User login
SNOT-22 may help identify patients with undiagnosed OSA
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
REPORTING FROM THE TRIOLOGICAL CSM
Key clinical point: Obstructive sleep apnea (OSA) should be suspected in patients with sleep dysfunction as their primary complaint without the significant nasal drainage and anosmia that characterizes chronic rhinosinusitis.
Major finding: Sleep and psychological domain scores on the SNOT-22 were not significantly different between patients with chronic rhinosinusitis and those with OSA, although OSA patients were more likely to choose a sleep-related symptom as their most important complaint (P less than .001).
Study details: A retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey.
Disclosures: Dr. Jang reported receiving research funding from Olympus.
Treating preeclampsia
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Single-dose tafenoquine appears to prevent malaria relapse
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: In DETECTIVE, 6-month rates of freedom from recurrence from Plasmodium vivax infection were 62% with tafenoquine, 70% with primaquine, and 28% with placebo.
Study details: Two randomized, phase 3, double-blind controlled trials of patients with confirmed P. vivax infection (DETECTIVE and GATHER) and without deficient G6PD activity.
Disclosures: GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having financial disclosures.
Source: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
Oral GLP-1 receptor agonist pioneered in T2DM trial
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
REPORTING FROM EASD 2018
Key clinical point: A novel oral formulation of semaglutide proved better than placebo for diabetes control and weight loss in patients with T2DM.
Major finding: Mean change in hemoglobin A1c (baseline to week 26) – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%.
Study details: Phase 3a, multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 individuals with T2DM being treated with diet and exercise only.
Disclosures: The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk. She also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards of, undertaking ad hoc consultancy work for, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
Source: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 – PIONEER Trial; Bailey C. EASD 2018, Session S18 – PIONEER Trial.
mRECIST response to kinase inhibitors predicts survival in HCC
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
REPORTING FROM THE 2019 GI CANCERS SYMPOSIUM
Key clinical point: .
Major finding: Median overall survival was a respective 22.4 months and 11.4 months in patients who did and did not have a response according to mRECIST criteria (HR, 0.61; P less than .0001).
Study details: A retrospective post hoc analysis of a phase 3 randomized controlled trial of lenvatinib versus sorafenib among 954 patients with untreated, unresectable HCC (REFLECT trial).
Disclosures: Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
Source: Kudo M et al. 2019 GI Cancers Symposium, Abstract 186.
Coffee shop founder provides mental health intervention
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
Guideline public comment period framework
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.
2018 AGA legislative wins
To those who took time to advocate on behalf of your profession and patients, thank you. Because of your efforts, we achieved several key successes that benefit clinicians, researchers and patients.
Together we were able to help advance several AGA policy priorities — administrative burden relief, digestive disease research and funding, and patient access and protection — as well as the science and practice of gastroenterology.
This year, we will be counting on you, our members, to again lead the charge to achieve AGA’s mission — empowering clinicians and researchers to improve digestive health — by calling on legislators and regulators to ensure the voice of gastroenterology continue to be heard.
NIH funding increase
AGA advocated and secured a $2 billion increase in NIH funding for fiscal year (FY) 2019. When added to increases from the two previous fiscal years, NIH’s funding has increased by 30 percent over the past three years, which is the largest increase since the doubling period in the last decade.
IPAB repeal prevents automatic Medicare cuts
Congress repealed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act (ACA). AGA and all of organized medicine long opposed IPAB since its sole purpose was to make budgetary cuts to Medicare if it reached a certain threshold of spending.
MIPS changes means more flexibility for physicians
AGA and the physician community were successful in securing flexibility under the new Medicare Quality Payment Program and the Merit-based Incentive Payment System (MIPS) that were created under the Medicare Access and CHIP Reauthorization Act. The changes give CMS more flexibility in implementing the program and will ensure that physicians have an opportunity to be successful in MIPS.
500 AGA members prevent radical changes to outpatient documentation
In response to a CMS proposal to radically change how outpatient evaluation and management (E/M) services are documented, more than 500 AGA members urged CMS not to move forward with its plan. As a result, CMS withdrew or delayed many of the proposed changes to E/M services that negatively impacted reimbursement. CMS did move forward with several changes to E/M documentation in an effort to reduce administrative burden.
AGA members send more than 940 letters to Congress
AGA launched the Congressional Advocates Program to provide an infrastructure and tools for members to effectively advocate on behalf of their profession and patients. AGA members heeded our calls to action and sent more than 940 letters sent to Congress and federal agencies throughout 2018. We thank our advocates whose participation makes a difference.
