User login
Diabetes targets remain elusive for patients
Some things never change: In 2005, most adults with diabetes missed their treatment targets. In 2016, most adults with diabetes missed their treatment targets. And during that time, from 2005 to 2016, around 96% of men and 94% of women were linked to care.
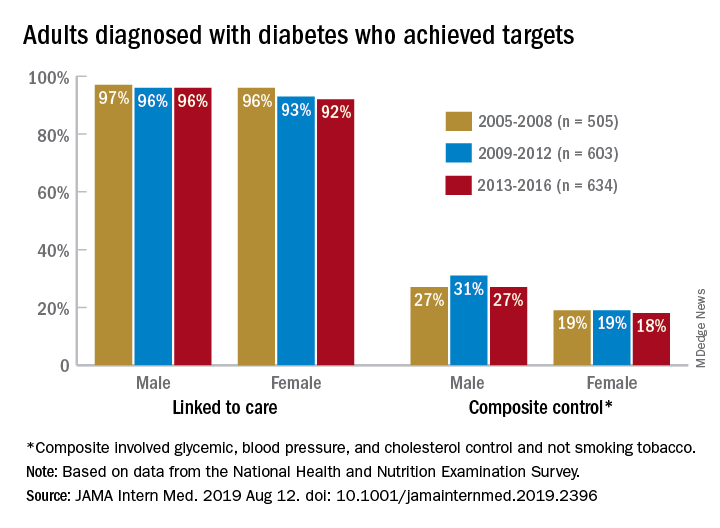
“Fewer than one in four American adults with diagnosed diabetes achieve a controlled level of blood sugar, blood pressure, and cholesterol, and do not smoke tobacco. Our results suggest that, despite major advances in diabetes drug discovery and movement to develop innovative care delivery models over the past two decades, achievement of diabetes care targets has not improved in the United States since 2005,” Pooyan Kazemian, PhD, of Massachusetts General Hospital, Boston, said in a written statement.
During 2013-2016, only 23% of adults with diabetes met a combined composite target of glycemic (HbA1c below a liberal personalized level), blood pressure (less than 140/90 mm Hg), and cholesterol (LDL cholesterol level less than 100 mg/dL) control, as well as not smoking tobacco, Dr. Kazemian and associates reported in JAMA Internal Medicine. The corresponding figures were 25% (2009-2012) and 23% (2005-2008) for the two earlier time periods covered in the study,
The investigators used data for 1,742 nonpregnant adults from the National Health and Nutrition Examination Survey to evaluate the diabetes care cascade, which they defined as “diagnosis, linkage to care, achievement of individual treatment targets, and a composite of all individual targets.”
In 2013-2016, 94% of those diagnosed were linked to care, 64% met their HbA1c target, 70% achieved blood pressure control, 57% met the cholesterol target, and 85% were nonsmokers. When targets were combined, 41% achieved blood pressure and cholesterol control, and 25% met the glycemic, blood pressure, and cholesterol targets, they said.
“We found that none of the U.S. diabetes care variables improved from 2005 to 2016,” Dr. Kazemian and associates noted. Women were less likely than men to meet their treatment goals (see graph) over the course of the study, as were adults aged 18-44 years and black and Hispanic individuals.
“Recent advances in [treatments for diabetes] have not effectively reached the populations at risk and may indicate an immediate need for better approaches to the delivery of diabetes care, including a continued focus on reaching underserved populations with persistent disparities in care,” they wrote.
The study was supported by the Boston Area Diabetes Endocrinology Research Center and Massachusetts General Hospital. One investigator reported that her husband has equity in Apolo1bio. No other disclosures were reported.
SOURCE: Kazemian P et al. JAMA Intern Med. 2019 Aug 12. doi: 10.1001/jamainternmed.2019.2396.
Some things never change: In 2005, most adults with diabetes missed their treatment targets. In 2016, most adults with diabetes missed their treatment targets. And during that time, from 2005 to 2016, around 96% of men and 94% of women were linked to care.
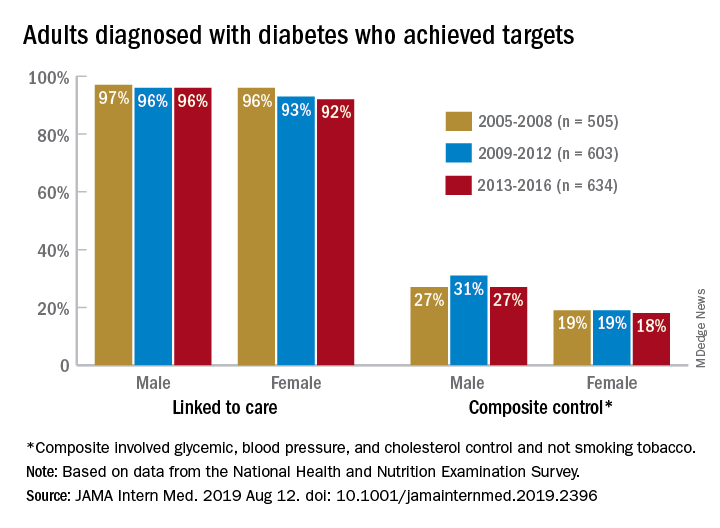
“Fewer than one in four American adults with diagnosed diabetes achieve a controlled level of blood sugar, blood pressure, and cholesterol, and do not smoke tobacco. Our results suggest that, despite major advances in diabetes drug discovery and movement to develop innovative care delivery models over the past two decades, achievement of diabetes care targets has not improved in the United States since 2005,” Pooyan Kazemian, PhD, of Massachusetts General Hospital, Boston, said in a written statement.
During 2013-2016, only 23% of adults with diabetes met a combined composite target of glycemic (HbA1c below a liberal personalized level), blood pressure (less than 140/90 mm Hg), and cholesterol (LDL cholesterol level less than 100 mg/dL) control, as well as not smoking tobacco, Dr. Kazemian and associates reported in JAMA Internal Medicine. The corresponding figures were 25% (2009-2012) and 23% (2005-2008) for the two earlier time periods covered in the study,
The investigators used data for 1,742 nonpregnant adults from the National Health and Nutrition Examination Survey to evaluate the diabetes care cascade, which they defined as “diagnosis, linkage to care, achievement of individual treatment targets, and a composite of all individual targets.”
In 2013-2016, 94% of those diagnosed were linked to care, 64% met their HbA1c target, 70% achieved blood pressure control, 57% met the cholesterol target, and 85% were nonsmokers. When targets were combined, 41% achieved blood pressure and cholesterol control, and 25% met the glycemic, blood pressure, and cholesterol targets, they said.
“We found that none of the U.S. diabetes care variables improved from 2005 to 2016,” Dr. Kazemian and associates noted. Women were less likely than men to meet their treatment goals (see graph) over the course of the study, as were adults aged 18-44 years and black and Hispanic individuals.
“Recent advances in [treatments for diabetes] have not effectively reached the populations at risk and may indicate an immediate need for better approaches to the delivery of diabetes care, including a continued focus on reaching underserved populations with persistent disparities in care,” they wrote.
The study was supported by the Boston Area Diabetes Endocrinology Research Center and Massachusetts General Hospital. One investigator reported that her husband has equity in Apolo1bio. No other disclosures were reported.
SOURCE: Kazemian P et al. JAMA Intern Med. 2019 Aug 12. doi: 10.1001/jamainternmed.2019.2396.
Some things never change: In 2005, most adults with diabetes missed their treatment targets. In 2016, most adults with diabetes missed their treatment targets. And during that time, from 2005 to 2016, around 96% of men and 94% of women were linked to care.
