allergic profile associated with the Baxter heparin.
Baxter has said it cannot confirm that heparin has caused any fatalities as a result of an allergic reaction. The company said there are 4 cases in which patients received Baxter heparin and suffered an allergic-type reaction to the drug.
Baxter also said there is not yet enough medical data available to draw a firm conclusion that the reaction caused death. In each of these cases, the patient had multiple underlying complex medical conditions. Three of the 4 patients had undergone, or were in the process of undergoing, invasive cardiac surgery.
The heparin saga began January 17 of this year, when Baxter recalled the first batch of heparin after receiving reports of the allergic reactions. Recalls of the drug have continued since that time.
The FDA released the news of the contaminant’s source March 14 and the discovery of its structure March 19. ![]()
The US Food and Drug Administration (FDA) has identified the structure and source of the contaminant found in lots of heparin.
The contaminant, which has been linked to severe allergic reactions and deaths, was found in crude lots of heparin at a Chinese processing plant. The substance has been identified as over-sulfated chondroitin sulfate.
Researchers initially had difficulty identifying the contaminant because it is so similar to heparin. Over-sulfated chondroitin sulfate has approximately the same molecular weight as heparin, and both materials belong to the class of molecules known as glucosaminoglycans (GAGs).
It is still unknown whether the over-sulfated chondroitin sulfate was a byproduct of the heparin production process or if it was intentionally added to the active pharmaceutical ingredient.
After learning about the source of the over-sulfated chondroitin sulfate, the FDA issued a border alert that requires all finished heparin, as well as heparin source material, to be tested before it is allowed into the US. Five heparin manufacturers, companies that supply most of the heparin used in this country, have agreed to conduct the tests.
Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said the agency would test heparin products made by companies that cannot conduct the testing themselves. Any product that is not tested or fails the tests will be destroyed.
Scientific Protein Laboratories is the company that supplied crude heparin from the Changzhou plant in China to the biopharmaceutical company Baxter. Scientific Protein Laboratories has said it is cooperating with the FDA, and the Changzhou plant is not currently producing heparin.
In addition to the new testing instituted at the US borders, the FDA said heparin testing is now being conducted worldwide. Germany and Japan are among the countries that have started testing.
Germany recalled heparin last week after a cluster of about 100 serious allergic reactions, including hypotension and anaphylaxis. Japan has also recalled heparin but has not reported any adverse events linked to heparin injections.
Both Scientific Protein Laboratories and Baxter have conducted massive voluntary recalls of heparin products. Since Baxter recalled all of its heparin vials, there have been no additional deaths.
Last week, the FDA received 785 reports of adverse events associated with heparin. Those reports included 46 deaths, but Dr Woodcock said only 19 were related to the allergic profile associated with the Baxter heparin.
Baxter has said it cannot confirm that heparin has caused any fatalities as a result of an allergic reaction. The company said there are 4 cases in which patients received Baxter heparin and suffered an allergic-type reaction to the drug.
Baxter also said there is not yet enough medical data available to draw a firm conclusion that the reaction caused death. In each of these cases, the patient had multiple underlying complex medical conditions. Three of the 4 patients had undergone, or were in the process of undergoing, invasive cardiac surgery.
The heparin saga began January 17 of this year, when Baxter recalled the first batch of heparin after receiving reports of the allergic reactions. Recalls of the drug have continued since that time.
The FDA released the news of the contaminant’s source March 14 and the discovery of its structure March 19. ![]()
The US Food and Drug Administration (FDA) has identified the structure and source of the contaminant found in lots of heparin.
The contaminant, which has been linked to severe allergic reactions and deaths, was found in crude lots of heparin at a Chinese processing plant. The substance has been identified as over-sulfated chondroitin sulfate.
Researchers initially had difficulty identifying the contaminant because it is so similar to heparin. Over-sulfated chondroitin sulfate has approximately the same molecular weight as heparin, and both materials belong to the class of molecules known as glucosaminoglycans (GAGs).
It is still unknown whether the over-sulfated chondroitin sulfate was a byproduct of the heparin production process or if it was intentionally added to the active pharmaceutical ingredient.
After learning about the source of the over-sulfated chondroitin sulfate, the FDA issued a border alert that requires all finished heparin, as well as heparin source material, to be tested before it is allowed into the US. Five heparin manufacturers, companies that supply most of the heparin used in this country, have agreed to conduct the tests.
Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said the agency would test heparin products made by companies that cannot conduct the testing themselves. Any product that is not tested or fails the tests will be destroyed.
Scientific Protein Laboratories is the company that supplied crude heparin from the Changzhou plant in China to the biopharmaceutical company Baxter. Scientific Protein Laboratories has said it is cooperating with the FDA, and the Changzhou plant is not currently producing heparin.
In addition to the new testing instituted at the US borders, the FDA said heparin testing is now being conducted worldwide. Germany and Japan are among the countries that have started testing.
Germany recalled heparin last week after a cluster of about 100 serious allergic reactions, including hypotension and anaphylaxis. Japan has also recalled heparin but has not reported any adverse events linked to heparin injections.
Both Scientific Protein Laboratories and Baxter have conducted massive voluntary recalls of heparin products. Since Baxter recalled all of its heparin vials, there have been no additional deaths.
Last week, the FDA received 785 reports of adverse events associated with heparin. Those reports included 46 deaths, but Dr Woodcock said only 19 were related to the allergic profile associated with the Baxter heparin.
Baxter has said it cannot confirm that heparin has caused any fatalities as a result of an allergic reaction. The company said there are 4 cases in which patients received Baxter heparin and suffered an allergic-type reaction to the drug.
Baxter also said there is not yet enough medical data available to draw a firm conclusion that the reaction caused death. In each of these cases, the patient had multiple underlying complex medical conditions. Three of the 4 patients had undergone, or were in the process of undergoing, invasive cardiac surgery.
The heparin saga began January 17 of this year, when Baxter recalled the first batch of heparin after receiving reports of the allergic reactions. Recalls of the drug have continued since that time.
The FDA released the news of the contaminant’s source March 14 and the discovery of its structure March 19. ![]()
Proceedings of the 2nd Heart-Brain Summit
Supplement Editor:
Marc S. Penn, MD, PhD
Contents*†
Introduction: Heart-brain medicine: Update 2007
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, (3) SciDHon
Depression in coronary artery disease: Does treatment help?
Peter A. Shapiro, MD
Case study in heart-brain interplay: A 53-year-old woman recovering from mitral valve repair
Thomas D. Callahan, IV, MD; Ubaid Khokhar, MD; Leo Pozuelo, MD; and James B. Young, MD
Emotional predictors and behavioral triggers of acute coronary syndrome
Karina W. Davidson, PhD
Impacts of depression and emotional distress on cardiac disease
Wei Jiang, MD
Inflammation as a link between brain injury and heart damage: The model of subarachnoid hemorrhage
Hazem Antar Mashaly, MD, and J. Javier Provencio, MD
Biofeedback: An overview in the context of heart-brain medicine
Michael G. McKee, PhD
Biofeedback therapy in cardiovascular disease: Rationale and research overview
Christine S. Moravec, PhD
Helping children and adults with hypnosis and biofeedback
Karen Olness, MD
Clinical hypnosis for reduction of atrial fibrillation after coronary artery bypass graft surgery
Roberto Novoa, MD, and Tracy Hammonds, BA
Depression and coronary heart disease: Association and implications for treatment
James A. Blumenthal, PhD
Cardiovascular autonomic dysfunction in patients with movement disorders
Benjamin L. Walter, MD
Deep brain stimulation: How does it work?
Jerrold L. Vitek, MD, PhD
Sudden unexpected death in epilepsy: Impact, mechanisms, and prevention
Lara Jehi, MD, and Imad M. Najm, MD
Evaluating brain function in patients with disorders of consciousness
Tristan Bekinschtein, PhD, and Facundo Manes, MD
Preconditioning paradigms and pathways in the brain
Karl B. Shpargel; Walid Jalabi, PhD; Yongming Jin; Alisher Dadabayev, MD; Marc S. Penn, MD, PhD,
and Bruce D. Trapp, PhD
Post-stroke exercise rehabilitation:What we know about retraining the motor system and how it may apply to retraining the heart
Andreas Luft, MD; Richard Macko, MD; Larry Forrester, PhD; Andrew Goldberg, MD; and Daniel F. Hanley, MD
Hippocampal volume change in the Alzheimer Disease Cholesterol-Lowering Treatment trial
D. Larry Sparks, PhD; Susan K. Lemieux, PhD; Marc W. Haut, PhD; Leslie C. Baxter, PhD; Sterling C. Johnson, PhD; Lisa M. Sparks, BS; Hemalatha Sampath, BSEE; Jean E. Lopez, RN; Marwan H. Sabbagh, MD; and Donald J. Connor, PhD
Heart-brain interactions in cardiac arrhythmias: Role of the autonomic nervous system
Douglas P. Zipes, MD
Insular Alzheimer disease pathology and the psychometric correlates of mortality
Donald R. Royall, MD
Poster abstracts
* These proceedings represent the large majority of presentations at the 2nd Heart-Brain Summit, but five Summit presentations were not able to be captured for publication here.
† Articles in these proceedings were either submitted as manuscripts by the Summit faculty or developed by the Cleveland Clinic Journal of Medicine staff from transcripts of audiotaped Summit presentations and then revised and approved by the Summit faculty.
Supplement Editor:
Marc S. Penn, MD, PhD
Contents*†
Introduction: Heart-brain medicine: Update 2007
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, (3) SciDHon
Depression in coronary artery disease: Does treatment help?
Peter A. Shapiro, MD
Case study in heart-brain interplay: A 53-year-old woman recovering from mitral valve repair
Thomas D. Callahan, IV, MD; Ubaid Khokhar, MD; Leo Pozuelo, MD; and James B. Young, MD
Emotional predictors and behavioral triggers of acute coronary syndrome
Karina W. Davidson, PhD
Impacts of depression and emotional distress on cardiac disease
Wei Jiang, MD
Inflammation as a link between brain injury and heart damage: The model of subarachnoid hemorrhage
Hazem Antar Mashaly, MD, and J. Javier Provencio, MD
Biofeedback: An overview in the context of heart-brain medicine
Michael G. McKee, PhD
Biofeedback therapy in cardiovascular disease: Rationale and research overview
Christine S. Moravec, PhD
Helping children and adults with hypnosis and biofeedback
Karen Olness, MD
Clinical hypnosis for reduction of atrial fibrillation after coronary artery bypass graft surgery
Roberto Novoa, MD, and Tracy Hammonds, BA
Depression and coronary heart disease: Association and implications for treatment
James A. Blumenthal, PhD
Cardiovascular autonomic dysfunction in patients with movement disorders
Benjamin L. Walter, MD
Deep brain stimulation: How does it work?
Jerrold L. Vitek, MD, PhD
Sudden unexpected death in epilepsy: Impact, mechanisms, and prevention
Lara Jehi, MD, and Imad M. Najm, MD
Evaluating brain function in patients with disorders of consciousness
Tristan Bekinschtein, PhD, and Facundo Manes, MD
Preconditioning paradigms and pathways in the brain
Karl B. Shpargel; Walid Jalabi, PhD; Yongming Jin; Alisher Dadabayev, MD; Marc S. Penn, MD, PhD,
and Bruce D. Trapp, PhD
Post-stroke exercise rehabilitation:What we know about retraining the motor system and how it may apply to retraining the heart
Andreas Luft, MD; Richard Macko, MD; Larry Forrester, PhD; Andrew Goldberg, MD; and Daniel F. Hanley, MD
Hippocampal volume change in the Alzheimer Disease Cholesterol-Lowering Treatment trial
D. Larry Sparks, PhD; Susan K. Lemieux, PhD; Marc W. Haut, PhD; Leslie C. Baxter, PhD; Sterling C. Johnson, PhD; Lisa M. Sparks, BS; Hemalatha Sampath, BSEE; Jean E. Lopez, RN; Marwan H. Sabbagh, MD; and Donald J. Connor, PhD
Heart-brain interactions in cardiac arrhythmias: Role of the autonomic nervous system
Douglas P. Zipes, MD
Insular Alzheimer disease pathology and the psychometric correlates of mortality
Donald R. Royall, MD
Poster abstracts
* These proceedings represent the large majority of presentations at the 2nd Heart-Brain Summit, but five Summit presentations were not able to be captured for publication here.
† Articles in these proceedings were either submitted as manuscripts by the Summit faculty or developed by the Cleveland Clinic Journal of Medicine staff from transcripts of audiotaped Summit presentations and then revised and approved by the Summit faculty.
Supplement Editor:
Marc S. Penn, MD, PhD
Contents*†
Introduction: Heart-brain medicine: Update 2007
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, (3) SciDHon
Depression in coronary artery disease: Does treatment help?