To those who took time to advocate on behalf of your profession and patients, thank you. Because of your efforts, we achieved several key successes that benefit clinicians, researchers and patients.
Together we were able to help advance several AGA policy priorities — administrative burden relief, digestive disease research and funding, and patient access and protection — as well as the science and practice of gastroenterology.
This year, we will be counting on you, our members, to again lead the charge to achieve AGA’s mission — empowering clinicians and researchers to improve digestive health — by calling on legislators and regulators to ensure the voice of gastroenterology continue to be heard.
NIH funding increase
AGA advocated and secured a $2 billion increase in NIH funding for fiscal year (FY) 2019. When added to increases from the two previous fiscal years, NIH’s funding has increased by 30 percent over the past three years, which is the largest increase since the doubling period in the last decade.
IPAB repeal prevents automatic Medicare cuts
Congress repealed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act (ACA). AGA and all of organized medicine long opposed IPAB since its sole purpose was to make budgetary cuts to Medicare if it reached a certain threshold of spending.
MIPS changes means more flexibility for physicians
AGA and the physician community were successful in securing flexibility under the new Medicare Quality Payment Program and the Merit-based Incentive Payment System (MIPS) that were created under the Medicare Access and CHIP Reauthorization Act. The changes give CMS more flexibility in implementing the program and will ensure that physicians have an opportunity to be successful in MIPS.
500 AGA members prevent radical changes to outpatient documentation
In response to a CMS proposal to radically change how outpatient evaluation and management (E/M) services are documented, more than 500 AGA members urged CMS not to move forward with its plan. As a result, CMS withdrew or delayed many of the proposed changes to E/M services that negatively impacted reimbursement. CMS did move forward with several changes to E/M documentation in an effort to reduce administrative burden.
AGA members send more than 940 letters to Congress
AGA launched the Congressional Advocates Program to provide an infrastructure and tools for members to effectively advocate on behalf of their profession and patients. AGA members heeded our calls to action and sent more than 940 letters sent to Congress and federal agencies throughout 2018. We thank our advocates whose participation makes a difference.
To those who took time to advocate on behalf of your profession and patients, thank you. Because of your efforts, we achieved several key successes that benefit clinicians, researchers and patients.
Together we were able to help advance several AGA policy priorities — administrative burden relief, digestive disease research and funding, and patient access and protection — as well as the science and practice of gastroenterology.
This year, we will be counting on you, our members, to again lead the charge to achieve AGA’s mission — empowering clinicians and researchers to improve digestive health — by calling on legislators and regulators to ensure the voice of gastroenterology continue to be heard.
NIH funding increase
AGA advocated and secured a $2 billion increase in NIH funding for fiscal year (FY) 2019. When added to increases from the two previous fiscal years, NIH’s funding has increased by 30 percent over the past three years, which is the largest increase since the doubling period in the last decade.
IPAB repeal prevents automatic Medicare cuts
Congress repealed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act (ACA). AGA and all of organized medicine long opposed IPAB since its sole purpose was to make budgetary cuts to Medicare if it reached a certain threshold of spending.
MIPS changes means more flexibility for physicians
AGA and the physician community were successful in securing flexibility under the new Medicare Quality Payment Program and the Merit-based Incentive Payment System (MIPS) that were created under the Medicare Access and CHIP Reauthorization Act. The changes give CMS more flexibility in implementing the program and will ensure that physicians have an opportunity to be successful in MIPS.
500 AGA members prevent radical changes to outpatient documentation
In response to a CMS proposal to radically change how outpatient evaluation and management (E/M) services are documented, more than 500 AGA members urged CMS not to move forward with its plan. As a result, CMS withdrew or delayed many of the proposed changes to E/M services that negatively impacted reimbursement. CMS did move forward with several changes to E/M documentation in an effort to reduce administrative burden.
AGA members send more than 940 letters to Congress
AGA launched the Congressional Advocates Program to provide an infrastructure and tools for members to effectively advocate on behalf of their profession and patients. AGA members heeded our calls to action and sent more than 940 letters sent to Congress and federal agencies throughout 2018. We thank our advocates whose participation makes a difference.
Subclinical hypothyroidism boosts immediate risk of heart failure
CHICAGO – The short-term risk of developing heart failure in patients with newly identified hypothyroidism, be it overt or subclinical, is double that of euthyroid individuals, Caroline H. Noergaard, MD, reported at the American Heart Association scientific sessions.