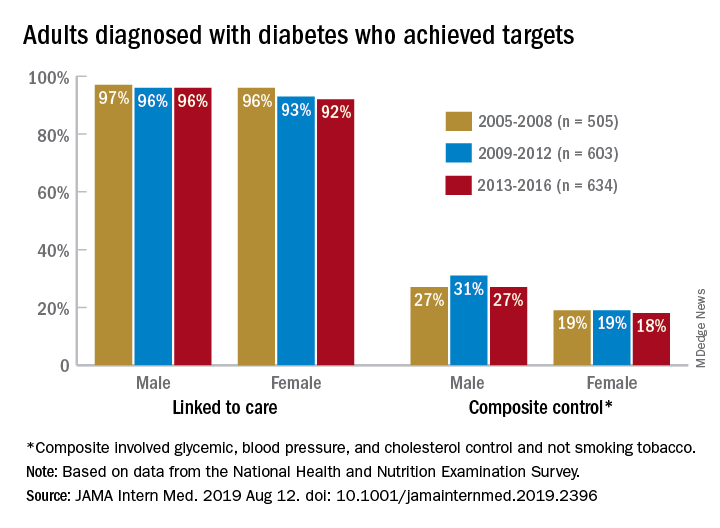
“Fewer than one in four American adults with diagnosed diabetes achieve a controlled level of blood sugar, blood pressure, and cholesterol, and do not smoke tobacco. Our results suggest that, despite major advances in diabetes drug discovery and movement to develop innovative care delivery models over the past two decades, achievement of diabetes care targets has not improved in the United States since 2005,” Pooyan Kazemian, PhD, of Massachusetts General Hospital, Boston, said in a written statement.
During 2013-2016, only 23% of adults with diabetes met a combined composite target of glycemic (HbA1c below a liberal personalized level), blood pressure (less than 140/90 mm Hg), and cholesterol (LDL cholesterol level less than 100 mg/dL) control, as well as not smoking tobacco, Dr. Kazemian and associates reported in JAMA Internal Medicine. The corresponding figures were 25% (2009-2012) and 23% (2005-2008) for the two earlier time periods covered in the study,
The investigators used data for 1,742 nonpregnant adults from the National Health and Nutrition Examination Survey to evaluate the diabetes care cascade, which they defined as “diagnosis, linkage to care, achievement of individual treatment targets, and a composite of all individual targets.”
In 2013-2016, 94% of those diagnosed were linked to care, 64% met their HbA1c target, 70% achieved blood pressure control, 57% met the cholesterol target, and 85% were nonsmokers. When targets were combined, 41% achieved blood pressure and cholesterol control, and 25% met the glycemic, blood pressure, and cholesterol targets, they said.
“We found that none of the U.S. diabetes care variables improved from 2005 to 2016,” Dr. Kazemian and associates noted. Women were less likely than men to meet their treatment goals (see graph) over the course of the study, as were adults aged 18-44 years and black and Hispanic individuals.
“Recent advances in [treatments for diabetes] have not effectively reached the populations at risk and may indicate an immediate need for better approaches to the delivery of diabetes care, including a continued focus on reaching underserved populations with persistent disparities in care,” they wrote.
The study was supported by the Boston Area Diabetes Endocrinology Research Center and Massachusetts General Hospital. One investigator reported that her husband has equity in Apolo1bio. No other disclosures were reported.
SOURCE: Kazemian P et al. JAMA Intern Med. 2019 Aug 12. doi: 10.1001/jamainternmed.2019.2396.
FROM JAMA INTERNAL MEDICINE
USPSTF draft guidance calls for drug use screening
according to a draft recommendation statement now available for public comment.
The statement defines illicit drug use as “use of illegal drugs and the nonmedical use of prescription psychoactive medications (i.e., use for reasons, for duration, in amounts, or with frequency other than prescribed or use by persons other than the prescribed individual).”
The guidelines do not apply to individuals younger than 18 years, for whom the USPSTF found insufficient evidence to recommend routine screening, or to adults currently diagnosed or in treatment for a drug use disorder.
In the draft recommendation statement, available online, the USPSTF noted that several screening tools are available for use in primary care practices, including the BSTAD (Brief Screener for Tobacco, Alcohol, and Other Drugs) that consists of six questions. The task force noted that they have found “adequate evidence” that these screening tools can detect illicit drug use. In addition, they wrote that no studies offer evidence of benefits versus harms of these screening tools, and evidence of harms associated with screening are limited.
Screening intervals can be simplified by screening young adults whenever they seek medical services and when clinicians suspect illicit drug use, the USPSTF said.
When the draft recommendation is finalized, it will replace the 2008 recommendation, which found insufficient evidence for screening in adults, as well as in adolescents. New evidence since 2008 supports the value of screening for adults aged 18 years and older, including pregnant and postpartum women.
The draft recommendations are based on the results of two systematic evidence reviews that assessed the accuracy and harms of routine illicit drug use screening. The USPSTF’s review included 12 studies on the accuracy of 15 screening tools. Overall, the sensitivity of direct screening tools to identify “unhealthy use of ‘any drug’ (including illegal drugs and nonmedical use of prescription drugs) in the past month or year” ranged from 0.71 to 0.94, and the specificity ranged from 0.87 to 0.97.
Based on the current evidence, the USPSTF assigned drug screening for adults a grade B recommendation, defined as “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.”
For treatment, the Task Force found evidence to support strategies including pharmacotherapy with naltrexone, buprenorphine, and methadone, as well as for psychosocial interventions.
The USPSTF acknowledged that many factors may affect a clinicians’ decision of whether to implement the drug screening recommendation. “In many communities, affordable, accessible, and timely services for diagnostic assessment and treatment for patients with positive screening results are in limited supply or unaffordable. Providers should be aware of any state requirements for mandatory screening or reporting of screening results to medicolegal authorities and understand the positive and negative implications of reporting,” they wrote.
The draft recommendations also identified several research gaps including the effectiveness of screening for illicit drug use in adolescents, the optimal screening interval for all patients, the accuracy of screening tools for detecting opioids, the accuracy of screening within the same population, the benefits of naloxone as rescue therapy, and nonmedical use of other prescription drugs, as well as ways to improve access to care for those diagnosed with drug use disorders.
The draft recommendation is available for public comment until Sept. 9, 2019, at 8 p.m. EST.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
according to a draft recommendation statement now available for public comment.
The statement defines illicit drug use as “use of illegal drugs and the nonmedical use of prescription psychoactive medications (i.e., use for reasons, for duration, in amounts, or with frequency other than prescribed or use by persons other than the prescribed individual).”
The guidelines do not apply to individuals younger than 18 years, for whom the USPSTF found insufficient evidence to recommend routine screening, or to adults currently diagnosed or in treatment for a drug use disorder.
In the draft recommendation statement, available online, the USPSTF noted that several screening tools are available for use in primary care practices, including the BSTAD (Brief Screener for Tobacco, Alcohol, and Other Drugs) that consists of six questions. The task force noted that they have found “adequate evidence” that these screening tools can detect illicit drug use. In addition, they wrote that no studies offer evidence of benefits versus harms of these screening tools, and evidence of harms associated with screening are limited.
Screening intervals can be simplified by screening young adults whenever they seek medical services and when clinicians suspect illicit drug use, the USPSTF said.
When the draft recommendation is finalized, it will replace the 2008 recommendation, which found insufficient evidence for screening in adults, as well as in adolescents. New evidence since 2008 supports the value of screening for adults aged 18 years and older, including pregnant and postpartum women.
The draft recommendations are based on the results of two systematic evidence reviews that assessed the accuracy and harms of routine illicit drug use screening. The USPSTF’s review included 12 studies on the accuracy of 15 screening tools. Overall, the sensitivity of direct screening tools to identify “unhealthy use of ‘any drug’ (including illegal drugs and nonmedical use of prescription drugs) in the past month or year” ranged from 0.71 to 0.94, and the specificity ranged from 0.87 to 0.97.
Based on the current evidence, the USPSTF assigned drug screening for adults a grade B recommendation, defined as “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.”
For treatment, the Task Force found evidence to support strategies including pharmacotherapy with naltrexone, buprenorphine, and methadone, as well as for psychosocial interventions.
The USPSTF acknowledged that many factors may affect a clinicians’ decision of whether to implement the drug screening recommendation. “In many communities, affordable, accessible, and timely services for diagnostic assessment and treatment for patients with positive screening results are in limited supply or unaffordable. Providers should be aware of any state requirements for mandatory screening or reporting of screening results to medicolegal authorities and understand the positive and negative implications of reporting,” they wrote.
The draft recommendations also identified several research gaps including the effectiveness of screening for illicit drug use in adolescents, the optimal screening interval for all patients, the accuracy of screening tools for detecting opioids, the accuracy of screening within the same population, the benefits of naloxone as rescue therapy, and nonmedical use of other prescription drugs, as well as ways to improve access to care for those diagnosed with drug use disorders.
