User login
Keep Calm and Log On: Telemedicine for COVID-19 Pandemic Response
The field of telemedicine, in which clinicians use remote evaluation and monitoring to diagnose and treat patients, has grown substantially over the past decade. Its roles in acute care medicine settings are diverse, including virtual intensive care unit (ICU) care, after-hours medical admissions, cross coverage, and, most aptly, disaster management.1
At HealthPartners, a large integrated healthcare delivery and financing system based in the Twin Cities region of Minnesota, we have used provider-initiated telemedicine in hospital medicine for more than 2 years, providing evening and nighttime hospitalist coverage to our rural hospitals. We additionally provide a 24/7 nurse practitioner-staffed virtual clinic called Virtuwell.2 Because we are now immersed in a global pandemic, we have taken steps to bolster our telemedicine infrastructure to meet increasing needs.
SARS-CoV-2, the causative agent of COVID-19, is a novel coronavirus with the capability to cause severe illness in roughly 14% of those infected.3 According to some estimates, the virus may infect up to 60% of the US population in the next year.4 As the pandemic looms over the country and the healthcare community, telemedicine can offer tools to help respond to this crisis. Healthcare systems leveraging telemedicine for patient care will gain several advantages, including workforce sustainability, reduction of provider burnout, limitation of provider exposure, and reduction of personal protective equipment (PPE) waste (Table). Telemedicine can also facilitate staffing of both large and small facilities that find themselves overwhelmed with pandemic-related patient overload (PRPO). Although telemedicine holds promise for pandemic response, this technology has limitations. It requires robust IT infrastructure, training of both nurses and physicians, and modifications to integrate within hospital workflows. In this article, we summarize key clinical needs that telemedicine can meet, implementation challenges, and important business considerations.
BACKGROUND
Our organization currently uses telemedicine to provide after-hours hospital medicine coverage from 6
APPLICATIONS
Patient Triage
Limiting exposure in the community and in the acute care setting is key to “flattening the curve” in pandemics.5 Triaging patients by telephone and online surveys is an important method to prevent high-risk patients from exposing others to infection. For example, since March 9, 2020, over 20,000 patients have called in weekly for COVID-19 screening. Although our organization introduced drive-up testing to reduce exposure, patients are still presenting to our clinics and emergency rooms in need of screening and testing. In several of our clinics, patients have been roomed alone to facilitate screening in the room by use of Google Duo, a free video chat product. Rooms with telemedicine capabilities allow patients with potentially communicable infections to be evaluated and observed while avoiding the risk of viral transmission. Additional considerations could include self-administered nasal swabs; although this has comparable efficacy to staff-administered swabs,6 it has not yet been implemented in our clinics.
Direct Care
Virtual care, specifically synchronous video and audio provider-initiated services, is a well-established modality to provide direct care to patients in acute care and ambulatory settings.7 Telemedicine can be deployed to care for hospitalized patients in most locations as long as they meet the operational requirements described below. With a bedside nurse or other facilitator, patients can be interviewed and examined using a high definition camera and digital peripherals, including stethoscopes, otoscopes, ophthalmoscopes, and dermatoscopes. COVID-19 patients or patients under investigation may be seen in this manner. In-person visits should remain part of patients’ care as an important part of the provider-patient relationship8; however, telemedicine could still be deployed to provide direct care and monitoring to these patients while minimizing exposure to healthcare personnel. Additionally, telemedicine can be used for specialist consultations that are likely in high demand with COVID-19, including infectious disease, cardiology, and pulmonology.
Exposure Reduction and Resource Allocation
Currently in the United States there are concerns for shortages of PPE including surgical masks and N95 respirators. Telemedicine can reduce provider exposure, increase provider efficiency, and curtail PPE utilization by minimizing the number and frequency of in-room visits while still allowing virtual visits for direct patient care. For instance, our nursing staff is currently using telemedicine to conduct hourly rounding and limit unnecessary in-room visits.
We recommend keeping telemedicine equipment within individual isolation rooms intended for COVID-19 patients in order to eliminate the need for repeated cleaning. For other patients, a mobile cart could be used. Most commercial video software can autoanswer calls to allow for staff-free history taking. For a thorough physical exam, a bedside facilitator is need for use of digital stethoscopes and similar peripherals.
Provider Shortages and Reducing Burnout
Because SARS-CoV-2 is a highly contagious pathogen that can spread prior to symptom presentation, current CDC guidelines recommend self-monitoring at home for health care workers who have a healthcare-related exposure to a COVID-19 patient.9 This can leave significant gaps in coverage for healthcare systems. For example, in Vacaville, California, one positive case resulted in over 200 health care workers unable to work on site.10
Large volumes of acutely ill patients, coupled with the risk of ill or quarantined providers, means provider shortages due to PRPO are likely to occur and threaten hospitals’ ability to care for patients with or without COVID-19. Furthermore, given increased patient loads, frontline staff are at exceptionally high risk of burnout in pandemic situations. Hospital medicine teams will need contingency plans to meet the needs. Using telemedicine to protect the workforce and maintain staffing levels will reduce that risk.
Telehospitalists can see and examine patients, write orders, and maintain patient service lines much like in-person providers. Recently, we have used it when providers are ill or self-monitoring. In multisite systems, telehospitalists who are privileged in multiple hospitals can be efficiently deployed to meet patient care needs and relieve overburdened providers across hundreds of miles or more.
Enabling patient rooms for telemedicine allows telehospitalists and other providers to see hospitalized patients. Furthermore, quarantined hospitalists can continue to work and support in-person clinical services during PRPO. Providers in high-risk groups (eg, older, immunosuppressed, pregnant) can also continue caring for patients with telemedicine while maintaining safety. As schools close, telemedicine can help providers navigate the challenge between patient care and childcare responsibilities.
OPERATIONAL REQUIREMENTS
The basic element of telemedicine involves a computer or monitor with an internet-connected camera and a HIPAA-compliant video application, but implementation can vary.
Recent changes have allowed the use of popular video chat software such as FaceTime, Skype, or Google Duo for patient interactions; with a tablet attached to a stand, organizations can easily create a mobile telemedicine workstation. Larger monitors or mounted screens can be used in patient areas where portability is not required. A strong network infrastructure and robust IT support are also necessary; as of 2016, 24 million Americans did not have broadband access, and even areas that do can struggle with wireless connectivity in hospitals with thick concrete walls and lack of wi-fi extenders.11
With the addition of a digital stethoscope, hospitalists can perform a thorough history and physical with the aid of bedside staff. This requires dedicated training for all members of the care team in order to optimize the virtual hospitalist’s “telepresence” and create a seamless patient experience. Provider education is imperative: Creating a virtual telepresence is essential in building a strong provider-patient relationship. We have used simulation training to prepare new telehospitalists.
An overlooked, but important, operational requirement is patient education and awareness. In the absence of introduction and onboarding, telemedicine can be viewed by patients as impersonal; however, with proper implementation, high patient satisfaction has been demonstrated in other virtual care experiences.12
FINANCIAL CONSIDERATIONS
Though several health systems offer “tele-ICU” services, the number of hospital medicine programs is more limited. The cost of building a program can be significant, with outlays for equipment, IT support, provider salaries, and training. While all 50 states and the District of Columbia cover some form of fee-for-service live video with Medicaid, only 40, along with DC, have parity laws with commercial payors. Medicare has historically had more restrictions, limiting covered services to specific types of originating sites in certain geographic areas. Furthermore, growth of telehospitalist programs has been hampered by the lack of reimbursement for “primary care services.”13
With passage of the Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020, geographic and site restrictions have been waived for Medicare reimbursement.14 Providers must still demonstrate a prior relationship with patients, which requires at least one encounter with the patient in the past 3 years by the same provider or one with a similar tax identification number (TIN). All hospitalists within our group are identified with a common TIN, which helps to meet this requirement for patient with recent admissions. However, clear guidance on reimbursement for primary care services by acute care providers is still lacking. As the utility of telemedicine is demonstrated in the hospital setting, we hope further changes may be enacted.
Organizations must properly credential and privilege telehospitalists. Telemedicine services may fall under either core or “delegated” privileges depending on the individual hospital. Additionally, while malpractice insurance does typically cover telemedicine services, each organization should verify this with their particular carrier.
SUMMARY
The COVID-19 pandemic has created a systemic challenge for healthcare systems across the nation. As hospitalists continue to be on the front lines, organizations can leverage telemedicine to support their patients, protect their clinicians, and conserve scarce resources. Building out a virtual care program is intricate and requires significant operational support. Laying the groundwork now can prepare institutions to provide necessary care for patients, not just in the current pandemic, but in numerous emergency health care situations in the future.
1. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745-74. https://doi.org/10.1001/jamainternmed.2018.1314.
2. Virtuwell. HealthPartners. 2020. https://www.virtuwell.com.
3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
4. Powell A. Coronavirus screening may miss two-thirds of infected travelers entering U.S. The Harvard Gazette. 2020. https://news.harvard.edu/gazette/story/2020/03/hundreds-of-u-s-coronavirus-cases-may-have-slipped-through-screenings/. Accessed March 13, 2020.
5. Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007:104(18);7582-7587. https://doi.org/10.1073/pnas.0610941104.
6. Akmatov MK, Gatzemeier A, Schughart, K, Pessler F. Equivalence of self- and staff-collected nasal swabs for the detection of viral respiratory pathogens. PLoS One. 2012:7(11);e48508. https://doi.org/10.1371/journal.pone.0048508.
7. Centers for Medicare & Medicaid Services. Telehealth Services. 2019. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Telehealth Srvcsfctsht.pdf. Accessed March 14, 2020.
8. Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015;163(10):787-789. https://doi.org/10.7326/M15-0498.
9. Centers for Disease Control and Prevention. Healthcare Personnel with Potential Exposure to COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed March 13, 2020.
10. Gold J. Surging Health Care Worker Quarantines Raise Concerns as Coronavirus Spreads. Kaiser Health News. 2020. https://khn.org/news/surging-health-care-worker-quarantines-raise-concerns-as-coronavirus-spreads/. Accessed March 12, 2020.
11. Federal Communications Commission. 2018 Broadband Deployment Report. 2018. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Accessed March 13, 2020.
12. Martinez KA, Rood M, Jhangiani N, et al. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J Gen Intern Med. 2018;33(10):1768-1773. https://doi.org/10.1007/s11606-018-4621-5.
13. Centers for Medicare & Medicaid Services. List of Telehealth Services. 2019. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes. Accessed March 13, 2020.
14. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, H.R. 6074, 116th Cong. 2020. https://congress.gov/bill/116th-congress/house-bill/6074/. Accessed March 13, 2020.
The field of telemedicine, in which clinicians use remote evaluation and monitoring to diagnose and treat patients, has grown substantially over the past decade. Its roles in acute care medicine settings are diverse, including virtual intensive care unit (ICU) care, after-hours medical admissions, cross coverage, and, most aptly, disaster management.1
At HealthPartners, a large integrated healthcare delivery and financing system based in the Twin Cities region of Minnesota, we have used provider-initiated telemedicine in hospital medicine for more than 2 years, providing evening and nighttime hospitalist coverage to our rural hospitals. We additionally provide a 24/7 nurse practitioner-staffed virtual clinic called Virtuwell.2 Because we are now immersed in a global pandemic, we have taken steps to bolster our telemedicine infrastructure to meet increasing needs.
SARS-CoV-2, the causative agent of COVID-19, is a novel coronavirus with the capability to cause severe illness in roughly 14% of those infected.3 According to some estimates, the virus may infect up to 60% of the US population in the next year.4 As the pandemic looms over the country and the healthcare community, telemedicine can offer tools to help respond to this crisis. Healthcare systems leveraging telemedicine for patient care will gain several advantages, including workforce sustainability, reduction of provider burnout, limitation of provider exposure, and reduction of personal protective equipment (PPE) waste (Table). Telemedicine can also facilitate staffing of both large and small facilities that find themselves overwhelmed with pandemic-related patient overload (PRPO). Although telemedicine holds promise for pandemic response, this technology has limitations. It requires robust IT infrastructure, training of both nurses and physicians, and modifications to integrate within hospital workflows. In this article, we summarize key clinical needs that telemedicine can meet, implementation challenges, and important business considerations.
BACKGROUND
Our organization currently uses telemedicine to provide after-hours hospital medicine coverage from 6
APPLICATIONS
Patient Triage
Limiting exposure in the community and in the acute care setting is key to “flattening the curve” in pandemics.5 Triaging patients by telephone and online surveys is an important method to prevent high-risk patients from exposing others to infection. For example, since March 9, 2020, over 20,000 patients have called in weekly for COVID-19 screening. Although our organization introduced drive-up testing to reduce exposure, patients are still presenting to our clinics and emergency rooms in need of screening and testing. In several of our clinics, patients have been roomed alone to facilitate screening in the room by use of Google Duo, a free video chat product. Rooms with telemedicine capabilities allow patients with potentially communicable infections to be evaluated and observed while avoiding the risk of viral transmission. Additional considerations could include self-administered nasal swabs; although this has comparable efficacy to staff-administered swabs,6 it has not yet been implemented in our clinics.
Direct Care
Virtual care, specifically synchronous video and audio provider-initiated services, is a well-established modality to provide direct care to patients in acute care and ambulatory settings.7 Telemedicine can be deployed to care for hospitalized patients in most locations as long as they meet the operational requirements described below. With a bedside nurse or other facilitator, patients can be interviewed and examined using a high definition camera and digital peripherals, including stethoscopes, otoscopes, ophthalmoscopes, and dermatoscopes. COVID-19 patients or patients under investigation may be seen in this manner. In-person visits should remain part of patients’ care as an important part of the provider-patient relationship8; however, telemedicine could still be deployed to provide direct care and monitoring to these patients while minimizing exposure to healthcare personnel. Additionally, telemedicine can be used for specialist consultations that are likely in high demand with COVID-19, including infectious disease, cardiology, and pulmonology.
Exposure Reduction and Resource Allocation
Currently in the United States there are concerns for shortages of PPE including surgical masks and N95 respirators. Telemedicine can reduce provider exposure, increase provider efficiency, and curtail PPE utilization by minimizing the number and frequency of in-room visits while still allowing virtual visits for direct patient care. For instance, our nursing staff is currently using telemedicine to conduct hourly rounding and limit unnecessary in-room visits.
We recommend keeping telemedicine equipment within individual isolation rooms intended for COVID-19 patients in order to eliminate the need for repeated cleaning. For other patients, a mobile cart could be used. Most commercial video software can autoanswer calls to allow for staff-free history taking. For a thorough physical exam, a bedside facilitator is need for use of digital stethoscopes and similar peripherals.
Provider Shortages and Reducing Burnout
Because SARS-CoV-2 is a highly contagious pathogen that can spread prior to symptom presentation, current CDC guidelines recommend self-monitoring at home for health care workers who have a healthcare-related exposure to a COVID-19 patient.9 This can leave significant gaps in coverage for healthcare systems. For example, in Vacaville, California, one positive case resulted in over 200 health care workers unable to work on site.10
Large volumes of acutely ill patients, coupled with the risk of ill or quarantined providers, means provider shortages due to PRPO are likely to occur and threaten hospitals’ ability to care for patients with or without COVID-19. Furthermore, given increased patient loads, frontline staff are at exceptionally high risk of burnout in pandemic situations. Hospital medicine teams will need contingency plans to meet the needs. Using telemedicine to protect the workforce and maintain staffing levels will reduce that risk.
Telehospitalists can see and examine patients, write orders, and maintain patient service lines much like in-person providers. Recently, we have used it when providers are ill or self-monitoring. In multisite systems, telehospitalists who are privileged in multiple hospitals can be efficiently deployed to meet patient care needs and relieve overburdened providers across hundreds of miles or more.
Enabling patient rooms for telemedicine allows telehospitalists and other providers to see hospitalized patients. Furthermore, quarantined hospitalists can continue to work and support in-person clinical services during PRPO. Providers in high-risk groups (eg, older, immunosuppressed, pregnant) can also continue caring for patients with telemedicine while maintaining safety. As schools close, telemedicine can help providers navigate the challenge between patient care and childcare responsibilities.
OPERATIONAL REQUIREMENTS
The basic element of telemedicine involves a computer or monitor with an internet-connected camera and a HIPAA-compliant video application, but implementation can vary.
Recent changes have allowed the use of popular video chat software such as FaceTime, Skype, or Google Duo for patient interactions; with a tablet attached to a stand, organizations can easily create a mobile telemedicine workstation. Larger monitors or mounted screens can be used in patient areas where portability is not required. A strong network infrastructure and robust IT support are also necessary; as of 2016, 24 million Americans did not have broadband access, and even areas that do can struggle with wireless connectivity in hospitals with thick concrete walls and lack of wi-fi extenders.11
With the addition of a digital stethoscope, hospitalists can perform a thorough history and physical with the aid of bedside staff. This requires dedicated training for all members of the care team in order to optimize the virtual hospitalist’s “telepresence” and create a seamless patient experience. Provider education is imperative: Creating a virtual telepresence is essential in building a strong provider-patient relationship. We have used simulation training to prepare new telehospitalists.
An overlooked, but important, operational requirement is patient education and awareness. In the absence of introduction and onboarding, telemedicine can be viewed by patients as impersonal; however, with proper implementation, high patient satisfaction has been demonstrated in other virtual care experiences.12
FINANCIAL CONSIDERATIONS
Though several health systems offer “tele-ICU” services, the number of hospital medicine programs is more limited. The cost of building a program can be significant, with outlays for equipment, IT support, provider salaries, and training. While all 50 states and the District of Columbia cover some form of fee-for-service live video with Medicaid, only 40, along with DC, have parity laws with commercial payors. Medicare has historically had more restrictions, limiting covered services to specific types of originating sites in certain geographic areas. Furthermore, growth of telehospitalist programs has been hampered by the lack of reimbursement for “primary care services.”13
With passage of the Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020, geographic and site restrictions have been waived for Medicare reimbursement.14 Providers must still demonstrate a prior relationship with patients, which requires at least one encounter with the patient in the past 3 years by the same provider or one with a similar tax identification number (TIN). All hospitalists within our group are identified with a common TIN, which helps to meet this requirement for patient with recent admissions. However, clear guidance on reimbursement for primary care services by acute care providers is still lacking. As the utility of telemedicine is demonstrated in the hospital setting, we hope further changes may be enacted.
Organizations must properly credential and privilege telehospitalists. Telemedicine services may fall under either core or “delegated” privileges depending on the individual hospital. Additionally, while malpractice insurance does typically cover telemedicine services, each organization should verify this with their particular carrier.
SUMMARY
The COVID-19 pandemic has created a systemic challenge for healthcare systems across the nation. As hospitalists continue to be on the front lines, organizations can leverage telemedicine to support their patients, protect their clinicians, and conserve scarce resources. Building out a virtual care program is intricate and requires significant operational support. Laying the groundwork now can prepare institutions to provide necessary care for patients, not just in the current pandemic, but in numerous emergency health care situations in the future.
The field of telemedicine, in which clinicians use remote evaluation and monitoring to diagnose and treat patients, has grown substantially over the past decade. Its roles in acute care medicine settings are diverse, including virtual intensive care unit (ICU) care, after-hours medical admissions, cross coverage, and, most aptly, disaster management.1
At HealthPartners, a large integrated healthcare delivery and financing system based in the Twin Cities region of Minnesota, we have used provider-initiated telemedicine in hospital medicine for more than 2 years, providing evening and nighttime hospitalist coverage to our rural hospitals. We additionally provide a 24/7 nurse practitioner-staffed virtual clinic called Virtuwell.2 Because we are now immersed in a global pandemic, we have taken steps to bolster our telemedicine infrastructure to meet increasing needs.
SARS-CoV-2, the causative agent of COVID-19, is a novel coronavirus with the capability to cause severe illness in roughly 14% of those infected.3 According to some estimates, the virus may infect up to 60% of the US population in the next year.4 As the pandemic looms over the country and the healthcare community, telemedicine can offer tools to help respond to this crisis. Healthcare systems leveraging telemedicine for patient care will gain several advantages, including workforce sustainability, reduction of provider burnout, limitation of provider exposure, and reduction of personal protective equipment (PPE) waste (Table). Telemedicine can also facilitate staffing of both large and small facilities that find themselves overwhelmed with pandemic-related patient overload (PRPO). Although telemedicine holds promise for pandemic response, this technology has limitations. It requires robust IT infrastructure, training of both nurses and physicians, and modifications to integrate within hospital workflows. In this article, we summarize key clinical needs that telemedicine can meet, implementation challenges, and important business considerations.
BACKGROUND
Our organization currently uses telemedicine to provide after-hours hospital medicine coverage from 6
APPLICATIONS
Patient Triage
Limiting exposure in the community and in the acute care setting is key to “flattening the curve” in pandemics.5 Triaging patients by telephone and online surveys is an important method to prevent high-risk patients from exposing others to infection. For example, since March 9, 2020, over 20,000 patients have called in weekly for COVID-19 screening. Although our organization introduced drive-up testing to reduce exposure, patients are still presenting to our clinics and emergency rooms in need of screening and testing. In several of our clinics, patients have been roomed alone to facilitate screening in the room by use of Google Duo, a free video chat product. Rooms with telemedicine capabilities allow patients with potentially communicable infections to be evaluated and observed while avoiding the risk of viral transmission. Additional considerations could include self-administered nasal swabs; although this has comparable efficacy to staff-administered swabs,6 it has not yet been implemented in our clinics.
Direct Care
Virtual care, specifically synchronous video and audio provider-initiated services, is a well-established modality to provide direct care to patients in acute care and ambulatory settings.7 Telemedicine can be deployed to care for hospitalized patients in most locations as long as they meet the operational requirements described below. With a bedside nurse or other facilitator, patients can be interviewed and examined using a high definition camera and digital peripherals, including stethoscopes, otoscopes, ophthalmoscopes, and dermatoscopes. COVID-19 patients or patients under investigation may be seen in this manner. In-person visits should remain part of patients’ care as an important part of the provider-patient relationship8; however, telemedicine could still be deployed to provide direct care and monitoring to these patients while minimizing exposure to healthcare personnel. Additionally, telemedicine can be used for specialist consultations that are likely in high demand with COVID-19, including infectious disease, cardiology, and pulmonology.
Exposure Reduction and Resource Allocation
Currently in the United States there are concerns for shortages of PPE including surgical masks and N95 respirators. Telemedicine can reduce provider exposure, increase provider efficiency, and curtail PPE utilization by minimizing the number and frequency of in-room visits while still allowing virtual visits for direct patient care. For instance, our nursing staff is currently using telemedicine to conduct hourly rounding and limit unnecessary in-room visits.
We recommend keeping telemedicine equipment within individual isolation rooms intended for COVID-19 patients in order to eliminate the need for repeated cleaning. For other patients, a mobile cart could be used. Most commercial video software can autoanswer calls to allow for staff-free history taking. For a thorough physical exam, a bedside facilitator is need for use of digital stethoscopes and similar peripherals.
