User login
Treatments linked to death in COVID patients with thoracic cancers
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
FROM ASCO 2020
Older adults boost muscle mass after bariatric surgery
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
FROM MISS
First validated classification criteria for discoid lupus erythematosus unveiled
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
FROM AAD 20
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Myocardial Injury Among Postoperative Patients: Where Is the Wisdom in Our Knowledge?
The ability to detect myocardial injury has never been more advanced. With the availability of high-sensitivity troponin testing, microscopic evidence of myocyte death can now be detected, often within an hour or so of the inciting event. This, in turn, has facilitated quicker and more accurate identification and treatment of affected patients. However, these advances in detection have, in some cases, outstripped our understanding of the etiology and appropriate management of troponin elevation.
This dilemma is particularly apparent among patients undergoing noncardiac surgery. Annually, over 200 million of these surgeries occur worldwide, many in patients with elevated cardiac risk or overt cardiac disease. Naturally, physicians treating these patients are concerned that the stress of surgery will provoke myocardial injury. Since symptoms are often masked in the immediate postoperative period because of sedating or analgesic medications, many physicians rely on troponin testing to detect signs of myocardial injury. With the increased sensitivity of these assays, the prevalence of troponin elevation has increased, which currently affects nearly one in five postoperative patients. This knowledge, however, doesn’t lend itself to a clear management strategy, particularly in those patients with no other objective evidence of infarction. To paraphrase T.S. Eliot, have we lost the wisdom in our knowledge?
In this journal issue, Cohn and colleagues summarize the current information around this phenomenon of myocardial injury after noncardiac surgery, or MINS.1 Consistent with the literature, they define MINS as an acute rise and/or fall in troponin (above the assay’s upper limit of normal) at any point in the 30 days following noncardiac surgery. Importantly, MINS is an umbrella term that can indicate either a myocardial infarction (MI) or nonischemic myocardial injury (NIMI). An MI exists if there are clinical signs of ischemia and/or objective evidence of infarction on imaging.
The authors found that MINS is highly prevalent (19.6%) and associated with both cardiac disease and perioperative hemodynamic stress. Between 2.9% and 13.5% of MINS patients experienced 30-day adverse cardiac events, with higher rates in patients with higher troponin elevations and/or accompanying ischemic symptoms. The authors suggested MINS management with standard cardio-protective medications, such as statins, beta-blockers, and angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers. For those patients at low bleeding risk, they also suggested dabigatran based on the recent MANAGE trial. Finally, they noted that US cardiac society guidelines suggested no screening for MINS, while the European and Canadian guidelines advocated for screening in patients at high risk for cardiac complications.
The authors are to be congratulated for highlighting an important and vexing area of postoperative management. To date, it has been difficult to chart the best path forward for these patients because we could “see” the issue, thanks to increasingly sensitive troponin assays, but we didn’t know what to do once we found it.
So what rationale exists to justify screening? Some advocate that the presence of MINS suggests a need for further imaging and closer monitoring of these patients to identify those with an MI. Indeed, several recent MINS registry studies have found that 20% to 40% of MINS patients had definitive evidence of MI.2-4 But what about those patients with troponin elevation and no evidence of MI? A small, propensity-matched, observational study of MINS patients, including those without MI, noted positive associations between cardioprotective medications, such as aspirin and statins, and cardiac outcomes.5 In addition, the MANAGE trial suggested that MINS patients, with or without evidence of an MI, receiving dabigatran had reduced vascular events without increased bleeding complications.6 With this growing base of evidence, the rationale for systematic screening for MINS appears to be standing on stronger footing.
As noted by the authors, the recommendations for MINS screening differ across three major cardiovascular societies. How does the practicing clinician make sense of this discordant advice? Differences often occur when the evidence is of moderate or low quality, which means guideline committees must make their own interpretations of equivocal findings. Another driver of discordant recommendations is the timing of the guidelines. Both the US and European guidelines were published in 2014, while the Canadian guidelines were published in 2017. Over time, experience with postoperative troponin testing increased, which may have influenced the Canadian guidelines. Finally, many members of the Canadian guideline writing committee were the ones conducting the various studies identifying management options for MINS patients, which may have guided their ultimate recommendation. Regardless, practicing physicians should collectively view the guidelines as acceptable “guardrails” to guide their practice. Selection of the appropriate strategy can then be tailored to the individual patient’s risks and benefits, as well as available management options.
In this era of high-sensitivity troponin testing, we now possess an exquisite opportunity to “see” minute levels of myocardial injury among postoperative patients. Our growing ability to effectively act on this knowledge will enable us to make wise decisions with our patients to optimize their cardiac outcomes during the vulnerable postoperative period.
1. Cohn SL, Rohatgi N, Patel P, Whinney C. Clinical progress note: myocardial injury after noncardiac surgery. J Hosp Med. 2020;15(7):412-415. https://doi.org/10.12788/jhm.3448
2. Puelacher C, Lurati Buse G, Seeberger D, et al. Perioperative myocardial injury after noncardiac surgery: incidence, mortality, and characterization. Circulation. 2018;137(12):1221-1232. https://doi.org/10.1161/circulationaha.117.030114.
3. Botto F, Alonso-Coello P, Chan MTV, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120(3):564-578. https://doi.org/10.1097/aln.0000000000000113
4. Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317(16):1642-1651. https://doi.org/10.1001/jama.2017.4360
5. Foucrier A, Rodseth R, Aissaoui M, et al. The long-term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053-1063. https://doi.org/10.1213/ane.0000000000000302
6. Devereaux PJ, Duceppe E, Guyatt G, et al. Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet. 2018;391(10137):2325-2334. https://doi.org/10.1016/s0140-6736(18)30832-8
The ability to detect myocardial injury has never been more advanced. With the availability of high-sensitivity troponin testing, microscopic evidence of myocyte death can now be detected, often within an hour or so of the inciting event. This, in turn, has facilitated quicker and more accurate identification and treatment of affected patients. However, these advances in detection have, in some cases, outstripped our understanding of the etiology and appropriate management of troponin elevation.
This dilemma is particularly apparent among patients undergoing noncardiac surgery. Annually, over 200 million of these surgeries occur worldwide, many in patients with elevated cardiac risk or overt cardiac disease. Naturally, physicians treating these patients are concerned that the stress of surgery will provoke myocardial injury. Since symptoms are often masked in the immediate postoperative period because of sedating or analgesic medications, many physicians rely on troponin testing to detect signs of myocardial injury. With the increased sensitivity of these assays, the prevalence of troponin elevation has increased, which currently affects nearly one in five postoperative patients. This knowledge, however, doesn’t lend itself to a clear management strategy, particularly in those patients with no other objective evidence of infarction. To paraphrase T.S. Eliot, have we lost the wisdom in our knowledge?
In this journal issue, Cohn and colleagues summarize the current information around this phenomenon of myocardial injury after noncardiac surgery, or MINS.1 Consistent with the literature, they define MINS as an acute rise and/or fall in troponin (above the assay’s upper limit of normal) at any point in the 30 days following noncardiac surgery. Importantly, MINS is an umbrella term that can indicate either a myocardial infarction (MI) or nonischemic myocardial injury (NIMI). An MI exists if there are clinical signs of ischemia and/or objective evidence of infarction on imaging.
The authors found that MINS is highly prevalent (19.6%) and associated with both cardiac disease and perioperative hemodynamic stress. Between 2.9% and 13.5% of MINS patients experienced 30-day adverse cardiac events, with higher rates in patients with higher troponin elevations and/or accompanying ischemic symptoms. The authors suggested MINS management with standard cardio-protective medications, such as statins, beta-blockers, and angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers. For those patients at low bleeding risk, they also suggested dabigatran based on the recent MANAGE trial. Finally, they noted that US cardiac society guidelines suggested no screening for MINS, while the European and Canadian guidelines advocated for screening in patients at high risk for cardiac complications.
The authors are to be congratulated for highlighting an important and vexing area of postoperative management. To date, it has been difficult to chart the best path forward for these patients because we could “see” the issue, thanks to increasingly sensitive troponin assays, but we didn’t know what to do once we found it.
So what rationale exists to justify screening? Some advocate that the presence of MINS suggests a need for further imaging and closer monitoring of these patients to identify those with an MI. Indeed, several recent MINS registry studies have found that 20% to 40% of MINS patients had definitive evidence of MI.2-4 But what about those patients with troponin elevation and no evidence of MI? A small, propensity-matched, observational study of MINS patients, including those without MI, noted positive associations between cardioprotective medications, such as aspirin and statins, and cardiac outcomes.5 In addition, the MANAGE trial suggested that MINS patients, with or without evidence of an MI, receiving dabigatran had reduced vascular events without increased bleeding complications.6 With this growing base of evidence, the rationale for systematic screening for MINS appears to be standing on stronger footing.
