User login
Irregular macule on back
The FP suspected that this could be a melanoma and took out his dermatoscope. (See “Dermoscopy in family medicine: A primer.”) The FP was initially concerned about melanoma because the lesion appeared chaotic, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the macule was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was >6 mm, but the history was insufficient to say whether it was Enlarging. Of course, 4 out of 5 positive criteria requires a tissue diagnosis.
Dermoscopy added evidence for regression in the center and an atypical network in the brown and black areas. The FP performed a deep shave biopsy (saucerization) with 2 mm margins to provide full sampling for the pathologist. (See the Watch & Learn video on “Shave biopsy.”) The depth of the tissue biopsy was approximately 1 to 1.5 mm, which was adequate for a lesion of this type. The pathology report confirmed melanoma in situ.
On a return visit, the FP performed a local wide excision with 5 mm margins down to the deep fat. The surgical specimen revealed only the scar at the biopsy site with no remaining cancer. This reassured the patient because it should provide a cure very near 100%. The FP provided counseling about sun protection and the need for regular skin exams.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP suspected that this could be a melanoma and took out his dermatoscope. (See “Dermoscopy in family medicine: A primer.”) The FP was initially concerned about melanoma because the lesion appeared chaotic, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the macule was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was >6 mm, but the history was insufficient to say whether it was Enlarging. Of course, 4 out of 5 positive criteria requires a tissue diagnosis.
Dermoscopy added evidence for regression in the center and an atypical network in the brown and black areas. The FP performed a deep shave biopsy (saucerization) with 2 mm margins to provide full sampling for the pathologist. (See the Watch & Learn video on “Shave biopsy.”) The depth of the tissue biopsy was approximately 1 to 1.5 mm, which was adequate for a lesion of this type. The pathology report confirmed melanoma in situ.
On a return visit, the FP performed a local wide excision with 5 mm margins down to the deep fat. The surgical specimen revealed only the scar at the biopsy site with no remaining cancer. This reassured the patient because it should provide a cure very near 100%. The FP provided counseling about sun protection and the need for regular skin exams.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP suspected that this could be a melanoma and took out his dermatoscope. (See “Dermoscopy in family medicine: A primer.”) The FP was initially concerned about melanoma because the lesion appeared chaotic, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the macule was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was >6 mm, but the history was insufficient to say whether it was Enlarging. Of course, 4 out of 5 positive criteria requires a tissue diagnosis.
Dermoscopy added evidence for regression in the center and an atypical network in the brown and black areas. The FP performed a deep shave biopsy (saucerization) with 2 mm margins to provide full sampling for the pathologist. (See the Watch & Learn video on “Shave biopsy.”) The depth of the tissue biopsy was approximately 1 to 1.5 mm, which was adequate for a lesion of this type. The pathology report confirmed melanoma in situ.
On a return visit, the FP performed a local wide excision with 5 mm margins down to the deep fat. The surgical specimen revealed only the scar at the biopsy site with no remaining cancer. This reassured the patient because it should provide a cure very near 100%. The FP provided counseling about sun protection and the need for regular skin exams.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill; 2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
Love hormone plein air, posh preused Kleenex, and dieting plague vectors
Paint me like one of your French girls
If you’re trying to think of a fun Valentine’s activity, look no further than paint night! Normally associated with a ladies night out (and heavy on the wine), a recent study found that painting releases high levels of the “love hormone”, a.k.a. oxytocin, in men.
Researchers compared the levels of oxytocin with partners painting and partners playing board games, and were surprised by the results: While all the couples released oxytocin during these activities, men in paint class had the highest levels – twice as much as any other group.
Feel free to cite this study next time your man complains about being dragged to a paint-and-sip. Painting partners also experienced more touching than the gaming group (unless you count throwing Monopoly pieces at your significant other as touching).
You won’t get me sick, I’ll get me sick!
There are certain items that, after being used once, you really wouldn’t want to reuse. A snotty, mucus-filled tissue is pretty high up on that list ... or so you would hope. But that’s not thinking with real American entrepreneurial spirit! Welcome to Vaev Tissue, a startup based in Los Angeles that sells used tissues containing germs from a sick person for the bargain price of $79.99.
Yes, you read that correctly. They sell an $80 used tissue. The purpose, according to Vaev’s mission statement, is “to get sick on your own terms,” as “using a tissue that carries a human sneeze is safer than needles or pills.”
As you might expect, the tissues are popular with young parents and adults who are “critical” of vaccines. Who else could hear advice from actual doctors who told Time magazine that “there is nothing positive that can come from this, only things that are adverse,” or that the tissues are an “incredible liability,” and continue on, regardless?
And if you’re thinking, “If these people want to get sick, why not just have someone sneeze on them?” Don’t be ridiculous. Focus testers responded highly negatively to simply being handed a dirty tissue. The premium packaging and high price tag are a necessity.
Our advice? Well, as tempting as all this sounds, we think we’ll stick with washing our hands and not sticking used tissues in our faces. You know, like reasonable people.
Why Bullwinkle thinks pink
Flying squirrels are secretly doing their best flamingo impression – who knew? A forestry professor discovered, by happy accident, that flying squirrels are fluorescent – they glow hot pink under ultraviolet light.
Turns out, almost all species of gliders – even blue-helmeted Rocket “Rocky” J. Squirrel – are members of the Pink Ladies. They are one of the very few glowing mammals; the only other known mammalian species to have fluorescent fur are certain opossums.
But why do these airborne rodents glow pink? Is it because of an overintake of bubblegum? Are flying squirrels just really flamboyant but also shy? Are they huge fans of the singer Pink?
A biologist involved in studying these colorful critters hypothesized that the reason is slightly more related to environment than musical preference. Flying squirrels are nocturnal, making them most active when UV light is most prominent. The garish glow might have something to do with nighttime perception.
However, we don’t know the answer for sure. And in the meantime, we can choose to believe flying squirrels eat way too much cotton candy.
Buzz, feed, diet. Repeat
Guns don’t hurt this mass murderer. Police can’t arrest it. Background checks are pointless. A border wall won’t keep it out. So, how do you stop a mosquito?
Diet drugs.
Because female mosquitoes transmit malaria, Zika, and other diseases when they move from person to person feeding on human blood, investigators sought to curb that appetite by chemically re-creating the feeling of fullness they get after a big meal.
The lady killers in their study – Aedes aegypti, to be exact – when given an antiobesity drug that suppresses human appetite by activating neuropeptide receptors that regulate food intake, turned away from a tempting piece of nylon stocking that had been worn by one of the researchers. Further work showed that treated mosquitoes were as disinterested in feeding on a live mouse as mosquitoes that had already enjoyed a full blood meal.
The LOTME research staff (What? Of course, we have a research staff. You don’t?) is working on the mosquito problem too, although we’ve taken a somewhat different approach: The “volunteers” who walk into the mosquito-filled room wear a sign that says, “My blood will make your butt look bigger.”
Paint me like one of your French girls
If you’re trying to think of a fun Valentine’s activity, look no further than paint night! Normally associated with a ladies night out (and heavy on the wine), a recent study found that painting releases high levels of the “love hormone”, a.k.a. oxytocin, in men.
Researchers compared the levels of oxytocin with partners painting and partners playing board games, and were surprised by the results: While all the couples released oxytocin during these activities, men in paint class had the highest levels – twice as much as any other group.
Feel free to cite this study next time your man complains about being dragged to a paint-and-sip. Painting partners also experienced more touching than the gaming group (unless you count throwing Monopoly pieces at your significant other as touching).
You won’t get me sick, I’ll get me sick!
There are certain items that, after being used once, you really wouldn’t want to reuse. A snotty, mucus-filled tissue is pretty high up on that list ... or so you would hope. But that’s not thinking with real American entrepreneurial spirit! Welcome to Vaev Tissue, a startup based in Los Angeles that sells used tissues containing germs from a sick person for the bargain price of $79.99.
Yes, you read that correctly. They sell an $80 used tissue. The purpose, according to Vaev’s mission statement, is “to get sick on your own terms,” as “using a tissue that carries a human sneeze is safer than needles or pills.”
As you might expect, the tissues are popular with young parents and adults who are “critical” of vaccines. Who else could hear advice from actual doctors who told Time magazine that “there is nothing positive that can come from this, only things that are adverse,” or that the tissues are an “incredible liability,” and continue on, regardless?
And if you’re thinking, “If these people want to get sick, why not just have someone sneeze on them?” Don’t be ridiculous. Focus testers responded highly negatively to simply being handed a dirty tissue. The premium packaging and high price tag are a necessity.
Our advice? Well, as tempting as all this sounds, we think we’ll stick with washing our hands and not sticking used tissues in our faces. You know, like reasonable people.
Why Bullwinkle thinks pink
Flying squirrels are secretly doing their best flamingo impression – who knew? A forestry professor discovered, by happy accident, that flying squirrels are fluorescent – they glow hot pink under ultraviolet light.
Turns out, almost all species of gliders – even blue-helmeted Rocket “Rocky” J. Squirrel – are members of the Pink Ladies. They are one of the very few glowing mammals; the only other known mammalian species to have fluorescent fur are certain opossums.
But why do these airborne rodents glow pink? Is it because of an overintake of bubblegum? Are flying squirrels just really flamboyant but also shy? Are they huge fans of the singer Pink?
A biologist involved in studying these colorful critters hypothesized that the reason is slightly more related to environment than musical preference. Flying squirrels are nocturnal, making them most active when UV light is most prominent. The garish glow might have something to do with nighttime perception.
However, we don’t know the answer for sure. And in the meantime, we can choose to believe flying squirrels eat way too much cotton candy.
Buzz, feed, diet. Repeat
Guns don’t hurt this mass murderer. Police can’t arrest it. Background checks are pointless. A border wall won’t keep it out. So, how do you stop a mosquito?
Diet drugs.
Because female mosquitoes transmit malaria, Zika, and other diseases when they move from person to person feeding on human blood, investigators sought to curb that appetite by chemically re-creating the feeling of fullness they get after a big meal.
The lady killers in their study – Aedes aegypti, to be exact – when given an antiobesity drug that suppresses human appetite by activating neuropeptide receptors that regulate food intake, turned away from a tempting piece of nylon stocking that had been worn by one of the researchers. Further work showed that treated mosquitoes were as disinterested in feeding on a live mouse as mosquitoes that had already enjoyed a full blood meal.
The LOTME research staff (What? Of course, we have a research staff. You don’t?) is working on the mosquito problem too, although we’ve taken a somewhat different approach: The “volunteers” who walk into the mosquito-filled room wear a sign that says, “My blood will make your butt look bigger.”
Paint me like one of your French girls
If you’re trying to think of a fun Valentine’s activity, look no further than paint night! Normally associated with a ladies night out (and heavy on the wine), a recent study found that painting releases high levels of the “love hormone”, a.k.a. oxytocin, in men.
Researchers compared the levels of oxytocin with partners painting and partners playing board games, and were surprised by the results: While all the couples released oxytocin during these activities, men in paint class had the highest levels – twice as much as any other group.
Feel free to cite this study next time your man complains about being dragged to a paint-and-sip. Painting partners also experienced more touching than the gaming group (unless you count throwing Monopoly pieces at your significant other as touching).
You won’t get me sick, I’ll get me sick!
There are certain items that, after being used once, you really wouldn’t want to reuse. A snotty, mucus-filled tissue is pretty high up on that list ... or so you would hope. But that’s not thinking with real American entrepreneurial spirit! Welcome to Vaev Tissue, a startup based in Los Angeles that sells used tissues containing germs from a sick person for the bargain price of $79.99.
Yes, you read that correctly. They sell an $80 used tissue. The purpose, according to Vaev’s mission statement, is “to get sick on your own terms,” as “using a tissue that carries a human sneeze is safer than needles or pills.”
As you might expect, the tissues are popular with young parents and adults who are “critical” of vaccines. Who else could hear advice from actual doctors who told Time magazine that “there is nothing positive that can come from this, only things that are adverse,” or that the tissues are an “incredible liability,” and continue on, regardless?
And if you’re thinking, “If these people want to get sick, why not just have someone sneeze on them?” Don’t be ridiculous. Focus testers responded highly negatively to simply being handed a dirty tissue. The premium packaging and high price tag are a necessity.
Our advice? Well, as tempting as all this sounds, we think we’ll stick with washing our hands and not sticking used tissues in our faces. You know, like reasonable people.
Why Bullwinkle thinks pink
Flying squirrels are secretly doing their best flamingo impression – who knew? A forestry professor discovered, by happy accident, that flying squirrels are fluorescent – they glow hot pink under ultraviolet light.
Turns out, almost all species of gliders – even blue-helmeted Rocket “Rocky” J. Squirrel – are members of the Pink Ladies. They are one of the very few glowing mammals; the only other known mammalian species to have fluorescent fur are certain opossums.
But why do these airborne rodents glow pink? Is it because of an overintake of bubblegum? Are flying squirrels just really flamboyant but also shy? Are they huge fans of the singer Pink?
A biologist involved in studying these colorful critters hypothesized that the reason is slightly more related to environment than musical preference. Flying squirrels are nocturnal, making them most active when UV light is most prominent. The garish glow might have something to do with nighttime perception.
However, we don’t know the answer for sure. And in the meantime, we can choose to believe flying squirrels eat way too much cotton candy.
Buzz, feed, diet. Repeat
Guns don’t hurt this mass murderer. Police can’t arrest it. Background checks are pointless. A border wall won’t keep it out. So, how do you stop a mosquito?
Diet drugs.
Because female mosquitoes transmit malaria, Zika, and other diseases when they move from person to person feeding on human blood, investigators sought to curb that appetite by chemically re-creating the feeling of fullness they get after a big meal.
