User login
Poly-L-lactic Acid for the Treatment of Trauma-Induced Facial Lipoatrophy and Asymmetry
Trolamine-Containing Topical Emulsion: Clinical Applications in Dermatology
Vaccine update: New CDC recommendations from 2007
The year 2007 was rather calm, compared to the 3 previous years in regards to new vaccines and vaccine recommendations. Although no breakthrough vaccine products came onto the market in 2007, there were new recommendations and licensure for new age groups for existing vaccines and a recall of some lots of Hib vaccines.
Meningococcal vaccine
Recommendations on the use of the quadrivalent meningococcal conjugate vaccine (MCV4) have evolved since its licensure in 2005 for use in persons 11 to 55 years of age. The first set of recommendations focused on universal vaccination of preteens, aged 11 to 12, those entering high school who had not received the vaccine previously, and others at risk for meningococcal disease including college freshmen living in dormitories.1 The MCV4 was preferred to the older polysaccharide vaccine (MPSV4) which was recommended only for children aged 2 to 10 and adults over age 55 at increased risk.
In 2007, the CDC changed 2 of the 2005 recommendations:
- The first, in August, simplified the recommendations for teens, making MCV4 universally recommended for all those aged 11 to 18 at the earliest opportunity.2
- The second, in December, followed FDA approval for use of MCV4 in children aged 2 to 10 years. The CDC now recommends MCV4 as the preferred vaccine in this age group for those at risk (TABLE 1).3
TABLE 1
Populations at increased risk for meningococcal disease who should receive quadrivalent meningococcal conjugate vaccine
|
If someone at ongoing risk for meningococcal disease has been previously vaccinated with MPSV4, they should be revaccinated 3 years later with MCV4. It is not known if repeat doses of MCV4 will be needed, and if so, after what amount of time.
The MCV4 has been linked to Guillain-Barré syndrome (GBS), and a history of GBS is a precaution for its use. For those with a history of GBS who need protection against meningococcal infection, MPSV4 is an alternative.
Hepatitis A vaccine
Widespread use of inactivated hepatitis A vaccine (HAV), first licensed in 1995, has markedly reduced the incidence of hepatitis A infection (FIGURE). Recommendations for its use have been periodically revised; current recommendations include universal vaccination of all children at age 12 to 23 months, catch-up vaccination in older children in areas of high prevalence, and vaccination of those at increased risk for hepatitis A including travelers to endemic areas, users of illicit drugs and men who have sex with men.4
FIGURE
Reduction in incidence of hepatitis A infection
Source: Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2006; 55(RR-07).
For those unvaccinated who are acutely exposed to hepatitis A virus and those traveling to areas of high prevalence who do not have time to complete the 2 doses of HAV, the only prevention available until recently has been IG. This has now changed and HAV can be used in both groups. The new recommendation for postexposure prophylaxis is that either a single dose of HAV or use of IG is acceptable.5 At ages 12 months to 40 years, vaccine is preferred. For those over age 40, IG is preferred but vaccine is acceptable. For children less than 12 months, the immune suppressed, and those with chronic liver disease, IG should be used.
Those traveling or working in countries with high rates of hepatitis A can be protected with either HAV or IG. A single dose of HAV is sufficient for healthy people, with a second dose at the recommended interval to complete the series. Those under age 12 months, those who choose not to receive the vaccine, and those who are allergic to the vaccine should be offered IG. Both IG and HAV should be considered for individuals who plan to travel within 2 weeks of the first HAV dose; those over age 40, the immune compromised, and those with chronic liver disease or other chronic medical conditions.
Live attenuated influenza vaccine
FluMist, the live attenuated influenza vaccine (LAIV), which is administered as an intranasal spray, is now approved for use among those 2 to 4 years of age.6 Previously, the LAIV was approved only for healthy, non pregnant persons, 5 to 49 years of age. The LAIV may actually be the preferred product in children as it has been shown to prevent more influenza illness than the trivalent inactivated vaccine (TIV). The LAIV should not be used in anyone with a condition listed in TABLE 2 and should not be administered to children under age 5 who have recurrent wheezing.
FluMist has also been modified in several advantageous ways:
- The dose in the sprayer is now 0.2 mL (previously 0.5 mL). One half of the dose should be administered in each nostril.
- The product no longer has to be stored frozen; it should be kept at 35° to 46°F.
- When 2 doses are needed in children under age 9 being vaccinated for the first time, the interval between doses is now 4 weeks (previously 6 weeks).
TABLE 2
LAIV (FluMist) should not be used in these groups
|
Children under age 9 years who receive only 1 dose of vaccine (either TIV or LAIV) the first year they are vaccinated should receive 2 doses the next year.6 If they fail to receive 2 doses in the next year, only a single dose is recommended after that. This is a slight modification of the previous recommendation that only 1 dose was recommended in this situation.7
Alternative schedule for combined hepatitis A and B vaccine
The FDA approved an alternate, 4-dose schedule for the combined hepatitis A and hepatitis B vaccine (Twinrix): at 0, 7, 21 days, and 12 months.8 It was previously approved only for a 3-dose schedule: at 0, 1, and 6 months. The new alternative schedule allows greater protection for travelers who need to depart in less than a month’s time.
Merck recalls some lots of Hib vaccine
On December 11, 2007, Merck announced a voluntary recall of specific lots of Haemophilus influenza type b (Hib) conjugate vaccine products: 10 lots of a monovalent Hib vaccine, PedvaxHIB, and 2 lots of a combined hepatitis B/Hib vaccine, Comvax.
Consult Merck’s Web site for the lots involved and for instructions on returning vaccine (www.merckvaccines. com/PCHRecall.pdf). The recall was prompted by concern about equipment sterility, although no vaccine has been shown to be contaminated. Children vaccinated with Merck products do not need to be revaccinated or obtain any special follow-up.
Shortage expected. It is unknown when Merck will resume production, but it is not anticipated until at least late in 2008. Other Hib-containing products are produced by Sanofi Pasteur but the supply of these products will not make up for the expected shortage.
Interim recommendations. The recall resulted in interim recommendations from the CDC.9 These recommendations are complicated because the dosing schedule for Hib vaccine differs by the product and the age of receipt of first vaccine when children are not on schedule. TABLE 3 lists the Hib-containing products, the recommended primary series schedule, and booster dose.
TABLE 3
Hib products
| PRIMARY SERIES | BOOSTER | |||
|---|---|---|---|---|
| Merck Products | ||||
| PedvaxHIB | Monovalent Hib vaccine | 2, 4 months | 12–15 months* | |
| Comvax | Combined Hib/hepatitis B vaccine | 2, 4 months | 12–15 months* | |
| Sanofi Pasteur products | ||||
| ActHIB | Monovalent hib vaccine | 2, 4, 6 months | 12–15 months* | |
| TriHIBit | DTaP/Hib vaccine | Not licensed for this age group | 15–18 months* | |
| * Can follow a primary series of any product or serve as the only dose for a child up to 59 months, not previously immunized. | ||||
The main points are:
- Defer the booster dose at age 12 to 15 months until the shortage is resolved, except for high-risk children.
- High-risk children, who should continue to receive the booster at ages 12 to 15 months, include those with asplenia, sickle cell disease, HIV infection, and certain other immune deficiencies and cancers, and American Indian/Alaskan Native children.
- Physicians should keep track of children who have the booster deferred so they can be vaccinated when the supply improves.
- Non-recalled lots of PedvaxHIB and Comvax in the CDC stockpile will be prioritized to providers who care for predominantly American Indian/Alaskan Native children, who are at markedly in creased risk of Hib infection.
- If a child has received only 1 dose of PedvaxHIB or Comvax, their primary series can be completed with ActHIB, but 3 total doses are needed.
Children through age 59 months who are behind schedule should complete a primary series according to published recommendations.10 Physicians should call their local health department if they have any questions about what to do in a specific case.
1. CDC. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005;54(RR-7):1-21.
2. CDC. Revised recommendations of the Advisory Committee on Immunization Practices to vaccinate all persons aged 11-18 years with meningococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep 2007;56:794-795.
3. CDC. Recommendation from the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MCV4) in children aged 2-10 years at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep 2007;56:1265-1266.
4. CDC. Update: prevention of hepatitis A after exposure to hepatitis A virus and in international travelers. Updated recommendations of the ACIP. MMWR Morb Mortal Wkly Rep 2007;56:1080-1084.
5. Advisory Committee on Immunization Practices (ACIP), Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006;55(RR-07):1-23.
6. CDC. Expansion of use of live attenuated influenza vaccine to children aged 2-4 years and other Flu-Mist changes for the 2007-2008 influenza season. MMWR Morb Mortal Wkly Rep 2007;56:1217-1219.
7. Fiore AE, Shay DK, Haber P, et al. Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep 2007;56(RR-6):1-54.
8. CDC. FDA approval of an alternate dosing schedule for a combined hepatitis A and B vaccine (Twinrix). MMWR Morb Mortal Wkly Rep 2007;56:1057.-
9. CDC. Interim recommendations for the use of Haemophilus influenza Type b (Hib) conjugate vaccines related to the recall of certain lots of Hib-containing vaccines (PedvaxHIB and Comvax). MMWR Morb Mortal Wkly Rep 2007;56:1318-1320.
10. CDC. Catch-up immunization schedule for persons aged 4 months-18 years who start late or are more than one month behind. Available at www.cdc.gov/vaccines/recs/schedules/downloads/child/2007/child-schedule-color-print.pdf. Accessed February 11, 2008.
The year 2007 was rather calm, compared to the 3 previous years in regards to new vaccines and vaccine recommendations. Although no breakthrough vaccine products came onto the market in 2007, there were new recommendations and licensure for new age groups for existing vaccines and a recall of some lots of Hib vaccines.
Meningococcal vaccine
Recommendations on the use of the quadrivalent meningococcal conjugate vaccine (MCV4) have evolved since its licensure in 2005 for use in persons 11 to 55 years of age. The first set of recommendations focused on universal vaccination of preteens, aged 11 to 12, those entering high school who had not received the vaccine previously, and others at risk for meningococcal disease including college freshmen living in dormitories.1 The MCV4 was preferred to the older polysaccharide vaccine (MPSV4) which was recommended only for children aged 2 to 10 and adults over age 55 at increased risk.
In 2007, the CDC changed 2 of the 2005 recommendations:
- The first, in August, simplified the recommendations for teens, making MCV4 universally recommended for all those aged 11 to 18 at the earliest opportunity.2
- The second, in December, followed FDA approval for use of MCV4 in children aged 2 to 10 years. The CDC now recommends MCV4 as the preferred vaccine in this age group for those at risk (TABLE 1).3
TABLE 1
Populations at increased risk for meningococcal disease who should receive quadrivalent meningococcal conjugate vaccine
|
If someone at ongoing risk for meningococcal disease has been previously vaccinated with MPSV4, they should be revaccinated 3 years later with MCV4. It is not known if repeat doses of MCV4 will be needed, and if so, after what amount of time.
The MCV4 has been linked to Guillain-Barré syndrome (GBS), and a history of GBS is a precaution for its use. For those with a history of GBS who need protection against meningococcal infection, MPSV4 is an alternative.
Hepatitis A vaccine
Widespread use of inactivated hepatitis A vaccine (HAV), first licensed in 1995, has markedly reduced the incidence of hepatitis A infection (FIGURE). Recommendations for its use have been periodically revised; current recommendations include universal vaccination of all children at age 12 to 23 months, catch-up vaccination in older children in areas of high prevalence, and vaccination of those at increased risk for hepatitis A including travelers to endemic areas, users of illicit drugs and men who have sex with men.4
FIGURE
Reduction in incidence of hepatitis A infection
Source: Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2006; 55(RR-07).
For those unvaccinated who are acutely exposed to hepatitis A virus and those traveling to areas of high prevalence who do not have time to complete the 2 doses of HAV, the only prevention available until recently has been IG. This has now changed and HAV can be used in both groups. The new recommendation for postexposure prophylaxis is that either a single dose of HAV or use of IG is acceptable.5 At ages 12 months to 40 years, vaccine is preferred. For those over age 40, IG is preferred but vaccine is acceptable. For children less than 12 months, the immune suppressed, and those with chronic liver disease, IG should be used.
Those traveling or working in countries with high rates of hepatitis A can be protected with either HAV or IG. A single dose of HAV is sufficient for healthy people, with a second dose at the recommended interval to complete the series. Those under age 12 months, those who choose not to receive the vaccine, and those who are allergic to the vaccine should be offered IG. Both IG and HAV should be considered for individuals who plan to travel within 2 weeks of the first HAV dose; those over age 40, the immune compromised, and those with chronic liver disease or other chronic medical conditions.
Live attenuated influenza vaccine
FluMist, the live attenuated influenza vaccine (LAIV), which is administered as an intranasal spray, is now approved for use among those 2 to 4 years of age.6 Previously, the LAIV was approved only for healthy, non pregnant persons, 5 to 49 years of age. The LAIV may actually be the preferred product in children as it has been shown to prevent more influenza illness than the trivalent inactivated vaccine (TIV). The LAIV should not be used in anyone with a condition listed in TABLE 2 and should not be administered to children under age 5 who have recurrent wheezing.
FluMist has also been modified in several advantageous ways:
- The dose in the sprayer is now 0.2 mL (previously 0.5 mL). One half of the dose should be administered in each nostril.
- The product no longer has to be stored frozen; it should be kept at 35° to 46°F.
- When 2 doses are needed in children under age 9 being vaccinated for the first time, the interval between doses is now 4 weeks (previously 6 weeks).
TABLE 2
LAIV (FluMist) should not be used in these groups
|
Children under age 9 years who receive only 1 dose of vaccine (either TIV or LAIV) the first year they are vaccinated should receive 2 doses the next year.6 If they fail to receive 2 doses in the next year, only a single dose is recommended after that. This is a slight modification of the previous recommendation that only 1 dose was recommended in this situation.7
Alternative schedule for combined hepatitis A and B vaccine
The FDA approved an alternate, 4-dose schedule for the combined hepatitis A and hepatitis B vaccine (Twinrix): at 0, 7, 21 days, and 12 months.8 It was previously approved only for a 3-dose schedule: at 0, 1, and 6 months. The new alternative schedule allows greater protection for travelers who need to depart in less than a month’s time.
Merck recalls some lots of Hib vaccine
On December 11, 2007, Merck announced a voluntary recall of specific lots of Haemophilus influenza type b (Hib) conjugate vaccine products: 10 lots of a monovalent Hib vaccine, PedvaxHIB, and 2 lots of a combined hepatitis B/Hib vaccine, Comvax.
Consult Merck’s Web site for the lots involved and for instructions on returning vaccine (www.merckvaccines. com/PCHRecall.pdf). The recall was prompted by concern about equipment sterility, although no vaccine has been shown to be contaminated. Children vaccinated with Merck products do not need to be revaccinated or obtain any special follow-up.
Shortage expected. It is unknown when Merck will resume production, but it is not anticipated until at least late in 2008. Other Hib-containing products are produced by Sanofi Pasteur but the supply of these products will not make up for the expected shortage.
Interim recommendations. The recall resulted in interim recommendations from the CDC.9 These recommendations are complicated because the dosing schedule for Hib vaccine differs by the product and the age of receipt of first vaccine when children are not on schedule. TABLE 3 lists the Hib-containing products, the recommended primary series schedule, and booster dose.
TABLE 3
Hib products
| PRIMARY SERIES | BOOSTER | |||
|---|---|---|---|---|
| Merck Products | ||||
| PedvaxHIB | Monovalent Hib vaccine | 2, 4 months | 12–15 months* | |
| Comvax | Combined Hib/hepatitis B vaccine | 2, 4 months | 12–15 months* | |
| Sanofi Pasteur products | ||||
| ActHIB | Monovalent hib vaccine | 2, 4, 6 months | 12–15 months* | |
| TriHIBit | DTaP/Hib vaccine | Not licensed for this age group | 15–18 months* | |
| * Can follow a primary series of any product or serve as the only dose for a child up to 59 months, not previously immunized. | ||||
The main points are:
- Defer the booster dose at age 12 to 15 months until the shortage is resolved, except for high-risk children.
- High-risk children, who should continue to receive the booster at ages 12 to 15 months, include those with asplenia, sickle cell disease, HIV infection, and certain other immune deficiencies and cancers, and American Indian/Alaskan Native children.
- Physicians should keep track of children who have the booster deferred so they can be vaccinated when the supply improves.
- Non-recalled lots of PedvaxHIB and Comvax in the CDC stockpile will be prioritized to providers who care for predominantly American Indian/Alaskan Native children, who are at markedly in creased risk of Hib infection.
- If a child has received only 1 dose of PedvaxHIB or Comvax, their primary series can be completed with ActHIB, but 3 total doses are needed.
Children through age 59 months who are behind schedule should complete a primary series according to published recommendations.10 Physicians should call their local health department if they have any questions about what to do in a specific case.
The year 2007 was rather calm, compared to the 3 previous years in regards to new vaccines and vaccine recommendations. Although no breakthrough vaccine products came onto the market in 2007, there were new recommendations and licensure for new age groups for existing vaccines and a recall of some lots of Hib vaccines.
Meningococcal vaccine
Recommendations on the use of the quadrivalent meningococcal conjugate vaccine (MCV4) have evolved since its licensure in 2005 for use in persons 11 to 55 years of age. The first set of recommendations focused on universal vaccination of preteens, aged 11 to 12, those entering high school who had not received the vaccine previously, and others at risk for meningococcal disease including college freshmen living in dormitories.1 The MCV4 was preferred to the older polysaccharide vaccine (MPSV4) which was recommended only for children aged 2 to 10 and adults over age 55 at increased risk.
In 2007, the CDC changed 2 of the 2005 recommendations:
- The first, in August, simplified the recommendations for teens, making MCV4 universally recommended for all those aged 11 to 18 at the earliest opportunity.2
- The second, in December, followed FDA approval for use of MCV4 in children aged 2 to 10 years. The CDC now recommends MCV4 as the preferred vaccine in this age group for those at risk (TABLE 1).3
TABLE 1
Populations at increased risk for meningococcal disease who should receive quadrivalent meningococcal conjugate vaccine
|
If someone at ongoing risk for meningococcal disease has been previously vaccinated with MPSV4, they should be revaccinated 3 years later with MCV4. It is not known if repeat doses of MCV4 will be needed, and if so, after what amount of time.
The MCV4 has been linked to Guillain-Barré syndrome (GBS), and a history of GBS is a precaution for its use. For those with a history of GBS who need protection against meningococcal infection, MPSV4 is an alternative.
Hepatitis A vaccine
Widespread use of inactivated hepatitis A vaccine (HAV), first licensed in 1995, has markedly reduced the incidence of hepatitis A infection (FIGURE). Recommendations for its use have been periodically revised; current recommendations include universal vaccination of all children at age 12 to 23 months, catch-up vaccination in older children in areas of high prevalence, and vaccination of those at increased risk for hepatitis A including travelers to endemic areas, users of illicit drugs and men who have sex with men.4
FIGURE
Reduction in incidence of hepatitis A infection
Source: Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2006; 55(RR-07).
For those unvaccinated who are acutely exposed to hepatitis A virus and those traveling to areas of high prevalence who do not have time to complete the 2 doses of HAV, the only prevention available until recently has been IG. This has now changed and HAV can be used in both groups. The new recommendation for postexposure prophylaxis is that either a single dose of HAV or use of IG is acceptable.5 At ages 12 months to 40 years, vaccine is preferred. For those over age 40, IG is preferred but vaccine is acceptable. For children less than 12 months, the immune suppressed, and those with chronic liver disease, IG should be used.
Those traveling or working in countries with high rates of hepatitis A can be protected with either HAV or IG. A single dose of HAV is sufficient for healthy people, with a second dose at the recommended interval to complete the series. Those under age 12 months, those who choose not to receive the vaccine, and those who are allergic to the vaccine should be offered IG. Both IG and HAV should be considered for individuals who plan to travel within 2 weeks of the first HAV dose; those over age 40, the immune compromised, and those with chronic liver disease or other chronic medical conditions.
Live attenuated influenza vaccine
FluMist, the live attenuated influenza vaccine (LAIV), which is administered as an intranasal spray, is now approved for use among those 2 to 4 years of age.6 Previously, the LAIV was approved only for healthy, non pregnant persons, 5 to 49 years of age. The LAIV may actually be the preferred product in children as it has been shown to prevent more influenza illness than the trivalent inactivated vaccine (TIV). The LAIV should not be used in anyone with a condition listed in TABLE 2 and should not be administered to children under age 5 who have recurrent wheezing.
FluMist has also been modified in several advantageous ways:
- The dose in the sprayer is now 0.2 mL (previously 0.5 mL). One half of the dose should be administered in each nostril.
- The product no longer has to be stored frozen; it should be kept at 35° to 46°F.
- When 2 doses are needed in children under age 9 being vaccinated for the first time, the interval between doses is now 4 weeks (previously 6 weeks).
TABLE 2
LAIV (FluMist) should not be used in these groups
|
Children under age 9 years who receive only 1 dose of vaccine (either TIV or LAIV) the first year they are vaccinated should receive 2 doses the next year.6 If they fail to receive 2 doses in the next year, only a single dose is recommended after that. This is a slight modification of the previous recommendation that only 1 dose was recommended in this situation.7
Alternative schedule for combined hepatitis A and B vaccine
The FDA approved an alternate, 4-dose schedule for the combined hepatitis A and hepatitis B vaccine (Twinrix): at 0, 7, 21 days, and 12 months.8 It was previously approved only for a 3-dose schedule: at 0, 1, and 6 months. The new alternative schedule allows greater protection for travelers who need to depart in less than a month’s time.
Merck recalls some lots of Hib vaccine
On December 11, 2007, Merck announced a voluntary recall of specific lots of Haemophilus influenza type b (Hib) conjugate vaccine products: 10 lots of a monovalent Hib vaccine, PedvaxHIB, and 2 lots of a combined hepatitis B/Hib vaccine, Comvax.
Consult Merck’s Web site for the lots involved and for instructions on returning vaccine (www.merckvaccines. com/PCHRecall.pdf). The recall was prompted by concern about equipment sterility, although no vaccine has been shown to be contaminated. Children vaccinated with Merck products do not need to be revaccinated or obtain any special follow-up.
Shortage expected. It is unknown when Merck will resume production, but it is not anticipated until at least late in 2008. Other Hib-containing products are produced by Sanofi Pasteur but the supply of these products will not make up for the expected shortage.
Interim recommendations. The recall resulted in interim recommendations from the CDC.9 These recommendations are complicated because the dosing schedule for Hib vaccine differs by the product and the age of receipt of first vaccine when children are not on schedule. TABLE 3 lists the Hib-containing products, the recommended primary series schedule, and booster dose.
TABLE 3
Hib products
| PRIMARY SERIES | BOOSTER | |||
|---|---|---|---|---|
| Merck Products | ||||
| PedvaxHIB | Monovalent Hib vaccine | 2, 4 months | 12–15 months* | |
| Comvax | Combined Hib/hepatitis B vaccine | 2, 4 months | 12–15 months* | |
| Sanofi Pasteur products | ||||
| ActHIB | Monovalent hib vaccine | 2, 4, 6 months | 12–15 months* | |
| TriHIBit | DTaP/Hib vaccine | Not licensed for this age group | 15–18 months* | |
| * Can follow a primary series of any product or serve as the only dose for a child up to 59 months, not previously immunized. | ||||
The main points are:
- Defer the booster dose at age 12 to 15 months until the shortage is resolved, except for high-risk children.
- High-risk children, who should continue to receive the booster at ages 12 to 15 months, include those with asplenia, sickle cell disease, HIV infection, and certain other immune deficiencies and cancers, and American Indian/Alaskan Native children.
- Physicians should keep track of children who have the booster deferred so they can be vaccinated when the supply improves.
- Non-recalled lots of PedvaxHIB and Comvax in the CDC stockpile will be prioritized to providers who care for predominantly American Indian/Alaskan Native children, who are at markedly in creased risk of Hib infection.
- If a child has received only 1 dose of PedvaxHIB or Comvax, their primary series can be completed with ActHIB, but 3 total doses are needed.
Children through age 59 months who are behind schedule should complete a primary series according to published recommendations.10 Physicians should call their local health department if they have any questions about what to do in a specific case.
1. CDC. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005;54(RR-7):1-21.
2. CDC. Revised recommendations of the Advisory Committee on Immunization Practices to vaccinate all persons aged 11-18 years with meningococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep 2007;56:794-795.
3. CDC. Recommendation from the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MCV4) in children aged 2-10 years at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep 2007;56:1265-1266.
4. CDC. Update: prevention of hepatitis A after exposure to hepatitis A virus and in international travelers. Updated recommendations of the ACIP. MMWR Morb Mortal Wkly Rep 2007;56:1080-1084.
5. Advisory Committee on Immunization Practices (ACIP), Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006;55(RR-07):1-23.
6. CDC. Expansion of use of live attenuated influenza vaccine to children aged 2-4 years and other Flu-Mist changes for the 2007-2008 influenza season. MMWR Morb Mortal Wkly Rep 2007;56:1217-1219.
7. Fiore AE, Shay DK, Haber P, et al. Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep 2007;56(RR-6):1-54.
8. CDC. FDA approval of an alternate dosing schedule for a combined hepatitis A and B vaccine (Twinrix). MMWR Morb Mortal Wkly Rep 2007;56:1057.-
9. CDC. Interim recommendations for the use of Haemophilus influenza Type b (Hib) conjugate vaccines related to the recall of certain lots of Hib-containing vaccines (PedvaxHIB and Comvax). MMWR Morb Mortal Wkly Rep 2007;56:1318-1320.
10. CDC. Catch-up immunization schedule for persons aged 4 months-18 years who start late or are more than one month behind. Available at www.cdc.gov/vaccines/recs/schedules/downloads/child/2007/child-schedule-color-print.pdf. Accessed February 11, 2008.
1. CDC. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005;54(RR-7):1-21.
2. CDC. Revised recommendations of the Advisory Committee on Immunization Practices to vaccinate all persons aged 11-18 years with meningococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep 2007;56:794-795.
3. CDC. Recommendation from the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MCV4) in children aged 2-10 years at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep 2007;56:1265-1266.
4. CDC. Update: prevention of hepatitis A after exposure to hepatitis A virus and in international travelers. Updated recommendations of the ACIP. MMWR Morb Mortal Wkly Rep 2007;56:1080-1084.
5. Advisory Committee on Immunization Practices (ACIP), Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006;55(RR-07):1-23.
6. CDC. Expansion of use of live attenuated influenza vaccine to children aged 2-4 years and other Flu-Mist changes for the 2007-2008 influenza season. MMWR Morb Mortal Wkly Rep 2007;56:1217-1219.
7. Fiore AE, Shay DK, Haber P, et al. Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep 2007;56(RR-6):1-54.
8. CDC. FDA approval of an alternate dosing schedule for a combined hepatitis A and B vaccine (Twinrix). MMWR Morb Mortal Wkly Rep 2007;56:1057.-
9. CDC. Interim recommendations for the use of Haemophilus influenza Type b (Hib) conjugate vaccines related to the recall of certain lots of Hib-containing vaccines (PedvaxHIB and Comvax). MMWR Morb Mortal Wkly Rep 2007;56:1318-1320.
10. CDC. Catch-up immunization schedule for persons aged 4 months-18 years who start late or are more than one month behind. Available at www.cdc.gov/vaccines/recs/schedules/downloads/child/2007/child-schedule-color-print.pdf. Accessed February 11, 2008.
Getting patients to exercise more: A systematic review of underserved populations
- Use focused, brief (2–3 minute) physical activity counseling with patients (B).
- Have large-print, easy-to-understand program materials available to supplement your discussion (B). Provide patients with a simple written plan of their physical activity goals (B). Focus on a limited number of concepts to avoid information overload (B).
- Address patients’ financial and logistical barriers to participation and adherence (B).
- Encourage flexibility in patients’ choices for exercise, and incorporate cultural adaptations (such as preferences for music, dance, or group activities) where appropriate (B).
- Use trained support staff, preferably representing the community of interest, to promote physical activity in your patients (B).
Strength of recommendation (SOR)
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Fewer than half of all Americans get sufficient physical activity, defined as 30 minutes or more per day, at least 5 times per week.1 The need to increase physical activity applies particularly to underserved populations: they are even less likely to get enough physical activity, and are thus even more likely to suffer greater burden of disease.2,3
The purpose of this systematic review was to assess clinical trials of clinician-initiated counseling interventions for promoting physical activity in under-served populations. We define under-served populations as individuals from minority ethnic backgrounds (such as African Americans, Hispanics, and Asian Americans), or vulnerable populations such as people with low educational attainment, low income, lack of insurance, or those residing in rural communities.
Primary care interventions are linked to a change in habits
Primary care physicians can have a significant impact on their patients’ physical activity. Individuals with a regular primary care physician are more likely to report attempts to change their physical activity habits.4 However, underserved populations are more likely to have inconsistent access to medical care, which may contribute to their greater risk of conditions linked to inadequate physical activity, such as diabetes, hypertension, and obesity.
Only about 25% of patients in primary care settings report receiving any counseling on physical activity.5 Those who are middle-aged or have a baccalaureate degree or higher are more likely to report such advice; African Americans and foreign-born immigrants are less likely to report it.
A study by Taira et al6 examined the relationship between patient income and discussion of health risk behaviors. Low-income patients were more likely to be obese and smoke than high-income patients; however, physicians were less likely to discuss diet and exercise with low-income patients. Among all the patients with whom some discussion occurred in this study, low-income patients were much more likely to attempt to change behavior based on physician advice than were high-income patients.
Clinical trials within7,8 and outside the US9-11 support the potential value of physical activity counseling in primary care. In these studies, as little as 3 to 5 minutes of patient-clinician communication about physical activity was linked to short-term improvement in patients’ exercise habits. As few as 2 or 3 office visits over 6 months were associated with increases in patients’ physical activity levels up to 1 year later. Other features that contributed to their success included having a brief (<3 minutes) counseling component for clinicians, supplementing the counseling with a written exercise prescription, having follow-up contact, and tailoring the counseling to patients’ needs and concerns.
These results are promising for primary care clinicians, whose longitudinal relationships with their patients afford them repeated opportunities to intervene to promote physical activity.
Few studies have focused on the underserved
A review by Taylor et al2 of physical activity interventions in low-income, ethnic minority, or disabled populations identified 14 community-based studies, mostly with quasi-experimental “pre/post” study designs. Ten studies included ethnic minorities, but physical activity was documented in just 2 studies at baseline, and these 2 studies did not include any postintervention follow-up. None of the 10 interventions was conducted in a primary care setting.