As noted by the authors, the recommendations for MINS screening differ across three major cardiovascular societies. How does the practicing clinician make sense of this discordant advice? Differences often occur when the evidence is of moderate or low quality, which means guideline committees must make their own interpretations of equivocal findings. Another driver of discordant recommendations is the timing of the guidelines. Both the US and European guidelines were published in 2014, while the Canadian guidelines were published in 2017. Over time, experience with postoperative troponin testing increased, which may have influenced the Canadian guidelines. Finally, many members of the Canadian guideline writing committee were the ones conducting the various studies identifying management options for MINS patients, which may have guided their ultimate recommendation. Regardless, practicing physicians should collectively view the guidelines as acceptable “guardrails” to guide their practice. Selection of the appropriate strategy can then be tailored to the individual patient’s risks and benefits, as well as available management options.
In this era of high-sensitivity troponin testing, we now possess an exquisite opportunity to “see” minute levels of myocardial injury among postoperative patients. Our growing ability to effectively act on this knowledge will enable us to make wise decisions with our patients to optimize their cardiac outcomes during the vulnerable postoperative period.
The ability to detect myocardial injury has never been more advanced. With the availability of high-sensitivity troponin testing, microscopic evidence of myocyte death can now be detected, often within an hour or so of the inciting event. This, in turn, has facilitated quicker and more accurate identification and treatment of affected patients. However, these advances in detection have, in some cases, outstripped our understanding of the etiology and appropriate management of troponin elevation.
This dilemma is particularly apparent among patients undergoing noncardiac surgery. Annually, over 200 million of these surgeries occur worldwide, many in patients with elevated cardiac risk or overt cardiac disease. Naturally, physicians treating these patients are concerned that the stress of surgery will provoke myocardial injury. Since symptoms are often masked in the immediate postoperative period because of sedating or analgesic medications, many physicians rely on troponin testing to detect signs of myocardial injury. With the increased sensitivity of these assays, the prevalence of troponin elevation has increased, which currently affects nearly one in five postoperative patients. This knowledge, however, doesn’t lend itself to a clear management strategy, particularly in those patients with no other objective evidence of infarction. To paraphrase T.S. Eliot, have we lost the wisdom in our knowledge?
In this journal issue, Cohn and colleagues summarize the current information around this phenomenon of myocardial injury after noncardiac surgery, or MINS.1 Consistent with the literature, they define MINS as an acute rise and/or fall in troponin (above the assay’s upper limit of normal) at any point in the 30 days following noncardiac surgery. Importantly, MINS is an umbrella term that can indicate either a myocardial infarction (MI) or nonischemic myocardial injury (NIMI). An MI exists if there are clinical signs of ischemia and/or objective evidence of infarction on imaging.
The authors found that MINS is highly prevalent (19.6%) and associated with both cardiac disease and perioperative hemodynamic stress. Between 2.9% and 13.5% of MINS patients experienced 30-day adverse cardiac events, with higher rates in patients with higher troponin elevations and/or accompanying ischemic symptoms. The authors suggested MINS management with standard cardio-protective medications, such as statins, beta-blockers, and angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers. For those patients at low bleeding risk, they also suggested dabigatran based on the recent MANAGE trial. Finally, they noted that US cardiac society guidelines suggested no screening for MINS, while the European and Canadian guidelines advocated for screening in patients at high risk for cardiac complications.
The authors are to be congratulated for highlighting an important and vexing area of postoperative management. To date, it has been difficult to chart the best path forward for these patients because we could “see” the issue, thanks to increasingly sensitive troponin assays, but we didn’t know what to do once we found it.
So what rationale exists to justify screening? Some advocate that the presence of MINS suggests a need for further imaging and closer monitoring of these patients to identify those with an MI. Indeed, several recent MINS registry studies have found that 20% to 40% of MINS patients had definitive evidence of MI.2-4 But what about those patients with troponin elevation and no evidence of MI? A small, propensity-matched, observational study of MINS patients, including those without MI, noted positive associations between cardioprotective medications, such as aspirin and statins, and cardiac outcomes.5 In addition, the MANAGE trial suggested that MINS patients, with or without evidence of an MI, receiving dabigatran had reduced vascular events without increased bleeding complications.6 With this growing base of evidence, the rationale for systematic screening for MINS appears to be standing on stronger footing.
As noted by the authors, the recommendations for MINS screening differ across three major cardiovascular societies. How does the practicing clinician make sense of this discordant advice? Differences often occur when the evidence is of moderate or low quality, which means guideline committees must make their own interpretations of equivocal findings. Another driver of discordant recommendations is the timing of the guidelines. Both the US and European guidelines were published in 2014, while the Canadian guidelines were published in 2017. Over time, experience with postoperative troponin testing increased, which may have influenced the Canadian guidelines. Finally, many members of the Canadian guideline writing committee were the ones conducting the various studies identifying management options for MINS patients, which may have guided their ultimate recommendation. Regardless, practicing physicians should collectively view the guidelines as acceptable “guardrails” to guide their practice. Selection of the appropriate strategy can then be tailored to the individual patient’s risks and benefits, as well as available management options.
In this era of high-sensitivity troponin testing, we now possess an exquisite opportunity to “see” minute levels of myocardial injury among postoperative patients. Our growing ability to effectively act on this knowledge will enable us to make wise decisions with our patients to optimize their cardiac outcomes during the vulnerable postoperative period.
1. Cohn SL, Rohatgi N, Patel P, Whinney C. Clinical progress note: myocardial injury after noncardiac surgery. J Hosp Med. 2020;15(7):412-415. https://doi.org/10.12788/jhm.3448
2. Puelacher C, Lurati Buse G, Seeberger D, et al. Perioperative myocardial injury after noncardiac surgery: incidence, mortality, and characterization. Circulation. 2018;137(12):1221-1232. https://doi.org/10.1161/circulationaha.117.030114.
3. Botto F, Alonso-Coello P, Chan MTV, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120(3):564-578. https://doi.org/10.1097/aln.0000000000000113
4. Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317(16):1642-1651. https://doi.org/10.1001/jama.2017.4360
5. Foucrier A, Rodseth R, Aissaoui M, et al. The long-term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053-1063. https://doi.org/10.1213/ane.0000000000000302
6. Devereaux PJ, Duceppe E, Guyatt G, et al. Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet. 2018;391(10137):2325-2334. https://doi.org/10.1016/s0140-6736(18)30832-8
1. Cohn SL, Rohatgi N, Patel P, Whinney C. Clinical progress note: myocardial injury after noncardiac surgery. J Hosp Med. 2020;15(7):412-415. https://doi.org/10.12788/jhm.3448
2. Puelacher C, Lurati Buse G, Seeberger D, et al. Perioperative myocardial injury after noncardiac surgery: incidence, mortality, and characterization. Circulation. 2018;137(12):1221-1232. https://doi.org/10.1161/circulationaha.117.030114.
3. Botto F, Alonso-Coello P, Chan MTV, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120(3):564-578. https://doi.org/10.1097/aln.0000000000000113
4. Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317(16):1642-1651. https://doi.org/10.1001/jama.2017.4360
5. Foucrier A, Rodseth R, Aissaoui M, et al. The long-term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053-1063. https://doi.org/10.1213/ane.0000000000000302
6. Devereaux PJ, Duceppe E, Guyatt G, et al. Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet. 2018;391(10137):2325-2334. https://doi.org/10.1016/s0140-6736(18)30832-8
© 2020 Society of Hospital Medicine
Aspiring to Treat Wisely: Challenges in Diagnosing and Optimizing Antibiotic Therapy for Aspiration Pneumonia
In this issue of the Journal of Hospital Medicine, Dr. Thomson and colleagues present an analysis of 4,700 hospitalizations in the Pediatric Health Information System (PHIS) database to compare the effectiveness of different antibiotic regimens for children with neurological impairment and aspiration pneumonia.1 After adjusting for potential confounders, including illness severity markers and demographic factors, they observed that receiving anaerobic coverage was associated with improvements in rates of acute respiratory failure, intensive care unit (ICU) transfer frequency, and length of stay. Given that the authors used an administrative database, several considerations limit the generalizability of the current study. These limitations include that only patients hospitalized at freestanding children’s hospitals were included, the incomplete ability to assess illness severity, and the absence of validated clinical criteria for the diagnosis of aspiration pneumonia. Despite the limitations of a retrospective study using administrative data, the authors should be commended for their rigorous analyses and for their important contribution to the care of this understudied population.