The lady killers in their study – Aedes aegypti, to be exact – when given an antiobesity drug that suppresses human appetite by activating neuropeptide receptors that regulate food intake, turned away from a tempting piece of nylon stocking that had been worn by one of the researchers. Further work showed that treated mosquitoes were as disinterested in feeding on a live mouse as mosquitoes that had already enjoyed a full blood meal.
The LOTME research staff (What? Of course, we have a research staff. You don’t?) is working on the mosquito problem too, although we’ve taken a somewhat different approach: The “volunteers” who walk into the mosquito-filled room wear a sign that says, “My blood will make your butt look bigger.”
E-cigarettes beat nicotine patch for smoking cessation
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The rate of smokers who continued to use e-cigarettes after 1 year was “fairly high,” which might be problematic.
Major finding: Abstinence from smoking at 52 weeks was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001).
Study details: Randomized study of 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service.
Disclosures: Dr. Hajek reported grants and fees from Pfizer unrelated to the present study.The coauthors reported disclosures related to Pfizer, and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
Source: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
What makes women leave surgical training?
LONDON – Being unable to take leave and experiencing poor mental health are just two of the reasons uncovered that may help explain why despite having wanted to be a surgeon for many years, a study of women in surgical training has found. The results were presented at a press briefing and published in a special edition of the Lancet.
These factors are in addition to some previously identified, such as the long working hours, fatigue and sleep deprivation, unpredictable lifestyle and its effects on maintaining personal relationships, and the ability to both start and maintain a family life. Then there are the more serious issues of sexism and discrimination, bullying, and sexual harassment and assault that women face in a still male-dominated field that have been noted in prior studies.
“Women are underrepresented in surgery and leave training in higher proportions than men,” study lead Rhea Liang, MBChB, and coauthors wrote (Lancet. 2019;393:541-9). Previous attempts to understand why this is the case “have been confounded by not fully understanding the problem,” they suggested in the briefing. Their research took a more qualitative and feminist approach than other studies, consulting women who had chosen to leave rather than those who continued their surgical training.
Dr. Liang is a consultant general and breast surgeon based at the Gold Coast Hospital and Health Service in Robina, Australia, who personally interviewed women who had decided to leave their surgical training, some as early as 6 months and others up to 4 years after initiation, for reasons other than underperformance.
A “snowball approach” was used to recruit women whereby women who had agreed to participate were asked to refer others. Although only 12 women were interviewed, it’s quality over quantity, Dr. Liang said in a response to a Twitter comment on the study size. “The study is carried out in Australia where about 300 training places are offered across all the specialties annually. About 30% are women; 20% of those women choose to leave. So, if you do the maths, you’ll see that we actually recruited quite well,” she said at the briefing.
According to The Royal College of Practitioners, women made up a very small percentage of consultant surgeons in England in 2016 (11.1%), which didn’t change much by 2018 (12.2%). This is despite a high percentage (58%) of women being accepted onto university courses in medicine and dentistry (58% in 2016). So why so do so few women end up as surgeons?
“Training is a ‘pinch point’ at which women leave surgery,” Tim Dornan, PhD, noted at the launch of the special edition of the Lancet in which the findings appear. Dr. Dornan is professor of medical and interprofessional education at Queen’s University Belfast (Ireland) and one of the coauthors of the research.
This choice to leave surgery deprives society of able surgeons-to-be,” Dr. Dornan said, noting that there was evidence to suggest that women make as good, if not better, surgeons than men. The decision to leave also deprives women of career opportunities and potentially deprives patients of receiving the best surgical care.
“Something very striking about this research is that women who left within an average of 6-18 months after starting surgical training might have wanted to be surgeons from their teenage years, so it seems something happens at that pinch point which makes women to choose to leave.”
Qualitative research is a good way to understand causality in complex social systems, Dr. Dornan explained. Furthermore, “it’s equitable. If you use an open exploratory method, it’s entirely up to the participants to frame the research, it’s not done a priori, and it has the potential for great policy impact.”
Dr. Liang and team found that multiple factors played a role in the decision to leave surgical training, which on their own might be seemingly small, but when stacked on top of each other formed a tower, which was in danger of toppling after a threshold of three or four factors was reached. To exhaustion and lack of opportunity to learn, for example, could be added bullying, and then being denied leave while it is granted for a male colleague for a similar requested reason. The cumulative impact of these factors may all add up to create the impetus to leave.
“Just as a tower of blocks can rebalanced with small adjustments, out study indicates that relatively small interventions (e.g., a cup of tea or a supportive chat) could have been effective in preventing them choosing to leave,” she said.
However, they advocate targeting interventions at all trainees and not just women, to reduce gender differences as focusing on women would be more likely to exaggerate the “otherness” of women further and alienate male trainees. They suggest: “Women might be best helped by interventions that are alert to the possibility of unplanned negative effects, do not unduly focus on gender, and address multiple factors.”
“If you really want to benefit women you should benefit everybody and address the root problem, which is the harsh conditions of training,” Dr. Dornan said. “The prediction would be that, if you do that, then you will actually retain men as well as women.”
The research appears in a special edition of the Lancet that promotes advancing women in science, medicine, and global health.
SOURCE: Liang R et al. Lancet. 2019;393:541-9.
LONDON – Being unable to take leave and experiencing poor mental health are just two of the reasons uncovered that may help explain why despite having wanted to be a surgeon for many years, a study of women in surgical training has found. The results were presented at a press briefing and published in a special edition of the Lancet.
These factors are in addition to some previously identified, such as the long working hours, fatigue and sleep deprivation, unpredictable lifestyle and its effects on maintaining personal relationships, and the ability to both start and maintain a family life. Then there are the more serious issues of sexism and discrimination, bullying, and sexual harassment and assault that women face in a still male-dominated field that have been noted in prior studies.
“Women are underrepresented in surgery and leave training in higher proportions than men,” study lead Rhea Liang, MBChB, and coauthors wrote (Lancet. 2019;393:541-9). Previous attempts to understand why this is the case “have been confounded by not fully understanding the problem,” they suggested in the briefing. Their research took a more qualitative and feminist approach than other studies, consulting women who had chosen to leave rather than those who continued their surgical training.
Dr. Liang is a consultant general and breast surgeon based at the Gold Coast Hospital and Health Service in Robina, Australia, who personally interviewed women who had decided to leave their surgical training, some as early as 6 months and others up to 4 years after initiation, for reasons other than underperformance.
A “snowball approach” was used to recruit women whereby women who had agreed to participate were asked to refer others. Although only 12 women were interviewed, it’s quality over quantity, Dr. Liang said in a response to a Twitter comment on the study size. “The study is carried out in Australia where about 300 training places are offered across all the specialties annually. About 30% are women; 20% of those women choose to leave. So, if you do the maths, you’ll see that we actually recruited quite well,” she said at the briefing.
According to The Royal College of Practitioners, women made up a very small percentage of consultant surgeons in England in 2016 (11.1%), which didn’t change much by 2018 (12.2%). This is despite a high percentage (58%) of women being accepted onto university courses in medicine and dentistry (58% in 2016). So why so do so few women end up as surgeons?
“Training is a ‘pinch point’ at which women leave surgery,” Tim Dornan, PhD, noted at the launch of the special edition of the Lancet in which the findings appear. Dr. Dornan is professor of medical and interprofessional education at Queen’s University Belfast (Ireland) and one of the coauthors of the research.
This choice to leave surgery deprives society of able surgeons-to-be,” Dr. Dornan said, noting that there was evidence to suggest that women make as good, if not better, surgeons than men. The decision to leave also deprives women of career opportunities and potentially deprives patients of receiving the best surgical care.
“Something very striking about this research is that women who left within an average of 6-18 months after starting surgical training might have wanted to be surgeons from their teenage years, so it seems something happens at that pinch point which makes women to choose to leave.”
Qualitative research is a good way to understand causality in complex social systems, Dr. Dornan explained. Furthermore, “it’s equitable. If you use an open exploratory method, it’s entirely up to the participants to frame the research, it’s not done a priori, and it has the potential for great policy impact.”
Dr. Liang and team found that multiple factors played a role in the decision to leave surgical training, which on their own might be seemingly small, but when stacked on top of each other formed a tower, which was in danger of toppling after a threshold of three or four factors was reached. To exhaustion and lack of opportunity to learn, for example, could be added bullying, and then being denied leave while it is granted for a male colleague for a similar requested reason. The cumulative impact of these factors may all add up to create the impetus to leave.
“Just as a tower of blocks can rebalanced with small adjustments, out study indicates that relatively small interventions (e.g., a cup of tea or a supportive chat) could have been effective in preventing them choosing to leave,” she said.
However, they advocate targeting interventions at all trainees and not just women, to reduce gender differences as focusing on women would be more likely to exaggerate the “otherness” of women further and alienate male trainees. They suggest: “Women might be best helped by interventions that are alert to the possibility of unplanned negative effects, do not unduly focus on gender, and address multiple factors.”
“If you really want to benefit women you should benefit everybody and address the root problem, which is the harsh conditions of training,” Dr. Dornan said. “The prediction would be that, if you do that, then you will actually retain men as well as women.”
The research appears in a special edition of the Lancet that promotes advancing women in science, medicine, and global health.
SOURCE: Liang R et al. Lancet. 2019;393:541-9.
LONDON – Being unable to take leave and experiencing poor mental health are just two of the reasons uncovered that may help explain why despite having wanted to be a surgeon for many years, a study of women in surgical training has found. The results were presented at a press briefing and published in a special edition of the Lancet.
These factors are in addition to some previously identified, such as the long working hours, fatigue and sleep deprivation, unpredictable lifestyle and its effects on maintaining personal relationships, and the ability to both start and maintain a family life. Then there are the more serious issues of sexism and discrimination, bullying, and sexual harassment and assault that women face in a still male-dominated field that have been noted in prior studies.
“Women are underrepresented in surgery and leave training in higher proportions than men,” study lead Rhea Liang, MBChB, and coauthors wrote (Lancet. 2019;393:541-9). Previous attempts to understand why this is the case “have been confounded by not fully understanding the problem,” they suggested in the briefing. Their research took a more qualitative and feminist approach than other studies, consulting women who had chosen to leave rather than those who continued their surgical training.
Dr. Liang is a consultant general and breast surgeon based at the Gold Coast Hospital and Health Service in Robina, Australia, who personally interviewed women who had decided to leave their surgical training, some as early as 6 months and others up to 4 years after initiation, for reasons other than underperformance.
A “snowball approach” was used to recruit women whereby women who had agreed to participate were asked to refer others. Although only 12 women were interviewed, it’s quality over quantity, Dr. Liang said in a response to a Twitter comment on the study size. “The study is carried out in Australia where about 300 training places are offered across all the specialties annually. About 30% are women; 20% of those women choose to leave. So, if you do the maths, you’ll see that we actually recruited quite well,” she said at the briefing.
According to The Royal College of Practitioners, women made up a very small percentage of consultant surgeons in England in 2016 (11.1%), which didn’t change much by 2018 (12.2%). This is despite a high percentage (58%) of women being accepted onto university courses in medicine and dentistry (58% in 2016). So why so do so few women end up as surgeons?
“Training is a ‘pinch point’ at which women leave surgery,” Tim Dornan, PhD, noted at the launch of the special edition of the Lancet in which the findings appear. Dr. Dornan is professor of medical and interprofessional education at Queen’s University Belfast (Ireland) and one of the coauthors of the research.
This choice to leave surgery deprives society of able surgeons-to-be,” Dr. Dornan said, noting that there was evidence to suggest that women make as good, if not better, surgeons than men. The decision to leave also deprives women of career opportunities and potentially deprives patients of receiving the best surgical care.
“Something very striking about this research is that women who left within an average of 6-18 months after starting surgical training might have wanted to be surgeons from their teenage years, so it seems something happens at that pinch point which makes women to choose to leave.”
Qualitative research is a good way to understand causality in complex social systems, Dr. Dornan explained. Furthermore, “it’s equitable. If you use an open exploratory method, it’s entirely up to the participants to frame the research, it’s not done a priori, and it has the potential for great policy impact.”
Dr. Liang and team found that multiple factors played a role in the decision to leave surgical training, which on their own might be seemingly small, but when stacked on top of each other formed a tower, which was in danger of toppling after a threshold of three or four factors was reached. To exhaustion and lack of opportunity to learn, for example, could be added bullying, and then being denied leave while it is granted for a male colleague for a similar requested reason. The cumulative impact of these factors may all add up to create the impetus to leave.
“Just as a tower of blocks can rebalanced with small adjustments, out study indicates that relatively small interventions (e.g., a cup of tea or a supportive chat) could have been effective in preventing them choosing to leave,” she said.
However, they advocate targeting interventions at all trainees and not just women, to reduce gender differences as focusing on women would be more likely to exaggerate the “otherness” of women further and alienate male trainees. They suggest: “Women might be best helped by interventions that are alert to the possibility of unplanned negative effects, do not unduly focus on gender, and address multiple factors.”
“If you really want to benefit women you should benefit everybody and address the root problem, which is the harsh conditions of training,” Dr. Dornan said. “The prediction would be that, if you do that, then you will actually retain men as well as women.”
The research appears in a special edition of the Lancet that promotes advancing women in science, medicine, and global health.
SOURCE: Liang R et al. Lancet. 2019;393:541-9.
FROM A LAUNCH EVENT HELD BY THE LANCET
Key clinical point: Women leave surgical training for multiple reasons; interventions should focus on surgical training conditions not gender.
Major finding: Six new reasons identified: unavailability of leave; a distinction between valid and invalid reasons for leave; poor mental health; absence of interactions with women in surgery section and other supports; fear of repercussion; lack of pathways for independent and specific support.
Study details: Qualitative study of 12 women who chose to leave their surgical training after 6 months to 4 years.
Disclosures: No financial conflicts of interest were reported.
Source: Liang R et al. Lancet. 2019;393:541-9.