Peter A. Shapiro, MD
Case study in heart-brain interplay: A 53-year-old woman recovering from mitral valve repair
Thomas D. Callahan, IV, MD; Ubaid Khokhar, MD; Leo Pozuelo, MD; and James B. Young, MD
Emotional predictors and behavioral triggers of acute coronary syndrome
Karina W. Davidson, PhD
Impacts of depression and emotional distress on cardiac disease
Wei Jiang, MD
Inflammation as a link between brain injury and heart damage: The model of subarachnoid hemorrhage
Hazem Antar Mashaly, MD, and J. Javier Provencio, MD
Biofeedback: An overview in the context of heart-brain medicine
Michael G. McKee, PhD
Biofeedback therapy in cardiovascular disease: Rationale and research overview
Christine S. Moravec, PhD
Helping children and adults with hypnosis and biofeedback
Karen Olness, MD
Clinical hypnosis for reduction of atrial fibrillation after coronary artery bypass graft surgery
Roberto Novoa, MD, and Tracy Hammonds, BA
Depression and coronary heart disease: Association and implications for treatment
James A. Blumenthal, PhD
Cardiovascular autonomic dysfunction in patients with movement disorders
Benjamin L. Walter, MD
Deep brain stimulation: How does it work?
Jerrold L. Vitek, MD, PhD
Sudden unexpected death in epilepsy: Impact, mechanisms, and prevention
Lara Jehi, MD, and Imad M. Najm, MD
Evaluating brain function in patients with disorders of consciousness
Tristan Bekinschtein, PhD, and Facundo Manes, MD
Preconditioning paradigms and pathways in the brain
Karl B. Shpargel; Walid Jalabi, PhD; Yongming Jin; Alisher Dadabayev, MD; Marc S. Penn, MD, PhD,
and Bruce D. Trapp, PhD
Post-stroke exercise rehabilitation:What we know about retraining the motor system and how it may apply to retraining the heart
Andreas Luft, MD; Richard Macko, MD; Larry Forrester, PhD; Andrew Goldberg, MD; and Daniel F. Hanley, MD
Hippocampal volume change in the Alzheimer Disease Cholesterol-Lowering Treatment trial
D. Larry Sparks, PhD; Susan K. Lemieux, PhD; Marc W. Haut, PhD; Leslie C. Baxter, PhD; Sterling C. Johnson, PhD; Lisa M. Sparks, BS; Hemalatha Sampath, BSEE; Jean E. Lopez, RN; Marwan H. Sabbagh, MD; and Donald J. Connor, PhD
Heart-brain interactions in cardiac arrhythmias: Role of the autonomic nervous system
Douglas P. Zipes, MD
Insular Alzheimer disease pathology and the psychometric correlates of mortality
Donald R. Royall, MD
Poster abstracts
* These proceedings represent the large majority of presentations at the 2nd Heart-Brain Summit, but five Summit presentations were not able to be captured for publication here.
† Articles in these proceedings were either submitted as manuscripts by the Summit faculty or developed by the Cleveland Clinic Journal of Medicine staff from transcripts of audiotaped Summit presentations and then revised and approved by the Summit faculty.
Post-stroke exercise rehabilitation: What we know about retraining the motor system and how it may apply to retraining the heart
Ideally, rehabilitation following a stroke that leads to functional deficit will result in a rapid return to normal function. In the real world, however, a rapid improvement in function is rarely achieved. Between 80% and 90% of stroke survivors have a motor deficit, with impairments in walking being the most common motor deficits.1 Most stroke survivors have a diminished fitness reserve that is stable and resistant to routine rehabilitative interventions. Recent research has begun to assess the value of exercise and other modalities of training during this period of stability to improve function long after cessation of other therapeutic interventions. This article will review this research and provide insight into those issues in post-stroke rehabilitation that remain to be addressed and may affect heart and brain physiology.
STROKE REDUCES AEROBIC CAPACITY
At all ages, the fitness level of stroke survivors, as measured by maximum oxygen consumption, is reduced by approximately 50% below that of an age-matched normal population. In a study comparing peak oxygen consumption during treadmill walking between stroke survivors and age-matched sedentary controls, we found that the stroke participants had an approximately 50% lower level of peak fitness relative to the control subjects.2 During treadmill walking at self-selected speeds, the stroke volunteers used 75% of their functional capacity, compared with 27% for the age-matched healthy controls. Furthermore, compared with the controls, the stroke subjects demonstrated a poorer economy of gait that required greater oxygen consumption to sustain their self-selected walking speeds.
CLINICAL TRIALS OF POST-STROKE EXERCISE REHABILITATION
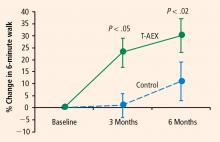
In light of the efficacy of treadmill exercise in cardiac rehabilitation, we are evaluating whether treadmill exercise can similarly improve fitness, endurance, and walking velocity in stroke survivors. We have completed 6 months of treadmill training in two separate cohorts that show highly consistent results in terms of improved walking abilities in hemiparetic stroke subjects.3,4 A third cohort is in progress to confirm these findings and examine the effects of intensity on the functional benefits5 and mechanisms6 underlying the effects of treadmill training.
Treadmill exercise results in functional benefits and improved glucose metabolism
The first cohort was a before-and-after comparison of stable stroke survivors who underwent a three-times-weekly treadmill exercise program for 6 months.3 Peak exercise capacity testing (VO2peak) revealed functional benefits with minimal cardiac and injury risk compared with baseline, demonstrating the feasibility and safety of treadmill exercise therapy in stroke-impaired adults.
Potential mechanisms for the benefits
These findings raise the question of whether these beneficial effects of treadmill exercise are attributable to muscle training effects, cardiopulmonary circulatory training effects, or perhaps neural mechanisms involving economy of gait movements and neuroplasticity of the motor system.
This question is being examined in our third cohort, now under investigation. This cohort will evaluate the effects of treadmill exercise on 32 chronically disabled stroke survivors in a single-center study design that is randomizing 64 subjects to 6 months of three-times-weekly treadmill training or conventional physiotherapy.6 Similar to our prior studies, subjects are randomized at least 6 months after their index stroke; this lengthy interval is deliberate because subjects are considered to be in a “plateau” phase of recovery, as they have previously completed rehabilitative therapy.
Activation will be measured in five prespecified “regions of interest”: the precentral gyrus, the postcentral gyrus, the supplementary motor area, the midbrain, and the cerebellum (anterior/posterior lobes). Difference activation maps of post-training minus pretraining fMRIs of paretic knee movement across all patients undergoing treadmill therapy will then be analyzed. The control group, which will receive dose-matched stretching activity from physical therapy, can be contrasted by comparing the patterns of pre/post differences in each region. This will allow for assessment of increased regional activation in the brain that should be specific to the treadmill training intervention. Furthermore, if a specifically localized regional activation difference is found, then individual fMRI and VO2 training responses (VO2peak, increase in walking speeds) can be correlated to further assess the relationship between regional activation and magnitude of functional response to the treadmill intervention.
DISCUSSION AND CONCLUSIONS
Central control of walking
Control of gait in animals is mediated by the cortex, brainstem/cerebellum,9,10 and spinal cord—the so-called cervical gait and lumbar gait pattern-generating areas of the spinal cord. In humans, cortical and spinal gait pattern areas are thought to be major regulatory centers of ambulation. Whether the cortical areas influence ambulatory recovery mediated by exercise training or whether the recruitment of spinal gait areas is needed to improve motor control after stroke is not known in humans. We will test the hypothesis that the recruitment of cortical and/or subcortical areas is relevant to some or all of the exercise-induced neuroplasticity response to treadmill rehabilitation. If a consistent pattern of brain regional activation is associated with an improvement in walking ability, this finding will suggest potential brain targets for neurally directed rehabilitation interventions. If brain targets for rehabilitation produce viable therapeutic improvement in walking and cardiocirculatory performance (such as VO2), this will be further evidence of heart-brain interactions.
Future research directions
Studies to date demonstrate that long-term treadmill exercise affects both the brain and cardiac physiology. This has holistic implications for the function of the whole person as well. Yet several pressing issues continue to confront researchers in post-stroke rehabilitation. One is the optimal therapeutic target and the intensity of the rehabilitative effort. Is this improvement solely a response of muscle and cardiac tissue to exercise, or is it possible that improved neuromotor control is a critical component to a major recovery of walking function? Furthermore, the most efficacious elements of rehabilitative therapy are not known. Should treadmill training be high- or low-intensity, and should it be accompanied by strength training, agility and flexibility activities, or other elements directed at reacquisition of finer degrees of gait-related motor training and neuropsychological input, as achieved by tai-chi or yoga? Another issue is the proper dose of rehabilitative therapy, which has barely been explored, although recent preliminary work suggests that the response is dose-dependent. Finally, predictors of response have not been established because the mechanisms of therapy and surrogate markers for early response are not well understood.
Our future research plans are to assess whether a better understanding of neural targets for rehabilitative treatment will be a fruitful avenue to improve recovery. Additionally, this plan will assess whether fMRI can serve as a surrogate marker of recovery by offering a noninvasive means to measure response to rehabilitation.
- Mayo NE, Wood-Dauphinee S, Ahmed S, et al. Disablement following stroke. Disabil Rehabil 1999; 21:258–268.
- Michael K, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Top Stroke Rehabil 2007; 14:5–12.
- Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil 2001; 82:879–884.
- Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke. A randomized, controlled trial. Stroke 2005; 36:2206–2211.
- Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP, Macko RF. Treadmill aerobic training improves glucose tolerance and indices of insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke 2007; 38:2752–2758.
- Luft AR, Macko R, Forrester L, Villagra F, Hanley D. Subcortical reorganization induced by aerobic locomotor training in chronic stroke survivors [abstract]. Poster presented at: Annual Meeting of the Society for Neuroscience; November 15, 2005; Washington, DC.
- Luft AR, Smith GV, Forrester L, et al. Comparing brain activation associated with isolated upper and lower limb movement across corresponding joints. Hum Brain Mapping 2002; 17:131–140.
- Luft AR, Forrester L, Macko RF, et al. Brain activation of lower extremity movement in chronically impaired stroke survivors. Neuroimage 2005; 26:184–194.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. I. The effects of bilateral pyramidal lesions. Brain 1968; 91:1–14.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. II. The effects of lesions of the descending brain-stem pathways. Brain 1968; 91:15–36.
Ideally, rehabilitation following a stroke that leads to functional deficit will result in a rapid return to normal function. In the real world, however, a rapid improvement in function is rarely achieved. Between 80% and 90% of stroke survivors have a motor deficit, with impairments in walking being the most common motor deficits.1 Most stroke survivors have a diminished fitness reserve that is stable and resistant to routine rehabilitative interventions. Recent research has begun to assess the value of exercise and other modalities of training during this period of stability to improve function long after cessation of other therapeutic interventions. This article will review this research and provide insight into those issues in post-stroke rehabilitation that remain to be addressed and may affect heart and brain physiology.
STROKE REDUCES AEROBIC CAPACITY
At all ages, the fitness level of stroke survivors, as measured by maximum oxygen consumption, is reduced by approximately 50% below that of an age-matched normal population. In a study comparing peak oxygen consumption during treadmill walking between stroke survivors and age-matched sedentary controls, we found that the stroke participants had an approximately 50% lower level of peak fitness relative to the control subjects.2 During treadmill walking at self-selected speeds, the stroke volunteers used 75% of their functional capacity, compared with 27% for the age-matched healthy controls. Furthermore, compared with the controls, the stroke subjects demonstrated a poorer economy of gait that required greater oxygen consumption to sustain their self-selected walking speeds.
CLINICAL TRIALS OF POST-STROKE EXERCISE REHABILITATION
In light of the efficacy of treadmill exercise in cardiac rehabilitation, we are evaluating whether treadmill exercise can similarly improve fitness, endurance, and walking velocity in stroke survivors. We have completed 6 months of treadmill training in two separate cohorts that show highly consistent results in terms of improved walking abilities in hemiparetic stroke subjects.3,4 A third cohort is in progress to confirm these findings and examine the effects of intensity on the functional benefits5 and mechanisms6 underlying the effects of treadmill training.
Treadmill exercise results in functional benefits and improved glucose metabolism
The first cohort was a before-and-after comparison of stable stroke survivors who underwent a three-times-weekly treadmill exercise program for 6 months.3 Peak exercise capacity testing (VO2peak) revealed functional benefits with minimal cardiac and injury risk compared with baseline, demonstrating the feasibility and safety of treadmill exercise therapy in stroke-impaired adults.
Potential mechanisms for the benefits
These findings raise the question of whether these beneficial effects of treadmill exercise are attributable to muscle training effects, cardiopulmonary circulatory training effects, or perhaps neural mechanisms involving economy of gait movements and neuroplasticity of the motor system.
This question is being examined in our third cohort, now under investigation. This cohort will evaluate the effects of treadmill exercise on 32 chronically disabled stroke survivors in a single-center study design that is randomizing 64 subjects to 6 months of three-times-weekly treadmill training or conventional physiotherapy.6 Similar to our prior studies, subjects are randomized at least 6 months after their index stroke; this lengthy interval is deliberate because subjects are considered to be in a “plateau” phase of recovery, as they have previously completed rehabilitative therapy.
