User login
COVID-19 and the precipitous dismantlement of societal norms
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
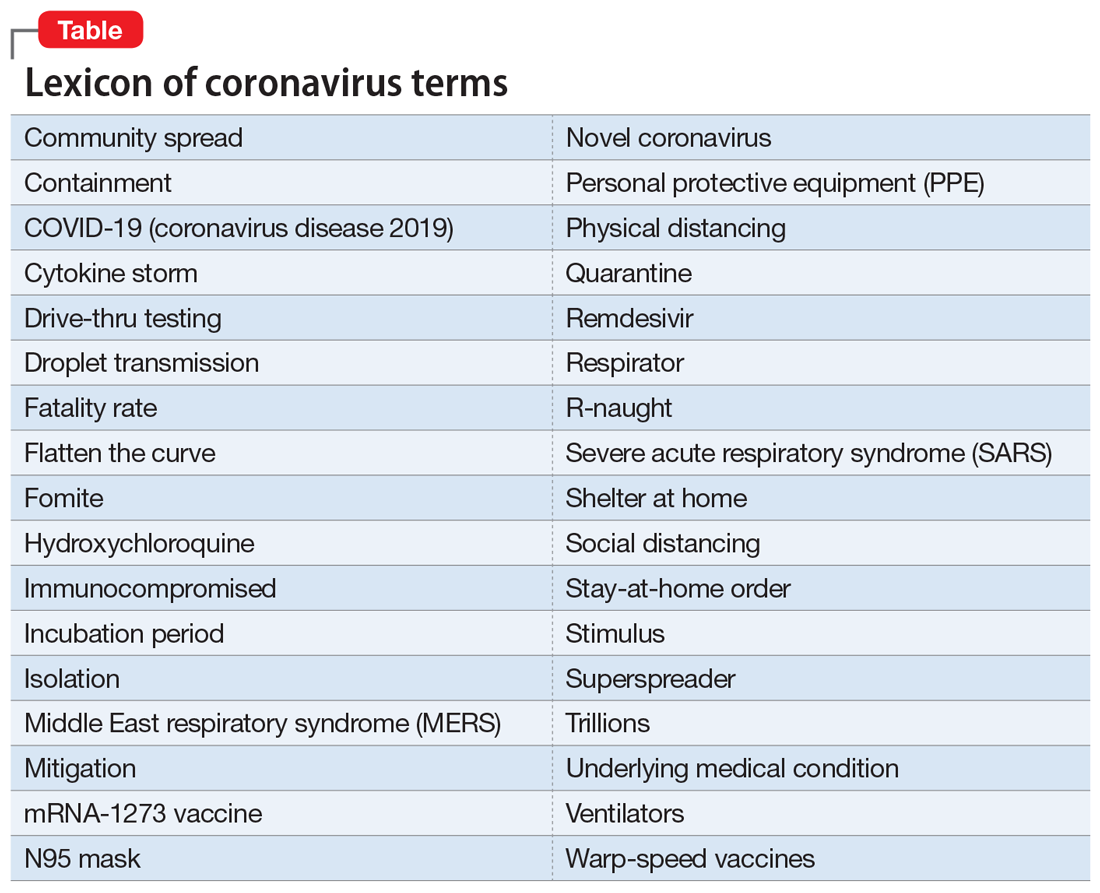
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
New-onset psychosis while being treated for coronavirus
CASE Agitated, psychotic, and COVID-19–positive
Mr. G, age 56, is brought to the emergency department (ED) by emergency medical services (EMS) after his girlfriend reports that he was trying to climb into the “fiery furnace” to “burn the devil within him.” Mr. G had recently tested positive for coronavirus disease 2019 (COVID-19) via polymerase chain reaction and had been receiving treatment for it. In the ED, he is distressed and repeatedly exclaims, “The devil is alive!” He insists on covering himself with blankets, despite diaphoresis and soaking through his clothing within minutes. Because he does not respond to attempted redirection, the ED clinicians administer a single dose of IM haloperidol, 2 mg, for agitation.
HISTORY Multiple ED visits and hospitalizations
Mr. G, who has no known psychiatric history, lives with his girlfriend of 10 years. His medical history includes chronic obstructive pulmonary disease and prostate cancer. In 2015, he had a radical prostatectomy, without chemotherapy. His social history includes childhood neglect, which prompted him to leave home when he was a teenager. Mr. G had earned his general education development certificate and worked at a small retail store.
Mr. G had no previous history of mental health treatment per self-report, collateral information from his girlfriend, and chart review. He reported no known family psychiatric history. He did not endorse past psychiatric admissions or suicide attempts, nor previous periods of mania, depression, or psychosis. He said he used illicit substances as a teen, but denied using alcohol, tobacco products, or illicit substances in the past 20 years.
Mr. G recently had multiple ED visits and hospitalizations due to ongoing signs and symptoms associated with his COVID-19 diagnosis, primarily worsening shortness of breath and cough. Eleven days before EMS brought him to the ED at his girlfriend’s request, Mr. G had presented to the ED with chief complaints of shortness of breath and dry cough (Day 0). He reported that he had been “running a fever” for 2 days. In the ED, his initial vital signs were notable only for a temperature of 100.9°F (38.28°C). He was diagnosed with “acute viral syndrome” and received 1 dose of IV ceftriaxone, 2 g, and IV azithromycin, 500 mg. On Day 2, the ED clinicians prescribed a 4-day course of oral azithromycin, 250 mg/d, and discharged him home.
On Day 3, Mr. G returned to the ED with similar complaints—congestion and productive cough. He tested positive for COVID-19, and the ED discharged him home with quarantine instructions. Hours later, he returned to the ED via EMS with chief complaints of chest pain, diarrhea, and myalgias. He was prescribed a 5-day course ofoseltamivir, 75 mg twice daily, and azithromycin, 250 mg/d. The ED again discharged him home.
On Day 4, Mr. G returned to the ED for a fourth time. His chief complaint was worsening shortness of breath. His oxygen saturation was 94% on room air; it improved to 96% on 2 L of oxygen. His chest X-ray showed diffuse reticulonodular opacities throughout his bilateral lung fields and increased airspace opacification in the bilateral lower lobes. The ED admitted Mr. G to an internal medicine unit, where the primary treatment team enrolled him in a clinical trial. As part of the trial, Mr. G received hydroxychloroquine, 400 mg, on Day 4 and Day 5. The placebo-controlled component of the trial involved Mr. G receiving daily infusions of either remdesivir or placebo on Day 6 through Day 8. On Day 8, Mr. G was discharged home.
On Day 9, Mr. G returned to the ED with a chief complaint that his “thermometer wasn’t working” at home. The ED readmitted him to the internal medicine unit. On Day 9 through Day 11, Mr. G received daily doses of
Continue to: During the second hospitalization...
During the second hospitalization, nursing staff reported that Mr. G seemed religiously preoccupied and once reported seeing angels and demons. He was observed sitting in a chair praying to Allah that he would “come in on a horse to chop all the workers’ heads off.”
On Day 11, Mr. G was discharged home. Later that evening, the EMS brought him back in the ED due to his girlfriend’s concerns about his mental state.
EVALUATION Talks to God
On Day 12, psychiatry is consulted to evaluate Mr. G’s new-onset psychosis. Mr. G is alert and oriented to person, place, and time. His speech is loud, though the amount and rate are unremarkable. He displays no psychomotor agitation. His thought process is tangential and focuses on religious themes, specifically referring to Islam. He reports auditory hallucinations of God speaking directly to him. Mr. G states, “I am here because of a miraculous transformation from death back to life. Do you believe in God? Which God do you believe in? There are 2 Gods and only one of them is the true God. He is the God of all the 7 heavens and His true name is Allah, only one God, one faith. Allah is a ball of energy.”
Mr. G’s girlfriend provides collateral information that Mr. G had been raised Christian but was not religious as an adult. She says that he had never spoken about being Muslim. She adds that she had never known him to speak much about religion.
[polldaddy:10572249]
The authors’ observations
The etiology of new-onset psychosis can be related to several factors, including primary psychiatric illnesses, use of illicit substances, sequelae of general medical conditions, or adverse effects of prescribed medications. We considered each of these in the differential diagnosis for Mr. G.
Continue to: Psychiatric illness or illicit substance use
Psychiatric illness or illicit substance use. Because Mr. G was 56 years old and had no known psychiatric history or family psychiatric history, a primary psychiatric illness seemed less likely. Substance-induced psychosis related to illicit substance use also seemed unlikely because he denied using illicit substances, and an expanded urine drug screen was negative.