Optimizing appropriate antibiotic therapy for children with suspected aspiration pneumonia is challenging for several reasons. First, previous epidemiological studies demonstrated that viruses cause most pediatric community-acquired pneumonia2; however, we lack tools to identify patients who do not require antibiotic therapy. Second, current clinical guidelines on community-acquired pneumonia do not address aspiration pneumonia diagnosis and management.3 Similar to community-acquired pneumonia, aspiration pneumonia is a clinical diagnosis supported by patient history and laboratory and radiographic data. Given the lack of a gold standard, diagnosis of aspiration pneumonia is difficult to confirm. Previous studies using the PHIS database have demonstrated that, compared with children with nonaspiration pneumonia, those with aspiration pneumonia International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes feature higher rates of mortality, ICU-level care, and 30-day readmission rates.4,5 However, in these studies, patients with an ICD-9-CM code for aspiration pneumonia were also more medically complex, with a higher number of complex chronic conditions and rates of technology use. Lastly, aspiration pneumonia is occasionally synonymous with pneumonia in medically complex patients, which leads to the increased exposure to broad-spectrum antibiotics. The exposure to broad-spectrum antibiotics causes complications, such as Clostridioides difficile infection and potential antibiotic resistance in a patient population that already experiences significant antibiotic exposure.
Growing concerns about antibiotic overuse and the declining prevalence of anaerobic isolates among adult pneumonia patients recently prompted the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) to discourage routine anaerobic coverage among adults with suspected aspiration pneumonia and no abscess or empyema.6 These guidelines overturn years of habit for most adult hospitalists, although the IDSA and ATS acknowledge the extremely low quality of evidence informing the recommendation. Thus, the dilemma is whether the IDSA/ATS guidelines should be reconciled with the conclusions of Thomson et al. The answer is “not necessarily.” Fundamentally, different causes of neurological impairment, such as dementia and stroke, afflict elderly adults with aspiration pneumonia along with important differences in physiological and microbiological exposures. Instead, adult and pediatric hospitalists can find common ground around the shared uncertainty and variability in diagnosing aspiration pneumonia and the need for more credible evidence. Unfortunately, wide variation in diagnosis and coding practices might complicate the efforts to reproduce Thomson’s rigorous retrospective cohort study in large adult databases7 given that Medicare-quality comparison programs may have inadvertently encouraged changes in coding behaviors during the last decade. Attributing pneumonia cases to aspiration removed high-risk patients from reporting cohorts, thus improving a hospital’s apparent mortality rate for community-acquired pneumonia. Although the United States Centers for Medicare & Medicaid Services amended rules in 2017 to address this concern, years of overdiagnosis of aspiration pneumonia possibly biased adult administrative data sets.
Although the association between the use of anaerobic antibiotic coverage and improved pediatric outcomes is promising, these results also point out the need for rigorous prospective studies to improve the evidence base for the diagnosis and treatment of suspected aspiration pneumonia in hospitalized patients of all ages. Given the heterogeneity in the use of aspiration pneumonia diagnoses, foundational work might include assessing the factors that influence clinicians in deciding on the diagnosis of aspiration pneumonia (versus community-acquired pneumonia). On the patient side, parallel trials may start with multicenter, prospective cohort studies to gain insights into the demographic, clinical, and laboratory factors that are associated with the diagnosis of aspiration pneumonia. This research direction may lead to the development and standardization of diagnostic criteria for aspiration pneumonia. Ultimately, prospective randomized controlled trials are needed to assess the comparative effectiveness of different antibiotic choices on clinical outcomes.
1. Thomson J, Hall M, Ambroggio L, et al. Antibiotics for aspiration pneumonia in neurologically impaired children. J Hosp Med. 2020;15(7):395-402. https://doi.org/10.12788/jhm.3338
2. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870
3. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-76. https://doi.org/10.1093/cid/cir531
4. Hirsch AW, Monuteaux MC, Fruchtman G, Bachur RG, Neuman MI. Characteristics of children hospitalized with aspiration pneumonia. Hosp Pediatr. 2016;6(11):659-666. https://doi.org/10.1542/hpeds.2016-0064
5. Thomson J, Hall M, Ambroggio L, et al. Aspiration and non-aspiration pneumonia in hospitalized children with neurologic impairment. Pediatrics. 2016;137(2):1-10. https://doi.org/10.1542/peds.2015-1612
6. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581ST
7. Lindenauer PK, Strait KM, Grady JN, et al. Variation in the diagnosis of aspiration pneumonia and association with hospital pneumonia outcomes. Ann Am Thorac Soc. 2018;15(5):562-569. https://doi.org/10.1513/AnnalsATS.201709-728OC
In this issue of the Journal of Hospital Medicine, Dr. Thomson and colleagues present an analysis of 4,700 hospitalizations in the Pediatric Health Information System (PHIS) database to compare the effectiveness of different antibiotic regimens for children with neurological impairment and aspiration pneumonia.1 After adjusting for potential confounders, including illness severity markers and demographic factors, they observed that receiving anaerobic coverage was associated with improvements in rates of acute respiratory failure, intensive care unit (ICU) transfer frequency, and length of stay. Given that the authors used an administrative database, several considerations limit the generalizability of the current study. These limitations include that only patients hospitalized at freestanding children’s hospitals were included, the incomplete ability to assess illness severity, and the absence of validated clinical criteria for the diagnosis of aspiration pneumonia. Despite the limitations of a retrospective study using administrative data, the authors should be commended for their rigorous analyses and for their important contribution to the care of this understudied population.
Optimizing appropriate antibiotic therapy for children with suspected aspiration pneumonia is challenging for several reasons. First, previous epidemiological studies demonstrated that viruses cause most pediatric community-acquired pneumonia2; however, we lack tools to identify patients who do not require antibiotic therapy. Second, current clinical guidelines on community-acquired pneumonia do not address aspiration pneumonia diagnosis and management.3 Similar to community-acquired pneumonia, aspiration pneumonia is a clinical diagnosis supported by patient history and laboratory and radiographic data. Given the lack of a gold standard, diagnosis of aspiration pneumonia is difficult to confirm. Previous studies using the PHIS database have demonstrated that, compared with children with nonaspiration pneumonia, those with aspiration pneumonia International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes feature higher rates of mortality, ICU-level care, and 30-day readmission rates.4,5 However, in these studies, patients with an ICD-9-CM code for aspiration pneumonia were also more medically complex, with a higher number of complex chronic conditions and rates of technology use. Lastly, aspiration pneumonia is occasionally synonymous with pneumonia in medically complex patients, which leads to the increased exposure to broad-spectrum antibiotics. The exposure to broad-spectrum antibiotics causes complications, such as Clostridioides difficile infection and potential antibiotic resistance in a patient population that already experiences significant antibiotic exposure.
Growing concerns about antibiotic overuse and the declining prevalence of anaerobic isolates among adult pneumonia patients recently prompted the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) to discourage routine anaerobic coverage among adults with suspected aspiration pneumonia and no abscess or empyema.6 These guidelines overturn years of habit for most adult hospitalists, although the IDSA and ATS acknowledge the extremely low quality of evidence informing the recommendation. Thus, the dilemma is whether the IDSA/ATS guidelines should be reconciled with the conclusions of Thomson et al. The answer is “not necessarily.” Fundamentally, different causes of neurological impairment, such as dementia and stroke, afflict elderly adults with aspiration pneumonia along with important differences in physiological and microbiological exposures. Instead, adult and pediatric hospitalists can find common ground around the shared uncertainty and variability in diagnosing aspiration pneumonia and the need for more credible evidence. Unfortunately, wide variation in diagnosis and coding practices might complicate the efforts to reproduce Thomson’s rigorous retrospective cohort study in large adult databases7 given that Medicare-quality comparison programs may have inadvertently encouraged changes in coding behaviors during the last decade. Attributing pneumonia cases to aspiration removed high-risk patients from reporting cohorts, thus improving a hospital’s apparent mortality rate for community-acquired pneumonia. Although the United States Centers for Medicare & Medicaid Services amended rules in 2017 to address this concern, years of overdiagnosis of aspiration pneumonia possibly biased adult administrative data sets.
Although the association between the use of anaerobic antibiotic coverage and improved pediatric outcomes is promising, these results also point out the need for rigorous prospective studies to improve the evidence base for the diagnosis and treatment of suspected aspiration pneumonia in hospitalized patients of all ages. Given the heterogeneity in the use of aspiration pneumonia diagnoses, foundational work might include assessing the factors that influence clinicians in deciding on the diagnosis of aspiration pneumonia (versus community-acquired pneumonia). On the patient side, parallel trials may start with multicenter, prospective cohort studies to gain insights into the demographic, clinical, and laboratory factors that are associated with the diagnosis of aspiration pneumonia. This research direction may lead to the development and standardization of diagnostic criteria for aspiration pneumonia. Ultimately, prospective randomized controlled trials are needed to assess the comparative effectiveness of different antibiotic choices on clinical outcomes.