The draft recommendation is available for public comment until Sept. 9, 2019, at 8 p.m. EST.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
according to a draft recommendation statement now available for public comment.
The statement defines illicit drug use as “use of illegal drugs and the nonmedical use of prescription psychoactive medications (i.e., use for reasons, for duration, in amounts, or with frequency other than prescribed or use by persons other than the prescribed individual).”
The guidelines do not apply to individuals younger than 18 years, for whom the USPSTF found insufficient evidence to recommend routine screening, or to adults currently diagnosed or in treatment for a drug use disorder.
In the draft recommendation statement, available online, the USPSTF noted that several screening tools are available for use in primary care practices, including the BSTAD (Brief Screener for Tobacco, Alcohol, and Other Drugs) that consists of six questions. The task force noted that they have found “adequate evidence” that these screening tools can detect illicit drug use. In addition, they wrote that no studies offer evidence of benefits versus harms of these screening tools, and evidence of harms associated with screening are limited.
Screening intervals can be simplified by screening young adults whenever they seek medical services and when clinicians suspect illicit drug use, the USPSTF said.
When the draft recommendation is finalized, it will replace the 2008 recommendation, which found insufficient evidence for screening in adults, as well as in adolescents. New evidence since 2008 supports the value of screening for adults aged 18 years and older, including pregnant and postpartum women.
The draft recommendations are based on the results of two systematic evidence reviews that assessed the accuracy and harms of routine illicit drug use screening. The USPSTF’s review included 12 studies on the accuracy of 15 screening tools. Overall, the sensitivity of direct screening tools to identify “unhealthy use of ‘any drug’ (including illegal drugs and nonmedical use of prescription drugs) in the past month or year” ranged from 0.71 to 0.94, and the specificity ranged from 0.87 to 0.97.
Based on the current evidence, the USPSTF assigned drug screening for adults a grade B recommendation, defined as “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.”
For treatment, the Task Force found evidence to support strategies including pharmacotherapy with naltrexone, buprenorphine, and methadone, as well as for psychosocial interventions.
The USPSTF acknowledged that many factors may affect a clinicians’ decision of whether to implement the drug screening recommendation. “In many communities, affordable, accessible, and timely services for diagnostic assessment and treatment for patients with positive screening results are in limited supply or unaffordable. Providers should be aware of any state requirements for mandatory screening or reporting of screening results to medicolegal authorities and understand the positive and negative implications of reporting,” they wrote.
The draft recommendations also identified several research gaps including the effectiveness of screening for illicit drug use in adolescents, the optimal screening interval for all patients, the accuracy of screening tools for detecting opioids, the accuracy of screening within the same population, the benefits of naloxone as rescue therapy, and nonmedical use of other prescription drugs, as well as ways to improve access to care for those diagnosed with drug use disorders.
The draft recommendation is available for public comment until Sept. 9, 2019, at 8 p.m. EST.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
FROM THE USPSTF
Lamotrigine-Induced Cutaneous Pseudolymphoma
To the Editor:
An 8-year-old girl presented with new lesions on the scalp that were mildly painful to palpation and had been increasing in size and number over the last 2 months. Her medical history was remarkable for seizures, keratosis pilaris, and seborrheic dermatitis. The seizures had been well controlled on oxcarbazepine; however, she was switched to lamotrigine 6 months prior to presentation under the care of her neurologist. The patient was not taking other oral medications, and she denied any trauma/insect bites to the affected area or systemic symptoms such as fever, fatigue, weight loss, nausea, swollen lymph nodes, or night sweats. Physical examination revealed 3 well-circumscribed, pink, slightly scaly, indurated nodules on the frontal and vertex scalp (Figure 1). She reported pain on palpation of the lesions. Treatment with ketoconazole shampoo and high-potency topical corticosteroids was ineffective.
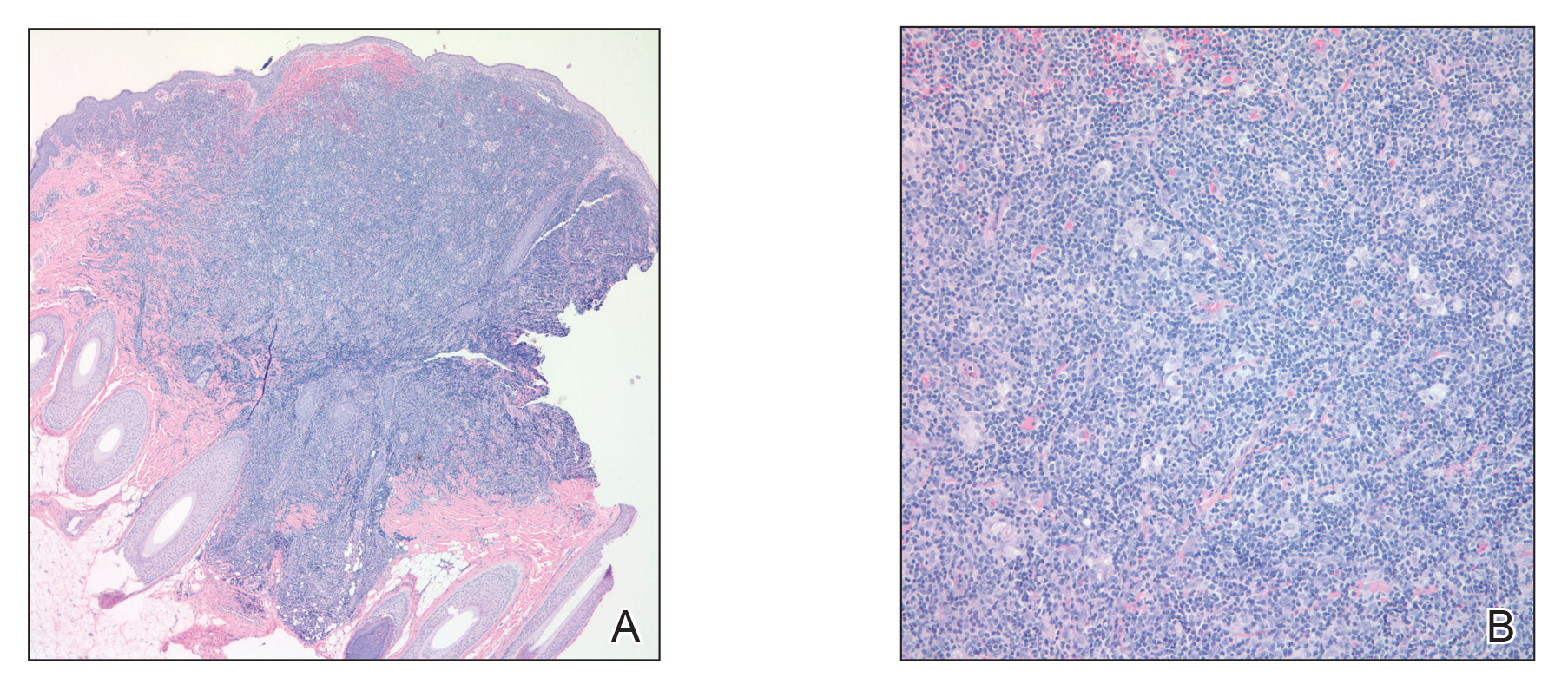
Over a period of 2 months after the initial presentation, the patient developed a total of 9 scalp lesions. Testing was performed 4 months after presentation of lesions. Bacterial and fungal cultures of the lesional skin of the scalp were negative. Two biopsies of lesions on the scalp were performed, the first of which showed a nonspecific lymphohistiocytic infiltrate. The second biopsy revealed a dense, nodular, atypical dermal lymphoid infiltrate composed primarily of round regular lymphocytes intermixed with some larger, more irregular lymphocytes and few scattered mitoses (Figure 2).
Immunohistochemical studies revealed small B-cell lymphoma 2–positive lymphocytes with a 2:1 mixture of CD3+ T cells and CD20+CD79a+ B cells. The T cells expressed CD2, CD5, and CD43, and a subset showed a loss of CD7. The CD4:CD8 ratio was 10 to 1. No follicular dendritic networks were noted with CD21 and CD23. Rare, scattered, medium-sized CD30 cells were noted. Staining for CD10, B-cell lymphoma 6, anaplastic lymphoma kinase, Epstein-Barr virus–encoded RNA 1, IgD, and IgM were negative. The plasma cells had a κ/λ free light chain ratio of 2 to 1. Ki-67 was positive in 15% of lymphoid cells. Polymerase chain reaction analysis of T-cell receptor gene rearrangement revealed a peak at 228 bp in a predominantly polyclonal background. A thorough systemic workup including complete blood cell count, immunoglobulin assay, bone marrow transplant panel, comprehensive metabolic panel, lactate dehydrogenase test, inflammatory markers, and viral testing failed to reveal any evidence of underlying malignancy.