Another recent review12 found that studies that were ethnically inclusive placed greater emphasis on involving communities and building coalitions right from study inception, and they tailored messages (and messengers) that were culturally specific. Several of these studies showed better outcomes among ethnic minority participants than the white participants they sampled.
Taken together, previous reviews have examined the effectiveness of primary care interventions for the general population,13,14 as well as community-based programs for underserved populations.2 However, little information exists about effective physical activity counseling strategies for underserved groups in primary care.
Methods
Looking for studies in underserved populations
We conducted a systematic review of the literature involving clinical trials in the US, looking for trials where counseling interventions are initiated by primary care clinicians, and that assessed behavioral change related to physical activity.
Inclusion criteria
TABLE 1 shows the inclusion criteria and search terms for the literature review. We searched Ovid, Medline, CINAHL, PsycINFO, PubMed, Cochrane, and HealthSTAR for studies published between 1966 and 2005. We also searched bibliographies of retrieved articles, and contacted experts in the field in an effort to obtain other relevant data.
The principal investigator (JKC) reviewed titles and abstracts of all potentially relevant articles to determine whether they met eligibility criteria. Studies that met the criteria were retrieved and abstracted.
Using these predefined criteria, data were extracted from each eligible article. Studies were also rated according to the Strength of Recommendation Taxonomy (SORT), because of its emphasis on patient-oriented outcomes and the quality, quantity, and consistency of evidence.15
TABLE 1
Inclusion criteria and search terms
| For inclusion, studies must have: | ||
| ||
| The key terms used for the literature search were: | ||
| ambulatory care | health communication | program evaluation |
| behavioral interventions | health promotion | socioeconomic factors |
| behavior therapy | intervention studies | underserved populations |
| body mass index | obesity | urban populations |
| community health | outpatient clinic | weight control |
| exercise | physical activity | weight loss |
| family physicians | poverty | weight management |
| health behavior change | primary health care | |
Results
6 of 8 studies report increases in physical activity
We reviewed a total of 253 titles and abstracts. Eight studies16-23 met our inclusion criteria. We were not able to locate any clinical trials that both 1) examined the effect of primary care clinician counseling on physical activity outcomes, and 2) had a study population focused on an underserved group. TABLE 2 (available at www.jfponline.com) shows the characteristics of these 8 studies.
Although we sought trials that defined “primary care clinician” as a professional—such as MD, nurse practitioner (NP), or physician assistant (PA)—who provides longitudinal primary health care, several of these studies considered dieticians, exercise physiologists, or health care workers as primary care clinicians.
Only 1 study20 examined physical activity counseling with an intervention that incorporated a follow-up visit by the primary care clinician, and looked at the long-term effect on physical activity as an outcome. Thus, the degree to which the clinician’s counseling influenced the physical activity outcome in these studies is unclear.
Identifying underserved groups
Information on race or ethnicity (which tended to be reported as a single variable), level of education, and income of participants was reported in the demographic data of all studies’ results, but relationships between these variables and physical activity outcomes were not consistently reported. One study23 stratified participants by race/ethnicity and health center; 2 studies16,21 reported analyses and findings for participants according to ethnicity, income, and educational level, as that was their focus.
Overall, however, it is not clear to what extent the interventions succeeded for various underserved groups, even if they were included as participants.
Study designs and the nature of exercise interventions
Seven16,18-23 of these studies (88%) were randomized controlled trials; the unit of randomization and control group varied. Trials were conducted at 1 or multiple (up to 11) primary care sites. Use of more than 1 method to recruit participants—such as mailings, use of office staff to promote/recruit, advertising, and community announcements—tended to be most effective.
Intervention types included phone and mail interventions,17-23 computer-based interventions,18,19,21 visits from a community health worker,22,23 group classes,16,22,23 directly supervised physical activity sessions,16,22,23 clinician counseling,16-23 and prescription protocols (eg, written, guided action plans).17-23 Those delivering the intervention varied, and included primary care physicians,17-23 nurse practitioners or physician assistants,17-19,23,23 nutritionists,16 exercise physiologists,16 community health educators,20,22,23 and other study personnel.19,21 Specific elements of interventions that were likely to contribute to patients’ success included addressing financial or environmental/safety issues for exercise,16 use of trained office staff to provide exercise counseling,18-20,23 and offering flexibility in choice by tailoring the goals and plans to the patients’ needs and interests.17-23
The “dose” of clinician counseling varied from very brief (1 to 3 minutes of direct contact on 1 occasion) to more extended (>5 minutes of direct counseling over repeated intervals). Duration of follow-up for the 8 studies ranged from 4 months to 2 years.
Several studies designed their interventions to make the clinician counseling brief,17-20,23 in order to enhance feasibility for busy primary care settings. Three studies16,21,22 described strategies they used for tailoring the intervention to a specific culture, or for addressing issues of literacy for the written materials. Two studies16,22 reported that their study staffs were ethnically or culturally representative of the targeted population.
The difficulty of maintaining adherence to physical activity
Three studies18,19,21 reported having difficulty with attrition among their minority participants; they did not, however, include information specific to minorities in their physical activity outcomes. Studies with highest retention rates (>80%) tended to specifically address barriers to participation, including cultural issues, or they used a “lead-in” period.16,20,21,23
The studies with the best adherence and retention among black and Hispanic participants, and those participants with low educational attainment,16,21 used baseline qualitative data regarding management of health behaviors when they designed their interventions. For example, 1 study16 mentioned cultural adaptations derived from prior qualitative work—such as using program materials that extensively depicted African American individuals, families, and community settings—and using language in the intervention reflecting social values and situations relevant to African Americans.
How exercise data were reported
Six of the 8 (75%) studies16,17,19,20,22,23 reported some improvement in short-term physical activity outcomes (TABLE 2, available at www.jfponline.com); however, there was considerable heterogeneity in how these studies measured physical activity outcomes. All 8 incorporated a self-report measure of physical activity, such as the Patient-centered Assessment and Counseling for Exercise (PACE),17-19 Paffenbarger Physical Activity Questionnaire (PPAQ),17 7-day Physical Activity Recall (PAR),17,20,21,23 and other self-report recall measures to assess physical activity. (A RESOURCE LIST of these instruments is available at www.jfponline.com.) Two studies also measured “states of change,”17,20 but these states were not consistently defined.
Three studies17,20,23 included objective measures of physical activity, such as accelerometers; in these studies, there was not substantial variance in physical activity outcomes between the objective and subjective measures.
Discussion
More study needed in the underserved
This review reflects in part the difficult task of designing and implementing realistic interventions for the underserved in primary care. However, interventions must be replicated in these populations before we can necessarily assume that findings from other trials are generalizable, due to issues of access, financial resources, health literacy, beliefs, cultural differences, self-efficacy, and other logistic barriers to traditional care that disproportionately affect underserved groups.
Integrate known personal, social, and environmental factors
Several studies24-26 have explored the social, demographic, and environmental factors associated with physical activity in minority populations. These studies shed light on the reasons why clinical trials that focus on white, affluent, educated populations might not be generalizable to underserved groups.
To be maximally effective, any interventions for promoting physical activity in the underserved need to find ways to address any cultural or financial barriers, and incorporate factors associated with success. For example, among African American and Hispanic women, having lower “social role strain,” higher attendance at religious services, and a greater feeling that one’s neighborhood was safe were all associated with increased likelihood of exercise.24-26 Such studies suggest that differences in beliefs, resources, self-efficacy, prior experience, and competing life demands can all contribute to promoting physical activity in some underserved groups. Practically, such findings encourage clinicians to work with patients to help them identify sources of social support and positive influences on their health, and help them articulate internal strengths and personal attributes to succeed in behavioral change.
Despite the variations in training or means of communication in the studies we identified, 2 studies used interventions that were successful at explicitly anticipated and addressed barriers to physical activity.16,21 These 2 studies also had interventionists who represented the communities of interest, and they used cultural adaptations to promote exercise where appropriate. Thus, limited data suggest that some primary care–based programs improve physical activity in underserved patients, but the effects of communication from the primary care clinician on physical activity is lacking, consistent with other work in the field.12,27
Promising strategies include office prompts, brief counseling
Primary care clinicians face many time pressures, fiscal constraints, administrative burdens, and competing priorities; these make addressing health promotion behaviors such as physical activity quite difficult. These issues are magnified for clinicians practicing in medically underserved areas. Despite these many challenges, promising opportunities do exist.
On a systems level, practice-based systems to manage chronic diseases have been successfully developed and implemented in the primary care setting; such systems can be tested to promote physical activity, as well. These practice-based approaches include patient registry data, office prompts, and other electronic systems to promote clinician counseling. For example, studies in this review using computer-based programs in primary care offices were feasible and effective.18,19,21
Bodenheimer28 has argued for a redesign of primary care systems to more effectively address chronic conditions rather than acute care needs. Several health care systems have successfully implemented the pillars of such a redesign imperative, and they have shown convincingly the promise of addressing competing priorities, physician competence and confidence, motivation, and durability in improving patient self-management.28
At the level of the clinician-patient relationship, data suggest that patient physical activity can be increased (at least in the short term) by counseling that:
- is brief (5 minutes or less)17-20,23
- is focused/goal-oriented17-23
- is molded to the patient’s specific health needs17-23
- is delivered over multiple contacts (whether it be office visits, telephone, or group sessions)17-23
- contains a written plan to achieve goals.17-23
We do not know what “dose-response” relationship exists for primary care clinician communication with patients over the long term, and what effect repeated counseling would have on long-term sustainability of physical activity levels. This is even less clear for underserved groups. It is also unknown to what extent collaborative links with community programs might increase physical activity when added to primary care–based counseling. Future research should evaluate the optimal “dose-response” to the interventions, the effect of repeated visits and continuity of care, and the effect of community-based referrals for physical activity programs for underserved populations in primary care.
Limitations of this review
Because our inclusion criteria were strict, we omitted potentially meaningful studies that were less directly relevant to our aims. For example, there has been substantial creative community-based work with underserved populations in the US to promote physical activity, and many innovations have been designed by researchers outside the US. Results from these programs and trials should be incorporated into primary care settings working with underserved populations.
Another limitation is that our definition of “underserved” is not the only possible definition. The most marginalized underserved groups with the least access to the health care system (such as the uninsured or homeless) were more likely to be omitted from our results, because we wanted to examine physical activity programs among patients in primary care settings.
Finally, this review did not address the need to understand the connection between sustained improvements in physical activity and patient-oriented health outcomes for underserved populations.
Conclusion
Information on exercise counseling interventions in primary care for the underserved is limited: these groups have not been included in the majority of clinical trials of physical activity thus far. Physical activity interventions need to be replicated in underserved populations before we can assume their results are generalizable. Though characteristics of existing studies show promise, future research on physical activity in underserved populations should assess the effect of practice-based systems on reducing barriers and promoting physical activity, the dose-response effect of clinician counseling on physical activity outcomes, and the effect of the physician-patient relationship and continuity of care on physical activity outcomes.
Funding
This study was supported by grant 1R25CA102618 from the National Cancer Institute.
Correspondence
Jennifer K. Carroll, MD, MPH, University of Rochester School of Medicine, Family Medicine Research Programs, 1381 South Avenue, Rochester, NY 14620; jennifer_carroll@urmc.rochester.edu
1. Centers for Disease Control and Prevention. Prevalence of physical activity, including lifestyle activities among adults—United States, 2000-2001. MMWR Morb Mortal Wkly Rep 2003;52:764-769.
2. Taylor WC, Baranowski T, Young DR. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med 1998;15:334-343.
3. Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Prev Med 2000;18:46-53.
4. Mainous AG, Diaz VA, Koopman RJ, Everett CJ. Having a regular physician and attempted weight loss after screening for hypertension or hypercholesterolemia. Int J Obes (Lond) 2005;29:223-227.
5. Honda K. Factors underlying variation in receipt of physician advice on diet and exercise: Applications of the behavioral model of health care utilization. Am J Health Promot 2004;18:370-377.
6. Taira DA, Safran DG, Seto TB, Rogers WH, Tarlov AR. The relationship between patient income and physician discussion of health risk behaviors. JAMA 1997;278:1412-1417.
7. Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services research Team. Prev Med 1995;24:492-497.
8. Norris SL, Grothaus LC, Buchner DM, Pratt M. Effectiveness of physician-based assessment and counseling for exercise in a staff model HMO. Prev Med 2000;30:513-523.
9. Swinburn BA, Walter LG, Arroll B, Tilyard MW, Russell DG. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health 1998;88:288-291.
10. Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ 1995;310:1099-1104.
11. Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns 1999;36:181-192.
12. Yancey AK, Kumanyika SK, Ponce NA, McCarthy WM, Fielding JE. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chron Dis 2004;1:1-18.
13. Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2002;137:208-215.
14. Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract 2000;49:158-168.
15. Ebell Mh, Siwek J, Weiss BD, et al. Simplifying the language of evidence to improve patient care: Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. J Fam Pract 2004;53:111-120.
16. Agurs-Collins TD, Kumanyika SK, Ten Have TR, Adams-Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997;20:1503-1511.
17. Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med 1996;25:225-233.
18. Calfas KJ, Sallis JF, Zabinski MF, et al. Preliminary evaluation of a multi-component program for nutrition and physical activity change in primary care: PACE+ for adults. Prev Med 2002;34:153-161.
19. Patrick K, Sallis JF, Prochaska JJ, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med 2001;155:940-946.
20. Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med 2005;29:247-255.
21. Staten LK, Gregory-Mercado KY, Ranger-Moore J, et al. Provider counseling, health education, and community health workers: The arizona WISEWOMAN project. J Womens Health (Larchmt) 2004;13:547-556.
22. Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obesity Res 2002;10:22-32.
23. Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The activity counseling Trial: A randomized controlled trial. JAMA 2001;286:677-687.
24. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern Latinas. Am J Prev Med 2003;25:69-76.
25. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern African-American women. Am J Prev Med 2003;25:45-52.
26. Rohm YD, Voorhees CC. Personal, social, and environmental correlates of physical activity in urban african-american women. Am J Prev Med 2003;25:38-44.
27. Yancey AK. Building capacity to prevent and control chronic disease in underserved communities: Expanding the wisdom of WISEWOMAN in intervening at the environmental level. J Womens Health (Larchmt) 2004;13:644-649.
28. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, Part 2. JAMA 2002;288:1909-1914.
- Use focused, brief (2–3 minute) physical activity counseling with patients (B).
- Have large-print, easy-to-understand program materials available to supplement your discussion (B). Provide patients with a simple written plan of their physical activity goals (B). Focus on a limited number of concepts to avoid information overload (B).
- Address patients’ financial and logistical barriers to participation and adherence (B).
- Encourage flexibility in patients’ choices for exercise, and incorporate cultural adaptations (such as preferences for music, dance, or group activities) where appropriate (B).
- Use trained support staff, preferably representing the community of interest, to promote physical activity in your patients (B).
Strength of recommendation (SOR)
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Fewer than half of all Americans get sufficient physical activity, defined as 30 minutes or more per day, at least 5 times per week.1 The need to increase physical activity applies particularly to underserved populations: they are even less likely to get enough physical activity, and are thus even more likely to suffer greater burden of disease.2,3
The purpose of this systematic review was to assess clinical trials of clinician-initiated counseling interventions for promoting physical activity in under-served populations. We define under-served populations as individuals from minority ethnic backgrounds (such as African Americans, Hispanics, and Asian Americans), or vulnerable populations such as people with low educational attainment, low income, lack of insurance, or those residing in rural communities.
Primary care interventions are linked to a change in habits
Primary care physicians can have a significant impact on their patients’ physical activity. Individuals with a regular primary care physician are more likely to report attempts to change their physical activity habits.4 However, underserved populations are more likely to have inconsistent access to medical care, which may contribute to their greater risk of conditions linked to inadequate physical activity, such as diabetes, hypertension, and obesity.
Only about 25% of patients in primary care settings report receiving any counseling on physical activity.5 Those who are middle-aged or have a baccalaureate degree or higher are more likely to report such advice; African Americans and foreign-born immigrants are less likely to report it.
A study by Taira et al6 examined the relationship between patient income and discussion of health risk behaviors. Low-income patients were more likely to be obese and smoke than high-income patients; however, physicians were less likely to discuss diet and exercise with low-income patients. Among all the patients with whom some discussion occurred in this study, low-income patients were much more likely to attempt to change behavior based on physician advice than were high-income patients.
Clinical trials within7,8 and outside the US9-11 support the potential value of physical activity counseling in primary care. In these studies, as little as 3 to 5 minutes of patient-clinician communication about physical activity was linked to short-term improvement in patients’ exercise habits. As few as 2 or 3 office visits over 6 months were associated with increases in patients’ physical activity levels up to 1 year later. Other features that contributed to their success included having a brief (<3 minutes) counseling component for clinicians, supplementing the counseling with a written exercise prescription, having follow-up contact, and tailoring the counseling to patients’ needs and concerns.
These results are promising for primary care clinicians, whose longitudinal relationships with their patients afford them repeated opportunities to intervene to promote physical activity.
Few studies have focused on the underserved
A review by Taylor et al2 of physical activity interventions in low-income, ethnic minority, or disabled populations identified 14 community-based studies, mostly with quasi-experimental “pre/post” study designs. Ten studies included ethnic minorities, but physical activity was documented in just 2 studies at baseline, and these 2 studies did not include any postintervention follow-up. None of the 10 interventions was conducted in a primary care setting.
Another recent review12 found that studies that were ethnically inclusive placed greater emphasis on involving communities and building coalitions right from study inception, and they tailored messages (and messengers) that were culturally specific. Several of these studies showed better outcomes among ethnic minority participants than the white participants they sampled.
Taken together, previous reviews have examined the effectiveness of primary care interventions for the general population,13,14 as well as community-based programs for underserved populations.2 However, little information exists about effective physical activity counseling strategies for underserved groups in primary care.
Methods
Looking for studies in underserved populations
We conducted a systematic review of the literature involving clinical trials in the US, looking for trials where counseling interventions are initiated by primary care clinicians, and that assessed behavioral change related to physical activity.
Inclusion criteria
TABLE 1 shows the inclusion criteria and search terms for the literature review. We searched Ovid, Medline, CINAHL, PsycINFO, PubMed, Cochrane, and HealthSTAR for studies published between 1966 and 2005. We also searched bibliographies of retrieved articles, and contacted experts in the field in an effort to obtain other relevant data.
The principal investigator (JKC) reviewed titles and abstracts of all potentially relevant articles to determine whether they met eligibility criteria. Studies that met the criteria were retrieved and abstracted.
Using these predefined criteria, data were extracted from each eligible article. Studies were also rated according to the Strength of Recommendation Taxonomy (SORT), because of its emphasis on patient-oriented outcomes and the quality, quantity, and consistency of evidence.15
TABLE 1
Inclusion criteria and search terms
| For inclusion, studies must have: | ||
| ||
| The key terms used for the literature search were: | ||
| ambulatory care | health communication | program evaluation |
| behavioral interventions | health promotion | socioeconomic factors |
| behavior therapy | intervention studies | underserved populations |
| body mass index | obesity | urban populations |
| community health | outpatient clinic | weight control |
| exercise | physical activity | weight loss |
| family physicians | poverty | weight management |
| health behavior change | primary health care | |
Results
6 of 8 studies report increases in physical activity
We reviewed a total of 253 titles and abstracts. Eight studies16-23 met our inclusion criteria. We were not able to locate any clinical trials that both 1) examined the effect of primary care clinician counseling on physical activity outcomes, and 2) had a study population focused on an underserved group. TABLE 2 (available at www.jfponline.com) shows the characteristics of these 8 studies.
Although we sought trials that defined “primary care clinician” as a professional—such as MD, nurse practitioner (NP), or physician assistant (PA)—who provides longitudinal primary health care, several of these studies considered dieticians, exercise physiologists, or health care workers as primary care clinicians.
Only 1 study20 examined physical activity counseling with an intervention that incorporated a follow-up visit by the primary care clinician, and looked at the long-term effect on physical activity as an outcome. Thus, the degree to which the clinician’s counseling influenced the physical activity outcome in these studies is unclear.
Identifying underserved groups
Information on race or ethnicity (which tended to be reported as a single variable), level of education, and income of participants was reported in the demographic data of all studies’ results, but relationships between these variables and physical activity outcomes were not consistently reported. One study23 stratified participants by race/ethnicity and health center; 2 studies16,21 reported analyses and findings for participants according to ethnicity, income, and educational level, as that was their focus.
Overall, however, it is not clear to what extent the interventions succeeded for various underserved groups, even if they were included as participants.
Study designs and the nature of exercise interventions
Seven16,18-23 of these studies (88%) were randomized controlled trials; the unit of randomization and control group varied. Trials were conducted at 1 or multiple (up to 11) primary care sites. Use of more than 1 method to recruit participants—such as mailings, use of office staff to promote/recruit, advertising, and community announcements—tended to be most effective.
Intervention types included phone and mail interventions,17-23 computer-based interventions,18,19,21 visits from a community health worker,22,23 group classes,16,22,23 directly supervised physical activity sessions,16,22,23 clinician counseling,16-23 and prescription protocols (eg, written, guided action plans).17-23 Those delivering the intervention varied, and included primary care physicians,17-23 nurse practitioners or physician assistants,17-19,23,23 nutritionists,16 exercise physiologists,16 community health educators,20,22,23 and other study personnel.19,21 Specific elements of interventions that were likely to contribute to patients’ success included addressing financial or environmental/safety issues for exercise,16 use of trained office staff to provide exercise counseling,18-20,23 and offering flexibility in choice by tailoring the goals and plans to the patients’ needs and interests.17-23
The “dose” of clinician counseling varied from very brief (1 to 3 minutes of direct contact on 1 occasion) to more extended (>5 minutes of direct counseling over repeated intervals). Duration of follow-up for the 8 studies ranged from 4 months to 2 years.
Several studies designed their interventions to make the clinician counseling brief,17-20,23 in order to enhance feasibility for busy primary care settings. Three studies16,21,22 described strategies they used for tailoring the intervention to a specific culture, or for addressing issues of literacy for the written materials. Two studies16,22 reported that their study staffs were ethnically or culturally representative of the targeted population.
The difficulty of maintaining adherence to physical activity
Three studies18,19,21 reported having difficulty with attrition among their minority participants; they did not, however, include information specific to minorities in their physical activity outcomes. Studies with highest retention rates (>80%) tended to specifically address barriers to participation, including cultural issues, or they used a “lead-in” period.16,20,21,23
The studies with the best adherence and retention among black and Hispanic participants, and those participants with low educational attainment,16,21 used baseline qualitative data regarding management of health behaviors when they designed their interventions. For example, 1 study16 mentioned cultural adaptations derived from prior qualitative work—such as using program materials that extensively depicted African American individuals, families, and community settings—and using language in the intervention reflecting social values and situations relevant to African Americans.
How exercise data were reported
Six of the 8 (75%) studies16,17,19,20,22,23 reported some improvement in short-term physical activity outcomes (TABLE 2, available at www.jfponline.com); however, there was considerable heterogeneity in how these studies measured physical activity outcomes. All 8 incorporated a self-report measure of physical activity, such as the Patient-centered Assessment and Counseling for Exercise (PACE),17-19 Paffenbarger Physical Activity Questionnaire (PPAQ),17 7-day Physical Activity Recall (PAR),17,20,21,23 and other self-report recall measures to assess physical activity. (A RESOURCE LIST of these instruments is available at www.jfponline.com.) Two studies also measured “states of change,”17,20 but these states were not consistently defined.
Three studies17,20,23 included objective measures of physical activity, such as accelerometers; in these studies, there was not substantial variance in physical activity outcomes between the objective and subjective measures.
Discussion
More study needed in the underserved
This review reflects in part the difficult task of designing and implementing realistic interventions for the underserved in primary care. However, interventions must be replicated in these populations before we can necessarily assume that findings from other trials are generalizable, due to issues of access, financial resources, health literacy, beliefs, cultural differences, self-efficacy, and other logistic barriers to traditional care that disproportionately affect underserved groups.
Integrate known personal, social, and environmental factors
Several studies24-26 have explored the social, demographic, and environmental factors associated with physical activity in minority populations. These studies shed light on the reasons why clinical trials that focus on white, affluent, educated populations might not be generalizable to underserved groups.
To be maximally effective, any interventions for promoting physical activity in the underserved need to find ways to address any cultural or financial barriers, and incorporate factors associated with success. For example, among African American and Hispanic women, having lower “social role strain,” higher attendance at religious services, and a greater feeling that one’s neighborhood was safe were all associated with increased likelihood of exercise.24-26 Such studies suggest that differences in beliefs, resources, self-efficacy, prior experience, and competing life demands can all contribute to promoting physical activity in some underserved groups. Practically, such findings encourage clinicians to work with patients to help them identify sources of social support and positive influences on their health, and help them articulate internal strengths and personal attributes to succeed in behavioral change.
Despite the variations in training or means of communication in the studies we identified, 2 studies used interventions that were successful at explicitly anticipated and addressed barriers to physical activity.16,21 These 2 studies also had interventionists who represented the communities of interest, and they used cultural adaptations to promote exercise where appropriate. Thus, limited data suggest that some primary care–based programs improve physical activity in underserved patients, but the effects of communication from the primary care clinician on physical activity is lacking, consistent with other work in the field.12,27
Promising strategies include office prompts, brief counseling
Primary care clinicians face many time pressures, fiscal constraints, administrative burdens, and competing priorities; these make addressing health promotion behaviors such as physical activity quite difficult. These issues are magnified for clinicians practicing in medically underserved areas. Despite these many challenges, promising opportunities do exist.
On a systems level, practice-based systems to manage chronic diseases have been successfully developed and implemented in the primary care setting; such systems can be tested to promote physical activity, as well. These practice-based approaches include patient registry data, office prompts, and other electronic systems to promote clinician counseling. For example, studies in this review using computer-based programs in primary care offices were feasible and effective.18,19,21
Bodenheimer28 has argued for a redesign of primary care systems to more effectively address chronic conditions rather than acute care needs. Several health care systems have successfully implemented the pillars of such a redesign imperative, and they have shown convincingly the promise of addressing competing priorities, physician competence and confidence, motivation, and durability in improving patient self-management.28
At the level of the clinician-patient relationship, data suggest that patient physical activity can be increased (at least in the short term) by counseling that:
- is brief (5 minutes or less)17-20,23
- is focused/goal-oriented17-23
- is molded to the patient’s specific health needs17-23
- is delivered over multiple contacts (whether it be office visits, telephone, or group sessions)17-23
- contains a written plan to achieve goals.17-23
We do not know what “dose-response” relationship exists for primary care clinician communication with patients over the long term, and what effect repeated counseling would have on long-term sustainability of physical activity levels. This is even less clear for underserved groups. It is also unknown to what extent collaborative links with community programs might increase physical activity when added to primary care–based counseling. Future research should evaluate the optimal “dose-response” to the interventions, the effect of repeated visits and continuity of care, and the effect of community-based referrals for physical activity programs for underserved populations in primary care.
Limitations of this review
Because our inclusion criteria were strict, we omitted potentially meaningful studies that were less directly relevant to our aims. For example, there has been substantial creative community-based work with underserved populations in the US to promote physical activity, and many innovations have been designed by researchers outside the US. Results from these programs and trials should be incorporated into primary care settings working with underserved populations.
Another limitation is that our definition of “underserved” is not the only possible definition. The most marginalized underserved groups with the least access to the health care system (such as the uninsured or homeless) were more likely to be omitted from our results, because we wanted to examine physical activity programs among patients in primary care settings.
Finally, this review did not address the need to understand the connection between sustained improvements in physical activity and patient-oriented health outcomes for underserved populations.
Conclusion
Information on exercise counseling interventions in primary care for the underserved is limited: these groups have not been included in the majority of clinical trials of physical activity thus far. Physical activity interventions need to be replicated in underserved populations before we can assume their results are generalizable. Though characteristics of existing studies show promise, future research on physical activity in underserved populations should assess the effect of practice-based systems on reducing barriers and promoting physical activity, the dose-response effect of clinician counseling on physical activity outcomes, and the effect of the physician-patient relationship and continuity of care on physical activity outcomes.
Funding
This study was supported by grant 1R25CA102618 from the National Cancer Institute.
Correspondence
Jennifer K. Carroll, MD, MPH, University of Rochester School of Medicine, Family Medicine Research Programs, 1381 South Avenue, Rochester, NY 14620; jennifer_carroll@urmc.rochester.edu
- Use focused, brief (2–3 minute) physical activity counseling with patients (B).
- Have large-print, easy-to-understand program materials available to supplement your discussion (B). Provide patients with a simple written plan of their physical activity goals (B). Focus on a limited number of concepts to avoid information overload (B).
- Address patients’ financial and logistical barriers to participation and adherence (B).
- Encourage flexibility in patients’ choices for exercise, and incorporate cultural adaptations (such as preferences for music, dance, or group activities) where appropriate (B).
- Use trained support staff, preferably representing the community of interest, to promote physical activity in your patients (B).
Strength of recommendation (SOR)
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Fewer than half of all Americans get sufficient physical activity, defined as 30 minutes or more per day, at least 5 times per week.1 The need to increase physical activity applies particularly to underserved populations: they are even less likely to get enough physical activity, and are thus even more likely to suffer greater burden of disease.2,3
The purpose of this systematic review was to assess clinical trials of clinician-initiated counseling interventions for promoting physical activity in under-served populations. We define under-served populations as individuals from minority ethnic backgrounds (such as African Americans, Hispanics, and Asian Americans), or vulnerable populations such as people with low educational attainment, low income, lack of insurance, or those residing in rural communities.
Primary care interventions are linked to a change in habits
Primary care physicians can have a significant impact on their patients’ physical activity. Individuals with a regular primary care physician are more likely to report attempts to change their physical activity habits.4 However, underserved populations are more likely to have inconsistent access to medical care, which may contribute to their greater risk of conditions linked to inadequate physical activity, such as diabetes, hypertension, and obesity.
Only about 25% of patients in primary care settings report receiving any counseling on physical activity.5 Those who are middle-aged or have a baccalaureate degree or higher are more likely to report such advice; African Americans and foreign-born immigrants are less likely to report it.
A study by Taira et al6 examined the relationship between patient income and discussion of health risk behaviors. Low-income patients were more likely to be obese and smoke than high-income patients; however, physicians were less likely to discuss diet and exercise with low-income patients. Among all the patients with whom some discussion occurred in this study, low-income patients were much more likely to attempt to change behavior based on physician advice than were high-income patients.