Activation will be measured in five prespecified “regions of interest”: the precentral gyrus, the postcentral gyrus, the supplementary motor area, the midbrain, and the cerebellum (anterior/posterior lobes). Difference activation maps of post-training minus pretraining fMRIs of paretic knee movement across all patients undergoing treadmill therapy will then be analyzed. The control group, which will receive dose-matched stretching activity from physical therapy, can be contrasted by comparing the patterns of pre/post differences in each region. This will allow for assessment of increased regional activation in the brain that should be specific to the treadmill training intervention. Furthermore, if a specifically localized regional activation difference is found, then individual fMRI and VO2 training responses (VO2peak, increase in walking speeds) can be correlated to further assess the relationship between regional activation and magnitude of functional response to the treadmill intervention.
DISCUSSION AND CONCLUSIONS
Central control of walking
Control of gait in animals is mediated by the cortex, brainstem/cerebellum,9,10 and spinal cord—the so-called cervical gait and lumbar gait pattern-generating areas of the spinal cord. In humans, cortical and spinal gait pattern areas are thought to be major regulatory centers of ambulation. Whether the cortical areas influence ambulatory recovery mediated by exercise training or whether the recruitment of spinal gait areas is needed to improve motor control after stroke is not known in humans. We will test the hypothesis that the recruitment of cortical and/or subcortical areas is relevant to some or all of the exercise-induced neuroplasticity response to treadmill rehabilitation. If a consistent pattern of brain regional activation is associated with an improvement in walking ability, this finding will suggest potential brain targets for neurally directed rehabilitation interventions. If brain targets for rehabilitation produce viable therapeutic improvement in walking and cardiocirculatory performance (such as VO2), this will be further evidence of heart-brain interactions.
Future research directions
Studies to date demonstrate that long-term treadmill exercise affects both the brain and cardiac physiology. This has holistic implications for the function of the whole person as well. Yet several pressing issues continue to confront researchers in post-stroke rehabilitation. One is the optimal therapeutic target and the intensity of the rehabilitative effort. Is this improvement solely a response of muscle and cardiac tissue to exercise, or is it possible that improved neuromotor control is a critical component to a major recovery of walking function? Furthermore, the most efficacious elements of rehabilitative therapy are not known. Should treadmill training be high- or low-intensity, and should it be accompanied by strength training, agility and flexibility activities, or other elements directed at reacquisition of finer degrees of gait-related motor training and neuropsychological input, as achieved by tai-chi or yoga? Another issue is the proper dose of rehabilitative therapy, which has barely been explored, although recent preliminary work suggests that the response is dose-dependent. Finally, predictors of response have not been established because the mechanisms of therapy and surrogate markers for early response are not well understood.
Our future research plans are to assess whether a better understanding of neural targets for rehabilitative treatment will be a fruitful avenue to improve recovery. Additionally, this plan will assess whether fMRI can serve as a surrogate marker of recovery by offering a noninvasive means to measure response to rehabilitation.
Ideally, rehabilitation following a stroke that leads to functional deficit will result in a rapid return to normal function. In the real world, however, a rapid improvement in function is rarely achieved. Between 80% and 90% of stroke survivors have a motor deficit, with impairments in walking being the most common motor deficits.1 Most stroke survivors have a diminished fitness reserve that is stable and resistant to routine rehabilitative interventions. Recent research has begun to assess the value of exercise and other modalities of training during this period of stability to improve function long after cessation of other therapeutic interventions. This article will review this research and provide insight into those issues in post-stroke rehabilitation that remain to be addressed and may affect heart and brain physiology.
STROKE REDUCES AEROBIC CAPACITY
At all ages, the fitness level of stroke survivors, as measured by maximum oxygen consumption, is reduced by approximately 50% below that of an age-matched normal population. In a study comparing peak oxygen consumption during treadmill walking between stroke survivors and age-matched sedentary controls, we found that the stroke participants had an approximately 50% lower level of peak fitness relative to the control subjects.2 During treadmill walking at self-selected speeds, the stroke volunteers used 75% of their functional capacity, compared with 27% for the age-matched healthy controls. Furthermore, compared with the controls, the stroke subjects demonstrated a poorer economy of gait that required greater oxygen consumption to sustain their self-selected walking speeds.
CLINICAL TRIALS OF POST-STROKE EXERCISE REHABILITATION
In light of the efficacy of treadmill exercise in cardiac rehabilitation, we are evaluating whether treadmill exercise can similarly improve fitness, endurance, and walking velocity in stroke survivors. We have completed 6 months of treadmill training in two separate cohorts that show highly consistent results in terms of improved walking abilities in hemiparetic stroke subjects.3,4 A third cohort is in progress to confirm these findings and examine the effects of intensity on the functional benefits5 and mechanisms6 underlying the effects of treadmill training.
Treadmill exercise results in functional benefits and improved glucose metabolism
The first cohort was a before-and-after comparison of stable stroke survivors who underwent a three-times-weekly treadmill exercise program for 6 months.3 Peak exercise capacity testing (VO2peak) revealed functional benefits with minimal cardiac and injury risk compared with baseline, demonstrating the feasibility and safety of treadmill exercise therapy in stroke-impaired adults.
Potential mechanisms for the benefits
These findings raise the question of whether these beneficial effects of treadmill exercise are attributable to muscle training effects, cardiopulmonary circulatory training effects, or perhaps neural mechanisms involving economy of gait movements and neuroplasticity of the motor system.
This question is being examined in our third cohort, now under investigation. This cohort will evaluate the effects of treadmill exercise on 32 chronically disabled stroke survivors in a single-center study design that is randomizing 64 subjects to 6 months of three-times-weekly treadmill training or conventional physiotherapy.6 Similar to our prior studies, subjects are randomized at least 6 months after their index stroke; this lengthy interval is deliberate because subjects are considered to be in a “plateau” phase of recovery, as they have previously completed rehabilitative therapy.
Activation will be measured in five prespecified “regions of interest”: the precentral gyrus, the postcentral gyrus, the supplementary motor area, the midbrain, and the cerebellum (anterior/posterior lobes). Difference activation maps of post-training minus pretraining fMRIs of paretic knee movement across all patients undergoing treadmill therapy will then be analyzed. The control group, which will receive dose-matched stretching activity from physical therapy, can be contrasted by comparing the patterns of pre/post differences in each region. This will allow for assessment of increased regional activation in the brain that should be specific to the treadmill training intervention. Furthermore, if a specifically localized regional activation difference is found, then individual fMRI and VO2 training responses (VO2peak, increase in walking speeds) can be correlated to further assess the relationship between regional activation and magnitude of functional response to the treadmill intervention.
DISCUSSION AND CONCLUSIONS
Central control of walking
Control of gait in animals is mediated by the cortex, brainstem/cerebellum,9,10 and spinal cord—the so-called cervical gait and lumbar gait pattern-generating areas of the spinal cord. In humans, cortical and spinal gait pattern areas are thought to be major regulatory centers of ambulation. Whether the cortical areas influence ambulatory recovery mediated by exercise training or whether the recruitment of spinal gait areas is needed to improve motor control after stroke is not known in humans. We will test the hypothesis that the recruitment of cortical and/or subcortical areas is relevant to some or all of the exercise-induced neuroplasticity response to treadmill rehabilitation. If a consistent pattern of brain regional activation is associated with an improvement in walking ability, this finding will suggest potential brain targets for neurally directed rehabilitation interventions. If brain targets for rehabilitation produce viable therapeutic improvement in walking and cardiocirculatory performance (such as VO2), this will be further evidence of heart-brain interactions.
Future research directions
Studies to date demonstrate that long-term treadmill exercise affects both the brain and cardiac physiology. This has holistic implications for the function of the whole person as well. Yet several pressing issues continue to confront researchers in post-stroke rehabilitation. One is the optimal therapeutic target and the intensity of the rehabilitative effort. Is this improvement solely a response of muscle and cardiac tissue to exercise, or is it possible that improved neuromotor control is a critical component to a major recovery of walking function? Furthermore, the most efficacious elements of rehabilitative therapy are not known. Should treadmill training be high- or low-intensity, and should it be accompanied by strength training, agility and flexibility activities, or other elements directed at reacquisition of finer degrees of gait-related motor training and neuropsychological input, as achieved by tai-chi or yoga? Another issue is the proper dose of rehabilitative therapy, which has barely been explored, although recent preliminary work suggests that the response is dose-dependent. Finally, predictors of response have not been established because the mechanisms of therapy and surrogate markers for early response are not well understood.
Our future research plans are to assess whether a better understanding of neural targets for rehabilitative treatment will be a fruitful avenue to improve recovery. Additionally, this plan will assess whether fMRI can serve as a surrogate marker of recovery by offering a noninvasive means to measure response to rehabilitation.
- Mayo NE, Wood-Dauphinee S, Ahmed S, et al. Disablement following stroke. Disabil Rehabil 1999; 21:258–268.
- Michael K, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Top Stroke Rehabil 2007; 14:5–12.
- Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil 2001; 82:879–884.
- Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke. A randomized, controlled trial. Stroke 2005; 36:2206–2211.
- Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP, Macko RF. Treadmill aerobic training improves glucose tolerance and indices of insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke 2007; 38:2752–2758.
- Luft AR, Macko R, Forrester L, Villagra F, Hanley D. Subcortical reorganization induced by aerobic locomotor training in chronic stroke survivors [abstract]. Poster presented at: Annual Meeting of the Society for Neuroscience; November 15, 2005; Washington, DC.
- Luft AR, Smith GV, Forrester L, et al. Comparing brain activation associated with isolated upper and lower limb movement across corresponding joints. Hum Brain Mapping 2002; 17:131–140.
- Luft AR, Forrester L, Macko RF, et al. Brain activation of lower extremity movement in chronically impaired stroke survivors. Neuroimage 2005; 26:184–194.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. I. The effects of bilateral pyramidal lesions. Brain 1968; 91:1–14.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. II. The effects of lesions of the descending brain-stem pathways. Brain 1968; 91:15–36.
- Mayo NE, Wood-Dauphinee S, Ahmed S, et al. Disablement following stroke. Disabil Rehabil 1999; 21:258–268.
- Michael K, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Top Stroke Rehabil 2007; 14:5–12.
- Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil 2001; 82:879–884.
- Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke. A randomized, controlled trial. Stroke 2005; 36:2206–2211.
- Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP, Macko RF. Treadmill aerobic training improves glucose tolerance and indices of insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke 2007; 38:2752–2758.
- Luft AR, Macko R, Forrester L, Villagra F, Hanley D. Subcortical reorganization induced by aerobic locomotor training in chronic stroke survivors [abstract]. Poster presented at: Annual Meeting of the Society for Neuroscience; November 15, 2005; Washington, DC.
- Luft AR, Smith GV, Forrester L, et al. Comparing brain activation associated with isolated upper and lower limb movement across corresponding joints. Hum Brain Mapping 2002; 17:131–140.
- Luft AR, Forrester L, Macko RF, et al. Brain activation of lower extremity movement in chronically impaired stroke survivors. Neuroimage 2005; 26:184–194.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. I. The effects of bilateral pyramidal lesions. Brain 1968; 91:1–14.
- Lawrence DG, Kuypers HG. The functional organization of the motor system in the monkey. II. The effects of lesions of the descending brain-stem pathways. Brain 1968; 91:15–36.
Team Approach
Team Approach
Question: We work with a large orthopedic group. We would like to propose a more formal structure to this. We are interested in building business and partnerships. Do you know of any articles or references to support hospitalists doing this, or any sources to show the orthopedic group we can and would improve outcomes and their work life and workload?
Julie Lepzinski, director,
hospitalist medicine group,
Michigan
Dr. Hospitalist responds: I commend you and your hospitalist group for taking the initiative to develop a relationship with your orthopedics colleagues. Many hospitalist groups are exploring such relationships with not only orthopedists but also with other surgical and medical subspecialists.
As you mentioned, the opportunity exists to improve your group’s income and improve orthopedist work life. More importantly, there is a real opportunity to improve the medical care of patients admitted to the hospital primarily with orthopedic problems.
There are published data from an academic medical center on a hospitalist-orthopedics co-management model. Huddleston, et al., studied the effect of such a co-management model on the care of patients after elective hip and knee arthroplasty at the Mayo Clinic.1 They found that “the co-management medical hospitalist-orthopedic team model reduced minor postoperative complication rates with no statistically significant difference in length of stay or cost. The nurses and surgeons strongly preferred the co-management hospitalist model.”
This study would seem to support your notion that orthopedists may prefer the involvement of hospitalists in the care of their patients. Hospitalist involvement reduced minor complications (urinary tract infections, fever, electrolyte abnormalities). However, investigators did not find that hospitalist co-management reduced major postoperative complications (death, myocardial infarction, renal failure requiring hemodialysis) or intermediate ones (heart failure, pulmonary embolus, ileus, pneumonia).
Mayo Clinic hospitalists also studied the impact of a hospitalist-orthopedist co-management model of the care on elderly patients admitted to their hospital with hip fracture.2 Phy, et al., found that, “In elderly patients with hip fracture, a hospitalist model decreased time to surgery, time from surgery to dismissal and length of stay without adversely affecting inpatient deaths or 30-day readmission rates.” This study demonstrated that hospitalist co-management can decrease hospital length of stay in this population of patients.
