User login
Providing Extraordinary Availability
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
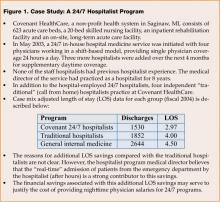
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
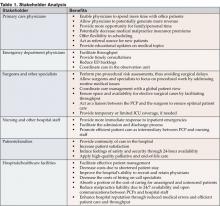
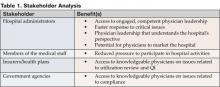
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
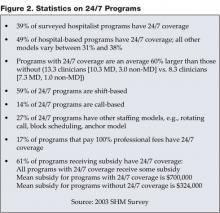
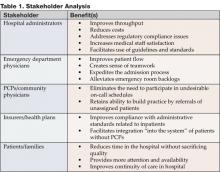
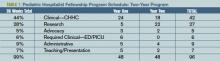
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
Leading Hospital Medical Staffs
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
Improving Physician's Practices
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Treating Unassigned Patients
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.
Introduction from the Editor
As editor of this supplement to The Hospitalist, I would like to introduce these eight papers prepared by the SHM Benchmarks Committee by identifying the unifying themes and consistent messages.
In all of the papers, the value provided by hospitalists comes across loud and clear. The authors not only cite statistics and published research studies, they provide examples and quotes from acknowledged hospitalist experts and leaders. However, perhaps more importantly, the papers convey a strong rationale as to WHY hospitalist programs provide value. Figure 1 attempts to describe this rationale. It depicts three elements:
- The characteristics of hospitalists: These are immutable attributes that uniquely define this new physician specialty.
- The expertise of hospitalists: As they practice hospital medicine, hospitalists have developed a unique combination of knowledge, skills, and relationships
- The value added by hospitalists: Hospitalists impact a wide range of issues that address the patient care, financial, and strategic goals of the hospital.
The Characteristics of Hospitalists
What attributes differentiate hospitalists from other medical specialties?
The first attribute describes what hospitalists do: they practice hospital medicine; for the most part, hospitalists have an inpatient practice. Their day consists of admitting, rounding, managing, discharging, and consulting for hospitalized patients.
The second attribute describes where hospitalists practice; they have a consistent presence in the hospital. As a consequence, hospitalists do similar things and relate to the same people in the same place on a daily basis.
The third attribute describes how hospitalists are organized. A hospitalist program is a cohesive physician group, and like any other medical group, the members develop a common organizational identity, a consistent practice philosophy, and a balance of individual and communal goals.
The Expertise of Hospitalists
What skills, knowledge, and relationships are unique to the specialty of hospital medicine?
As inpatient generalists, hospitalists continually treat the most common reasons for admission, thus acquiring exceptional clinical knowledge of these conditions and issues involved in managing patients with multiple co-morbidities. In addition, hospitalists are familiar with the clinical tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have impatient clinical skills, including diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination and oversight, and the performance of technical procedures.
Through their constant presence in the hospital, hospitalists develop exceptional organizational knowledge and relationships. They are quite familiar with the flow of patients through their hospital, including hospital processes, procedures, rules, regulations, and information systems. They understand "how to get things done" in their facility and often have good relationships with other healthcare professionals and hospital departments.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of healthcare industry issues. These include comprehension of the payer/insurance rules, state and Federal regulations, public health initiatives, recently enacted or pending healthcare legislation, and financial issues facing their hospital.
The Value Added by Hospitalists
How do hospitalists add value to the major stakeholders in the healthcare industry: hospitals, physicians, and health plans?
Each of the eight papers describes a different dimension of the benefits provided by hospital medicine programs.
First, hospitalists provide an effective solution to hospital that are having a difficult time organizing their medical staff to provide on-call coverage for unassigned patient care, both in the ED and subsequent to admission.
A second issue of concern for hospitals relates to the fact that many physicians are no longer able or willing to serve on hospital committees or play a medical staff leadership role. Hospitalists have emerged as strong candidates to play this role in their hospitals.
Third, hospitalists provide value by helping to improve physician practices, including primary care physicians, surgeons, emergency physicians and specialists.
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. A fourth value added by hospitalists relates to the extraordinary coverage (24/7) provided by many hospital medicine programs.
The dominant challenge facing American hospitals relates to financial pressures. Published research studies have consistently documented that hospital medicine programs generate resource utilization savings.
Improved throughput management is a sixth value added by hospitalists. Many hospitals are operating at or close to capacity, creating a crisis of bed availability. Hospitalists are uniquely qualified to address these patient flow issues.
A seventh dimension of the value provided by hospitalists relates to the formal and informal education they provide. In a formal capacity, hospitalists are teachers of clinical and non-clinical inpatient skills to medical students, residents, and fellows. In an informal role, hospitalists impart knowledge to other physicians, healthcare professionals, patients, families, and hospital administrators.
Hospitalists make major contributions to the healthcare quality and patient safety, the eighth aspect of value added by this new specialty. Hospitalists can reduce medical errors, improve the process of care, and achieve better patient outcomes.
Conclusion
Hospital medicine has developed as a specialty with unique characteristics and expertise. Hospilalists have specialized skills, knowledge, and relationships that contribute value to hospitals, physicians, patients, and health plans. These benefits include and go significantly beyond the delivery of quality patient care to hospital inpatients. The hospital medicine specialty continues to grow at a significant rate because of the broad-based positive impact made by hospitalists.
Joseph A. Miller, Editor
Mr. Miller can be contacted at josephamiller@yahoo.com
As editor of this supplement to The Hospitalist, I would like to introduce these eight papers prepared by the SHM Benchmarks Committee by identifying the unifying themes and consistent messages.
In all of the papers, the value provided by hospitalists comes across loud and clear. The authors not only cite statistics and published research studies, they provide examples and quotes from acknowledged hospitalist experts and leaders. However, perhaps more importantly, the papers convey a strong rationale as to WHY hospitalist programs provide value. Figure 1 attempts to describe this rationale. It depicts three elements:
- The characteristics of hospitalists: These are immutable attributes that uniquely define this new physician specialty.
- The expertise of hospitalists: As they practice hospital medicine, hospitalists have developed a unique combination of knowledge, skills, and relationships
- The value added by hospitalists: Hospitalists impact a wide range of issues that address the patient care, financial, and strategic goals of the hospital.
The Characteristics of Hospitalists
What attributes differentiate hospitalists from other medical specialties?
The first attribute describes what hospitalists do: they practice hospital medicine; for the most part, hospitalists have an inpatient practice. Their day consists of admitting, rounding, managing, discharging, and consulting for hospitalized patients.
The second attribute describes where hospitalists practice; they have a consistent presence in the hospital. As a consequence, hospitalists do similar things and relate to the same people in the same place on a daily basis.
The third attribute describes how hospitalists are organized. A hospitalist program is a cohesive physician group, and like any other medical group, the members develop a common organizational identity, a consistent practice philosophy, and a balance of individual and communal goals.
The Expertise of Hospitalists
What skills, knowledge, and relationships are unique to the specialty of hospital medicine?
As inpatient generalists, hospitalists continually treat the most common reasons for admission, thus acquiring exceptional clinical knowledge of these conditions and issues involved in managing patients with multiple co-morbidities. In addition, hospitalists are familiar with the clinical tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have impatient clinical skills, including diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination and oversight, and the performance of technical procedures.
Through their constant presence in the hospital, hospitalists develop exceptional organizational knowledge and relationships. They are quite familiar with the flow of patients through their hospital, including hospital processes, procedures, rules, regulations, and information systems. They understand "how to get things done" in their facility and often have good relationships with other healthcare professionals and hospital departments.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of healthcare industry issues. These include comprehension of the payer/insurance rules, state and Federal regulations, public health initiatives, recently enacted or pending healthcare legislation, and financial issues facing their hospital.
The Value Added by Hospitalists
How do hospitalists add value to the major stakeholders in the healthcare industry: hospitals, physicians, and health plans?
Each of the eight papers describes a different dimension of the benefits provided by hospital medicine programs.
First, hospitalists provide an effective solution to hospital that are having a difficult time organizing their medical staff to provide on-call coverage for unassigned patient care, both in the ED and subsequent to admission.
A second issue of concern for hospitals relates to the fact that many physicians are no longer able or willing to serve on hospital committees or play a medical staff leadership role. Hospitalists have emerged as strong candidates to play this role in their hospitals.
Third, hospitalists provide value by helping to improve physician practices, including primary care physicians, surgeons, emergency physicians and specialists.
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. A fourth value added by hospitalists relates to the extraordinary coverage (24/7) provided by many hospital medicine programs.
The dominant challenge facing American hospitals relates to financial pressures. Published research studies have consistently documented that hospital medicine programs generate resource utilization savings.
Improved throughput management is a sixth value added by hospitalists. Many hospitals are operating at or close to capacity, creating a crisis of bed availability. Hospitalists are uniquely qualified to address these patient flow issues.
A seventh dimension of the value provided by hospitalists relates to the formal and informal education they provide. In a formal capacity, hospitalists are teachers of clinical and non-clinical inpatient skills to medical students, residents, and fellows. In an informal role, hospitalists impart knowledge to other physicians, healthcare professionals, patients, families, and hospital administrators.
Hospitalists make major contributions to the healthcare quality and patient safety, the eighth aspect of value added by this new specialty. Hospitalists can reduce medical errors, improve the process of care, and achieve better patient outcomes.
Conclusion
Hospital medicine has developed as a specialty with unique characteristics and expertise. Hospilalists have specialized skills, knowledge, and relationships that contribute value to hospitals, physicians, patients, and health plans. These benefits include and go significantly beyond the delivery of quality patient care to hospital inpatients. The hospital medicine specialty continues to grow at a significant rate because of the broad-based positive impact made by hospitalists.
Joseph A. Miller, Editor
Mr. Miller can be contacted at josephamiller@yahoo.com
As editor of this supplement to The Hospitalist, I would like to introduce these eight papers prepared by the SHM Benchmarks Committee by identifying the unifying themes and consistent messages.
In all of the papers, the value provided by hospitalists comes across loud and clear. The authors not only cite statistics and published research studies, they provide examples and quotes from acknowledged hospitalist experts and leaders. However, perhaps more importantly, the papers convey a strong rationale as to WHY hospitalist programs provide value. Figure 1 attempts to describe this rationale. It depicts three elements:
- The characteristics of hospitalists: These are immutable attributes that uniquely define this new physician specialty.
- The expertise of hospitalists: As they practice hospital medicine, hospitalists have developed a unique combination of knowledge, skills, and relationships
- The value added by hospitalists: Hospitalists impact a wide range of issues that address the patient care, financial, and strategic goals of the hospital.
The Characteristics of Hospitalists
What attributes differentiate hospitalists from other medical specialties?
The first attribute describes what hospitalists do: they practice hospital medicine; for the most part, hospitalists have an inpatient practice. Their day consists of admitting, rounding, managing, discharging, and consulting for hospitalized patients.
The second attribute describes where hospitalists practice; they have a consistent presence in the hospital. As a consequence, hospitalists do similar things and relate to the same people in the same place on a daily basis.
The third attribute describes how hospitalists are organized. A hospitalist program is a cohesive physician group, and like any other medical group, the members develop a common organizational identity, a consistent practice philosophy, and a balance of individual and communal goals.
The Expertise of Hospitalists
What skills, knowledge, and relationships are unique to the specialty of hospital medicine?
As inpatient generalists, hospitalists continually treat the most common reasons for admission, thus acquiring exceptional clinical knowledge of these conditions and issues involved in managing patients with multiple co-morbidities. In addition, hospitalists are familiar with the clinical tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have impatient clinical skills, including diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination and oversight, and the performance of technical procedures.
Through their constant presence in the hospital, hospitalists develop exceptional organizational knowledge and relationships. They are quite familiar with the flow of patients through their hospital, including hospital processes, procedures, rules, regulations, and information systems. They understand "how to get things done" in their facility and often have good relationships with other healthcare professionals and hospital departments.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of healthcare industry issues. These include comprehension of the payer/insurance rules, state and Federal regulations, public health initiatives, recently enacted or pending healthcare legislation, and financial issues facing their hospital.
The Value Added by Hospitalists
How do hospitalists add value to the major stakeholders in the healthcare industry: hospitals, physicians, and health plans?
Each of the eight papers describes a different dimension of the benefits provided by hospital medicine programs.
First, hospitalists provide an effective solution to hospital that are having a difficult time organizing their medical staff to provide on-call coverage for unassigned patient care, both in the ED and subsequent to admission.
A second issue of concern for hospitals relates to the fact that many physicians are no longer able or willing to serve on hospital committees or play a medical staff leadership role. Hospitalists have emerged as strong candidates to play this role in their hospitals.
Third, hospitalists provide value by helping to improve physician practices, including primary care physicians, surgeons, emergency physicians and specialists.
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. A fourth value added by hospitalists relates to the extraordinary coverage (24/7) provided by many hospital medicine programs.
The dominant challenge facing American hospitals relates to financial pressures. Published research studies have consistently documented that hospital medicine programs generate resource utilization savings.
Improved throughput management is a sixth value added by hospitalists. Many hospitals are operating at or close to capacity, creating a crisis of bed availability. Hospitalists are uniquely qualified to address these patient flow issues.
A seventh dimension of the value provided by hospitalists relates to the formal and informal education they provide. In a formal capacity, hospitalists are teachers of clinical and non-clinical inpatient skills to medical students, residents, and fellows. In an informal role, hospitalists impart knowledge to other physicians, healthcare professionals, patients, families, and hospital administrators.
Hospitalists make major contributions to the healthcare quality and patient safety, the eighth aspect of value added by this new specialty. Hospitalists can reduce medical errors, improve the process of care, and achieve better patient outcomes.
Conclusion
Hospital medicine has developed as a specialty with unique characteristics and expertise. Hospilalists have specialized skills, knowledge, and relationships that contribute value to hospitals, physicians, patients, and health plans. These benefits include and go significantly beyond the delivery of quality patient care to hospital inpatients. The hospital medicine specialty continues to grow at a significant rate because of the broad-based positive impact made by hospitalists.
Joseph A. Miller, Editor
Mr. Miller can be contacted at josephamiller@yahoo.com
The Future Role of Hospitalists
Since the mid 1990s when Robert Wachter and Lee Goldman first coined the term ''hospitalist',' we have seen the nation's hospitals and health systems open their doors to these ''specialists in inpatient medicine'' (1). We have also seen publications and academic studies that outline the benefits of implementing hospitalist programs. As the CEO of an integrated delivery system, I can recount firsthand how our hospitalist program, in existence since 1995, has improved patient care in our facilities. Not only have our hospitalists saved the system thousands of days in length of stay and reduced our costs per day, but they have also improved quality of care. In addition, members of our hospitalist groups have emerged as physician liaisons, championing education and training initiatives and serving as a bridge between the medical staff and management.
As our experience and the articles included in this supplement suggest, hospitalists add value on multiple levels and have imbedded a new model of care within the nation's hospitals. What's next? How will hospitalists continue to improve the comprehensiveness and continuity of healthcare across the patient care continuum? And, perhaps more importantly, how do we get there from here?
While hospitalist programs are burgeoning, many hospitals and health systems have yet to realize the full value added by hospitalist programs. As it relates to the healthcare industry, hospitalist programs are still in their infancy. Early adopters continue to refine and modify program models to meet changing physician and patient needs as well as to decrease the financial cost to the hospital. In addition, preliminary results of an AHA study (2) on hospitalist programs suggest that larger hospitals have a higher probability of having a hospitalist program than smaller hospitals. The same study also suggests that hospitalists have a greater impact on smaller hospitals. As a result, the population of hospitals that benefits the most from hospitalist programs has barely begun to realize the value of such programs. The message is the same for both early and late adopters. ''When you come to the fork in the road, take it'' (Yogi Berra).
In looking farther to the future, one role that hospitalists may increasingly assume is that of change agent. In August 2004, Robert Wachter gave an interview to Health Leaders describing how hospitalists can "contribute to the notion of changing systems'' (3). In the article, The Emerging Role of ''hospitalists" in the American Health Care System, Wachter and Goldman explain that the hospitalist model "creates a core group of faculty members whose inpatient work is more than a marginal activity and who are thus committed to quality improvement in the hospital'' (1). As the work of hospitalists generates from within the hospital, they have a personal stake in the hospital systems and the improvement of these systems (1). The nature of the hospitalist’s work ideally situates him to act as a change agent, enabling him to identify process improvement initiatives and corral physician support. As a result, hospitalists will increasingly serve as administrative partners and leaders of medical staff initiatives to help facilitate organizational change.
In addition to serving as change agents, hospitalists themselves may become the solution to some of the systems that need changing. They are already helping to solve on-call challenges by providing 24/7 coverage and by taking call. Hospitalists have also assumed a greater role in caring for patients in the ED by managing patients that otherwise would have been admitted by on-call medicine physicians. As more and more physicians decrease the time they spend in the hospital and as more patients are admitted with chronic care needs, the hospitalist will play an integral role in meeting these challenges.
Hospitalists may also become more involved in providing continuity to the delivery of healthcare services. Consider the opportunities that exist to involve hospitalists in improving preoperative and postoperative patient care. For example, hospitalists could play a role in the management of patients who require perioperative beta-blockers to decrease cardiac events in major non-cardiac surgery. Hospitalists may also continue to diversify their clinical roles by coordinating care in ICUs where intensivists are unavailable or by caring for patients in post-acute settings (4,5).
With the ability to manage varying aspects of a patient's care, hospitalists can help resolve the disconnect that exists as a patient moves across the continuum of care. A patient may enter the system through the ICU, followed by a transfer to a Medicine Unit, and then be discharged to his primary care physician or a nursing home. The reality of ineffective communication and incomplete hand-offs may result in poor information exchange that impacts the care of the patient. By involving a hospitalist in this process, the coordination of patient care becomes seamless and the chance for medical error decreases.
In order to expand the current hospitalist model to the clinically diverse and dynamic model of the future, all stakeholders, from management to physicians, must take proactive steps. Part of this process will involve the development of an economic model that accounts for the value that hospitalist programs bring. The more quantifiable these programs become, the easier it will be to prove their value and implement them in capital-strapped facilities. Another part of moving the hospitalist model to the future centers on relationship management. A lack of understanding of the benefits that hospitalists provide and the roles that they assume in hospitals prevents collaboration with other specialties. Lines of communication must be opened and issues of distrust resolved to facilitate the relationship between hospitalists, the medical staff, and management. Finally we must educate the community about the benefits of hospitalists in the delivery of patient care. The success of hospitalist programs is just as dependent on the development of an external support network as it is on the existence of a strong internal infrastructure.
Without a doubt, hospitalists add value to our nation's hospitals. An exciting debate is emerging about how hospitalists will continue to change the model of healthcare as we know it, and what implications this will have for our hospitals and health systems.
References
- Wachter RM Goldman L. The emerging role of ''hospitalists'' in the American healthcare system. N Engl J Med. 1996;335:514-7.
- 2003 American Hospital Association (AHA) Annual Survey (preliminary results)
- Olsen K, Wachter R. The word on medical mistakes. Healthleaders News. Aug 20, 2004.
- Pham HH, Devers K, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-7.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
Since the mid 1990s when Robert Wachter and Lee Goldman first coined the term ''hospitalist',' we have seen the nation's hospitals and health systems open their doors to these ''specialists in inpatient medicine'' (1). We have also seen publications and academic studies that outline the benefits of implementing hospitalist programs. As the CEO of an integrated delivery system, I can recount firsthand how our hospitalist program, in existence since 1995, has improved patient care in our facilities. Not only have our hospitalists saved the system thousands of days in length of stay and reduced our costs per day, but they have also improved quality of care. In addition, members of our hospitalist groups have emerged as physician liaisons, championing education and training initiatives and serving as a bridge between the medical staff and management.
As our experience and the articles included in this supplement suggest, hospitalists add value on multiple levels and have imbedded a new model of care within the nation's hospitals. What's next? How will hospitalists continue to improve the comprehensiveness and continuity of healthcare across the patient care continuum? And, perhaps more importantly, how do we get there from here?
While hospitalist programs are burgeoning, many hospitals and health systems have yet to realize the full value added by hospitalist programs. As it relates to the healthcare industry, hospitalist programs are still in their infancy. Early adopters continue to refine and modify program models to meet changing physician and patient needs as well as to decrease the financial cost to the hospital. In addition, preliminary results of an AHA study (2) on hospitalist programs suggest that larger hospitals have a higher probability of having a hospitalist program than smaller hospitals. The same study also suggests that hospitalists have a greater impact on smaller hospitals. As a result, the population of hospitals that benefits the most from hospitalist programs has barely begun to realize the value of such programs. The message is the same for both early and late adopters. ''When you come to the fork in the road, take it'' (Yogi Berra).
In looking farther to the future, one role that hospitalists may increasingly assume is that of change agent. In August 2004, Robert Wachter gave an interview to Health Leaders describing how hospitalists can "contribute to the notion of changing systems'' (3). In the article, The Emerging Role of ''hospitalists" in the American Health Care System, Wachter and Goldman explain that the hospitalist model "creates a core group of faculty members whose inpatient work is more than a marginal activity and who are thus committed to quality improvement in the hospital'' (1). As the work of hospitalists generates from within the hospital, they have a personal stake in the hospital systems and the improvement of these systems (1). The nature of the hospitalist’s work ideally situates him to act as a change agent, enabling him to identify process improvement initiatives and corral physician support. As a result, hospitalists will increasingly serve as administrative partners and leaders of medical staff initiatives to help facilitate organizational change.
In addition to serving as change agents, hospitalists themselves may become the solution to some of the systems that need changing. They are already helping to solve on-call challenges by providing 24/7 coverage and by taking call. Hospitalists have also assumed a greater role in caring for patients in the ED by managing patients that otherwise would have been admitted by on-call medicine physicians. As more and more physicians decrease the time they spend in the hospital and as more patients are admitted with chronic care needs, the hospitalist will play an integral role in meeting these challenges.
Hospitalists may also become more involved in providing continuity to the delivery of healthcare services. Consider the opportunities that exist to involve hospitalists in improving preoperative and postoperative patient care. For example, hospitalists could play a role in the management of patients who require perioperative beta-blockers to decrease cardiac events in major non-cardiac surgery. Hospitalists may also continue to diversify their clinical roles by coordinating care in ICUs where intensivists are unavailable or by caring for patients in post-acute settings (4,5).
With the ability to manage varying aspects of a patient's care, hospitalists can help resolve the disconnect that exists as a patient moves across the continuum of care. A patient may enter the system through the ICU, followed by a transfer to a Medicine Unit, and then be discharged to his primary care physician or a nursing home. The reality of ineffective communication and incomplete hand-offs may result in poor information exchange that impacts the care of the patient. By involving a hospitalist in this process, the coordination of patient care becomes seamless and the chance for medical error decreases.
In order to expand the current hospitalist model to the clinically diverse and dynamic model of the future, all stakeholders, from management to physicians, must take proactive steps. Part of this process will involve the development of an economic model that accounts for the value that hospitalist programs bring. The more quantifiable these programs become, the easier it will be to prove their value and implement them in capital-strapped facilities. Another part of moving the hospitalist model to the future centers on relationship management. A lack of understanding of the benefits that hospitalists provide and the roles that they assume in hospitals prevents collaboration with other specialties. Lines of communication must be opened and issues of distrust resolved to facilitate the relationship between hospitalists, the medical staff, and management. Finally we must educate the community about the benefits of hospitalists in the delivery of patient care. The success of hospitalist programs is just as dependent on the development of an external support network as it is on the existence of a strong internal infrastructure.
Without a doubt, hospitalists add value to our nation's hospitals. An exciting debate is emerging about how hospitalists will continue to change the model of healthcare as we know it, and what implications this will have for our hospitals and health systems.
References
- Wachter RM Goldman L. The emerging role of ''hospitalists'' in the American healthcare system. N Engl J Med. 1996;335:514-7.
- 2003 American Hospital Association (AHA) Annual Survey (preliminary results)
- Olsen K, Wachter R. The word on medical mistakes. Healthleaders News. Aug 20, 2004.
- Pham HH, Devers K, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-7.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
Since the mid 1990s when Robert Wachter and Lee Goldman first coined the term ''hospitalist',' we have seen the nation's hospitals and health systems open their doors to these ''specialists in inpatient medicine'' (1). We have also seen publications and academic studies that outline the benefits of implementing hospitalist programs. As the CEO of an integrated delivery system, I can recount firsthand how our hospitalist program, in existence since 1995, has improved patient care in our facilities. Not only have our hospitalists saved the system thousands of days in length of stay and reduced our costs per day, but they have also improved quality of care. In addition, members of our hospitalist groups have emerged as physician liaisons, championing education and training initiatives and serving as a bridge between the medical staff and management.
As our experience and the articles included in this supplement suggest, hospitalists add value on multiple levels and have imbedded a new model of care within the nation's hospitals. What's next? How will hospitalists continue to improve the comprehensiveness and continuity of healthcare across the patient care continuum? And, perhaps more importantly, how do we get there from here?
While hospitalist programs are burgeoning, many hospitals and health systems have yet to realize the full value added by hospitalist programs. As it relates to the healthcare industry, hospitalist programs are still in their infancy. Early adopters continue to refine and modify program models to meet changing physician and patient needs as well as to decrease the financial cost to the hospital. In addition, preliminary results of an AHA study (2) on hospitalist programs suggest that larger hospitals have a higher probability of having a hospitalist program than smaller hospitals. The same study also suggests that hospitalists have a greater impact on smaller hospitals. As a result, the population of hospitals that benefits the most from hospitalist programs has barely begun to realize the value of such programs. The message is the same for both early and late adopters. ''When you come to the fork in the road, take it'' (Yogi Berra).
In looking farther to the future, one role that hospitalists may increasingly assume is that of change agent. In August 2004, Robert Wachter gave an interview to Health Leaders describing how hospitalists can "contribute to the notion of changing systems'' (3). In the article, The Emerging Role of ''hospitalists" in the American Health Care System, Wachter and Goldman explain that the hospitalist model "creates a core group of faculty members whose inpatient work is more than a marginal activity and who are thus committed to quality improvement in the hospital'' (1). As the work of hospitalists generates from within the hospital, they have a personal stake in the hospital systems and the improvement of these systems (1). The nature of the hospitalist’s work ideally situates him to act as a change agent, enabling him to identify process improvement initiatives and corral physician support. As a result, hospitalists will increasingly serve as administrative partners and leaders of medical staff initiatives to help facilitate organizational change.
In addition to serving as change agents, hospitalists themselves may become the solution to some of the systems that need changing. They are already helping to solve on-call challenges by providing 24/7 coverage and by taking call. Hospitalists have also assumed a greater role in caring for patients in the ED by managing patients that otherwise would have been admitted by on-call medicine physicians. As more and more physicians decrease the time they spend in the hospital and as more patients are admitted with chronic care needs, the hospitalist will play an integral role in meeting these challenges.
