User login
Tips for treating patients with late-life depression
Late-life depression is the onset of a major depressive disorder in an individual ≥ 60 years of age. Depressive illness compromises quality of life and is especially troublesome for older people. The prevalence of depression among individuals > 65 years of age is about 4% in women and 3% in men.1 The estimated lifetime prevalence is approximately 24% for women and 10% for men.2 Three factors account for this disparity: women exhibit greater susceptibility to depression; the illness persists longer in women than it does in men; and the probability of death related to depression is lower in women.2
Beyond its direct mental and emotional impacts, depression takes a financial toll; health care costs are higher for those with depression than for those without depression.3 Unpaid caregiver expense is the largest indirect financial burden with late-life depression.4 Additional indirect costs include less work productivity, early retirement, and diminished financial security.4
Many individuals with depression never receive treatment. Fortunately, there are many interventions in the primary care arsenal that can be used to treat older patients with depression and dramatically improve mood, comfort, and function.
The interactions of emotional and physical health
The pathophysiology of depression remains unclear. However, numerous factors are known to contribute to, exacerbate, or prolong depression among elderly populations. Insufficient social engagement and support is strongly associated with depressive mood.5 The loss of independence in giving up automobile driving can compromise self-confidence.6 Sleep difficulties predispose to, and predict, the emergence of a mood disorder, independent of other symptoms.7 Age-related hearing deficits also are associated with depression.8
There is a close relationship between emotional and physical health.9 Depression adds to the likelihood of medical illness, and somatic pathology increases the risk for mood disorders.9 Depression has been linked with obesity, frailty, diabetes, cognitive impairment, and terminal illness.9
Inflammatory markers and depression may also be related. Plasma levels of interleukin-6 and C-reactive protein were measured in a longitudinal aging study.14 A high level of interleukin-6, but not C-reactive protein, correlated with an increased prevalence of depression in older people.
Chronic cerebral ischemia can result in a “vascular depression”13 in which disruption of prefrontal systems by ischemic lesions is hypothesized to be an important factor in developing despair. Psychomotor retardation, executive dysfunction, severe disability, and a heightened risk for relapse are common features of vascular depression.15 Poststroke depression often follows a cerebrovascular episode16; the exact pathogenic mechanism is unknown.17
Continue to: A summation of common risk factors
A summation of common risk factors. A personal or family history of depression increases the risk for late-life depression. Other risk factors are female gender, bereavement, sleep disturbance, and disability.18 Poor general health, chronic pain, cognitive impairment, poor social support, and medical comorbidities with impaired functioning increase the likelihood of resultant mood disorders.18
Somatic complaints may overshadow diagnostic symptoms
Manifestations of depression include disturbed sleep and reductions in appetite, concentration, activity, and energy for daily function.19 These features, of course, may accompany medical disorders and some normal physiologic changes among elderly people. We find that while older individuals may report a sad mood, disturbed sleep, or other dysfunctions, they frequently emphasize their somatic complaints much more prominently than their emotions. This can make it difficult to recognize clinical depression.
For a diagnosis of major depression, 5 of the following 9 symptoms must be present for most of the day or nearly every day over a period of at least 2 weeks19: depressed mood; diminished interest in most activities; significant weight loss or decreased appetite; insomnia or hypersomnia; agitation or retardation; fatigue or loss of energy; feelings of worthlessness or guilt; diminished concentration; and recurrent thoughts of death or suicide.19
Planning difficulties, apathy, disability, and anhedonia frequently occur. Executive dysfunction and inefficacy of antidepressant pharmacotherapy are related to compromised frontal-striatal-limbic pathways.20 Since difficulties with planning and organization are associated with suboptimal response to antidepressant medications, a psychotherapeutic focus on these executive functions can augment drug-induced benefit.
Rule out these alternative diagnoses
Dementias can manifest as depression. Other brain pathologies, particularly Parkinson disease or stroke, also should be ruled out. Overmedication can simulate depression, so be sure to review the prescription and over-the-counter agents a patient is taking. Some medications can occasionally precipitate a clinical depression; these include stimulants, steroids, methyldopa, triptans, chemotherapeutic agents, and immunologic drugs, to name a few.19
Continue to: Pharmacotherapy, Yes, but first, consider these factors
Pharmacotherapy, Yes, but first, consider these factors
Maintaining a close patient–doctor relationship augments all therapeutic interventions. Good eye contact when listening to and counseling patients is key, as is providing close follow-up appointments.
Encourage social interactions with family and friends, which can be particularly productive. Encouraging spiritual endeavors, such as attendance at religious services, can be beneficial.21
Recommend exercise. Physical exercise yields positive outcomes22; it can enhance mood, improve sleep, and help to diminish anxiety. Encourage patients with depression to take a daily walk during the day; doing so can enhance emotional outlook, health, and even socialization.
What treatment will best serve your patient?
It’s important when caring for patients with depression to assess and address suicidal ideation. Depression with a previous suicide attempt is a strong risk factor for suicide. Inquire about suicidal intent or death wishes, access to guns, and other life-ending behaviors. Whenever suicide is an active issue, immediate crisis management is required. Psychiatric referral is an option, and hospitalization may be indicated. Advise family members to remove firearms or restrict access, be with the patient as much as possible, and assist at intervention planning and implementation.
It is worth mentioning, here, the connection between chronic pain and suicidal ideation. Pain management reduces suicidal ideation, regardless of depression severity.23
Continue to: Psychotherapy and pharmacotherapies...
Psychotherapy and pharmacotherapies offered for the treatment of depression in geriatric practices are both effective, without much difference seen in efficacy.24 Psychotherapy might include direct physician and family support to the patient or referral to a mental health professional. Base treatment choices on clinical access, patient preference, and medical contraindications and other illnesses.
Pros and cons of various pharmacotherapies
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed first for elderly patients with depression.25 Escitalopram is often better tolerated than paroxetine, which exhibits muscarinic antagonism and enzyme inhibition of cytochrome P450-2D6.26 Escitalopram also has fewer pharmaceutical interactions compared with sertraline.26
Generally, when prescribing an antidepressant drug, stay with the initial choice, gradually increasing the dose as clinically needed to its maximum limit. Suicidal ideation may be worsened by too quickly switching from one antidepressant to another or by co-prescribing anxiolytic or hypnotic medicines. Benzodiazepines have addictive and disinhibiting properties and should be avoided, if possible.27 For patients withinsomnia, consider initially selecting a sedating antidepressant medication such as paroxetine or mirtazapine to augment sleep.
Alternatives to SSRIs. Nonselective serotonin reuptake inhibitors have similar efficacy as SSRIs. However, escitalopram is as effective as venlafaxine (a selective serotonin and norepinephrine reuptake inhibitor [SSNRI]) and is better tolerated.28 Duloxetine, another SSNRI, improves mood and often diminishes chronic pain.29 Mirtazapine, an alpha-2 antagonist, might cause fewer drug-drug interactions and is effective, well tolerated, and especially helpful for patients with anxiety or insomnia.30 Dry mouth, sedation, and weight gain are common adverse effects of mirtazapine. Obesity precautions are often necessary during mirtazapine therapy; this includes monitoring body weight and metabolic profiles, instituting dietary changes, and recommending an exercise regimen. In contrast to SSRIs, mirtazapine might induce less sexual dysfunction.31
Tricyclic antidepressant drugs can also be effective but may worsen cardiac conduction abnormalities, prostatic hypertrophy, or narrow angle glaucoma. Tricyclic antidepressants may be useful in patients without cardiac disease who have not responded to an SSRI or an SSNRI.
Continue to: The role of aripiprazole
The role of aripiprazole. Elderly patients not achieving remission from depression with antidepressant agents alone may benefit from co-prescribing aripiprazole.32 As an adjunct, aripiprazole is effective in achieving and sustaining remission
Minimize risks and maximize benefits of antidepressants by following these recommendations:
- Ascertain whether any antidepressant treatments have worked well in the past.
- Start with an SSRI if no other antidepressant treatment has worked in the past.
- Counsel patients about the need for treatment adherence. Antidepressants may take 2 weeks to 2 months to provide noticeable improvement.
- Prescribe up to the maximum drug dose if needed to enhance benefit.
- Use a mood measurement tool (eg, the Patient Health Questionnaire-9) to help evaluate treatment response.
Try a different class of drugs for patients who do not respond to treatment. For patients who have a partial response, augment with bupropion XL, mirtazapine, aripiprazole, or quetiapine.33 Sertraline and nortriptyline are similarly effective on a population-wide basis, with sertraline having less-problematic adverse effects.34 Trial-and-error treatments in practice may find one patient responding only to sertraline and another patient only to nortriptyline.
Combinations of different drug classes may provide benefit for patients not responding to a single antidepressant. In geriatric patients, combined treatment with methylphenidate and citalopram enhances mood and well-being.35 Compared with either drug alone, the combination yielded an augmented clinical response profile and a higher rate of remission. Cognitive functioning, energy, and mood improve even with methylphenidate alone, especially when fatigue is an issue. However, addictive properties limit its use to cases in which conventional antidepressant medications are not effective or indicated, and only when drug refills are closely monitored.
The challenges of advancing age. Antidepressant treatment needs increase with advanced age.36 As mentioned earlier, elderly people often have medical illnesses complicating their depression and frequently are dealing with pain from the medical illness. When dementia coexists with depression, the efficacy of pharmacotherapies is compromised.
Continue to: When drug-related interventions fail
When drug-related interventions fail, therapy ought to be more psychologically focused.37 Psychotherapy is usually helpful and is particularly indicated when recovery is suboptimal. Counseling might come from the treating physician or referral to a psychotherapist.
Nasal esketamine can be efficacious when supplementing antidepressant pharmacotherapy among older patients with treatment-resistant depression.38 Elderly individuals responding to antidepressants do not benefit from adjunctive donepezil to correct mild cognitive impairment.39 There is no advantage to off-label cholinesterase inhibitor prescribing for patients with both depression and dementia.
Other options. Electroconvulsive therapy (ECT) does not cause long-term cognitive problems and is reserved for treatment-resistant cases.40 Patients with depression who also have had previous cognitive impairment often improve in mental ability following ECT.41
A promising new option. Transcranial magnetic stimulation (TMS) is a promising, relatively new therapeutic option for treating refractory cases of depressive mood disorders. In TMS, an electromagnetic coil that creates a magnetic field is placed over the left dorsolateral prefrontal cortex (which is responsible for mood regulation). Referral for TMS administration may offer new hope for older patients with treatment-resistant depression.42
Keep comorbidities in mind as you address depression
Coexisting psychiatric illnesses worsen emotions. Geriatric patients are susceptible to psychiatric comorbidities that include substance abuse, obsessive-compulsive characteristics, dysfunctional eating, and panic disorder.19 Myocardial and cerebral infarctions are detrimental to mental health, especially soon after such events.43 Poststroke depression magnifies the risk for disability and mortality,16,17 yet antidepressant pharmacotherapy often enhances prognoses. Along with early intervention algorithm-based plans and inclusion of a depression care manager, antidepressants often diminish poststroke depression severity.44 Even when cancer is present, depression care reduces mortality.44 So with this in mind, persist with antidepressant treatment, which will often benefit an elderly individual with depression.
Continue to: When possible, get ahead of depression before it sets in
When possible, get ahead of depression before it sets in
Social participation and employment help to sustain an optimistic, euthymic mood.45 Maintaining good physical health, in part through consistent activity levels (including exercise), can help prevent depression. Since persistent sleep disturbance predicts depression among those with a depression history, optimizing sleep among geriatric adults can avoid or alleviate depression.46
Sleep hygiene education for patients is also helpful. A regular waking time often promotes a better sleeping schedule. Restful sleep also is more likely when an individual avoids excess caffeine, exercises during the day, and uses the bed only for sleeping (not for listening to music or watching television).
Because inflammation may precede depression, anti-inflammatory medications have been proposed as potential treatment, but such pharmacotherapies are often ineffective. Older adults generally do not benefit from low-dose aspirin administration to prevent depression.47 Low vitamin D levels can contribute to depression, yet vitamin D supplementation may not improve mood.48
Offering hope. Tell your patients that if they are feeling depressed, they should make an appointment with you, their primary care physician, because there are medications they can take and counseling they can avail themselves of that could help.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville-Psychiatry, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
1. Steffens DC, Skoog I, Norton MC, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Arch Gen Psych. 2000;57:601-607. doi: 10.1001/ archpsyc.57.6.601
2. Barry LC, Allore HG, Guo Z, et al. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psych. 2008;65:172-178. doi: 10.1001/archgenpsychiatry.2007.17
3. Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psych. 2003;60:897-903. doi: 10.1001/archpsyc.60.9.897
4. Snow CE, Abrams RC. The indirect costs of late-life depression in the United States: a literature review and perspective. Geriatrics. 2016;1,30. doi.org/10.3390/geriatrics/1040030
5. George LK, Blazer DG, Hughes D, et al. Social support and the outcome of major depression. Br J Psych. 1989;154:478-485. doi: 10.1192/bjp.154.4.478
6. Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol Psychol Soc Sci. 2001;56:S343-S351. doi: 10.1093/geronb/56.6.s343
7. Cho HJ, Lavretsky H, Olmstead R, et al. Sleep disturbance and depression recurrence in community dwelling older adults—a prospective study. Am J Psych. 2008;165:1543-1550. doi: 10.1176/appi.ajp.2008.07121882
8. Golub JS, Brewster KK, Brickman AM, et al. Subclinical hearing loss is associated with depressive symptoms. Am J Geriatr Psychiatry. 2020;28:545-556. doi: 10.1016/j.jagp.2019.12.008
9. Alexopoulos GS. Mechanisms and treatment of late-life depression. Focus (Am Psychiatr Publ). 2021;19:340-354. doi: 10.1176/appi.focus.19304
10. Starkstein SE, Preziosi TJ, Bolduc PL, et al. Depression in Parkinson’s disease. J Nerv Ment Disord. 1990;178:27-31. doi: 10.1097/00005053-199001000-00005
11. Gilman SE, Abraham HE. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alco Depend. 2001;63:277-286. doi: 10.1016/s0376-8716(00)00216-7
12. Parmelee PA, Katz IR, Lawton MP. The relation of pain to depression among institutionalized aged. J Gerontol. 1991;46:P15-P21. doi: 10.1093/geronj/46.1.p15
13. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psych. 1997;54:915-922. doi: 10.1001/archpsyc.1997.01830220033006
14. Bremmer MA, Beekman AT, Deeg DJ, et al. Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord. 2008;106:249-255. doi: 10.1016/j.jad.2007.07.002
15. Taylor WD, Aizenstein HJ, Alexopoulos GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psych. 2013;18:963-974. doi: 10.1038/mp.2013.20
16. Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psych. 2016;173:221-231. doi: 10.1176/appi.ajp.2015.15030363
17. Cai W, Mueller C, Li YJ, et al. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:102-109. doi: 10.1016/ j.arr.2019.01.013
18. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psych. 2003;160:1147-1156. doi: 10.1176/appi.ajp.160.6.1147
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 2013:160-168.
20. Pimontel MA, Rindskopf D, Rutherford BR, et al. A meta-analysis of executive dysfunction and antidepressant treatment response in late-life depression. Am J Geriatr Psych. 2016;24:31-34. doi: 10.1016/j.jagp.2015.05.010
21. Koenig HG, Cohen HJ, Blazer DG, et al. Religious coping and depression in elderly hospitalized medically ill men. Am J Psychiatry. 1992;149:1693-1700. doi: 10.1176/ajp.149.12.1693
22. Blake H, Mo P, Malik S, et al. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil. 2009;10:873-887. doi: 10.1177/0269215509337449
23. Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081-1091. doi: 10.1001/jama.291.9.1081
24. Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493-1501. doi: 10.1176/ajp.2006.163.9.1493
25. Solai LK, Mulsant BH, Pollack BG. Selective serotonin reuptake inhibitors for late-life depression: a comparative review. Drugs Aging. 2001;18:355-368. doi: 10.2165/00002512-200118050-00006
26. Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline. Are they all alike? Int Clin Psychopharmacol. 2014;29:185-196. doi: 10.1097/YIC.0000000000000023
27. Hedna K, Sundell KA, Hamidi A, et al. Antidepressants and suicidal behaviour in late life: a prospective population-based study of use patterns in new users aged 75 and above. Eur J Clin Pharmacol. 2018;74:201-208. doi: 10.1007/s00228-017-2360-x
28. Bielski RJ, Ventura D, Chang CC. A double-blind comparison of escitalopram and venlafaxine extended release in the treatment of major depressive disorder. J Clin Psychiatry. 2004;65:1190-1196. doi: 10.4088/jcp.v65n0906
29. Robinson M, Oakes TM, Raskin J, et al. Acute and long-term treatment of late-life major depressive disorder: duloxetine versus placebo. Am J Geriatr Psychiatry. 2014;22:34-45. doi: 10.1016/ j.jagp.2013.01.019
30. Holm KJ, Markham A. Mirtazapine: a review of its use in major depression. Drugs. 1999;57:607-631. doi: 10.2165/00003495-199957040-00010
31. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7:249-264. doi: 10.1111/j.1527-3458.2001.tb00198.x
32. Lenze EJ, Mulsant BH, Blumberger DM, et al. Efficacy, safety and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised double-blind, placebo-controlled trial. Lancet. 2015;386:2404-2412. doi: 10.1016/S0140-6736(15)00308-6
33. Lenze EJ, Oughli HA. Antidepressant treatment for late-life depression: considering risks and benefits. J Am Geriatr Soc. 2019;67:1555-1556. doi: 10.1111/jgs.15964
34. Bondareff W, Alpert M, Friedhoff AJ, et al: Comparison of sertraline and nortriptyline in the treatment of major depressive disorder in late life. Am J Psychiatry. 2000;157:729-736. doi: 10.1176/appi.ajp.157.5.729
35. Lavretsky H, Reinlieb M, St Cyr N. Citalopram, methylphenidate, or their combination in geriatric depression: a randomized, double-blind, placebo controlled trial. Am J Psych. 2015;72:561-569. doi: 10.1176/appi.ajp.2014.14070889
36. Arthur A, Savva GM, Barnes LE, et al. Changing prevalence and treatment of depression among older people over two decades. Br J Psychiatry. 2020;21:49-54. doi: 10.1192/bjp.2019.193
37. Zuidersma M, Chua K-C, Hellier J, et al. Sertraline and mirtazapine versus placebo in subgroups of depression in dementia: findings from the HTA-SADD randomized controlled trial. Am J Geriatr Psychiatry. 2019;27:920-931. doi: 10.1016/ j.jagp.2019.03.021
38. Ochs-Ross R, Wajs E, Daly EJ, et al. Comparison of long-term efficacy and safety of esketamine nasal spray plus oral antidepressant in younger versus older patients with treatment-resistant depression: post-hoc analysis of SUSTAIN-2, a long-term open-label phase 3 safety and efficacy study. Am J Geriatr Psychiatry. 2022;30:541-556. doi: 10.1016/j.jagp.2021.09.014
39. Devanand DP, Pelton GH, D’Antonio K, et al. Donepezil treatment in patients with depression and cognitive impairment on stable antidepressant treatment: a randomized controlled trial. Am J Geriatr Psychiatry. 2018;26:1050-1060. doi: 10.1016/ j.jagp.2018.05.008
40. Obbels J, Vansteelandt K, Verwijk E, et al. MMSE changes during and after ECT in late life depression: a prospective study. Am J Geriatr Psychiatry. 2019;27:934-944. doi: 10.1016/ j.jagp.2019.04.006
41. Wagenmakers MJ, Vansteelandt K, van Exel E, et al. Transient cognitive impairment and white matter hyperintensities in severely depressed older patients treated with electroconvulsive therapy. Am J Geriatr Psychiatry. 2021:29:1117-1128. doi: 10.1016/j.jagp.2020.12.028
42. Trevizol AP, Goldberger KW, Mulsant BH, et al. Unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant late-life depression. Int J Ger Psychiatry. 2019;34:822-827. doi: 10.1002/gps.5091
43. Aben I, Verhey F, Stik J, et al. A comparative study into the one year cumulative incidence of depression after stroke and myocardial infarction. J Neurol Neurosurg Psychiatry. 2003;74:581-585. doi: 10.1136/jnnp.74.5.581
44. Gallo JJ, Bogner HR, Morales KH, et al. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146:689-698. doi: 10.7326/0003-4819-146-10-200705150-00002
45. Lee J, Jang SN, Cho SL. Gender differences in the trajectories and the risk factors of depressive symptoms in later life. Int Psychogeriatr. 2017;29:1495-1505. doi: 10.1017/S1041610217000709
46. Lee E, Cho HJ, Olmstead R, et al. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults. Sleep. 2013;36:1685-1691. doi: 10.5665/sleep.3128
47. Berk M, Woods RL, Nelson MR, et al. Effect of aspirin vs placebo on the prevention of depression in older people: a randomized clinical trial. J Am Med A Psych. 2020;77:1012-1020. doi: 10.1001/jamapsychiatry.2020.1214
48. Okereke OI, Reynolds CF, Mischoulon D, et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2020;324:471-480. doi: 10.1001/jama.2020.10224
Late-life depression is the onset of a major depressive disorder in an individual ≥ 60 years of age. Depressive illness compromises quality of life and is especially troublesome for older people. The prevalence of depression among individuals > 65 years of age is about 4% in women and 3% in men.1 The estimated lifetime prevalence is approximately 24% for women and 10% for men.2 Three factors account for this disparity: women exhibit greater susceptibility to depression; the illness persists longer in women than it does in men; and the probability of death related to depression is lower in women.2
Beyond its direct mental and emotional impacts, depression takes a financial toll; health care costs are higher for those with depression than for those without depression.3 Unpaid caregiver expense is the largest indirect financial burden with late-life depression.4 Additional indirect costs include less work productivity, early retirement, and diminished financial security.4
Many individuals with depression never receive treatment. Fortunately, there are many interventions in the primary care arsenal that can be used to treat older patients with depression and dramatically improve mood, comfort, and function.