Irregularly Hyperpigmented Plaque on the Right Heel
The Diagnosis: Pigmented Bowen Disease
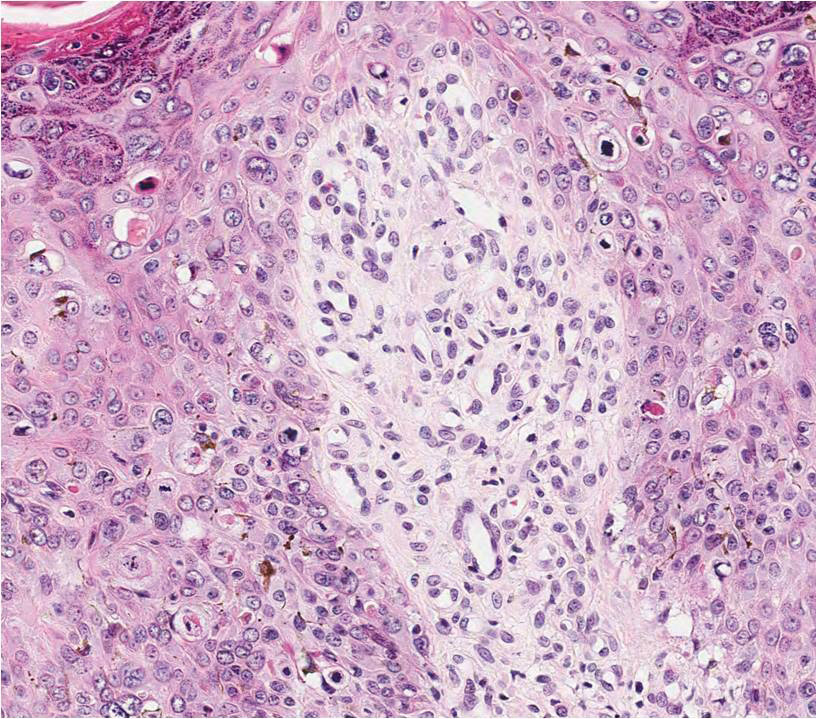
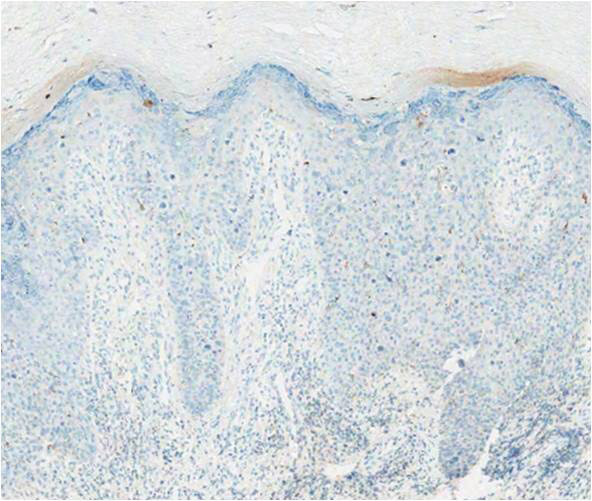
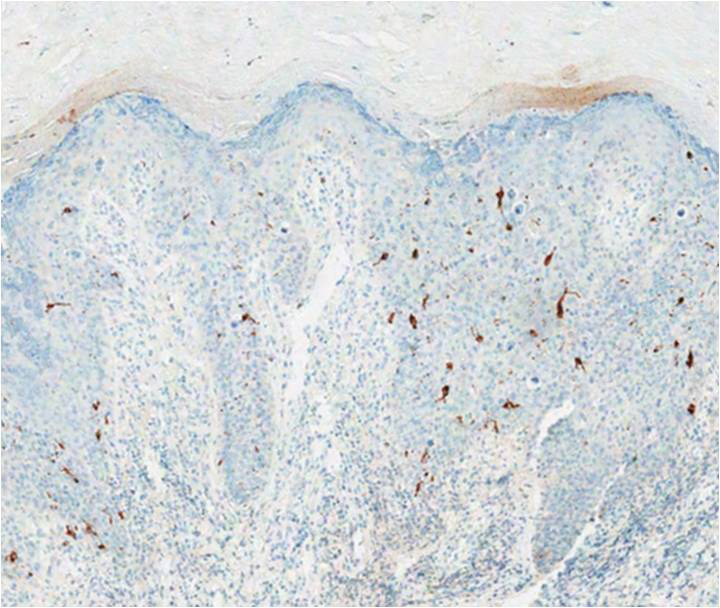
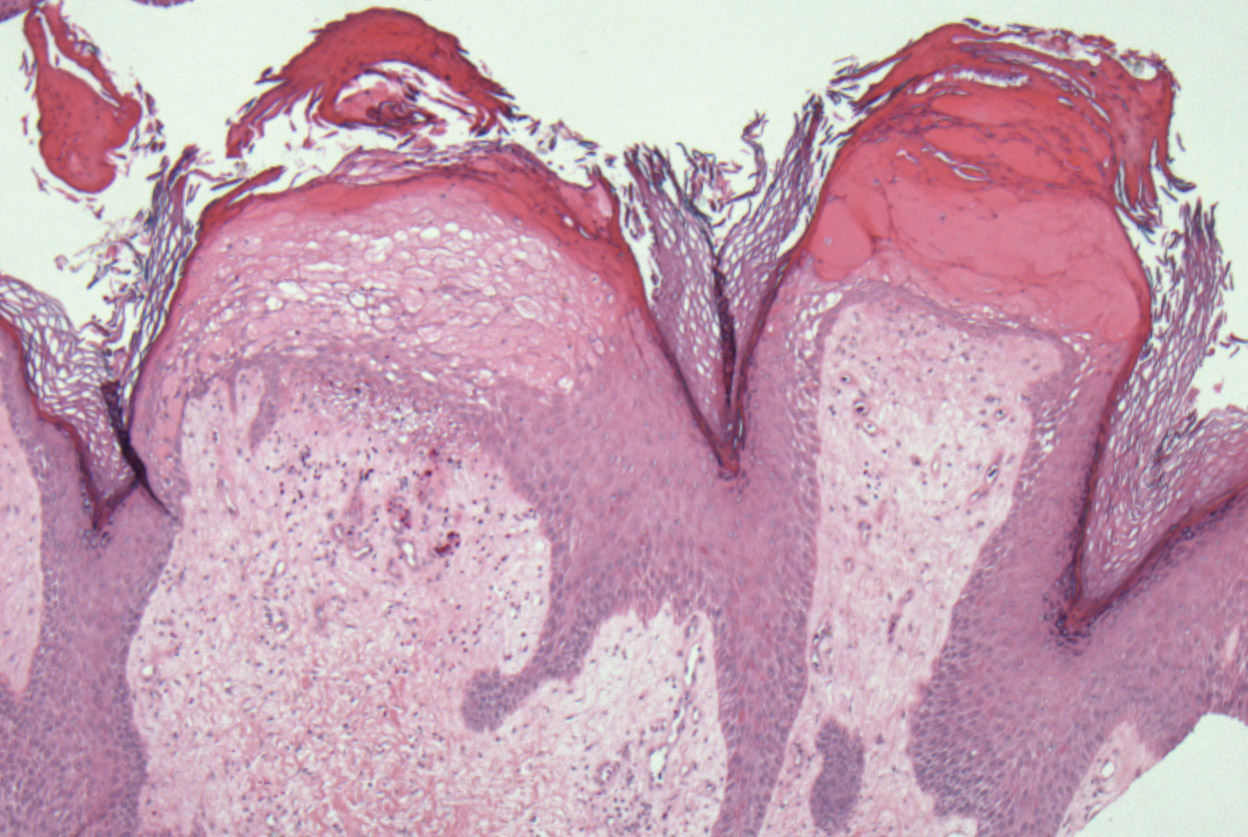
A biopsy of the lesion was performed for suspected acral malignant melanoma. Hematoxylin and eosin staining revealed acanthosis, elongation of rete ridges, and keratinocytes in complete disorder with atypical mitoses and pleomorphism affecting the full layer of the epidermis (Figure 1). The basement membrane was intact. Melanin pigmentation was increased in the lower epidermis and the upper dermis, and a lymphohistiocytic inflammatory infiltrate was present in the dermis. Staining for carcinoembryonic antigen (Figure 2) and melanoma
antigen (Figure 3) recognized by T cells (melan-A) both revealed negative results. Histopathologic findings led to the diagnosis of pigmented Bowen disease (BD).
Pigmented BD is a rare variant that accounts for 1.7% (N=420) to 5.5% (N=951) of all cases of BD.1,2 It is reported to affect men more than women and to be more prevalent in individuals with higher Fitzpatrick skin types.3 Furthermore, exposure to UV radiation, chemicals (eg, arsenic), or human papillomavirus, as well as immunosuppression, are known to be related to pigmented BD.2,4 Clinically, pigmented BD commonly involves nonexposed areas such as the anogenital area, trunk, and extremities, unlike typical BD that involves sun-exposed areas.5 In addition, it most frequently presents as a well-delineated, irregularly pigmented, asymptomatic
plaque and not as a scaly erythematous plaque. Therefore, the clinical diagnosis may be challenging. The differential diagnosis includes malignant melanoma, pigmented extramammary Paget disease, pigmented basal cell carcinoma, seborrheic keratosis, pigmented actinic keratosis, solar lentigo, and melanocytic nevi.
Histopathologically, a varying amount of melanin deposit is noted on hematoxylin and eosin staining, along with features of BD, including disarrayed atypical keratinocytes involving the full epidermis but not the basement membrane, with atypical individual cell keratinization.3,5,6 Pigmented extramammary Paget disease can mimic pigmented BD clinically and pathologically, but Paget cells stain positive for anticytokeratin (CAM 5.2), carcinoembryonic antigen, and mucicarmine, whereas cells in pigmented BD stain negative.7 Moreover, negative staining for human melanoma black, melan-A, and S-100 helps differentiate malignant melanoma from pigmented BD.8
The prognosis of pigmented BD is similar to classic BD and is independent of the presence of melanin pigment.6 Therefore, the treatment options do not differ from those for typical BD and include surgical excision, cryotherapy, laser ablation, topical imiquimod or 5-fluorouracil, curettage, electrosurgery, and photodynamic therapy (PDT).
In our case, the patient and her family did not want surgical removal; therefore, 1 course of fractional laser-assisted PDT and 2 courses of ablative laser-assisted PDT were performed. Unfortunately, the lesion persisted, possibly because it was too large and pigmented. Two months later, ingenol mebutate gel 0.05% was applied (4 courses) after using an ablative laser over 3 consecutive days with a 1-month interval between courses. The lesion resolved without any adverse events.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease [published online January 15, 2010]. J Am Acad Dermatol. 2010;62:597-604.
- Ragi G, Turner MS, Klein LE, et al. Pigmented Bowen’s disease and review of 420 Bowen’s disease lesions. J Dermatol Surg Oncol. 1988;14:765-769.
- Hernandez C, Ivkovic A, Fowler A. Growing plaque on foot. J Fam Pract. 2008;57:603-605.
- Hwang SW, Kim JW, Park SW, et al. Two cases of pigmented Bowen’s disease. Ann Dermatol 2002;14:127-129.
- Wilmer EM, Lee KC, Higgins W 2nd, et al. Hyperpigmented palmar plaque: an unexpected diagnosis of Bowen disease. Dermatol Online J. 2013;19:18573.
- Brinca A, Teixeira V, Gonçalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-884.
- Hilliard NJ, Huang C, Andea A. Pigmented extramammary Paget’s disease of the axilla mimicking melanoma: case report and review of the literature. J Cutan Pathol. 2009;36:995-1000.
- Öztürk Durmaz E, Dog˘ an Ekici I, Ozian F, et al. Pigmented Bowen’s disease of the genitalia masquerading as malignant melanoma. Acta Dermatovenerol Croat. 2015;23:130-133.
The Diagnosis: Pigmented Bowen Disease
A biopsy of the lesion was performed for suspected acral malignant melanoma. Hematoxylin and eosin staining revealed acanthosis, elongation of rete ridges, and keratinocytes in complete disorder with atypical mitoses and pleomorphism affecting the full layer of the epidermis (Figure 1). The basement membrane was intact. Melanin pigmentation was increased in the lower epidermis and the upper dermis, and a lymphohistiocytic inflammatory infiltrate was present in the dermis. Staining for carcinoembryonic antigen (Figure 2) and melanoma
antigen (Figure 3) recognized by T cells (melan-A) both revealed negative results. Histopathologic findings led to the diagnosis of pigmented Bowen disease (BD).
Pigmented BD is a rare variant that accounts for 1.7% (N=420) to 5.5% (N=951) of all cases of BD.1,2 It is reported to affect men more than women and to be more prevalent in individuals with higher Fitzpatrick skin types.3 Furthermore, exposure to UV radiation, chemicals (eg, arsenic), or human papillomavirus, as well as immunosuppression, are known to be related to pigmented BD.2,4 Clinically, pigmented BD commonly involves nonexposed areas such as the anogenital area, trunk, and extremities, unlike typical BD that involves sun-exposed areas.5 In addition, it most frequently presents as a well-delineated, irregularly pigmented, asymptomatic
plaque and not as a scaly erythematous plaque. Therefore, the clinical diagnosis may be challenging. The differential diagnosis includes malignant melanoma, pigmented extramammary Paget disease, pigmented basal cell carcinoma, seborrheic keratosis, pigmented actinic keratosis, solar lentigo, and melanocytic nevi.
Histopathologically, a varying amount of melanin deposit is noted on hematoxylin and eosin staining, along with features of BD, including disarrayed atypical keratinocytes involving the full epidermis but not the basement membrane, with atypical individual cell keratinization.3,5,6 Pigmented extramammary Paget disease can mimic pigmented BD clinically and pathologically, but Paget cells stain positive for anticytokeratin (CAM 5.2), carcinoembryonic antigen, and mucicarmine, whereas cells in pigmented BD stain negative.7 Moreover, negative staining for human melanoma black, melan-A, and S-100 helps differentiate malignant melanoma from pigmented BD.8
The prognosis of pigmented BD is similar to classic BD and is independent of the presence of melanin pigment.6 Therefore, the treatment options do not differ from those for typical BD and include surgical excision, cryotherapy, laser ablation, topical imiquimod or 5-fluorouracil, curettage, electrosurgery, and photodynamic therapy (PDT).
