User login
Enchondromatosis
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
The Anorectic Heart
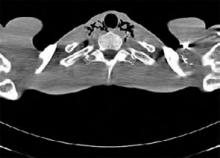
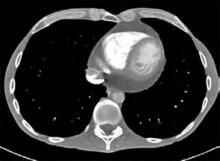
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Get Control
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
Capitol Gains
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Physician Payment Reform, P4P, AHRQ
SHM’s Public Policy Committee (PPC) monitors federal legislation and regulations affecting hospital medicine and recommending appropriate action by SHM. SHM works independently and through coalitions with like-minded organizations in pursuit of its policy objectives. This month, I’ll update you on PPC’s major activities in the past six months.
Physician Payment Reform
Late last year, as Congress debated whether to address pending reductions in 2007 Medicare payments to physicians before adjourning, PPC spearheaded a number of activities to influence debate on the issue. These efforts included:
- Sending a letter from then-SHM President Mary Jo Gorman, MD, MBA, to members of the key health committees, urging lawmakers to take action to avert the scheduled 5% cut in Medicare physician fees and enact a positive payment update that accurately reflects increases in practice costs;
- Launching a new advocacy tool that allows SHM members to quickly e-mail their members of Congress in opposition to the pending fee cut. In less than two weeks, 130 members sent nearly 390 messages to the U.S. House of Representatives and the Senate; and
- Lobbying Congress to ensure that any pay-for-reporting program for physicians be voluntary and based on valid measures developed by the medical profession.
The legislation approved by Congress (H.R. 6111) averted the 5% cut, as advocated by SHM, freezing rates at 2006 levels. Continuation of the current payment rates, combined with increases in evaluation and management services proposed by CMS and supported by SHM as part of the five-year review, translated into an average gain per hospitalist of approximately 8.8% on their Medicare billings.
A scheduled 10% cut in 2008 Medicare payments to physicians will dominate this year’s legislative agenda. The PPC will continue to oppose cuts in the physician update and advocate for a more permanent solution to the annual payment reductions caused by the flawed sustainable growth rate.
Pay for Performance
Together with SHM’s Performance and Standards Task Force (PSTF), the PPC has spent countless hours working to position SHM to influence the debate over pay for performance on Capitol Hill and with CMS. This has involved Hill visits by PPC members and staff in addition to conference calls, meetings, and communications with CMS officials. Part of the committee’s role is also to educate SHM members on how their practices will be affected by legislative and regulatory action in this area.
Under the new Physician Quality Reporting Initiative (PQRI) mandated under H.R. 6111, SHM members and other eligible professionals who successfully report quality measures on claims for dates of service from July 1 to Dec. 31 may earn a bonus payment, subject to a cap, of 1.5% of total allowed charges for covered Medicare physician fee schedule services.
Because measures were not originally developed for hospital medicine, PPC, PSTF, and staff actively lobbied CMS and the AMA’s Physician Consortium for Performance Improvement (PCPI) for changes to the measures that would allow wider reporting by SHM members. Significantly, PCPI accepted SHM’s recommendations, paving the way for hospitalist participation in this voluntary program. Had SHM not been at the table, hospitalists would have had only a limited opportunity to qualify for a 1.5% increase in their Medicare payments through participation in the PQRI program. SHM will also take the lead in developing measures on care transitions through the PCPI for 2009, which will position hospital medicine as the premier advocate for this important issue.
Funding for AHRQ
One of SHM’s legislative priorities is to advocate for increased funding for the Agency for Healthcare Research and Quality (AHRQ), whose mission is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. As part of this effort, we participate in the Friends of AHRQ, a voluntary coalition of more than 130 organizations that supports the AHRQ by sending joint letters to key members of Congress, making joint visits to members of Congress and their staff, and holding briefings to demonstrate the importance of AHRQ research.
In March, SHM and 50 other members of the coalition sent a letter to the chairs and ranking members of the House and Senate Appropriations committees recommending that AHRQ receive $350 million in FY 2008, an increase of $31 million over FY 2007. The groups pointed out that while AHRQ is charged with supporting research to improve healthcare quality, reduce costs, advance patient safety, decrease medical errors, eliminate healthcare disparities, and broaden access to essential services, “precarious funding levels threaten the agency’s ability to achieve this important mission, at a time when healthcare costs are at an all-time high.”
Funding for NIH and Other Agencies
SHM also routinely joins with other organizations in urging Congress to increase funding for the National Institutes of Health (NIH) and other public health programs.
A Feb. 26 letter, signed by SHM and 405 other health organizations, urged Congress to increase FY 2008 funding for public health programs by an additional $4 billion, or 7.8%, above the FY 2007 level. The letter states that this increase in the FY 2008 budget for Function 550 discretionary health programs such as NIH, AHRQ, and CDC will “reverse the erosion of support for the continuum of biomedical, behavioral and health services research, community-based disease prevention and health promotion, basic and targeted services for the medically uninsured and those with disabilities, health professions education, and robust regulation of the nation’s food and drug supply.”
Access to Care
Recognizing SHM member interest—and that of the 110th Congress—in initiatives to expand healthcare coverage to the nation’s 47 million uninsured, the PPC is reviewing legislative proposals being considered in this area.
At the committee’s recommendation, SHM sent a letter of support for the Health Partnership Act (S. 325/H.R. 506), which would establish a grant program to promote the development of innovative health coverage initiatives at the state level. In the letter, then-SHM President Mary Jo Gorman, MD, MBA, commended the sponsors for “giving state and local governments the flexibility to test a variety of options for improving access so they can address the unique needs of their uninsured populations.”
She noted that many hospitalist programs exist to manage the burgeoning population of uninsured and underinsured patients who require hospitalization, and offered SHM’s help in moving the bill through Congress.
Grass-roots Advocacy
Politically active members are an organization’s best resource when it comes to influencing healthcare policy on Capitol Hill. Building on the relationships established during SHM’s first Advocacy Day held during the 2006 annual meeting, PPC members traveled to Washington D.C., in February to brief members of Congress and their staffs on SHM’s 2007 legislative priorities, including support for initiatives designed to improve the quality, safety, and cost effectiveness of inpatient medical care.
More than 30 appointments were scheduled with lawmakers and their staffs, many of whom sit on the key congressional committees with jurisdiction over the Medicare and Medicaid programs. Each PPC member had from five to eight visits. They continued the process of educating Congress about the specialty of hospital medicine that began during Advocacy Day and the role of hospitalists in improving the quality of care provided in our nation’s hospitals. It was time well spent. Lawmakers and their staffs were eager to learn about hospital medicine and our support for increased funding for AHRQ, pay-for-reporting, and legislation like the Health Partnership Act.
Allendorf is senior adviser, advocacy and government relations, for SHM.
New Task Force, New Chair, Improved Patient Care
SHM’s HQPS Committee makes tremendous progress
By Shannon Roach
The past year has been successful and productive for the SHM Health Quality and Patient Safety (HQPS) Committee. Under the leadership of Lakshmi Halasyamani, MD, HQPS has strengthened its national leadership role in inpatient quality improvement efforts, most notably in the areas of reducing DVTs, improving glycemic control and management of patients with heart failure. Additionally, HQPS has strengthened relationships with partner organizations and created new alliances. HQPS has participated in the development of training activities and clinical support tools for quality improvement efforts.
Hand-Off Standards
The Hand-Off Standards and Communication Task Force was formed to create a formally recognized set of standards for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service. The standards ensure that care is coordinated and that important clinical care issues are effectively managed. The development methodology mirrors that of the Discharge Planning Checklist and includes a literature review, panel of experts, presentation to and input from membership. Vineet Arora, MD, has led this development in collaboration with Sunil Kripalani, MD, Efren Manjarrez, MD, Dan Dressler, MD, Preetha Basaviah, MD, and Lakshmi Halasyamani, MD.
The Hand-Off Standards checklist was unveiled at the 2007 Annual Meeting from May 23-25 in Dallas, where attendees reviewed and voted on the standards in order to provide the Task Force with a final draft to present to the Expert Panel for a final review. Effective hand-offs require program policy, verbal exchange, and content exchange. A research agenda was also proposed to evaluate these standards rigorously, put emphasis on controlled interventions, and to encourage SHM and other organizations to fund research and innovations in this area.
Medication Reconciliation
The Medication Reconciliation Task Force is charged with understanding the state of and leading work related to Medication Reconciliation. In support of that, the Task Force submitted a grant proposal to AHRQ to provide funding for a multidisciplinary conference to identify barriers and develop strategies for Quality Improvement in this area.
Heart Failure
Dr. Halasyamani, former HQPS chair, was a key participant in the development of the Heart Failure Resource Room, which launched in February 2006. As part of the Heart Failure Education and Quality Improvement Initiative, there have been both clinical tools and CME/CE additions to this Web-based resource (visit www.hospitalmedicine.org and click “Quality & Safety” then click “Quality Improvement Resource Rooms”). The Quality Improvement Workbook, the Palliative Care CME Module, and Didactic Slide Sets are all housed in the Resource Room along with the recently developed Clinical Tools focusing on Team Communication, Discharge Planning and Polypharmacy.
The Tools include an Inpatient Goal Sheet, a Hospitalist Admission and Daily Rounding Checklist, a Conceptual Model for Teamwork, two reference guides: Patient Education and High Risk Medications for the Heart Failure Patient, and Heart Failure, specific elements of which were integrated into the SHM Discharge Planning Checklist.
Additional CME/CE modules have also been integrated into the Heart Failure Resource Room: Palliative Care for Patients with Heart Failure and Optimizing the Heart Failure Discharge Transition.
A CD-ROM including all these new resources was given to attendees of the Annual Meeting.