The interactions of emotional and physical health
The pathophysiology of depression remains unclear. However, numerous factors are known to contribute to, exacerbate, or prolong depression among elderly populations. Insufficient social engagement and support is strongly associated with depressive mood.5 The loss of independence in giving up automobile driving can compromise self-confidence.6 Sleep difficulties predispose to, and predict, the emergence of a mood disorder, independent of other symptoms.7 Age-related hearing deficits also are associated with depression.8
There is a close relationship between emotional and physical health.9 Depression adds to the likelihood of medical illness, and somatic pathology increases the risk for mood disorders.9 Depression has been linked with obesity, frailty, diabetes, cognitive impairment, and terminal illness.9
Inflammatory markers and depression may also be related. Plasma levels of interleukin-6 and C-reactive protein were measured in a longitudinal aging study.14 A high level of interleukin-6, but not C-reactive protein, correlated with an increased prevalence of depression in older people.
Chronic cerebral ischemia can result in a “vascular depression”13 in which disruption of prefrontal systems by ischemic lesions is hypothesized to be an important factor in developing despair. Psychomotor retardation, executive dysfunction, severe disability, and a heightened risk for relapse are common features of vascular depression.15 Poststroke depression often follows a cerebrovascular episode16; the exact pathogenic mechanism is unknown.17
Continue to: A summation of common risk factors
A summation of common risk factors. A personal or family history of depression increases the risk for late-life depression. Other risk factors are female gender, bereavement, sleep disturbance, and disability.18 Poor general health, chronic pain, cognitive impairment, poor social support, and medical comorbidities with impaired functioning increase the likelihood of resultant mood disorders.18
Somatic complaints may overshadow diagnostic symptoms
Manifestations of depression include disturbed sleep and reductions in appetite, concentration, activity, and energy for daily function.19 These features, of course, may accompany medical disorders and some normal physiologic changes among elderly people. We find that while older individuals may report a sad mood, disturbed sleep, or other dysfunctions, they frequently emphasize their somatic complaints much more prominently than their emotions. This can make it difficult to recognize clinical depression.
For a diagnosis of major depression, 5 of the following 9 symptoms must be present for most of the day or nearly every day over a period of at least 2 weeks19: depressed mood; diminished interest in most activities; significant weight loss or decreased appetite; insomnia or hypersomnia; agitation or retardation; fatigue or loss of energy; feelings of worthlessness or guilt; diminished concentration; and recurrent thoughts of death or suicide.19
Planning difficulties, apathy, disability, and anhedonia frequently occur. Executive dysfunction and inefficacy of antidepressant pharmacotherapy are related to compromised frontal-striatal-limbic pathways.20 Since difficulties with planning and organization are associated with suboptimal response to antidepressant medications, a psychotherapeutic focus on these executive functions can augment drug-induced benefit.
Rule out these alternative diagnoses
Dementias can manifest as depression. Other brain pathologies, particularly Parkinson disease or stroke, also should be ruled out. Overmedication can simulate depression, so be sure to review the prescription and over-the-counter agents a patient is taking. Some medications can occasionally precipitate a clinical depression; these include stimulants, steroids, methyldopa, triptans, chemotherapeutic agents, and immunologic drugs, to name a few.19
Continue to: Pharmacotherapy, Yes, but first, consider these factors
Pharmacotherapy, Yes, but first, consider these factors
Maintaining a close patient–doctor relationship augments all therapeutic interventions. Good eye contact when listening to and counseling patients is key, as is providing close follow-up appointments.
Encourage social interactions with family and friends, which can be particularly productive. Encouraging spiritual endeavors, such as attendance at religious services, can be beneficial.21
Recommend exercise. Physical exercise yields positive outcomes22; it can enhance mood, improve sleep, and help to diminish anxiety. Encourage patients with depression to take a daily walk during the day; doing so can enhance emotional outlook, health, and even socialization.
What treatment will best serve your patient?
It’s important when caring for patients with depression to assess and address suicidal ideation. Depression with a previous suicide attempt is a strong risk factor for suicide. Inquire about suicidal intent or death wishes, access to guns, and other life-ending behaviors. Whenever suicide is an active issue, immediate crisis management is required. Psychiatric referral is an option, and hospitalization may be indicated. Advise family members to remove firearms or restrict access, be with the patient as much as possible, and assist at intervention planning and implementation.
It is worth mentioning, here, the connection between chronic pain and suicidal ideation. Pain management reduces suicidal ideation, regardless of depression severity.23
Continue to: Psychotherapy and pharmacotherapies...
Psychotherapy and pharmacotherapies offered for the treatment of depression in geriatric practices are both effective, without much difference seen in efficacy.24 Psychotherapy might include direct physician and family support to the patient or referral to a mental health professional. Base treatment choices on clinical access, patient preference, and medical contraindications and other illnesses.
Pros and cons of various pharmacotherapies
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed first for elderly patients with depression.25 Escitalopram is often better tolerated than paroxetine, which exhibits muscarinic antagonism and enzyme inhibition of cytochrome P450-2D6.26 Escitalopram also has fewer pharmaceutical interactions compared with sertraline.26
Generally, when prescribing an antidepressant drug, stay with the initial choice, gradually increasing the dose as clinically needed to its maximum limit. Suicidal ideation may be worsened by too quickly switching from one antidepressant to another or by co-prescribing anxiolytic or hypnotic medicines. Benzodiazepines have addictive and disinhibiting properties and should be avoided, if possible.27 For patients withinsomnia, consider initially selecting a sedating antidepressant medication such as paroxetine or mirtazapine to augment sleep.
Alternatives to SSRIs. Nonselective serotonin reuptake inhibitors have similar efficacy as SSRIs. However, escitalopram is as effective as venlafaxine (a selective serotonin and norepinephrine reuptake inhibitor [SSNRI]) and is better tolerated.28 Duloxetine, another SSNRI, improves mood and often diminishes chronic pain.29 Mirtazapine, an alpha-2 antagonist, might cause fewer drug-drug interactions and is effective, well tolerated, and especially helpful for patients with anxiety or insomnia.30 Dry mouth, sedation, and weight gain are common adverse effects of mirtazapine. Obesity precautions are often necessary during mirtazapine therapy; this includes monitoring body weight and metabolic profiles, instituting dietary changes, and recommending an exercise regimen. In contrast to SSRIs, mirtazapine might induce less sexual dysfunction.31
Tricyclic antidepressant drugs can also be effective but may worsen cardiac conduction abnormalities, prostatic hypertrophy, or narrow angle glaucoma. Tricyclic antidepressants may be useful in patients without cardiac disease who have not responded to an SSRI or an SSNRI.
Continue to: The role of aripiprazole
The role of aripiprazole. Elderly patients not achieving remission from depression with antidepressant agents alone may benefit from co-prescribing aripiprazole.32 As an adjunct, aripiprazole is effective in achieving and sustaining remission
Minimize risks and maximize benefits of antidepressants by following these recommendations:
- Ascertain whether any antidepressant treatments have worked well in the past.
- Start with an SSRI if no other antidepressant treatment has worked in the past.
- Counsel patients about the need for treatment adherence. Antidepressants may take 2 weeks to 2 months to provide noticeable improvement.
- Prescribe up to the maximum drug dose if needed to enhance benefit.
- Use a mood measurement tool (eg, the Patient Health Questionnaire-9) to help evaluate treatment response.
Try a different class of drugs for patients who do not respond to treatment. For patients who have a partial response, augment with bupropion XL, mirtazapine, aripiprazole, or quetiapine.33 Sertraline and nortriptyline are similarly effective on a population-wide basis, with sertraline having less-problematic adverse effects.34 Trial-and-error treatments in practice may find one patient responding only to sertraline and another patient only to nortriptyline.
Combinations of different drug classes may provide benefit for patients not responding to a single antidepressant. In geriatric patients, combined treatment with methylphenidate and citalopram enhances mood and well-being.35 Compared with either drug alone, the combination yielded an augmented clinical response profile and a higher rate of remission. Cognitive functioning, energy, and mood improve even with methylphenidate alone, especially when fatigue is an issue. However, addictive properties limit its use to cases in which conventional antidepressant medications are not effective or indicated, and only when drug refills are closely monitored.
The challenges of advancing age. Antidepressant treatment needs increase with advanced age.36 As mentioned earlier, elderly people often have medical illnesses complicating their depression and frequently are dealing with pain from the medical illness. When dementia coexists with depression, the efficacy of pharmacotherapies is compromised.
Continue to: When drug-related interventions fail
When drug-related interventions fail, therapy ought to be more psychologically focused.37 Psychotherapy is usually helpful and is particularly indicated when recovery is suboptimal. Counseling might come from the treating physician or referral to a psychotherapist.
Nasal esketamine can be efficacious when supplementing antidepressant pharmacotherapy among older patients with treatment-resistant depression.38 Elderly individuals responding to antidepressants do not benefit from adjunctive donepezil to correct mild cognitive impairment.39 There is no advantage to off-label cholinesterase inhibitor prescribing for patients with both depression and dementia.
Other options. Electroconvulsive therapy (ECT) does not cause long-term cognitive problems and is reserved for treatment-resistant cases.40 Patients with depression who also have had previous cognitive impairment often improve in mental ability following ECT.41
A promising new option. Transcranial magnetic stimulation (TMS) is a promising, relatively new therapeutic option for treating refractory cases of depressive mood disorders. In TMS, an electromagnetic coil that creates a magnetic field is placed over the left dorsolateral prefrontal cortex (which is responsible for mood regulation). Referral for TMS administration may offer new hope for older patients with treatment-resistant depression.42
Keep comorbidities in mind as you address depression
Coexisting psychiatric illnesses worsen emotions. Geriatric patients are susceptible to psychiatric comorbidities that include substance abuse, obsessive-compulsive characteristics, dysfunctional eating, and panic disorder.19 Myocardial and cerebral infarctions are detrimental to mental health, especially soon after such events.43 Poststroke depression magnifies the risk for disability and mortality,16,17 yet antidepressant pharmacotherapy often enhances prognoses. Along with early intervention algorithm-based plans and inclusion of a depression care manager, antidepressants often diminish poststroke depression severity.44 Even when cancer is present, depression care reduces mortality.44 So with this in mind, persist with antidepressant treatment, which will often benefit an elderly individual with depression.
Continue to: When possible, get ahead of depression before it sets in
When possible, get ahead of depression before it sets in
Social participation and employment help to sustain an optimistic, euthymic mood.45 Maintaining good physical health, in part through consistent activity levels (including exercise), can help prevent depression. Since persistent sleep disturbance predicts depression among those with a depression history, optimizing sleep among geriatric adults can avoid or alleviate depression.46
Sleep hygiene education for patients is also helpful. A regular waking time often promotes a better sleeping schedule. Restful sleep also is more likely when an individual avoids excess caffeine, exercises during the day, and uses the bed only for sleeping (not for listening to music or watching television).
Because inflammation may precede depression, anti-inflammatory medications have been proposed as potential treatment, but such pharmacotherapies are often ineffective. Older adults generally do not benefit from low-dose aspirin administration to prevent depression.47 Low vitamin D levels can contribute to depression, yet vitamin D supplementation may not improve mood.48
Offering hope. Tell your patients that if they are feeling depressed, they should make an appointment with you, their primary care physician, because there are medications they can take and counseling they can avail themselves of that could help.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville-Psychiatry, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
Late-life depression is the onset of a major depressive disorder in an individual ≥ 60 years of age. Depressive illness compromises quality of life and is especially troublesome for older people. The prevalence of depression among individuals > 65 years of age is about 4% in women and 3% in men.1 The estimated lifetime prevalence is approximately 24% for women and 10% for men.2 Three factors account for this disparity: women exhibit greater susceptibility to depression; the illness persists longer in women than it does in men; and the probability of death related to depression is lower in women.2
Beyond its direct mental and emotional impacts, depression takes a financial toll; health care costs are higher for those with depression than for those without depression.3 Unpaid caregiver expense is the largest indirect financial burden with late-life depression.4 Additional indirect costs include less work productivity, early retirement, and diminished financial security.4
Many individuals with depression never receive treatment. Fortunately, there are many interventions in the primary care arsenal that can be used to treat older patients with depression and dramatically improve mood, comfort, and function.
The interactions of emotional and physical health
The pathophysiology of depression remains unclear. However, numerous factors are known to contribute to, exacerbate, or prolong depression among elderly populations. Insufficient social engagement and support is strongly associated with depressive mood.5 The loss of independence in giving up automobile driving can compromise self-confidence.6 Sleep difficulties predispose to, and predict, the emergence of a mood disorder, independent of other symptoms.7 Age-related hearing deficits also are associated with depression.8
There is a close relationship between emotional and physical health.9 Depression adds to the likelihood of medical illness, and somatic pathology increases the risk for mood disorders.9 Depression has been linked with obesity, frailty, diabetes, cognitive impairment, and terminal illness.9
Inflammatory markers and depression may also be related. Plasma levels of interleukin-6 and C-reactive protein were measured in a longitudinal aging study.14 A high level of interleukin-6, but not C-reactive protein, correlated with an increased prevalence of depression in older people.
Chronic cerebral ischemia can result in a “vascular depression”13 in which disruption of prefrontal systems by ischemic lesions is hypothesized to be an important factor in developing despair. Psychomotor retardation, executive dysfunction, severe disability, and a heightened risk for relapse are common features of vascular depression.15 Poststroke depression often follows a cerebrovascular episode16; the exact pathogenic mechanism is unknown.17
Continue to: A summation of common risk factors
A summation of common risk factors. A personal or family history of depression increases the risk for late-life depression. Other risk factors are female gender, bereavement, sleep disturbance, and disability.18 Poor general health, chronic pain, cognitive impairment, poor social support, and medical comorbidities with impaired functioning increase the likelihood of resultant mood disorders.18
Somatic complaints may overshadow diagnostic symptoms
Manifestations of depression include disturbed sleep and reductions in appetite, concentration, activity, and energy for daily function.19 These features, of course, may accompany medical disorders and some normal physiologic changes among elderly people. We find that while older individuals may report a sad mood, disturbed sleep, or other dysfunctions, they frequently emphasize their somatic complaints much more prominently than their emotions. This can make it difficult to recognize clinical depression.
For a diagnosis of major depression, 5 of the following 9 symptoms must be present for most of the day or nearly every day over a period of at least 2 weeks19: depressed mood; diminished interest in most activities; significant weight loss or decreased appetite; insomnia or hypersomnia; agitation or retardation; fatigue or loss of energy; feelings of worthlessness or guilt; diminished concentration; and recurrent thoughts of death or suicide.19
Planning difficulties, apathy, disability, and anhedonia frequently occur. Executive dysfunction and inefficacy of antidepressant pharmacotherapy are related to compromised frontal-striatal-limbic pathways.20 Since difficulties with planning and organization are associated with suboptimal response to antidepressant medications, a psychotherapeutic focus on these executive functions can augment drug-induced benefit.
Rule out these alternative diagnoses
Dementias can manifest as depression. Other brain pathologies, particularly Parkinson disease or stroke, also should be ruled out. Overmedication can simulate depression, so be sure to review the prescription and over-the-counter agents a patient is taking. Some medications can occasionally precipitate a clinical depression; these include stimulants, steroids, methyldopa, triptans, chemotherapeutic agents, and immunologic drugs, to name a few.19
Continue to: Pharmacotherapy, Yes, but first, consider these factors
Pharmacotherapy, Yes, but first, consider these factors
Maintaining a close patient–doctor relationship augments all therapeutic interventions. Good eye contact when listening to and counseling patients is key, as is providing close follow-up appointments.
Encourage social interactions with family and friends, which can be particularly productive. Encouraging spiritual endeavors, such as attendance at religious services, can be beneficial.21
Recommend exercise. Physical exercise yields positive outcomes22; it can enhance mood, improve sleep, and help to diminish anxiety. Encourage patients with depression to take a daily walk during the day; doing so can enhance emotional outlook, health, and even socialization.
What treatment will best serve your patient?
It’s important when caring for patients with depression to assess and address suicidal ideation. Depression with a previous suicide attempt is a strong risk factor for suicide. Inquire about suicidal intent or death wishes, access to guns, and other life-ending behaviors. Whenever suicide is an active issue, immediate crisis management is required. Psychiatric referral is an option, and hospitalization may be indicated. Advise family members to remove firearms or restrict access, be with the patient as much as possible, and assist at intervention planning and implementation.
It is worth mentioning, here, the connection between chronic pain and suicidal ideation. Pain management reduces suicidal ideation, regardless of depression severity.23
Continue to: Psychotherapy and pharmacotherapies...
Psychotherapy and pharmacotherapies offered for the treatment of depression in geriatric practices are both effective, without much difference seen in efficacy.24 Psychotherapy might include direct physician and family support to the patient or referral to a mental health professional. Base treatment choices on clinical access, patient preference, and medical contraindications and other illnesses.
Pros and cons of various pharmacotherapies
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed first for elderly patients with depression.25 Escitalopram is often better tolerated than paroxetine, which exhibits muscarinic antagonism and enzyme inhibition of cytochrome P450-2D6.26 Escitalopram also has fewer pharmaceutical interactions compared with sertraline.26
Generally, when prescribing an antidepressant drug, stay with the initial choice, gradually increasing the dose as clinically needed to its maximum limit. Suicidal ideation may be worsened by too quickly switching from one antidepressant to another or by co-prescribing anxiolytic or hypnotic medicines. Benzodiazepines have addictive and disinhibiting properties and should be avoided, if possible.27 For patients withinsomnia, consider initially selecting a sedating antidepressant medication such as paroxetine or mirtazapine to augment sleep.
Alternatives to SSRIs. Nonselective serotonin reuptake inhibitors have similar efficacy as SSRIs. However, escitalopram is as effective as venlafaxine (a selective serotonin and norepinephrine reuptake inhibitor [SSNRI]) and is better tolerated.28 Duloxetine, another SSNRI, improves mood and often diminishes chronic pain.29 Mirtazapine, an alpha-2 antagonist, might cause fewer drug-drug interactions and is effective, well tolerated, and especially helpful for patients with anxiety or insomnia.30 Dry mouth, sedation, and weight gain are common adverse effects of mirtazapine. Obesity precautions are often necessary during mirtazapine therapy; this includes monitoring body weight and metabolic profiles, instituting dietary changes, and recommending an exercise regimen. In contrast to SSRIs, mirtazapine might induce less sexual dysfunction.31
Tricyclic antidepressant drugs can also be effective but may worsen cardiac conduction abnormalities, prostatic hypertrophy, or narrow angle glaucoma. Tricyclic antidepressants may be useful in patients without cardiac disease who have not responded to an SSRI or an SSNRI.
Continue to: The role of aripiprazole
The role of aripiprazole. Elderly patients not achieving remission from depression with antidepressant agents alone may benefit from co-prescribing aripiprazole.32 As an adjunct, aripiprazole is effective in achieving and sustaining remission
Minimize risks and maximize benefits of antidepressants by following these recommendations:
- Ascertain whether any antidepressant treatments have worked well in the past.
- Start with an SSRI if no other antidepressant treatment has worked in the past.
- Counsel patients about the need for treatment adherence. Antidepressants may take 2 weeks to 2 months to provide noticeable improvement.
- Prescribe up to the maximum drug dose if needed to enhance benefit.
- Use a mood measurement tool (eg, the Patient Health Questionnaire-9) to help evaluate treatment response.
Try a different class of drugs for patients who do not respond to treatment. For patients who have a partial response, augment with bupropion XL, mirtazapine, aripiprazole, or quetiapine.33 Sertraline and nortriptyline are similarly effective on a population-wide basis, with sertraline having less-problematic adverse effects.34 Trial-and-error treatments in practice may find one patient responding only to sertraline and another patient only to nortriptyline.
Combinations of different drug classes may provide benefit for patients not responding to a single antidepressant. In geriatric patients, combined treatment with methylphenidate and citalopram enhances mood and well-being.35 Compared with either drug alone, the combination yielded an augmented clinical response profile and a higher rate of remission. Cognitive functioning, energy, and mood improve even with methylphenidate alone, especially when fatigue is an issue. However, addictive properties limit its use to cases in which conventional antidepressant medications are not effective or indicated, and only when drug refills are closely monitored.
The challenges of advancing age. Antidepressant treatment needs increase with advanced age.36 As mentioned earlier, elderly people often have medical illnesses complicating their depression and frequently are dealing with pain from the medical illness. When dementia coexists with depression, the efficacy of pharmacotherapies is compromised.
Continue to: When drug-related interventions fail
When drug-related interventions fail, therapy ought to be more psychologically focused.37 Psychotherapy is usually helpful and is particularly indicated when recovery is suboptimal. Counseling might come from the treating physician or referral to a psychotherapist.