In this issue of the Journal of Hospital Medicine, Dr. Thomson and colleagues present an analysis of 4,700 hospitalizations in the Pediatric Health Information System (PHIS) database to compare the effectiveness of different antibiotic regimens for children with neurological impairment and aspiration pneumonia.1 After adjusting for potential confounders, including illness severity markers and demographic factors, they observed that receiving anaerobic coverage was associated with improvements in rates of acute respiratory failure, intensive care unit (ICU) transfer frequency, and length of stay. Given that the authors used an administrative database, several considerations limit the generalizability of the current study. These limitations include that only patients hospitalized at freestanding children’s hospitals were included, the incomplete ability to assess illness severity, and the absence of validated clinical criteria for the diagnosis of aspiration pneumonia. Despite the limitations of a retrospective study using administrative data, the authors should be commended for their rigorous analyses and for their important contribution to the care of this understudied population.
Optimizing appropriate antibiotic therapy for children with suspected aspiration pneumonia is challenging for several reasons. First, previous epidemiological studies demonstrated that viruses cause most pediatric community-acquired pneumonia2; however, we lack tools to identify patients who do not require antibiotic therapy. Second, current clinical guidelines on community-acquired pneumonia do not address aspiration pneumonia diagnosis and management.3 Similar to community-acquired pneumonia, aspiration pneumonia is a clinical diagnosis supported by patient history and laboratory and radiographic data. Given the lack of a gold standard, diagnosis of aspiration pneumonia is difficult to confirm. Previous studies using the PHIS database have demonstrated that, compared with children with nonaspiration pneumonia, those with aspiration pneumonia International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes feature higher rates of mortality, ICU-level care, and 30-day readmission rates.4,5 However, in these studies, patients with an ICD-9-CM code for aspiration pneumonia were also more medically complex, with a higher number of complex chronic conditions and rates of technology use. Lastly, aspiration pneumonia is occasionally synonymous with pneumonia in medically complex patients, which leads to the increased exposure to broad-spectrum antibiotics. The exposure to broad-spectrum antibiotics causes complications, such as Clostridioides difficile infection and potential antibiotic resistance in a patient population that already experiences significant antibiotic exposure.
Growing concerns about antibiotic overuse and the declining prevalence of anaerobic isolates among adult pneumonia patients recently prompted the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) to discourage routine anaerobic coverage among adults with suspected aspiration pneumonia and no abscess or empyema.6 These guidelines overturn years of habit for most adult hospitalists, although the IDSA and ATS acknowledge the extremely low quality of evidence informing the recommendation. Thus, the dilemma is whether the IDSA/ATS guidelines should be reconciled with the conclusions of Thomson et al. The answer is “not necessarily.” Fundamentally, different causes of neurological impairment, such as dementia and stroke, afflict elderly adults with aspiration pneumonia along with important differences in physiological and microbiological exposures. Instead, adult and pediatric hospitalists can find common ground around the shared uncertainty and variability in diagnosing aspiration pneumonia and the need for more credible evidence. Unfortunately, wide variation in diagnosis and coding practices might complicate the efforts to reproduce Thomson’s rigorous retrospective cohort study in large adult databases7 given that Medicare-quality comparison programs may have inadvertently encouraged changes in coding behaviors during the last decade. Attributing pneumonia cases to aspiration removed high-risk patients from reporting cohorts, thus improving a hospital’s apparent mortality rate for community-acquired pneumonia. Although the United States Centers for Medicare & Medicaid Services amended rules in 2017 to address this concern, years of overdiagnosis of aspiration pneumonia possibly biased adult administrative data sets.
Although the association between the use of anaerobic antibiotic coverage and improved pediatric outcomes is promising, these results also point out the need for rigorous prospective studies to improve the evidence base for the diagnosis and treatment of suspected aspiration pneumonia in hospitalized patients of all ages. Given the heterogeneity in the use of aspiration pneumonia diagnoses, foundational work might include assessing the factors that influence clinicians in deciding on the diagnosis of aspiration pneumonia (versus community-acquired pneumonia). On the patient side, parallel trials may start with multicenter, prospective cohort studies to gain insights into the demographic, clinical, and laboratory factors that are associated with the diagnosis of aspiration pneumonia. This research direction may lead to the development and standardization of diagnostic criteria for aspiration pneumonia. Ultimately, prospective randomized controlled trials are needed to assess the comparative effectiveness of different antibiotic choices on clinical outcomes.
1. Thomson J, Hall M, Ambroggio L, et al. Antibiotics for aspiration pneumonia in neurologically impaired children. J Hosp Med. 2020;15(7):395-402. https://doi.org/10.12788/jhm.3338
2. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870
3. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-76. https://doi.org/10.1093/cid/cir531
4. Hirsch AW, Monuteaux MC, Fruchtman G, Bachur RG, Neuman MI. Characteristics of children hospitalized with aspiration pneumonia. Hosp Pediatr. 2016;6(11):659-666. https://doi.org/10.1542/hpeds.2016-0064
5. Thomson J, Hall M, Ambroggio L, et al. Aspiration and non-aspiration pneumonia in hospitalized children with neurologic impairment. Pediatrics. 2016;137(2):1-10. https://doi.org/10.1542/peds.2015-1612
6. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581ST
7. Lindenauer PK, Strait KM, Grady JN, et al. Variation in the diagnosis of aspiration pneumonia and association with hospital pneumonia outcomes. Ann Am Thorac Soc. 2018;15(5):562-569. https://doi.org/10.1513/AnnalsATS.201709-728OC
1. Thomson J, Hall M, Ambroggio L, et al. Antibiotics for aspiration pneumonia in neurologically impaired children. J Hosp Med. 2020;15(7):395-402. https://doi.org/10.12788/jhm.3338
2. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870
3. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-76. https://doi.org/10.1093/cid/cir531
4. Hirsch AW, Monuteaux MC, Fruchtman G, Bachur RG, Neuman MI. Characteristics of children hospitalized with aspiration pneumonia. Hosp Pediatr. 2016;6(11):659-666. https://doi.org/10.1542/hpeds.2016-0064
5. Thomson J, Hall M, Ambroggio L, et al. Aspiration and non-aspiration pneumonia in hospitalized children with neurologic impairment. Pediatrics. 2016;137(2):1-10. https://doi.org/10.1542/peds.2015-1612
6. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581ST
7. Lindenauer PK, Strait KM, Grady JN, et al. Variation in the diagnosis of aspiration pneumonia and association with hospital pneumonia outcomes. Ann Am Thorac Soc. 2018;15(5):562-569. https://doi.org/10.1513/AnnalsATS.201709-728OC
© 2020 Society of Hospital Medicine
Defining Competence in the Evolving Field of Pediatric Hospital Medicine
Core competencies are intended to provide defined expectations in a field of medicine. The newly published Pediatric Hospital Medicine (PHM) Core Competencies: 2020 Revision are an update of the original 2010 competencies1 with added and restructured content based on relevance to current practice.2,3 This is timely given the 2017 update to the Society of Hospital Medicine (SHM) core competencies4 and recent designation of PHM as a boarded subspecialty by the American Board of Pediatrics (ABP). The competencies help define the knowledge, skills, and attitudes of a pediatric hospital medicine specialist and inform curriculum development to achieve the determined expectations.
In this update to the PHM core competencies, key adjustments were made to the editorial process. Importantly, a community hospitalist was added to the editorial team; this change better reflects the proportion of care provided to hospitalized children at community sites nationwide.5 Content updates were considered using a two-pronged needs assessment: (1) review of recent PHM conference, textbook, and handbook content and (2) survey of the SHM, Academic Pediatric Association, and American Academy of Pediatrics stakeholder groups. These processes led to the addition of 12 chapters, the major revision of 7 chapters, and the addition of content to 29 of the original chapters.
The increased focus on mental health in the sections “Common Clinical Diagnoses and Conditions” and “Specialized Services” is a necessary update. Chapters on neonatal abstinence syndrome (NAS), substance abuse, and altered mental status were added to the “Common Clinical Diagnoses and Conditions” section. The increasing incidence of NAS has been well described, and the field of PHM has been instrumental in improving care for these patients.6 Children hospitalized with mental health diagnoses constitute a substantial portion of pediatric inpatient admissions,7 and we anticipate that it will be a continued area of need in PHM. Therefore, the addition of chapters on acute and chronic behavioral and psychiatric conditions in the “Specialized Services” section is noteworthy. In contrast, with the added chapters on constipation and gastrointestinal and digestive disorders, the gastrointestinal disorders may be disproportionately represented in the updated competencies and may be an area to streamline in future iterations.