Hospitalists may also become more involved in providing continuity to the delivery of healthcare services. Consider the opportunities that exist to involve hospitalists in improving preoperative and postoperative patient care. For example, hospitalists could play a role in the management of patients who require perioperative beta-blockers to decrease cardiac events in major non-cardiac surgery. Hospitalists may also continue to diversify their clinical roles by coordinating care in ICUs where intensivists are unavailable or by caring for patients in post-acute settings (4,5).
With the ability to manage varying aspects of a patient's care, hospitalists can help resolve the disconnect that exists as a patient moves across the continuum of care. A patient may enter the system through the ICU, followed by a transfer to a Medicine Unit, and then be discharged to his primary care physician or a nursing home. The reality of ineffective communication and incomplete hand-offs may result in poor information exchange that impacts the care of the patient. By involving a hospitalist in this process, the coordination of patient care becomes seamless and the chance for medical error decreases.
In order to expand the current hospitalist model to the clinically diverse and dynamic model of the future, all stakeholders, from management to physicians, must take proactive steps. Part of this process will involve the development of an economic model that accounts for the value that hospitalist programs bring. The more quantifiable these programs become, the easier it will be to prove their value and implement them in capital-strapped facilities. Another part of moving the hospitalist model to the future centers on relationship management. A lack of understanding of the benefits that hospitalists provide and the roles that they assume in hospitals prevents collaboration with other specialties. Lines of communication must be opened and issues of distrust resolved to facilitate the relationship between hospitalists, the medical staff, and management. Finally we must educate the community about the benefits of hospitalists in the delivery of patient care. The success of hospitalist programs is just as dependent on the development of an external support network as it is on the existence of a strong internal infrastructure.
Without a doubt, hospitalists add value to our nation's hospitals. An exciting debate is emerging about how hospitalists will continue to change the model of healthcare as we know it, and what implications this will have for our hospitals and health systems.
References
- Wachter RM Goldman L. The emerging role of ''hospitalists'' in the American healthcare system. N Engl J Med. 1996;335:514-7.
- 2003 American Hospital Association (AHA) Annual Survey (preliminary results)
- Olsen K, Wachter R. The word on medical mistakes. Healthleaders News. Aug 20, 2004.
- Pham HH, Devers K, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-7.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
Publication as Patient
I was in my office perusing patient records when I got the call. I’d been selected to be the new Physician Editor of The Hospitalist. I felt surprised—and excited. Then, harsh reality set in: My first deadline was only three weeks away. I checked my pulse—117 and irregularly irregular, good. I brewed some foxglove tea, chewed on some willow bark, and prepared to work.
Deja Vu
I found myself experiencing an unusual sensation. What was the emotion I was feeling? A fine mixture of dread and excitement, with an overlay of angst. I’d had this sensation before, but when?
I looked at the May issue of The Hospitalist. How was I going to continue to produce a quality publication—and improve upon it? The people who had supported my selection as editor were counting on me; my mom was counting on me. Heck, even I was even counting on me.
I drew a blank. Where would I go with this? That’s when it hit me: the sense of being in a situation that I wanted, only to discover I wasn’t ready. The tidal forces of time and pressure descended upon me.
In a flash I knew what was happening. I was suffering from delayed post-traumatic residency syndrome. It was 1985, and I was back in Houston’s old Ben Taub Hospital. (Reminiscing is a sure sign of early senescence.) I was the intern coming on service, a very busy general medicine service. Among my new patients, I had to pick up an elderly gentleman who had been ill for years and who had been in the hospital for more than a month. His chart was missing, he was unresponsive, and his family was AWOL.
My beeper kept going off. There was a code on the other side of the hospital, and the ED was calling. Should I give the patient heparin? How do I dose it? Should I give antibiotics and, if so, which ones? Should I draw blood cultures? My circuits totally overloaded.
My resident came to my rescue, with a cup of coffee and good advice: Settle down, find the old records, obtain a history, and perform a physical exam before I even thought about therapeutic intervention.
This was exactly what I needed to do as physician editor. I turned to my current resident-equivalent, in this case Lisa Dionne from John Wiley & Sons—the editorial Yang to my Yin. She gave me the same advice my resident had decades before: Get the back issues of The Hospitalist from SHM, see where it was going, where it had been, learn the terminology, and get organized. Luckily the SHM staff is a lot more responsive then the medical records department at Ben Taub was.
Then, as with any patient, I had to ask some basic questions. What initial symptoms caused the development of The Hospitalist? How long had the publication been present? What made it better, and what made it worse? Was it progressing or was it unchanged? Was I having chest pain? What was SHM, and why did it exist? What did a hospitalist want to read? What was a hospitalist, and why would anyone want to be one?
Why I’m a Hospitalist
That final question seemed the heart of my issue. I pondered what forces drove me to become a hospitalist and why I enjoyed it so much.
When I finished my residency I went into private practice. Like most residents of the time I was totally unprepared for ambulatory care. I could run a code, knew all the latest diagnostic tests, and could even quote a few articles.
But the first time I saw a young man with chronic back pain who wanted to go on disability, or an elderly lady with osteoporosis and breast cancer who wondered if she could take quinine for leg cramps, I was lost. It only took a decade or two for me to feel vaguely competent. Meantime I did some hard time in the hospital, but my focus shifted tectonically toward the outpatient. When my running partner Mitchell Wilson decided to start one of the early hospitalist programs (at the University of Texas) my hospital time ever more rapidly receded.
At the same time, the forces of capitalism were at work: IPAs and IPOs, practice management groups, university expansions and contractions, hospital closings. This was the new shifting sand (or shifting dullness) of medical practice. I was ready for a change, but could I give up my comfortably cluttered office, my established, fairly well-tuned patients, my six-year-old National Geographic magazines in the waiting room? Would going back to the hospital feel like being a resident again? There was only one way to find out.
I said goodbye to the beach and the fire ants, loaded my truck like Jed Clampett, and moved to Rochester—Minn., that is—frozen tundra, lots of geese. Under the auspices of Jeanne Huddleston and the Mayo Clinic Inpatient Internal Medicine Team, I joined the world of hospitalists.
New Beginnings
My first impression of life as a hospitalist was that I was cold. Frigid really. Of course it was winter in Minnesota, so I guess I should have expected that. I rapidly discovered that it was a lot nicer being a member of the consulting staff than a member of the house staff. In some ways I felt like an intern again. It was difficult to believe, but hospital medicine had changed over the last decade or two; however, the patients hadn’t.
I was armed with acceptable history taking and exam skills. I had a superb support system in the nurse practitioners and physician assistants who carried my load the first few weeks. My colleagues were supportive. I muddled through and, after several years, felt like I was back to my baseline level of moderate competence.
Though my story is immensely fascinating (to me) from an autobiographical standpoint, does it answer the question of why I enjoy being a hospitalist? Usually people ask me, “What is a hospitalist?” I usually explain that I’m an internist—not an intern—though some days I feel like the latter. The taxonomy of hospitalists is fairly diverse. Some of us come straight from residency, for others it’s the resolution of a mid-career crisis.
One of my favorite things about being a hospitalist is the control I have over my schedule. As an outpatient doctor I had a timetable to keep based on the waiting patient. If I got behind, waxed conversational, or got involved with a family, my day was ruined. Patients got mad at me; my nurses were aggravated.
In the hospital, I have a body of work I must do each day. It’s predictably unpredictable at the beginning of the shift. I have a certain number of patients to see, discharge, and admit. I risk acute medical emergencies, unexpected families who want an update on their mother’s condition, and similar hospitalist activities of daily life (aka HADLs). The volume of work is variable: Some days are difficult, some aren’t. The complexity of cases is stimulating and makes continued learning a necessity. Instead of being isolated in an office I interact with other physicians and staff. The most stimulating aspect I experience is the sensation that hospital medicine is an evolving field and there are hundreds of dedicated colleagues out there trying to make it better.
My goal as physician editor is to work with SHM members to continue to produce a great source of hospitalist information. The Hospitalist readers include internists, family practitioners, pediatricians, nurse practitioners, and physician assistants. They also comprise administrators, businesspeople, and legislators. I perceive important topics to involve medical management, education, communication, economics, government regulation, ethics, and palliative care, as well as the activities of our society, chapters, and members.
With the team from John Wiley & Sons and the support of SHM administration and the members, I hope to accomplish this task. My patient all those years ago survived and left the hospital. I only can hope that The Hospitalist will thrive as well. TH
Jamie Newman, MD, FACP, is senior associate consultant, Hospital Internal Medicine, associate professor of internal medicine and medical history, Mayo Clinic College of Medicine at the Mayo Clinic College of Medicine, Rochester, Minn.
I was in my office perusing patient records when I got the call. I’d been selected to be the new Physician Editor of The Hospitalist. I felt surprised—and excited. Then, harsh reality set in: My first deadline was only three weeks away. I checked my pulse—117 and irregularly irregular, good. I brewed some foxglove tea, chewed on some willow bark, and prepared to work.
Deja Vu
I found myself experiencing an unusual sensation. What was the emotion I was feeling? A fine mixture of dread and excitement, with an overlay of angst. I’d had this sensation before, but when?
I looked at the May issue of The Hospitalist. How was I going to continue to produce a quality publication—and improve upon it? The people who had supported my selection as editor were counting on me; my mom was counting on me. Heck, even I was even counting on me.
I drew a blank. Where would I go with this? That’s when it hit me: the sense of being in a situation that I wanted, only to discover I wasn’t ready. The tidal forces of time and pressure descended upon me.
In a flash I knew what was happening. I was suffering from delayed post-traumatic residency syndrome. It was 1985, and I was back in Houston’s old Ben Taub Hospital. (Reminiscing is a sure sign of early senescence.) I was the intern coming on service, a very busy general medicine service. Among my new patients, I had to pick up an elderly gentleman who had been ill for years and who had been in the hospital for more than a month. His chart was missing, he was unresponsive, and his family was AWOL.
My beeper kept going off. There was a code on the other side of the hospital, and the ED was calling. Should I give the patient heparin? How do I dose it? Should I give antibiotics and, if so, which ones? Should I draw blood cultures? My circuits totally overloaded.
My resident came to my rescue, with a cup of coffee and good advice: Settle down, find the old records, obtain a history, and perform a physical exam before I even thought about therapeutic intervention.
This was exactly what I needed to do as physician editor. I turned to my current resident-equivalent, in this case Lisa Dionne from John Wiley & Sons—the editorial Yang to my Yin. She gave me the same advice my resident had decades before: Get the back issues of The Hospitalist from SHM, see where it was going, where it had been, learn the terminology, and get organized. Luckily the SHM staff is a lot more responsive then the medical records department at Ben Taub was.
Then, as with any patient, I had to ask some basic questions. What initial symptoms caused the development of The Hospitalist? How long had the publication been present? What made it better, and what made it worse? Was it progressing or was it unchanged? Was I having chest pain? What was SHM, and why did it exist? What did a hospitalist want to read? What was a hospitalist, and why would anyone want to be one?
Why I’m a Hospitalist
That final question seemed the heart of my issue. I pondered what forces drove me to become a hospitalist and why I enjoyed it so much.
When I finished my residency I went into private practice. Like most residents of the time I was totally unprepared for ambulatory care. I could run a code, knew all the latest diagnostic tests, and could even quote a few articles.
But the first time I saw a young man with chronic back pain who wanted to go on disability, or an elderly lady with osteoporosis and breast cancer who wondered if she could take quinine for leg cramps, I was lost. It only took a decade or two for me to feel vaguely competent. Meantime I did some hard time in the hospital, but my focus shifted tectonically toward the outpatient. When my running partner Mitchell Wilson decided to start one of the early hospitalist programs (at the University of Texas) my hospital time ever more rapidly receded.
At the same time, the forces of capitalism were at work: IPAs and IPOs, practice management groups, university expansions and contractions, hospital closings. This was the new shifting sand (or shifting dullness) of medical practice. I was ready for a change, but could I give up my comfortably cluttered office, my established, fairly well-tuned patients, my six-year-old National Geographic magazines in the waiting room? Would going back to the hospital feel like being a resident again? There was only one way to find out.
I said goodbye to the beach and the fire ants, loaded my truck like Jed Clampett, and moved to Rochester—Minn., that is—frozen tundra, lots of geese. Under the auspices of Jeanne Huddleston and the Mayo Clinic Inpatient Internal Medicine Team, I joined the world of hospitalists.
New Beginnings
My first impression of life as a hospitalist was that I was cold. Frigid really. Of course it was winter in Minnesota, so I guess I should have expected that. I rapidly discovered that it was a lot nicer being a member of the consulting staff than a member of the house staff. In some ways I felt like an intern again. It was difficult to believe, but hospital medicine had changed over the last decade or two; however, the patients hadn’t.
I was armed with acceptable history taking and exam skills. I had a superb support system in the nurse practitioners and physician assistants who carried my load the first few weeks. My colleagues were supportive. I muddled through and, after several years, felt like I was back to my baseline level of moderate competence.
Though my story is immensely fascinating (to me) from an autobiographical standpoint, does it answer the question of why I enjoy being a hospitalist? Usually people ask me, “What is a hospitalist?” I usually explain that I’m an internist—not an intern—though some days I feel like the latter. The taxonomy of hospitalists is fairly diverse. Some of us come straight from residency, for others it’s the resolution of a mid-career crisis.
One of my favorite things about being a hospitalist is the control I have over my schedule. As an outpatient doctor I had a timetable to keep based on the waiting patient. If I got behind, waxed conversational, or got involved with a family, my day was ruined. Patients got mad at me; my nurses were aggravated.
In the hospital, I have a body of work I must do each day. It’s predictably unpredictable at the beginning of the shift. I have a certain number of patients to see, discharge, and admit. I risk acute medical emergencies, unexpected families who want an update on their mother’s condition, and similar hospitalist activities of daily life (aka HADLs). The volume of work is variable: Some days are difficult, some aren’t. The complexity of cases is stimulating and makes continued learning a necessity. Instead of being isolated in an office I interact with other physicians and staff. The most stimulating aspect I experience is the sensation that hospital medicine is an evolving field and there are hundreds of dedicated colleagues out there trying to make it better.
My goal as physician editor is to work with SHM members to continue to produce a great source of hospitalist information. The Hospitalist readers include internists, family practitioners, pediatricians, nurse practitioners, and physician assistants. They also comprise administrators, businesspeople, and legislators. I perceive important topics to involve medical management, education, communication, economics, government regulation, ethics, and palliative care, as well as the activities of our society, chapters, and members.
With the team from John Wiley & Sons and the support of SHM administration and the members, I hope to accomplish this task. My patient all those years ago survived and left the hospital. I only can hope that The Hospitalist will thrive as well. TH
Jamie Newman, MD, FACP, is senior associate consultant, Hospital Internal Medicine, associate professor of internal medicine and medical history, Mayo Clinic College of Medicine at the Mayo Clinic College of Medicine, Rochester, Minn.
I was in my office perusing patient records when I got the call. I’d been selected to be the new Physician Editor of The Hospitalist. I felt surprised—and excited. Then, harsh reality set in: My first deadline was only three weeks away. I checked my pulse—117 and irregularly irregular, good. I brewed some foxglove tea, chewed on some willow bark, and prepared to work.
Deja Vu
I found myself experiencing an unusual sensation. What was the emotion I was feeling? A fine mixture of dread and excitement, with an overlay of angst. I’d had this sensation before, but when?
I looked at the May issue of The Hospitalist. How was I going to continue to produce a quality publication—and improve upon it? The people who had supported my selection as editor were counting on me; my mom was counting on me. Heck, even I was even counting on me.
I drew a blank. Where would I go with this? That’s when it hit me: the sense of being in a situation that I wanted, only to discover I wasn’t ready. The tidal forces of time and pressure descended upon me.
In a flash I knew what was happening. I was suffering from delayed post-traumatic residency syndrome. It was 1985, and I was back in Houston’s old Ben Taub Hospital. (Reminiscing is a sure sign of early senescence.) I was the intern coming on service, a very busy general medicine service. Among my new patients, I had to pick up an elderly gentleman who had been ill for years and who had been in the hospital for more than a month. His chart was missing, he was unresponsive, and his family was AWOL.
My beeper kept going off. There was a code on the other side of the hospital, and the ED was calling. Should I give the patient heparin? How do I dose it? Should I give antibiotics and, if so, which ones? Should I draw blood cultures? My circuits totally overloaded.
My resident came to my rescue, with a cup of coffee and good advice: Settle down, find the old records, obtain a history, and perform a physical exam before I even thought about therapeutic intervention.
This was exactly what I needed to do as physician editor. I turned to my current resident-equivalent, in this case Lisa Dionne from John Wiley & Sons—the editorial Yang to my Yin. She gave me the same advice my resident had decades before: Get the back issues of The Hospitalist from SHM, see where it was going, where it had been, learn the terminology, and get organized. Luckily the SHM staff is a lot more responsive then the medical records department at Ben Taub was.
Then, as with any patient, I had to ask some basic questions. What initial symptoms caused the development of The Hospitalist? How long had the publication been present? What made it better, and what made it worse? Was it progressing or was it unchanged? Was I having chest pain? What was SHM, and why did it exist? What did a hospitalist want to read? What was a hospitalist, and why would anyone want to be one?
Why I’m a Hospitalist
That final question seemed the heart of my issue. I pondered what forces drove me to become a hospitalist and why I enjoyed it so much.
When I finished my residency I went into private practice. Like most residents of the time I was totally unprepared for ambulatory care. I could run a code, knew all the latest diagnostic tests, and could even quote a few articles.
But the first time I saw a young man with chronic back pain who wanted to go on disability, or an elderly lady with osteoporosis and breast cancer who wondered if she could take quinine for leg cramps, I was lost. It only took a decade or two for me to feel vaguely competent. Meantime I did some hard time in the hospital, but my focus shifted tectonically toward the outpatient. When my running partner Mitchell Wilson decided to start one of the early hospitalist programs (at the University of Texas) my hospital time ever more rapidly receded.
At the same time, the forces of capitalism were at work: IPAs and IPOs, practice management groups, university expansions and contractions, hospital closings. This was the new shifting sand (or shifting dullness) of medical practice. I was ready for a change, but could I give up my comfortably cluttered office, my established, fairly well-tuned patients, my six-year-old National Geographic magazines in the waiting room? Would going back to the hospital feel like being a resident again? There was only one way to find out.
I said goodbye to the beach and the fire ants, loaded my truck like Jed Clampett, and moved to Rochester—Minn., that is—frozen tundra, lots of geese. Under the auspices of Jeanne Huddleston and the Mayo Clinic Inpatient Internal Medicine Team, I joined the world of hospitalists.
New Beginnings
My first impression of life as a hospitalist was that I was cold. Frigid really. Of course it was winter in Minnesota, so I guess I should have expected that. I rapidly discovered that it was a lot nicer being a member of the consulting staff than a member of the house staff. In some ways I felt like an intern again. It was difficult to believe, but hospital medicine had changed over the last decade or two; however, the patients hadn’t.
I was armed with acceptable history taking and exam skills. I had a superb support system in the nurse practitioners and physician assistants who carried my load the first few weeks. My colleagues were supportive. I muddled through and, after several years, felt like I was back to my baseline level of moderate competence.
Though my story is immensely fascinating (to me) from an autobiographical standpoint, does it answer the question of why I enjoy being a hospitalist? Usually people ask me, “What is a hospitalist?” I usually explain that I’m an internist—not an intern—though some days I feel like the latter. The taxonomy of hospitalists is fairly diverse. Some of us come straight from residency, for others it’s the resolution of a mid-career crisis.
One of my favorite things about being a hospitalist is the control I have over my schedule. As an outpatient doctor I had a timetable to keep based on the waiting patient. If I got behind, waxed conversational, or got involved with a family, my day was ruined. Patients got mad at me; my nurses were aggravated.
In the hospital, I have a body of work I must do each day. It’s predictably unpredictable at the beginning of the shift. I have a certain number of patients to see, discharge, and admit. I risk acute medical emergencies, unexpected families who want an update on their mother’s condition, and similar hospitalist activities of daily life (aka HADLs). The volume of work is variable: Some days are difficult, some aren’t. The complexity of cases is stimulating and makes continued learning a necessity. Instead of being isolated in an office I interact with other physicians and staff. The most stimulating aspect I experience is the sensation that hospital medicine is an evolving field and there are hundreds of dedicated colleagues out there trying to make it better.
My goal as physician editor is to work with SHM members to continue to produce a great source of hospitalist information. The Hospitalist readers include internists, family practitioners, pediatricians, nurse practitioners, and physician assistants. They also comprise administrators, businesspeople, and legislators. I perceive important topics to involve medical management, education, communication, economics, government regulation, ethics, and palliative care, as well as the activities of our society, chapters, and members.
With the team from John Wiley & Sons and the support of SHM administration and the members, I hope to accomplish this task. My patient all those years ago survived and left the hospital. I only can hope that The Hospitalist will thrive as well. TH
Jamie Newman, MD, FACP, is senior associate consultant, Hospital Internal Medicine, associate professor of internal medicine and medical history, Mayo Clinic College of Medicine at the Mayo Clinic College of Medicine, Rochester, Minn.
Staph Endocarditis, METs, COPD CPGs & More
A review of staphylococcal Endocarditis
VG Fowler Jr, Miro JM, Hoen B, et al for the ICE Investigators. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005;June 22;293(24):3061-3062.
Agroup of infectious diseases experts from centers throughout the world formed the International Collaboration on Endocarditis (ICE) in 1999 to gain a global understanding of infective endocarditis. Using the Duke Criteria patients with definite infective endocarditis in a prospective manner, 275 variables were reported with these cases to a central database maintained at Duke University. The ICE-Prospective Cohort Study (ICE-PCS) enrolled 1,779 patients with infective endocarditis in 39 centers in 16 countries between June 15, 2000, and December 31, 2003, and has been described in a recent report. (Cabell CH, Abrutyn E. Infect Dis Clin North Am. 2002;16:255-72). Staphylococcus aureus was the most common cause of infective endocarditis in this group of patients (n=558; 31.6%); the authors characterized risk factors and clinical issues associated with these cases in this report.
By univariate analysis, compared with non-Staphylococcus aureus infective endocarditis, patients with infective endocarditis due to Staphylococcus aureus were more likely than patients with infective endocarditis due to other pathogens to be female (P<0.001), hemodialysis dependent (P<0.001), have diabetes mellitus (P=0.009), have other chronic illnesses (P<0.001), have a healthcare association (P<0.001), have higher rates of stroke (P<0.001), have systemic embolization (P<0.001), have persistent bacteremia (P<0.001), or die (P<0.001).
Although healthcare associated Staphylococcus aureus infective endocarditis was the most common form of Staphylococcus aureus infective endocarditis, more than 60% of healthcare-associated patients acquired the infection outside the hospital. This reflects the global trend in healthcare delivery patterns favoring ambulatory treatment (e.g., outpatient medication infusion via long-term IV access, hemodialysis)
Multivariate analysis, clinical features independently associated with Staphylococcus aureus infective endocarditis (versus non-Staphylococcus aureus infective endocarditis) were: IV drug use (OR, 9.3; 95% CI, 6.3-13.7); first clinical presentation less than one month after first symptoms (OR, 5.1; 95% CI, 3.2-8.2); healthcare-associated infection (OR, 2.9; 95% CI, 2.1-3.8), persistent bacteremia (OR, 2.3; 95% CI, 1.5-3.8), presence of a presumed intravascular device source (OR, 1.7; 95% CI, 1.2-2.6), stroke (OR, 1.6; 95% CI, 1.2-2.3), or diabetes mellitus (OR, 1.3; 95% CI, 1.1-1.8).
Patients from the United States with Staphylococcus aureus infective endocarditis were more likely to be hemodialysis-dependent, to be diabetic, to have a hemodialysis fistula or a chronic indwelling central catheter as a presumed source of infection, and to have a non-nosocomial healthcare association. Patients from the United States and Brazil were more likely to have Methicillin-resistant Staphyloccocus aureus (MRSA) than were patients from Europe, the Middle East, Australia, or New Zealand. In-hospital mortality rates were similar across regions, although American patients were significantly more likely to develop persistent bacteremia (25.6%, P<0.001).
Characteristics independently associated with mortality among patients with nonintravenous drug-use-associated Staphylococcus aureus infective endocarditis by multivariate analysis included stroke (OR, 3.67; 95% CI, 1.94-6.94), persistent bacteremia (OR, 3.06; 95% CI, 1.75-5.35), diagnosis in Southern Europe or the Middle East (OR, 3.21; 95% CI, 1.17-10.56).
This study establishes Staphylococcus aureus infective endocarditis as the leading cause of infective endocarditis in many regions of the world and spotlights the global emergence of healthcare contact as a risk factor for Staphylococcus aureus infective endocarditis. In a significant portion of these patients, an IV device was the presumed source of bacteremia; prosthetic cardiac devices (pacemakers, defibrillators, or prosthetic cardiac valves) were present in almost one-quarter of the patients.
MRSA was a significant cause of Staphylococcus aureus infective endocarditis and displayed regional variation, accounting for almost 40% of the infective endocarditis caused by Staphylococcus aureus in some regions. Patients with infective endocarditis caused by MRSA were significantly more likely to have pre-existing chronic conditions and healthcare associated infective endocarditis by both univariate and multivariate analysis. They also were often associated with persistent bacteremia. On the other hand, 20% of patients with MRSA infective endocarditis developed their infection in the absence of identifiable healthcare contact.
Limitations of this report include the fact that this is an observational study of patients from self-selected centers. Each center most likely represents a portion of the local population, making it difficult to generalize findings to the entire population centers from which this report originates. Represented hospitals were typically referral centers that have cardiac surgery programs and may have widely differing populations with varied risk factors. Advantages include the large size of this prospectively evaluated cohort and the ability to analyze regional variations between continents with a contemporary nature of the patient sample (2000-2003).
Infectious Endocarditis in Olmsted County, Minn.
Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA. 2005;293:3022-3028.
Tleyjeh and colleagues at the Mayo Clinic in Rochester, Minn., retrospectively studied 102 cases of infective endocarditis that occurred in 107 Olmsted County residents from 1970-2000. Main outcome measures were incidence of infective endocarditis, proportion of patients with underlying heart disease and causative micro-organisms and clinical characteristics. The records of all Olmsted County residents with infective endocarditis were identified and reviewed in detail. The definite and possible infective endocarditis cases as defined by modified Duke Criteria were used in the analysis.
The age- and gender-adjusted incidence of infective endocarditis ranged from 5.0 to 7.0 cases per 100,000 person-years during the study period and did not change significantly over time. There were 84 (79%) cases of native valve infective endocarditis and 23 (21%) cases of prosthetic valve infective endocarditis. Valves involved: aortic—36 (24%); mitral—49 (46%), aortic and mitral—12 (11%), right-sided or bilateral—8 (7%), or unknown—8 (7%). 16 (15%) had valve surgery within 42 days and the six-month mortality was 26% (n=28).