Nasal esketamine can be efficacious when supplementing antidepressant pharmacotherapy among older patients with treatment-resistant depression.38 Elderly individuals responding to antidepressants do not benefit from adjunctive donepezil to correct mild cognitive impairment.39 There is no advantage to off-label cholinesterase inhibitor prescribing for patients with both depression and dementia.
Other options. Electroconvulsive therapy (ECT) does not cause long-term cognitive problems and is reserved for treatment-resistant cases.40 Patients with depression who also have had previous cognitive impairment often improve in mental ability following ECT.41
A promising new option. Transcranial magnetic stimulation (TMS) is a promising, relatively new therapeutic option for treating refractory cases of depressive mood disorders. In TMS, an electromagnetic coil that creates a magnetic field is placed over the left dorsolateral prefrontal cortex (which is responsible for mood regulation). Referral for TMS administration may offer new hope for older patients with treatment-resistant depression.42
Keep comorbidities in mind as you address depression
Coexisting psychiatric illnesses worsen emotions. Geriatric patients are susceptible to psychiatric comorbidities that include substance abuse, obsessive-compulsive characteristics, dysfunctional eating, and panic disorder.19 Myocardial and cerebral infarctions are detrimental to mental health, especially soon after such events.43 Poststroke depression magnifies the risk for disability and mortality,16,17 yet antidepressant pharmacotherapy often enhances prognoses. Along with early intervention algorithm-based plans and inclusion of a depression care manager, antidepressants often diminish poststroke depression severity.44 Even when cancer is present, depression care reduces mortality.44 So with this in mind, persist with antidepressant treatment, which will often benefit an elderly individual with depression.
Continue to: When possible, get ahead of depression before it sets in
When possible, get ahead of depression before it sets in
Social participation and employment help to sustain an optimistic, euthymic mood.45 Maintaining good physical health, in part through consistent activity levels (including exercise), can help prevent depression. Since persistent sleep disturbance predicts depression among those with a depression history, optimizing sleep among geriatric adults can avoid or alleviate depression.46
Sleep hygiene education for patients is also helpful. A regular waking time often promotes a better sleeping schedule. Restful sleep also is more likely when an individual avoids excess caffeine, exercises during the day, and uses the bed only for sleeping (not for listening to music or watching television).
Because inflammation may precede depression, anti-inflammatory medications have been proposed as potential treatment, but such pharmacotherapies are often ineffective. Older adults generally do not benefit from low-dose aspirin administration to prevent depression.47 Low vitamin D levels can contribute to depression, yet vitamin D supplementation may not improve mood.48
Offering hope. Tell your patients that if they are feeling depressed, they should make an appointment with you, their primary care physician, because there are medications they can take and counseling they can avail themselves of that could help.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville-Psychiatry, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
1. Steffens DC, Skoog I, Norton MC, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Arch Gen Psych. 2000;57:601-607. doi: 10.1001/ archpsyc.57.6.601
2. Barry LC, Allore HG, Guo Z, et al. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psych. 2008;65:172-178. doi: 10.1001/archgenpsychiatry.2007.17
3. Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psych. 2003;60:897-903. doi: 10.1001/archpsyc.60.9.897
4. Snow CE, Abrams RC. The indirect costs of late-life depression in the United States: a literature review and perspective. Geriatrics. 2016;1,30. doi.org/10.3390/geriatrics/1040030
5. George LK, Blazer DG, Hughes D, et al. Social support and the outcome of major depression. Br J Psych. 1989;154:478-485. doi: 10.1192/bjp.154.4.478
6. Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol Psychol Soc Sci. 2001;56:S343-S351. doi: 10.1093/geronb/56.6.s343
7. Cho HJ, Lavretsky H, Olmstead R, et al. Sleep disturbance and depression recurrence in community dwelling older adults—a prospective study. Am J Psych. 2008;165:1543-1550. doi: 10.1176/appi.ajp.2008.07121882
8. Golub JS, Brewster KK, Brickman AM, et al. Subclinical hearing loss is associated with depressive symptoms. Am J Geriatr Psychiatry. 2020;28:545-556. doi: 10.1016/j.jagp.2019.12.008
9. Alexopoulos GS. Mechanisms and treatment of late-life depression. Focus (Am Psychiatr Publ). 2021;19:340-354. doi: 10.1176/appi.focus.19304
10. Starkstein SE, Preziosi TJ, Bolduc PL, et al. Depression in Parkinson’s disease. J Nerv Ment Disord. 1990;178:27-31. doi: 10.1097/00005053-199001000-00005
11. Gilman SE, Abraham HE. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alco Depend. 2001;63:277-286. doi: 10.1016/s0376-8716(00)00216-7
12. Parmelee PA, Katz IR, Lawton MP. The relation of pain to depression among institutionalized aged. J Gerontol. 1991;46:P15-P21. doi: 10.1093/geronj/46.1.p15
13. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psych. 1997;54:915-922. doi: 10.1001/archpsyc.1997.01830220033006
14. Bremmer MA, Beekman AT, Deeg DJ, et al. Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord. 2008;106:249-255. doi: 10.1016/j.jad.2007.07.002
15. Taylor WD, Aizenstein HJ, Alexopoulos GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psych. 2013;18:963-974. doi: 10.1038/mp.2013.20
16. Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psych. 2016;173:221-231. doi: 10.1176/appi.ajp.2015.15030363
17. Cai W, Mueller C, Li YJ, et al. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:102-109. doi: 10.1016/ j.arr.2019.01.013
18. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psych. 2003;160:1147-1156. doi: 10.1176/appi.ajp.160.6.1147
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 2013:160-168.
20. Pimontel MA, Rindskopf D, Rutherford BR, et al. A meta-analysis of executive dysfunction and antidepressant treatment response in late-life depression. Am J Geriatr Psych. 2016;24:31-34. doi: 10.1016/j.jagp.2015.05.010
21. Koenig HG, Cohen HJ, Blazer DG, et al. Religious coping and depression in elderly hospitalized medically ill men. Am J Psychiatry. 1992;149:1693-1700. doi: 10.1176/ajp.149.12.1693
22. Blake H, Mo P, Malik S, et al. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil. 2009;10:873-887. doi: 10.1177/0269215509337449
23. Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081-1091. doi: 10.1001/jama.291.9.1081
24. Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493-1501. doi: 10.1176/ajp.2006.163.9.1493
25. Solai LK, Mulsant BH, Pollack BG. Selective serotonin reuptake inhibitors for late-life depression: a comparative review. Drugs Aging. 2001;18:355-368. doi: 10.2165/00002512-200118050-00006
26. Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline. Are they all alike? Int Clin Psychopharmacol. 2014;29:185-196. doi: 10.1097/YIC.0000000000000023
27. Hedna K, Sundell KA, Hamidi A, et al. Antidepressants and suicidal behaviour in late life: a prospective population-based study of use patterns in new users aged 75 and above. Eur J Clin Pharmacol. 2018;74:201-208. doi: 10.1007/s00228-017-2360-x
28. Bielski RJ, Ventura D, Chang CC. A double-blind comparison of escitalopram and venlafaxine extended release in the treatment of major depressive disorder. J Clin Psychiatry. 2004;65:1190-1196. doi: 10.4088/jcp.v65n0906
29. Robinson M, Oakes TM, Raskin J, et al. Acute and long-term treatment of late-life major depressive disorder: duloxetine versus placebo. Am J Geriatr Psychiatry. 2014;22:34-45. doi: 10.1016/ j.jagp.2013.01.019
30. Holm KJ, Markham A. Mirtazapine: a review of its use in major depression. Drugs. 1999;57:607-631. doi: 10.2165/00003495-199957040-00010
31. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7:249-264. doi: 10.1111/j.1527-3458.2001.tb00198.x
32. Lenze EJ, Mulsant BH, Blumberger DM, et al. Efficacy, safety and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised double-blind, placebo-controlled trial. Lancet. 2015;386:2404-2412. doi: 10.1016/S0140-6736(15)00308-6
33. Lenze EJ, Oughli HA. Antidepressant treatment for late-life depression: considering risks and benefits. J Am Geriatr Soc. 2019;67:1555-1556. doi: 10.1111/jgs.15964
34. Bondareff W, Alpert M, Friedhoff AJ, et al: Comparison of sertraline and nortriptyline in the treatment of major depressive disorder in late life. Am J Psychiatry. 2000;157:729-736. doi: 10.1176/appi.ajp.157.5.729
35. Lavretsky H, Reinlieb M, St Cyr N. Citalopram, methylphenidate, or their combination in geriatric depression: a randomized, double-blind, placebo controlled trial. Am J Psych. 2015;72:561-569. doi: 10.1176/appi.ajp.2014.14070889
36. Arthur A, Savva GM, Barnes LE, et al. Changing prevalence and treatment of depression among older people over two decades. Br J Psychiatry. 2020;21:49-54. doi: 10.1192/bjp.2019.193
37. Zuidersma M, Chua K-C, Hellier J, et al. Sertraline and mirtazapine versus placebo in subgroups of depression in dementia: findings from the HTA-SADD randomized controlled trial. Am J Geriatr Psychiatry. 2019;27:920-931. doi: 10.1016/ j.jagp.2019.03.021
38. Ochs-Ross R, Wajs E, Daly EJ, et al. Comparison of long-term efficacy and safety of esketamine nasal spray plus oral antidepressant in younger versus older patients with treatment-resistant depression: post-hoc analysis of SUSTAIN-2, a long-term open-label phase 3 safety and efficacy study. Am J Geriatr Psychiatry. 2022;30:541-556. doi: 10.1016/j.jagp.2021.09.014
39. Devanand DP, Pelton GH, D’Antonio K, et al. Donepezil treatment in patients with depression and cognitive impairment on stable antidepressant treatment: a randomized controlled trial. Am J Geriatr Psychiatry. 2018;26:1050-1060. doi: 10.1016/ j.jagp.2018.05.008
40. Obbels J, Vansteelandt K, Verwijk E, et al. MMSE changes during and after ECT in late life depression: a prospective study. Am J Geriatr Psychiatry. 2019;27:934-944. doi: 10.1016/ j.jagp.2019.04.006
41. Wagenmakers MJ, Vansteelandt K, van Exel E, et al. Transient cognitive impairment and white matter hyperintensities in severely depressed older patients treated with electroconvulsive therapy. Am J Geriatr Psychiatry. 2021:29:1117-1128. doi: 10.1016/j.jagp.2020.12.028
42. Trevizol AP, Goldberger KW, Mulsant BH, et al. Unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant late-life depression. Int J Ger Psychiatry. 2019;34:822-827. doi: 10.1002/gps.5091
43. Aben I, Verhey F, Stik J, et al. A comparative study into the one year cumulative incidence of depression after stroke and myocardial infarction. J Neurol Neurosurg Psychiatry. 2003;74:581-585. doi: 10.1136/jnnp.74.5.581
44. Gallo JJ, Bogner HR, Morales KH, et al. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146:689-698. doi: 10.7326/0003-4819-146-10-200705150-00002
45. Lee J, Jang SN, Cho SL. Gender differences in the trajectories and the risk factors of depressive symptoms in later life. Int Psychogeriatr. 2017;29:1495-1505. doi: 10.1017/S1041610217000709
46. Lee E, Cho HJ, Olmstead R, et al. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults. Sleep. 2013;36:1685-1691. doi: 10.5665/sleep.3128
47. Berk M, Woods RL, Nelson MR, et al. Effect of aspirin vs placebo on the prevention of depression in older people: a randomized clinical trial. J Am Med A Psych. 2020;77:1012-1020. doi: 10.1001/jamapsychiatry.2020.1214
48. Okereke OI, Reynolds CF, Mischoulon D, et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2020;324:471-480. doi: 10.1001/jama.2020.10224
1. Steffens DC, Skoog I, Norton MC, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Arch Gen Psych. 2000;57:601-607. doi: 10.1001/ archpsyc.57.6.601
2. Barry LC, Allore HG, Guo Z, et al. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psych. 2008;65:172-178. doi: 10.1001/archgenpsychiatry.2007.17
3. Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psych. 2003;60:897-903. doi: 10.1001/archpsyc.60.9.897
4. Snow CE, Abrams RC. The indirect costs of late-life depression in the United States: a literature review and perspective. Geriatrics. 2016;1,30. doi.org/10.3390/geriatrics/1040030
5. George LK, Blazer DG, Hughes D, et al. Social support and the outcome of major depression. Br J Psych. 1989;154:478-485. doi: 10.1192/bjp.154.4.478
6. Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol Psychol Soc Sci. 2001;56:S343-S351. doi: 10.1093/geronb/56.6.s343
7. Cho HJ, Lavretsky H, Olmstead R, et al. Sleep disturbance and depression recurrence in community dwelling older adults—a prospective study. Am J Psych. 2008;165:1543-1550. doi: 10.1176/appi.ajp.2008.07121882
8. Golub JS, Brewster KK, Brickman AM, et al. Subclinical hearing loss is associated with depressive symptoms. Am J Geriatr Psychiatry. 2020;28:545-556. doi: 10.1016/j.jagp.2019.12.008
9. Alexopoulos GS. Mechanisms and treatment of late-life depression. Focus (Am Psychiatr Publ). 2021;19:340-354. doi: 10.1176/appi.focus.19304
10. Starkstein SE, Preziosi TJ, Bolduc PL, et al. Depression in Parkinson’s disease. J Nerv Ment Disord. 1990;178:27-31. doi: 10.1097/00005053-199001000-00005
11. Gilman SE, Abraham HE. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alco Depend. 2001;63:277-286. doi: 10.1016/s0376-8716(00)00216-7
12. Parmelee PA, Katz IR, Lawton MP. The relation of pain to depression among institutionalized aged. J Gerontol. 1991;46:P15-P21. doi: 10.1093/geronj/46.1.p15
13. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psych. 1997;54:915-922. doi: 10.1001/archpsyc.1997.01830220033006
14. Bremmer MA, Beekman AT, Deeg DJ, et al. Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord. 2008;106:249-255. doi: 10.1016/j.jad.2007.07.002
15. Taylor WD, Aizenstein HJ, Alexopoulos GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psych. 2013;18:963-974. doi: 10.1038/mp.2013.20
16. Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psych. 2016;173:221-231. doi: 10.1176/appi.ajp.2015.15030363
17. Cai W, Mueller C, Li YJ, et al. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:102-109. doi: 10.1016/ j.arr.2019.01.013
18. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psych. 2003;160:1147-1156. doi: 10.1176/appi.ajp.160.6.1147
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 2013:160-168.
20. Pimontel MA, Rindskopf D, Rutherford BR, et al. A meta-analysis of executive dysfunction and antidepressant treatment response in late-life depression. Am J Geriatr Psych. 2016;24:31-34. doi: 10.1016/j.jagp.2015.05.010
21. Koenig HG, Cohen HJ, Blazer DG, et al. Religious coping and depression in elderly hospitalized medically ill men. Am J Psychiatry. 1992;149:1693-1700. doi: 10.1176/ajp.149.12.1693
22. Blake H, Mo P, Malik S, et al. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil. 2009;10:873-887. doi: 10.1177/0269215509337449
23. Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081-1091. doi: 10.1001/jama.291.9.1081
24. Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493-1501. doi: 10.1176/ajp.2006.163.9.1493
25. Solai LK, Mulsant BH, Pollack BG. Selective serotonin reuptake inhibitors for late-life depression: a comparative review. Drugs Aging. 2001;18:355-368. doi: 10.2165/00002512-200118050-00006
26. Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline. Are they all alike? Int Clin Psychopharmacol. 2014;29:185-196. doi: 10.1097/YIC.0000000000000023
27. Hedna K, Sundell KA, Hamidi A, et al. Antidepressants and suicidal behaviour in late life: a prospective population-based study of use patterns in new users aged 75 and above. Eur J Clin Pharmacol. 2018;74:201-208. doi: 10.1007/s00228-017-2360-x
28. Bielski RJ, Ventura D, Chang CC. A double-blind comparison of escitalopram and venlafaxine extended release in the treatment of major depressive disorder. J Clin Psychiatry. 2004;65:1190-1196. doi: 10.4088/jcp.v65n0906
29. Robinson M, Oakes TM, Raskin J, et al. Acute and long-term treatment of late-life major depressive disorder: duloxetine versus placebo. Am J Geriatr Psychiatry. 2014;22:34-45. doi: 10.1016/ j.jagp.2013.01.019
30. Holm KJ, Markham A. Mirtazapine: a review of its use in major depression. Drugs. 1999;57:607-631. doi: 10.2165/00003495-199957040-00010
31. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7:249-264. doi: 10.1111/j.1527-3458.2001.tb00198.x
32. Lenze EJ, Mulsant BH, Blumberger DM, et al. Efficacy, safety and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised double-blind, placebo-controlled trial. Lancet. 2015;386:2404-2412. doi: 10.1016/S0140-6736(15)00308-6
33. Lenze EJ, Oughli HA. Antidepressant treatment for late-life depression: considering risks and benefits. J Am Geriatr Soc. 2019;67:1555-1556. doi: 10.1111/jgs.15964
34. Bondareff W, Alpert M, Friedhoff AJ, et al: Comparison of sertraline and nortriptyline in the treatment of major depressive disorder in late life. Am J Psychiatry. 2000;157:729-736. doi: 10.1176/appi.ajp.157.5.729
35. Lavretsky H, Reinlieb M, St Cyr N. Citalopram, methylphenidate, or their combination in geriatric depression: a randomized, double-blind, placebo controlled trial. Am J Psych. 2015;72:561-569. doi: 10.1176/appi.ajp.2014.14070889
36. Arthur A, Savva GM, Barnes LE, et al. Changing prevalence and treatment of depression among older people over two decades. Br J Psychiatry. 2020;21:49-54. doi: 10.1192/bjp.2019.193
37. Zuidersma M, Chua K-C, Hellier J, et al. Sertraline and mirtazapine versus placebo in subgroups of depression in dementia: findings from the HTA-SADD randomized controlled trial. Am J Geriatr Psychiatry. 2019;27:920-931. doi: 10.1016/ j.jagp.2019.03.021
38. Ochs-Ross R, Wajs E, Daly EJ, et al. Comparison of long-term efficacy and safety of esketamine nasal spray plus oral antidepressant in younger versus older patients with treatment-resistant depression: post-hoc analysis of SUSTAIN-2, a long-term open-label phase 3 safety and efficacy study. Am J Geriatr Psychiatry. 2022;30:541-556. doi: 10.1016/j.jagp.2021.09.014
39. Devanand DP, Pelton GH, D’Antonio K, et al. Donepezil treatment in patients with depression and cognitive impairment on stable antidepressant treatment: a randomized controlled trial. Am J Geriatr Psychiatry. 2018;26:1050-1060. doi: 10.1016/ j.jagp.2018.05.008
40. Obbels J, Vansteelandt K, Verwijk E, et al. MMSE changes during and after ECT in late life depression: a prospective study. Am J Geriatr Psychiatry. 2019;27:934-944. doi: 10.1016/ j.jagp.2019.04.006
41. Wagenmakers MJ, Vansteelandt K, van Exel E, et al. Transient cognitive impairment and white matter hyperintensities in severely depressed older patients treated with electroconvulsive therapy. Am J Geriatr Psychiatry. 2021:29:1117-1128. doi: 10.1016/j.jagp.2020.12.028
42. Trevizol AP, Goldberger KW, Mulsant BH, et al. Unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant late-life depression. Int J Ger Psychiatry. 2019;34:822-827. doi: 10.1002/gps.5091
43. Aben I, Verhey F, Stik J, et al. A comparative study into the one year cumulative incidence of depression after stroke and myocardial infarction. J Neurol Neurosurg Psychiatry. 2003;74:581-585. doi: 10.1136/jnnp.74.5.581
44. Gallo JJ, Bogner HR, Morales KH, et al. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146:689-698. doi: 10.7326/0003-4819-146-10-200705150-00002
45. Lee J, Jang SN, Cho SL. Gender differences in the trajectories and the risk factors of depressive symptoms in later life. Int Psychogeriatr. 2017;29:1495-1505. doi: 10.1017/S1041610217000709
46. Lee E, Cho HJ, Olmstead R, et al. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults. Sleep. 2013;36:1685-1691. doi: 10.5665/sleep.3128
47. Berk M, Woods RL, Nelson MR, et al. Effect of aspirin vs placebo on the prevention of depression in older people: a randomized clinical trial. J Am Med A Psych. 2020;77:1012-1020. doi: 10.1001/jamapsychiatry.2020.1214
48. Okereke OI, Reynolds CF, Mischoulon D, et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2020;324:471-480. doi: 10.1001/jama.2020.10224
PRACTICE RECOMMENDATIONS
› Begin treatment with a selective serotonin reuptake inhibitor (SSRI) unless another antidepressant has worked well in the past. A
› Consider augmenting therapy with bupropion XL, mirtazapine, aripiprazole, or quetiapine for any patient who responds only partially to an SSRI. C
› Add psychotherapy to antidepressant pharmacotherapy, particularly for patients who have difficulties with executive functions such as planning and organization. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
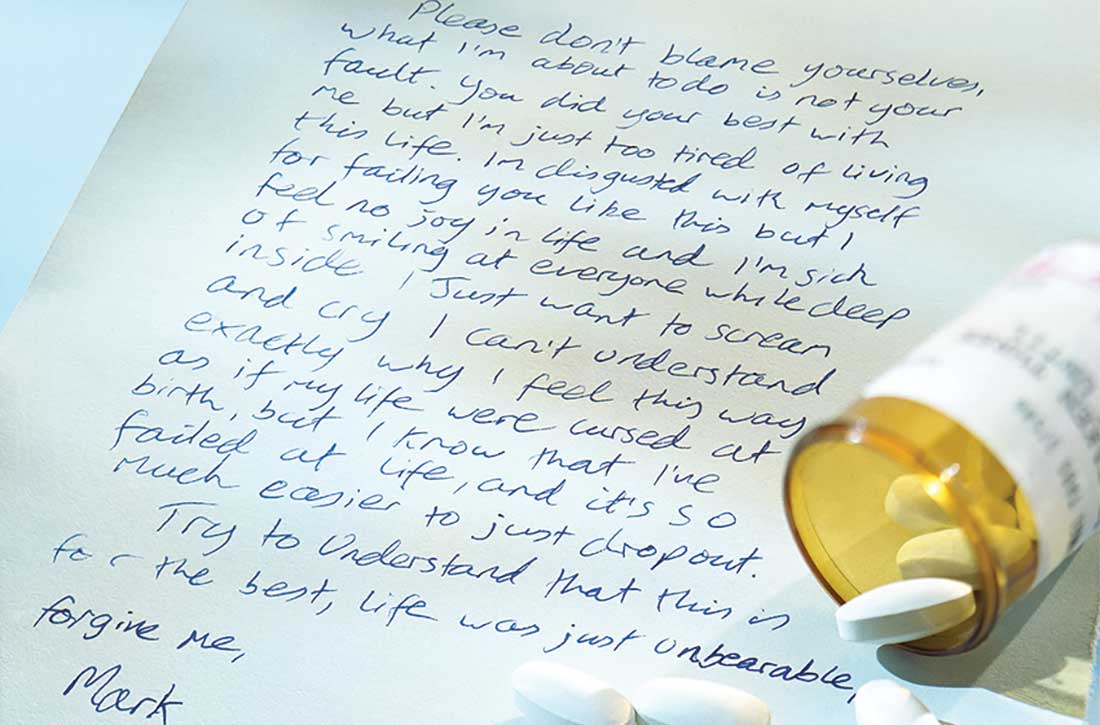
Evaluation after a suicide attempt: What to ask
In 2021, suicide was the 11th leading cause of death in the United States.1 Suicide resulted in 49,000 US deaths during 2021; it was the second most common cause of death in individuals age 10 to 34, and the fifth leading cause among children.1,2 Women are 3 to 4 times more likely than men to attempt suicide, but men are 4 times more likely to die by suicide.2
The evaluation of patients with suicidal ideation who have not made an attempt generally involves assessing 4 factors: the specific plan, access to lethal means, any recent social stressors, and the presence of a psychiatric disorder.3 The clinician should also assess which potential deterrents, such as religious beliefs or dependent children, might be present.