Clinical trials within7,8 and outside the US9-11 support the potential value of physical activity counseling in primary care. In these studies, as little as 3 to 5 minutes of patient-clinician communication about physical activity was linked to short-term improvement in patients’ exercise habits. As few as 2 or 3 office visits over 6 months were associated with increases in patients’ physical activity levels up to 1 year later. Other features that contributed to their success included having a brief (<3 minutes) counseling component for clinicians, supplementing the counseling with a written exercise prescription, having follow-up contact, and tailoring the counseling to patients’ needs and concerns.
These results are promising for primary care clinicians, whose longitudinal relationships with their patients afford them repeated opportunities to intervene to promote physical activity.
Few studies have focused on the underserved
A review by Taylor et al2 of physical activity interventions in low-income, ethnic minority, or disabled populations identified 14 community-based studies, mostly with quasi-experimental “pre/post” study designs. Ten studies included ethnic minorities, but physical activity was documented in just 2 studies at baseline, and these 2 studies did not include any postintervention follow-up. None of the 10 interventions was conducted in a primary care setting.
Another recent review12 found that studies that were ethnically inclusive placed greater emphasis on involving communities and building coalitions right from study inception, and they tailored messages (and messengers) that were culturally specific. Several of these studies showed better outcomes among ethnic minority participants than the white participants they sampled.
Taken together, previous reviews have examined the effectiveness of primary care interventions for the general population,13,14 as well as community-based programs for underserved populations.2 However, little information exists about effective physical activity counseling strategies for underserved groups in primary care.
Methods
Looking for studies in underserved populations
We conducted a systematic review of the literature involving clinical trials in the US, looking for trials where counseling interventions are initiated by primary care clinicians, and that assessed behavioral change related to physical activity.
Inclusion criteria
TABLE 1 shows the inclusion criteria and search terms for the literature review. We searched Ovid, Medline, CINAHL, PsycINFO, PubMed, Cochrane, and HealthSTAR for studies published between 1966 and 2005. We also searched bibliographies of retrieved articles, and contacted experts in the field in an effort to obtain other relevant data.
The principal investigator (JKC) reviewed titles and abstracts of all potentially relevant articles to determine whether they met eligibility criteria. Studies that met the criteria were retrieved and abstracted.
Using these predefined criteria, data were extracted from each eligible article. Studies were also rated according to the Strength of Recommendation Taxonomy (SORT), because of its emphasis on patient-oriented outcomes and the quality, quantity, and consistency of evidence.15
TABLE 1
Inclusion criteria and search terms
| For inclusion, studies must have: | ||
| ||
| The key terms used for the literature search were: | ||
| ambulatory care | health communication | program evaluation |
| behavioral interventions | health promotion | socioeconomic factors |
| behavior therapy | intervention studies | underserved populations |
| body mass index | obesity | urban populations |
| community health | outpatient clinic | weight control |
| exercise | physical activity | weight loss |
| family physicians | poverty | weight management |
| health behavior change | primary health care | |
Results
6 of 8 studies report increases in physical activity
We reviewed a total of 253 titles and abstracts. Eight studies16-23 met our inclusion criteria. We were not able to locate any clinical trials that both 1) examined the effect of primary care clinician counseling on physical activity outcomes, and 2) had a study population focused on an underserved group. TABLE 2 (available at www.jfponline.com) shows the characteristics of these 8 studies.
Although we sought trials that defined “primary care clinician” as a professional—such as MD, nurse practitioner (NP), or physician assistant (PA)—who provides longitudinal primary health care, several of these studies considered dieticians, exercise physiologists, or health care workers as primary care clinicians.
Only 1 study20 examined physical activity counseling with an intervention that incorporated a follow-up visit by the primary care clinician, and looked at the long-term effect on physical activity as an outcome. Thus, the degree to which the clinician’s counseling influenced the physical activity outcome in these studies is unclear.
Identifying underserved groups
Information on race or ethnicity (which tended to be reported as a single variable), level of education, and income of participants was reported in the demographic data of all studies’ results, but relationships between these variables and physical activity outcomes were not consistently reported. One study23 stratified participants by race/ethnicity and health center; 2 studies16,21 reported analyses and findings for participants according to ethnicity, income, and educational level, as that was their focus.
Overall, however, it is not clear to what extent the interventions succeeded for various underserved groups, even if they were included as participants.
Study designs and the nature of exercise interventions
Seven16,18-23 of these studies (88%) were randomized controlled trials; the unit of randomization and control group varied. Trials were conducted at 1 or multiple (up to 11) primary care sites. Use of more than 1 method to recruit participants—such as mailings, use of office staff to promote/recruit, advertising, and community announcements—tended to be most effective.
Intervention types included phone and mail interventions,17-23 computer-based interventions,18,19,21 visits from a community health worker,22,23 group classes,16,22,23 directly supervised physical activity sessions,16,22,23 clinician counseling,16-23 and prescription protocols (eg, written, guided action plans).17-23 Those delivering the intervention varied, and included primary care physicians,17-23 nurse practitioners or physician assistants,17-19,23,23 nutritionists,16 exercise physiologists,16 community health educators,20,22,23 and other study personnel.19,21 Specific elements of interventions that were likely to contribute to patients’ success included addressing financial or environmental/safety issues for exercise,16 use of trained office staff to provide exercise counseling,18-20,23 and offering flexibility in choice by tailoring the goals and plans to the patients’ needs and interests.17-23
The “dose” of clinician counseling varied from very brief (1 to 3 minutes of direct contact on 1 occasion) to more extended (>5 minutes of direct counseling over repeated intervals). Duration of follow-up for the 8 studies ranged from 4 months to 2 years.
Several studies designed their interventions to make the clinician counseling brief,17-20,23 in order to enhance feasibility for busy primary care settings. Three studies16,21,22 described strategies they used for tailoring the intervention to a specific culture, or for addressing issues of literacy for the written materials. Two studies16,22 reported that their study staffs were ethnically or culturally representative of the targeted population.
The difficulty of maintaining adherence to physical activity
Three studies18,19,21 reported having difficulty with attrition among their minority participants; they did not, however, include information specific to minorities in their physical activity outcomes. Studies with highest retention rates (>80%) tended to specifically address barriers to participation, including cultural issues, or they used a “lead-in” period.16,20,21,23
The studies with the best adherence and retention among black and Hispanic participants, and those participants with low educational attainment,16,21 used baseline qualitative data regarding management of health behaviors when they designed their interventions. For example, 1 study16 mentioned cultural adaptations derived from prior qualitative work—such as using program materials that extensively depicted African American individuals, families, and community settings—and using language in the intervention reflecting social values and situations relevant to African Americans.
How exercise data were reported
Six of the 8 (75%) studies16,17,19,20,22,23 reported some improvement in short-term physical activity outcomes (TABLE 2, available at www.jfponline.com); however, there was considerable heterogeneity in how these studies measured physical activity outcomes. All 8 incorporated a self-report measure of physical activity, such as the Patient-centered Assessment and Counseling for Exercise (PACE),17-19 Paffenbarger Physical Activity Questionnaire (PPAQ),17 7-day Physical Activity Recall (PAR),17,20,21,23 and other self-report recall measures to assess physical activity. (A RESOURCE LIST of these instruments is available at www.jfponline.com.) Two studies also measured “states of change,”17,20 but these states were not consistently defined.
Three studies17,20,23 included objective measures of physical activity, such as accelerometers; in these studies, there was not substantial variance in physical activity outcomes between the objective and subjective measures.
Discussion
More study needed in the underserved
This review reflects in part the difficult task of designing and implementing realistic interventions for the underserved in primary care. However, interventions must be replicated in these populations before we can necessarily assume that findings from other trials are generalizable, due to issues of access, financial resources, health literacy, beliefs, cultural differences, self-efficacy, and other logistic barriers to traditional care that disproportionately affect underserved groups.
Integrate known personal, social, and environmental factors
Several studies24-26 have explored the social, demographic, and environmental factors associated with physical activity in minority populations. These studies shed light on the reasons why clinical trials that focus on white, affluent, educated populations might not be generalizable to underserved groups.
To be maximally effective, any interventions for promoting physical activity in the underserved need to find ways to address any cultural or financial barriers, and incorporate factors associated with success. For example, among African American and Hispanic women, having lower “social role strain,” higher attendance at religious services, and a greater feeling that one’s neighborhood was safe were all associated with increased likelihood of exercise.24-26 Such studies suggest that differences in beliefs, resources, self-efficacy, prior experience, and competing life demands can all contribute to promoting physical activity in some underserved groups. Practically, such findings encourage clinicians to work with patients to help them identify sources of social support and positive influences on their health, and help them articulate internal strengths and personal attributes to succeed in behavioral change.
Despite the variations in training or means of communication in the studies we identified, 2 studies used interventions that were successful at explicitly anticipated and addressed barriers to physical activity.16,21 These 2 studies also had interventionists who represented the communities of interest, and they used cultural adaptations to promote exercise where appropriate. Thus, limited data suggest that some primary care–based programs improve physical activity in underserved patients, but the effects of communication from the primary care clinician on physical activity is lacking, consistent with other work in the field.12,27
Promising strategies include office prompts, brief counseling
Primary care clinicians face many time pressures, fiscal constraints, administrative burdens, and competing priorities; these make addressing health promotion behaviors such as physical activity quite difficult. These issues are magnified for clinicians practicing in medically underserved areas. Despite these many challenges, promising opportunities do exist.
On a systems level, practice-based systems to manage chronic diseases have been successfully developed and implemented in the primary care setting; such systems can be tested to promote physical activity, as well. These practice-based approaches include patient registry data, office prompts, and other electronic systems to promote clinician counseling. For example, studies in this review using computer-based programs in primary care offices were feasible and effective.18,19,21
Bodenheimer28 has argued for a redesign of primary care systems to more effectively address chronic conditions rather than acute care needs. Several health care systems have successfully implemented the pillars of such a redesign imperative, and they have shown convincingly the promise of addressing competing priorities, physician competence and confidence, motivation, and durability in improving patient self-management.28
At the level of the clinician-patient relationship, data suggest that patient physical activity can be increased (at least in the short term) by counseling that:
- is brief (5 minutes or less)17-20,23
- is focused/goal-oriented17-23
- is molded to the patient’s specific health needs17-23
- is delivered over multiple contacts (whether it be office visits, telephone, or group sessions)17-23
- contains a written plan to achieve goals.17-23
We do not know what “dose-response” relationship exists for primary care clinician communication with patients over the long term, and what effect repeated counseling would have on long-term sustainability of physical activity levels. This is even less clear for underserved groups. It is also unknown to what extent collaborative links with community programs might increase physical activity when added to primary care–based counseling. Future research should evaluate the optimal “dose-response” to the interventions, the effect of repeated visits and continuity of care, and the effect of community-based referrals for physical activity programs for underserved populations in primary care.
Limitations of this review
Because our inclusion criteria were strict, we omitted potentially meaningful studies that were less directly relevant to our aims. For example, there has been substantial creative community-based work with underserved populations in the US to promote physical activity, and many innovations have been designed by researchers outside the US. Results from these programs and trials should be incorporated into primary care settings working with underserved populations.
Another limitation is that our definition of “underserved” is not the only possible definition. The most marginalized underserved groups with the least access to the health care system (such as the uninsured or homeless) were more likely to be omitted from our results, because we wanted to examine physical activity programs among patients in primary care settings.
Finally, this review did not address the need to understand the connection between sustained improvements in physical activity and patient-oriented health outcomes for underserved populations.
Conclusion
Information on exercise counseling interventions in primary care for the underserved is limited: these groups have not been included in the majority of clinical trials of physical activity thus far. Physical activity interventions need to be replicated in underserved populations before we can assume their results are generalizable. Though characteristics of existing studies show promise, future research on physical activity in underserved populations should assess the effect of practice-based systems on reducing barriers and promoting physical activity, the dose-response effect of clinician counseling on physical activity outcomes, and the effect of the physician-patient relationship and continuity of care on physical activity outcomes.
Funding
This study was supported by grant 1R25CA102618 from the National Cancer Institute.
Correspondence
Jennifer K. Carroll, MD, MPH, University of Rochester School of Medicine, Family Medicine Research Programs, 1381 South Avenue, Rochester, NY 14620; jennifer_carroll@urmc.rochester.edu
1. Centers for Disease Control and Prevention. Prevalence of physical activity, including lifestyle activities among adults—United States, 2000-2001. MMWR Morb Mortal Wkly Rep 2003;52:764-769.
2. Taylor WC, Baranowski T, Young DR. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med 1998;15:334-343.
3. Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Prev Med 2000;18:46-53.
4. Mainous AG, Diaz VA, Koopman RJ, Everett CJ. Having a regular physician and attempted weight loss after screening for hypertension or hypercholesterolemia. Int J Obes (Lond) 2005;29:223-227.
5. Honda K. Factors underlying variation in receipt of physician advice on diet and exercise: Applications of the behavioral model of health care utilization. Am J Health Promot 2004;18:370-377.
6. Taira DA, Safran DG, Seto TB, Rogers WH, Tarlov AR. The relationship between patient income and physician discussion of health risk behaviors. JAMA 1997;278:1412-1417.
7. Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services research Team. Prev Med 1995;24:492-497.
8. Norris SL, Grothaus LC, Buchner DM, Pratt M. Effectiveness of physician-based assessment and counseling for exercise in a staff model HMO. Prev Med 2000;30:513-523.
9. Swinburn BA, Walter LG, Arroll B, Tilyard MW, Russell DG. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health 1998;88:288-291.
10. Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ 1995;310:1099-1104.
11. Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns 1999;36:181-192.
12. Yancey AK, Kumanyika SK, Ponce NA, McCarthy WM, Fielding JE. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chron Dis 2004;1:1-18.
13. Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2002;137:208-215.
14. Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract 2000;49:158-168.
15. Ebell Mh, Siwek J, Weiss BD, et al. Simplifying the language of evidence to improve patient care: Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. J Fam Pract 2004;53:111-120.
16. Agurs-Collins TD, Kumanyika SK, Ten Have TR, Adams-Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997;20:1503-1511.
17. Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med 1996;25:225-233.
18. Calfas KJ, Sallis JF, Zabinski MF, et al. Preliminary evaluation of a multi-component program for nutrition and physical activity change in primary care: PACE+ for adults. Prev Med 2002;34:153-161.
19. Patrick K, Sallis JF, Prochaska JJ, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med 2001;155:940-946.
20. Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med 2005;29:247-255.
21. Staten LK, Gregory-Mercado KY, Ranger-Moore J, et al. Provider counseling, health education, and community health workers: The arizona WISEWOMAN project. J Womens Health (Larchmt) 2004;13:547-556.
22. Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obesity Res 2002;10:22-32.
23. Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The activity counseling Trial: A randomized controlled trial. JAMA 2001;286:677-687.
24. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern Latinas. Am J Prev Med 2003;25:69-76.
25. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern African-American women. Am J Prev Med 2003;25:45-52.
26. Rohm YD, Voorhees CC. Personal, social, and environmental correlates of physical activity in urban african-american women. Am J Prev Med 2003;25:38-44.
27. Yancey AK. Building capacity to prevent and control chronic disease in underserved communities: Expanding the wisdom of WISEWOMAN in intervening at the environmental level. J Womens Health (Larchmt) 2004;13:644-649.
28. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, Part 2. JAMA 2002;288:1909-1914.
1. Centers for Disease Control and Prevention. Prevalence of physical activity, including lifestyle activities among adults—United States, 2000-2001. MMWR Morb Mortal Wkly Rep 2003;52:764-769.
2. Taylor WC, Baranowski T, Young DR. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med 1998;15:334-343.
3. Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Prev Med 2000;18:46-53.
4. Mainous AG, Diaz VA, Koopman RJ, Everett CJ. Having a regular physician and attempted weight loss after screening for hypertension or hypercholesterolemia. Int J Obes (Lond) 2005;29:223-227.
5. Honda K. Factors underlying variation in receipt of physician advice on diet and exercise: Applications of the behavioral model of health care utilization. Am J Health Promot 2004;18:370-377.
6. Taira DA, Safran DG, Seto TB, Rogers WH, Tarlov AR. The relationship between patient income and physician discussion of health risk behaviors. JAMA 1997;278:1412-1417.
7. Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services research Team. Prev Med 1995;24:492-497.
8. Norris SL, Grothaus LC, Buchner DM, Pratt M. Effectiveness of physician-based assessment and counseling for exercise in a staff model HMO. Prev Med 2000;30:513-523.
9. Swinburn BA, Walter LG, Arroll B, Tilyard MW, Russell DG. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health 1998;88:288-291.
10. Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ 1995;310:1099-1104.
11. Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns 1999;36:181-192.
12. Yancey AK, Kumanyika SK, Ponce NA, McCarthy WM, Fielding JE. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chron Dis 2004;1:1-18.
13. Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2002;137:208-215.
14. Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract 2000;49:158-168.
15. Ebell Mh, Siwek J, Weiss BD, et al. Simplifying the language of evidence to improve patient care: Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. J Fam Pract 2004;53:111-120.
16. Agurs-Collins TD, Kumanyika SK, Ten Have TR, Adams-Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997;20:1503-1511.
17. Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med 1996;25:225-233.
18. Calfas KJ, Sallis JF, Zabinski MF, et al. Preliminary evaluation of a multi-component program for nutrition and physical activity change in primary care: PACE+ for adults. Prev Med 2002;34:153-161.
19. Patrick K, Sallis JF, Prochaska JJ, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med 2001;155:940-946.
20. Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med 2005;29:247-255.
21. Staten LK, Gregory-Mercado KY, Ranger-Moore J, et al. Provider counseling, health education, and community health workers: The arizona WISEWOMAN project. J Womens Health (Larchmt) 2004;13:547-556.
22. Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obesity Res 2002;10:22-32.
23. Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The activity counseling Trial: A randomized controlled trial. JAMA 2001;286:677-687.
24. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern Latinas. Am J Prev Med 2003;25:69-76.
25. Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern African-American women. Am J Prev Med 2003;25:45-52.
26. Rohm YD, Voorhees CC. Personal, social, and environmental correlates of physical activity in urban african-american women. Am J Prev Med 2003;25:38-44.
27. Yancey AK. Building capacity to prevent and control chronic disease in underserved communities: Expanding the wisdom of WISEWOMAN in intervening at the environmental level. J Womens Health (Larchmt) 2004;13:644-649.
28. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, Part 2. JAMA 2002;288:1909-1914.
Clinical Hospital Medicine Fellowships
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
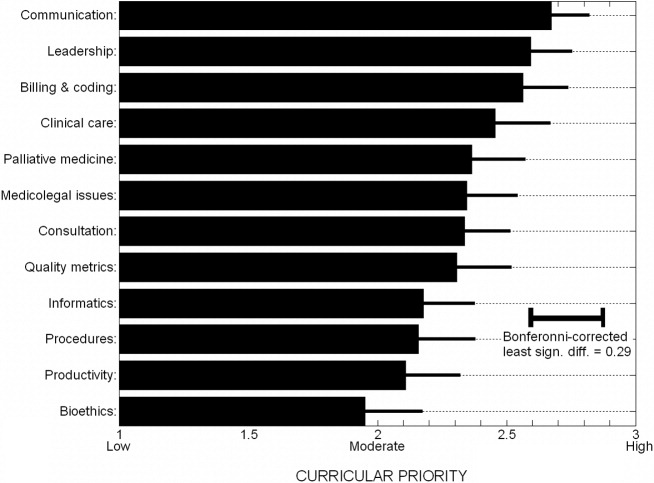
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
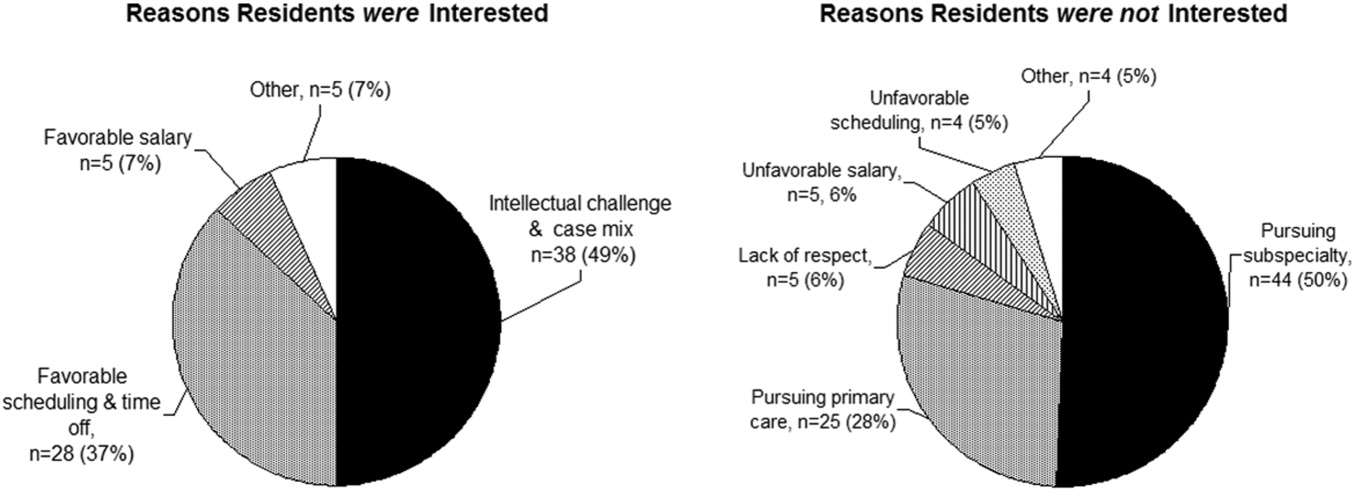
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
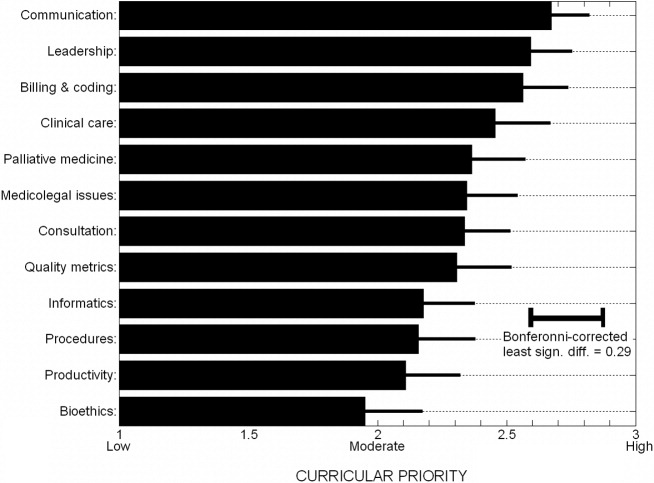
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
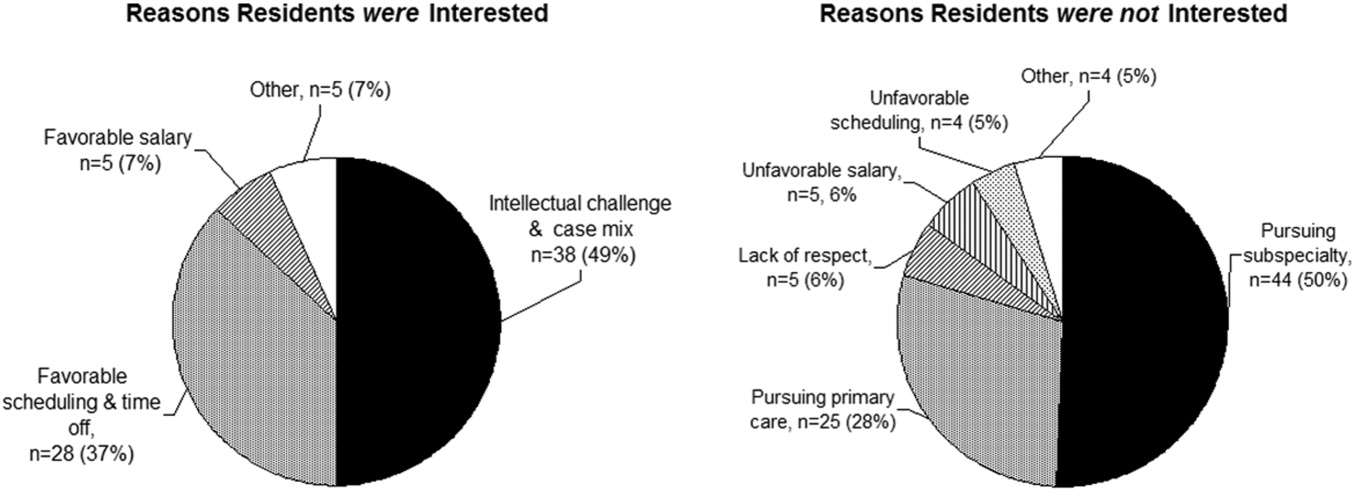
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
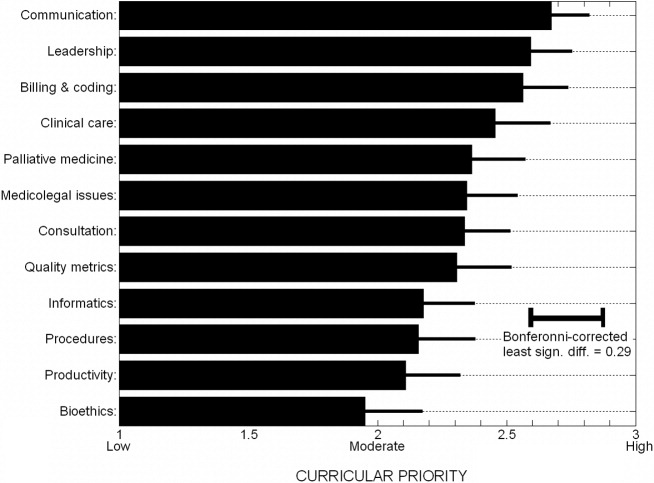
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
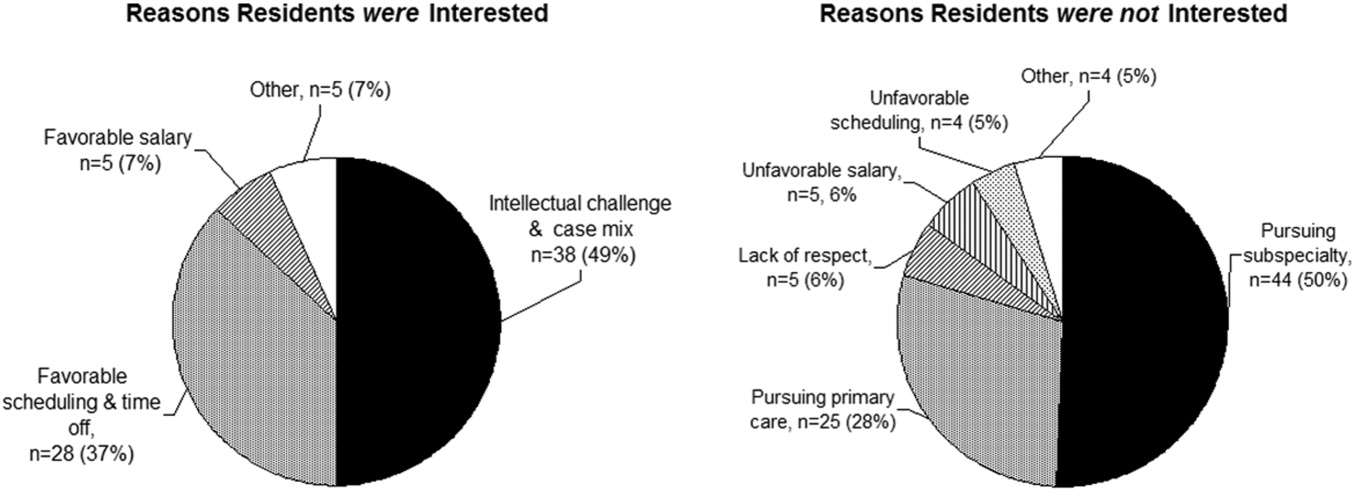
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
Copyright © 2008 Society of Hospital Medicine

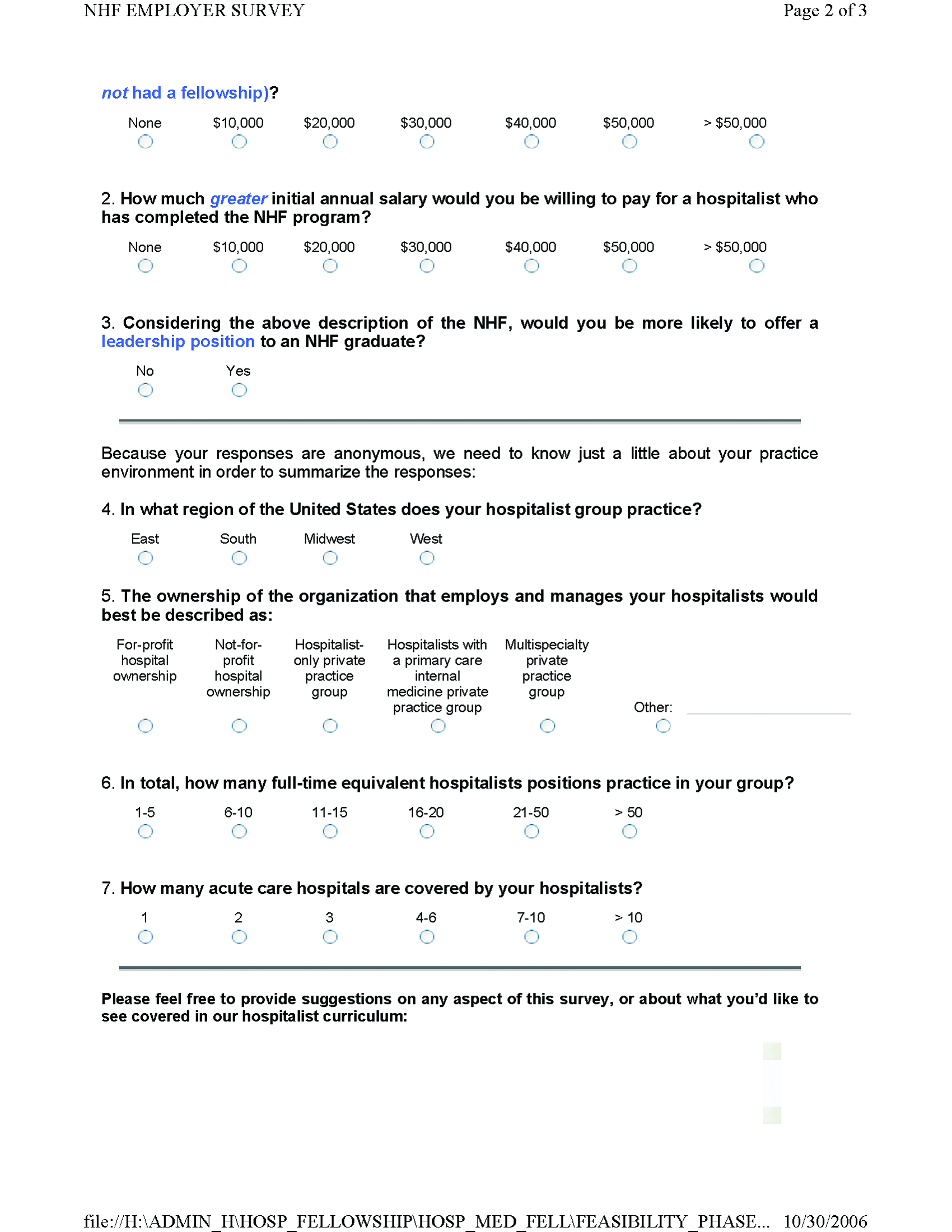

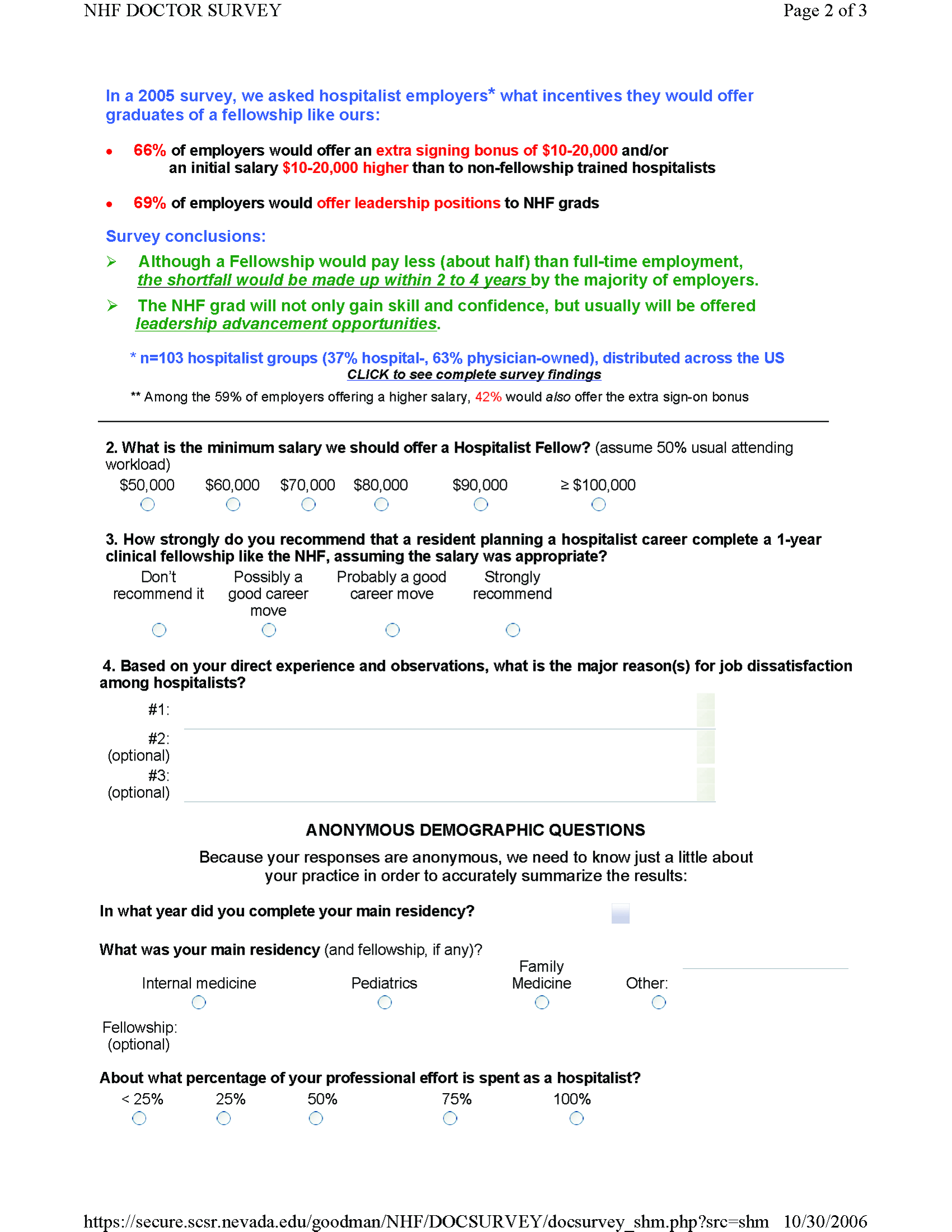
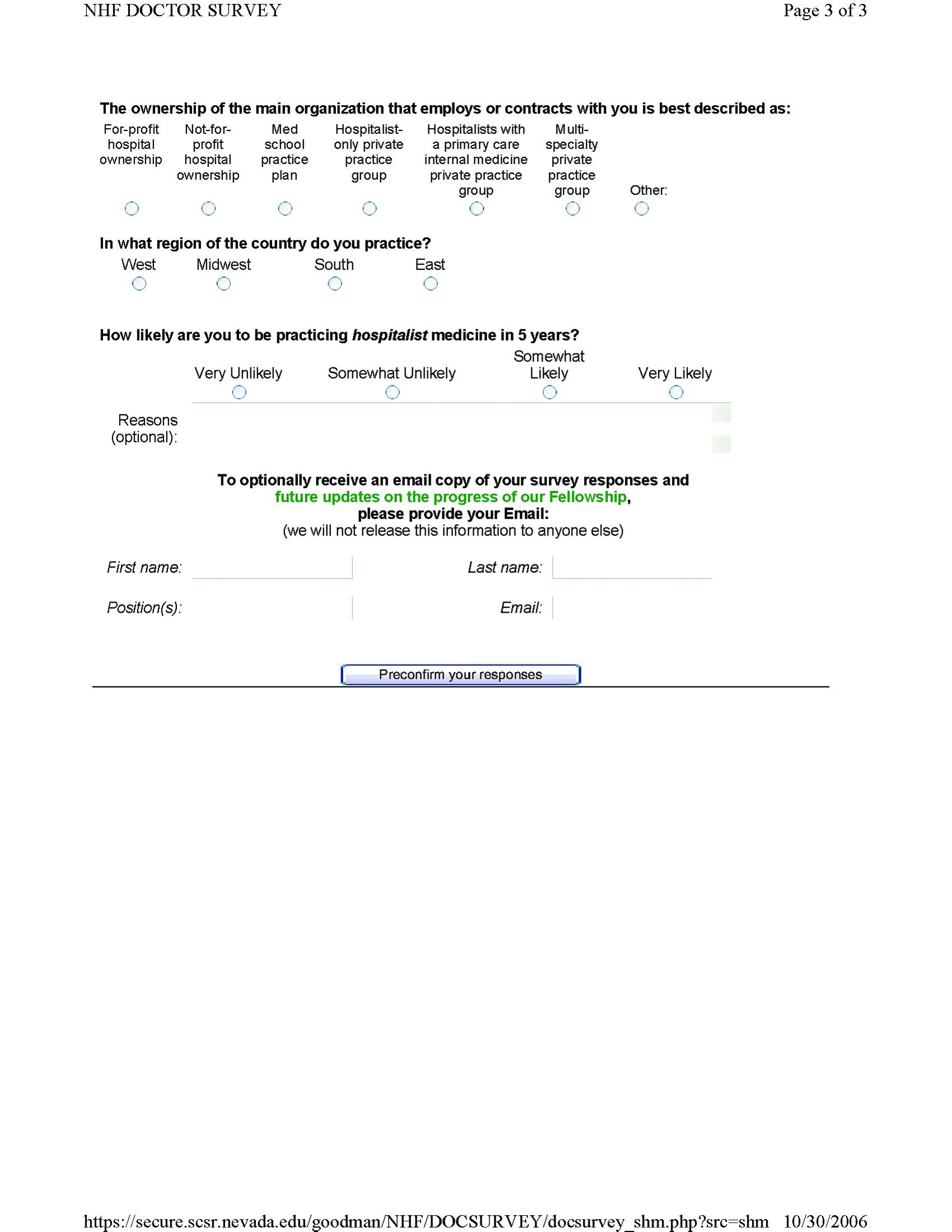

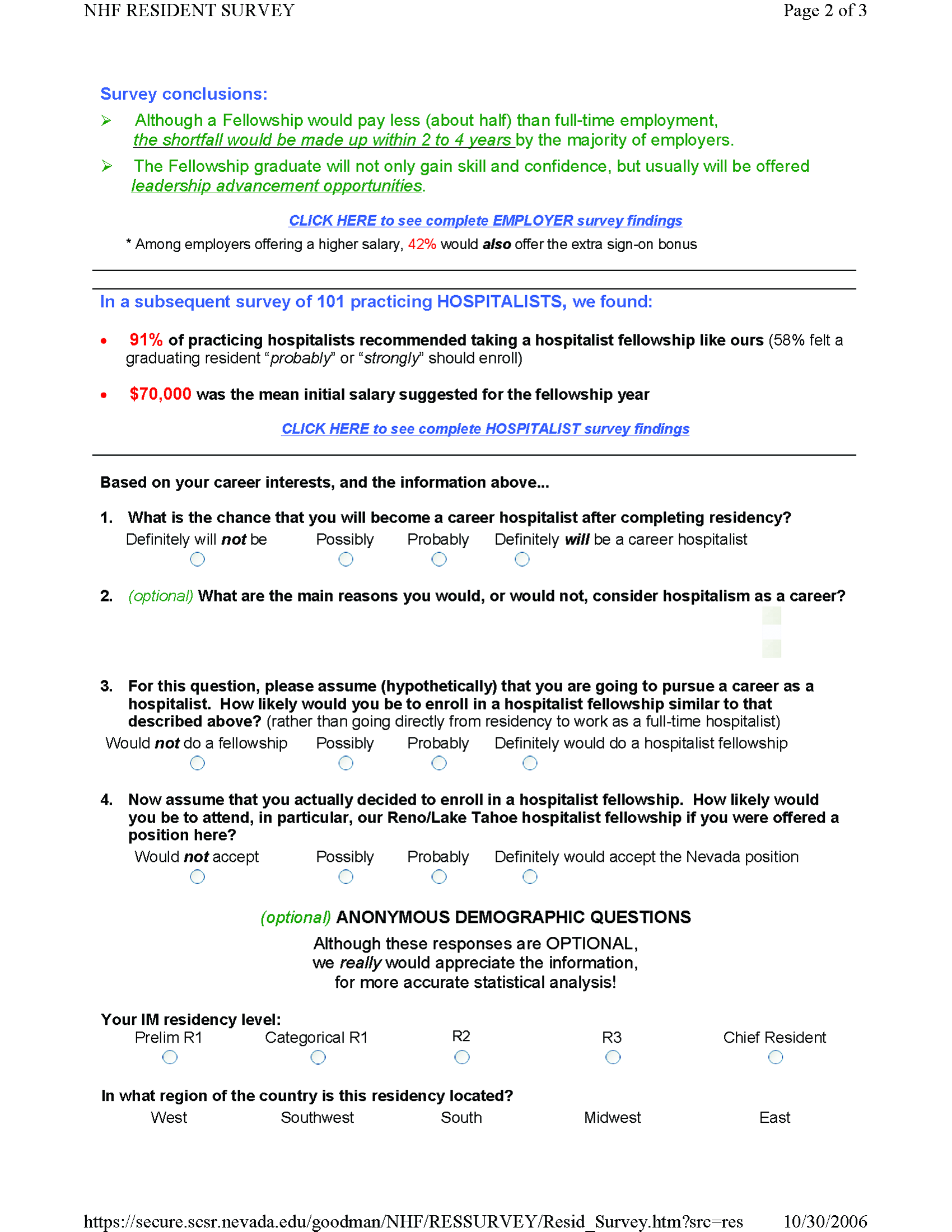
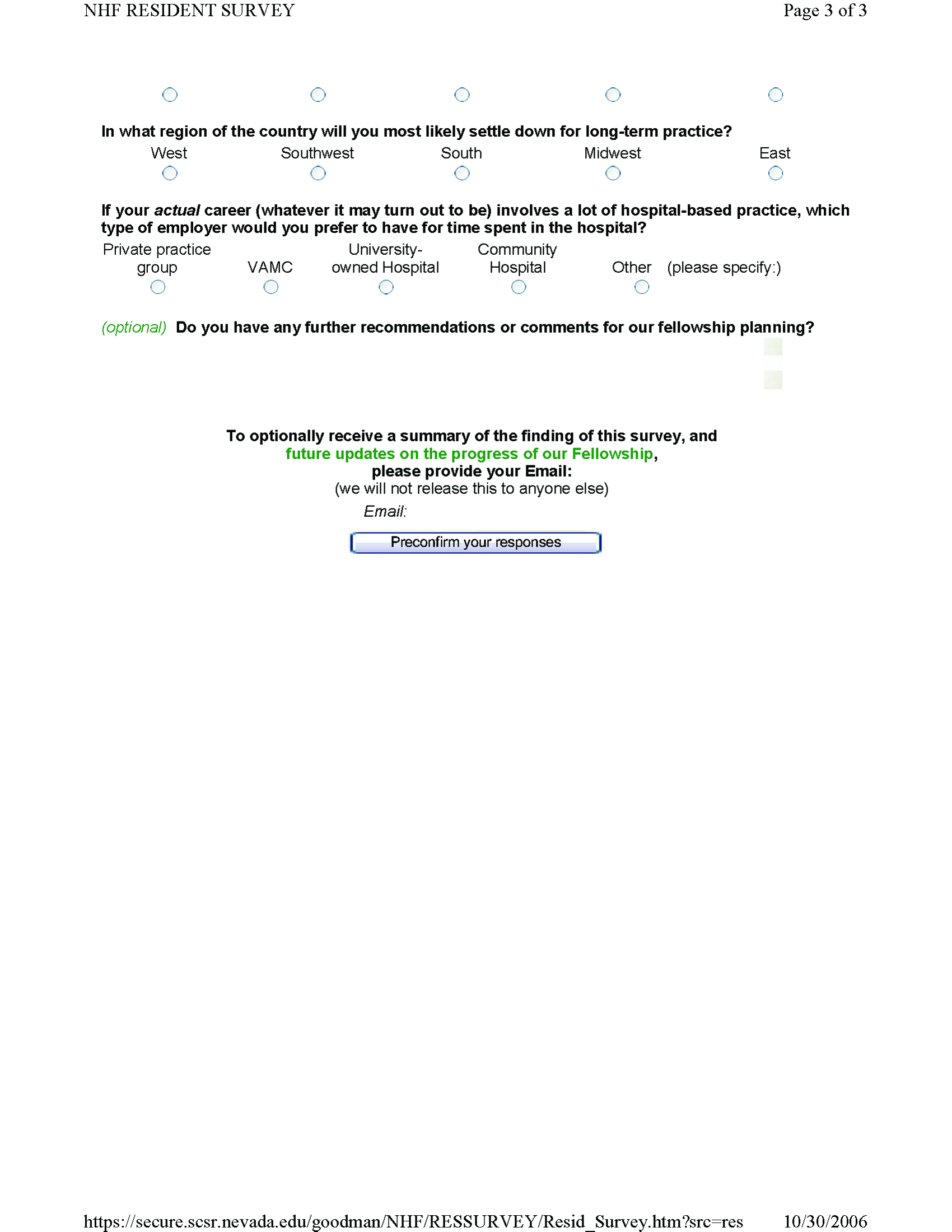
Erythema multiforme secondary to HSV labialis precipitating sickle cell pain crisis
A 28‐year‐old man with sickle cell anemia was admitted with generalized pain. He noted an upper lip lesion 2 weeks prior to admission. He subsequently developed generalized pain in his legs, chest, and back typical of his pain crises. At admission he noted subjective fevers without chills for a week. Vital signs revealed a blood pressure of 135/80, a pulse of 81, a respiratory rate of 16, and an initial temperature of 37.7C. On examination he had scleral icterus and a large upper lip ulcer (Fig. 1). His hospital course was complicated by persistent fevers, a hepatic sequestration crisis, persistent hemolytic anemia requiring blood transfusion, and ultimately the identification of iris‐shaped targetoid lesions on the palms (Fig. 2).These lesions were believed to be consistent with erythema multiforme (EM) secondary to his recent HSV labialis, confirmed by a herpes culture. The patient recovered uneventfully after a 10‐day hospitalization. Erythema multiforme is an acute, self‐limited, but sometimes recurrent dermatologic condition considered to be a distinct hypersensitivity reaction.1 It is associated with certain infections such as herpes simplex 1 and 2, Mycoplasma pneumoniae and fungal infections, and a number of medications in the classes barbiturates, nonsteroidal anti‐inflammatory drugs, penicillins, hydantoins, phenothiazines, and sulfonamides.2 EM is diagnosed clinically by the characteristic rash on the hands and feet, with some cases involving the oral cavity. Treatment is typically focused on resolving the underlying infection or removing the offending drug. Dermatologic manifestations usually improve over 3‐5 weeks without residual sequelae.


- ,,.Understanding the pathogenesis of HSV‐associated erythema multiforme.Dermatology.1998;197:219–222.
- ,,.Erythema multiforme.Am Fam Physician.2006;74:1883–1888.
A 28‐year‐old man with sickle cell anemia was admitted with generalized pain. He noted an upper lip lesion 2 weeks prior to admission. He subsequently developed generalized pain in his legs, chest, and back typical of his pain crises. At admission he noted subjective fevers without chills for a week. Vital signs revealed a blood pressure of 135/80, a pulse of 81, a respiratory rate of 16, and an initial temperature of 37.7C. On examination he had scleral icterus and a large upper lip ulcer (Fig. 1). His hospital course was complicated by persistent fevers, a hepatic sequestration crisis, persistent hemolytic anemia requiring blood transfusion, and ultimately the identification of iris‐shaped targetoid lesions on the palms (Fig. 2).These lesions were believed to be consistent with erythema multiforme (EM) secondary to his recent HSV labialis, confirmed by a herpes culture. The patient recovered uneventfully after a 10‐day hospitalization. Erythema multiforme is an acute, self‐limited, but sometimes recurrent dermatologic condition considered to be a distinct hypersensitivity reaction.1 It is associated with certain infections such as herpes simplex 1 and 2, Mycoplasma pneumoniae and fungal infections, and a number of medications in the classes barbiturates, nonsteroidal anti‐inflammatory drugs, penicillins, hydantoins, phenothiazines, and sulfonamides.2 EM is diagnosed clinically by the characteristic rash on the hands and feet, with some cases involving the oral cavity. Treatment is typically focused on resolving the underlying infection or removing the offending drug. Dermatologic manifestations usually improve over 3‐5 weeks without residual sequelae.


A 28‐year‐old man with sickle cell anemia was admitted with generalized pain. He noted an upper lip lesion 2 weeks prior to admission. He subsequently developed generalized pain in his legs, chest, and back typical of his pain crises. At admission he noted subjective fevers without chills for a week. Vital signs revealed a blood pressure of 135/80, a pulse of 81, a respiratory rate of 16, and an initial temperature of 37.7C. On examination he had scleral icterus and a large upper lip ulcer (Fig. 1). His hospital course was complicated by persistent fevers, a hepatic sequestration crisis, persistent hemolytic anemia requiring blood transfusion, and ultimately the identification of iris‐shaped targetoid lesions on the palms (Fig. 2).These lesions were believed to be consistent with erythema multiforme (EM) secondary to his recent HSV labialis, confirmed by a herpes culture. The patient recovered uneventfully after a 10‐day hospitalization. Erythema multiforme is an acute, self‐limited, but sometimes recurrent dermatologic condition considered to be a distinct hypersensitivity reaction.1 It is associated with certain infections such as herpes simplex 1 and 2, Mycoplasma pneumoniae and fungal infections, and a number of medications in the classes barbiturates, nonsteroidal anti‐inflammatory drugs, penicillins, hydantoins, phenothiazines, and sulfonamides.2 EM is diagnosed clinically by the characteristic rash on the hands and feet, with some cases involving the oral cavity. Treatment is typically focused on resolving the underlying infection or removing the offending drug. Dermatologic manifestations usually improve over 3‐5 weeks without residual sequelae.


- ,,.Understanding the pathogenesis of HSV‐associated erythema multiforme.Dermatology.1998;197:219–222.
- ,,.Erythema multiforme.Am Fam Physician.2006;74:1883–1888.
- ,,.Understanding the pathogenesis of HSV‐associated erythema multiforme.Dermatology.1998;197:219–222.
- ,,.Erythema multiforme.Am Fam Physician.2006;74:1883–1888.
Patients' Predilections Regarding Informed Consent
The cornerstones of American medical ethics include respect for patient autonomy and beneficence. Although informed consent is required for surgical procedures and transfusion of blood products, the overwhelming majority of medical treatments administered by physicians to hospitalized patients are given without discussing risks, benefits, and alternatives. Although patients may sign a general permission‐to‐treat form on admission to the hospital, informed consent for medical treatments is generally ad hoc, and there are no national standards or mandates. We hypothesized that given the choice, hospitalized patients would want to participate in informed decision making, especially for therapies associated with substantial risks and benefits.
METHODS
The Institutional Review Board of Bridgeport Hospital approved this study. Each day between June and August 2006, the hospital's admitting department provided investigators with a list that included names and locations of all patients admitted to the Department of Medicine inpatient service. All the patients were eligible for participation in the study. Patients were excluded if they were in a comatose state, were encephalopathic, or were judged to be severely demented. In addition, patients were assessed during the scripted intervention to ascertain whether they had the capacity to make informed decisions based on their ability: (a) to understand the presented information, (b) to consider the information in relation to their personal values, and (c) to communicate their wishes. If personnel doubted an individual's capacity in any of these 3 areas, they were not included in the study.
Study personnel read directly from the script (see Appendix) and recorded answers. Study personnel were permitted to reread questions but did not provide additional guidance beyond the questionnaire. Patients whose primary language was not English were interviewed through in‐house or 3‐way telephone (remote) translators.
Statistical analyses included the chi‐square test to examine responses across the 3 categories of answers (ie, always consent, qualified consent, waive consent) and simple comparisons of percentages. A P value < .05 was considered statistically significant.
RESULTS
A total of 634 patients were admitted to the medicine service during the study period June‐August 2006. Of these, 158 were judged to lack sufficient capacity by study personnel and were excluded from the study. Ninety‐five refused to participate, and 171 were discharged before the questionnaire could be administered. Two hundred and ten patients answered the questionnaire. They ranged in age from 18 to 96 years (mean age standard error, 63.3 1.1 years). One hundred and three (49%) were men, and 107 (51%) were women. A majority (67.5%) were white, 20% (42) were African American, and 11.9% (25) were Hispanic. Most (87.6%) had at least a high school education, and 35% had a college‐/graduate‐level education. Sixty‐seven percent had at least 2 comorbid conditions in addition to their principal reason for hospitalization. Their average acute physiology and chronic health care evaluation (APACHE II) score was 7.5 0.3 (median 7; range 0‐22).
Figure 1 shows the distribution of answers to each of the 4 questions.
Question 1: Permission for Administration of Diuretics
One hundred and ninety‐three patients (92%) wished to participate in choosing whether to receive diuretics for congestive heart failure (CHF). Of these, 58 (28%) wanted their treating physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and thirty‐five (64%) wanted to be able to give permission if time allowed. Only 8% thought doctors should just give diuretics for CHF without seeking permission.
The pattern of response did not differ by sex, race, number of comorbid conditions, or primary admission diagnosis. Age (>65 vs. <65 years) was significantly associated with predilections to waive permission for administration of diuretics (Pearson chi‐square test P = .01). For example, 36.9% of the younger patients (<65 years) wanted to be consulted under all circumstances compared with only 18.7% of the more elderly patients (P = .004).
Question 2: Permission for Potassium Replacement
Overall, 178 patients (85%) wished to participate in decision making regarding potassium supplementation, and 51 (24%) wanted the managing physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and twenty‐seven patients (61%) responded that they would like to be able to give permission if time allowed. Only 15% thought doctors should just give potassium replacement without seeking their permission. Similar to the responses to diuretic replacement, the pattern of responses differed by age but not by sex, race, level of education, or number of comorbid conditions. Thirty‐one percent of the younger patients wanted to give permission at all times compared with 17.8% of the older patients (P = .03).
Question 3: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Less Than 5%
If the risk of cerebral hemorrhage was less than 5%, only 15 patients (7%) thought it should be given without seeking their permission. A third of the younger patients compared with 24.5% of the elderly patients would want to be consulted for their permission at all times (P = .18). The pattern of responses also did not differ by sex, race or level of education.
Question 4: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Greater Than 20%
Overall, 85 patients (40.8%) would want a discussion and their permission no matter what prior to initiating high‐risk thrombolysis. One hundred and thirteen patients (54%) would want to be able to give permission if time allowed. This pattern of response differed by level of education and by age. Forty‐four percent of those with at least a high school education would want to give permission compared with 19% of those without a high school education (P = .016). Four percent of those with at least a high school education would yield the need for permission at all times compared with 11.5% of those without a high school education (P = .09). Only 1 elderly patient (0.9%) would waive the need for permission at all times compared with 9 younger patients (8.7%; P = .01).
DISCUSSION
The principal finding of this study is that most medical patients prefer to participate in making decisions about their medical care during acute hospitalization, even for relatively low‐risk treatments like potassium supplementation and administration of diuretics. Very few patients were prepared to waive consent and grant their physicians the absolute right to administer therapies such as thrombolysis, even if the risk of bleeding was estimated to be less than 5%. Whereas the elderly patients were less likely to prefer being asked to consent to treatments than were younger patients, most would want to be informed of even trivial therapies if time allowed.
In some situations older patients (65 years old) were more likely than younger patients (<65 years old) to allow their physicians to make unilateral decisions regarding their health care. This could be explained by those age 65 and older having grown up when physician paternalism was more prevalent in American medicine. In the 1970s physician paternalism waned, and respect for patient autonomy emerged as the dominant physicianpatient model. Patients who became adults after 1970 know only this relationship with their physician, and so it makes sense that they would be more inclined to prefer a participatory model.
These data complement and extend a series of studies we conducted with patients admitted to Bridgeport Hospital. Our data suggest that our patients wish to consent for end‐of‐life decisions,1, 2 invasive procedures,3 and, now, to be apprised of medical therapies administered during hospitalization. At the same time, we have found that consent practices at many centers are not consistent with these patient predilections.1, 2, 4 Our study suffered from having a small sample size obtained in one geographic location; so results should be generalized cautiously. Nonetheless, insofar as the expectations of patients for participation are not being met by the health care system in Connecticut (and we suspect elsewhere), clinicians, hospital administrators, and health care policy makers might consider whether more rigorous and explicit consent practices and policies are required. Another important limitation of the study was that patients included may not have entirely understood the implications of their answers (ie, how cumbersome to the system and bothersome to the patient seeking consent for every therapy could become). In fact, we cannot be certain that all patients truly understood the questions, some of which were complex. Nonetheless, these results support that considered in the abstract, most patients prefer to consent for medical therapies. Had the implications for safety and expediency been explained in detail, it is possible that patients would have waived the need to give consent for treatments with minimal risk. The questionnaire also presents an abbreviated list of risks and benefits for each intervention, and although it refers to the formal process of informed consent in its preamble, it uses terminology (ie, permission) that may not reflect the complexity of informed consent. Nonetheless, our goal was to examine the degree to which patients wished to participate in their medical decision making. Notwithstanding these weaknesses of the survey instrument, the data suggest patients want to be in the loop whenever possible.
There are no national standards of consent for medical treatments. The Veterans' Administration, which has led the way in many areas of patients' rights, has a policy:
Treatments and Procedures That Do Not Require Signature Consent. Treatments and procedures that are low risk and are within broadly accepted standards of medical practice (e.g., administration of most drugs or for the performance of minor procedures such as routine X‐rays) do not require signature consent. However, the informed consent process must be documented in the medical record.
Compliance with this standard (ie, consent for every new medication) is not routine in most acute care hospitals. Although some clinicians obtain formal consent for high‐risk therapies (perhaps out of respect for autonomy, perhaps to reduce medical‐legal liability), there are no explicit decision rules to guide clinicians regarding for which treatments they should obtain formal consent. Accordingly, some might obtain formal consent for thrombolysis for massive pulmonary embolus, and others might not. It is not clear that the consent‐to‐treat form signed during hospital admission would legally cover all medical therapies during hospitalization. The legal standard for informed consent is what any reasonable patient would want to consent for. Our data suggest that most reasonable patients wish to at least assent and perhaps consent for much of what they receive during hospitalization. Although we have been unable to find case law predicated entirely on failure to obtain consent prior to administration of a therapy that caused a complication, it is plausible that the reasonable patient standard could be used in this manner. Regardless, it is impractical to require consent for the thousands of medical therapies administered each day in hospitals. Requiring consent for all therapies, if respected rigidly, would threaten the safety and efficiency of American hospitals. Naturally, a balance betweem respect for autonomy, that is, informed consent for the riskiest therapies, and efficiency is necessary. Explicit guidelines issued by accrediting agencies or the federal government would be helpful. The rules for consent (and/or assent) should be more explicit and less arbitrary, that is, determined independently by each clinician.
In conclusion, these data demonstrate that when considered in the abstract, that is, without explaining the logistical hurdles that it would create, inpatients wish to participate in decision making for both low‐ and high‐risk treatments. Clinicians are faced with demands and obligations that preclude full consent for the myriad low‐risk treatments administered daily to hospitalized patients. Some treatments are likely to be covered implicitly under the general consent‐to‐treat process and paperwork. Nonetheless, clinicians should consider explaining the principal risks and benefits of moderate‐risk treatments in order to secure informed assent. Full informed consent may be most appropriate for very high‐risk therapies. Patients expect and deserve frequent communication with caregivers that balances their safety with their right to self‐determination.
APPENDIX
QUESTIONNAIRE
Good morning/afternoon/evening. My name is Dr. _____________, and I am working with Dr. Constantine Manthous in a study to determine what patients want to know about their treatments during hospitalization. The research will not effect your care in any way, and if it is published, your confidential medical information will be protected and will not be mentioned in any publications. In fact, the questions I will ask do not apply to your care plans but are what ifs to find out for what kinds of treatments patients' want to provide permission called informed consent. Informed consent is when a doctor explains a treatment or procedure to the patient, including its risks, benefits, and alternatives, and asks permission before doing it. Are you feeling up to answering 4 questions that should take about 5‐10 minutes? Thank you.