Provider Shortages and Reducing Burnout
Because SARS-CoV-2 is a highly contagious pathogen that can spread prior to symptom presentation, current CDC guidelines recommend self-monitoring at home for health care workers who have a healthcare-related exposure to a COVID-19 patient.9 This can leave significant gaps in coverage for healthcare systems. For example, in Vacaville, California, one positive case resulted in over 200 health care workers unable to work on site.10
Large volumes of acutely ill patients, coupled with the risk of ill or quarantined providers, means provider shortages due to PRPO are likely to occur and threaten hospitals’ ability to care for patients with or without COVID-19. Furthermore, given increased patient loads, frontline staff are at exceptionally high risk of burnout in pandemic situations. Hospital medicine teams will need contingency plans to meet the needs. Using telemedicine to protect the workforce and maintain staffing levels will reduce that risk.
Telehospitalists can see and examine patients, write orders, and maintain patient service lines much like in-person providers. Recently, we have used it when providers are ill or self-monitoring. In multisite systems, telehospitalists who are privileged in multiple hospitals can be efficiently deployed to meet patient care needs and relieve overburdened providers across hundreds of miles or more.
Enabling patient rooms for telemedicine allows telehospitalists and other providers to see hospitalized patients. Furthermore, quarantined hospitalists can continue to work and support in-person clinical services during PRPO. Providers in high-risk groups (eg, older, immunosuppressed, pregnant) can also continue caring for patients with telemedicine while maintaining safety. As schools close, telemedicine can help providers navigate the challenge between patient care and childcare responsibilities.
OPERATIONAL REQUIREMENTS
The basic element of telemedicine involves a computer or monitor with an internet-connected camera and a HIPAA-compliant video application, but implementation can vary.
Recent changes have allowed the use of popular video chat software such as FaceTime, Skype, or Google Duo for patient interactions; with a tablet attached to a stand, organizations can easily create a mobile telemedicine workstation. Larger monitors or mounted screens can be used in patient areas where portability is not required. A strong network infrastructure and robust IT support are also necessary; as of 2016, 24 million Americans did not have broadband access, and even areas that do can struggle with wireless connectivity in hospitals with thick concrete walls and lack of wi-fi extenders.11
With the addition of a digital stethoscope, hospitalists can perform a thorough history and physical with the aid of bedside staff. This requires dedicated training for all members of the care team in order to optimize the virtual hospitalist’s “telepresence” and create a seamless patient experience. Provider education is imperative: Creating a virtual telepresence is essential in building a strong provider-patient relationship. We have used simulation training to prepare new telehospitalists.
An overlooked, but important, operational requirement is patient education and awareness. In the absence of introduction and onboarding, telemedicine can be viewed by patients as impersonal; however, with proper implementation, high patient satisfaction has been demonstrated in other virtual care experiences.12
FINANCIAL CONSIDERATIONS
Though several health systems offer “tele-ICU” services, the number of hospital medicine programs is more limited. The cost of building a program can be significant, with outlays for equipment, IT support, provider salaries, and training. While all 50 states and the District of Columbia cover some form of fee-for-service live video with Medicaid, only 40, along with DC, have parity laws with commercial payors. Medicare has historically had more restrictions, limiting covered services to specific types of originating sites in certain geographic areas. Furthermore, growth of telehospitalist programs has been hampered by the lack of reimbursement for “primary care services.”13
With passage of the Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020, geographic and site restrictions have been waived for Medicare reimbursement.14 Providers must still demonstrate a prior relationship with patients, which requires at least one encounter with the patient in the past 3 years by the same provider or one with a similar tax identification number (TIN). All hospitalists within our group are identified with a common TIN, which helps to meet this requirement for patient with recent admissions. However, clear guidance on reimbursement for primary care services by acute care providers is still lacking. As the utility of telemedicine is demonstrated in the hospital setting, we hope further changes may be enacted.
Organizations must properly credential and privilege telehospitalists. Telemedicine services may fall under either core or “delegated” privileges depending on the individual hospital. Additionally, while malpractice insurance does typically cover telemedicine services, each organization should verify this with their particular carrier.
SUMMARY
The COVID-19 pandemic has created a systemic challenge for healthcare systems across the nation. As hospitalists continue to be on the front lines, organizations can leverage telemedicine to support their patients, protect their clinicians, and conserve scarce resources. Building out a virtual care program is intricate and requires significant operational support. Laying the groundwork now can prepare institutions to provide necessary care for patients, not just in the current pandemic, but in numerous emergency health care situations in the future.
1. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745-74. https://doi.org/10.1001/jamainternmed.2018.1314.
2. Virtuwell. HealthPartners. 2020. https://www.virtuwell.com.
3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
4. Powell A. Coronavirus screening may miss two-thirds of infected travelers entering U.S. The Harvard Gazette. 2020. https://news.harvard.edu/gazette/story/2020/03/hundreds-of-u-s-coronavirus-cases-may-have-slipped-through-screenings/. Accessed March 13, 2020.
5. Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007:104(18);7582-7587. https://doi.org/10.1073/pnas.0610941104.
6. Akmatov MK, Gatzemeier A, Schughart, K, Pessler F. Equivalence of self- and staff-collected nasal swabs for the detection of viral respiratory pathogens. PLoS One. 2012:7(11);e48508. https://doi.org/10.1371/journal.pone.0048508.
7. Centers for Medicare & Medicaid Services. Telehealth Services. 2019. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Telehealth Srvcsfctsht.pdf. Accessed March 14, 2020.
8. Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015;163(10):787-789. https://doi.org/10.7326/M15-0498.
9. Centers for Disease Control and Prevention. Healthcare Personnel with Potential Exposure to COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed March 13, 2020.
10. Gold J. Surging Health Care Worker Quarantines Raise Concerns as Coronavirus Spreads. Kaiser Health News. 2020. https://khn.org/news/surging-health-care-worker-quarantines-raise-concerns-as-coronavirus-spreads/. Accessed March 12, 2020.
11. Federal Communications Commission. 2018 Broadband Deployment Report. 2018. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Accessed March 13, 2020.
12. Martinez KA, Rood M, Jhangiani N, et al. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J Gen Intern Med. 2018;33(10):1768-1773. https://doi.org/10.1007/s11606-018-4621-5.
13. Centers for Medicare & Medicaid Services. List of Telehealth Services. 2019. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes. Accessed March 13, 2020.
14. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, H.R. 6074, 116th Cong. 2020. https://congress.gov/bill/116th-congress/house-bill/6074/. Accessed March 13, 2020.
1. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745-74. https://doi.org/10.1001/jamainternmed.2018.1314.
2. Virtuwell. HealthPartners. 2020. https://www.virtuwell.com.
3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
4. Powell A. Coronavirus screening may miss two-thirds of infected travelers entering U.S. The Harvard Gazette. 2020. https://news.harvard.edu/gazette/story/2020/03/hundreds-of-u-s-coronavirus-cases-may-have-slipped-through-screenings/. Accessed March 13, 2020.
5. Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007:104(18);7582-7587. https://doi.org/10.1073/pnas.0610941104.
6. Akmatov MK, Gatzemeier A, Schughart, K, Pessler F. Equivalence of self- and staff-collected nasal swabs for the detection of viral respiratory pathogens. PLoS One. 2012:7(11);e48508. https://doi.org/10.1371/journal.pone.0048508.
7. Centers for Medicare & Medicaid Services. Telehealth Services. 2019. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Telehealth Srvcsfctsht.pdf. Accessed March 14, 2020.
8. Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015;163(10):787-789. https://doi.org/10.7326/M15-0498.
9. Centers for Disease Control and Prevention. Healthcare Personnel with Potential Exposure to COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed March 13, 2020.
10. Gold J. Surging Health Care Worker Quarantines Raise Concerns as Coronavirus Spreads. Kaiser Health News. 2020. https://khn.org/news/surging-health-care-worker-quarantines-raise-concerns-as-coronavirus-spreads/. Accessed March 12, 2020.
11. Federal Communications Commission. 2018 Broadband Deployment Report. 2018. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Accessed March 13, 2020.
12. Martinez KA, Rood M, Jhangiani N, et al. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J Gen Intern Med. 2018;33(10):1768-1773. https://doi.org/10.1007/s11606-018-4621-5.
13. Centers for Medicare & Medicaid Services. List of Telehealth Services. 2019. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes. Accessed March 13, 2020.
14. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, H.R. 6074, 116th Cong. 2020. https://congress.gov/bill/116th-congress/house-bill/6074/. Accessed March 13, 2020.
© 2020 Society of Hospital Medicine
Close your practice temporarily ... or longer? Your decision during COVID-19
On March 19, 2020, Gene Dorio, MD, a geriatrician at a two-physician practice in Santa Clarita, Calif., called his staff together to decide whether to stay open in the face of the COVID-19 pandemic.
“We have seven people, and I did not want to put any of them at risk,” he said. “We don’t want to put patients at risk, either.” The practice had been operating successfully for many years.
The practice’s finances were being threatened by an abrupt and very significant decline in patient visits. “People have been canceling all the time,” he said. “They’re canceling out of fear. I saw 5 patients today, and I usually see 10-14 patients a day.”
After much discussion, “we decided to stay open,” he said. “That’s the most important thing we can do for our patients and this community.”
The staff will meet again in a few weeks to reassess their future. “This is a fluid situation,” Dr. Dorio said. If things do not improve financially, he does not rule out the possibility of having to close.
At medical practices across the country, the COVID-19 pandemic is threatening not only the lives of staff and patients but also the economic well-being of the practices themselves, and many are contemplating closing.
Many patients are not showing up for appointments. In addition, practices such as Dr. Dorio’s are advising older patients, who are at higher risk for mortality, not to come in, and they are canceling nonurgent visits. “Financially speaking, we are shooting ourselves in the foot,” Dr. Dorio said.
In addition, many hospitals are canceling elective procedures, which are an important source of income for a wide array of specialists, including gastroenterologists, orthopedic surgeons, and cardiologists. The thinking is that elective surgeries would take away important resources from COVID-19 patients and that elective-surgery patients would be put at risk of getting the virus.
The financial pain for practices came abruptly, says Steve Messinger, president of ECG Management Consultants in Washington, D.C. “The first half of March was somewhat normal for practices. In the second half of March, things escalated dramatically.”
In the past few weeks, “there has been a significant drop-off in the number of claims at health insurers,” Mr. Messinger said. “This loss of volume is reminiscent of what we saw during the Great Recession of 2008-2009.”
Hoping to stay open: Here’s what to try first
“Most doctors are hoping that this will be a temporary slowdown of their practices,” said A. Michael La Penna, a practice management advisor in Grand Rapids, Mich. “It’s human nature to assume that relative normalcy will return fairly soon, so just hang in there.”
Some physicians who are putting off closing may be hoping for some kind of financial rescue. On March 19, the American Medical Association and several other major physician groups asked Congressional leaders to take several actions, including providing “dedicated financial support to all physicians and their practices who are experiencing adverse economic impact on their practices from suspending elective visits and procedures.”
Practices that have decided to stay open are radically changing their operations.
Phil Boucher, MD, a pediatrician in Lincoln, Neb., is trying to keep his office open by strategically reorganizing the way he schedules patient visits and by seeing patients via telemedicine.
Practices have also been separating well patients from sick ones. Dr. Boucher has started conducting well visits, such as seeing babies who are brought in for vaccination, in the morning and sick visits in the afternoon.
Dr. Boucher also says he has postponed physical examinations for the next school year until the summer, so that children are not put at risk for exposure at the practice. “Usually we like to space out the physicals so we won’t get overwhelmed in the summer, but we have no choice.”
“The concern is that you don’t want a lot of patients in your office at any one time,” said Gregory Mertz, a physician practice manager in Virginia Beach.
A group of urologists in Fredericksburg, Va., who are Mr. Mertz’s clients, have limited their practice to urgent visits, and patients are screened before coming in for an appointment. “When patients call, someone talks to the patient over the phone and determine whether they should come in,” said Mr. Mertz.
Telemedicine can help doctors keep seeing patients
Many practices have started using telemedicine as a way to distance staff from patients and avoid transmission of the virus. Medicare payment restrictions have been temporarily waived so that telemedicine can be provided throughout the country and can originate in patients’ homes.
Medicare is also temporarily allowing telemedicine visits via patients’ smartphones if they have a video connection such as Skype or FaceTime, and they must ensure patient privacy. In addition, Medicare has allowed practices to waive collecting copays for telemedicine. Reportedly, some private insurers have followed suit.
Dr. Boucher just started using telemedicine. “A couple of weeks ago I would have told you I could only use telemedicine on 5% of my patients, but now I think it’s more like 30%-40%,” he said. “It works for patients on medications, children with rashes, and parents with some sick children. You can eyeball the patient and say, ‘Let’s wait and see how things go.’ ”
But Dr. Dorio finds it less useful. “It would be nice if all the patients knew how to use FaceTime or Skype, but many seniors do not,” he said.
The sad decision to cut staff
Now that practices are seeing fewer patients, they are forced to consider reducing staff. “Staff is largest expense other than real estate, so practices have to closely manage their staffing,” Mr. Mertz said. “On a weekly or even daily basis, the practice has to match staffing to patient demand.”
Some staff may seek time off to take care of children who are now released from school. Others may be quarantined if they are suspected of having been infected by the virus. And some staff may be repurposed for other work, such as phone triaging or wiping down surfaces.
“The practice may decide: ‘I don’t need you this month,’ ” Mr. Mertz said. “Then the staff member can get unemployment as long are they have exhausted the paid leave they had coming to them.”
Many doctors want to keep all their staff on board. “In that case, the practice could impose shorter work weeks for existing staff,” said Elizabeth Woodcock, a practice management consultant in Atlanta. “Many people might have to work on a temporary basis.”
Trying to make the closure temporary
Most practices are still receiving income from past billing, since the reduction in volume started recently, so they have a few weeks or longer to decide what to do next, Mr. La Penna says. He suggests that they use the time to plan for the future.
“You need to have a plan for what you will do if this situation continues. When the risk is unknown, as is the case with this pandemic, people tend to plan for the best and fear the worst,” he said. “But it makes more sense to plan for the worst and hope for the best.”
Mr. La Penna advises practices to thoroughly analyze their operations. That analysis should include defining ongoing expenses and deciding how to handle them, developing a time-off policy for employees, and holding off on new hires and purchases.
He advises being transparent about your plans. “Be very public and forthcoming about the measures the practice is taking to avoid a complete shutdown, but keep your options open. Communicate with referral sources at every stage so that they stay in the loop.”
Procedure-oriented practices should follow the rules on elective procedures, Mr. La Penna says. “Conform to your association’s national guidelines on performing elective surgery or procedures,” he said. “If you do not follow those guidelines, you may be liable if your patient develops the virus.”
The AMA has compiled a list of actions to help keep your practice open. Here are some highlights:
- Determine the minimal cash flow you’d need. Develop a contingency plan based on estimates of minimum cash flow to stay afloat.
- Track your losses and expenses. You’ll need a record to make a claim through your business insurance policy. The policy may or may not cover COVID-19-related liabilities. Contact your broker to find out.
- Keep track of impending defaults. Review existing loan documents and financial covenants to determine whether a slowdown of business or collections could trigger a default.
- Negotiate with lenders. Contact vendors, landlords, and creditors to discuss reasonable accommodations for cash-flow disruptions. Consider asking them for forbearance, forgiveness, or a standstill, and agree to establish a process for keeping them informed over time.
- Get a low-interest loan. The Small Business Administration has begun to administer low-interest loans funded by numerous states, counties, and municipalities.
- Keep up with policy changes. State, local, and federal laws and regulations that affect practices are changing rapidly. Assign a staff member to follow these changes in the news and on government websites.
Closing your office may be the only option
Still, many practices may have to close – hopefully, most closures will be temporary, but some could end up being permanent.
“If you want to close your practice temporarily, you can get a short-term loan, try to defer payments, and wait for circumstances to improve,” Mr. La Penna said. “You’ll need to spend a few weeks winding down your practice, and you’ll want to make sure employees and patients don’t drift off.”
However, many practices may have no choice but to go permanently out of business, Mr. La Penna says.
The problem for many practices is that they typically distribute income among partners and have not retained earnings to cushion them from a financial disaster, Mr. Messinger says. “Some higher-performing practices have a cash surplus of perhaps 2 months, if that. They could take out loans and use lines of credit, but some of them already have outstanding loans for equipment or accounts receivables.”
Older physicians who were planning retirement may decide to retire early. “Anecdotally, there are a number of doctors who are ready to call it quits,” said Louis Weinstein, MD, chair of the AMA Senior Physicians Section. “This virus is the last straw. Their thought is: ‘Get out before you get sick.’ One colleague was going to close in a year from now but decided to speed it up.”
To find the specific steps needed to shut down a practice, check with physician organizations, practice managers, and health care attorneys. For example, the American Association of Family Physicians provides a Closing Your Practice Checklist, which specifies what you should do 60-90 days and 30-60 days before closing.
Employed physicians’ concerns
While private practices wrestle with staying open, there are potentially some grim or unhappy prospects for employed physicians too.
Many hospitals are in difficult economic straits and may not be able to afford paying doctors who aren’t working. But some experts are more optimistic.
“In many cases, I think the hospital will pay their salary even though their volume is down,” Mr. Mertz said. And Mr. Messinger said: “Hospitals may put employed physicians with low volume on an ‘RVU [relative value unit] holiday’ for a while. They don’t want to have a destabilized workforce.”
“When employed surgeons can’t do elective procedures, suddenly they can’t meet their productivity targets to get bonuses,” Mr. La Penna said. Productivity measures are typically based on RVUs. Mr. La Penna says he is working with a 100-physician practice where RVU payments that had been projected for the remainder of the year are expected to fall by half.
Some employed physicians have a guaranteed base pay that is not affected by RVUs, but in many cases, pay is based purely on productivity, says Andrew Hajde, assistant director of association content at the Medical Group Management Association. “If their volume goes down, they are in danger of not getting paid,” he said.
A version of this article originally appeared on Medscape.com.
On March 19, 2020, Gene Dorio, MD, a geriatrician at a two-physician practice in Santa Clarita, Calif., called his staff together to decide whether to stay open in the face of the COVID-19 pandemic.
“We have seven people, and I did not want to put any of them at risk,” he said. “We don’t want to put patients at risk, either.” The practice had been operating successfully for many years.
The practice’s finances were being threatened by an abrupt and very significant decline in patient visits. “People have been canceling all the time,” he said. “They’re canceling out of fear. I saw 5 patients today, and I usually see 10-14 patients a day.”
After much discussion, “we decided to stay open,” he said. “That’s the most important thing we can do for our patients and this community.”
The staff will meet again in a few weeks to reassess their future. “This is a fluid situation,” Dr. Dorio said. If things do not improve financially, he does not rule out the possibility of having to close.
At medical practices across the country, the COVID-19 pandemic is threatening not only the lives of staff and patients but also the economic well-being of the practices themselves, and many are contemplating closing.
Many patients are not showing up for appointments. In addition, practices such as Dr. Dorio’s are advising older patients, who are at higher risk for mortality, not to come in, and they are canceling nonurgent visits. “Financially speaking, we are shooting ourselves in the foot,” Dr. Dorio said.
In addition, many hospitals are canceling elective procedures, which are an important source of income for a wide array of specialists, including gastroenterologists, orthopedic surgeons, and cardiologists. The thinking is that elective surgeries would take away important resources from COVID-19 patients and that elective-surgery patients would be put at risk of getting the virus.
The financial pain for practices came abruptly, says Steve Messinger, president of ECG Management Consultants in Washington, D.C. “The first half of March was somewhat normal for practices. In the second half of March, things escalated dramatically.”
In the past few weeks, “there has been a significant drop-off in the number of claims at health insurers,” Mr. Messinger said. “This loss of volume is reminiscent of what we saw during the Great Recession of 2008-2009.”
Hoping to stay open: Here’s what to try first
“Most doctors are hoping that this will be a temporary slowdown of their practices,” said A. Michael La Penna, a practice management advisor in Grand Rapids, Mich. “It’s human nature to assume that relative normalcy will return fairly soon, so just hang in there.”
Some physicians who are putting off closing may be hoping for some kind of financial rescue. On March 19, the American Medical Association and several other major physician groups asked Congressional leaders to take several actions, including providing “dedicated financial support to all physicians and their practices who are experiencing adverse economic impact on their practices from suspending elective visits and procedures.”
Practices that have decided to stay open are radically changing their operations.
Phil Boucher, MD, a pediatrician in Lincoln, Neb., is trying to keep his office open by strategically reorganizing the way he schedules patient visits and by seeing patients via telemedicine.
Practices have also been separating well patients from sick ones. Dr. Boucher has started conducting well visits, such as seeing babies who are brought in for vaccination, in the morning and sick visits in the afternoon.
Dr. Boucher also says he has postponed physical examinations for the next school year until the summer, so that children are not put at risk for exposure at the practice. “Usually we like to space out the physicals so we won’t get overwhelmed in the summer, but we have no choice.”
“The concern is that you don’t want a lot of patients in your office at any one time,” said Gregory Mertz, a physician practice manager in Virginia Beach.
A group of urologists in Fredericksburg, Va., who are Mr. Mertz’s clients, have limited their practice to urgent visits, and patients are screened before coming in for an appointment. “When patients call, someone talks to the patient over the phone and determine whether they should come in,” said Mr. Mertz.
Telemedicine can help doctors keep seeing patients
Many practices have started using telemedicine as a way to distance staff from patients and avoid transmission of the virus. Medicare payment restrictions have been temporarily waived so that telemedicine can be provided throughout the country and can originate in patients’ homes.
Medicare is also temporarily allowing telemedicine visits via patients’ smartphones if they have a video connection such as Skype or FaceTime, and they must ensure patient privacy. In addition, Medicare has allowed practices to waive collecting copays for telemedicine. Reportedly, some private insurers have followed suit.
Dr. Boucher just started using telemedicine. “A couple of weeks ago I would have told you I could only use telemedicine on 5% of my patients, but now I think it’s more like 30%-40%,” he said. “It works for patients on medications, children with rashes, and parents with some sick children. You can eyeball the patient and say, ‘Let’s wait and see how things go.’ ”
But Dr. Dorio finds it less useful. “It would be nice if all the patients knew how to use FaceTime or Skype, but many seniors do not,” he said.
The sad decision to cut staff
Now that practices are seeing fewer patients, they are forced to consider reducing staff. “Staff is largest expense other than real estate, so practices have to closely manage their staffing,” Mr. Mertz said. “On a weekly or even daily basis, the practice has to match staffing to patient demand.”
Some staff may seek time off to take care of children who are now released from school. Others may be quarantined if they are suspected of having been infected by the virus. And some staff may be repurposed for other work, such as phone triaging or wiping down surfaces.