After conferring with the patient’s neurologist, lamotrigine was discontinued. Within a few weeks of cessation, the scalp lesions resolved without recurrence at 9-month follow-up. In addition to the lack of clinical, histological, or immunohistochemical evidence of underlying malignancy, the temporal association of the development of lesions after starting lamotrigine and rapid resolution upon its discontinuation suggested a diagnosis of lamotrigine-induced cutaneous pseudolymphoma.
Cutaneous pseudolymphoma is a term used to describe a heterogenous group of benign reactive T-cell, B-cell, or mixed-cell lymphoproliferative processes that resemble cutaneous lymphomas clinically and/or histopathologically.1 Historically, these types of proliferations have been classified under many alternative names that originally served to describe only B-cell–type proliferations. With advances in immunohistochemistry allowing for more specific cell marker identification, cutaneous pseudolymphomas often are found to contain a mixture of T-cell and B-cell populations, which also led to identifying and describing T-cell–type pseudolymphomas.2
The clinical appearance of cutaneous pseudolymphoma is variable, ranging from discrete nodules or papules to even confluent erythroderma in certain cases.2 The high clinical variability further complicates diagnosis. Although our patient presented with 9 individual nodular lesions, this finding alone is not sufficient to have high suspicion for cutaneous pseudolymphoma without including a much broader differential diagnosis. In our case, the differential diagnosis also included cutaneous lymphoma, arthropod bite reaction, lymphomatoid papulosis, tumid lupus, follicular mucinosis, lymphocytic infiltrate of Jessner, and leukemia cutis.
The primary concern regarding diagnosis of cutaneous pseudolymphoma is the clinician’s ability to effectively differentiate this entity from a true malignant lymphoma. Immunostaining has some value by identification of heterogeneous cell–type populations with a mixed T-cell and B-cell infiltrate that is more characteristic of a benign reactive process. Subsequent polymerase chain reaction analysis can detect the presence or absence of monoclonal T-cell receptor gene rearrangement or immunoglobulin heavy chain rearrangement.3 If these monoclonal rearrangements are absent, a benign diagnosis is favored; however, these rearrangements also have been shown to exist in a case of cutaneous pseudolymphoma that earned the final diagnosis when removal of the offending agent led to spontaneous lesion regression, similar to our case.4
Many different entities have been described as causative factors for the development of cutaneous pseudolymphoma. Of those that have been considered causative, simple categories have emerged, including endogenous, exogenous, and iatrogenic causes. One potential endogenous etiology of cutaneous pseudolymphoma is IgG4-related disease.5 A multitude of exogenous causes have been reported, including several cases of cutaneous pseudolymphoma developing in a prior tattoo site.6 Viruses, specifically molluscum contagiosum, also have been implicated as exogenous causes, and a report of cutaneous pseudolymphoma development at a prior site of herpes zoster lesions has been described.7 Development of cutaneous pseudolymphoma in vaccination sites also has been reported,8 as well as more obscure inciting events such as Leishmania donovani infection and medicinal leech therapy.9
A considerable number of reported cases of cutaneous pseudolymphoma have been attributed to drugs, including monoclonal antibodies,10 herbal supplements,11 and a multitude of other medications.1 As a class, anticonvulsants are considered more likely to cause lymph node pseudolymphomas than strictly cutaneous pseudolymphomas12; however, many drugs in this class of medications have been described in the development of cutaneous pseudolymphoma.3 A review of the literature by Ploysangam et al1 revealed reports of the development of cutaneous pseudolymphomas after administration of phenytoin, carbamazepine, mephenytoin, trimethadione, phenobarbital, primidone, butabarbital, methsuximide, phensuximide, and valproic acid.
Our patient represents a rare case of strictly cutaneous pseudolymphoma caused by administration of lamotrigine. Our case demonstrated a clear temporal relation between the cessation of lamotrigine and rapid and spontaneous disappearance of cutaneous lesions. We found another case of pseudolymphoma in which lamotrigine was deemed causative, but only lymph node involvement was observed.12
Proper diagnosis of cutaneous pseudolymphoma is important not only with regard to the initial differentiation from true malignant lymphoma but in allowing for appropriate follow-up and vigilant surveillance. Cases of progression from cutaneous pseudolymphoma to true lymphoma have been reported.1,2 It is recommended that watchful follow-up for these patients be carried out until at least 5 years after the diagnosis of cutaneous pseudolymphoma is made to rule out the possibility of malignant transformation, particularly in idiopathic cases.13
- Ploysangam T, Breneman D, Mutasim D. Cutaneous pseudolymphomas. J Am Acad Dermatol. 1998;38:877-898.
- Bergman R. Pseudolymphoma and cutaneous lymphoma: facts and controversies. Clin Dermatol. 2010;28:568-574.
- Braddock S, Harrington D, Vose J. Generalized nodular cutaneous pseudolymphoma associated with phenytoin therapy. J Am Acad Dermatol. 1992;27:337-340.
- Cogrel O, Beylot-Barry M, Vergier B, et al. Sodium valproate-induced cutaneous pseudolymphoma followed by recurrence with carbamazepine. Br J Dermatol. 2001;144:1235-1238.
- Cheuk W, Lee K, Chong L, et al. IgG4-related sclerosing disease: a potential new etiology of cutaneous pseudolymphoma. Am J Surg Pathol. 2009;33:1713-1719.
- Marchesi A, Parodi P, Brioschi M, et al. Tattoo ink-related cutaneous pseudolymphomas: a rare but significant complication. case report and review of the literature. Aesthetic Plast Surg. 2014;38:471-478.
- Gonzalez J, Sanz A, Martin T, et al. Cutaneous pseudolymphoma associated with molluscum contagiosum: a case report. Int J Dermatol. 2008;47:502-504.
- Maubec E, Pinquier L, Viguier M, et al. Vaccination-induced cutaneous pseudolymphoma. J Am Acad Dermatol. 2005;52:623-629.
- Altamura D, Calonje E, Liau J, et al. Diffuse cutaneous pseudolymphoma due to therapy with medicinal leeches. JAMA Dermatol. 2014;150:783-784.
- Imafuku S, Ito K, Nakayama J. Cutaneous pseudolymphoma induced by adalimumab and reproduced by infliximab in a patient with arthopathic psoriasis. Br J Dermatol. 2011;166:675-678.
- Meyer S, Vogt T, Obermann EC, et al. Cutaneous pseudolymphoma induced by Cimicifuga racemosa. Dermatology. 2007;214:94-96.
- Pathak P, McLachlan R. Drug-induced pseudolymphoma secondary to lamotrigine. Neurology. 1998;50:1509-1510.
- Prabu V, Shivani A, Pawar V. Idiopathic cutaneous pseudolymphoma: an enigma. Indian Dermatol Online J. 2014;5:224-226.
To the Editor:
An 8-year-old girl presented with new lesions on the scalp that were mildly painful to palpation and had been increasing in size and number over the last 2 months. Her medical history was remarkable for seizures, keratosis pilaris, and seborrheic dermatitis. The seizures had been well controlled on oxcarbazepine; however, she was switched to lamotrigine 6 months prior to presentation under the care of her neurologist. The patient was not taking other oral medications, and she denied any trauma/insect bites to the affected area or systemic symptoms such as fever, fatigue, weight loss, nausea, swollen lymph nodes, or night sweats. Physical examination revealed 3 well-circumscribed, pink, slightly scaly, indurated nodules on the frontal and vertex scalp (Figure 1). She reported pain on palpation of the lesions. Treatment with ketoconazole shampoo and high-potency topical corticosteroids was ineffective.