Again, these questions do not apply to your illness or treatments.
If you had fluid on your lungs, a medicine called a diuretic could be given to make you pass more urine to help get the fluid out of the lungs. The benefits are that it can help you breathe easier. The risks are that it will make you have to urinate more often (>50%), and sometimes minerals in the blood get low and can cause the heart to beat abnormally (<1%) if enough replacement minerals aren't given to keep up with losses in the urine. The alternative to receiving this medicine would be not to receive it, which risks continued shortness of breath, and rarely (<5%) untreated patients may need a breathing machine to help breathing. Which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without asking my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there were time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
When a diuretic is given, minerals in the blood can be lost in the urine. If the minerals in the blood get too low, the heart can have abnormal beats that are rarely (<1%) life‐threatening. Doctors can give replacement minerals. The risks of replacement are minimal, and the alternative is not to give the minerals, risking abnormal heartbeats. Which best summarizes your preference?
If I needed replacement minerals, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give me the minerals. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed replacement minerals, I'd want the doctor to talk it over with me first to get my permission no matter what.
During hospitalization, sometimes blood clots can form in the legs and travel to the lungs. Very rarely (<1%), the blood clots can cause shortness of breath and the blood pressure to drop to a dangerous level. In this case there is a medicine called tpa that can dissolve the blood clot. It almost always dissolves the clot, improves breathlessness, and improves heart function. But there is a small risk (<5%) that it can cause serious bleeding into the brain (called a stroke). Which best summarizes your preference?
If I needed tpa for life‐threatening blood clots, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give the tpa. But if there was time and I was able, I'd want the doctor to talk it over with me first to get my permission.
If I needed tpa for life‐threatening blood clots, I'd want the doctor to talk it over with me first to get my permission no matter what.
In the previous example, what if the serious brain bleeding from the clot‐busting drug happened in more than 20% of cases, which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
- ,,,,.Patient, physician and family member understanding of living wills.Am J Respir Crit Care Med.2002;166:1430–1435.
- ,,,,,.Hospitalized patients want to choose whether to receive life‐sustaining therapies.J Hosp Med.2006;1:161–167.
- ,,,,,.Informed consent for invasive medical procedures. From the patient's perspective.Conn Med.2003;67:529–533.
- ,,,.Informed consent for medical procedures: Local and national practices.Chest.2003;124:1978–1984.
- Department of Veterans Affairs. VHA informed consent for clinical treatments and procedures. 2003. Available at: http://www.va.gov/ETHICS/docs/policy/VHA_Handbook_1004‐1_Informed_Consent_Policy_20030129.pdf. Accessed September 5,2006.
The cornerstones of American medical ethics include respect for patient autonomy and beneficence. Although informed consent is required for surgical procedures and transfusion of blood products, the overwhelming majority of medical treatments administered by physicians to hospitalized patients are given without discussing risks, benefits, and alternatives. Although patients may sign a general permission‐to‐treat form on admission to the hospital, informed consent for medical treatments is generally ad hoc, and there are no national standards or mandates. We hypothesized that given the choice, hospitalized patients would want to participate in informed decision making, especially for therapies associated with substantial risks and benefits.
METHODS
The Institutional Review Board of Bridgeport Hospital approved this study. Each day between June and August 2006, the hospital's admitting department provided investigators with a list that included names and locations of all patients admitted to the Department of Medicine inpatient service. All the patients were eligible for participation in the study. Patients were excluded if they were in a comatose state, were encephalopathic, or were judged to be severely demented. In addition, patients were assessed during the scripted intervention to ascertain whether they had the capacity to make informed decisions based on their ability: (a) to understand the presented information, (b) to consider the information in relation to their personal values, and (c) to communicate their wishes. If personnel doubted an individual's capacity in any of these 3 areas, they were not included in the study.
Study personnel read directly from the script (see Appendix) and recorded answers. Study personnel were permitted to reread questions but did not provide additional guidance beyond the questionnaire. Patients whose primary language was not English were interviewed through in‐house or 3‐way telephone (remote) translators.
Statistical analyses included the chi‐square test to examine responses across the 3 categories of answers (ie, always consent, qualified consent, waive consent) and simple comparisons of percentages. A P value < .05 was considered statistically significant.
RESULTS
A total of 634 patients were admitted to the medicine service during the study period June‐August 2006. Of these, 158 were judged to lack sufficient capacity by study personnel and were excluded from the study. Ninety‐five refused to participate, and 171 were discharged before the questionnaire could be administered. Two hundred and ten patients answered the questionnaire. They ranged in age from 18 to 96 years (mean age standard error, 63.3 1.1 years). One hundred and three (49%) were men, and 107 (51%) were women. A majority (67.5%) were white, 20% (42) were African American, and 11.9% (25) were Hispanic. Most (87.6%) had at least a high school education, and 35% had a college‐/graduate‐level education. Sixty‐seven percent had at least 2 comorbid conditions in addition to their principal reason for hospitalization. Their average acute physiology and chronic health care evaluation (APACHE II) score was 7.5 0.3 (median 7; range 0‐22).
Figure 1 shows the distribution of answers to each of the 4 questions.
Question 1: Permission for Administration of Diuretics
One hundred and ninety‐three patients (92%) wished to participate in choosing whether to receive diuretics for congestive heart failure (CHF). Of these, 58 (28%) wanted their treating physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and thirty‐five (64%) wanted to be able to give permission if time allowed. Only 8% thought doctors should just give diuretics for CHF without seeking permission.
The pattern of response did not differ by sex, race, number of comorbid conditions, or primary admission diagnosis. Age (>65 vs. <65 years) was significantly associated with predilections to waive permission for administration of diuretics (Pearson chi‐square test P = .01). For example, 36.9% of the younger patients (<65 years) wanted to be consulted under all circumstances compared with only 18.7% of the more elderly patients (P = .004).
Question 2: Permission for Potassium Replacement
Overall, 178 patients (85%) wished to participate in decision making regarding potassium supplementation, and 51 (24%) wanted the managing physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and twenty‐seven patients (61%) responded that they would like to be able to give permission if time allowed. Only 15% thought doctors should just give potassium replacement without seeking their permission. Similar to the responses to diuretic replacement, the pattern of responses differed by age but not by sex, race, level of education, or number of comorbid conditions. Thirty‐one percent of the younger patients wanted to give permission at all times compared with 17.8% of the older patients (P = .03).
Question 3: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Less Than 5%
If the risk of cerebral hemorrhage was less than 5%, only 15 patients (7%) thought it should be given without seeking their permission. A third of the younger patients compared with 24.5% of the elderly patients would want to be consulted for their permission at all times (P = .18). The pattern of responses also did not differ by sex, race or level of education.
Question 4: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Greater Than 20%
Overall, 85 patients (40.8%) would want a discussion and their permission no matter what prior to initiating high‐risk thrombolysis. One hundred and thirteen patients (54%) would want to be able to give permission if time allowed. This pattern of response differed by level of education and by age. Forty‐four percent of those with at least a high school education would want to give permission compared with 19% of those without a high school education (P = .016). Four percent of those with at least a high school education would yield the need for permission at all times compared with 11.5% of those without a high school education (P = .09). Only 1 elderly patient (0.9%) would waive the need for permission at all times compared with 9 younger patients (8.7%; P = .01).
DISCUSSION
The principal finding of this study is that most medical patients prefer to participate in making decisions about their medical care during acute hospitalization, even for relatively low‐risk treatments like potassium supplementation and administration of diuretics. Very few patients were prepared to waive consent and grant their physicians the absolute right to administer therapies such as thrombolysis, even if the risk of bleeding was estimated to be less than 5%. Whereas the elderly patients were less likely to prefer being asked to consent to treatments than were younger patients, most would want to be informed of even trivial therapies if time allowed.
In some situations older patients (65 years old) were more likely than younger patients (<65 years old) to allow their physicians to make unilateral decisions regarding their health care. This could be explained by those age 65 and older having grown up when physician paternalism was more prevalent in American medicine. In the 1970s physician paternalism waned, and respect for patient autonomy emerged as the dominant physicianpatient model. Patients who became adults after 1970 know only this relationship with their physician, and so it makes sense that they would be more inclined to prefer a participatory model.
These data complement and extend a series of studies we conducted with patients admitted to Bridgeport Hospital. Our data suggest that our patients wish to consent for end‐of‐life decisions,1, 2 invasive procedures,3 and, now, to be apprised of medical therapies administered during hospitalization. At the same time, we have found that consent practices at many centers are not consistent with these patient predilections.1, 2, 4 Our study suffered from having a small sample size obtained in one geographic location; so results should be generalized cautiously. Nonetheless, insofar as the expectations of patients for participation are not being met by the health care system in Connecticut (and we suspect elsewhere), clinicians, hospital administrators, and health care policy makers might consider whether more rigorous and explicit consent practices and policies are required. Another important limitation of the study was that patients included may not have entirely understood the implications of their answers (ie, how cumbersome to the system and bothersome to the patient seeking consent for every therapy could become). In fact, we cannot be certain that all patients truly understood the questions, some of which were complex. Nonetheless, these results support that considered in the abstract, most patients prefer to consent for medical therapies. Had the implications for safety and expediency been explained in detail, it is possible that patients would have waived the need to give consent for treatments with minimal risk. The questionnaire also presents an abbreviated list of risks and benefits for each intervention, and although it refers to the formal process of informed consent in its preamble, it uses terminology (ie, permission) that may not reflect the complexity of informed consent. Nonetheless, our goal was to examine the degree to which patients wished to participate in their medical decision making. Notwithstanding these weaknesses of the survey instrument, the data suggest patients want to be in the loop whenever possible.
There are no national standards of consent for medical treatments. The Veterans' Administration, which has led the way in many areas of patients' rights, has a policy:
Treatments and Procedures That Do Not Require Signature Consent. Treatments and procedures that are low risk and are within broadly accepted standards of medical practice (e.g., administration of most drugs or for the performance of minor procedures such as routine X‐rays) do not require signature consent. However, the informed consent process must be documented in the medical record.
Compliance with this standard (ie, consent for every new medication) is not routine in most acute care hospitals. Although some clinicians obtain formal consent for high‐risk therapies (perhaps out of respect for autonomy, perhaps to reduce medical‐legal liability), there are no explicit decision rules to guide clinicians regarding for which treatments they should obtain formal consent. Accordingly, some might obtain formal consent for thrombolysis for massive pulmonary embolus, and others might not. It is not clear that the consent‐to‐treat form signed during hospital admission would legally cover all medical therapies during hospitalization. The legal standard for informed consent is what any reasonable patient would want to consent for. Our data suggest that most reasonable patients wish to at least assent and perhaps consent for much of what they receive during hospitalization. Although we have been unable to find case law predicated entirely on failure to obtain consent prior to administration of a therapy that caused a complication, it is plausible that the reasonable patient standard could be used in this manner. Regardless, it is impractical to require consent for the thousands of medical therapies administered each day in hospitals. Requiring consent for all therapies, if respected rigidly, would threaten the safety and efficiency of American hospitals. Naturally, a balance betweem respect for autonomy, that is, informed consent for the riskiest therapies, and efficiency is necessary. Explicit guidelines issued by accrediting agencies or the federal government would be helpful. The rules for consent (and/or assent) should be more explicit and less arbitrary, that is, determined independently by each clinician.
In conclusion, these data demonstrate that when considered in the abstract, that is, without explaining the logistical hurdles that it would create, inpatients wish to participate in decision making for both low‐ and high‐risk treatments. Clinicians are faced with demands and obligations that preclude full consent for the myriad low‐risk treatments administered daily to hospitalized patients. Some treatments are likely to be covered implicitly under the general consent‐to‐treat process and paperwork. Nonetheless, clinicians should consider explaining the principal risks and benefits of moderate‐risk treatments in order to secure informed assent. Full informed consent may be most appropriate for very high‐risk therapies. Patients expect and deserve frequent communication with caregivers that balances their safety with their right to self‐determination.
APPENDIX
QUESTIONNAIRE
Good morning/afternoon/evening. My name is Dr. _____________, and I am working with Dr. Constantine Manthous in a study to determine what patients want to know about their treatments during hospitalization. The research will not effect your care in any way, and if it is published, your confidential medical information will be protected and will not be mentioned in any publications. In fact, the questions I will ask do not apply to your care plans but are what ifs to find out for what kinds of treatments patients' want to provide permission called informed consent. Informed consent is when a doctor explains a treatment or procedure to the patient, including its risks, benefits, and alternatives, and asks permission before doing it. Are you feeling up to answering 4 questions that should take about 5‐10 minutes? Thank you.
Again, these questions do not apply to your illness or treatments.
If you had fluid on your lungs, a medicine called a diuretic could be given to make you pass more urine to help get the fluid out of the lungs. The benefits are that it can help you breathe easier. The risks are that it will make you have to urinate more often (>50%), and sometimes minerals in the blood get low and can cause the heart to beat abnormally (<1%) if enough replacement minerals aren't given to keep up with losses in the urine. The alternative to receiving this medicine would be not to receive it, which risks continued shortness of breath, and rarely (<5%) untreated patients may need a breathing machine to help breathing. Which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without asking my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there were time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
When a diuretic is given, minerals in the blood can be lost in the urine. If the minerals in the blood get too low, the heart can have abnormal beats that are rarely (<1%) life‐threatening. Doctors can give replacement minerals. The risks of replacement are minimal, and the alternative is not to give the minerals, risking abnormal heartbeats. Which best summarizes your preference?
If I needed replacement minerals, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give me the minerals. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed replacement minerals, I'd want the doctor to talk it over with me first to get my permission no matter what.
During hospitalization, sometimes blood clots can form in the legs and travel to the lungs. Very rarely (<1%), the blood clots can cause shortness of breath and the blood pressure to drop to a dangerous level. In this case there is a medicine called tpa that can dissolve the blood clot. It almost always dissolves the clot, improves breathlessness, and improves heart function. But there is a small risk (<5%) that it can cause serious bleeding into the brain (called a stroke). Which best summarizes your preference?
If I needed tpa for life‐threatening blood clots, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give the tpa. But if there was time and I was able, I'd want the doctor to talk it over with me first to get my permission.
If I needed tpa for life‐threatening blood clots, I'd want the doctor to talk it over with me first to get my permission no matter what.
In the previous example, what if the serious brain bleeding from the clot‐busting drug happened in more than 20% of cases, which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
The cornerstones of American medical ethics include respect for patient autonomy and beneficence. Although informed consent is required for surgical procedures and transfusion of blood products, the overwhelming majority of medical treatments administered by physicians to hospitalized patients are given without discussing risks, benefits, and alternatives. Although patients may sign a general permission‐to‐treat form on admission to the hospital, informed consent for medical treatments is generally ad hoc, and there are no national standards or mandates. We hypothesized that given the choice, hospitalized patients would want to participate in informed decision making, especially for therapies associated with substantial risks and benefits.
METHODS
The Institutional Review Board of Bridgeport Hospital approved this study. Each day between June and August 2006, the hospital's admitting department provided investigators with a list that included names and locations of all patients admitted to the Department of Medicine inpatient service. All the patients were eligible for participation in the study. Patients were excluded if they were in a comatose state, were encephalopathic, or were judged to be severely demented. In addition, patients were assessed during the scripted intervention to ascertain whether they had the capacity to make informed decisions based on their ability: (a) to understand the presented information, (b) to consider the information in relation to their personal values, and (c) to communicate their wishes. If personnel doubted an individual's capacity in any of these 3 areas, they were not included in the study.
Study personnel read directly from the script (see Appendix) and recorded answers. Study personnel were permitted to reread questions but did not provide additional guidance beyond the questionnaire. Patients whose primary language was not English were interviewed through in‐house or 3‐way telephone (remote) translators.
Statistical analyses included the chi‐square test to examine responses across the 3 categories of answers (ie, always consent, qualified consent, waive consent) and simple comparisons of percentages. A P value < .05 was considered statistically significant.
RESULTS
A total of 634 patients were admitted to the medicine service during the study period June‐August 2006. Of these, 158 were judged to lack sufficient capacity by study personnel and were excluded from the study. Ninety‐five refused to participate, and 171 were discharged before the questionnaire could be administered. Two hundred and ten patients answered the questionnaire. They ranged in age from 18 to 96 years (mean age standard error, 63.3 1.1 years). One hundred and three (49%) were men, and 107 (51%) were women. A majority (67.5%) were white, 20% (42) were African American, and 11.9% (25) were Hispanic. Most (87.6%) had at least a high school education, and 35% had a college‐/graduate‐level education. Sixty‐seven percent had at least 2 comorbid conditions in addition to their principal reason for hospitalization. Their average acute physiology and chronic health care evaluation (APACHE II) score was 7.5 0.3 (median 7; range 0‐22).
Figure 1 shows the distribution of answers to each of the 4 questions.
Question 1: Permission for Administration of Diuretics
One hundred and ninety‐three patients (92%) wished to participate in choosing whether to receive diuretics for congestive heart failure (CHF). Of these, 58 (28%) wanted their treating physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and thirty‐five (64%) wanted to be able to give permission if time allowed. Only 8% thought doctors should just give diuretics for CHF without seeking permission.
The pattern of response did not differ by sex, race, number of comorbid conditions, or primary admission diagnosis. Age (>65 vs. <65 years) was significantly associated with predilections to waive permission for administration of diuretics (Pearson chi‐square test P = .01). For example, 36.9% of the younger patients (<65 years) wanted to be consulted under all circumstances compared with only 18.7% of the more elderly patients (P = .004).
Question 2: Permission for Potassium Replacement
Overall, 178 patients (85%) wished to participate in decision making regarding potassium supplementation, and 51 (24%) wanted the managing physicians to obtain their permission no matter what, even if there was an acute matter of life and death. One hundred and twenty‐seven patients (61%) responded that they would like to be able to give permission if time allowed. Only 15% thought doctors should just give potassium replacement without seeking their permission. Similar to the responses to diuretic replacement, the pattern of responses differed by age but not by sex, race, level of education, or number of comorbid conditions. Thirty‐one percent of the younger patients wanted to give permission at all times compared with 17.8% of the older patients (P = .03).
Question 3: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Less Than 5%
If the risk of cerebral hemorrhage was less than 5%, only 15 patients (7%) thought it should be given without seeking their permission. A third of the younger patients compared with 24.5% of the elderly patients would want to be consulted for their permission at all times (P = .18). The pattern of responses also did not differ by sex, race or level of education.
Question 4: Permission for Thrombolysis of Pulmonary Embolus if Risk of Cerebral Bleed Was Greater Than 20%
Overall, 85 patients (40.8%) would want a discussion and their permission no matter what prior to initiating high‐risk thrombolysis. One hundred and thirteen patients (54%) would want to be able to give permission if time allowed. This pattern of response differed by level of education and by age. Forty‐four percent of those with at least a high school education would want to give permission compared with 19% of those without a high school education (P = .016). Four percent of those with at least a high school education would yield the need for permission at all times compared with 11.5% of those without a high school education (P = .09). Only 1 elderly patient (0.9%) would waive the need for permission at all times compared with 9 younger patients (8.7%; P = .01).
DISCUSSION
The principal finding of this study is that most medical patients prefer to participate in making decisions about their medical care during acute hospitalization, even for relatively low‐risk treatments like potassium supplementation and administration of diuretics. Very few patients were prepared to waive consent and grant their physicians the absolute right to administer therapies such as thrombolysis, even if the risk of bleeding was estimated to be less than 5%. Whereas the elderly patients were less likely to prefer being asked to consent to treatments than were younger patients, most would want to be informed of even trivial therapies if time allowed.
In some situations older patients (65 years old) were more likely than younger patients (<65 years old) to allow their physicians to make unilateral decisions regarding their health care. This could be explained by those age 65 and older having grown up when physician paternalism was more prevalent in American medicine. In the 1970s physician paternalism waned, and respect for patient autonomy emerged as the dominant physicianpatient model. Patients who became adults after 1970 know only this relationship with their physician, and so it makes sense that they would be more inclined to prefer a participatory model.
These data complement and extend a series of studies we conducted with patients admitted to Bridgeport Hospital. Our data suggest that our patients wish to consent for end‐of‐life decisions,1, 2 invasive procedures,3 and, now, to be apprised of medical therapies administered during hospitalization. At the same time, we have found that consent practices at many centers are not consistent with these patient predilections.1, 2, 4 Our study suffered from having a small sample size obtained in one geographic location; so results should be generalized cautiously. Nonetheless, insofar as the expectations of patients for participation are not being met by the health care system in Connecticut (and we suspect elsewhere), clinicians, hospital administrators, and health care policy makers might consider whether more rigorous and explicit consent practices and policies are required. Another important limitation of the study was that patients included may not have entirely understood the implications of their answers (ie, how cumbersome to the system and bothersome to the patient seeking consent for every therapy could become). In fact, we cannot be certain that all patients truly understood the questions, some of which were complex. Nonetheless, these results support that considered in the abstract, most patients prefer to consent for medical therapies. Had the implications for safety and expediency been explained in detail, it is possible that patients would have waived the need to give consent for treatments with minimal risk. The questionnaire also presents an abbreviated list of risks and benefits for each intervention, and although it refers to the formal process of informed consent in its preamble, it uses terminology (ie, permission) that may not reflect the complexity of informed consent. Nonetheless, our goal was to examine the degree to which patients wished to participate in their medical decision making. Notwithstanding these weaknesses of the survey instrument, the data suggest patients want to be in the loop whenever possible.
There are no national standards of consent for medical treatments. The Veterans' Administration, which has led the way in many areas of patients' rights, has a policy:
Treatments and Procedures That Do Not Require Signature Consent. Treatments and procedures that are low risk and are within broadly accepted standards of medical practice (e.g., administration of most drugs or for the performance of minor procedures such as routine X‐rays) do not require signature consent. However, the informed consent process must be documented in the medical record.
Compliance with this standard (ie, consent for every new medication) is not routine in most acute care hospitals. Although some clinicians obtain formal consent for high‐risk therapies (perhaps out of respect for autonomy, perhaps to reduce medical‐legal liability), there are no explicit decision rules to guide clinicians regarding for which treatments they should obtain formal consent. Accordingly, some might obtain formal consent for thrombolysis for massive pulmonary embolus, and others might not. It is not clear that the consent‐to‐treat form signed during hospital admission would legally cover all medical therapies during hospitalization. The legal standard for informed consent is what any reasonable patient would want to consent for. Our data suggest that most reasonable patients wish to at least assent and perhaps consent for much of what they receive during hospitalization. Although we have been unable to find case law predicated entirely on failure to obtain consent prior to administration of a therapy that caused a complication, it is plausible that the reasonable patient standard could be used in this manner. Regardless, it is impractical to require consent for the thousands of medical therapies administered each day in hospitals. Requiring consent for all therapies, if respected rigidly, would threaten the safety and efficiency of American hospitals. Naturally, a balance betweem respect for autonomy, that is, informed consent for the riskiest therapies, and efficiency is necessary. Explicit guidelines issued by accrediting agencies or the federal government would be helpful. The rules for consent (and/or assent) should be more explicit and less arbitrary, that is, determined independently by each clinician.
In conclusion, these data demonstrate that when considered in the abstract, that is, without explaining the logistical hurdles that it would create, inpatients wish to participate in decision making for both low‐ and high‐risk treatments. Clinicians are faced with demands and obligations that preclude full consent for the myriad low‐risk treatments administered daily to hospitalized patients. Some treatments are likely to be covered implicitly under the general consent‐to‐treat process and paperwork. Nonetheless, clinicians should consider explaining the principal risks and benefits of moderate‐risk treatments in order to secure informed assent. Full informed consent may be most appropriate for very high‐risk therapies. Patients expect and deserve frequent communication with caregivers that balances their safety with their right to self‐determination.
APPENDIX
QUESTIONNAIRE
Good morning/afternoon/evening. My name is Dr. _____________, and I am working with Dr. Constantine Manthous in a study to determine what patients want to know about their treatments during hospitalization. The research will not effect your care in any way, and if it is published, your confidential medical information will be protected and will not be mentioned in any publications. In fact, the questions I will ask do not apply to your care plans but are what ifs to find out for what kinds of treatments patients' want to provide permission called informed consent. Informed consent is when a doctor explains a treatment or procedure to the patient, including its risks, benefits, and alternatives, and asks permission before doing it. Are you feeling up to answering 4 questions that should take about 5‐10 minutes? Thank you.
Again, these questions do not apply to your illness or treatments.
If you had fluid on your lungs, a medicine called a diuretic could be given to make you pass more urine to help get the fluid out of the lungs. The benefits are that it can help you breathe easier. The risks are that it will make you have to urinate more often (>50%), and sometimes minerals in the blood get low and can cause the heart to beat abnormally (<1%) if enough replacement minerals aren't given to keep up with losses in the urine. The alternative to receiving this medicine would be not to receive it, which risks continued shortness of breath, and rarely (<5%) untreated patients may need a breathing machine to help breathing. Which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without asking my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there were time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
When a diuretic is given, minerals in the blood can be lost in the urine. If the minerals in the blood get too low, the heart can have abnormal beats that are rarely (<1%) life‐threatening. Doctors can give replacement minerals. The risks of replacement are minimal, and the alternative is not to give the minerals, risking abnormal heartbeats. Which best summarizes your preference?
If I needed replacement minerals, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give me the minerals. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed replacement minerals, I'd want the doctor to talk it over with me first to get my permission no matter what.
During hospitalization, sometimes blood clots can form in the legs and travel to the lungs. Very rarely (<1%), the blood clots can cause shortness of breath and the blood pressure to drop to a dangerous level. In this case there is a medicine called tpa that can dissolve the blood clot. It almost always dissolves the clot, improves breathlessness, and improves heart function. But there is a small risk (<5%) that it can cause serious bleeding into the brain (called a stroke). Which best summarizes your preference?
If I needed tpa for life‐threatening blood clots, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give the tpa. But if there was time and I was able, I'd want the doctor to talk it over with me first to get my permission.
If I needed tpa for life‐threatening blood clots, I'd want the doctor to talk it over with me first to get my permission no matter what.
In the previous example, what if the serious brain bleeding from the clot‐busting drug happened in more than 20% of cases, which best summarizes your preference?
If I needed this treatment, the doctor should give it to me without needing my permission.
If it was a question of life or death and there wasn't enough time to talk it over, I'd want the doctor to just give it. But if there was time, I'd want the doctor to talk it over with me first to get my permission.
If I needed this treatment, I'd want the doctor to talk it over with me first to get my permission no matter what.
- ,,,,.Patient, physician and family member understanding of living wills.Am J Respir Crit Care Med.2002;166:1430–1435.
- ,,,,,.Hospitalized patients want to choose whether to receive life‐sustaining therapies.J Hosp Med.2006;1:161–167.
- ,,,,,.Informed consent for invasive medical procedures. From the patient's perspective.Conn Med.2003;67:529–533.
- ,,,.Informed consent for medical procedures: Local and national practices.Chest.2003;124:1978–1984.
- Department of Veterans Affairs. VHA informed consent for clinical treatments and procedures. 2003. Available at: http://www.va.gov/ETHICS/docs/policy/VHA_Handbook_1004‐1_Informed_Consent_Policy_20030129.pdf. Accessed September 5,2006.
- ,,,,.Patient, physician and family member understanding of living wills.Am J Respir Crit Care Med.2002;166:1430–1435.
- ,,,,,.Hospitalized patients want to choose whether to receive life‐sustaining therapies.J Hosp Med.2006;1:161–167.
- ,,,,,.Informed consent for invasive medical procedures. From the patient's perspective.Conn Med.2003;67:529–533.
- ,,,.Informed consent for medical procedures: Local and national practices.Chest.2003;124:1978–1984.
- Department of Veterans Affairs. VHA informed consent for clinical treatments and procedures. 2003. Available at: http://www.va.gov/ETHICS/docs/policy/VHA_Handbook_1004‐1_Informed_Consent_Policy_20030129.pdf. Accessed September 5,2006.
Copyright © 2008 Society of Hospital Medicine
Editorial
We live in a moment of history where change is so speeded up that we begin to see the present only when it is already disappearing.
Two years ago we published the first issue of the Journal of Hospital Medicine and declared, Our goal is that JHM become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.1 That first issue was just one of many steps toward this ambition. At the completion of its first year, JHM was selected for indexing and inclusion in the National Library of Medicine's Medical Literature Analysis and Retrieval System Online (MEDLINE), the primary component of PubMed. Following this huge step, we welcomed a remarkable increase in submissions and will have exceeded 300 in our second year, an approximately 50% increase from our first year!
As important, JHM quickly became a valuable benefit of membership in the Society of Hospital Medicine, and the innumerable compliments received by the staff reflect the diligent efforts of a remarkable editorial staff and work by our reviewers. With profound gratitude we list on page 86 these 325 reviewers who donated their priceless time and expertise to enhancing the quality of the manuscripts. To handle the marked increase in submissions, we are expanding and modifying our editorial staff. Please welcome Sunil Kripalani (Vanderbilt) and Daniel Brotman (Johns Hopkins), who join our previous six associate editors and all eight will now serve as JHM's deputy editors. Seven new associate editors also join our team. Among them, Tom Baudendistel (California Pacific Medical Center, San Francisco), Eric Alper (UMass Memorial Health Care, Worcester), Brian Harte (Cleveland Clinic), and Rehan Qayyum (Johns Hopkins) will all focus on optimizing content for practicing hospitalists. Paul Aronowitz will continue to develop our Images section as an associate editor. Recognizing the growing number of pediatric hospitalists, Lisa Zauotis (Childrens Hospital of Philadelphia) and Erin Stucky (Children's Hospital San Diego) join JHM as the other 2 new associate editors. Finally, we welcome new Editorial Board members Mary C. Ottolini (Children's National Medical Center), Douglas Carlson (St. Louis Children's Hospital), and Daniel Rauch (NYU Children's Hospital). The welcome addition of these nationally recognized academicians prepares us for continued growth in manuscript submissions to JHM.
Although we could not excel without the editors, reviewers and our terrific new managing editor, Phaedra McGuinness, we would not survive without the authors who submit their manuscripts to JHMthey are responsible for the caliber of the journal, and we are immensely indebted to them. Originally, we hoped to include individuals involved in all aspects of hospital care,1 and fortunately this is now happening. Complementing hospitalists are nurses and pharmacists2 who recognize the importance of teamwork in the care of hospitalized patients. I encourage all members of the hospital care team to send us the results of their research, teaching, and quality improvement efforts.