Infective endocarditis is a disease of the older individual in this population, with a mean age ranging from 54.1 years in 1980-1984 to 67.4 years in 1995-2000 (P=0.24 for trend). There was a male predominance (67%-83%), which did not significantly change over time.
Mitral valve prolapse was the most frequent underlying valvular heart disease. Viridans streptococci were the most common causative organisms (n=47; 44%) followed by Staphylococcus aureus (n=28 cases; 26%).
The overall average crude infective endocarditis incidence of the period 1970-2000 was 4.95 per 100,000 person-years. The age- and gender-adjusted annual incidence was 6.06 per 100,000 (95% CI, 4.89-7.22). There was no time trend for either streptococcus or Staphylococcus aureus infective endocarditis: the annual adjusted incidence of viridans group streptococcal infective endocarditis was 1.7 to 3.5 cases per 100,000 person years while Staphylococcus aureus infective endocarditis had an annual adjusted incidence of 1.0-2.2 cases per 100,000. The incidence rates of viridans group streptococcal and Staphylococcus aureus infective endocarditis have not changed significantly over time in this population.
Potential limitations of this study include possible incomplete case finding or recognition of the retrospective nature of the case reviews. The homogeneity of the patient population studied (primarily elderly white males with a low prevalence of intravenous drug use) limits the ability to generalize the results. Advantages include the fact that this is a population-based study at a medical center with detailed medical records of virtually all residents of a single county. This allows us to view the clinical features and etiologic factors of primarily left-sided infective endocarditis without the referral bias that tends to taint other studies typically published out of large medical centers with larger geographic referral bases.
Computers and Adverse Drug Events
Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med. 2005;165:1111-1116.
Adverse drug events account for a significant number of hospital admissions and the ensuing costs associated with these hospitalizations. Electronic endeavors, such as computerized physician order entry (CPOE), bar code systems, and electronic medical records attempt to reduce the preventable adverse drug events.
Nebeker, et al. attempted to assess the effects of the implementation of CPOE and other computerized medication systems on adverse drug events in a tertiary care Veterans Administration Medical Center. They used an observational study design whereby 937 out of 2,306 newly admitted patients from several hospital wards were randomly chosen and assigned to a pharmacist reviewer during a 20-week period.
They reviewed complete medical records of hospital stays every other day to document adverse drug events. Not only were traditional adverse drug events identified, but harm from overdoses and/or inappropriate dose reductions or discontinuations, as well as intolerable harm from dose titration, were documented as adverse drug events. The harms caused by the drugs were considered only if the drugs were started in the hospital.
Harms were classified based on prior literature and included standards for pharmacological typology, causality assessment, error type, event terminology, drug class, seriousness index, and medication error category indexing. Additional uncommon classifications were also used, including additional resource utilization. Consensus meetings were held weekly to confirm classification of adverse drug events. Of the admissions reviewed, 483 adverse drug events were identified of which 93% were drug reactions while 7% were due to over- or underdosing. Of the drug reactions, 90% were considered dose-dependent while 10% were considered to be idiosyncratic.
Two different indexing scales were used in classifying the harms. Using the LDS Hospital Scale, it was suggested that 91% of the adverse drug events caused moderate harm while 9% caused serious harm. Using the National Coordinating Council for Medication Error Reporting and Prevention indexing, it was suggested that 87% of the adverse drug events fell into category E (requiring treatment) and 4% into category F (requiring prolonged hospitalization). Twenty-seven percent of the total adverse drug events were thought to be due to errors, including execution and planning steps. Sixty-one percent of errors occurred with the ordering mechanism while 25% of the errors occurred in the monitoring process.
This study highlighted rates of adverse drug events five to 19 times higher than baseline. The authors explained this higher-than-expected rate in part by study elements, such as the use of clinical pharmacists as reviewers, iterative case reviews, and accessible electronic data that make adverse drug events more noticeable.
Weaknesses of this study included issues of comparability of CPOEs because there were significant feature differences among commercial software programs. In addition, this was an observational study lacking a control group. The authors felt that their study did not support the idea that the computerized patient record of the study institution had caused adverse drug events. Rather, the study supported the idea that the system increased the visibility of adverse drug events compared with a paper system. In addition, the authors recommended that the choice of CPOEs be carefully considered, with a focus on decision support features when integrated into a healthcare organization.
The Questionable Benefit of Medical Emergency Teams
Hillman K, Chen J, Cretikos M, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. MERIT study investigators. Lancet. 2005;365:2091-2097.
Previous studies have reported that the MET system reduces the incidence of cardiac arrests, deaths, and unplanned ICU admissions. A MET is a preplanned group of healthcare practitioners who respond to acute patient deteriorations in hospitalized patients.
METs are usually identical to hospital code teams, with the exception that they respond prior to a patient’s developing cardiac arrest. This early response has been shown to significantly decrease unexpected hospital mortality in hospitals in the United States, Australia, and Great Britain. Even though the system has been reported since 1995, few hospitals have knowledge of or experience with METs.
Unexpected hospital deaths and cardiac arrests are often preceded by clinical warning signs. In addition, unplanned ICU admissions may be foreshadowed by abnormalities in the patient’s vital signs that may progress if appropriate interventions are not undertaken. METs assess patients with abnormal physical findings or when there is a concern about the patient’s condition. These patients have findings that may precede a serious event or cardiac arrest, but otherwise don’t meet existing criteria to call a code.
The theory is that if a MET responds to see a patient who is becoming unstable (see “Table 1: MET Calling Criteria,” at left), early interventions may reduce the likelihood of arrest. Published studies have shown a reduction in cardiac arrests and ICU length of stay in virtually all systems in which MET has been introduced (although most studies are hampered by the use of historical controls).
The MERIT study randomized 23 hospitals in Australia to continue functioning as usual (n=11) or to introduce a MET system (n=12). The study sites included a wide range of tertiary, metropolitan, and non-metropolitan hospitals in different states across Australia. The primary outcome was the composite of cardiac arrest, unexpected death, or unplanned ICU admission during the six-month study period after MET activation, using intention to treat analysis.
A four-month educational period was undertaken with the MET centers prior to initiation of the trial. Control hospitals did not receive any education about the MET concept. This was followed by a six-month trial period. Cardiac arrest teams were maintained at all hospitals. The MET consisted of at least one doctor and a nurse from the ED or ICU.
The eligible patients included those residing on a medical ward (including critical care units); the ICUs, OR, postoperative recovery areas, and ED areas were not regarded as general wards.
The primary outcome for the study was the composite outcome of the incidence (events divided by number of eligible patients admitted to the hospital and residing on a medical ward during the study period) of:
- Cardiac arrests without a pre-existing “not-for-resuscitation” (NFR) order;
- Unplanned ICU admissions; and
- Unexpected deaths (those without a pre-existing NFR order).
The results of the study:
- During the study period, the overall rate of calls for the cardiac arrest team or MET was significantly higher in intervention hospitals than in control hospitals. Calls not associated with events were more common in MET hospitals than in controls. Half of the total calls were not associated with a cardiac arrest or unexpected death, whereas in MET hospitals more than 80% of calls were not associated with a cardiac arrest or death (P<0.0001).
- In patients with documented MET calling criteria in association with cardiac arrest or unexpected death, the call rate was similar in MET and control hospitals.
- There were no significant differences between the MET and control hospitals for any outcome.
- The response to changes in vital signs was not adequate—even in MET centers.
These findings are surprising in view of previously reported findings using the MET system. Potential reasons for lack of difference between MET centers and controls include:
- Number of study sites or the duration of the study may not have been adequate for implementation or education;
- Hospitals may already be efficient in detecting and managing unstable patients;
- Patient selection criteria may have been overly restricted. For example, other studies have used 30 respirations per minute for tachypnea as a calling criterion compared with 36 breaths per minute used in this trial;
- Knowledge of the study may have leaked to control hospitals;
- Cardiac arrest teams function as METs at times: Nearly half of the calls to cardiac arrest teams in control hospitals were made without a cardiac arrest or unexpected death; and
- The selected outcomes may not be sensitive enough.
Even though this large, multicenter controlled trial was unable to show a significant benefit of METs, we should not be discouraged from performing further controlled trials in different settings. The use of METs is clearly an exciting and evolving area of medicine.
Barriers to Patient Safety
Amalberti R, Auroy Y, Berwick D, Barach P. Five system barriers to achieving ultrasafe health care. Ann Intern Med. 2005;142:756-764
Patient safety in our healthcare system is a growing concern. One area of dialogue concerning preventable healthcare-associated harms involves the comparability of the healthcare industry with non-medical industries, such as aviation and nuclear power, that have adapted successful strategies shown to provide ultrasafe environments. Amalberti, et al. discuss risk assessment in a variety of industries and explain the need for a benchmarking approach in order to optimize or achieve safety in the healthcare field.
The authors identify five systemic barriers from literature that are fundamentally connected to the ability of the healthcare field to achieve an extremely safe environment.
Barrier 1—acceptance of limitations on maximum performance: The first barrier is the type of expected performance in the field. This is illustrated by the tradeoffs associated with ultrasafety versus productivity. The amount of risk involved was directly related to the limits placed on maximum performance. The first barrier is the acceptance that every system has limits. When a producer exceeds their limit, then safety suffers. An example used is that of blood donation: The limits of collection speed are weighed against the needed screening process.
Barrier 2—abandonment of professional autonomy: The second barrier concerns the concept of professional autonomy. While more teamwork and regulations reduce individual autonomy, this appears to improve safety in the healthcare environment. The bottom line is the importance of teamwork. The example used is that of traffic on a highway: Autonomous units work together to function safely.
Barrier 3—transition from the mindset of craftsman to that of an equivalent actor: The third barrier to achieving high levels of safety includes an equivalent actor mindset. This entails establishing a reliable standard of excellent care in lieu of focusing on individuality, similar to the notion that passengers on an airline usually do not know their pilots, but have established confidence in the airline itself.
Barrier 4—the need for system-level arbitration to optimize safety strategies: The fourth barrier identified is a need for system-level arbitration to optimize safety strategies. This need results from the pressure for justice (usually through litigation) once an accident occurs. Top-down arbitration of safety will be less successful than system level design.
Barrier 5—the need to simplify professional rules and regulations: The final barrier results from the many of layers of guidelines as they serve to create an environment of excellence. This barrier necessitates the removal of these layers to simplify the environment. Existing guidelines should be distilled down to those shown to promote quality and safety. Byzantine rules can obscure the goal of safety and glorify rules, for rules sake.
Certain structural limitations within the field, such as worker shortages in the face of increasing public demands and the reliance of the field on trainees such as students, interns, and residents, create other hurdles. The authors conclude by suggesting a two-tiered system of healthcare whereby ultrasafety could be more easily accomplished in areas of medicine considered more stable (first tier), and a second tier of care that would include the more unstable conditions, and thus inherently, represent the higher risk situations where errors are more likely to occur.
Another provocative point of this article is the need to move toward educating and training teams—not individuals.
The Importance of Implementing COPD Guidelines
Harvey PA, Murphy MC, Dornom E, et al. Implementing evidence-based guidelines: inpatient management of chronic obstructive pulmonary disease. Intern Med J. 2005;35:151-155.
COPD is a common diagnosis that sometimes requires hospitalization. Evidence-based guidelines for disease management, including that of hospitalized patients, exist, but there is a paucity of knowledge about the actual quality of care delivered in the hospital as it aligns with published guidelines. This study by Harvey, et al. explores the quality of care delivered in the hospital for patients with COPD, while at the same time investigating an intervention for the medical staff in an effort to improve adherence to evidenced-based guidelines of the disease.
Using ICD-10 codes for a COPD diagnosis, the study incorporated a retrospective chart review of 49 hospital admissions prior to the intervention and 35 admissions after the intervention in a hospital in Melbourne, Australia. Data were collected pertaining to the hospital management of COPD as it compared with what the authors considered to be Level A—or the highest level of evidence summarized from several professional organizations. The intervention delivered to the medical staff included a summarized presentation of the results from the initial audit of the 49 charts, as well as an educational package that was given to them following the presentation.
Except for inappropriate use of intravenous aminophylline, of which there was a 100% concordance to Level A guidelines, the initiation of systemic steroids (intravenous and/or oral) had the highest concordance rate of 80% and 83%, pre- and postintervention respectively. Appropriate steroid duration (seven to 14 days) had the lowest concordance rates at 10% and 29%, pre- and postintervention respectively.
In addition, preintervention concordance (10%) involving steroid duration was the only rate considered significantly different in the postintervention group (29%). While concordance rates were high for the use of any type of nebulized bronchodilator (96% preintervention and 80% postintervention), the Level A guidelines the authors used suggested that beta-agonist bronchodilators should be used alone prior to the initiation of ipratropium bromide. The concordance rates for this guideline were 27% preintervention and 34% postintervention.
Largely, the authors felt their intervention failed to improve concordance rates to the Level A guidelines investigated and also that their findings of variable and lower concordance rates across the board corroborated other similar studies. The major weaknesses of this study included the small sample size and the nonrandomness of the sampling.
In addition, the authors report that the particular hospital studied included junior doctors who rotated on and off service, which likely prevented the effects of the intervention from being measured on a provider level. In spite of the weaknesses in the study, the article brings to light the need for a more effective translation of evidence-based guidelines to actual practice, especially in the practice of COPD management in the hospital. Further methods of guideline implementation in the clinic setting must be elucidated to improve the care patients with COPD receive in the hospital.
Not all Troponin Elevations Are Myocardial Infarctions
Jeremais A, Gibson CM. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med. 2005;142:786-791.
Troponins are regulatory proteins that control the calcium-mediated interaction of actin and myosin during muscle contraction. All muscle tissue contains troponins, but cardiac troponin T and I have amino acid sequences that are different from skeletal and smooth muscle troponins, allowing them to be detectable by monoclonal antibody-based assays.
In the event of reversible or irreversible cell damage—or possibly even from transiently increased cell membrane permeability—cardiac troponins are released from myocytes into circulation. This characteristic provides a sensitive test for detecting myocardial injury and damage; however, this test is not specific for acute coronary syndromes. And any disorder that causes myocyte damage may cause an elevated troponin.
The 2002 American College of Cardiology/American Heart Association practice guidelines for unstable angina and non-ST-segment elevation myocardial infarction acknowledge that the myocardial necrosis signified by troponin elevation may not necessarily be caused by atherosclerotic coronary artery disease. Such nonthrombotic troponin elevation can be caused by four basic mechanisms, as discussed by Dr. Jeremias and Dr. Gibson.
- Demand ischemia refers to a mismatch between myocardial oxygen demand and supply in the absence of flow-limiting epicardial stenosis. Conditions such as sepsis or septic shock and the systemic inflammatory response syndrome, hypotension or hypovolemia, tachyarrhythmias, and left ventricular hypertrophy can all cause release of cardiac troponin.
- Myocardial ischemia in the absence of fixed obstructive coronary disease can be caused by coronary vasospasm, acute stroke or intracranial hemorrhage, and ingestion of sympathomimetics.
- Direct myocardial damage can be seen in cardiac contusion, direct current cardioversion, cardiac infiltrative disorders such as amyloidosis, certain chemotherapy agents, myocarditis, pericarditis, and cardiac transplantation.
- Myocardial strain occurs when volume and pressure overload of the left and/or right ventricle cause excessive wall tension. Congestive heat failure, acute pulmonary embolism, and chronic pulmonary hypertension can lead to myocardial strain and troponin elevation.
Another condition that can lead to persistently elevated cardiac troponins is end-stage renal disease. This elevation may be due to small areas of clinically silent myocardial necrosis, an increased left ventricular mass, or possibly from impaired renal troponin excretion. Although troponins are believed to be cleared by the reticuloendothelial system, recent evidence shows that troponin T is fragmented into molecules that are small enough to be renally excreted.
In summary, elevated troponin can be found in many clinical settings and is associated with impaired short- and long-term survival. TH
A review of staphylococcal Endocarditis
VG Fowler Jr, Miro JM, Hoen B, et al for the ICE Investigators. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005;June 22;293(24):3061-3062.
Agroup of infectious diseases experts from centers throughout the world formed the International Collaboration on Endocarditis (ICE) in 1999 to gain a global understanding of infective endocarditis. Using the Duke Criteria patients with definite infective endocarditis in a prospective manner, 275 variables were reported with these cases to a central database maintained at Duke University. The ICE-Prospective Cohort Study (ICE-PCS) enrolled 1,779 patients with infective endocarditis in 39 centers in 16 countries between June 15, 2000, and December 31, 2003, and has been described in a recent report. (Cabell CH, Abrutyn E. Infect Dis Clin North Am. 2002;16:255-72). Staphylococcus aureus was the most common cause of infective endocarditis in this group of patients (n=558; 31.6%); the authors characterized risk factors and clinical issues associated with these cases in this report.
By univariate analysis, compared with non-Staphylococcus aureus infective endocarditis, patients with infective endocarditis due to Staphylococcus aureus were more likely than patients with infective endocarditis due to other pathogens to be female (P<0.001), hemodialysis dependent (P<0.001), have diabetes mellitus (P=0.009), have other chronic illnesses (P<0.001), have a healthcare association (P<0.001), have higher rates of stroke (P<0.001), have systemic embolization (P<0.001), have persistent bacteremia (P<0.001), or die (P<0.001).
Although healthcare associated Staphylococcus aureus infective endocarditis was the most common form of Staphylococcus aureus infective endocarditis, more than 60% of healthcare-associated patients acquired the infection outside the hospital. This reflects the global trend in healthcare delivery patterns favoring ambulatory treatment (e.g., outpatient medication infusion via long-term IV access, hemodialysis)
Multivariate analysis, clinical features independently associated with Staphylococcus aureus infective endocarditis (versus non-Staphylococcus aureus infective endocarditis) were: IV drug use (OR, 9.3; 95% CI, 6.3-13.7); first clinical presentation less than one month after first symptoms (OR, 5.1; 95% CI, 3.2-8.2); healthcare-associated infection (OR, 2.9; 95% CI, 2.1-3.8), persistent bacteremia (OR, 2.3; 95% CI, 1.5-3.8), presence of a presumed intravascular device source (OR, 1.7; 95% CI, 1.2-2.6), stroke (OR, 1.6; 95% CI, 1.2-2.3), or diabetes mellitus (OR, 1.3; 95% CI, 1.1-1.8).
Patients from the United States with Staphylococcus aureus infective endocarditis were more likely to be hemodialysis-dependent, to be diabetic, to have a hemodialysis fistula or a chronic indwelling central catheter as a presumed source of infection, and to have a non-nosocomial healthcare association. Patients from the United States and Brazil were more likely to have Methicillin-resistant Staphyloccocus aureus (MRSA) than were patients from Europe, the Middle East, Australia, or New Zealand. In-hospital mortality rates were similar across regions, although American patients were significantly more likely to develop persistent bacteremia (25.6%, P<0.001).
Characteristics independently associated with mortality among patients with nonintravenous drug-use-associated Staphylococcus aureus infective endocarditis by multivariate analysis included stroke (OR, 3.67; 95% CI, 1.94-6.94), persistent bacteremia (OR, 3.06; 95% CI, 1.75-5.35), diagnosis in Southern Europe or the Middle East (OR, 3.21; 95% CI, 1.17-10.56).
This study establishes Staphylococcus aureus infective endocarditis as the leading cause of infective endocarditis in many regions of the world and spotlights the global emergence of healthcare contact as a risk factor for Staphylococcus aureus infective endocarditis. In a significant portion of these patients, an IV device was the presumed source of bacteremia; prosthetic cardiac devices (pacemakers, defibrillators, or prosthetic cardiac valves) were present in almost one-quarter of the patients.
MRSA was a significant cause of Staphylococcus aureus infective endocarditis and displayed regional variation, accounting for almost 40% of the infective endocarditis caused by Staphylococcus aureus in some regions. Patients with infective endocarditis caused by MRSA were significantly more likely to have pre-existing chronic conditions and healthcare associated infective endocarditis by both univariate and multivariate analysis. They also were often associated with persistent bacteremia. On the other hand, 20% of patients with MRSA infective endocarditis developed their infection in the absence of identifiable healthcare contact.
Limitations of this report include the fact that this is an observational study of patients from self-selected centers. Each center most likely represents a portion of the local population, making it difficult to generalize findings to the entire population centers from which this report originates. Represented hospitals were typically referral centers that have cardiac surgery programs and may have widely differing populations with varied risk factors. Advantages include the large size of this prospectively evaluated cohort and the ability to analyze regional variations between continents with a contemporary nature of the patient sample (2000-2003).
Infectious Endocarditis in Olmsted County, Minn.
Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA. 2005;293:3022-3028.
Tleyjeh and colleagues at the Mayo Clinic in Rochester, Minn., retrospectively studied 102 cases of infective endocarditis that occurred in 107 Olmsted County residents from 1970-2000. Main outcome measures were incidence of infective endocarditis, proportion of patients with underlying heart disease and causative micro-organisms and clinical characteristics. The records of all Olmsted County residents with infective endocarditis were identified and reviewed in detail. The definite and possible infective endocarditis cases as defined by modified Duke Criteria were used in the analysis.
The age- and gender-adjusted incidence of infective endocarditis ranged from 5.0 to 7.0 cases per 100,000 person-years during the study period and did not change significantly over time. There were 84 (79%) cases of native valve infective endocarditis and 23 (21%) cases of prosthetic valve infective endocarditis. Valves involved: aortic—36 (24%); mitral—49 (46%), aortic and mitral—12 (11%), right-sided or bilateral—8 (7%), or unknown—8 (7%). 16 (15%) had valve surgery within 42 days and the six-month mortality was 26% (n=28).
Infective endocarditis is a disease of the older individual in this population, with a mean age ranging from 54.1 years in 1980-1984 to 67.4 years in 1995-2000 (P=0.24 for trend). There was a male predominance (67%-83%), which did not significantly change over time.
Mitral valve prolapse was the most frequent underlying valvular heart disease. Viridans streptococci were the most common causative organisms (n=47; 44%) followed by Staphylococcus aureus (n=28 cases; 26%).
The overall average crude infective endocarditis incidence of the period 1970-2000 was 4.95 per 100,000 person-years. The age- and gender-adjusted annual incidence was 6.06 per 100,000 (95% CI, 4.89-7.22). There was no time trend for either streptococcus or Staphylococcus aureus infective endocarditis: the annual adjusted incidence of viridans group streptococcal infective endocarditis was 1.7 to 3.5 cases per 100,000 person years while Staphylococcus aureus infective endocarditis had an annual adjusted incidence of 1.0-2.2 cases per 100,000. The incidence rates of viridans group streptococcal and Staphylococcus aureus infective endocarditis have not changed significantly over time in this population.
Potential limitations of this study include possible incomplete case finding or recognition of the retrospective nature of the case reviews. The homogeneity of the patient population studied (primarily elderly white males with a low prevalence of intravenous drug use) limits the ability to generalize the results. Advantages include the fact that this is a population-based study at a medical center with detailed medical records of virtually all residents of a single county. This allows us to view the clinical features and etiologic factors of primarily left-sided infective endocarditis without the referral bias that tends to taint other studies typically published out of large medical centers with larger geographic referral bases.
Computers and Adverse Drug Events
Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med. 2005;165:1111-1116.
Adverse drug events account for a significant number of hospital admissions and the ensuing costs associated with these hospitalizations. Electronic endeavors, such as computerized physician order entry (CPOE), bar code systems, and electronic medical records attempt to reduce the preventable adverse drug events.
Nebeker, et al. attempted to assess the effects of the implementation of CPOE and other computerized medication systems on adverse drug events in a tertiary care Veterans Administration Medical Center. They used an observational study design whereby 937 out of 2,306 newly admitted patients from several hospital wards were randomly chosen and assigned to a pharmacist reviewer during a 20-week period.
They reviewed complete medical records of hospital stays every other day to document adverse drug events. Not only were traditional adverse drug events identified, but harm from overdoses and/or inappropriate dose reductions or discontinuations, as well as intolerable harm from dose titration, were documented as adverse drug events. The harms caused by the drugs were considered only if the drugs were started in the hospital.
Harms were classified based on prior literature and included standards for pharmacological typology, causality assessment, error type, event terminology, drug class, seriousness index, and medication error category indexing. Additional uncommon classifications were also used, including additional resource utilization. Consensus meetings were held weekly to confirm classification of adverse drug events. Of the admissions reviewed, 483 adverse drug events were identified of which 93% were drug reactions while 7% were due to over- or underdosing. Of the drug reactions, 90% were considered dose-dependent while 10% were considered to be idiosyncratic.
Two different indexing scales were used in classifying the harms. Using the LDS Hospital Scale, it was suggested that 91% of the adverse drug events caused moderate harm while 9% caused serious harm. Using the National Coordinating Council for Medication Error Reporting and Prevention indexing, it was suggested that 87% of the adverse drug events fell into category E (requiring treatment) and 4% into category F (requiring prolonged hospitalization). Twenty-seven percent of the total adverse drug events were thought to be due to errors, including execution and planning steps. Sixty-one percent of errors occurred with the ordering mechanism while 25% of the errors occurred in the monitoring process.
This study highlighted rates of adverse drug events five to 19 times higher than baseline. The authors explained this higher-than-expected rate in part by study elements, such as the use of clinical pharmacists as reviewers, iterative case reviews, and accessible electronic data that make adverse drug events more noticeable.
Weaknesses of this study included issues of comparability of CPOEs because there were significant feature differences among commercial software programs. In addition, this was an observational study lacking a control group. The authors felt that their study did not support the idea that the computerized patient record of the study institution had caused adverse drug events. Rather, the study supported the idea that the system increased the visibility of adverse drug events compared with a paper system. In addition, the authors recommended that the choice of CPOEs be carefully considered, with a focus on decision support features when integrated into a healthcare organization.
The Questionable Benefit of Medical Emergency Teams
Hillman K, Chen J, Cretikos M, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. MERIT study investigators. Lancet. 2005;365:2091-2097.
Previous studies have reported that the MET system reduces the incidence of cardiac arrests, deaths, and unplanned ICU admissions. A MET is a preplanned group of healthcare practitioners who respond to acute patient deteriorations in hospitalized patients.
METs are usually identical to hospital code teams, with the exception that they respond prior to a patient’s developing cardiac arrest. This early response has been shown to significantly decrease unexpected hospital mortality in hospitals in the United States, Australia, and Great Britain. Even though the system has been reported since 1995, few hospitals have knowledge of or experience with METs.
Unexpected hospital deaths and cardiac arrests are often preceded by clinical warning signs. In addition, unplanned ICU admissions may be foreshadowed by abnormalities in the patient’s vital signs that may progress if appropriate interventions are not undertaken. METs assess patients with abnormal physical findings or when there is a concern about the patient’s condition. These patients have findings that may precede a serious event or cardiac arrest, but otherwise don’t meet existing criteria to call a code.