“This is really important clinically. The association with heart failure has previously been shown in both overt and subclinical hyperthyroidism, but it’s actually new knowledge that hypothyroidism is associated with immediate risk of heart failure. And a lot of people have subclinical hypothyroidism,” said Dr. Noergaard, a PhD student in epidemiology at Aalborg (Denmark) University.
Also at the meeting, Jeffrey L. Anderson, MD, reported that free thyroxine levels within the normal reference range were associated in graded fashion with an increased prevalence and incidence of atrial fibrillation in a large Utah study, a finding that provides independent confirmation of an earlier report by investigators from the population-based Rotterdam Study.
“These findings validate those of the Rotterdam Study in a much larger dataset and may have important clinical implications, including a redefinition of the reference range and the target-free T4 levels for thyroxine replacement therapy,” observed Dr. Anderson, professor of internal medicine at the University of Utah, Salt Lake City, and a research cardiologist at the Intermountain Medical Center Heart Institute.
Hypothyroidism and heart failure
Dr. Noergaard presented a retrospective study of over 1 million Copenhagen-area adults (mean age, 50 years) with no history of heart failure, who had their first thyroid function test. She and her coinvestigators turned to comprehensive Danish national health care registries to determine how many of these individuals were diagnosed with new-onset heart failure within 90 days after their thyroid function test.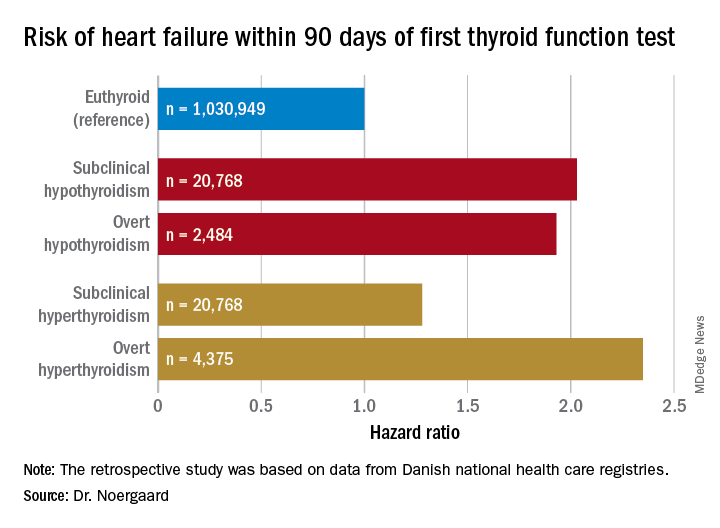
Subclinical hypothyroidism was defined by a thyroid-stimulating hormone level greater than 5 mIU/L and a free T4 of 9-22 pmol/L. Overt hypothyroidism required a TSH greater than 5 mIU/L with a free T4 less than 9 pmol/L.
Free T4 predicts atrial fibrillation risk
Dr. Anderson presented a retrospective analysis of 174,914 adult patients in the Intermountain Healthcare EMR database, none of whom were on thyroid replacement at entry. The patients, who were a mean age of 64 years and 65% women, were followed for an average of 6.3 years. Of these, 88.4% had a free T4 within the normal reference range of 0.75-1.5 ng/dL, 7.4% had a value below the cutoff for normal, and 4.2% had a free T4 above the reference range.
Upon dividing the patients within the normal range into quartiles based upon their free T4 level, he and his coinvestigators found that the baseline prevalence of atrial fibrillation was 8.7% in those in quartile 1, 9.3% in quartile 2, 10.5% in quartile 3, and 12.6% in quartile 4. In a multivariate analysis adjusted for potential confounders, the risk of prevalent atrial fibrillation was increased by 11% for patients in quartile 2, compared with those in the first quartile, by 22% in quartile 3, and by 40% in quartile 4.
The incidence of new-onset atrial fibrillation during 3 years of follow-up was 4.1% in patients in normal-range quartile 1, 4.3% in quartile 2, 4.5% in quartile 3, and 5.2% in the top normal-range quartile. The odds of developing atrial fibrillation were increased by 8% and 16% in quartiles 3 and 4, compared with quartile 1.
Serum TSH and free T3 levels showed no consistent relationship with atrial fibrillation.