Mental health clinicians are often called upon to evaluate a patient after a suicide attempt to assess intent for continued self-harm and to determine appropriate disposition. Such an evaluation must consider multiple factors, including the method used, premeditation, consequences of the attempt, the presence of severe depression and/or psychosis, and the role of substance use. Assessment after a suicide attempt differs from the examination of individuals who harbor suicidal thoughts but have not made an attempt; the latter group may be more likely to respond to interventions such as intensive outpatient care, mobilization of family support, and religious proscriptions against suicide. However, for patients who make an attempt to end their life, whatever potential safeguards or deterrents to suicide that were in place obviously did not prevent the self-harm act. The consequences of the attempt, such as disabling injuries or medical complications, and possible involuntary commitment, need to be considered. Assessment of the patient’s feelings about having survived the attempt is important because the psychological impact of the attempt on family members may serve to intensify the patient’s depression and make a subsequent attempt more likely.
Many individuals who think of suicide have communicated self-harm thoughts or intentions, but such comments are often minimized or ignored. There is a common but erroneous belief that if patients are encouraged to discuss thoughts of self-harm, they will be more likely to act upon them. Because the opposite is true,4 clinicians should ask vulnerable patients about suicidal ideation or intent. Importantly, noncompliance with life-saving medical care, risk-taking behaviors, and substance use may also signal a desire for self-harm. Passive thoughts of death, typified by comments such as “I don’t care whether I wake up or not,” should also be elicited. Many patients who think of suicide speak of being in a “bad place” where reason and logic give way to an intense desire to end their misery.
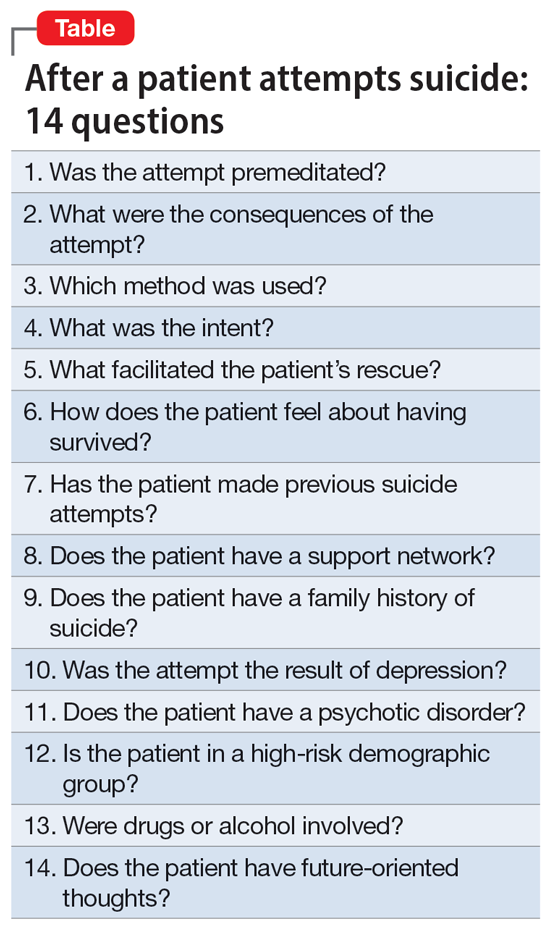
The evaluation of a patient who has attempted suicide is an important component of providing psychiatric care. This article reflects our 45 years of evaluating such patients. As such, it reflects our clinical experience and is not evidence-based. We offer a checklist of 14 questions that we have found helpful when determining if it would be best for a patient to receive inpatient psychiatric hospitalization or a discharge referral for outpatient care (Table). Questions 1 through 6 are specific for patients who have made a suicide attempt, while questions 7 through 14 are helpful for assessing global risk factors for suicide.
1. Was the attempt premeditated?
Determining premeditation vs impulsivity is an essential element of the assessment following a suicide attempt. Many such acts may occur without forethought in response to an unexpected stressor, such as an altercation between partners or family conflicts. Impulsive attempts can occur when an individual is involved in a distressing event and/or while intoxicated. Conversely, premeditation involves forethought and planning, which may increase the risk of suicide in the near future.
Examples of premeditated behavior include:
- Contemplating the attempt days or weeks beforehand
- Researching the effects of a medication or combination of medications in terms of potential lethality
- Engaging in behavior that would decrease the likelihood of their body being discovered after the attempt
- Obtaining weapons and/or stockpiling pills
- Canvassing potential sites such as bridges or tall buildings
- Engaging in a suicide attempt “practice run”
- Leaving a suicide note or message on social media
- Making funeral arrangements, such as choosing burial clothing
- Writing a will and arranging for the custody of dependent children
- Purchasing life insurance that does not deny payment of benefits in cases of death by suicide.
Continue to: Patients with a premeditated...
Patients with a premeditated suicide attempt generally do not expect to survive and are often surprised or upset that the act was not fatal. The presence of indicators that the attempt was premeditated should direct the disposition more toward hospitalization than discharge. In assessing the impact of premeditation, it is important to gauge not just the examples listed above, but also the patient’s perception of these issues (such as potential loss of child custody). Consider how much the patient is emotionally affected by such thinking.
2. What were the consequences of the attempt?
Assessing the reason for the attempt (if any) and determining whether the inciting circumstance has changed due to the suicide attempt are an important part of the evaluation. A suicide attempt may result in reconciliation with and/or renewed support from family members or partners, who might not have been aware of the patient’s emotional distress. Such unexpected support often results in the patient exhibiting improved mood and affect, and possibly temporary resolution of suicidal thoughts. This “flight into health” may be short-lived, but it also may be enough to engage the patient in a therapeutic alliance. That may permit a discharge with safe disposition to the outpatient clinic while in the custody of a family member, partner, or close friend.
Alternatively, some people experience a troubling worsening of precipitants following a suicide attempt. Preexisting medical conditions and financial, occupational, and/or social woes may be exacerbated. Child custody determinations may be affected, assuming the patient understands the possibility of this adverse consequence. Violent methods may result in disfigurement and body image issues. Individuals from small, close-knit communities may experience stigmatization and unwanted notoriety because of their suicide attempt. Such negative consequences may render some patients more likely to make another attempt to die by suicide. It is crucial to consider how a suicide attempt may have changed the original stress that led to the attempt.
3. Which method was used?
Most fatal suicides in the US are by firearms, and many individuals who survive such attempts do so because of unfamiliarity with the weapon, gun malfunction, faulty aim, or alcohol use.5-7 Some survivors report intending to shoot themselves in the heart, but instead suffered shoulder injuries. Unfortunately, for a patient who survives self-inflicted gunshot wounds, the sequelae of chronic pain, multiple surgical procedures, disability, and disfigurement may serve as constant negative reminders of the event. Some individuals with suicidal intent eschew the idea of using firearms because they hope to avoid having a family member be the first to discover them. Witnessing the aftermath of a fatal suicide by gunshot can induce symptoms of posttraumatic stress disorder in family members and/or partners.8
For a patient with self-inflicted gunshot wounds, always determine whether the weapon has been secured or if the patient still has access to it. Asking about weapon availability is essential during the evaluation of any patient with depression, major life crises, or other factors that may yield a desire to die; this is especially true for individuals with substance use disorders (SUDs). Whenever readily available to such individuals, weapons need to be safely removed.
Continue to: Other self-harm methods...
Other self-harm methods with a high degree of lethality include jumping from bridges or buildings, poisonings, self-immolation, cutting, and hangings. Individuals who choose these approaches generally do not intend to survive. Many of these methods also entail premeditation, as in the case of individuals who canvass bridges and note time when traffic is light so they are less likely to be interrupted. Between 1937 and 2012, there were >1,600 deaths by suicide from San Francisco’s Golden Gate Bridge.9 Patients who choose highly lethal methods are often irritated during the postattempt evaluation because their plans were not fatal. Usually, patients who choose such potentially lethal methods are hospitalized initially on medical and surgical floors, and receive most of their psychiatric care from consultation psychiatrists. Following discharge, these patients may be at high risk for subsequent suicide attempts.
In the US, the most common method of attempting suicide is by overdose.4 Lethality is determined by the agent or combination of substances ingested, the amount taken, the person’s health status, and the length of time before they are discovered. Many patients mistakenly assume that readily available agents such as acetaminophen and aspirin are less likely to be fatal than prescription medications. Evaluators may want to assess for suicidality in individuals with erratic, risk-taking behaviors, who are at especially high risk for death. Learning about the method the patient used can help the clinician determine the imminent risk of another suicide attempt. The more potentially fatal the patient’s method, the more serious their suicide intent, and the higher the risk they will make another suicide attempt, possibly using an even more lethal method.
4. What was the intent?
“What did you want to happen when you made this attempt?” Many patients will respond that they wanted to die, sleep, not wake up, or did not care what happened. Others say it was a gesture to evoke a certain response from another person. If this is the case, it is important to know whether the desired outcome was achieved. These so-called gestures often involve making sure the intended person is aware of the attempt, often by writing a letter, sending a text, or posting on social media. Such behaviors may be exhibited by patients with personality disorders. While such attempts often are impulsive, if the attempt fails to generate the anticipated effect, the patient may try to gain more attention by escalating their suicide actions.
Conversely, if a spouse or partner reconciles with the patient solely because of a suicide attempt, this may set a pattern for future self-harm events in which the patient hopes to achieve the same outcome. Nevertheless, it is better to err for safety because some of these patients will make another attempt, just to prove that they should have been taken more seriously. An exploration of such intent can help the evaluation because even supposed “gestures” can have dangerous consequences. Acts that do not result in the desired outcome should precipitate hospitalization rather than discharge.
5. What facilitated the patient’s rescue?
“Why is this patient still alive?” Determine if the patient did anything to save themself, such as calling an ambulance, inducing emesis, telling someone what they did, or coming to the hospital on their own. If yes, asking them what changed their mind may provide information about what exists in their lives to potentially prevent future attempts, or about wishes to stay alive. These issues can be used to guide outpatient therapy.
Continue to: How does the patient feel about having survived?
6. How does the patient feel about having survived?
When a patient is asked how they feel about having survived a suicide attempt, some will label their act “stupid” and profess embarrassment. Others exhibit future-oriented thought, which is a very good prognostic sign. More ominous is subsequent dysphoria or lamenting that “I could not even do this right.” Patients often express anger toward anyone who rescued them, especially those whose attempts were carefully planned or were discovered by accident. Some patients might also express ambivalence about having survived.
The patient’s response to this question may be shaped by their desire to avoid hospitalization, so beyond their verbal answers, be attentive to clinical cues that may suggest the patient is not being fully transparent. Anger or ambivalence about having survived, a lack of future-oriented thought, and a restricted affect despite verbalizing joy about still being alive are features that suggest psychiatric hospitalization may be warranted.
7. Has the patient made previous suicide attempts?
Compared to individuals with no previous suicide attempts, patients with a history of suicide attempts are 30 to 40 times more likely to die by suicide.2 Many patients who present after a suicide attempt have tried to kill themselves multiple times. Exploring the number of past attempts, how recent the attempts were, and what dispositions were made can be of benefit. Reviewing the potential lethality of past attempts (eg, was hospitalization required, was the patient placed in an intensive care unit, and/or was intubation needed) is recommended. If outpatient care was suggested or medication prescribed, was the patient adherent? Consider asking about passive suicidal behavior, such as not seeking care for medical issues, discontinuing life-saving medication, or engaging in reckless behavior. While such behaviors may not have been classified as a suicide attempt, it might indicate a feeling of indifference toward staying alive. A patient with a past attempt, especially if recent, merits consideration for inpatient care. Once again, referring previously nonadherent patients to outpatient treatment is less likely to be effective.
8. Does the patient have a support network?
Before discharging a patient who has made a suicide attempt, consider the quality of their support network. Gauging the response of the family and friends to the patient’s attempt can be beneficial. Indifference or resentment on the part of loved ones is a bad sign. Some patients have access to support networks they either did not know were available or chose not to utilize. In other instances, after realizing how depressed the patient has been, the family might provide a new safety net. Strong religious affiliations can also be valuable because devout spirituality can be a deterrent to suicide behaviors.10 For an individual whose attempt was motivated by loneliness or feeling unloved or underappreciated, a newly realized support network can be an additional protective deterrent.
9. Does the patient have a family history of suicide?
There may be a familial component to suicide. Knowing about any suicide history in the family contributes to future therapeutic planning. The clinician may want to explore the patient’s family suicide history in detail because such information can have substantial impact on the patient’s motivation for attempting suicide. The evaluator may want to determine if the anniversary of a family suicide is coming. Triggers for a suicide attempt could include the anniversary of a death, birthdays, family-oriented holidays, and similar events. It is productive to understand how the patient feels about family members who have died by suicide. Some will empathize with the deceased, commenting that they did the “right thing.” Others, upon realizing how their own attempt affected others, will be remorseful and determined not to inflict more pain on their family. Such patients may need to be reminded of the misery associated with their family being left without them. These understandings are helpful at setting a safe disposition. However, a history of death by suicide in the family should always be thoroughly evaluated, regardless of the patient’s attitude about that death.
Continue to: Was the attempt the result of depression?
10. Was the attempt the result of depression?
For a patient experiencing depressive symptoms, the prognosis is less positive; they are more likely to harbor serious intent, premeditation, hopelessness, and social isolation, and less likely to express future-oriented thought. They often exhibit a temporary “flight into health.” Such progress is often transitory and may not represent recovery. Because mood disorders may still be present despite a temporary improvement, inpatient and pharmacologic treatment may be needed. If a patient’s suicide attempt occurred as a result of severe depression, it is possible they will make another suicide attempt unless their depression is addressed in a safe and secure setting, such as inpatient hospitalization, or through close family observation while the patient is receiving intensive outpatient treatment.
11. Does the patient have a psychotic disorder?
Many patients with a psychotic illness die following their first attempt without ever having contact with a mental health professional.11 Features of psychosis might include malevolent auditory hallucinations that suggest self-destruction.11 Such “voices” can be intense and self-deprecating; many patients with this type of hallucination report having made a suicide attempt “just to make the voices stop.”
Symptoms of paranoia can make it less likely for individuals with psychosis to confide in family members, friends, or medical personnel. Religious elements are often of a delusional nature and can be dangerous. Psychosis is more difficult to hide than depression and the presence of psychoses concurrent with major depressive disorder (MDD) increases the probability of suicidality.11 Psychosis secondary to substance use may diminish inhibitions and heighten impulsivity, thereby exacerbating the likelihood of self-harm. Usually, the presence of psychotic features precipitating or following a suicide attempt leads to psychiatric hospitalization.
12. Is the patient in a high-risk demographic group?
When evaluating a patient who has attempted suicide, it helps to consider not just what they did, but who they are. Specifically, does the individual belong to a demographic group that traditionally has a high rate of suicide? For example, patients who are Native American or Alaska Natives warrant extra caution.2 Older White males, especially those who are divorced, widowed, retired, and/or have chronic health problems, are also at greater risk. Compared to the general population, individuals age >80 have a massively elevated chance for self-induced death.12 Some of the reasons include:
- medical comorbidities make surviving an attempt less likely
- access to large amounts of medications
- more irreversible issues, such as chronic pain, disability, or widowhood
- living alone, which may delay discovery.
Patients who are members of any of these demographic groups may deserve serious consideration for inpatient psychiatric admission, regardless of other factors.
Continue to: Were drugs or alcohol involved?
13. Were drugs or alcohol involved?
This factor is unique in that it is both a chronic risk factor (SUDs) and a warning sign for imminent suicide, as in the case of an individual who gets intoxicated to disinhibit their fear of death so they can attempt suicide. Alcohol use disorders are associated with depression and suicide. Overdoses by fentanyl and other opiates have become more frequent.13 In many cases, fatalities are unintentional because users overestimate their tolerance or ingest contaminated substances.14 Disinhibition by alcohol and/or other drugs is a risk factor for attempting suicide and can intensify the depth of MDD. Some patients will ingest substances before an attempt just to give them the courage to act; many think of suicide only when intoxicated. Toxicology screens are indicated as part of the evaluation after a suicide attempt.
Depressive and suicidal thoughts often occur in people “coming down” from cocaine or other stimulants. These circumstances require determining whether to refer the patient for treatment for an SUD or psychiatric hospitalization.
In summary, getting intoxicated solely to diminish anxiety about suicide is a dangerous feature, whereas attempting suicide due to intoxication is less concerning. The latter patient may not consider suicide unless they become intoxicated again. When available, dual diagnosis treatment facilities can be an appropriate referral for such patients. Emergency department holding beds can allow these individuals to detoxify prior to the evaluation.
14. Does the patient have future-oriented thoughts?
When evaluating a patient who has attempted suicide, the presence of future planning and anticipation can be reassuring, but these features should be carefully assessed.14-16
After-the-fact comments may be more reliable when a patient offers them spontaneously, as opposed to in response to direct questioning.
- the specificity of the future plans
- corroboration from the family and others about the patient’s previous investment in the upcoming event
- whether the patient mentions such plans spontaneously or only in response to direct questioning
- the patient’s emotional expression or affect when discussing their future
- whether such plans are reasonable, grandiose, and/or unrealistic.
Bottom Line
When assessing a patient after a suicide attempt, both the patient’s presentation and history and the clinician’s instincts are important. Careful consideration of the method, stated intent, premeditation vs impulsivity, feelings about having survived, presence of psychiatric illness, high-risk demographic, postattempt demeanor and affect, quality of support, presence of self-rescue behaviors, future-oriented thoughts, and other factors can help in making the appropriate disposition.
Related Resources
- Kim H, Kim Y, Shin MH, et al. Early psychiatric referral after attempted suicide helps prevent suicide reattempts: a longitudinal national cohort study in South Korea. Front Psychiatry. 2022;13:607892. doi:10.3389/fpsyt.2022.607892
- Michaud L, Berva S, Ostertag L, et al. When to discharge and when to voluntary or compulsory hospitalize? Factors associated with treatment decision after self-harm. Psychiatry Res. 2022;317:114810. doi:10.1016/j.psychres.2022.114810
1. Ten Leading Causes of Death, United States 2020. Centers for Disease Control and Prevention WISQARS. Accessed March 4, 2022. https://wisqars.cdc.gov/data/lcd/home
2. Norris D, Clark MS. Evaluation and treatment of suicidal patients. Am Fam Physician. 2012;15;85(6):602-605.
3. Gliatto MF, Rai AK. Evaluation and treatment patients with suicidal ideation. Am Fam Phys. 1999;59(6):1500-1506.
4. Dazzi T, Gribble R, Wessely S, et al. Does asking about suicide and related behaviors induce suicidal ideation? What is the evidence? Psychol Med. 2014;44(16):3361-3363.