Building Partnerships
HQPS has been strengthening partnerships with other professional, regulatory and advocacy groups. These partnerships are intended to improve safety and take a leadership role in setting the national agenda for key quality improvement areas. We now have official liaisons with Academy of Health-System Pharmacists (AHSP), National Transitions of Care Coalition (NTOCC), Institute for Healthcare Improvement (IHI), and Transforming Care at the Bedside (TCAB).
HQPS members also serve as leaders in national efforts to define and improve care transitions including the American Board of Internal Medicine’s Stepping up to the Plate program, and Hartford’s Safe Steps.
SHM’s Public Policy Committee (PPC) monitors federal legislation and regulations affecting hospital medicine and recommending appropriate action by SHM. SHM works independently and through coalitions with like-minded organizations in pursuit of its policy objectives. This month, I’ll update you on PPC’s major activities in the past six months.
Physician Payment Reform
Late last year, as Congress debated whether to address pending reductions in 2007 Medicare payments to physicians before adjourning, PPC spearheaded a number of activities to influence debate on the issue. These efforts included:
- Sending a letter from then-SHM President Mary Jo Gorman, MD, MBA, to members of the key health committees, urging lawmakers to take action to avert the scheduled 5% cut in Medicare physician fees and enact a positive payment update that accurately reflects increases in practice costs;
- Launching a new advocacy tool that allows SHM members to quickly e-mail their members of Congress in opposition to the pending fee cut. In less than two weeks, 130 members sent nearly 390 messages to the U.S. House of Representatives and the Senate; and
- Lobbying Congress to ensure that any pay-for-reporting program for physicians be voluntary and based on valid measures developed by the medical profession.
The legislation approved by Congress (H.R. 6111) averted the 5% cut, as advocated by SHM, freezing rates at 2006 levels. Continuation of the current payment rates, combined with increases in evaluation and management services proposed by CMS and supported by SHM as part of the five-year review, translated into an average gain per hospitalist of approximately 8.8% on their Medicare billings.
A scheduled 10% cut in 2008 Medicare payments to physicians will dominate this year’s legislative agenda. The PPC will continue to oppose cuts in the physician update and advocate for a more permanent solution to the annual payment reductions caused by the flawed sustainable growth rate.
Pay for Performance
Together with SHM’s Performance and Standards Task Force (PSTF), the PPC has spent countless hours working to position SHM to influence the debate over pay for performance on Capitol Hill and with CMS. This has involved Hill visits by PPC members and staff in addition to conference calls, meetings, and communications with CMS officials. Part of the committee’s role is also to educate SHM members on how their practices will be affected by legislative and regulatory action in this area.
Under the new Physician Quality Reporting Initiative (PQRI) mandated under H.R. 6111, SHM members and other eligible professionals who successfully report quality measures on claims for dates of service from July 1 to Dec. 31 may earn a bonus payment, subject to a cap, of 1.5% of total allowed charges for covered Medicare physician fee schedule services.
Because measures were not originally developed for hospital medicine, PPC, PSTF, and staff actively lobbied CMS and the AMA’s Physician Consortium for Performance Improvement (PCPI) for changes to the measures that would allow wider reporting by SHM members. Significantly, PCPI accepted SHM’s recommendations, paving the way for hospitalist participation in this voluntary program. Had SHM not been at the table, hospitalists would have had only a limited opportunity to qualify for a 1.5% increase in their Medicare payments through participation in the PQRI program. SHM will also take the lead in developing measures on care transitions through the PCPI for 2009, which will position hospital medicine as the premier advocate for this important issue.
Funding for AHRQ
One of SHM’s legislative priorities is to advocate for increased funding for the Agency for Healthcare Research and Quality (AHRQ), whose mission is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. As part of this effort, we participate in the Friends of AHRQ, a voluntary coalition of more than 130 organizations that supports the AHRQ by sending joint letters to key members of Congress, making joint visits to members of Congress and their staff, and holding briefings to demonstrate the importance of AHRQ research.
In March, SHM and 50 other members of the coalition sent a letter to the chairs and ranking members of the House and Senate Appropriations committees recommending that AHRQ receive $350 million in FY 2008, an increase of $31 million over FY 2007. The groups pointed out that while AHRQ is charged with supporting research to improve healthcare quality, reduce costs, advance patient safety, decrease medical errors, eliminate healthcare disparities, and broaden access to essential services, “precarious funding levels threaten the agency’s ability to achieve this important mission, at a time when healthcare costs are at an all-time high.”
Funding for NIH and Other Agencies
SHM also routinely joins with other organizations in urging Congress to increase funding for the National Institutes of Health (NIH) and other public health programs.
A Feb. 26 letter, signed by SHM and 405 other health organizations, urged Congress to increase FY 2008 funding for public health programs by an additional $4 billion, or 7.8%, above the FY 2007 level. The letter states that this increase in the FY 2008 budget for Function 550 discretionary health programs such as NIH, AHRQ, and CDC will “reverse the erosion of support for the continuum of biomedical, behavioral and health services research, community-based disease prevention and health promotion, basic and targeted services for the medically uninsured and those with disabilities, health professions education, and robust regulation of the nation’s food and drug supply.”
Access to Care
Recognizing SHM member interest—and that of the 110th Congress—in initiatives to expand healthcare coverage to the nation’s 47 million uninsured, the PPC is reviewing legislative proposals being considered in this area.
At the committee’s recommendation, SHM sent a letter of support for the Health Partnership Act (S. 325/H.R. 506), which would establish a grant program to promote the development of innovative health coverage initiatives at the state level. In the letter, then-SHM President Mary Jo Gorman, MD, MBA, commended the sponsors for “giving state and local governments the flexibility to test a variety of options for improving access so they can address the unique needs of their uninsured populations.”
She noted that many hospitalist programs exist to manage the burgeoning population of uninsured and underinsured patients who require hospitalization, and offered SHM’s help in moving the bill through Congress.
Grass-roots Advocacy
Politically active members are an organization’s best resource when it comes to influencing healthcare policy on Capitol Hill. Building on the relationships established during SHM’s first Advocacy Day held during the 2006 annual meeting, PPC members traveled to Washington D.C., in February to brief members of Congress and their staffs on SHM’s 2007 legislative priorities, including support for initiatives designed to improve the quality, safety, and cost effectiveness of inpatient medical care.
More than 30 appointments were scheduled with lawmakers and their staffs, many of whom sit on the key congressional committees with jurisdiction over the Medicare and Medicaid programs. Each PPC member had from five to eight visits. They continued the process of educating Congress about the specialty of hospital medicine that began during Advocacy Day and the role of hospitalists in improving the quality of care provided in our nation’s hospitals. It was time well spent. Lawmakers and their staffs were eager to learn about hospital medicine and our support for increased funding for AHRQ, pay-for-reporting, and legislation like the Health Partnership Act.
Allendorf is senior adviser, advocacy and government relations, for SHM.
New Task Force, New Chair, Improved Patient Care
SHM’s HQPS Committee makes tremendous progress
By Shannon Roach
The past year has been successful and productive for the SHM Health Quality and Patient Safety (HQPS) Committee. Under the leadership of Lakshmi Halasyamani, MD, HQPS has strengthened its national leadership role in inpatient quality improvement efforts, most notably in the areas of reducing DVTs, improving glycemic control and management of patients with heart failure. Additionally, HQPS has strengthened relationships with partner organizations and created new alliances. HQPS has participated in the development of training activities and clinical support tools for quality improvement efforts.
Hand-Off Standards
The Hand-Off Standards and Communication Task Force was formed to create a formally recognized set of standards for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service. The standards ensure that care is coordinated and that important clinical care issues are effectively managed. The development methodology mirrors that of the Discharge Planning Checklist and includes a literature review, panel of experts, presentation to and input from membership. Vineet Arora, MD, has led this development in collaboration with Sunil Kripalani, MD, Efren Manjarrez, MD, Dan Dressler, MD, Preetha Basaviah, MD, and Lakshmi Halasyamani, MD.
The Hand-Off Standards checklist was unveiled at the 2007 Annual Meeting from May 23-25 in Dallas, where attendees reviewed and voted on the standards in order to provide the Task Force with a final draft to present to the Expert Panel for a final review. Effective hand-offs require program policy, verbal exchange, and content exchange. A research agenda was also proposed to evaluate these standards rigorously, put emphasis on controlled interventions, and to encourage SHM and other organizations to fund research and innovations in this area.
Medication Reconciliation
The Medication Reconciliation Task Force is charged with understanding the state of and leading work related to Medication Reconciliation. In support of that, the Task Force submitted a grant proposal to AHRQ to provide funding for a multidisciplinary conference to identify barriers and develop strategies for Quality Improvement in this area.
Heart Failure
Dr. Halasyamani, former HQPS chair, was a key participant in the development of the Heart Failure Resource Room, which launched in February 2006. As part of the Heart Failure Education and Quality Improvement Initiative, there have been both clinical tools and CME/CE additions to this Web-based resource (visit www.hospitalmedicine.org and click “Quality & Safety” then click “Quality Improvement Resource Rooms”). The Quality Improvement Workbook, the Palliative Care CME Module, and Didactic Slide Sets are all housed in the Resource Room along with the recently developed Clinical Tools focusing on Team Communication, Discharge Planning and Polypharmacy.
The Tools include an Inpatient Goal Sheet, a Hospitalist Admission and Daily Rounding Checklist, a Conceptual Model for Teamwork, two reference guides: Patient Education and High Risk Medications for the Heart Failure Patient, and Heart Failure, specific elements of which were integrated into the SHM Discharge Planning Checklist.
Additional CME/CE modules have also been integrated into the Heart Failure Resource Room: Palliative Care for Patients with Heart Failure and Optimizing the Heart Failure Discharge Transition.
A CD-ROM including all these new resources was given to attendees of the Annual Meeting.