As the specialty of hospital medicine continues to evolve, now with more than 20,000 hospitalists, JHM will develop with it. I am honored and grateful to collaborate with such a remarkable group of colleagues as we build the premier journal for the fastest growing specialty in the history of medicine in the United States. On to year 3!
P.S. Our tenuous hold on life confronted me this past Thanksgiving holiday. A fellow hospitalist and dear friend died unexpectedly. Two years before, he posted on the wall of the office shared with his colleagues the following quote:
What we do for ourselves fades, but what we do for another may be etched into eternity.
The smile and humanity of John Allen Garner (19632007) is etched into the lives of his family, many friends and colleagues, and innumerable grateful patients.
- .Hospital medicine's evolution—the next steps.J Hosp Med.2006;1:1–2.
- ,,, et al.ASHP–SHM joint statement on hospitalist–pharmacist collaboration.Am J Health‐Syst Pharm.2008;65:260–263.
We live in a moment of history where change is so speeded up that we begin to see the present only when it is already disappearing.
Two years ago we published the first issue of the Journal of Hospital Medicine and declared, Our goal is that JHM become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.1 That first issue was just one of many steps toward this ambition. At the completion of its first year, JHM was selected for indexing and inclusion in the National Library of Medicine's Medical Literature Analysis and Retrieval System Online (MEDLINE), the primary component of PubMed. Following this huge step, we welcomed a remarkable increase in submissions and will have exceeded 300 in our second year, an approximately 50% increase from our first year!
As important, JHM quickly became a valuable benefit of membership in the Society of Hospital Medicine, and the innumerable compliments received by the staff reflect the diligent efforts of a remarkable editorial staff and work by our reviewers. With profound gratitude we list on page 86 these 325 reviewers who donated their priceless time and expertise to enhancing the quality of the manuscripts. To handle the marked increase in submissions, we are expanding and modifying our editorial staff. Please welcome Sunil Kripalani (Vanderbilt) and Daniel Brotman (Johns Hopkins), who join our previous six associate editors and all eight will now serve as JHM's deputy editors. Seven new associate editors also join our team. Among them, Tom Baudendistel (California Pacific Medical Center, San Francisco), Eric Alper (UMass Memorial Health Care, Worcester), Brian Harte (Cleveland Clinic), and Rehan Qayyum (Johns Hopkins) will all focus on optimizing content for practicing hospitalists. Paul Aronowitz will continue to develop our Images section as an associate editor. Recognizing the growing number of pediatric hospitalists, Lisa Zauotis (Childrens Hospital of Philadelphia) and Erin Stucky (Children's Hospital San Diego) join JHM as the other 2 new associate editors. Finally, we welcome new Editorial Board members Mary C. Ottolini (Children's National Medical Center), Douglas Carlson (St. Louis Children's Hospital), and Daniel Rauch (NYU Children's Hospital). The welcome addition of these nationally recognized academicians prepares us for continued growth in manuscript submissions to JHM.
Although we could not excel without the editors, reviewers and our terrific new managing editor, Phaedra McGuinness, we would not survive without the authors who submit their manuscripts to JHMthey are responsible for the caliber of the journal, and we are immensely indebted to them. Originally, we hoped to include individuals involved in all aspects of hospital care,1 and fortunately this is now happening. Complementing hospitalists are nurses and pharmacists2 who recognize the importance of teamwork in the care of hospitalized patients. I encourage all members of the hospital care team to send us the results of their research, teaching, and quality improvement efforts.
As the specialty of hospital medicine continues to evolve, now with more than 20,000 hospitalists, JHM will develop with it. I am honored and grateful to collaborate with such a remarkable group of colleagues as we build the premier journal for the fastest growing specialty in the history of medicine in the United States. On to year 3!
P.S. Our tenuous hold on life confronted me this past Thanksgiving holiday. A fellow hospitalist and dear friend died unexpectedly. Two years before, he posted on the wall of the office shared with his colleagues the following quote:
What we do for ourselves fades, but what we do for another may be etched into eternity.
The smile and humanity of John Allen Garner (19632007) is etched into the lives of his family, many friends and colleagues, and innumerable grateful patients.
We live in a moment of history where change is so speeded up that we begin to see the present only when it is already disappearing.
Two years ago we published the first issue of the Journal of Hospital Medicine and declared, Our goal is that JHM become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.1 That first issue was just one of many steps toward this ambition. At the completion of its first year, JHM was selected for indexing and inclusion in the National Library of Medicine's Medical Literature Analysis and Retrieval System Online (MEDLINE), the primary component of PubMed. Following this huge step, we welcomed a remarkable increase in submissions and will have exceeded 300 in our second year, an approximately 50% increase from our first year!
As important, JHM quickly became a valuable benefit of membership in the Society of Hospital Medicine, and the innumerable compliments received by the staff reflect the diligent efforts of a remarkable editorial staff and work by our reviewers. With profound gratitude we list on page 86 these 325 reviewers who donated their priceless time and expertise to enhancing the quality of the manuscripts. To handle the marked increase in submissions, we are expanding and modifying our editorial staff. Please welcome Sunil Kripalani (Vanderbilt) and Daniel Brotman (Johns Hopkins), who join our previous six associate editors and all eight will now serve as JHM's deputy editors. Seven new associate editors also join our team. Among them, Tom Baudendistel (California Pacific Medical Center, San Francisco), Eric Alper (UMass Memorial Health Care, Worcester), Brian Harte (Cleveland Clinic), and Rehan Qayyum (Johns Hopkins) will all focus on optimizing content for practicing hospitalists. Paul Aronowitz will continue to develop our Images section as an associate editor. Recognizing the growing number of pediatric hospitalists, Lisa Zauotis (Childrens Hospital of Philadelphia) and Erin Stucky (Children's Hospital San Diego) join JHM as the other 2 new associate editors. Finally, we welcome new Editorial Board members Mary C. Ottolini (Children's National Medical Center), Douglas Carlson (St. Louis Children's Hospital), and Daniel Rauch (NYU Children's Hospital). The welcome addition of these nationally recognized academicians prepares us for continued growth in manuscript submissions to JHM.
Although we could not excel without the editors, reviewers and our terrific new managing editor, Phaedra McGuinness, we would not survive without the authors who submit their manuscripts to JHMthey are responsible for the caliber of the journal, and we are immensely indebted to them. Originally, we hoped to include individuals involved in all aspects of hospital care,1 and fortunately this is now happening. Complementing hospitalists are nurses and pharmacists2 who recognize the importance of teamwork in the care of hospitalized patients. I encourage all members of the hospital care team to send us the results of their research, teaching, and quality improvement efforts.
As the specialty of hospital medicine continues to evolve, now with more than 20,000 hospitalists, JHM will develop with it. I am honored and grateful to collaborate with such a remarkable group of colleagues as we build the premier journal for the fastest growing specialty in the history of medicine in the United States. On to year 3!
P.S. Our tenuous hold on life confronted me this past Thanksgiving holiday. A fellow hospitalist and dear friend died unexpectedly. Two years before, he posted on the wall of the office shared with his colleagues the following quote:
What we do for ourselves fades, but what we do for another may be etched into eternity.
The smile and humanity of John Allen Garner (19632007) is etched into the lives of his family, many friends and colleagues, and innumerable grateful patients.
- .Hospital medicine's evolution—the next steps.J Hosp Med.2006;1:1–2.
- ,,, et al.ASHP–SHM joint statement on hospitalist–pharmacist collaboration.Am J Health‐Syst Pharm.2008;65:260–263.
- .Hospital medicine's evolution—the next steps.J Hosp Med.2006;1:1–2.
- ,,, et al.ASHP–SHM joint statement on hospitalist–pharmacist collaboration.Am J Health‐Syst Pharm.2008;65:260–263.
Thinking Inside the Box
A 65‐year‐old man was referred for evaluation of worsening ascites and end‐stage liver disease. The patient had been well until 1 year ago, when he developed lower extremity edema and abdominal distention. After evaluation by his primary care physician, he was given a diagnosis of cryptogenic cirrhosis. He underwent several paracenteses and was placed on furosemide and spironolactone. The patient had been stable on his diuretic regimen until 2 weeks previously, when he suddenly developed worsening edema and ascites, along with dizziness, nausea, and hypotension. His physician stopped the diuretics and referred him to the hospital.
Before diagnosing a patient with cryptogenic cirrhosis, it is necessary to exclude common etiologies of cirrhosis such as alcohol, viral hepatitis, and non‐alcoholic fatty liver disease and numerous uncommon causes, including Wilson's disease, hemochromatosis, Budd‐Chiari, and biliary cirrhosis. It is also important to remember that patients with liver disease are not immune to extrahepatic causes of ascites, such as peritoneal carcinomatosis and tuberculous ascites. Simultaneously, reasons for chronic liver disease decompensating acutely must be considered: medication nonadherence, excess salt intake, hepatotoxicity from acetaminophen or alcohol, and other acute insults, such as hepatocellular carcinoma, an intervening infection (especially spontaneous bacterial peritonitis), ascending cholangitis, or a flare of chronic viral hepatitis.
Past medical and surgical history included diabetes mellitus (diagnosed 10 years previously), obstructive sleep apnea, hypertension, hypothyroidism, and mild chronic kidney disease. Medications included levothyroxine, lactulose, sulfamethoxazole, pioglitazone (started 4 months prior), and ibuprofen. Furosemide and spironolactone had been discontinued 2 weeks previously. He currently resided in the Central Valley of California. He had lived in Thailand from age 7 to 17 and traveled to India more than 1 year ago. He did not smoke and had never used intravenous drugs or received a blood transfusion. He rarely drank alcohol. He worked as a chemist. There was no family history of liver disease.
There is no obvious explanation for the underlying liver disease or the acute decompensation. Sulfamethoxazole is a rare cause of allergic or granulomatous hepatitis. Pioglitazone is a thiazolinedione which in earlier formulations was linked to hepatitis but can be excluded as a cause of this patient's cirrhosis because it was started after liver disease was detected. As a chemist, he might have been exposed to carbon tetrachloride, a known hepatotoxin. Obstructive sleep apnea causes pulmonary hypertension, but severe ascites and acute hepatic decompensation would be unusual. Ibuprofen might precipitate worsening renal function and fluid accumulation. Time in Thailand and India raises the possibility of tuberculous ascites.
The patient had no headache, vision changes, abdominal pain, emesis, melena, hematochezia, chest pain, palpitations, dysuria, polyuria, pruritus, dark urine, or rashes. He reported difficulty with concentration when lactulose was decreased. He noted worsening exercise tolerance with dyspnea after 10 steps and reported a weight gain of 12 pounds in the past 2 weeks.
On examination, temperature was 36.8C; blood pressure, 129/87 mm Hg; heart rate, 85 beats per minute; respirations, 20 per minute; and oxygen saturation, 94% on room air. He was uncomfortable but alert. There was no scleral icterus or conjunctival pallor. Jugular venous pressure was elevated. The lungs were clear, and the heart was regular, with no murmur, rub, or gallops. The abdomen was massively distended with a fluid wave; the liver and spleen could not be palpated. There was pitting edema of the sacrum and lower extremities. There was no asterixis, palmar erythema, spider angiomata, or skin discoloration.
The additional history and physical exam suggest that the primary problem may lie outside the liver, especially as signs of advanced liver disease (other than ascites) are absent. Dyspnea on exertion is consistent with the physical stress of a large volume of ascites or could be secondary to several pulmonary complications associated with liver disease, including portopulmonary hypertension, hepatopulmonary syndrome, or hepatic hydrothorax. Alternatively, the dyspnea raises the possibility that the ascites is not related to a primary liver disorder but rather to anemia or to a cardiac disorder, such as chronic left ventricular failure, isolated right‐sided heart failure, or constrictive pericarditis. These diagnoses are suggested by the elevated jugular venous pressure, which is atypical in cirrhosis.
Although portal hypertension accounts for most cases of ascites, peritoneal fluid should be examined to exclude peritoneal carcinomatosis and tuberculous ascites. I am interested in the results of an echocardiogram.
Initial laboratory studies demonstrated a sodium concentration of 136 mEq/dL; potassium, 4.7 mEq/dL; chloride, 99 mEq/dL; bicarbonate, 24 mEq/dL; blood urea nitrogen, 54 mg/dL; creatinine, 3.3 mg/dL (increased from baseline of 1.6 mg/dL 4 months previously); white cell count, 7000/mm3; hemoglobin, 10.5 g/dL; MCV, 89 fL; platelet count, 205,000/mm3; bilirubin, 0.6 mg/dL; aspartate aminotransferase, 15 U/L; alanine aminotransferase, 8 U/L; alkaline phosphatase, 102 U/L; albumin, 4.2 g/dL; total protein, 8.2 g/dL; international normalized ratio, 1.2; and partial thromboplastin time, 31.8 seconds. A urine dipstick demonstrated 1+ protein. The chest radiograph was normal. Electrocardiogram had borderline low voltage with nonspecific T‐wave abnormalities. Additional studies showed a serum iron concentration of 49 mg/dL, transferrin saturation of 16%, total iron binding capacity of 310 mg/dL, and ferritin of 247 mg/mL. Hemoglobin A1c was 7.0%. Acute and chronic antibodies to hepatitis A, B, and C viruses were negative. The following study results were normal or negative: antinuclear antibody, alpha‐1‐antitrypsin, ceruloplasmin, alpha‐fetoprotein, carcinoembryonic antigen, and 24‐hour urinary copper. The thyroid function studies were normal. A purified protein derivative (PPD) skin test was nonreactive.
There continues to be a paucity of evidence of a primary liver disorder. The hepatic enzymes and tests of liver synthetic function are normal, and there is no pancytopenia, as might result from hypersplenism. I remain most suspicious of either a primary cardiac or pericardial disorder with secondary hepatic congestion or a disease that simultaneously affects the heart and liver.
The reasons for the low voltage on the electrocardiogram include processes that infiltrate the myocardium (amyloidosis, sarcoidosis, hemochromatosis, and myxedema fluid) and processes that increase the distance between the myocardium and surface electrodes, such as adipose tissue, air (from emphysema or pneumothorax), or pericardial effusion. Pericardial effusion may present subacutely with predominant features of right ventricular failure. Low voltage, liver disease, and possible heart failure raise the possibility of amyloidosis or hemochromatosis. The low transferrin saturation renders hemochromatosis unlikely. Although normal alkaline phosphatase and serum albumin are not characteristic when AL amyloid affects the liver and kidneys, serum and urine protein electrophoresis and immunofixation should be considered.
With paracentesis 3.5 L of ascitic fluid was removed. The red cell count was 4000/mm3, and white blood cell count was 505/mm3, of which 25% were polymorphonuclear cells, 22% were lymphocytes, and 53% were monocytes. Additional peritoneal fluid chemistries included albumin of 3.0 g/dL and total protein of 5.3 g/dL. Abdominal ultrasound with Doppler demonstrated a liver of normal size and echogenicity with patent hepatic arteries, hepatic veins, and portal vein. There was mild splenomegaly with normal kidneys. Evaluation for a possible liver transplant was initiated. Blood, urine, and peritoneal fluid cultures demonstrated no growth. Echocardiography demonstrated borderline concentric left ventricular hypertrophy, normal right and left ventricular function, dilated superior and inferior vena cavae, and no pericardial effusion or thickening.
The serum‐ascites albumin gradient (SAAG) of 1.2 is consistent with portal hypertension as the cause of the ascites. The Doppler findings exclude postsinusoidal causes of portal hypertension from hepatic vein obstruction or thrombosis. The combination of the elevated SAAG, elevated jugular venous pressure, borderline low voltage on ECG, and elevated peritoneal total protein make cardiac and pericardial disease the leading considerations. Given the normal ventricular function, I am concerned about elevated intracardiac pressures resulting from pericardial disease or restrictive cardiomyopathy. At this point, right heart catheterization would be useful for assessing intracardiac pressures.
On the fourth hospital day, paracentesis was repeated, and 15 L of fluid was removed. A transjugular liver biopsy demonstrated diffuse patchy fibrosis consistent with early cirrhosis and minor intralobular changes with minimal ballooning. There was no steatosis, active inflammation, granulomata, iron deposition, or evidence of viral hepatitis. Right heart catheterization revealed a right atrial pressure of 18 cm H20, right ventricular pressure of 34/20 cm H20, pulmonary artery pressure of 34/18 cm H20 (mean 25), pulmonary capillary wedge pressure of 20 cm H20, cardiac output of 5.8 L/min, and cardiac index of 2.5 L/min/m2.
The mild hepatic histologic abnormalities do not support an intrinsic liver disease as the cause of his massive ascites and end‐stage liver disease physiology. Cardiac catheterization demonstrates equalization of diastolic pressures, which suggests constrictive pericarditis or restrictive cardiomyopathy. Despite the normal chest radiograph and nonreactive PPD, tuberculosis would be my leading explanation for constrictive pericarditis given the time spent in areas endemic with TB. Although lateral chest radiography may demonstrate pericardial calcifications, magnetic resonance imaging (MRI) is the best imaging modality to detect constrictive pericarditis. Alternately, cardiac amyloidosis could cause restrictive cardiomyopathy and has not been definitively excluded. A cardiac MRI to assess the pericardium would be my next test, and I would request Congo red stains of the liver biopsy. If these tests are unrevealing, endomyocardial biopsy may be necessary.
The cardiac MRI revealed a severely thickened 7‐mm pericardium (normal < 3 mm) most prominent over the right atrium and ventricle. The right ventricle was described as bullet‐shaped, suggesting constrictive pericardial disease (Fig. 1). Left heart catheterization to evaluate coronary anatomy and left ventricular pressures revealed no significant coronary arterial disease and demonstrated an elevated left ventricular end‐diastolic pressure consistent with constrictive pericarditis. Endomyocardial biopsy showed no evidence of infiltrative disease, granulomata, or other significant abnormality. The following day the patient underwent pericardiectomy. Postoperatively, his ascites was easily managed with low doses of diuretics. The pericardial tissue revealed chronic inflammatory cells and dense collagenous fibrosis characteristic of constrictive pericarditis without evidence of malignancy or granulomatous disease. Pericardial cultures were negative for bacteria, viruses, fungi, and mycobacteria.
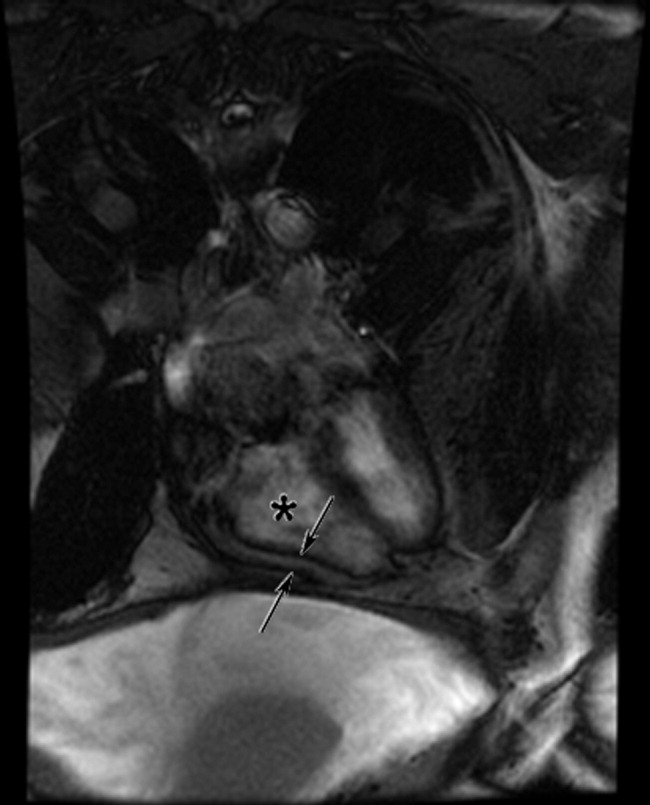
DISCUSSION
Constrictive pericarditis is characterized by chronic fibrous thickening of the once‐elastic pericardial sac and can occur following any disease process that affects the pericardium (Table 1).1, 2 The challenge in the diagnosis of constrictive pericarditis lies in the recognition of this slowly progressive and uncommon disease. In many cases, nonspecific symptoms of reduced cardiac output and insidious right‐sided heart failure are present for 12 months or longer before a diagnosis is established.1, 3 A typical presentation of constrictive pericarditis is peripheral edema, ascites, and hepatomegaly, a combination that may understandably lead to a misdiagnosis of chronic liver disease and even subject a patient to the unnecessary risk of a liver biopsy, as in this case.
|
Cryptogenic cirrhosis, the initial diagnosis of this patient, is a term used only after excluding the common and uncommon causes of cirrhosis (Table 2).46 With expanded knowledge of the causes of cirrhosis, especially nonalcoholic fatty liver disease, the number of cases of cirrhosis considered to be cryptogenic has decreased from nearly one‐third of all cases in 1960 to approximately 5% in a modern series.7, 8 Chronic or repetitive heart failure can lead to progressive hepatic fibrosis and cirrhosis. Distinguishing features compared to other causes of cirrhosis include an ascitic protein concentration greater than 2.5 g/dL, relatively preserved synthetic function, and infrequent stigmata of end‐stage liver disease such as spider angiomata or pronounced jaundice.9, 10
|
Most common
|
Less common
|
A key exam feature that distinguishes cardiac cirrhosis from other causes of liver failure is an elevated jugular venous pressure. Hepatic causes of cirrhosis induce increased nitric oxide production, which leads to splanchnic and peripheral arterial vasodilatation with a reduced effective circulating volume and normal or low jugular venous pressure.11, 12 Therefore, a patient with cirrhosis and ascites having an elevated jugular venous pressure should prompt echocardiographic evaluation.13 When echocardiography excludes ventricular dysfunction, valvular abnormalities, and pulmonary hypertension, constrictive pericarditis and restrictive cardiomyopathy remain important diagnostic considerations.
In both constrictive pericarditis and restrictive cardiomyopathy, ventricular filling is limited. Pressures in the chambers rise abruptly and rapidly during ventricular filling until equilibrium is reached in early diastole. This can be conceptualized as the cardiac chambers being constrained by the limitations of a rigid external box. In constrictive pericarditis, the rigid external box is the fibrosed and thickened pericardial sac, which loses its elasticity and impairs filling of the ventricles. In restrictive cardiomyopathy, the stiff myocardium limits ventricular filling.
There is considerable overlap in the clinical, echocardiographic, and hemodynamic findings of constrictive pericarditis and restrictive cardiomyopathy.14 Both may present insidiously with progressive heart failure. Echocardiography demonstrates impaired diastolic function. Cardiac hemodynamics demonstrate abrupt and rapid early diastolic filling, elevated and equal ventricular end‐diastolic pressures, and reduced stroke volume and cardiac output. A diagnosis of constrictive pericarditis is favored when a marked inspiratory increase in right ventricular pressures and decrease in left ventricular pressures are seen on heart catheterization or a similar inspiratory increase in transvalvular flow velocities across the tricuspid valve compared with the mitral valve is shown by echocardiography. This finding results from normal inspiratory increases in intrathoracic pressures, which are unable to be transmitted through the rigid pericardium but continue to augment venous return to the right side of the heart. As many as one‐third of patients with pericardial constriction lack these characteristic findings on echocardiogram.14
The results of pericardial imaging may suggest a diagnosis of constrictive pericarditis. Lateral chest radiography demonstrates pericardial calcifications in less than 30% of cases.15 Cardiac computed tomography (CT) and MRI are the best imaging modalities for detecting an increase in pericardial thickness (3 mm or greater).16 However, in as many as 20% of patients with surgically confirmed constrictive pericarditis, CT and MRI will demonstrate a pericardium of normal thickness.17
When faced with the diagnostic conundrum of constrictive pericarditis versus restrictive cardiomyopathy, strong clinical suspicion, thorough echocardiography, careful hemodynamic assessment with right and left heart catheterization,14, 18 pericardial imaging, and sometimes endomyocardial biopsy to exclude restrictive cardiomyopathy are often needed before proceeding to pericardiectomy, which carries a significant surgical risk but can also be curative.
This case highlights many of the features of constrictive pericarditis, the challenges and delay in its diagnosis, and its occasional misdiagnosis as chronic liver disease. Clinicians may recognize the typical combination of cirrhosis (or suspected cirrhosis), high SAAG ascites, and edema as characteristic of advanced intrinsic liver disease. However, they must not be seduced into immediate pattern recognition when contrary evidencesuch as elevated neck veins, elevated ascitic total protein, or relatively preserved hepatic synthetic functionaccompanies that picture. Under such circumstances, they must remember to think outside the box and bear in mind that the heart may be trapped inside a box.
Take‐Home Points
-
Constrictive pericarditis is often unrecognized initially, resulting in delayed diagnosis. Patients typically present with nonspecific signs and symptoms of low cardiac output and progressive right‐sided heart failure. Clinical suspicion is key to prompt diagnosis and pericardiectomy, which may be curative.
-
Distinguishing features in the presentation of cardiac or pericardial etiologies of ascites and cirrhosis include elevated neck veins, elevated ascitic protein content, relatively preserved hepatic synthetic function, and absence of the stigmata of end‐stage liver disease.
-
Constrictive pericarditis and restrictive cardiomyopathy can present with a similar clinical picture and hemodynamics showing impaired ventricular filling. Right and left heart catheterization, pericardial imaging, and endomyocardial biopsy may differentiate the 2 conditions. For constrictive pericarditis, surgical and pathological confirmation is the gold standard for diagnosis and the only definitive treatment.
- ,,, et al.Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy.Circulation.1999;100:1380–1386.
- ,,, et al.Constrictive pericarditis: etiology and cause‐specific survival after pericardiectomy.J Am Coll Cardiol.2004;43:1445–1452.
- .Chronic constrictive pericarditis.Am J Cardiol.1961;7:48–61.
- American Gastroenterological Association.AGA technical review on the evaluation of liver chemistry tests.Gastroenterology.2002;123:1367–1384.
- ,.AASLD practice guidelines: evaluation of the patient for liver transplantation.Hepatology.2005;41:1–26.
- Feldman M,Friedman LS,Brandt LJ, eds.Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management.Philadelphia:Saunders Elsevier;2006.
- ,,, et al.Cirrhosis of the liver: a study of alcoholic and nonalcoholic patients in Boston and London.N Engl J Med.1960;261:1–9.
- ,,, et al.Liver transplantation for cryptogenic cirrhosis.Liver Transpl Surg.1997;3:359–364.
- ,,, et al.Heart diseases affecting the liver and liver disease affecting the heart.Am Heart J.2000;140:111–120.
- ,,.The liver in heart failure.Clin Liver Dis.2002;6:947–967.
- ,,, et al.Portal hypertension: from pathophysiology to clinical practice.Liver Int.2005;25:1079–1090.
- .Portal hypertension.Curr Opin Gastroenterol.2006;22:254–262.
- ,,, et al.Negative influences of ascites on the cardiac function of cirrhotic patients.Am J Med.1975;59:165–170.
- .Constrictive pericarditis in the modern era: a diagnostic dilemma.Heart.2001;86:619–623.
- ,,, et al.Calcific constrictive pericarditis: is it still with us?Ann Intern Med.2000;132:444–450.
- ,,,,,.CT and MR imaging of pericardial disease.Radiographics.2003;23:S167–S180.
- ,,, et al.Constrictive pericarditis in 26 patients with histologically normal pericardial thickness.Circulation.2003;108:1852–1857.
- ,,, et al.Value of dynamic respiratory changes in left and right ventricular pressures for the diagnosis of constrictive pericarditis.Circulation.1996;93:2007–2013.
A 65‐year‐old man was referred for evaluation of worsening ascites and end‐stage liver disease. The patient had been well until 1 year ago, when he developed lower extremity edema and abdominal distention. After evaluation by his primary care physician, he was given a diagnosis of cryptogenic cirrhosis. He underwent several paracenteses and was placed on furosemide and spironolactone. The patient had been stable on his diuretic regimen until 2 weeks previously, when he suddenly developed worsening edema and ascites, along with dizziness, nausea, and hypotension. His physician stopped the diuretics and referred him to the hospital.
Before diagnosing a patient with cryptogenic cirrhosis, it is necessary to exclude common etiologies of cirrhosis such as alcohol, viral hepatitis, and non‐alcoholic fatty liver disease and numerous uncommon causes, including Wilson's disease, hemochromatosis, Budd‐Chiari, and biliary cirrhosis. It is also important to remember that patients with liver disease are not immune to extrahepatic causes of ascites, such as peritoneal carcinomatosis and tuberculous ascites. Simultaneously, reasons for chronic liver disease decompensating acutely must be considered: medication nonadherence, excess salt intake, hepatotoxicity from acetaminophen or alcohol, and other acute insults, such as hepatocellular carcinoma, an intervening infection (especially spontaneous bacterial peritonitis), ascending cholangitis, or a flare of chronic viral hepatitis.
Past medical and surgical history included diabetes mellitus (diagnosed 10 years previously), obstructive sleep apnea, hypertension, hypothyroidism, and mild chronic kidney disease. Medications included levothyroxine, lactulose, sulfamethoxazole, pioglitazone (started 4 months prior), and ibuprofen. Furosemide and spironolactone had been discontinued 2 weeks previously. He currently resided in the Central Valley of California. He had lived in Thailand from age 7 to 17 and traveled to India more than 1 year ago. He did not smoke and had never used intravenous drugs or received a blood transfusion. He rarely drank alcohol. He worked as a chemist. There was no family history of liver disease.
There is no obvious explanation for the underlying liver disease or the acute decompensation. Sulfamethoxazole is a rare cause of allergic or granulomatous hepatitis. Pioglitazone is a thiazolinedione which in earlier formulations was linked to hepatitis but can be excluded as a cause of this patient's cirrhosis because it was started after liver disease was detected. As a chemist, he might have been exposed to carbon tetrachloride, a known hepatotoxin. Obstructive sleep apnea causes pulmonary hypertension, but severe ascites and acute hepatic decompensation would be unusual. Ibuprofen might precipitate worsening renal function and fluid accumulation. Time in Thailand and India raises the possibility of tuberculous ascites.
The patient had no headache, vision changes, abdominal pain, emesis, melena, hematochezia, chest pain, palpitations, dysuria, polyuria, pruritus, dark urine, or rashes. He reported difficulty with concentration when lactulose was decreased. He noted worsening exercise tolerance with dyspnea after 10 steps and reported a weight gain of 12 pounds in the past 2 weeks.
