User login
Possible role of enterovirus infection in acute flaccid myelitis cases detected
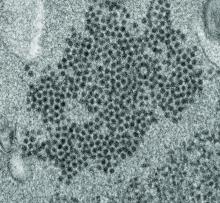
High levels of enterovirus (EV) peptides were found in the cerebrospinal fluid (CSF) and serum samples of individuals with acute flaccid myelitis (AFM) that were not present in a variety of control individuals, according to the results of a small study of patients with and without AFM published online in mBio.
In 2018, CSF samples from AFM patients were investigated by viral-capture high-throughput sequencing. These CSF and serum samples, as well as those from multiple controls, were tested for antibodies to human EVs using peptide microarrays, according to Nischay Mishra, PhD, of Columbia University, New York, and colleagues.
Although EV RNA was confirmed in CSF from only 1 adult AFM case and 1 non-AFM case, antibodies to EV peptides were present in 11 of 14 AFM patients (79%), which was a significantly higher rate than in control groups, including non-AFM patients (1 of 5, or 20%), children with Kawasaki disease (0 of 10), and adults with non-AFM CNS diseases (2 of 11, 18%), according to the authors.
In addition, 6 of 14 (43%) CSF samples and 8 of 11 (73%) serum samples from AFM patients were immunoreactive to an EV-D68–specific peptide, whereas samples from the three control groups were not immunoreactive in either CSF or sera. Previous studies have suggested that infection with EV-D68 and EV-A71 may contribute to AFM.
“There have been 570 confirmed cases since CDC began tracking AFM in August 2014. AFM outbreaks were reported to the CDC in 2014, 2016, and 2018. AFM affects the spinal cord and is characterized by the sudden onset of muscle weakness in one or more limbs. Spikes in AFM cases, primarily in children, have coincided in time and location with outbreaks of EV-D68 and a related enterovirus, EV-A71,” according to an NIH media advisory discussing the article.
In particular, as the study authors point out, a potential link to EV-D68 has also been based on the presence of viral RNA in some respiratory and stool specimens and the observation that EV-D68 infection can result in spinal cord infection.
“While other etiologies of AFM continue to be investigated, our study provides further evidence that EV infection may be a factor in AFM. In the absence of direct detection of a pathogen, antibody evidence of pathogen exposure within the CNS can be an important indicator of the underlying cause of disease,” Dr. Mishra and his colleagues added.
“These initial results may provide avenues to further explore how exposure to EV may contribute to AFM as well as the development of diagnostic tools and treatments,” the researchers concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no competing financial interests.
SOURCE: Mishra N et al. mBio. 2019 Aug;10(4):e01903-19.
High levels of enterovirus (EV) peptides were found in the cerebrospinal fluid (CSF) and serum samples of individuals with acute flaccid myelitis (AFM) that were not present in a variety of control individuals, according to the results of a small study of patients with and without AFM published online in mBio.
In 2018, CSF samples from AFM patients were investigated by viral-capture high-throughput sequencing. These CSF and serum samples, as well as those from multiple controls, were tested for antibodies to human EVs using peptide microarrays, according to Nischay Mishra, PhD, of Columbia University, New York, and colleagues.
Although EV RNA was confirmed in CSF from only 1 adult AFM case and 1 non-AFM case, antibodies to EV peptides were present in 11 of 14 AFM patients (79%), which was a significantly higher rate than in control groups, including non-AFM patients (1 of 5, or 20%), children with Kawasaki disease (0 of 10), and adults with non-AFM CNS diseases (2 of 11, 18%), according to the authors.
In addition, 6 of 14 (43%) CSF samples and 8 of 11 (73%) serum samples from AFM patients were immunoreactive to an EV-D68–specific peptide, whereas samples from the three control groups were not immunoreactive in either CSF or sera. Previous studies have suggested that infection with EV-D68 and EV-A71 may contribute to AFM.
“There have been 570 confirmed cases since CDC began tracking AFM in August 2014. AFM outbreaks were reported to the CDC in 2014, 2016, and 2018. AFM affects the spinal cord and is characterized by the sudden onset of muscle weakness in one or more limbs. Spikes in AFM cases, primarily in children, have coincided in time and location with outbreaks of EV-D68 and a related enterovirus, EV-A71,” according to an NIH media advisory discussing the article.
In particular, as the study authors point out, a potential link to EV-D68 has also been based on the presence of viral RNA in some respiratory and stool specimens and the observation that EV-D68 infection can result in spinal cord infection.
“While other etiologies of AFM continue to be investigated, our study provides further evidence that EV infection may be a factor in AFM. In the absence of direct detection of a pathogen, antibody evidence of pathogen exposure within the CNS can be an important indicator of the underlying cause of disease,” Dr. Mishra and his colleagues added.
“These initial results may provide avenues to further explore how exposure to EV may contribute to AFM as well as the development of diagnostic tools and treatments,” the researchers concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no competing financial interests.
SOURCE: Mishra N et al. mBio. 2019 Aug;10(4):e01903-19.
High levels of enterovirus (EV) peptides were found in the cerebrospinal fluid (CSF) and serum samples of individuals with acute flaccid myelitis (AFM) that were not present in a variety of control individuals, according to the results of a small study of patients with and without AFM published online in mBio.
In 2018, CSF samples from AFM patients were investigated by viral-capture high-throughput sequencing. These CSF and serum samples, as well as those from multiple controls, were tested for antibodies to human EVs using peptide microarrays, according to Nischay Mishra, PhD, of Columbia University, New York, and colleagues.
Although EV RNA was confirmed in CSF from only 1 adult AFM case and 1 non-AFM case, antibodies to EV peptides were present in 11 of 14 AFM patients (79%), which was a significantly higher rate than in control groups, including non-AFM patients (1 of 5, or 20%), children with Kawasaki disease (0 of 10), and adults with non-AFM CNS diseases (2 of 11, 18%), according to the authors.
In addition, 6 of 14 (43%) CSF samples and 8 of 11 (73%) serum samples from AFM patients were immunoreactive to an EV-D68–specific peptide, whereas samples from the three control groups were not immunoreactive in either CSF or sera. Previous studies have suggested that infection with EV-D68 and EV-A71 may contribute to AFM.
“There have been 570 confirmed cases since CDC began tracking AFM in August 2014. AFM outbreaks were reported to the CDC in 2014, 2016, and 2018. AFM affects the spinal cord and is characterized by the sudden onset of muscle weakness in one or more limbs. Spikes in AFM cases, primarily in children, have coincided in time and location with outbreaks of EV-D68 and a related enterovirus, EV-A71,” according to an NIH media advisory discussing the article.
In particular, as the study authors point out, a potential link to EV-D68 has also been based on the presence of viral RNA in some respiratory and stool specimens and the observation that EV-D68 infection can result in spinal cord infection.
“While other etiologies of AFM continue to be investigated, our study provides further evidence that EV infection may be a factor in AFM. In the absence of direct detection of a pathogen, antibody evidence of pathogen exposure within the CNS can be an important indicator of the underlying cause of disease,” Dr. Mishra and his colleagues added.
“These initial results may provide avenues to further explore how exposure to EV may contribute to AFM as well as the development of diagnostic tools and treatments,” the researchers concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no competing financial interests.
SOURCE: Mishra N et al. mBio. 2019 Aug;10(4):e01903-19.
FROM MBIO
Key clinical point:
Major finding: EV peptide antibodies were present in 11 of 14 AFM patients (79%), significantly higher than in controls.