“The practice may decide: ‘I don’t need you this month,’ ” Mr. Mertz said. “Then the staff member can get unemployment as long are they have exhausted the paid leave they had coming to them.”
Many doctors want to keep all their staff on board. “In that case, the practice could impose shorter work weeks for existing staff,” said Elizabeth Woodcock, a practice management consultant in Atlanta. “Many people might have to work on a temporary basis.”
Trying to make the closure temporary
Most practices are still receiving income from past billing, since the reduction in volume started recently, so they have a few weeks or longer to decide what to do next, Mr. La Penna says. He suggests that they use the time to plan for the future.
“You need to have a plan for what you will do if this situation continues. When the risk is unknown, as is the case with this pandemic, people tend to plan for the best and fear the worst,” he said. “But it makes more sense to plan for the worst and hope for the best.”
Mr. La Penna advises practices to thoroughly analyze their operations. That analysis should include defining ongoing expenses and deciding how to handle them, developing a time-off policy for employees, and holding off on new hires and purchases.
He advises being transparent about your plans. “Be very public and forthcoming about the measures the practice is taking to avoid a complete shutdown, but keep your options open. Communicate with referral sources at every stage so that they stay in the loop.”
Procedure-oriented practices should follow the rules on elective procedures, Mr. La Penna says. “Conform to your association’s national guidelines on performing elective surgery or procedures,” he said. “If you do not follow those guidelines, you may be liable if your patient develops the virus.”
The AMA has compiled a list of actions to help keep your practice open. Here are some highlights:
- Determine the minimal cash flow you’d need. Develop a contingency plan based on estimates of minimum cash flow to stay afloat.
- Track your losses and expenses. You’ll need a record to make a claim through your business insurance policy. The policy may or may not cover COVID-19-related liabilities. Contact your broker to find out.
- Keep track of impending defaults. Review existing loan documents and financial covenants to determine whether a slowdown of business or collections could trigger a default.
- Negotiate with lenders. Contact vendors, landlords, and creditors to discuss reasonable accommodations for cash-flow disruptions. Consider asking them for forbearance, forgiveness, or a standstill, and agree to establish a process for keeping them informed over time.
- Get a low-interest loan. The Small Business Administration has begun to administer low-interest loans funded by numerous states, counties, and municipalities.
- Keep up with policy changes. State, local, and federal laws and regulations that affect practices are changing rapidly. Assign a staff member to follow these changes in the news and on government websites.
Closing your office may be the only option
Still, many practices may have to close – hopefully, most closures will be temporary, but some could end up being permanent.
“If you want to close your practice temporarily, you can get a short-term loan, try to defer payments, and wait for circumstances to improve,” Mr. La Penna said. “You’ll need to spend a few weeks winding down your practice, and you’ll want to make sure employees and patients don’t drift off.”
However, many practices may have no choice but to go permanently out of business, Mr. La Penna says.
The problem for many practices is that they typically distribute income among partners and have not retained earnings to cushion them from a financial disaster, Mr. Messinger says. “Some higher-performing practices have a cash surplus of perhaps 2 months, if that. They could take out loans and use lines of credit, but some of them already have outstanding loans for equipment or accounts receivables.”
Older physicians who were planning retirement may decide to retire early. “Anecdotally, there are a number of doctors who are ready to call it quits,” said Louis Weinstein, MD, chair of the AMA Senior Physicians Section. “This virus is the last straw. Their thought is: ‘Get out before you get sick.’ One colleague was going to close in a year from now but decided to speed it up.”
To find the specific steps needed to shut down a practice, check with physician organizations, practice managers, and health care attorneys. For example, the American Association of Family Physicians provides a Closing Your Practice Checklist, which specifies what you should do 60-90 days and 30-60 days before closing.
Employed physicians’ concerns
While private practices wrestle with staying open, there are potentially some grim or unhappy prospects for employed physicians too.
Many hospitals are in difficult economic straits and may not be able to afford paying doctors who aren’t working. But some experts are more optimistic.
“In many cases, I think the hospital will pay their salary even though their volume is down,” Mr. Mertz said. And Mr. Messinger said: “Hospitals may put employed physicians with low volume on an ‘RVU [relative value unit] holiday’ for a while. They don’t want to have a destabilized workforce.”
“When employed surgeons can’t do elective procedures, suddenly they can’t meet their productivity targets to get bonuses,” Mr. La Penna said. Productivity measures are typically based on RVUs. Mr. La Penna says he is working with a 100-physician practice where RVU payments that had been projected for the remainder of the year are expected to fall by half.
Some employed physicians have a guaranteed base pay that is not affected by RVUs, but in many cases, pay is based purely on productivity, says Andrew Hajde, assistant director of association content at the Medical Group Management Association. “If their volume goes down, they are in danger of not getting paid,” he said.
A version of this article originally appeared on Medscape.com.
On March 19, 2020, Gene Dorio, MD, a geriatrician at a two-physician practice in Santa Clarita, Calif., called his staff together to decide whether to stay open in the face of the COVID-19 pandemic.
“We have seven people, and I did not want to put any of them at risk,” he said. “We don’t want to put patients at risk, either.” The practice had been operating successfully for many years.
The practice’s finances were being threatened by an abrupt and very significant decline in patient visits. “People have been canceling all the time,” he said. “They’re canceling out of fear. I saw 5 patients today, and I usually see 10-14 patients a day.”
After much discussion, “we decided to stay open,” he said. “That’s the most important thing we can do for our patients and this community.”
The staff will meet again in a few weeks to reassess their future. “This is a fluid situation,” Dr. Dorio said. If things do not improve financially, he does not rule out the possibility of having to close.
At medical practices across the country, the COVID-19 pandemic is threatening not only the lives of staff and patients but also the economic well-being of the practices themselves, and many are contemplating closing.
Many patients are not showing up for appointments. In addition, practices such as Dr. Dorio’s are advising older patients, who are at higher risk for mortality, not to come in, and they are canceling nonurgent visits. “Financially speaking, we are shooting ourselves in the foot,” Dr. Dorio said.
In addition, many hospitals are canceling elective procedures, which are an important source of income for a wide array of specialists, including gastroenterologists, orthopedic surgeons, and cardiologists. The thinking is that elective surgeries would take away important resources from COVID-19 patients and that elective-surgery patients would be put at risk of getting the virus.
The financial pain for practices came abruptly, says Steve Messinger, president of ECG Management Consultants in Washington, D.C. “The first half of March was somewhat normal for practices. In the second half of March, things escalated dramatically.”
In the past few weeks, “there has been a significant drop-off in the number of claims at health insurers,” Mr. Messinger said. “This loss of volume is reminiscent of what we saw during the Great Recession of 2008-2009.”
Hoping to stay open: Here’s what to try first
“Most doctors are hoping that this will be a temporary slowdown of their practices,” said A. Michael La Penna, a practice management advisor in Grand Rapids, Mich. “It’s human nature to assume that relative normalcy will return fairly soon, so just hang in there.”
Some physicians who are putting off closing may be hoping for some kind of financial rescue. On March 19, the American Medical Association and several other major physician groups asked Congressional leaders to take several actions, including providing “dedicated financial support to all physicians and their practices who are experiencing adverse economic impact on their practices from suspending elective visits and procedures.”
Practices that have decided to stay open are radically changing their operations.
Phil Boucher, MD, a pediatrician in Lincoln, Neb., is trying to keep his office open by strategically reorganizing the way he schedules patient visits and by seeing patients via telemedicine.
Practices have also been separating well patients from sick ones. Dr. Boucher has started conducting well visits, such as seeing babies who are brought in for vaccination, in the morning and sick visits in the afternoon.
Dr. Boucher also says he has postponed physical examinations for the next school year until the summer, so that children are not put at risk for exposure at the practice. “Usually we like to space out the physicals so we won’t get overwhelmed in the summer, but we have no choice.”
“The concern is that you don’t want a lot of patients in your office at any one time,” said Gregory Mertz, a physician practice manager in Virginia Beach.
A group of urologists in Fredericksburg, Va., who are Mr. Mertz’s clients, have limited their practice to urgent visits, and patients are screened before coming in for an appointment. “When patients call, someone talks to the patient over the phone and determine whether they should come in,” said Mr. Mertz.
Telemedicine can help doctors keep seeing patients
Many practices have started using telemedicine as a way to distance staff from patients and avoid transmission of the virus. Medicare payment restrictions have been temporarily waived so that telemedicine can be provided throughout the country and can originate in patients’ homes.
Medicare is also temporarily allowing telemedicine visits via patients’ smartphones if they have a video connection such as Skype or FaceTime, and they must ensure patient privacy. In addition, Medicare has allowed practices to waive collecting copays for telemedicine. Reportedly, some private insurers have followed suit.
Dr. Boucher just started using telemedicine. “A couple of weeks ago I would have told you I could only use telemedicine on 5% of my patients, but now I think it’s more like 30%-40%,” he said. “It works for patients on medications, children with rashes, and parents with some sick children. You can eyeball the patient and say, ‘Let’s wait and see how things go.’ ”
But Dr. Dorio finds it less useful. “It would be nice if all the patients knew how to use FaceTime or Skype, but many seniors do not,” he said.
The sad decision to cut staff
Now that practices are seeing fewer patients, they are forced to consider reducing staff. “Staff is largest expense other than real estate, so practices have to closely manage their staffing,” Mr. Mertz said. “On a weekly or even daily basis, the practice has to match staffing to patient demand.”
Some staff may seek time off to take care of children who are now released from school. Others may be quarantined if they are suspected of having been infected by the virus. And some staff may be repurposed for other work, such as phone triaging or wiping down surfaces.
“The practice may decide: ‘I don’t need you this month,’ ” Mr. Mertz said. “Then the staff member can get unemployment as long are they have exhausted the paid leave they had coming to them.”
Many doctors want to keep all their staff on board. “In that case, the practice could impose shorter work weeks for existing staff,” said Elizabeth Woodcock, a practice management consultant in Atlanta. “Many people might have to work on a temporary basis.”
Trying to make the closure temporary
Most practices are still receiving income from past billing, since the reduction in volume started recently, so they have a few weeks or longer to decide what to do next, Mr. La Penna says. He suggests that they use the time to plan for the future.
“You need to have a plan for what you will do if this situation continues. When the risk is unknown, as is the case with this pandemic, people tend to plan for the best and fear the worst,” he said. “But it makes more sense to plan for the worst and hope for the best.”
Mr. La Penna advises practices to thoroughly analyze their operations. That analysis should include defining ongoing expenses and deciding how to handle them, developing a time-off policy for employees, and holding off on new hires and purchases.
He advises being transparent about your plans. “Be very public and forthcoming about the measures the practice is taking to avoid a complete shutdown, but keep your options open. Communicate with referral sources at every stage so that they stay in the loop.”
Procedure-oriented practices should follow the rules on elective procedures, Mr. La Penna says. “Conform to your association’s national guidelines on performing elective surgery or procedures,” he said. “If you do not follow those guidelines, you may be liable if your patient develops the virus.”
The AMA has compiled a list of actions to help keep your practice open. Here are some highlights:
- Determine the minimal cash flow you’d need. Develop a contingency plan based on estimates of minimum cash flow to stay afloat.
- Track your losses and expenses. You’ll need a record to make a claim through your business insurance policy. The policy may or may not cover COVID-19-related liabilities. Contact your broker to find out.
- Keep track of impending defaults. Review existing loan documents and financial covenants to determine whether a slowdown of business or collections could trigger a default.
- Negotiate with lenders. Contact vendors, landlords, and creditors to discuss reasonable accommodations for cash-flow disruptions. Consider asking them for forbearance, forgiveness, or a standstill, and agree to establish a process for keeping them informed over time.
- Get a low-interest loan. The Small Business Administration has begun to administer low-interest loans funded by numerous states, counties, and municipalities.
- Keep up with policy changes. State, local, and federal laws and regulations that affect practices are changing rapidly. Assign a staff member to follow these changes in the news and on government websites.
Closing your office may be the only option
Still, many practices may have to close – hopefully, most closures will be temporary, but some could end up being permanent.
“If you want to close your practice temporarily, you can get a short-term loan, try to defer payments, and wait for circumstances to improve,” Mr. La Penna said. “You’ll need to spend a few weeks winding down your practice, and you’ll want to make sure employees and patients don’t drift off.”
However, many practices may have no choice but to go permanently out of business, Mr. La Penna says.
The problem for many practices is that they typically distribute income among partners and have not retained earnings to cushion them from a financial disaster, Mr. Messinger says. “Some higher-performing practices have a cash surplus of perhaps 2 months, if that. They could take out loans and use lines of credit, but some of them already have outstanding loans for equipment or accounts receivables.”
Older physicians who were planning retirement may decide to retire early. “Anecdotally, there are a number of doctors who are ready to call it quits,” said Louis Weinstein, MD, chair of the AMA Senior Physicians Section. “This virus is the last straw. Their thought is: ‘Get out before you get sick.’ One colleague was going to close in a year from now but decided to speed it up.”
To find the specific steps needed to shut down a practice, check with physician organizations, practice managers, and health care attorneys. For example, the American Association of Family Physicians provides a Closing Your Practice Checklist, which specifies what you should do 60-90 days and 30-60 days before closing.
Employed physicians’ concerns
While private practices wrestle with staying open, there are potentially some grim or unhappy prospects for employed physicians too.
Many hospitals are in difficult economic straits and may not be able to afford paying doctors who aren’t working. But some experts are more optimistic.
“In many cases, I think the hospital will pay their salary even though their volume is down,” Mr. Mertz said. And Mr. Messinger said: “Hospitals may put employed physicians with low volume on an ‘RVU [relative value unit] holiday’ for a while. They don’t want to have a destabilized workforce.”
“When employed surgeons can’t do elective procedures, suddenly they can’t meet their productivity targets to get bonuses,” Mr. La Penna said. Productivity measures are typically based on RVUs. Mr. La Penna says he is working with a 100-physician practice where RVU payments that had been projected for the remainder of the year are expected to fall by half.
Some employed physicians have a guaranteed base pay that is not affected by RVUs, but in many cases, pay is based purely on productivity, says Andrew Hajde, assistant director of association content at the Medical Group Management Association. “If their volume goes down, they are in danger of not getting paid,” he said.
A version of this article originally appeared on Medscape.com.
Focus on factors that can be controlled during surgery for a good cosmetic result
ORLANDO – Some is to focus on those within a surgeon’s control, Robert H. Gotkin, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Patients often judge the surgeon by the appearance of the scar. Not fair, but that’s what happens,” said Dr. Gotkin, director of plastic surgery at a private practice in Greenvale, N.Y.
What’s in a surgeon’s control? An accurate diagnosis, operating plan, knowledge of relevant anatomy, surgical technique, and tools for managing and modulating scars, he noted. Achieving a good cosmetic outcome starts before surgery with proper surgical planning, which includes a backup plan on “how to get out of trouble.” Visualize the ideal outcome of surgery in three dimensions, and know the relevant anatomy to help with surgical marking, as well as relevant muscular and vascular anatomy, and motor nerve danger zones, he advised. When performing facial reconstruction, reconstruct defects using the cosmetic units of the face, and place scars at the borders of cosmetic units, if possible, he said.
An order of priorities during surgery is also important. In the same way a vending machine that spits out ingredients to make a coffee in the wrong order will not result in a cup of coffee, he said, the surgical plan must be in an order that makes sense.
Tension is “one of the greatest enemies in surgery,” Dr. Gotkin said. Too much tension on a closure, for example, can cut off the blood supply and result in tissue ischemia, which could result in infection and dehiscence. It’s important to know one’s limitations during surgery and when in doubt, not to perform the surgery, he added. “Never do today what you can put off until tomorrow, because a lot of things heal and get better on their own,” he said.
Tools for good surgical outcome
A surgeon performing dermatologic procedures needs an operating room with good lighting, and a set of sharp surgical instruments. Use needle holders that do not lock, and handle needles with instruments instead of your fingers to hold the needles with just the right amount of tension, Dr. Gotkin said.
“There is no question” that palming a needle holder should not be done, he added. “Granted, this is a little dogmatic, but there is no use for palming a needle holder in surgery. It makes you much less accurate.”
Suture material is another important consideration. Surgeons have their pick of braided or monofilament sutures available in absorbable and nonabsorbable material. Absorbable sutures are made with synthetic materials such as polyglactin 910 (Vicryl), poliglecaprone 25 (Monocryl) and polydioxanone (PDS), while nonabsorbable sutures include those manufactured with polypropylene (Prolene). Nonabsorbable suture materials made of polyester and stainless steel exist, but are not commonly used in dermatologic surgery, he said.
The most common needles Dr. Gotkin uses in his practice are the Ethicon P-3, P-1, PS-2, and PS-6 types for precision point reverse cutting, and the PC-1 and PC-3 types for precision cosmetic procedures. Other needles that have similar shapes are marketed under different names, he noted. For local anesthesia, surgeons can use either lidocaine hydrochloride with epinephrine, 1% (1:100,000 u) for a rapid-onset, short-acting effect, or bupivacaine hydrochloride with epinephrine, 0.5% (1:200,000 u) for a slower-onset, long-acting effect. Dr. Gotkin recommends using a combination of both in a half-half mixture (1:150,000 epinephrine) with a buffer of sodium bicarbonate since both are acidic. Instead of stretching the skin before inserting the needle, he advised pinching or rubbing the skin to distract the patient from the injection instead of stretching the skin. Small gauge needles (such as 30-gauge or 27-gauge) are best for administering local anesthetic, he said.
Factor patient health into planning
When planning surgery, consider a patient’s comorbidities, previous surgeries, as well as current medications; those include anticoagulants or systemic steroids, which can affect the outcome of surgery. For patients who have had previous surgeries, determine whether they had any surgical complications, or experienced adverse outcomes such as keloids, hypertrophic scars, or soft tissue infections.
When planning your surgical “roadmap,” the general area of the surgery can factor into how a wound heals. Consider the vascularity of local tissues, and any tension in local tissues that can increase tension on the skin such as in the scalp, the foot, the ankle, or the back. Use the patient’s relaxed skin tension lines to minimize scarring. Since they were developed while experimenting on cadavers, the Langer lines of skin tension are not always ideal to use, and Kraissl’s lines, developed by a plastic surgeon, are a better guide for surgical planning, Dr. Gotkin said.
He also advised placing surgical markers on a patient in the way they’ll be lying during surgery. “I always tell people to crosshatch the fusiform design before surgery, because once you make the incision, they may open up and everything gets distorted, particularly when a patient’s lying down,” he said. “We have to put these markings on while the patient is sitting. Then, when you put your sutures in, you can use those lines to line everything up, so that you end up with a scar that fits in how you designed it when the patient was upright.” The rule is a 3:1 or 4:1 ratio for length/width when designing a fusiform incision for excision of a lesion.
Incisions are made perpendicular to the surface of the skin instead of beveled. “Repair in tension” rather than layers, Dr. Gotkin said. “It’s important when you put a needle in the skin, pronate so that the needle goes in at 90 degrees from the skin surface,” he explained. “Follow the curve of the needle through and supinate as you’re putting the needle through. That way, you get the right amount of tension and the right amount of tissue in the grasp of the needle.”
When tying sutures, Dr. Gotkin said he uses a hand tie in addition to an instrument tie, everting the skin edges as he closes subcuticular and cuticular sutures.
During surgery, gentle handling of tissues with forceps that have teeth, rather than a smooth surface, will help avoid crushing the skin. “That’s very important in plastic surgery, and it’s very important in any surgical procedure that you do,” he said.
These technical factors are “completely under the control of the surgeon,” but above all, a good surgical plan following an accurate diagnosis is most likely to yield the best result for patients, Dr. Gotkin said. “An architect wouldn’t build a house without blueprints, so you have to do the same thing when you’re doing surgery.”
Dr. Gotkin reported no relevant financial disclosures.
ORLANDO – Some is to focus on those within a surgeon’s control, Robert H. Gotkin, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Patients often judge the surgeon by the appearance of the scar. Not fair, but that’s what happens,” said Dr. Gotkin, director of plastic surgery at a private practice in Greenvale, N.Y.
What’s in a surgeon’s control? An accurate diagnosis, operating plan, knowledge of relevant anatomy, surgical technique, and tools for managing and modulating scars, he noted. Achieving a good cosmetic outcome starts before surgery with proper surgical planning, which includes a backup plan on “how to get out of trouble.” Visualize the ideal outcome of surgery in three dimensions, and know the relevant anatomy to help with surgical marking, as well as relevant muscular and vascular anatomy, and motor nerve danger zones, he advised. When performing facial reconstruction, reconstruct defects using the cosmetic units of the face, and place scars at the borders of cosmetic units, if possible, he said.
An order of priorities during surgery is also important. In the same way a vending machine that spits out ingredients to make a coffee in the wrong order will not result in a cup of coffee, he said, the surgical plan must be in an order that makes sense.
Tension is “one of the greatest enemies in surgery,” Dr. Gotkin said. Too much tension on a closure, for example, can cut off the blood supply and result in tissue ischemia, which could result in infection and dehiscence. It’s important to know one’s limitations during surgery and when in doubt, not to perform the surgery, he added. “Never do today what you can put off until tomorrow, because a lot of things heal and get better on their own,” he said.
Tools for good surgical outcome
A surgeon performing dermatologic procedures needs an operating room with good lighting, and a set of sharp surgical instruments. Use needle holders that do not lock, and handle needles with instruments instead of your fingers to hold the needles with just the right amount of tension, Dr. Gotkin said.
“There is no question” that palming a needle holder should not be done, he added. “Granted, this is a little dogmatic, but there is no use for palming a needle holder in surgery. It makes you much less accurate.”
Suture material is another important consideration. Surgeons have their pick of braided or monofilament sutures available in absorbable and nonabsorbable material. Absorbable sutures are made with synthetic materials such as polyglactin 910 (Vicryl), poliglecaprone 25 (Monocryl) and polydioxanone (PDS), while nonabsorbable sutures include those manufactured with polypropylene (Prolene). Nonabsorbable suture materials made of polyester and stainless steel exist, but are not commonly used in dermatologic surgery, he said.
The most common needles Dr. Gotkin uses in his practice are the Ethicon P-3, P-1, PS-2, and PS-6 types for precision point reverse cutting, and the PC-1 and PC-3 types for precision cosmetic procedures. Other needles that have similar shapes are marketed under different names, he noted. For local anesthesia, surgeons can use either lidocaine hydrochloride with epinephrine, 1% (1:100,000 u) for a rapid-onset, short-acting effect, or bupivacaine hydrochloride with epinephrine, 0.5% (1:200,000 u) for a slower-onset, long-acting effect. Dr. Gotkin recommends using a combination of both in a half-half mixture (1:150,000 epinephrine) with a buffer of sodium bicarbonate since both are acidic. Instead of stretching the skin before inserting the needle, he advised pinching or rubbing the skin to distract the patient from the injection instead of stretching the skin. Small gauge needles (such as 30-gauge or 27-gauge) are best for administering local anesthetic, he said.