The Utah findings confirm in a large U.S. population the earlier report from the Rotterdam Study (J Clin Endocrinol Metab. 2015 Oct;100(10):3718-24).
Dr. Noergaard and Dr. Anderson reported having no financial conflicts regarding their studies, which were carried out free of commercial support.
CHICAGO – The short-term risk of developing heart failure in patients with newly identified hypothyroidism, be it overt or subclinical, is double that of euthyroid individuals, Caroline H. Noergaard, MD, reported at the American Heart Association scientific sessions.
“This is really important clinically. The association with heart failure has previously been shown in both overt and subclinical hyperthyroidism, but it’s actually new knowledge that hypothyroidism is associated with immediate risk of heart failure. And a lot of people have subclinical hypothyroidism,” said Dr. Noergaard, a PhD student in epidemiology at Aalborg (Denmark) University.
Also at the meeting, Jeffrey L. Anderson, MD, reported that free thyroxine levels within the normal reference range were associated in graded fashion with an increased prevalence and incidence of atrial fibrillation in a large Utah study, a finding that provides independent confirmation of an earlier report by investigators from the population-based Rotterdam Study.
“These findings validate those of the Rotterdam Study in a much larger dataset and may have important clinical implications, including a redefinition of the reference range and the target-free T4 levels for thyroxine replacement therapy,” observed Dr. Anderson, professor of internal medicine at the University of Utah, Salt Lake City, and a research cardiologist at the Intermountain Medical Center Heart Institute.
Hypothyroidism and heart failure
Dr. Noergaard presented a retrospective study of over 1 million Copenhagen-area adults (mean age, 50 years) with no history of heart failure, who had their first thyroid function test. She and her coinvestigators turned to comprehensive Danish national health care registries to determine how many of these individuals were diagnosed with new-onset heart failure within 90 days after their thyroid function test.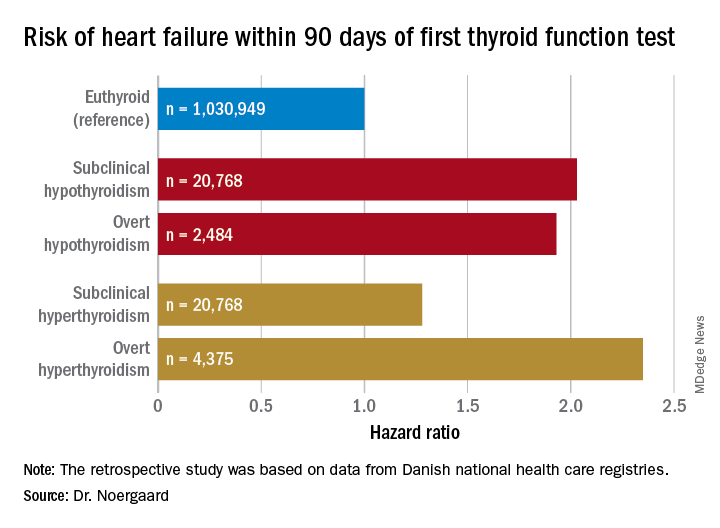
Subclinical hypothyroidism was defined by a thyroid-stimulating hormone level greater than 5 mIU/L and a free T4 of 9-22 pmol/L. Overt hypothyroidism required a TSH greater than 5 mIU/L with a free T4 less than 9 pmol/L.
Free T4 predicts atrial fibrillation risk
Dr. Anderson presented a retrospective analysis of 174,914 adult patients in the Intermountain Healthcare EMR database, none of whom were on thyroid replacement at entry. The patients, who were a mean age of 64 years and 65% women, were followed for an average of 6.3 years. Of these, 88.4% had a free T4 within the normal reference range of 0.75-1.5 ng/dL, 7.4% had a value below the cutoff for normal, and 4.2% had a free T4 above the reference range.
Upon dividing the patients within the normal range into quartiles based upon their free T4 level, he and his coinvestigators found that the baseline prevalence of atrial fibrillation was 8.7% in those in quartile 1, 9.3% in quartile 2, 10.5% in quartile 3, and 12.6% in quartile 4. In a multivariate analysis adjusted for potential confounders, the risk of prevalent atrial fibrillation was increased by 11% for patients in quartile 2, compared with those in the first quartile, by 22% in quartile 3, and by 40% in quartile 4.