In our case, the patient and her family did not want surgical removal; therefore, 1 course of fractional laser-assisted PDT and 2 courses of ablative laser-assisted PDT were performed. Unfortunately, the lesion persisted, possibly because it was too large and pigmented. Two months later, ingenol mebutate gel 0.05% was applied (4 courses) after using an ablative laser over 3 consecutive days with a 1-month interval between courses. The lesion resolved without any adverse events.
The Diagnosis: Pigmented Bowen Disease
A biopsy of the lesion was performed for suspected acral malignant melanoma. Hematoxylin and eosin staining revealed acanthosis, elongation of rete ridges, and keratinocytes in complete disorder with atypical mitoses and pleomorphism affecting the full layer of the epidermis (Figure 1). The basement membrane was intact. Melanin pigmentation was increased in the lower epidermis and the upper dermis, and a lymphohistiocytic inflammatory infiltrate was present in the dermis. Staining for carcinoembryonic antigen (Figure 2) and melanoma
antigen (Figure 3) recognized by T cells (melan-A) both revealed negative results. Histopathologic findings led to the diagnosis of pigmented Bowen disease (BD).
Pigmented BD is a rare variant that accounts for 1.7% (N=420) to 5.5% (N=951) of all cases of BD.1,2 It is reported to affect men more than women and to be more prevalent in individuals with higher Fitzpatrick skin types.3 Furthermore, exposure to UV radiation, chemicals (eg, arsenic), or human papillomavirus, as well as immunosuppression, are known to be related to pigmented BD.2,4 Clinically, pigmented BD commonly involves nonexposed areas such as the anogenital area, trunk, and extremities, unlike typical BD that involves sun-exposed areas.5 In addition, it most frequently presents as a well-delineated, irregularly pigmented, asymptomatic
plaque and not as a scaly erythematous plaque. Therefore, the clinical diagnosis may be challenging. The differential diagnosis includes malignant melanoma, pigmented extramammary Paget disease, pigmented basal cell carcinoma, seborrheic keratosis, pigmented actinic keratosis, solar lentigo, and melanocytic nevi.
Histopathologically, a varying amount of melanin deposit is noted on hematoxylin and eosin staining, along with features of BD, including disarrayed atypical keratinocytes involving the full epidermis but not the basement membrane, with atypical individual cell keratinization.3,5,6 Pigmented extramammary Paget disease can mimic pigmented BD clinically and pathologically, but Paget cells stain positive for anticytokeratin (CAM 5.2), carcinoembryonic antigen, and mucicarmine, whereas cells in pigmented BD stain negative.7 Moreover, negative staining for human melanoma black, melan-A, and S-100 helps differentiate malignant melanoma from pigmented BD.8
The prognosis of pigmented BD is similar to classic BD and is independent of the presence of melanin pigment.6 Therefore, the treatment options do not differ from those for typical BD and include surgical excision, cryotherapy, laser ablation, topical imiquimod or 5-fluorouracil, curettage, electrosurgery, and photodynamic therapy (PDT).
In our case, the patient and her family did not want surgical removal; therefore, 1 course of fractional laser-assisted PDT and 2 courses of ablative laser-assisted PDT were performed. Unfortunately, the lesion persisted, possibly because it was too large and pigmented. Two months later, ingenol mebutate gel 0.05% was applied (4 courses) after using an ablative laser over 3 consecutive days with a 1-month interval between courses. The lesion resolved without any adverse events.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease [published online January 15, 2010]. J Am Acad Dermatol. 2010;62:597-604.
- Ragi G, Turner MS, Klein LE, et al. Pigmented Bowen’s disease and review of 420 Bowen’s disease lesions. J Dermatol Surg Oncol. 1988;14:765-769.
- Hernandez C, Ivkovic A, Fowler A. Growing plaque on foot. J Fam Pract. 2008;57:603-605.
- Hwang SW, Kim JW, Park SW, et al. Two cases of pigmented Bowen’s disease. Ann Dermatol 2002;14:127-129.
- Wilmer EM, Lee KC, Higgins W 2nd, et al. Hyperpigmented palmar plaque: an unexpected diagnosis of Bowen disease. Dermatol Online J. 2013;19:18573.
- Brinca A, Teixeira V, Gonçalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-884.
- Hilliard NJ, Huang C, Andea A. Pigmented extramammary Paget’s disease of the axilla mimicking melanoma: case report and review of the literature. J Cutan Pathol. 2009;36:995-1000.
- Öztürk Durmaz E, Dog˘ an Ekici I, Ozian F, et al. Pigmented Bowen’s disease of the genitalia masquerading as malignant melanoma. Acta Dermatovenerol Croat. 2015;23:130-133.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease [published online January 15, 2010]. J Am Acad Dermatol. 2010;62:597-604.
- Ragi G, Turner MS, Klein LE, et al. Pigmented Bowen’s disease and review of 420 Bowen’s disease lesions. J Dermatol Surg Oncol. 1988;14:765-769.
- Hernandez C, Ivkovic A, Fowler A. Growing plaque on foot. J Fam Pract. 2008;57:603-605.
- Hwang SW, Kim JW, Park SW, et al. Two cases of pigmented Bowen’s disease. Ann Dermatol 2002;14:127-129.
- Wilmer EM, Lee KC, Higgins W 2nd, et al. Hyperpigmented palmar plaque: an unexpected diagnosis of Bowen disease. Dermatol Online J. 2013;19:18573.
- Brinca A, Teixeira V, Gonçalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-884.
- Hilliard NJ, Huang C, Andea A. Pigmented extramammary Paget’s disease of the axilla mimicking melanoma: case report and review of the literature. J Cutan Pathol. 2009;36:995-1000.
- Öztürk Durmaz E, Dog˘ an Ekici I, Ozian F, et al. Pigmented Bowen’s disease of the genitalia masquerading as malignant melanoma. Acta Dermatovenerol Croat. 2015;23:130-133.
A 56-year-old woman presented with an asymptomatic plaque on the right heel that had grown
steadily over the last year. Pigmented lesions were not appreciated on other sites, and lymph nodes were not enlarged. Her medical history was otherwise normal, except for bilateral hearing loss due to encephalitis at the age of 5 years. None of her family members had similar symptoms. Physical examination revealed a well-defined, irregularly hyperpigmented plaque on the right heel.
Cutaneous Collagenous Vasculopathy
To the Editor:
Cutaneous microangiopathy describes pathology of the small blood vessels within the dermis.
We report a case of CCV in a 41-year-old woman who presented for evaluation of a rash on the bilateral lower extremities of 7 to 8 months’ duration. The eruption had started on the left ankle and spread over several weeks to the bilateral dorsal feet followed by the ankles and shins. The patient noted associated swelling and a pressure like dysesthesia of the lower legs. She was otherwise in good health, though she had started an oral contraceptive 1 year prior for heavy menstrual bleeding. A review of systems was negative for deep vein thrombosis, pulmonary embolus, and other thromboembolic phenomena, and the patient had no history of hepatic or renal dysfunction, cancer, or heart disease. Her family history was negative for clotting disorders or bleeding diatheses.
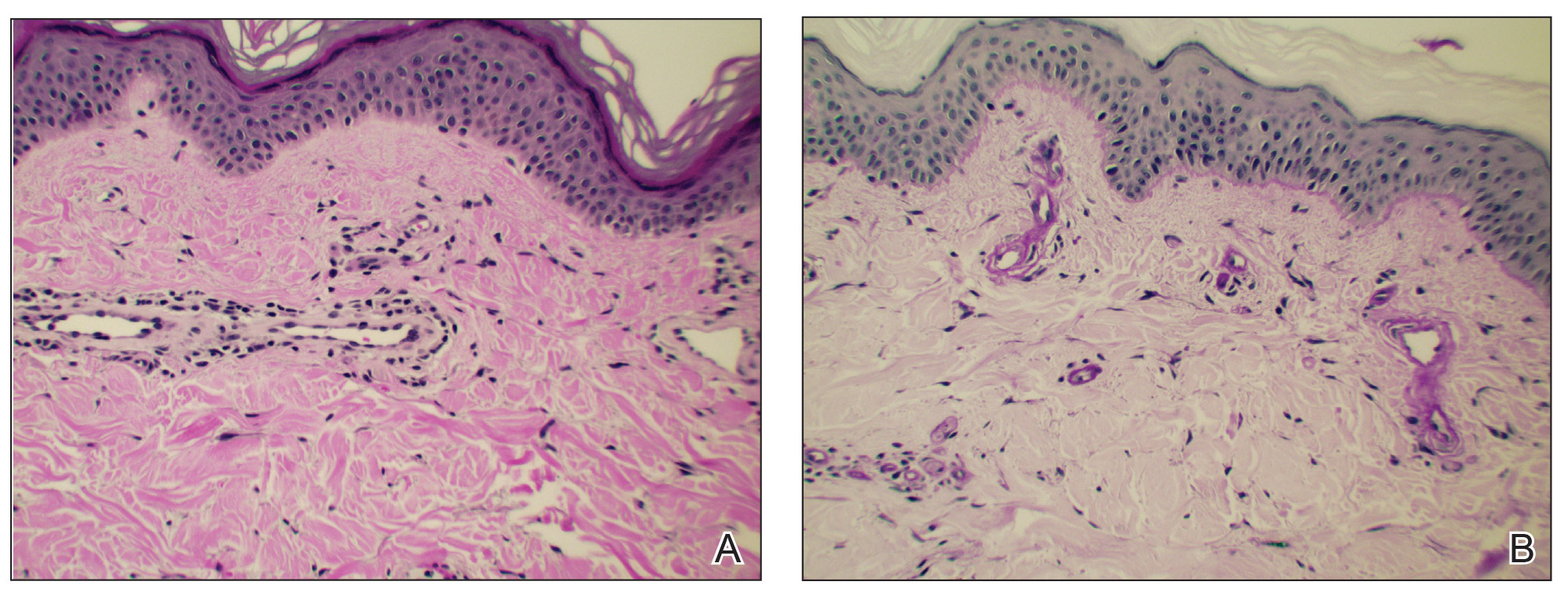
On physical examination, telangiectatic matting was present on the bilateral ankles and dorsal feet with an associated blanchable erythema (Figure 1). The matting extended into a fine, mottled, pretibial telangiectasia associated with Schamberg purpura. She had no pitting edema, and both dorsalis pedis and posterior popliteal pulses were intact and symmetric bilaterally. No popliteal lymphadenopathy or palpable cords were present.
Two punch biopsies taken from the erythematous telangiectatic area on the left foot and metatarsal region demonstrated an unremarkable epidermis without interface change, thickening of the epidermal basement membrane, or single-cell dyskeratosis. There was mild dilatation of blood vessels within the superficial dermis with mild perivascular lymphocytic inflammation and rare extravasated erythrocytes. Leukocytoclastic debris, fibrinoid necrosis of vessel walls, and endothelial cell necrosis were not seen. As is classic in CCV, the vessel walls appeared thickened by eosinophilic hyaline material, which was periodic acid–Schiff positive and diastase resistant (Figure 2). Sclerotic thickening of collagen bundles or absence of periadnexal adipose tissue was not seen. CD34 immunohistochemical staining demonstrated normal retained CD34 interstitial dermal positivity, which excluded morphea. Additionally, direct immunofluorescence testing was negative for IgG, IgA, IgM, C3, fibrin, and C1q. Nodular reduplication of vessels or other changes of stasis were not seen. Fibrin thrombi or neoplastic cells were not identified. The clinical and histopathologic findings were suggestive of CCV.
Prior case reports of CCV have described a similar clinical manifestation with blanching macules that occur symmetrically on the lower extremities and spread cephalically.1-6 A distinction from hereditary hemorrhagic telangiectasia is the noninvolvement of mucous membranes and nails. The etiology of this rare microangiopathy has not been elucidated, though disease concurrence with local trauma, stressful events such as childbirth, and diabetes mellitus has been documented.6 As the body of literature continues to grow, more research regarding the etiology, mechanism, prognosis, and treatment options will enhance our understanding of CCV.
- Bondier L, Tardieu M, Leveque P, et al. Cutaneous collagenous vasculopathy: report of two cases presenting as disseminated telangiectasias and review of the literature. Am J Dermatopathol. 2017;39:682-688.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and ultrastructural study. J Cutan Pathol. 2000;27:40-48.
- Lloyd BM, Pruden SJ, Lind AC, et al. Cutaneous collagenous vasculopathy: report of the first pediatric case. Pediatr Dermatol. 2011;28:598-599.
- Salama S, Chorneyko K, Belovic B. Cutaneous collagenous vasculopathy associated with intravascular occlusive fibrin thrombi. J Cutan Pathol. 2014;41:386-393.
- Perez A, Wain ME, Robson A, et al. Cutaneous collagenous vasculopathy with generalized telangiectasia in two female patients. J Am Acad Dermatol. 2010;63:882-885.
- Burdick LM, Losher S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
To the Editor:
Cutaneous microangiopathy describes pathology of the small blood vessels within the dermis.
We report a case of CCV in a 41-year-old woman who presented for evaluation of a rash on the bilateral lower extremities of 7 to 8 months’ duration. The eruption had started on the left ankle and spread over several weeks to the bilateral dorsal feet followed by the ankles and shins. The patient noted associated swelling and a pressure like dysesthesia of the lower legs. She was otherwise in good health, though she had started an oral contraceptive 1 year prior for heavy menstrual bleeding. A review of systems was negative for deep vein thrombosis, pulmonary embolus, and other thromboembolic phenomena, and the patient had no history of hepatic or renal dysfunction, cancer, or heart disease. Her family history was negative for clotting disorders or bleeding diatheses.