Building Partnerships
HQPS has been strengthening partnerships with other professional, regulatory and advocacy groups. These partnerships are intended to improve safety and take a leadership role in setting the national agenda for key quality improvement areas. We now have official liaisons with Academy of Health-System Pharmacists (AHSP), National Transitions of Care Coalition (NTOCC), Institute for Healthcare Improvement (IHI), and Transforming Care at the Bedside (TCAB).
HQPS members also serve as leaders in national efforts to define and improve care transitions including the American Board of Internal Medicine’s Stepping up to the Plate program, and Hartford’s Safe Steps.
SHM’s Public Policy Committee (PPC) monitors federal legislation and regulations affecting hospital medicine and recommending appropriate action by SHM. SHM works independently and through coalitions with like-minded organizations in pursuit of its policy objectives. This month, I’ll update you on PPC’s major activities in the past six months.
Physician Payment Reform
Late last year, as Congress debated whether to address pending reductions in 2007 Medicare payments to physicians before adjourning, PPC spearheaded a number of activities to influence debate on the issue. These efforts included:
- Sending a letter from then-SHM President Mary Jo Gorman, MD, MBA, to members of the key health committees, urging lawmakers to take action to avert the scheduled 5% cut in Medicare physician fees and enact a positive payment update that accurately reflects increases in practice costs;
- Launching a new advocacy tool that allows SHM members to quickly e-mail their members of Congress in opposition to the pending fee cut. In less than two weeks, 130 members sent nearly 390 messages to the U.S. House of Representatives and the Senate; and
- Lobbying Congress to ensure that any pay-for-reporting program for physicians be voluntary and based on valid measures developed by the medical profession.
The legislation approved by Congress (H.R. 6111) averted the 5% cut, as advocated by SHM, freezing rates at 2006 levels. Continuation of the current payment rates, combined with increases in evaluation and management services proposed by CMS and supported by SHM as part of the five-year review, translated into an average gain per hospitalist of approximately 8.8% on their Medicare billings.
A scheduled 10% cut in 2008 Medicare payments to physicians will dominate this year’s legislative agenda. The PPC will continue to oppose cuts in the physician update and advocate for a more permanent solution to the annual payment reductions caused by the flawed sustainable growth rate.
Pay for Performance
Together with SHM’s Performance and Standards Task Force (PSTF), the PPC has spent countless hours working to position SHM to influence the debate over pay for performance on Capitol Hill and with CMS. This has involved Hill visits by PPC members and staff in addition to conference calls, meetings, and communications with CMS officials. Part of the committee’s role is also to educate SHM members on how their practices will be affected by legislative and regulatory action in this area.
Under the new Physician Quality Reporting Initiative (PQRI) mandated under H.R. 6111, SHM members and other eligible professionals who successfully report quality measures on claims for dates of service from July 1 to Dec. 31 may earn a bonus payment, subject to a cap, of 1.5% of total allowed charges for covered Medicare physician fee schedule services.
Because measures were not originally developed for hospital medicine, PPC, PSTF, and staff actively lobbied CMS and the AMA’s Physician Consortium for Performance Improvement (PCPI) for changes to the measures that would allow wider reporting by SHM members. Significantly, PCPI accepted SHM’s recommendations, paving the way for hospitalist participation in this voluntary program. Had SHM not been at the table, hospitalists would have had only a limited opportunity to qualify for a 1.5% increase in their Medicare payments through participation in the PQRI program. SHM will also take the lead in developing measures on care transitions through the PCPI for 2009, which will position hospital medicine as the premier advocate for this important issue.
Funding for AHRQ
One of SHM’s legislative priorities is to advocate for increased funding for the Agency for Healthcare Research and Quality (AHRQ), whose mission is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. As part of this effort, we participate in the Friends of AHRQ, a voluntary coalition of more than 130 organizations that supports the AHRQ by sending joint letters to key members of Congress, making joint visits to members of Congress and their staff, and holding briefings to demonstrate the importance of AHRQ research.
In March, SHM and 50 other members of the coalition sent a letter to the chairs and ranking members of the House and Senate Appropriations committees recommending that AHRQ receive $350 million in FY 2008, an increase of $31 million over FY 2007. The groups pointed out that while AHRQ is charged with supporting research to improve healthcare quality, reduce costs, advance patient safety, decrease medical errors, eliminate healthcare disparities, and broaden access to essential services, “precarious funding levels threaten the agency’s ability to achieve this important mission, at a time when healthcare costs are at an all-time high.”
Funding for NIH and Other Agencies
SHM also routinely joins with other organizations in urging Congress to increase funding for the National Institutes of Health (NIH) and other public health programs.
A Feb. 26 letter, signed by SHM and 405 other health organizations, urged Congress to increase FY 2008 funding for public health programs by an additional $4 billion, or 7.8%, above the FY 2007 level. The letter states that this increase in the FY 2008 budget for Function 550 discretionary health programs such as NIH, AHRQ, and CDC will “reverse the erosion of support for the continuum of biomedical, behavioral and health services research, community-based disease prevention and health promotion, basic and targeted services for the medically uninsured and those with disabilities, health professions education, and robust regulation of the nation’s food and drug supply.”
Access to Care
Recognizing SHM member interest—and that of the 110th Congress—in initiatives to expand healthcare coverage to the nation’s 47 million uninsured, the PPC is reviewing legislative proposals being considered in this area.
At the committee’s recommendation, SHM sent a letter of support for the Health Partnership Act (S. 325/H.R. 506), which would establish a grant program to promote the development of innovative health coverage initiatives at the state level. In the letter, then-SHM President Mary Jo Gorman, MD, MBA, commended the sponsors for “giving state and local governments the flexibility to test a variety of options for improving access so they can address the unique needs of their uninsured populations.”
She noted that many hospitalist programs exist to manage the burgeoning population of uninsured and underinsured patients who require hospitalization, and offered SHM’s help in moving the bill through Congress.
Grass-roots Advocacy
Politically active members are an organization’s best resource when it comes to influencing healthcare policy on Capitol Hill. Building on the relationships established during SHM’s first Advocacy Day held during the 2006 annual meeting, PPC members traveled to Washington D.C., in February to brief members of Congress and their staffs on SHM’s 2007 legislative priorities, including support for initiatives designed to improve the quality, safety, and cost effectiveness of inpatient medical care.
More than 30 appointments were scheduled with lawmakers and their staffs, many of whom sit on the key congressional committees with jurisdiction over the Medicare and Medicaid programs. Each PPC member had from five to eight visits. They continued the process of educating Congress about the specialty of hospital medicine that began during Advocacy Day and the role of hospitalists in improving the quality of care provided in our nation’s hospitals. It was time well spent. Lawmakers and their staffs were eager to learn about hospital medicine and our support for increased funding for AHRQ, pay-for-reporting, and legislation like the Health Partnership Act.
Allendorf is senior adviser, advocacy and government relations, for SHM.
New Task Force, New Chair, Improved Patient Care
SHM’s HQPS Committee makes tremendous progress
By Shannon Roach
The past year has been successful and productive for the SHM Health Quality and Patient Safety (HQPS) Committee. Under the leadership of Lakshmi Halasyamani, MD, HQPS has strengthened its national leadership role in inpatient quality improvement efforts, most notably in the areas of reducing DVTs, improving glycemic control and management of patients with heart failure. Additionally, HQPS has strengthened relationships with partner organizations and created new alliances. HQPS has participated in the development of training activities and clinical support tools for quality improvement efforts.
Hand-Off Standards
The Hand-Off Standards and Communication Task Force was formed to create a formally recognized set of standards for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service. The standards ensure that care is coordinated and that important clinical care issues are effectively managed. The development methodology mirrors that of the Discharge Planning Checklist and includes a literature review, panel of experts, presentation to and input from membership. Vineet Arora, MD, has led this development in collaboration with Sunil Kripalani, MD, Efren Manjarrez, MD, Dan Dressler, MD, Preetha Basaviah, MD, and Lakshmi Halasyamani, MD.
The Hand-Off Standards checklist was unveiled at the 2007 Annual Meeting from May 23-25 in Dallas, where attendees reviewed and voted on the standards in order to provide the Task Force with a final draft to present to the Expert Panel for a final review. Effective hand-offs require program policy, verbal exchange, and content exchange. A research agenda was also proposed to evaluate these standards rigorously, put emphasis on controlled interventions, and to encourage SHM and other organizations to fund research and innovations in this area.
Medication Reconciliation
The Medication Reconciliation Task Force is charged with understanding the state of and leading work related to Medication Reconciliation. In support of that, the Task Force submitted a grant proposal to AHRQ to provide funding for a multidisciplinary conference to identify barriers and develop strategies for Quality Improvement in this area.
Heart Failure
Dr. Halasyamani, former HQPS chair, was a key participant in the development of the Heart Failure Resource Room, which launched in February 2006. As part of the Heart Failure Education and Quality Improvement Initiative, there have been both clinical tools and CME/CE additions to this Web-based resource (visit www.hospitalmedicine.org and click “Quality & Safety” then click “Quality Improvement Resource Rooms”). The Quality Improvement Workbook, the Palliative Care CME Module, and Didactic Slide Sets are all housed in the Resource Room along with the recently developed Clinical Tools focusing on Team Communication, Discharge Planning and Polypharmacy.
The Tools include an Inpatient Goal Sheet, a Hospitalist Admission and Daily Rounding Checklist, a Conceptual Model for Teamwork, two reference guides: Patient Education and High Risk Medications for the Heart Failure Patient, and Heart Failure, specific elements of which were integrated into the SHM Discharge Planning Checklist.
Additional CME/CE modules have also been integrated into the Heart Failure Resource Room: Palliative Care for Patients with Heart Failure and Optimizing the Heart Failure Discharge Transition.
A CD-ROM including all these new resources was given to attendees of the Annual Meeting.