Recognition of changing procedural needs in the inpatient pediatric setting, particularly with the growing population of children with medical complexity, resulted in removal of suprapubic bladder taps and addition of vesicostomy care to the “Core Skills” section. In future updates, it will be important to continue to remove practices that are no longer relevant or widespread and include advances in procedural skills applicable to PHM such as point-of-care ultrasound.8
The “Healthcare Systems” section highlights additional skills ranging from quality improvement and research to family-centered care that PHM physicians bring to healthcare institutions. According to a recent survey of early-career hospitalists, skills in these areas are often not adequately developed during residency training.9 Therefore, the competencies outlined in this section are a key part of proposed PHM fellowship curricula10 and should be recognized as potential development opportunities for junior faculty in the field. This section also highlights the increasing medical complexity of patients and evolving role of PHM expertise in comanagement and consultation to improve quality and safety of care. Appreciating the unique needs of underserved communities is another important addition in the new chapter on family-centered care.
Looking ahead to future updates, we appreciate that the editors commented on diversity in both editorship and authorship. In line with the recent call for improved representation of women and racial and ethnic minorities in academic medicine by the Journal of Hospital Medicine,11 future core competency publications should broadly consider diversity in editors, authors, and reviewers and more explicitly address methods for increasing diversity. We also anticipate that technological advances, such as telemedicine and remote patient monitoring, will be at the forefront in subsequent updates, which will allow higher levels of care to be provided outside of the traditional hospital structure. With the recent inauguration of the ABP PHM certification exam and the first cycle of Accreditation Council for Graduate Medical Education accreditation for PHM fellowships, these updated competencies are timely and relevant. The authors’ ongoing efforts are crucial for our young and evolving field as we strive to improve the health of all hospitalized children.
Disclosures
The authors have nothing to disclose.
1. Stucky ER, Ottolini MC, Maniscalco J. Pediatric Hospital Medicine Core Competencies: development and methodology. J Hosp Med. 2010;5(6):339-343. https://doi.org/10.1002/jhm.843
2. Gage S, Maniscalco J, Fisher E, Teferi S, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision; a framework for curriculum development by the Society of Hospital Medicine with acknowledgment to pediatric hospitalists from the Academic Pediatric Association and the American Academy of Pediatrics. J Hosp Med. 2020;15(S1):1-155
3. Maniscalco J, Gage S, Teferi S, Stucky Fisher E. The Pediatric Hospital Medicine Core Competencies 2020 Revision: introduction and methodology. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
4. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the Core Competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
5. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States: pediatric hospitalization epidemiology. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624
6. Holmes AV, Atwood EC, Whalen B, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics. 2016;137(6):e20152929. https://doi.org/10.1542/peds.2015-2929
7. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. https://doi.org/10.1542/peds.2013-3165
8. Conlon TW, Nishisaki A, Singh Y, et al. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144(4):e20191402. https://doi.org/10.1542/peds.2019-1402
9. Librizzi J, Winer JC, Banach L, Davis A. Perceived core competency achievements of fellowship and non-fellowship-trained early career pediatric hospitalists: early career pediatric hospitalists. J Hosp Med. 2015;10(6):373-379. https://doi.org/10.1002/jhm.2337
10. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for Pediatric Hospital Medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
11. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247
Core competencies are intended to provide defined expectations in a field of medicine. The newly published Pediatric Hospital Medicine (PHM) Core Competencies: 2020 Revision are an update of the original 2010 competencies1 with added and restructured content based on relevance to current practice.2,3 This is timely given the 2017 update to the Society of Hospital Medicine (SHM) core competencies4 and recent designation of PHM as a boarded subspecialty by the American Board of Pediatrics (ABP). The competencies help define the knowledge, skills, and attitudes of a pediatric hospital medicine specialist and inform curriculum development to achieve the determined expectations.
In this update to the PHM core competencies, key adjustments were made to the editorial process. Importantly, a community hospitalist was added to the editorial team; this change better reflects the proportion of care provided to hospitalized children at community sites nationwide.5 Content updates were considered using a two-pronged needs assessment: (1) review of recent PHM conference, textbook, and handbook content and (2) survey of the SHM, Academic Pediatric Association, and American Academy of Pediatrics stakeholder groups. These processes led to the addition of 12 chapters, the major revision of 7 chapters, and the addition of content to 29 of the original chapters.
The increased focus on mental health in the sections “Common Clinical Diagnoses and Conditions” and “Specialized Services” is a necessary update. Chapters on neonatal abstinence syndrome (NAS), substance abuse, and altered mental status were added to the “Common Clinical Diagnoses and Conditions” section. The increasing incidence of NAS has been well described, and the field of PHM has been instrumental in improving care for these patients.6 Children hospitalized with mental health diagnoses constitute a substantial portion of pediatric inpatient admissions,7 and we anticipate that it will be a continued area of need in PHM. Therefore, the addition of chapters on acute and chronic behavioral and psychiatric conditions in the “Specialized Services” section is noteworthy. In contrast, with the added chapters on constipation and gastrointestinal and digestive disorders, the gastrointestinal disorders may be disproportionately represented in the updated competencies and may be an area to streamline in future iterations.
Recognition of changing procedural needs in the inpatient pediatric setting, particularly with the growing population of children with medical complexity, resulted in removal of suprapubic bladder taps and addition of vesicostomy care to the “Core Skills” section. In future updates, it will be important to continue to remove practices that are no longer relevant or widespread and include advances in procedural skills applicable to PHM such as point-of-care ultrasound.8
The “Healthcare Systems” section highlights additional skills ranging from quality improvement and research to family-centered care that PHM physicians bring to healthcare institutions. According to a recent survey of early-career hospitalists, skills in these areas are often not adequately developed during residency training.9 Therefore, the competencies outlined in this section are a key part of proposed PHM fellowship curricula10 and should be recognized as potential development opportunities for junior faculty in the field. This section also highlights the increasing medical complexity of patients and evolving role of PHM expertise in comanagement and consultation to improve quality and safety of care. Appreciating the unique needs of underserved communities is another important addition in the new chapter on family-centered care.
Looking ahead to future updates, we appreciate that the editors commented on diversity in both editorship and authorship. In line with the recent call for improved representation of women and racial and ethnic minorities in academic medicine by the Journal of Hospital Medicine,11 future core competency publications should broadly consider diversity in editors, authors, and reviewers and more explicitly address methods for increasing diversity. We also anticipate that technological advances, such as telemedicine and remote patient monitoring, will be at the forefront in subsequent updates, which will allow higher levels of care to be provided outside of the traditional hospital structure. With the recent inauguration of the ABP PHM certification exam and the first cycle of Accreditation Council for Graduate Medical Education accreditation for PHM fellowships, these updated competencies are timely and relevant. The authors’ ongoing efforts are crucial for our young and evolving field as we strive to improve the health of all hospitalized children.
Disclosures
The authors have nothing to disclose.
Core competencies are intended to provide defined expectations in a field of medicine. The newly published Pediatric Hospital Medicine (PHM) Core Competencies: 2020 Revision are an update of the original 2010 competencies1 with added and restructured content based on relevance to current practice.2,3 This is timely given the 2017 update to the Society of Hospital Medicine (SHM) core competencies4 and recent designation of PHM as a boarded subspecialty by the American Board of Pediatrics (ABP). The competencies help define the knowledge, skills, and attitudes of a pediatric hospital medicine specialist and inform curriculum development to achieve the determined expectations.
In this update to the PHM core competencies, key adjustments were made to the editorial process. Importantly, a community hospitalist was added to the editorial team; this change better reflects the proportion of care provided to hospitalized children at community sites nationwide.5 Content updates were considered using a two-pronged needs assessment: (1) review of recent PHM conference, textbook, and handbook content and (2) survey of the SHM, Academic Pediatric Association, and American Academy of Pediatrics stakeholder groups. These processes led to the addition of 12 chapters, the major revision of 7 chapters, and the addition of content to 29 of the original chapters.
The increased focus on mental health in the sections “Common Clinical Diagnoses and Conditions” and “Specialized Services” is a necessary update. Chapters on neonatal abstinence syndrome (NAS), substance abuse, and altered mental status were added to the “Common Clinical Diagnoses and Conditions” section. The increasing incidence of NAS has been well described, and the field of PHM has been instrumental in improving care for these patients.6 Children hospitalized with mental health diagnoses constitute a substantial portion of pediatric inpatient admissions,7 and we anticipate that it will be a continued area of need in PHM. Therefore, the addition of chapters on acute and chronic behavioral and psychiatric conditions in the “Specialized Services” section is noteworthy. In contrast, with the added chapters on constipation and gastrointestinal and digestive disorders, the gastrointestinal disorders may be disproportionately represented in the updated competencies and may be an area to streamline in future iterations.