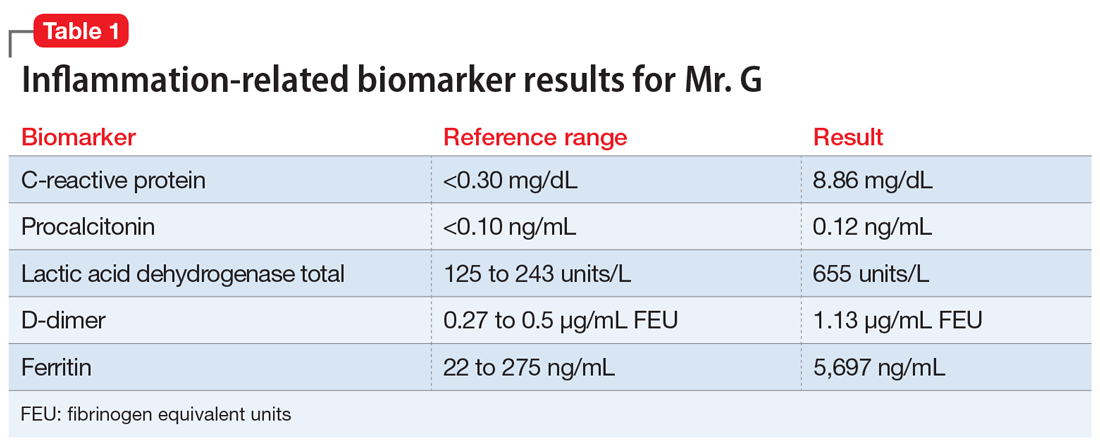
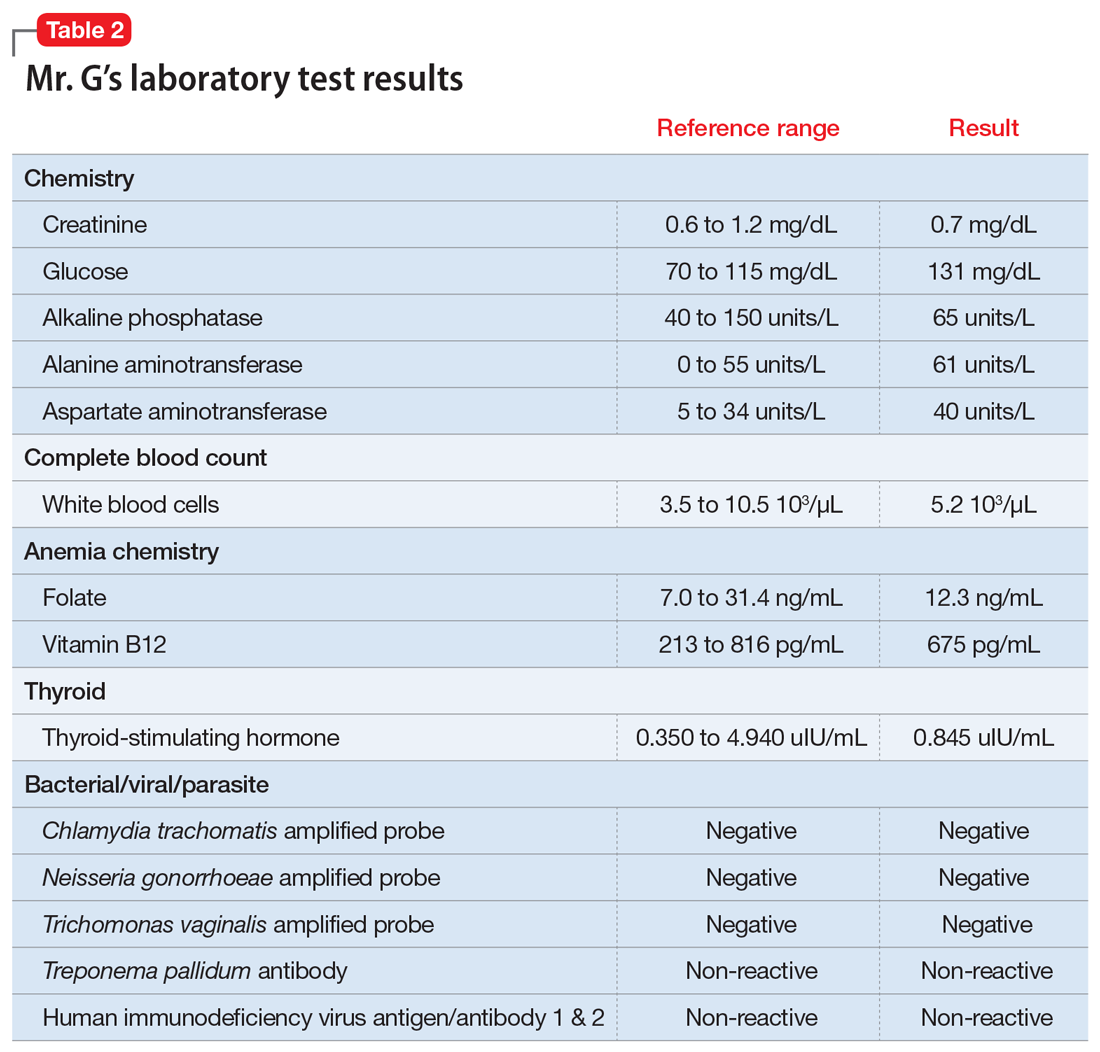
Psychosis due to a general medical condition. Results from Mr. G’s laboratory workup show marked elevation in multiple inflammation-related biomarkers (Table 1), consistent with the inflammatory profile seen with COVID-19 infection. However, results from several laboratory tests for potential etiologies of new-onset psychosis due to a general medical condition were negative (Table 2). Based on Mr. G’s history of prostate cancer, we considered the possibility of metastatic space-occupying lesions of the brain; however, Mr. G’s head CT showed no acute intracranial abnormalities. Another possible etiology we considered was COVID-19–induced encephalitis; however, Mr. G’s brain MRI with and without contrast showed no evidence of acute or chronic intracranial changes.
Medication-induced psychosis. After largely ruling out primary psychiatric illnesses, illicit substances, and sequelae of general medical conditions, we turned our attention to prescribed medications as a potential etiology of Mr. G’s new-onset psychosis. During his initial hospitalization, Mr. G had been prescribed 2 doses of hydroxychloroquine, 400 mg, to treat his diagnosis of COVID-19. Because none of the other medications he received were reported to have neuropsychiatric adverse effects, including psychosis, hydroxychloroquine-induced psychosis was therefore the primary team’s working diagnosis.
EVALUATION Request to leave AMA
On Day 13, Mr. G requests to leave the hospital against medical advice (AMA). Until this point, he had voluntarily remained in the hospital, which he repeatedly referred to as “Heaven.” When asked to describe his medical condition, Mr. G replies, “God told me my condition is far beyond man’s understanding.” He denies that he is positive for COVID-19. He states, “I am cured, and the real fight has just begun.”
At the recommendation of the psychiatry consultation-liaison (C-L) service, the primary treatment team determines that Mr. G does not have capacity to leave AMA. The team is concerned that because of his psychotic symptoms, Mr. G would be unable to understand and follow his quarantine instructions. He remains hospitalized on a medical hold.
Continue to: The authors' observations
The authors’ observations
One important consideration this case highlighted was potential third-party responsibility clinicians and hospital systems may face if they discharge a patient with a communicable illness who is unable to follow precautions based on a psychiatric condition.1 That concern was based on Mr. G’s reported desire to pursue missions “beyond man’s understanding,” which he felt compelled to complete, and which could unnecessarily place the public at risk. The psychiatry C-L service consulted the local health department and conferred with the hospital’s legal representatives, who agreed with the plan to keep Mr. G in the hospital for his safety as well as for the public’s safety.
TREATMENT Oral haloperidol
The psychiatry C-L service recommends initiating an antipsychotic. On Day 13, Mr. G starts oral haloperidol, 2.5 mg twice a day, to address his ongoing psychotic symptoms. On Day 14, the treatment team increases the dosage to 5 mg twice a day. Mr. G tolerates the haloperidol and gradually begins to improve. He demonstrates improved sleep, normal speech volume, less religious preoccupation, and a considerably improved understanding of his medical condition.
The authors’ observations
Mr. G’s initial psychiatric evaluation demonstrated an acute onset of psychotic symptoms, without evidence of delirium. Psychosis secondary to a general medical condition (such as COVID-19) and hydroxychloroquine-induced psychotic disorder topped our initial considerations in the differential diagnosis of this case. While the exact neuropsychiatric sequelae of COVID-19 are not yet clear, previous experiences with viral pandemics and case studies from the current pandemic demonstrate a wide variety of possible neuropsychiatric manifestations. Mood symptoms, psychosis, and encephalopathy represent some of the neuropsychiatric complications observed with past viral pandemics.2 Neuropsychiatric symptoms may be triggered by the virus itself, or from the host’s immune response to the infection.3 To further complicate matters, neuropsychiatric symptoms may manifest during the acute viral infection, or may surface later, as subacute or chronic neuropsychiatric illness.
Neuropsychiatric adverse events
Mr. G developed psychotic symptoms within the first few days of receiving hydroxychloroquine, which is consistent with the scant literature on this topic.8 Based on the available information, hydroxychloroquine remains the most likely etiology of his new-onset psychotic symptoms. Mr. G’s case is one example of the possible neuropsychiatric presentations clinicians may face while treating a novel viral illness.
Continue to: OUTCOME Homeward-bound
OUTCOME Homeward-bound
By Day 18, Mr. G’s psychotic symptoms have significantly improved. He is able to rationally process information about his COVID-19 diagnosis and the recommended quarantine instructions he needs to follow after discharge. He is cleared by infection control and discharged home to return to living with his girlfriend.
Mr. G attends his follow-up psychiatric appointment remotely 2 weeks after discharge. He reports that since discharge, he has continued taking his prescribed haloperidol, 5 mg twice a day. He demonstrates improved insight into his medical condition, acknowledging his COVID-19–positive status, and confirms that he has been following quarantine instructions. He does not report ongoing auditory or visual hallucinations, and is no longer religiously preoccupied. He says he is looking forward to being medically cleared to return to work.
The authors’ observations
This case highlights the need for prospective, longitudinal screening and monitoring of neuropsychiatric symptoms as part of the public health response to COVID-19. The case also highlights the importance of careful monitoring for adverse events, including neuropsychiatric symptoms, during clinical trials that involve experimental treatments. The long-term prognosis for individuals such as Mr. G who develop neuropsychiatric symptoms during acute COVID-19 infection remains unknown. Similarly, subacute and chronic neuropsychiatric manifestations that may develop after resolution of acute COVID-19 infection are unknown at this time. However, we can learn from past viral pandemics and anticipate that neuropsychiatric sequelae are likely to occur and should be part of the public health response to the pandemic.
Bottom Line
The coronavirus disease 2019 pandemic provides multiple clinical challenges pertinent to psychiatry. Neuropsychiatric symptoms may manifest from delirium, viral infection, host immune response, or adverse reactions to experimental treatments. These potential neuropsychiatric symptoms may complicate medical treatment. They can also raise important ethical and legal considerations, such as weighing patient autonomy vs third-party responsibility to the public at large.
Related Resources
- Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. 2020. doi: 10.1016/j.psym.2020.05.012.
- Vlessides M. COVID-19 and psychosis: is there a link? Medscape Medical News. https://www.medscape.com/viewarticle/930224. Published May 8, 2020.
Drug Brand Names
Azithromycin • Zithromax
Ceftriaxone • Rocephin
Chloroquine • Aralen
Haloperidol • Haldol
Hydroxychloroquine • Plaquenil
Levofloxacin • Levaquin
Oseltamivir • Tamiflu
1. Ghossoub E, Newman WJ. COVID-19 and the duty to protect from communicable diseases. [published online ahead of print, May 8, 2020]. J Am Acad Psychiatry Law.