On physical examination, telangiectatic matting was present on the bilateral ankles and dorsal feet with an associated blanchable erythema (Figure 1). The matting extended into a fine, mottled, pretibial telangiectasia associated with Schamberg purpura. She had no pitting edema, and both dorsalis pedis and posterior popliteal pulses were intact and symmetric bilaterally. No popliteal lymphadenopathy or palpable cords were present.
Two punch biopsies taken from the erythematous telangiectatic area on the left foot and metatarsal region demonstrated an unremarkable epidermis without interface change, thickening of the epidermal basement membrane, or single-cell dyskeratosis. There was mild dilatation of blood vessels within the superficial dermis with mild perivascular lymphocytic inflammation and rare extravasated erythrocytes. Leukocytoclastic debris, fibrinoid necrosis of vessel walls, and endothelial cell necrosis were not seen. As is classic in CCV, the vessel walls appeared thickened by eosinophilic hyaline material, which was periodic acid–Schiff positive and diastase resistant (Figure 2). Sclerotic thickening of collagen bundles or absence of periadnexal adipose tissue was not seen. CD34 immunohistochemical staining demonstrated normal retained CD34 interstitial dermal positivity, which excluded morphea. Additionally, direct immunofluorescence testing was negative for IgG, IgA, IgM, C3, fibrin, and C1q. Nodular reduplication of vessels or other changes of stasis were not seen. Fibrin thrombi or neoplastic cells were not identified. The clinical and histopathologic findings were suggestive of CCV.
Prior case reports of CCV have described a similar clinical manifestation with blanching macules that occur symmetrically on the lower extremities and spread cephalically.1-6 A distinction from hereditary hemorrhagic telangiectasia is the noninvolvement of mucous membranes and nails. The etiology of this rare microangiopathy has not been elucidated, though disease concurrence with local trauma, stressful events such as childbirth, and diabetes mellitus has been documented.6 As the body of literature continues to grow, more research regarding the etiology, mechanism, prognosis, and treatment options will enhance our understanding of CCV.
To the Editor:
Cutaneous microangiopathy describes pathology of the small blood vessels within the dermis.
We report a case of CCV in a 41-year-old woman who presented for evaluation of a rash on the bilateral lower extremities of 7 to 8 months’ duration. The eruption had started on the left ankle and spread over several weeks to the bilateral dorsal feet followed by the ankles and shins. The patient noted associated swelling and a pressure like dysesthesia of the lower legs. She was otherwise in good health, though she had started an oral contraceptive 1 year prior for heavy menstrual bleeding. A review of systems was negative for deep vein thrombosis, pulmonary embolus, and other thromboembolic phenomena, and the patient had no history of hepatic or renal dysfunction, cancer, or heart disease. Her family history was negative for clotting disorders or bleeding diatheses.
On physical examination, telangiectatic matting was present on the bilateral ankles and dorsal feet with an associated blanchable erythema (Figure 1). The matting extended into a fine, mottled, pretibial telangiectasia associated with Schamberg purpura. She had no pitting edema, and both dorsalis pedis and posterior popliteal pulses were intact and symmetric bilaterally. No popliteal lymphadenopathy or palpable cords were present.
Two punch biopsies taken from the erythematous telangiectatic area on the left foot and metatarsal region demonstrated an unremarkable epidermis without interface change, thickening of the epidermal basement membrane, or single-cell dyskeratosis. There was mild dilatation of blood vessels within the superficial dermis with mild perivascular lymphocytic inflammation and rare extravasated erythrocytes. Leukocytoclastic debris, fibrinoid necrosis of vessel walls, and endothelial cell necrosis were not seen. As is classic in CCV, the vessel walls appeared thickened by eosinophilic hyaline material, which was periodic acid–Schiff positive and diastase resistant (Figure 2). Sclerotic thickening of collagen bundles or absence of periadnexal adipose tissue was not seen. CD34 immunohistochemical staining demonstrated normal retained CD34 interstitial dermal positivity, which excluded morphea. Additionally, direct immunofluorescence testing was negative for IgG, IgA, IgM, C3, fibrin, and C1q. Nodular reduplication of vessels or other changes of stasis were not seen. Fibrin thrombi or neoplastic cells were not identified. The clinical and histopathologic findings were suggestive of CCV.
Prior case reports of CCV have described a similar clinical manifestation with blanching macules that occur symmetrically on the lower extremities and spread cephalically.1-6 A distinction from hereditary hemorrhagic telangiectasia is the noninvolvement of mucous membranes and nails. The etiology of this rare microangiopathy has not been elucidated, though disease concurrence with local trauma, stressful events such as childbirth, and diabetes mellitus has been documented.6 As the body of literature continues to grow, more research regarding the etiology, mechanism, prognosis, and treatment options will enhance our understanding of CCV.
- Bondier L, Tardieu M, Leveque P, et al. Cutaneous collagenous vasculopathy: report of two cases presenting as disseminated telangiectasias and review of the literature. Am J Dermatopathol. 2017;39:682-688.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and ultrastructural study. J Cutan Pathol. 2000;27:40-48.
- Lloyd BM, Pruden SJ, Lind AC, et al. Cutaneous collagenous vasculopathy: report of the first pediatric case. Pediatr Dermatol. 2011;28:598-599.
- Salama S, Chorneyko K, Belovic B. Cutaneous collagenous vasculopathy associated with intravascular occlusive fibrin thrombi. J Cutan Pathol. 2014;41:386-393.
- Perez A, Wain ME, Robson A, et al. Cutaneous collagenous vasculopathy with generalized telangiectasia in two female patients. J Am Acad Dermatol. 2010;63:882-885.
- Burdick LM, Losher S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
- Bondier L, Tardieu M, Leveque P, et al. Cutaneous collagenous vasculopathy: report of two cases presenting as disseminated telangiectasias and review of the literature. Am J Dermatopathol. 2017;39:682-688.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and ultrastructural study. J Cutan Pathol. 2000;27:40-48.
- Lloyd BM, Pruden SJ, Lind AC, et al. Cutaneous collagenous vasculopathy: report of the first pediatric case. Pediatr Dermatol. 2011;28:598-599.
- Salama S, Chorneyko K, Belovic B. Cutaneous collagenous vasculopathy associated with intravascular occlusive fibrin thrombi. J Cutan Pathol. 2014;41:386-393.
- Perez A, Wain ME, Robson A, et al. Cutaneous collagenous vasculopathy with generalized telangiectasia in two female patients. J Am Acad Dermatol. 2010;63:882-885.
- Burdick LM, Losher S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
Practice Points
- In cutaneous collagenous vasculopathy (CCV), skin biopsy may demonstrate eosinophilic hyaline thickening of superficial dermal blood vessels with mild perivascular lymphocytic inflammation and rare extravasated erythrocytes.
- Lack of mucous membrane and nail involvement differentiates CCV from hereditary hemorrhagic telangiectasia.
Elephantiasis Nostras Verrucosa Secondary to Scleroderma
To the Editor:
Elephantiasis nostras verrucosa (ENV) is a skin disorder caused by marked underlying lymphedema that leads to hyperkeratosis, papillomatosis, and verrucous growths on the epidermis.1 The pathophysiology of ENV relates to noninfectious lymphatic obstruction and lymphatic fibrosis secondary to venous stasis, malignancy, radiation therapy, or trauma.2 We present an unusual case of lymphedema and subsequent ENV limited to the arms and hands in a patient with scleroderma, an autoimmune fibrosing disorder.
A 54-year-old woman with a 5-year history of scleroderma presented to our dermatology clinic for treatment of progressive skin changes including pruritus, tightness, finger ulcerations, and pus exuding from papules on the dorsal arms and hands. She had been experiencing several systemic symptoms including dysphagia and lung involvement, necessitating oxygen therapy and a continuous positive airway pressure device for pulmonary arterial hypertension. A computed tomography scan of the lungs demonstrated an increase in ground-glass infiltrates in the right lower lobe and an air-fluid level in the esophagus. At the time of presentation, she was being treated with bosentan and sildenafil for pulmonary arterial hypertension, in addition to prednisone, venlafaxine, lansoprazole, metoclopramide, levothyroxine, temazepam, aspirin, and oxycodone. In the 2 years prior to presentation, she had been treated with intravenous cyclophosphamide once monthly for 6 months, adalimumab for 1 year, and 1 session of photodynamic therapy to the arms, all without benefit.
Physical examination showed cutaneous signs of scleroderma including marked sclerosis of the skin on the face, hands, V of the neck, proximal arms, and mid and proximal thighs. Excoriated papules with overlying crusting and pustulation were superimposed on the sclerotic skin of the arms (Figure 1).
A superinfection was diagnosed and treated with cephalexin 500 mg 4 times daily for 2 weeks; thereafter, mupirocin cream twice daily was used as needed. She was prescribed fexofenadine 180 mg twice daily and doxepin 20 mg at bedtime for pruritus.
At 3-week follow-up, a trial of narrowband UVB therapy was recommended for control of pruritus. Two weeks later, a modified wet-wrap regimen using clobetasol ointment 0.5% twice daily covered with wet gauze followed by a self-adherent dressing was initiated only on the right arm for comparison purposes. This treatment was not successful. A biopsy taken from the left arm showed lymphedema with perivascular fibroplasia and epidermal hyperplasia consistent with ENV (Figure 2).
Two months after her initial presentation, we instituted treatment with tazarotene gel 0.1% twice daily to the arms as well as a water-based topical emulsion to the finger ulcerations and a healing ointment to the hands. A month later, the patient reported no benefit with tazarotene. She desired more flexibility in her arms and hands; therefore, after a discussion with her rheumatologist, biweekly psoralen plus UVA (PUVA) therapy was initiated. Five months after presentation, methotrexate (MTX) 15 mg once weekly with folic acid 1 mg once daily was added. The PUVA therapy and MTX were stopped 3 months later due to lack of treatment benefit.
The patient was referred to vascular medicine for possible compression therapy. It was determined that her vasculature was intact, but compression therapy was contraindicated due to underlying systemic sclerosis. She was subsequently prescribed mycophenolate mofetil 1000 mg twice daily by her rheumatologist. The options of serial excisions or laser resurfacing were presented, but she declined.
Elephantiasis nostras verrucosa is differentiated from elephantiasis tropica, which is caused by a filarial infection of the lymphatic system. The chronic obstructive lymphedema characteristic of ENV can present as a result of various primary or secondary etiologies including trauma, malignancy, venous stasis, inflammation, or infection.3 In systemic sclerosis, extravascular fibrosis theoretically can lead to lymphatic obstruction and subsequent lymphatic stasis. In turn, the pathophysiology of dermal and subcutaneous fibrosis likely reflects autoantibodies (eg, anticardiolipin antibodies) that can damage lymphatic and nonlymphatic vessels.4,5
As the underlying mechanism of ENV, fibrosis of lymphatic vessels in systemic sclerosis is not well documented. Characteristic features of systemic sclerosis include extensive fibrosis, fibroproliferative vasculopathy, and inflammation, which are all possible mechanisms for the internal lymphatic obstruction resulting in the skin changes observed in ENV.6 It seemed unusual that the fibrotic changes of lymphatic vessels in our patient were extensive enough to cause ENV of the upper extremities; lower extremity involvement is the more common presentation because of the greater likelihood of lymphedema manifesting in the legs and feet. Lower extremity ENV has been reported in association with scleroderma.7,8
Regarding therapeutic options, Boyd et al9 reported a good response in a patient with ENV of the abdomen who was treated with topical tazarotene. Additionally, PUVA and MTX have been reported to be beneficial for the progressive skin changes of systemic sclerosis.10 Mycophenolate mofetil has been used in patients who fail MTX therapy because of its antifibrotic properties without the side-effect profiles of other immunosuppressives, such as imatinib.10,11 In our patient, skin lesions persisted following these varied approaches, and compression therapy was not advised due to the underlying sclerosis.
Because options for medical treatment of severe ENV are limited, surgical debridement of the affected limb often remains the only viable option in advanced cases.12 A PubMed search of articles indexed for MEDLINE using the terms elephantiasis (MeSH terms) or elephantiasis (all fields) and scleroderma, systemic (MeSH terms) or scleroderma (all fields) and systemic (all fields) or systemic scleroderma (all fields) or scleroderma (all fields) or scleroderma, localized (MeSH terms) or scleroderma (all fields) and localized (all fields) or localized scleroderma (all fields) yielded only 1 other case report of lower extremity ENV in a patient with systemic sclerosis who ultimately required bilateral leg amputation.8 When possible, avoiding lymphostasis through compression and control of any underlying infections is important in the treatment and prevention of ENV.3
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
- Schissel DJ, Hivnor C, Elston DM. Elephantiasis nostras verrucosa. Cutis. 1998;62:77-80.
- Duckworth A, Husain J, DeHeer P. Elephantiasis nostras verrucosa or ‘mossy foot lesions’ in lymphedema praecox. J Am Podiatr Med Assoc. 2008;98:66-69.
- Assous N, Allanore Y, Batteaux F, et al. Prevalence of antiphospholipid antibodies in systemic sclerosis and association with primitive pulmonary arterial hypertension and endothelial injury. Clin Exp Rheumatol. 2005;23:199-204.
- Derrett-Smith EC, Dooley A, Gilbane AJ, et al. Endothelial injury in a transforming growth-factor-dependent mouse model of scleroderma induces pulmonary arterial hypertension. Arthritis Rheum. 2013;65:2928-2939.
- Pattanaik M, Brown M, Postlethwaite A. Vascular involvement in systemic sclerosis (scleroderma). J Inflamm Res. 2011;4:105-125.