Over a period of 2 months after the initial presentation, the patient developed a total of 9 scalp lesions. Testing was performed 4 months after presentation of lesions. Bacterial and fungal cultures of the lesional skin of the scalp were negative. Two biopsies of lesions on the scalp were performed, the first of which showed a nonspecific lymphohistiocytic infiltrate. The second biopsy revealed a dense, nodular, atypical dermal lymphoid infiltrate composed primarily of round regular lymphocytes intermixed with some larger, more irregular lymphocytes and few scattered mitoses (Figure 2).
Immunohistochemical studies revealed small B-cell lymphoma 2–positive lymphocytes with a 2:1 mixture of CD3+ T cells and CD20+CD79a+ B cells. The T cells expressed CD2, CD5, and CD43, and a subset showed a loss of CD7. The CD4:CD8 ratio was 10 to 1. No follicular dendritic networks were noted with CD21 and CD23. Rare, scattered, medium-sized CD30 cells were noted. Staining for CD10, B-cell lymphoma 6, anaplastic lymphoma kinase, Epstein-Barr virus–encoded RNA 1, IgD, and IgM were negative. The plasma cells had a κ/λ free light chain ratio of 2 to 1. Ki-67 was positive in 15% of lymphoid cells. Polymerase chain reaction analysis of T-cell receptor gene rearrangement revealed a peak at 228 bp in a predominantly polyclonal background. A thorough systemic workup including complete blood cell count, immunoglobulin assay, bone marrow transplant panel, comprehensive metabolic panel, lactate dehydrogenase test, inflammatory markers, and viral testing failed to reveal any evidence of underlying malignancy.
After conferring with the patient’s neurologist, lamotrigine was discontinued. Within a few weeks of cessation, the scalp lesions resolved without recurrence at 9-month follow-up. In addition to the lack of clinical, histological, or immunohistochemical evidence of underlying malignancy, the temporal association of the development of lesions after starting lamotrigine and rapid resolution upon its discontinuation suggested a diagnosis of lamotrigine-induced cutaneous pseudolymphoma.
Cutaneous pseudolymphoma is a term used to describe a heterogenous group of benign reactive T-cell, B-cell, or mixed-cell lymphoproliferative processes that resemble cutaneous lymphomas clinically and/or histopathologically.1 Historically, these types of proliferations have been classified under many alternative names that originally served to describe only B-cell–type proliferations. With advances in immunohistochemistry allowing for more specific cell marker identification, cutaneous pseudolymphomas often are found to contain a mixture of T-cell and B-cell populations, which also led to identifying and describing T-cell–type pseudolymphomas.2
The clinical appearance of cutaneous pseudolymphoma is variable, ranging from discrete nodules or papules to even confluent erythroderma in certain cases.2 The high clinical variability further complicates diagnosis. Although our patient presented with 9 individual nodular lesions, this finding alone is not sufficient to have high suspicion for cutaneous pseudolymphoma without including a much broader differential diagnosis. In our case, the differential diagnosis also included cutaneous lymphoma, arthropod bite reaction, lymphomatoid papulosis, tumid lupus, follicular mucinosis, lymphocytic infiltrate of Jessner, and leukemia cutis.
The primary concern regarding diagnosis of cutaneous pseudolymphoma is the clinician’s ability to effectively differentiate this entity from a true malignant lymphoma. Immunostaining has some value by identification of heterogeneous cell–type populations with a mixed T-cell and B-cell infiltrate that is more characteristic of a benign reactive process. Subsequent polymerase chain reaction analysis can detect the presence or absence of monoclonal T-cell receptor gene rearrangement or immunoglobulin heavy chain rearrangement.3 If these monoclonal rearrangements are absent, a benign diagnosis is favored; however, these rearrangements also have been shown to exist in a case of cutaneous pseudolymphoma that earned the final diagnosis when removal of the offending agent led to spontaneous lesion regression, similar to our case.4
Many different entities have been described as causative factors for the development of cutaneous pseudolymphoma. Of those that have been considered causative, simple categories have emerged, including endogenous, exogenous, and iatrogenic causes. One potential endogenous etiology of cutaneous pseudolymphoma is IgG4-related disease.5 A multitude of exogenous causes have been reported, including several cases of cutaneous pseudolymphoma developing in a prior tattoo site.6 Viruses, specifically molluscum contagiosum, also have been implicated as exogenous causes, and a report of cutaneous pseudolymphoma development at a prior site of herpes zoster lesions has been described.7 Development of cutaneous pseudolymphoma in vaccination sites also has been reported,8 as well as more obscure inciting events such as Leishmania donovani infection and medicinal leech therapy.9
A considerable number of reported cases of cutaneous pseudolymphoma have been attributed to drugs, including monoclonal antibodies,10 herbal supplements,11 and a multitude of other medications.1 As a class, anticonvulsants are considered more likely to cause lymph node pseudolymphomas than strictly cutaneous pseudolymphomas12; however, many drugs in this class of medications have been described in the development of cutaneous pseudolymphoma.3 A review of the literature by Ploysangam et al1 revealed reports of the development of cutaneous pseudolymphomas after administration of phenytoin, carbamazepine, mephenytoin, trimethadione, phenobarbital, primidone, butabarbital, methsuximide, phensuximide, and valproic acid.
Our patient represents a rare case of strictly cutaneous pseudolymphoma caused by administration of lamotrigine. Our case demonstrated a clear temporal relation between the cessation of lamotrigine and rapid and spontaneous disappearance of cutaneous lesions. We found another case of pseudolymphoma in which lamotrigine was deemed causative, but only lymph node involvement was observed.12
Proper diagnosis of cutaneous pseudolymphoma is important not only with regard to the initial differentiation from true malignant lymphoma but in allowing for appropriate follow-up and vigilant surveillance. Cases of progression from cutaneous pseudolymphoma to true lymphoma have been reported.1,2 It is recommended that watchful follow-up for these patients be carried out until at least 5 years after the diagnosis of cutaneous pseudolymphoma is made to rule out the possibility of malignant transformation, particularly in idiopathic cases.13
To the Editor:
An 8-year-old girl presented with new lesions on the scalp that were mildly painful to palpation and had been increasing in size and number over the last 2 months. Her medical history was remarkable for seizures, keratosis pilaris, and seborrheic dermatitis. The seizures had been well controlled on oxcarbazepine; however, she was switched to lamotrigine 6 months prior to presentation under the care of her neurologist. The patient was not taking other oral medications, and she denied any trauma/insect bites to the affected area or systemic symptoms such as fever, fatigue, weight loss, nausea, swollen lymph nodes, or night sweats. Physical examination revealed 3 well-circumscribed, pink, slightly scaly, indurated nodules on the frontal and vertex scalp (Figure 1). She reported pain on palpation of the lesions. Treatment with ketoconazole shampoo and high-potency topical corticosteroids was ineffective.
Over a period of 2 months after the initial presentation, the patient developed a total of 9 scalp lesions. Testing was performed 4 months after presentation of lesions. Bacterial and fungal cultures of the lesional skin of the scalp were negative. Two biopsies of lesions on the scalp were performed, the first of which showed a nonspecific lymphohistiocytic infiltrate. The second biopsy revealed a dense, nodular, atypical dermal lymphoid infiltrate composed primarily of round regular lymphocytes intermixed with some larger, more irregular lymphocytes and few scattered mitoses (Figure 2).
Immunohistochemical studies revealed small B-cell lymphoma 2–positive lymphocytes with a 2:1 mixture of CD3+ T cells and CD20+CD79a+ B cells. The T cells expressed CD2, CD5, and CD43, and a subset showed a loss of CD7. The CD4:CD8 ratio was 10 to 1. No follicular dendritic networks were noted with CD21 and CD23. Rare, scattered, medium-sized CD30 cells were noted. Staining for CD10, B-cell lymphoma 6, anaplastic lymphoma kinase, Epstein-Barr virus–encoded RNA 1, IgD, and IgM were negative. The plasma cells had a κ/λ free light chain ratio of 2 to 1. Ki-67 was positive in 15% of lymphoid cells. Polymerase chain reaction analysis of T-cell receptor gene rearrangement revealed a peak at 228 bp in a predominantly polyclonal background. A thorough systemic workup including complete blood cell count, immunoglobulin assay, bone marrow transplant panel, comprehensive metabolic panel, lactate dehydrogenase test, inflammatory markers, and viral testing failed to reveal any evidence of underlying malignancy.