Study details: A peptide microarray analysis was performed on CSF and sera from 14 AFM patients, as well as three control groups of 5 pediatric and adult patients with a non-AFM CNS diseases, 10 children with Kawasaki disease, and 10 adult patients with non-AFM CNS diseases.
Disclosures: The study was funded by the National Institutes of Health. The authors reported that they had no conflicts.
Source: Mishra N et al. mBio. 2019 Aug;10(4):e01903-19.
Low benefits spur alternative drug cost proposals
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
Serum neurofilament light chain level may indicate MS disease activity
according to an investigation published online August 12 in JAMA Neurology. Furthermore, changes in sNfL levels are associated with disability worsening, and sNfL levels may be influenced by treatment. These data support the potential of sNfL as an objective surrogate of ongoing MS disease activity, according to the researchers.
Neuronal and axonal loss increase levels of NfL in cerebrospinal fluid (CSF) in patients with MS. Previous research indicated that sNfL levels are correlated with CSF levels of NfL and are associated with clinical and imaging measures of disease activity. For the purpose of repeated sampling, collecting blood from patients would be more practical than performing lumbar punctures, said the investigators. No long-term studies of sNfL concentrations and their associations with MS disease outcomes had been performed, however.
Ester Cantó, PhD, of the University of California, San Francisco (UCSF), and colleagues examined data from the prospective Expression, Proteomics, Imaging, Clinical (EPIC) study to assess sNfL as a biomarker of MS disease activity and progression. The ongoing EPIC study is being conducted at UCSF. Dr. Cantó and colleagues analyzed data collected from July 1, 2004, through August 31, 2017, for 607 patients with MS. Participants underwent clinical examinations and serum sample collections annually for 5 years, then at various time points for as long as 12 years. The median follow-up duration was 10 years. The researchers measured sNfL levels with a sensitive single-molecule array platform and compared them with clinical and MRI variables using univariable and multivariable analyses. Dr. Cantó and colleagues chose disability progression, defined as clinically significant worsening on the Expanded Disability Status Scale (EDSS) score, and brain fraction atrophy as their primary outcomes.
The population’s mean age was 42.5 years. About 70% of participants were women, and all were of non-Hispanic European descent. At baseline, sNfL levels were significantly associated with EDSS score, MS subtype, and treatment status.
Dr. Cantó and colleagues found a significant interaction between EDSS worsening and change in levels of sNfL over time. Baseline sNfL levels were associated with approximately 11.6% of the variance in participants’ brain fraction atrophy at year 10. When the investigators controlled for sex, age, and disease duration, they found that baseline sNfL levels were associated with 18% of the variance in brain fraction atrophy at year 10. After 5 years’ follow-up, active treatment was associated with lower levels of sNfL. High-efficacy treatments were associated with greater decreases in sNfL levels, compared with platform therapies.
More frequent sample acquisition could provide greater detail about changes in sNfL levels, wrote Dr. Cantó and colleagues. They acknowledged that their study had insufficient power for the researchers to assess the outcomes of individual MS therapies. Other limitations included the lack of data on NfL stability and the lack of a group of healthy controls.
“For an individual patient, the biomarker prognostic power of sNfL level for clinical and MRI outcomes was limited,” said the investigators. “Further prospective studies are necessary to assess the assay’s utility for decision making in individual patients.”
The National Institutes of Health and the U.S. National MS Society supported the study. Several of the investigators received compensation from Novartis, which provided funds for the reagents needed for the single-molecule array assay.
SOURCE: Cantó E et al. JAMA Neurol. 2019 Aug. 12. doi: 10.1001/jamaneurol.2019.2137.
according to an investigation published online August 12 in JAMA Neurology. Furthermore, changes in sNfL levels are associated with disability worsening, and sNfL levels may be influenced by treatment. These data support the potential of sNfL as an objective surrogate of ongoing MS disease activity, according to the researchers.
Neuronal and axonal loss increase levels of NfL in cerebrospinal fluid (CSF) in patients with MS. Previous research indicated that sNfL levels are correlated with CSF levels of NfL and are associated with clinical and imaging measures of disease activity. For the purpose of repeated sampling, collecting blood from patients would be more practical than performing lumbar punctures, said the investigators. No long-term studies of sNfL concentrations and their associations with MS disease outcomes had been performed, however.
Ester Cantó, PhD, of the University of California, San Francisco (UCSF), and colleagues examined data from the prospective Expression, Proteomics, Imaging, Clinical (EPIC) study to assess sNfL as a biomarker of MS disease activity and progression. The ongoing EPIC study is being conducted at UCSF. Dr. Cantó and colleagues analyzed data collected from July 1, 2004, through August 31, 2017, for 607 patients with MS. Participants underwent clinical examinations and serum sample collections annually for 5 years, then at various time points for as long as 12 years. The median follow-up duration was 10 years. The researchers measured sNfL levels with a sensitive single-molecule array platform and compared them with clinical and MRI variables using univariable and multivariable analyses. Dr. Cantó and colleagues chose disability progression, defined as clinically significant worsening on the Expanded Disability Status Scale (EDSS) score, and brain fraction atrophy as their primary outcomes.
The population’s mean age was 42.5 years. About 70% of participants were women, and all were of non-Hispanic European descent. At baseline, sNfL levels were significantly associated with EDSS score, MS subtype, and treatment status.
Dr. Cantó and colleagues found a significant interaction between EDSS worsening and change in levels of sNfL over time. Baseline sNfL levels were associated with approximately 11.6% of the variance in participants’ brain fraction atrophy at year 10. When the investigators controlled for sex, age, and disease duration, they found that baseline sNfL levels were associated with 18% of the variance in brain fraction atrophy at year 10. After 5 years’ follow-up, active treatment was associated with lower levels of sNfL. High-efficacy treatments were associated with greater decreases in sNfL levels, compared with platform therapies.
More frequent sample acquisition could provide greater detail about changes in sNfL levels, wrote Dr. Cantó and colleagues. They acknowledged that their study had insufficient power for the researchers to assess the outcomes of individual MS therapies. Other limitations included the lack of data on NfL stability and the lack of a group of healthy controls.
“For an individual patient, the biomarker prognostic power of sNfL level for clinical and MRI outcomes was limited,” said the investigators. “Further prospective studies are necessary to assess the assay’s utility for decision making in individual patients.”
The National Institutes of Health and the U.S. National MS Society supported the study. Several of the investigators received compensation from Novartis, which provided funds for the reagents needed for the single-molecule array assay.
SOURCE: Cantó E et al. JAMA Neurol. 2019 Aug. 12. doi: 10.1001/jamaneurol.2019.2137.
according to an investigation published online August 12 in JAMA Neurology. Furthermore, changes in sNfL levels are associated with disability worsening, and sNfL levels may be influenced by treatment. These data support the potential of sNfL as an objective surrogate of ongoing MS disease activity, according to the researchers.
Neuronal and axonal loss increase levels of NfL in cerebrospinal fluid (CSF) in patients with MS. Previous research indicated that sNfL levels are correlated with CSF levels of NfL and are associated with clinical and imaging measures of disease activity. For the purpose of repeated sampling, collecting blood from patients would be more practical than performing lumbar punctures, said the investigators. No long-term studies of sNfL concentrations and their associations with MS disease outcomes had been performed, however.
Ester Cantó, PhD, of the University of California, San Francisco (UCSF), and colleagues examined data from the prospective Expression, Proteomics, Imaging, Clinical (EPIC) study to assess sNfL as a biomarker of MS disease activity and progression. The ongoing EPIC study is being conducted at UCSF. Dr. Cantó and colleagues analyzed data collected from July 1, 2004, through August 31, 2017, for 607 patients with MS. Participants underwent clinical examinations and serum sample collections annually for 5 years, then at various time points for as long as 12 years. The median follow-up duration was 10 years. The researchers measured sNfL levels with a sensitive single-molecule array platform and compared them with clinical and MRI variables using univariable and multivariable analyses. Dr. Cantó and colleagues chose disability progression, defined as clinically significant worsening on the Expanded Disability Status Scale (EDSS) score, and brain fraction atrophy as their primary outcomes.