The theory is that if a MET responds to see a patient who is becoming unstable (see “Table 1: MET Calling Criteria,” at left), early interventions may reduce the likelihood of arrest. Published studies have shown a reduction in cardiac arrests and ICU length of stay in virtually all systems in which MET has been introduced (although most studies are hampered by the use of historical controls).
The MERIT study randomized 23 hospitals in Australia to continue functioning as usual (n=11) or to introduce a MET system (n=12). The study sites included a wide range of tertiary, metropolitan, and non-metropolitan hospitals in different states across Australia. The primary outcome was the composite of cardiac arrest, unexpected death, or unplanned ICU admission during the six-month study period after MET activation, using intention to treat analysis.
A four-month educational period was undertaken with the MET centers prior to initiation of the trial. Control hospitals did not receive any education about the MET concept. This was followed by a six-month trial period. Cardiac arrest teams were maintained at all hospitals. The MET consisted of at least one doctor and a nurse from the ED or ICU.
The eligible patients included those residing on a medical ward (including critical care units); the ICUs, OR, postoperative recovery areas, and ED areas were not regarded as general wards.
The primary outcome for the study was the composite outcome of the incidence (events divided by number of eligible patients admitted to the hospital and residing on a medical ward during the study period) of:
- Cardiac arrests without a pre-existing “not-for-resuscitation” (NFR) order;
- Unplanned ICU admissions; and
- Unexpected deaths (those without a pre-existing NFR order).
The results of the study:
- During the study period, the overall rate of calls for the cardiac arrest team or MET was significantly higher in intervention hospitals than in control hospitals. Calls not associated with events were more common in MET hospitals than in controls. Half of the total calls were not associated with a cardiac arrest or unexpected death, whereas in MET hospitals more than 80% of calls were not associated with a cardiac arrest or death (P<0.0001).
- In patients with documented MET calling criteria in association with cardiac arrest or unexpected death, the call rate was similar in MET and control hospitals.
- There were no significant differences between the MET and control hospitals for any outcome.
- The response to changes in vital signs was not adequate—even in MET centers.
These findings are surprising in view of previously reported findings using the MET system. Potential reasons for lack of difference between MET centers and controls include:
- Number of study sites or the duration of the study may not have been adequate for implementation or education;
- Hospitals may already be efficient in detecting and managing unstable patients;
- Patient selection criteria may have been overly restricted. For example, other studies have used 30 respirations per minute for tachypnea as a calling criterion compared with 36 breaths per minute used in this trial;
- Knowledge of the study may have leaked to control hospitals;
- Cardiac arrest teams function as METs at times: Nearly half of the calls to cardiac arrest teams in control hospitals were made without a cardiac arrest or unexpected death; and
- The selected outcomes may not be sensitive enough.
Even though this large, multicenter controlled trial was unable to show a significant benefit of METs, we should not be discouraged from performing further controlled trials in different settings. The use of METs is clearly an exciting and evolving area of medicine.
Barriers to Patient Safety
Amalberti R, Auroy Y, Berwick D, Barach P. Five system barriers to achieving ultrasafe health care. Ann Intern Med. 2005;142:756-764
Patient safety in our healthcare system is a growing concern. One area of dialogue concerning preventable healthcare-associated harms involves the comparability of the healthcare industry with non-medical industries, such as aviation and nuclear power, that have adapted successful strategies shown to provide ultrasafe environments. Amalberti, et al. discuss risk assessment in a variety of industries and explain the need for a benchmarking approach in order to optimize or achieve safety in the healthcare field.
The authors identify five systemic barriers from literature that are fundamentally connected to the ability of the healthcare field to achieve an extremely safe environment.
Barrier 1—acceptance of limitations on maximum performance: The first barrier is the type of expected performance in the field. This is illustrated by the tradeoffs associated with ultrasafety versus productivity. The amount of risk involved was directly related to the limits placed on maximum performance. The first barrier is the acceptance that every system has limits. When a producer exceeds their limit, then safety suffers. An example used is that of blood donation: The limits of collection speed are weighed against the needed screening process.
Barrier 2—abandonment of professional autonomy: The second barrier concerns the concept of professional autonomy. While more teamwork and regulations reduce individual autonomy, this appears to improve safety in the healthcare environment. The bottom line is the importance of teamwork. The example used is that of traffic on a highway: Autonomous units work together to function safely.
Barrier 3—transition from the mindset of craftsman to that of an equivalent actor: The third barrier to achieving high levels of safety includes an equivalent actor mindset. This entails establishing a reliable standard of excellent care in lieu of focusing on individuality, similar to the notion that passengers on an airline usually do not know their pilots, but have established confidence in the airline itself.
Barrier 4—the need for system-level arbitration to optimize safety strategies: The fourth barrier identified is a need for system-level arbitration to optimize safety strategies. This need results from the pressure for justice (usually through litigation) once an accident occurs. Top-down arbitration of safety will be less successful than system level design.
Barrier 5—the need to simplify professional rules and regulations: The final barrier results from the many of layers of guidelines as they serve to create an environment of excellence. This barrier necessitates the removal of these layers to simplify the environment. Existing guidelines should be distilled down to those shown to promote quality and safety. Byzantine rules can obscure the goal of safety and glorify rules, for rules sake.
Certain structural limitations within the field, such as worker shortages in the face of increasing public demands and the reliance of the field on trainees such as students, interns, and residents, create other hurdles. The authors conclude by suggesting a two-tiered system of healthcare whereby ultrasafety could be more easily accomplished in areas of medicine considered more stable (first tier), and a second tier of care that would include the more unstable conditions, and thus inherently, represent the higher risk situations where errors are more likely to occur.
Another provocative point of this article is the need to move toward educating and training teams—not individuals.
The Importance of Implementing COPD Guidelines
Harvey PA, Murphy MC, Dornom E, et al. Implementing evidence-based guidelines: inpatient management of chronic obstructive pulmonary disease. Intern Med J. 2005;35:151-155.
COPD is a common diagnosis that sometimes requires hospitalization. Evidence-based guidelines for disease management, including that of hospitalized patients, exist, but there is a paucity of knowledge about the actual quality of care delivered in the hospital as it aligns with published guidelines. This study by Harvey, et al. explores the quality of care delivered in the hospital for patients with COPD, while at the same time investigating an intervention for the medical staff in an effort to improve adherence to evidenced-based guidelines of the disease.
Using ICD-10 codes for a COPD diagnosis, the study incorporated a retrospective chart review of 49 hospital admissions prior to the intervention and 35 admissions after the intervention in a hospital in Melbourne, Australia. Data were collected pertaining to the hospital management of COPD as it compared with what the authors considered to be Level A—or the highest level of evidence summarized from several professional organizations. The intervention delivered to the medical staff included a summarized presentation of the results from the initial audit of the 49 charts, as well as an educational package that was given to them following the presentation.
Except for inappropriate use of intravenous aminophylline, of which there was a 100% concordance to Level A guidelines, the initiation of systemic steroids (intravenous and/or oral) had the highest concordance rate of 80% and 83%, pre- and postintervention respectively. Appropriate steroid duration (seven to 14 days) had the lowest concordance rates at 10% and 29%, pre- and postintervention respectively.
In addition, preintervention concordance (10%) involving steroid duration was the only rate considered significantly different in the postintervention group (29%). While concordance rates were high for the use of any type of nebulized bronchodilator (96% preintervention and 80% postintervention), the Level A guidelines the authors used suggested that beta-agonist bronchodilators should be used alone prior to the initiation of ipratropium bromide. The concordance rates for this guideline were 27% preintervention and 34% postintervention.
Largely, the authors felt their intervention failed to improve concordance rates to the Level A guidelines investigated and also that their findings of variable and lower concordance rates across the board corroborated other similar studies. The major weaknesses of this study included the small sample size and the nonrandomness of the sampling.
In addition, the authors report that the particular hospital studied included junior doctors who rotated on and off service, which likely prevented the effects of the intervention from being measured on a provider level. In spite of the weaknesses in the study, the article brings to light the need for a more effective translation of evidence-based guidelines to actual practice, especially in the practice of COPD management in the hospital. Further methods of guideline implementation in the clinic setting must be elucidated to improve the care patients with COPD receive in the hospital.
Not all Troponin Elevations Are Myocardial Infarctions
Jeremais A, Gibson CM. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med. 2005;142:786-791.
Troponins are regulatory proteins that control the calcium-mediated interaction of actin and myosin during muscle contraction. All muscle tissue contains troponins, but cardiac troponin T and I have amino acid sequences that are different from skeletal and smooth muscle troponins, allowing them to be detectable by monoclonal antibody-based assays.
In the event of reversible or irreversible cell damage—or possibly even from transiently increased cell membrane permeability—cardiac troponins are released from myocytes into circulation. This characteristic provides a sensitive test for detecting myocardial injury and damage; however, this test is not specific for acute coronary syndromes. And any disorder that causes myocyte damage may cause an elevated troponin.
The 2002 American College of Cardiology/American Heart Association practice guidelines for unstable angina and non-ST-segment elevation myocardial infarction acknowledge that the myocardial necrosis signified by troponin elevation may not necessarily be caused by atherosclerotic coronary artery disease. Such nonthrombotic troponin elevation can be caused by four basic mechanisms, as discussed by Dr. Jeremias and Dr. Gibson.
- Demand ischemia refers to a mismatch between myocardial oxygen demand and supply in the absence of flow-limiting epicardial stenosis. Conditions such as sepsis or septic shock and the systemic inflammatory response syndrome, hypotension or hypovolemia, tachyarrhythmias, and left ventricular hypertrophy can all cause release of cardiac troponin.
- Myocardial ischemia in the absence of fixed obstructive coronary disease can be caused by coronary vasospasm, acute stroke or intracranial hemorrhage, and ingestion of sympathomimetics.
- Direct myocardial damage can be seen in cardiac contusion, direct current cardioversion, cardiac infiltrative disorders such as amyloidosis, certain chemotherapy agents, myocarditis, pericarditis, and cardiac transplantation.
- Myocardial strain occurs when volume and pressure overload of the left and/or right ventricle cause excessive wall tension. Congestive heat failure, acute pulmonary embolism, and chronic pulmonary hypertension can lead to myocardial strain and troponin elevation.
Another condition that can lead to persistently elevated cardiac troponins is end-stage renal disease. This elevation may be due to small areas of clinically silent myocardial necrosis, an increased left ventricular mass, or possibly from impaired renal troponin excretion. Although troponins are believed to be cleared by the reticuloendothelial system, recent evidence shows that troponin T is fragmented into molecules that are small enough to be renally excreted.
In summary, elevated troponin can be found in many clinical settings and is associated with impaired short- and long-term survival. TH
A review of staphylococcal Endocarditis
VG Fowler Jr, Miro JM, Hoen B, et al for the ICE Investigators. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005;June 22;293(24):3061-3062.
Agroup of infectious diseases experts from centers throughout the world formed the International Collaboration on Endocarditis (ICE) in 1999 to gain a global understanding of infective endocarditis. Using the Duke Criteria patients with definite infective endocarditis in a prospective manner, 275 variables were reported with these cases to a central database maintained at Duke University. The ICE-Prospective Cohort Study (ICE-PCS) enrolled 1,779 patients with infective endocarditis in 39 centers in 16 countries between June 15, 2000, and December 31, 2003, and has been described in a recent report. (Cabell CH, Abrutyn E. Infect Dis Clin North Am. 2002;16:255-72). Staphylococcus aureus was the most common cause of infective endocarditis in this group of patients (n=558; 31.6%); the authors characterized risk factors and clinical issues associated with these cases in this report.
By univariate analysis, compared with non-Staphylococcus aureus infective endocarditis, patients with infective endocarditis due to Staphylococcus aureus were more likely than patients with infective endocarditis due to other pathogens to be female (P<0.001), hemodialysis dependent (P<0.001), have diabetes mellitus (P=0.009), have other chronic illnesses (P<0.001), have a healthcare association (P<0.001), have higher rates of stroke (P<0.001), have systemic embolization (P<0.001), have persistent bacteremia (P<0.001), or die (P<0.001).
Although healthcare associated Staphylococcus aureus infective endocarditis was the most common form of Staphylococcus aureus infective endocarditis, more than 60% of healthcare-associated patients acquired the infection outside the hospital. This reflects the global trend in healthcare delivery patterns favoring ambulatory treatment (e.g., outpatient medication infusion via long-term IV access, hemodialysis)
Multivariate analysis, clinical features independently associated with Staphylococcus aureus infective endocarditis (versus non-Staphylococcus aureus infective endocarditis) were: IV drug use (OR, 9.3; 95% CI, 6.3-13.7); first clinical presentation less than one month after first symptoms (OR, 5.1; 95% CI, 3.2-8.2); healthcare-associated infection (OR, 2.9; 95% CI, 2.1-3.8), persistent bacteremia (OR, 2.3; 95% CI, 1.5-3.8), presence of a presumed intravascular device source (OR, 1.7; 95% CI, 1.2-2.6), stroke (OR, 1.6; 95% CI, 1.2-2.3), or diabetes mellitus (OR, 1.3; 95% CI, 1.1-1.8).
Patients from the United States with Staphylococcus aureus infective endocarditis were more likely to be hemodialysis-dependent, to be diabetic, to have a hemodialysis fistula or a chronic indwelling central catheter as a presumed source of infection, and to have a non-nosocomial healthcare association. Patients from the United States and Brazil were more likely to have Methicillin-resistant Staphyloccocus aureus (MRSA) than were patients from Europe, the Middle East, Australia, or New Zealand. In-hospital mortality rates were similar across regions, although American patients were significantly more likely to develop persistent bacteremia (25.6%, P<0.001).
Characteristics independently associated with mortality among patients with nonintravenous drug-use-associated Staphylococcus aureus infective endocarditis by multivariate analysis included stroke (OR, 3.67; 95% CI, 1.94-6.94), persistent bacteremia (OR, 3.06; 95% CI, 1.75-5.35), diagnosis in Southern Europe or the Middle East (OR, 3.21; 95% CI, 1.17-10.56).
This study establishes Staphylococcus aureus infective endocarditis as the leading cause of infective endocarditis in many regions of the world and spotlights the global emergence of healthcare contact as a risk factor for Staphylococcus aureus infective endocarditis. In a significant portion of these patients, an IV device was the presumed source of bacteremia; prosthetic cardiac devices (pacemakers, defibrillators, or prosthetic cardiac valves) were present in almost one-quarter of the patients.
MRSA was a significant cause of Staphylococcus aureus infective endocarditis and displayed regional variation, accounting for almost 40% of the infective endocarditis caused by Staphylococcus aureus in some regions. Patients with infective endocarditis caused by MRSA were significantly more likely to have pre-existing chronic conditions and healthcare associated infective endocarditis by both univariate and multivariate analysis. They also were often associated with persistent bacteremia. On the other hand, 20% of patients with MRSA infective endocarditis developed their infection in the absence of identifiable healthcare contact.
Limitations of this report include the fact that this is an observational study of patients from self-selected centers. Each center most likely represents a portion of the local population, making it difficult to generalize findings to the entire population centers from which this report originates. Represented hospitals were typically referral centers that have cardiac surgery programs and may have widely differing populations with varied risk factors. Advantages include the large size of this prospectively evaluated cohort and the ability to analyze regional variations between continents with a contemporary nature of the patient sample (2000-2003).
Infectious Endocarditis in Olmsted County, Minn.
Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA. 2005;293:3022-3028.
Tleyjeh and colleagues at the Mayo Clinic in Rochester, Minn., retrospectively studied 102 cases of infective endocarditis that occurred in 107 Olmsted County residents from 1970-2000. Main outcome measures were incidence of infective endocarditis, proportion of patients with underlying heart disease and causative micro-organisms and clinical characteristics. The records of all Olmsted County residents with infective endocarditis were identified and reviewed in detail. The definite and possible infective endocarditis cases as defined by modified Duke Criteria were used in the analysis.
The age- and gender-adjusted incidence of infective endocarditis ranged from 5.0 to 7.0 cases per 100,000 person-years during the study period and did not change significantly over time. There were 84 (79%) cases of native valve infective endocarditis and 23 (21%) cases of prosthetic valve infective endocarditis. Valves involved: aortic—36 (24%); mitral—49 (46%), aortic and mitral—12 (11%), right-sided or bilateral—8 (7%), or unknown—8 (7%). 16 (15%) had valve surgery within 42 days and the six-month mortality was 26% (n=28).
Infective endocarditis is a disease of the older individual in this population, with a mean age ranging from 54.1 years in 1980-1984 to 67.4 years in 1995-2000 (P=0.24 for trend). There was a male predominance (67%-83%), which did not significantly change over time.
Mitral valve prolapse was the most frequent underlying valvular heart disease. Viridans streptococci were the most common causative organisms (n=47; 44%) followed by Staphylococcus aureus (n=28 cases; 26%).
The overall average crude infective endocarditis incidence of the period 1970-2000 was 4.95 per 100,000 person-years. The age- and gender-adjusted annual incidence was 6.06 per 100,000 (95% CI, 4.89-7.22). There was no time trend for either streptococcus or Staphylococcus aureus infective endocarditis: the annual adjusted incidence of viridans group streptococcal infective endocarditis was 1.7 to 3.5 cases per 100,000 person years while Staphylococcus aureus infective endocarditis had an annual adjusted incidence of 1.0-2.2 cases per 100,000. The incidence rates of viridans group streptococcal and Staphylococcus aureus infective endocarditis have not changed significantly over time in this population.
Potential limitations of this study include possible incomplete case finding or recognition of the retrospective nature of the case reviews. The homogeneity of the patient population studied (primarily elderly white males with a low prevalence of intravenous drug use) limits the ability to generalize the results. Advantages include the fact that this is a population-based study at a medical center with detailed medical records of virtually all residents of a single county. This allows us to view the clinical features and etiologic factors of primarily left-sided infective endocarditis without the referral bias that tends to taint other studies typically published out of large medical centers with larger geographic referral bases.
Computers and Adverse Drug Events
Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med. 2005;165:1111-1116.
Adverse drug events account for a significant number of hospital admissions and the ensuing costs associated with these hospitalizations. Electronic endeavors, such as computerized physician order entry (CPOE), bar code systems, and electronic medical records attempt to reduce the preventable adverse drug events.
Nebeker, et al. attempted to assess the effects of the implementation of CPOE and other computerized medication systems on adverse drug events in a tertiary care Veterans Administration Medical Center. They used an observational study design whereby 937 out of 2,306 newly admitted patients from several hospital wards were randomly chosen and assigned to a pharmacist reviewer during a 20-week period.
They reviewed complete medical records of hospital stays every other day to document adverse drug events. Not only were traditional adverse drug events identified, but harm from overdoses and/or inappropriate dose reductions or discontinuations, as well as intolerable harm from dose titration, were documented as adverse drug events. The harms caused by the drugs were considered only if the drugs were started in the hospital.
Harms were classified based on prior literature and included standards for pharmacological typology, causality assessment, error type, event terminology, drug class, seriousness index, and medication error category indexing. Additional uncommon classifications were also used, including additional resource utilization. Consensus meetings were held weekly to confirm classification of adverse drug events. Of the admissions reviewed, 483 adverse drug events were identified of which 93% were drug reactions while 7% were due to over- or underdosing. Of the drug reactions, 90% were considered dose-dependent while 10% were considered to be idiosyncratic.
Two different indexing scales were used in classifying the harms. Using the LDS Hospital Scale, it was suggested that 91% of the adverse drug events caused moderate harm while 9% caused serious harm. Using the National Coordinating Council for Medication Error Reporting and Prevention indexing, it was suggested that 87% of the adverse drug events fell into category E (requiring treatment) and 4% into category F (requiring prolonged hospitalization). Twenty-seven percent of the total adverse drug events were thought to be due to errors, including execution and planning steps. Sixty-one percent of errors occurred with the ordering mechanism while 25% of the errors occurred in the monitoring process.
This study highlighted rates of adverse drug events five to 19 times higher than baseline. The authors explained this higher-than-expected rate in part by study elements, such as the use of clinical pharmacists as reviewers, iterative case reviews, and accessible electronic data that make adverse drug events more noticeable.
Weaknesses of this study included issues of comparability of CPOEs because there were significant feature differences among commercial software programs. In addition, this was an observational study lacking a control group. The authors felt that their study did not support the idea that the computerized patient record of the study institution had caused adverse drug events. Rather, the study supported the idea that the system increased the visibility of adverse drug events compared with a paper system. In addition, the authors recommended that the choice of CPOEs be carefully considered, with a focus on decision support features when integrated into a healthcare organization.
The Questionable Benefit of Medical Emergency Teams
Hillman K, Chen J, Cretikos M, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. MERIT study investigators. Lancet. 2005;365:2091-2097.
Previous studies have reported that the MET system reduces the incidence of cardiac arrests, deaths, and unplanned ICU admissions. A MET is a preplanned group of healthcare practitioners who respond to acute patient deteriorations in hospitalized patients.
METs are usually identical to hospital code teams, with the exception that they respond prior to a patient’s developing cardiac arrest. This early response has been shown to significantly decrease unexpected hospital mortality in hospitals in the United States, Australia, and Great Britain. Even though the system has been reported since 1995, few hospitals have knowledge of or experience with METs.
Unexpected hospital deaths and cardiac arrests are often preceded by clinical warning signs. In addition, unplanned ICU admissions may be foreshadowed by abnormalities in the patient’s vital signs that may progress if appropriate interventions are not undertaken. METs assess patients with abnormal physical findings or when there is a concern about the patient’s condition. These patients have findings that may precede a serious event or cardiac arrest, but otherwise don’t meet existing criteria to call a code.
The theory is that if a MET responds to see a patient who is becoming unstable (see “Table 1: MET Calling Criteria,” at left), early interventions may reduce the likelihood of arrest. Published studies have shown a reduction in cardiac arrests and ICU length of stay in virtually all systems in which MET has been introduced (although most studies are hampered by the use of historical controls).
The MERIT study randomized 23 hospitals in Australia to continue functioning as usual (n=11) or to introduce a MET system (n=12). The study sites included a wide range of tertiary, metropolitan, and non-metropolitan hospitals in different states across Australia. The primary outcome was the composite of cardiac arrest, unexpected death, or unplanned ICU admission during the six-month study period after MET activation, using intention to treat analysis.
A four-month educational period was undertaken with the MET centers prior to initiation of the trial. Control hospitals did not receive any education about the MET concept. This was followed by a six-month trial period. Cardiac arrest teams were maintained at all hospitals. The MET consisted of at least one doctor and a nurse from the ED or ICU.
The eligible patients included those residing on a medical ward (including critical care units); the ICUs, OR, postoperative recovery areas, and ED areas were not regarded as general wards.
The primary outcome for the study was the composite outcome of the incidence (events divided by number of eligible patients admitted to the hospital and residing on a medical ward during the study period) of:
- Cardiac arrests without a pre-existing “not-for-resuscitation” (NFR) order;
- Unplanned ICU admissions; and
- Unexpected deaths (those without a pre-existing NFR order).
The results of the study:
- During the study period, the overall rate of calls for the cardiac arrest team or MET was significantly higher in intervention hospitals than in control hospitals. Calls not associated with events were more common in MET hospitals than in controls. Half of the total calls were not associated with a cardiac arrest or unexpected death, whereas in MET hospitals more than 80% of calls were not associated with a cardiac arrest or death (P<0.0001).
- In patients with documented MET calling criteria in association with cardiac arrest or unexpected death, the call rate was similar in MET and control hospitals.
- There were no significant differences between the MET and control hospitals for any outcome.
- The response to changes in vital signs was not adequate—even in MET centers.
These findings are surprising in view of previously reported findings using the MET system. Potential reasons for lack of difference between MET centers and controls include:
- Number of study sites or the duration of the study may not have been adequate for implementation or education;
- Hospitals may already be efficient in detecting and managing unstable patients;
- Patient selection criteria may have been overly restricted. For example, other studies have used 30 respirations per minute for tachypnea as a calling criterion compared with 36 breaths per minute used in this trial;
- Knowledge of the study may have leaked to control hospitals;
- Cardiac arrest teams function as METs at times: Nearly half of the calls to cardiac arrest teams in control hospitals were made without a cardiac arrest or unexpected death; and
- The selected outcomes may not be sensitive enough.
Even though this large, multicenter controlled trial was unable to show a significant benefit of METs, we should not be discouraged from performing further controlled trials in different settings. The use of METs is clearly an exciting and evolving area of medicine.
Barriers to Patient Safety
Amalberti R, Auroy Y, Berwick D, Barach P. Five system barriers to achieving ultrasafe health care. Ann Intern Med. 2005;142:756-764
Patient safety in our healthcare system is a growing concern. One area of dialogue concerning preventable healthcare-associated harms involves the comparability of the healthcare industry with non-medical industries, such as aviation and nuclear power, that have adapted successful strategies shown to provide ultrasafe environments. Amalberti, et al. discuss risk assessment in a variety of industries and explain the need for a benchmarking approach in order to optimize or achieve safety in the healthcare field.
The authors identify five systemic barriers from literature that are fundamentally connected to the ability of the healthcare field to achieve an extremely safe environment.
Barrier 1—acceptance of limitations on maximum performance: The first barrier is the type of expected performance in the field. This is illustrated by the tradeoffs associated with ultrasafety versus productivity. The amount of risk involved was directly related to the limits placed on maximum performance. The first barrier is the acceptance that every system has limits. When a producer exceeds their limit, then safety suffers. An example used is that of blood donation: The limits of collection speed are weighed against the needed screening process.
Barrier 2—abandonment of professional autonomy: The second barrier concerns the concept of professional autonomy. While more teamwork and regulations reduce individual autonomy, this appears to improve safety in the healthcare environment. The bottom line is the importance of teamwork. The example used is that of traffic on a highway: Autonomous units work together to function safely.
Barrier 3—transition from the mindset of craftsman to that of an equivalent actor: The third barrier to achieving high levels of safety includes an equivalent actor mindset. This entails establishing a reliable standard of excellent care in lieu of focusing on individuality, similar to the notion that passengers on an airline usually do not know their pilots, but have established confidence in the airline itself.
Barrier 4—the need for system-level arbitration to optimize safety strategies: The fourth barrier identified is a need for system-level arbitration to optimize safety strategies. This need results from the pressure for justice (usually through litigation) once an accident occurs. Top-down arbitration of safety will be less successful than system level design.
Barrier 5—the need to simplify professional rules and regulations: The final barrier results from the many of layers of guidelines as they serve to create an environment of excellence. This barrier necessitates the removal of these layers to simplify the environment. Existing guidelines should be distilled down to those shown to promote quality and safety. Byzantine rules can obscure the goal of safety and glorify rules, for rules sake.
Certain structural limitations within the field, such as worker shortages in the face of increasing public demands and the reliance of the field on trainees such as students, interns, and residents, create other hurdles. The authors conclude by suggesting a two-tiered system of healthcare whereby ultrasafety could be more easily accomplished in areas of medicine considered more stable (first tier), and a second tier of care that would include the more unstable conditions, and thus inherently, represent the higher risk situations where errors are more likely to occur.