After conferring with the patient’s neurologist, lamotrigine was discontinued. Within a few weeks of cessation, the scalp lesions resolved without recurrence at 9-month follow-up. In addition to the lack of clinical, histological, or immunohistochemical evidence of underlying malignancy, the temporal association of the development of lesions after starting lamotrigine and rapid resolution upon its discontinuation suggested a diagnosis of lamotrigine-induced cutaneous pseudolymphoma.
Cutaneous pseudolymphoma is a term used to describe a heterogenous group of benign reactive T-cell, B-cell, or mixed-cell lymphoproliferative processes that resemble cutaneous lymphomas clinically and/or histopathologically.1 Historically, these types of proliferations have been classified under many alternative names that originally served to describe only B-cell–type proliferations. With advances in immunohistochemistry allowing for more specific cell marker identification, cutaneous pseudolymphomas often are found to contain a mixture of T-cell and B-cell populations, which also led to identifying and describing T-cell–type pseudolymphomas.2
The clinical appearance of cutaneous pseudolymphoma is variable, ranging from discrete nodules or papules to even confluent erythroderma in certain cases.2 The high clinical variability further complicates diagnosis. Although our patient presented with 9 individual nodular lesions, this finding alone is not sufficient to have high suspicion for cutaneous pseudolymphoma without including a much broader differential diagnosis. In our case, the differential diagnosis also included cutaneous lymphoma, arthropod bite reaction, lymphomatoid papulosis, tumid lupus, follicular mucinosis, lymphocytic infiltrate of Jessner, and leukemia cutis.
The primary concern regarding diagnosis of cutaneous pseudolymphoma is the clinician’s ability to effectively differentiate this entity from a true malignant lymphoma. Immunostaining has some value by identification of heterogeneous cell–type populations with a mixed T-cell and B-cell infiltrate that is more characteristic of a benign reactive process. Subsequent polymerase chain reaction analysis can detect the presence or absence of monoclonal T-cell receptor gene rearrangement or immunoglobulin heavy chain rearrangement.3 If these monoclonal rearrangements are absent, a benign diagnosis is favored; however, these rearrangements also have been shown to exist in a case of cutaneous pseudolymphoma that earned the final diagnosis when removal of the offending agent led to spontaneous lesion regression, similar to our case.4
Many different entities have been described as causative factors for the development of cutaneous pseudolymphoma. Of those that have been considered causative, simple categories have emerged, including endogenous, exogenous, and iatrogenic causes. One potential endogenous etiology of cutaneous pseudolymphoma is IgG4-related disease.5 A multitude of exogenous causes have been reported, including several cases of cutaneous pseudolymphoma developing in a prior tattoo site.6 Viruses, specifically molluscum contagiosum, also have been implicated as exogenous causes, and a report of cutaneous pseudolymphoma development at a prior site of herpes zoster lesions has been described.7 Development of cutaneous pseudolymphoma in vaccination sites also has been reported,8 as well as more obscure inciting events such as Leishmania donovani infection and medicinal leech therapy.9
A considerable number of reported cases of cutaneous pseudolymphoma have been attributed to drugs, including monoclonal antibodies,10 herbal supplements,11 and a multitude of other medications.1 As a class, anticonvulsants are considered more likely to cause lymph node pseudolymphomas than strictly cutaneous pseudolymphomas12; however, many drugs in this class of medications have been described in the development of cutaneous pseudolymphoma.3 A review of the literature by Ploysangam et al1 revealed reports of the development of cutaneous pseudolymphomas after administration of phenytoin, carbamazepine, mephenytoin, trimethadione, phenobarbital, primidone, butabarbital, methsuximide, phensuximide, and valproic acid.
Our patient represents a rare case of strictly cutaneous pseudolymphoma caused by administration of lamotrigine. Our case demonstrated a clear temporal relation between the cessation of lamotrigine and rapid and spontaneous disappearance of cutaneous lesions. We found another case of pseudolymphoma in which lamotrigine was deemed causative, but only lymph node involvement was observed.12
Proper diagnosis of cutaneous pseudolymphoma is important not only with regard to the initial differentiation from true malignant lymphoma but in allowing for appropriate follow-up and vigilant surveillance. Cases of progression from cutaneous pseudolymphoma to true lymphoma have been reported.1,2 It is recommended that watchful follow-up for these patients be carried out until at least 5 years after the diagnosis of cutaneous pseudolymphoma is made to rule out the possibility of malignant transformation, particularly in idiopathic cases.13
- Ploysangam T, Breneman D, Mutasim D. Cutaneous pseudolymphomas. J Am Acad Dermatol. 1998;38:877-898.
- Bergman R. Pseudolymphoma and cutaneous lymphoma: facts and controversies. Clin Dermatol. 2010;28:568-574.
- Braddock S, Harrington D, Vose J. Generalized nodular cutaneous pseudolymphoma associated with phenytoin therapy. J Am Acad Dermatol. 1992;27:337-340.
- Cogrel O, Beylot-Barry M, Vergier B, et al. Sodium valproate-induced cutaneous pseudolymphoma followed by recurrence with carbamazepine. Br J Dermatol. 2001;144:1235-1238.
- Cheuk W, Lee K, Chong L, et al. IgG4-related sclerosing disease: a potential new etiology of cutaneous pseudolymphoma. Am J Surg Pathol. 2009;33:1713-1719.
- Marchesi A, Parodi P, Brioschi M, et al. Tattoo ink-related cutaneous pseudolymphomas: a rare but significant complication. case report and review of the literature. Aesthetic Plast Surg. 2014;38:471-478.
- Gonzalez J, Sanz A, Martin T, et al. Cutaneous pseudolymphoma associated with molluscum contagiosum: a case report. Int J Dermatol. 2008;47:502-504.
- Maubec E, Pinquier L, Viguier M, et al. Vaccination-induced cutaneous pseudolymphoma. J Am Acad Dermatol. 2005;52:623-629.
- Altamura D, Calonje E, Liau J, et al. Diffuse cutaneous pseudolymphoma due to therapy with medicinal leeches. JAMA Dermatol. 2014;150:783-784.
- Imafuku S, Ito K, Nakayama J. Cutaneous pseudolymphoma induced by adalimumab and reproduced by infliximab in a patient with arthopathic psoriasis. Br J Dermatol. 2011;166:675-678.
- Meyer S, Vogt T, Obermann EC, et al. Cutaneous pseudolymphoma induced by Cimicifuga racemosa. Dermatology. 2007;214:94-96.
- Pathak P, McLachlan R. Drug-induced pseudolymphoma secondary to lamotrigine. Neurology. 1998;50:1509-1510.
- Prabu V, Shivani A, Pawar V. Idiopathic cutaneous pseudolymphoma: an enigma. Indian Dermatol Online J. 2014;5:224-226.
- Ploysangam T, Breneman D, Mutasim D. Cutaneous pseudolymphomas. J Am Acad Dermatol. 1998;38:877-898.
- Bergman R. Pseudolymphoma and cutaneous lymphoma: facts and controversies. Clin Dermatol. 2010;28:568-574.
- Braddock S, Harrington D, Vose J. Generalized nodular cutaneous pseudolymphoma associated with phenytoin therapy. J Am Acad Dermatol. 1992;27:337-340.
- Cogrel O, Beylot-Barry M, Vergier B, et al. Sodium valproate-induced cutaneous pseudolymphoma followed by recurrence with carbamazepine. Br J Dermatol. 2001;144:1235-1238.
- Cheuk W, Lee K, Chong L, et al. IgG4-related sclerosing disease: a potential new etiology of cutaneous pseudolymphoma. Am J Surg Pathol. 2009;33:1713-1719.
- Marchesi A, Parodi P, Brioschi M, et al. Tattoo ink-related cutaneous pseudolymphomas: a rare but significant complication. case report and review of the literature. Aesthetic Plast Surg. 2014;38:471-478.
- Gonzalez J, Sanz A, Martin T, et al. Cutaneous pseudolymphoma associated with molluscum contagiosum: a case report. Int J Dermatol. 2008;47:502-504.
- Maubec E, Pinquier L, Viguier M, et al. Vaccination-induced cutaneous pseudolymphoma. J Am Acad Dermatol. 2005;52:623-629.