Building Partnerships
HQPS has been strengthening partnerships with other professional, regulatory and advocacy groups. These partnerships are intended to improve safety and take a leadership role in setting the national agenda for key quality improvement areas. We now have official liaisons with Academy of Health-System Pharmacists (AHSP), National Transitions of Care Coalition (NTOCC), Institute for Healthcare Improvement (IHI), and Transforming Care at the Bedside (TCAB).
HQPS members also serve as leaders in national efforts to define and improve care transitions including the American Board of Internal Medicine’s Stepping up to the Plate program, and Hartford’s Safe Steps.
Key Keynotes
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
Hospitalists, Healthcare Reform, and the Presidential Election
Even though the 2008 elections seem very far away, the presidential nomination process is in full swing. Obviously, the No. 1 issue for most Americans is the war in Iraq. But, interestingly, the No. 2 item on many peoples’ list is healthcare reform. This is of particular interest to hospitalists because they are not only young and early in their careers, but clearly at the center of acute healthcare.
There are opportunities to reshape the financing and delivery of healthcare in a way that will be better for our patients and for hospitalists for many years to come. This will require us to be lucky, which I define as being prepared when opportunities present themselves and being ready to step up and change even when the future is not clearly defined.
The driving forces are several, not the least of which is the fact that in the richest country on Earth almost 50 million Americans still have no health coverage. We know these people eventually find their way to emergency rooms and are admitted to hospitals, but studies show the uninsured are sicker and die more quickly than the insured population. The uninsured are not the unemployed or the illegal aliens, but generally those with full-time jobs, our neighbors, our friends, and often our children of working age.
Because of a failure to adopt a national policy, several states have decided to move forward with their own attempts to insure all their citizens. Massachusetts enacted its landmark plan in 2006. (See The Hospitalist, May 2007, p. 1.) California Gov. Arnold Schwarzenegger has proposed a broad plan to insure the 6 million Californians without coverage. Schwarzenegger’s plan would require sacrifice by all constituencies and would be financed in part by taxing 3%-4% of each physician’s gross collections and an equal percentage on the revenue of hospitals. As you might imagine, this has led to the usual squawking from physician and hospital organizations. He has also called on contributions from the state’s general fund and support from the federal government.
At a national level, the American College of Physicians has developed its Patient Centered Medical Home proposal and has drawn support from the American Academy of Pediatrics, the American Academy of Family Physicians, and others. Basically, this plan calls for changes in the payment structure to recognize the coordination of care in managing chronic illness and taking care of the patient over time. This is a marked departure from our current system, which pays by the episode of care—the visit or the procedure. In many ways this approach harkens back to the best of managed care without being dragged down by managed care’s image of rationing care and limiting resources.
There are increasing calls to develop a single-payer plan to squeeze out the funds now “wasted” on the insurance industry and unnecessary administrative cost. In a perfect world this would allow for >90% of the healthcare dollar to go for patient-care services at a time where some insurance companies retain as much of 30% of every health dollar for profit and administration.
Some say we have elements of this process in place in covering seniors and the disabled with Medicare, in covering the very poor with Medicaid, and in covering children with S-CHIP (State Children’s Health Insurance Program). Much of this discussion overlooks the fact that in order to support Medicare, Medicaid, and S-CHIP, there needs to be cost-shifting to the tune of >125% that now comes out of private insurance payments. This also needs to be thought of in context of a population that craves choice and freedom in their healthcare and are very suspicious of enlarging government programs.
Some are calling for DRGs (diagnosis related groups) for hospital care for the physician component, much as exist for the hospital facility charge. This case-based approach may work well for the hospitalist model, where efficiencies could result and rewards can be tied to performance. More modeling and projections need to be done before this can be a viable option.
This leads to thoughts of how much pay for performance (P4P) will be a part of any healthcare reform. Some see this as the panacea. Others see P4P as motivating systems or institutions, but doing little to change individual physician behaviors. Some feel performance standards need to be part of the equation because institutions need to provide a transparent accountability of just how good a job they are doing. Hospitalists are in a position to provide leadership and direction as quality and documentation of performance become valued.
All this is woven through a political process that is media- and sound-bite driven.
While Hillary Clinton probably has more insider knowledge of healthcare reform concepts, she is so associated with the failed Clinton plans of the early 1990s that she may be reluctant to make healthcare her main policy direction.
John Edwards and Barack Obama, who want to speak for the “other America,” seem positioned to take on healthcare reform as a way to level the playing field and bring the 50 million uninsured at least up to some sort of healthcare access parity with the rest of Americans. Any proposal that tries to include another 50 million people will by necessity cause a revolution in the current system with marked, probably seismic, shifts in payment and delivery of care.
As the Republican candidates get sorted out, expect healthcare reform as a popular issue that isn’t a war issue to take a higher priority, much the way Al Gore and George Bush were touting their own approaches to a pharmacy benefit for seniors in 2000.
Hospital medicine at age 10 can no longer sit on the sidelines and wait to see what will happen. SHM, along with other national partners in hospital medicine, must start developing the hospital medicine strategy so we can be active participants in the reform discussions. The current system of reimbursement at the level of the visit or the procedure does not recognize the full value hospitalists can bring in improving quality, reducing resource use, increasing throughput and efficiency, etc. In addition, being on the front lines, catching everyone who is acutely ill and needs hospitalization regardless of ability to pay, puts us squarely in the middle of dealing with those Americans who lack insurance.
The good news is that hospitalists present many fewer barriers than other physician groups. We know we will be measured and that we need to prove our performance. We know we will treat the uninsured. There is no escape. We know many of us will still practice in 2025 and 2030, and we need to fix the system now because we will live in this space for many years to come.
Reforming healthcare—an industry that accounts for $2 trillion and 16% of the GDP—is staggering, but signs appear to indicate change is coming. SHM and hospitalists everywhere are ready to be part of the solution. TH
Dr. Wellikson has been CEO of SHM since 2000.
Even though the 2008 elections seem very far away, the presidential nomination process is in full swing. Obviously, the No. 1 issue for most Americans is the war in Iraq. But, interestingly, the No. 2 item on many peoples’ list is healthcare reform. This is of particular interest to hospitalists because they are not only young and early in their careers, but clearly at the center of acute healthcare.
There are opportunities to reshape the financing and delivery of healthcare in a way that will be better for our patients and for hospitalists for many years to come. This will require us to be lucky, which I define as being prepared when opportunities present themselves and being ready to step up and change even when the future is not clearly defined.
The driving forces are several, not the least of which is the fact that in the richest country on Earth almost 50 million Americans still have no health coverage. We know these people eventually find their way to emergency rooms and are admitted to hospitals, but studies show the uninsured are sicker and die more quickly than the insured population. The uninsured are not the unemployed or the illegal aliens, but generally those with full-time jobs, our neighbors, our friends, and often our children of working age.
Because of a failure to adopt a national policy, several states have decided to move forward with their own attempts to insure all their citizens. Massachusetts enacted its landmark plan in 2006. (See The Hospitalist, May 2007, p. 1.) California Gov. Arnold Schwarzenegger has proposed a broad plan to insure the 6 million Californians without coverage. Schwarzenegger’s plan would require sacrifice by all constituencies and would be financed in part by taxing 3%-4% of each physician’s gross collections and an equal percentage on the revenue of hospitals. As you might imagine, this has led to the usual squawking from physician and hospital organizations. He has also called on contributions from the state’s general fund and support from the federal government.
At a national level, the American College of Physicians has developed its Patient Centered Medical Home proposal and has drawn support from the American Academy of Pediatrics, the American Academy of Family Physicians, and others. Basically, this plan calls for changes in the payment structure to recognize the coordination of care in managing chronic illness and taking care of the patient over time. This is a marked departure from our current system, which pays by the episode of care—the visit or the procedure. In many ways this approach harkens back to the best of managed care without being dragged down by managed care’s image of rationing care and limiting resources.
There are increasing calls to develop a single-payer plan to squeeze out the funds now “wasted” on the insurance industry and unnecessary administrative cost. In a perfect world this would allow for >90% of the healthcare dollar to go for patient-care services at a time where some insurance companies retain as much of 30% of every health dollar for profit and administration.
Some say we have elements of this process in place in covering seniors and the disabled with Medicare, in covering the very poor with Medicaid, and in covering children with S-CHIP (State Children’s Health Insurance Program). Much of this discussion overlooks the fact that in order to support Medicare, Medicaid, and S-CHIP, there needs to be cost-shifting to the tune of >125% that now comes out of private insurance payments. This also needs to be thought of in context of a population that craves choice and freedom in their healthcare and are very suspicious of enlarging government programs.
Some are calling for DRGs (diagnosis related groups) for hospital care for the physician component, much as exist for the hospital facility charge. This case-based approach may work well for the hospitalist model, where efficiencies could result and rewards can be tied to performance. More modeling and projections need to be done before this can be a viable option.
This leads to thoughts of how much pay for performance (P4P) will be a part of any healthcare reform. Some see this as the panacea. Others see P4P as motivating systems or institutions, but doing little to change individual physician behaviors. Some feel performance standards need to be part of the equation because institutions need to provide a transparent accountability of just how good a job they are doing. Hospitalists are in a position to provide leadership and direction as quality and documentation of performance become valued.
All this is woven through a political process that is media- and sound-bite driven.
While Hillary Clinton probably has more insider knowledge of healthcare reform concepts, she is so associated with the failed Clinton plans of the early 1990s that she may be reluctant to make healthcare her main policy direction.
John Edwards and Barack Obama, who want to speak for the “other America,” seem positioned to take on healthcare reform as a way to level the playing field and bring the 50 million uninsured at least up to some sort of healthcare access parity with the rest of Americans. Any proposal that tries to include another 50 million people will by necessity cause a revolution in the current system with marked, probably seismic, shifts in payment and delivery of care.