5. Lewiecki EM, Miller SA. Suicide, guns and public policy. Am J Public Health. 2013;103(1):27-31.
6. Frierson RL. Women who shoot themselves. Hosp Community Psychiatry. 1989;40(8):841-843.
7. Frierson RL, Lippmann SB. Psychiatric consultation for patients with self-inflicted gunshot wounds. Psychosomatics. 1990;31(1):67-74.
8. Mitchell AM, Terhorst L. PTSD symptoms in survivors bereaved by the suicide of a significant other. J Am Psychiatr Nurses Assoc. 2017;23(1):61-65.
9. Bateson J. The Golden Gate Bridge’s fatal flaw. Los Angeles Times. May 25, 2012. Accessed March 2, 2022. https://www.latimes.com/opinion/la-xpm-2012-may-25-la-oe-adv-bateson-golden-gate-20120525-story.html
10. Dervic K, Oquendoma MA, Grunebaum MF, et al. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161(12):2303-2308.
11. Nordentoft H, Madsen T, Fedyszyn IF. Suicidal behavior and mortality in first episode psychosis. J Nerv Ment Dis. 2015;203(5):387-392.
12. Frierson R, Lippmann S. Suicide attempts by the old and the very old. Arch Intern Med. 1991;151(1):141-144.
13. Braden JB, Edlund MJ, Sullivan MD. Suicide deaths with opiate poisonings in the United States: 1999-2014. Am J Public Health. 2017;107(3):421-426.
14. Morin KA, Acharya S, Eibl JK, et al: Evidence of increased fentanyl use during the COVID-19 pandemic among opioid agonist treated patients in Ontario, Canada. Int J Drug Policy. 2021;90:103088.
15. Shobassy A, Abu-Mohammad AS. Assessing imminent suicide risk: what about future planning? Current Psychiatry. 2022;21(2):12-17.
16. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
17. Macleod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2010;44(Pt 4):495-504.
In 2021, suicide was the 11th leading cause of death in the United States.1 Suicide resulted in 49,000 US deaths during 2021; it was the second most common cause of death in individuals age 10 to 34, and the fifth leading cause among children.1,2 Women are 3 to 4 times more likely than men to attempt suicide, but men are 4 times more likely to die by suicide.2
The evaluation of patients with suicidal ideation who have not made an attempt generally involves assessing 4 factors: the specific plan, access to lethal means, any recent social stressors, and the presence of a psychiatric disorder.3 The clinician should also assess which potential deterrents, such as religious beliefs or dependent children, might be present.
Mental health clinicians are often called upon to evaluate a patient after a suicide attempt to assess intent for continued self-harm and to determine appropriate disposition. Such an evaluation must consider multiple factors, including the method used, premeditation, consequences of the attempt, the presence of severe depression and/or psychosis, and the role of substance use. Assessment after a suicide attempt differs from the examination of individuals who harbor suicidal thoughts but have not made an attempt; the latter group may be more likely to respond to interventions such as intensive outpatient care, mobilization of family support, and religious proscriptions against suicide. However, for patients who make an attempt to end their life, whatever potential safeguards or deterrents to suicide that were in place obviously did not prevent the self-harm act. The consequences of the attempt, such as disabling injuries or medical complications, and possible involuntary commitment, need to be considered. Assessment of the patient’s feelings about having survived the attempt is important because the psychological impact of the attempt on family members may serve to intensify the patient’s depression and make a subsequent attempt more likely.
Many individuals who think of suicide have communicated self-harm thoughts or intentions, but such comments are often minimized or ignored. There is a common but erroneous belief that if patients are encouraged to discuss thoughts of self-harm, they will be more likely to act upon them. Because the opposite is true,4 clinicians should ask vulnerable patients about suicidal ideation or intent. Importantly, noncompliance with life-saving medical care, risk-taking behaviors, and substance use may also signal a desire for self-harm. Passive thoughts of death, typified by comments such as “I don’t care whether I wake up or not,” should also be elicited. Many patients who think of suicide speak of being in a “bad place” where reason and logic give way to an intense desire to end their misery.
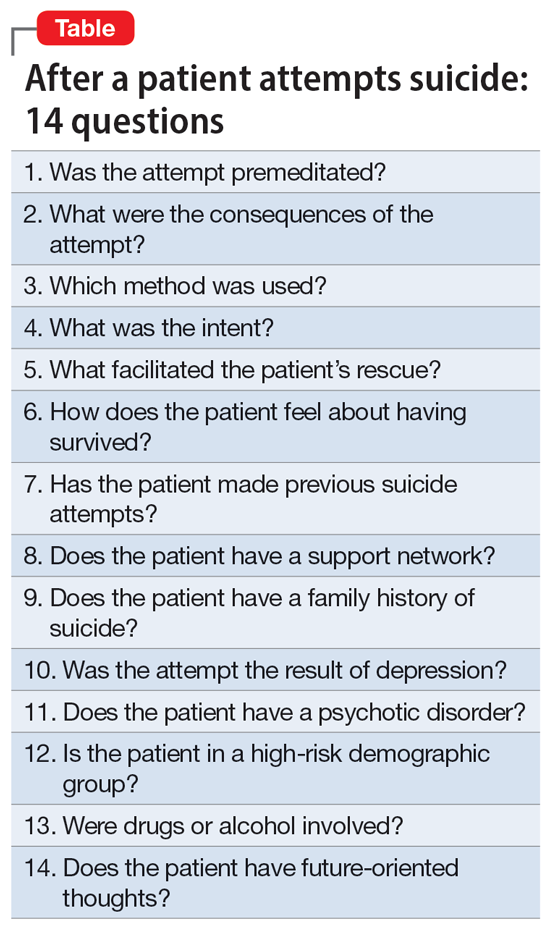
The evaluation of a patient who has attempted suicide is an important component of providing psychiatric care. This article reflects our 45 years of evaluating such patients. As such, it reflects our clinical experience and is not evidence-based. We offer a checklist of 14 questions that we have found helpful when determining if it would be best for a patient to receive inpatient psychiatric hospitalization or a discharge referral for outpatient care (Table). Questions 1 through 6 are specific for patients who have made a suicide attempt, while questions 7 through 14 are helpful for assessing global risk factors for suicide.
1. Was the attempt premeditated?
Determining premeditation vs impulsivity is an essential element of the assessment following a suicide attempt. Many such acts may occur without forethought in response to an unexpected stressor, such as an altercation between partners or family conflicts. Impulsive attempts can occur when an individual is involved in a distressing event and/or while intoxicated. Conversely, premeditation involves forethought and planning, which may increase the risk of suicide in the near future.
Examples of premeditated behavior include:
- Contemplating the attempt days or weeks beforehand
- Researching the effects of a medication or combination of medications in terms of potential lethality
- Engaging in behavior that would decrease the likelihood of their body being discovered after the attempt
- Obtaining weapons and/or stockpiling pills
- Canvassing potential sites such as bridges or tall buildings
- Engaging in a suicide attempt “practice run”
- Leaving a suicide note or message on social media
- Making funeral arrangements, such as choosing burial clothing
- Writing a will and arranging for the custody of dependent children
- Purchasing life insurance that does not deny payment of benefits in cases of death by suicide.
Continue to: Patients with a premeditated...
Patients with a premeditated suicide attempt generally do not expect to survive and are often surprised or upset that the act was not fatal. The presence of indicators that the attempt was premeditated should direct the disposition more toward hospitalization than discharge. In assessing the impact of premeditation, it is important to gauge not just the examples listed above, but also the patient’s perception of these issues (such as potential loss of child custody). Consider how much the patient is emotionally affected by such thinking.
2. What were the consequences of the attempt?
Assessing the reason for the attempt (if any) and determining whether the inciting circumstance has changed due to the suicide attempt are an important part of the evaluation. A suicide attempt may result in reconciliation with and/or renewed support from family members or partners, who might not have been aware of the patient’s emotional distress. Such unexpected support often results in the patient exhibiting improved mood and affect, and possibly temporary resolution of suicidal thoughts. This “flight into health” may be short-lived, but it also may be enough to engage the patient in a therapeutic alliance. That may permit a discharge with safe disposition to the outpatient clinic while in the custody of a family member, partner, or close friend.
Alternatively, some people experience a troubling worsening of precipitants following a suicide attempt. Preexisting medical conditions and financial, occupational, and/or social woes may be exacerbated. Child custody determinations may be affected, assuming the patient understands the possibility of this adverse consequence. Violent methods may result in disfigurement and body image issues. Individuals from small, close-knit communities may experience stigmatization and unwanted notoriety because of their suicide attempt. Such negative consequences may render some patients more likely to make another attempt to die by suicide. It is crucial to consider how a suicide attempt may have changed the original stress that led to the attempt.
3. Which method was used?
Most fatal suicides in the US are by firearms, and many individuals who survive such attempts do so because of unfamiliarity with the weapon, gun malfunction, faulty aim, or alcohol use.5-7 Some survivors report intending to shoot themselves in the heart, but instead suffered shoulder injuries. Unfortunately, for a patient who survives self-inflicted gunshot wounds, the sequelae of chronic pain, multiple surgical procedures, disability, and disfigurement may serve as constant negative reminders of the event. Some individuals with suicidal intent eschew the idea of using firearms because they hope to avoid having a family member be the first to discover them. Witnessing the aftermath of a fatal suicide by gunshot can induce symptoms of posttraumatic stress disorder in family members and/or partners.8
For a patient with self-inflicted gunshot wounds, always determine whether the weapon has been secured or if the patient still has access to it. Asking about weapon availability is essential during the evaluation of any patient with depression, major life crises, or other factors that may yield a desire to die; this is especially true for individuals with substance use disorders (SUDs). Whenever readily available to such individuals, weapons need to be safely removed.
Continue to: Other self-harm methods...
Other self-harm methods with a high degree of lethality include jumping from bridges or buildings, poisonings, self-immolation, cutting, and hangings. Individuals who choose these approaches generally do not intend to survive. Many of these methods also entail premeditation, as in the case of individuals who canvass bridges and note time when traffic is light so they are less likely to be interrupted. Between 1937 and 2012, there were >1,600 deaths by suicide from San Francisco’s Golden Gate Bridge.9 Patients who choose highly lethal methods are often irritated during the postattempt evaluation because their plans were not fatal. Usually, patients who choose such potentially lethal methods are hospitalized initially on medical and surgical floors, and receive most of their psychiatric care from consultation psychiatrists. Following discharge, these patients may be at high risk for subsequent suicide attempts.
In the US, the most common method of attempting suicide is by overdose.4 Lethality is determined by the agent or combination of substances ingested, the amount taken, the person’s health status, and the length of time before they are discovered. Many patients mistakenly assume that readily available agents such as acetaminophen and aspirin are less likely to be fatal than prescription medications. Evaluators may want to assess for suicidality in individuals with erratic, risk-taking behaviors, who are at especially high risk for death. Learning about the method the patient used can help the clinician determine the imminent risk of another suicide attempt. The more potentially fatal the patient’s method, the more serious their suicide intent, and the higher the risk they will make another suicide attempt, possibly using an even more lethal method.
4. What was the intent?
“What did you want to happen when you made this attempt?” Many patients will respond that they wanted to die, sleep, not wake up, or did not care what happened. Others say it was a gesture to evoke a certain response from another person. If this is the case, it is important to know whether the desired outcome was achieved. These so-called gestures often involve making sure the intended person is aware of the attempt, often by writing a letter, sending a text, or posting on social media. Such behaviors may be exhibited by patients with personality disorders. While such attempts often are impulsive, if the attempt fails to generate the anticipated effect, the patient may try to gain more attention by escalating their suicide actions.
Conversely, if a spouse or partner reconciles with the patient solely because of a suicide attempt, this may set a pattern for future self-harm events in which the patient hopes to achieve the same outcome. Nevertheless, it is better to err for safety because some of these patients will make another attempt, just to prove that they should have been taken more seriously. An exploration of such intent can help the evaluation because even supposed “gestures” can have dangerous consequences. Acts that do not result in the desired outcome should precipitate hospitalization rather than discharge.
5. What facilitated the patient’s rescue?
“Why is this patient still alive?” Determine if the patient did anything to save themself, such as calling an ambulance, inducing emesis, telling someone what they did, or coming to the hospital on their own. If yes, asking them what changed their mind may provide information about what exists in their lives to potentially prevent future attempts, or about wishes to stay alive. These issues can be used to guide outpatient therapy.
Continue to: How does the patient feel about having survived?
6. How does the patient feel about having survived?
When a patient is asked how they feel about having survived a suicide attempt, some will label their act “stupid” and profess embarrassment. Others exhibit future-oriented thought, which is a very good prognostic sign. More ominous is subsequent dysphoria or lamenting that “I could not even do this right.” Patients often express anger toward anyone who rescued them, especially those whose attempts were carefully planned or were discovered by accident. Some patients might also express ambivalence about having survived.
The patient’s response to this question may be shaped by their desire to avoid hospitalization, so beyond their verbal answers, be attentive to clinical cues that may suggest the patient is not being fully transparent. Anger or ambivalence about having survived, a lack of future-oriented thought, and a restricted affect despite verbalizing joy about still being alive are features that suggest psychiatric hospitalization may be warranted.
7. Has the patient made previous suicide attempts?
Compared to individuals with no previous suicide attempts, patients with a history of suicide attempts are 30 to 40 times more likely to die by suicide.2 Many patients who present after a suicide attempt have tried to kill themselves multiple times. Exploring the number of past attempts, how recent the attempts were, and what dispositions were made can be of benefit. Reviewing the potential lethality of past attempts (eg, was hospitalization required, was the patient placed in an intensive care unit, and/or was intubation needed) is recommended. If outpatient care was suggested or medication prescribed, was the patient adherent? Consider asking about passive suicidal behavior, such as not seeking care for medical issues, discontinuing life-saving medication, or engaging in reckless behavior. While such behaviors may not have been classified as a suicide attempt, it might indicate a feeling of indifference toward staying alive. A patient with a past attempt, especially if recent, merits consideration for inpatient care. Once again, referring previously nonadherent patients to outpatient treatment is less likely to be effective.
8. Does the patient have a support network?
Before discharging a patient who has made a suicide attempt, consider the quality of their support network. Gauging the response of the family and friends to the patient’s attempt can be beneficial. Indifference or resentment on the part of loved ones is a bad sign. Some patients have access to support networks they either did not know were available or chose not to utilize. In other instances, after realizing how depressed the patient has been, the family might provide a new safety net. Strong religious affiliations can also be valuable because devout spirituality can be a deterrent to suicide behaviors.10 For an individual whose attempt was motivated by loneliness or feeling unloved or underappreciated, a newly realized support network can be an additional protective deterrent.
9. Does the patient have a family history of suicide?
There may be a familial component to suicide. Knowing about any suicide history in the family contributes to future therapeutic planning. The clinician may want to explore the patient’s family suicide history in detail because such information can have substantial impact on the patient’s motivation for attempting suicide. The evaluator may want to determine if the anniversary of a family suicide is coming. Triggers for a suicide attempt could include the anniversary of a death, birthdays, family-oriented holidays, and similar events. It is productive to understand how the patient feels about family members who have died by suicide. Some will empathize with the deceased, commenting that they did the “right thing.” Others, upon realizing how their own attempt affected others, will be remorseful and determined not to inflict more pain on their family. Such patients may need to be reminded of the misery associated with their family being left without them. These understandings are helpful at setting a safe disposition. However, a history of death by suicide in the family should always be thoroughly evaluated, regardless of the patient’s attitude about that death.
Continue to: Was the attempt the result of depression?
10. Was the attempt the result of depression?
For a patient experiencing depressive symptoms, the prognosis is less positive; they are more likely to harbor serious intent, premeditation, hopelessness, and social isolation, and less likely to express future-oriented thought. They often exhibit a temporary “flight into health.” Such progress is often transitory and may not represent recovery. Because mood disorders may still be present despite a temporary improvement, inpatient and pharmacologic treatment may be needed. If a patient’s suicide attempt occurred as a result of severe depression, it is possible they will make another suicide attempt unless their depression is addressed in a safe and secure setting, such as inpatient hospitalization, or through close family observation while the patient is receiving intensive outpatient treatment.
11. Does the patient have a psychotic disorder?
Many patients with a psychotic illness die following their first attempt without ever having contact with a mental health professional.11 Features of psychosis might include malevolent auditory hallucinations that suggest self-destruction.11 Such “voices” can be intense and self-deprecating; many patients with this type of hallucination report having made a suicide attempt “just to make the voices stop.”
Symptoms of paranoia can make it less likely for individuals with psychosis to confide in family members, friends, or medical personnel. Religious elements are often of a delusional nature and can be dangerous. Psychosis is more difficult to hide than depression and the presence of psychoses concurrent with major depressive disorder (MDD) increases the probability of suicidality.11 Psychosis secondary to substance use may diminish inhibitions and heighten impulsivity, thereby exacerbating the likelihood of self-harm. Usually, the presence of psychotic features precipitating or following a suicide attempt leads to psychiatric hospitalization.
12. Is the patient in a high-risk demographic group?
When evaluating a patient who has attempted suicide, it helps to consider not just what they did, but who they are. Specifically, does the individual belong to a demographic group that traditionally has a high rate of suicide? For example, patients who are Native American or Alaska Natives warrant extra caution.2 Older White males, especially those who are divorced, widowed, retired, and/or have chronic health problems, are also at greater risk. Compared to the general population, individuals age >80 have a massively elevated chance for self-induced death.12 Some of the reasons include:
- medical comorbidities make surviving an attempt less likely
- access to large amounts of medications
- more irreversible issues, such as chronic pain, disability, or widowhood
- living alone, which may delay discovery.
Patients who are members of any of these demographic groups may deserve serious consideration for inpatient psychiatric admission, regardless of other factors.
Continue to: Were drugs or alcohol involved?
13. Were drugs or alcohol involved?
This factor is unique in that it is both a chronic risk factor (SUDs) and a warning sign for imminent suicide, as in the case of an individual who gets intoxicated to disinhibit their fear of death so they can attempt suicide. Alcohol use disorders are associated with depression and suicide. Overdoses by fentanyl and other opiates have become more frequent.13 In many cases, fatalities are unintentional because users overestimate their tolerance or ingest contaminated substances.14 Disinhibition by alcohol and/or other drugs is a risk factor for attempting suicide and can intensify the depth of MDD. Some patients will ingest substances before an attempt just to give them the courage to act; many think of suicide only when intoxicated. Toxicology screens are indicated as part of the evaluation after a suicide attempt.
Depressive and suicidal thoughts often occur in people “coming down” from cocaine or other stimulants. These circumstances require determining whether to refer the patient for treatment for an SUD or psychiatric hospitalization.
In summary, getting intoxicated solely to diminish anxiety about suicide is a dangerous feature, whereas attempting suicide due to intoxication is less concerning. The latter patient may not consider suicide unless they become intoxicated again. When available, dual diagnosis treatment facilities can be an appropriate referral for such patients. Emergency department holding beds can allow these individuals to detoxify prior to the evaluation.
14. Does the patient have future-oriented thoughts?
When evaluating a patient who has attempted suicide, the presence of future planning and anticipation can be reassuring, but these features should be carefully assessed.14-16
After-the-fact comments may be more reliable when a patient offers them spontaneously, as opposed to in response to direct questioning.
- the specificity of the future plans
- corroboration from the family and others about the patient’s previous investment in the upcoming event
- whether the patient mentions such plans spontaneously or only in response to direct questioning
- the patient’s emotional expression or affect when discussing their future
- whether such plans are reasonable, grandiose, and/or unrealistic.
Bottom Line
When assessing a patient after a suicide attempt, both the patient’s presentation and history and the clinician’s instincts are important. Careful consideration of the method, stated intent, premeditation vs impulsivity, feelings about having survived, presence of psychiatric illness, high-risk demographic, postattempt demeanor and affect, quality of support, presence of self-rescue behaviors, future-oriented thoughts, and other factors can help in making the appropriate disposition.
Related Resources
- Kim H, Kim Y, Shin MH, et al. Early psychiatric referral after attempted suicide helps prevent suicide reattempts: a longitudinal national cohort study in South Korea. Front Psychiatry. 2022;13:607892. doi:10.3389/fpsyt.2022.607892
- Michaud L, Berva S, Ostertag L, et al. When to discharge and when to voluntary or compulsory hospitalize? Factors associated with treatment decision after self-harm. Psychiatry Res. 2022;317:114810. doi:10.1016/j.psychres.2022.114810
In 2021, suicide was the 11th leading cause of death in the United States.1 Suicide resulted in 49,000 US deaths during 2021; it was the second most common cause of death in individuals age 10 to 34, and the fifth leading cause among children.1,2 Women are 3 to 4 times more likely than men to attempt suicide, but men are 4 times more likely to die by suicide.2
The evaluation of patients with suicidal ideation who have not made an attempt generally involves assessing 4 factors: the specific plan, access to lethal means, any recent social stressors, and the presence of a psychiatric disorder.3 The clinician should also assess which potential deterrents, such as religious beliefs or dependent children, might be present.
Mental health clinicians are often called upon to evaluate a patient after a suicide attempt to assess intent for continued self-harm and to determine appropriate disposition. Such an evaluation must consider multiple factors, including the method used, premeditation, consequences of the attempt, the presence of severe depression and/or psychosis, and the role of substance use. Assessment after a suicide attempt differs from the examination of individuals who harbor suicidal thoughts but have not made an attempt; the latter group may be more likely to respond to interventions such as intensive outpatient care, mobilization of family support, and religious proscriptions against suicide. However, for patients who make an attempt to end their life, whatever potential safeguards or deterrents to suicide that were in place obviously did not prevent the self-harm act. The consequences of the attempt, such as disabling injuries or medical complications, and possible involuntary commitment, need to be considered. Assessment of the patient’s feelings about having survived the attempt is important because the psychological impact of the attempt on family members may serve to intensify the patient’s depression and make a subsequent attempt more likely.