The population’s mean age was 42.5 years. About 70% of participants were women, and all were of non-Hispanic European descent. At baseline, sNfL levels were significantly associated with EDSS score, MS subtype, and treatment status.
Dr. Cantó and colleagues found a significant interaction between EDSS worsening and change in levels of sNfL over time. Baseline sNfL levels were associated with approximately 11.6% of the variance in participants’ brain fraction atrophy at year 10. When the investigators controlled for sex, age, and disease duration, they found that baseline sNfL levels were associated with 18% of the variance in brain fraction atrophy at year 10. After 5 years’ follow-up, active treatment was associated with lower levels of sNfL. High-efficacy treatments were associated with greater decreases in sNfL levels, compared with platform therapies.
More frequent sample acquisition could provide greater detail about changes in sNfL levels, wrote Dr. Cantó and colleagues. They acknowledged that their study had insufficient power for the researchers to assess the outcomes of individual MS therapies. Other limitations included the lack of data on NfL stability and the lack of a group of healthy controls.
“For an individual patient, the biomarker prognostic power of sNfL level for clinical and MRI outcomes was limited,” said the investigators. “Further prospective studies are necessary to assess the assay’s utility for decision making in individual patients.”
The National Institutes of Health and the U.S. National MS Society supported the study. Several of the investigators received compensation from Novartis, which provided funds for the reagents needed for the single-molecule array assay.
SOURCE: Cantó E et al. JAMA Neurol. 2019 Aug. 12. doi: 10.1001/jamaneurol.2019.2137.
FROM JAMA NEUROLOGY
Key clinical point: Serum neurofilament light chain level has potential as a surrogate of ongoing MS disease activity.
Major finding: Serum neurofilament light chain level is associated with brain fraction atrophy.
Study details: An ongoing, prospective, observational study of 607 patients with MS.
Disclosures: The National Institutes of Health and the U.S. National MS Society supported the study. Several of the investigators received compensation from Novartis, which provided funds for the reagents needed for the single-molecule array assay.
Source: Cantó E et al. JAMA Neurol. 2019 Aug 12. doi: 10.1001/jamaneurol.2019.2137.
Midlife hypertension is associated with subsequent risk of dementia
Uncontrolled hypertension among individuals aged 45-65 years of age is associated with an increased risk of subsequent dementia, according to a relatively large prospective population-based cohort study that followed patients for almost 30 years.
Even though previously published studies have not conclusively linked blood pressure control with a reduction in dementia risk, a second study, published simultaneously, did link blood pressure control with a smaller increase in white matter lesions, which are a marker of dementia risk. However, a reduction in total brain volume that accompanied this protection raised concern.
In the first of the two reports published Aug. 13 in JAMA, individuals 45-65 years of age participating in the Atherosclerosis Risk in Communities (ARIC) study were followed for cognitive function in relation to blood pressure. The baseline visit took place in 1987-1989. Cognitive function was also evaluated at the fifth visit, which took place in 2011-2013, and the sixth visit, which took place in 2016-2017.
At the sixth visit, the incidence of dementia among patients who were normotensive at baseline and also normotensive at the fifth visit was 1.31 per 100 person-years. For those with hypertension (greater than 140/90 mm Hg) at the fifth visit but normotensive at baseline, the incidence was 1.99 per 100 patient-years. For those with hypertension at both time points, the incidence was 4.26 per 100 patient-years.
When translated into hazard ratios, those with midlife and late-life hypertension were nearly 50% more likely to develop dementia (HR, 1.49) relative to those who remained normotensive. For those who had only midlife hypertension, the risk was also significantly increased (HR, 1.41) relative to those who remained normotensive at both time points.
Those with midlife hypertension but late-life hypotension were also found to be at greater risk of dementia (HR, 1.62) relative to those who remained normotensive.
These data support the premise that uncontrolled midlife hypertension increases risk of dementia but do not touch on whether blood pressure reductions reduce this risk. However, a second study published simultaneously provided at least some evidence that blood pressure control might offer some protection.
In this report, which is a substudy of the previously published Systolic Blood Pressure Intervention Trial (SPRINT) MIND trial, brain volume changes were evaluated via MRI in 449 of the more than 2,000 patients included in the previously published trial (Williamson JD et al. JAMA. 2019;321[6]:553-61).
After a median 3.4 years of follow-up, mean white matter lesion volume increased only 0.92 cm3 in patients receiving intensive systolic blood pressure control, defined as less than 120 mm Hg, versus 1.45 cm3 in those with higher systolic blood pressures.
These substudy data are encouraging, but it is important to recognize that the previously published and larger SPRINT MIND trial did not achieve its endpoint. In that study, the protection against dementia was nonsignificant (HR, 0.83; 95% confidence interval, 0.67-1.04).
In addition, the lower loss in white matter volume with intensive blood pressure lowering in the MRI substudy was accompanied with a greater loss in total brain volume (–30.6 vs. –26.9 cm3), which is considered a potentially negative effect.
As a result, the picture for risk management remains unclear, according to an editorial that accompanied publication of both studies.
“The important clinical question is whether changes of a few cubic millimeters in white matter hyperintensity volume or brain make a difference on brain function,” observed the author of the editorial, Shyam Prabhakaran, MD, of the department of neurology at the University of Chicago.
He believes that there are several findings from both studies that are “encouraging” in regard to blood pressure control for the prevention of dementia, but he also listed many unanswered questions, including why benefits observed to date have been so modest. He speculated that meaningful clinical benefits might depend on a multimodal approach that includes modification of other vascular risk factors, such as elevated lipids.
He also suggested that many issues regarding intensive blood pressure control for preventing dementia are unresolved, suggesting the need for more studies.
Not least, “later blood-pressure lowering interventions require careful monitoring for the potential cognitive harm associated with late-life hypotension,” Dr. Prabhakaran noted. Calling the effects of blood pressure control on brain health “nuanced,” he concluded that there is an opportunity for blood pressure modifications to prevent dementia, but stressed that optimal blood pressure targets for the purposes of preventing dementia are unknown.
The ARIC and SPRINT studies are supported by the National Institutes of Health. Several authors reported relationships with industry but no conflicts of interest relevant to this study.
SOURCES: Walker KA et al. JAMA. 2019;322(6):535-45; SPRINT MIND investigators. JAMA. 2019;322(6):524-34; Prabhakaran S. JAMA. 2019;322(6):512-3
Uncontrolled hypertension among individuals aged 45-65 years of age is associated with an increased risk of subsequent dementia, according to a relatively large prospective population-based cohort study that followed patients for almost 30 years.
Even though previously published studies have not conclusively linked blood pressure control with a reduction in dementia risk, a second study, published simultaneously, did link blood pressure control with a smaller increase in white matter lesions, which are a marker of dementia risk. However, a reduction in total brain volume that accompanied this protection raised concern.
In the first of the two reports published Aug. 13 in JAMA, individuals 45-65 years of age participating in the Atherosclerosis Risk in Communities (ARIC) study were followed for cognitive function in relation to blood pressure. The baseline visit took place in 1987-1989. Cognitive function was also evaluated at the fifth visit, which took place in 2011-2013, and the sixth visit, which took place in 2016-2017.