Recognition of changing procedural needs in the inpatient pediatric setting, particularly with the growing population of children with medical complexity, resulted in removal of suprapubic bladder taps and addition of vesicostomy care to the “Core Skills” section. In future updates, it will be important to continue to remove practices that are no longer relevant or widespread and include advances in procedural skills applicable to PHM such as point-of-care ultrasound.8
The “Healthcare Systems” section highlights additional skills ranging from quality improvement and research to family-centered care that PHM physicians bring to healthcare institutions. According to a recent survey of early-career hospitalists, skills in these areas are often not adequately developed during residency training.9 Therefore, the competencies outlined in this section are a key part of proposed PHM fellowship curricula10 and should be recognized as potential development opportunities for junior faculty in the field. This section also highlights the increasing medical complexity of patients and evolving role of PHM expertise in comanagement and consultation to improve quality and safety of care. Appreciating the unique needs of underserved communities is another important addition in the new chapter on family-centered care.
Looking ahead to future updates, we appreciate that the editors commented on diversity in both editorship and authorship. In line with the recent call for improved representation of women and racial and ethnic minorities in academic medicine by the Journal of Hospital Medicine,11 future core competency publications should broadly consider diversity in editors, authors, and reviewers and more explicitly address methods for increasing diversity. We also anticipate that technological advances, such as telemedicine and remote patient monitoring, will be at the forefront in subsequent updates, which will allow higher levels of care to be provided outside of the traditional hospital structure. With the recent inauguration of the ABP PHM certification exam and the first cycle of Accreditation Council for Graduate Medical Education accreditation for PHM fellowships, these updated competencies are timely and relevant. The authors’ ongoing efforts are crucial for our young and evolving field as we strive to improve the health of all hospitalized children.
Disclosures
The authors have nothing to disclose.
1. Stucky ER, Ottolini MC, Maniscalco J. Pediatric Hospital Medicine Core Competencies: development and methodology. J Hosp Med. 2010;5(6):339-343. https://doi.org/10.1002/jhm.843
2. Gage S, Maniscalco J, Fisher E, Teferi S, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision; a framework for curriculum development by the Society of Hospital Medicine with acknowledgment to pediatric hospitalists from the Academic Pediatric Association and the American Academy of Pediatrics. J Hosp Med. 2020;15(S1):1-155
3. Maniscalco J, Gage S, Teferi S, Stucky Fisher E. The Pediatric Hospital Medicine Core Competencies 2020 Revision: introduction and methodology. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
4. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the Core Competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
5. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States: pediatric hospitalization epidemiology. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624
6. Holmes AV, Atwood EC, Whalen B, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics. 2016;137(6):e20152929. https://doi.org/10.1542/peds.2015-2929
7. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. https://doi.org/10.1542/peds.2013-3165
8. Conlon TW, Nishisaki A, Singh Y, et al. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144(4):e20191402. https://doi.org/10.1542/peds.2019-1402
9. Librizzi J, Winer JC, Banach L, Davis A. Perceived core competency achievements of fellowship and non-fellowship-trained early career pediatric hospitalists: early career pediatric hospitalists. J Hosp Med. 2015;10(6):373-379. https://doi.org/10.1002/jhm.2337
10. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for Pediatric Hospital Medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
11. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247
1. Stucky ER, Ottolini MC, Maniscalco J. Pediatric Hospital Medicine Core Competencies: development and methodology. J Hosp Med. 2010;5(6):339-343. https://doi.org/10.1002/jhm.843
2. Gage S, Maniscalco J, Fisher E, Teferi S, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision; a framework for curriculum development by the Society of Hospital Medicine with acknowledgment to pediatric hospitalists from the Academic Pediatric Association and the American Academy of Pediatrics. J Hosp Med. 2020;15(S1):1-155
3. Maniscalco J, Gage S, Teferi S, Stucky Fisher E. The Pediatric Hospital Medicine Core Competencies 2020 Revision: introduction and methodology. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
4. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the Core Competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
5. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States: pediatric hospitalization epidemiology. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624
6. Holmes AV, Atwood EC, Whalen B, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics. 2016;137(6):e20152929. https://doi.org/10.1542/peds.2015-2929
7. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. https://doi.org/10.1542/peds.2013-3165
8. Conlon TW, Nishisaki A, Singh Y, et al. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144(4):e20191402. https://doi.org/10.1542/peds.2019-1402
9. Librizzi J, Winer JC, Banach L, Davis A. Perceived core competency achievements of fellowship and non-fellowship-trained early career pediatric hospitalists: early career pediatric hospitalists. J Hosp Med. 2015;10(6):373-379. https://doi.org/10.1002/jhm.2337
10. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for Pediatric Hospital Medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
11. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247
© 2020 Society of Hospital Medicine
Report describes intoxication with new psychoactive substance
When evaluated at local emergency departments, lethargy and slurred speech were the most common clinical findings.
One student had mild respiratory depression with a respiratory rate of 10 breaths per minute.
“All patients had sufficient clinical improvement within 6 hours such that they could be discharged from the hospital,” according to a description of the cases that was published online in Pediatrics.
The report is the first to detail clinical toxicity from flualprazolam, and “it is likely that physicians will again encounter patients” with intoxication from this new psychoactive drug, said Adam Blumenberg, MD, of Oregon Health & Science University in Portland and colleagues.
Internet purchasing has increased rates of exposure to new psychoactive substances since the early 2000s, and law enforcement agents have seized tons of these drugs. “In the United States, the incidence of exposures to designer benzodiazepines in particular has been rising since 2014,” the authors said.
According to an addiction researcher, the COVID-19 pandemic may exacerbate abuse of designer benzodiazepines.
“This is an important paper describing what medical examiners, pathologists, and emergency rooms have been seeing recently – an increase in designer benzodiazepines,” commented Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis. “Recent increases in these drugs have started to be seen in many locations as the traditional drugs of abuse, grown and distributed in bulk, have been disrupted” by the pandemic, he said in an interview. Although it may be too early for such cases to appear in Centers for Disease Control and Prevention reports, they can be described in studies like this one and, “I suspect, sadly, in medical examiner case reports.”
Flualprazolam, known colloquially as Hulk, is structurally related to the Food and Drug Administration–approved drugs alprazolam and triazolam. During 1 week in June 2019, the patients in Oregon received the drug as a free sample from another student from their Oregon high school. They believed it was commercial Xanax (alprazolam). “The flualprazolam tablets were identical in appearance and labeling to 2-mg tablets of alprazolam,” according to the report. “This indicates an intentionally counterfeit product entering the drug supply chain.”
Five of the six patients were boys, and they ranged in age from 14 to 16 years. The patient with mild respiratory depression received 0.4-mg naloxone, which physicians gave empirically because of the unknown identity of the drug, but did not respond. Two of the six patients initially felt drowsy but were asymptomatic during the clinical evaluation.
A urine immunoassay was performed in five of the patients, and all tested positive for benzodiazepines. One patient also tested positive for cannabinoids. Analysis of a tablet fragment revealed that it contained flualprazolam.
“Although flualprazolam intoxication cannot be clinically differentiated from that of other benzodiazepines without advanced testing, patient management should be the same,” Dr. Blumenberg and coauthors said. “For mild to moderate intoxication, patients should be treated with close monitoring and supportive care until symptom resolution. The benzodiazepine antidote flumazenil may be considered a safe and effective antidote in pediatric patients with significant CNS or respiratory depression. In patients for whom there is a concern of benzodiazepine dependence and flumazenil-induced seizures, airway protection and mechanical ventilation may be considered.”
Although patients rarely die from isolated benzodiazepine toxicity, death from respiratory depression or aspiration is more common when benzodiazepine toxicity occurs “in combination with alcohol, opioids, or other sedatives,” the authors noted. In addition, counterfeit alprazolam tablets have contained adulterants such as fentanyl and the opioid U-47700, which can be deadly.
The authors had no relevant financial disclosures, and there was no external funding for the study.
SOURCE: Blumenberg A et al. Pediatrics. 2020 Jun 24. doi: 10.1542/peds.2019-2953.
When evaluated at local emergency departments, lethargy and slurred speech were the most common clinical findings.
One student had mild respiratory depression with a respiratory rate of 10 breaths per minute.
“All patients had sufficient clinical improvement within 6 hours such that they could be discharged from the hospital,” according to a description of the cases that was published online in Pediatrics.
The report is the first to detail clinical toxicity from flualprazolam, and “it is likely that physicians will again encounter patients” with intoxication from this new psychoactive drug, said Adam Blumenberg, MD, of Oregon Health & Science University in Portland and colleagues.