Many individuals who think of suicide have communicated self-harm thoughts or intentions, but such comments are often minimized or ignored. There is a common but erroneous belief that if patients are encouraged to discuss thoughts of self-harm, they will be more likely to act upon them. Because the opposite is true,4 clinicians should ask vulnerable patients about suicidal ideation or intent. Importantly, noncompliance with life-saving medical care, risk-taking behaviors, and substance use may also signal a desire for self-harm. Passive thoughts of death, typified by comments such as “I don’t care whether I wake up or not,” should also be elicited. Many patients who think of suicide speak of being in a “bad place” where reason and logic give way to an intense desire to end their misery.
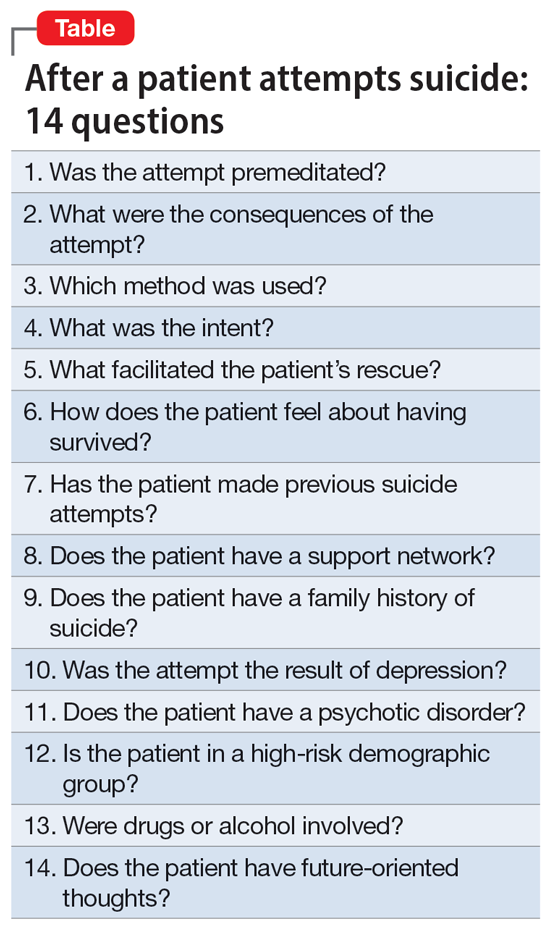
The evaluation of a patient who has attempted suicide is an important component of providing psychiatric care. This article reflects our 45 years of evaluating such patients. As such, it reflects our clinical experience and is not evidence-based. We offer a checklist of 14 questions that we have found helpful when determining if it would be best for a patient to receive inpatient psychiatric hospitalization or a discharge referral for outpatient care (Table). Questions 1 through 6 are specific for patients who have made a suicide attempt, while questions 7 through 14 are helpful for assessing global risk factors for suicide.
1. Was the attempt premeditated?
Determining premeditation vs impulsivity is an essential element of the assessment following a suicide attempt. Many such acts may occur without forethought in response to an unexpected stressor, such as an altercation between partners or family conflicts. Impulsive attempts can occur when an individual is involved in a distressing event and/or while intoxicated. Conversely, premeditation involves forethought and planning, which may increase the risk of suicide in the near future.
Examples of premeditated behavior include:
- Contemplating the attempt days or weeks beforehand
- Researching the effects of a medication or combination of medications in terms of potential lethality
- Engaging in behavior that would decrease the likelihood of their body being discovered after the attempt
- Obtaining weapons and/or stockpiling pills
- Canvassing potential sites such as bridges or tall buildings
- Engaging in a suicide attempt “practice run”
- Leaving a suicide note or message on social media
- Making funeral arrangements, such as choosing burial clothing
- Writing a will and arranging for the custody of dependent children
- Purchasing life insurance that does not deny payment of benefits in cases of death by suicide.
Continue to: Patients with a premeditated...
Patients with a premeditated suicide attempt generally do not expect to survive and are often surprised or upset that the act was not fatal. The presence of indicators that the attempt was premeditated should direct the disposition more toward hospitalization than discharge. In assessing the impact of premeditation, it is important to gauge not just the examples listed above, but also the patient’s perception of these issues (such as potential loss of child custody). Consider how much the patient is emotionally affected by such thinking.
2. What were the consequences of the attempt?
Assessing the reason for the attempt (if any) and determining whether the inciting circumstance has changed due to the suicide attempt are an important part of the evaluation. A suicide attempt may result in reconciliation with and/or renewed support from family members or partners, who might not have been aware of the patient’s emotional distress. Such unexpected support often results in the patient exhibiting improved mood and affect, and possibly temporary resolution of suicidal thoughts. This “flight into health” may be short-lived, but it also may be enough to engage the patient in a therapeutic alliance. That may permit a discharge with safe disposition to the outpatient clinic while in the custody of a family member, partner, or close friend.
Alternatively, some people experience a troubling worsening of precipitants following a suicide attempt. Preexisting medical conditions and financial, occupational, and/or social woes may be exacerbated. Child custody determinations may be affected, assuming the patient understands the possibility of this adverse consequence. Violent methods may result in disfigurement and body image issues. Individuals from small, close-knit communities may experience stigmatization and unwanted notoriety because of their suicide attempt. Such negative consequences may render some patients more likely to make another attempt to die by suicide. It is crucial to consider how a suicide attempt may have changed the original stress that led to the attempt.
3. Which method was used?
Most fatal suicides in the US are by firearms, and many individuals who survive such attempts do so because of unfamiliarity with the weapon, gun malfunction, faulty aim, or alcohol use.5-7 Some survivors report intending to shoot themselves in the heart, but instead suffered shoulder injuries. Unfortunately, for a patient who survives self-inflicted gunshot wounds, the sequelae of chronic pain, multiple surgical procedures, disability, and disfigurement may serve as constant negative reminders of the event. Some individuals with suicidal intent eschew the idea of using firearms because they hope to avoid having a family member be the first to discover them. Witnessing the aftermath of a fatal suicide by gunshot can induce symptoms of posttraumatic stress disorder in family members and/or partners.8
For a patient with self-inflicted gunshot wounds, always determine whether the weapon has been secured or if the patient still has access to it. Asking about weapon availability is essential during the evaluation of any patient with depression, major life crises, or other factors that may yield a desire to die; this is especially true for individuals with substance use disorders (SUDs). Whenever readily available to such individuals, weapons need to be safely removed.
Continue to: Other self-harm methods...
Other self-harm methods with a high degree of lethality include jumping from bridges or buildings, poisonings, self-immolation, cutting, and hangings. Individuals who choose these approaches generally do not intend to survive. Many of these methods also entail premeditation, as in the case of individuals who canvass bridges and note time when traffic is light so they are less likely to be interrupted. Between 1937 and 2012, there were >1,600 deaths by suicide from San Francisco’s Golden Gate Bridge.9 Patients who choose highly lethal methods are often irritated during the postattempt evaluation because their plans were not fatal. Usually, patients who choose such potentially lethal methods are hospitalized initially on medical and surgical floors, and receive most of their psychiatric care from consultation psychiatrists. Following discharge, these patients may be at high risk for subsequent suicide attempts.
In the US, the most common method of attempting suicide is by overdose.4 Lethality is determined by the agent or combination of substances ingested, the amount taken, the person’s health status, and the length of time before they are discovered. Many patients mistakenly assume that readily available agents such as acetaminophen and aspirin are less likely to be fatal than prescription medications. Evaluators may want to assess for suicidality in individuals with erratic, risk-taking behaviors, who are at especially high risk for death. Learning about the method the patient used can help the clinician determine the imminent risk of another suicide attempt. The more potentially fatal the patient’s method, the more serious their suicide intent, and the higher the risk they will make another suicide attempt, possibly using an even more lethal method.
4. What was the intent?
“What did you want to happen when you made this attempt?” Many patients will respond that they wanted to die, sleep, not wake up, or did not care what happened. Others say it was a gesture to evoke a certain response from another person. If this is the case, it is important to know whether the desired outcome was achieved. These so-called gestures often involve making sure the intended person is aware of the attempt, often by writing a letter, sending a text, or posting on social media. Such behaviors may be exhibited by patients with personality disorders. While such attempts often are impulsive, if the attempt fails to generate the anticipated effect, the patient may try to gain more attention by escalating their suicide actions.
Conversely, if a spouse or partner reconciles with the patient solely because of a suicide attempt, this may set a pattern for future self-harm events in which the patient hopes to achieve the same outcome. Nevertheless, it is better to err for safety because some of these patients will make another attempt, just to prove that they should have been taken more seriously. An exploration of such intent can help the evaluation because even supposed “gestures” can have dangerous consequences. Acts that do not result in the desired outcome should precipitate hospitalization rather than discharge.
5. What facilitated the patient’s rescue?
“Why is this patient still alive?” Determine if the patient did anything to save themself, such as calling an ambulance, inducing emesis, telling someone what they did, or coming to the hospital on their own. If yes, asking them what changed their mind may provide information about what exists in their lives to potentially prevent future attempts, or about wishes to stay alive. These issues can be used to guide outpatient therapy.
Continue to: How does the patient feel about having survived?
6. How does the patient feel about having survived?
When a patient is asked how they feel about having survived a suicide attempt, some will label their act “stupid” and profess embarrassment. Others exhibit future-oriented thought, which is a very good prognostic sign. More ominous is subsequent dysphoria or lamenting that “I could not even do this right.” Patients often express anger toward anyone who rescued them, especially those whose attempts were carefully planned or were discovered by accident. Some patients might also express ambivalence about having survived.
The patient’s response to this question may be shaped by their desire to avoid hospitalization, so beyond their verbal answers, be attentive to clinical cues that may suggest the patient is not being fully transparent. Anger or ambivalence about having survived, a lack of future-oriented thought, and a restricted affect despite verbalizing joy about still being alive are features that suggest psychiatric hospitalization may be warranted.
7. Has the patient made previous suicide attempts?
Compared to individuals with no previous suicide attempts, patients with a history of suicide attempts are 30 to 40 times more likely to die by suicide.2 Many patients who present after a suicide attempt have tried to kill themselves multiple times. Exploring the number of past attempts, how recent the attempts were, and what dispositions were made can be of benefit. Reviewing the potential lethality of past attempts (eg, was hospitalization required, was the patient placed in an intensive care unit, and/or was intubation needed) is recommended. If outpatient care was suggested or medication prescribed, was the patient adherent? Consider asking about passive suicidal behavior, such as not seeking care for medical issues, discontinuing life-saving medication, or engaging in reckless behavior. While such behaviors may not have been classified as a suicide attempt, it might indicate a feeling of indifference toward staying alive. A patient with a past attempt, especially if recent, merits consideration for inpatient care. Once again, referring previously nonadherent patients to outpatient treatment is less likely to be effective.
8. Does the patient have a support network?
Before discharging a patient who has made a suicide attempt, consider the quality of their support network. Gauging the response of the family and friends to the patient’s attempt can be beneficial. Indifference or resentment on the part of loved ones is a bad sign. Some patients have access to support networks they either did not know were available or chose not to utilize. In other instances, after realizing how depressed the patient has been, the family might provide a new safety net. Strong religious affiliations can also be valuable because devout spirituality can be a deterrent to suicide behaviors.10 For an individual whose attempt was motivated by loneliness or feeling unloved or underappreciated, a newly realized support network can be an additional protective deterrent.
9. Does the patient have a family history of suicide?
There may be a familial component to suicide. Knowing about any suicide history in the family contributes to future therapeutic planning. The clinician may want to explore the patient’s family suicide history in detail because such information can have substantial impact on the patient’s motivation for attempting suicide. The evaluator may want to determine if the anniversary of a family suicide is coming. Triggers for a suicide attempt could include the anniversary of a death, birthdays, family-oriented holidays, and similar events. It is productive to understand how the patient feels about family members who have died by suicide. Some will empathize with the deceased, commenting that they did the “right thing.” Others, upon realizing how their own attempt affected others, will be remorseful and determined not to inflict more pain on their family. Such patients may need to be reminded of the misery associated with their family being left without them. These understandings are helpful at setting a safe disposition. However, a history of death by suicide in the family should always be thoroughly evaluated, regardless of the patient’s attitude about that death.
Continue to: Was the attempt the result of depression?
10. Was the attempt the result of depression?
For a patient experiencing depressive symptoms, the prognosis is less positive; they are more likely to harbor serious intent, premeditation, hopelessness, and social isolation, and less likely to express future-oriented thought. They often exhibit a temporary “flight into health.” Such progress is often transitory and may not represent recovery. Because mood disorders may still be present despite a temporary improvement, inpatient and pharmacologic treatment may be needed. If a patient’s suicide attempt occurred as a result of severe depression, it is possible they will make another suicide attempt unless their depression is addressed in a safe and secure setting, such as inpatient hospitalization, or through close family observation while the patient is receiving intensive outpatient treatment.
11. Does the patient have a psychotic disorder?
Many patients with a psychotic illness die following their first attempt without ever having contact with a mental health professional.11 Features of psychosis might include malevolent auditory hallucinations that suggest self-destruction.11 Such “voices” can be intense and self-deprecating; many patients with this type of hallucination report having made a suicide attempt “just to make the voices stop.”
Symptoms of paranoia can make it less likely for individuals with psychosis to confide in family members, friends, or medical personnel. Religious elements are often of a delusional nature and can be dangerous. Psychosis is more difficult to hide than depression and the presence of psychoses concurrent with major depressive disorder (MDD) increases the probability of suicidality.11 Psychosis secondary to substance use may diminish inhibitions and heighten impulsivity, thereby exacerbating the likelihood of self-harm. Usually, the presence of psychotic features precipitating or following a suicide attempt leads to psychiatric hospitalization.
12. Is the patient in a high-risk demographic group?
When evaluating a patient who has attempted suicide, it helps to consider not just what they did, but who they are. Specifically, does the individual belong to a demographic group that traditionally has a high rate of suicide? For example, patients who are Native American or Alaska Natives warrant extra caution.2 Older White males, especially those who are divorced, widowed, retired, and/or have chronic health problems, are also at greater risk. Compared to the general population, individuals age >80 have a massively elevated chance for self-induced death.12 Some of the reasons include:
- medical comorbidities make surviving an attempt less likely
- access to large amounts of medications
- more irreversible issues, such as chronic pain, disability, or widowhood
- living alone, which may delay discovery.
Patients who are members of any of these demographic groups may deserve serious consideration for inpatient psychiatric admission, regardless of other factors.
Continue to: Were drugs or alcohol involved?
13. Were drugs or alcohol involved?
This factor is unique in that it is both a chronic risk factor (SUDs) and a warning sign for imminent suicide, as in the case of an individual who gets intoxicated to disinhibit their fear of death so they can attempt suicide. Alcohol use disorders are associated with depression and suicide. Overdoses by fentanyl and other opiates have become more frequent.13 In many cases, fatalities are unintentional because users overestimate their tolerance or ingest contaminated substances.14 Disinhibition by alcohol and/or other drugs is a risk factor for attempting suicide and can intensify the depth of MDD. Some patients will ingest substances before an attempt just to give them the courage to act; many think of suicide only when intoxicated. Toxicology screens are indicated as part of the evaluation after a suicide attempt.
Depressive and suicidal thoughts often occur in people “coming down” from cocaine or other stimulants. These circumstances require determining whether to refer the patient for treatment for an SUD or psychiatric hospitalization.
In summary, getting intoxicated solely to diminish anxiety about suicide is a dangerous feature, whereas attempting suicide due to intoxication is less concerning. The latter patient may not consider suicide unless they become intoxicated again. When available, dual diagnosis treatment facilities can be an appropriate referral for such patients. Emergency department holding beds can allow these individuals to detoxify prior to the evaluation.
14. Does the patient have future-oriented thoughts?
When evaluating a patient who has attempted suicide, the presence of future planning and anticipation can be reassuring, but these features should be carefully assessed.14-16
After-the-fact comments may be more reliable when a patient offers them spontaneously, as opposed to in response to direct questioning.
- the specificity of the future plans
- corroboration from the family and others about the patient’s previous investment in the upcoming event
- whether the patient mentions such plans spontaneously or only in response to direct questioning
- the patient’s emotional expression or affect when discussing their future
- whether such plans are reasonable, grandiose, and/or unrealistic.
Bottom Line
When assessing a patient after a suicide attempt, both the patient’s presentation and history and the clinician’s instincts are important. Careful consideration of the method, stated intent, premeditation vs impulsivity, feelings about having survived, presence of psychiatric illness, high-risk demographic, postattempt demeanor and affect, quality of support, presence of self-rescue behaviors, future-oriented thoughts, and other factors can help in making the appropriate disposition.
Related Resources
- Kim H, Kim Y, Shin MH, et al. Early psychiatric referral after attempted suicide helps prevent suicide reattempts: a longitudinal national cohort study in South Korea. Front Psychiatry. 2022;13:607892. doi:10.3389/fpsyt.2022.607892
- Michaud L, Berva S, Ostertag L, et al. When to discharge and when to voluntary or compulsory hospitalize? Factors associated with treatment decision after self-harm. Psychiatry Res. 2022;317:114810. doi:10.1016/j.psychres.2022.114810
1. Ten Leading Causes of Death, United States 2020. Centers for Disease Control and Prevention WISQARS. Accessed March 4, 2022. https://wisqars.cdc.gov/data/lcd/home
2. Norris D, Clark MS. Evaluation and treatment of suicidal patients. Am Fam Physician. 2012;15;85(6):602-605.
3. Gliatto MF, Rai AK. Evaluation and treatment patients with suicidal ideation. Am Fam Phys. 1999;59(6):1500-1506.
4. Dazzi T, Gribble R, Wessely S, et al. Does asking about suicide and related behaviors induce suicidal ideation? What is the evidence? Psychol Med. 2014;44(16):3361-3363.
5. Lewiecki EM, Miller SA. Suicide, guns and public policy. Am J Public Health. 2013;103(1):27-31.
6. Frierson RL. Women who shoot themselves. Hosp Community Psychiatry. 1989;40(8):841-843.
7. Frierson RL, Lippmann SB. Psychiatric consultation for patients with self-inflicted gunshot wounds. Psychosomatics. 1990;31(1):67-74.
8. Mitchell AM, Terhorst L. PTSD symptoms in survivors bereaved by the suicide of a significant other. J Am Psychiatr Nurses Assoc. 2017;23(1):61-65.
9. Bateson J. The Golden Gate Bridge’s fatal flaw. Los Angeles Times. May 25, 2012. Accessed March 2, 2022. https://www.latimes.com/opinion/la-xpm-2012-may-25-la-oe-adv-bateson-golden-gate-20120525-story.html
10. Dervic K, Oquendoma MA, Grunebaum MF, et al. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161(12):2303-2308.
11. Nordentoft H, Madsen T, Fedyszyn IF. Suicidal behavior and mortality in first episode psychosis. J Nerv Ment Dis. 2015;203(5):387-392.
12. Frierson R, Lippmann S. Suicide attempts by the old and the very old. Arch Intern Med. 1991;151(1):141-144.
13. Braden JB, Edlund MJ, Sullivan MD. Suicide deaths with opiate poisonings in the United States: 1999-2014. Am J Public Health. 2017;107(3):421-426.
14. Morin KA, Acharya S, Eibl JK, et al: Evidence of increased fentanyl use during the COVID-19 pandemic among opioid agonist treated patients in Ontario, Canada. Int J Drug Policy. 2021;90:103088.
15. Shobassy A, Abu-Mohammad AS. Assessing imminent suicide risk: what about future planning? Current Psychiatry. 2022;21(2):12-17.
16. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
17. Macleod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2010;44(Pt 4):495-504.
1. Ten Leading Causes of Death, United States 2020. Centers for Disease Control and Prevention WISQARS. Accessed March 4, 2022. https://wisqars.cdc.gov/data/lcd/home
2. Norris D, Clark MS. Evaluation and treatment of suicidal patients. Am Fam Physician. 2012;15;85(6):602-605.
3. Gliatto MF, Rai AK. Evaluation and treatment patients with suicidal ideation. Am Fam Phys. 1999;59(6):1500-1506.
4. Dazzi T, Gribble R, Wessely S, et al. Does asking about suicide and related behaviors induce suicidal ideation? What is the evidence? Psychol Med. 2014;44(16):3361-3363.
5. Lewiecki EM, Miller SA. Suicide, guns and public policy. Am J Public Health. 2013;103(1):27-31.
6. Frierson RL. Women who shoot themselves. Hosp Community Psychiatry. 1989;40(8):841-843.
7. Frierson RL, Lippmann SB. Psychiatric consultation for patients with self-inflicted gunshot wounds. Psychosomatics. 1990;31(1):67-74.
8. Mitchell AM, Terhorst L. PTSD symptoms in survivors bereaved by the suicide of a significant other. J Am Psychiatr Nurses Assoc. 2017;23(1):61-65.