2. Menninger Ka. Psychoses associated with influenza: I. general data: statistical analysis. JAMA. 1919;72(4):235-241.
3. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior, and Immunity. 2020. doi:10.1016/j.bbi.2020.04.027.
4. Alkadi HO. Antimalarial drug toxicity: a review. Chemotherapy. 2007;53(6):385-391.
5. Bogaczewicz A, Sobów T. Psychiatric adverse effects of chloroquine. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-114.
6. Sato K, Mano T, Iwata A, et al. Neuropsychiatric adverse events of chloroquine: a real-world pharmacovigilance study using the FDA Adverse Event Reporting System (FAERS) database. Biosci Trends. 2020;14(2):139-143.
7. Cortegiani A, Ingoglia G, Ippolito M, et al. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279-283.
8. Das P, Rai A, Chopra A, et al. Psychosis likely induced by hydroxychloroquine in a patient with chronic Q fever: a case report and clinically relevant review of pharmacology. Psychosomatics. 2014;55(4):409-413.
CASE Agitated, psychotic, and COVID-19–positive
Mr. G, age 56, is brought to the emergency department (ED) by emergency medical services (EMS) after his girlfriend reports that he was trying to climb into the “fiery furnace” to “burn the devil within him.” Mr. G had recently tested positive for coronavirus disease 2019 (COVID-19) via polymerase chain reaction and had been receiving treatment for it. In the ED, he is distressed and repeatedly exclaims, “The devil is alive!” He insists on covering himself with blankets, despite diaphoresis and soaking through his clothing within minutes. Because he does not respond to attempted redirection, the ED clinicians administer a single dose of IM haloperidol, 2 mg, for agitation.
HISTORY Multiple ED visits and hospitalizations
Mr. G, who has no known psychiatric history, lives with his girlfriend of 10 years. His medical history includes chronic obstructive pulmonary disease and prostate cancer. In 2015, he had a radical prostatectomy, without chemotherapy. His social history includes childhood neglect, which prompted him to leave home when he was a teenager. Mr. G had earned his general education development certificate and worked at a small retail store.
Mr. G had no previous history of mental health treatment per self-report, collateral information from his girlfriend, and chart review. He reported no known family psychiatric history. He did not endorse past psychiatric admissions or suicide attempts, nor previous periods of mania, depression, or psychosis. He said he used illicit substances as a teen, but denied using alcohol, tobacco products, or illicit substances in the past 20 years.
Mr. G recently had multiple ED visits and hospitalizations due to ongoing signs and symptoms associated with his COVID-19 diagnosis, primarily worsening shortness of breath and cough. Eleven days before EMS brought him to the ED at his girlfriend’s request, Mr. G had presented to the ED with chief complaints of shortness of breath and dry cough (Day 0). He reported that he had been “running a fever” for 2 days. In the ED, his initial vital signs were notable only for a temperature of 100.9°F (38.28°C). He was diagnosed with “acute viral syndrome” and received 1 dose of IV ceftriaxone, 2 g, and IV azithromycin, 500 mg. On Day 2, the ED clinicians prescribed a 4-day course of oral azithromycin, 250 mg/d, and discharged him home.
On Day 3, Mr. G returned to the ED with similar complaints—congestion and productive cough. He tested positive for COVID-19, and the ED discharged him home with quarantine instructions. Hours later, he returned to the ED via EMS with chief complaints of chest pain, diarrhea, and myalgias. He was prescribed a 5-day course ofoseltamivir, 75 mg twice daily, and azithromycin, 250 mg/d. The ED again discharged him home.
On Day 4, Mr. G returned to the ED for a fourth time. His chief complaint was worsening shortness of breath. His oxygen saturation was 94% on room air; it improved to 96% on 2 L of oxygen. His chest X-ray showed diffuse reticulonodular opacities throughout his bilateral lung fields and increased airspace opacification in the bilateral lower lobes. The ED admitted Mr. G to an internal medicine unit, where the primary treatment team enrolled him in a clinical trial. As part of the trial, Mr. G received hydroxychloroquine, 400 mg, on Day 4 and Day 5. The placebo-controlled component of the trial involved Mr. G receiving daily infusions of either remdesivir or placebo on Day 6 through Day 8. On Day 8, Mr. G was discharged home.
On Day 9, Mr. G returned to the ED with a chief complaint that his “thermometer wasn’t working” at home. The ED readmitted him to the internal medicine unit. On Day 9 through Day 11, Mr. G received daily doses of
Continue to: During the second hospitalization...
During the second hospitalization, nursing staff reported that Mr. G seemed religiously preoccupied and once reported seeing angels and demons. He was observed sitting in a chair praying to Allah that he would “come in on a horse to chop all the workers’ heads off.”
On Day 11, Mr. G was discharged home. Later that evening, the EMS brought him back in the ED due to his girlfriend’s concerns about his mental state.
EVALUATION Talks to God
On Day 12, psychiatry is consulted to evaluate Mr. G’s new-onset psychosis. Mr. G is alert and oriented to person, place, and time. His speech is loud, though the amount and rate are unremarkable. He displays no psychomotor agitation. His thought process is tangential and focuses on religious themes, specifically referring to Islam. He reports auditory hallucinations of God speaking directly to him. Mr. G states, “I am here because of a miraculous transformation from death back to life. Do you believe in God? Which God do you believe in? There are 2 Gods and only one of them is the true God. He is the God of all the 7 heavens and His true name is Allah, only one God, one faith. Allah is a ball of energy.”
Mr. G’s girlfriend provides collateral information that Mr. G had been raised Christian but was not religious as an adult. She says that he had never spoken about being Muslim. She adds that she had never known him to speak much about religion.
[polldaddy:10572249]
The authors’ observations
The etiology of new-onset psychosis can be related to several factors, including primary psychiatric illnesses, use of illicit substances, sequelae of general medical conditions, or adverse effects of prescribed medications. We considered each of these in the differential diagnosis for Mr. G.
Continue to: Psychiatric illness or illicit substance use
Psychiatric illness or illicit substance use. Because Mr. G was 56 years old and had no known psychiatric history or family psychiatric history, a primary psychiatric illness seemed less likely. Substance-induced psychosis related to illicit substance use also seemed unlikely because he denied using illicit substances, and an expanded urine drug screen was negative.
Psychosis due to a general medical condition. Results from Mr. G’s laboratory workup show marked elevation in multiple inflammation-related biomarkers (Table 1), consistent with the inflammatory profile seen with COVID-19 infection. However, results from several laboratory tests for potential etiologies of new-onset psychosis due to a general medical condition were negative (Table 2). Based on Mr. G’s history of prostate cancer, we considered the possibility of metastatic space-occupying lesions of the brain; however, Mr. G’s head CT showed no acute intracranial abnormalities. Another possible etiology we considered was COVID-19–induced encephalitis; however, Mr. G’s brain MRI with and without contrast showed no evidence of acute or chronic intracranial changes.
Medication-induced psychosis. After largely ruling out primary psychiatric illnesses, illicit substances, and sequelae of general medical conditions, we turned our attention to prescribed medications as a potential etiology of Mr. G’s new-onset psychosis. During his initial hospitalization, Mr. G had been prescribed 2 doses of hydroxychloroquine, 400 mg, to treat his diagnosis of COVID-19. Because none of the other medications he received were reported to have neuropsychiatric adverse effects, including psychosis, hydroxychloroquine-induced psychosis was therefore the primary team’s working diagnosis.
EVALUATION Request to leave AMA
On Day 13, Mr. G requests to leave the hospital against medical advice (AMA). Until this point, he had voluntarily remained in the hospital, which he repeatedly referred to as “Heaven.” When asked to describe his medical condition, Mr. G replies, “God told me my condition is far beyond man’s understanding.” He denies that he is positive for COVID-19. He states, “I am cured, and the real fight has just begun.”
At the recommendation of the psychiatry consultation-liaison (C-L) service, the primary treatment team determines that Mr. G does not have capacity to leave AMA. The team is concerned that because of his psychotic symptoms, Mr. G would be unable to understand and follow his quarantine instructions. He remains hospitalized on a medical hold.
Continue to: The authors' observations
The authors’ observations
One important consideration this case highlighted was potential third-party responsibility clinicians and hospital systems may face if they discharge a patient with a communicable illness who is unable to follow precautions based on a psychiatric condition.1 That concern was based on Mr. G’s reported desire to pursue missions “beyond man’s understanding,” which he felt compelled to complete, and which could unnecessarily place the public at risk. The psychiatry C-L service consulted the local health department and conferred with the hospital’s legal representatives, who agreed with the plan to keep Mr. G in the hospital for his safety as well as for the public’s safety.
TREATMENT Oral haloperidol
The psychiatry C-L service recommends initiating an antipsychotic. On Day 13, Mr. G starts oral haloperidol, 2.5 mg twice a day, to address his ongoing psychotic symptoms. On Day 14, the treatment team increases the dosage to 5 mg twice a day. Mr. G tolerates the haloperidol and gradually begins to improve. He demonstrates improved sleep, normal speech volume, less religious preoccupation, and a considerably improved understanding of his medical condition.
The authors’ observations
Mr. G’s initial psychiatric evaluation demonstrated an acute onset of psychotic symptoms, without evidence of delirium. Psychosis secondary to a general medical condition (such as COVID-19) and hydroxychloroquine-induced psychotic disorder topped our initial considerations in the differential diagnosis of this case. While the exact neuropsychiatric sequelae of COVID-19 are not yet clear, previous experiences with viral pandemics and case studies from the current pandemic demonstrate a wide variety of possible neuropsychiatric manifestations. Mood symptoms, psychosis, and encephalopathy represent some of the neuropsychiatric complications observed with past viral pandemics.2 Neuropsychiatric symptoms may be triggered by the virus itself, or from the host’s immune response to the infection.3 To further complicate matters, neuropsychiatric symptoms may manifest during the acute viral infection, or may surface later, as subacute or chronic neuropsychiatric illness.
Neuropsychiatric adverse events
Mr. G developed psychotic symptoms within the first few days of receiving hydroxychloroquine, which is consistent with the scant literature on this topic.8 Based on the available information, hydroxychloroquine remains the most likely etiology of his new-onset psychotic symptoms. Mr. G’s case is one example of the possible neuropsychiatric presentations clinicians may face while treating a novel viral illness.