Factor patient health into planning
When planning surgery, consider a patient’s comorbidities, previous surgeries, as well as current medications; those include anticoagulants or systemic steroids, which can affect the outcome of surgery. For patients who have had previous surgeries, determine whether they had any surgical complications, or experienced adverse outcomes such as keloids, hypertrophic scars, or soft tissue infections.
When planning your surgical “roadmap,” the general area of the surgery can factor into how a wound heals. Consider the vascularity of local tissues, and any tension in local tissues that can increase tension on the skin such as in the scalp, the foot, the ankle, or the back. Use the patient’s relaxed skin tension lines to minimize scarring. Since they were developed while experimenting on cadavers, the Langer lines of skin tension are not always ideal to use, and Kraissl’s lines, developed by a plastic surgeon, are a better guide for surgical planning, Dr. Gotkin said.
He also advised placing surgical markers on a patient in the way they’ll be lying during surgery. “I always tell people to crosshatch the fusiform design before surgery, because once you make the incision, they may open up and everything gets distorted, particularly when a patient’s lying down,” he said. “We have to put these markings on while the patient is sitting. Then, when you put your sutures in, you can use those lines to line everything up, so that you end up with a scar that fits in how you designed it when the patient was upright.” The rule is a 3:1 or 4:1 ratio for length/width when designing a fusiform incision for excision of a lesion.
Incisions are made perpendicular to the surface of the skin instead of beveled. “Repair in tension” rather than layers, Dr. Gotkin said. “It’s important when you put a needle in the skin, pronate so that the needle goes in at 90 degrees from the skin surface,” he explained. “Follow the curve of the needle through and supinate as you’re putting the needle through. That way, you get the right amount of tension and the right amount of tissue in the grasp of the needle.”
When tying sutures, Dr. Gotkin said he uses a hand tie in addition to an instrument tie, everting the skin edges as he closes subcuticular and cuticular sutures.
During surgery, gentle handling of tissues with forceps that have teeth, rather than a smooth surface, will help avoid crushing the skin. “That’s very important in plastic surgery, and it’s very important in any surgical procedure that you do,” he said.
These technical factors are “completely under the control of the surgeon,” but above all, a good surgical plan following an accurate diagnosis is most likely to yield the best result for patients, Dr. Gotkin said. “An architect wouldn’t build a house without blueprints, so you have to do the same thing when you’re doing surgery.”
Dr. Gotkin reported no relevant financial disclosures.
ORLANDO – Some is to focus on those within a surgeon’s control, Robert H. Gotkin, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Patients often judge the surgeon by the appearance of the scar. Not fair, but that’s what happens,” said Dr. Gotkin, director of plastic surgery at a private practice in Greenvale, N.Y.
What’s in a surgeon’s control? An accurate diagnosis, operating plan, knowledge of relevant anatomy, surgical technique, and tools for managing and modulating scars, he noted. Achieving a good cosmetic outcome starts before surgery with proper surgical planning, which includes a backup plan on “how to get out of trouble.” Visualize the ideal outcome of surgery in three dimensions, and know the relevant anatomy to help with surgical marking, as well as relevant muscular and vascular anatomy, and motor nerve danger zones, he advised. When performing facial reconstruction, reconstruct defects using the cosmetic units of the face, and place scars at the borders of cosmetic units, if possible, he said.
An order of priorities during surgery is also important. In the same way a vending machine that spits out ingredients to make a coffee in the wrong order will not result in a cup of coffee, he said, the surgical plan must be in an order that makes sense.
Tension is “one of the greatest enemies in surgery,” Dr. Gotkin said. Too much tension on a closure, for example, can cut off the blood supply and result in tissue ischemia, which could result in infection and dehiscence. It’s important to know one’s limitations during surgery and when in doubt, not to perform the surgery, he added. “Never do today what you can put off until tomorrow, because a lot of things heal and get better on their own,” he said.
Tools for good surgical outcome
A surgeon performing dermatologic procedures needs an operating room with good lighting, and a set of sharp surgical instruments. Use needle holders that do not lock, and handle needles with instruments instead of your fingers to hold the needles with just the right amount of tension, Dr. Gotkin said.
“There is no question” that palming a needle holder should not be done, he added. “Granted, this is a little dogmatic, but there is no use for palming a needle holder in surgery. It makes you much less accurate.”
Suture material is another important consideration. Surgeons have their pick of braided or monofilament sutures available in absorbable and nonabsorbable material. Absorbable sutures are made with synthetic materials such as polyglactin 910 (Vicryl), poliglecaprone 25 (Monocryl) and polydioxanone (PDS), while nonabsorbable sutures include those manufactured with polypropylene (Prolene). Nonabsorbable suture materials made of polyester and stainless steel exist, but are not commonly used in dermatologic surgery, he said.
The most common needles Dr. Gotkin uses in his practice are the Ethicon P-3, P-1, PS-2, and PS-6 types for precision point reverse cutting, and the PC-1 and PC-3 types for precision cosmetic procedures. Other needles that have similar shapes are marketed under different names, he noted. For local anesthesia, surgeons can use either lidocaine hydrochloride with epinephrine, 1% (1:100,000 u) for a rapid-onset, short-acting effect, or bupivacaine hydrochloride with epinephrine, 0.5% (1:200,000 u) for a slower-onset, long-acting effect. Dr. Gotkin recommends using a combination of both in a half-half mixture (1:150,000 epinephrine) with a buffer of sodium bicarbonate since both are acidic. Instead of stretching the skin before inserting the needle, he advised pinching or rubbing the skin to distract the patient from the injection instead of stretching the skin. Small gauge needles (such as 30-gauge or 27-gauge) are best for administering local anesthetic, he said.
Factor patient health into planning
When planning surgery, consider a patient’s comorbidities, previous surgeries, as well as current medications; those include anticoagulants or systemic steroids, which can affect the outcome of surgery. For patients who have had previous surgeries, determine whether they had any surgical complications, or experienced adverse outcomes such as keloids, hypertrophic scars, or soft tissue infections.
When planning your surgical “roadmap,” the general area of the surgery can factor into how a wound heals. Consider the vascularity of local tissues, and any tension in local tissues that can increase tension on the skin such as in the scalp, the foot, the ankle, or the back. Use the patient’s relaxed skin tension lines to minimize scarring. Since they were developed while experimenting on cadavers, the Langer lines of skin tension are not always ideal to use, and Kraissl’s lines, developed by a plastic surgeon, are a better guide for surgical planning, Dr. Gotkin said.
He also advised placing surgical markers on a patient in the way they’ll be lying during surgery. “I always tell people to crosshatch the fusiform design before surgery, because once you make the incision, they may open up and everything gets distorted, particularly when a patient’s lying down,” he said. “We have to put these markings on while the patient is sitting. Then, when you put your sutures in, you can use those lines to line everything up, so that you end up with a scar that fits in how you designed it when the patient was upright.” The rule is a 3:1 or 4:1 ratio for length/width when designing a fusiform incision for excision of a lesion.
Incisions are made perpendicular to the surface of the skin instead of beveled. “Repair in tension” rather than layers, Dr. Gotkin said. “It’s important when you put a needle in the skin, pronate so that the needle goes in at 90 degrees from the skin surface,” he explained. “Follow the curve of the needle through and supinate as you’re putting the needle through. That way, you get the right amount of tension and the right amount of tissue in the grasp of the needle.”
When tying sutures, Dr. Gotkin said he uses a hand tie in addition to an instrument tie, everting the skin edges as he closes subcuticular and cuticular sutures.
During surgery, gentle handling of tissues with forceps that have teeth, rather than a smooth surface, will help avoid crushing the skin. “That’s very important in plastic surgery, and it’s very important in any surgical procedure that you do,” he said.
These technical factors are “completely under the control of the surgeon,” but above all, a good surgical plan following an accurate diagnosis is most likely to yield the best result for patients, Dr. Gotkin said. “An architect wouldn’t build a house without blueprints, so you have to do the same thing when you’re doing surgery.”
Dr. Gotkin reported no relevant financial disclosures.
EXPERT ANALYSIS FROM ODAC 2020
An Unusual Presentation of Calciphylaxis
To the Editor:
Calciphylaxis (also known as calcific uremic arteriolopathy and calcifying panniculitis) is a rare vasculopathy affecting the small vessels.1 It is characterized by cutaneous ischemia and necrosis secondary to calcification. It is most commonly seen in patients with end-stage renal disease (ESRD) and hyperparathyroidism.1-3 Histopathologic features that are consistent with the diagnosis of calciphylaxis include calcification of medium-sized vessels in the deep dermis or subcutaneous fat as well as smaller distal vessels that supply the papillary dermis and epidermis.4,5 Although it commonly presents as well-demarcated, painful, purplish lesions that evolve into necrotic eschars, calciphylaxis rarely can present with hemorrhagic or serous bullous lesions followed by ulceration, as was seen in our patient.1,5,6 We report this uncommon presentation to highlight the variety in clinical appearance of calciphylaxis and the importance of early diagnosis.
A 43-year-old woman presented to the emergency department for evaluation of chest and abdominal pain that began 1 day prior to presentation. She had a history of systemic lupus erythematosus and ESRD secondary to poststreptococcal glomerulonephritis and was currently on peritoneal dialysis. The patient was admitted for peritonitis and treated with broad-spectrum antibiotics. At the time of admission, the patient also was noted to have several painful bullae on the legs. Her medical history also was remarkable for cerebral infarction, fibromyalgia, cerebral artery occlusion with cerebral infarction, sciatica, hyperlipidemia, deep vein thrombosis, and seizures. She had no history of herpes simplex virus. Surgical history was remarkable for tubal ligation, nephrectomy and kidney transplant, parathyroidectomy, and cholecystectomy. The patient’s medications included sevelamer carbonate, prednisone, epogen, calcium carbonate, esomeprazole, ondansetron, topical gentamicin, and atorvastatin.
Skin examination was performed by the inpatient dermatology service and revealed several tense, 1- to 5-cm, nonhemorrhagic bullae on the thighs and lower legs, some that had ruptured. The lesions were notably tender to palpation. No surrounding erythema, ecchymosis, or warmth was appreciated. The Nikolsky sign was negative. The patient also was noted to have at least grade 2 to 3+ pitting edema of the bilateral legs. The oral and conjunctival mucosae were unremarkable.
Antinuclear antibody, double-stranded DNA, and anti-Smith antibody levels were negative. A punch biopsy of the left lateral thigh revealed intraepidermal vesicular dermatitis with dermal edema suggestive of edema bullae and direct immunofluorescence was negative for immune complex and complement deposition.
Conservative therapy with wound care was recommended. The patient continued to report persistent severe skin pain and developed a subcutaneous nodule on the right inner thigh 1 week later, prompting a second biopsy. Results of the excisional biopsy were nondiagnostic but were suggestive of calciphylaxis, revealing subepidermal bullae with epidermal necrosis, a scant perivascular lymphocytic infiltrate, and extravasated erythrocytes. No evidence of calcification was seen within the vessels. The patient was then started on sodium thiosulfate with hemodialysis for treatment of presumed calciphylaxis.
Despite meticulous wound care and treatment with sodium thiosulfate, the patient developed ulcerations with necrotic eschars on the bilateral buttocks, hips, and thighs 1 month later (Figure 1). She subsequently worsened over the next few weeks. She developed sepsis and was transferred to the intensive care unit. A third biopsy was performed, finally confirming the diagnosis of calciphylaxis. Histopathology revealed small blood vessels with basophilic granular deposits in the walls consistent with calcium in the subcutaneous tissue (highlighted with the von Kossa stain), as well as thrombi in the lumens of some vessels; early fat necrosis; focal epidermal necrosis with underlying congested blood vessels with deposits in their walls; a perivascular infiltrate predominately of lymphocytes and neutrophils with scattered nuclear dust; and thick, hyalinized, closely crowded collagen bundles in the reticular dermis and in a widened subcutaneous septum (Figures 2 and 3).
Supportive care and pain control were continued, but the overall prognosis was determined to be very poor, and the patient eventually was discharged to hospice and died.
Although calciphylaxis is commonly seen in patients with ESRD and hyperparathyroidism, patients without renal disease also may develop the condition.2,3 Prior epidemiologic studies have shown a prevalence of 1% in patients with chronic kidney disease and up to 4% in those receiving dialysis.2-5 The average age at presentation is 48 years.6,7 Although calciphylaxis has been noted to affect males and females equally, some studies have suggested a female predominance.5-8
The etiology of calciphylaxis is unknown, but ESRD requiring dialysis, primary or secondary hyperparathyroidism, obesity, diabetes mellitus, skin trauma, and/or a hypercoagulable state may put patients at increased risk for developing this disease.2,3 Other risk factors include systemic corticosteroids, liver disease, increased serum aluminum, and increased erythrocyte sedimentation rate. Although high calcium-phosphate product has been noted as a risk factor in prior studies, one retrospective study found that it does not reliably confirm or exclude a diagnosis of calciphylaxis.8
The pathogenesis of calciphylaxis is not well understood; however, some researchers suggest that an imbalance in calcium-phosphate homeostasis may lead to calciphylaxis; that is, elevated calcium and phosphate levels exceed their solubility and deposit in the walls of small- and medium-sized arteries, which consequently leads to ischemic necrosis and gangrene of the surrounding tissue.9
Clinically, calciphylaxis has an indolent onset and usually presents as well-demarcated, painful, purplish, mottled lesions that evolve into necrotic gray-black eschars and gangrene in adjacent tissues.1,5,6 The ischemic process may even extend to the muscle layer.5 Other common presentations include mild erythematous patches; livedo reticularis; painful nodules; necrotic ulcerating lesions; and more rarely flaccid, hemorrhagic, or serous bullous lesions followed by ulceration, as was seen in our patient.6,9,10 Lesions usually begin at sites of trauma and seem to be distributed symmetrically.5,6 The most commonly affected locations are the legs, specifically the medial thighs, as well as the abdomen and buttocks, but lesions also can be found at more distal sites such as the breasts, tongue, vulva, penis, fingers, and toes.5,6,10 The head and neck region rarely is affected. Although uncommon, calciphylaxis may affect other organs, including the lungs, stomach, kidneys, and adrenal glands.5 The accompanying systemic symptoms and findings may include muscle weakness, tenderness, or myositis with rhabdomyolysis; calcific cerebral embolism; dementia and infarction of the central nervous system; acute respiratory failure; heart disease; atrioventricular block; and calcification of the cardiac conduction system.6 Unlike other forms of peripheral vascular disease, distal pulses are present in calciphylaxis, as blood flow usually is preserved distal and deep to the areas of necrosis.5,6
A careful history and thorough physical examination are important first steps in the diagnosis of this condition.2,10 Although there are no definitive laboratory tests, elevated serum calcium, phosphorous, and calcium-phosphate product levels, as well as parathyroid hormone level, may be suggestive of calciphylaxis.2,5 Leukocytosis may occur if an infection is present.5
The most accurate method to confirm the diagnosis is a deep incisional biopsy from an erythematous, slightly purpuric area adjacent to the necrotic lesion.2,10,11 The histopathologic features used to make the diagnosis include calcification of medium-sized vessels, particularly the intimal or medial layers, in the deep dermis and subcutaneous fat in addition to lobular capillaries of the subcutaneous fat.5,10 These vessels, including the smaller distal vessels that supply the papillary dermis and epidermis, also may be thrombosed due to calcification, leading to vascular occlusion and subsequently ischemic necrosis of the overlying epidermis.10 Other findings may include pseudoxanthoma elasticum changes, panniculitis, and subcutaneous fat necrosis.4,10
The differential diagnosis for calciphylaxis includes peripheral vascular disease, vasculitis, juvenile dermatomyositis, proteins C and S deficiencies, cryofibrinogenemia, calcinosis cutis, and tumoral calcinosis.2 Polyarteritis nodosa, Sjögren syndrome, atherosclerotic peripheral vascular disease, pyoderma gangrenosum, systemic lupus erythematosus, necrotizing fasciitis, septic embolism, and necrosis secondary to warfarin and heparin may mimic calciphylaxis.5
Treatment of calciphylaxis is multidimensional but primarily is supportive.6,11 Controlling calcium and phosphate levels and secondary hyperparathyroidism through diet and phosphate binders (eg, sevelamer hydrochloride) has been shown to be effective.6 Pamidronate, a bisphosphonate, inhibits arterial calcification in animal models and has been reported to treat calciphylaxis, resulting in marked pain reduction and ulcer healing.4,6 Cinacalcet, which functions as a calcimimetic, has been implicated in the treatment of calciphylaxis. It has been used to treat primary and secondary hyperparathyroidism and to normalize serum calcium levels; it also may be used as an alternative to parathyroidectomy.4,6 Intravenous administration of sodium thiosulfate, a potent antioxidant and chelator of calcium, has been helpful in reversing signs and symptoms of calciphylaxis.6,12 It also has been shown to effectively remove extra calcium during peritoneal dialysis.6 Parathyroidectomy has been useful in patients with markedly elevated parathyroid hormone levels, as it suppresses or eliminates the sensitizing agent causing hypercalcemia, elevated calcium-phosphate product, and hyperparathyroidism.1,2,6,13
Wound care and prevention of sepsis are essential in the treatment of calciphylaxis. Management options include surgical debridement, hydrocolloid and biologic dressings, skin grafts, systemic antibiotics, oral pentoxifylline combined with maggot therapy, nutritional support, hyperbaric oxygen therapy, and revascularization and amputation when other interventions have failed. Pain control with analgesics and correction of thrombosis in the skin and blood vessels via anticoagulation therapy also are important complementary treatments.6
The clinical outcome of calciphylaxis is dependent on early diagnosis, antimicrobial therapy, and wound management,9 but overall, the prognosis usually is poor and has a high mortality rate. The most common causes of death are infection and sepsis.1,9 A study of 7 cases reported 100% mortality,14 but other studies have suggested a mortality rate of 60% to 80%.4,10 Female sex and obesity are poor prognostic indicators.2 A better prognosis has been appreciated in cases in which lesions occur at distal sites (eg, lower legs, hands) compared to more proximal sites (eg, abdomen), where 25% and 75% mortalities have been noted, respectively.10,14,15 In one study, the overall mortality rate was 45% in patients with calciphylaxis at 1 year.6 The rate was 41% in patients with plaques only and 67% in those who presented with ulceration. Patients who survive often experience a high degree of morbidity and prolonged hospitalization; these patients often are severely debilitated, especially in the case of limb amputation.6
Our report of calciphylaxis demonstrates the diversity in clinical presentation and emphasizes the importance of early and accurate diagnosis in reducing morbidity and mortality. In our case, the patient presented with skin pain and tense nonhemorrhagic bullae without underlying ecchymotic or erythematous lesions as the earliest sign of calciphylaxis. Physicians should have a high degree of suspicion in the setting of dialysis-dependent ESRD patients with bullae, extreme pain, and continuous decline. We hope that this case will help increase awareness of the varying presentations of this condition.
- Hanafusa T, Yamaguchi Y, Tani M, et al. Intractable wounds caused by calcific uremic arteriolopathy treated with bisphosphonates. J Am Acad Dermatol. 2001;57:1021-1025.
- Somorin AO, Harbi AA, Subaity Y, et al. Calciphylaxis: case report and literature review. Afr J Med Sci. 2002;31:175-178.
- Barreiros HM, Goulão J, Cunha H, et al. Calciphylaxis: a diagnostic and therapeutic challenge. J Dermatol Case Rep. 2013;2:69-70.
- Vedvyas C, Winterfield LS, Vleugels RA. Calciphylaxis: a systematic review of existing and emerging therapies. J Am Acad Dermatol. 2012;67:E253-E260.
- Beitz JM. Calciphylaxis: a case study with differential diagnosis. Ostomy Wound Manag. 2003;49:28-38.
- Daudén E, Oñate M. Calciphylaxis. Dermatol Clin. 2008;26:557-568.
- Oh DH, Eulau D, Tokugawa DA, et al. Five cases of calciphylaxis and a review of the literature. J Am Acad Dermatol. 1999;40:979-987.
- Weenig RH, Sewell LD, Davis MDP, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-578.
- Hanvesakul R, Silva MA, Hejmadi R, et al. Calciphylaxis following kidney transplantation: a case report. J Med Cases. 2009;3:9297.
- Kouba DJ, Owens NM, Barrett TL, et al. An unusual case of calciphylaxis. J Cutan Med Surg. 2004;8:19-22.
- Arch-Ferrer JE, Beenken SW, Rue LW, et al. Therapy for calciphylaxis: an outcome analysis. Surgery. 2003;134:941-945.
- Cicone JS, Petronis JB, Embert CD, et al. Successful treatment of calciphylaxis with intravenous sodium thiosulfate. Am J Kidney Dis. 2004;43:1104-1108.
- Mirza I, Chaubay D, Gunderia H, et al. An unusual presentation of calciphylaxis due to primary hyperparathyroidism. Arch Pathol Lab Med. 2001;125:1351-1353.
- Alain J, Poulin YP, Cloutier RA, et al. Calciphylaxis: seven new cases. J Cutan Med Surg. 2000;4:213-218.
- Hafner J, Keusch G, Wahl C, et al. Calciphylaxis: a syndrome of skin necrosis and acral gangrene in chronic renal failure. Vasa. 1998;27:137-143.
To the Editor:
Calciphylaxis (also known as calcific uremic arteriolopathy and calcifying panniculitis) is a rare vasculopathy affecting the small vessels.1 It is characterized by cutaneous ischemia and necrosis secondary to calcification. It is most commonly seen in patients with end-stage renal disease (ESRD) and hyperparathyroidism.1-3 Histopathologic features that are consistent with the diagnosis of calciphylaxis include calcification of medium-sized vessels in the deep dermis or subcutaneous fat as well as smaller distal vessels that supply the papillary dermis and epidermis.4,5 Although it commonly presents as well-demarcated, painful, purplish lesions that evolve into necrotic eschars, calciphylaxis rarely can present with hemorrhagic or serous bullous lesions followed by ulceration, as was seen in our patient.1,5,6 We report this uncommon presentation to highlight the variety in clinical appearance of calciphylaxis and the importance of early diagnosis.
A 43-year-old woman presented to the emergency department for evaluation of chest and abdominal pain that began 1 day prior to presentation. She had a history of systemic lupus erythematosus and ESRD secondary to poststreptococcal glomerulonephritis and was currently on peritoneal dialysis. The patient was admitted for peritonitis and treated with broad-spectrum antibiotics. At the time of admission, the patient also was noted to have several painful bullae on the legs. Her medical history also was remarkable for cerebral infarction, fibromyalgia, cerebral artery occlusion with cerebral infarction, sciatica, hyperlipidemia, deep vein thrombosis, and seizures. She had no history of herpes simplex virus. Surgical history was remarkable for tubal ligation, nephrectomy and kidney transplant, parathyroidectomy, and cholecystectomy. The patient’s medications included sevelamer carbonate, prednisone, epogen, calcium carbonate, esomeprazole, ondansetron, topical gentamicin, and atorvastatin.