At the sixth visit, the incidence of dementia among patients who were normotensive at baseline and also normotensive at the fifth visit was 1.31 per 100 person-years. For those with hypertension (greater than 140/90 mm Hg) at the fifth visit but normotensive at baseline, the incidence was 1.99 per 100 patient-years. For those with hypertension at both time points, the incidence was 4.26 per 100 patient-years.
When translated into hazard ratios, those with midlife and late-life hypertension were nearly 50% more likely to develop dementia (HR, 1.49) relative to those who remained normotensive. For those who had only midlife hypertension, the risk was also significantly increased (HR, 1.41) relative to those who remained normotensive at both time points.
Those with midlife hypertension but late-life hypotension were also found to be at greater risk of dementia (HR, 1.62) relative to those who remained normotensive.
These data support the premise that uncontrolled midlife hypertension increases risk of dementia but do not touch on whether blood pressure reductions reduce this risk. However, a second study published simultaneously provided at least some evidence that blood pressure control might offer some protection.
In this report, which is a substudy of the previously published Systolic Blood Pressure Intervention Trial (SPRINT) MIND trial, brain volume changes were evaluated via MRI in 449 of the more than 2,000 patients included in the previously published trial (Williamson JD et al. JAMA. 2019;321[6]:553-61).
After a median 3.4 years of follow-up, mean white matter lesion volume increased only 0.92 cm3 in patients receiving intensive systolic blood pressure control, defined as less than 120 mm Hg, versus 1.45 cm3 in those with higher systolic blood pressures.
These substudy data are encouraging, but it is important to recognize that the previously published and larger SPRINT MIND trial did not achieve its endpoint. In that study, the protection against dementia was nonsignificant (HR, 0.83; 95% confidence interval, 0.67-1.04).
In addition, the lower loss in white matter volume with intensive blood pressure lowering in the MRI substudy was accompanied with a greater loss in total brain volume (–30.6 vs. –26.9 cm3), which is considered a potentially negative effect.
As a result, the picture for risk management remains unclear, according to an editorial that accompanied publication of both studies.
“The important clinical question is whether changes of a few cubic millimeters in white matter hyperintensity volume or brain make a difference on brain function,” observed the author of the editorial, Shyam Prabhakaran, MD, of the department of neurology at the University of Chicago.
He believes that there are several findings from both studies that are “encouraging” in regard to blood pressure control for the prevention of dementia, but he also listed many unanswered questions, including why benefits observed to date have been so modest. He speculated that meaningful clinical benefits might depend on a multimodal approach that includes modification of other vascular risk factors, such as elevated lipids.
He also suggested that many issues regarding intensive blood pressure control for preventing dementia are unresolved, suggesting the need for more studies.
Not least, “later blood-pressure lowering interventions require careful monitoring for the potential cognitive harm associated with late-life hypotension,” Dr. Prabhakaran noted. Calling the effects of blood pressure control on brain health “nuanced,” he concluded that there is an opportunity for blood pressure modifications to prevent dementia, but stressed that optimal blood pressure targets for the purposes of preventing dementia are unknown.
The ARIC and SPRINT studies are supported by the National Institutes of Health. Several authors reported relationships with industry but no conflicts of interest relevant to this study.
SOURCES: Walker KA et al. JAMA. 2019;322(6):535-45; SPRINT MIND investigators. JAMA. 2019;322(6):524-34; Prabhakaran S. JAMA. 2019;322(6):512-3
Uncontrolled hypertension among individuals aged 45-65 years of age is associated with an increased risk of subsequent dementia, according to a relatively large prospective population-based cohort study that followed patients for almost 30 years.
Even though previously published studies have not conclusively linked blood pressure control with a reduction in dementia risk, a second study, published simultaneously, did link blood pressure control with a smaller increase in white matter lesions, which are a marker of dementia risk. However, a reduction in total brain volume that accompanied this protection raised concern.
In the first of the two reports published Aug. 13 in JAMA, individuals 45-65 years of age participating in the Atherosclerosis Risk in Communities (ARIC) study were followed for cognitive function in relation to blood pressure. The baseline visit took place in 1987-1989. Cognitive function was also evaluated at the fifth visit, which took place in 2011-2013, and the sixth visit, which took place in 2016-2017.
At the sixth visit, the incidence of dementia among patients who were normotensive at baseline and also normotensive at the fifth visit was 1.31 per 100 person-years. For those with hypertension (greater than 140/90 mm Hg) at the fifth visit but normotensive at baseline, the incidence was 1.99 per 100 patient-years. For those with hypertension at both time points, the incidence was 4.26 per 100 patient-years.
When translated into hazard ratios, those with midlife and late-life hypertension were nearly 50% more likely to develop dementia (HR, 1.49) relative to those who remained normotensive. For those who had only midlife hypertension, the risk was also significantly increased (HR, 1.41) relative to those who remained normotensive at both time points.
Those with midlife hypertension but late-life hypotension were also found to be at greater risk of dementia (HR, 1.62) relative to those who remained normotensive.
These data support the premise that uncontrolled midlife hypertension increases risk of dementia but do not touch on whether blood pressure reductions reduce this risk. However, a second study published simultaneously provided at least some evidence that blood pressure control might offer some protection.
In this report, which is a substudy of the previously published Systolic Blood Pressure Intervention Trial (SPRINT) MIND trial, brain volume changes were evaluated via MRI in 449 of the more than 2,000 patients included in the previously published trial (Williamson JD et al. JAMA. 2019;321[6]:553-61).
After a median 3.4 years of follow-up, mean white matter lesion volume increased only 0.92 cm3 in patients receiving intensive systolic blood pressure control, defined as less than 120 mm Hg, versus 1.45 cm3 in those with higher systolic blood pressures.
These substudy data are encouraging, but it is important to recognize that the previously published and larger SPRINT MIND trial did not achieve its endpoint. In that study, the protection against dementia was nonsignificant (HR, 0.83; 95% confidence interval, 0.67-1.04).
In addition, the lower loss in white matter volume with intensive blood pressure lowering in the MRI substudy was accompanied with a greater loss in total brain volume (–30.6 vs. –26.9 cm3), which is considered a potentially negative effect.
As a result, the picture for risk management remains unclear, according to an editorial that accompanied publication of both studies.
“The important clinical question is whether changes of a few cubic millimeters in white matter hyperintensity volume or brain make a difference on brain function,” observed the author of the editorial, Shyam Prabhakaran, MD, of the department of neurology at the University of Chicago.
He believes that there are several findings from both studies that are “encouraging” in regard to blood pressure control for the prevention of dementia, but he also listed many unanswered questions, including why benefits observed to date have been so modest. He speculated that meaningful clinical benefits might depend on a multimodal approach that includes modification of other vascular risk factors, such as elevated lipids.
He also suggested that many issues regarding intensive blood pressure control for preventing dementia are unresolved, suggesting the need for more studies.
Not least, “later blood-pressure lowering interventions require careful monitoring for the potential cognitive harm associated with late-life hypotension,” Dr. Prabhakaran noted. Calling the effects of blood pressure control on brain health “nuanced,” he concluded that there is an opportunity for blood pressure modifications to prevent dementia, but stressed that optimal blood pressure targets for the purposes of preventing dementia are unknown.
The ARIC and SPRINT studies are supported by the National Institutes of Health. Several authors reported relationships with industry but no conflicts of interest relevant to this study.
SOURCES: Walker KA et al. JAMA. 2019;322(6):535-45; SPRINT MIND investigators. JAMA. 2019;322(6):524-34; Prabhakaran S. JAMA. 2019;322(6):512-3
FROM JAMA
Bisphosphonates improve BMD in pediatric rheumatic disease
Prophylactic treatment with bisphosphonates could significantly improve bone mineral density (BMD) in children and adolescents receiving steroids for chronic rheumatic disease, a study has found.