Continue to: OUTCOME Homeward-bound
OUTCOME Homeward-bound
By Day 18, Mr. G’s psychotic symptoms have significantly improved. He is able to rationally process information about his COVID-19 diagnosis and the recommended quarantine instructions he needs to follow after discharge. He is cleared by infection control and discharged home to return to living with his girlfriend.
Mr. G attends his follow-up psychiatric appointment remotely 2 weeks after discharge. He reports that since discharge, he has continued taking his prescribed haloperidol, 5 mg twice a day. He demonstrates improved insight into his medical condition, acknowledging his COVID-19–positive status, and confirms that he has been following quarantine instructions. He does not report ongoing auditory or visual hallucinations, and is no longer religiously preoccupied. He says he is looking forward to being medically cleared to return to work.
The authors’ observations
This case highlights the need for prospective, longitudinal screening and monitoring of neuropsychiatric symptoms as part of the public health response to COVID-19. The case also highlights the importance of careful monitoring for adverse events, including neuropsychiatric symptoms, during clinical trials that involve experimental treatments. The long-term prognosis for individuals such as Mr. G who develop neuropsychiatric symptoms during acute COVID-19 infection remains unknown. Similarly, subacute and chronic neuropsychiatric manifestations that may develop after resolution of acute COVID-19 infection are unknown at this time. However, we can learn from past viral pandemics and anticipate that neuropsychiatric sequelae are likely to occur and should be part of the public health response to the pandemic.
Bottom Line
The coronavirus disease 2019 pandemic provides multiple clinical challenges pertinent to psychiatry. Neuropsychiatric symptoms may manifest from delirium, viral infection, host immune response, or adverse reactions to experimental treatments. These potential neuropsychiatric symptoms may complicate medical treatment. They can also raise important ethical and legal considerations, such as weighing patient autonomy vs third-party responsibility to the public at large.
Related Resources
- Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. 2020. doi: 10.1016/j.psym.2020.05.012.
- Vlessides M. COVID-19 and psychosis: is there a link? Medscape Medical News. https://www.medscape.com/viewarticle/930224. Published May 8, 2020.
Drug Brand Names
Azithromycin • Zithromax
Ceftriaxone • Rocephin
Chloroquine • Aralen
Haloperidol • Haldol
Hydroxychloroquine • Plaquenil
Levofloxacin • Levaquin
Oseltamivir • Tamiflu
CASE Agitated, psychotic, and COVID-19–positive
Mr. G, age 56, is brought to the emergency department (ED) by emergency medical services (EMS) after his girlfriend reports that he was trying to climb into the “fiery furnace” to “burn the devil within him.” Mr. G had recently tested positive for coronavirus disease 2019 (COVID-19) via polymerase chain reaction and had been receiving treatment for it. In the ED, he is distressed and repeatedly exclaims, “The devil is alive!” He insists on covering himself with blankets, despite diaphoresis and soaking through his clothing within minutes. Because he does not respond to attempted redirection, the ED clinicians administer a single dose of IM haloperidol, 2 mg, for agitation.
HISTORY Multiple ED visits and hospitalizations
Mr. G, who has no known psychiatric history, lives with his girlfriend of 10 years. His medical history includes chronic obstructive pulmonary disease and prostate cancer. In 2015, he had a radical prostatectomy, without chemotherapy. His social history includes childhood neglect, which prompted him to leave home when he was a teenager. Mr. G had earned his general education development certificate and worked at a small retail store.
Mr. G had no previous history of mental health treatment per self-report, collateral information from his girlfriend, and chart review. He reported no known family psychiatric history. He did not endorse past psychiatric admissions or suicide attempts, nor previous periods of mania, depression, or psychosis. He said he used illicit substances as a teen, but denied using alcohol, tobacco products, or illicit substances in the past 20 years.
Mr. G recently had multiple ED visits and hospitalizations due to ongoing signs and symptoms associated with his COVID-19 diagnosis, primarily worsening shortness of breath and cough. Eleven days before EMS brought him to the ED at his girlfriend’s request, Mr. G had presented to the ED with chief complaints of shortness of breath and dry cough (Day 0). He reported that he had been “running a fever” for 2 days. In the ED, his initial vital signs were notable only for a temperature of 100.9°F (38.28°C). He was diagnosed with “acute viral syndrome” and received 1 dose of IV ceftriaxone, 2 g, and IV azithromycin, 500 mg. On Day 2, the ED clinicians prescribed a 4-day course of oral azithromycin, 250 mg/d, and discharged him home.
On Day 3, Mr. G returned to the ED with similar complaints—congestion and productive cough. He tested positive for COVID-19, and the ED discharged him home with quarantine instructions. Hours later, he returned to the ED via EMS with chief complaints of chest pain, diarrhea, and myalgias. He was prescribed a 5-day course ofoseltamivir, 75 mg twice daily, and azithromycin, 250 mg/d. The ED again discharged him home.
On Day 4, Mr. G returned to the ED for a fourth time. His chief complaint was worsening shortness of breath. His oxygen saturation was 94% on room air; it improved to 96% on 2 L of oxygen. His chest X-ray showed diffuse reticulonodular opacities throughout his bilateral lung fields and increased airspace opacification in the bilateral lower lobes. The ED admitted Mr. G to an internal medicine unit, where the primary treatment team enrolled him in a clinical trial. As part of the trial, Mr. G received hydroxychloroquine, 400 mg, on Day 4 and Day 5. The placebo-controlled component of the trial involved Mr. G receiving daily infusions of either remdesivir or placebo on Day 6 through Day 8. On Day 8, Mr. G was discharged home.
On Day 9, Mr. G returned to the ED with a chief complaint that his “thermometer wasn’t working” at home. The ED readmitted him to the internal medicine unit. On Day 9 through Day 11, Mr. G received daily doses of
Continue to: During the second hospitalization...
During the second hospitalization, nursing staff reported that Mr. G seemed religiously preoccupied and once reported seeing angels and demons. He was observed sitting in a chair praying to Allah that he would “come in on a horse to chop all the workers’ heads off.”
On Day 11, Mr. G was discharged home. Later that evening, the EMS brought him back in the ED due to his girlfriend’s concerns about his mental state.
EVALUATION Talks to God
On Day 12, psychiatry is consulted to evaluate Mr. G’s new-onset psychosis. Mr. G is alert and oriented to person, place, and time. His speech is loud, though the amount and rate are unremarkable. He displays no psychomotor agitation. His thought process is tangential and focuses on religious themes, specifically referring to Islam. He reports auditory hallucinations of God speaking directly to him. Mr. G states, “I am here because of a miraculous transformation from death back to life. Do you believe in God? Which God do you believe in? There are 2 Gods and only one of them is the true God. He is the God of all the 7 heavens and His true name is Allah, only one God, one faith. Allah is a ball of energy.”
Mr. G’s girlfriend provides collateral information that Mr. G had been raised Christian but was not religious as an adult. She says that he had never spoken about being Muslim. She adds that she had never known him to speak much about religion.
[polldaddy:10572249]
The authors’ observations
The etiology of new-onset psychosis can be related to several factors, including primary psychiatric illnesses, use of illicit substances, sequelae of general medical conditions, or adverse effects of prescribed medications. We considered each of these in the differential diagnosis for Mr. G.
Continue to: Psychiatric illness or illicit substance use
Psychiatric illness or illicit substance use. Because Mr. G was 56 years old and had no known psychiatric history or family psychiatric history, a primary psychiatric illness seemed less likely. Substance-induced psychosis related to illicit substance use also seemed unlikely because he denied using illicit substances, and an expanded urine drug screen was negative.
Psychosis due to a general medical condition. Results from Mr. G’s laboratory workup show marked elevation in multiple inflammation-related biomarkers (Table 1), consistent with the inflammatory profile seen with COVID-19 infection. However, results from several laboratory tests for potential etiologies of new-onset psychosis due to a general medical condition were negative (Table 2). Based on Mr. G’s history of prostate cancer, we considered the possibility of metastatic space-occupying lesions of the brain; however, Mr. G’s head CT showed no acute intracranial abnormalities. Another possible etiology we considered was COVID-19–induced encephalitis; however, Mr. G’s brain MRI with and without contrast showed no evidence of acute or chronic intracranial changes.
Medication-induced psychosis. After largely ruling out primary psychiatric illnesses, illicit substances, and sequelae of general medical conditions, we turned our attention to prescribed medications as a potential etiology of Mr. G’s new-onset psychosis. During his initial hospitalization, Mr. G had been prescribed 2 doses of hydroxychloroquine, 400 mg, to treat his diagnosis of COVID-19. Because none of the other medications he received were reported to have neuropsychiatric adverse effects, including psychosis, hydroxychloroquine-induced psychosis was therefore the primary team’s working diagnosis.
EVALUATION Request to leave AMA
On Day 13, Mr. G requests to leave the hospital against medical advice (AMA). Until this point, he had voluntarily remained in the hospital, which he repeatedly referred to as “Heaven.” When asked to describe his medical condition, Mr. G replies, “God told me my condition is far beyond man’s understanding.” He denies that he is positive for COVID-19. He states, “I am cured, and the real fight has just begun.”
At the recommendation of the psychiatry consultation-liaison (C-L) service, the primary treatment team determines that Mr. G does not have capacity to leave AMA. The team is concerned that because of his psychotic symptoms, Mr. G would be unable to understand and follow his quarantine instructions. He remains hospitalized on a medical hold.
Continue to: The authors' observations
The authors’ observations
One important consideration this case highlighted was potential third-party responsibility clinicians and hospital systems may face if they discharge a patient with a communicable illness who is unable to follow precautions based on a psychiatric condition.1 That concern was based on Mr. G’s reported desire to pursue missions “beyond man’s understanding,” which he felt compelled to complete, and which could unnecessarily place the public at risk. The psychiatry C-L service consulted the local health department and conferred with the hospital’s legal representatives, who agreed with the plan to keep Mr. G in the hospital for his safety as well as for the public’s safety.