Internet purchasing has increased rates of exposure to new psychoactive substances since the early 2000s, and law enforcement agents have seized tons of these drugs. “In the United States, the incidence of exposures to designer benzodiazepines in particular has been rising since 2014,” the authors said.
According to an addiction researcher, the COVID-19 pandemic may exacerbate abuse of designer benzodiazepines.
“This is an important paper describing what medical examiners, pathologists, and emergency rooms have been seeing recently – an increase in designer benzodiazepines,” commented Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis. “Recent increases in these drugs have started to be seen in many locations as the traditional drugs of abuse, grown and distributed in bulk, have been disrupted” by the pandemic, he said in an interview. Although it may be too early for such cases to appear in Centers for Disease Control and Prevention reports, they can be described in studies like this one and, “I suspect, sadly, in medical examiner case reports.”
Flualprazolam, known colloquially as Hulk, is structurally related to the Food and Drug Administration–approved drugs alprazolam and triazolam. During 1 week in June 2019, the patients in Oregon received the drug as a free sample from another student from their Oregon high school. They believed it was commercial Xanax (alprazolam). “The flualprazolam tablets were identical in appearance and labeling to 2-mg tablets of alprazolam,” according to the report. “This indicates an intentionally counterfeit product entering the drug supply chain.”
Five of the six patients were boys, and they ranged in age from 14 to 16 years. The patient with mild respiratory depression received 0.4-mg naloxone, which physicians gave empirically because of the unknown identity of the drug, but did not respond. Two of the six patients initially felt drowsy but were asymptomatic during the clinical evaluation.
A urine immunoassay was performed in five of the patients, and all tested positive for benzodiazepines. One patient also tested positive for cannabinoids. Analysis of a tablet fragment revealed that it contained flualprazolam.
“Although flualprazolam intoxication cannot be clinically differentiated from that of other benzodiazepines without advanced testing, patient management should be the same,” Dr. Blumenberg and coauthors said. “For mild to moderate intoxication, patients should be treated with close monitoring and supportive care until symptom resolution. The benzodiazepine antidote flumazenil may be considered a safe and effective antidote in pediatric patients with significant CNS or respiratory depression. In patients for whom there is a concern of benzodiazepine dependence and flumazenil-induced seizures, airway protection and mechanical ventilation may be considered.”
Although patients rarely die from isolated benzodiazepine toxicity, death from respiratory depression or aspiration is more common when benzodiazepine toxicity occurs “in combination with alcohol, opioids, or other sedatives,” the authors noted. In addition, counterfeit alprazolam tablets have contained adulterants such as fentanyl and the opioid U-47700, which can be deadly.
The authors had no relevant financial disclosures, and there was no external funding for the study.
SOURCE: Blumenberg A et al. Pediatrics. 2020 Jun 24. doi: 10.1542/peds.2019-2953.
When evaluated at local emergency departments, lethargy and slurred speech were the most common clinical findings.
One student had mild respiratory depression with a respiratory rate of 10 breaths per minute.
“All patients had sufficient clinical improvement within 6 hours such that they could be discharged from the hospital,” according to a description of the cases that was published online in Pediatrics.
The report is the first to detail clinical toxicity from flualprazolam, and “it is likely that physicians will again encounter patients” with intoxication from this new psychoactive drug, said Adam Blumenberg, MD, of Oregon Health & Science University in Portland and colleagues.
Internet purchasing has increased rates of exposure to new psychoactive substances since the early 2000s, and law enforcement agents have seized tons of these drugs. “In the United States, the incidence of exposures to designer benzodiazepines in particular has been rising since 2014,” the authors said.
According to an addiction researcher, the COVID-19 pandemic may exacerbate abuse of designer benzodiazepines.
“This is an important paper describing what medical examiners, pathologists, and emergency rooms have been seeing recently – an increase in designer benzodiazepines,” commented Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis. “Recent increases in these drugs have started to be seen in many locations as the traditional drugs of abuse, grown and distributed in bulk, have been disrupted” by the pandemic, he said in an interview. Although it may be too early for such cases to appear in Centers for Disease Control and Prevention reports, they can be described in studies like this one and, “I suspect, sadly, in medical examiner case reports.”
Flualprazolam, known colloquially as Hulk, is structurally related to the Food and Drug Administration–approved drugs alprazolam and triazolam. During 1 week in June 2019, the patients in Oregon received the drug as a free sample from another student from their Oregon high school. They believed it was commercial Xanax (alprazolam). “The flualprazolam tablets were identical in appearance and labeling to 2-mg tablets of alprazolam,” according to the report. “This indicates an intentionally counterfeit product entering the drug supply chain.”
Five of the six patients were boys, and they ranged in age from 14 to 16 years. The patient with mild respiratory depression received 0.4-mg naloxone, which physicians gave empirically because of the unknown identity of the drug, but did not respond. Two of the six patients initially felt drowsy but were asymptomatic during the clinical evaluation.
A urine immunoassay was performed in five of the patients, and all tested positive for benzodiazepines. One patient also tested positive for cannabinoids. Analysis of a tablet fragment revealed that it contained flualprazolam.
“Although flualprazolam intoxication cannot be clinically differentiated from that of other benzodiazepines without advanced testing, patient management should be the same,” Dr. Blumenberg and coauthors said. “For mild to moderate intoxication, patients should be treated with close monitoring and supportive care until symptom resolution. The benzodiazepine antidote flumazenil may be considered a safe and effective antidote in pediatric patients with significant CNS or respiratory depression. In patients for whom there is a concern of benzodiazepine dependence and flumazenil-induced seizures, airway protection and mechanical ventilation may be considered.”
Although patients rarely die from isolated benzodiazepine toxicity, death from respiratory depression or aspiration is more common when benzodiazepine toxicity occurs “in combination with alcohol, opioids, or other sedatives,” the authors noted. In addition, counterfeit alprazolam tablets have contained adulterants such as fentanyl and the opioid U-47700, which can be deadly.
The authors had no relevant financial disclosures, and there was no external funding for the study.
SOURCE: Blumenberg A et al. Pediatrics. 2020 Jun 24. doi: 10.1542/peds.2019-2953.
FROM PEDIATRICS
Black women at highest risk for asthma
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
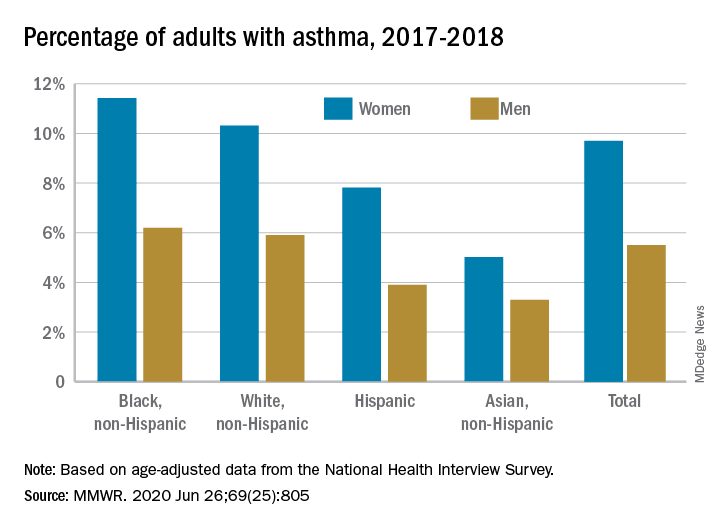
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
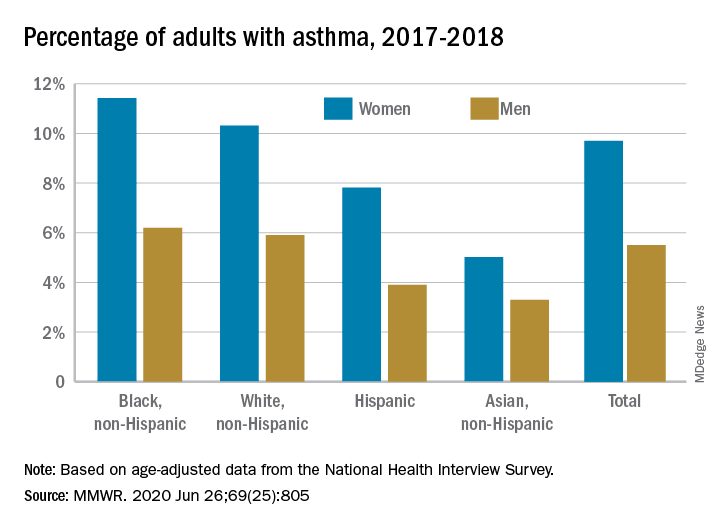
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
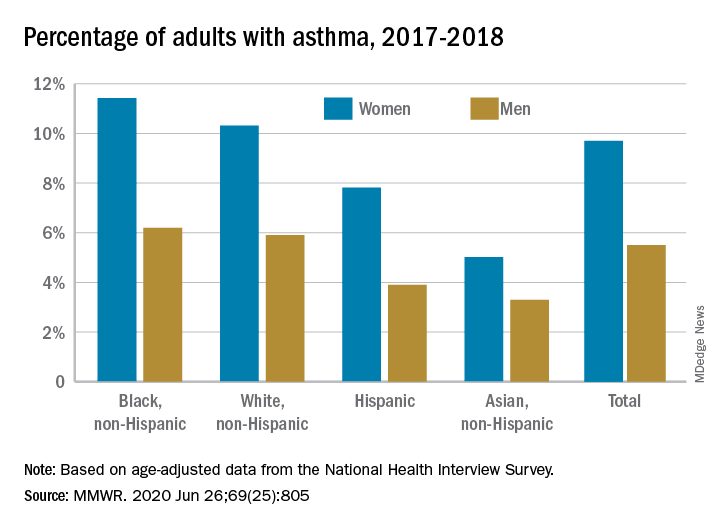
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
FROM MMWR
Encourage parents to follow pediatric plans for vaccination
Outpatient medical care has been severely disrupted during the COVID-19 pandemic with a reduction of nearly 70% in outpatient visits since March before starting to rebound, Melinda Wharton, MD, said at the virtual meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Pediatrics was among the hardest hit specialties, with a 62% reduction in outpatient visits by April 5, said Dr. Wharton, director of the immunization services division at the CDC’s National Center for Immunization and Respiratory Diseases. However, visits for all pediatric age groups increased in May, compared with April, and the CDC emphasized the need to educate families about the importance of routine vaccination and well-child visits, Dr. Wharton said.