- Kerchner K, Fleischer A, Yosipovitch G. Lower extremity lymphedema update: pathophysiology, diagnosis and treatment guidelines. J Am Acad Dermatol. 2008;59:324-331.
- Chatterjee S, Karai L. Elephantiasis nostras verrucosa in a patient with systemic sclerosis. Clin Exp Dermatol. 2009;34:e696-e698.
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004;3:446-448.
- Fett, N. Scleroderma: nomenclature, etiology, pathogenesis, prognosis, and treatments: facts and controversies. Clin Dermatol. 2013;31:432-437.
- Moinzadeh P, Krieg T, Hunzelmann N. Imatinib treatment of generalized localized scleroderma (morphea). J Am Acad Dermatol. 2010;63:e102-e104.
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941.
To the Editor:
Elephantiasis nostras verrucosa (ENV) is a skin disorder caused by marked underlying lymphedema that leads to hyperkeratosis, papillomatosis, and verrucous growths on the epidermis.1 The pathophysiology of ENV relates to noninfectious lymphatic obstruction and lymphatic fibrosis secondary to venous stasis, malignancy, radiation therapy, or trauma.2 We present an unusual case of lymphedema and subsequent ENV limited to the arms and hands in a patient with scleroderma, an autoimmune fibrosing disorder.
A 54-year-old woman with a 5-year history of scleroderma presented to our dermatology clinic for treatment of progressive skin changes including pruritus, tightness, finger ulcerations, and pus exuding from papules on the dorsal arms and hands. She had been experiencing several systemic symptoms including dysphagia and lung involvement, necessitating oxygen therapy and a continuous positive airway pressure device for pulmonary arterial hypertension. A computed tomography scan of the lungs demonstrated an increase in ground-glass infiltrates in the right lower lobe and an air-fluid level in the esophagus. At the time of presentation, she was being treated with bosentan and sildenafil for pulmonary arterial hypertension, in addition to prednisone, venlafaxine, lansoprazole, metoclopramide, levothyroxine, temazepam, aspirin, and oxycodone. In the 2 years prior to presentation, she had been treated with intravenous cyclophosphamide once monthly for 6 months, adalimumab for 1 year, and 1 session of photodynamic therapy to the arms, all without benefit.
Physical examination showed cutaneous signs of scleroderma including marked sclerosis of the skin on the face, hands, V of the neck, proximal arms, and mid and proximal thighs. Excoriated papules with overlying crusting and pustulation were superimposed on the sclerotic skin of the arms (Figure 1).
A superinfection was diagnosed and treated with cephalexin 500 mg 4 times daily for 2 weeks; thereafter, mupirocin cream twice daily was used as needed. She was prescribed fexofenadine 180 mg twice daily and doxepin 20 mg at bedtime for pruritus.
At 3-week follow-up, a trial of narrowband UVB therapy was recommended for control of pruritus. Two weeks later, a modified wet-wrap regimen using clobetasol ointment 0.5% twice daily covered with wet gauze followed by a self-adherent dressing was initiated only on the right arm for comparison purposes. This treatment was not successful. A biopsy taken from the left arm showed lymphedema with perivascular fibroplasia and epidermal hyperplasia consistent with ENV (Figure 2).
Two months after her initial presentation, we instituted treatment with tazarotene gel 0.1% twice daily to the arms as well as a water-based topical emulsion to the finger ulcerations and a healing ointment to the hands. A month later, the patient reported no benefit with tazarotene. She desired more flexibility in her arms and hands; therefore, after a discussion with her rheumatologist, biweekly psoralen plus UVA (PUVA) therapy was initiated. Five months after presentation, methotrexate (MTX) 15 mg once weekly with folic acid 1 mg once daily was added. The PUVA therapy and MTX were stopped 3 months later due to lack of treatment benefit.
The patient was referred to vascular medicine for possible compression therapy. It was determined that her vasculature was intact, but compression therapy was contraindicated due to underlying systemic sclerosis. She was subsequently prescribed mycophenolate mofetil 1000 mg twice daily by her rheumatologist. The options of serial excisions or laser resurfacing were presented, but she declined.
Elephantiasis nostras verrucosa is differentiated from elephantiasis tropica, which is caused by a filarial infection of the lymphatic system. The chronic obstructive lymphedema characteristic of ENV can present as a result of various primary or secondary etiologies including trauma, malignancy, venous stasis, inflammation, or infection.3 In systemic sclerosis, extravascular fibrosis theoretically can lead to lymphatic obstruction and subsequent lymphatic stasis. In turn, the pathophysiology of dermal and subcutaneous fibrosis likely reflects autoantibodies (eg, anticardiolipin antibodies) that can damage lymphatic and nonlymphatic vessels.4,5
As the underlying mechanism of ENV, fibrosis of lymphatic vessels in systemic sclerosis is not well documented. Characteristic features of systemic sclerosis include extensive fibrosis, fibroproliferative vasculopathy, and inflammation, which are all possible mechanisms for the internal lymphatic obstruction resulting in the skin changes observed in ENV.6 It seemed unusual that the fibrotic changes of lymphatic vessels in our patient were extensive enough to cause ENV of the upper extremities; lower extremity involvement is the more common presentation because of the greater likelihood of lymphedema manifesting in the legs and feet. Lower extremity ENV has been reported in association with scleroderma.7,8
Regarding therapeutic options, Boyd et al9 reported a good response in a patient with ENV of the abdomen who was treated with topical tazarotene. Additionally, PUVA and MTX have been reported to be beneficial for the progressive skin changes of systemic sclerosis.10 Mycophenolate mofetil has been used in patients who fail MTX therapy because of its antifibrotic properties without the side-effect profiles of other immunosuppressives, such as imatinib.10,11 In our patient, skin lesions persisted following these varied approaches, and compression therapy was not advised due to the underlying sclerosis.
Because options for medical treatment of severe ENV are limited, surgical debridement of the affected limb often remains the only viable option in advanced cases.12 A PubMed search of articles indexed for MEDLINE using the terms elephantiasis (MeSH terms) or elephantiasis (all fields) and scleroderma, systemic (MeSH terms) or scleroderma (all fields) and systemic (all fields) or systemic scleroderma (all fields) or scleroderma (all fields) or scleroderma, localized (MeSH terms) or scleroderma (all fields) and localized (all fields) or localized scleroderma (all fields) yielded only 1 other case report of lower extremity ENV in a patient with systemic sclerosis who ultimately required bilateral leg amputation.8 When possible, avoiding lymphostasis through compression and control of any underlying infections is important in the treatment and prevention of ENV.3
To the Editor:
Elephantiasis nostras verrucosa (ENV) is a skin disorder caused by marked underlying lymphedema that leads to hyperkeratosis, papillomatosis, and verrucous growths on the epidermis.1 The pathophysiology of ENV relates to noninfectious lymphatic obstruction and lymphatic fibrosis secondary to venous stasis, malignancy, radiation therapy, or trauma.2 We present an unusual case of lymphedema and subsequent ENV limited to the arms and hands in a patient with scleroderma, an autoimmune fibrosing disorder.
A 54-year-old woman with a 5-year history of scleroderma presented to our dermatology clinic for treatment of progressive skin changes including pruritus, tightness, finger ulcerations, and pus exuding from papules on the dorsal arms and hands. She had been experiencing several systemic symptoms including dysphagia and lung involvement, necessitating oxygen therapy and a continuous positive airway pressure device for pulmonary arterial hypertension. A computed tomography scan of the lungs demonstrated an increase in ground-glass infiltrates in the right lower lobe and an air-fluid level in the esophagus. At the time of presentation, she was being treated with bosentan and sildenafil for pulmonary arterial hypertension, in addition to prednisone, venlafaxine, lansoprazole, metoclopramide, levothyroxine, temazepam, aspirin, and oxycodone. In the 2 years prior to presentation, she had been treated with intravenous cyclophosphamide once monthly for 6 months, adalimumab for 1 year, and 1 session of photodynamic therapy to the arms, all without benefit.
Physical examination showed cutaneous signs of scleroderma including marked sclerosis of the skin on the face, hands, V of the neck, proximal arms, and mid and proximal thighs. Excoriated papules with overlying crusting and pustulation were superimposed on the sclerotic skin of the arms (Figure 1).
A superinfection was diagnosed and treated with cephalexin 500 mg 4 times daily for 2 weeks; thereafter, mupirocin cream twice daily was used as needed. She was prescribed fexofenadine 180 mg twice daily and doxepin 20 mg at bedtime for pruritus.
At 3-week follow-up, a trial of narrowband UVB therapy was recommended for control of pruritus. Two weeks later, a modified wet-wrap regimen using clobetasol ointment 0.5% twice daily covered with wet gauze followed by a self-adherent dressing was initiated only on the right arm for comparison purposes. This treatment was not successful. A biopsy taken from the left arm showed lymphedema with perivascular fibroplasia and epidermal hyperplasia consistent with ENV (Figure 2).
Two months after her initial presentation, we instituted treatment with tazarotene gel 0.1% twice daily to the arms as well as a water-based topical emulsion to the finger ulcerations and a healing ointment to the hands. A month later, the patient reported no benefit with tazarotene. She desired more flexibility in her arms and hands; therefore, after a discussion with her rheumatologist, biweekly psoralen plus UVA (PUVA) therapy was initiated. Five months after presentation, methotrexate (MTX) 15 mg once weekly with folic acid 1 mg once daily was added. The PUVA therapy and MTX were stopped 3 months later due to lack of treatment benefit.
The patient was referred to vascular medicine for possible compression therapy. It was determined that her vasculature was intact, but compression therapy was contraindicated due to underlying systemic sclerosis. She was subsequently prescribed mycophenolate mofetil 1000 mg twice daily by her rheumatologist. The options of serial excisions or laser resurfacing were presented, but she declined.
Elephantiasis nostras verrucosa is differentiated from elephantiasis tropica, which is caused by a filarial infection of the lymphatic system. The chronic obstructive lymphedema characteristic of ENV can present as a result of various primary or secondary etiologies including trauma, malignancy, venous stasis, inflammation, or infection.3 In systemic sclerosis, extravascular fibrosis theoretically can lead to lymphatic obstruction and subsequent lymphatic stasis. In turn, the pathophysiology of dermal and subcutaneous fibrosis likely reflects autoantibodies (eg, anticardiolipin antibodies) that can damage lymphatic and nonlymphatic vessels.4,5
As the underlying mechanism of ENV, fibrosis of lymphatic vessels in systemic sclerosis is not well documented. Characteristic features of systemic sclerosis include extensive fibrosis, fibroproliferative vasculopathy, and inflammation, which are all possible mechanisms for the internal lymphatic obstruction resulting in the skin changes observed in ENV.6 It seemed unusual that the fibrotic changes of lymphatic vessels in our patient were extensive enough to cause ENV of the upper extremities; lower extremity involvement is the more common presentation because of the greater likelihood of lymphedema manifesting in the legs and feet. Lower extremity ENV has been reported in association with scleroderma.7,8
Regarding therapeutic options, Boyd et al9 reported a good response in a patient with ENV of the abdomen who was treated with topical tazarotene. Additionally, PUVA and MTX have been reported to be beneficial for the progressive skin changes of systemic sclerosis.10 Mycophenolate mofetil has been used in patients who fail MTX therapy because of its antifibrotic properties without the side-effect profiles of other immunosuppressives, such as imatinib.10,11 In our patient, skin lesions persisted following these varied approaches, and compression therapy was not advised due to the underlying sclerosis.
Because options for medical treatment of severe ENV are limited, surgical debridement of the affected limb often remains the only viable option in advanced cases.12 A PubMed search of articles indexed for MEDLINE using the terms elephantiasis (MeSH terms) or elephantiasis (all fields) and scleroderma, systemic (MeSH terms) or scleroderma (all fields) and systemic (all fields) or systemic scleroderma (all fields) or scleroderma (all fields) or scleroderma, localized (MeSH terms) or scleroderma (all fields) and localized (all fields) or localized scleroderma (all fields) yielded only 1 other case report of lower extremity ENV in a patient with systemic sclerosis who ultimately required bilateral leg amputation.8 When possible, avoiding lymphostasis through compression and control of any underlying infections is important in the treatment and prevention of ENV.3
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
- Schissel DJ, Hivnor C, Elston DM. Elephantiasis nostras verrucosa. Cutis. 1998;62:77-80.
- Duckworth A, Husain J, DeHeer P. Elephantiasis nostras verrucosa or ‘mossy foot lesions’ in lymphedema praecox. J Am Podiatr Med Assoc. 2008;98:66-69.
- Assous N, Allanore Y, Batteaux F, et al. Prevalence of antiphospholipid antibodies in systemic sclerosis and association with primitive pulmonary arterial hypertension and endothelial injury. Clin Exp Rheumatol. 2005;23:199-204.
- Derrett-Smith EC, Dooley A, Gilbane AJ, et al. Endothelial injury in a transforming growth-factor-dependent mouse model of scleroderma induces pulmonary arterial hypertension. Arthritis Rheum. 2013;65:2928-2939.
- Pattanaik M, Brown M, Postlethwaite A. Vascular involvement in systemic sclerosis (scleroderma). J Inflamm Res. 2011;4:105-125.
- Kerchner K, Fleischer A, Yosipovitch G. Lower extremity lymphedema update: pathophysiology, diagnosis and treatment guidelines. J Am Acad Dermatol. 2008;59:324-331.
- Chatterjee S, Karai L. Elephantiasis nostras verrucosa in a patient with systemic sclerosis. Clin Exp Dermatol. 2009;34:e696-e698.
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004;3:446-448.
- Fett, N. Scleroderma: nomenclature, etiology, pathogenesis, prognosis, and treatments: facts and controversies. Clin Dermatol. 2013;31:432-437.
- Moinzadeh P, Krieg T, Hunzelmann N. Imatinib treatment of generalized localized scleroderma (morphea). J Am Acad Dermatol. 2010;63:e102-e104.