Skin examination was performed by the inpatient dermatology service and revealed several tense, 1- to 5-cm, nonhemorrhagic bullae on the thighs and lower legs, some that had ruptured. The lesions were notably tender to palpation. No surrounding erythema, ecchymosis, or warmth was appreciated. The Nikolsky sign was negative. The patient also was noted to have at least grade 2 to 3+ pitting edema of the bilateral legs. The oral and conjunctival mucosae were unremarkable.
Antinuclear antibody, double-stranded DNA, and anti-Smith antibody levels were negative. A punch biopsy of the left lateral thigh revealed intraepidermal vesicular dermatitis with dermal edema suggestive of edema bullae and direct immunofluorescence was negative for immune complex and complement deposition.
Conservative therapy with wound care was recommended. The patient continued to report persistent severe skin pain and developed a subcutaneous nodule on the right inner thigh 1 week later, prompting a second biopsy. Results of the excisional biopsy were nondiagnostic but were suggestive of calciphylaxis, revealing subepidermal bullae with epidermal necrosis, a scant perivascular lymphocytic infiltrate, and extravasated erythrocytes. No evidence of calcification was seen within the vessels. The patient was then started on sodium thiosulfate with hemodialysis for treatment of presumed calciphylaxis.
Despite meticulous wound care and treatment with sodium thiosulfate, the patient developed ulcerations with necrotic eschars on the bilateral buttocks, hips, and thighs 1 month later (Figure 1). She subsequently worsened over the next few weeks. She developed sepsis and was transferred to the intensive care unit. A third biopsy was performed, finally confirming the diagnosis of calciphylaxis. Histopathology revealed small blood vessels with basophilic granular deposits in the walls consistent with calcium in the subcutaneous tissue (highlighted with the von Kossa stain), as well as thrombi in the lumens of some vessels; early fat necrosis; focal epidermal necrosis with underlying congested blood vessels with deposits in their walls; a perivascular infiltrate predominately of lymphocytes and neutrophils with scattered nuclear dust; and thick, hyalinized, closely crowded collagen bundles in the reticular dermis and in a widened subcutaneous septum (Figures 2 and 3).
Supportive care and pain control were continued, but the overall prognosis was determined to be very poor, and the patient eventually was discharged to hospice and died.
Although calciphylaxis is commonly seen in patients with ESRD and hyperparathyroidism, patients without renal disease also may develop the condition.2,3 Prior epidemiologic studies have shown a prevalence of 1% in patients with chronic kidney disease and up to 4% in those receiving dialysis.2-5 The average age at presentation is 48 years.6,7 Although calciphylaxis has been noted to affect males and females equally, some studies have suggested a female predominance.5-8
The etiology of calciphylaxis is unknown, but ESRD requiring dialysis, primary or secondary hyperparathyroidism, obesity, diabetes mellitus, skin trauma, and/or a hypercoagulable state may put patients at increased risk for developing this disease.2,3 Other risk factors include systemic corticosteroids, liver disease, increased serum aluminum, and increased erythrocyte sedimentation rate. Although high calcium-phosphate product has been noted as a risk factor in prior studies, one retrospective study found that it does not reliably confirm or exclude a diagnosis of calciphylaxis.8
The pathogenesis of calciphylaxis is not well understood; however, some researchers suggest that an imbalance in calcium-phosphate homeostasis may lead to calciphylaxis; that is, elevated calcium and phosphate levels exceed their solubility and deposit in the walls of small- and medium-sized arteries, which consequently leads to ischemic necrosis and gangrene of the surrounding tissue.9
Clinically, calciphylaxis has an indolent onset and usually presents as well-demarcated, painful, purplish, mottled lesions that evolve into necrotic gray-black eschars and gangrene in adjacent tissues.1,5,6 The ischemic process may even extend to the muscle layer.5 Other common presentations include mild erythematous patches; livedo reticularis; painful nodules; necrotic ulcerating lesions; and more rarely flaccid, hemorrhagic, or serous bullous lesions followed by ulceration, as was seen in our patient.6,9,10 Lesions usually begin at sites of trauma and seem to be distributed symmetrically.5,6 The most commonly affected locations are the legs, specifically the medial thighs, as well as the abdomen and buttocks, but lesions also can be found at more distal sites such as the breasts, tongue, vulva, penis, fingers, and toes.5,6,10 The head and neck region rarely is affected. Although uncommon, calciphylaxis may affect other organs, including the lungs, stomach, kidneys, and adrenal glands.5 The accompanying systemic symptoms and findings may include muscle weakness, tenderness, or myositis with rhabdomyolysis; calcific cerebral embolism; dementia and infarction of the central nervous system; acute respiratory failure; heart disease; atrioventricular block; and calcification of the cardiac conduction system.6 Unlike other forms of peripheral vascular disease, distal pulses are present in calciphylaxis, as blood flow usually is preserved distal and deep to the areas of necrosis.5,6
A careful history and thorough physical examination are important first steps in the diagnosis of this condition.2,10 Although there are no definitive laboratory tests, elevated serum calcium, phosphorous, and calcium-phosphate product levels, as well as parathyroid hormone level, may be suggestive of calciphylaxis.2,5 Leukocytosis may occur if an infection is present.5
The most accurate method to confirm the diagnosis is a deep incisional biopsy from an erythematous, slightly purpuric area adjacent to the necrotic lesion.2,10,11 The histopathologic features used to make the diagnosis include calcification of medium-sized vessels, particularly the intimal or medial layers, in the deep dermis and subcutaneous fat in addition to lobular capillaries of the subcutaneous fat.5,10 These vessels, including the smaller distal vessels that supply the papillary dermis and epidermis, also may be thrombosed due to calcification, leading to vascular occlusion and subsequently ischemic necrosis of the overlying epidermis.10 Other findings may include pseudoxanthoma elasticum changes, panniculitis, and subcutaneous fat necrosis.4,10
The differential diagnosis for calciphylaxis includes peripheral vascular disease, vasculitis, juvenile dermatomyositis, proteins C and S deficiencies, cryofibrinogenemia, calcinosis cutis, and tumoral calcinosis.2 Polyarteritis nodosa, Sjögren syndrome, atherosclerotic peripheral vascular disease, pyoderma gangrenosum, systemic lupus erythematosus, necrotizing fasciitis, septic embolism, and necrosis secondary to warfarin and heparin may mimic calciphylaxis.5
Treatment of calciphylaxis is multidimensional but primarily is supportive.6,11 Controlling calcium and phosphate levels and secondary hyperparathyroidism through diet and phosphate binders (eg, sevelamer hydrochloride) has been shown to be effective.6 Pamidronate, a bisphosphonate, inhibits arterial calcification in animal models and has been reported to treat calciphylaxis, resulting in marked pain reduction and ulcer healing.4,6 Cinacalcet, which functions as a calcimimetic, has been implicated in the treatment of calciphylaxis. It has been used to treat primary and secondary hyperparathyroidism and to normalize serum calcium levels; it also may be used as an alternative to parathyroidectomy.4,6 Intravenous administration of sodium thiosulfate, a potent antioxidant and chelator of calcium, has been helpful in reversing signs and symptoms of calciphylaxis.6,12 It also has been shown to effectively remove extra calcium during peritoneal dialysis.6 Parathyroidectomy has been useful in patients with markedly elevated parathyroid hormone levels, as it suppresses or eliminates the sensitizing agent causing hypercalcemia, elevated calcium-phosphate product, and hyperparathyroidism.1,2,6,13
Wound care and prevention of sepsis are essential in the treatment of calciphylaxis. Management options include surgical debridement, hydrocolloid and biologic dressings, skin grafts, systemic antibiotics, oral pentoxifylline combined with maggot therapy, nutritional support, hyperbaric oxygen therapy, and revascularization and amputation when other interventions have failed. Pain control with analgesics and correction of thrombosis in the skin and blood vessels via anticoagulation therapy also are important complementary treatments.6
The clinical outcome of calciphylaxis is dependent on early diagnosis, antimicrobial therapy, and wound management,9 but overall, the prognosis usually is poor and has a high mortality rate. The most common causes of death are infection and sepsis.1,9 A study of 7 cases reported 100% mortality,14 but other studies have suggested a mortality rate of 60% to 80%.4,10 Female sex and obesity are poor prognostic indicators.2 A better prognosis has been appreciated in cases in which lesions occur at distal sites (eg, lower legs, hands) compared to more proximal sites (eg, abdomen), where 25% and 75% mortalities have been noted, respectively.10,14,15 In one study, the overall mortality rate was 45% in patients with calciphylaxis at 1 year.6 The rate was 41% in patients with plaques only and 67% in those who presented with ulceration. Patients who survive often experience a high degree of morbidity and prolonged hospitalization; these patients often are severely debilitated, especially in the case of limb amputation.6
Our report of calciphylaxis demonstrates the diversity in clinical presentation and emphasizes the importance of early and accurate diagnosis in reducing morbidity and mortality. In our case, the patient presented with skin pain and tense nonhemorrhagic bullae without underlying ecchymotic or erythematous lesions as the earliest sign of calciphylaxis. Physicians should have a high degree of suspicion in the setting of dialysis-dependent ESRD patients with bullae, extreme pain, and continuous decline. We hope that this case will help increase awareness of the varying presentations of this condition.
To the Editor:
Calciphylaxis (also known as calcific uremic arteriolopathy and calcifying panniculitis) is a rare vasculopathy affecting the small vessels.1 It is characterized by cutaneous ischemia and necrosis secondary to calcification. It is most commonly seen in patients with end-stage renal disease (ESRD) and hyperparathyroidism.1-3 Histopathologic features that are consistent with the diagnosis of calciphylaxis include calcification of medium-sized vessels in the deep dermis or subcutaneous fat as well as smaller distal vessels that supply the papillary dermis and epidermis.4,5 Although it commonly presents as well-demarcated, painful, purplish lesions that evolve into necrotic eschars, calciphylaxis rarely can present with hemorrhagic or serous bullous lesions followed by ulceration, as was seen in our patient.1,5,6 We report this uncommon presentation to highlight the variety in clinical appearance of calciphylaxis and the importance of early diagnosis.
A 43-year-old woman presented to the emergency department for evaluation of chest and abdominal pain that began 1 day prior to presentation. She had a history of systemic lupus erythematosus and ESRD secondary to poststreptococcal glomerulonephritis and was currently on peritoneal dialysis. The patient was admitted for peritonitis and treated with broad-spectrum antibiotics. At the time of admission, the patient also was noted to have several painful bullae on the legs. Her medical history also was remarkable for cerebral infarction, fibromyalgia, cerebral artery occlusion with cerebral infarction, sciatica, hyperlipidemia, deep vein thrombosis, and seizures. She had no history of herpes simplex virus. Surgical history was remarkable for tubal ligation, nephrectomy and kidney transplant, parathyroidectomy, and cholecystectomy. The patient’s medications included sevelamer carbonate, prednisone, epogen, calcium carbonate, esomeprazole, ondansetron, topical gentamicin, and atorvastatin.
Skin examination was performed by the inpatient dermatology service and revealed several tense, 1- to 5-cm, nonhemorrhagic bullae on the thighs and lower legs, some that had ruptured. The lesions were notably tender to palpation. No surrounding erythema, ecchymosis, or warmth was appreciated. The Nikolsky sign was negative. The patient also was noted to have at least grade 2 to 3+ pitting edema of the bilateral legs. The oral and conjunctival mucosae were unremarkable.
Antinuclear antibody, double-stranded DNA, and anti-Smith antibody levels were negative. A punch biopsy of the left lateral thigh revealed intraepidermal vesicular dermatitis with dermal edema suggestive of edema bullae and direct immunofluorescence was negative for immune complex and complement deposition.
Conservative therapy with wound care was recommended. The patient continued to report persistent severe skin pain and developed a subcutaneous nodule on the right inner thigh 1 week later, prompting a second biopsy. Results of the excisional biopsy were nondiagnostic but were suggestive of calciphylaxis, revealing subepidermal bullae with epidermal necrosis, a scant perivascular lymphocytic infiltrate, and extravasated erythrocytes. No evidence of calcification was seen within the vessels. The patient was then started on sodium thiosulfate with hemodialysis for treatment of presumed calciphylaxis.
Despite meticulous wound care and treatment with sodium thiosulfate, the patient developed ulcerations with necrotic eschars on the bilateral buttocks, hips, and thighs 1 month later (Figure 1). She subsequently worsened over the next few weeks. She developed sepsis and was transferred to the intensive care unit. A third biopsy was performed, finally confirming the diagnosis of calciphylaxis. Histopathology revealed small blood vessels with basophilic granular deposits in the walls consistent with calcium in the subcutaneous tissue (highlighted with the von Kossa stain), as well as thrombi in the lumens of some vessels; early fat necrosis; focal epidermal necrosis with underlying congested blood vessels with deposits in their walls; a perivascular infiltrate predominately of lymphocytes and neutrophils with scattered nuclear dust; and thick, hyalinized, closely crowded collagen bundles in the reticular dermis and in a widened subcutaneous septum (Figures 2 and 3).
Supportive care and pain control were continued, but the overall prognosis was determined to be very poor, and the patient eventually was discharged to hospice and died.
Although calciphylaxis is commonly seen in patients with ESRD and hyperparathyroidism, patients without renal disease also may develop the condition.2,3 Prior epidemiologic studies have shown a prevalence of 1% in patients with chronic kidney disease and up to 4% in those receiving dialysis.2-5 The average age at presentation is 48 years.6,7 Although calciphylaxis has been noted to affect males and females equally, some studies have suggested a female predominance.5-8
The etiology of calciphylaxis is unknown, but ESRD requiring dialysis, primary or secondary hyperparathyroidism, obesity, diabetes mellitus, skin trauma, and/or a hypercoagulable state may put patients at increased risk for developing this disease.2,3 Other risk factors include systemic corticosteroids, liver disease, increased serum aluminum, and increased erythrocyte sedimentation rate. Although high calcium-phosphate product has been noted as a risk factor in prior studies, one retrospective study found that it does not reliably confirm or exclude a diagnosis of calciphylaxis.8
The pathogenesis of calciphylaxis is not well understood; however, some researchers suggest that an imbalance in calcium-phosphate homeostasis may lead to calciphylaxis; that is, elevated calcium and phosphate levels exceed their solubility and deposit in the walls of small- and medium-sized arteries, which consequently leads to ischemic necrosis and gangrene of the surrounding tissue.9
Clinically, calciphylaxis has an indolent onset and usually presents as well-demarcated, painful, purplish, mottled lesions that evolve into necrotic gray-black eschars and gangrene in adjacent tissues.1,5,6 The ischemic process may even extend to the muscle layer.5 Other common presentations include mild erythematous patches; livedo reticularis; painful nodules; necrotic ulcerating lesions; and more rarely flaccid, hemorrhagic, or serous bullous lesions followed by ulceration, as was seen in our patient.6,9,10 Lesions usually begin at sites of trauma and seem to be distributed symmetrically.5,6 The most commonly affected locations are the legs, specifically the medial thighs, as well as the abdomen and buttocks, but lesions also can be found at more distal sites such as the breasts, tongue, vulva, penis, fingers, and toes.5,6,10 The head and neck region rarely is affected. Although uncommon, calciphylaxis may affect other organs, including the lungs, stomach, kidneys, and adrenal glands.5 The accompanying systemic symptoms and findings may include muscle weakness, tenderness, or myositis with rhabdomyolysis; calcific cerebral embolism; dementia and infarction of the central nervous system; acute respiratory failure; heart disease; atrioventricular block; and calcification of the cardiac conduction system.6 Unlike other forms of peripheral vascular disease, distal pulses are present in calciphylaxis, as blood flow usually is preserved distal and deep to the areas of necrosis.5,6
A careful history and thorough physical examination are important first steps in the diagnosis of this condition.2,10 Although there are no definitive laboratory tests, elevated serum calcium, phosphorous, and calcium-phosphate product levels, as well as parathyroid hormone level, may be suggestive of calciphylaxis.2,5 Leukocytosis may occur if an infection is present.5
The most accurate method to confirm the diagnosis is a deep incisional biopsy from an erythematous, slightly purpuric area adjacent to the necrotic lesion.2,10,11 The histopathologic features used to make the diagnosis include calcification of medium-sized vessels, particularly the intimal or medial layers, in the deep dermis and subcutaneous fat in addition to lobular capillaries of the subcutaneous fat.5,10 These vessels, including the smaller distal vessels that supply the papillary dermis and epidermis, also may be thrombosed due to calcification, leading to vascular occlusion and subsequently ischemic necrosis of the overlying epidermis.10 Other findings may include pseudoxanthoma elasticum changes, panniculitis, and subcutaneous fat necrosis.4,10
The differential diagnosis for calciphylaxis includes peripheral vascular disease, vasculitis, juvenile dermatomyositis, proteins C and S deficiencies, cryofibrinogenemia, calcinosis cutis, and tumoral calcinosis.2 Polyarteritis nodosa, Sjögren syndrome, atherosclerotic peripheral vascular disease, pyoderma gangrenosum, systemic lupus erythematosus, necrotizing fasciitis, septic embolism, and necrosis secondary to warfarin and heparin may mimic calciphylaxis.5
Treatment of calciphylaxis is multidimensional but primarily is supportive.6,11 Controlling calcium and phosphate levels and secondary hyperparathyroidism through diet and phosphate binders (eg, sevelamer hydrochloride) has been shown to be effective.6 Pamidronate, a bisphosphonate, inhibits arterial calcification in animal models and has been reported to treat calciphylaxis, resulting in marked pain reduction and ulcer healing.4,6 Cinacalcet, which functions as a calcimimetic, has been implicated in the treatment of calciphylaxis. It has been used to treat primary and secondary hyperparathyroidism and to normalize serum calcium levels; it also may be used as an alternative to parathyroidectomy.4,6 Intravenous administration of sodium thiosulfate, a potent antioxidant and chelator of calcium, has been helpful in reversing signs and symptoms of calciphylaxis.6,12 It also has been shown to effectively remove extra calcium during peritoneal dialysis.6 Parathyroidectomy has been useful in patients with markedly elevated parathyroid hormone levels, as it suppresses or eliminates the sensitizing agent causing hypercalcemia, elevated calcium-phosphate product, and hyperparathyroidism.1,2,6,13
Wound care and prevention of sepsis are essential in the treatment of calciphylaxis. Management options include surgical debridement, hydrocolloid and biologic dressings, skin grafts, systemic antibiotics, oral pentoxifylline combined with maggot therapy, nutritional support, hyperbaric oxygen therapy, and revascularization and amputation when other interventions have failed. Pain control with analgesics and correction of thrombosis in the skin and blood vessels via anticoagulation therapy also are important complementary treatments.6
The clinical outcome of calciphylaxis is dependent on early diagnosis, antimicrobial therapy, and wound management,9 but overall, the prognosis usually is poor and has a high mortality rate. The most common causes of death are infection and sepsis.1,9 A study of 7 cases reported 100% mortality,14 but other studies have suggested a mortality rate of 60% to 80%.4,10 Female sex and obesity are poor prognostic indicators.2 A better prognosis has been appreciated in cases in which lesions occur at distal sites (eg, lower legs, hands) compared to more proximal sites (eg, abdomen), where 25% and 75% mortalities have been noted, respectively.10,14,15 In one study, the overall mortality rate was 45% in patients with calciphylaxis at 1 year.6 The rate was 41% in patients with plaques only and 67% in those who presented with ulceration. Patients who survive often experience a high degree of morbidity and prolonged hospitalization; these patients often are severely debilitated, especially in the case of limb amputation.6
Our report of calciphylaxis demonstrates the diversity in clinical presentation and emphasizes the importance of early and accurate diagnosis in reducing morbidity and mortality. In our case, the patient presented with skin pain and tense nonhemorrhagic bullae without underlying ecchymotic or erythematous lesions as the earliest sign of calciphylaxis. Physicians should have a high degree of suspicion in the setting of dialysis-dependent ESRD patients with bullae, extreme pain, and continuous decline. We hope that this case will help increase awareness of the varying presentations of this condition.
- Hanafusa T, Yamaguchi Y, Tani M, et al. Intractable wounds caused by calcific uremic arteriolopathy treated with bisphosphonates. J Am Acad Dermatol. 2001;57:1021-1025.
- Somorin AO, Harbi AA, Subaity Y, et al. Calciphylaxis: case report and literature review. Afr J Med Sci. 2002;31:175-178.
- Barreiros HM, Goulão J, Cunha H, et al. Calciphylaxis: a diagnostic and therapeutic challenge. J Dermatol Case Rep. 2013;2:69-70.
- Vedvyas C, Winterfield LS, Vleugels RA. Calciphylaxis: a systematic review of existing and emerging therapies. J Am Acad Dermatol. 2012;67:E253-E260.
- Beitz JM. Calciphylaxis: a case study with differential diagnosis. Ostomy Wound Manag. 2003;49:28-38.
- Daudén E, Oñate M. Calciphylaxis. Dermatol Clin. 2008;26:557-568.
- Oh DH, Eulau D, Tokugawa DA, et al. Five cases of calciphylaxis and a review of the literature. J Am Acad Dermatol. 1999;40:979-987.
- Weenig RH, Sewell LD, Davis MDP, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-578.
- Hanvesakul R, Silva MA, Hejmadi R, et al. Calciphylaxis following kidney transplantation: a case report. J Med Cases. 2009;3:9297.
- Kouba DJ, Owens NM, Barrett TL, et al. An unusual case of calciphylaxis. J Cutan Med Surg. 2004;8:19-22.
- Arch-Ferrer JE, Beenken SW, Rue LW, et al. Therapy for calciphylaxis: an outcome analysis. Surgery. 2003;134:941-945.
- Cicone JS, Petronis JB, Embert CD, et al. Successful treatment of calciphylaxis with intravenous sodium thiosulfate. Am J Kidney Dis. 2004;43:1104-1108.
- Mirza I, Chaubay D, Gunderia H, et al. An unusual presentation of calciphylaxis due to primary hyperparathyroidism. Arch Pathol Lab Med. 2001;125:1351-1353.
- Alain J, Poulin YP, Cloutier RA, et al. Calciphylaxis: seven new cases. J Cutan Med Surg. 2000;4:213-218.
- Hafner J, Keusch G, Wahl C, et al. Calciphylaxis: a syndrome of skin necrosis and acral gangrene in chronic renal failure. Vasa. 1998;27:137-143.
- Hanafusa T, Yamaguchi Y, Tani M, et al. Intractable wounds caused by calcific uremic arteriolopathy treated with bisphosphonates. J Am Acad Dermatol. 2001;57:1021-1025.
- Somorin AO, Harbi AA, Subaity Y, et al. Calciphylaxis: case report and literature review. Afr J Med Sci. 2002;31:175-178.