On examination, temperature was 36.8C; blood pressure, 129/87 mm Hg; heart rate, 85 beats per minute; respirations, 20 per minute; and oxygen saturation, 94% on room air. He was uncomfortable but alert. There was no scleral icterus or conjunctival pallor. Jugular venous pressure was elevated. The lungs were clear, and the heart was regular, with no murmur, rub, or gallops. The abdomen was massively distended with a fluid wave; the liver and spleen could not be palpated. There was pitting edema of the sacrum and lower extremities. There was no asterixis, palmar erythema, spider angiomata, or skin discoloration.
The additional history and physical exam suggest that the primary problem may lie outside the liver, especially as signs of advanced liver disease (other than ascites) are absent. Dyspnea on exertion is consistent with the physical stress of a large volume of ascites or could be secondary to several pulmonary complications associated with liver disease, including portopulmonary hypertension, hepatopulmonary syndrome, or hepatic hydrothorax. Alternatively, the dyspnea raises the possibility that the ascites is not related to a primary liver disorder but rather to anemia or to a cardiac disorder, such as chronic left ventricular failure, isolated right‐sided heart failure, or constrictive pericarditis. These diagnoses are suggested by the elevated jugular venous pressure, which is atypical in cirrhosis.
Although portal hypertension accounts for most cases of ascites, peritoneal fluid should be examined to exclude peritoneal carcinomatosis and tuberculous ascites. I am interested in the results of an echocardiogram.
Initial laboratory studies demonstrated a sodium concentration of 136 mEq/dL; potassium, 4.7 mEq/dL; chloride, 99 mEq/dL; bicarbonate, 24 mEq/dL; blood urea nitrogen, 54 mg/dL; creatinine, 3.3 mg/dL (increased from baseline of 1.6 mg/dL 4 months previously); white cell count, 7000/mm3; hemoglobin, 10.5 g/dL; MCV, 89 fL; platelet count, 205,000/mm3; bilirubin, 0.6 mg/dL; aspartate aminotransferase, 15 U/L; alanine aminotransferase, 8 U/L; alkaline phosphatase, 102 U/L; albumin, 4.2 g/dL; total protein, 8.2 g/dL; international normalized ratio, 1.2; and partial thromboplastin time, 31.8 seconds. A urine dipstick demonstrated 1+ protein. The chest radiograph was normal. Electrocardiogram had borderline low voltage with nonspecific T‐wave abnormalities. Additional studies showed a serum iron concentration of 49 mg/dL, transferrin saturation of 16%, total iron binding capacity of 310 mg/dL, and ferritin of 247 mg/mL. Hemoglobin A1c was 7.0%. Acute and chronic antibodies to hepatitis A, B, and C viruses were negative. The following study results were normal or negative: antinuclear antibody, alpha‐1‐antitrypsin, ceruloplasmin, alpha‐fetoprotein, carcinoembryonic antigen, and 24‐hour urinary copper. The thyroid function studies were normal. A purified protein derivative (PPD) skin test was nonreactive.
There continues to be a paucity of evidence of a primary liver disorder. The hepatic enzymes and tests of liver synthetic function are normal, and there is no pancytopenia, as might result from hypersplenism. I remain most suspicious of either a primary cardiac or pericardial disorder with secondary hepatic congestion or a disease that simultaneously affects the heart and liver.
The reasons for the low voltage on the electrocardiogram include processes that infiltrate the myocardium (amyloidosis, sarcoidosis, hemochromatosis, and myxedema fluid) and processes that increase the distance between the myocardium and surface electrodes, such as adipose tissue, air (from emphysema or pneumothorax), or pericardial effusion. Pericardial effusion may present subacutely with predominant features of right ventricular failure. Low voltage, liver disease, and possible heart failure raise the possibility of amyloidosis or hemochromatosis. The low transferrin saturation renders hemochromatosis unlikely. Although normal alkaline phosphatase and serum albumin are not characteristic when AL amyloid affects the liver and kidneys, serum and urine protein electrophoresis and immunofixation should be considered.
With paracentesis 3.5 L of ascitic fluid was removed. The red cell count was 4000/mm3, and white blood cell count was 505/mm3, of which 25% were polymorphonuclear cells, 22% were lymphocytes, and 53% were monocytes. Additional peritoneal fluid chemistries included albumin of 3.0 g/dL and total protein of 5.3 g/dL. Abdominal ultrasound with Doppler demonstrated a liver of normal size and echogenicity with patent hepatic arteries, hepatic veins, and portal vein. There was mild splenomegaly with normal kidneys. Evaluation for a possible liver transplant was initiated. Blood, urine, and peritoneal fluid cultures demonstrated no growth. Echocardiography demonstrated borderline concentric left ventricular hypertrophy, normal right and left ventricular function, dilated superior and inferior vena cavae, and no pericardial effusion or thickening.
The serum‐ascites albumin gradient (SAAG) of 1.2 is consistent with portal hypertension as the cause of the ascites. The Doppler findings exclude postsinusoidal causes of portal hypertension from hepatic vein obstruction or thrombosis. The combination of the elevated SAAG, elevated jugular venous pressure, borderline low voltage on ECG, and elevated peritoneal total protein make cardiac and pericardial disease the leading considerations. Given the normal ventricular function, I am concerned about elevated intracardiac pressures resulting from pericardial disease or restrictive cardiomyopathy. At this point, right heart catheterization would be useful for assessing intracardiac pressures.
On the fourth hospital day, paracentesis was repeated, and 15 L of fluid was removed. A transjugular liver biopsy demonstrated diffuse patchy fibrosis consistent with early cirrhosis and minor intralobular changes with minimal ballooning. There was no steatosis, active inflammation, granulomata, iron deposition, or evidence of viral hepatitis. Right heart catheterization revealed a right atrial pressure of 18 cm H20, right ventricular pressure of 34/20 cm H20, pulmonary artery pressure of 34/18 cm H20 (mean 25), pulmonary capillary wedge pressure of 20 cm H20, cardiac output of 5.8 L/min, and cardiac index of 2.5 L/min/m2.
The mild hepatic histologic abnormalities do not support an intrinsic liver disease as the cause of his massive ascites and end‐stage liver disease physiology. Cardiac catheterization demonstrates equalization of diastolic pressures, which suggests constrictive pericarditis or restrictive cardiomyopathy. Despite the normal chest radiograph and nonreactive PPD, tuberculosis would be my leading explanation for constrictive pericarditis given the time spent in areas endemic with TB. Although lateral chest radiography may demonstrate pericardial calcifications, magnetic resonance imaging (MRI) is the best imaging modality to detect constrictive pericarditis. Alternately, cardiac amyloidosis could cause restrictive cardiomyopathy and has not been definitively excluded. A cardiac MRI to assess the pericardium would be my next test, and I would request Congo red stains of the liver biopsy. If these tests are unrevealing, endomyocardial biopsy may be necessary.
The cardiac MRI revealed a severely thickened 7‐mm pericardium (normal < 3 mm) most prominent over the right atrium and ventricle. The right ventricle was described as bullet‐shaped, suggesting constrictive pericardial disease (Fig. 1). Left heart catheterization to evaluate coronary anatomy and left ventricular pressures revealed no significant coronary arterial disease and demonstrated an elevated left ventricular end‐diastolic pressure consistent with constrictive pericarditis. Endomyocardial biopsy showed no evidence of infiltrative disease, granulomata, or other significant abnormality. The following day the patient underwent pericardiectomy. Postoperatively, his ascites was easily managed with low doses of diuretics. The pericardial tissue revealed chronic inflammatory cells and dense collagenous fibrosis characteristic of constrictive pericarditis without evidence of malignancy or granulomatous disease. Pericardial cultures were negative for bacteria, viruses, fungi, and mycobacteria.
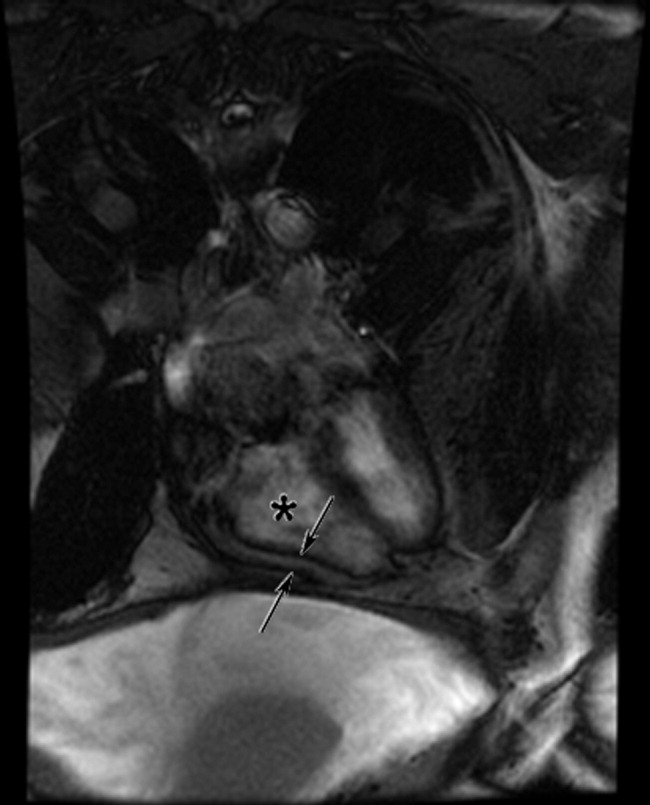
DISCUSSION
Constrictive pericarditis is characterized by chronic fibrous thickening of the once‐elastic pericardial sac and can occur following any disease process that affects the pericardium (Table 1).1, 2 The challenge in the diagnosis of constrictive pericarditis lies in the recognition of this slowly progressive and uncommon disease. In many cases, nonspecific symptoms of reduced cardiac output and insidious right‐sided heart failure are present for 12 months or longer before a diagnosis is established.1, 3 A typical presentation of constrictive pericarditis is peripheral edema, ascites, and hepatomegaly, a combination that may understandably lead to a misdiagnosis of chronic liver disease and even subject a patient to the unnecessary risk of a liver biopsy, as in this case.
|
Cryptogenic cirrhosis, the initial diagnosis of this patient, is a term used only after excluding the common and uncommon causes of cirrhosis (Table 2).46 With expanded knowledge of the causes of cirrhosis, especially nonalcoholic fatty liver disease, the number of cases of cirrhosis considered to be cryptogenic has decreased from nearly one‐third of all cases in 1960 to approximately 5% in a modern series.7, 8 Chronic or repetitive heart failure can lead to progressive hepatic fibrosis and cirrhosis. Distinguishing features compared to other causes of cirrhosis include an ascitic protein concentration greater than 2.5 g/dL, relatively preserved synthetic function, and infrequent stigmata of end‐stage liver disease such as spider angiomata or pronounced jaundice.9, 10
|
Most common
|
Less common
|
A key exam feature that distinguishes cardiac cirrhosis from other causes of liver failure is an elevated jugular venous pressure. Hepatic causes of cirrhosis induce increased nitric oxide production, which leads to splanchnic and peripheral arterial vasodilatation with a reduced effective circulating volume and normal or low jugular venous pressure.11, 12 Therefore, a patient with cirrhosis and ascites having an elevated jugular venous pressure should prompt echocardiographic evaluation.13 When echocardiography excludes ventricular dysfunction, valvular abnormalities, and pulmonary hypertension, constrictive pericarditis and restrictive cardiomyopathy remain important diagnostic considerations.
In both constrictive pericarditis and restrictive cardiomyopathy, ventricular filling is limited. Pressures in the chambers rise abruptly and rapidly during ventricular filling until equilibrium is reached in early diastole. This can be conceptualized as the cardiac chambers being constrained by the limitations of a rigid external box. In constrictive pericarditis, the rigid external box is the fibrosed and thickened pericardial sac, which loses its elasticity and impairs filling of the ventricles. In restrictive cardiomyopathy, the stiff myocardium limits ventricular filling.
There is considerable overlap in the clinical, echocardiographic, and hemodynamic findings of constrictive pericarditis and restrictive cardiomyopathy.14 Both may present insidiously with progressive heart failure. Echocardiography demonstrates impaired diastolic function. Cardiac hemodynamics demonstrate abrupt and rapid early diastolic filling, elevated and equal ventricular end‐diastolic pressures, and reduced stroke volume and cardiac output. A diagnosis of constrictive pericarditis is favored when a marked inspiratory increase in right ventricular pressures and decrease in left ventricular pressures are seen on heart catheterization or a similar inspiratory increase in transvalvular flow velocities across the tricuspid valve compared with the mitral valve is shown by echocardiography. This finding results from normal inspiratory increases in intrathoracic pressures, which are unable to be transmitted through the rigid pericardium but continue to augment venous return to the right side of the heart. As many as one‐third of patients with pericardial constriction lack these characteristic findings on echocardiogram.14
The results of pericardial imaging may suggest a diagnosis of constrictive pericarditis. Lateral chest radiography demonstrates pericardial calcifications in less than 30% of cases.15 Cardiac computed tomography (CT) and MRI are the best imaging modalities for detecting an increase in pericardial thickness (3 mm or greater).16 However, in as many as 20% of patients with surgically confirmed constrictive pericarditis, CT and MRI will demonstrate a pericardium of normal thickness.17
When faced with the diagnostic conundrum of constrictive pericarditis versus restrictive cardiomyopathy, strong clinical suspicion, thorough echocardiography, careful hemodynamic assessment with right and left heart catheterization,14, 18 pericardial imaging, and sometimes endomyocardial biopsy to exclude restrictive cardiomyopathy are often needed before proceeding to pericardiectomy, which carries a significant surgical risk but can also be curative.
This case highlights many of the features of constrictive pericarditis, the challenges and delay in its diagnosis, and its occasional misdiagnosis as chronic liver disease. Clinicians may recognize the typical combination of cirrhosis (or suspected cirrhosis), high SAAG ascites, and edema as characteristic of advanced intrinsic liver disease. However, they must not be seduced into immediate pattern recognition when contrary evidencesuch as elevated neck veins, elevated ascitic total protein, or relatively preserved hepatic synthetic functionaccompanies that picture. Under such circumstances, they must remember to think outside the box and bear in mind that the heart may be trapped inside a box.
Take‐Home Points
-
Constrictive pericarditis is often unrecognized initially, resulting in delayed diagnosis. Patients typically present with nonspecific signs and symptoms of low cardiac output and progressive right‐sided heart failure. Clinical suspicion is key to prompt diagnosis and pericardiectomy, which may be curative.
-
Distinguishing features in the presentation of cardiac or pericardial etiologies of ascites and cirrhosis include elevated neck veins, elevated ascitic protein content, relatively preserved hepatic synthetic function, and absence of the stigmata of end‐stage liver disease.
-
Constrictive pericarditis and restrictive cardiomyopathy can present with a similar clinical picture and hemodynamics showing impaired ventricular filling. Right and left heart catheterization, pericardial imaging, and endomyocardial biopsy may differentiate the 2 conditions. For constrictive pericarditis, surgical and pathological confirmation is the gold standard for diagnosis and the only definitive treatment.
A 65‐year‐old man was referred for evaluation of worsening ascites and end‐stage liver disease. The patient had been well until 1 year ago, when he developed lower extremity edema and abdominal distention. After evaluation by his primary care physician, he was given a diagnosis of cryptogenic cirrhosis. He underwent several paracenteses and was placed on furosemide and spironolactone. The patient had been stable on his diuretic regimen until 2 weeks previously, when he suddenly developed worsening edema and ascites, along with dizziness, nausea, and hypotension. His physician stopped the diuretics and referred him to the hospital.
Before diagnosing a patient with cryptogenic cirrhosis, it is necessary to exclude common etiologies of cirrhosis such as alcohol, viral hepatitis, and non‐alcoholic fatty liver disease and numerous uncommon causes, including Wilson's disease, hemochromatosis, Budd‐Chiari, and biliary cirrhosis. It is also important to remember that patients with liver disease are not immune to extrahepatic causes of ascites, such as peritoneal carcinomatosis and tuberculous ascites. Simultaneously, reasons for chronic liver disease decompensating acutely must be considered: medication nonadherence, excess salt intake, hepatotoxicity from acetaminophen or alcohol, and other acute insults, such as hepatocellular carcinoma, an intervening infection (especially spontaneous bacterial peritonitis), ascending cholangitis, or a flare of chronic viral hepatitis.
Past medical and surgical history included diabetes mellitus (diagnosed 10 years previously), obstructive sleep apnea, hypertension, hypothyroidism, and mild chronic kidney disease. Medications included levothyroxine, lactulose, sulfamethoxazole, pioglitazone (started 4 months prior), and ibuprofen. Furosemide and spironolactone had been discontinued 2 weeks previously. He currently resided in the Central Valley of California. He had lived in Thailand from age 7 to 17 and traveled to India more than 1 year ago. He did not smoke and had never used intravenous drugs or received a blood transfusion. He rarely drank alcohol. He worked as a chemist. There was no family history of liver disease.
There is no obvious explanation for the underlying liver disease or the acute decompensation. Sulfamethoxazole is a rare cause of allergic or granulomatous hepatitis. Pioglitazone is a thiazolinedione which in earlier formulations was linked to hepatitis but can be excluded as a cause of this patient's cirrhosis because it was started after liver disease was detected. As a chemist, he might have been exposed to carbon tetrachloride, a known hepatotoxin. Obstructive sleep apnea causes pulmonary hypertension, but severe ascites and acute hepatic decompensation would be unusual. Ibuprofen might precipitate worsening renal function and fluid accumulation. Time in Thailand and India raises the possibility of tuberculous ascites.
The patient had no headache, vision changes, abdominal pain, emesis, melena, hematochezia, chest pain, palpitations, dysuria, polyuria, pruritus, dark urine, or rashes. He reported difficulty with concentration when lactulose was decreased. He noted worsening exercise tolerance with dyspnea after 10 steps and reported a weight gain of 12 pounds in the past 2 weeks.
On examination, temperature was 36.8C; blood pressure, 129/87 mm Hg; heart rate, 85 beats per minute; respirations, 20 per minute; and oxygen saturation, 94% on room air. He was uncomfortable but alert. There was no scleral icterus or conjunctival pallor. Jugular venous pressure was elevated. The lungs were clear, and the heart was regular, with no murmur, rub, or gallops. The abdomen was massively distended with a fluid wave; the liver and spleen could not be palpated. There was pitting edema of the sacrum and lower extremities. There was no asterixis, palmar erythema, spider angiomata, or skin discoloration.
The additional history and physical exam suggest that the primary problem may lie outside the liver, especially as signs of advanced liver disease (other than ascites) are absent. Dyspnea on exertion is consistent with the physical stress of a large volume of ascites or could be secondary to several pulmonary complications associated with liver disease, including portopulmonary hypertension, hepatopulmonary syndrome, or hepatic hydrothorax. Alternatively, the dyspnea raises the possibility that the ascites is not related to a primary liver disorder but rather to anemia or to a cardiac disorder, such as chronic left ventricular failure, isolated right‐sided heart failure, or constrictive pericarditis. These diagnoses are suggested by the elevated jugular venous pressure, which is atypical in cirrhosis.
Although portal hypertension accounts for most cases of ascites, peritoneal fluid should be examined to exclude peritoneal carcinomatosis and tuberculous ascites. I am interested in the results of an echocardiogram.
Initial laboratory studies demonstrated a sodium concentration of 136 mEq/dL; potassium, 4.7 mEq/dL; chloride, 99 mEq/dL; bicarbonate, 24 mEq/dL; blood urea nitrogen, 54 mg/dL; creatinine, 3.3 mg/dL (increased from baseline of 1.6 mg/dL 4 months previously); white cell count, 7000/mm3; hemoglobin, 10.5 g/dL; MCV, 89 fL; platelet count, 205,000/mm3; bilirubin, 0.6 mg/dL; aspartate aminotransferase, 15 U/L; alanine aminotransferase, 8 U/L; alkaline phosphatase, 102 U/L; albumin, 4.2 g/dL; total protein, 8.2 g/dL; international normalized ratio, 1.2; and partial thromboplastin time, 31.8 seconds. A urine dipstick demonstrated 1+ protein. The chest radiograph was normal. Electrocardiogram had borderline low voltage with nonspecific T‐wave abnormalities. Additional studies showed a serum iron concentration of 49 mg/dL, transferrin saturation of 16%, total iron binding capacity of 310 mg/dL, and ferritin of 247 mg/mL. Hemoglobin A1c was 7.0%. Acute and chronic antibodies to hepatitis A, B, and C viruses were negative. The following study results were normal or negative: antinuclear antibody, alpha‐1‐antitrypsin, ceruloplasmin, alpha‐fetoprotein, carcinoembryonic antigen, and 24‐hour urinary copper. The thyroid function studies were normal. A purified protein derivative (PPD) skin test was nonreactive.
There continues to be a paucity of evidence of a primary liver disorder. The hepatic enzymes and tests of liver synthetic function are normal, and there is no pancytopenia, as might result from hypersplenism. I remain most suspicious of either a primary cardiac or pericardial disorder with secondary hepatic congestion or a disease that simultaneously affects the heart and liver.
The reasons for the low voltage on the electrocardiogram include processes that infiltrate the myocardium (amyloidosis, sarcoidosis, hemochromatosis, and myxedema fluid) and processes that increase the distance between the myocardium and surface electrodes, such as adipose tissue, air (from emphysema or pneumothorax), or pericardial effusion. Pericardial effusion may present subacutely with predominant features of right ventricular failure. Low voltage, liver disease, and possible heart failure raise the possibility of amyloidosis or hemochromatosis. The low transferrin saturation renders hemochromatosis unlikely. Although normal alkaline phosphatase and serum albumin are not characteristic when AL amyloid affects the liver and kidneys, serum and urine protein electrophoresis and immunofixation should be considered.
With paracentesis 3.5 L of ascitic fluid was removed. The red cell count was 4000/mm3, and white blood cell count was 505/mm3, of which 25% were polymorphonuclear cells, 22% were lymphocytes, and 53% were monocytes. Additional peritoneal fluid chemistries included albumin of 3.0 g/dL and total protein of 5.3 g/dL. Abdominal ultrasound with Doppler demonstrated a liver of normal size and echogenicity with patent hepatic arteries, hepatic veins, and portal vein. There was mild splenomegaly with normal kidneys. Evaluation for a possible liver transplant was initiated. Blood, urine, and peritoneal fluid cultures demonstrated no growth. Echocardiography demonstrated borderline concentric left ventricular hypertrophy, normal right and left ventricular function, dilated superior and inferior vena cavae, and no pericardial effusion or thickening.
The serum‐ascites albumin gradient (SAAG) of 1.2 is consistent with portal hypertension as the cause of the ascites. The Doppler findings exclude postsinusoidal causes of portal hypertension from hepatic vein obstruction or thrombosis. The combination of the elevated SAAG, elevated jugular venous pressure, borderline low voltage on ECG, and elevated peritoneal total protein make cardiac and pericardial disease the leading considerations. Given the normal ventricular function, I am concerned about elevated intracardiac pressures resulting from pericardial disease or restrictive cardiomyopathy. At this point, right heart catheterization would be useful for assessing intracardiac pressures.
On the fourth hospital day, paracentesis was repeated, and 15 L of fluid was removed. A transjugular liver biopsy demonstrated diffuse patchy fibrosis consistent with early cirrhosis and minor intralobular changes with minimal ballooning. There was no steatosis, active inflammation, granulomata, iron deposition, or evidence of viral hepatitis. Right heart catheterization revealed a right atrial pressure of 18 cm H20, right ventricular pressure of 34/20 cm H20, pulmonary artery pressure of 34/18 cm H20 (mean 25), pulmonary capillary wedge pressure of 20 cm H20, cardiac output of 5.8 L/min, and cardiac index of 2.5 L/min/m2.
The mild hepatic histologic abnormalities do not support an intrinsic liver disease as the cause of his massive ascites and end‐stage liver disease physiology. Cardiac catheterization demonstrates equalization of diastolic pressures, which suggests constrictive pericarditis or restrictive cardiomyopathy. Despite the normal chest radiograph and nonreactive PPD, tuberculosis would be my leading explanation for constrictive pericarditis given the time spent in areas endemic with TB. Although lateral chest radiography may demonstrate pericardial calcifications, magnetic resonance imaging (MRI) is the best imaging modality to detect constrictive pericarditis. Alternately, cardiac amyloidosis could cause restrictive cardiomyopathy and has not been definitively excluded. A cardiac MRI to assess the pericardium would be my next test, and I would request Congo red stains of the liver biopsy. If these tests are unrevealing, endomyocardial biopsy may be necessary.
The cardiac MRI revealed a severely thickened 7‐mm pericardium (normal < 3 mm) most prominent over the right atrium and ventricle. The right ventricle was described as bullet‐shaped, suggesting constrictive pericardial disease (Fig. 1). Left heart catheterization to evaluate coronary anatomy and left ventricular pressures revealed no significant coronary arterial disease and demonstrated an elevated left ventricular end‐diastolic pressure consistent with constrictive pericarditis. Endomyocardial biopsy showed no evidence of infiltrative disease, granulomata, or other significant abnormality. The following day the patient underwent pericardiectomy. Postoperatively, his ascites was easily managed with low doses of diuretics. The pericardial tissue revealed chronic inflammatory cells and dense collagenous fibrosis characteristic of constrictive pericarditis without evidence of malignancy or granulomatous disease. Pericardial cultures were negative for bacteria, viruses, fungi, and mycobacteria.
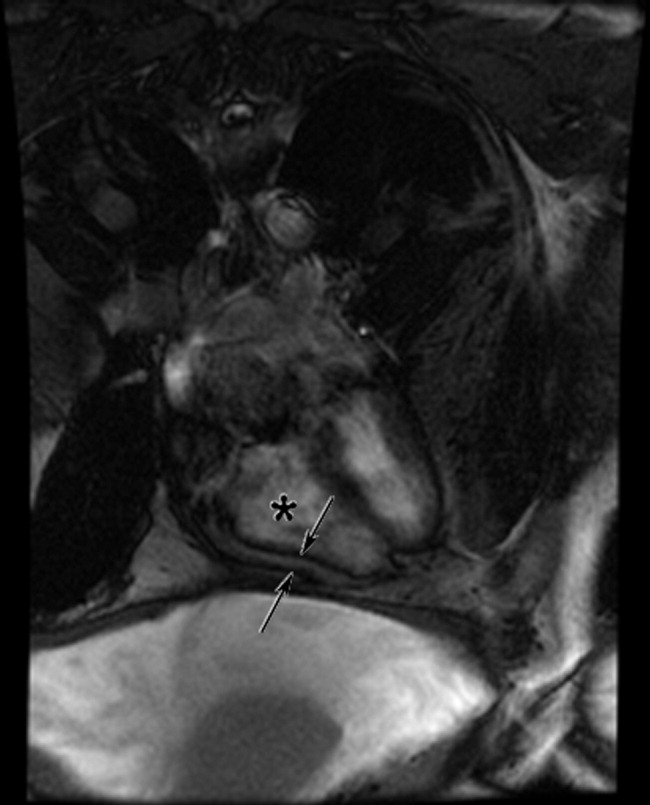
DISCUSSION
Constrictive pericarditis is characterized by chronic fibrous thickening of the once‐elastic pericardial sac and can occur following any disease process that affects the pericardium (Table 1).1, 2 The challenge in the diagnosis of constrictive pericarditis lies in the recognition of this slowly progressive and uncommon disease. In many cases, nonspecific symptoms of reduced cardiac output and insidious right‐sided heart failure are present for 12 months or longer before a diagnosis is established.1, 3 A typical presentation of constrictive pericarditis is peripheral edema, ascites, and hepatomegaly, a combination that may understandably lead to a misdiagnosis of chronic liver disease and even subject a patient to the unnecessary risk of a liver biopsy, as in this case.
|
Cryptogenic cirrhosis, the initial diagnosis of this patient, is a term used only after excluding the common and uncommon causes of cirrhosis (Table 2).46 With expanded knowledge of the causes of cirrhosis, especially nonalcoholic fatty liver disease, the number of cases of cirrhosis considered to be cryptogenic has decreased from nearly one‐third of all cases in 1960 to approximately 5% in a modern series.7, 8 Chronic or repetitive heart failure can lead to progressive hepatic fibrosis and cirrhosis. Distinguishing features compared to other causes of cirrhosis include an ascitic protein concentration greater than 2.5 g/dL, relatively preserved synthetic function, and infrequent stigmata of end‐stage liver disease such as spider angiomata or pronounced jaundice.9, 10
|
Most common
|
Less common
|
A key exam feature that distinguishes cardiac cirrhosis from other causes of liver failure is an elevated jugular venous pressure. Hepatic causes of cirrhosis induce increased nitric oxide production, which leads to splanchnic and peripheral arterial vasodilatation with a reduced effective circulating volume and normal or low jugular venous pressure.11, 12 Therefore, a patient with cirrhosis and ascites having an elevated jugular venous pressure should prompt echocardiographic evaluation.13 When echocardiography excludes ventricular dysfunction, valvular abnormalities, and pulmonary hypertension, constrictive pericarditis and restrictive cardiomyopathy remain important diagnostic considerations.
In both constrictive pericarditis and restrictive cardiomyopathy, ventricular filling is limited. Pressures in the chambers rise abruptly and rapidly during ventricular filling until equilibrium is reached in early diastole. This can be conceptualized as the cardiac chambers being constrained by the limitations of a rigid external box. In constrictive pericarditis, the rigid external box is the fibrosed and thickened pericardial sac, which loses its elasticity and impairs filling of the ventricles. In restrictive cardiomyopathy, the stiff myocardium limits ventricular filling.
There is considerable overlap in the clinical, echocardiographic, and hemodynamic findings of constrictive pericarditis and restrictive cardiomyopathy.14 Both may present insidiously with progressive heart failure. Echocardiography demonstrates impaired diastolic function. Cardiac hemodynamics demonstrate abrupt and rapid early diastolic filling, elevated and equal ventricular end‐diastolic pressures, and reduced stroke volume and cardiac output. A diagnosis of constrictive pericarditis is favored when a marked inspiratory increase in right ventricular pressures and decrease in left ventricular pressures are seen on heart catheterization or a similar inspiratory increase in transvalvular flow velocities across the tricuspid valve compared with the mitral valve is shown by echocardiography. This finding results from normal inspiratory increases in intrathoracic pressures, which are unable to be transmitted through the rigid pericardium but continue to augment venous return to the right side of the heart. As many as one‐third of patients with pericardial constriction lack these characteristic findings on echocardiogram.14
The results of pericardial imaging may suggest a diagnosis of constrictive pericarditis. Lateral chest radiography demonstrates pericardial calcifications in less than 30% of cases.15 Cardiac computed tomography (CT) and MRI are the best imaging modalities for detecting an increase in pericardial thickness (3 mm or greater).16 However, in as many as 20% of patients with surgically confirmed constrictive pericarditis, CT and MRI will demonstrate a pericardium of normal thickness.17
When faced with the diagnostic conundrum of constrictive pericarditis versus restrictive cardiomyopathy, strong clinical suspicion, thorough echocardiography, careful hemodynamic assessment with right and left heart catheterization,14, 18 pericardial imaging, and sometimes endomyocardial biopsy to exclude restrictive cardiomyopathy are often needed before proceeding to pericardiectomy, which carries a significant surgical risk but can also be curative.