9. Bateson J. The Golden Gate Bridge’s fatal flaw. Los Angeles Times. May 25, 2012. Accessed March 2, 2022. https://www.latimes.com/opinion/la-xpm-2012-may-25-la-oe-adv-bateson-golden-gate-20120525-story.html
10. Dervic K, Oquendoma MA, Grunebaum MF, et al. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161(12):2303-2308.
11. Nordentoft H, Madsen T, Fedyszyn IF. Suicidal behavior and mortality in first episode psychosis. J Nerv Ment Dis. 2015;203(5):387-392.
12. Frierson R, Lippmann S. Suicide attempts by the old and the very old. Arch Intern Med. 1991;151(1):141-144.
13. Braden JB, Edlund MJ, Sullivan MD. Suicide deaths with opiate poisonings in the United States: 1999-2014. Am J Public Health. 2017;107(3):421-426.
14. Morin KA, Acharya S, Eibl JK, et al: Evidence of increased fentanyl use during the COVID-19 pandemic among opioid agonist treated patients in Ontario, Canada. Int J Drug Policy. 2021;90:103088.
15. Shobassy A, Abu-Mohammad AS. Assessing imminent suicide risk: what about future planning? Current Psychiatry. 2022;21(2):12-17.
16. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
17. Macleod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2010;44(Pt 4):495-504.
Intermittent fasting: What to tell patients
Intermittent fasting is the purposeful, restricted intake of food (and sometimes water), usually for health or religious reasons. Common forms are alternative-day fasting or time-restricted fasting, with variable ratios of days or hours for fasting and eating/drinking.1 For example, fasting during Ramadan, the ninth month of the Islamic calendar, occurs from dawn to sunset, for a variable duration due to latitude and seasonal shifts.2 Clinicians are likely to care for a patient who occasionally fasts. While there are potential benefits of fasting, clinicians need to consider the implications for patients who fast, particularly those receiving psychotropic medications.
Potential benefits for weight loss, mood
Some research suggests fasting is popular and may have benefits for an individual’s physical and mental health. In a 2020 online poll (N = 1,241), 24% of respondents said they had tried intermittent fasting, and 87% said the practice was very effective (50%) or somewhat effective (37%) in helping them lose weight.3 While more randomized control trials are needed to examine the practice’s effectiveness in promoting and maintaining weight loss, fasting has been linked to better glucose control in both humans and animals, and patients may have better adherence with fasting compared to caloric restriction alone.1 Improved mood, alertness, tranquility, and sometimes euphoria have been documented among individuals who fast, but these benefits may not be sustained.4 A prospective study of 462 participants who fasted during Ramadan found the practice reduced depression in patients with diabetes, possibly due to mindfulness, decreased inflammation from improved insulin sensitivity, and/or social cohesion.5
Be aware of the potential risks
Fasting may either improve or destabilize mood in people with bipolar disorder by disrupting circadian rhythm and sleep.2 Fasting might exacerbate underlying eating disorders.2 Increased dehydration escalates the risk for orthostatic hypotension, which might require discontinuing clozapine.6 Hypotension and toxicity might arise during lithium pharmacotherapy. The Table4 summarizes things to consider when caring for a patient who fasts while receiving pharmacotherapy.
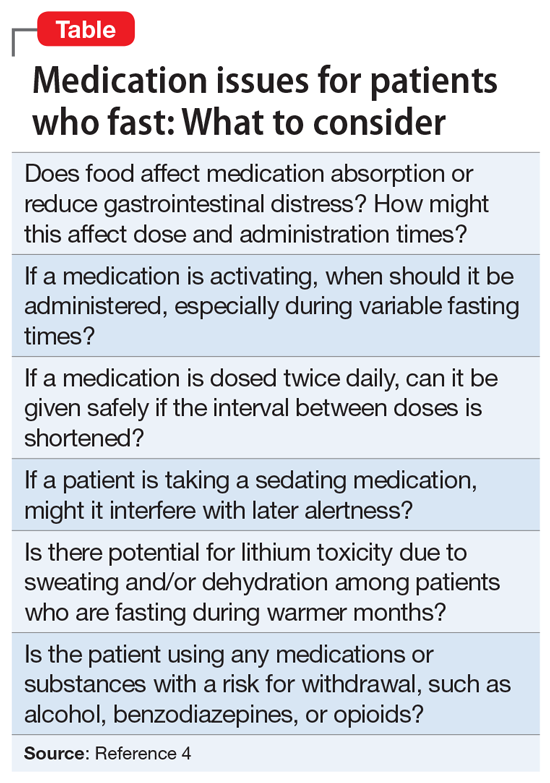
Provide patients with guidance
Advise patients not to fast if you believe it might exacerbate their mental illness, and encourage them to discuss with their primary care physicians any potential worsening of physical illnesses.2 When caring for a patient who fasts for religious reasons, consider consulting with the patient’s religious leaders.2 If patients choose to fast, monitor them for mood destabilization and/or medication adverse effects. If possible, avoid altering drug treatment regimens during fasting, and carefully monitor whenever a pharmaceutical change is necessary. When appropriate, the use of long-acting injectable medications may minimize adverse effects while maintaining mood stability. Encourage patients who fast to ensure they remain hydrated and practice sleep hygiene while they fast.7
1. Dong TA, Sandesara PB, Dhindsa DS, et al. Intermittent fasting: a heart healthy dietary pattern? Am J Med. 2020;133(8):901-907.
2. Fond G, Macgregor A, Leboyer M, et al. Fasting in mood disorders: neurobiology and effectiveness. A review of the literature. Psychiatry Res. 2013;209(3):253-258.
3. Ballard J. Americans say this popular diet is effective and inexpensive. YouGov. February 24, 2020. Accessed January 6, 2022. https://today.yougov.com/topics/food/articles-reports/2020/02/24/most-effective-diet-intermittent-fasting-poll
4. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.
5. Al-Ozairi E, AlAwadhi MM, Al-Ozairi A, et al. A prospective study of the effect of fasting during the month of Ramadan on depression and diabetes distress in people with type 2 diabetes. Diabet Res Clin Pract. 2019;153:145-149.
6. Chehovich C, Demler TL, Leppien E. Impact of Ramadan fasting on medical and psychiatric health. Int Clin Psychopharmacol. 2019;34(6):317-322.
7. Farooq S, Nazar Z, Akhtar J, et al. Effect of fasting during Ramadan on serum lithium level and mental state in bipolar affective disorder. Int Clin Psychopharmacol. 2010;25(6):323-327.
Intermittent fasting is the purposeful, restricted intake of food (and sometimes water), usually for health or religious reasons. Common forms are alternative-day fasting or time-restricted fasting, with variable ratios of days or hours for fasting and eating/drinking.1 For example, fasting during Ramadan, the ninth month of the Islamic calendar, occurs from dawn to sunset, for a variable duration due to latitude and seasonal shifts.2 Clinicians are likely to care for a patient who occasionally fasts. While there are potential benefits of fasting, clinicians need to consider the implications for patients who fast, particularly those receiving psychotropic medications.
Potential benefits for weight loss, mood
Some research suggests fasting is popular and may have benefits for an individual’s physical and mental health. In a 2020 online poll (N = 1,241), 24% of respondents said they had tried intermittent fasting, and 87% said the practice was very effective (50%) or somewhat effective (37%) in helping them lose weight.3 While more randomized control trials are needed to examine the practice’s effectiveness in promoting and maintaining weight loss, fasting has been linked to better glucose control in both humans and animals, and patients may have better adherence with fasting compared to caloric restriction alone.1 Improved mood, alertness, tranquility, and sometimes euphoria have been documented among individuals who fast, but these benefits may not be sustained.4 A prospective study of 462 participants who fasted during Ramadan found the practice reduced depression in patients with diabetes, possibly due to mindfulness, decreased inflammation from improved insulin sensitivity, and/or social cohesion.5
Be aware of the potential risks
Fasting may either improve or destabilize mood in people with bipolar disorder by disrupting circadian rhythm and sleep.2 Fasting might exacerbate underlying eating disorders.2 Increased dehydration escalates the risk for orthostatic hypotension, which might require discontinuing clozapine.6 Hypotension and toxicity might arise during lithium pharmacotherapy. The Table4 summarizes things to consider when caring for a patient who fasts while receiving pharmacotherapy.
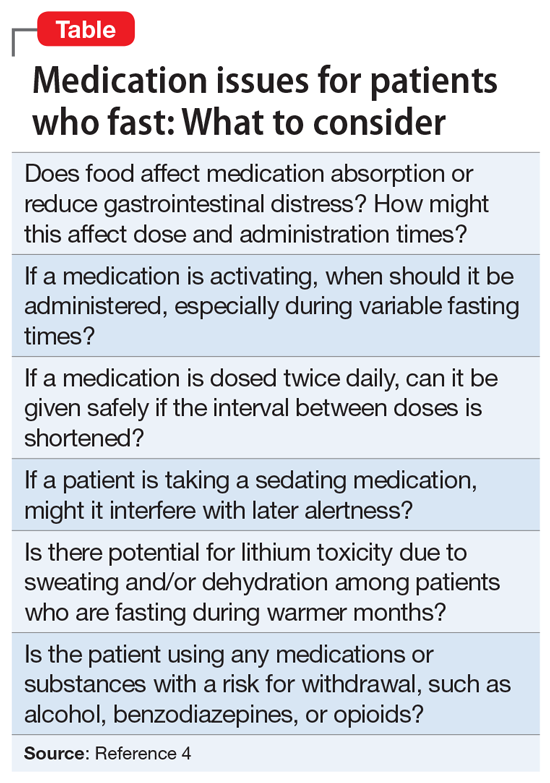
Provide patients with guidance
Advise patients not to fast if you believe it might exacerbate their mental illness, and encourage them to discuss with their primary care physicians any potential worsening of physical illnesses.2 When caring for a patient who fasts for religious reasons, consider consulting with the patient’s religious leaders.2 If patients choose to fast, monitor them for mood destabilization and/or medication adverse effects. If possible, avoid altering drug treatment regimens during fasting, and carefully monitor whenever a pharmaceutical change is necessary. When appropriate, the use of long-acting injectable medications may minimize adverse effects while maintaining mood stability. Encourage patients who fast to ensure they remain hydrated and practice sleep hygiene while they fast.7
Intermittent fasting is the purposeful, restricted intake of food (and sometimes water), usually for health or religious reasons. Common forms are alternative-day fasting or time-restricted fasting, with variable ratios of days or hours for fasting and eating/drinking.1 For example, fasting during Ramadan, the ninth month of the Islamic calendar, occurs from dawn to sunset, for a variable duration due to latitude and seasonal shifts.2 Clinicians are likely to care for a patient who occasionally fasts. While there are potential benefits of fasting, clinicians need to consider the implications for patients who fast, particularly those receiving psychotropic medications.
Potential benefits for weight loss, mood
Some research suggests fasting is popular and may have benefits for an individual’s physical and mental health. In a 2020 online poll (N = 1,241), 24% of respondents said they had tried intermittent fasting, and 87% said the practice was very effective (50%) or somewhat effective (37%) in helping them lose weight.3 While more randomized control trials are needed to examine the practice’s effectiveness in promoting and maintaining weight loss, fasting has been linked to better glucose control in both humans and animals, and patients may have better adherence with fasting compared to caloric restriction alone.1 Improved mood, alertness, tranquility, and sometimes euphoria have been documented among individuals who fast, but these benefits may not be sustained.4 A prospective study of 462 participants who fasted during Ramadan found the practice reduced depression in patients with diabetes, possibly due to mindfulness, decreased inflammation from improved insulin sensitivity, and/or social cohesion.5
Be aware of the potential risks
Fasting may either improve or destabilize mood in people with bipolar disorder by disrupting circadian rhythm and sleep.2 Fasting might exacerbate underlying eating disorders.2 Increased dehydration escalates the risk for orthostatic hypotension, which might require discontinuing clozapine.6 Hypotension and toxicity might arise during lithium pharmacotherapy. The Table4 summarizes things to consider when caring for a patient who fasts while receiving pharmacotherapy.
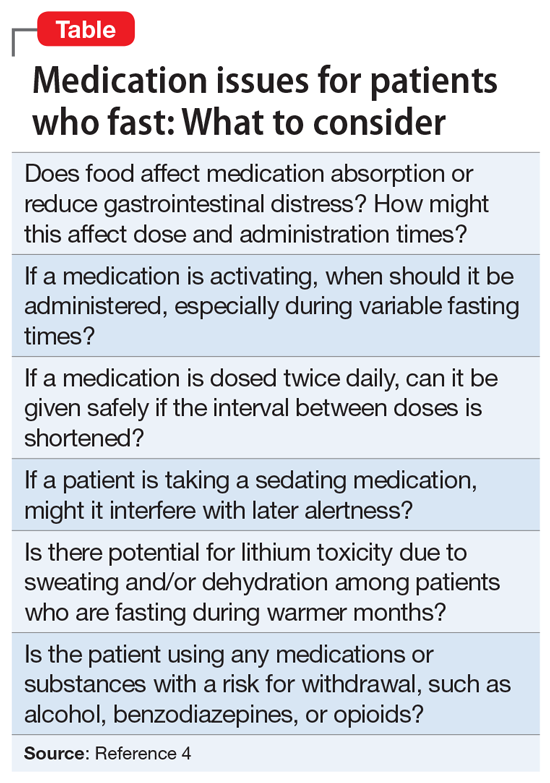
Provide patients with guidance
Advise patients not to fast if you believe it might exacerbate their mental illness, and encourage them to discuss with their primary care physicians any potential worsening of physical illnesses.2 When caring for a patient who fasts for religious reasons, consider consulting with the patient’s religious leaders.2 If patients choose to fast, monitor them for mood destabilization and/or medication adverse effects. If possible, avoid altering drug treatment regimens during fasting, and carefully monitor whenever a pharmaceutical change is necessary. When appropriate, the use of long-acting injectable medications may minimize adverse effects while maintaining mood stability. Encourage patients who fast to ensure they remain hydrated and practice sleep hygiene while they fast.7
1. Dong TA, Sandesara PB, Dhindsa DS, et al. Intermittent fasting: a heart healthy dietary pattern? Am J Med. 2020;133(8):901-907.
2. Fond G, Macgregor A, Leboyer M, et al. Fasting in mood disorders: neurobiology and effectiveness. A review of the literature. Psychiatry Res. 2013;209(3):253-258.
3. Ballard J. Americans say this popular diet is effective and inexpensive. YouGov. February 24, 2020. Accessed January 6, 2022. https://today.yougov.com/topics/food/articles-reports/2020/02/24/most-effective-diet-intermittent-fasting-poll
4. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.
5. Al-Ozairi E, AlAwadhi MM, Al-Ozairi A, et al. A prospective study of the effect of fasting during the month of Ramadan on depression and diabetes distress in people with type 2 diabetes. Diabet Res Clin Pract. 2019;153:145-149.
6. Chehovich C, Demler TL, Leppien E. Impact of Ramadan fasting on medical and psychiatric health. Int Clin Psychopharmacol. 2019;34(6):317-322.
7. Farooq S, Nazar Z, Akhtar J, et al. Effect of fasting during Ramadan on serum lithium level and mental state in bipolar affective disorder. Int Clin Psychopharmacol. 2010;25(6):323-327.
1. Dong TA, Sandesara PB, Dhindsa DS, et al. Intermittent fasting: a heart healthy dietary pattern? Am J Med. 2020;133(8):901-907.
2. Fond G, Macgregor A, Leboyer M, et al. Fasting in mood disorders: neurobiology and effectiveness. A review of the literature. Psychiatry Res. 2013;209(3):253-258.
3. Ballard J. Americans say this popular diet is effective and inexpensive. YouGov. February 24, 2020. Accessed January 6, 2022. https://today.yougov.com/topics/food/articles-reports/2020/02/24/most-effective-diet-intermittent-fasting-poll
4. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.
5. Al-Ozairi E, AlAwadhi MM, Al-Ozairi A, et al. A prospective study of the effect of fasting during the month of Ramadan on depression and diabetes distress in people with type 2 diabetes. Diabet Res Clin Pract. 2019;153:145-149.
6. Chehovich C, Demler TL, Leppien E. Impact of Ramadan fasting on medical and psychiatric health. Int Clin Psychopharmacol. 2019;34(6):317-322.
7. Farooq S, Nazar Z, Akhtar J, et al. Effect of fasting during Ramadan on serum lithium level and mental state in bipolar affective disorder. Int Clin Psychopharmacol. 2010;25(6):323-327.
Building a better work/life balance
Physician burnout is a common and serious problem. In a 2017 survey of >14,000 US physicians across 27 specialties, 42% reported burnout,1 which typically is defined as a long-term stress reaction marked by emotional exhaustion, depersonalization, and a lack of sense of personal accomplishment.2
Creating a focused, yet comfortable professional life is essential for preventing burnout. For our patients’ sake and for our own personal fulfillment, there is much we can do to maintain a healthy professional and home life balance. This article describes the factors that contribute to physician burnout, and outlines steps you can take to improve your work/life balance.
The multifactorial roots of stress
Many physicians frequently blend their professional and personal lives. Most are absorbed in their practices, which leaves limited time for family interactions, daily life, or wellness.
Work hours are often long, and schedules are filled with obligations. In recent years, changes to medical practice have resulted in many additional responsibilities for physicians, such as administrative tasks and adapting to electronic health care, particularly to the use of electronic health records (EHRs). This has escalated workload and worries while diminishing patient interaction, creating more distant clinical relationships and providing less financial remuneration. Monetary pressures to see more patients limit the quality of care. Overload often forces physicians to stay at work late and/or labor excessive hours at home with less family interaction. The introduction of EHRs escalated this trend, while detracting from a healthy family, personal, and professional life. Addressing cumbersome documentation requirements while striving to maintain contact with patients is frustrating.3
Physician job dissatisfaction has worsened over time. Burnout escalates errors, diminishes patient rapport and safety, and produces suboptimal outcomes, all resulting in declining professional satisfaction.
Improving your work/life balance
The following strategies can help you make changes to better balance your professional and personal lives.
Assess priorities and goals. Before taking steps to achieve an optimal work-home balance, first review medical, spousal, and parental expectations. Social support is key.
Continue to: Identify stressors
Identify stressors. Use self-report questionnaires and collegial discussions to assess for the presence and/or severity of burnout. Prevention and/or intervention at personal and organizational levels can positively impact physician well-being.4
Focus on self-care. Prioritize your personal health care, sleep hygiene, exercise routines, quality of diet, and recreational activities. Do not self-prescribe medications, and avoid excessive alcohol use.5
Make changes to your practice. In your office, make efforts to maximize social connectiveness. Consider assigning routine tasks to other staff members. Upgrading your typing skills, employing medical records scribes, and/or using voice recording systems can reduce your workload.5
Advocate for better legislation. Both through professional medical organizations and at government levels, work to modify regulations that require physicians to spend their time on nonclinical tasks. This might include advocating to simplify EHRs and insurance company reimbursement requirements to decrease paperwork and reduce barriers to prescribing. Stress management seminars, which typically are offered at state and national conferences, can foster interpersonal and professional competencies throughout one’s medical career.6 Medical licensure boards should make efforts to reduce the stigma of reporting mental health issues; they should assure confidentiality protection and help for those who seek assistance.5
1. Peckham C. Medscape psychiatrist lifestyle report: race and ethnicity, bias and burnout. Medscape. Published January 11, 2017. Accessed July 12, 2021. http://www.medscape.com/features/slideshow/lifestyle/2017/psychiatry#page=1
2. Agency for Healthcare Research and Quality. Physician burnout. Published July 2017. Accessed July 13, 2021. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
3. Lippmann S. Can shrinks “shrink” the electronic health record? Internet and Psychiatry. December 19, 2019. Accessed on August 15, 2020. https://www.internetandpsychiatry.com/wp/editorials/can-shrinks-shrink-the-electronic-health-record/
4. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
5. Mohanty D, Prabhu A, Lippmann S. Physician burnout: signs and solutions. J Fam Pract. 2019;68(8):442-446.
6. McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Arch Intern Med. 1991;151(11):2273-2277.
Physician burnout is a common and serious problem. In a 2017 survey of >14,000 US physicians across 27 specialties, 42% reported burnout,1 which typically is defined as a long-term stress reaction marked by emotional exhaustion, depersonalization, and a lack of sense of personal accomplishment.2
Creating a focused, yet comfortable professional life is essential for preventing burnout. For our patients’ sake and for our own personal fulfillment, there is much we can do to maintain a healthy professional and home life balance. This article describes the factors that contribute to physician burnout, and outlines steps you can take to improve your work/life balance.
The multifactorial roots of stress
Many physicians frequently blend their professional and personal lives. Most are absorbed in their practices, which leaves limited time for family interactions, daily life, or wellness.
Work hours are often long, and schedules are filled with obligations. In recent years, changes to medical practice have resulted in many additional responsibilities for physicians, such as administrative tasks and adapting to electronic health care, particularly to the use of electronic health records (EHRs). This has escalated workload and worries while diminishing patient interaction, creating more distant clinical relationships and providing less financial remuneration. Monetary pressures to see more patients limit the quality of care. Overload often forces physicians to stay at work late and/or labor excessive hours at home with less family interaction. The introduction of EHRs escalated this trend, while detracting from a healthy family, personal, and professional life. Addressing cumbersome documentation requirements while striving to maintain contact with patients is frustrating.3
Physician job dissatisfaction has worsened over time. Burnout escalates errors, diminishes patient rapport and safety, and produces suboptimal outcomes, all resulting in declining professional satisfaction.
Improving your work/life balance
The following strategies can help you make changes to better balance your professional and personal lives.