We should recognize the obvious limitations of these studies. They were done at a single large academic institution with a largely Caucasian population at the turn of the century (2000-2001), early in the hospitalist movement. The hospitalist movement has matured, with approximately 20,000 hospitalists in the country. I hope we will soon see more robust data coming from multicenter trials that include a more diverse population of patients as well as a mix of community and academic institutions.
Start an HMG?
Question: We own a medical clinic in Arizona and are thinking of starting a hospitalist group as a separate business entity. Are you aware of any recommended reading or articles on how to start one, if it’s profitable, and in what shape or form? And most important--regarding the current trends and projections--I wonder if the need has changed, as most hospitals reduce their number of vendors.
Shawn Toloui, president and owner,
1st Care Medical Clinic,
Phoenix, Ariz.
Dr. Hospitalist responds: These are the kind of questions people have been asking since the term “hospitalist” was coined in 1996. Over the past decade, we have seen an explosion in the number of hospitalists in the country. Few folks in the 1990s thought there would be 20,000 hospitalists today.
If I understand you correctly, you are concerned that because many hospitals are reducing their numbers of vendors, this may have an adverse effect on the need for hospitalists. Hospitals will engage in business relationships with hospitalists as long as the hospitalists can bring solutions to problems and fulfill needs. To understand this better, let’s examine the reasons the numbers of hospitalists have grown over the past decade.
Costs: When Medicare started paying hospitals based on diagnosis-related groups (DRGs) in the early ’80s, this forced hospitals to “manage” patients’ length of stay. The DRG system pays a fixed fee regardless of the length of stay but allows for an adjusted higher payment based on a hospital’s case mix index (a measure of how “sick” patients are in a given hospital).
This reimbursement system encourages hospitals to take care of ill patients but also to “manage” their length of stay. It is difficult for doctors to manage any hospitalized patients from outpatient offices, let alone sick patients. Hospitals and payers found that hospitalists are able to manage sick patients and reduce costs, mostly by being available to admit, manage, and discharge patients in a timely manner. This increased throughput of patients also allows hospitals to put another patient in a bed sooner, bringing additional revenue.
Quality: By serendipity, the hospitalist movement coincided with the quality movement. Hospitalists have helped reduce variations in care by working locally to develop and implement clinical-care pathways. Hospitalists have also served as partners for hospitals to achieve compliance with payer quality mandates.
For example, in 2003, Medicare began requiring hospitals to report a handful of diagnosis-based quality measures it called the Core Measures. The number of measures continues to grow. In 2007, Medicare tied hospital reimbursement to performance on the Core Measures. I hear from hospital administrators that they find it easier to educate and work with a small group of hospitalists, rather than a large medical staff, to achieve optimal results on these measures.
Satisfaction: The exodus of primary care physicians (PCPs) from the hospital has fueled much of the growth in hospital medicine. PCPs have found it increasingly difficult to care for hospitalized patients while juggling the demands of a busy outpatient practice. In hospitalists, nurses have found a physician partner who is available physically to work with them in the care of acutely ill patients.
PCPs and nurses have been very satisfied with the hospitalist model of care. Although provider satisfaction is important, satisfaction in healthcare begins and ends with patients. Despite the discontinuity of care of meeting a new provider during hospitalization, patients have been satisfied with hospitalist care. Patients view hospitalists as providers available to provide for their acute needs while also communicating with the patients’ outpatient providers to understand their long-term needs.
I expect the number of hospitalists to grow over the next decade, albeit at a slower pace as most programs begin to fill their available positions. SHM believes the numbers of hospitalists will grow to 40,000.
There are a number of resources that can help you understand how to develop, manage, and grow a hospitalist program. I suggest you visit the “Practice Resources” section of the SHM Web site at www.hospitalmedicine.org. In particular, I recommend the “Best Practices in Managing a Hospital Medicine Program,” held twice a year. The spring program is held in conjunction with the SHM Annual Meeting in San Diego, April 3-5. The fall program is held in conjunction with the University of California, San Francisco’s “Management of the Hospitalized Patient” course in San Francisco. Also, the book Hospitalists: A Guide to Building and Sustaining a Successful Program by SHM Senior Vice President Joe Miller and SHM cofounders John Nelson, MD, and Winthrop F. Whitcomb, MD, is a must read for anybody looking to build a hospitalist program. TH
References
- Huddleston JM, Long KH, Naessens JM, Vanness DJ, Larson D, Trousdale R, Plevak M, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004 July 6;141(1):28-38.
- Phy MP, Vanness DJ, Melton JL, Hallong K, Schleck C, Larson DR, Huddleston PM. et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165:796-801.
Team Approach
Question: We work with a large orthopedic group. We would like to propose a more formal structure to this. We are interested in building business and partnerships. Do you know of any articles or references to support hospitalists doing this, or any sources to show the orthopedic group we can and would improve outcomes and their work life and workload?
Julie Lepzinski, director,
hospitalist medicine group,
Michigan
Dr. Hospitalist responds: I commend you and your hospitalist group for taking the initiative to develop a relationship with your orthopedics colleagues. Many hospitalist groups are exploring such relationships with not only orthopedists but also with other surgical and medical subspecialists.
As you mentioned, the opportunity exists to improve your group’s income and improve orthopedist work life. More importantly, there is a real opportunity to improve the medical care of patients admitted to the hospital primarily with orthopedic problems.
There are published data from an academic medical center on a hospitalist-orthopedics co-management model. Huddleston, et al., studied the effect of such a co-management model on the care of patients after elective hip and knee arthroplasty at the Mayo Clinic.1 They found that “the co-management medical hospitalist-orthopedic team model reduced minor postoperative complication rates with no statistically significant difference in length of stay or cost. The nurses and surgeons strongly preferred the co-management hospitalist model.”
This study would seem to support your notion that orthopedists may prefer the involvement of hospitalists in the care of their patients. Hospitalist involvement reduced minor complications (urinary tract infections, fever, electrolyte abnormalities). However, investigators did not find that hospitalist co-management reduced major postoperative complications (death, myocardial infarction, renal failure requiring hemodialysis) or intermediate ones (heart failure, pulmonary embolus, ileus, pneumonia).
Mayo Clinic hospitalists also studied the impact of a hospitalist-orthopedist co-management model of the care on elderly patients admitted to their hospital with hip fracture.2 Phy, et al., found that, “In elderly patients with hip fracture, a hospitalist model decreased time to surgery, time from surgery to dismissal and length of stay without adversely affecting inpatient deaths or 30-day readmission rates.” This study demonstrated that hospitalist co-management can decrease hospital length of stay in this population of patients.
We should recognize the obvious limitations of these studies. They were done at a single large academic institution with a largely Caucasian population at the turn of the century (2000-2001), early in the hospitalist movement. The hospitalist movement has matured, with approximately 20,000 hospitalists in the country. I hope we will soon see more robust data coming from multicenter trials that include a more diverse population of patients as well as a mix of community and academic institutions.
Start an HMG?
Question: We own a medical clinic in Arizona and are thinking of starting a hospitalist group as a separate business entity. Are you aware of any recommended reading or articles on how to start one, if it’s profitable, and in what shape or form? And most important--regarding the current trends and projections--I wonder if the need has changed, as most hospitals reduce their number of vendors.
Shawn Toloui, president and owner,
1st Care Medical Clinic,
Phoenix, Ariz.
Dr. Hospitalist responds: These are the kind of questions people have been asking since the term “hospitalist” was coined in 1996. Over the past decade, we have seen an explosion in the number of hospitalists in the country. Few folks in the 1990s thought there would be 20,000 hospitalists today.
If I understand you correctly, you are concerned that because many hospitals are reducing their numbers of vendors, this may have an adverse effect on the need for hospitalists. Hospitals will engage in business relationships with hospitalists as long as the hospitalists can bring solutions to problems and fulfill needs. To understand this better, let’s examine the reasons the numbers of hospitalists have grown over the past decade.
Costs: When Medicare started paying hospitals based on diagnosis-related groups (DRGs) in the early ’80s, this forced hospitals to “manage” patients’ length of stay. The DRG system pays a fixed fee regardless of the length of stay but allows for an adjusted higher payment based on a hospital’s case mix index (a measure of how “sick” patients are in a given hospital).
This reimbursement system encourages hospitals to take care of ill patients but also to “manage” their length of stay. It is difficult for doctors to manage any hospitalized patients from outpatient offices, let alone sick patients. Hospitals and payers found that hospitalists are able to manage sick patients and reduce costs, mostly by being available to admit, manage, and discharge patients in a timely manner. This increased throughput of patients also allows hospitals to put another patient in a bed sooner, bringing additional revenue.
Quality: By serendipity, the hospitalist movement coincided with the quality movement. Hospitalists have helped reduce variations in care by working locally to develop and implement clinical-care pathways. Hospitalists have also served as partners for hospitals to achieve compliance with payer quality mandates.
For example, in 2003, Medicare began requiring hospitals to report a handful of diagnosis-based quality measures it called the Core Measures. The number of measures continues to grow. In 2007, Medicare tied hospital reimbursement to performance on the Core Measures. I hear from hospital administrators that they find it easier to educate and work with a small group of hospitalists, rather than a large medical staff, to achieve optimal results on these measures.
Satisfaction: The exodus of primary care physicians (PCPs) from the hospital has fueled much of the growth in hospital medicine. PCPs have found it increasingly difficult to care for hospitalized patients while juggling the demands of a busy outpatient practice. In hospitalists, nurses have found a physician partner who is available physically to work with them in the care of acutely ill patients.
PCPs and nurses have been very satisfied with the hospitalist model of care. Although provider satisfaction is important, satisfaction in healthcare begins and ends with patients. Despite the discontinuity of care of meeting a new provider during hospitalization, patients have been satisfied with hospitalist care. Patients view hospitalists as providers available to provide for their acute needs while also communicating with the patients’ outpatient providers to understand their long-term needs.
I expect the number of hospitalists to grow over the next decade, albeit at a slower pace as most programs begin to fill their available positions. SHM believes the numbers of hospitalists will grow to 40,000.
There are a number of resources that can help you understand how to develop, manage, and grow a hospitalist program. I suggest you visit the “Practice Resources” section of the SHM Web site at www.hospitalmedicine.org. In particular, I recommend the “Best Practices in Managing a Hospital Medicine Program,” held twice a year. The spring program is held in conjunction with the SHM Annual Meeting in San Diego, April 3-5. The fall program is held in conjunction with the University of California, San Francisco’s “Management of the Hospitalized Patient” course in San Francisco. Also, the book Hospitalists: A Guide to Building and Sustaining a Successful Program by SHM Senior Vice President Joe Miller and SHM cofounders John Nelson, MD, and Winthrop F. Whitcomb, MD, is a must read for anybody looking to build a hospitalist program. TH
References
- Huddleston JM, Long KH, Naessens JM, Vanness DJ, Larson D, Trousdale R, Plevak M, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004 July 6;141(1):28-38.
- Phy MP, Vanness DJ, Melton JL, Hallong K, Schleck C, Larson DR, Huddleston PM. et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165:796-801.
Team Approach
Question: We work with a large orthopedic group. We would like to propose a more formal structure to this. We are interested in building business and partnerships. Do you know of any articles or references to support hospitalists doing this, or any sources to show the orthopedic group we can and would improve outcomes and their work life and workload?
Julie Lepzinski, director,
hospitalist medicine group,
Michigan
Dr. Hospitalist responds: I commend you and your hospitalist group for taking the initiative to develop a relationship with your orthopedics colleagues. Many hospitalist groups are exploring such relationships with not only orthopedists but also with other surgical and medical subspecialists.
As you mentioned, the opportunity exists to improve your group’s income and improve orthopedist work life. More importantly, there is a real opportunity to improve the medical care of patients admitted to the hospital primarily with orthopedic problems.
There are published data from an academic medical center on a hospitalist-orthopedics co-management model. Huddleston, et al., studied the effect of such a co-management model on the care of patients after elective hip and knee arthroplasty at the Mayo Clinic.1 They found that “the co-management medical hospitalist-orthopedic team model reduced minor postoperative complication rates with no statistically significant difference in length of stay or cost. The nurses and surgeons strongly preferred the co-management hospitalist model.”
This study would seem to support your notion that orthopedists may prefer the involvement of hospitalists in the care of their patients. Hospitalist involvement reduced minor complications (urinary tract infections, fever, electrolyte abnormalities). However, investigators did not find that hospitalist co-management reduced major postoperative complications (death, myocardial infarction, renal failure requiring hemodialysis) or intermediate ones (heart failure, pulmonary embolus, ileus, pneumonia).
Mayo Clinic hospitalists also studied the impact of a hospitalist-orthopedist co-management model of the care on elderly patients admitted to their hospital with hip fracture.2 Phy, et al., found that, “In elderly patients with hip fracture, a hospitalist model decreased time to surgery, time from surgery to dismissal and length of stay without adversely affecting inpatient deaths or 30-day readmission rates.” This study demonstrated that hospitalist co-management can decrease hospital length of stay in this population of patients.