A paper published in EClinicalMedicine reported the outcomes of a multicenter, double-dummy, double-blind, placebo-controlled trial involving 217 patients who were receiving steroid therapy for juvenile idiopathic arthritis, juvenile systemic lupus erythematosus, juvenile dermatomyositis, or juvenile vasculitis. The patients were randomized to risedronate, alfacalcidol, or placebo, and all of the participants received 500 mg calcium and 400 IU vitamin D daily.
Lumbar spine and total body (less head) BMD increased in all groups, but the greatest increase was seen in patients treated with risedronate.
After 1 year, lumbar spine and total body (less head) BMD had increased in all groups, compared with baseline, but the greatest increase was seen in patients who had been treated with risedronate.
The lumbar spine areal BMD z score remained the same in the placebo group (−1.15 to −1.13), decreased from −0.96 to −1.00 in the alfacalcidol group, and increased from −0.99 to −0.75 in the risedronate group.
The change in z scores was significantly different between placebo and risedronate groups, and between risedronate and alfacalcidol groups, but not between placebo and alfacalcidol.
“The acquisition of adequate peak bone mass is not only important for the young person in reducing fracture risk but also has significant implications for the development of osteoporosis in later life, if peak bone mass is suboptimal,” wrote Madeleine Rooney, MBBCH, from the Queens University of Belfast, Northern Ireland, and associates.
There were no significant differences between the three groups in fracture rates. However, researchers were also able to compare Genant scores for vertebral fractures in 187 patients with pre- and posttreatment lateral spinal x-rays. That showed that the 54 patients in the placebo arm and 52 patients in the alfacalcidol arm had no change in their baseline Genant score of 0 (normal). However, although all 53 patients in the risedronate group had a Genant score of 0 at baseline, at 1-year follow-up, 2 patients had a Genant score of 1 (mild fracture), and 1 patient had a score of 3 (severe fracture).
In biochemical parameters, researchers saw a drop in parathyroid hormone in the placebo and alfacalcidol groups, but a rise in the risedronate group. However, the authors were not able to see any changes in bone markers that might have indicated which patients responded better to treatment.
Around 90% of participants in each group were also being treated with disease-modifying antirheumatic drugs. The rates of biologic use were 10.5% in the placebo group, 23.9% in the alfacalcidol group, and 10.1% in the risedronate group.
The researchers also noted a 7% higher rate of serious adverse events in the risedronate group, but emphasized that there were no differences in events related to the treatment.
In an accompanying editorial, Ian R. Reid, MBBCH, of the department of medicine, University of Auckland (New Zealand) noted that the study was an important step toward finding interventions for the prevention of steroid-induced bone loss in children. “The present study indicates that risedronate, and probably other potent bisphosphonates, can provide bone preservation in children and young people receiving therapeutic doses of glucocorticoid drugs, whereas alfacalcidol is without benefit. The targeted use of bisphosphonates in children and young people judged to be at significant fracture risk is appropriate. However, whether preventing loss of bone density will reduce fracture incidence remains to be established.”
The study was funded by Arthritis Research UK. No conflicts of interest were declared.
SOURCE: Rooney M et al. EClinicalMedicine. 2019 Jul 3. doi: 10.1016/j.eclinm.2019.06.004.
Prophylactic treatment with bisphosphonates could significantly improve bone mineral density (BMD) in children and adolescents receiving steroids for chronic rheumatic disease, a study has found.
A paper published in EClinicalMedicine reported the outcomes of a multicenter, double-dummy, double-blind, placebo-controlled trial involving 217 patients who were receiving steroid therapy for juvenile idiopathic arthritis, juvenile systemic lupus erythematosus, juvenile dermatomyositis, or juvenile vasculitis. The patients were randomized to risedronate, alfacalcidol, or placebo, and all of the participants received 500 mg calcium and 400 IU vitamin D daily.
Lumbar spine and total body (less head) BMD increased in all groups, but the greatest increase was seen in patients treated with risedronate.
After 1 year, lumbar spine and total body (less head) BMD had increased in all groups, compared with baseline, but the greatest increase was seen in patients who had been treated with risedronate.
The lumbar spine areal BMD z score remained the same in the placebo group (−1.15 to −1.13), decreased from −0.96 to −1.00 in the alfacalcidol group, and increased from −0.99 to −0.75 in the risedronate group.
The change in z scores was significantly different between placebo and risedronate groups, and between risedronate and alfacalcidol groups, but not between placebo and alfacalcidol.
“The acquisition of adequate peak bone mass is not only important for the young person in reducing fracture risk but also has significant implications for the development of osteoporosis in later life, if peak bone mass is suboptimal,” wrote Madeleine Rooney, MBBCH, from the Queens University of Belfast, Northern Ireland, and associates.
There were no significant differences between the three groups in fracture rates. However, researchers were also able to compare Genant scores for vertebral fractures in 187 patients with pre- and posttreatment lateral spinal x-rays. That showed that the 54 patients in the placebo arm and 52 patients in the alfacalcidol arm had no change in their baseline Genant score of 0 (normal). However, although all 53 patients in the risedronate group had a Genant score of 0 at baseline, at 1-year follow-up, 2 patients had a Genant score of 1 (mild fracture), and 1 patient had a score of 3 (severe fracture).
In biochemical parameters, researchers saw a drop in parathyroid hormone in the placebo and alfacalcidol groups, but a rise in the risedronate group. However, the authors were not able to see any changes in bone markers that might have indicated which patients responded better to treatment.
Around 90% of participants in each group were also being treated with disease-modifying antirheumatic drugs. The rates of biologic use were 10.5% in the placebo group, 23.9% in the alfacalcidol group, and 10.1% in the risedronate group.
The researchers also noted a 7% higher rate of serious adverse events in the risedronate group, but emphasized that there were no differences in events related to the treatment.
In an accompanying editorial, Ian R. Reid, MBBCH, of the department of medicine, University of Auckland (New Zealand) noted that the study was an important step toward finding interventions for the prevention of steroid-induced bone loss in children. “The present study indicates that risedronate, and probably other potent bisphosphonates, can provide bone preservation in children and young people receiving therapeutic doses of glucocorticoid drugs, whereas alfacalcidol is without benefit. The targeted use of bisphosphonates in children and young people judged to be at significant fracture risk is appropriate. However, whether preventing loss of bone density will reduce fracture incidence remains to be established.”
The study was funded by Arthritis Research UK. No conflicts of interest were declared.
SOURCE: Rooney M et al. EClinicalMedicine. 2019 Jul 3. doi: 10.1016/j.eclinm.2019.06.004.
Prophylactic treatment with bisphosphonates could significantly improve bone mineral density (BMD) in children and adolescents receiving steroids for chronic rheumatic disease, a study has found.
A paper published in EClinicalMedicine reported the outcomes of a multicenter, double-dummy, double-blind, placebo-controlled trial involving 217 patients who were receiving steroid therapy for juvenile idiopathic arthritis, juvenile systemic lupus erythematosus, juvenile dermatomyositis, or juvenile vasculitis. The patients were randomized to risedronate, alfacalcidol, or placebo, and all of the participants received 500 mg calcium and 400 IU vitamin D daily.
Lumbar spine and total body (less head) BMD increased in all groups, but the greatest increase was seen in patients treated with risedronate.
After 1 year, lumbar spine and total body (less head) BMD had increased in all groups, compared with baseline, but the greatest increase was seen in patients who had been treated with risedronate.