- Barreiros HM, Goulão J, Cunha H, et al. Calciphylaxis: a diagnostic and therapeutic challenge. J Dermatol Case Rep. 2013;2:69-70.
- Vedvyas C, Winterfield LS, Vleugels RA. Calciphylaxis: a systematic review of existing and emerging therapies. J Am Acad Dermatol. 2012;67:E253-E260.
- Beitz JM. Calciphylaxis: a case study with differential diagnosis. Ostomy Wound Manag. 2003;49:28-38.
- Daudén E, Oñate M. Calciphylaxis. Dermatol Clin. 2008;26:557-568.
- Oh DH, Eulau D, Tokugawa DA, et al. Five cases of calciphylaxis and a review of the literature. J Am Acad Dermatol. 1999;40:979-987.
- Weenig RH, Sewell LD, Davis MDP, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-578.
- Hanvesakul R, Silva MA, Hejmadi R, et al. Calciphylaxis following kidney transplantation: a case report. J Med Cases. 2009;3:9297.
- Kouba DJ, Owens NM, Barrett TL, et al. An unusual case of calciphylaxis. J Cutan Med Surg. 2004;8:19-22.
- Arch-Ferrer JE, Beenken SW, Rue LW, et al. Therapy for calciphylaxis: an outcome analysis. Surgery. 2003;134:941-945.
- Cicone JS, Petronis JB, Embert CD, et al. Successful treatment of calciphylaxis with intravenous sodium thiosulfate. Am J Kidney Dis. 2004;43:1104-1108.
- Mirza I, Chaubay D, Gunderia H, et al. An unusual presentation of calciphylaxis due to primary hyperparathyroidism. Arch Pathol Lab Med. 2001;125:1351-1353.
- Alain J, Poulin YP, Cloutier RA, et al. Calciphylaxis: seven new cases. J Cutan Med Surg. 2000;4:213-218.
- Hafner J, Keusch G, Wahl C, et al. Calciphylaxis: a syndrome of skin necrosis and acral gangrene in chronic renal failure. Vasa. 1998;27:137-143.
Practice Points
- Calciphylaxis is a rare microvascular occlusion syndrome characterized by cutaneous ischemia and necrosis secondary to calcification.
- Clinically, lesions present with severely painful, violaceous, retiform patches and plaques, and less commonly bullae that progress to necrotic ulcers on the buttocks, legs, or abdomen, which is most often associated with end-stage renal disease and hyperparathyroidism.
- The diagnosis is made through deep wedge or excisional biopsy and shows calcification of medium-sized vessels in the deep dermis and subcutaneous fat. Treatment requires a multidisciplinary approach, but morbidity and mortality remain high.
States allow doctors to practice across state lines during COVID-19 crisis
Legal orders and waivers of licensing requirements could change the way many doctors see patients during the COVID-19 crisis.
A number of states have already taken steps to waive their requirement that a physician be licensed in the state in order to provide care to patients. California and Florida are among the states that have done so – through their respective declarations of statewide emergency. More states are sure to follow.
Another route around traditional medical licensing requirements is the Uniform Emergency Volunteer Health Practitioner Act (UEVHPA), which – in the 20 or so states that have adopted it – can take effect once a statewide emergency is declared. This law lets volunteer health practitioners who are licensed in another state practice in the state where the emergency was declared, without first needing to obtain a license there. The practitioner need only be in good standing with any state in which he or she is currently licensed and be registered as a volunteer in the system. The Washington State Department of Health was one of the first such departments to invoke the UEVHPA in response to the coronavirus.
“The waiving of state licensure requirements should help ease a number of stress points of the current crisis in ways that benefit society,” said Gregory A. Hood, MD, an internist in Lexington, Ky., who is on the advisory board of Medscape Business of Medicine.
“As many have chosen to shelter in place, hoping to ride out the end of winter and, optimistically, the COVID-19 pandemic, there are physicians with second homes in South Carolina, Florida, and elsewhere who could be envisioned being brought into service to ease staffing shortfalls should the crisis exceed available resources.
“However, likely the most novel, necessary, and widespread impact of the waiving of licensure requirements will be aiding physicians in practicing telehealth video visits, as now authorized by Medicare and (hopefully) commercial insurers,” said Dr. Hood.
“Historically, there has been concern regarding the fact that most state medical boards require the physician to be licensed in the state where the patient resides or is located,” he said. “[Recently] I was able to conduct a video visit with a patient in Florida, at her initiation, over the potential of a broken bone. The case should be expected to have fallen under an emergency, but this waiver provides reassuring clarity.
“With the assistance of her boyfriend performing elements of the physical examination under my direction, we were able to establish a probable diagnosis, as well as a treatment plan – all while avoiding her exposing herself by leaving voluntary self-isolation or consuming resources in the emergency room,” Dr. Hood said.
Elsewhere, in response to the COVID-19 pandemic, the Federation of State Medical Boards has announced that it will act to verify licenses and credentials for doctors wishing to practice across state lines.
The “emergency exception” to in-state licensing requirements
Most state medical boards recognize some version of an exception to the in-state licensing requirement if a doctor or other healthcare professional is providing emergency care to a patient. But these exceptions rarely define what qualifies as an emergency. So, whether treatment of a COVID-19 patient or treatment of a non-COVID-19 patient who requires care in a triage setting constitutes an emergency – so that the exception to the licensing requirement applies—has been something of an open question.
What’s more, many states have laid out various exceptions to the exception. For example, in some states, the person providing the emergency treatment cannot be doing so in exchange for monetary compensation. Elsewhere, the emergency treatment must be provided outside of a traditional health care setting (not in a hospital or doctor’s office) to qualify under the exception.
Is expedited medical licensing an option?
There are ways for a care provider to obtain a medical license in some states without relying on the traditional (and often time-intensive) process. In Ohio, for example, the state’s medical board can issue an expedited license to practice medicine, although the care provider still needs to submit an application – in other words, expedited licensing can’t be granted retroactively. And in many states – including California, where medical board staff is required to complete initial review of an application within 60 working days – an expedited application isn’t an option (at least not yet).
Around 30 states have joined the Interstate Medical Licensure Compact, which makes it easier for doctors to get licensed in multiple states through an expedited application process. According to the Interstate Medical Licensure Compact Commission, around 80% of doctors meet the criteria for licensing through the Compact.
Why licensing matters
State medical boards and other licensing agencies protect patients by making sure that an individual who practices medicine in the state is qualified to do so. That means scrutinizing applications to practice medicine in the state, reviewing credentials, and ensuring fitness to practice.
The practice of medicine without a license is typically considered a criminal act and is punishable by a variety of different sanctions (criminal, administrative, and professional). What’s more, the fact that a care provider was practicing medicine without a license could set the table for allegations of medical malpractice.
From a liability standpoint, if a doctor or other clinician treats a patient in a state where the clinician is unlicensed, then it’s a near certainty that any medical liability insurance the doctor carries will not apply to the treatment scenario. Suppose a patient is given substandard care and suffers harm at some point within the unlicensed treatment setting, and the patient files a malpractice lawsuit. In that situation, the doctor (and not an insurance company with so-called “deep pockets”) will be on the financial hook for the patient’s harm.
Doctors and other health care providers continue to serve the most critical of roles in our nation’s response to the COVID-19 pandemic. Like most things related to COVID-19, the information presented here is sure to change.
David Goguen is a legal editor at Nolo whose work focuses on claimants’ rights in personal injury cases. He is a member of the California State Bar and has more than a decade of experience in litigation and legal publishing. He is a graduate of the University of San Francisco School of Law.
A version of this article originally appeared on Medscape.com.
Legal orders and waivers of licensing requirements could change the way many doctors see patients during the COVID-19 crisis.
A number of states have already taken steps to waive their requirement that a physician be licensed in the state in order to provide care to patients. California and Florida are among the states that have done so – through their respective declarations of statewide emergency. More states are sure to follow.
Another route around traditional medical licensing requirements is the Uniform Emergency Volunteer Health Practitioner Act (UEVHPA), which – in the 20 or so states that have adopted it – can take effect once a statewide emergency is declared. This law lets volunteer health practitioners who are licensed in another state practice in the state where the emergency was declared, without first needing to obtain a license there. The practitioner need only be in good standing with any state in which he or she is currently licensed and be registered as a volunteer in the system. The Washington State Department of Health was one of the first such departments to invoke the UEVHPA in response to the coronavirus.
“The waiving of state licensure requirements should help ease a number of stress points of the current crisis in ways that benefit society,” said Gregory A. Hood, MD, an internist in Lexington, Ky., who is on the advisory board of Medscape Business of Medicine.
“As many have chosen to shelter in place, hoping to ride out the end of winter and, optimistically, the COVID-19 pandemic, there are physicians with second homes in South Carolina, Florida, and elsewhere who could be envisioned being brought into service to ease staffing shortfalls should the crisis exceed available resources.
“However, likely the most novel, necessary, and widespread impact of the waiving of licensure requirements will be aiding physicians in practicing telehealth video visits, as now authorized by Medicare and (hopefully) commercial insurers,” said Dr. Hood.
“Historically, there has been concern regarding the fact that most state medical boards require the physician to be licensed in the state where the patient resides or is located,” he said. “[Recently] I was able to conduct a video visit with a patient in Florida, at her initiation, over the potential of a broken bone. The case should be expected to have fallen under an emergency, but this waiver provides reassuring clarity.
“With the assistance of her boyfriend performing elements of the physical examination under my direction, we were able to establish a probable diagnosis, as well as a treatment plan – all while avoiding her exposing herself by leaving voluntary self-isolation or consuming resources in the emergency room,” Dr. Hood said.
Elsewhere, in response to the COVID-19 pandemic, the Federation of State Medical Boards has announced that it will act to verify licenses and credentials for doctors wishing to practice across state lines.
The “emergency exception” to in-state licensing requirements
Most state medical boards recognize some version of an exception to the in-state licensing requirement if a doctor or other healthcare professional is providing emergency care to a patient. But these exceptions rarely define what qualifies as an emergency. So, whether treatment of a COVID-19 patient or treatment of a non-COVID-19 patient who requires care in a triage setting constitutes an emergency – so that the exception to the licensing requirement applies—has been something of an open question.
What’s more, many states have laid out various exceptions to the exception. For example, in some states, the person providing the emergency treatment cannot be doing so in exchange for monetary compensation. Elsewhere, the emergency treatment must be provided outside of a traditional health care setting (not in a hospital or doctor’s office) to qualify under the exception.
Is expedited medical licensing an option?
There are ways for a care provider to obtain a medical license in some states without relying on the traditional (and often time-intensive) process. In Ohio, for example, the state’s medical board can issue an expedited license to practice medicine, although the care provider still needs to submit an application – in other words, expedited licensing can’t be granted retroactively. And in many states – including California, where medical board staff is required to complete initial review of an application within 60 working days – an expedited application isn’t an option (at least not yet).
Around 30 states have joined the Interstate Medical Licensure Compact, which makes it easier for doctors to get licensed in multiple states through an expedited application process. According to the Interstate Medical Licensure Compact Commission, around 80% of doctors meet the criteria for licensing through the Compact.
Why licensing matters
State medical boards and other licensing agencies protect patients by making sure that an individual who practices medicine in the state is qualified to do so. That means scrutinizing applications to practice medicine in the state, reviewing credentials, and ensuring fitness to practice.
The practice of medicine without a license is typically considered a criminal act and is punishable by a variety of different sanctions (criminal, administrative, and professional). What’s more, the fact that a care provider was practicing medicine without a license could set the table for allegations of medical malpractice.
From a liability standpoint, if a doctor or other clinician treats a patient in a state where the clinician is unlicensed, then it’s a near certainty that any medical liability insurance the doctor carries will not apply to the treatment scenario. Suppose a patient is given substandard care and suffers harm at some point within the unlicensed treatment setting, and the patient files a malpractice lawsuit. In that situation, the doctor (and not an insurance company with so-called “deep pockets”) will be on the financial hook for the patient’s harm.
Doctors and other health care providers continue to serve the most critical of roles in our nation’s response to the COVID-19 pandemic. Like most things related to COVID-19, the information presented here is sure to change.
David Goguen is a legal editor at Nolo whose work focuses on claimants’ rights in personal injury cases. He is a member of the California State Bar and has more than a decade of experience in litigation and legal publishing. He is a graduate of the University of San Francisco School of Law.
A version of this article originally appeared on Medscape.com.
Legal orders and waivers of licensing requirements could change the way many doctors see patients during the COVID-19 crisis.
A number of states have already taken steps to waive their requirement that a physician be licensed in the state in order to provide care to patients. California and Florida are among the states that have done so – through their respective declarations of statewide emergency. More states are sure to follow.
Another route around traditional medical licensing requirements is the Uniform Emergency Volunteer Health Practitioner Act (UEVHPA), which – in the 20 or so states that have adopted it – can take effect once a statewide emergency is declared. This law lets volunteer health practitioners who are licensed in another state practice in the state where the emergency was declared, without first needing to obtain a license there. The practitioner need only be in good standing with any state in which he or she is currently licensed and be registered as a volunteer in the system. The Washington State Department of Health was one of the first such departments to invoke the UEVHPA in response to the coronavirus.
“The waiving of state licensure requirements should help ease a number of stress points of the current crisis in ways that benefit society,” said Gregory A. Hood, MD, an internist in Lexington, Ky., who is on the advisory board of Medscape Business of Medicine.
“As many have chosen to shelter in place, hoping to ride out the end of winter and, optimistically, the COVID-19 pandemic, there are physicians with second homes in South Carolina, Florida, and elsewhere who could be envisioned being brought into service to ease staffing shortfalls should the crisis exceed available resources.
“However, likely the most novel, necessary, and widespread impact of the waiving of licensure requirements will be aiding physicians in practicing telehealth video visits, as now authorized by Medicare and (hopefully) commercial insurers,” said Dr. Hood.
“Historically, there has been concern regarding the fact that most state medical boards require the physician to be licensed in the state where the patient resides or is located,” he said. “[Recently] I was able to conduct a video visit with a patient in Florida, at her initiation, over the potential of a broken bone. The case should be expected to have fallen under an emergency, but this waiver provides reassuring clarity.
“With the assistance of her boyfriend performing elements of the physical examination under my direction, we were able to establish a probable diagnosis, as well as a treatment plan – all while avoiding her exposing herself by leaving voluntary self-isolation or consuming resources in the emergency room,” Dr. Hood said.
Elsewhere, in response to the COVID-19 pandemic, the Federation of State Medical Boards has announced that it will act to verify licenses and credentials for doctors wishing to practice across state lines.
The “emergency exception” to in-state licensing requirements
Most state medical boards recognize some version of an exception to the in-state licensing requirement if a doctor or other healthcare professional is providing emergency care to a patient. But these exceptions rarely define what qualifies as an emergency. So, whether treatment of a COVID-19 patient or treatment of a non-COVID-19 patient who requires care in a triage setting constitutes an emergency – so that the exception to the licensing requirement applies—has been something of an open question.
What’s more, many states have laid out various exceptions to the exception. For example, in some states, the person providing the emergency treatment cannot be doing so in exchange for monetary compensation. Elsewhere, the emergency treatment must be provided outside of a traditional health care setting (not in a hospital or doctor’s office) to qualify under the exception.
Is expedited medical licensing an option?
There are ways for a care provider to obtain a medical license in some states without relying on the traditional (and often time-intensive) process. In Ohio, for example, the state’s medical board can issue an expedited license to practice medicine, although the care provider still needs to submit an application – in other words, expedited licensing can’t be granted retroactively. And in many states – including California, where medical board staff is required to complete initial review of an application within 60 working days – an expedited application isn’t an option (at least not yet).
Around 30 states have joined the Interstate Medical Licensure Compact, which makes it easier for doctors to get licensed in multiple states through an expedited application process. According to the Interstate Medical Licensure Compact Commission, around 80% of doctors meet the criteria for licensing through the Compact.
Why licensing matters
State medical boards and other licensing agencies protect patients by making sure that an individual who practices medicine in the state is qualified to do so. That means scrutinizing applications to practice medicine in the state, reviewing credentials, and ensuring fitness to practice.
The practice of medicine without a license is typically considered a criminal act and is punishable by a variety of different sanctions (criminal, administrative, and professional). What’s more, the fact that a care provider was practicing medicine without a license could set the table for allegations of medical malpractice.
From a liability standpoint, if a doctor or other clinician treats a patient in a state where the clinician is unlicensed, then it’s a near certainty that any medical liability insurance the doctor carries will not apply to the treatment scenario. Suppose a patient is given substandard care and suffers harm at some point within the unlicensed treatment setting, and the patient files a malpractice lawsuit. In that situation, the doctor (and not an insurance company with so-called “deep pockets”) will be on the financial hook for the patient’s harm.
Doctors and other health care providers continue to serve the most critical of roles in our nation’s response to the COVID-19 pandemic. Like most things related to COVID-19, the information presented here is sure to change.
David Goguen is a legal editor at Nolo whose work focuses on claimants’ rights in personal injury cases. He is a member of the California State Bar and has more than a decade of experience in litigation and legal publishing. He is a graduate of the University of San Francisco School of Law.
A version of this article originally appeared on Medscape.com.
Predictors of bacteremia in children hospitalized with community-acquired pneumonia
Children with bacteremia had longer lengths of stay
Clinical question: Are blood cultures warranted in specific subsets of children hospitalized with community-acquired pneumonia (CAP)?
Background: Guidelines from the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America recommend obtaining blood cultures in children hospitalized with moderate to severe community-acquired pneumonia. This group of authors recently published a study showing the prevalence of bacteremia of 2.5% in a cohort of generally healthy children hospitalized with CAP who had blood cultures obtained, with only 0.4% harboring a pathogen not susceptible to penicillin. They found low yield for blood cultures in children hospitalized with CAP.
Study design: Retrospective Cohort Study.
Setting: Pediatric Health Information System Plus (PHIS+) database (six institutions).
Synopsis: Secondary analysis of prior study of children aged 3 months to 18 years hospitalized with CAP between 2007 to 2011. For the secondary analysis only children in whom a blood culture was obtained on the initial or second day of hospitalization were studied. CAP was defined by a primary ICD-9 discharge diagnosis code for pneumonia or a primary ICD-9 discharge diagnosis code for pleural effusion with a secondary diagnosis code for pneumonia. Children transferred into the study institution and children with complex chronic conditions were excluded from the study. The primary outcome was the presence of bacteremia based on pathogen detection in the initial blood culture. Bacteria were labeled as pathogens or contaminants.
A total of 7,509 children were included in the initial study. Of them, 2,568 (34.2%) had a blood culture obtained on the initial or second day of hospitalization; 65 (2.5%) of the children with blood cultures obtained on admission had bacteremia. The most common penicillin-susceptible blood pathogen isolated was Streptococcus pneumoniae (n = 47). Eleven children (0.4%) had bacteremia with a pathogen not susceptible to penicillin. Children with bacteremia had a higher median admission white blood cell (WBC) count than did those without bacteremia (17.5 × 103 cells per mcL vs. 12.4 × 103 cells per mcL; P < .01) and definite radiographic pneumonia on admission chest radiograph (P < .01). C-reactive protein and erythrocyte sedimentation rate were also higher in children with bacteremia but were only obtained in 35% and 15% of patients, respectively. Children with bacteremia had a higher prevalence of complicated pneumonia on admission (P = .06) than did children without bacteremia. Children with bacteremia had longer lengths of stay (4 days vs. 2 days; P < .01) and were more likely to be admitted to an ICU (P < .01) than were children without bacteremia.
This study is limited by its sample because all of the patients were cared for at tertiary care hospitals. It is also limited by its timing; the PHIS+ data set spans the introduction of the 13-valent pneumococcal vaccine, and so the current prevalence of bacteremia in CAP may be lower than that found in the study.
Bottom line: The prevalence of bacteremia was low among a cohort of generally healthy children hospitalized with CAP, and no features strongly predicted the presence of bacteremia. The authors recommend that blood cultures in children with CAP should be limited to patients admitted to the ICU.
Citation: Lipsett SC et al. Predictors of Bacteremia in Children Hospitalized With Community-Acquired Pneumonia. Hosp Pediatr. 2019 Oct;9(10):770-8.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.
Children with bacteremia had longer lengths of stay
Children with bacteremia had longer lengths of stay
Clinical question: Are blood cultures warranted in specific subsets of children hospitalized with community-acquired pneumonia (CAP)?
Background: Guidelines from the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America recommend obtaining blood cultures in children hospitalized with moderate to severe community-acquired pneumonia. This group of authors recently published a study showing the prevalence of bacteremia of 2.5% in a cohort of generally healthy children hospitalized with CAP who had blood cultures obtained, with only 0.4% harboring a pathogen not susceptible to penicillin. They found low yield for blood cultures in children hospitalized with CAP.
Study design: Retrospective Cohort Study.
Setting: Pediatric Health Information System Plus (PHIS+) database (six institutions).
Synopsis: Secondary analysis of prior study of children aged 3 months to 18 years hospitalized with CAP between 2007 to 2011. For the secondary analysis only children in whom a blood culture was obtained on the initial or second day of hospitalization were studied. CAP was defined by a primary ICD-9 discharge diagnosis code for pneumonia or a primary ICD-9 discharge diagnosis code for pleural effusion with a secondary diagnosis code for pneumonia. Children transferred into the study institution and children with complex chronic conditions were excluded from the study. The primary outcome was the presence of bacteremia based on pathogen detection in the initial blood culture. Bacteria were labeled as pathogens or contaminants.
A total of 7,509 children were included in the initial study. Of them, 2,568 (34.2%) had a blood culture obtained on the initial or second day of hospitalization; 65 (2.5%) of the children with blood cultures obtained on admission had bacteremia. The most common penicillin-susceptible blood pathogen isolated was Streptococcus pneumoniae (n = 47). Eleven children (0.4%) had bacteremia with a pathogen not susceptible to penicillin. Children with bacteremia had a higher median admission white blood cell (WBC) count than did those without bacteremia (17.5 × 103 cells per mcL vs. 12.4 × 103 cells per mcL; P < .01) and definite radiographic pneumonia on admission chest radiograph (P < .01). C-reactive protein and erythrocyte sedimentation rate were also higher in children with bacteremia but were only obtained in 35% and 15% of patients, respectively. Children with bacteremia had a higher prevalence of complicated pneumonia on admission (P = .06) than did children without bacteremia. Children with bacteremia had longer lengths of stay (4 days vs. 2 days; P < .01) and were more likely to be admitted to an ICU (P < .01) than were children without bacteremia.
This study is limited by its sample because all of the patients were cared for at tertiary care hospitals. It is also limited by its timing; the PHIS+ data set spans the introduction of the 13-valent pneumococcal vaccine, and so the current prevalence of bacteremia in CAP may be lower than that found in the study.