We should recognize the obvious limitations of these studies. They were done at a single large academic institution with a largely Caucasian population at the turn of the century (2000-2001), early in the hospitalist movement. The hospitalist movement has matured, with approximately 20,000 hospitalists in the country. I hope we will soon see more robust data coming from multicenter trials that include a more diverse population of patients as well as a mix of community and academic institutions.
Start an HMG?
Question: We own a medical clinic in Arizona and are thinking of starting a hospitalist group as a separate business entity. Are you aware of any recommended reading or articles on how to start one, if it’s profitable, and in what shape or form? And most important--regarding the current trends and projections--I wonder if the need has changed, as most hospitals reduce their number of vendors.
Shawn Toloui, president and owner,
1st Care Medical Clinic,
Phoenix, Ariz.
Dr. Hospitalist responds: These are the kind of questions people have been asking since the term “hospitalist” was coined in 1996. Over the past decade, we have seen an explosion in the number of hospitalists in the country. Few folks in the 1990s thought there would be 20,000 hospitalists today.
If I understand you correctly, you are concerned that because many hospitals are reducing their numbers of vendors, this may have an adverse effect on the need for hospitalists. Hospitals will engage in business relationships with hospitalists as long as the hospitalists can bring solutions to problems and fulfill needs. To understand this better, let’s examine the reasons the numbers of hospitalists have grown over the past decade.
Costs: When Medicare started paying hospitals based on diagnosis-related groups (DRGs) in the early ’80s, this forced hospitals to “manage” patients’ length of stay. The DRG system pays a fixed fee regardless of the length of stay but allows for an adjusted higher payment based on a hospital’s case mix index (a measure of how “sick” patients are in a given hospital).
This reimbursement system encourages hospitals to take care of ill patients but also to “manage” their length of stay. It is difficult for doctors to manage any hospitalized patients from outpatient offices, let alone sick patients. Hospitals and payers found that hospitalists are able to manage sick patients and reduce costs, mostly by being available to admit, manage, and discharge patients in a timely manner. This increased throughput of patients also allows hospitals to put another patient in a bed sooner, bringing additional revenue.
Quality: By serendipity, the hospitalist movement coincided with the quality movement. Hospitalists have helped reduce variations in care by working locally to develop and implement clinical-care pathways. Hospitalists have also served as partners for hospitals to achieve compliance with payer quality mandates.
For example, in 2003, Medicare began requiring hospitals to report a handful of diagnosis-based quality measures it called the Core Measures. The number of measures continues to grow. In 2007, Medicare tied hospital reimbursement to performance on the Core Measures. I hear from hospital administrators that they find it easier to educate and work with a small group of hospitalists, rather than a large medical staff, to achieve optimal results on these measures.
Satisfaction: The exodus of primary care physicians (PCPs) from the hospital has fueled much of the growth in hospital medicine. PCPs have found it increasingly difficult to care for hospitalized patients while juggling the demands of a busy outpatient practice. In hospitalists, nurses have found a physician partner who is available physically to work with them in the care of acutely ill patients.
PCPs and nurses have been very satisfied with the hospitalist model of care. Although provider satisfaction is important, satisfaction in healthcare begins and ends with patients. Despite the discontinuity of care of meeting a new provider during hospitalization, patients have been satisfied with hospitalist care. Patients view hospitalists as providers available to provide for their acute needs while also communicating with the patients’ outpatient providers to understand their long-term needs.
I expect the number of hospitalists to grow over the next decade, albeit at a slower pace as most programs begin to fill their available positions. SHM believes the numbers of hospitalists will grow to 40,000.
There are a number of resources that can help you understand how to develop, manage, and grow a hospitalist program. I suggest you visit the “Practice Resources” section of the SHM Web site at www.hospitalmedicine.org. In particular, I recommend the “Best Practices in Managing a Hospital Medicine Program,” held twice a year. The spring program is held in conjunction with the SHM Annual Meeting in San Diego, April 3-5. The fall program is held in conjunction with the University of California, San Francisco’s “Management of the Hospitalized Patient” course in San Francisco. Also, the book Hospitalists: A Guide to Building and Sustaining a Successful Program by SHM Senior Vice President Joe Miller and SHM cofounders John Nelson, MD, and Winthrop F. Whitcomb, MD, is a must read for anybody looking to build a hospitalist program. TH
References
- Huddleston JM, Long KH, Naessens JM, Vanness DJ, Larson D, Trousdale R, Plevak M, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004 July 6;141(1):28-38.
- Phy MP, Vanness DJ, Melton JL, Hallong K, Schleck C, Larson DR, Huddleston PM. et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165:796-801.
Nocturnal Economics
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
Lessons of the Deposed
Recently I served as an expert witness in two cases; in each a hospitalist was being sued. While I can’t share details of these confidential cases, I can share my insights using a couple of hypothetical cases that illustrate the key lessons I learned:
- A 75-year-old woman was admitted by orthopedics after a fall requiring hip fracture repair. A hospitalist automatically saw her per the standing agreement. The hospitalist adjusted her diabetes regimen and held her aspirin because of bleeding. On the evening prior to discharge she developed right lower-extremity pain. The on-call orthopedist ordered a lower-extremity ultrasound from home.
The patient felt better the next morning and was discharged with hospitalist recommendations to increase her basal insulin, restart her aspirin, and follow up with her primary care provider (PCP). Three days later the patient presented in respiratory extremis and died in the emergency department. Post-mortem chart review noted a sonographic venous thrombosis in the right femoral vein that went unnoticed during her hospital stay.
- A 58-year-old woman was admitted after an uncomplicated appendectomy. On post-op day two, the surgeon asked the hospitalist to see the patient for a depressed mood. The hospitalist recommended starting an antidepressant and following up with her PCP after discharge. She also noted that the patient had right lower-extremity pain and swelling and recommended an ultrasound for workup of a deep venous thrombosis (DVT). The hospitalist did not see the patient again, and the ultrasound was not completed. Two days after discharge, the patient died at home after complaining of chest pain. Post-mortem autopsy revealed massive pulmonary embolism.
Two difficult cases, indeed. And I learned plenty from them:
Lesson one: Most lawsuits do not stem from deficiencies of medical knowledge.
In both cases, the hospitalists’ clinical reasoning was sound. In the first he was unaware of the patient’s overnight symptoms, which were not documented in the chart because the patient was not seen by the on-call orthopedist—a major systems error and lack of professionalism. This was compounded by a system that did not alert providers that an ultrasound was ordered or read as abnormal.
In the second case, the hospitalist got it right and made the correct recommendation—but the surgeon didn’t follow through.
Lesson two: Clarify your role—consultant or co-manager.
The differences between consultant and co-manager are subtle but crucial.
A consult is a request to answer a specific question: “Is this patient depressed, and how would you manage this problem?” This results in a detailed, focused appraisal of that issue, culminating in a note listing recommendations for further evaluation and management. It is the primary team’s responsibility to follow up on recommendations as they deem appropriate.
With this decision-making capacity, the primary team accepts near-full clinical and medical legal responsibility. As long as the consultant does due diligence and makes sound recommendations, it is unlikely he/she will be successfully sued for a bad outcome if the recommendations are not followed.
However, the hospitalist movement has changed this landscape considerably. We often function in a co-management model with our consulting colleagues, each of us caring for the issues within our respective scope of expertise.
This paradigm demands a level of responsibility sharing and communication that differs significantly from the traditional consultative model.
Knowing which model you are functioning under and who is responsible for which problems can be tricky. In the first case, who owned the decision-making for the patient’s DVT work-up?
The orthopedist may assume his role is focused on the care of the hip fracture surgery, while all else is the hospitalist’s purview. The hospitalist may assume DVT is a complication of the hip fracture surgery and is the orthopedist’s responsibility.
The second case seems easier as the hospitalist was clearly functioning as a consultant and therefore his obligation ends with his recommendation to further evaluate for DVT.
Or does it?
Lesson three: Communication is imperative.
The role we are functioning in—consultant versus co-manager—is not always intuitive. This perplexity can be further exacerbated by poor communication.
In both cases the hospitalists’ role was not established up front. Further, the hospitalists and their colleagues never spoke directly about the case or the management decisions.
In the second case the surgeon saw the recommendation but presumed the hospitalist would write the order for the ultrasound because they were co-managing the patient. He argued that he is not expert in the care of DVT and could not determine if the recommendation was sound. He assumed the hospitalist would appropriately evaluate this situation and complete the work-up if warranted. Because the hospitalist did not, the surgeon assumed the hospitalist was no longer concerned about DVT.
The hospitalist countered that she was specifically consulted to answer a question about depression. The recommendations regarding the swollen calf were also done in a consultative fashion, and the decision to obtain the ultrasound would fall to the surgeon.
The hospitalist argued that because the surgeon did not consult her again for this specific issue, she assumed he was comfortable evaluating and managing DVT.
This foray into the legal system reminded me that our patients trust we will give them the best care. When system and communication inadequacies get in the way of this, we can get sued—but our patients can lose their lives. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Recently I served as an expert witness in two cases; in each a hospitalist was being sued. While I can’t share details of these confidential cases, I can share my insights using a couple of hypothetical cases that illustrate the key lessons I learned:
- A 75-year-old woman was admitted by orthopedics after a fall requiring hip fracture repair. A hospitalist automatically saw her per the standing agreement. The hospitalist adjusted her diabetes regimen and held her aspirin because of bleeding. On the evening prior to discharge she developed right lower-extremity pain. The on-call orthopedist ordered a lower-extremity ultrasound from home.
The patient felt better the next morning and was discharged with hospitalist recommendations to increase her basal insulin, restart her aspirin, and follow up with her primary care provider (PCP). Three days later the patient presented in respiratory extremis and died in the emergency department. Post-mortem chart review noted a sonographic venous thrombosis in the right femoral vein that went unnoticed during her hospital stay.
- A 58-year-old woman was admitted after an uncomplicated appendectomy. On post-op day two, the surgeon asked the hospitalist to see the patient for a depressed mood. The hospitalist recommended starting an antidepressant and following up with her PCP after discharge. She also noted that the patient had right lower-extremity pain and swelling and recommended an ultrasound for workup of a deep venous thrombosis (DVT). The hospitalist did not see the patient again, and the ultrasound was not completed. Two days after discharge, the patient died at home after complaining of chest pain. Post-mortem autopsy revealed massive pulmonary embolism.
Two difficult cases, indeed. And I learned plenty from them:
Lesson one: Most lawsuits do not stem from deficiencies of medical knowledge.
In both cases, the hospitalists’ clinical reasoning was sound. In the first he was unaware of the patient’s overnight symptoms, which were not documented in the chart because the patient was not seen by the on-call orthopedist—a major systems error and lack of professionalism. This was compounded by a system that did not alert providers that an ultrasound was ordered or read as abnormal.
In the second case, the hospitalist got it right and made the correct recommendation—but the surgeon didn’t follow through.
Lesson two: Clarify your role—consultant or co-manager.
The differences between consultant and co-manager are subtle but crucial.
A consult is a request to answer a specific question: “Is this patient depressed, and how would you manage this problem?” This results in a detailed, focused appraisal of that issue, culminating in a note listing recommendations for further evaluation and management. It is the primary team’s responsibility to follow up on recommendations as they deem appropriate.
With this decision-making capacity, the primary team accepts near-full clinical and medical legal responsibility. As long as the consultant does due diligence and makes sound recommendations, it is unlikely he/she will be successfully sued for a bad outcome if the recommendations are not followed.
However, the hospitalist movement has changed this landscape considerably. We often function in a co-management model with our consulting colleagues, each of us caring for the issues within our respective scope of expertise.
This paradigm demands a level of responsibility sharing and communication that differs significantly from the traditional consultative model.
Knowing which model you are functioning under and who is responsible for which problems can be tricky. In the first case, who owned the decision-making for the patient’s DVT work-up?
The orthopedist may assume his role is focused on the care of the hip fracture surgery, while all else is the hospitalist’s purview. The hospitalist may assume DVT is a complication of the hip fracture surgery and is the orthopedist’s responsibility.
The second case seems easier as the hospitalist was clearly functioning as a consultant and therefore his obligation ends with his recommendation to further evaluate for DVT.
Or does it?
Lesson three: Communication is imperative.
The role we are functioning in—consultant versus co-manager—is not always intuitive. This perplexity can be further exacerbated by poor communication.
In both cases the hospitalists’ role was not established up front. Further, the hospitalists and their colleagues never spoke directly about the case or the management decisions.
In the second case the surgeon saw the recommendation but presumed the hospitalist would write the order for the ultrasound because they were co-managing the patient. He argued that he is not expert in the care of DVT and could not determine if the recommendation was sound. He assumed the hospitalist would appropriately evaluate this situation and complete the work-up if warranted. Because the hospitalist did not, the surgeon assumed the hospitalist was no longer concerned about DVT.
The hospitalist countered that she was specifically consulted to answer a question about depression. The recommendations regarding the swollen calf were also done in a consultative fashion, and the decision to obtain the ultrasound would fall to the surgeon.