The lumbar spine areal BMD z score remained the same in the placebo group (−1.15 to −1.13), decreased from −0.96 to −1.00 in the alfacalcidol group, and increased from −0.99 to −0.75 in the risedronate group.
The change in z scores was significantly different between placebo and risedronate groups, and between risedronate and alfacalcidol groups, but not between placebo and alfacalcidol.
“The acquisition of adequate peak bone mass is not only important for the young person in reducing fracture risk but also has significant implications for the development of osteoporosis in later life, if peak bone mass is suboptimal,” wrote Madeleine Rooney, MBBCH, from the Queens University of Belfast, Northern Ireland, and associates.
There were no significant differences between the three groups in fracture rates. However, researchers were also able to compare Genant scores for vertebral fractures in 187 patients with pre- and posttreatment lateral spinal x-rays. That showed that the 54 patients in the placebo arm and 52 patients in the alfacalcidol arm had no change in their baseline Genant score of 0 (normal). However, although all 53 patients in the risedronate group had a Genant score of 0 at baseline, at 1-year follow-up, 2 patients had a Genant score of 1 (mild fracture), and 1 patient had a score of 3 (severe fracture).
In biochemical parameters, researchers saw a drop in parathyroid hormone in the placebo and alfacalcidol groups, but a rise in the risedronate group. However, the authors were not able to see any changes in bone markers that might have indicated which patients responded better to treatment.
Around 90% of participants in each group were also being treated with disease-modifying antirheumatic drugs. The rates of biologic use were 10.5% in the placebo group, 23.9% in the alfacalcidol group, and 10.1% in the risedronate group.
The researchers also noted a 7% higher rate of serious adverse events in the risedronate group, but emphasized that there were no differences in events related to the treatment.
In an accompanying editorial, Ian R. Reid, MBBCH, of the department of medicine, University of Auckland (New Zealand) noted that the study was an important step toward finding interventions for the prevention of steroid-induced bone loss in children. “The present study indicates that risedronate, and probably other potent bisphosphonates, can provide bone preservation in children and young people receiving therapeutic doses of glucocorticoid drugs, whereas alfacalcidol is without benefit. The targeted use of bisphosphonates in children and young people judged to be at significant fracture risk is appropriate. However, whether preventing loss of bone density will reduce fracture incidence remains to be established.”
The study was funded by Arthritis Research UK. No conflicts of interest were declared.
SOURCE: Rooney M et al. EClinicalMedicine. 2019 Jul 3. doi: 10.1016/j.eclinm.2019.06.004.
FROM ECLINICALMEDICINE
Heart of the Matter
During the last year, the field of psoriasis has continued to expand, with new therapies, new guidelines, and further understanding of the impact of treatment on associated comorbidities.
One of the most exciting prospects of the treatment of psoriasis with biologics is the potential for the reduction in major adverse cardiovascular events (MACEs). It has been well established that psoriasis is associated with increased cardiovascular risk.1,2 Ahlehoff et al1 conducted a cohort study of the entire Danish population 18 years and older followed from 1997 to 2006 by individual-level linkage of nationwide registers. They concluded that psoriasis is associated with increased risk for adverse cardiovascular events and all-cause mortality. Young age, severe skin affection, and/or psoriatic arthritis (PsA) carry the most risk. They suggested that patients with psoriasis may be candidates for early cardiovascular risk factor modification.1
Ogdie et al2 endeavored to quantify the risk for MACE among patients with PsA, rheumatoid arthritis (RA), and psoriasis without known PsA compared to the general population after adjusting for traditional cardiovascular risk factors. Patients with PsA (N=8706), RA (N=41,752), psoriasis (N=138,424), and unexposed controls (N=81,573) were identified. After adjustment for traditional risk factors, the risk for MACE was higher in patients with PsA not prescribed a disease-modifying antirheumatic drug (DMARD)(hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.03-1.49), patients with RA (no DMARD: HR, 1.39; 95% CI, 1.28-1.50; DMARD: HR, 1.58; 95% CI, 1.46-1.70), patients with psoriasis not prescribed a DMARD (HR, 1.08; 95% CI, 1.02-1.15), and patients with severe psoriasis (DMARD: HR, 1.42; 95% CI, 1.17-1.73).2 These data are one aspect of our increasing insight into the management of psoriasis.
To expand on the new guidelines and new therapies presented in 2019, this issue includes review articles looking at these facets. Wu and Weinberg3 review the impact of diet on psoriasis. Pithadia et al4 explain the American Academy of Dermatology and National Psoriasis Foundation guidelines of care for the management of psoriasis with biologics for the prescribing dermatologist, with an emphasis on the most clinically significant considerations during each step of treatment with biologic therapies (ie, choosing a biologic, initiating therapy, assessing treatment response, switching biologics). Havnaer et al5 provide an update on the newly approved and pipeline systemic agents for psoriasis.
We hope that you find this issue enjoyable and informative.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Wu AG, Weinberg JM. The impact of diet on psoriasis. Cutis. 2019;104(suppl 2):7-10.
- Pithadia DJ, Reynolds KA, Lee EB, et al. Translating the 2019 AAD-NPF guidelines of care for the management of psoriasis with biologics to clinical practice. Cutis. 2019;104(suppl 2):12-16, 20.
- Havnaer A, Weinberg JM, Han G. Systemic therapies in psoriasis: an update on newly approved and pipeline biologics and oral treatments. Cutis. 2019;104(suppl 2):17-20.
During the last year, the field of psoriasis has continued to expand, with new therapies, new guidelines, and further understanding of the impact of treatment on associated comorbidities.
One of the most exciting prospects of the treatment of psoriasis with biologics is the potential for the reduction in major adverse cardiovascular events (MACEs). It has been well established that psoriasis is associated with increased cardiovascular risk.1,2 Ahlehoff et al1 conducted a cohort study of the entire Danish population 18 years and older followed from 1997 to 2006 by individual-level linkage of nationwide registers. They concluded that psoriasis is associated with increased risk for adverse cardiovascular events and all-cause mortality. Young age, severe skin affection, and/or psoriatic arthritis (PsA) carry the most risk. They suggested that patients with psoriasis may be candidates for early cardiovascular risk factor modification.1
Ogdie et al2 endeavored to quantify the risk for MACE among patients with PsA, rheumatoid arthritis (RA), and psoriasis without known PsA compared to the general population after adjusting for traditional cardiovascular risk factors. Patients with PsA (N=8706), RA (N=41,752), psoriasis (N=138,424), and unexposed controls (N=81,573) were identified. After adjustment for traditional risk factors, the risk for MACE was higher in patients with PsA not prescribed a disease-modifying antirheumatic drug (DMARD)(hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.03-1.49), patients with RA (no DMARD: HR, 1.39; 95% CI, 1.28-1.50; DMARD: HR, 1.58; 95% CI, 1.46-1.70), patients with psoriasis not prescribed a DMARD (HR, 1.08; 95% CI, 1.02-1.15), and patients with severe psoriasis (DMARD: HR, 1.42; 95% CI, 1.17-1.73).2 These data are one aspect of our increasing insight into the management of psoriasis.
To expand on the new guidelines and new therapies presented in 2019, this issue includes review articles looking at these facets. Wu and Weinberg3 review the impact of diet on psoriasis. Pithadia et al4 explain the American Academy of Dermatology and National Psoriasis Foundation guidelines of care for the management of psoriasis with biologics for the prescribing dermatologist, with an emphasis on the most clinically significant considerations during each step of treatment with biologic therapies (ie, choosing a biologic, initiating therapy, assessing treatment response, switching biologics). Havnaer et al5 provide an update on the newly approved and pipeline systemic agents for psoriasis.