TREATMENT Oral haloperidol
The psychiatry C-L service recommends initiating an antipsychotic. On Day 13, Mr. G starts oral haloperidol, 2.5 mg twice a day, to address his ongoing psychotic symptoms. On Day 14, the treatment team increases the dosage to 5 mg twice a day. Mr. G tolerates the haloperidol and gradually begins to improve. He demonstrates improved sleep, normal speech volume, less religious preoccupation, and a considerably improved understanding of his medical condition.
The authors’ observations
Mr. G’s initial psychiatric evaluation demonstrated an acute onset of psychotic symptoms, without evidence of delirium. Psychosis secondary to a general medical condition (such as COVID-19) and hydroxychloroquine-induced psychotic disorder topped our initial considerations in the differential diagnosis of this case. While the exact neuropsychiatric sequelae of COVID-19 are not yet clear, previous experiences with viral pandemics and case studies from the current pandemic demonstrate a wide variety of possible neuropsychiatric manifestations. Mood symptoms, psychosis, and encephalopathy represent some of the neuropsychiatric complications observed with past viral pandemics.2 Neuropsychiatric symptoms may be triggered by the virus itself, or from the host’s immune response to the infection.3 To further complicate matters, neuropsychiatric symptoms may manifest during the acute viral infection, or may surface later, as subacute or chronic neuropsychiatric illness.
Neuropsychiatric adverse events
Mr. G developed psychotic symptoms within the first few days of receiving hydroxychloroquine, which is consistent with the scant literature on this topic.8 Based on the available information, hydroxychloroquine remains the most likely etiology of his new-onset psychotic symptoms. Mr. G’s case is one example of the possible neuropsychiatric presentations clinicians may face while treating a novel viral illness.
Continue to: OUTCOME Homeward-bound
OUTCOME Homeward-bound
By Day 18, Mr. G’s psychotic symptoms have significantly improved. He is able to rationally process information about his COVID-19 diagnosis and the recommended quarantine instructions he needs to follow after discharge. He is cleared by infection control and discharged home to return to living with his girlfriend.
Mr. G attends his follow-up psychiatric appointment remotely 2 weeks after discharge. He reports that since discharge, he has continued taking his prescribed haloperidol, 5 mg twice a day. He demonstrates improved insight into his medical condition, acknowledging his COVID-19–positive status, and confirms that he has been following quarantine instructions. He does not report ongoing auditory or visual hallucinations, and is no longer religiously preoccupied. He says he is looking forward to being medically cleared to return to work.
The authors’ observations
This case highlights the need for prospective, longitudinal screening and monitoring of neuropsychiatric symptoms as part of the public health response to COVID-19. The case also highlights the importance of careful monitoring for adverse events, including neuropsychiatric symptoms, during clinical trials that involve experimental treatments. The long-term prognosis for individuals such as Mr. G who develop neuropsychiatric symptoms during acute COVID-19 infection remains unknown. Similarly, subacute and chronic neuropsychiatric manifestations that may develop after resolution of acute COVID-19 infection are unknown at this time. However, we can learn from past viral pandemics and anticipate that neuropsychiatric sequelae are likely to occur and should be part of the public health response to the pandemic.
Bottom Line
The coronavirus disease 2019 pandemic provides multiple clinical challenges pertinent to psychiatry. Neuropsychiatric symptoms may manifest from delirium, viral infection, host immune response, or adverse reactions to experimental treatments. These potential neuropsychiatric symptoms may complicate medical treatment. They can also raise important ethical and legal considerations, such as weighing patient autonomy vs third-party responsibility to the public at large.
Related Resources
- Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. 2020. doi: 10.1016/j.psym.2020.05.012.
- Vlessides M. COVID-19 and psychosis: is there a link? Medscape Medical News. https://www.medscape.com/viewarticle/930224. Published May 8, 2020.
Drug Brand Names
Azithromycin • Zithromax
Ceftriaxone • Rocephin
Chloroquine • Aralen
Haloperidol • Haldol
Hydroxychloroquine • Plaquenil
Levofloxacin • Levaquin
Oseltamivir • Tamiflu
1. Ghossoub E, Newman WJ. COVID-19 and the duty to protect from communicable diseases. [published online ahead of print, May 8, 2020]. J Am Acad Psychiatry Law.
2. Menninger Ka. Psychoses associated with influenza: I. general data: statistical analysis. JAMA. 1919;72(4):235-241.
3. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior, and Immunity. 2020. doi:10.1016/j.bbi.2020.04.027.
4. Alkadi HO. Antimalarial drug toxicity: a review. Chemotherapy. 2007;53(6):385-391.
5. Bogaczewicz A, Sobów T. Psychiatric adverse effects of chloroquine. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-114.
6. Sato K, Mano T, Iwata A, et al. Neuropsychiatric adverse events of chloroquine: a real-world pharmacovigilance study using the FDA Adverse Event Reporting System (FAERS) database. Biosci Trends. 2020;14(2):139-143.
7. Cortegiani A, Ingoglia G, Ippolito M, et al. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279-283.
8. Das P, Rai A, Chopra A, et al. Psychosis likely induced by hydroxychloroquine in a patient with chronic Q fever: a case report and clinically relevant review of pharmacology. Psychosomatics. 2014;55(4):409-413.
1. Ghossoub E, Newman WJ. COVID-19 and the duty to protect from communicable diseases. [published online ahead of print, May 8, 2020]. J Am Acad Psychiatry Law.
2. Menninger Ka. Psychoses associated with influenza: I. general data: statistical analysis. JAMA. 1919;72(4):235-241.
3. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior, and Immunity. 2020. doi:10.1016/j.bbi.2020.04.027.
4. Alkadi HO. Antimalarial drug toxicity: a review. Chemotherapy. 2007;53(6):385-391.
5. Bogaczewicz A, Sobów T. Psychiatric adverse effects of chloroquine. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-114.
6. Sato K, Mano T, Iwata A, et al. Neuropsychiatric adverse events of chloroquine: a real-world pharmacovigilance study using the FDA Adverse Event Reporting System (FAERS) database. Biosci Trends. 2020;14(2):139-143.
7. Cortegiani A, Ingoglia G, Ippolito M, et al. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279-283.
8. Das P, Rai A, Chopra A, et al. Psychosis likely induced by hydroxychloroquine in a patient with chronic Q fever: a case report and clinically relevant review of pharmacology. Psychosomatics. 2014;55(4):409-413.
How to best use digital technology to help your patients
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
Social media attention increases citation rates for rheumatology journal articles
Social media might be the way to go for authors hoping to bump up the number of times their articles are cited by other articles, according to a presentation at the annual European Congress of Rheumatology that showed how Altmetric scores influence citation rates in journals.
Altmetrics are nontraditional bibliometrics designed to calculate scholarly impact based on online attention. The Altmetric Attention Score and donut provide a collated record of online attention. The colorful badge, which accompanies an increasing number of journal papers online, offers readers a full record of all original shares and mentions of an individual piece of scholarly content across a range of platforms, including Twitter, Facebook, online news media, blogs, Google+, Mendeley, and others.
Dimensions badges, also found on journal sites, count citations from any kind of scientific or mainstream publication. Journal citations remain one of the most recognized proxies for impact in medical research.
Assessing data from over 2,000 articles published in the two official journals of the European League Against Rheumatism – Annals of the Rheumatic Diseases (ARD) and RMD Open – during January 2015–November 2019, Paul Studenic, MD, PhD (@Stiddyo), of the Medical University of Vienna, and coauthor Caroline Ospelt, MD, PhD (@CarolineOspelt), of University Hospital Zürich, found that Altmetric Attention Scores are higher for articles published more recently, with Twitter showing by far the highest activity among the score’s subcategories.
“The total number of Twitter mentions increased by 2.8 per year from 2015 to 2019, indicating that more recently published articles were more often picked up on Twitter,” Dr. Studenic said in an interview. He noted that only original tweets that link to an article are given a full count of 1, while retweets or reposts have less impact on the score.
There are exceptions to this finding that newer articles have higher scores than older articles, he noted. A rheumatology article with one of the highest Altmetric Attention Scores (407) is a piece on the effect of habitual knuckle cracking that published in ARD in 1990. “It has one of the most colorful donuts with 42 news outlets, plus blogs, tweets, Facebook pages, Wikipedia mentions, and Mendeley reads,” Dr. Studenic said. But the article’s citation count is only 20.
“I would not say that the Altmetric Score has anything to do with the quality of the study, it’s just a measure of online popularity. So, you might be a brilliant research team that published a perfect study, but it is not of that much interest to editors, or it might not be tweeted by the journal itself because it was not found to be that interesting. In this case you will get your citations through your scientific community,” he said.
“Particularly if you look now at Altmetric Scores for what is being published on COVID-19, the numbers do not represent at all any profoundness of scientific quality, but there is a lot of tweeting of these articles and a lot of attention,” he said.
Overall, the odds for reaching the top 25% of citations increased with the time since publication. The time since publication accounted for 10% of the variability in the probability of reaching the top 25% of citations, whereas the Altmetric Attention Score accounted for about 5% of the variability.
Besides time since publication and Altmetric Attention Score, the type of article also influences citation count, the researchers found. The Altmetric Attention Score was more likely to boost the citation rate for original research and editorials, but it did little for correspondences.
The influence of Altmetric Attention Score on citation count of editorials added 16% to the 12% of variability explained by publication time. “We never found an effect for correspondence articles,” Dr. Studenic added.
Online popularity is something more likely to favor younger researchers, given their greater engagement online, he said. But he stressed that social media savvy is not absolutely necessary. “If you aren’t on social media and you want to build up a network, you can still do it by other means and your manuscript will still be seen, but I would say in that case that the attention kind of runs behind your back, whereas if you’re active on social media, you can steer it more effectively.”
The study had no outside funding. Both authors are social media advisers to ARD and RMD Open, and Dr. Ospelt is an associate editor of RMD Open and an editorial board member of ARD. Dr. Studenic reported receiving research or grant support from AbbVie, and Dr. Ospelt reported receiving consultancy fees from Gilead Sciences.
SOURCE: Studenic P and Ospelt C. Ann Rheum Dis. 2020 Jun;79(suppl 1):208.