The hospitalist argued that because the surgeon did not consult her again for this specific issue, she assumed he was comfortable evaluating and managing DVT.
This foray into the legal system reminded me that our patients trust we will give them the best care. When system and communication inadequacies get in the way of this, we can get sued—but our patients can lose their lives. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Recently I served as an expert witness in two cases; in each a hospitalist was being sued. While I can’t share details of these confidential cases, I can share my insights using a couple of hypothetical cases that illustrate the key lessons I learned:
- A 75-year-old woman was admitted by orthopedics after a fall requiring hip fracture repair. A hospitalist automatically saw her per the standing agreement. The hospitalist adjusted her diabetes regimen and held her aspirin because of bleeding. On the evening prior to discharge she developed right lower-extremity pain. The on-call orthopedist ordered a lower-extremity ultrasound from home.
The patient felt better the next morning and was discharged with hospitalist recommendations to increase her basal insulin, restart her aspirin, and follow up with her primary care provider (PCP). Three days later the patient presented in respiratory extremis and died in the emergency department. Post-mortem chart review noted a sonographic venous thrombosis in the right femoral vein that went unnoticed during her hospital stay.
- A 58-year-old woman was admitted after an uncomplicated appendectomy. On post-op day two, the surgeon asked the hospitalist to see the patient for a depressed mood. The hospitalist recommended starting an antidepressant and following up with her PCP after discharge. She also noted that the patient had right lower-extremity pain and swelling and recommended an ultrasound for workup of a deep venous thrombosis (DVT). The hospitalist did not see the patient again, and the ultrasound was not completed. Two days after discharge, the patient died at home after complaining of chest pain. Post-mortem autopsy revealed massive pulmonary embolism.
Two difficult cases, indeed. And I learned plenty from them:
Lesson one: Most lawsuits do not stem from deficiencies of medical knowledge.
In both cases, the hospitalists’ clinical reasoning was sound. In the first he was unaware of the patient’s overnight symptoms, which were not documented in the chart because the patient was not seen by the on-call orthopedist—a major systems error and lack of professionalism. This was compounded by a system that did not alert providers that an ultrasound was ordered or read as abnormal.
In the second case, the hospitalist got it right and made the correct recommendation—but the surgeon didn’t follow through.
Lesson two: Clarify your role—consultant or co-manager.
The differences between consultant and co-manager are subtle but crucial.
A consult is a request to answer a specific question: “Is this patient depressed, and how would you manage this problem?” This results in a detailed, focused appraisal of that issue, culminating in a note listing recommendations for further evaluation and management. It is the primary team’s responsibility to follow up on recommendations as they deem appropriate.
With this decision-making capacity, the primary team accepts near-full clinical and medical legal responsibility. As long as the consultant does due diligence and makes sound recommendations, it is unlikely he/she will be successfully sued for a bad outcome if the recommendations are not followed.
However, the hospitalist movement has changed this landscape considerably. We often function in a co-management model with our consulting colleagues, each of us caring for the issues within our respective scope of expertise.
This paradigm demands a level of responsibility sharing and communication that differs significantly from the traditional consultative model.
Knowing which model you are functioning under and who is responsible for which problems can be tricky. In the first case, who owned the decision-making for the patient’s DVT work-up?
The orthopedist may assume his role is focused on the care of the hip fracture surgery, while all else is the hospitalist’s purview. The hospitalist may assume DVT is a complication of the hip fracture surgery and is the orthopedist’s responsibility.
The second case seems easier as the hospitalist was clearly functioning as a consultant and therefore his obligation ends with his recommendation to further evaluate for DVT.
Or does it?
Lesson three: Communication is imperative.
The role we are functioning in—consultant versus co-manager—is not always intuitive. This perplexity can be further exacerbated by poor communication.
In both cases the hospitalists’ role was not established up front. Further, the hospitalists and their colleagues never spoke directly about the case or the management decisions.
In the second case the surgeon saw the recommendation but presumed the hospitalist would write the order for the ultrasound because they were co-managing the patient. He argued that he is not expert in the care of DVT and could not determine if the recommendation was sound. He assumed the hospitalist would appropriately evaluate this situation and complete the work-up if warranted. Because the hospitalist did not, the surgeon assumed the hospitalist was no longer concerned about DVT.
The hospitalist countered that she was specifically consulted to answer a question about depression. The recommendations regarding the swollen calf were also done in a consultative fashion, and the decision to obtain the ultrasound would fall to the surgeon.
The hospitalist argued that because the surgeon did not consult her again for this specific issue, she assumed he was comfortable evaluating and managing DVT.
This foray into the legal system reminded me that our patients trust we will give them the best care. When system and communication inadequacies get in the way of this, we can get sued—but our patients can lose their lives. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
SHM Chooses Greatness
We have reached an important milestone: SHM is 10 years old. As with all such anniversaries, it’s a good a time to reflect upon what we’ve achieved and decide our future objectives.
But to assess SHM’s progress, we must first know more about its past. The society was formed with the following objectives, found in our mission statement and declaration of goals:
Mission Statement
SHM is dedicated to promoting the highest quality care for all hospitalized patients. The society is committed to promoting excellence in the practice of hospital medicine through education, advocacy, and research.
Goals
- Promote high-quality care for all hospitalized patients;
- Promote education and research in hospital medicine;
- Promote teamwork to achieve the best possible care for hospitalized patients;
- Advocate a career path that will attract and retain the highest quality hospitalists;
- Define the competencies, activities, and needs of the hospitalist community; and
- Propose, support, and promote changes to the healthcare system that lead to higher quality, more efficient care for all hospitalized patients.
These are commendable goals, indeed. Achieving them is the responsibility of our Board of Directors, which is tasked with providing governance and guiding the society and its members in accordance with these objectives.
How does the SHM and our board make these real-world choices? Let’s take a closer look at the board and its thinking.
SHM’s bottom line is the care of our patients. It is the fundamental goal that sets us apart from for-profit companies where success is measured purely by financial returns. SHM and other medical societies also differ from for-profits in other fundamental ways. Our boards are composed of unpaid volunteers, and our power structures are diffuse rather than concentrated in a single, powerful CEO.
In addition, our board, like the boards of other medical societies, hires the CEO, provides for the election of board officers, and approves and manages the budget. It also supplies the leadership to guide our programs and evaluate our progress toward the goals it has set. Along with our executive staff, the board also oversees all strategic planning, relationships with other organizations, allocation of resources, membership growth, advocacy, and fundraising.
These functions and responsibilities are all attributes of good social-sector organizations. But our board strives for more than that. We want greatness, as defined by business researcher and author Jim Collins, in his monograph Good to Great and the Social Sectors. Assessing greatness, he says, comes down to one critical question: “How effectively do we deliver on our mission and make a distinctive impact, relative to our resources?”
There are seven key criteria derived from Collins’ research on greatness that you can use to assess the effectiveness of the SHM board.
- Were the activities we engaged in consistent with the mission?
- How much impact did we make, relative to our resources?
- What qualitative and quantitative achievements did the organization reach over the past year?
- Do the board’s actions and decisions endure, even when board members and officers change?
- Is the organization growing in terms of resources (revenues, membership, contributors)?
- Does the board build on its successes?
- Is the board clear about tough choices regarding what it can and cannot do?
It is in SHM’s single-minded allegiance to our mission where our choices have stood out from those of other medical societies. Some other societies spend [time and money] on protecting turf, defending professional fees, or advocating for higher reimbursement. Our prime focus—straight from our mission statement—has always been upon our patients. Our priorities revolve around patients and the hospital care setting. They revolve around how we can improve patient care, preserve resources, advance the education of our members, advance hospital medicine research, and partner with other healthcare professionals.
These are laudatory aims, but we have to remember that we work in an environment of limited—and competing—organizational resources. The board must make hard and sometimes unpopular choices regarding which projects, positions, or initiatives we undertake, and which we must say no to. This is the reality we live with. This is the discipline the board must exercise. We simply cannot do it all. And that means we cannot please everyone all the time.
The board hears its members when they ask, “Why aren’t you doing this?”—“this” being a variety of valuable projects competing for more valuable time and resources.
One of the board’s thornier issues has been deciding whether or not to accept money from Big Pharma, as some other medical organizations do. Other contentious issues include whether to weigh in on appropriate workloads for individual physicians or lobby for more reimbursement, especially from Medicare. Reasonable people can and do have differing opinions on these and other difficult issues. But the board must weigh each issue against our mission and goals and make a final judgment.
The board is responsible not only for what we do but how we do it. We must be thorough in our decision-making to avoid—or at least mitigate—unintended consequences. We must endeavor to always remain ethical in all our positions and dealings. As we focus on these important and difficult issues, the board will hold to one overriding principle: Make SHM a great organization that believes in its core values while constantly adapting to a changing environment.
Collins summed it up this way: “Greatness is not a function of circumstance. Greatness, it turns out, is a matter of conscious choice and discipline.” TH
Dr. Holman is the president of SHM.
We have reached an important milestone: SHM is 10 years old. As with all such anniversaries, it’s a good a time to reflect upon what we’ve achieved and decide our future objectives.
But to assess SHM’s progress, we must first know more about its past. The society was formed with the following objectives, found in our mission statement and declaration of goals:
Mission Statement
SHM is dedicated to promoting the highest quality care for all hospitalized patients. The society is committed to promoting excellence in the practice of hospital medicine through education, advocacy, and research.
Goals
- Promote high-quality care for all hospitalized patients;
- Promote education and research in hospital medicine;
- Promote teamwork to achieve the best possible care for hospitalized patients;
- Advocate a career path that will attract and retain the highest quality hospitalists;
- Define the competencies, activities, and needs of the hospitalist community; and
- Propose, support, and promote changes to the healthcare system that lead to higher quality, more efficient care for all hospitalized patients.
These are commendable goals, indeed. Achieving them is the responsibility of our Board of Directors, which is tasked with providing governance and guiding the society and its members in accordance with these objectives.
How does the SHM and our board make these real-world choices? Let’s take a closer look at the board and its thinking.
SHM’s bottom line is the care of our patients. It is the fundamental goal that sets us apart from for-profit companies where success is measured purely by financial returns. SHM and other medical societies also differ from for-profits in other fundamental ways. Our boards are composed of unpaid volunteers, and our power structures are diffuse rather than concentrated in a single, powerful CEO.
In addition, our board, like the boards of other medical societies, hires the CEO, provides for the election of board officers, and approves and manages the budget. It also supplies the leadership to guide our programs and evaluate our progress toward the goals it has set. Along with our executive staff, the board also oversees all strategic planning, relationships with other organizations, allocation of resources, membership growth, advocacy, and fundraising.
These functions and responsibilities are all attributes of good social-sector organizations. But our board strives for more than that. We want greatness, as defined by business researcher and author Jim Collins, in his monograph Good to Great and the Social Sectors. Assessing greatness, he says, comes down to one critical question: “How effectively do we deliver on our mission and make a distinctive impact, relative to our resources?”
There are seven key criteria derived from Collins’ research on greatness that you can use to assess the effectiveness of the SHM board.
- Were the activities we engaged in consistent with the mission?
- How much impact did we make, relative to our resources?
- What qualitative and quantitative achievements did the organization reach over the past year?
- Do the board’s actions and decisions endure, even when board members and officers change?
- Is the organization growing in terms of resources (revenues, membership, contributors)?
- Does the board build on its successes?
- Is the board clear about tough choices regarding what it can and cannot do?
It is in SHM’s single-minded allegiance to our mission where our choices have stood out from those of other medical societies. Some other societies spend [time and money] on protecting turf, defending professional fees, or advocating for higher reimbursement. Our prime focus—straight from our mission statement—has always been upon our patients. Our priorities revolve around patients and the hospital care setting. They revolve around how we can improve patient care, preserve resources, advance the education of our members, advance hospital medicine research, and partner with other healthcare professionals.
These are laudatory aims, but we have to remember that we work in an environment of limited—and competing—organizational resources. The board must make hard and sometimes unpopular choices regarding which projects, positions, or initiatives we undertake, and which we must say no to. This is the reality we live with. This is the discipline the board must exercise. We simply cannot do it all. And that means we cannot please everyone all the time.
The board hears its members when they ask, “Why aren’t you doing this?”—“this” being a variety of valuable projects competing for more valuable time and resources.
One of the board’s thornier issues has been deciding whether or not to accept money from Big Pharma, as some other medical organizations do. Other contentious issues include whether to weigh in on appropriate workloads for individual physicians or lobby for more reimbursement, especially from Medicare. Reasonable people can and do have differing opinions on these and other difficult issues. But the board must weigh each issue against our mission and goals and make a final judgment.
The board is responsible not only for what we do but how we do it. We must be thorough in our decision-making to avoid—or at least mitigate—unintended consequences. We must endeavor to always remain ethical in all our positions and dealings. As we focus on these important and difficult issues, the board will hold to one overriding principle: Make SHM a great organization that believes in its core values while constantly adapting to a changing environment.