Another provocative point of this article is the need to move toward educating and training teams—not individuals.
The Importance of Implementing COPD Guidelines
Harvey PA, Murphy MC, Dornom E, et al. Implementing evidence-based guidelines: inpatient management of chronic obstructive pulmonary disease. Intern Med J. 2005;35:151-155.
COPD is a common diagnosis that sometimes requires hospitalization. Evidence-based guidelines for disease management, including that of hospitalized patients, exist, but there is a paucity of knowledge about the actual quality of care delivered in the hospital as it aligns with published guidelines. This study by Harvey, et al. explores the quality of care delivered in the hospital for patients with COPD, while at the same time investigating an intervention for the medical staff in an effort to improve adherence to evidenced-based guidelines of the disease.
Using ICD-10 codes for a COPD diagnosis, the study incorporated a retrospective chart review of 49 hospital admissions prior to the intervention and 35 admissions after the intervention in a hospital in Melbourne, Australia. Data were collected pertaining to the hospital management of COPD as it compared with what the authors considered to be Level A—or the highest level of evidence summarized from several professional organizations. The intervention delivered to the medical staff included a summarized presentation of the results from the initial audit of the 49 charts, as well as an educational package that was given to them following the presentation.
Except for inappropriate use of intravenous aminophylline, of which there was a 100% concordance to Level A guidelines, the initiation of systemic steroids (intravenous and/or oral) had the highest concordance rate of 80% and 83%, pre- and postintervention respectively. Appropriate steroid duration (seven to 14 days) had the lowest concordance rates at 10% and 29%, pre- and postintervention respectively.
In addition, preintervention concordance (10%) involving steroid duration was the only rate considered significantly different in the postintervention group (29%). While concordance rates were high for the use of any type of nebulized bronchodilator (96% preintervention and 80% postintervention), the Level A guidelines the authors used suggested that beta-agonist bronchodilators should be used alone prior to the initiation of ipratropium bromide. The concordance rates for this guideline were 27% preintervention and 34% postintervention.
Largely, the authors felt their intervention failed to improve concordance rates to the Level A guidelines investigated and also that their findings of variable and lower concordance rates across the board corroborated other similar studies. The major weaknesses of this study included the small sample size and the nonrandomness of the sampling.
In addition, the authors report that the particular hospital studied included junior doctors who rotated on and off service, which likely prevented the effects of the intervention from being measured on a provider level. In spite of the weaknesses in the study, the article brings to light the need for a more effective translation of evidence-based guidelines to actual practice, especially in the practice of COPD management in the hospital. Further methods of guideline implementation in the clinic setting must be elucidated to improve the care patients with COPD receive in the hospital.
Not all Troponin Elevations Are Myocardial Infarctions
Jeremais A, Gibson CM. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med. 2005;142:786-791.
Troponins are regulatory proteins that control the calcium-mediated interaction of actin and myosin during muscle contraction. All muscle tissue contains troponins, but cardiac troponin T and I have amino acid sequences that are different from skeletal and smooth muscle troponins, allowing them to be detectable by monoclonal antibody-based assays.
In the event of reversible or irreversible cell damage—or possibly even from transiently increased cell membrane permeability—cardiac troponins are released from myocytes into circulation. This characteristic provides a sensitive test for detecting myocardial injury and damage; however, this test is not specific for acute coronary syndromes. And any disorder that causes myocyte damage may cause an elevated troponin.
The 2002 American College of Cardiology/American Heart Association practice guidelines for unstable angina and non-ST-segment elevation myocardial infarction acknowledge that the myocardial necrosis signified by troponin elevation may not necessarily be caused by atherosclerotic coronary artery disease. Such nonthrombotic troponin elevation can be caused by four basic mechanisms, as discussed by Dr. Jeremias and Dr. Gibson.
- Demand ischemia refers to a mismatch between myocardial oxygen demand and supply in the absence of flow-limiting epicardial stenosis. Conditions such as sepsis or septic shock and the systemic inflammatory response syndrome, hypotension or hypovolemia, tachyarrhythmias, and left ventricular hypertrophy can all cause release of cardiac troponin.
- Myocardial ischemia in the absence of fixed obstructive coronary disease can be caused by coronary vasospasm, acute stroke or intracranial hemorrhage, and ingestion of sympathomimetics.
- Direct myocardial damage can be seen in cardiac contusion, direct current cardioversion, cardiac infiltrative disorders such as amyloidosis, certain chemotherapy agents, myocarditis, pericarditis, and cardiac transplantation.
- Myocardial strain occurs when volume and pressure overload of the left and/or right ventricle cause excessive wall tension. Congestive heat failure, acute pulmonary embolism, and chronic pulmonary hypertension can lead to myocardial strain and troponin elevation.
Another condition that can lead to persistently elevated cardiac troponins is end-stage renal disease. This elevation may be due to small areas of clinically silent myocardial necrosis, an increased left ventricular mass, or possibly from impaired renal troponin excretion. Although troponins are believed to be cleared by the reticuloendothelial system, recent evidence shows that troponin T is fragmented into molecules that are small enough to be renally excreted.
In summary, elevated troponin can be found in many clinical settings and is associated with impaired short- and long-term survival. TH
PEDIATRIC SPECIAL SECTION: Sibling Rivalry
In the flourishing metropolitan area of Atlanta, hospitalists and community-based physicians at Children’s Healthcare of Atlanta thrive within their niches, riding waves of opportunity fueled by the region’s burgeoning population. Jay Berkelhamer, MD, senior vice president of medical affairs at Children’s Healthcare of Atlanta calls his city “one of the most dynamic growth centers in the United States. Within 10 years we are estimated to have at least 150,000 more kids in Atlanta, leading to even greater opportunities for hospitalists and private practice primary care and specialty pediatricians.”
Two Hospitals, One system
Children’s Hospital of Atlanta’s hospitalist program is, in fact, two separate programs: one at Egleston, the other at Scottish Rite. The parent organization links the two and manages each hospital’s mission, structure, hiring, compensation, and outcomes.

—David Hall, MD
The six Egleston full-time equivalent hospitalists, or “cat herders,” as Corinne Taylor, MD, Egleston’s chief of medical affairs, describes them, are employees of Emory University Medical School. Most Egleston hospitalists are parents of young children and work four days a week, allowing them a balance of career and family life. Employed by the medical school and working at an academic medical center, they receive a salary, benefits, and other support services. Side by side with interns and residents, Egleston’s hospitalists see Atlanta’s sickest, frailest, and most at-risk children: the uninsured, underinsured immigrant and local population.
At Egleston the pediatric hospitalists are like their counterparts who treat adult patients in other settings. They deal with many patients with chronic conditions that lead to repeat hospitalizations.
“We see lots of ex-preemies with multiple problems such as asthma, seizures, cerebral palsy, and gastric problems,” says Dr. Taylor. “Some are ventilator-dependent and need lots of care.”
She relishes the clinical discipline that being a hospitalist at an academic medical center presents. “I do my homework every day and enjoy the stimulation of teaching our house officers,” explains Dr. Taylor. “Working with adult learners on the chronic conditions we manage and the cases with puzzling symptoms is exciting.”
Dr. Taylor’s boss is this hospitalist program’s founder, Joseph Snitzer, MD (see “Joseph Snitzer, MD: A hospital medicine pioneer”). Being hospital-based frees Dr. Snitzer to observe an endless parade of clinical challenges, including complex rheumatology cases, lupus, tumors, infected shunts, seizures, exotic infections, oncology diagnoses, and more.
“People call us from rural hospitals and private practices for help with diagnoses,” explains Dr. Snitzer. “We’re not smarter than anyone else. We just see a lot more than most other physicians.”
Scottish Rite
Across town at Scottish Rite, a nonprofit hospital, the hospitalists cope with the demands of a steady influx of new Atlantans. David Hall, MD, is Scottish Rite’s medical director. He was a former Egleston hospitalist and a private practitioner for 10 years in Baltimore before he relocated to Atlanta.
“We don’t have house officers, and there is a resident on call only one night a week,” says Dr. Hall. “Pediatricians in the community need to have their patients admitted 24/7, and we also have to admit from the emergency department at night. With our hospitalists taking calls at night and working all the next day, sometimes they would be on for 36 hours straight. As our service has grown, we’ve realized that this model was not sustainable.”
To reduce the burnout from their growing patient loads, the hospitalists changed their model. As of August 1, 2005, hospitalists at Scottish Rite began working either eight- or 12-hour shifts.
“Until we gain some experience with the shift system, we know we will struggle with continuity and handoffs,” adds Dr. Hall. Scottish Rite is also increasing its complement of moonlighting private practice pediatricians who want to keep their hospital skills current by covering the heavy workload.
Dr. Hall says recruiting new hospitalists isn’t a problem. Many local physicians want to do this work—especially right after residency. Comparing being a hospitalist with his 10 years in private practice, he says, “In my office practice I’d be sitting 20 feet away from a colleague, and there wasn’t much interaction. Now I’m learning something new every day and discussing interesting patients with other doctors. Building these ongoing relationships is great.”
Benefits, Culture, and More
The compensation and benefits packages at Egleston and Scottish Rite reflect that they are two separate hospitals in one system. Egleston’s hospitalists are employed by the medical school and receive a straight salary, with no incentive or at risk components. Scottish Rite’s hospitalists are hospital employees and have 20% of their salary at risk with productivity, quality improvement, and patient satisfaction incentives.
Although the different compensation systems may lead to discrepancies in pay, Dr. Berkelhamer explains that the policy of Children’s Hospital of Atlanta is to offer market-based salaries to all hospitalists. “Part of my job is to ensure that Dr. Snitzer and Dr. Hall are empowered to hire the physicians they want,” he says.
The hospitals have different corporate cultures as well. “The Scottish Rite group is very comfortable with lots of hands-on work while those at Egleston like to spend more time teaching,” says Dr. Berkelhamer.
Dr. Taylor, who trained with Dr. Snitzer and had a private practice in Atlanta for five years before becoming a full-time Egleston hospitalist in 1993, also acknowledges the different cultures at Egleston and Scottish Rite.
“We are two hospitals that come to the table and work together,” she observes. “Although we are in separate locations and may approach things differently, we practice the same type of medicine.”
Dr. Berkelhamer, who works with both sets of hospitalists, reinforces the observation that their clinical practices are consistent: “Surveys on patient and community physician satisfaction are the same, as are outcomes and productivity data.”
Special Issues for Both Hospitals
As part of a growing medical specialty in a dynamic region of the country, hospitalists at Children’s Hospital of Atlanta must confront a number of issues—some unique to them, others that reflect national trends. With different compensation and productivity systems, the two sets of hospitalists must collaborate to practice one brand of medicine.
An important formal step in their collaboration is the computerized medical and order entry system scheduled for spring 2006 implementation. The hospitalists are working together to develop clinical pathways and standardized orders based on their culling through best practices and evidence-based medicine guidelines. A newly appointed chief quality officer will keep the project on track.
Atlanta’s growth presents other issues for the hospitalists. With a constant influx of new community-based pediatricians Dr. Taylor finds that the hospitalists sometimes have trouble communicating with them to coordinate care.
“There are now at least 1,000 primary care and subspecialty pediatricians in Atlanta,” she says. “Trying to build trust and to track personal preferences with so many doctors is difficult. Fortunately we have electronic medical records so we can share important data with them.”
The hospitals’ social workers and case managers represent added glue to hold the communication together. Another of Atlanta’s challenges: It has only two medical schools from which to draw local hospitalists and other pediatricians, Emory University and the smaller Morehouse University. While not insurmountable, it means that most pediatricians practicing in the area must relocate to Atlanta.
What the Future Holds
And then there are issues that transcend Atlanta. Dr. Snitzer feels the national movement for hospitalists to become a specialty will happen sooner rather than later. In line with that movement, Children’s Hospital of Atlanta will have its first hospitalist fellowship in 2007. (For more information on pediatric hospital medicine fellowships, see “Pediatric Fellowship Offered,” below.)
For Dr. Hall, hospitalist compensation in a boomtown rankles. “People can’t really make money being hospitalists,” he explains. “Most need some subsidy to keep the programs going.”
The pay issues are being addressed, albeit slowly. Dr. Hall is encouraged by the campaign of pediatric intensivists to have coding and payment upgrades; he sees it as a template for higher hospitalist reimbursement schedules. “We only get paid for one visit a day, but we often see a patient several times a day,” he says. “Reimbursement should reflect what we really do.”
Both hospitals will have new buildings, each with 250 beds, more surgical suites, and expanded emergency departments by early 2007. That should lead to more hospitalist hiring—not surprising for a hospital that pioneered having inpatient physicians more than 20 years ago. TH
Writer Marlene Piturro is based in New York.
PEDIATRIC SPECIAL SECTION:
NEWS
Pediatric Fellowship Offered
Children’s Hospitalists of San Diego offers program
The Pediatric Hospitalist program at Children’s Hospital and Health Center of San Diego (CHHC) began in 1978. The current hospitalists are employed by Children’s Specialists of San Diego (CSSD), a 180-member pediatric-only specialty medical group. Inpatient care is provided for 75% of all general pediatric patients at the 233-bed tertiary care CHHC. Program consultation is offered at nearby Palomar Medical Center, a 23-bed unit within a larger 319-bed community hospital with a trauma center.
The hospitalists are the primary teaching faculty for the house staff and medical students who come from the University of California San Diego (UCSD), Balboa Naval Hospital, Pendleton Naval Medical Center, and Scripps Family Medicine. All hospitalists are board-certified pediatricians and have additional degrees or postresidency training, such as chief residency or fellowship experience.
Hospitalists fulfill many leadership roles in the hospital and community when not on service. A detailed list is available in a previous issue of The Hospitalist (Nov/Dec 2004;8(6):59-60). Current research includes an Agency for Healthcare Research and Quality (AHRQ) safety grant on medication errors, a bronchiolitis clinical trial, juvenile justice research on hepatitis B, a Hispanic cultural competency grant from the California Endowment, spiratory syncytial virus immunoprophylaxis outcomes in a managed population, and primary care perceptions of pediatric dentistry. Thus the hospitalist program has a long history of strong commitment to children and the core aspects of pediatric hospital medicine.
The Fellowship
The CSSD Pediatric Hospitalist Fellowship Program goal is to train highly motivated pediatricians for careers in academic and clinical hospital medicine. Over a two-year period instruction is provided in clinical, advocacy, administrative, teaching, and research aspects of pediatric hospital medicine. Clinical education emphasizes inpatient acute care, including intensive care and emergency transport at the busy main campus at CHHC. Outpatient clinical care offers experiences in adolescent juvenile hall medicine, hospice, and child protection. The diverse clinical exposure, teaching from local and national leaders, and volume of patients ensure graduates of this program are well prepared for any clinical hospitalist position.
The staff gains administrative experience via both hospital and medical group quality improvement activities. This work is directed by the medical director for CSSD and the physician advisor for quality management for CHHC, both of whom are CSSD pediatric hospitalists. Skills in process improvement, continuous quality improvement, risk management, organizational management and leadership are honed during the fellowship. Opportunity exists to take courses through the American College of Physician Executives if the trainee desires a future in administrative hospitalist medicine.
Academics and teaching are a core value of the pediatric hospitalist service. The fellow participates in the monthly division journal club and internal case review. Daily teaching while on the clinical service includes bedside rounds, management rounds, and attending rounds. Pediatric hospitalists are the primary inpatient teaching staff and as such have a significant responsibility for daily house staff education. The fellow participates in noon conferences and other educational venues under the guidance of the director of inpatient teaching (also a pediatric hospitalist).
Advocacy skills are learned through experiences in the juvenile hall system, Center for Child Protection, the American Academy of Pediatrics (AAP), and at the local and state level for children’s services funding. Under the leadership of the medical directors for the Center for Child Protection and the A.B. and Jessie Polinsky Center for Abused Children, the fellow participates in case review and observes expert child abuse testimony in court. Discussions with legislators in Sacramento focus upon protection of the California Children’s Services system, which supports critically ill state-funded children. The fellow learns AAP local and national structure, participating in conferences and chapter events.
Research is expected during this two-year fellowship program. Formal clinical research training is part of the first year curriculum of UCSD’s Clinical Research Enhancement through Supplemental Training (CREST) program. The first year of this two-year CREST program includes weekly classes covering epidemiology, patient-oriented research, health services research, and informatics. Those dedicated to completion of a master’s degree during the two-year program may integrate this training with a more intense curriculum schedule. A research project and mentor is chosen after the first quarter of the first year. Research may be in any area of pediatric hospitalist medicine. Research is presented at either Pediatric Academic Societies, Society of Hospital Medicine, or other similar forum upon completion.
The schedule is flexible, but follows the template. (See Table 1, p. 30: “Pediatric Hospitalist Fellowship Program Schedule.”)
One fellowship position is offered every year, with application submissions accepted through Dec. 1, interviews granted Dec. 15-Feb. 1 and final selection by Feb. 15. You can obtain an application from the CSSD Web site “Fellowships” page (http://childrensspecialists. com/body.cfm?id=580) or by e-mailing Fellowship Coordinator Susan Stafford at sstafford@chsd.org.
PEDIATRIC SPECIAL SECTION:
IN THE LITERATURE
Retrospective Study Attempts Criteria for Diagnosing MAS
Reviews by Julia Simmons, MD
Ravelli A, Magni-Manzoni S, Pistorio A, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005;146(5):598-604.
Macrophage activating syndrome (MAS) is a complication of connective tissue disorders, most often associated with active systemic juvenile idiopathic arthritis (S-JIA). It is a rare disorder and the exact incidence is unknown. It is characterized by uncontrolled activation and proliferation of T-lymphocytes and macrophages. If not recognized and treated aggressively, MAS can be life threatening.
In this article, the authors’ purpose was to review the available clinical, laboratory, and histopathologic data in patients with active S-JIA and in those with active S-JIA complicated by MAS. The goal was to develop criteria to diagnose MAS.
The retrospective study was designed using the classification, criteria approach. The index cases included patients with MAS complicating S-JIA. The “confusable” condition was active S-JIA. There were 74 patients in the index cases. Seventeen of the cases were observed at the authors’ institution. These patients were diagnosed with S-JIA using the International League of Association for Rheumatology criteria. They were identified using a database search. Fifty-seven of the cases were obtained from a Medline search. Of these 74 patients, eight were disqualified because they did not meet the definition of S-JIA, and 11 were excluded because of insufficient data. The control group contained 37 patients observed at the authors’ sites. The sensitivity rate, specificity rate, area under receiver operating characteristic curve, and diagnostic odds ratio were applied to the data to differentiate MAS complicating S-JIA from S-JIA.
The study results found hemorrhages and central nervous dysfunction were the strongest clinical discriminating factors. The strongest laboratory discriminators included thrombocytopenia, leukopenia, elevated aspartate aminotransferase, and hypofibrinogenemia. Histopathological criterion included evidence of macrophage hemophagocytosis in the bone marrow aspirate. Other useful discriminators included hypertriglyceridemia, elevated ferritin, hepatomegaly, hand hyponatremia. Final guidelines were developed after analyzing the statistics and determining the clinical importance: “The diagnosis of MAS requires the presence of any two or more laboratory criteria or of any two or three or more clinical and/or laboratory criteria. A bone marrow aspirate for the demonstration of hemophagocytosis may be required only in doubtful cases.”
In summary, MAS complicating S-JIA is a disorder without concrete diagnostic criteria. The authors have performed preliminary studies to diagnose MAS. They appropriately recognized the need for prospective larger clinical studies.
HNL Helps Distinguish Infections
Fjaertoft G, Foucard T, Xu S, et al. Human neutrophil lipocalin (HNL) as a diagnostic tool in children with acute infections: a study of the kinetics. Acta Pediatrica costarricense. 2005;94:661-666.
In pediatrics, the clinician is often faced with the diagnostic challenge of differentiating a bacterial infectious process from a viral infection. History, physical exam, and laboratory data make the distinction. In this article, the authors’ purpose was to assess the kinetics of HNL with viral and bacterial infections. Further, they assess the response of HNL when the infection is treated with antibiotics. The response of HNL is compared with that of C-reactive protein.
In the study, 92 patients with a median age of 26 months were hospitalized because they required systemic antibiotics or because of the severity of their medical condition. Upon admission and on hospital days one, two, and three, the C-reactive protein, white blood cell count with differential, and HNL were measured. The patients were retrospectively classified into five groups: true bacterial infection (n=28), true viral infection (n=4), suspected bacterial infection (n=18), suspected viral (n=34), and other.
A true bacterial infection required bacterial isolation from blood, urine, or cerebrospinal fluid culture, or radiographic demonstration of pneumonia. Patients were classified as having a suspected bacterial infection if they had a nonspecific diagnosis, but an elevated C-reactive protein and erythrocyte sedimentation rate. A true viral infection required isolation of a virus. If a patient did not meet any of the above criteria, the person was classified as having a suspected viral infection. Those patients in the “other” group were diagnosed with Kawasaki disease, Borrelia meningitis, and one undiagnosed patient. The patients were classified using history, exam, and laboratory values including white blood cell count, erythrocyte sedimentation rate, C-reactive protein, and cultures. HNL values were not used in the classification.
The results demonstrated that both C-reactive protein and HNL are elevated with true bacterial infections compared with viral illnesses. Neither C-reactive protein nor HNL were significantly different in true bacterial infections versus suspected bacterial infections. The optimal cut-off for C-reactive protein was 59 mg/L with 93% sensitivity and 68% specificity. The optimal cutoff for HNL was 217 micrograms/L with 90% sensitivity and 74% specificity. In patients with true bacterial infections, HNL was highest at admission and decreased one day after admission. In contrast, the C-reactive protein values were similar on the day of admission and on hospital day one. C-reactive protein decreased significantly on days two and three of hospitalization. After hospital day one, HNL was elevated in only 11% of patients with true bacterial infection in contrast to 83% patients with elevated C-reactive protein.
In summary, HNL may be a useful marker to distinguish bacterial and viral illnesses. In comparison with C-reactive protein, it normalizes more rapidly after appropriate antibiotic therapy is initiated. In the future, HNL may be a useful marker in monitoring the response to antibiotic therapy.
CEDKA in Peds
Lawrence SE, Cummings EA, Gaboury I, et al. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. . 2005;146:688-692.
New onset insulin dependent diabetes mellitus is complicated by diabetic ketoacidosis (DKA) in 15% to 67% of patients. The incidence of cerebral edema in diabetic ketoacidosis (CEDKA) has been reported as 0.4-3.1. In the article, the authors seek to determine the incidence, outcome, and risk factors for cerebral edema in DKA in patients younger than 16.
The study was case-controlled with an active Canadian surveillance study. The authors surveyed pediatricians for a two-year period. During this time in Canada, all physicians were requested to submit reports monthly on patients with CEDKA younger than 16.
Thirteen cases were identified and the incidence of CEDKA was 0.51%. Overall mortality from cerebral edema was 0.15%. Increased blood urea nitrogen, degree of dehydration, hyperglycemia, and lower initial bicarbonate were associated with CEDKA. TH
In the flourishing metropolitan area of Atlanta, hospitalists and community-based physicians at Children’s Healthcare of Atlanta thrive within their niches, riding waves of opportunity fueled by the region’s burgeoning population. Jay Berkelhamer, MD, senior vice president of medical affairs at Children’s Healthcare of Atlanta calls his city “one of the most dynamic growth centers in the United States. Within 10 years we are estimated to have at least 150,000 more kids in Atlanta, leading to even greater opportunities for hospitalists and private practice primary care and specialty pediatricians.”
Two Hospitals, One system
Children’s Hospital of Atlanta’s hospitalist program is, in fact, two separate programs: one at Egleston, the other at Scottish Rite. The parent organization links the two and manages each hospital’s mission, structure, hiring, compensation, and outcomes.

—David Hall, MD
The six Egleston full-time equivalent hospitalists, or “cat herders,” as Corinne Taylor, MD, Egleston’s chief of medical affairs, describes them, are employees of Emory University Medical School. Most Egleston hospitalists are parents of young children and work four days a week, allowing them a balance of career and family life. Employed by the medical school and working at an academic medical center, they receive a salary, benefits, and other support services. Side by side with interns and residents, Egleston’s hospitalists see Atlanta’s sickest, frailest, and most at-risk children: the uninsured, underinsured immigrant and local population.
At Egleston the pediatric hospitalists are like their counterparts who treat adult patients in other settings. They deal with many patients with chronic conditions that lead to repeat hospitalizations.
“We see lots of ex-preemies with multiple problems such as asthma, seizures, cerebral palsy, and gastric problems,” says Dr. Taylor. “Some are ventilator-dependent and need lots of care.”
She relishes the clinical discipline that being a hospitalist at an academic medical center presents. “I do my homework every day and enjoy the stimulation of teaching our house officers,” explains Dr. Taylor. “Working with adult learners on the chronic conditions we manage and the cases with puzzling symptoms is exciting.”
Dr. Taylor’s boss is this hospitalist program’s founder, Joseph Snitzer, MD (see “Joseph Snitzer, MD: A hospital medicine pioneer”). Being hospital-based frees Dr. Snitzer to observe an endless parade of clinical challenges, including complex rheumatology cases, lupus, tumors, infected shunts, seizures, exotic infections, oncology diagnoses, and more.
“People call us from rural hospitals and private practices for help with diagnoses,” explains Dr. Snitzer. “We’re not smarter than anyone else. We just see a lot more than most other physicians.”
Scottish Rite
Across town at Scottish Rite, a nonprofit hospital, the hospitalists cope with the demands of a steady influx of new Atlantans. David Hall, MD, is Scottish Rite’s medical director. He was a former Egleston hospitalist and a private practitioner for 10 years in Baltimore before he relocated to Atlanta.
“We don’t have house officers, and there is a resident on call only one night a week,” says Dr. Hall. “Pediatricians in the community need to have their patients admitted 24/7, and we also have to admit from the emergency department at night. With our hospitalists taking calls at night and working all the next day, sometimes they would be on for 36 hours straight. As our service has grown, we’ve realized that this model was not sustainable.”
To reduce the burnout from their growing patient loads, the hospitalists changed their model. As of August 1, 2005, hospitalists at Scottish Rite began working either eight- or 12-hour shifts.
“Until we gain some experience with the shift system, we know we will struggle with continuity and handoffs,” adds Dr. Hall. Scottish Rite is also increasing its complement of moonlighting private practice pediatricians who want to keep their hospital skills current by covering the heavy workload.
Dr. Hall says recruiting new hospitalists isn’t a problem. Many local physicians want to do this work—especially right after residency. Comparing being a hospitalist with his 10 years in private practice, he says, “In my office practice I’d be sitting 20 feet away from a colleague, and there wasn’t much interaction. Now I’m learning something new every day and discussing interesting patients with other doctors. Building these ongoing relationships is great.”