The CDC strategies to support routine childhood vaccination include monitoring vaccination service delivery to inform targeted interventions, said Dr. Wharton. In addition, the CDC will continue to support providers by identifying gaps in the Vaccines For Children (VFC) program network, increasing VFC funding, developing guidance materials, and identifying policy interventions.
Many small practices have struggled during the pandemic, and financial support is available through the Provider Relief Fund, which is now available to all Medicaid and Children’s Health Insurance Program (CHIP) providers, said Dr. Wharton.
because more families may now qualify for the program because of changes in job status and income, and parents may not be aware that their children may be eligible, she said.
“Vaccination is an essential medical service for all children and adolescents, ideally in the medical home,” Dr. Wharton said. The CDC’s interim guidance for immunization during the COVID-19 pandemic calls for administering all current or overdue vaccines according to the routine immunization schedule during the same visit, and implementing strategies to get patients caught up, prioritizing newborns, infants, and children up to age 24 months. The guidance includes details on safe delivery of vaccines, including physical distance and the use of personal protective equipment.
In addition, encourage parents to return for well-child visits, and use reminder systems to help keep patients current on visits and vaccines. “Discuss the safety protocols that have been put in place,” Dr. Wharton emphasized. The CDC also offers resources for providers to help communicate with parents about routine vaccination.
Looking ahead, back-to-school vaccination requirements “provide a critical checkpoint for children’s vaccination status,” Dr. Wharton said. Catch-up vaccination during the summer will help clinical capacity manage back-to-school and influenza vaccination in the fall, she emphasized. “Influenza vaccination will be an important strategy to decrease stress on our health care system.”
Flu vaccination strategies should focus on adults at higher risk for COVID-19 infections, such as health care providers. In addition, identifying and reducing disparities will be important for future COVID-19 vaccines, as well as for the flu this season, she noted.
View the complete guidance online.
Dr. Wharton had no relevant financial disclosures.
Outpatient medical care has been severely disrupted during the COVID-19 pandemic with a reduction of nearly 70% in outpatient visits since March before starting to rebound, Melinda Wharton, MD, said at the virtual meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Pediatrics was among the hardest hit specialties, with a 62% reduction in outpatient visits by April 5, said Dr. Wharton, director of the immunization services division at the CDC’s National Center for Immunization and Respiratory Diseases. However, visits for all pediatric age groups increased in May, compared with April, and the CDC emphasized the need to educate families about the importance of routine vaccination and well-child visits, Dr. Wharton said.
The CDC strategies to support routine childhood vaccination include monitoring vaccination service delivery to inform targeted interventions, said Dr. Wharton. In addition, the CDC will continue to support providers by identifying gaps in the Vaccines For Children (VFC) program network, increasing VFC funding, developing guidance materials, and identifying policy interventions.
Many small practices have struggled during the pandemic, and financial support is available through the Provider Relief Fund, which is now available to all Medicaid and Children’s Health Insurance Program (CHIP) providers, said Dr. Wharton.
because more families may now qualify for the program because of changes in job status and income, and parents may not be aware that their children may be eligible, she said.
“Vaccination is an essential medical service for all children and adolescents, ideally in the medical home,” Dr. Wharton said. The CDC’s interim guidance for immunization during the COVID-19 pandemic calls for administering all current or overdue vaccines according to the routine immunization schedule during the same visit, and implementing strategies to get patients caught up, prioritizing newborns, infants, and children up to age 24 months. The guidance includes details on safe delivery of vaccines, including physical distance and the use of personal protective equipment.
In addition, encourage parents to return for well-child visits, and use reminder systems to help keep patients current on visits and vaccines. “Discuss the safety protocols that have been put in place,” Dr. Wharton emphasized. The CDC also offers resources for providers to help communicate with parents about routine vaccination.
Looking ahead, back-to-school vaccination requirements “provide a critical checkpoint for children’s vaccination status,” Dr. Wharton said. Catch-up vaccination during the summer will help clinical capacity manage back-to-school and influenza vaccination in the fall, she emphasized. “Influenza vaccination will be an important strategy to decrease stress on our health care system.”
Flu vaccination strategies should focus on adults at higher risk for COVID-19 infections, such as health care providers. In addition, identifying and reducing disparities will be important for future COVID-19 vaccines, as well as for the flu this season, she noted.
View the complete guidance online.
Dr. Wharton had no relevant financial disclosures.
Outpatient medical care has been severely disrupted during the COVID-19 pandemic with a reduction of nearly 70% in outpatient visits since March before starting to rebound, Melinda Wharton, MD, said at the virtual meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Pediatrics was among the hardest hit specialties, with a 62% reduction in outpatient visits by April 5, said Dr. Wharton, director of the immunization services division at the CDC’s National Center for Immunization and Respiratory Diseases. However, visits for all pediatric age groups increased in May, compared with April, and the CDC emphasized the need to educate families about the importance of routine vaccination and well-child visits, Dr. Wharton said.
The CDC strategies to support routine childhood vaccination include monitoring vaccination service delivery to inform targeted interventions, said Dr. Wharton. In addition, the CDC will continue to support providers by identifying gaps in the Vaccines For Children (VFC) program network, increasing VFC funding, developing guidance materials, and identifying policy interventions.
Many small practices have struggled during the pandemic, and financial support is available through the Provider Relief Fund, which is now available to all Medicaid and Children’s Health Insurance Program (CHIP) providers, said Dr. Wharton.
because more families may now qualify for the program because of changes in job status and income, and parents may not be aware that their children may be eligible, she said.
“Vaccination is an essential medical service for all children and adolescents, ideally in the medical home,” Dr. Wharton said. The CDC’s interim guidance for immunization during the COVID-19 pandemic calls for administering all current or overdue vaccines according to the routine immunization schedule during the same visit, and implementing strategies to get patients caught up, prioritizing newborns, infants, and children up to age 24 months. The guidance includes details on safe delivery of vaccines, including physical distance and the use of personal protective equipment.
In addition, encourage parents to return for well-child visits, and use reminder systems to help keep patients current on visits and vaccines. “Discuss the safety protocols that have been put in place,” Dr. Wharton emphasized. The CDC also offers resources for providers to help communicate with parents about routine vaccination.
Looking ahead, back-to-school vaccination requirements “provide a critical checkpoint for children’s vaccination status,” Dr. Wharton said. Catch-up vaccination during the summer will help clinical capacity manage back-to-school and influenza vaccination in the fall, she emphasized. “Influenza vaccination will be an important strategy to decrease stress on our health care system.”
Flu vaccination strategies should focus on adults at higher risk for COVID-19 infections, such as health care providers. In addition, identifying and reducing disparities will be important for future COVID-19 vaccines, as well as for the flu this season, she noted.
View the complete guidance online.
Dr. Wharton had no relevant financial disclosures.