Social media might be the way to go for authors hoping to bump up the number of times their articles are cited by other articles, according to a presentation at the annual European Congress of Rheumatology that showed how Altmetric scores influence citation rates in journals.
Altmetrics are nontraditional bibliometrics designed to calculate scholarly impact based on online attention. The Altmetric Attention Score and donut provide a collated record of online attention. The colorful badge, which accompanies an increasing number of journal papers online, offers readers a full record of all original shares and mentions of an individual piece of scholarly content across a range of platforms, including Twitter, Facebook, online news media, blogs, Google+, Mendeley, and others.
Dimensions badges, also found on journal sites, count citations from any kind of scientific or mainstream publication. Journal citations remain one of the most recognized proxies for impact in medical research.
Assessing data from over 2,000 articles published in the two official journals of the European League Against Rheumatism – Annals of the Rheumatic Diseases (ARD) and RMD Open – during January 2015–November 2019, Paul Studenic, MD, PhD (@Stiddyo), of the Medical University of Vienna, and coauthor Caroline Ospelt, MD, PhD (@CarolineOspelt), of University Hospital Zürich, found that Altmetric Attention Scores are higher for articles published more recently, with Twitter showing by far the highest activity among the score’s subcategories.
“The total number of Twitter mentions increased by 2.8 per year from 2015 to 2019, indicating that more recently published articles were more often picked up on Twitter,” Dr. Studenic said in an interview. He noted that only original tweets that link to an article are given a full count of 1, while retweets or reposts have less impact on the score.
There are exceptions to this finding that newer articles have higher scores than older articles, he noted. A rheumatology article with one of the highest Altmetric Attention Scores (407) is a piece on the effect of habitual knuckle cracking that published in ARD in 1990. “It has one of the most colorful donuts with 42 news outlets, plus blogs, tweets, Facebook pages, Wikipedia mentions, and Mendeley reads,” Dr. Studenic said. But the article’s citation count is only 20.
“I would not say that the Altmetric Score has anything to do with the quality of the study, it’s just a measure of online popularity. So, you might be a brilliant research team that published a perfect study, but it is not of that much interest to editors, or it might not be tweeted by the journal itself because it was not found to be that interesting. In this case you will get your citations through your scientific community,” he said.
“Particularly if you look now at Altmetric Scores for what is being published on COVID-19, the numbers do not represent at all any profoundness of scientific quality, but there is a lot of tweeting of these articles and a lot of attention,” he said.
Overall, the odds for reaching the top 25% of citations increased with the time since publication. The time since publication accounted for 10% of the variability in the probability of reaching the top 25% of citations, whereas the Altmetric Attention Score accounted for about 5% of the variability.
Besides time since publication and Altmetric Attention Score, the type of article also influences citation count, the researchers found. The Altmetric Attention Score was more likely to boost the citation rate for original research and editorials, but it did little for correspondences.
The influence of Altmetric Attention Score on citation count of editorials added 16% to the 12% of variability explained by publication time. “We never found an effect for correspondence articles,” Dr. Studenic added.
Online popularity is something more likely to favor younger researchers, given their greater engagement online, he said. But he stressed that social media savvy is not absolutely necessary. “If you aren’t on social media and you want to build up a network, you can still do it by other means and your manuscript will still be seen, but I would say in that case that the attention kind of runs behind your back, whereas if you’re active on social media, you can steer it more effectively.”
The study had no outside funding. Both authors are social media advisers to ARD and RMD Open, and Dr. Ospelt is an associate editor of RMD Open and an editorial board member of ARD. Dr. Studenic reported receiving research or grant support from AbbVie, and Dr. Ospelt reported receiving consultancy fees from Gilead Sciences.
SOURCE: Studenic P and Ospelt C. Ann Rheum Dis. 2020 Jun;79(suppl 1):208.
Social media might be the way to go for authors hoping to bump up the number of times their articles are cited by other articles, according to a presentation at the annual European Congress of Rheumatology that showed how Altmetric scores influence citation rates in journals.
Altmetrics are nontraditional bibliometrics designed to calculate scholarly impact based on online attention. The Altmetric Attention Score and donut provide a collated record of online attention. The colorful badge, which accompanies an increasing number of journal papers online, offers readers a full record of all original shares and mentions of an individual piece of scholarly content across a range of platforms, including Twitter, Facebook, online news media, blogs, Google+, Mendeley, and others.
Dimensions badges, also found on journal sites, count citations from any kind of scientific or mainstream publication. Journal citations remain one of the most recognized proxies for impact in medical research.
Assessing data from over 2,000 articles published in the two official journals of the European League Against Rheumatism – Annals of the Rheumatic Diseases (ARD) and RMD Open – during January 2015–November 2019, Paul Studenic, MD, PhD (@Stiddyo), of the Medical University of Vienna, and coauthor Caroline Ospelt, MD, PhD (@CarolineOspelt), of University Hospital Zürich, found that Altmetric Attention Scores are higher for articles published more recently, with Twitter showing by far the highest activity among the score’s subcategories.
“The total number of Twitter mentions increased by 2.8 per year from 2015 to 2019, indicating that more recently published articles were more often picked up on Twitter,” Dr. Studenic said in an interview. He noted that only original tweets that link to an article are given a full count of 1, while retweets or reposts have less impact on the score.
There are exceptions to this finding that newer articles have higher scores than older articles, he noted. A rheumatology article with one of the highest Altmetric Attention Scores (407) is a piece on the effect of habitual knuckle cracking that published in ARD in 1990. “It has one of the most colorful donuts with 42 news outlets, plus blogs, tweets, Facebook pages, Wikipedia mentions, and Mendeley reads,” Dr. Studenic said. But the article’s citation count is only 20.
“I would not say that the Altmetric Score has anything to do with the quality of the study, it’s just a measure of online popularity. So, you might be a brilliant research team that published a perfect study, but it is not of that much interest to editors, or it might not be tweeted by the journal itself because it was not found to be that interesting. In this case you will get your citations through your scientific community,” he said.
“Particularly if you look now at Altmetric Scores for what is being published on COVID-19, the numbers do not represent at all any profoundness of scientific quality, but there is a lot of tweeting of these articles and a lot of attention,” he said.
Overall, the odds for reaching the top 25% of citations increased with the time since publication. The time since publication accounted for 10% of the variability in the probability of reaching the top 25% of citations, whereas the Altmetric Attention Score accounted for about 5% of the variability.
Besides time since publication and Altmetric Attention Score, the type of article also influences citation count, the researchers found. The Altmetric Attention Score was more likely to boost the citation rate for original research and editorials, but it did little for correspondences.
The influence of Altmetric Attention Score on citation count of editorials added 16% to the 12% of variability explained by publication time. “We never found an effect for correspondence articles,” Dr. Studenic added.
Online popularity is something more likely to favor younger researchers, given their greater engagement online, he said. But he stressed that social media savvy is not absolutely necessary. “If you aren’t on social media and you want to build up a network, you can still do it by other means and your manuscript will still be seen, but I would say in that case that the attention kind of runs behind your back, whereas if you’re active on social media, you can steer it more effectively.”
The study had no outside funding. Both authors are social media advisers to ARD and RMD Open, and Dr. Ospelt is an associate editor of RMD Open and an editorial board member of ARD. Dr. Studenic reported receiving research or grant support from AbbVie, and Dr. Ospelt reported receiving consultancy fees from Gilead Sciences.
SOURCE: Studenic P and Ospelt C. Ann Rheum Dis. 2020 Jun;79(suppl 1):208.
FROM THE EULAR 2020 E-CONGRESS
Daily Recap: Docs are good at saving money; SARS-CoV-2 vaccine trials advance
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Novel SERD, LSZ102, shows promise for pretreated ER+ breast cancer
The oral selective estrogen receptor degrader (SERD) LSZ102 plus either ribociclib or alpelisib shows manageable safety and encouraging clinical activity in heavily pretreated estrogen receptor (ER)–positive breast cancer patients who progressed after prior endocrine therapy, according to interim results of an open-label phase 1/1b study.
The effects seen in the study, which is the first to report on an oral SERD in combination with both CDK4/6 and PI3Ka inhibitors, occurred regardless of ESR1 and PIK3CA mutations, said Komal Jhaveri, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Jhaveri reported the results at the European Society of Medical Oncology: Breast Cancer virtual meeting.
The overall response rate (ORR) among 78 patients enrolled in an LSZ102 monotherapy arm (arm A) was 1.3%, and the progression-free survival (PFS) was 1.8 months. The clinical benefit rate (CBR) was 9.1%.
Among 76 patients enrolled in an LSZ102+ribociclib arm (arm B), the ORR was 15.8%, the PFS was 6.2 months, and the CBR was 35.5%.
Among the 39 patients enrolled in an LSZ102+alpelisib arm (arm C), the ORR was 5.4%, the PFS was 3.5 months, and the CBR was 18.9%.
After the data cutoff, one additional partial response (PR) was reported in arm C, Dr. Jhaveri said, noting that two of three confirmed responses were in known PIKC3A-mutant patients.
Study participants were aged 18 years and older with a confirmed diagnosis of ER-positive breast cancer and good performance status, as well as evidence of progression after endocrine therapy for metastatic disease or evidence of progression while on therapy or within 12 months from the end of adjuvant therapy.
“For all arms, prior fulvestrant, CDK46 inhibitor, or chemotherapy were allowed. For arm C, patients with or without PIK3C were eligible, and no prior treatment with PIK3, mTOR, or AKT inhibitors was allowed,” Dr. Jhaveri said.
Dosing in the LSZ102 monotherapy arm ranged from 200 to 900 mg. Arm B patients received LSZ102 at doses of 200-600 mg and ribociclib at doses of 200-600 mg. Both continuous ribociclib and 3 weeks on/1 week off dosing were evaluated. Arm C patients received LSZ102 at doses of 300-450 mg and alpelisib at 200-300 mg.
The recommended expansion doses were 450 mg daily of LSZ102 for arm A and 450 mg LSZ102 with 400 mg of daily ribociclib for arm B. For arm C, they were 300 mg LSZ102 with 250 mg of alpelisib daily.
Of note, two of three patients with a PR in arm C had received 300 mg LSZ102 and 300 mg alpelisib, Dr. Jhaveri said.