The incidence of new-onset atrial fibrillation during 3 years of follow-up was 4.1% in patients in normal-range quartile 1, 4.3% in quartile 2, 4.5% in quartile 3, and 5.2% in the top normal-range quartile. The odds of developing atrial fibrillation were increased by 8% and 16% in quartiles 3 and 4, compared with quartile 1.
Serum TSH and free T3 levels showed no consistent relationship with atrial fibrillation.
The Utah findings confirm in a large U.S. population the earlier report from the Rotterdam Study (J Clin Endocrinol Metab. 2015 Oct;100(10):3718-24).
Dr. Noergaard and Dr. Anderson reported having no financial conflicts regarding their studies, which were carried out free of commercial support.
CHICAGO – The short-term risk of developing heart failure in patients with newly identified hypothyroidism, be it overt or subclinical, is double that of euthyroid individuals, Caroline H. Noergaard, MD, reported at the American Heart Association scientific sessions.
“This is really important clinically. The association with heart failure has previously been shown in both overt and subclinical hyperthyroidism, but it’s actually new knowledge that hypothyroidism is associated with immediate risk of heart failure. And a lot of people have subclinical hypothyroidism,” said Dr. Noergaard, a PhD student in epidemiology at Aalborg (Denmark) University.
Also at the meeting, Jeffrey L. Anderson, MD, reported that free thyroxine levels within the normal reference range were associated in graded fashion with an increased prevalence and incidence of atrial fibrillation in a large Utah study, a finding that provides independent confirmation of an earlier report by investigators from the population-based Rotterdam Study.
“These findings validate those of the Rotterdam Study in a much larger dataset and may have important clinical implications, including a redefinition of the reference range and the target-free T4 levels for thyroxine replacement therapy,” observed Dr. Anderson, professor of internal medicine at the University of Utah, Salt Lake City, and a research cardiologist at the Intermountain Medical Center Heart Institute.
Hypothyroidism and heart failure
Dr. Noergaard presented a retrospective study of over 1 million Copenhagen-area adults (mean age, 50 years) with no history of heart failure, who had their first thyroid function test. She and her coinvestigators turned to comprehensive Danish national health care registries to determine how many of these individuals were diagnosed with new-onset heart failure within 90 days after their thyroid function test.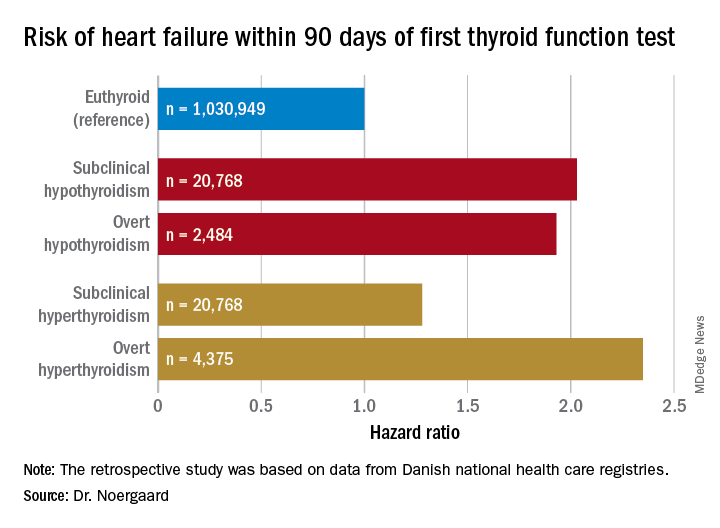
Subclinical hypothyroidism was defined by a thyroid-stimulating hormone level greater than 5 mIU/L and a free T4 of 9-22 pmol/L. Overt hypothyroidism required a TSH greater than 5 mIU/L with a free T4 less than 9 pmol/L.
Free T4 predicts atrial fibrillation risk
Dr. Anderson presented a retrospective analysis of 174,914 adult patients in the Intermountain Healthcare EMR database, none of whom were on thyroid replacement at entry. The patients, who were a mean age of 64 years and 65% women, were followed for an average of 6.3 years. Of these, 88.4% had a free T4 within the normal reference range of 0.75-1.5 ng/dL, 7.4% had a value below the cutoff for normal, and 4.2% had a free T4 above the reference range.
Upon dividing the patients within the normal range into quartiles based upon their free T4 level, he and his coinvestigators found that the baseline prevalence of atrial fibrillation was 8.7% in those in quartile 1, 9.3% in quartile 2, 10.5% in quartile 3, and 12.6% in quartile 4. In a multivariate analysis adjusted for potential confounders, the risk of prevalent atrial fibrillation was increased by 11% for patients in quartile 2, compared with those in the first quartile, by 22% in quartile 3, and by 40% in quartile 4.