As the Republican candidates get sorted out, expect healthcare reform as a popular issue that isn’t a war issue to take a higher priority, much the way Al Gore and George Bush were touting their own approaches to a pharmacy benefit for seniors in 2000.
Hospital medicine at age 10 can no longer sit on the sidelines and wait to see what will happen. SHM, along with other national partners in hospital medicine, must start developing the hospital medicine strategy so we can be active participants in the reform discussions. The current system of reimbursement at the level of the visit or the procedure does not recognize the full value hospitalists can bring in improving quality, reducing resource use, increasing throughput and efficiency, etc. In addition, being on the front lines, catching everyone who is acutely ill and needs hospitalization regardless of ability to pay, puts us squarely in the middle of dealing with those Americans who lack insurance.
The good news is that hospitalists present many fewer barriers than other physician groups. We know we will be measured and that we need to prove our performance. We know we will treat the uninsured. There is no escape. We know many of us will still practice in 2025 and 2030, and we need to fix the system now because we will live in this space for many years to come.
Reforming healthcare—an industry that accounts for $2 trillion and 16% of the GDP—is staggering, but signs appear to indicate change is coming. SHM and hospitalists everywhere are ready to be part of the solution. TH
Dr. Wellikson has been CEO of SHM since 2000.
Even though the 2008 elections seem very far away, the presidential nomination process is in full swing. Obviously, the No. 1 issue for most Americans is the war in Iraq. But, interestingly, the No. 2 item on many peoples’ list is healthcare reform. This is of particular interest to hospitalists because they are not only young and early in their careers, but clearly at the center of acute healthcare.
There are opportunities to reshape the financing and delivery of healthcare in a way that will be better for our patients and for hospitalists for many years to come. This will require us to be lucky, which I define as being prepared when opportunities present themselves and being ready to step up and change even when the future is not clearly defined.
The driving forces are several, not the least of which is the fact that in the richest country on Earth almost 50 million Americans still have no health coverage. We know these people eventually find their way to emergency rooms and are admitted to hospitals, but studies show the uninsured are sicker and die more quickly than the insured population. The uninsured are not the unemployed or the illegal aliens, but generally those with full-time jobs, our neighbors, our friends, and often our children of working age.
Because of a failure to adopt a national policy, several states have decided to move forward with their own attempts to insure all their citizens. Massachusetts enacted its landmark plan in 2006. (See The Hospitalist, May 2007, p. 1.) California Gov. Arnold Schwarzenegger has proposed a broad plan to insure the 6 million Californians without coverage. Schwarzenegger’s plan would require sacrifice by all constituencies and would be financed in part by taxing 3%-4% of each physician’s gross collections and an equal percentage on the revenue of hospitals. As you might imagine, this has led to the usual squawking from physician and hospital organizations. He has also called on contributions from the state’s general fund and support from the federal government.
At a national level, the American College of Physicians has developed its Patient Centered Medical Home proposal and has drawn support from the American Academy of Pediatrics, the American Academy of Family Physicians, and others. Basically, this plan calls for changes in the payment structure to recognize the coordination of care in managing chronic illness and taking care of the patient over time. This is a marked departure from our current system, which pays by the episode of care—the visit or the procedure. In many ways this approach harkens back to the best of managed care without being dragged down by managed care’s image of rationing care and limiting resources.
There are increasing calls to develop a single-payer plan to squeeze out the funds now “wasted” on the insurance industry and unnecessary administrative cost. In a perfect world this would allow for >90% of the healthcare dollar to go for patient-care services at a time where some insurance companies retain as much of 30% of every health dollar for profit and administration.
Some say we have elements of this process in place in covering seniors and the disabled with Medicare, in covering the very poor with Medicaid, and in covering children with S-CHIP (State Children’s Health Insurance Program). Much of this discussion overlooks the fact that in order to support Medicare, Medicaid, and S-CHIP, there needs to be cost-shifting to the tune of >125% that now comes out of private insurance payments. This also needs to be thought of in context of a population that craves choice and freedom in their healthcare and are very suspicious of enlarging government programs.
Some are calling for DRGs (diagnosis related groups) for hospital care for the physician component, much as exist for the hospital facility charge. This case-based approach may work well for the hospitalist model, where efficiencies could result and rewards can be tied to performance. More modeling and projections need to be done before this can be a viable option.
This leads to thoughts of how much pay for performance (P4P) will be a part of any healthcare reform. Some see this as the panacea. Others see P4P as motivating systems or institutions, but doing little to change individual physician behaviors. Some feel performance standards need to be part of the equation because institutions need to provide a transparent accountability of just how good a job they are doing. Hospitalists are in a position to provide leadership and direction as quality and documentation of performance become valued.
All this is woven through a political process that is media- and sound-bite driven.
While Hillary Clinton probably has more insider knowledge of healthcare reform concepts, she is so associated with the failed Clinton plans of the early 1990s that she may be reluctant to make healthcare her main policy direction.
John Edwards and Barack Obama, who want to speak for the “other America,” seem positioned to take on healthcare reform as a way to level the playing field and bring the 50 million uninsured at least up to some sort of healthcare access parity with the rest of Americans. Any proposal that tries to include another 50 million people will by necessity cause a revolution in the current system with marked, probably seismic, shifts in payment and delivery of care.
As the Republican candidates get sorted out, expect healthcare reform as a popular issue that isn’t a war issue to take a higher priority, much the way Al Gore and George Bush were touting their own approaches to a pharmacy benefit for seniors in 2000.
Hospital medicine at age 10 can no longer sit on the sidelines and wait to see what will happen. SHM, along with other national partners in hospital medicine, must start developing the hospital medicine strategy so we can be active participants in the reform discussions. The current system of reimbursement at the level of the visit or the procedure does not recognize the full value hospitalists can bring in improving quality, reducing resource use, increasing throughput and efficiency, etc. In addition, being on the front lines, catching everyone who is acutely ill and needs hospitalization regardless of ability to pay, puts us squarely in the middle of dealing with those Americans who lack insurance.
The good news is that hospitalists present many fewer barriers than other physician groups. We know we will be measured and that we need to prove our performance. We know we will treat the uninsured. There is no escape. We know many of us will still practice in 2025 and 2030, and we need to fix the system now because we will live in this space for many years to come.
Reforming healthcare—an industry that accounts for $2 trillion and 16% of the GDP—is staggering, but signs appear to indicate change is coming. SHM and hospitalists everywhere are ready to be part of the solution. TH
Dr. Wellikson has been CEO of SHM since 2000.
What's Your Diagnosis?
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.
A Performance Metrics Primer
Hospitalists are no strangers to performance measurement. Every day, their performance is measured, formally and informally, by their sponsoring organizations, by third-party payers, and by patients.
But many hospitalists are not engaged in producing or reviewing that performance data.
“Historically, hospitalist groups have relied on the hospital to collect the data and present it to them—and still do, to a great extent, even today,” says Marc B. Westle, DO, FACP, president and managing partner for a large private hospital medicine group (HMG), Asheville Hospitalist Group in North Carolina.
This often puts hospitalists at a disadvantage, says Dr. Westle. If hospitalist groups don’t get involved with data reporting and analysis, they can’t have meaningful discussions with their hospitals.
With a background in hospital administration, Leslie Flores, MHA, co-principal of Nelson/Flores Associates, LLC, is well acquainted with the challenges of collecting and reporting hospital data. Through her consulting work with partner John Nelson, MD, she has found that sponsoring organizations often don’t review performance data with hospitalists. Hospitalists may examine their performance one way, while the hospital uses a different set of metrics, or analytical techniques. This disconnect, she notes, “leads to differences in interpretations and understandings that can occur between the hospital folks and the doctors when they try to present information.”
A new white paper produced by SHM’s Benchmarks Committee, “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards,” aims to change these scenarios by encouraging hospitalists to take charge of their performance reporting. Geared to multiple levels of expertise with performance metrics, the white paper offers “some real, practical advice as to how you capture this information and then how you look at it,” says Joe Miller, SHM senior vice president and staff liaison to the Benchmarks Committee.
— Daniel Rauch, MD, FAAP
Select a Metric
The Benchmarks Committee used a Delphi process to rank the importance of various metrics and produced a list of 10 on which they would focus. The clearly written introduction walks readers through a step-by-step process intended to help HMGs decide which performance metrics they will measure.
Flores, editor of the white paper project, cautions that the “magic 10” metrics selected by the committee don’t necessarily represent the most important metrics for each practice. “We wanted to stimulate hospitalists to think about how they view their own performance and to create a common language and understanding of what some key issues and expectations should be for hospitalists’ performance monitoring,” she says. “They can use this document as a starting point and then come up with performance metrics that really matter to their practice.”
Choosing metrics to measure and report on for the hospitalist service will depend on a variety of variables particular to that group, including:
- The HMG’s original mission;
- The expectations of the hospital or other sponsoring organization (such as a multispecialty group) for the return on their investment;
- Key outcomes and/or performance measures sought by payers, regulators, and other stakeholders; and
- The practice’s high-priority issues.
Regarding the last item, Flores recalls one HMG that decided to include on its dashboard a survey of how it used consulting physicians from the community. This component was chosen to address the concerns of other specialists in the community, who feared the hospitalists were using only their own medical group’s specialists for consultations.
To further guide choices of metrics, the white paper uses a uniform template to organize each section. Whether the metric is descriptive (volume, data, case mix), operational (hospital cost, productivity, provider satisfaction, length of stay, patient satisfaction), or clinical (mortality data, readmission rate, JCAHO core measures), the user finds a description in each section titled, “Why this metric is important.”
Daniel Rauch, MD, FAAP, explains why a pediatric hospitalist group might choose to focus on referring provider satisfaction rather than volume data—perhaps a more critical metric for adult hospitalist groups.
“Our volume data [a descriptive metric] will depend on who’s referring to us and the availability of subspecialists, as opposed to market share and the notability of the institution in the local environment,” he notes.