Arm A and arm B results were presented at the San Antonio Breast Cancer Symposium in 2018 and 2019, respectively. The current report updates those findings and presents arm C data for the first time, Dr. Jhaveri said.
LSZ102 was relatively well-tolerated as a single agent and in combination with ribociclib and alpelisib, according to Dr. Jhaveri. The most frequent adverse events were gastrointestinal toxicities, including nausea, vomiting, diarrhea, and decreased appetite, which occurred across all arms.
Neutropenia and aspartate aminotransferase abnormalities, including grade 3 cases, were reported in arm B and were most likely driven by the ribociclib, Dr. Jhaveri said. Grade 3 hypoglycemia and skin rash commonly occurred in arm C, most likely driven by the alpelisib.
Five dose-limiting toxicities occurred in four patients in arm A, three occurred in two patients in arm B, and seven occurred in seven patients in arm C.
Paired biopsies collected at the time of screening and at day 15 of cycle 1 showed consistent down-regulation of ER protein levels across arms.
“No substantial dose-dependent down-regulation of the ER was observed with increasing doses of LSZ,” Dr. Jhaveri said.
Circulating tumor DNA (ctDNA) analysis showed that the dominant mutations across the arms were ESR1, PIK3CA, and TP53. These were not shown to correlate with response and were not enriched upon progression in patients with matched baseline and end-of-treatment samples, she noted.
An exploratory analysis, conducted in “a preliminary attempt to correlate clinical activity with specific mutations,” showed that, in arms B and C, respectively, ORR, CBR, and PFS weren’t correlated with the presence or absence of ESR1 and PIK3CA mutations, respectively, or the absence of detectable ctDNA from baseline samples, Dr. Jhaveri said.
“While numerically higher responses and better CBR were seen in patients with undetectable ctDNA at baseline, no statistically significant difference in any of these outcomes was observed in arms B and C,” she said.
In arm C, the numbers were small at the time of data cutoff, but incoming data suggest relatively enhanced activity of the LSZ102 plus alpelisib combination in PIKC3A-mutant patients, she noted.
“We know that inhibiting ER signaling is the mainstay of treatment for ER-positive breast cancer,” Dr. Jhaveri explained, adding that aromatase inhibitors, estrogen receptor modulators, and SERDs are important classes of antiestrogenic agents, but fulvestrant is the only approved SERD. These are effective, but many patients develop resistance, she said.
“Proposed mechanisms for endocrine resistance include activation of the cell-cycle and cell-survival signaling pathways, or of the PI3K-AKT-mTOR pathway,” Dr. Jhaveri said. “To that end, ribociclib, a CDK46 inhibitor plus fulvestrant improved survival compared to fulvestrant alone in patients with ER-positive metastatic breast cancer.”
More recently, the PI3K inhibitor alpelisib plus fulvestrant also nearly doubled PFS vs. fulvestrant alone in PIKC3A-mutant, ER-positive metastatic breast cancer, which led to the approval of the combination in the United States.
Another mechanism of endocrine resistance includes acquisition of activating mutations in the estrogen receptor gene itself that allow tumors to survive and proliferate without depending on estrogen.
EGFR mutations appear to predict resistance to aromatase inhibitor therapies, but not outcomes in patients treated with fulvestrant. However, fulvestrant, which is delivered by intramuscular injection, has its own limitations, Dr. Jhaveri said.
“LSZ102 is a novel SERD that could achieve higher exposure than fulvestrant, leading to enhanced efficacy,” she said, noting that it was shown in preclinical models to have activity and to be synergistic in combination with ribociclib and alpelisib, forming the basis for the current study.
Invited discussant, Saverio Cinieri, MD, of Ospedale Antonio Perrino, Brindisi, Italy, said the study “elegantly demonstrated that estrogen receptor protein is down-regulated by LSZ102; [that] the genomic landscape of heavily pretreated patients is dominated by mutations in ESR1, PIK3CA, and TP53; [that] common mutations do not correlate with response and are not enriched on progression; [and that] ctDNA analysis at baseline shows similar outcomes with LSZ plus ribociclib or alpelisib, regardless of mutational status.”
LSZ102 is one of four new-generation SERDs in early-phase studies, he said, concluding that “in the COVID-19 era, the use of oral therapies will be even more necessary to limit access to the hospital.”
Dr. Cinieri also said that overcoming the limitations “of a molecule like the intramuscularly administered fulvestrant goes in this direction,” and that “the clinical efficacy and the biomolecular profile of LSZ102 seems to be able to meet these real needs.”
This study was funded by Novartis. Dr. Jhaveri reported advisory and consultancy roles and/or research grants or other funding to her institution from Novartis, ADC Therapeutics, Pfizer, and numerous other pharmaceutical and biotechnology companies. Dr. Cinieri reported relationships with Lily Oncology, Pfizer, Roche, AstraZeneca, Amgen, Novartis, including honoraria, grant and research support to his institution, advisory board participation, and scientific meeting support.
sworcester@mdedge.com
SOURCE: Jhaveri K et al. ESMO Breast Cancer, Abstract LBA1.
The oral selective estrogen receptor degrader (SERD) LSZ102 plus either ribociclib or alpelisib shows manageable safety and encouraging clinical activity in heavily pretreated estrogen receptor (ER)–positive breast cancer patients who progressed after prior endocrine therapy, according to interim results of an open-label phase 1/1b study.
The effects seen in the study, which is the first to report on an oral SERD in combination with both CDK4/6 and PI3Ka inhibitors, occurred regardless of ESR1 and PIK3CA mutations, said Komal Jhaveri, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Jhaveri reported the results at the European Society of Medical Oncology: Breast Cancer virtual meeting.
The overall response rate (ORR) among 78 patients enrolled in an LSZ102 monotherapy arm (arm A) was 1.3%, and the progression-free survival (PFS) was 1.8 months. The clinical benefit rate (CBR) was 9.1%.
Among 76 patients enrolled in an LSZ102+ribociclib arm (arm B), the ORR was 15.8%, the PFS was 6.2 months, and the CBR was 35.5%.
Among the 39 patients enrolled in an LSZ102+alpelisib arm (arm C), the ORR was 5.4%, the PFS was 3.5 months, and the CBR was 18.9%.
After the data cutoff, one additional partial response (PR) was reported in arm C, Dr. Jhaveri said, noting that two of three confirmed responses were in known PIKC3A-mutant patients.
Study participants were aged 18 years and older with a confirmed diagnosis of ER-positive breast cancer and good performance status, as well as evidence of progression after endocrine therapy for metastatic disease or evidence of progression while on therapy or within 12 months from the end of adjuvant therapy.
“For all arms, prior fulvestrant, CDK46 inhibitor, or chemotherapy were allowed. For arm C, patients with or without PIK3C were eligible, and no prior treatment with PIK3, mTOR, or AKT inhibitors was allowed,” Dr. Jhaveri said.
Dosing in the LSZ102 monotherapy arm ranged from 200 to 900 mg. Arm B patients received LSZ102 at doses of 200-600 mg and ribociclib at doses of 200-600 mg. Both continuous ribociclib and 3 weeks on/1 week off dosing were evaluated. Arm C patients received LSZ102 at doses of 300-450 mg and alpelisib at 200-300 mg.
The recommended expansion doses were 450 mg daily of LSZ102 for arm A and 450 mg LSZ102 with 400 mg of daily ribociclib for arm B. For arm C, they were 300 mg LSZ102 with 250 mg of alpelisib daily.
Of note, two of three patients with a PR in arm C had received 300 mg LSZ102 and 300 mg alpelisib, Dr. Jhaveri said.
Arm A and arm B results were presented at the San Antonio Breast Cancer Symposium in 2018 and 2019, respectively. The current report updates those findings and presents arm C data for the first time, Dr. Jhaveri said.
LSZ102 was relatively well-tolerated as a single agent and in combination with ribociclib and alpelisib, according to Dr. Jhaveri. The most frequent adverse events were gastrointestinal toxicities, including nausea, vomiting, diarrhea, and decreased appetite, which occurred across all arms.
Neutropenia and aspartate aminotransferase abnormalities, including grade 3 cases, were reported in arm B and were most likely driven by the ribociclib, Dr. Jhaveri said. Grade 3 hypoglycemia and skin rash commonly occurred in arm C, most likely driven by the alpelisib.
Five dose-limiting toxicities occurred in four patients in arm A, three occurred in two patients in arm B, and seven occurred in seven patients in arm C.
Paired biopsies collected at the time of screening and at day 15 of cycle 1 showed consistent down-regulation of ER protein levels across arms.
“No substantial dose-dependent down-regulation of the ER was observed with increasing doses of LSZ,” Dr. Jhaveri said.
Circulating tumor DNA (ctDNA) analysis showed that the dominant mutations across the arms were ESR1, PIK3CA, and TP53. These were not shown to correlate with response and were not enriched upon progression in patients with matched baseline and end-of-treatment samples, she noted.
An exploratory analysis, conducted in “a preliminary attempt to correlate clinical activity with specific mutations,” showed that, in arms B and C, respectively, ORR, CBR, and PFS weren’t correlated with the presence or absence of ESR1 and PIK3CA mutations, respectively, or the absence of detectable ctDNA from baseline samples, Dr. Jhaveri said.
“While numerically higher responses and better CBR were seen in patients with undetectable ctDNA at baseline, no statistically significant difference in any of these outcomes was observed in arms B and C,” she said.
In arm C, the numbers were small at the time of data cutoff, but incoming data suggest relatively enhanced activity of the LSZ102 plus alpelisib combination in PIKC3A-mutant patients, she noted.
“We know that inhibiting ER signaling is the mainstay of treatment for ER-positive breast cancer,” Dr. Jhaveri explained, adding that aromatase inhibitors, estrogen receptor modulators, and SERDs are important classes of antiestrogenic agents, but fulvestrant is the only approved SERD. These are effective, but many patients develop resistance, she said.
“Proposed mechanisms for endocrine resistance include activation of the cell-cycle and cell-survival signaling pathways, or of the PI3K-AKT-mTOR pathway,” Dr. Jhaveri said. “To that end, ribociclib, a CDK46 inhibitor plus fulvestrant improved survival compared to fulvestrant alone in patients with ER-positive metastatic breast cancer.”