We hope that you find this issue enjoyable and informative.
During the last year, the field of psoriasis has continued to expand, with new therapies, new guidelines, and further understanding of the impact of treatment on associated comorbidities.
One of the most exciting prospects of the treatment of psoriasis with biologics is the potential for the reduction in major adverse cardiovascular events (MACEs). It has been well established that psoriasis is associated with increased cardiovascular risk.1,2 Ahlehoff et al1 conducted a cohort study of the entire Danish population 18 years and older followed from 1997 to 2006 by individual-level linkage of nationwide registers. They concluded that psoriasis is associated with increased risk for adverse cardiovascular events and all-cause mortality. Young age, severe skin affection, and/or psoriatic arthritis (PsA) carry the most risk. They suggested that patients with psoriasis may be candidates for early cardiovascular risk factor modification.1
Ogdie et al2 endeavored to quantify the risk for MACE among patients with PsA, rheumatoid arthritis (RA), and psoriasis without known PsA compared to the general population after adjusting for traditional cardiovascular risk factors. Patients with PsA (N=8706), RA (N=41,752), psoriasis (N=138,424), and unexposed controls (N=81,573) were identified. After adjustment for traditional risk factors, the risk for MACE was higher in patients with PsA not prescribed a disease-modifying antirheumatic drug (DMARD)(hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.03-1.49), patients with RA (no DMARD: HR, 1.39; 95% CI, 1.28-1.50; DMARD: HR, 1.58; 95% CI, 1.46-1.70), patients with psoriasis not prescribed a DMARD (HR, 1.08; 95% CI, 1.02-1.15), and patients with severe psoriasis (DMARD: HR, 1.42; 95% CI, 1.17-1.73).2 These data are one aspect of our increasing insight into the management of psoriasis.
To expand on the new guidelines and new therapies presented in 2019, this issue includes review articles looking at these facets. Wu and Weinberg3 review the impact of diet on psoriasis. Pithadia et al4 explain the American Academy of Dermatology and National Psoriasis Foundation guidelines of care for the management of psoriasis with biologics for the prescribing dermatologist, with an emphasis on the most clinically significant considerations during each step of treatment with biologic therapies (ie, choosing a biologic, initiating therapy, assessing treatment response, switching biologics). Havnaer et al5 provide an update on the newly approved and pipeline systemic agents for psoriasis.
We hope that you find this issue enjoyable and informative.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Wu AG, Weinberg JM. The impact of diet on psoriasis. Cutis. 2019;104(suppl 2):7-10.
- Pithadia DJ, Reynolds KA, Lee EB, et al. Translating the 2019 AAD-NPF guidelines of care for the management of psoriasis with biologics to clinical practice. Cutis. 2019;104(suppl 2):12-16, 20.
- Havnaer A, Weinberg JM, Han G. Systemic therapies in psoriasis: an update on newly approved and pipeline biologics and oral treatments. Cutis. 2019;104(suppl 2):17-20.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Wu AG, Weinberg JM. The impact of diet on psoriasis. Cutis. 2019;104(suppl 2):7-10.
- Pithadia DJ, Reynolds KA, Lee EB, et al. Translating the 2019 AAD-NPF guidelines of care for the management of psoriasis with biologics to clinical practice. Cutis. 2019;104(suppl 2):12-16, 20.
- Havnaer A, Weinberg JM, Han G. Systemic therapies in psoriasis: an update on newly approved and pipeline biologics and oral treatments. Cutis. 2019;104(suppl 2):17-20.
Survey: PCI use has declined in ES-SCLC
A nationwide survey of radiation oncologists showed a decline in the use of prophylactic cranial irradiation (PCI) for extensive-stage small cell lung cancer (ES-SCLC) after the release of phase 3 study results by Takahashi et al.
The recent study by Toshiaki Takahashi, MD, and colleagues (Lancet Oncol. 2017;18[5]:663-71) demonstrated no overall survival benefit when comparing active magnetic resonance imaging surveillance with PCI in patients with ES-SCLC. The results challenged the formerly accepted belief of the benefit of PCI for patients with ES-SCLC.
“We conducted a nationwide survey study of radiation oncologists to assess changes in the use of PCI for patients with ES-SCLC following publication of the trial by Takahashi et al.,” wrote Olsi Gjyshi, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and colleagues. The findings were reported in a research letter published in JAMA Network Open.
Dr. Gjyshi and colleagues distributed the anonymous survey to 3,851 United States–based radiation oncologists registered with the American Society for Radiation Oncology (ASTRO). In total, 487 members (12.6%) completed the survey.
After analysis, the researchers found that 72% of respondents regularly offered PCI to patients before the publication of the study by Takahashi et al., while only 44% do so currently (difference, 28%; 95% confidence interval, 25%-31%; P less than .001).
With respect to radiation oncologists in private versus academic settings, no significant difference in practice patterns was observed (P = .71).
“Regression analysis showed no difference in likelihood of offering PCI based on practice setting, location, or size; volume of patients treated for lung cancer; or years in practice,” the researchers wrote.
In respondents unaware of the Takahashi et al. study, 85% continued to propose PCI, which was greater than those aware of the trial (odds ratio, 0.11; 95% CI, 0.04-0.32; P less than .001).
The researchers acknowledged a key limitation of the study was that radiation oncologists familiar with the study by Dr. Takahashi and colleagues may have been more apt to respond to the survey. As a result, participation bias could have influenced the results.
“These results highlight the continued lack of consensus for PCI in SCLC and support ongoing investigations,” they concluded.
No funding sources were reported. One co-author reported financial affiliations with Novocure, Inc. The other authors reported no conflicts of interest.
SOURCE: Gjyshi O et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9135.
A nationwide survey of radiation oncologists showed a decline in the use of prophylactic cranial irradiation (PCI) for extensive-stage small cell lung cancer (ES-SCLC) after the release of phase 3 study results by Takahashi et al.
The recent study by Toshiaki Takahashi, MD, and colleagues (Lancet Oncol. 2017;18[5]:663-71) demonstrated no overall survival benefit when comparing active magnetic resonance imaging surveillance with PCI in patients with ES-SCLC. The results challenged the formerly accepted belief of the benefit of PCI for patients with ES-SCLC.
“We conducted a nationwide survey study of radiation oncologists to assess changes in the use of PCI for patients with ES-SCLC following publication of the trial by Takahashi et al.,” wrote Olsi Gjyshi, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and colleagues. The findings were reported in a research letter published in JAMA Network Open.
Dr. Gjyshi and colleagues distributed the anonymous survey to 3,851 United States–based radiation oncologists registered with the American Society for Radiation Oncology (ASTRO). In total, 487 members (12.6%) completed the survey.
After analysis, the researchers found that 72% of respondents regularly offered PCI to patients before the publication of the study by Takahashi et al., while only 44% do so currently (difference, 28%; 95% confidence interval, 25%-31%; P less than .001).
With respect to radiation oncologists in private versus academic settings, no significant difference in practice patterns was observed (P = .71).
“Regression analysis showed no difference in likelihood of offering PCI based on practice setting, location, or size; volume of patients treated for lung cancer; or years in practice,” the researchers wrote.
In respondents unaware of the Takahashi et al. study, 85% continued to propose PCI, which was greater than those aware of the trial (odds ratio, 0.11; 95% CI, 0.04-0.32; P less than .001).
The researchers acknowledged a key limitation of the study was that radiation oncologists familiar with the study by Dr. Takahashi and colleagues may have been more apt to respond to the survey. As a result, participation bias could have influenced the results.