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941.
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
- Schissel DJ, Hivnor C, Elston DM. Elephantiasis nostras verrucosa. Cutis. 1998;62:77-80.
- Duckworth A, Husain J, DeHeer P. Elephantiasis nostras verrucosa or ‘mossy foot lesions’ in lymphedema praecox. J Am Podiatr Med Assoc. 2008;98:66-69.
- Assous N, Allanore Y, Batteaux F, et al. Prevalence of antiphospholipid antibodies in systemic sclerosis and association with primitive pulmonary arterial hypertension and endothelial injury. Clin Exp Rheumatol. 2005;23:199-204.
- Derrett-Smith EC, Dooley A, Gilbane AJ, et al. Endothelial injury in a transforming growth-factor-dependent mouse model of scleroderma induces pulmonary arterial hypertension. Arthritis Rheum. 2013;65:2928-2939.
- Pattanaik M, Brown M, Postlethwaite A. Vascular involvement in systemic sclerosis (scleroderma). J Inflamm Res. 2011;4:105-125.
- Kerchner K, Fleischer A, Yosipovitch G. Lower extremity lymphedema update: pathophysiology, diagnosis and treatment guidelines. J Am Acad Dermatol. 2008;59:324-331.
- Chatterjee S, Karai L. Elephantiasis nostras verrucosa in a patient with systemic sclerosis. Clin Exp Dermatol. 2009;34:e696-e698.
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004;3:446-448.
- Fett, N. Scleroderma: nomenclature, etiology, pathogenesis, prognosis, and treatments: facts and controversies. Clin Dermatol. 2013;31:432-437.
- Moinzadeh P, Krieg T, Hunzelmann N. Imatinib treatment of generalized localized scleroderma (morphea). J Am Acad Dermatol. 2010;63:e102-e104.
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941.
Practice Points
- Scleroderma rarely may lead to elephantiasis nostras verrucosa (ENV) of the upper extremities.
- Avoiding lymphostasis through compression and control of concomitant skin and soft tissue infections is important in the treatment and prevention of ENV.
Neurofibromatosis Type 1 in the Setting of Systemic Lupus Erythematosus
To the Editor:
Patients with concurrent neurofibromatosis type 1 (NF-1) and systemic lupus erythematosus (SLE) rarely have been reported in the literature. Neurofibromatosis type 1 is one of the most common genetic disorders, with a worldwide birth incidence of 1 in 2500 individuals and prevalence of 1 in 4000 individuals.1 The incidence and prevalence of SLE varies widely depending on race and geographic location. Estimated incidence rates for SLE range from 1 to 25 per 100,000 individuals annually in North America, South America, Europe, and Asia.2,3 The reported worldwide prevalence is 20 to 150 cases per 100,000 individuals annually.2,4,5
Given the high prevalence of both conditions, the association between SLE and NF-1 likely is underrecognized; therefore, identifying more patients with concurrent SLE and NF-1 and describing the interplay between the 2 conditions may have important therapeutic implications. We present the case of a middle-aged woman with a history of SLE who had cutaneous lesions characteristic of NF-1 to further the understanding of these concurrent conditions.
A middle-aged woman presented to our academic dermatology clinic for evaluation and removal of dark spots that had been present diffusely on the trunk and extremities since birth. She reported a history of SLE with lupus nephritis, hypertension, and a nodular goiter following a partial thyroidectomy. She noted that she did not seek treatment for the skin findings sooner because she was more concerned about her other medical conditions; however, because she felt these conditions were now stable, she decided to seek treatment for the “rash.” Physical examination revealed hundreds of café au lait macules and numerous neurofibromas diffusely distributed on the trunk and extremities (Figure 1) as well as bilateral axillary freckling. A clinical diagnosis of NF-1 was made.
When questioned, the patient reported that she may have been diagnosed with NF-1 in the past by another physician, but she did not recall it specifically. The patient was advised that there were no treatments for the café au lait macules. We notified her other physicians of the NF-1 diagnosis so she could be monitored for systemic conditions related to NF-1, including optic gliomas, pheochromocytoma, renal artery stenosis, and internal neurofibromas. We also referred the patient for genetic counseling; of note, the patient reported she had 4 children without any evidence of similar skin lesions or chronic health problems.
A PubMed search of articles indexed for MEDLINE using the terms systemic lupus and neurofibromatosis yielded 8 cases of patients having both SLE and NF-1 (including our case).6-11 Our patient reported having multiple lesions since birth, decades before the onset and diagnosis of SLE. In 3 other cases, patients were diagnosed with SLE and then presented with neurofibromas, leading to NF-1 diagnosis.In the discussion of those 3 cases, it was proposed that immune system alterations caused by SLE leading to viral illness may have predisposed the patients to the development of tumors and other collagen diseases, or it could be coincidental.6,7 In another case, a patient with NF-1 developed SLE, which was thought to be coincidental.8 Akyuz et al9 described the case of a pediatric patient with NF-1 who subsequently was diagnosed with SLE. The authors suggested that the lack of neurofibromin contributed to the development of SLE, an autoimmune condition. Under normal circumstances, neurofibromin acts as a guanosine triphosphatase–activating protein for RAS in T cells.10 CD8+ T-cell function also is impaired in patients with SLE.9 Additionally, it has been reported that anti–double-stranded DNA antibodies and immune complexes were present in NF-1 patients, even though there were low titers.12 Thus, the authors proposed that the lack of neurofibromin led to dysregulation of the RAS pathway and impairment of T cells, creating an immune milieu that predisposed the patient to development of SLE. Our case gives additional credence to this theory, as our patient had a similar clinical course: the café au lait macules were present since birth and the symptoms of SLE surfaced much later in her late 20s and 30s. Another case by Makino and Tampo10 described a patient with a history of SLE who was later diagnosed with NF-1 based on choroidal findings highly specific for NF-1 but did not have other classic findings of NF-1. The authors mentioned that there might be a potential relationship between these two disorders but did not speculate any theory in particular for their case.10
The interplay between an autoimmune condition such as SLE and NF-1, a condition traditionally thought to be due to a genetic mutation, may have greater clinical and therapeutic implications beyond just these two disorders. Although it is well established that RAS pathway disruption causes NF-1, it has been uncovered that dysfunction in the RAS pathway also can contribute to melanoma oncogenesis.13,14 These insights have led to the development of and approval of targeted drugs designed to inhibit the RAS pathway (eg, vemurafenib, dabrafenib, trametinib).14-17 Melanoma also is considered a “model” tumor for studying the relationship between the immune system and cancer.18
Our case also is instructive in another point: our patient had never sought treatment for her skin lesions, as she said she had other more serious health conditions. Closer evaluation of her skin condition may have led to earlier diagnosis of NF-1, which has important health implications. The average lifespan of patients with NF-1 is 10 to 15 years lower than the general population, with cancer being the leading cause of death.20 Malignant peripheral nerve sheath tumors are the most common malignant tumors observed in such patients.21-23 Other cancers that are associated with NF-1 include rhabdomyosarcomas, gastrointestinal stromal tumors, neuroectodermal tumors, pheochromocytomas, and breast carcinomas.23
To make a clinical diagnosis of NF-1, a patient must have 2 of 7 cardinal clinical features as defined by the National Institutes of Health (Table).24 In our patient with hundreds of café au lait macules and dozens of neurofibromas, the diagnosis was clear; however, in other patients, the skin findings of NF-1 may not be as prominent. A patient could meet criteria for NF-1 diagnosis with the inconspicuous presentation of 6 café au lait macules and either 1 plexiform neurofibroma or 2 neurofibromas (of any type) on the entire body.
We recommend that patients with SLE undergo skin examinations to look for more subtle presentations of NF-1. Earlier diagnosis will help to initiate close monitoring of the disorder’s associated systemic health risks. In addition, the identification of more patients with both NF-1 and SLE may help shed light on the etiology of both conditions.
- Carey JC, Baty BJ, Johnson JP, et al. The genetic aspects of neurofibromatosis. Ann N Y Acad Sci. 1986;486:45-56.
- Pons-Estel GJ, Alarcón GS, Scofield L, et al. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39:257-268.
- Danchenko N, Satia JA, Anthony MS. Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus. 2006;15:308-318.
- Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
- Chakravarty EF, Bush TM, Manzi S, et al. Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum. 2007;56:2092-2094.
- Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
- Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
- Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. a matter of coincidence? Clin Rhematol. 2003;22:496-497.
- Akyuz SG, Caltik A, Bulbul M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheumatol Int. 2012;32:2345-47.
- Makino S, Tampo H. Rare and unusual choroidal abnormalities in a patient with systemic lupus erythematosus. Case Rep Ophthalmol. 2013;4:81-86.
- Galvan JM, Hofkamp MP. Usefulness of intrapartum magnetic resonance imaging for a parturient with neurofibromatosis type I during induction of labor for preeclampsia. Proc (Bayl Univ Med Cent). 2018;31:92-93.
- Gerosa PL, Vai C, Bizzozer L, et al. Immunological and clinical surveillance in Recklinghausen’s neurofibromatosis (NF1). Panminerva Med. 1993;35:80-85.
- Busca R, Abbe P, Mantoux F, et al. RAS mediates the cAMP-dependent activation of extracellular signal-regulated kinases (ERKs) in melanocytes. EMBO J. 2000;19:2900-2910.
- Sullivan RJ, Flaherty K. MAP kinase signaling and inhibition in melanoma. Oncogene. 2013;32:2373-2379.
- Hennessy BT, Smith DL, Ram PT, et al. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov. 2005;12:988-1004.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380:358-365.
- Maio M. Melanoma as a model tumour for immuno-oncology. Ann Oncol. 2012;23:(suppl 8):viii10-4.
- Zmajkovicova K, Jesenberger V, Catalanotti F, et al. MEK1 is required for PTEN membrane recruitment, AKT regulation, and the maintenance of peripheral tolerance. Mol Cell. 2013;50:43-55.
- Patil S, Chamberlain RS. Neoplasms associated with germline and somatic NF1 gene mutations. Oncologist. 2012;17:101-116.
- Carroll SL, Ratner N. How does the Schwann cell lineage form tumors in NF1? Glia. 2008;56:1590-1605.
- Rasmussen SA, Friedman JM. NF1 gene and neurofibromatosis 1. Am J Epidemiol. 2000;151:33-40.
- Yohay K. Neurofibromatosis type 1 and associated malignancies. Curr Neurol Neurosci Rep. 2009;9:247-253.
- Neurofibromatosis. conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45:575-78.
To the Editor:
Patients with concurrent neurofibromatosis type 1 (NF-1) and systemic lupus erythematosus (SLE) rarely have been reported in the literature. Neurofibromatosis type 1 is one of the most common genetic disorders, with a worldwide birth incidence of 1 in 2500 individuals and prevalence of 1 in 4000 individuals.1 The incidence and prevalence of SLE varies widely depending on race and geographic location. Estimated incidence rates for SLE range from 1 to 25 per 100,000 individuals annually in North America, South America, Europe, and Asia.2,3 The reported worldwide prevalence is 20 to 150 cases per 100,000 individuals annually.2,4,5
Given the high prevalence of both conditions, the association between SLE and NF-1 likely is underrecognized; therefore, identifying more patients with concurrent SLE and NF-1 and describing the interplay between the 2 conditions may have important therapeutic implications. We present the case of a middle-aged woman with a history of SLE who had cutaneous lesions characteristic of NF-1 to further the understanding of these concurrent conditions.
A middle-aged woman presented to our academic dermatology clinic for evaluation and removal of dark spots that had been present diffusely on the trunk and extremities since birth. She reported a history of SLE with lupus nephritis, hypertension, and a nodular goiter following a partial thyroidectomy. She noted that she did not seek treatment for the skin findings sooner because she was more concerned about her other medical conditions; however, because she felt these conditions were now stable, she decided to seek treatment for the “rash.” Physical examination revealed hundreds of café au lait macules and numerous neurofibromas diffusely distributed on the trunk and extremities (Figure 1) as well as bilateral axillary freckling. A clinical diagnosis of NF-1 was made.
When questioned, the patient reported that she may have been diagnosed with NF-1 in the past by another physician, but she did not recall it specifically. The patient was advised that there were no treatments for the café au lait macules. We notified her other physicians of the NF-1 diagnosis so she could be monitored for systemic conditions related to NF-1, including optic gliomas, pheochromocytoma, renal artery stenosis, and internal neurofibromas. We also referred the patient for genetic counseling; of note, the patient reported she had 4 children without any evidence of similar skin lesions or chronic health problems.