Dr. Rauch, director of the Pediatric Hospitalist Program at New York University School of Medicine in New York City and editor of the Provider Satisfaction section of the white paper, co-presented the pediatric hospitalist perspective on the white paper with Flores at the Annual Meeting.
Much more critical to the success of a pediatric hospitalist service is nurturing relationships with local pediatricians, who traditionally want to retain their ability to manage patients under all circumstances. As a result, the pediatric hospitalist group might choose to survey its referring providers to learn how it can provide better service and take advantage of positive survey responses to market its service. (These interventions are outlined in “Performance Metric Seven: Provider Satisfaction.”)
Finding the Data
Once a group has selected its performance metrics, it faces many logistical and political challenges to obtain the pertinent data. Again, the white paper’s template furnishes clear direction on data sources for each metric.
To begin, hospitalists must understand their practicing environment. Many smaller rural or freestanding hospitals do not have the IT decision-support resources to generate customized reports for hospitalists. “For instance, the hospital may be able to furnish information about length of stay for the hospital in general, but [may] not [be able] to break out LOS numbers for the hospitalist group compared to other physicians,” explains Flores. In addition, some billing services can’t or won’t provide information on volume, charges, and collections to the hospitalist group.
“The other challenge is more of a cultural or philosophical one,” says Flores. “Very often, hospitals or other sponsoring entities are reluctant to share financial information, in particular, with the hospitalists, because they are afraid that the hospitalists will use the information inappropriately—or that they’ll somehow become more powerful by virtue of having that information. And, in fact, that’s what we really want: to be more powerful—but in a constructive, positive way.”
In this case, HMGs may need to invest time to ensure organizations that the information won’t be used against them and that its only goal is to improve practice performance.
“Finding the data is not always easy,” concedes Burke T. Kealey, MD, assistant medical director of hospital medicine for HealthPartners Medical Group in St. Paul, Minn., and chair of SHM’s Benchmarks Committee. “Some organizations can give you a lot of these data sets pretty easily, and some are not going to produce many of them at all. And, when you cross organizational boundaries, there are political considerations. For example, if you’re a national hospitalist company trying to get data from individual hospitals, it might be difficult.” (Dr. Kealey co-presented at the workshop on the white paper for adult HMGs with Flores at the 2007 SHM Annual Meeting in Dallas.)
Sources of data will vary from metric to metric. To obtain data for measuring volume (often used as an indicator for staffing requirements and scheduling), hospitalists need to access hospital admission/discharge/transfer systems, health-plan data systems, or the hospital medicine service billing system. For an operational metric like provider satisfaction, the hospitalist group may have to float its own referring provider survey (by mail, by phone, or in person) to gain understanding of how it is viewed by referring physicians.
How to Interpret the Data
Obtaining the data is only half the battle. Another core tool in the white paper is the template section “Unique Measurement and Analysis Considerations,” which guides hospitalists as they attempt to verify the validity of their data and ensure valid comparisons.
Dr. Westle’s group has studiously tracked its performance metrics for years; other groups may have little experience in this domain. Another critical step in creating dashboard reports, he states, is understanding how the data are collected and ensuring the data are accurate and attributed appropriately.
“The way clinical cases are coded ought to be the subject of some concern and scrutiny,” says John Novotny, MD, director of the Section of Hospital Medicine of the Allen Division at Columbia University Medical Center in New York City and another Benchmarks Committee member. “There may be a natural inclination to accept the performance information provided to us by the hospital, but the processes that generated these data need to be well understood to gauge the accuracy and acceptability of any conclusions drawn.”
With a background in statistics and information technology, Dr. Novotny cautions that “some assessment of the validity of comparisons within or between groups or to benchmark figures should be included in every analysis or report—to justify any conclusions drawn and to avoid the statistical pitfalls common to these data.”
He advises HMGs to run the numbers by someone with expertise in data interpretation, especially before reports are published or submitted for public review. These issues come up frequently in the analysis of frequency data, such as the number of deaths occurring in a group for a particular diagnosis over a period of time, where the numbers might be relatively small.
For example, if five deaths are observed in a subset of 20 patients, the statistic of a 25% death rate comes with such low precision that the true underlying death rate might fall anywhere between 8% and 50%.
“This is a limitation inherent in drawing conclusions from relatively small data sets, akin to driving down a narrow highway with a very loose steering wheel—avoiding the ravines is a challenge,” he says.
Dr. Novotny contributed the section on mortality metrics for the white paper. Although a group’s raw mortality data may be easily obtained, “HMGs should be wary of the smaller numbers resulting from stratifying the data by service, DRG [diagnosis-related group], or time periods,” he explains.
Instead, as suggested in the “Interventions” section, the HMG might want to take the additional approach of documenting the use of processes thought to have a positive impact on the risk of mortality in hospitalized patients. Potentially useful processes under development and discussion in the literature include interdisciplinary rounds, effective inter-provider communication, and ventilator care protocols, among others.
“We need to show that not only do we track our mortality figures, we analyze and respond to them by improving our patient care,” Dr. Novotny says. “We need to show that we’re making patient care safer.”
At the Ochsner Health Center in New Orleans, the HMG decided to track readmission rates for congestive heart failure—the primary DRG for inpatient care, and compare its rates with those of other services. Because heart failure is traditionally the bailiwick of cardiology, “you might think that the cardiology service would have the best outcomes,” says Steven Deitelzweig, MD, vice president of medical affairs and system chairman.
But, using order sets that align with JCAHO standards and best care as demonstrated by evidence in cardiology, Dr. Deitelzweig’s hospitalist group “was able to demonstrate statistically and objectively that our outcomes were better, adjusting for case mix.”
Make Your Own Case
Once the infrastructure for tracking and reporting productivity is in place, hospitalists can use performance metrics to build their own case, remarks Dr. Kealey. The white paper furnishes several examples of customized dashboards. Some use a visual display to illustrate improvement or maintenance in key performance areas.
Dr. Westle notes that metrics reports can be used in a variety of ways, including:
- Negotiating with the hospital;
- Managing a practice internally (i.e., tracking the productivity of established and new full-time equivalent employees (FTEs) and compensating physicians for their productivity); and
- Negotiating with third-party payers who increasingly rely on pay-for-performance measures. For instance, Dr. Westle says, if a group can track its cost per case for the top 15 DRGs and show those costs are less than the national average, this “puts the hospitalist group at a significant advantage when talking to insurance companies about pay for performance.”
Dr. Deitelzweig reports that his HMG at the Ochsner Health Center posts monthly updates of its dashboard results in the halls of its department and others. “Whether it’s readmission rates, patient satisfaction, or hand washing, it’s up there for all to see,” he says. He believes that this type of transparency is not only a good reminder for staff but benefits patients, as well. “It’s helpful because it highlights for your department members the goals of the department and that those are aligned with patient satisfaction and best outcomes.”
Conclusion
“If hospitalists can work with their hospitals to understand how various data elements are defined, collected and reported,” says Flores, “this will enable them to develop a greater understanding of what the information means, correct any misinterpretations on the hospital’s part, and gain a greater confidence in the information’s credibility and reliability. Hospitalists should work closely with their sponsoring organizations to define metrics and reports that are mutually credible and meaningful, so that all parties are looking at the same things and understanding them the same way.”
Participating in the white paper project gave Dr. Rauch a better appreciation of the value of measuring performance. His advice to first-timers: “It may seem overwhelming at first to do an all-encompassing dashboard, but even if you pick just a couple things to start with, this puts down on paper what your worth is. When you can point to how your services are improving or maintaining over time, that’s the picture that says a thousand words.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Hospitalists are no strangers to performance measurement. Every day, their performance is measured, formally and informally, by their sponsoring organizations, by third-party payers, and by patients.
But many hospitalists are not engaged in producing or reviewing that performance data.
“Historically, hospitalist groups have relied on the hospital to collect the data and present it to them—and still do, to a great extent, even today,” says Marc B. Westle, DO, FACP, president and managing partner for a large private hospital medicine group (HMG), Asheville Hospitalist Group in North Carolina.
This often puts hospitalists at a disadvantage, says Dr. Westle. If hospitalist groups don’t get involved with data reporting and analysis, they can’t have meaningful discussions with their hospitals.
With a background in hospital administration, Leslie Flores, MHA, co-principal of Nelson/Flores Associates, LLC, is well acquainted with the challenges of collecting and reporting hospital data. Through her consulting work with partner John Nelson, MD, she has found that sponsoring organizations often don’t review performance data with hospitalists. Hospitalists may examine their performance one way, while the hospital uses a different set of metrics, or analytical techniques. This disconnect, she notes, “leads to differences in interpretations and understandings that can occur between the hospital folks and the doctors when they try to present information.”
A new white paper produced by SHM’s Benchmarks Committee, “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards,” aims to change these scenarios by encouraging hospitalists to take charge of their performance reporting. Geared to multiple levels of expertise with performance metrics, the white paper offers “some real, practical advice as to how you capture this information and then how you look at it,” says Joe Miller, SHM senior vice president and staff liaison to the Benchmarks Committee.
— Daniel Rauch, MD, FAAP
Select a Metric
The Benchmarks Committee used a Delphi process to rank the importance of various metrics and produced a list of 10 on which they would focus. The clearly written introduction walks readers through a step-by-step process intended to help HMGs decide which performance metrics they will measure.
Flores, editor of the white paper project, cautions that the “magic 10” metrics selected by the committee don’t necessarily represent the most important metrics for each practice. “We wanted to stimulate hospitalists to think about how they view their own performance and to create a common language and understanding of what some key issues and expectations should be for hospitalists’ performance monitoring,” she says. “They can use this document as a starting point and then come up with performance metrics that really matter to their practice.”