“These results highlight the continued lack of consensus for PCI in SCLC and support ongoing investigations,” they concluded.
No funding sources were reported. One co-author reported financial affiliations with Novocure, Inc. The other authors reported no conflicts of interest.
SOURCE: Gjyshi O et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9135.
A nationwide survey of radiation oncologists showed a decline in the use of prophylactic cranial irradiation (PCI) for extensive-stage small cell lung cancer (ES-SCLC) after the release of phase 3 study results by Takahashi et al.
The recent study by Toshiaki Takahashi, MD, and colleagues (Lancet Oncol. 2017;18[5]:663-71) demonstrated no overall survival benefit when comparing active magnetic resonance imaging surveillance with PCI in patients with ES-SCLC. The results challenged the formerly accepted belief of the benefit of PCI for patients with ES-SCLC.
“We conducted a nationwide survey study of radiation oncologists to assess changes in the use of PCI for patients with ES-SCLC following publication of the trial by Takahashi et al.,” wrote Olsi Gjyshi, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and colleagues. The findings were reported in a research letter published in JAMA Network Open.
Dr. Gjyshi and colleagues distributed the anonymous survey to 3,851 United States–based radiation oncologists registered with the American Society for Radiation Oncology (ASTRO). In total, 487 members (12.6%) completed the survey.
After analysis, the researchers found that 72% of respondents regularly offered PCI to patients before the publication of the study by Takahashi et al., while only 44% do so currently (difference, 28%; 95% confidence interval, 25%-31%; P less than .001).
With respect to radiation oncologists in private versus academic settings, no significant difference in practice patterns was observed (P = .71).
“Regression analysis showed no difference in likelihood of offering PCI based on practice setting, location, or size; volume of patients treated for lung cancer; or years in practice,” the researchers wrote.
In respondents unaware of the Takahashi et al. study, 85% continued to propose PCI, which was greater than those aware of the trial (odds ratio, 0.11; 95% CI, 0.04-0.32; P less than .001).
The researchers acknowledged a key limitation of the study was that radiation oncologists familiar with the study by Dr. Takahashi and colleagues may have been more apt to respond to the survey. As a result, participation bias could have influenced the results.
“These results highlight the continued lack of consensus for PCI in SCLC and support ongoing investigations,” they concluded.
No funding sources were reported. One co-author reported financial affiliations with Novocure, Inc. The other authors reported no conflicts of interest.
SOURCE: Gjyshi O et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9135.
FROM JAMA NETWORK OPEN
Vaccination Not Associated With Increased Risk of MS
Key clinical point: Data do not support an association between vaccination and increased risk of MS.
Major finding: The odds of MS were lower in participants who received vaccination, compared with participants without autoimmune disease (odds ratio, 0.870).
Study details: A systematic retrospective analysis of claims data for 12,262 patients with MS and 210,773 controls.
Disclosures: A grant from the German Federal Ministry of Education and Research Competence Network MS supported the study. The authors had no relevant conflicts.
Citation: Hapfelmeier A et al. Neurology. 2019 Jul 30. doi: 10.1212/WNL.0000000000008012.
Key clinical point: Data do not support an association between vaccination and increased risk of MS.
Major finding: The odds of MS were lower in participants who received vaccination, compared with participants without autoimmune disease (odds ratio, 0.870).
Study details: A systematic retrospective analysis of claims data for 12,262 patients with MS and 210,773 controls.
Disclosures: A grant from the German Federal Ministry of Education and Research Competence Network MS supported the study. The authors had no relevant conflicts.
Citation: Hapfelmeier A et al. Neurology. 2019 Jul 30. doi: 10.1212/WNL.0000000000008012.
Key clinical point: Data do not support an association between vaccination and increased risk of MS.
Major finding: The odds of MS were lower in participants who received vaccination, compared with participants without autoimmune disease (odds ratio, 0.870).
Study details: A systematic retrospective analysis of claims data for 12,262 patients with MS and 210,773 controls.
Disclosures: A grant from the German Federal Ministry of Education and Research Competence Network MS supported the study. The authors had no relevant conflicts.
Citation: Hapfelmeier A et al. Neurology. 2019 Jul 30. doi: 10.1212/WNL.0000000000008012.
Black Holes Associated With Impaired Cognition in MS
Key clinical point: Evaluating black holes as part of routine clinical practice could be a quick method for screening people with MS for referral to a comprehensive cognitive assessment.
Major finding: Mean Symbol Digit Modalities Test score was 49.0 in patients without a black hole and 42.9 in patients with at least one black hole.
Study details: A prospective study of 226 patients with MS.
Disclosures: The investigators had no disclosures and conducted their study without financial support.
Citation: Özakbas S et al. CMSC 2019, Abstract IMG02.
Key clinical point: Evaluating black holes as part of routine clinical practice could be a quick method for screening people with MS for referral to a comprehensive cognitive assessment.
Major finding: Mean Symbol Digit Modalities Test score was 49.0 in patients without a black hole and 42.9 in patients with at least one black hole.
Study details: A prospective study of 226 patients with MS.
Disclosures: The investigators had no disclosures and conducted their study without financial support.
Citation: Özakbas S et al. CMSC 2019, Abstract IMG02.
Key clinical point: Evaluating black holes as part of routine clinical practice could be a quick method for screening people with MS for referral to a comprehensive cognitive assessment.
Major finding: Mean Symbol Digit Modalities Test score was 49.0 in patients without a black hole and 42.9 in patients with at least one black hole.
Study details: A prospective study of 226 patients with MS.
Disclosures: The investigators had no disclosures and conducted their study without financial support.
Citation: Özakbas S et al. CMSC 2019, Abstract IMG02.
Neutrophils May Decline in Patients on Fingolimod
Key clinical point: Neutrophil levels may decline in patients with relapsing multiple sclerosis (MS) who have been on fingolimod for 2 or more years.
Major finding: In a cohort of patients continuously treated with fingolimod for at least 2 years, neutrophils declined over 6 months by about 9%, from an average of 3,698.56 cells per microliter to 3,336.13 cells per microliter.
Study details: Analysis of interim, 6-month data from the ongoing, open-label, phase 4 FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The interim results include data from 216 treatment-experienced patients and 166 treatment-naive patients.
Disclosures: Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
Citation: Mao-Draayer Y et al. CMSC 2019, Abstract DXM03.
Key clinical point: Neutrophil levels may decline in patients with relapsing multiple sclerosis (MS) who have been on fingolimod for 2 or more years.
Major finding: In a cohort of patients continuously treated with fingolimod for at least 2 years, neutrophils declined over 6 months by about 9%, from an average of 3,698.56 cells per microliter to 3,336.13 cells per microliter.
Study details: Analysis of interim, 6-month data from the ongoing, open-label, phase 4 FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The interim results include data from 216 treatment-experienced patients and 166 treatment-naive patients.
Disclosures: Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
Citation: Mao-Draayer Y et al. CMSC 2019, Abstract DXM03.
Key clinical point: Neutrophil levels may decline in patients with relapsing multiple sclerosis (MS) who have been on fingolimod for 2 or more years.
Major finding: In a cohort of patients continuously treated with fingolimod for at least 2 years, neutrophils declined over 6 months by about 9%, from an average of 3,698.56 cells per microliter to 3,336.13 cells per microliter.
Study details: Analysis of interim, 6-month data from the ongoing, open-label, phase 4 FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The interim results include data from 216 treatment-experienced patients and 166 treatment-naive patients.
Disclosures: Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
Citation: Mao-Draayer Y et al. CMSC 2019, Abstract DXM03.