The incidence of new-onset atrial fibrillation during 3 years of follow-up was 4.1% in patients in normal-range quartile 1, 4.3% in quartile 2, 4.5% in quartile 3, and 5.2% in the top normal-range quartile. The odds of developing atrial fibrillation were increased by 8% and 16% in quartiles 3 and 4, compared with quartile 1.
Serum TSH and free T3 levels showed no consistent relationship with atrial fibrillation.
The Utah findings confirm in a large U.S. population the earlier report from the Rotterdam Study (J Clin Endocrinol Metab. 2015 Oct;100(10):3718-24).
Dr. Noergaard and Dr. Anderson reported having no financial conflicts regarding their studies, which were carried out free of commercial support.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Both subclinical and overt hypothyroidism are associated with a 100% increased risk of being diagnosed with heart failure, compared with euthyroid individuals.
Study details: This was a retrospective study of the association between free thyroxine levels and short-term risk of developing heart failure in more than 1 million Copenhagen-area patients.
Disclosures: The presenter reported having no financial conflicts regarding the Danish study, conducted free of commercial support.
New study determines factors that can send flu patients to the ICU
Numerous independent factors – including a history of obstructive/central sleep apnea syndrome (OSAS/CSAS) or myocardial infarction, along with a body mass index greater than 30 g/m2 – could be related to ICU admission and subsequent high mortality rates in influenza patients, according to an analysis of patients in the Netherlands who were treated during the influenza epidemic of 2015-2016.
Along with determining these factors, lead author M.C. Beumer, of Radboud University Medical Center, the Netherlands, and his coauthors found that “coinfections with bacterial, fungal, and viral pathogens developed more often in patients who were admitted to the ICU.” The study was published in the Journal of Critical Care.
The coauthors reviewed 199 influenza patients who were admitted to two medical centers in the Netherlands during October 2015–April 2016. Of those patients, 45 (23%) were admitted to the ICU, primarily because of respiratory failure, and their mortality rate was 17/45 (38%) versus an overall mortality rate of 18/199 (9%).
Compared with patients in the normal ward, patients admitted to the ICU more frequently had a history of OSAS/CSAS (11% vs. 3%; P = .03) and MI (20% vs. 6%; P = .007), along with a BMI higher than 30 g/m2 (30% vs. 15%; P = .04) and dyspnea as a symptom (77% vs. 48%,; P = .001). In addition, more ICU-admitted patients had influenza A rather than influenza B, compared with those not admitted (87% vs. 66%; P = .009).
Pulmonary coinfections – including bacterial, fungal, and viral pathogens – were also proportionally higher among the 45 ICU patients (56% vs. 20%; P less than .0001). The most common bacterial pathogens were Staphylococcus aureus (11%) and Streptococcus pneumoniae (7%) while Aspergillus fumigatus (18%) and Pneumocystis jirovecii (7%) topped the fungal pathogens.
Mr. Beumer and his colleagues noted potential limitations of their work, including the selection of patients from among the “most severely ill” contributing to an ICU admission rate that surpassed the 5%-10% described elsewhere. They also admitted that their study relied on a “relatively small sample size,” focusing on one seasonal influenza outbreak. However, “despite the limited validity,” they reiterated that “the identified factors may contribute to a complicated disease course and could represent a tool for early recognition of the influenza patients at risk for a complicated disease course.”
The authors reported no conflicts of interest.
SOURCE: Beumer MC et al. J Crit Care. 2019;50:59-65.
.
Numerous independent factors – including a history of obstructive/central sleep apnea syndrome (OSAS/CSAS) or myocardial infarction, along with a body mass index greater than 30 g/m2 – could be related to ICU admission and subsequent high mortality rates in influenza patients, according to an analysis of patients in the Netherlands who were treated during the influenza epidemic of 2015-2016.
Along with determining these factors, lead author M.C. Beumer, of Radboud University Medical Center, the Netherlands, and his coauthors found that “coinfections with bacterial, fungal, and viral pathogens developed more often in patients who were admitted to the ICU.” The study was published in the Journal of Critical Care.
The coauthors reviewed 199 influenza patients who were admitted to two medical centers in the Netherlands during October 2015–April 2016. Of those patients, 45 (23%) were admitted to the ICU, primarily because of respiratory failure, and their mortality rate was 17/45 (38%) versus an overall mortality rate of 18/199 (9%).