- Altamura D, Calonje E, Liau J, et al. Diffuse cutaneous pseudolymphoma due to therapy with medicinal leeches. JAMA Dermatol. 2014;150:783-784.
- Imafuku S, Ito K, Nakayama J. Cutaneous pseudolymphoma induced by adalimumab and reproduced by infliximab in a patient with arthopathic psoriasis. Br J Dermatol. 2011;166:675-678.
- Meyer S, Vogt T, Obermann EC, et al. Cutaneous pseudolymphoma induced by Cimicifuga racemosa. Dermatology. 2007;214:94-96.
- Pathak P, McLachlan R. Drug-induced pseudolymphoma secondary to lamotrigine. Neurology. 1998;50:1509-1510.
- Prabu V, Shivani A, Pawar V. Idiopathic cutaneous pseudolymphoma: an enigma. Indian Dermatol Online J. 2014;5:224-226.
Practice Points
- Cutaneous pseudolymphomas are a heterogenous group of benign T-cell, B-cell, or mixed-cell lymphoproliferative processes that resemble cutaneous lymphomas clinically and/or histopathologically.
- Cutaneous pseudolymphomas have many causative factors, including medications, infections, tattoo ink, vaccinations, and insect bites.
- Lamotrigine is a potential inciting factor of cutaneous pseudolymphoma.
Social determinants of health gaining prominence
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
Rozlytrek approved for ROS1-positive metastatic NSCLC, cancers with NTRK gene fusion defects
Rozlytrek (entrectinib) has been approved to treat cancers with neurotrophic tyrosine receptor kinase (NTRK) gene fusion defects in adults and adolescents for whom there are no effective treatments, the Food and Drug Administration announced in a press release.
Entrectinib was also approved for the treatment of adults with metastatic non–small cell lung cancers that are ROS1-positive.
“We are in an exciting era of innovation in cancer treatment as we continue to see development in tissue-agnostic therapies, which have the potential to transform cancer treatment. We’re seeing continued advances in the use of biomarkers to guide drug development and the more targeted delivery of medicine,” FDA Acting Commissioner Ned Sharpless, MD, said in the release.
This is the third time the agency has approved a cancer treatment based on a common biomarker across different types of tumors rather than on the original tumor’s location. The previous tissue-agnostic indications approved by the FDA were pembrolizumab (Keytruda) for tumors with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) tumors in 2017 and larotrectinib (Vitrakvi) for NTRK gene fusion tumors in 2018.
The approval of entrectinib was granted to Genentech. “Rozlytrek is the first FDA-approved treatment that selectively targets both ROS1 and NTRK fusions, and, importantly, has also shown responses in these rare cancer types that have spread to the brain,” Sandra Horning, MD, chief medical officer and head of global product development for Genentech, said in a separate press release.
Foundation Medicine will submit Foundation One CDx to the FDA for approval as a companion diagnostic for entrectinib, according to the Genentech release; an FDA-approved companion diagnostic for entrectinib is not available at this time.
“Today’s approval includes an indication for pediatric patients, 12 years of age and older, who have NTRK fusion–positive tumors by relying on efficacy information obtained primarily in adults,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Efficacy in adolescents was derived from adult data and safety was demonstrated in 30 pediatric patients.”
Entrectinib was evaluated in four clinical trials that included 54 adults with NTRK fusion–positive tumors. The overall response rate was 57%, with 7.4% of patients having complete disappearance of the tumor. Among the 31 patients with tumor shrinkage, 61% had tumor shrinkage persist for 9 months or longer. The most common cancer locations were the lung, salivary gland, breast, thyroid, and colon/rectum.
Clinical studies evaluated 51 adults with ROS1-positive lung cancer. The overall response rate was 78%, with 5.9% of patients having complete disappearance of their cancer. Among the 40 patients with tumor shrinkage, 55% had tumor shrinkage persist for 12 months or longer.
The most serious side effects of entrectinib are heart failure, central nervous system effects, changes in sleep pattern, skeletal fractures, hepatotoxicity, hyperuricemia, QT prolongation, and vision disorders. Females of reproductive age and males with a female partner of reproductive potential are advised to use effective contraception during treatment; the drug may cause harm to a developing fetus or newborn baby.
Genentech must provide additional clinical trial data to the FDA as a condition of the approval.
Rozlytrek (entrectinib) has been approved to treat cancers with neurotrophic tyrosine receptor kinase (NTRK) gene fusion defects in adults and adolescents for whom there are no effective treatments, the Food and Drug Administration announced in a press release.
Entrectinib was also approved for the treatment of adults with metastatic non–small cell lung cancers that are ROS1-positive.
“We are in an exciting era of innovation in cancer treatment as we continue to see development in tissue-agnostic therapies, which have the potential to transform cancer treatment. We’re seeing continued advances in the use of biomarkers to guide drug development and the more targeted delivery of medicine,” FDA Acting Commissioner Ned Sharpless, MD, said in the release.
This is the third time the agency has approved a cancer treatment based on a common biomarker across different types of tumors rather than on the original tumor’s location. The previous tissue-agnostic indications approved by the FDA were pembrolizumab (Keytruda) for tumors with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) tumors in 2017 and larotrectinib (Vitrakvi) for NTRK gene fusion tumors in 2018.
The approval of entrectinib was granted to Genentech. “Rozlytrek is the first FDA-approved treatment that selectively targets both ROS1 and NTRK fusions, and, importantly, has also shown responses in these rare cancer types that have spread to the brain,” Sandra Horning, MD, chief medical officer and head of global product development for Genentech, said in a separate press release.
Foundation Medicine will submit Foundation One CDx to the FDA for approval as a companion diagnostic for entrectinib, according to the Genentech release; an FDA-approved companion diagnostic for entrectinib is not available at this time.
“Today’s approval includes an indication for pediatric patients, 12 years of age and older, who have NTRK fusion–positive tumors by relying on efficacy information obtained primarily in adults,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Efficacy in adolescents was derived from adult data and safety was demonstrated in 30 pediatric patients.”
Entrectinib was evaluated in four clinical trials that included 54 adults with NTRK fusion–positive tumors. The overall response rate was 57%, with 7.4% of patients having complete disappearance of the tumor. Among the 31 patients with tumor shrinkage, 61% had tumor shrinkage persist for 9 months or longer. The most common cancer locations were the lung, salivary gland, breast, thyroid, and colon/rectum.
Clinical studies evaluated 51 adults with ROS1-positive lung cancer. The overall response rate was 78%, with 5.9% of patients having complete disappearance of their cancer. Among the 40 patients with tumor shrinkage, 55% had tumor shrinkage persist for 12 months or longer.
The most serious side effects of entrectinib are heart failure, central nervous system effects, changes in sleep pattern, skeletal fractures, hepatotoxicity, hyperuricemia, QT prolongation, and vision disorders. Females of reproductive age and males with a female partner of reproductive potential are advised to use effective contraception during treatment; the drug may cause harm to a developing fetus or newborn baby.
Genentech must provide additional clinical trial data to the FDA as a condition of the approval.
Rozlytrek (entrectinib) has been approved to treat cancers with neurotrophic tyrosine receptor kinase (NTRK) gene fusion defects in adults and adolescents for whom there are no effective treatments, the Food and Drug Administration announced in a press release.
Entrectinib was also approved for the treatment of adults with metastatic non–small cell lung cancers that are ROS1-positive.
“We are in an exciting era of innovation in cancer treatment as we continue to see development in tissue-agnostic therapies, which have the potential to transform cancer treatment. We’re seeing continued advances in the use of biomarkers to guide drug development and the more targeted delivery of medicine,” FDA Acting Commissioner Ned Sharpless, MD, said in the release.
This is the third time the agency has approved a cancer treatment based on a common biomarker across different types of tumors rather than on the original tumor’s location. The previous tissue-agnostic indications approved by the FDA were pembrolizumab (Keytruda) for tumors with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) tumors in 2017 and larotrectinib (Vitrakvi) for NTRK gene fusion tumors in 2018.
The approval of entrectinib was granted to Genentech. “Rozlytrek is the first FDA-approved treatment that selectively targets both ROS1 and NTRK fusions, and, importantly, has also shown responses in these rare cancer types that have spread to the brain,” Sandra Horning, MD, chief medical officer and head of global product development for Genentech, said in a separate press release.