Benefits, Culture, and More
The compensation and benefits packages at Egleston and Scottish Rite reflect that they are two separate hospitals in one system. Egleston’s hospitalists are employed by the medical school and receive a straight salary, with no incentive or at risk components. Scottish Rite’s hospitalists are hospital employees and have 20% of their salary at risk with productivity, quality improvement, and patient satisfaction incentives.
Although the different compensation systems may lead to discrepancies in pay, Dr. Berkelhamer explains that the policy of Children’s Hospital of Atlanta is to offer market-based salaries to all hospitalists. “Part of my job is to ensure that Dr. Snitzer and Dr. Hall are empowered to hire the physicians they want,” he says.
The hospitals have different corporate cultures as well. “The Scottish Rite group is very comfortable with lots of hands-on work while those at Egleston like to spend more time teaching,” says Dr. Berkelhamer.
Dr. Taylor, who trained with Dr. Snitzer and had a private practice in Atlanta for five years before becoming a full-time Egleston hospitalist in 1993, also acknowledges the different cultures at Egleston and Scottish Rite.
“We are two hospitals that come to the table and work together,” she observes. “Although we are in separate locations and may approach things differently, we practice the same type of medicine.”
Dr. Berkelhamer, who works with both sets of hospitalists, reinforces the observation that their clinical practices are consistent: “Surveys on patient and community physician satisfaction are the same, as are outcomes and productivity data.”
Special Issues for Both Hospitals
As part of a growing medical specialty in a dynamic region of the country, hospitalists at Children’s Hospital of Atlanta must confront a number of issues—some unique to them, others that reflect national trends. With different compensation and productivity systems, the two sets of hospitalists must collaborate to practice one brand of medicine.
An important formal step in their collaboration is the computerized medical and order entry system scheduled for spring 2006 implementation. The hospitalists are working together to develop clinical pathways and standardized orders based on their culling through best practices and evidence-based medicine guidelines. A newly appointed chief quality officer will keep the project on track.
Atlanta’s growth presents other issues for the hospitalists. With a constant influx of new community-based pediatricians Dr. Taylor finds that the hospitalists sometimes have trouble communicating with them to coordinate care.
“There are now at least 1,000 primary care and subspecialty pediatricians in Atlanta,” she says. “Trying to build trust and to track personal preferences with so many doctors is difficult. Fortunately we have electronic medical records so we can share important data with them.”
The hospitals’ social workers and case managers represent added glue to hold the communication together. Another of Atlanta’s challenges: It has only two medical schools from which to draw local hospitalists and other pediatricians, Emory University and the smaller Morehouse University. While not insurmountable, it means that most pediatricians practicing in the area must relocate to Atlanta.
What the Future Holds
And then there are issues that transcend Atlanta. Dr. Snitzer feels the national movement for hospitalists to become a specialty will happen sooner rather than later. In line with that movement, Children’s Hospital of Atlanta will have its first hospitalist fellowship in 2007. (For more information on pediatric hospital medicine fellowships, see “Pediatric Fellowship Offered,” below.)
For Dr. Hall, hospitalist compensation in a boomtown rankles. “People can’t really make money being hospitalists,” he explains. “Most need some subsidy to keep the programs going.”
The pay issues are being addressed, albeit slowly. Dr. Hall is encouraged by the campaign of pediatric intensivists to have coding and payment upgrades; he sees it as a template for higher hospitalist reimbursement schedules. “We only get paid for one visit a day, but we often see a patient several times a day,” he says. “Reimbursement should reflect what we really do.”
Both hospitals will have new buildings, each with 250 beds, more surgical suites, and expanded emergency departments by early 2007. That should lead to more hospitalist hiring—not surprising for a hospital that pioneered having inpatient physicians more than 20 years ago. TH
Writer Marlene Piturro is based in New York.
PEDIATRIC SPECIAL SECTION:
NEWS
Pediatric Fellowship Offered
Children’s Hospitalists of San Diego offers program
The Pediatric Hospitalist program at Children’s Hospital and Health Center of San Diego (CHHC) began in 1978. The current hospitalists are employed by Children’s Specialists of San Diego (CSSD), a 180-member pediatric-only specialty medical group. Inpatient care is provided for 75% of all general pediatric patients at the 233-bed tertiary care CHHC. Program consultation is offered at nearby Palomar Medical Center, a 23-bed unit within a larger 319-bed community hospital with a trauma center.
The hospitalists are the primary teaching faculty for the house staff and medical students who come from the University of California San Diego (UCSD), Balboa Naval Hospital, Pendleton Naval Medical Center, and Scripps Family Medicine. All hospitalists are board-certified pediatricians and have additional degrees or postresidency training, such as chief residency or fellowship experience.
Hospitalists fulfill many leadership roles in the hospital and community when not on service. A detailed list is available in a previous issue of The Hospitalist (Nov/Dec 2004;8(6):59-60). Current research includes an Agency for Healthcare Research and Quality (AHRQ) safety grant on medication errors, a bronchiolitis clinical trial, juvenile justice research on hepatitis B, a Hispanic cultural competency grant from the California Endowment, spiratory syncytial virus immunoprophylaxis outcomes in a managed population, and primary care perceptions of pediatric dentistry. Thus the hospitalist program has a long history of strong commitment to children and the core aspects of pediatric hospital medicine.
The Fellowship
The CSSD Pediatric Hospitalist Fellowship Program goal is to train highly motivated pediatricians for careers in academic and clinical hospital medicine. Over a two-year period instruction is provided in clinical, advocacy, administrative, teaching, and research aspects of pediatric hospital medicine. Clinical education emphasizes inpatient acute care, including intensive care and emergency transport at the busy main campus at CHHC. Outpatient clinical care offers experiences in adolescent juvenile hall medicine, hospice, and child protection. The diverse clinical exposure, teaching from local and national leaders, and volume of patients ensure graduates of this program are well prepared for any clinical hospitalist position.
The staff gains administrative experience via both hospital and medical group quality improvement activities. This work is directed by the medical director for CSSD and the physician advisor for quality management for CHHC, both of whom are CSSD pediatric hospitalists. Skills in process improvement, continuous quality improvement, risk management, organizational management and leadership are honed during the fellowship. Opportunity exists to take courses through the American College of Physician Executives if the trainee desires a future in administrative hospitalist medicine.
Academics and teaching are a core value of the pediatric hospitalist service. The fellow participates in the monthly division journal club and internal case review. Daily teaching while on the clinical service includes bedside rounds, management rounds, and attending rounds. Pediatric hospitalists are the primary inpatient teaching staff and as such have a significant responsibility for daily house staff education. The fellow participates in noon conferences and other educational venues under the guidance of the director of inpatient teaching (also a pediatric hospitalist).
Advocacy skills are learned through experiences in the juvenile hall system, Center for Child Protection, the American Academy of Pediatrics (AAP), and at the local and state level for children’s services funding. Under the leadership of the medical directors for the Center for Child Protection and the A.B. and Jessie Polinsky Center for Abused Children, the fellow participates in case review and observes expert child abuse testimony in court. Discussions with legislators in Sacramento focus upon protection of the California Children’s Services system, which supports critically ill state-funded children. The fellow learns AAP local and national structure, participating in conferences and chapter events.
Research is expected during this two-year fellowship program. Formal clinical research training is part of the first year curriculum of UCSD’s Clinical Research Enhancement through Supplemental Training (CREST) program. The first year of this two-year CREST program includes weekly classes covering epidemiology, patient-oriented research, health services research, and informatics. Those dedicated to completion of a master’s degree during the two-year program may integrate this training with a more intense curriculum schedule. A research project and mentor is chosen after the first quarter of the first year. Research may be in any area of pediatric hospitalist medicine. Research is presented at either Pediatric Academic Societies, Society of Hospital Medicine, or other similar forum upon completion.
The schedule is flexible, but follows the template. (See Table 1, p. 30: “Pediatric Hospitalist Fellowship Program Schedule.”)
One fellowship position is offered every year, with application submissions accepted through Dec. 1, interviews granted Dec. 15-Feb. 1 and final selection by Feb. 15. You can obtain an application from the CSSD Web site “Fellowships” page (http://childrensspecialists. com/body.cfm?id=580) or by e-mailing Fellowship Coordinator Susan Stafford at sstafford@chsd.org.
PEDIATRIC SPECIAL SECTION:
IN THE LITERATURE
Retrospective Study Attempts Criteria for Diagnosing MAS
Reviews by Julia Simmons, MD
Ravelli A, Magni-Manzoni S, Pistorio A, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005;146(5):598-604.
Macrophage activating syndrome (MAS) is a complication of connective tissue disorders, most often associated with active systemic juvenile idiopathic arthritis (S-JIA). It is a rare disorder and the exact incidence is unknown. It is characterized by uncontrolled activation and proliferation of T-lymphocytes and macrophages. If not recognized and treated aggressively, MAS can be life threatening.
In this article, the authors’ purpose was to review the available clinical, laboratory, and histopathologic data in patients with active S-JIA and in those with active S-JIA complicated by MAS. The goal was to develop criteria to diagnose MAS.
The retrospective study was designed using the classification, criteria approach. The index cases included patients with MAS complicating S-JIA. The “confusable” condition was active S-JIA. There were 74 patients in the index cases. Seventeen of the cases were observed at the authors’ institution. These patients were diagnosed with S-JIA using the International League of Association for Rheumatology criteria. They were identified using a database search. Fifty-seven of the cases were obtained from a Medline search. Of these 74 patients, eight were disqualified because they did not meet the definition of S-JIA, and 11 were excluded because of insufficient data. The control group contained 37 patients observed at the authors’ sites. The sensitivity rate, specificity rate, area under receiver operating characteristic curve, and diagnostic odds ratio were applied to the data to differentiate MAS complicating S-JIA from S-JIA.
The study results found hemorrhages and central nervous dysfunction were the strongest clinical discriminating factors. The strongest laboratory discriminators included thrombocytopenia, leukopenia, elevated aspartate aminotransferase, and hypofibrinogenemia. Histopathological criterion included evidence of macrophage hemophagocytosis in the bone marrow aspirate. Other useful discriminators included hypertriglyceridemia, elevated ferritin, hepatomegaly, hand hyponatremia. Final guidelines were developed after analyzing the statistics and determining the clinical importance: “The diagnosis of MAS requires the presence of any two or more laboratory criteria or of any two or three or more clinical and/or laboratory criteria. A bone marrow aspirate for the demonstration of hemophagocytosis may be required only in doubtful cases.”
In summary, MAS complicating S-JIA is a disorder without concrete diagnostic criteria. The authors have performed preliminary studies to diagnose MAS. They appropriately recognized the need for prospective larger clinical studies.
HNL Helps Distinguish Infections
Fjaertoft G, Foucard T, Xu S, et al. Human neutrophil lipocalin (HNL) as a diagnostic tool in children with acute infections: a study of the kinetics. Acta Pediatrica costarricense. 2005;94:661-666.
In pediatrics, the clinician is often faced with the diagnostic challenge of differentiating a bacterial infectious process from a viral infection. History, physical exam, and laboratory data make the distinction. In this article, the authors’ purpose was to assess the kinetics of HNL with viral and bacterial infections. Further, they assess the response of HNL when the infection is treated with antibiotics. The response of HNL is compared with that of C-reactive protein.
In the study, 92 patients with a median age of 26 months were hospitalized because they required systemic antibiotics or because of the severity of their medical condition. Upon admission and on hospital days one, two, and three, the C-reactive protein, white blood cell count with differential, and HNL were measured. The patients were retrospectively classified into five groups: true bacterial infection (n=28), true viral infection (n=4), suspected bacterial infection (n=18), suspected viral (n=34), and other.
A true bacterial infection required bacterial isolation from blood, urine, or cerebrospinal fluid culture, or radiographic demonstration of pneumonia. Patients were classified as having a suspected bacterial infection if they had a nonspecific diagnosis, but an elevated C-reactive protein and erythrocyte sedimentation rate. A true viral infection required isolation of a virus. If a patient did not meet any of the above criteria, the person was classified as having a suspected viral infection. Those patients in the “other” group were diagnosed with Kawasaki disease, Borrelia meningitis, and one undiagnosed patient. The patients were classified using history, exam, and laboratory values including white blood cell count, erythrocyte sedimentation rate, C-reactive protein, and cultures. HNL values were not used in the classification.
The results demonstrated that both C-reactive protein and HNL are elevated with true bacterial infections compared with viral illnesses. Neither C-reactive protein nor HNL were significantly different in true bacterial infections versus suspected bacterial infections. The optimal cut-off for C-reactive protein was 59 mg/L with 93% sensitivity and 68% specificity. The optimal cutoff for HNL was 217 micrograms/L with 90% sensitivity and 74% specificity. In patients with true bacterial infections, HNL was highest at admission and decreased one day after admission. In contrast, the C-reactive protein values were similar on the day of admission and on hospital day one. C-reactive protein decreased significantly on days two and three of hospitalization. After hospital day one, HNL was elevated in only 11% of patients with true bacterial infection in contrast to 83% patients with elevated C-reactive protein.
In summary, HNL may be a useful marker to distinguish bacterial and viral illnesses. In comparison with C-reactive protein, it normalizes more rapidly after appropriate antibiotic therapy is initiated. In the future, HNL may be a useful marker in monitoring the response to antibiotic therapy.
CEDKA in Peds
Lawrence SE, Cummings EA, Gaboury I, et al. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. . 2005;146:688-692.
New onset insulin dependent diabetes mellitus is complicated by diabetic ketoacidosis (DKA) in 15% to 67% of patients. The incidence of cerebral edema in diabetic ketoacidosis (CEDKA) has been reported as 0.4-3.1. In the article, the authors seek to determine the incidence, outcome, and risk factors for cerebral edema in DKA in patients younger than 16.
The study was case-controlled with an active Canadian surveillance study. The authors surveyed pediatricians for a two-year period. During this time in Canada, all physicians were requested to submit reports monthly on patients with CEDKA younger than 16.
Thirteen cases were identified and the incidence of CEDKA was 0.51%. Overall mortality from cerebral edema was 0.15%. Increased blood urea nitrogen, degree of dehydration, hyperglycemia, and lower initial bicarbonate were associated with CEDKA. TH
In the flourishing metropolitan area of Atlanta, hospitalists and community-based physicians at Children’s Healthcare of Atlanta thrive within their niches, riding waves of opportunity fueled by the region’s burgeoning population. Jay Berkelhamer, MD, senior vice president of medical affairs at Children’s Healthcare of Atlanta calls his city “one of the most dynamic growth centers in the United States. Within 10 years we are estimated to have at least 150,000 more kids in Atlanta, leading to even greater opportunities for hospitalists and private practice primary care and specialty pediatricians.”
Two Hospitals, One system
Children’s Hospital of Atlanta’s hospitalist program is, in fact, two separate programs: one at Egleston, the other at Scottish Rite. The parent organization links the two and manages each hospital’s mission, structure, hiring, compensation, and outcomes.

—David Hall, MD
The six Egleston full-time equivalent hospitalists, or “cat herders,” as Corinne Taylor, MD, Egleston’s chief of medical affairs, describes them, are employees of Emory University Medical School. Most Egleston hospitalists are parents of young children and work four days a week, allowing them a balance of career and family life. Employed by the medical school and working at an academic medical center, they receive a salary, benefits, and other support services. Side by side with interns and residents, Egleston’s hospitalists see Atlanta’s sickest, frailest, and most at-risk children: the uninsured, underinsured immigrant and local population.
At Egleston the pediatric hospitalists are like their counterparts who treat adult patients in other settings. They deal with many patients with chronic conditions that lead to repeat hospitalizations.
“We see lots of ex-preemies with multiple problems such as asthma, seizures, cerebral palsy, and gastric problems,” says Dr. Taylor. “Some are ventilator-dependent and need lots of care.”
She relishes the clinical discipline that being a hospitalist at an academic medical center presents. “I do my homework every day and enjoy the stimulation of teaching our house officers,” explains Dr. Taylor. “Working with adult learners on the chronic conditions we manage and the cases with puzzling symptoms is exciting.”
Dr. Taylor’s boss is this hospitalist program’s founder, Joseph Snitzer, MD (see “Joseph Snitzer, MD: A hospital medicine pioneer”). Being hospital-based frees Dr. Snitzer to observe an endless parade of clinical challenges, including complex rheumatology cases, lupus, tumors, infected shunts, seizures, exotic infections, oncology diagnoses, and more.
“People call us from rural hospitals and private practices for help with diagnoses,” explains Dr. Snitzer. “We’re not smarter than anyone else. We just see a lot more than most other physicians.”
Scottish Rite
Across town at Scottish Rite, a nonprofit hospital, the hospitalists cope with the demands of a steady influx of new Atlantans. David Hall, MD, is Scottish Rite’s medical director. He was a former Egleston hospitalist and a private practitioner for 10 years in Baltimore before he relocated to Atlanta.
“We don’t have house officers, and there is a resident on call only one night a week,” says Dr. Hall. “Pediatricians in the community need to have their patients admitted 24/7, and we also have to admit from the emergency department at night. With our hospitalists taking calls at night and working all the next day, sometimes they would be on for 36 hours straight. As our service has grown, we’ve realized that this model was not sustainable.”
To reduce the burnout from their growing patient loads, the hospitalists changed their model. As of August 1, 2005, hospitalists at Scottish Rite began working either eight- or 12-hour shifts.
“Until we gain some experience with the shift system, we know we will struggle with continuity and handoffs,” adds Dr. Hall. Scottish Rite is also increasing its complement of moonlighting private practice pediatricians who want to keep their hospital skills current by covering the heavy workload.
Dr. Hall says recruiting new hospitalists isn’t a problem. Many local physicians want to do this work—especially right after residency. Comparing being a hospitalist with his 10 years in private practice, he says, “In my office practice I’d be sitting 20 feet away from a colleague, and there wasn’t much interaction. Now I’m learning something new every day and discussing interesting patients with other doctors. Building these ongoing relationships is great.”
Benefits, Culture, and More
The compensation and benefits packages at Egleston and Scottish Rite reflect that they are two separate hospitals in one system. Egleston’s hospitalists are employed by the medical school and receive a straight salary, with no incentive or at risk components. Scottish Rite’s hospitalists are hospital employees and have 20% of their salary at risk with productivity, quality improvement, and patient satisfaction incentives.
Although the different compensation systems may lead to discrepancies in pay, Dr. Berkelhamer explains that the policy of Children’s Hospital of Atlanta is to offer market-based salaries to all hospitalists. “Part of my job is to ensure that Dr. Snitzer and Dr. Hall are empowered to hire the physicians they want,” he says.
The hospitals have different corporate cultures as well. “The Scottish Rite group is very comfortable with lots of hands-on work while those at Egleston like to spend more time teaching,” says Dr. Berkelhamer.
Dr. Taylor, who trained with Dr. Snitzer and had a private practice in Atlanta for five years before becoming a full-time Egleston hospitalist in 1993, also acknowledges the different cultures at Egleston and Scottish Rite.
“We are two hospitals that come to the table and work together,” she observes. “Although we are in separate locations and may approach things differently, we practice the same type of medicine.”
Dr. Berkelhamer, who works with both sets of hospitalists, reinforces the observation that their clinical practices are consistent: “Surveys on patient and community physician satisfaction are the same, as are outcomes and productivity data.”
Special Issues for Both Hospitals
As part of a growing medical specialty in a dynamic region of the country, hospitalists at Children’s Hospital of Atlanta must confront a number of issues—some unique to them, others that reflect national trends. With different compensation and productivity systems, the two sets of hospitalists must collaborate to practice one brand of medicine.
An important formal step in their collaboration is the computerized medical and order entry system scheduled for spring 2006 implementation. The hospitalists are working together to develop clinical pathways and standardized orders based on their culling through best practices and evidence-based medicine guidelines. A newly appointed chief quality officer will keep the project on track.
Atlanta’s growth presents other issues for the hospitalists. With a constant influx of new community-based pediatricians Dr. Taylor finds that the hospitalists sometimes have trouble communicating with them to coordinate care.
“There are now at least 1,000 primary care and subspecialty pediatricians in Atlanta,” she says. “Trying to build trust and to track personal preferences with so many doctors is difficult. Fortunately we have electronic medical records so we can share important data with them.”
The hospitals’ social workers and case managers represent added glue to hold the communication together. Another of Atlanta’s challenges: It has only two medical schools from which to draw local hospitalists and other pediatricians, Emory University and the smaller Morehouse University. While not insurmountable, it means that most pediatricians practicing in the area must relocate to Atlanta.
What the Future Holds
And then there are issues that transcend Atlanta. Dr. Snitzer feels the national movement for hospitalists to become a specialty will happen sooner rather than later. In line with that movement, Children’s Hospital of Atlanta will have its first hospitalist fellowship in 2007. (For more information on pediatric hospital medicine fellowships, see “Pediatric Fellowship Offered,” below.)
For Dr. Hall, hospitalist compensation in a boomtown rankles. “People can’t really make money being hospitalists,” he explains. “Most need some subsidy to keep the programs going.”
The pay issues are being addressed, albeit slowly. Dr. Hall is encouraged by the campaign of pediatric intensivists to have coding and payment upgrades; he sees it as a template for higher hospitalist reimbursement schedules. “We only get paid for one visit a day, but we often see a patient several times a day,” he says. “Reimbursement should reflect what we really do.”
Both hospitals will have new buildings, each with 250 beds, more surgical suites, and expanded emergency departments by early 2007. That should lead to more hospitalist hiring—not surprising for a hospital that pioneered having inpatient physicians more than 20 years ago. TH
Writer Marlene Piturro is based in New York.
PEDIATRIC SPECIAL SECTION:
NEWS
Pediatric Fellowship Offered
Children’s Hospitalists of San Diego offers program
The Pediatric Hospitalist program at Children’s Hospital and Health Center of San Diego (CHHC) began in 1978. The current hospitalists are employed by Children’s Specialists of San Diego (CSSD), a 180-member pediatric-only specialty medical group. Inpatient care is provided for 75% of all general pediatric patients at the 233-bed tertiary care CHHC. Program consultation is offered at nearby Palomar Medical Center, a 23-bed unit within a larger 319-bed community hospital with a trauma center.
The hospitalists are the primary teaching faculty for the house staff and medical students who come from the University of California San Diego (UCSD), Balboa Naval Hospital, Pendleton Naval Medical Center, and Scripps Family Medicine. All hospitalists are board-certified pediatricians and have additional degrees or postresidency training, such as chief residency or fellowship experience.
Hospitalists fulfill many leadership roles in the hospital and community when not on service. A detailed list is available in a previous issue of The Hospitalist (Nov/Dec 2004;8(6):59-60). Current research includes an Agency for Healthcare Research and Quality (AHRQ) safety grant on medication errors, a bronchiolitis clinical trial, juvenile justice research on hepatitis B, a Hispanic cultural competency grant from the California Endowment, spiratory syncytial virus immunoprophylaxis outcomes in a managed population, and primary care perceptions of pediatric dentistry. Thus the hospitalist program has a long history of strong commitment to children and the core aspects of pediatric hospital medicine.
The Fellowship
The CSSD Pediatric Hospitalist Fellowship Program goal is to train highly motivated pediatricians for careers in academic and clinical hospital medicine. Over a two-year period instruction is provided in clinical, advocacy, administrative, teaching, and research aspects of pediatric hospital medicine. Clinical education emphasizes inpatient acute care, including intensive care and emergency transport at the busy main campus at CHHC. Outpatient clinical care offers experiences in adolescent juvenile hall medicine, hospice, and child protection. The diverse clinical exposure, teaching from local and national leaders, and volume of patients ensure graduates of this program are well prepared for any clinical hospitalist position.
The staff gains administrative experience via both hospital and medical group quality improvement activities. This work is directed by the medical director for CSSD and the physician advisor for quality management for CHHC, both of whom are CSSD pediatric hospitalists. Skills in process improvement, continuous quality improvement, risk management, organizational management and leadership are honed during the fellowship. Opportunity exists to take courses through the American College of Physician Executives if the trainee desires a future in administrative hospitalist medicine.
Academics and teaching are a core value of the pediatric hospitalist service. The fellow participates in the monthly division journal club and internal case review. Daily teaching while on the clinical service includes bedside rounds, management rounds, and attending rounds. Pediatric hospitalists are the primary inpatient teaching staff and as such have a significant responsibility for daily house staff education. The fellow participates in noon conferences and other educational venues under the guidance of the director of inpatient teaching (also a pediatric hospitalist).
Advocacy skills are learned through experiences in the juvenile hall system, Center for Child Protection, the American Academy of Pediatrics (AAP), and at the local and state level for children’s services funding. Under the leadership of the medical directors for the Center for Child Protection and the A.B. and Jessie Polinsky Center for Abused Children, the fellow participates in case review and observes expert child abuse testimony in court. Discussions with legislators in Sacramento focus upon protection of the California Children’s Services system, which supports critically ill state-funded children. The fellow learns AAP local and national structure, participating in conferences and chapter events.
Research is expected during this two-year fellowship program. Formal clinical research training is part of the first year curriculum of UCSD’s Clinical Research Enhancement through Supplemental Training (CREST) program. The first year of this two-year CREST program includes weekly classes covering epidemiology, patient-oriented research, health services research, and informatics. Those dedicated to completion of a master’s degree during the two-year program may integrate this training with a more intense curriculum schedule. A research project and mentor is chosen after the first quarter of the first year. Research may be in any area of pediatric hospitalist medicine. Research is presented at either Pediatric Academic Societies, Society of Hospital Medicine, or other similar forum upon completion.
The schedule is flexible, but follows the template. (See Table 1, p. 30: “Pediatric Hospitalist Fellowship Program Schedule.”)
One fellowship position is offered every year, with application submissions accepted through Dec. 1, interviews granted Dec. 15-Feb. 1 and final selection by Feb. 15. You can obtain an application from the CSSD Web site “Fellowships” page (http://childrensspecialists. com/body.cfm?id=580) or by e-mailing Fellowship Coordinator Susan Stafford at sstafford@chsd.org.
PEDIATRIC SPECIAL SECTION:
IN THE LITERATURE
Retrospective Study Attempts Criteria for Diagnosing MAS
Reviews by Julia Simmons, MD
Ravelli A, Magni-Manzoni S, Pistorio A, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005;146(5):598-604.
Macrophage activating syndrome (MAS) is a complication of connective tissue disorders, most often associated with active systemic juvenile idiopathic arthritis (S-JIA). It is a rare disorder and the exact incidence is unknown. It is characterized by uncontrolled activation and proliferation of T-lymphocytes and macrophages. If not recognized and treated aggressively, MAS can be life threatening.
In this article, the authors’ purpose was to review the available clinical, laboratory, and histopathologic data in patients with active S-JIA and in those with active S-JIA complicated by MAS. The goal was to develop criteria to diagnose MAS.