Collins summed it up this way: “Greatness is not a function of circumstance. Greatness, it turns out, is a matter of conscious choice and discipline.” TH
Dr. Holman is the president of SHM.
We have reached an important milestone: SHM is 10 years old. As with all such anniversaries, it’s a good a time to reflect upon what we’ve achieved and decide our future objectives.
But to assess SHM’s progress, we must first know more about its past. The society was formed with the following objectives, found in our mission statement and declaration of goals:
Mission Statement
SHM is dedicated to promoting the highest quality care for all hospitalized patients. The society is committed to promoting excellence in the practice of hospital medicine through education, advocacy, and research.
Goals
- Promote high-quality care for all hospitalized patients;
- Promote education and research in hospital medicine;
- Promote teamwork to achieve the best possible care for hospitalized patients;
- Advocate a career path that will attract and retain the highest quality hospitalists;
- Define the competencies, activities, and needs of the hospitalist community; and
- Propose, support, and promote changes to the healthcare system that lead to higher quality, more efficient care for all hospitalized patients.
These are commendable goals, indeed. Achieving them is the responsibility of our Board of Directors, which is tasked with providing governance and guiding the society and its members in accordance with these objectives.
How does the SHM and our board make these real-world choices? Let’s take a closer look at the board and its thinking.
SHM’s bottom line is the care of our patients. It is the fundamental goal that sets us apart from for-profit companies where success is measured purely by financial returns. SHM and other medical societies also differ from for-profits in other fundamental ways. Our boards are composed of unpaid volunteers, and our power structures are diffuse rather than concentrated in a single, powerful CEO.
In addition, our board, like the boards of other medical societies, hires the CEO, provides for the election of board officers, and approves and manages the budget. It also supplies the leadership to guide our programs and evaluate our progress toward the goals it has set. Along with our executive staff, the board also oversees all strategic planning, relationships with other organizations, allocation of resources, membership growth, advocacy, and fundraising.
These functions and responsibilities are all attributes of good social-sector organizations. But our board strives for more than that. We want greatness, as defined by business researcher and author Jim Collins, in his monograph Good to Great and the Social Sectors. Assessing greatness, he says, comes down to one critical question: “How effectively do we deliver on our mission and make a distinctive impact, relative to our resources?”
There are seven key criteria derived from Collins’ research on greatness that you can use to assess the effectiveness of the SHM board.
- Were the activities we engaged in consistent with the mission?
- How much impact did we make, relative to our resources?
- What qualitative and quantitative achievements did the organization reach over the past year?
- Do the board’s actions and decisions endure, even when board members and officers change?
- Is the organization growing in terms of resources (revenues, membership, contributors)?
- Does the board build on its successes?
- Is the board clear about tough choices regarding what it can and cannot do?
It is in SHM’s single-minded allegiance to our mission where our choices have stood out from those of other medical societies. Some other societies spend [time and money] on protecting turf, defending professional fees, or advocating for higher reimbursement. Our prime focus—straight from our mission statement—has always been upon our patients. Our priorities revolve around patients and the hospital care setting. They revolve around how we can improve patient care, preserve resources, advance the education of our members, advance hospital medicine research, and partner with other healthcare professionals.
These are laudatory aims, but we have to remember that we work in an environment of limited—and competing—organizational resources. The board must make hard and sometimes unpopular choices regarding which projects, positions, or initiatives we undertake, and which we must say no to. This is the reality we live with. This is the discipline the board must exercise. We simply cannot do it all. And that means we cannot please everyone all the time.
The board hears its members when they ask, “Why aren’t you doing this?”—“this” being a variety of valuable projects competing for more valuable time and resources.
One of the board’s thornier issues has been deciding whether or not to accept money from Big Pharma, as some other medical organizations do. Other contentious issues include whether to weigh in on appropriate workloads for individual physicians or lobby for more reimbursement, especially from Medicare. Reasonable people can and do have differing opinions on these and other difficult issues. But the board must weigh each issue against our mission and goals and make a final judgment.
The board is responsible not only for what we do but how we do it. We must be thorough in our decision-making to avoid—or at least mitigate—unintended consequences. We must endeavor to always remain ethical in all our positions and dealings. As we focus on these important and difficult issues, the board will hold to one overriding principle: Make SHM a great organization that believes in its core values while constantly adapting to a changing environment.
Collins summed it up this way: “Greatness is not a function of circumstance. Greatness, it turns out, is a matter of conscious choice and discipline.” TH
Dr. Holman is the president of SHM.
One for the Ages
A t 77, Robert Eddy, MD, is a busy fellow. As a hospitalist at the 278-bed Brantford General Hospital in Brantford, Ontario, Canada, he works an average of 70 hours a week.
What keeps him going?
“After a long day at work I really look forward to my gin and tonic,” he says. “I have a picture of it in my mind when I’m driving home.”
On a more serious note, Dr. Eddy attributes his career longevity to good health, good genes, never smoking, and not overdoing the booze.
“I’m very lucky,” he says. “As a doctor you can keep going as long as you don’t have major health problems. My dad died in his 90s, so longevity runs in my family.”
Dr. Eddy rises early to do paperwork at his home office, then drives 20 minutes to the hospital and performs his hospitalist duties five mornings a week, Monday through Friday. On an average day he sees 12 inpatients, completes his charts, then grabs a quick lunch before heading out to see patients in a shared office practice in Burford, about nine miles away.
Scheduling around his hospitalist work and the office practice, he also makes house calls and nursing home visits to his sickest and frailest patients. He covers for his community-based colleagues and hospitalists, and twice a month organizes CME meetings for family physicians. From March to July he adds a temporary assignment at St. Joseph’s Villa in Dundas, tending to 70 patients at that retirement community.
Janice Legere, MD, medical director of the hospitalist program of Brantford General Hospital, calls him “a country guy with a very dry sense of humor. The other hospitalists look up to him because he is the real deal as a doctor.”
Not bad for a gentleman born in the same year and month as the beginning of the Great Depression—October 1929. In his sixth decade of medicine, Dr. Eddy may be the oldest practicing hospitalist.
—Sandra Eddy, wife of Robert Eddy, MD, hospitalist at Brantford General Hospital in Ontario, Canada
No Sign of Slowing
Although he has practiced medicine for more than 52 years, retirement is not on his agenda.
“I closed my solo practice in 1999 because I didn’t want to work so hard, but I’m busier than ever now,” he says.
While Dr. Eddy and his second wife, Sandra, seriously discuss the possibility of his retirement every year, they have reupped for the hospitalist work, office practice, and house/nursing home visits at least through 2008. As they describe it, the overburdened Canadian healthcare system needs every qualified pair of physician hands it can get.
Ontario’s healthcare system can ill afford to lose someone of Dr. Eddy’s commitment, knowledge, and experience.
“I love medicine and am very lucky to have the energy and the stamina to keep going,” Dr. Eddy says. “I enjoy seeing hospitalized patients because I have as much time as I need to do a general assessment of their medical condition. I get my mind around the whole patient.”
His wife affirms Dr. Eddy’s commitment.
“We have been together for 28 years, and we have a good marriage,” she says. ‘‘But he is on call 24/7, and medicine always comes first. Then there’s us.”
But Dr. Eddy’s not just a nose-to-the-grindstone type of guy—he and Sandra do relax together. Along with his nightly after-work gin and tonic and an annual week’s trip to Las Vegas, they enjoy outings to the local casino, golf, dinners with friends, and frequent visits from three grandchildren.
“I enjoy the variety in my career as a physician and the quality of my life,” he concludes.
The New Hospitalist
Becoming a hospitalist seemed a logical step for Dr. Eddy when he opted to leave full-time office practice in 1999. Brantford General Hospital, where he had admitting privileges, covered a catchment area of 80,000 people.
When the only two other hospitals in the area were closed, Brantford General was overwhelmed. Adding to the systemic distress, 80% of community doctors had given up their hospital privileges. Hospitalists were urgently needed to pick up the slack. Dr. Eddy went for it.
In Canada, hospital throughput isn’t a priority. The system lacks enough sub-acute and rehab beds to discharge patients from hospitals in a timely fashion, leaving patients hospitalized longer compared with similar care in the United States. The average length of stay for heart failure is 6.1 days in the U.S. versus 8.5 days in Canada; for aortic aneurysm repair it’s seven days (U.S.) versus nine days (Canada), according to the Journal of Cardiology.
Those bottlenecks lead to hospitalized patients ready for a less acute level of care occupying beds needed for acute patients. For example, patients wait months for knee replacement surgery, then spend three to four weeks on the rehab ward in the hospital. A step-down facility would probably be ideal but doesn’t exist. “There are people lying in the ER overnight, people who need to be in palliative care units who are in acute care beds,” Dr. Eddy notes. “It is very tough.”
As a family physician, Dr. Eddy favored a hospitalist career because he would have the time to do a general assessment—a whole-patient, complete check-up. He doesn’t admit patients or work in the ED (“Not my forte; I’m not looking for more stress,” he says), but works on the general medical units.
According to Dr. Legere, the septuagenarian physician works approximately 75% of full-time hospitalist hours. He puts in at least 40 weeks a year and covers at least 10 weekends for the hospitalist service.
Hospitalist Larry Kramer, MD, who has worked side by side with Dr. Eddy since 2002, calls him a compassionate, sensitive physician attuned to the small kindnesses patients and family appreciate, such as remembering everyone’s name.
“He’s an excellent team member, always open to referrals and consultations,” says Dr. Kramer, who’s also impressed with Dr. Eddy’s interest in mastering a Palm Pilot when he discovered how much easier and faster it was to access clinical and pharmaceutical information. “He didn’t grow up with computers, but he sure learned how to use his Palm,” adds Dr. Kramer.
The Office Practice
When he started his hospitalist career, Dr. Eddy fully intended to relinquish the office practice to another family physician. It didn’t happen that way—there were about 200 patients he couldn’t give up.
“They are elderly, and I make house calls if it’s too much of a burden for them to come to the office,” he says. “I also see them in nursing homes or retirement homes.” He also covers the office practice for the month of August so his practice partner can have the month off.
His wife, who fields home office phone calls, attends to the issues of 200 special patients and also tries to guide those looking for a primary care doctor to someone else willing to take them.
“My wife works very hard at managing my private practice,” says Dr. Eddy. “She’s a people person but is not soft-minded at all. She helps a lot of patients find primary care physicians who will take them on as well as fielding calls from my private patients.”
The Ontario Health Insurance Plan (OHIP) pays him on a fee-for-service basis. In 2000, when bureaucrats tried to avoid reimbursing him for making house calls by stipulating that at least 50% had to be for palliative care, he made a list of all 200 patients. He made his case for palliative care—“they’ll all die within four years.” The medical establishment accepted it, and he continues making house calls—for which he says the health authorities are relaxing the regulations.
As if the hospitalist and office practice weren’t enough, Dr. Eddy runs a small group practice CME program sponsored by McMaster University and the College of Family Physicians of Canada. “Six of us family physicians get together to discuss three cases based on handouts and a fact section” he says. The CME group meets twice a month for eight months of the year.
In short, Dr. Eddy describes himself as having energy to burn. His hospitalist colleague Dr. Kramer seconds that.
“The amount of work he does is phenomenal,” Dr. Kramer says. “He is very thorough, and it’s remarkable to see how much he still loves practicing medicine. It’s hard to believe that when he’s finished with his hospitalist job he heads off to his office practice, house calls, and nursing home work.”
And what does Dr. Eddy think of his colleagues?
“They seem quite young,” he says of Brantford’s cadre of six full-time and six part-time hospitalists. “But come to think of it most are in their 40s, and some in their 50s and 60s. Maybe they aren’t so young.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
A t 77, Robert Eddy, MD, is a busy fellow. As a hospitalist at the 278-bed Brantford General Hospital in Brantford, Ontario, Canada, he works an average of 70 hours a week.
What keeps him going?
“After a long day at work I really look forward to my gin and tonic,” he says. “I have a picture of it in my mind when I’m driving home.”
On a more serious note, Dr. Eddy attributes his career longevity to good health, good genes, never smoking, and not overdoing the booze.
“I’m very lucky,” he says. “As a doctor you can keep going as long as you don’t have major health problems. My dad died in his 90s, so longevity runs in my family.”
Dr. Eddy rises early to do paperwork at his home office, then drives 20 minutes to the hospital and performs his hospitalist duties five mornings a week, Monday through Friday. On an average day he sees 12 inpatients, completes his charts, then grabs a quick lunch before heading out to see patients in a shared office practice in Burford, about nine miles away.
Scheduling around his hospitalist work and the office practice, he also makes house calls and nursing home visits to his sickest and frailest patients. He covers for his community-based colleagues and hospitalists, and twice a month organizes CME meetings for family physicians. From March to July he adds a temporary assignment at St. Joseph’s Villa in Dundas, tending to 70 patients at that retirement community.
Janice Legere, MD, medical director of the hospitalist program of Brantford General Hospital, calls him “a country guy with a very dry sense of humor. The other hospitalists look up to him because he is the real deal as a doctor.”