Bottom line: The prevalence of bacteremia was low among a cohort of generally healthy children hospitalized with CAP, and no features strongly predicted the presence of bacteremia. The authors recommend that blood cultures in children with CAP should be limited to patients admitted to the ICU.
Citation: Lipsett SC et al. Predictors of Bacteremia in Children Hospitalized With Community-Acquired Pneumonia. Hosp Pediatr. 2019 Oct;9(10):770-8.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.
Clinical question: Are blood cultures warranted in specific subsets of children hospitalized with community-acquired pneumonia (CAP)?
Background: Guidelines from the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America recommend obtaining blood cultures in children hospitalized with moderate to severe community-acquired pneumonia. This group of authors recently published a study showing the prevalence of bacteremia of 2.5% in a cohort of generally healthy children hospitalized with CAP who had blood cultures obtained, with only 0.4% harboring a pathogen not susceptible to penicillin. They found low yield for blood cultures in children hospitalized with CAP.
Study design: Retrospective Cohort Study.
Setting: Pediatric Health Information System Plus (PHIS+) database (six institutions).
Synopsis: Secondary analysis of prior study of children aged 3 months to 18 years hospitalized with CAP between 2007 to 2011. For the secondary analysis only children in whom a blood culture was obtained on the initial or second day of hospitalization were studied. CAP was defined by a primary ICD-9 discharge diagnosis code for pneumonia or a primary ICD-9 discharge diagnosis code for pleural effusion with a secondary diagnosis code for pneumonia. Children transferred into the study institution and children with complex chronic conditions were excluded from the study. The primary outcome was the presence of bacteremia based on pathogen detection in the initial blood culture. Bacteria were labeled as pathogens or contaminants.
A total of 7,509 children were included in the initial study. Of them, 2,568 (34.2%) had a blood culture obtained on the initial or second day of hospitalization; 65 (2.5%) of the children with blood cultures obtained on admission had bacteremia. The most common penicillin-susceptible blood pathogen isolated was Streptococcus pneumoniae (n = 47). Eleven children (0.4%) had bacteremia with a pathogen not susceptible to penicillin. Children with bacteremia had a higher median admission white blood cell (WBC) count than did those without bacteremia (17.5 × 103 cells per mcL vs. 12.4 × 103 cells per mcL; P < .01) and definite radiographic pneumonia on admission chest radiograph (P < .01). C-reactive protein and erythrocyte sedimentation rate were also higher in children with bacteremia but were only obtained in 35% and 15% of patients, respectively. Children with bacteremia had a higher prevalence of complicated pneumonia on admission (P = .06) than did children without bacteremia. Children with bacteremia had longer lengths of stay (4 days vs. 2 days; P < .01) and were more likely to be admitted to an ICU (P < .01) than were children without bacteremia.
This study is limited by its sample because all of the patients were cared for at tertiary care hospitals. It is also limited by its timing; the PHIS+ data set spans the introduction of the 13-valent pneumococcal vaccine, and so the current prevalence of bacteremia in CAP may be lower than that found in the study.
Bottom line: The prevalence of bacteremia was low among a cohort of generally healthy children hospitalized with CAP, and no features strongly predicted the presence of bacteremia. The authors recommend that blood cultures in children with CAP should be limited to patients admitted to the ICU.
Citation: Lipsett SC et al. Predictors of Bacteremia in Children Hospitalized With Community-Acquired Pneumonia. Hosp Pediatr. 2019 Oct;9(10):770-8.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.
Firings, furloughs, and pay cuts in advance of COVID-19 surge
Doctors at a Boston-area hospital learned via video conferencing that they would be receiving a 20% pay cut – a slap in the face at the precise moment that those on the front lines of the COVID-19 pandemic need a pat on the back (and more N95 respirators).
But Steward Health Care System*, which runs the hospital and dozens of others around the country, did the math and decided that the pay cuts were necessary to survive what they called “a seismic shock to our system.” They also announced furloughs for a large number of their nonclinical staff.
Spirits sank after the announcement. “It was devastating,” said one Boston doctor, who works for Steward and asked not to be identified for fear of retribution. “I didn’t say much during the call because I was so panicked, and I didn’t want to be crying on the call.”
Someone else did speak up, a senior colleague who warned that such a cut would kill morale at a time when physicians were already feeling vulnerable because of other shortages, including personal protective equipment. (Requests for interviews with Steward Health Care System executives were declined.)
Furloughs, layoffs, and even firings are happening elsewhere too. Hospitals in virus hotspots have already come up short on beds and face masks. Now a shortage of cash is prompting many to fire some of their health care workers, furlough them temporarily, or – like Steward Health Care System – slash their pay checks.
Despite almost $200 billion earmarked for hospital systems in the recently passed federal stimulus package, many hospitals are still in dire financial straits. Most make the majority of their money through so-called elective procedures, such as knee replacements and cataract surgeries, almost all of which have been postponed in order to conserve personal protective equipment and minimize spread of the virus. Those cancellations translate to a significant financial hit.
On top of that, hospitals will lose an average of $1,800 on every COVID-19 case, according to projections by Strata Decision Technology, a health care financial planning and analytic company. Some, they estimate, may lose much more, between $6,000 and $8,000 per patient. And hospitals were already hurting. According to a report from Bloomberg, at least 30 hospitals entered bankruptcy in 2019.
“This pressure on institutions to control costs has been around for several years,” said Steve Lefar, executive director of the data science division of Strata Decision Technology and lead author of the study. “This is just making it incredibly acute for them.”
Many hospital executives are bracing for months of hardship, leading to wrenching decisions to furlough or lay off staff, suspend bonuses, or cut pay – even as some short-staffed hospitals in COVID-19 hotspots are issuing pleas for doctors to come out of retirement.
Forward thinking?
While most furloughs and layoffs so far have affected people who don’t work directly with patients, many on the front lines have been hit with pay cuts or withheld bonuses or retirement contributions. In Massachusetts, the state’s medical society has asked Governor Charlie Baker for financial relief for health care workers in the form of grants, no-interest or forgivable small-business loans for physician practices, and deferment of medical student loan payments.
At St. Alexius Hospital in St. Louis, Sonny Saggar, MD, was fired as CEO after he clashed with a bankruptcy trustee. Dr. Saggar had proposed offering open beds to other hospital systems during the pandemic – an idea that, he said, was turned down out of concern for the bottom line.
“This is one of those times where we need to put down our search for profit and money and just look after people’s lives. We’re supposed to have that calling in health care,” said Dr. Saggar, who has since been reinstated as chief strategy officer and director of the COVID task force and ED. He noted that he and the trustee have resolved differences over funding.
At St. Claire HealthCare in Morehead, Ky., 300 employees who were not involved in direct patient care – a quarter of the hospital’s staff – have been furloughed, something Donald Lloyd II, St. Claire HealthCare’s CEO as of May 1, described as forward thinking.
To prepare for the influx of COVID-19 patients, the hospital shut down elective procedures early. “Prudence dictates the need to be extremely proactive,” Mr. Lloyd said. “We need to devote our limited resources to frontline clinical teams.”
Other hospitals are making similar moves, although many are not doing so publicly. Mr. Lloyd decided to put out a press release because he found it offensive that the federal government was “bailing out airlines and cruise lines before our frontline men and women caring for patients.”
Massachusetts-based Atrius Health, for instance, placed many staffers on a 1-month furlough, while simultaneously withholding a percentage of working physicians’ paychecks, saying that they plan to pay them back at a later date. TriHealth, in Cincinnati, looked elsewhere for ways to save money. Instead of cutting physician salaries, 11 executives took a 20% pay cut.
There are both better and worse ways to go about such staff reductions, according to Mr. Lefar. If reductions have to be made, it would be best if CEOs keep cuts as far away as possible from the front lines of patient care.
“My bias is to start with pay reductions for high-paid executives, then furloughs, and beyond that layoffs,” he said. (Furloughs allow employees to be brought back and receive unemployment benefits while not working.) “Anyone related to patient care – these are the people who are getting the country through this, these are the heroes.”
After the pandemic
Large hospital systems that can designate separate buildings for COVID-19 care may fare best financially, Mr. Lefar said. By retaining a clean, noninfectious facility, such setups could allow for an earlier return to regular procedures – as long as rapid COVID-19 testing becomes available.
Smaller hospitals, nearly half of which run at a financial loss, according to the Chartis Center for Rural Health, face the additional burdens of both limited capacity and a limited ability to separate COVID-19 care.
Mostly, Mr. Lefar said, it’s a matter of doing whatever is necessary to get through the worst of it. “A lot of what is deemed elective or scheduled will come back,” he said. “Right now it’s crisis mode. ... I think it’s going to be a rough 6-9 months, but we will get back to it.”
*Correction, 4/7/20: An earlier version of this article misstated the name of a hospital in the Boston area run by Steward Health Care System.
A version of this article originally appeared on Medscape.com.
Doctors at a Boston-area hospital learned via video conferencing that they would be receiving a 20% pay cut – a slap in the face at the precise moment that those on the front lines of the COVID-19 pandemic need a pat on the back (and more N95 respirators).
But Steward Health Care System*, which runs the hospital and dozens of others around the country, did the math and decided that the pay cuts were necessary to survive what they called “a seismic shock to our system.” They also announced furloughs for a large number of their nonclinical staff.
Spirits sank after the announcement. “It was devastating,” said one Boston doctor, who works for Steward and asked not to be identified for fear of retribution. “I didn’t say much during the call because I was so panicked, and I didn’t want to be crying on the call.”
Someone else did speak up, a senior colleague who warned that such a cut would kill morale at a time when physicians were already feeling vulnerable because of other shortages, including personal protective equipment. (Requests for interviews with Steward Health Care System executives were declined.)
Furloughs, layoffs, and even firings are happening elsewhere too. Hospitals in virus hotspots have already come up short on beds and face masks. Now a shortage of cash is prompting many to fire some of their health care workers, furlough them temporarily, or – like Steward Health Care System – slash their pay checks.
Despite almost $200 billion earmarked for hospital systems in the recently passed federal stimulus package, many hospitals are still in dire financial straits. Most make the majority of their money through so-called elective procedures, such as knee replacements and cataract surgeries, almost all of which have been postponed in order to conserve personal protective equipment and minimize spread of the virus. Those cancellations translate to a significant financial hit.
On top of that, hospitals will lose an average of $1,800 on every COVID-19 case, according to projections by Strata Decision Technology, a health care financial planning and analytic company. Some, they estimate, may lose much more, between $6,000 and $8,000 per patient. And hospitals were already hurting. According to a report from Bloomberg, at least 30 hospitals entered bankruptcy in 2019.
“This pressure on institutions to control costs has been around for several years,” said Steve Lefar, executive director of the data science division of Strata Decision Technology and lead author of the study. “This is just making it incredibly acute for them.”
Many hospital executives are bracing for months of hardship, leading to wrenching decisions to furlough or lay off staff, suspend bonuses, or cut pay – even as some short-staffed hospitals in COVID-19 hotspots are issuing pleas for doctors to come out of retirement.
Forward thinking?
While most furloughs and layoffs so far have affected people who don’t work directly with patients, many on the front lines have been hit with pay cuts or withheld bonuses or retirement contributions. In Massachusetts, the state’s medical society has asked Governor Charlie Baker for financial relief for health care workers in the form of grants, no-interest or forgivable small-business loans for physician practices, and deferment of medical student loan payments.
At St. Alexius Hospital in St. Louis, Sonny Saggar, MD, was fired as CEO after he clashed with a bankruptcy trustee. Dr. Saggar had proposed offering open beds to other hospital systems during the pandemic – an idea that, he said, was turned down out of concern for the bottom line.
“This is one of those times where we need to put down our search for profit and money and just look after people’s lives. We’re supposed to have that calling in health care,” said Dr. Saggar, who has since been reinstated as chief strategy officer and director of the COVID task force and ED. He noted that he and the trustee have resolved differences over funding.
At St. Claire HealthCare in Morehead, Ky., 300 employees who were not involved in direct patient care – a quarter of the hospital’s staff – have been furloughed, something Donald Lloyd II, St. Claire HealthCare’s CEO as of May 1, described as forward thinking.
To prepare for the influx of COVID-19 patients, the hospital shut down elective procedures early. “Prudence dictates the need to be extremely proactive,” Mr. Lloyd said. “We need to devote our limited resources to frontline clinical teams.”
Other hospitals are making similar moves, although many are not doing so publicly. Mr. Lloyd decided to put out a press release because he found it offensive that the federal government was “bailing out airlines and cruise lines before our frontline men and women caring for patients.”
Massachusetts-based Atrius Health, for instance, placed many staffers on a 1-month furlough, while simultaneously withholding a percentage of working physicians’ paychecks, saying that they plan to pay them back at a later date. TriHealth, in Cincinnati, looked elsewhere for ways to save money. Instead of cutting physician salaries, 11 executives took a 20% pay cut.
There are both better and worse ways to go about such staff reductions, according to Mr. Lefar. If reductions have to be made, it would be best if CEOs keep cuts as far away as possible from the front lines of patient care.
“My bias is to start with pay reductions for high-paid executives, then furloughs, and beyond that layoffs,” he said. (Furloughs allow employees to be brought back and receive unemployment benefits while not working.) “Anyone related to patient care – these are the people who are getting the country through this, these are the heroes.”
After the pandemic
Large hospital systems that can designate separate buildings for COVID-19 care may fare best financially, Mr. Lefar said. By retaining a clean, noninfectious facility, such setups could allow for an earlier return to regular procedures – as long as rapid COVID-19 testing becomes available.
Smaller hospitals, nearly half of which run at a financial loss, according to the Chartis Center for Rural Health, face the additional burdens of both limited capacity and a limited ability to separate COVID-19 care.
Mostly, Mr. Lefar said, it’s a matter of doing whatever is necessary to get through the worst of it. “A lot of what is deemed elective or scheduled will come back,” he said. “Right now it’s crisis mode. ... I think it’s going to be a rough 6-9 months, but we will get back to it.”
*Correction, 4/7/20: An earlier version of this article misstated the name of a hospital in the Boston area run by Steward Health Care System.
A version of this article originally appeared on Medscape.com.
Doctors at a Boston-area hospital learned via video conferencing that they would be receiving a 20% pay cut – a slap in the face at the precise moment that those on the front lines of the COVID-19 pandemic need a pat on the back (and more N95 respirators).
But Steward Health Care System*, which runs the hospital and dozens of others around the country, did the math and decided that the pay cuts were necessary to survive what they called “a seismic shock to our system.” They also announced furloughs for a large number of their nonclinical staff.
Spirits sank after the announcement. “It was devastating,” said one Boston doctor, who works for Steward and asked not to be identified for fear of retribution. “I didn’t say much during the call because I was so panicked, and I didn’t want to be crying on the call.”
Someone else did speak up, a senior colleague who warned that such a cut would kill morale at a time when physicians were already feeling vulnerable because of other shortages, including personal protective equipment. (Requests for interviews with Steward Health Care System executives were declined.)
Furloughs, layoffs, and even firings are happening elsewhere too. Hospitals in virus hotspots have already come up short on beds and face masks. Now a shortage of cash is prompting many to fire some of their health care workers, furlough them temporarily, or – like Steward Health Care System – slash their pay checks.
Despite almost $200 billion earmarked for hospital systems in the recently passed federal stimulus package, many hospitals are still in dire financial straits. Most make the majority of their money through so-called elective procedures, such as knee replacements and cataract surgeries, almost all of which have been postponed in order to conserve personal protective equipment and minimize spread of the virus. Those cancellations translate to a significant financial hit.
On top of that, hospitals will lose an average of $1,800 on every COVID-19 case, according to projections by Strata Decision Technology, a health care financial planning and analytic company. Some, they estimate, may lose much more, between $6,000 and $8,000 per patient. And hospitals were already hurting. According to a report from Bloomberg, at least 30 hospitals entered bankruptcy in 2019.
“This pressure on institutions to control costs has been around for several years,” said Steve Lefar, executive director of the data science division of Strata Decision Technology and lead author of the study. “This is just making it incredibly acute for them.”
Many hospital executives are bracing for months of hardship, leading to wrenching decisions to furlough or lay off staff, suspend bonuses, or cut pay – even as some short-staffed hospitals in COVID-19 hotspots are issuing pleas for doctors to come out of retirement.
Forward thinking?
While most furloughs and layoffs so far have affected people who don’t work directly with patients, many on the front lines have been hit with pay cuts or withheld bonuses or retirement contributions. In Massachusetts, the state’s medical society has asked Governor Charlie Baker for financial relief for health care workers in the form of grants, no-interest or forgivable small-business loans for physician practices, and deferment of medical student loan payments.
At St. Alexius Hospital in St. Louis, Sonny Saggar, MD, was fired as CEO after he clashed with a bankruptcy trustee. Dr. Saggar had proposed offering open beds to other hospital systems during the pandemic – an idea that, he said, was turned down out of concern for the bottom line.
“This is one of those times where we need to put down our search for profit and money and just look after people’s lives. We’re supposed to have that calling in health care,” said Dr. Saggar, who has since been reinstated as chief strategy officer and director of the COVID task force and ED. He noted that he and the trustee have resolved differences over funding.
At St. Claire HealthCare in Morehead, Ky., 300 employees who were not involved in direct patient care – a quarter of the hospital’s staff – have been furloughed, something Donald Lloyd II, St. Claire HealthCare’s CEO as of May 1, described as forward thinking.
To prepare for the influx of COVID-19 patients, the hospital shut down elective procedures early. “Prudence dictates the need to be extremely proactive,” Mr. Lloyd said. “We need to devote our limited resources to frontline clinical teams.”
Other hospitals are making similar moves, although many are not doing so publicly. Mr. Lloyd decided to put out a press release because he found it offensive that the federal government was “bailing out airlines and cruise lines before our frontline men and women caring for patients.”
Massachusetts-based Atrius Health, for instance, placed many staffers on a 1-month furlough, while simultaneously withholding a percentage of working physicians’ paychecks, saying that they plan to pay them back at a later date. TriHealth, in Cincinnati, looked elsewhere for ways to save money. Instead of cutting physician salaries, 11 executives took a 20% pay cut.
There are both better and worse ways to go about such staff reductions, according to Mr. Lefar. If reductions have to be made, it would be best if CEOs keep cuts as far away as possible from the front lines of patient care.
“My bias is to start with pay reductions for high-paid executives, then furloughs, and beyond that layoffs,” he said. (Furloughs allow employees to be brought back and receive unemployment benefits while not working.) “Anyone related to patient care – these are the people who are getting the country through this, these are the heroes.”
After the pandemic
Large hospital systems that can designate separate buildings for COVID-19 care may fare best financially, Mr. Lefar said. By retaining a clean, noninfectious facility, such setups could allow for an earlier return to regular procedures – as long as rapid COVID-19 testing becomes available.
Smaller hospitals, nearly half of which run at a financial loss, according to the Chartis Center for Rural Health, face the additional burdens of both limited capacity and a limited ability to separate COVID-19 care.
Mostly, Mr. Lefar said, it’s a matter of doing whatever is necessary to get through the worst of it. “A lot of what is deemed elective or scheduled will come back,” he said. “Right now it’s crisis mode. ... I think it’s going to be a rough 6-9 months, but we will get back to it.”
*Correction, 4/7/20: An earlier version of this article misstated the name of a hospital in the Boston area run by Steward Health Care System.
A version of this article originally appeared on Medscape.com.
Rise in autism prevalence indicates earlier diagnosis
The prevalence of autism spectrum disorder in 4-year-olds rose from 2014 to 2016, indicating more early identification of ASD among the children born in 2012, compared with 2008, according to the Centers for Disease Control and Prevention.
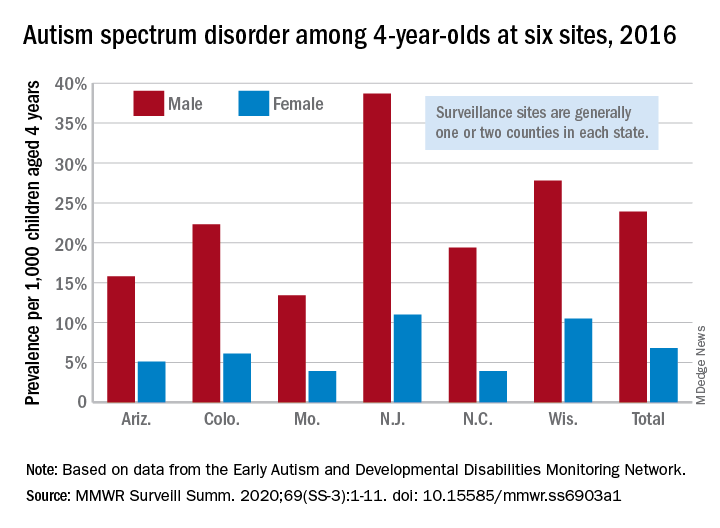
Data from individual surveillance sites in the CDC’s Early Autism and Developmental Disabilities Monitoring (Early ADDM) Network, however, show “wide variability in estimates [that] could reflect variable success in improving community identification,” Kelly A. Shaw, PhD, and associates wrote in MMWR Surveillance Summaries.
they reported.
“In addition, the cumulative incidence of ASD diagnoses at age 48 months was higher for children born in 2012 than for children born in 2008, which indicates a higher rate of diagnosis for the younger cohort,” wrote Dr. Shaw of the CDC’s National Center on Birth Defects and Developmental Disabilities, Atlanta, and associates.
A closer look at the six Early ADDM Network sites shows considerable variation in prevalence. The New Jersey site, consisting of one full county and part of another that includes metropolitan Newark, reported a rate of 25.3 per 1,000 – 38.7 for males and 11.0 for females – while the rates for Missouri – one county in metropolitan St. Louis – were 13.4 (male), 3.9 (female), and 8.8 (combined), the investigators wrote.
ASD prevalence across the six sites was 3.5 times higher among males (23.9 per 1,000) than females (6.8). “Cumulative incidence patterns also differed by sex, with a steady increase in diagnoses with age for boys but an apparent plateau for girls at approximately age 36 months,” they noted.
The median age at earliest diagnosis was 33 months for all sites, with North Carolina lowest at 29 months and Wisconsin highest at 36 months.
The overall median, Dr. Shaw and associates pointed out, is “well above the youngest age at which ASD can be identified, [so] work remains to improve early diagnosis so children can receive timely services.”
SOURCE: Shaw KA et al. MMWR Surveill Summ. 2020;69(SS-3):1-11. doi: 10.15585/mmwr.ss6903a1.
The prevalence of autism spectrum disorder in 4-year-olds rose from 2014 to 2016, indicating more early identification of ASD among the children born in 2012, compared with 2008, according to the Centers for Disease Control and Prevention.