A PubMed search of articles indexed for MEDLINE using the terms systemic lupus and neurofibromatosis yielded 8 cases of patients having both SLE and NF-1 (including our case).6-11 Our patient reported having multiple lesions since birth, decades before the onset and diagnosis of SLE. In 3 other cases, patients were diagnosed with SLE and then presented with neurofibromas, leading to NF-1 diagnosis.In the discussion of those 3 cases, it was proposed that immune system alterations caused by SLE leading to viral illness may have predisposed the patients to the development of tumors and other collagen diseases, or it could be coincidental.6,7 In another case, a patient with NF-1 developed SLE, which was thought to be coincidental.8 Akyuz et al9 described the case of a pediatric patient with NF-1 who subsequently was diagnosed with SLE. The authors suggested that the lack of neurofibromin contributed to the development of SLE, an autoimmune condition. Under normal circumstances, neurofibromin acts as a guanosine triphosphatase–activating protein for RAS in T cells.10 CD8+ T-cell function also is impaired in patients with SLE.9 Additionally, it has been reported that anti–double-stranded DNA antibodies and immune complexes were present in NF-1 patients, even though there were low titers.12 Thus, the authors proposed that the lack of neurofibromin led to dysregulation of the RAS pathway and impairment of T cells, creating an immune milieu that predisposed the patient to development of SLE. Our case gives additional credence to this theory, as our patient had a similar clinical course: the café au lait macules were present since birth and the symptoms of SLE surfaced much later in her late 20s and 30s. Another case by Makino and Tampo10 described a patient with a history of SLE who was later diagnosed with NF-1 based on choroidal findings highly specific for NF-1 but did not have other classic findings of NF-1. The authors mentioned that there might be a potential relationship between these two disorders but did not speculate any theory in particular for their case.10
The interplay between an autoimmune condition such as SLE and NF-1, a condition traditionally thought to be due to a genetic mutation, may have greater clinical and therapeutic implications beyond just these two disorders. Although it is well established that RAS pathway disruption causes NF-1, it has been uncovered that dysfunction in the RAS pathway also can contribute to melanoma oncogenesis.13,14 These insights have led to the development of and approval of targeted drugs designed to inhibit the RAS pathway (eg, vemurafenib, dabrafenib, trametinib).14-17 Melanoma also is considered a “model” tumor for studying the relationship between the immune system and cancer.18
Our case also is instructive in another point: our patient had never sought treatment for her skin lesions, as she said she had other more serious health conditions. Closer evaluation of her skin condition may have led to earlier diagnosis of NF-1, which has important health implications. The average lifespan of patients with NF-1 is 10 to 15 years lower than the general population, with cancer being the leading cause of death.20 Malignant peripheral nerve sheath tumors are the most common malignant tumors observed in such patients.21-23 Other cancers that are associated with NF-1 include rhabdomyosarcomas, gastrointestinal stromal tumors, neuroectodermal tumors, pheochromocytomas, and breast carcinomas.23
To make a clinical diagnosis of NF-1, a patient must have 2 of 7 cardinal clinical features as defined by the National Institutes of Health (Table).24 In our patient with hundreds of café au lait macules and dozens of neurofibromas, the diagnosis was clear; however, in other patients, the skin findings of NF-1 may not be as prominent. A patient could meet criteria for NF-1 diagnosis with the inconspicuous presentation of 6 café au lait macules and either 1 plexiform neurofibroma or 2 neurofibromas (of any type) on the entire body.
We recommend that patients with SLE undergo skin examinations to look for more subtle presentations of NF-1. Earlier diagnosis will help to initiate close monitoring of the disorder’s associated systemic health risks. In addition, the identification of more patients with both NF-1 and SLE may help shed light on the etiology of both conditions.
To the Editor:
Patients with concurrent neurofibromatosis type 1 (NF-1) and systemic lupus erythematosus (SLE) rarely have been reported in the literature. Neurofibromatosis type 1 is one of the most common genetic disorders, with a worldwide birth incidence of 1 in 2500 individuals and prevalence of 1 in 4000 individuals.1 The incidence and prevalence of SLE varies widely depending on race and geographic location. Estimated incidence rates for SLE range from 1 to 25 per 100,000 individuals annually in North America, South America, Europe, and Asia.2,3 The reported worldwide prevalence is 20 to 150 cases per 100,000 individuals annually.2,4,5
Given the high prevalence of both conditions, the association between SLE and NF-1 likely is underrecognized; therefore, identifying more patients with concurrent SLE and NF-1 and describing the interplay between the 2 conditions may have important therapeutic implications. We present the case of a middle-aged woman with a history of SLE who had cutaneous lesions characteristic of NF-1 to further the understanding of these concurrent conditions.
A middle-aged woman presented to our academic dermatology clinic for evaluation and removal of dark spots that had been present diffusely on the trunk and extremities since birth. She reported a history of SLE with lupus nephritis, hypertension, and a nodular goiter following a partial thyroidectomy. She noted that she did not seek treatment for the skin findings sooner because she was more concerned about her other medical conditions; however, because she felt these conditions were now stable, she decided to seek treatment for the “rash.” Physical examination revealed hundreds of café au lait macules and numerous neurofibromas diffusely distributed on the trunk and extremities (Figure 1) as well as bilateral axillary freckling. A clinical diagnosis of NF-1 was made.
When questioned, the patient reported that she may have been diagnosed with NF-1 in the past by another physician, but she did not recall it specifically. The patient was advised that there were no treatments for the café au lait macules. We notified her other physicians of the NF-1 diagnosis so she could be monitored for systemic conditions related to NF-1, including optic gliomas, pheochromocytoma, renal artery stenosis, and internal neurofibromas. We also referred the patient for genetic counseling; of note, the patient reported she had 4 children without any evidence of similar skin lesions or chronic health problems.
A PubMed search of articles indexed for MEDLINE using the terms systemic lupus and neurofibromatosis yielded 8 cases of patients having both SLE and NF-1 (including our case).6-11 Our patient reported having multiple lesions since birth, decades before the onset and diagnosis of SLE. In 3 other cases, patients were diagnosed with SLE and then presented with neurofibromas, leading to NF-1 diagnosis.In the discussion of those 3 cases, it was proposed that immune system alterations caused by SLE leading to viral illness may have predisposed the patients to the development of tumors and other collagen diseases, or it could be coincidental.6,7 In another case, a patient with NF-1 developed SLE, which was thought to be coincidental.8 Akyuz et al9 described the case of a pediatric patient with NF-1 who subsequently was diagnosed with SLE. The authors suggested that the lack of neurofibromin contributed to the development of SLE, an autoimmune condition. Under normal circumstances, neurofibromin acts as a guanosine triphosphatase–activating protein for RAS in T cells.10 CD8+ T-cell function also is impaired in patients with SLE.9 Additionally, it has been reported that anti–double-stranded DNA antibodies and immune complexes were present in NF-1 patients, even though there were low titers.12 Thus, the authors proposed that the lack of neurofibromin led to dysregulation of the RAS pathway and impairment of T cells, creating an immune milieu that predisposed the patient to development of SLE. Our case gives additional credence to this theory, as our patient had a similar clinical course: the café au lait macules were present since birth and the symptoms of SLE surfaced much later in her late 20s and 30s. Another case by Makino and Tampo10 described a patient with a history of SLE who was later diagnosed with NF-1 based on choroidal findings highly specific for NF-1 but did not have other classic findings of NF-1. The authors mentioned that there might be a potential relationship between these two disorders but did not speculate any theory in particular for their case.10
The interplay between an autoimmune condition such as SLE and NF-1, a condition traditionally thought to be due to a genetic mutation, may have greater clinical and therapeutic implications beyond just these two disorders. Although it is well established that RAS pathway disruption causes NF-1, it has been uncovered that dysfunction in the RAS pathway also can contribute to melanoma oncogenesis.13,14 These insights have led to the development of and approval of targeted drugs designed to inhibit the RAS pathway (eg, vemurafenib, dabrafenib, trametinib).14-17 Melanoma also is considered a “model” tumor for studying the relationship between the immune system and cancer.18
Our case also is instructive in another point: our patient had never sought treatment for her skin lesions, as she said she had other more serious health conditions. Closer evaluation of her skin condition may have led to earlier diagnosis of NF-1, which has important health implications. The average lifespan of patients with NF-1 is 10 to 15 years lower than the general population, with cancer being the leading cause of death.20 Malignant peripheral nerve sheath tumors are the most common malignant tumors observed in such patients.21-23 Other cancers that are associated with NF-1 include rhabdomyosarcomas, gastrointestinal stromal tumors, neuroectodermal tumors, pheochromocytomas, and breast carcinomas.23
To make a clinical diagnosis of NF-1, a patient must have 2 of 7 cardinal clinical features as defined by the National Institutes of Health (Table).24 In our patient with hundreds of café au lait macules and dozens of neurofibromas, the diagnosis was clear; however, in other patients, the skin findings of NF-1 may not be as prominent. A patient could meet criteria for NF-1 diagnosis with the inconspicuous presentation of 6 café au lait macules and either 1 plexiform neurofibroma or 2 neurofibromas (of any type) on the entire body.
We recommend that patients with SLE undergo skin examinations to look for more subtle presentations of NF-1. Earlier diagnosis will help to initiate close monitoring of the disorder’s associated systemic health risks. In addition, the identification of more patients with both NF-1 and SLE may help shed light on the etiology of both conditions.
- Carey JC, Baty BJ, Johnson JP, et al. The genetic aspects of neurofibromatosis. Ann N Y Acad Sci. 1986;486:45-56.
- Pons-Estel GJ, Alarcón GS, Scofield L, et al. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39:257-268.
- Danchenko N, Satia JA, Anthony MS. Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus. 2006;15:308-318.
- Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
- Chakravarty EF, Bush TM, Manzi S, et al. Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum. 2007;56:2092-2094.
- Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
- Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
- Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. a matter of coincidence? Clin Rhematol. 2003;22:496-497.
- Akyuz SG, Caltik A, Bulbul M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheumatol Int. 2012;32:2345-47.
- Makino S, Tampo H. Rare and unusual choroidal abnormalities in a patient with systemic lupus erythematosus. Case Rep Ophthalmol. 2013;4:81-86.
- Galvan JM, Hofkamp MP. Usefulness of intrapartum magnetic resonance imaging for a parturient with neurofibromatosis type I during induction of labor for preeclampsia. Proc (Bayl Univ Med Cent). 2018;31:92-93.
- Gerosa PL, Vai C, Bizzozer L, et al. Immunological and clinical surveillance in Recklinghausen’s neurofibromatosis (NF1). Panminerva Med. 1993;35:80-85.
- Busca R, Abbe P, Mantoux F, et al. RAS mediates the cAMP-dependent activation of extracellular signal-regulated kinases (ERKs) in melanocytes. EMBO J. 2000;19:2900-2910.
- Sullivan RJ, Flaherty K. MAP kinase signaling and inhibition in melanoma. Oncogene. 2013;32:2373-2379.
- Hennessy BT, Smith DL, Ram PT, et al. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov. 2005;12:988-1004.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380:358-365.
- Maio M. Melanoma as a model tumour for immuno-oncology. Ann Oncol. 2012;23:(suppl 8):viii10-4.
- Zmajkovicova K, Jesenberger V, Catalanotti F, et al. MEK1 is required for PTEN membrane recruitment, AKT regulation, and the maintenance of peripheral tolerance. Mol Cell. 2013;50:43-55.
- Patil S, Chamberlain RS. Neoplasms associated with germline and somatic NF1 gene mutations. Oncologist. 2012;17:101-116.
- Carroll SL, Ratner N. How does the Schwann cell lineage form tumors in NF1? Glia. 2008;56:1590-1605.
- Rasmussen SA, Friedman JM. NF1 gene and neurofibromatosis 1. Am J Epidemiol. 2000;151:33-40.
- Yohay K. Neurofibromatosis type 1 and associated malignancies. Curr Neurol Neurosci Rep. 2009;9:247-253.
- Neurofibromatosis. conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45:575-78.
- Carey JC, Baty BJ, Johnson JP, et al. The genetic aspects of neurofibromatosis. Ann N Y Acad Sci. 1986;486:45-56.
- Pons-Estel GJ, Alarcón GS, Scofield L, et al. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39:257-268.
- Danchenko N, Satia JA, Anthony MS. Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus. 2006;15:308-318.
- Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
- Chakravarty EF, Bush TM, Manzi S, et al. Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum. 2007;56:2092-2094.
- Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
- Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
- Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. a matter of coincidence? Clin Rhematol. 2003;22:496-497.
- Akyuz SG, Caltik A, Bulbul M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheumatol Int. 2012;32:2345-47.
- Makino S, Tampo H. Rare and unusual choroidal abnormalities in a patient with systemic lupus erythematosus. Case Rep Ophthalmol. 2013;4:81-86.
- Galvan JM, Hofkamp MP. Usefulness of intrapartum magnetic resonance imaging for a parturient with neurofibromatosis type I during induction of labor for preeclampsia. Proc (Bayl Univ Med Cent). 2018;31:92-93.
- Gerosa PL, Vai C, Bizzozer L, et al. Immunological and clinical surveillance in Recklinghausen’s neurofibromatosis (NF1). Panminerva Med. 1993;35:80-85.
- Busca R, Abbe P, Mantoux F, et al. RAS mediates the cAMP-dependent activation of extracellular signal-regulated kinases (ERKs) in melanocytes. EMBO J. 2000;19:2900-2910.
- Sullivan RJ, Flaherty K. MAP kinase signaling and inhibition in melanoma. Oncogene. 2013;32:2373-2379.
- Hennessy BT, Smith DL, Ram PT, et al. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov. 2005;12:988-1004.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380:358-365.
- Maio M. Melanoma as a model tumour for immuno-oncology. Ann Oncol. 2012;23:(suppl 8):viii10-4.
- Zmajkovicova K, Jesenberger V, Catalanotti F, et al. MEK1 is required for PTEN membrane recruitment, AKT regulation, and the maintenance of peripheral tolerance. Mol Cell. 2013;50:43-55.
- Patil S, Chamberlain RS. Neoplasms associated with germline and somatic NF1 gene mutations. Oncologist. 2012;17:101-116.
- Carroll SL, Ratner N. How does the Schwann cell lineage form tumors in NF1? Glia. 2008;56:1590-1605.
- Rasmussen SA, Friedman JM. NF1 gene and neurofibromatosis 1. Am J Epidemiol. 2000;151:33-40.
- Yohay K. Neurofibromatosis type 1 and associated malignancies. Curr Neurol Neurosci Rep. 2009;9:247-253.
- Neurofibromatosis. conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45:575-78.
Practice Points
- Patients with neurofibromatosis type 1 (NF-1) benefit from early diagnosis and long-term follow-up.
- Patients with systemic lupus erythematosus (SLE) may develop different malignancies given the immune dysregulation. We recommend that patients with SLE undergo detailed skin examinations to check for subtle clues for NF-1.
- Similarly, patients with NF-1 can develop SLE later in life.
An unplanned career
A focus on health system transformation
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
A focus on health system transformation
A focus on health system transformation
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
ONC aims to help docs, patients with information sharing in proposed rule
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”