Foundation Medicine will submit Foundation One CDx to the FDA for approval as a companion diagnostic for entrectinib, according to the Genentech release; an FDA-approved companion diagnostic for entrectinib is not available at this time.
“Today’s approval includes an indication for pediatric patients, 12 years of age and older, who have NTRK fusion–positive tumors by relying on efficacy information obtained primarily in adults,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Efficacy in adolescents was derived from adult data and safety was demonstrated in 30 pediatric patients.”
Entrectinib was evaluated in four clinical trials that included 54 adults with NTRK fusion–positive tumors. The overall response rate was 57%, with 7.4% of patients having complete disappearance of the tumor. Among the 31 patients with tumor shrinkage, 61% had tumor shrinkage persist for 9 months or longer. The most common cancer locations were the lung, salivary gland, breast, thyroid, and colon/rectum.
Clinical studies evaluated 51 adults with ROS1-positive lung cancer. The overall response rate was 78%, with 5.9% of patients having complete disappearance of their cancer. Among the 40 patients with tumor shrinkage, 55% had tumor shrinkage persist for 12 months or longer.
The most serious side effects of entrectinib are heart failure, central nervous system effects, changes in sleep pattern, skeletal fractures, hepatotoxicity, hyperuricemia, QT prolongation, and vision disorders. Females of reproductive age and males with a female partner of reproductive potential are advised to use effective contraception during treatment; the drug may cause harm to a developing fetus or newborn baby.
Genentech must provide additional clinical trial data to the FDA as a condition of the approval.
Consider hormones and mood in adolescent girls
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at pdnews@mdedge.com.
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at pdnews@mdedge.com.
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at pdnews@mdedge.com.
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
ALERT: Grandmother in the room!
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Doctors concerned about recent immigration changes
New Trump administration regulations will make it more difficult for immigrants to remain in the United States if they receive health care assistance – in sharp contrasts to a recent movement in medicine to address the social determinants of health.
Under longstanding immigration policy, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge.
Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The new regulation, published Aug. 14 in the Federal Register, allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program (SNAP), and several housing programs. The final regulation continues to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
The rule is not only unethical, but it will cause medical care to be unavailable to patients who are hardworking, have families to support, and often are employed in trades that are low-paying, said Alan R. Nelson, MD, an internist-endocrinologist and former special advisor to the CEO of the American College of Physicians.
“The rule not only flies in the face of efforts to confront social determinants of health and thereby reduce disparities in care and outcomes, but will strain emergency and safety net services at the local/county level and burden hospitals and clinics with more uncompensated care,” Dr. Nelson said in an interview. “Everybody loses.”
In a joint statement, the American Academy of Family Physicians, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the ACP, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
The change comes amid ongoing efforts among physicians and health care professionals to address health care disparities based on cultural differences and social factors. A number of medical schools, such as the University of Pennsylvania’s in Philadelphia, are enhancing their curriculum on social determinants of health to develop more sensitive and culturally competent physicians.
Meanwhile, the American Medical Association in April announced a collaboration with UnitedHealthcare that aims to address social and environmental factors that affect patients’ health by standardizing data collection of social determinants of health. The two groups support the creation of 23 new ICD-10 codes related to social determinants that would capture such factors as access to nutritious food, adequate and safe housing, available transportation, ability to pay for medications, and ability to pay for utilities.
William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said there appears to be a growing disconnect between government policy and evolving trends in population health.
“There are public policy issues evolving that I think will put the health care profession at odds with some of the economic regulation being put in place,” said Dr. Golden. “I think people are increasingly realizing that to manage population health, you have to go beyond treating lab values and X-rays. Social environment is a big driver in people’s health status. It’s no surprise that people who have lower educational obtainment and who have more challenging financial situations are often in more challenged health status. Add that to people who are now potentially not having access to health coverage, and I think it’s a set up for creating a population that will present to our [emergency rooms] with significant acute care challenges.”
This article was updated 8/22/2019.
New Trump administration regulations will make it more difficult for immigrants to remain in the United States if they receive health care assistance – in sharp contrasts to a recent movement in medicine to address the social determinants of health.
Under longstanding immigration policy, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge.
Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The new regulation, published Aug. 14 in the Federal Register, allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program (SNAP), and several housing programs. The final regulation continues to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
The rule is not only unethical, but it will cause medical care to be unavailable to patients who are hardworking, have families to support, and often are employed in trades that are low-paying, said Alan R. Nelson, MD, an internist-endocrinologist and former special advisor to the CEO of the American College of Physicians.
“The rule not only flies in the face of efforts to confront social determinants of health and thereby reduce disparities in care and outcomes, but will strain emergency and safety net services at the local/county level and burden hospitals and clinics with more uncompensated care,” Dr. Nelson said in an interview. “Everybody loses.”
In a joint statement, the American Academy of Family Physicians, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the ACP, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
The change comes amid ongoing efforts among physicians and health care professionals to address health care disparities based on cultural differences and social factors. A number of medical schools, such as the University of Pennsylvania’s in Philadelphia, are enhancing their curriculum on social determinants of health to develop more sensitive and culturally competent physicians.
Meanwhile, the American Medical Association in April announced a collaboration with UnitedHealthcare that aims to address social and environmental factors that affect patients’ health by standardizing data collection of social determinants of health. The two groups support the creation of 23 new ICD-10 codes related to social determinants that would capture such factors as access to nutritious food, adequate and safe housing, available transportation, ability to pay for medications, and ability to pay for utilities.
William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said there appears to be a growing disconnect between government policy and evolving trends in population health.
“There are public policy issues evolving that I think will put the health care profession at odds with some of the economic regulation being put in place,” said Dr. Golden. “I think people are increasingly realizing that to manage population health, you have to go beyond treating lab values and X-rays. Social environment is a big driver in people’s health status. It’s no surprise that people who have lower educational obtainment and who have more challenging financial situations are often in more challenged health status. Add that to people who are now potentially not having access to health coverage, and I think it’s a set up for creating a population that will present to our [emergency rooms] with significant acute care challenges.”
This article was updated 8/22/2019.
New Trump administration regulations will make it more difficult for immigrants to remain in the United States if they receive health care assistance – in sharp contrasts to a recent movement in medicine to address the social determinants of health.
Under longstanding immigration policy, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge.
Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The new regulation, published Aug. 14 in the Federal Register, allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program (SNAP), and several housing programs. The final regulation continues to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
The rule is not only unethical, but it will cause medical care to be unavailable to patients who are hardworking, have families to support, and often are employed in trades that are low-paying, said Alan R. Nelson, MD, an internist-endocrinologist and former special advisor to the CEO of the American College of Physicians.
“The rule not only flies in the face of efforts to confront social determinants of health and thereby reduce disparities in care and outcomes, but will strain emergency and safety net services at the local/county level and burden hospitals and clinics with more uncompensated care,” Dr. Nelson said in an interview. “Everybody loses.”
In a joint statement, the American Academy of Family Physicians, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the ACP, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
The change comes amid ongoing efforts among physicians and health care professionals to address health care disparities based on cultural differences and social factors. A number of medical schools, such as the University of Pennsylvania’s in Philadelphia, are enhancing their curriculum on social determinants of health to develop more sensitive and culturally competent physicians.
Meanwhile, the American Medical Association in April announced a collaboration with UnitedHealthcare that aims to address social and environmental factors that affect patients’ health by standardizing data collection of social determinants of health. The two groups support the creation of 23 new ICD-10 codes related to social determinants that would capture such factors as access to nutritious food, adequate and safe housing, available transportation, ability to pay for medications, and ability to pay for utilities.
William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said there appears to be a growing disconnect between government policy and evolving trends in population health.
“There are public policy issues evolving that I think will put the health care profession at odds with some of the economic regulation being put in place,” said Dr. Golden. “I think people are increasingly realizing that to manage population health, you have to go beyond treating lab values and X-rays. Social environment is a big driver in people’s health status. It’s no surprise that people who have lower educational obtainment and who have more challenging financial situations are often in more challenged health status. Add that to people who are now potentially not having access to health coverage, and I think it’s a set up for creating a population that will present to our [emergency rooms] with significant acute care challenges.”
This article was updated 8/22/2019.
Chernobyl vodka, music-enhanced cheese, and bong bacteria
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
CDC updates recommendation for serologic Lyme disease detection
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
FROM THE MMWR