Not bad for a gentleman born in the same year and month as the beginning of the Great Depression—October 1929. In his sixth decade of medicine, Dr. Eddy may be the oldest practicing hospitalist.
—Sandra Eddy, wife of Robert Eddy, MD, hospitalist at Brantford General Hospital in Ontario, Canada
No Sign of Slowing
Although he has practiced medicine for more than 52 years, retirement is not on his agenda.
“I closed my solo practice in 1999 because I didn’t want to work so hard, but I’m busier than ever now,” he says.
While Dr. Eddy and his second wife, Sandra, seriously discuss the possibility of his retirement every year, they have reupped for the hospitalist work, office practice, and house/nursing home visits at least through 2008. As they describe it, the overburdened Canadian healthcare system needs every qualified pair of physician hands it can get.
Ontario’s healthcare system can ill afford to lose someone of Dr. Eddy’s commitment, knowledge, and experience.
“I love medicine and am very lucky to have the energy and the stamina to keep going,” Dr. Eddy says. “I enjoy seeing hospitalized patients because I have as much time as I need to do a general assessment of their medical condition. I get my mind around the whole patient.”
His wife affirms Dr. Eddy’s commitment.
“We have been together for 28 years, and we have a good marriage,” she says. ‘‘But he is on call 24/7, and medicine always comes first. Then there’s us.”
But Dr. Eddy’s not just a nose-to-the-grindstone type of guy—he and Sandra do relax together. Along with his nightly after-work gin and tonic and an annual week’s trip to Las Vegas, they enjoy outings to the local casino, golf, dinners with friends, and frequent visits from three grandchildren.
“I enjoy the variety in my career as a physician and the quality of my life,” he concludes.
The New Hospitalist
Becoming a hospitalist seemed a logical step for Dr. Eddy when he opted to leave full-time office practice in 1999. Brantford General Hospital, where he had admitting privileges, covered a catchment area of 80,000 people.
When the only two other hospitals in the area were closed, Brantford General was overwhelmed. Adding to the systemic distress, 80% of community doctors had given up their hospital privileges. Hospitalists were urgently needed to pick up the slack. Dr. Eddy went for it.
In Canada, hospital throughput isn’t a priority. The system lacks enough sub-acute and rehab beds to discharge patients from hospitals in a timely fashion, leaving patients hospitalized longer compared with similar care in the United States. The average length of stay for heart failure is 6.1 days in the U.S. versus 8.5 days in Canada; for aortic aneurysm repair it’s seven days (U.S.) versus nine days (Canada), according to the Journal of Cardiology.
Those bottlenecks lead to hospitalized patients ready for a less acute level of care occupying beds needed for acute patients. For example, patients wait months for knee replacement surgery, then spend three to four weeks on the rehab ward in the hospital. A step-down facility would probably be ideal but doesn’t exist. “There are people lying in the ER overnight, people who need to be in palliative care units who are in acute care beds,” Dr. Eddy notes. “It is very tough.”
As a family physician, Dr. Eddy favored a hospitalist career because he would have the time to do a general assessment—a whole-patient, complete check-up. He doesn’t admit patients or work in the ED (“Not my forte; I’m not looking for more stress,” he says), but works on the general medical units.
According to Dr. Legere, the septuagenarian physician works approximately 75% of full-time hospitalist hours. He puts in at least 40 weeks a year and covers at least 10 weekends for the hospitalist service.
Hospitalist Larry Kramer, MD, who has worked side by side with Dr. Eddy since 2002, calls him a compassionate, sensitive physician attuned to the small kindnesses patients and family appreciate, such as remembering everyone’s name.
“He’s an excellent team member, always open to referrals and consultations,” says Dr. Kramer, who’s also impressed with Dr. Eddy’s interest in mastering a Palm Pilot when he discovered how much easier and faster it was to access clinical and pharmaceutical information. “He didn’t grow up with computers, but he sure learned how to use his Palm,” adds Dr. Kramer.
The Office Practice
When he started his hospitalist career, Dr. Eddy fully intended to relinquish the office practice to another family physician. It didn’t happen that way—there were about 200 patients he couldn’t give up.
“They are elderly, and I make house calls if it’s too much of a burden for them to come to the office,” he says. “I also see them in nursing homes or retirement homes.” He also covers the office practice for the month of August so his practice partner can have the month off.
His wife, who fields home office phone calls, attends to the issues of 200 special patients and also tries to guide those looking for a primary care doctor to someone else willing to take them.
“My wife works very hard at managing my private practice,” says Dr. Eddy. “She’s a people person but is not soft-minded at all. She helps a lot of patients find primary care physicians who will take them on as well as fielding calls from my private patients.”
The Ontario Health Insurance Plan (OHIP) pays him on a fee-for-service basis. In 2000, when bureaucrats tried to avoid reimbursing him for making house calls by stipulating that at least 50% had to be for palliative care, he made a list of all 200 patients. He made his case for palliative care—“they’ll all die within four years.” The medical establishment accepted it, and he continues making house calls—for which he says the health authorities are relaxing the regulations.
As if the hospitalist and office practice weren’t enough, Dr. Eddy runs a small group practice CME program sponsored by McMaster University and the College of Family Physicians of Canada. “Six of us family physicians get together to discuss three cases based on handouts and a fact section” he says. The CME group meets twice a month for eight months of the year.
In short, Dr. Eddy describes himself as having energy to burn. His hospitalist colleague Dr. Kramer seconds that.
“The amount of work he does is phenomenal,” Dr. Kramer says. “He is very thorough, and it’s remarkable to see how much he still loves practicing medicine. It’s hard to believe that when he’s finished with his hospitalist job he heads off to his office practice, house calls, and nursing home work.”
And what does Dr. Eddy think of his colleagues?
“They seem quite young,” he says of Brantford’s cadre of six full-time and six part-time hospitalists. “But come to think of it most are in their 40s, and some in their 50s and 60s. Maybe they aren’t so young.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
A t 77, Robert Eddy, MD, is a busy fellow. As a hospitalist at the 278-bed Brantford General Hospital in Brantford, Ontario, Canada, he works an average of 70 hours a week.
What keeps him going?
“After a long day at work I really look forward to my gin and tonic,” he says. “I have a picture of it in my mind when I’m driving home.”
On a more serious note, Dr. Eddy attributes his career longevity to good health, good genes, never smoking, and not overdoing the booze.
“I’m very lucky,” he says. “As a doctor you can keep going as long as you don’t have major health problems. My dad died in his 90s, so longevity runs in my family.”
Dr. Eddy rises early to do paperwork at his home office, then drives 20 minutes to the hospital and performs his hospitalist duties five mornings a week, Monday through Friday. On an average day he sees 12 inpatients, completes his charts, then grabs a quick lunch before heading out to see patients in a shared office practice in Burford, about nine miles away.
Scheduling around his hospitalist work and the office practice, he also makes house calls and nursing home visits to his sickest and frailest patients. He covers for his community-based colleagues and hospitalists, and twice a month organizes CME meetings for family physicians. From March to July he adds a temporary assignment at St. Joseph’s Villa in Dundas, tending to 70 patients at that retirement community.
Janice Legere, MD, medical director of the hospitalist program of Brantford General Hospital, calls him “a country guy with a very dry sense of humor. The other hospitalists look up to him because he is the real deal as a doctor.”
Not bad for a gentleman born in the same year and month as the beginning of the Great Depression—October 1929. In his sixth decade of medicine, Dr. Eddy may be the oldest practicing hospitalist.
—Sandra Eddy, wife of Robert Eddy, MD, hospitalist at Brantford General Hospital in Ontario, Canada
No Sign of Slowing
Although he has practiced medicine for more than 52 years, retirement is not on his agenda.
“I closed my solo practice in 1999 because I didn’t want to work so hard, but I’m busier than ever now,” he says.
While Dr. Eddy and his second wife, Sandra, seriously discuss the possibility of his retirement every year, they have reupped for the hospitalist work, office practice, and house/nursing home visits at least through 2008. As they describe it, the overburdened Canadian healthcare system needs every qualified pair of physician hands it can get.
Ontario’s healthcare system can ill afford to lose someone of Dr. Eddy’s commitment, knowledge, and experience.
“I love medicine and am very lucky to have the energy and the stamina to keep going,” Dr. Eddy says. “I enjoy seeing hospitalized patients because I have as much time as I need to do a general assessment of their medical condition. I get my mind around the whole patient.”
His wife affirms Dr. Eddy’s commitment.
“We have been together for 28 years, and we have a good marriage,” she says. ‘‘But he is on call 24/7, and medicine always comes first. Then there’s us.”
But Dr. Eddy’s not just a nose-to-the-grindstone type of guy—he and Sandra do relax together. Along with his nightly after-work gin and tonic and an annual week’s trip to Las Vegas, they enjoy outings to the local casino, golf, dinners with friends, and frequent visits from three grandchildren.
“I enjoy the variety in my career as a physician and the quality of my life,” he concludes.
The New Hospitalist
Becoming a hospitalist seemed a logical step for Dr. Eddy when he opted to leave full-time office practice in 1999. Brantford General Hospital, where he had admitting privileges, covered a catchment area of 80,000 people.
When the only two other hospitals in the area were closed, Brantford General was overwhelmed. Adding to the systemic distress, 80% of community doctors had given up their hospital privileges. Hospitalists were urgently needed to pick up the slack. Dr. Eddy went for it.
In Canada, hospital throughput isn’t a priority. The system lacks enough sub-acute and rehab beds to discharge patients from hospitals in a timely fashion, leaving patients hospitalized longer compared with similar care in the United States. The average length of stay for heart failure is 6.1 days in the U.S. versus 8.5 days in Canada; for aortic aneurysm repair it’s seven days (U.S.) versus nine days (Canada), according to the Journal of Cardiology.
Those bottlenecks lead to hospitalized patients ready for a less acute level of care occupying beds needed for acute patients. For example, patients wait months for knee replacement surgery, then spend three to four weeks on the rehab ward in the hospital. A step-down facility would probably be ideal but doesn’t exist. “There are people lying in the ER overnight, people who need to be in palliative care units who are in acute care beds,” Dr. Eddy notes. “It is very tough.”
As a family physician, Dr. Eddy favored a hospitalist career because he would have the time to do a general assessment—a whole-patient, complete check-up. He doesn’t admit patients or work in the ED (“Not my forte; I’m not looking for more stress,” he says), but works on the general medical units.
According to Dr. Legere, the septuagenarian physician works approximately 75% of full-time hospitalist hours. He puts in at least 40 weeks a year and covers at least 10 weekends for the hospitalist service.
Hospitalist Larry Kramer, MD, who has worked side by side with Dr. Eddy since 2002, calls him a compassionate, sensitive physician attuned to the small kindnesses patients and family appreciate, such as remembering everyone’s name.
“He’s an excellent team member, always open to referrals and consultations,” says Dr. Kramer, who’s also impressed with Dr. Eddy’s interest in mastering a Palm Pilot when he discovered how much easier and faster it was to access clinical and pharmaceutical information. “He didn’t grow up with computers, but he sure learned how to use his Palm,” adds Dr. Kramer.
The Office Practice
When he started his hospitalist career, Dr. Eddy fully intended to relinquish the office practice to another family physician. It didn’t happen that way—there were about 200 patients he couldn’t give up.
“They are elderly, and I make house calls if it’s too much of a burden for them to come to the office,” he says. “I also see them in nursing homes or retirement homes.” He also covers the office practice for the month of August so his practice partner can have the month off.
His wife, who fields home office phone calls, attends to the issues of 200 special patients and also tries to guide those looking for a primary care doctor to someone else willing to take them.
“My wife works very hard at managing my private practice,” says Dr. Eddy. “She’s a people person but is not soft-minded at all. She helps a lot of patients find primary care physicians who will take them on as well as fielding calls from my private patients.”
The Ontario Health Insurance Plan (OHIP) pays him on a fee-for-service basis. In 2000, when bureaucrats tried to avoid reimbursing him for making house calls by stipulating that at least 50% had to be for palliative care, he made a list of all 200 patients. He made his case for palliative care—“they’ll all die within four years.” The medical establishment accepted it, and he continues making house calls—for which he says the health authorities are relaxing the regulations.
As if the hospitalist and office practice weren’t enough, Dr. Eddy runs a small group practice CME program sponsored by McMaster University and the College of Family Physicians of Canada. “Six of us family physicians get together to discuss three cases based on handouts and a fact section” he says. The CME group meets twice a month for eight months of the year.
In short, Dr. Eddy describes himself as having energy to burn. His hospitalist colleague Dr. Kramer seconds that.
“The amount of work he does is phenomenal,” Dr. Kramer says. “He is very thorough, and it’s remarkable to see how much he still loves practicing medicine. It’s hard to believe that when he’s finished with his hospitalist job he heads off to his office practice, house calls, and nursing home work.”
And what does Dr. Eddy think of his colleagues?
“They seem quite young,” he says of Brantford’s cadre of six full-time and six part-time hospitalists. “But come to think of it most are in their 40s, and some in their 50s and 60s. Maybe they aren’t so young.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
What is the target blood glucose for noncritical care patients?
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.