This case highlights many of the features of constrictive pericarditis, the challenges and delay in its diagnosis, and its occasional misdiagnosis as chronic liver disease. Clinicians may recognize the typical combination of cirrhosis (or suspected cirrhosis), high SAAG ascites, and edema as characteristic of advanced intrinsic liver disease. However, they must not be seduced into immediate pattern recognition when contrary evidencesuch as elevated neck veins, elevated ascitic total protein, or relatively preserved hepatic synthetic functionaccompanies that picture. Under such circumstances, they must remember to think outside the box and bear in mind that the heart may be trapped inside a box.
Take‐Home Points
-
Constrictive pericarditis is often unrecognized initially, resulting in delayed diagnosis. Patients typically present with nonspecific signs and symptoms of low cardiac output and progressive right‐sided heart failure. Clinical suspicion is key to prompt diagnosis and pericardiectomy, which may be curative.
-
Distinguishing features in the presentation of cardiac or pericardial etiologies of ascites and cirrhosis include elevated neck veins, elevated ascitic protein content, relatively preserved hepatic synthetic function, and absence of the stigmata of end‐stage liver disease.
-
Constrictive pericarditis and restrictive cardiomyopathy can present with a similar clinical picture and hemodynamics showing impaired ventricular filling. Right and left heart catheterization, pericardial imaging, and endomyocardial biopsy may differentiate the 2 conditions. For constrictive pericarditis, surgical and pathological confirmation is the gold standard for diagnosis and the only definitive treatment.
- ,,, et al.Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy.Circulation.1999;100:1380–1386.
- ,,, et al.Constrictive pericarditis: etiology and cause‐specific survival after pericardiectomy.J Am Coll Cardiol.2004;43:1445–1452.
- .Chronic constrictive pericarditis.Am J Cardiol.1961;7:48–61.
- American Gastroenterological Association.AGA technical review on the evaluation of liver chemistry tests.Gastroenterology.2002;123:1367–1384.
- ,.AASLD practice guidelines: evaluation of the patient for liver transplantation.Hepatology.2005;41:1–26.
- Feldman M,Friedman LS,Brandt LJ, eds.Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management.Philadelphia:Saunders Elsevier;2006.
- ,,, et al.Cirrhosis of the liver: a study of alcoholic and nonalcoholic patients in Boston and London.N Engl J Med.1960;261:1–9.
- ,,, et al.Liver transplantation for cryptogenic cirrhosis.Liver Transpl Surg.1997;3:359–364.
- ,,, et al.Heart diseases affecting the liver and liver disease affecting the heart.Am Heart J.2000;140:111–120.
- ,,.The liver in heart failure.Clin Liver Dis.2002;6:947–967.
- ,,, et al.Portal hypertension: from pathophysiology to clinical practice.Liver Int.2005;25:1079–1090.
- .Portal hypertension.Curr Opin Gastroenterol.2006;22:254–262.
- ,,, et al.Negative influences of ascites on the cardiac function of cirrhotic patients.Am J Med.1975;59:165–170.
- .Constrictive pericarditis in the modern era: a diagnostic dilemma.Heart.2001;86:619–623.
- ,,, et al.Calcific constrictive pericarditis: is it still with us?Ann Intern Med.2000;132:444–450.
- ,,,,,.CT and MR imaging of pericardial disease.Radiographics.2003;23:S167–S180.
- ,,, et al.Constrictive pericarditis in 26 patients with histologically normal pericardial thickness.Circulation.2003;108:1852–1857.
- ,,, et al.Value of dynamic respiratory changes in left and right ventricular pressures for the diagnosis of constrictive pericarditis.Circulation.1996;93:2007–2013.
- ,,, et al.Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy.Circulation.1999;100:1380–1386.
- ,,, et al.Constrictive pericarditis: etiology and cause‐specific survival after pericardiectomy.J Am Coll Cardiol.2004;43:1445–1452.
- .Chronic constrictive pericarditis.Am J Cardiol.1961;7:48–61.
- American Gastroenterological Association.AGA technical review on the evaluation of liver chemistry tests.Gastroenterology.2002;123:1367–1384.
- ,.AASLD practice guidelines: evaluation of the patient for liver transplantation.Hepatology.2005;41:1–26.
- Feldman M,Friedman LS,Brandt LJ, eds.Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management.Philadelphia:Saunders Elsevier;2006.
- ,,, et al.Cirrhosis of the liver: a study of alcoholic and nonalcoholic patients in Boston and London.N Engl J Med.1960;261:1–9.
- ,,, et al.Liver transplantation for cryptogenic cirrhosis.Liver Transpl Surg.1997;3:359–364.
- ,,, et al.Heart diseases affecting the liver and liver disease affecting the heart.Am Heart J.2000;140:111–120.
- ,,.The liver in heart failure.Clin Liver Dis.2002;6:947–967.
- ,,, et al.Portal hypertension: from pathophysiology to clinical practice.Liver Int.2005;25:1079–1090.
- .Portal hypertension.Curr Opin Gastroenterol.2006;22:254–262.
- ,,, et al.Negative influences of ascites on the cardiac function of cirrhotic patients.Am J Med.1975;59:165–170.
- .Constrictive pericarditis in the modern era: a diagnostic dilemma.Heart.2001;86:619–623.
- ,,, et al.Calcific constrictive pericarditis: is it still with us?Ann Intern Med.2000;132:444–450.
- ,,,,,.CT and MR imaging of pericardial disease.Radiographics.2003;23:S167–S180.
- ,,, et al.Constrictive pericarditis in 26 patients with histologically normal pericardial thickness.Circulation.2003;108:1852–1857.
- ,,, et al.Value of dynamic respiratory changes in left and right ventricular pressures for the diagnosis of constrictive pericarditis.Circulation.1996;93:2007–2013.
Annual reviewers list
We deeply appreciate the involvement of our reviewers who made the Journal of Hospital Medicine so successful in its second year. Listed below are the many reviewers and volume of their contributions. They have our sincere gratitude.
Reviewed 4 or More Articles
Thomas E. Baudendistel (7)
Renee Patrice Bullock‐Palmer (4)
Vincent W. Chiang (4)
Jasminka M. Criley (4)
Gurpreet Dhaliwal (6)
Lorenzo Di Francesco (4)
Dana Edelson, MD (7)
Kellie L. Flood (5)
Jeffrey Glasheen (5)
Jeffrey L. Greenwald (4)
Brian Harte (11)
Sunil Kripalani (4)
Matthew Landler (4)
Greg Maynard (5)
Kevin J. O'Leary (4)
Sameer Parikh (6)
James C. Pile (6)
Jason S. Schneider (4)
Doug Wright (4)
Reviewed 3 Articles
Eric Alper
Alpesh Amin
Robert Neal Axon
David L. Blazes
Douglas Carlson
Param Dedhia
Margaret Fang
Jonathan M. Flacker
Rajesh Garg
Stephanie Grossman
Daniel Payson Hunt
Christopher Seoung Kim
Christopher P. Landrigan
Kristine H. Lethert
Marcia Levetown
David Liebovitz
David Likosky
Navneet Majhail
Jennifer Myers
Janet Nagamine
Daniel A. Rauch
Steve Ross
Danielle Bowen Scheurer
Jeffrey Lawrence Schnipper
Hiren Shah
Jason Stein
Reviewed 2 Articles
Nasim Afsarmanesh
Mel L. Anderson III
Vineet Arora
John Banja
Susan S. Braithwaite
Cynthia Jean Brown
Daniel Seth Budnitz
Beril Cakir
Rachel N. Caskey
Murtaza Cassoobhoy
Eva Chittenden
Eugene Shu‐Sen Chu
Steven L. Cohn
Randolph Cole
Nathan T. Connell
Richard I. Cook
Aashish Didwania
Daniel David Dressler
Matthew Eisen
Terry England
Leonard Samuel Feldman
Regina Fink
Raminder Singh Gill
Philip H. Goodman
Mohan Gounder
Susan Grant
Paul Grant
Sajeev Handa
Jeanne M. Huddleston
Carlos Manuel Isada
Amir K. Jaffer
Peter John Kaboli
Jennifer Kapo
Ariel R. Katz
Ujjaini Khanderia
Lisa Kirkland
Cindy J. Lai
Cecilia Lansang
Michael Edwin Lazarus
Bennett Leslie
Blake J. Lesselroth
Lee Lindquist
Michael Lubin
Michelle Magee
David Malkenson
Michael Matheny
Laurence McMahon
Donna Leco Mercado
Melissa Munsell
Brahmajee Nallamothu
James Newman
Vikas Parekh
Mohammed A. Qadeer
Kara Quan
Cate E. Ranheim
Sumant Ranji
Gustavo Rivero
John James Ross
Richard Saitz
Elias G. Sakalis
Maryam Sattari
Bradley Allen Sharpe
Tamara D. Simon
Jeff Sperring
Erin Stucky
Rebecca Sudore
Patrick John Torcson
Arpana Vidyarthi
Diane B. Wayne
Chad Whelan
Stephen Wilson
Jeanie Youngwerth
Iris Yung
Lisa B. Zaoutis
Thomas Zipp
Reviewed 1 Article
Adebola Adesanya
Deborah Adey
Bianca Borges Afonso
Dewesh Agrawal
Meenakshy Aiyer
Richard Keith Albert
Shafic S. Al‐Nammari
Wendy Anderson
Ashish Aneja
Armand H. M. Antommaria
Paul Aronowitz
Deepak Asudani
Andrew Auerbach
Ann Avery
Ahmed BaHammam
Thomas W. Barrett
Jeffrey Barsuk
John Alexander Batsis
Brent Beasley
Deepti Behl
Chaim Bell
Rachelle Bernacki
Jennifer Best
Nisha L. Bhatia
Richard D. Blondell
Bema Bonsu
Thomas Bookwalter
Jeffrey Boord
Debra Boyer
Dawn Brezina
Mandy Brown Belfort
Lucinda Bryant
Alfred Paul Burger
David Busch
Bill Carruth
Brian Carter
Peter J. Cawley
Shiven B. Chabria
Kevin Chan
Carol Chenoweth
Barbara Cleary
Jennifer Cohen
Curtiss B. Cook
Otto Costantini
Kenneth Covinsky
Donald Craven
Timothy J. Crone
Yvette Marie Cua
Ethan Ulysses Cumbler
A. Mark Dalzell
Jennifer Daru
Mellar Davis
William DeMarco
Thomas Donner
Abhijit Duggal
Beatrice Edwards
David Efron
Erin Egan
Kristin Englund
Edward Etchells
Mark Fagan
Tonya Fancher
Randy Joe Ferrance
Chris Feudtner
Christopher K. Finch
Kathleen M. Finn
Alan John Forster
Michael Sebastian Galindo
Joseph Michael Geskey
Roma Y. Gianchandani
Adit A. Ginde
Alan Go
Sherita Hill Golden
Jill Deborah Goldenberg
Adrienne Green
Brian Greffe
Douglas Gregory
Merik Gross
Munish Gupta
Lakshmi Halasyamani
Leslie W. Hall
Jennifer Hanrahan
Lee Hargraves
Gregory Adam Harlan
Michael Harper
Julie Hauer
Nicola Helm
Timothy Hoff
Eric Edwin Howell
Michael Howell
Stephen Hwang
Robert Hyzy
Brian Jack
Joshua Levi Jacobs
Jay Jahanmir
Neeta Jain
William Janssen
Michael Jibson
Karnjit Johl
Robert Kalayjian
Andrew Karson
Dan Kaul
Abel Ngo Kho
Flora Kisuule
Antonios E. Kopanakis
Collin Kroen
Damon Kwan
Alan Labonte
Robert Lash
Usman Latif
Joshua Lee
Sei Lee
Joseph Li
Peter K. Lindenauer
David Ling
Ian Logan
Vanessa London
Jennifer Lukela
Eusni Rahayu M. Tohit
Alejandro E. Macias
Jennifer Mack
Brian Mandell
Efren C. Manjarrez
Brian Markoff
George Mathew
Sarah McBride
Michael McFarlane
Sylvia Cheney McKean
David Meltzer
Franklin Michota
Sherif Mossad
Joseph Munsayac
Paul Murphree
Thomas Aquinas Murphy
Nina Naeger Murphy
Eric Neurmberger
Kathrin Nicolacakis
Craig Nielsen
Lise Nigrovic
Timothy O'Brien
Mary Ottolini
Thomas Andrew Owens
Robert Pascucci
Raffaele Pesavento
Diana Pi
Ann Poncelet
Maryjo Prince‐Paul
Rehan Qayyum
Hossam A. Rahman
Vijay Rajput
Shawn Ralston
Sadat Rashid
Kimberly Rask
Mathew J. Reeves
Robert Reilly
Larry Rhein
Erinn Rhodes
Willaim David Rifkin
Hilary F. Ryder
Camille Sabella
Sandeep Sachdeva
Sanjay Saint
David Schulman
Thomas Schwenk
Gregory B. Seymann
Hasan Shabbir
Samir S. Shah
Lisa Shah
Kaveh G. Shojania
Rebecca Shunk
Eric M. Siegal
Jeffrey Simmons
Siddhartha Singh
G. Randall Smith Jr.
Lailey Sooriash
Ted Speroff
Diane Stafford
Brett Stauffer
Andrea Stracciolini
Hemali Sudhalkar
Alan Taege
Benjamin Taylor
Jay Thomas
Rachel E. Thompson
Sharlene Toney
Joan Trey
Jennifer Michelle Trujillo
Alexander Turchin
Guillermo E. Umpierrez
Bobbak Vahid
Jay Vaidya
Tamara Vesel
Sally Vitali
Polychronopoulos Vlasis
Natalia Borisovna Volkova
Heidi Wald
H. Kenneth Walker
Jeff Wiese
Jonathan Winickoff
Bradford Winters
Scott Wright
David Zipes
We deeply appreciate the involvement of our reviewers who made the Journal of Hospital Medicine so successful in its second year. Listed below are the many reviewers and volume of their contributions. They have our sincere gratitude.
Reviewed 4 or More Articles
Thomas E. Baudendistel (7)
Renee Patrice Bullock‐Palmer (4)
Vincent W. Chiang (4)
Jasminka M. Criley (4)
Gurpreet Dhaliwal (6)
Lorenzo Di Francesco (4)
Dana Edelson, MD (7)
Kellie L. Flood (5)
Jeffrey Glasheen (5)
Jeffrey L. Greenwald (4)
Brian Harte (11)
Sunil Kripalani (4)
Matthew Landler (4)
Greg Maynard (5)
Kevin J. O'Leary (4)
Sameer Parikh (6)
James C. Pile (6)
Jason S. Schneider (4)
Doug Wright (4)
Reviewed 3 Articles
Eric Alper
Alpesh Amin
Robert Neal Axon
David L. Blazes
Douglas Carlson
Param Dedhia
Margaret Fang
Jonathan M. Flacker
Rajesh Garg
Stephanie Grossman
Daniel Payson Hunt
Christopher Seoung Kim
Christopher P. Landrigan
Kristine H. Lethert
Marcia Levetown
David Liebovitz
David Likosky
Navneet Majhail
Jennifer Myers
Janet Nagamine
Daniel A. Rauch
Steve Ross
Danielle Bowen Scheurer
Jeffrey Lawrence Schnipper
Hiren Shah
Jason Stein
Reviewed 2 Articles
Nasim Afsarmanesh
Mel L. Anderson III
Vineet Arora
John Banja
Susan S. Braithwaite
Cynthia Jean Brown
Daniel Seth Budnitz
Beril Cakir
Rachel N. Caskey
Murtaza Cassoobhoy
Eva Chittenden
Eugene Shu‐Sen Chu
Steven L. Cohn
Randolph Cole
Nathan T. Connell
Richard I. Cook
Aashish Didwania
Daniel David Dressler
Matthew Eisen
Terry England
Leonard Samuel Feldman
Regina Fink
Raminder Singh Gill
Philip H. Goodman
Mohan Gounder
Susan Grant
Paul Grant
Sajeev Handa
Jeanne M. Huddleston
Carlos Manuel Isada
Amir K. Jaffer
Peter John Kaboli
Jennifer Kapo
Ariel R. Katz
Ujjaini Khanderia
Lisa Kirkland
Cindy J. Lai
Cecilia Lansang
Michael Edwin Lazarus
Bennett Leslie
Blake J. Lesselroth
Lee Lindquist
Michael Lubin
Michelle Magee
David Malkenson
Michael Matheny
Laurence McMahon
Donna Leco Mercado
Melissa Munsell
Brahmajee Nallamothu
James Newman
Vikas Parekh
Mohammed A. Qadeer
Kara Quan
Cate E. Ranheim
Sumant Ranji
Gustavo Rivero
John James Ross
Richard Saitz
Elias G. Sakalis
Maryam Sattari
Bradley Allen Sharpe
Tamara D. Simon
Jeff Sperring
Erin Stucky
Rebecca Sudore
Patrick John Torcson
Arpana Vidyarthi
Diane B. Wayne
Chad Whelan
Stephen Wilson
Jeanie Youngwerth
Iris Yung
Lisa B. Zaoutis
Thomas Zipp
Reviewed 1 Article
Adebola Adesanya
Deborah Adey
Bianca Borges Afonso
Dewesh Agrawal
Meenakshy Aiyer
Richard Keith Albert
Shafic S. Al‐Nammari
Wendy Anderson
Ashish Aneja
Armand H. M. Antommaria
Paul Aronowitz
Deepak Asudani
Andrew Auerbach
Ann Avery
Ahmed BaHammam
Thomas W. Barrett
Jeffrey Barsuk
John Alexander Batsis
Brent Beasley
Deepti Behl
Chaim Bell
Rachelle Bernacki
Jennifer Best
Nisha L. Bhatia
Richard D. Blondell
Bema Bonsu
Thomas Bookwalter
Jeffrey Boord
Debra Boyer
Dawn Brezina
Mandy Brown Belfort
Lucinda Bryant
Alfred Paul Burger
David Busch
Bill Carruth
Brian Carter
Peter J. Cawley
Shiven B. Chabria
Kevin Chan
Carol Chenoweth
Barbara Cleary
Jennifer Cohen
Curtiss B. Cook
Otto Costantini
Kenneth Covinsky
Donald Craven
Timothy J. Crone
Yvette Marie Cua
Ethan Ulysses Cumbler
A. Mark Dalzell
Jennifer Daru
Mellar Davis
William DeMarco
Thomas Donner
Abhijit Duggal
Beatrice Edwards
David Efron
Erin Egan
Kristin Englund
Edward Etchells
Mark Fagan
Tonya Fancher
Randy Joe Ferrance
Chris Feudtner
Christopher K. Finch
Kathleen M. Finn
Alan John Forster
Michael Sebastian Galindo
Joseph Michael Geskey
Roma Y. Gianchandani
Adit A. Ginde
Alan Go
Sherita Hill Golden
Jill Deborah Goldenberg
Adrienne Green
Brian Greffe
Douglas Gregory
Merik Gross
Munish Gupta
Lakshmi Halasyamani
Leslie W. Hall
Jennifer Hanrahan
Lee Hargraves
Gregory Adam Harlan
Michael Harper
Julie Hauer
Nicola Helm
Timothy Hoff
Eric Edwin Howell
Michael Howell
Stephen Hwang
Robert Hyzy
Brian Jack
Joshua Levi Jacobs
Jay Jahanmir
Neeta Jain
William Janssen
Michael Jibson
Karnjit Johl
Robert Kalayjian
Andrew Karson
Dan Kaul
Abel Ngo Kho
Flora Kisuule
Antonios E. Kopanakis
Collin Kroen
Damon Kwan
Alan Labonte
Robert Lash
Usman Latif
Joshua Lee
Sei Lee
Joseph Li
Peter K. Lindenauer
David Ling
Ian Logan
Vanessa London
Jennifer Lukela
Eusni Rahayu M. Tohit
Alejandro E. Macias
Jennifer Mack
Brian Mandell
Efren C. Manjarrez
Brian Markoff
George Mathew
Sarah McBride
Michael McFarlane
Sylvia Cheney McKean
David Meltzer
Franklin Michota
Sherif Mossad
Joseph Munsayac
Paul Murphree
Thomas Aquinas Murphy
Nina Naeger Murphy
Eric Neurmberger
Kathrin Nicolacakis
Craig Nielsen
Lise Nigrovic
Timothy O'Brien
Mary Ottolini
Thomas Andrew Owens
Robert Pascucci
Raffaele Pesavento
Diana Pi
Ann Poncelet
Maryjo Prince‐Paul
Rehan Qayyum
Hossam A. Rahman
Vijay Rajput
Shawn Ralston
Sadat Rashid
Kimberly Rask
Mathew J. Reeves
Robert Reilly
Larry Rhein
Erinn Rhodes
Willaim David Rifkin
Hilary F. Ryder
Camille Sabella
Sandeep Sachdeva
Sanjay Saint
David Schulman
Thomas Schwenk
Gregory B. Seymann
Hasan Shabbir
Samir S. Shah
Lisa Shah
Kaveh G. Shojania
Rebecca Shunk
Eric M. Siegal
Jeffrey Simmons
Siddhartha Singh
G. Randall Smith Jr.
Lailey Sooriash
Ted Speroff
Diane Stafford
Brett Stauffer
Andrea Stracciolini
Hemali Sudhalkar
Alan Taege
Benjamin Taylor
Jay Thomas
Rachel E. Thompson
Sharlene Toney
Joan Trey
Jennifer Michelle Trujillo
Alexander Turchin
Guillermo E. Umpierrez
Bobbak Vahid
Jay Vaidya
Tamara Vesel
Sally Vitali
Polychronopoulos Vlasis
Natalia Borisovna Volkova
Heidi Wald
H. Kenneth Walker
Jeff Wiese
Jonathan Winickoff
Bradford Winters
Scott Wright
David Zipes
We deeply appreciate the involvement of our reviewers who made the Journal of Hospital Medicine so successful in its second year. Listed below are the many reviewers and volume of their contributions. They have our sincere gratitude.
Reviewed 4 or More Articles
Thomas E. Baudendistel (7)
Renee Patrice Bullock‐Palmer (4)
Vincent W. Chiang (4)
Jasminka M. Criley (4)
Gurpreet Dhaliwal (6)
Lorenzo Di Francesco (4)
Dana Edelson, MD (7)
Kellie L. Flood (5)
Jeffrey Glasheen (5)
Jeffrey L. Greenwald (4)
Brian Harte (11)
Sunil Kripalani (4)
Matthew Landler (4)
Greg Maynard (5)
Kevin J. O'Leary (4)
Sameer Parikh (6)
James C. Pile (6)
Jason S. Schneider (4)
Doug Wright (4)
Reviewed 3 Articles
Eric Alper
Alpesh Amin
Robert Neal Axon
David L. Blazes
Douglas Carlson
Param Dedhia
Margaret Fang
Jonathan M. Flacker
Rajesh Garg
Stephanie Grossman
Daniel Payson Hunt
Christopher Seoung Kim
Christopher P. Landrigan
Kristine H. Lethert
Marcia Levetown
David Liebovitz
David Likosky
Navneet Majhail
Jennifer Myers
Janet Nagamine
Daniel A. Rauch
Steve Ross
Danielle Bowen Scheurer
Jeffrey Lawrence Schnipper
Hiren Shah
Jason Stein
Reviewed 2 Articles
Nasim Afsarmanesh
Mel L. Anderson III
Vineet Arora
John Banja
Susan S. Braithwaite
Cynthia Jean Brown
Daniel Seth Budnitz
Beril Cakir
Rachel N. Caskey
Murtaza Cassoobhoy
Eva Chittenden
Eugene Shu‐Sen Chu
Steven L. Cohn
Randolph Cole
Nathan T. Connell
Richard I. Cook
Aashish Didwania
Daniel David Dressler
Matthew Eisen
Terry England
Leonard Samuel Feldman
Regina Fink
Raminder Singh Gill
Philip H. Goodman
Mohan Gounder
Susan Grant
Paul Grant
Sajeev Handa
Jeanne M. Huddleston
Carlos Manuel Isada
Amir K. Jaffer
Peter John Kaboli
Jennifer Kapo
Ariel R. Katz
Ujjaini Khanderia
Lisa Kirkland
Cindy J. Lai
Cecilia Lansang
Michael Edwin Lazarus
Bennett Leslie
Blake J. Lesselroth
Lee Lindquist
Michael Lubin
Michelle Magee
David Malkenson
Michael Matheny
Laurence McMahon
Donna Leco Mercado
Melissa Munsell
Brahmajee Nallamothu
James Newman
Vikas Parekh
Mohammed A. Qadeer
Kara Quan
Cate E. Ranheim
Sumant Ranji
Gustavo Rivero
John James Ross
Richard Saitz
Elias G. Sakalis
Maryam Sattari
Bradley Allen Sharpe
Tamara D. Simon
Jeff Sperring
Erin Stucky
Rebecca Sudore
Patrick John Torcson
Arpana Vidyarthi
Diane B. Wayne
Chad Whelan
Stephen Wilson
Jeanie Youngwerth
Iris Yung
Lisa B. Zaoutis
Thomas Zipp
Reviewed 1 Article
Adebola Adesanya
Deborah Adey
Bianca Borges Afonso
Dewesh Agrawal
Meenakshy Aiyer
Richard Keith Albert
Shafic S. Al‐Nammari
Wendy Anderson
Ashish Aneja
Armand H. M. Antommaria
Paul Aronowitz
Deepak Asudani
Andrew Auerbach
Ann Avery
Ahmed BaHammam
Thomas W. Barrett
Jeffrey Barsuk
John Alexander Batsis
Brent Beasley
Deepti Behl
Chaim Bell
Rachelle Bernacki
Jennifer Best
Nisha L. Bhatia
Richard D. Blondell
Bema Bonsu
Thomas Bookwalter
Jeffrey Boord
Debra Boyer
Dawn Brezina
Mandy Brown Belfort
Lucinda Bryant
Alfred Paul Burger
David Busch
Bill Carruth
Brian Carter
Peter J. Cawley
Shiven B. Chabria
Kevin Chan
Carol Chenoweth
Barbara Cleary
Jennifer Cohen
Curtiss B. Cook
Otto Costantini
Kenneth Covinsky
Donald Craven
Timothy J. Crone
Yvette Marie Cua
Ethan Ulysses Cumbler
A. Mark Dalzell
Jennifer Daru
Mellar Davis
William DeMarco
Thomas Donner
Abhijit Duggal
Beatrice Edwards
David Efron
Erin Egan
Kristin Englund
Edward Etchells
Mark Fagan
Tonya Fancher
Randy Joe Ferrance
Chris Feudtner
Christopher K. Finch
Kathleen M. Finn
Alan John Forster
Michael Sebastian Galindo
Joseph Michael Geskey
Roma Y. Gianchandani
Adit A. Ginde
Alan Go
Sherita Hill Golden
Jill Deborah Goldenberg
Adrienne Green
Brian Greffe
Douglas Gregory
Merik Gross
Munish Gupta
Lakshmi Halasyamani
Leslie W. Hall
Jennifer Hanrahan
Lee Hargraves
Gregory Adam Harlan
Michael Harper
Julie Hauer
Nicola Helm
Timothy Hoff
Eric Edwin Howell
Michael Howell
Stephen Hwang
Robert Hyzy
Brian Jack
Joshua Levi Jacobs
Jay Jahanmir
Neeta Jain
William Janssen
Michael Jibson
Karnjit Johl
Robert Kalayjian
Andrew Karson
Dan Kaul
Abel Ngo Kho
Flora Kisuule
Antonios E. Kopanakis
Collin Kroen
Damon Kwan
Alan Labonte
Robert Lash
Usman Latif
Joshua Lee
Sei Lee
Joseph Li
Peter K. Lindenauer
David Ling
Ian Logan
Vanessa London
Jennifer Lukela
Eusni Rahayu M. Tohit
Alejandro E. Macias
Jennifer Mack
Brian Mandell
Efren C. Manjarrez
Brian Markoff
George Mathew
Sarah McBride
Michael McFarlane
Sylvia Cheney McKean
David Meltzer
Franklin Michota
Sherif Mossad
Joseph Munsayac
Paul Murphree
Thomas Aquinas Murphy
Nina Naeger Murphy
Eric Neurmberger
Kathrin Nicolacakis
Craig Nielsen
Lise Nigrovic
Timothy O'Brien
Mary Ottolini
Thomas Andrew Owens
Robert Pascucci
Raffaele Pesavento
Diana Pi
Ann Poncelet
Maryjo Prince‐Paul
Rehan Qayyum
Hossam A. Rahman
Vijay Rajput
Shawn Ralston
Sadat Rashid
Kimberly Rask
Mathew J. Reeves
Robert Reilly
Larry Rhein
Erinn Rhodes
Willaim David Rifkin
Hilary F. Ryder
Camille Sabella
Sandeep Sachdeva
Sanjay Saint
David Schulman
Thomas Schwenk
Gregory B. Seymann
Hasan Shabbir
Samir S. Shah
Lisa Shah
Kaveh G. Shojania
Rebecca Shunk
Eric M. Siegal
Jeffrey Simmons
Siddhartha Singh
G. Randall Smith Jr.
Lailey Sooriash
Ted Speroff
Diane Stafford
Brett Stauffer
Andrea Stracciolini
Hemali Sudhalkar
Alan Taege
Benjamin Taylor
Jay Thomas
Rachel E. Thompson
Sharlene Toney
Joan Trey
Jennifer Michelle Trujillo
Alexander Turchin
Guillermo E. Umpierrez
Bobbak Vahid
Jay Vaidya
Tamara Vesel
Sally Vitali
Polychronopoulos Vlasis
Natalia Borisovna Volkova
Heidi Wald
H. Kenneth Walker
Jeff Wiese
Jonathan Winickoff
Bradford Winters
Scott Wright
David Zipes