The retrospective study was designed using the classification, criteria approach. The index cases included patients with MAS complicating S-JIA. The “confusable” condition was active S-JIA. There were 74 patients in the index cases. Seventeen of the cases were observed at the authors’ institution. These patients were diagnosed with S-JIA using the International League of Association for Rheumatology criteria. They were identified using a database search. Fifty-seven of the cases were obtained from a Medline search. Of these 74 patients, eight were disqualified because they did not meet the definition of S-JIA, and 11 were excluded because of insufficient data. The control group contained 37 patients observed at the authors’ sites. The sensitivity rate, specificity rate, area under receiver operating characteristic curve, and diagnostic odds ratio were applied to the data to differentiate MAS complicating S-JIA from S-JIA.
The study results found hemorrhages and central nervous dysfunction were the strongest clinical discriminating factors. The strongest laboratory discriminators included thrombocytopenia, leukopenia, elevated aspartate aminotransferase, and hypofibrinogenemia. Histopathological criterion included evidence of macrophage hemophagocytosis in the bone marrow aspirate. Other useful discriminators included hypertriglyceridemia, elevated ferritin, hepatomegaly, hand hyponatremia. Final guidelines were developed after analyzing the statistics and determining the clinical importance: “The diagnosis of MAS requires the presence of any two or more laboratory criteria or of any two or three or more clinical and/or laboratory criteria. A bone marrow aspirate for the demonstration of hemophagocytosis may be required only in doubtful cases.”
In summary, MAS complicating S-JIA is a disorder without concrete diagnostic criteria. The authors have performed preliminary studies to diagnose MAS. They appropriately recognized the need for prospective larger clinical studies.
HNL Helps Distinguish Infections
Fjaertoft G, Foucard T, Xu S, et al. Human neutrophil lipocalin (HNL) as a diagnostic tool in children with acute infections: a study of the kinetics. Acta Pediatrica costarricense. 2005;94:661-666.
In pediatrics, the clinician is often faced with the diagnostic challenge of differentiating a bacterial infectious process from a viral infection. History, physical exam, and laboratory data make the distinction. In this article, the authors’ purpose was to assess the kinetics of HNL with viral and bacterial infections. Further, they assess the response of HNL when the infection is treated with antibiotics. The response of HNL is compared with that of C-reactive protein.
In the study, 92 patients with a median age of 26 months were hospitalized because they required systemic antibiotics or because of the severity of their medical condition. Upon admission and on hospital days one, two, and three, the C-reactive protein, white blood cell count with differential, and HNL were measured. The patients were retrospectively classified into five groups: true bacterial infection (n=28), true viral infection (n=4), suspected bacterial infection (n=18), suspected viral (n=34), and other.
A true bacterial infection required bacterial isolation from blood, urine, or cerebrospinal fluid culture, or radiographic demonstration of pneumonia. Patients were classified as having a suspected bacterial infection if they had a nonspecific diagnosis, but an elevated C-reactive protein and erythrocyte sedimentation rate. A true viral infection required isolation of a virus. If a patient did not meet any of the above criteria, the person was classified as having a suspected viral infection. Those patients in the “other” group were diagnosed with Kawasaki disease, Borrelia meningitis, and one undiagnosed patient. The patients were classified using history, exam, and laboratory values including white blood cell count, erythrocyte sedimentation rate, C-reactive protein, and cultures. HNL values were not used in the classification.
The results demonstrated that both C-reactive protein and HNL are elevated with true bacterial infections compared with viral illnesses. Neither C-reactive protein nor HNL were significantly different in true bacterial infections versus suspected bacterial infections. The optimal cut-off for C-reactive protein was 59 mg/L with 93% sensitivity and 68% specificity. The optimal cutoff for HNL was 217 micrograms/L with 90% sensitivity and 74% specificity. In patients with true bacterial infections, HNL was highest at admission and decreased one day after admission. In contrast, the C-reactive protein values were similar on the day of admission and on hospital day one. C-reactive protein decreased significantly on days two and three of hospitalization. After hospital day one, HNL was elevated in only 11% of patients with true bacterial infection in contrast to 83% patients with elevated C-reactive protein.
In summary, HNL may be a useful marker to distinguish bacterial and viral illnesses. In comparison with C-reactive protein, it normalizes more rapidly after appropriate antibiotic therapy is initiated. In the future, HNL may be a useful marker in monitoring the response to antibiotic therapy.
CEDKA in Peds
Lawrence SE, Cummings EA, Gaboury I, et al. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. . 2005;146:688-692.
New onset insulin dependent diabetes mellitus is complicated by diabetic ketoacidosis (DKA) in 15% to 67% of patients. The incidence of cerebral edema in diabetic ketoacidosis (CEDKA) has been reported as 0.4-3.1. In the article, the authors seek to determine the incidence, outcome, and risk factors for cerebral edema in DKA in patients younger than 16.
The study was case-controlled with an active Canadian surveillance study. The authors surveyed pediatricians for a two-year period. During this time in Canada, all physicians were requested to submit reports monthly on patients with CEDKA younger than 16.
Thirteen cases were identified and the incidence of CEDKA was 0.51%. Overall mortality from cerebral edema was 0.15%. Increased blood urea nitrogen, degree of dehydration, hyperglycemia, and lower initial bicarbonate were associated with CEDKA. TH
The Role of Hospitalists in Stroke Management
Distinguishing the evolving role of the hospitalist in managing patients with stroke requires exploring a number of challenges, a couple of controversies, and some clear opportunities.
Challenges
Hospitalists and their specialist colleagues face a number of challenges associated with stroke management, including the nature of provider teamwork, whether patients present within the window of time for thrombolytic administration, whether hospitalists should administer those agents, and also the care of patients with intracerebral hemorrhage (ICH).
Specialty Support
Traditionally the neurologist has been the key clinician involved in the diagnosis and treatment of patients with stroke. And because a great many neurologists prefer to practice almost exclusively in the outpatient setting, a team of providers in the hospital must handle the current stroke care volume.
“Coming to the hospital can be a challenge for some of them, although there is a subset of neurologists who really like to be inside the hospital and look after acute issues with respect to neurology,” says Sandeep Sachdeva, MD, Swedish Medical Center in Seattle. “In our institution we’ve had enough neurologists, but most of them are busy with their outpatient practices so they’re not able to spend substantial time [in the hospital]. By default we have to look at the hospitalist program here as a resource for taking care of stroke patients.”1
Emergent evaluation and treatment of acute ischemic stroke is a hot-button issue, especially for community-based hospitals. Some neurologists can leave their office and attend to an acute ischemic stroke presenting to the emergency department, while others can’t. To address this issue some hospitals have developed stroke teams that usually consist of highly trained nurses/advanced registered nurse practitioners (ARNPs) working under the direction of a neurologist, as is the case at Swedish Medical Center. These stroke teams respond to acute strokes presenting in the emergency department and then assist the emergency department physician in expediting the patient evaluation and ensuring that no protocol violation occurs while emergent therapy, such as IV tPA, is administered.
The final decision for administering this medication rests with the emergency department physician and, in some instances, with the neurologist if he or she is able to evaluate the patient in the emergency department. Hospitalists must evaluate their comfort level, knowledge, and experience—and then discuss with their neurologists and emergency department physicians the development of—a care algorithm commensurate with national and local standards of care as it pertains to caring for patients who present with acute stroke.
With relatively little specialty support available, it becomes more important for communication between providers to be clear and reliable; and practitioners must determine the local standard of care.
“I think with stroke it’s a particularly vexing issue, especially when you get outside of metropolitan areas,” says Larry Goldstein, MD, director of the Duke University Stroke Center, Durham, N.C. “In metropolitan areas there may be hospitals with different capabilities that are not too far from one another. And it may make sense in that situation for one hospital to decide on their own: ‘We just don’t have the resources to be able to treat a specific condition, … and it might be better … for patients to not come here for that since we can’t offer the appropriate level of care for that condition.’”
But in rural and other less populated areas, he says “ … that community hospital may be the only game in town. And even though they … wouldn’t have everything that a tertiary care [or] quaternary care academic center would have, they could identify areas that are critically important for the acute care patients they are serving and develop the appropriate levels of competency in that area.”
Administering Thrombolytics
What is the standard by which an individual hospitalist is expected to practice, especially concerning the administration of tPA?
In that regard—without a doubt—patient safety comes first. “Whenever there’s confusion in my mind, I always think … first, do no harm,” says Dr. Sachdeva. “If this is an urban area and other hospitalists are not [administering] tPA, then they are not expected to do so and that may not meet the standard of care for that area. Rural hospitals have successfully been giving tPA to patients with acute ischemic stroke.
The caveat here is that appropriate planning as well as training of caregivers has to take place prior to starting IV tPA administration. “Rural hospitals that have the IV tPA capability usually do so in collaboration with larger regional institutions, academic or otherwise, where services of neurologists and neurosurgeons are available,” says Dr. Sachdeva. “Size of the institution should not be an impediment to IV tPA administration.”
As baby boomers age, the demand for better stroke care will increase, and hospitals as well as caregivers need to be prepared to meet the expectations of patients.
David Thurber, MD, medical director of the Cary Hospital Medicine Service, a division of Wake Medical Center, Cary, N.C., speaks of the need for specialty backup at community hospitals.
“For those people who practice in community hospitals, including myself,” he says, “it’s like being the pitcher on a baseball team: If you can’t field the outfield, you shouldn’t be pitching the ball because there’s nobody out there to catch it. So if you can’t get the backup of a neurologist, or of a neurosurgeon in the case of hemorrhagic stroke, in my opinion you have no business pushing tPA. Your obligation is to try, as many community hospitals have done with invasive cardiac procedures, such as emergent use of percutaneous coronary artery intervention, to transfer the patient to a facility where those can be done in a timely fashion.”
What should hospitalists do if they are expected to administer tPA and are unsure of their skill level?
“I would take this issue back to the administration of the hospital,” says Dr. Sachdeva, “and come up with a plan where the neurologists or the emergency department physicians feel motivated to give tPA.”
The most important element to consider when making the decision of whether to administer tPA is the quality of the history. “If there is any doubt about the time or the mechanism of stroke onset, then as practitioners we are very well justified in not giving tPA,” says Dr. Sachdeva, who believes there are more lawsuits for not giving tPA than for giving it. But if you withhold tPA and justify the decision with appropriate reasoning, that certainly places the individual on steadier legal ground.
Training and Competence
Stroke management is not a universally strong topic in medical education. “Not every medical school requires a rotation in the neurosciences or exposure to stroke treatment,” says Dr. Goldstein, “and it’s the same thing in residency programs, depending on which residency program you go through, be it as an internist or as an emergency physician. … So it begins in medical school and follows through residency, but as we know, our training only begins in those formal settings. In medicine, training is a lifelong activity. Things change all the time. And it would [take] appropriate levels of continuing education directly related to cerebrovascular disease to be able to understand modern diagnosis and modern therapeutics.”
Another issue is whether an institution will receive patients for stroke treatment. “Just as hospitals credential people to [perform] procedures, not every hospital can offer every therapy to every patient at the same level,” says Dr. Goldstein. “The thing that is inappropriate is to force people to do things for which they’re not trained.”
Although that is also partially an institutional decision, “institutions can’t have it both ways,” he explains. “They can’t say well, we’re going to be taking care of patients with X, Y, or Z, but then not have the facilities and personnel available to be able to acutely treat and stabilize patients even if they do require more advanced care somewhere else.”
Dr. Sachdeva’s team had to cover a considerable knowledge gap to bring his colleagues up to speed and competence by talking directly to the hospitalists and arranging CMEs for them, as well as by encouraging them to get certified in using the National Institutes of Health (NIH) stroke scale.
“The key is for hospitalists to make sure when they’re taking on an area of patient care that they feel comfortable doing that and not themselves be the default for any medical or surgical conditions,” says David Likosky, MD, who is board certified in neurology and internal medicine, and is the director of the Stroke Program of Evergreen Healthcare, Kirkland, Wash.
One way to become better prepared to manage stroke is to familiarize oneself with the National Institutes of Health (NIH) stroke scale. Online training for the NIH Stroke Scale (approved for two hours of category 1 CME credit from the NIH) is available at www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf.).
Excellent resources for developing protocols include the American Stroke Association/American Heart Association, the work of the Brain Attack Coalition (a group of professional, voluntary, and governmental entities dedicated to reducing the occurrence, disabilities, and death associated with stroke—www.stroke-site.org/), and the Web site (www.strokecenter.org), produced out of Washington University in St. Louis. SHM (www.hospitalmedicine.org), which is in the process of creating a Web-based stroke resource room, which—at press time—was scheduled to be live by August 1.
—David Thurber, MD
Systems and Monitoring
Having the right systems in place enables smooth patient assessment and treatment. First establish a means for education in stroke care for hospitalists and all support staff. Other important systems include having protocols for admitting [patients] for stroke care; setting up communication pathways for various disciplines involved in stroke care; having systems to gather, analyze, and monitor data; and having particularly good teamwork and response time.
William Likosky, MD, director of the Stroke Program at the Swedish Medical Center, Seattle, strongly believes in systems and processes of care, whereby a well-designed system should not only be able to prevent mistakes by an individual caregiver, but also to facilitate optimal evidence-based care in every case. As an institution Swedish Medical draws inspiration from the Institute of Healthcare Improvement’s campaign to prevent 100,000 avoidable deaths nationwide in its hospitalized patients. Since its inception at Swedish Medical two years ago, the stroke program is credited with preventing 22 deaths.
Of course any protocol’s worth will vary according to the effectiveness with which it is implemented. Developing protocols and care pathways is an avenue for hospitalists to take a leadership role in implementing evidence-based care, in co-ordinating care between different services, and eventually affecting resource utilization, quality of care, and patient satisfaction positively.
Protocols or pathways fail when they’re not patient-centered, when input isn’t solicited from other caregivers during the development phase, or when their implementation is not monitored. To Dr. Sachdeva, “the main issue is how you implement [the protocol], how you monitor the implementation, and how you fix the glitches or the problems that usually ensue when you’re rolling out a new protocol.”
Response and Feedback
Another imperative of any stroke program is its response time. “We monitor very closely our emergency department evaluation times for patients coming in within the window for giving tPA,” says Dr. Sachdeva. “We are strict about this because we want every patient to be evaluated within 45 minutes—anybody who is a candidate for possible intervention with acute thrombolytics—either IV or IA. Those times are monitored, and any time that 45-minute window is missed, we have an individual conversation with the people who were responsible, not as a confrontation, but [to ask], ‘What can we do to help you?’ And each time we do that we learn something new.
“Usually in these cases, there were things that were happening that were out of control and sometimes you can control them and sometimes you can’t,” he says. “Next time we try to manage the variables better. So we do have a hands-on continuous monitoring process that is not intrusive, and it gives us an idea of how we are holding up with certain quality parameters.”
Teamwork and Communication
One of the important systems is how well all involved work as a team. “Most of the time, IV tPA is given in the emergency department and the emergency department doctors now are very comfortable giving IV tPA with the telephonic help from a neurologist,” says Dr. Sachdeva. “But they also receive assistance from the stroke nurse, who consults on every stroke patient who is a candidate for emergent intervention in the emergency department.”
Swedish Medical maintains dedicated stroke nurses who act as facilitators to ensure everybody holds up their end of the bargain in stroke care. This includes a combination of nurses and nurse practitioners. But ultimately it is the emergency department physician’s decision in consultation with the neurologist by phone.
Part of their facilitation involves negotiating to cut down on time. “We don’t … rush our patients, but we cut down on avoidable delays,” says Dr. Sachdeva. “We try to get all the pertinent workup done as fast as we can, and then collate the data, make sure the data are disseminated to the parties that need the data, and decisions are made and appropriate treatment algorithms applied.”
These dedicated nurses are available in person for any acute stroke that falls within the window for an emergent intervention. “But if it is [an] acute stroke outside the window,” says Dr. Sachdeva, “they will consult telephonically to help you get certain things started, and then consult on the patient the next business day. They are available 24/7 both to the emergency department and to any floor area of the hospital. Anyplace that stroke can happen … they are there in a heartbeat. And the stroke nurses have been invaluable in assisting the hospitalists in day-to-day care of the stroke patients as well as in educating patients and their families.”
Controversies in Stroke Management
Although many hospitalists are uncomfortable treating ischemic strokes, far more may show discomfort at the idea of treating hemorrhagic strokes.
“Bleeding within the head carries a morbidity and mortality that sometimes is exaggerated in terms of its perception,” he says, “and once again, one has to look at the training that was given to most hospitalists during their residency. It was insufficient with respect to managing intracranial hemorrhages.”
Treating hemorrhagic strokes has traditionally been the preserve of neurosurgeons. “Some neurosurgeons are of the opinion that if there is no indication for surgical intervention for a particular ICH case, then the patient should be on the medical service,” says Dr. Sachdeva. “The medical side is feeling thoroughly unprepared to handle these.”
His team is looking at this issue at their institution to come up with appropriate algorithms regarding triage and care of patients with ICH.
Hospitalists and Stroke Management: Opportunities
One advantage of the hospitalist system in managing stroke is that hospitalists are readily available. Monitoring patients’ recovery for any emergent complications is also an important role for the hospitalist. Most often these complications are urinary tract infections, aspiration pneumonia, and deep venous thrombosis.
The team at Swedish refers to these high-risk complications as “dashboards,” likening them to the dashboard of an automobile that must be carefully watched.
Swedish Medical has seven markers for quality of care that the stroke team monitors. They have a statistician, people who gather the data, people who analyze the data, and those who then put the data in a graph format for the team to review trends reflecting quality of care.
This secondary prevention comes into play while coordinating care at the time of discharge. Hospitalists can start the ball rolling so a primary care physician or the facility to which the patient may next be transferred will continue the appropriate care for these patients.
Hospitalists could also take leadership role within their institutions in formulating pathways for emergent evaluation of strokes that occur in hospitalized patients.
“This is what most hospitalists should be able to do with adequate training,” says Dr. Sachdeva. “At the very least, hospitalists can positively impact stroke care by setting into place protocols, processes, and systems of care to ensure prevention DVTs, UTIs, aspiration pneumonias, and initiation of appropriate secondary prevention modalities for patients admitted with a diagnosis of stroke.”
Any institution that prevents these complications from developing should see an automatic benefit of those quality parameters in decreased length of stay, decreased utilization of resources, and improved patient satisfaction.
Follow-Up and Compliance
Having the undivided attention of the patient and his or her family at the time of hospitalization is a golden opportunity.
“We start patients on a vigorous, evidence-based secondary prevention regimen and by opening a dialogue with the patient and the family,” says Dr. Sachdeva. “Realize you’ve started something good; it needs to be followed up and reinforced on a regular basis either through their primary care provider or through a dedicated stroke follow-up clinic.”
The plan for handling a potential future brain attack is also outlined. One of the most noteworthy programs for secondary prevention of strokes is the one out of the University of California, Los Angeles called PROTECT—Preventing Recurrence of Thromboembolic Events through Coordinated Treatment (http://strokeprotect.mednet.ucla.edu/). (See p. 22.)2
Dr. Thurber, who is also president of the Piedmont Chapter of SHM, hopes that secondary prevention work by stroke teams around the country and the results of public education campaigns can help reduce the number of patients who present for stroke treatment outside the time window for thrombolytic therapy.
Communication with PCPs
If you have a dedicated group of primary care physicians that you work with, then they are, in effect, your customers. They should develop that program so they can give their input as how they would like communication and they can know what kind of care their patients will receive once admitted to the hospitalists or the hospitalist-neurologist team.
Call the primary care physicians at the time of discharge in order to convey the highlights of hospitalization and review key follow-up issues. Information can fall through the cracks, but the PROTECT program shows that this is rare if you use the tools provided as part of the program.1 Their data show that initiating secondary prevention modalities while the patient is hospitalized is important, but following up on them is just as important to good outcomes.
The discharging physician must partner with the primary care providers to maintain the momentum with respect to secondary prevention, re-enforcing education, and monitoring for development of side effects from the medications initiated during hospitalization.
Future Trends
Given the trends of an expanding hospitalist system, increasing time limitations for specialists, the relative dearth of neurologists, and uninviting circumstances for practice and compensation, neurologists will need to partner with a group of physicians who are structured to be available 24/7.
In his coauthored letter to the editor of Stroke, published in June 2005, Dr. Likosky challenged neurologists to avoid being “asleep at the wheel” in stroke prevention.1 “If neurologists want to be the ones taking care of stroke patients,” he said, “then they need to decide what role they want to play, because otherwise it’s going to be taken over by hospitalists, which may be the most appropriate thing.”
Conclusion
Challenges and opportunities characterize the work of hospitalists involved in stroke care. Good, ongoing training is imperative as are effective institutional systems and efficient monitoring of those systems. Protocols can be adapted to best serve an individual institution; the nature of their implementation and the teamwork or lack thereof will make the difference in the benefit to medical and institutional outcomes.
Recommendations for best performance in stroke care include keeping open channels of communication and good feedback systems, discussing controversies in order to seek resolutions and improve systems, and using the advantage of access to patients and their families to best begin follow-up and secondary prevention efforts. TH
Writer Andrea M. Sattinger will cover the malpractice crisis in healthcare in future issues of The Hospitalist.
References
- Likosky DJ. Who will care for our hospitalized patients? Stroke. 2005;36:1113-1114.
- Ovbiagele B, Saver JL, Fredieu A, et al. PROTECT: A coordinated stroke treatment program to prevent recurrent thromboembolic events. Neurology. 2004;63:1217-1222.
Distinguishing the evolving role of the hospitalist in managing patients with stroke requires exploring a number of challenges, a couple of controversies, and some clear opportunities.
Challenges
Hospitalists and their specialist colleagues face a number of challenges associated with stroke management, including the nature of provider teamwork, whether patients present within the window of time for thrombolytic administration, whether hospitalists should administer those agents, and also the care of patients with intracerebral hemorrhage (ICH).
Specialty Support
Traditionally the neurologist has been the key clinician involved in the diagnosis and treatment of patients with stroke. And because a great many neurologists prefer to practice almost exclusively in the outpatient setting, a team of providers in the hospital must handle the current stroke care volume.
“Coming to the hospital can be a challenge for some of them, although there is a subset of neurologists who really like to be inside the hospital and look after acute issues with respect to neurology,” says Sandeep Sachdeva, MD, Swedish Medical Center in Seattle. “In our institution we’ve had enough neurologists, but most of them are busy with their outpatient practices so they’re not able to spend substantial time [in the hospital]. By default we have to look at the hospitalist program here as a resource for taking care of stroke patients.”1
Emergent evaluation and treatment of acute ischemic stroke is a hot-button issue, especially for community-based hospitals. Some neurologists can leave their office and attend to an acute ischemic stroke presenting to the emergency department, while others can’t. To address this issue some hospitals have developed stroke teams that usually consist of highly trained nurses/advanced registered nurse practitioners (ARNPs) working under the direction of a neurologist, as is the case at Swedish Medical Center. These stroke teams respond to acute strokes presenting in the emergency department and then assist the emergency department physician in expediting the patient evaluation and ensuring that no protocol violation occurs while emergent therapy, such as IV tPA, is administered.
The final decision for administering this medication rests with the emergency department physician and, in some instances, with the neurologist if he or she is able to evaluate the patient in the emergency department. Hospitalists must evaluate their comfort level, knowledge, and experience—and then discuss with their neurologists and emergency department physicians the development of—a care algorithm commensurate with national and local standards of care as it pertains to caring for patients who present with acute stroke.
With relatively little specialty support available, it becomes more important for communication between providers to be clear and reliable; and practitioners must determine the local standard of care.
“I think with stroke it’s a particularly vexing issue, especially when you get outside of metropolitan areas,” says Larry Goldstein, MD, director of the Duke University Stroke Center, Durham, N.C. “In metropolitan areas there may be hospitals with different capabilities that are not too far from one another. And it may make sense in that situation for one hospital to decide on their own: ‘We just don’t have the resources to be able to treat a specific condition, … and it might be better … for patients to not come here for that since we can’t offer the appropriate level of care for that condition.’”
But in rural and other less populated areas, he says “ … that community hospital may be the only game in town. And even though they … wouldn’t have everything that a tertiary care [or] quaternary care academic center would have, they could identify areas that are critically important for the acute care patients they are serving and develop the appropriate levels of competency in that area.”
Administering Thrombolytics
What is the standard by which an individual hospitalist is expected to practice, especially concerning the administration of tPA?
In that regard—without a doubt—patient safety comes first. “Whenever there’s confusion in my mind, I always think … first, do no harm,” says Dr. Sachdeva. “If this is an urban area and other hospitalists are not [administering] tPA, then they are not expected to do so and that may not meet the standard of care for that area. Rural hospitals have successfully been giving tPA to patients with acute ischemic stroke.
The caveat here is that appropriate planning as well as training of caregivers has to take place prior to starting IV tPA administration. “Rural hospitals that have the IV tPA capability usually do so in collaboration with larger regional institutions, academic or otherwise, where services of neurologists and neurosurgeons are available,” says Dr. Sachdeva. “Size of the institution should not be an impediment to IV tPA administration.”
As baby boomers age, the demand for better stroke care will increase, and hospitals as well as caregivers need to be prepared to meet the expectations of patients.
David Thurber, MD, medical director of the Cary Hospital Medicine Service, a division of Wake Medical Center, Cary, N.C., speaks of the need for specialty backup at community hospitals.
“For those people who practice in community hospitals, including myself,” he says, “it’s like being the pitcher on a baseball team: If you can’t field the outfield, you shouldn’t be pitching the ball because there’s nobody out there to catch it. So if you can’t get the backup of a neurologist, or of a neurosurgeon in the case of hemorrhagic stroke, in my opinion you have no business pushing tPA. Your obligation is to try, as many community hospitals have done with invasive cardiac procedures, such as emergent use of percutaneous coronary artery intervention, to transfer the patient to a facility where those can be done in a timely fashion.”
What should hospitalists do if they are expected to administer tPA and are unsure of their skill level?
“I would take this issue back to the administration of the hospital,” says Dr. Sachdeva, “and come up with a plan where the neurologists or the emergency department physicians feel motivated to give tPA.”
The most important element to consider when making the decision of whether to administer tPA is the quality of the history. “If there is any doubt about the time or the mechanism of stroke onset, then as practitioners we are very well justified in not giving tPA,” says Dr. Sachdeva, who believes there are more lawsuits for not giving tPA than for giving it. But if you withhold tPA and justify the decision with appropriate reasoning, that certainly places the individual on steadier legal ground.
Training and Competence
Stroke management is not a universally strong topic in medical education. “Not every medical school requires a rotation in the neurosciences or exposure to stroke treatment,” says Dr. Goldstein, “and it’s the same thing in residency programs, depending on which residency program you go through, be it as an internist or as an emergency physician. … So it begins in medical school and follows through residency, but as we know, our training only begins in those formal settings. In medicine, training is a lifelong activity. Things change all the time. And it would [take] appropriate levels of continuing education directly related to cerebrovascular disease to be able to understand modern diagnosis and modern therapeutics.”