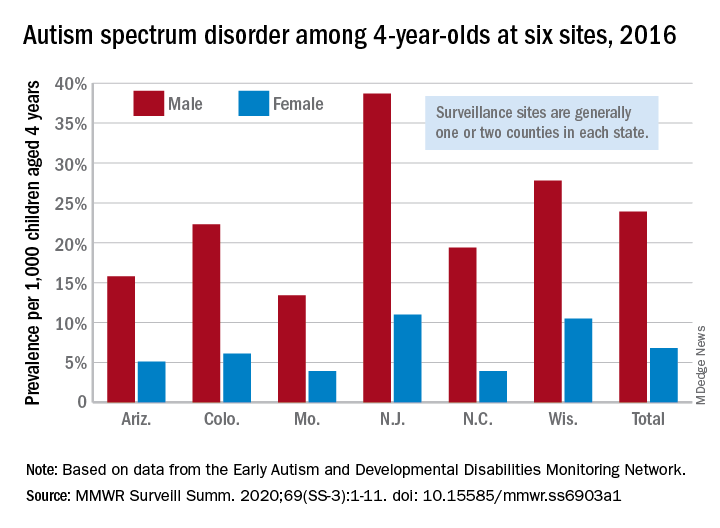
Data from individual surveillance sites in the CDC’s Early Autism and Developmental Disabilities Monitoring (Early ADDM) Network, however, show “wide variability in estimates [that] could reflect variable success in improving community identification,” Kelly A. Shaw, PhD, and associates wrote in MMWR Surveillance Summaries.
they reported.
“In addition, the cumulative incidence of ASD diagnoses at age 48 months was higher for children born in 2012 than for children born in 2008, which indicates a higher rate of diagnosis for the younger cohort,” wrote Dr. Shaw of the CDC’s National Center on Birth Defects and Developmental Disabilities, Atlanta, and associates.
A closer look at the six Early ADDM Network sites shows considerable variation in prevalence. The New Jersey site, consisting of one full county and part of another that includes metropolitan Newark, reported a rate of 25.3 per 1,000 – 38.7 for males and 11.0 for females – while the rates for Missouri – one county in metropolitan St. Louis – were 13.4 (male), 3.9 (female), and 8.8 (combined), the investigators wrote.
ASD prevalence across the six sites was 3.5 times higher among males (23.9 per 1,000) than females (6.8). “Cumulative incidence patterns also differed by sex, with a steady increase in diagnoses with age for boys but an apparent plateau for girls at approximately age 36 months,” they noted.
The median age at earliest diagnosis was 33 months for all sites, with North Carolina lowest at 29 months and Wisconsin highest at 36 months.
The overall median, Dr. Shaw and associates pointed out, is “well above the youngest age at which ASD can be identified, [so] work remains to improve early diagnosis so children can receive timely services.”
SOURCE: Shaw KA et al. MMWR Surveill Summ. 2020;69(SS-3):1-11. doi: 10.15585/mmwr.ss6903a1.
The prevalence of autism spectrum disorder in 4-year-olds rose from 2014 to 2016, indicating more early identification of ASD among the children born in 2012, compared with 2008, according to the Centers for Disease Control and Prevention.
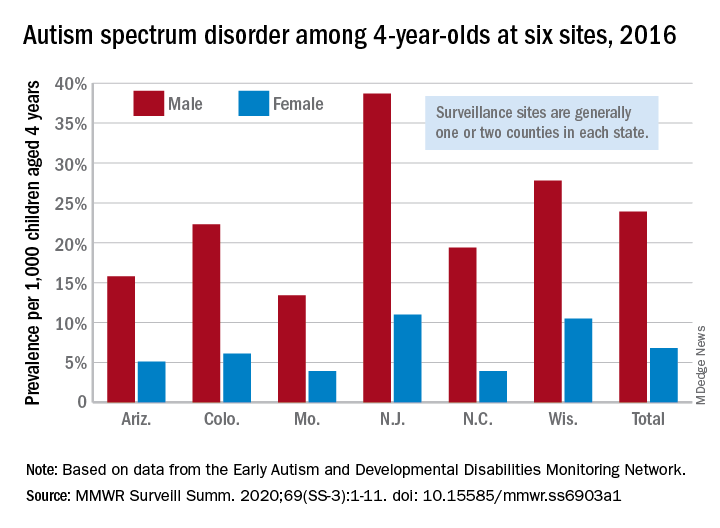
Data from individual surveillance sites in the CDC’s Early Autism and Developmental Disabilities Monitoring (Early ADDM) Network, however, show “wide variability in estimates [that] could reflect variable success in improving community identification,” Kelly A. Shaw, PhD, and associates wrote in MMWR Surveillance Summaries.
they reported.
“In addition, the cumulative incidence of ASD diagnoses at age 48 months was higher for children born in 2012 than for children born in 2008, which indicates a higher rate of diagnosis for the younger cohort,” wrote Dr. Shaw of the CDC’s National Center on Birth Defects and Developmental Disabilities, Atlanta, and associates.
A closer look at the six Early ADDM Network sites shows considerable variation in prevalence. The New Jersey site, consisting of one full county and part of another that includes metropolitan Newark, reported a rate of 25.3 per 1,000 – 38.7 for males and 11.0 for females – while the rates for Missouri – one county in metropolitan St. Louis – were 13.4 (male), 3.9 (female), and 8.8 (combined), the investigators wrote.
ASD prevalence across the six sites was 3.5 times higher among males (23.9 per 1,000) than females (6.8). “Cumulative incidence patterns also differed by sex, with a steady increase in diagnoses with age for boys but an apparent plateau for girls at approximately age 36 months,” they noted.
The median age at earliest diagnosis was 33 months for all sites, with North Carolina lowest at 29 months and Wisconsin highest at 36 months.
The overall median, Dr. Shaw and associates pointed out, is “well above the youngest age at which ASD can be identified, [so] work remains to improve early diagnosis so children can receive timely services.”
SOURCE: Shaw KA et al. MMWR Surveill Summ. 2020;69(SS-3):1-11. doi: 10.15585/mmwr.ss6903a1.
FROM MMWR SURVEILLANCE SUMMARIES
Behavior, family traits impact kids’ vulnerability as bullying targets
according to data from a large, cohort study of 1,760 children in Canada.
“Peer victimization is characterized by substantial individual variability in its timing, duration, and intensity,” but the specific variations in victimization patterns have not been well studied, wrote Sinziana I. Oncioiu, MPH, of the University of Bordeaux (France) and colleagues.
To better describe the trajectories of peer victimization and identify factors associated with them, the researchers used data from the Quebec Longitudinal Study of Child Development of children born in Quebec in 1997-1998 and followed from 5 months to 17 years of age. Participants reported being the target of a bully at least once in ages 6-17 years. The study included 862 boys and 898 girls; 59% provided data on being bullied seven or eight times out of a possible eight assessments in the study published in Pediatrics.
The researchers identified four trajectories of peer victimization for ages 6-17 years: low (33%), moderate emerging (30%), childhood limited (26%), and high chronic (11%). Low victimization was defined as low victimization throughout the follow-up period. Moderate-emerging victimization was defined as steady levels from 6-12 years, followed by adolescent victimization. Childhood-limited peer victimization was defined as a high level of bullying at 6 years of age, followed by a sharp decline from 6 to 17 years. High-chronic victimization was defined as persistently high victimization compared, with the other groups, although levels declined from 6 to 17 years.
Overall, in a multivariate analysis, children in the moderate-emerging, childhood-limited, and high-chronic groups were more likely than those in the low victimization group to demonstrate externalizing behavior problems in early childhood. In addition, children with a paternal history of antisocial behavior were significantly more likely to be in moderate-emerging and high-chronic groups, compared with the low group (odds ratios 1.54 and 1.93, respectively). Children living in a nonintact family in early childhood were significantly more likely to fall into the childhood-limited and high-chronic groups, compared with the low group.
The study findings were limited by several factors including lack of assessment of power imbalances between bullies and victims and a lack of differentiation between children who were both bullies and victims and those who were victims only, the researchers noted. The use of self-reports and some attrition of the study population also limited the results, they said.
However, the study’s large size and long-term follow-up strengthen the results, which support the need for targeted interventions to address individual and family vulnerabilities and prevent persistent victimization during children’s school years, the researchers concluded.
Pediatricians have an important role to play in reducing potential vulnerability to being bullied among their patients, Stephen S. Leff, PhD; Brooke S. Paskewich, PsyD; and Nathan J. Blum, MD, of Children’s Hospital of Philadelphia, wrote in an accompanying editorial.
“Given that nearly two-thirds of school-aged youth in the current study report peer victimization during elementary and/or middle school, this is an important period in which pediatricians can screen for victimization during well-child visits,” they said. It also is important to have resources and referral information available, whether it is in the practice, the community, or online. Anticipatory guidance also is valuable by defining bullying (“aggressive or mean behavior that happens repeatedly in the context of a power imbalance,”) forms of bullying (physical, verbal, using gossip, and social exclusion in real time or online), and the impact of bullying on children and families.
In addition, pediatricians should “recognize externalizing behaviors as risk factors for adverse outcomes and assist families in accessing evidence-based interventions such as family behavioral counseling or parent training,” the editorialists said. “There may also be value in pediatricians being more attuned to indicators of parental psychopathology so that they can make recommendations to address the parents’ mental health needs and better prepare parents to support their child’s social-emotional development.”
The study was supported by the Quebec Government Ministry of Health, Canadian Institute of Health Research, Quebec’s Health Research Fund, and other Canadian organizations and universities. The editorial was supported in part by the National Institutes of Health and the Department of Health and Human Services. The researchers and editorialists had no financial conflicts to disclose.
SOURCEs: Oncioiu SI et al. Pediatrics. 2020. doi: 10.1542/peds.2019-2654.
according to data from a large, cohort study of 1,760 children in Canada.
“Peer victimization is characterized by substantial individual variability in its timing, duration, and intensity,” but the specific variations in victimization patterns have not been well studied, wrote Sinziana I. Oncioiu, MPH, of the University of Bordeaux (France) and colleagues.
To better describe the trajectories of peer victimization and identify factors associated with them, the researchers used data from the Quebec Longitudinal Study of Child Development of children born in Quebec in 1997-1998 and followed from 5 months to 17 years of age. Participants reported being the target of a bully at least once in ages 6-17 years. The study included 862 boys and 898 girls; 59% provided data on being bullied seven or eight times out of a possible eight assessments in the study published in Pediatrics.
The researchers identified four trajectories of peer victimization for ages 6-17 years: low (33%), moderate emerging (30%), childhood limited (26%), and high chronic (11%). Low victimization was defined as low victimization throughout the follow-up period. Moderate-emerging victimization was defined as steady levels from 6-12 years, followed by adolescent victimization. Childhood-limited peer victimization was defined as a high level of bullying at 6 years of age, followed by a sharp decline from 6 to 17 years. High-chronic victimization was defined as persistently high victimization compared, with the other groups, although levels declined from 6 to 17 years.
Overall, in a multivariate analysis, children in the moderate-emerging, childhood-limited, and high-chronic groups were more likely than those in the low victimization group to demonstrate externalizing behavior problems in early childhood. In addition, children with a paternal history of antisocial behavior were significantly more likely to be in moderate-emerging and high-chronic groups, compared with the low group (odds ratios 1.54 and 1.93, respectively). Children living in a nonintact family in early childhood were significantly more likely to fall into the childhood-limited and high-chronic groups, compared with the low group.
The study findings were limited by several factors including lack of assessment of power imbalances between bullies and victims and a lack of differentiation between children who were both bullies and victims and those who were victims only, the researchers noted. The use of self-reports and some attrition of the study population also limited the results, they said.
However, the study’s large size and long-term follow-up strengthen the results, which support the need for targeted interventions to address individual and family vulnerabilities and prevent persistent victimization during children’s school years, the researchers concluded.
Pediatricians have an important role to play in reducing potential vulnerability to being bullied among their patients, Stephen S. Leff, PhD; Brooke S. Paskewich, PsyD; and Nathan J. Blum, MD, of Children’s Hospital of Philadelphia, wrote in an accompanying editorial.
“Given that nearly two-thirds of school-aged youth in the current study report peer victimization during elementary and/or middle school, this is an important period in which pediatricians can screen for victimization during well-child visits,” they said. It also is important to have resources and referral information available, whether it is in the practice, the community, or online. Anticipatory guidance also is valuable by defining bullying (“aggressive or mean behavior that happens repeatedly in the context of a power imbalance,”) forms of bullying (physical, verbal, using gossip, and social exclusion in real time or online), and the impact of bullying on children and families.
In addition, pediatricians should “recognize externalizing behaviors as risk factors for adverse outcomes and assist families in accessing evidence-based interventions such as family behavioral counseling or parent training,” the editorialists said. “There may also be value in pediatricians being more attuned to indicators of parental psychopathology so that they can make recommendations to address the parents’ mental health needs and better prepare parents to support their child’s social-emotional development.”
The study was supported by the Quebec Government Ministry of Health, Canadian Institute of Health Research, Quebec’s Health Research Fund, and other Canadian organizations and universities. The editorial was supported in part by the National Institutes of Health and the Department of Health and Human Services. The researchers and editorialists had no financial conflicts to disclose.
SOURCEs: Oncioiu SI et al. Pediatrics. 2020. doi: 10.1542/peds.2019-2654.
according to data from a large, cohort study of 1,760 children in Canada.
“Peer victimization is characterized by substantial individual variability in its timing, duration, and intensity,” but the specific variations in victimization patterns have not been well studied, wrote Sinziana I. Oncioiu, MPH, of the University of Bordeaux (France) and colleagues.
To better describe the trajectories of peer victimization and identify factors associated with them, the researchers used data from the Quebec Longitudinal Study of Child Development of children born in Quebec in 1997-1998 and followed from 5 months to 17 years of age. Participants reported being the target of a bully at least once in ages 6-17 years. The study included 862 boys and 898 girls; 59% provided data on being bullied seven or eight times out of a possible eight assessments in the study published in Pediatrics.
The researchers identified four trajectories of peer victimization for ages 6-17 years: low (33%), moderate emerging (30%), childhood limited (26%), and high chronic (11%). Low victimization was defined as low victimization throughout the follow-up period. Moderate-emerging victimization was defined as steady levels from 6-12 years, followed by adolescent victimization. Childhood-limited peer victimization was defined as a high level of bullying at 6 years of age, followed by a sharp decline from 6 to 17 years. High-chronic victimization was defined as persistently high victimization compared, with the other groups, although levels declined from 6 to 17 years.
Overall, in a multivariate analysis, children in the moderate-emerging, childhood-limited, and high-chronic groups were more likely than those in the low victimization group to demonstrate externalizing behavior problems in early childhood. In addition, children with a paternal history of antisocial behavior were significantly more likely to be in moderate-emerging and high-chronic groups, compared with the low group (odds ratios 1.54 and 1.93, respectively). Children living in a nonintact family in early childhood were significantly more likely to fall into the childhood-limited and high-chronic groups, compared with the low group.
The study findings were limited by several factors including lack of assessment of power imbalances between bullies and victims and a lack of differentiation between children who were both bullies and victims and those who were victims only, the researchers noted. The use of self-reports and some attrition of the study population also limited the results, they said.
However, the study’s large size and long-term follow-up strengthen the results, which support the need for targeted interventions to address individual and family vulnerabilities and prevent persistent victimization during children’s school years, the researchers concluded.
Pediatricians have an important role to play in reducing potential vulnerability to being bullied among their patients, Stephen S. Leff, PhD; Brooke S. Paskewich, PsyD; and Nathan J. Blum, MD, of Children’s Hospital of Philadelphia, wrote in an accompanying editorial.
“Given that nearly two-thirds of school-aged youth in the current study report peer victimization during elementary and/or middle school, this is an important period in which pediatricians can screen for victimization during well-child visits,” they said. It also is important to have resources and referral information available, whether it is in the practice, the community, or online. Anticipatory guidance also is valuable by defining bullying (“aggressive or mean behavior that happens repeatedly in the context of a power imbalance,”) forms of bullying (physical, verbal, using gossip, and social exclusion in real time or online), and the impact of bullying on children and families.
In addition, pediatricians should “recognize externalizing behaviors as risk factors for adverse outcomes and assist families in accessing evidence-based interventions such as family behavioral counseling or parent training,” the editorialists said. “There may also be value in pediatricians being more attuned to indicators of parental psychopathology so that they can make recommendations to address the parents’ mental health needs and better prepare parents to support their child’s social-emotional development.”
The study was supported by the Quebec Government Ministry of Health, Canadian Institute of Health Research, Quebec’s Health Research Fund, and other Canadian organizations and universities. The editorial was supported in part by the National Institutes of Health and the Department of Health and Human Services. The researchers and editorialists had no financial conflicts to disclose.
SOURCEs: Oncioiu SI et al. Pediatrics. 2020. doi: 10.1542/peds.2019-2654.
FROM PEDIATRICS
Key clinical point: Being targeted by bullies as children and adolescents may be affected in part by early childhood externalizing behavior and family vulnerability
Major finding: The researchers identified four distinct trajectories of peer victimization in the study population: low (33%), moderate emerging (30%), childhood limited (26%), and high chronic (11%).
Study details: The data come from a population-based cohort study of 1,760 Canadian children.
Disclosures: The study was supported by the Quebec Government Ministry of Health, Canadian Institute of Health Research, Quebec’s Health Research Fund, and other Canadian organizations and universities. The researchers had no financial conflicts to disclose.
Sources: Oncioiu SI et al. Pediatrics. 2020. doi: 10.1542/peds.2019-2654.
Failure is not an option
Gene Kranz was the NASA Flight Director during the Gemini and Apollo space flights, including Apollo 11 (moon landing) and Apollo 13. He has written: “When bad things happened, we just calmly laid out all the options and failure was not one of them. We never panicked and we never gave up on finding a solution.”
2019-nCoV (coronavirus, COVID-19) will define this generation of health care providers. First identified in Wuhan, China, in December 2019 and first appearing in the United States on January 19, 2020 (NEJM 2020;382:929). COVID-19 is a coronavirus similar to SARS and MERS. The U.S. Surgeon General and multiple endoscopy societies have recommended (strongly) that elective surgical and endoscopy procedures be deferred. Availability of testing has been slow, but many centers now have developed testing capabilities (including drive-through testing) with 6-hour result turnaround. We do not know the full pathophysiology, R0 (number of secondary cases attributed to an index infection), ease of community transmission, risk to providers, definition of people at high risk (for both acquisition and complications), and much key information n to base recommendations.
Health system and practice leaders do not yet have sufficient information to know which patients to defer, which patients should still be seen, visitor policies, how to segregate waiting rooms, or how to protect providers. Despite a lack of definitive knowledge, we must make critical decisions and know that recommendations can change hourly. As the Chief Clinical Officer at Michigan Medicine, I am spending 16 hours a day immersed in these decisions and find that one of my critical jobs is to keep people from panicking.
Schools, bars, restaurants, churches and other public gathering places are closing. Three countries (to date) have instituted complete quarantine. Digestive Disease Week® has been cancelled. We are entering a time in which normal life is altered and many changes will open up our thinking about long-term alternative processes.
COVID-19 will define this generation. The public will understand the real need for science, policies based on real facts, robust public health systems, and leaders who inspire confidence based on expert guidance. And, I believe we will see gastroenterologists, health systems, hospitals, and practices all showing us what our “finest hours” look like.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Gene Kranz was the NASA Flight Director during the Gemini and Apollo space flights, including Apollo 11 (moon landing) and Apollo 13. He has written: “When bad things happened, we just calmly laid out all the options and failure was not one of them. We never panicked and we never gave up on finding a solution.”
2019-nCoV (coronavirus, COVID-19) will define this generation of health care providers. First identified in Wuhan, China, in December 2019 and first appearing in the United States on January 19, 2020 (NEJM 2020;382:929). COVID-19 is a coronavirus similar to SARS and MERS. The U.S. Surgeon General and multiple endoscopy societies have recommended (strongly) that elective surgical and endoscopy procedures be deferred. Availability of testing has been slow, but many centers now have developed testing capabilities (including drive-through testing) with 6-hour result turnaround. We do not know the full pathophysiology, R0 (number of secondary cases attributed to an index infection), ease of community transmission, risk to providers, definition of people at high risk (for both acquisition and complications), and much key information n to base recommendations.
Health system and practice leaders do not yet have sufficient information to know which patients to defer, which patients should still be seen, visitor policies, how to segregate waiting rooms, or how to protect providers. Despite a lack of definitive knowledge, we must make critical decisions and know that recommendations can change hourly. As the Chief Clinical Officer at Michigan Medicine, I am spending 16 hours a day immersed in these decisions and find that one of my critical jobs is to keep people from panicking.
Schools, bars, restaurants, churches and other public gathering places are closing. Three countries (to date) have instituted complete quarantine. Digestive Disease Week® has been cancelled. We are entering a time in which normal life is altered and many changes will open up our thinking about long-term alternative processes.
COVID-19 will define this generation. The public will understand the real need for science, policies based on real facts, robust public health systems, and leaders who inspire confidence based on expert guidance. And, I believe we will see gastroenterologists, health systems, hospitals, and practices all showing us what our “finest hours” look like.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Gene Kranz was the NASA Flight Director during the Gemini and Apollo space flights, including Apollo 11 (moon landing) and Apollo 13. He has written: “When bad things happened, we just calmly laid out all the options and failure was not one of them. We never panicked and we never gave up on finding a solution.”
2019-nCoV (coronavirus, COVID-19) will define this generation of health care providers. First identified in Wuhan, China, in December 2019 and first appearing in the United States on January 19, 2020 (NEJM 2020;382:929). COVID-19 is a coronavirus similar to SARS and MERS. The U.S. Surgeon General and multiple endoscopy societies have recommended (strongly) that elective surgical and endoscopy procedures be deferred. Availability of testing has been slow, but many centers now have developed testing capabilities (including drive-through testing) with 6-hour result turnaround. We do not know the full pathophysiology, R0 (number of secondary cases attributed to an index infection), ease of community transmission, risk to providers, definition of people at high risk (for both acquisition and complications), and much key information n to base recommendations.
Health system and practice leaders do not yet have sufficient information to know which patients to defer, which patients should still be seen, visitor policies, how to segregate waiting rooms, or how to protect providers. Despite a lack of definitive knowledge, we must make critical decisions and know that recommendations can change hourly. As the Chief Clinical Officer at Michigan Medicine, I am spending 16 hours a day immersed in these decisions and find that one of my critical jobs is to keep people from panicking.
Schools, bars, restaurants, churches and other public gathering places are closing. Three countries (to date) have instituted complete quarantine. Digestive Disease Week® has been cancelled. We are entering a time in which normal life is altered and many changes will open up our thinking about long-term alternative processes.
COVID-19 will define this generation. The public will understand the real need for science, policies based on real facts, robust public health systems, and leaders who inspire confidence based on expert guidance. And, I believe we will see gastroenterologists, health systems, hospitals, and practices all showing us what our “finest hours” look like.
John I. Allen, MD, MBA, AGAF
Editor in Chief