Compared with patients in the normal ward, patients admitted to the ICU more frequently had a history of OSAS/CSAS (11% vs. 3%; P = .03) and MI (20% vs. 6%; P = .007), along with a BMI higher than 30 g/m2 (30% vs. 15%; P = .04) and dyspnea as a symptom (77% vs. 48%,; P = .001). In addition, more ICU-admitted patients had influenza A rather than influenza B, compared with those not admitted (87% vs. 66%; P = .009).
Pulmonary coinfections – including bacterial, fungal, and viral pathogens – were also proportionally higher among the 45 ICU patients (56% vs. 20%; P less than .0001). The most common bacterial pathogens were Staphylococcus aureus (11%) and Streptococcus pneumoniae (7%) while Aspergillus fumigatus (18%) and Pneumocystis jirovecii (7%) topped the fungal pathogens.
Mr. Beumer and his colleagues noted potential limitations of their work, including the selection of patients from among the “most severely ill” contributing to an ICU admission rate that surpassed the 5%-10% described elsewhere. They also admitted that their study relied on a “relatively small sample size,” focusing on one seasonal influenza outbreak. However, “despite the limited validity,” they reiterated that “the identified factors may contribute to a complicated disease course and could represent a tool for early recognition of the influenza patients at risk for a complicated disease course.”
The authors reported no conflicts of interest.
SOURCE: Beumer MC et al. J Crit Care. 2019;50:59-65.
.
Numerous independent factors – including a history of obstructive/central sleep apnea syndrome (OSAS/CSAS) or myocardial infarction, along with a body mass index greater than 30 g/m2 – could be related to ICU admission and subsequent high mortality rates in influenza patients, according to an analysis of patients in the Netherlands who were treated during the influenza epidemic of 2015-2016.
Along with determining these factors, lead author M.C. Beumer, of Radboud University Medical Center, the Netherlands, and his coauthors found that “coinfections with bacterial, fungal, and viral pathogens developed more often in patients who were admitted to the ICU.” The study was published in the Journal of Critical Care.
The coauthors reviewed 199 influenza patients who were admitted to two medical centers in the Netherlands during October 2015–April 2016. Of those patients, 45 (23%) were admitted to the ICU, primarily because of respiratory failure, and their mortality rate was 17/45 (38%) versus an overall mortality rate of 18/199 (9%).
Compared with patients in the normal ward, patients admitted to the ICU more frequently had a history of OSAS/CSAS (11% vs. 3%; P = .03) and MI (20% vs. 6%; P = .007), along with a BMI higher than 30 g/m2 (30% vs. 15%; P = .04) and dyspnea as a symptom (77% vs. 48%,; P = .001). In addition, more ICU-admitted patients had influenza A rather than influenza B, compared with those not admitted (87% vs. 66%; P = .009).
Pulmonary coinfections – including bacterial, fungal, and viral pathogens – were also proportionally higher among the 45 ICU patients (56% vs. 20%; P less than .0001). The most common bacterial pathogens were Staphylococcus aureus (11%) and Streptococcus pneumoniae (7%) while Aspergillus fumigatus (18%) and Pneumocystis jirovecii (7%) topped the fungal pathogens.
Mr. Beumer and his colleagues noted potential limitations of their work, including the selection of patients from among the “most severely ill” contributing to an ICU admission rate that surpassed the 5%-10% described elsewhere. They also admitted that their study relied on a “relatively small sample size,” focusing on one seasonal influenza outbreak. However, “despite the limited validity,” they reiterated that “the identified factors may contribute to a complicated disease course and could represent a tool for early recognition of the influenza patients at risk for a complicated disease course.”
The authors reported no conflicts of interest.
SOURCE: Beumer MC et al. J Crit Care. 2019;50:59-65.
.
FROM THE JOURNAL OF CRITICAL CARE
Key clinical point:
Major finding: Flu patients in the ICU more frequently had a history of obstructive/central sleep apnea syndrome (11% vs. 3%; P = .03) and MI (20% vs. 6%; P = .007), compared with non-ICU flu patients.
Study details: A retrospective cohort study of 199 flu patients who were admitted to two academic hospitals in the Netherlands.
Disclosures: The authors reported no conflicts of interest.
Source: Beumer MC et al. J Crit Care. 2019; 50:59-65.