More recently, the PI3K inhibitor alpelisib plus fulvestrant also nearly doubled PFS vs. fulvestrant alone in PIKC3A-mutant, ER-positive metastatic breast cancer, which led to the approval of the combination in the United States.
Another mechanism of endocrine resistance includes acquisition of activating mutations in the estrogen receptor gene itself that allow tumors to survive and proliferate without depending on estrogen.
EGFR mutations appear to predict resistance to aromatase inhibitor therapies, but not outcomes in patients treated with fulvestrant. However, fulvestrant, which is delivered by intramuscular injection, has its own limitations, Dr. Jhaveri said.
“LSZ102 is a novel SERD that could achieve higher exposure than fulvestrant, leading to enhanced efficacy,” she said, noting that it was shown in preclinical models to have activity and to be synergistic in combination with ribociclib and alpelisib, forming the basis for the current study.
Invited discussant, Saverio Cinieri, MD, of Ospedale Antonio Perrino, Brindisi, Italy, said the study “elegantly demonstrated that estrogen receptor protein is down-regulated by LSZ102; [that] the genomic landscape of heavily pretreated patients is dominated by mutations in ESR1, PIK3CA, and TP53; [that] common mutations do not correlate with response and are not enriched on progression; [and that] ctDNA analysis at baseline shows similar outcomes with LSZ plus ribociclib or alpelisib, regardless of mutational status.”
LSZ102 is one of four new-generation SERDs in early-phase studies, he said, concluding that “in the COVID-19 era, the use of oral therapies will be even more necessary to limit access to the hospital.”
Dr. Cinieri also said that overcoming the limitations “of a molecule like the intramuscularly administered fulvestrant goes in this direction,” and that “the clinical efficacy and the biomolecular profile of LSZ102 seems to be able to meet these real needs.”
This study was funded by Novartis. Dr. Jhaveri reported advisory and consultancy roles and/or research grants or other funding to her institution from Novartis, ADC Therapeutics, Pfizer, and numerous other pharmaceutical and biotechnology companies. Dr. Cinieri reported relationships with Lily Oncology, Pfizer, Roche, AstraZeneca, Amgen, Novartis, including honoraria, grant and research support to his institution, advisory board participation, and scientific meeting support.
sworcester@mdedge.com
SOURCE: Jhaveri K et al. ESMO Breast Cancer, Abstract LBA1.
The oral selective estrogen receptor degrader (SERD) LSZ102 plus either ribociclib or alpelisib shows manageable safety and encouraging clinical activity in heavily pretreated estrogen receptor (ER)–positive breast cancer patients who progressed after prior endocrine therapy, according to interim results of an open-label phase 1/1b study.
The effects seen in the study, which is the first to report on an oral SERD in combination with both CDK4/6 and PI3Ka inhibitors, occurred regardless of ESR1 and PIK3CA mutations, said Komal Jhaveri, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Jhaveri reported the results at the European Society of Medical Oncology: Breast Cancer virtual meeting.
The overall response rate (ORR) among 78 patients enrolled in an LSZ102 monotherapy arm (arm A) was 1.3%, and the progression-free survival (PFS) was 1.8 months. The clinical benefit rate (CBR) was 9.1%.
Among 76 patients enrolled in an LSZ102+ribociclib arm (arm B), the ORR was 15.8%, the PFS was 6.2 months, and the CBR was 35.5%.
Among the 39 patients enrolled in an LSZ102+alpelisib arm (arm C), the ORR was 5.4%, the PFS was 3.5 months, and the CBR was 18.9%.
After the data cutoff, one additional partial response (PR) was reported in arm C, Dr. Jhaveri said, noting that two of three confirmed responses were in known PIKC3A-mutant patients.
Study participants were aged 18 years and older with a confirmed diagnosis of ER-positive breast cancer and good performance status, as well as evidence of progression after endocrine therapy for metastatic disease or evidence of progression while on therapy or within 12 months from the end of adjuvant therapy.
“For all arms, prior fulvestrant, CDK46 inhibitor, or chemotherapy were allowed. For arm C, patients with or without PIK3C were eligible, and no prior treatment with PIK3, mTOR, or AKT inhibitors was allowed,” Dr. Jhaveri said.
Dosing in the LSZ102 monotherapy arm ranged from 200 to 900 mg. Arm B patients received LSZ102 at doses of 200-600 mg and ribociclib at doses of 200-600 mg. Both continuous ribociclib and 3 weeks on/1 week off dosing were evaluated. Arm C patients received LSZ102 at doses of 300-450 mg and alpelisib at 200-300 mg.
The recommended expansion doses were 450 mg daily of LSZ102 for arm A and 450 mg LSZ102 with 400 mg of daily ribociclib for arm B. For arm C, they were 300 mg LSZ102 with 250 mg of alpelisib daily.
Of note, two of three patients with a PR in arm C had received 300 mg LSZ102 and 300 mg alpelisib, Dr. Jhaveri said.
Arm A and arm B results were presented at the San Antonio Breast Cancer Symposium in 2018 and 2019, respectively. The current report updates those findings and presents arm C data for the first time, Dr. Jhaveri said.
LSZ102 was relatively well-tolerated as a single agent and in combination with ribociclib and alpelisib, according to Dr. Jhaveri. The most frequent adverse events were gastrointestinal toxicities, including nausea, vomiting, diarrhea, and decreased appetite, which occurred across all arms.
Neutropenia and aspartate aminotransferase abnormalities, including grade 3 cases, were reported in arm B and were most likely driven by the ribociclib, Dr. Jhaveri said. Grade 3 hypoglycemia and skin rash commonly occurred in arm C, most likely driven by the alpelisib.
Five dose-limiting toxicities occurred in four patients in arm A, three occurred in two patients in arm B, and seven occurred in seven patients in arm C.
Paired biopsies collected at the time of screening and at day 15 of cycle 1 showed consistent down-regulation of ER protein levels across arms.
“No substantial dose-dependent down-regulation of the ER was observed with increasing doses of LSZ,” Dr. Jhaveri said.
Circulating tumor DNA (ctDNA) analysis showed that the dominant mutations across the arms were ESR1, PIK3CA, and TP53. These were not shown to correlate with response and were not enriched upon progression in patients with matched baseline and end-of-treatment samples, she noted.
An exploratory analysis, conducted in “a preliminary attempt to correlate clinical activity with specific mutations,” showed that, in arms B and C, respectively, ORR, CBR, and PFS weren’t correlated with the presence or absence of ESR1 and PIK3CA mutations, respectively, or the absence of detectable ctDNA from baseline samples, Dr. Jhaveri said.
“While numerically higher responses and better CBR were seen in patients with undetectable ctDNA at baseline, no statistically significant difference in any of these outcomes was observed in arms B and C,” she said.
In arm C, the numbers were small at the time of data cutoff, but incoming data suggest relatively enhanced activity of the LSZ102 plus alpelisib combination in PIKC3A-mutant patients, she noted.
“We know that inhibiting ER signaling is the mainstay of treatment for ER-positive breast cancer,” Dr. Jhaveri explained, adding that aromatase inhibitors, estrogen receptor modulators, and SERDs are important classes of antiestrogenic agents, but fulvestrant is the only approved SERD. These are effective, but many patients develop resistance, she said.
“Proposed mechanisms for endocrine resistance include activation of the cell-cycle and cell-survival signaling pathways, or of the PI3K-AKT-mTOR pathway,” Dr. Jhaveri said. “To that end, ribociclib, a CDK46 inhibitor plus fulvestrant improved survival compared to fulvestrant alone in patients with ER-positive metastatic breast cancer.”
More recently, the PI3K inhibitor alpelisib plus fulvestrant also nearly doubled PFS vs. fulvestrant alone in PIKC3A-mutant, ER-positive metastatic breast cancer, which led to the approval of the combination in the United States.
Another mechanism of endocrine resistance includes acquisition of activating mutations in the estrogen receptor gene itself that allow tumors to survive and proliferate without depending on estrogen.
EGFR mutations appear to predict resistance to aromatase inhibitor therapies, but not outcomes in patients treated with fulvestrant. However, fulvestrant, which is delivered by intramuscular injection, has its own limitations, Dr. Jhaveri said.
“LSZ102 is a novel SERD that could achieve higher exposure than fulvestrant, leading to enhanced efficacy,” she said, noting that it was shown in preclinical models to have activity and to be synergistic in combination with ribociclib and alpelisib, forming the basis for the current study.
Invited discussant, Saverio Cinieri, MD, of Ospedale Antonio Perrino, Brindisi, Italy, said the study “elegantly demonstrated that estrogen receptor protein is down-regulated by LSZ102; [that] the genomic landscape of heavily pretreated patients is dominated by mutations in ESR1, PIK3CA, and TP53; [that] common mutations do not correlate with response and are not enriched on progression; [and that] ctDNA analysis at baseline shows similar outcomes with LSZ plus ribociclib or alpelisib, regardless of mutational status.”
LSZ102 is one of four new-generation SERDs in early-phase studies, he said, concluding that “in the COVID-19 era, the use of oral therapies will be even more necessary to limit access to the hospital.”
Dr. Cinieri also said that overcoming the limitations “of a molecule like the intramuscularly administered fulvestrant goes in this direction,” and that “the clinical efficacy and the biomolecular profile of LSZ102 seems to be able to meet these real needs.”
This study was funded by Novartis. Dr. Jhaveri reported advisory and consultancy roles and/or research grants or other funding to her institution from Novartis, ADC Therapeutics, Pfizer, and numerous other pharmaceutical and biotechnology companies. Dr. Cinieri reported relationships with Lily Oncology, Pfizer, Roche, AstraZeneca, Amgen, Novartis, including honoraria, grant and research support to his institution, advisory board participation, and scientific meeting support.
sworcester@mdedge.com
SOURCE: Jhaveri K et al. ESMO Breast Cancer, Abstract LBA1.
FROM ESMO BREAST CANCER 2020
Managing pain expectations is key to enhanced recovery
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
FROM MISS
Phase 3 COVID-19 vaccine trials launching in July, expert says
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
FROM PEDIATRIC DERMATOLOGY 2020
Many physicians live within their means and save, survey shows
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Pursue multimodal pain management in patients taking opioids
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
FROM MISS