Choosing metrics to measure and report on for the hospitalist service will depend on a variety of variables particular to that group, including:
- The HMG’s original mission;
- The expectations of the hospital or other sponsoring organization (such as a multispecialty group) for the return on their investment;
- Key outcomes and/or performance measures sought by payers, regulators, and other stakeholders; and
- The practice’s high-priority issues.
Regarding the last item, Flores recalls one HMG that decided to include on its dashboard a survey of how it used consulting physicians from the community. This component was chosen to address the concerns of other specialists in the community, who feared the hospitalists were using only their own medical group’s specialists for consultations.
To further guide choices of metrics, the white paper uses a uniform template to organize each section. Whether the metric is descriptive (volume, data, case mix), operational (hospital cost, productivity, provider satisfaction, length of stay, patient satisfaction), or clinical (mortality data, readmission rate, JCAHO core measures), the user finds a description in each section titled, “Why this metric is important.”
Daniel Rauch, MD, FAAP, explains why a pediatric hospitalist group might choose to focus on referring provider satisfaction rather than volume data—perhaps a more critical metric for adult hospitalist groups.
“Our volume data [a descriptive metric] will depend on who’s referring to us and the availability of subspecialists, as opposed to market share and the notability of the institution in the local environment,” he notes.
Dr. Rauch, director of the Pediatric Hospitalist Program at New York University School of Medicine in New York City and editor of the Provider Satisfaction section of the white paper, co-presented the pediatric hospitalist perspective on the white paper with Flores at the Annual Meeting.
Much more critical to the success of a pediatric hospitalist service is nurturing relationships with local pediatricians, who traditionally want to retain their ability to manage patients under all circumstances. As a result, the pediatric hospitalist group might choose to survey its referring providers to learn how it can provide better service and take advantage of positive survey responses to market its service. (These interventions are outlined in “Performance Metric Seven: Provider Satisfaction.”)
Finding the Data
Once a group has selected its performance metrics, it faces many logistical and political challenges to obtain the pertinent data. Again, the white paper’s template furnishes clear direction on data sources for each metric.
To begin, hospitalists must understand their practicing environment. Many smaller rural or freestanding hospitals do not have the IT decision-support resources to generate customized reports for hospitalists. “For instance, the hospital may be able to furnish information about length of stay for the hospital in general, but [may] not [be able] to break out LOS numbers for the hospitalist group compared to other physicians,” explains Flores. In addition, some billing services can’t or won’t provide information on volume, charges, and collections to the hospitalist group.
“The other challenge is more of a cultural or philosophical one,” says Flores. “Very often, hospitals or other sponsoring entities are reluctant to share financial information, in particular, with the hospitalists, because they are afraid that the hospitalists will use the information inappropriately—or that they’ll somehow become more powerful by virtue of having that information. And, in fact, that’s what we really want: to be more powerful—but in a constructive, positive way.”
In this case, HMGs may need to invest time to ensure organizations that the information won’t be used against them and that its only goal is to improve practice performance.
“Finding the data is not always easy,” concedes Burke T. Kealey, MD, assistant medical director of hospital medicine for HealthPartners Medical Group in St. Paul, Minn., and chair of SHM’s Benchmarks Committee. “Some organizations can give you a lot of these data sets pretty easily, and some are not going to produce many of them at all. And, when you cross organizational boundaries, there are political considerations. For example, if you’re a national hospitalist company trying to get data from individual hospitals, it might be difficult.” (Dr. Kealey co-presented at the workshop on the white paper for adult HMGs with Flores at the 2007 SHM Annual Meeting in Dallas.)
Sources of data will vary from metric to metric. To obtain data for measuring volume (often used as an indicator for staffing requirements and scheduling), hospitalists need to access hospital admission/discharge/transfer systems, health-plan data systems, or the hospital medicine service billing system. For an operational metric like provider satisfaction, the hospitalist group may have to float its own referring provider survey (by mail, by phone, or in person) to gain understanding of how it is viewed by referring physicians.
How to Interpret the Data
Obtaining the data is only half the battle. Another core tool in the white paper is the template section “Unique Measurement and Analysis Considerations,” which guides hospitalists as they attempt to verify the validity of their data and ensure valid comparisons.
Dr. Westle’s group has studiously tracked its performance metrics for years; other groups may have little experience in this domain. Another critical step in creating dashboard reports, he states, is understanding how the data are collected and ensuring the data are accurate and attributed appropriately.
“The way clinical cases are coded ought to be the subject of some concern and scrutiny,” says John Novotny, MD, director of the Section of Hospital Medicine of the Allen Division at Columbia University Medical Center in New York City and another Benchmarks Committee member. “There may be a natural inclination to accept the performance information provided to us by the hospital, but the processes that generated these data need to be well understood to gauge the accuracy and acceptability of any conclusions drawn.”
With a background in statistics and information technology, Dr. Novotny cautions that “some assessment of the validity of comparisons within or between groups or to benchmark figures should be included in every analysis or report—to justify any conclusions drawn and to avoid the statistical pitfalls common to these data.”
He advises HMGs to run the numbers by someone with expertise in data interpretation, especially before reports are published or submitted for public review. These issues come up frequently in the analysis of frequency data, such as the number of deaths occurring in a group for a particular diagnosis over a period of time, where the numbers might be relatively small.
For example, if five deaths are observed in a subset of 20 patients, the statistic of a 25% death rate comes with such low precision that the true underlying death rate might fall anywhere between 8% and 50%.
“This is a limitation inherent in drawing conclusions from relatively small data sets, akin to driving down a narrow highway with a very loose steering wheel—avoiding the ravines is a challenge,” he says.
Dr. Novotny contributed the section on mortality metrics for the white paper. Although a group’s raw mortality data may be easily obtained, “HMGs should be wary of the smaller numbers resulting from stratifying the data by service, DRG [diagnosis-related group], or time periods,” he explains.
Instead, as suggested in the “Interventions” section, the HMG might want to take the additional approach of documenting the use of processes thought to have a positive impact on the risk of mortality in hospitalized patients. Potentially useful processes under development and discussion in the literature include interdisciplinary rounds, effective inter-provider communication, and ventilator care protocols, among others.
“We need to show that not only do we track our mortality figures, we analyze and respond to them by improving our patient care,” Dr. Novotny says. “We need to show that we’re making patient care safer.”
At the Ochsner Health Center in New Orleans, the HMG decided to track readmission rates for congestive heart failure—the primary DRG for inpatient care, and compare its rates with those of other services. Because heart failure is traditionally the bailiwick of cardiology, “you might think that the cardiology service would have the best outcomes,” says Steven Deitelzweig, MD, vice president of medical affairs and system chairman.
But, using order sets that align with JCAHO standards and best care as demonstrated by evidence in cardiology, Dr. Deitelzweig’s hospitalist group “was able to demonstrate statistically and objectively that our outcomes were better, adjusting for case mix.”
Make Your Own Case
Once the infrastructure for tracking and reporting productivity is in place, hospitalists can use performance metrics to build their own case, remarks Dr. Kealey. The white paper furnishes several examples of customized dashboards. Some use a visual display to illustrate improvement or maintenance in key performance areas.
Dr. Westle notes that metrics reports can be used in a variety of ways, including:
- Negotiating with the hospital;
- Managing a practice internally (i.e., tracking the productivity of established and new full-time equivalent employees (FTEs) and compensating physicians for their productivity); and
- Negotiating with third-party payers who increasingly rely on pay-for-performance measures. For instance, Dr. Westle says, if a group can track its cost per case for the top 15 DRGs and show those costs are less than the national average, this “puts the hospitalist group at a significant advantage when talking to insurance companies about pay for performance.”
Dr. Deitelzweig reports that his HMG at the Ochsner Health Center posts monthly updates of its dashboard results in the halls of its department and others. “Whether it’s readmission rates, patient satisfaction, or hand washing, it’s up there for all to see,” he says. He believes that this type of transparency is not only a good reminder for staff but benefits patients, as well. “It’s helpful because it highlights for your department members the goals of the department and that those are aligned with patient satisfaction and best outcomes.”
Conclusion
“If hospitalists can work with their hospitals to understand how various data elements are defined, collected and reported,” says Flores, “this will enable them to develop a greater understanding of what the information means, correct any misinterpretations on the hospital’s part, and gain a greater confidence in the information’s credibility and reliability. Hospitalists should work closely with their sponsoring organizations to define metrics and reports that are mutually credible and meaningful, so that all parties are looking at the same things and understanding them the same way.”
Participating in the white paper project gave Dr. Rauch a better appreciation of the value of measuring performance. His advice to first-timers: “It may seem overwhelming at first to do an all-encompassing dashboard, but even if you pick just a couple things to start with, this puts down on paper what your worth is. When you can point to how your services are improving or maintaining over time, that’s the picture that says a thousand words.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Hospitalists are no strangers to performance measurement. Every day, their performance is measured, formally and informally, by their sponsoring organizations, by third-party payers, and by patients.
But many hospitalists are not engaged in producing or reviewing that performance data.
“Historically, hospitalist groups have relied on the hospital to collect the data and present it to them—and still do, to a great extent, even today,” says Marc B. Westle, DO, FACP, president and managing partner for a large private hospital medicine group (HMG), Asheville Hospitalist Group in North Carolina.
This often puts hospitalists at a disadvantage, says Dr. Westle. If hospitalist groups don’t get involved with data reporting and analysis, they can’t have meaningful discussions with their hospitals.
With a background in hospital administration, Leslie Flores, MHA, co-principal of Nelson/Flores Associates, LLC, is well acquainted with the challenges of collecting and reporting hospital data. Through her consulting work with partner John Nelson, MD, she has found that sponsoring organizations often don’t review performance data with hospitalists. Hospitalists may examine their performance one way, while the hospital uses a different set of metrics, or analytical techniques. This disconnect, she notes, “leads to differences in interpretations and understandings that can occur between the hospital folks and the doctors when they try to present information.”