Another issue is whether an institution will receive patients for stroke treatment. “Just as hospitals credential people to [perform] procedures, not every hospital can offer every therapy to every patient at the same level,” says Dr. Goldstein. “The thing that is inappropriate is to force people to do things for which they’re not trained.”
Although that is also partially an institutional decision, “institutions can’t have it both ways,” he explains. “They can’t say well, we’re going to be taking care of patients with X, Y, or Z, but then not have the facilities and personnel available to be able to acutely treat and stabilize patients even if they do require more advanced care somewhere else.”
Dr. Sachdeva’s team had to cover a considerable knowledge gap to bring his colleagues up to speed and competence by talking directly to the hospitalists and arranging CMEs for them, as well as by encouraging them to get certified in using the National Institutes of Health (NIH) stroke scale.
“The key is for hospitalists to make sure when they’re taking on an area of patient care that they feel comfortable doing that and not themselves be the default for any medical or surgical conditions,” says David Likosky, MD, who is board certified in neurology and internal medicine, and is the director of the Stroke Program of Evergreen Healthcare, Kirkland, Wash.
One way to become better prepared to manage stroke is to familiarize oneself with the National Institutes of Health (NIH) stroke scale. Online training for the NIH Stroke Scale (approved for two hours of category 1 CME credit from the NIH) is available at www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf.).
Excellent resources for developing protocols include the American Stroke Association/American Heart Association, the work of the Brain Attack Coalition (a group of professional, voluntary, and governmental entities dedicated to reducing the occurrence, disabilities, and death associated with stroke—www.stroke-site.org/), and the Web site (www.strokecenter.org), produced out of Washington University in St. Louis. SHM (www.hospitalmedicine.org), which is in the process of creating a Web-based stroke resource room, which—at press time—was scheduled to be live by August 1.
—David Thurber, MD
Systems and Monitoring
Having the right systems in place enables smooth patient assessment and treatment. First establish a means for education in stroke care for hospitalists and all support staff. Other important systems include having protocols for admitting [patients] for stroke care; setting up communication pathways for various disciplines involved in stroke care; having systems to gather, analyze, and monitor data; and having particularly good teamwork and response time.
William Likosky, MD, director of the Stroke Program at the Swedish Medical Center, Seattle, strongly believes in systems and processes of care, whereby a well-designed system should not only be able to prevent mistakes by an individual caregiver, but also to facilitate optimal evidence-based care in every case. As an institution Swedish Medical draws inspiration from the Institute of Healthcare Improvement’s campaign to prevent 100,000 avoidable deaths nationwide in its hospitalized patients. Since its inception at Swedish Medical two years ago, the stroke program is credited with preventing 22 deaths.
Of course any protocol’s worth will vary according to the effectiveness with which it is implemented. Developing protocols and care pathways is an avenue for hospitalists to take a leadership role in implementing evidence-based care, in co-ordinating care between different services, and eventually affecting resource utilization, quality of care, and patient satisfaction positively.
Protocols or pathways fail when they’re not patient-centered, when input isn’t solicited from other caregivers during the development phase, or when their implementation is not monitored. To Dr. Sachdeva, “the main issue is how you implement [the protocol], how you monitor the implementation, and how you fix the glitches or the problems that usually ensue when you’re rolling out a new protocol.”
Response and Feedback
Another imperative of any stroke program is its response time. “We monitor very closely our emergency department evaluation times for patients coming in within the window for giving tPA,” says Dr. Sachdeva. “We are strict about this because we want every patient to be evaluated within 45 minutes—anybody who is a candidate for possible intervention with acute thrombolytics—either IV or IA. Those times are monitored, and any time that 45-minute window is missed, we have an individual conversation with the people who were responsible, not as a confrontation, but [to ask], ‘What can we do to help you?’ And each time we do that we learn something new.
“Usually in these cases, there were things that were happening that were out of control and sometimes you can control them and sometimes you can’t,” he says. “Next time we try to manage the variables better. So we do have a hands-on continuous monitoring process that is not intrusive, and it gives us an idea of how we are holding up with certain quality parameters.”
Teamwork and Communication
One of the important systems is how well all involved work as a team. “Most of the time, IV tPA is given in the emergency department and the emergency department doctors now are very comfortable giving IV tPA with the telephonic help from a neurologist,” says Dr. Sachdeva. “But they also receive assistance from the stroke nurse, who consults on every stroke patient who is a candidate for emergent intervention in the emergency department.”
Swedish Medical maintains dedicated stroke nurses who act as facilitators to ensure everybody holds up their end of the bargain in stroke care. This includes a combination of nurses and nurse practitioners. But ultimately it is the emergency department physician’s decision in consultation with the neurologist by phone.
Part of their facilitation involves negotiating to cut down on time. “We don’t … rush our patients, but we cut down on avoidable delays,” says Dr. Sachdeva. “We try to get all the pertinent workup done as fast as we can, and then collate the data, make sure the data are disseminated to the parties that need the data, and decisions are made and appropriate treatment algorithms applied.”
These dedicated nurses are available in person for any acute stroke that falls within the window for an emergent intervention. “But if it is [an] acute stroke outside the window,” says Dr. Sachdeva, “they will consult telephonically to help you get certain things started, and then consult on the patient the next business day. They are available 24/7 both to the emergency department and to any floor area of the hospital. Anyplace that stroke can happen … they are there in a heartbeat. And the stroke nurses have been invaluable in assisting the hospitalists in day-to-day care of the stroke patients as well as in educating patients and their families.”
Controversies in Stroke Management
Although many hospitalists are uncomfortable treating ischemic strokes, far more may show discomfort at the idea of treating hemorrhagic strokes.
“Bleeding within the head carries a morbidity and mortality that sometimes is exaggerated in terms of its perception,” he says, “and once again, one has to look at the training that was given to most hospitalists during their residency. It was insufficient with respect to managing intracranial hemorrhages.”
Treating hemorrhagic strokes has traditionally been the preserve of neurosurgeons. “Some neurosurgeons are of the opinion that if there is no indication for surgical intervention for a particular ICH case, then the patient should be on the medical service,” says Dr. Sachdeva. “The medical side is feeling thoroughly unprepared to handle these.”
His team is looking at this issue at their institution to come up with appropriate algorithms regarding triage and care of patients with ICH.
Hospitalists and Stroke Management: Opportunities
One advantage of the hospitalist system in managing stroke is that hospitalists are readily available. Monitoring patients’ recovery for any emergent complications is also an important role for the hospitalist. Most often these complications are urinary tract infections, aspiration pneumonia, and deep venous thrombosis.
The team at Swedish refers to these high-risk complications as “dashboards,” likening them to the dashboard of an automobile that must be carefully watched.
Swedish Medical has seven markers for quality of care that the stroke team monitors. They have a statistician, people who gather the data, people who analyze the data, and those who then put the data in a graph format for the team to review trends reflecting quality of care.
This secondary prevention comes into play while coordinating care at the time of discharge. Hospitalists can start the ball rolling so a primary care physician or the facility to which the patient may next be transferred will continue the appropriate care for these patients.
Hospitalists could also take leadership role within their institutions in formulating pathways for emergent evaluation of strokes that occur in hospitalized patients.
“This is what most hospitalists should be able to do with adequate training,” says Dr. Sachdeva. “At the very least, hospitalists can positively impact stroke care by setting into place protocols, processes, and systems of care to ensure prevention DVTs, UTIs, aspiration pneumonias, and initiation of appropriate secondary prevention modalities for patients admitted with a diagnosis of stroke.”
Any institution that prevents these complications from developing should see an automatic benefit of those quality parameters in decreased length of stay, decreased utilization of resources, and improved patient satisfaction.
Follow-Up and Compliance
Having the undivided attention of the patient and his or her family at the time of hospitalization is a golden opportunity.
“We start patients on a vigorous, evidence-based secondary prevention regimen and by opening a dialogue with the patient and the family,” says Dr. Sachdeva. “Realize you’ve started something good; it needs to be followed up and reinforced on a regular basis either through their primary care provider or through a dedicated stroke follow-up clinic.”
The plan for handling a potential future brain attack is also outlined. One of the most noteworthy programs for secondary prevention of strokes is the one out of the University of California, Los Angeles called PROTECT—Preventing Recurrence of Thromboembolic Events through Coordinated Treatment (http://strokeprotect.mednet.ucla.edu/). (See p. 22.)2
Dr. Thurber, who is also president of the Piedmont Chapter of SHM, hopes that secondary prevention work by stroke teams around the country and the results of public education campaigns can help reduce the number of patients who present for stroke treatment outside the time window for thrombolytic therapy.
Communication with PCPs
If you have a dedicated group of primary care physicians that you work with, then they are, in effect, your customers. They should develop that program so they can give their input as how they would like communication and they can know what kind of care their patients will receive once admitted to the hospitalists or the hospitalist-neurologist team.
Call the primary care physicians at the time of discharge in order to convey the highlights of hospitalization and review key follow-up issues. Information can fall through the cracks, but the PROTECT program shows that this is rare if you use the tools provided as part of the program.1 Their data show that initiating secondary prevention modalities while the patient is hospitalized is important, but following up on them is just as important to good outcomes.
The discharging physician must partner with the primary care providers to maintain the momentum with respect to secondary prevention, re-enforcing education, and monitoring for development of side effects from the medications initiated during hospitalization.
Future Trends
Given the trends of an expanding hospitalist system, increasing time limitations for specialists, the relative dearth of neurologists, and uninviting circumstances for practice and compensation, neurologists will need to partner with a group of physicians who are structured to be available 24/7.
In his coauthored letter to the editor of Stroke, published in June 2005, Dr. Likosky challenged neurologists to avoid being “asleep at the wheel” in stroke prevention.1 “If neurologists want to be the ones taking care of stroke patients,” he said, “then they need to decide what role they want to play, because otherwise it’s going to be taken over by hospitalists, which may be the most appropriate thing.”
Conclusion
Challenges and opportunities characterize the work of hospitalists involved in stroke care. Good, ongoing training is imperative as are effective institutional systems and efficient monitoring of those systems. Protocols can be adapted to best serve an individual institution; the nature of their implementation and the teamwork or lack thereof will make the difference in the benefit to medical and institutional outcomes.
Recommendations for best performance in stroke care include keeping open channels of communication and good feedback systems, discussing controversies in order to seek resolutions and improve systems, and using the advantage of access to patients and their families to best begin follow-up and secondary prevention efforts. TH
Writer Andrea M. Sattinger will cover the malpractice crisis in healthcare in future issues of The Hospitalist.
References
- Likosky DJ. Who will care for our hospitalized patients? Stroke. 2005;36:1113-1114.
- Ovbiagele B, Saver JL, Fredieu A, et al. PROTECT: A coordinated stroke treatment program to prevent recurrent thromboembolic events. Neurology. 2004;63:1217-1222.
Distinguishing the evolving role of the hospitalist in managing patients with stroke requires exploring a number of challenges, a couple of controversies, and some clear opportunities.
Challenges
Hospitalists and their specialist colleagues face a number of challenges associated with stroke management, including the nature of provider teamwork, whether patients present within the window of time for thrombolytic administration, whether hospitalists should administer those agents, and also the care of patients with intracerebral hemorrhage (ICH).
Specialty Support
Traditionally the neurologist has been the key clinician involved in the diagnosis and treatment of patients with stroke. And because a great many neurologists prefer to practice almost exclusively in the outpatient setting, a team of providers in the hospital must handle the current stroke care volume.
“Coming to the hospital can be a challenge for some of them, although there is a subset of neurologists who really like to be inside the hospital and look after acute issues with respect to neurology,” says Sandeep Sachdeva, MD, Swedish Medical Center in Seattle. “In our institution we’ve had enough neurologists, but most of them are busy with their outpatient practices so they’re not able to spend substantial time [in the hospital]. By default we have to look at the hospitalist program here as a resource for taking care of stroke patients.”1
Emergent evaluation and treatment of acute ischemic stroke is a hot-button issue, especially for community-based hospitals. Some neurologists can leave their office and attend to an acute ischemic stroke presenting to the emergency department, while others can’t. To address this issue some hospitals have developed stroke teams that usually consist of highly trained nurses/advanced registered nurse practitioners (ARNPs) working under the direction of a neurologist, as is the case at Swedish Medical Center. These stroke teams respond to acute strokes presenting in the emergency department and then assist the emergency department physician in expediting the patient evaluation and ensuring that no protocol violation occurs while emergent therapy, such as IV tPA, is administered.
The final decision for administering this medication rests with the emergency department physician and, in some instances, with the neurologist if he or she is able to evaluate the patient in the emergency department. Hospitalists must evaluate their comfort level, knowledge, and experience—and then discuss with their neurologists and emergency department physicians the development of—a care algorithm commensurate with national and local standards of care as it pertains to caring for patients who present with acute stroke.
With relatively little specialty support available, it becomes more important for communication between providers to be clear and reliable; and practitioners must determine the local standard of care.
“I think with stroke it’s a particularly vexing issue, especially when you get outside of metropolitan areas,” says Larry Goldstein, MD, director of the Duke University Stroke Center, Durham, N.C. “In metropolitan areas there may be hospitals with different capabilities that are not too far from one another. And it may make sense in that situation for one hospital to decide on their own: ‘We just don’t have the resources to be able to treat a specific condition, … and it might be better … for patients to not come here for that since we can’t offer the appropriate level of care for that condition.’”
But in rural and other less populated areas, he says “ … that community hospital may be the only game in town. And even though they … wouldn’t have everything that a tertiary care [or] quaternary care academic center would have, they could identify areas that are critically important for the acute care patients they are serving and develop the appropriate levels of competency in that area.”
Administering Thrombolytics
What is the standard by which an individual hospitalist is expected to practice, especially concerning the administration of tPA?
In that regard—without a doubt—patient safety comes first. “Whenever there’s confusion in my mind, I always think … first, do no harm,” says Dr. Sachdeva. “If this is an urban area and other hospitalists are not [administering] tPA, then they are not expected to do so and that may not meet the standard of care for that area. Rural hospitals have successfully been giving tPA to patients with acute ischemic stroke.
The caveat here is that appropriate planning as well as training of caregivers has to take place prior to starting IV tPA administration. “Rural hospitals that have the IV tPA capability usually do so in collaboration with larger regional institutions, academic or otherwise, where services of neurologists and neurosurgeons are available,” says Dr. Sachdeva. “Size of the institution should not be an impediment to IV tPA administration.”
As baby boomers age, the demand for better stroke care will increase, and hospitals as well as caregivers need to be prepared to meet the expectations of patients.
David Thurber, MD, medical director of the Cary Hospital Medicine Service, a division of Wake Medical Center, Cary, N.C., speaks of the need for specialty backup at community hospitals.
“For those people who practice in community hospitals, including myself,” he says, “it’s like being the pitcher on a baseball team: If you can’t field the outfield, you shouldn’t be pitching the ball because there’s nobody out there to catch it. So if you can’t get the backup of a neurologist, or of a neurosurgeon in the case of hemorrhagic stroke, in my opinion you have no business pushing tPA. Your obligation is to try, as many community hospitals have done with invasive cardiac procedures, such as emergent use of percutaneous coronary artery intervention, to transfer the patient to a facility where those can be done in a timely fashion.”
What should hospitalists do if they are expected to administer tPA and are unsure of their skill level?
“I would take this issue back to the administration of the hospital,” says Dr. Sachdeva, “and come up with a plan where the neurologists or the emergency department physicians feel motivated to give tPA.”
The most important element to consider when making the decision of whether to administer tPA is the quality of the history. “If there is any doubt about the time or the mechanism of stroke onset, then as practitioners we are very well justified in not giving tPA,” says Dr. Sachdeva, who believes there are more lawsuits for not giving tPA than for giving it. But if you withhold tPA and justify the decision with appropriate reasoning, that certainly places the individual on steadier legal ground.
Training and Competence
Stroke management is not a universally strong topic in medical education. “Not every medical school requires a rotation in the neurosciences or exposure to stroke treatment,” says Dr. Goldstein, “and it’s the same thing in residency programs, depending on which residency program you go through, be it as an internist or as an emergency physician. … So it begins in medical school and follows through residency, but as we know, our training only begins in those formal settings. In medicine, training is a lifelong activity. Things change all the time. And it would [take] appropriate levels of continuing education directly related to cerebrovascular disease to be able to understand modern diagnosis and modern therapeutics.”
Another issue is whether an institution will receive patients for stroke treatment. “Just as hospitals credential people to [perform] procedures, not every hospital can offer every therapy to every patient at the same level,” says Dr. Goldstein. “The thing that is inappropriate is to force people to do things for which they’re not trained.”
Although that is also partially an institutional decision, “institutions can’t have it both ways,” he explains. “They can’t say well, we’re going to be taking care of patients with X, Y, or Z, but then not have the facilities and personnel available to be able to acutely treat and stabilize patients even if they do require more advanced care somewhere else.”
Dr. Sachdeva’s team had to cover a considerable knowledge gap to bring his colleagues up to speed and competence by talking directly to the hospitalists and arranging CMEs for them, as well as by encouraging them to get certified in using the National Institutes of Health (NIH) stroke scale.
“The key is for hospitalists to make sure when they’re taking on an area of patient care that they feel comfortable doing that and not themselves be the default for any medical or surgical conditions,” says David Likosky, MD, who is board certified in neurology and internal medicine, and is the director of the Stroke Program of Evergreen Healthcare, Kirkland, Wash.
One way to become better prepared to manage stroke is to familiarize oneself with the National Institutes of Health (NIH) stroke scale. Online training for the NIH Stroke Scale (approved for two hours of category 1 CME credit from the NIH) is available at www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf.).
Excellent resources for developing protocols include the American Stroke Association/American Heart Association, the work of the Brain Attack Coalition (a group of professional, voluntary, and governmental entities dedicated to reducing the occurrence, disabilities, and death associated with stroke—www.stroke-site.org/), and the Web site (www.strokecenter.org), produced out of Washington University in St. Louis. SHM (www.hospitalmedicine.org), which is in the process of creating a Web-based stroke resource room, which—at press time—was scheduled to be live by August 1.
—David Thurber, MD
Systems and Monitoring
Having the right systems in place enables smooth patient assessment and treatment. First establish a means for education in stroke care for hospitalists and all support staff. Other important systems include having protocols for admitting [patients] for stroke care; setting up communication pathways for various disciplines involved in stroke care; having systems to gather, analyze, and monitor data; and having particularly good teamwork and response time.
William Likosky, MD, director of the Stroke Program at the Swedish Medical Center, Seattle, strongly believes in systems and processes of care, whereby a well-designed system should not only be able to prevent mistakes by an individual caregiver, but also to facilitate optimal evidence-based care in every case. As an institution Swedish Medical draws inspiration from the Institute of Healthcare Improvement’s campaign to prevent 100,000 avoidable deaths nationwide in its hospitalized patients. Since its inception at Swedish Medical two years ago, the stroke program is credited with preventing 22 deaths.
Of course any protocol’s worth will vary according to the effectiveness with which it is implemented. Developing protocols and care pathways is an avenue for hospitalists to take a leadership role in implementing evidence-based care, in co-ordinating care between different services, and eventually affecting resource utilization, quality of care, and patient satisfaction positively.
Protocols or pathways fail when they’re not patient-centered, when input isn’t solicited from other caregivers during the development phase, or when their implementation is not monitored. To Dr. Sachdeva, “the main issue is how you implement [the protocol], how you monitor the implementation, and how you fix the glitches or the problems that usually ensue when you’re rolling out a new protocol.”
Response and Feedback
Another imperative of any stroke program is its response time. “We monitor very closely our emergency department evaluation times for patients coming in within the window for giving tPA,” says Dr. Sachdeva. “We are strict about this because we want every patient to be evaluated within 45 minutes—anybody who is a candidate for possible intervention with acute thrombolytics—either IV or IA. Those times are monitored, and any time that 45-minute window is missed, we have an individual conversation with the people who were responsible, not as a confrontation, but [to ask], ‘What can we do to help you?’ And each time we do that we learn something new.
“Usually in these cases, there were things that were happening that were out of control and sometimes you can control them and sometimes you can’t,” he says. “Next time we try to manage the variables better. So we do have a hands-on continuous monitoring process that is not intrusive, and it gives us an idea of how we are holding up with certain quality parameters.”
Teamwork and Communication
One of the important systems is how well all involved work as a team. “Most of the time, IV tPA is given in the emergency department and the emergency department doctors now are very comfortable giving IV tPA with the telephonic help from a neurologist,” says Dr. Sachdeva. “But they also receive assistance from the stroke nurse, who consults on every stroke patient who is a candidate for emergent intervention in the emergency department.”
Swedish Medical maintains dedicated stroke nurses who act as facilitators to ensure everybody holds up their end of the bargain in stroke care. This includes a combination of nurses and nurse practitioners. But ultimately it is the emergency department physician’s decision in consultation with the neurologist by phone.
Part of their facilitation involves negotiating to cut down on time. “We don’t … rush our patients, but we cut down on avoidable delays,” says Dr. Sachdeva. “We try to get all the pertinent workup done as fast as we can, and then collate the data, make sure the data are disseminated to the parties that need the data, and decisions are made and appropriate treatment algorithms applied.”
These dedicated nurses are available in person for any acute stroke that falls within the window for an emergent intervention. “But if it is [an] acute stroke outside the window,” says Dr. Sachdeva, “they will consult telephonically to help you get certain things started, and then consult on the patient the next business day. They are available 24/7 both to the emergency department and to any floor area of the hospital. Anyplace that stroke can happen … they are there in a heartbeat. And the stroke nurses have been invaluable in assisting the hospitalists in day-to-day care of the stroke patients as well as in educating patients and their families.”
Controversies in Stroke Management
Although many hospitalists are uncomfortable treating ischemic strokes, far more may show discomfort at the idea of treating hemorrhagic strokes.
“Bleeding within the head carries a morbidity and mortality that sometimes is exaggerated in terms of its perception,” he says, “and once again, one has to look at the training that was given to most hospitalists during their residency. It was insufficient with respect to managing intracranial hemorrhages.”
Treating hemorrhagic strokes has traditionally been the preserve of neurosurgeons. “Some neurosurgeons are of the opinion that if there is no indication for surgical intervention for a particular ICH case, then the patient should be on the medical service,” says Dr. Sachdeva. “The medical side is feeling thoroughly unprepared to handle these.”
His team is looking at this issue at their institution to come up with appropriate algorithms regarding triage and care of patients with ICH.
Hospitalists and Stroke Management: Opportunities
One advantage of the hospitalist system in managing stroke is that hospitalists are readily available. Monitoring patients’ recovery for any emergent complications is also an important role for the hospitalist. Most often these complications are urinary tract infections, aspiration pneumonia, and deep venous thrombosis.
The team at Swedish refers to these high-risk complications as “dashboards,” likening them to the dashboard of an automobile that must be carefully watched.
Swedish Medical has seven markers for quality of care that the stroke team monitors. They have a statistician, people who gather the data, people who analyze the data, and those who then put the data in a graph format for the team to review trends reflecting quality of care.
This secondary prevention comes into play while coordinating care at the time of discharge. Hospitalists can start the ball rolling so a primary care physician or the facility to which the patient may next be transferred will continue the appropriate care for these patients.
Hospitalists could also take leadership role within their institutions in formulating pathways for emergent evaluation of strokes that occur in hospitalized patients.
“This is what most hospitalists should be able to do with adequate training,” says Dr. Sachdeva. “At the very least, hospitalists can positively impact stroke care by setting into place protocols, processes, and systems of care to ensure prevention DVTs, UTIs, aspiration pneumonias, and initiation of appropriate secondary prevention modalities for patients admitted with a diagnosis of stroke.”
Any institution that prevents these complications from developing should see an automatic benefit of those quality parameters in decreased length of stay, decreased utilization of resources, and improved patient satisfaction.
Follow-Up and Compliance
Having the undivided attention of the patient and his or her family at the time of hospitalization is a golden opportunity.
“We start patients on a vigorous, evidence-based secondary prevention regimen and by opening a dialogue with the patient and the family,” says Dr. Sachdeva. “Realize you’ve started something good; it needs to be followed up and reinforced on a regular basis either through their primary care provider or through a dedicated stroke follow-up clinic.”
The plan for handling a potential future brain attack is also outlined. One of the most noteworthy programs for secondary prevention of strokes is the one out of the University of California, Los Angeles called PROTECT—Preventing Recurrence of Thromboembolic Events through Coordinated Treatment (http://strokeprotect.mednet.ucla.edu/). (See p. 22.)2
Dr. Thurber, who is also president of the Piedmont Chapter of SHM, hopes that secondary prevention work by stroke teams around the country and the results of public education campaigns can help reduce the number of patients who present for stroke treatment outside the time window for thrombolytic therapy.
Communication with PCPs
If you have a dedicated group of primary care physicians that you work with, then they are, in effect, your customers. They should develop that program so they can give their input as how they would like communication and they can know what kind of care their patients will receive once admitted to the hospitalists or the hospitalist-neurologist team.
Call the primary care physicians at the time of discharge in order to convey the highlights of hospitalization and review key follow-up issues. Information can fall through the cracks, but the PROTECT program shows that this is rare if you use the tools provided as part of the program.1 Their data show that initiating secondary prevention modalities while the patient is hospitalized is important, but following up on them is just as important to good outcomes.
The discharging physician must partner with the primary care providers to maintain the momentum with respect to secondary prevention, re-enforcing education, and monitoring for development of side effects from the medications initiated during hospitalization.
Future Trends
Given the trends of an expanding hospitalist system, increasing time limitations for specialists, the relative dearth of neurologists, and uninviting circumstances for practice and compensation, neurologists will need to partner with a group of physicians who are structured to be available 24/7.
In his coauthored letter to the editor of Stroke, published in June 2005, Dr. Likosky challenged neurologists to avoid being “asleep at the wheel” in stroke prevention.1 “If neurologists want to be the ones taking care of stroke patients,” he said, “then they need to decide what role they want to play, because otherwise it’s going to be taken over by hospitalists, which may be the most appropriate thing.”
Conclusion
Challenges and opportunities characterize the work of hospitalists involved in stroke care. Good, ongoing training is imperative as are effective institutional systems and efficient monitoring of those systems. Protocols can be adapted to best serve an individual institution; the nature of their implementation and the teamwork or lack thereof will make the difference in the benefit to medical and institutional outcomes.
Recommendations for best performance in stroke care include keeping open channels of communication and good feedback systems, discussing controversies in order to seek resolutions and improve systems, and using the advantage of access to patients and their families to best begin follow-up and secondary prevention efforts. TH
Writer Andrea M. Sattinger will cover the malpractice crisis in healthcare in future issues of The Hospitalist.
References
- Likosky DJ. Who will care for our hospitalized patients? Stroke. 2005;36:1113-1114.
- Ovbiagele B, Saver JL, Fredieu A, et al. PROTECT: A coordinated stroke treatment program to prevent recurrent thromboembolic events. Neurology. 2004;63:1217-1222.