A new white paper produced by SHM’s Benchmarks Committee, “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards,” aims to change these scenarios by encouraging hospitalists to take charge of their performance reporting. Geared to multiple levels of expertise with performance metrics, the white paper offers “some real, practical advice as to how you capture this information and then how you look at it,” says Joe Miller, SHM senior vice president and staff liaison to the Benchmarks Committee.
— Daniel Rauch, MD, FAAP
Select a Metric
The Benchmarks Committee used a Delphi process to rank the importance of various metrics and produced a list of 10 on which they would focus. The clearly written introduction walks readers through a step-by-step process intended to help HMGs decide which performance metrics they will measure.
Flores, editor of the white paper project, cautions that the “magic 10” metrics selected by the committee don’t necessarily represent the most important metrics for each practice. “We wanted to stimulate hospitalists to think about how they view their own performance and to create a common language and understanding of what some key issues and expectations should be for hospitalists’ performance monitoring,” she says. “They can use this document as a starting point and then come up with performance metrics that really matter to their practice.”
Choosing metrics to measure and report on for the hospitalist service will depend on a variety of variables particular to that group, including:
- The HMG’s original mission;
- The expectations of the hospital or other sponsoring organization (such as a multispecialty group) for the return on their investment;
- Key outcomes and/or performance measures sought by payers, regulators, and other stakeholders; and
- The practice’s high-priority issues.
Regarding the last item, Flores recalls one HMG that decided to include on its dashboard a survey of how it used consulting physicians from the community. This component was chosen to address the concerns of other specialists in the community, who feared the hospitalists were using only their own medical group’s specialists for consultations.
To further guide choices of metrics, the white paper uses a uniform template to organize each section. Whether the metric is descriptive (volume, data, case mix), operational (hospital cost, productivity, provider satisfaction, length of stay, patient satisfaction), or clinical (mortality data, readmission rate, JCAHO core measures), the user finds a description in each section titled, “Why this metric is important.”
Daniel Rauch, MD, FAAP, explains why a pediatric hospitalist group might choose to focus on referring provider satisfaction rather than volume data—perhaps a more critical metric for adult hospitalist groups.
“Our volume data [a descriptive metric] will depend on who’s referring to us and the availability of subspecialists, as opposed to market share and the notability of the institution in the local environment,” he notes.
Dr. Rauch, director of the Pediatric Hospitalist Program at New York University School of Medicine in New York City and editor of the Provider Satisfaction section of the white paper, co-presented the pediatric hospitalist perspective on the white paper with Flores at the Annual Meeting.
Much more critical to the success of a pediatric hospitalist service is nurturing relationships with local pediatricians, who traditionally want to retain their ability to manage patients under all circumstances. As a result, the pediatric hospitalist group might choose to survey its referring providers to learn how it can provide better service and take advantage of positive survey responses to market its service. (These interventions are outlined in “Performance Metric Seven: Provider Satisfaction.”)
Finding the Data
Once a group has selected its performance metrics, it faces many logistical and political challenges to obtain the pertinent data. Again, the white paper’s template furnishes clear direction on data sources for each metric.
To begin, hospitalists must understand their practicing environment. Many smaller rural or freestanding hospitals do not have the IT decision-support resources to generate customized reports for hospitalists. “For instance, the hospital may be able to furnish information about length of stay for the hospital in general, but [may] not [be able] to break out LOS numbers for the hospitalist group compared to other physicians,” explains Flores. In addition, some billing services can’t or won’t provide information on volume, charges, and collections to the hospitalist group.
“The other challenge is more of a cultural or philosophical one,” says Flores. “Very often, hospitals or other sponsoring entities are reluctant to share financial information, in particular, with the hospitalists, because they are afraid that the hospitalists will use the information inappropriately—or that they’ll somehow become more powerful by virtue of having that information. And, in fact, that’s what we really want: to be more powerful—but in a constructive, positive way.”
In this case, HMGs may need to invest time to ensure organizations that the information won’t be used against them and that its only goal is to improve practice performance.
“Finding the data is not always easy,” concedes Burke T. Kealey, MD, assistant medical director of hospital medicine for HealthPartners Medical Group in St. Paul, Minn., and chair of SHM’s Benchmarks Committee. “Some organizations can give you a lot of these data sets pretty easily, and some are not going to produce many of them at all. And, when you cross organizational boundaries, there are political considerations. For example, if you’re a national hospitalist company trying to get data from individual hospitals, it might be difficult.” (Dr. Kealey co-presented at the workshop on the white paper for adult HMGs with Flores at the 2007 SHM Annual Meeting in Dallas.)
Sources of data will vary from metric to metric. To obtain data for measuring volume (often used as an indicator for staffing requirements and scheduling), hospitalists need to access hospital admission/discharge/transfer systems, health-plan data systems, or the hospital medicine service billing system. For an operational metric like provider satisfaction, the hospitalist group may have to float its own referring provider survey (by mail, by phone, or in person) to gain understanding of how it is viewed by referring physicians.
How to Interpret the Data
Obtaining the data is only half the battle. Another core tool in the white paper is the template section “Unique Measurement and Analysis Considerations,” which guides hospitalists as they attempt to verify the validity of their data and ensure valid comparisons.
Dr. Westle’s group has studiously tracked its performance metrics for years; other groups may have little experience in this domain. Another critical step in creating dashboard reports, he states, is understanding how the data are collected and ensuring the data are accurate and attributed appropriately.
“The way clinical cases are coded ought to be the subject of some concern and scrutiny,” says John Novotny, MD, director of the Section of Hospital Medicine of the Allen Division at Columbia University Medical Center in New York City and another Benchmarks Committee member. “There may be a natural inclination to accept the performance information provided to us by the hospital, but the processes that generated these data need to be well understood to gauge the accuracy and acceptability of any conclusions drawn.”
With a background in statistics and information technology, Dr. Novotny cautions that “some assessment of the validity of comparisons within or between groups or to benchmark figures should be included in every analysis or report—to justify any conclusions drawn and to avoid the statistical pitfalls common to these data.”
He advises HMGs to run the numbers by someone with expertise in data interpretation, especially before reports are published or submitted for public review. These issues come up frequently in the analysis of frequency data, such as the number of deaths occurring in a group for a particular diagnosis over a period of time, where the numbers might be relatively small.
For example, if five deaths are observed in a subset of 20 patients, the statistic of a 25% death rate comes with such low precision that the true underlying death rate might fall anywhere between 8% and 50%.
“This is a limitation inherent in drawing conclusions from relatively small data sets, akin to driving down a narrow highway with a very loose steering wheel—avoiding the ravines is a challenge,” he says.
Dr. Novotny contributed the section on mortality metrics for the white paper. Although a group’s raw mortality data may be easily obtained, “HMGs should be wary of the smaller numbers resulting from stratifying the data by service, DRG [diagnosis-related group], or time periods,” he explains.
Instead, as suggested in the “Interventions” section, the HMG might want to take the additional approach of documenting the use of processes thought to have a positive impact on the risk of mortality in hospitalized patients. Potentially useful processes under development and discussion in the literature include interdisciplinary rounds, effective inter-provider communication, and ventilator care protocols, among others.
“We need to show that not only do we track our mortality figures, we analyze and respond to them by improving our patient care,” Dr. Novotny says. “We need to show that we’re making patient care safer.”
At the Ochsner Health Center in New Orleans, the HMG decided to track readmission rates for congestive heart failure—the primary DRG for inpatient care, and compare its rates with those of other services. Because heart failure is traditionally the bailiwick of cardiology, “you might think that the cardiology service would have the best outcomes,” says Steven Deitelzweig, MD, vice president of medical affairs and system chairman.
But, using order sets that align with JCAHO standards and best care as demonstrated by evidence in cardiology, Dr. Deitelzweig’s hospitalist group “was able to demonstrate statistically and objectively that our outcomes were better, adjusting for case mix.”
Make Your Own Case
Once the infrastructure for tracking and reporting productivity is in place, hospitalists can use performance metrics to build their own case, remarks Dr. Kealey. The white paper furnishes several examples of customized dashboards. Some use a visual display to illustrate improvement or maintenance in key performance areas.
Dr. Westle notes that metrics reports can be used in a variety of ways, including:
- Negotiating with the hospital;
- Managing a practice internally (i.e., tracking the productivity of established and new full-time equivalent employees (FTEs) and compensating physicians for their productivity); and
- Negotiating with third-party payers who increasingly rely on pay-for-performance measures. For instance, Dr. Westle says, if a group can track its cost per case for the top 15 DRGs and show those costs are less than the national average, this “puts the hospitalist group at a significant advantage when talking to insurance companies about pay for performance.”
Dr. Deitelzweig reports that his HMG at the Ochsner Health Center posts monthly updates of its dashboard results in the halls of its department and others. “Whether it’s readmission rates, patient satisfaction, or hand washing, it’s up there for all to see,” he says. He believes that this type of transparency is not only a good reminder for staff but benefits patients, as well. “It’s helpful because it highlights for your department members the goals of the department and that those are aligned with patient satisfaction and best outcomes.”
Conclusion
“If hospitalists can work with their hospitals to understand how various data elements are defined, collected and reported,” says Flores, “this will enable them to develop a greater understanding of what the information means, correct any misinterpretations on the hospital’s part, and gain a greater confidence in the information’s credibility and reliability. Hospitalists should work closely with their sponsoring organizations to define metrics and reports that are mutually credible and meaningful, so that all parties are looking at the same things and understanding them the same way.”
Participating in the white paper project gave Dr. Rauch a better appreciation of the value of measuring performance. His advice to first-timers: “It may seem overwhelming at first to do an all-encompassing dashboard, but even if you pick just a couple things to start with, this puts down on paper what your worth is. When you can point to how your services are improving or maintaining over time, that’s the picture that says a thousand words.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.