Assess priorities and goals. Before taking steps to achieve an optimal work-home balance, first review medical, spousal, and parental expectations. Social support is key.
Continue to: Identify stressors
Identify stressors. Use self-report questionnaires and collegial discussions to assess for the presence and/or severity of burnout. Prevention and/or intervention at personal and organizational levels can positively impact physician well-being.4
Focus on self-care. Prioritize your personal health care, sleep hygiene, exercise routines, quality of diet, and recreational activities. Do not self-prescribe medications, and avoid excessive alcohol use.5
Make changes to your practice. In your office, make efforts to maximize social connectiveness. Consider assigning routine tasks to other staff members. Upgrading your typing skills, employing medical records scribes, and/or using voice recording systems can reduce your workload.5
Advocate for better legislation. Both through professional medical organizations and at government levels, work to modify regulations that require physicians to spend their time on nonclinical tasks. This might include advocating to simplify EHRs and insurance company reimbursement requirements to decrease paperwork and reduce barriers to prescribing. Stress management seminars, which typically are offered at state and national conferences, can foster interpersonal and professional competencies throughout one’s medical career.6 Medical licensure boards should make efforts to reduce the stigma of reporting mental health issues; they should assure confidentiality protection and help for those who seek assistance.5
Physician burnout is a common and serious problem. In a 2017 survey of >14,000 US physicians across 27 specialties, 42% reported burnout,1 which typically is defined as a long-term stress reaction marked by emotional exhaustion, depersonalization, and a lack of sense of personal accomplishment.2
Creating a focused, yet comfortable professional life is essential for preventing burnout. For our patients’ sake and for our own personal fulfillment, there is much we can do to maintain a healthy professional and home life balance. This article describes the factors that contribute to physician burnout, and outlines steps you can take to improve your work/life balance.
The multifactorial roots of stress
Many physicians frequently blend their professional and personal lives. Most are absorbed in their practices, which leaves limited time for family interactions, daily life, or wellness.
Work hours are often long, and schedules are filled with obligations. In recent years, changes to medical practice have resulted in many additional responsibilities for physicians, such as administrative tasks and adapting to electronic health care, particularly to the use of electronic health records (EHRs). This has escalated workload and worries while diminishing patient interaction, creating more distant clinical relationships and providing less financial remuneration. Monetary pressures to see more patients limit the quality of care. Overload often forces physicians to stay at work late and/or labor excessive hours at home with less family interaction. The introduction of EHRs escalated this trend, while detracting from a healthy family, personal, and professional life. Addressing cumbersome documentation requirements while striving to maintain contact with patients is frustrating.3
Physician job dissatisfaction has worsened over time. Burnout escalates errors, diminishes patient rapport and safety, and produces suboptimal outcomes, all resulting in declining professional satisfaction.
Improving your work/life balance
The following strategies can help you make changes to better balance your professional and personal lives.
Assess priorities and goals. Before taking steps to achieve an optimal work-home balance, first review medical, spousal, and parental expectations. Social support is key.
Continue to: Identify stressors
Identify stressors. Use self-report questionnaires and collegial discussions to assess for the presence and/or severity of burnout. Prevention and/or intervention at personal and organizational levels can positively impact physician well-being.4
Focus on self-care. Prioritize your personal health care, sleep hygiene, exercise routines, quality of diet, and recreational activities. Do not self-prescribe medications, and avoid excessive alcohol use.5
Make changes to your practice. In your office, make efforts to maximize social connectiveness. Consider assigning routine tasks to other staff members. Upgrading your typing skills, employing medical records scribes, and/or using voice recording systems can reduce your workload.5
Advocate for better legislation. Both through professional medical organizations and at government levels, work to modify regulations that require physicians to spend their time on nonclinical tasks. This might include advocating to simplify EHRs and insurance company reimbursement requirements to decrease paperwork and reduce barriers to prescribing. Stress management seminars, which typically are offered at state and national conferences, can foster interpersonal and professional competencies throughout one’s medical career.6 Medical licensure boards should make efforts to reduce the stigma of reporting mental health issues; they should assure confidentiality protection and help for those who seek assistance.5
1. Peckham C. Medscape psychiatrist lifestyle report: race and ethnicity, bias and burnout. Medscape. Published January 11, 2017. Accessed July 12, 2021. http://www.medscape.com/features/slideshow/lifestyle/2017/psychiatry#page=1
2. Agency for Healthcare Research and Quality. Physician burnout. Published July 2017. Accessed July 13, 2021. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
3. Lippmann S. Can shrinks “shrink” the electronic health record? Internet and Psychiatry. December 19, 2019. Accessed on August 15, 2020. https://www.internetandpsychiatry.com/wp/editorials/can-shrinks-shrink-the-electronic-health-record/
4. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
5. Mohanty D, Prabhu A, Lippmann S. Physician burnout: signs and solutions. J Fam Pract. 2019;68(8):442-446.
6. McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Arch Intern Med. 1991;151(11):2273-2277.
1. Peckham C. Medscape psychiatrist lifestyle report: race and ethnicity, bias and burnout. Medscape. Published January 11, 2017. Accessed July 12, 2021. http://www.medscape.com/features/slideshow/lifestyle/2017/psychiatry#page=1
2. Agency for Healthcare Research and Quality. Physician burnout. Published July 2017. Accessed July 13, 2021. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
3. Lippmann S. Can shrinks “shrink” the electronic health record? Internet and Psychiatry. December 19, 2019. Accessed on August 15, 2020. https://www.internetandpsychiatry.com/wp/editorials/can-shrinks-shrink-the-electronic-health-record/
4. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
5. Mohanty D, Prabhu A, Lippmann S. Physician burnout: signs and solutions. J Fam Pract. 2019;68(8):442-446.
6. McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Arch Intern Med. 1991;151(11):2273-2277.
Let’s apply the lessons from the AIDS crisis to the COVID-19 pandemic
In 2020, COVID-19 disrupted our medical system, and life in general. In the 1980s, the AIDS epidemic devastated communities and overwhelmed hospitals. There were lessons learned from the AIDS epidemic that can be applied to the current situation.
Patients with HIV-spectrum illness faced stigmatization and societal indifference, including rejection by family members, increased rates of suicide, fears of sexual and/or intrauterine transmission, substance abuse issues, and alterations of body image for those with wasting syndromes and disfiguring Kaposi lesions. AIDS prevention strategies such as the provision of condoms and needle exchange programs were controversial, and many caregivers exposed to contaminated fluids had to endure months of antiretroviral treatment.
Similar to the AIDS epidemic, the COVID-19 pandemic has had significant psychological implications for patients and caregivers. Patients with COVID-19 infections also face feelings of guilt over potentially exposing a family member to the virus; devastating socioeconomic issues; restrictive hospital visitation policies for family members; disease news oversaturation; and feelings of hopelessness. People with AIDS in the 1980s faced the possibility of dying alone, and there was initial skepticism about medications to treat HIV—just as some individuals are now uneasy about recently introduced coronavirus vaccines.
The similarities of both diseases allow us some foresight on how to deal with current COVID-19 issues. Looking back on the AIDS epidemic should teach us to prioritize attending to the mental health of sufferers and caregivers, creating advocacy and support groups for when a patient’s family is unavailable, instilling public confidence in treatment options, maintaining staff morale, addressing substance abuse (due to COVID-related stress), and depoliticizing prevention strategies. Addressing these issues is especially critical for minority populations.
As respected medical care leaders, we can provide and draw extra attention to the needs of patients’ family members and health care personnel during this COVID-19 pandemic. Hopefully, the distribution of vaccines will shorten some of our communal and professional distress.
Robert Frierson, MD
Steven Lippmann, MD
Louisville, KY
In 2020, COVID-19 disrupted our medical system, and life in general. In the 1980s, the AIDS epidemic devastated communities and overwhelmed hospitals. There were lessons learned from the AIDS epidemic that can be applied to the current situation.
Patients with HIV-spectrum illness faced stigmatization and societal indifference, including rejection by family members, increased rates of suicide, fears of sexual and/or intrauterine transmission, substance abuse issues, and alterations of body image for those with wasting syndromes and disfiguring Kaposi lesions. AIDS prevention strategies such as the provision of condoms and needle exchange programs were controversial, and many caregivers exposed to contaminated fluids had to endure months of antiretroviral treatment.
Similar to the AIDS epidemic, the COVID-19 pandemic has had significant psychological implications for patients and caregivers. Patients with COVID-19 infections also face feelings of guilt over potentially exposing a family member to the virus; devastating socioeconomic issues; restrictive hospital visitation policies for family members; disease news oversaturation; and feelings of hopelessness. People with AIDS in the 1980s faced the possibility of dying alone, and there was initial skepticism about medications to treat HIV—just as some individuals are now uneasy about recently introduced coronavirus vaccines.
The similarities of both diseases allow us some foresight on how to deal with current COVID-19 issues. Looking back on the AIDS epidemic should teach us to prioritize attending to the mental health of sufferers and caregivers, creating advocacy and support groups for when a patient’s family is unavailable, instilling public confidence in treatment options, maintaining staff morale, addressing substance abuse (due to COVID-related stress), and depoliticizing prevention strategies. Addressing these issues is especially critical for minority populations.
As respected medical care leaders, we can provide and draw extra attention to the needs of patients’ family members and health care personnel during this COVID-19 pandemic. Hopefully, the distribution of vaccines will shorten some of our communal and professional distress.
Robert Frierson, MD
Steven Lippmann, MD
Louisville, KY
In 2020, COVID-19 disrupted our medical system, and life in general. In the 1980s, the AIDS epidemic devastated communities and overwhelmed hospitals. There were lessons learned from the AIDS epidemic that can be applied to the current situation.
Patients with HIV-spectrum illness faced stigmatization and societal indifference, including rejection by family members, increased rates of suicide, fears of sexual and/or intrauterine transmission, substance abuse issues, and alterations of body image for those with wasting syndromes and disfiguring Kaposi lesions. AIDS prevention strategies such as the provision of condoms and needle exchange programs were controversial, and many caregivers exposed to contaminated fluids had to endure months of antiretroviral treatment.
Similar to the AIDS epidemic, the COVID-19 pandemic has had significant psychological implications for patients and caregivers. Patients with COVID-19 infections also face feelings of guilt over potentially exposing a family member to the virus; devastating socioeconomic issues; restrictive hospital visitation policies for family members; disease news oversaturation; and feelings of hopelessness. People with AIDS in the 1980s faced the possibility of dying alone, and there was initial skepticism about medications to treat HIV—just as some individuals are now uneasy about recently introduced coronavirus vaccines.
The similarities of both diseases allow us some foresight on how to deal with current COVID-19 issues. Looking back on the AIDS epidemic should teach us to prioritize attending to the mental health of sufferers and caregivers, creating advocacy and support groups for when a patient’s family is unavailable, instilling public confidence in treatment options, maintaining staff morale, addressing substance abuse (due to COVID-related stress), and depoliticizing prevention strategies. Addressing these issues is especially critical for minority populations.
As respected medical care leaders, we can provide and draw extra attention to the needs of patients’ family members and health care personnel during this COVID-19 pandemic. Hopefully, the distribution of vaccines will shorten some of our communal and professional distress.
Robert Frierson, MD
Steven Lippmann, MD
Louisville, KY
Improving your experience with electronic health records
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
Plan now to address the COVID-19 mental health fallout
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
Lofexidine: An option for treating opioid withdrawal
Opioid use disorder (OUD) and deaths by opioid overdose are a major public health concern, especially with the advent of synthetic opioids such as fentanyl.1 Enrolling patients with OUD into substance abuse treatment programs can be a difficult hurdle to cross because patients do not want to experience withdrawal. The fear of withdrawal leads many individuals to refuse appropriate interventions. For these patients, consider the alpha-2 agonist lofexidine, which was FDA-approved in 2018 to help diminish the signs and symptoms of opioid withdrawal.1-3 Use of lofexidine might encourage more patients with OUD to accept substance abuse treatment.1,4,5
How to prescribe lofexidine
For decades, clinicians in Britain have prescribed lofexidine to attenuate opioid withdrawal.1An analog of clonidine, lofexidine is reportedly less likely than clonidine to induce hypotension.1,4 While this agent does not diminish drug toxicity, it can provide symptomatic relief for patients undergoing opioid withdrawal, and is efficacious as a supplement to and/or replacement for methadone, buprenorphine, clonidine, or other symptomatic pharmacotherapies.1,4,5
Lofexidine is available in 0.18-mg tablets. For patients experiencing overt symptoms of opioid withdrawal, initially prescribe 3 0.18-mg tablets, 4 times a day.3 The recommended maximum dosage is 2.88 mg/d, and each dose generally should not exceed 0.72 mg/d. Lofexidine may be continued for up to 14 days, with dosing guided by symptoms. Initiate a taper once the patient no longer experiences withdrawal symptoms.3
Adverse effects. Lofexidine’s efficacy and safety were evaluated in 3 randomized, double-blind, placebo-controlled trials that included 935 participants dependent on short-acting opioids who were experiencing abrupt opioid withdrawal and received lofexidine, 2.16 or 2.88 mg/d, or placebo.3 The most common adverse effects of lofexidine were insomnia, orthostatic hypotension, bradycardia, hypotension, dizziness, somnolence, sedation, and dry mouth.3 In the 3 trials, these effects were reported by ≥10% of patients receiving lofexidine, and occurred more frequently compared with placebo (Table3).
Take precautions when prescribing lofexidine because it can cause QT prolongation and CNS depression, especially when co-administered with sedative agents.3 It also can result in rebound hypertension once discontinued. This may be minimized by gradually reducing the dosage.3
A pathway to OUD treatment
Lofexidine can help relieve symptoms of opioid withdrawal, such as stomach cramps, muscle spasms or twitching, feeling cold, muscular tension, and aches and pains.1-5 This new option might help clinicians encourage more patients with OUD to fully engage in substance abuse treatment.
1. Rehman SU, Maqsood MH, Bajwa H, et al. Clinical efficacy and safety profile of lofexidine hydrochloride in treating opioid withdrawal symptoms: a review of literature. Cureus. 2019;11(6):e4827. doi: 10.7759/cureus.4827.
2. FDA approves the first non-opioid treatment for management of opioid withdrawal symptoms in adults. US Food & Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm607884.htm. Published May 16, 2018. Accessed December 13, 2019.
3. Lucemyra [package insert]. Louisville, KY: US WorldMeds, LLC; 2018.
4. Carnwath T, Hardman J. Randomized double-blind comparison of lofexidine and clonidine in the out-patient treatment of opiate withdrawal. Drug Alcohol Depend. 1998;50(3):251-254.
5. Gonzalez G, Oliveto A, Kosten TR. Combating opiate dependence: a comparison among the available pharmacological options. Exp Opin Pharmacother. 2004;5(4):713-725.
Opioid use disorder (OUD) and deaths by opioid overdose are a major public health concern, especially with the advent of synthetic opioids such as fentanyl.1 Enrolling patients with OUD into substance abuse treatment programs can be a difficult hurdle to cross because patients do not want to experience withdrawal. The fear of withdrawal leads many individuals to refuse appropriate interventions. For these patients, consider the alpha-2 agonist lofexidine, which was FDA-approved in 2018 to help diminish the signs and symptoms of opioid withdrawal.1-3 Use of lofexidine might encourage more patients with OUD to accept substance abuse treatment.1,4,5
How to prescribe lofexidine
For decades, clinicians in Britain have prescribed lofexidine to attenuate opioid withdrawal.1An analog of clonidine, lofexidine is reportedly less likely than clonidine to induce hypotension.1,4 While this agent does not diminish drug toxicity, it can provide symptomatic relief for patients undergoing opioid withdrawal, and is efficacious as a supplement to and/or replacement for methadone, buprenorphine, clonidine, or other symptomatic pharmacotherapies.1,4,5
Lofexidine is available in 0.18-mg tablets. For patients experiencing overt symptoms of opioid withdrawal, initially prescribe 3 0.18-mg tablets, 4 times a day.3 The recommended maximum dosage is 2.88 mg/d, and each dose generally should not exceed 0.72 mg/d. Lofexidine may be continued for up to 14 days, with dosing guided by symptoms. Initiate a taper once the patient no longer experiences withdrawal symptoms.3
Adverse effects. Lofexidine’s efficacy and safety were evaluated in 3 randomized, double-blind, placebo-controlled trials that included 935 participants dependent on short-acting opioids who were experiencing abrupt opioid withdrawal and received lofexidine, 2.16 or 2.88 mg/d, or placebo.3 The most common adverse effects of lofexidine were insomnia, orthostatic hypotension, bradycardia, hypotension, dizziness, somnolence, sedation, and dry mouth.3 In the 3 trials, these effects were reported by ≥10% of patients receiving lofexidine, and occurred more frequently compared with placebo (Table3).
Take precautions when prescribing lofexidine because it can cause QT prolongation and CNS depression, especially when co-administered with sedative agents.3 It also can result in rebound hypertension once discontinued. This may be minimized by gradually reducing the dosage.3
A pathway to OUD treatment
Lofexidine can help relieve symptoms of opioid withdrawal, such as stomach cramps, muscle spasms or twitching, feeling cold, muscular tension, and aches and pains.1-5 This new option might help clinicians encourage more patients with OUD to fully engage in substance abuse treatment.
Opioid use disorder (OUD) and deaths by opioid overdose are a major public health concern, especially with the advent of synthetic opioids such as fentanyl.1 Enrolling patients with OUD into substance abuse treatment programs can be a difficult hurdle to cross because patients do not want to experience withdrawal. The fear of withdrawal leads many individuals to refuse appropriate interventions. For these patients, consider the alpha-2 agonist lofexidine, which was FDA-approved in 2018 to help diminish the signs and symptoms of opioid withdrawal.1-3 Use of lofexidine might encourage more patients with OUD to accept substance abuse treatment.1,4,5
How to prescribe lofexidine
For decades, clinicians in Britain have prescribed lofexidine to attenuate opioid withdrawal.1An analog of clonidine, lofexidine is reportedly less likely than clonidine to induce hypotension.1,4 While this agent does not diminish drug toxicity, it can provide symptomatic relief for patients undergoing opioid withdrawal, and is efficacious as a supplement to and/or replacement for methadone, buprenorphine, clonidine, or other symptomatic pharmacotherapies.1,4,5
Lofexidine is available in 0.18-mg tablets. For patients experiencing overt symptoms of opioid withdrawal, initially prescribe 3 0.18-mg tablets, 4 times a day.3 The recommended maximum dosage is 2.88 mg/d, and each dose generally should not exceed 0.72 mg/d. Lofexidine may be continued for up to 14 days, with dosing guided by symptoms. Initiate a taper once the patient no longer experiences withdrawal symptoms.3
Adverse effects. Lofexidine’s efficacy and safety were evaluated in 3 randomized, double-blind, placebo-controlled trials that included 935 participants dependent on short-acting opioids who were experiencing abrupt opioid withdrawal and received lofexidine, 2.16 or 2.88 mg/d, or placebo.3 The most common adverse effects of lofexidine were insomnia, orthostatic hypotension, bradycardia, hypotension, dizziness, somnolence, sedation, and dry mouth.3 In the 3 trials, these effects were reported by ≥10% of patients receiving lofexidine, and occurred more frequently compared with placebo (Table3).
Take precautions when prescribing lofexidine because it can cause QT prolongation and CNS depression, especially when co-administered with sedative agents.3 It also can result in rebound hypertension once discontinued. This may be minimized by gradually reducing the dosage.3
A pathway to OUD treatment
Lofexidine can help relieve symptoms of opioid withdrawal, such as stomach cramps, muscle spasms or twitching, feeling cold, muscular tension, and aches and pains.1-5 This new option might help clinicians encourage more patients with OUD to fully engage in substance abuse treatment.
1. Rehman SU, Maqsood MH, Bajwa H, et al. Clinical efficacy and safety profile of lofexidine hydrochloride in treating opioid withdrawal symptoms: a review of literature. Cureus. 2019;11(6):e4827. doi: 10.7759/cureus.4827.
2. FDA approves the first non-opioid treatment for management of opioid withdrawal symptoms in adults. US Food & Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm607884.htm. Published May 16, 2018. Accessed December 13, 2019.
3. Lucemyra [package insert]. Louisville, KY: US WorldMeds, LLC; 2018.
4. Carnwath T, Hardman J. Randomized double-blind comparison of lofexidine and clonidine in the out-patient treatment of opiate withdrawal. Drug Alcohol Depend. 1998;50(3):251-254.
5. Gonzalez G, Oliveto A, Kosten TR. Combating opiate dependence: a comparison among the available pharmacological options. Exp Opin Pharmacother. 2004;5(4):713-725.
1. Rehman SU, Maqsood MH, Bajwa H, et al. Clinical efficacy and safety profile of lofexidine hydrochloride in treating opioid withdrawal symptoms: a review of literature. Cureus. 2019;11(6):e4827. doi: 10.7759/cureus.4827.
2. FDA approves the first non-opioid treatment for management of opioid withdrawal symptoms in adults. US Food & Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm607884.htm. Published May 16, 2018. Accessed December 13, 2019.
3. Lucemyra [package insert]. Louisville, KY: US WorldMeds, LLC; 2018.
4. Carnwath T, Hardman J. Randomized double-blind comparison of lofexidine and clonidine in the out-patient treatment of opiate withdrawal. Drug Alcohol Depend. 1998;50(3):251-254.
5. Gonzalez G, Oliveto A, Kosten TR. Combating opiate dependence: a comparison among the available pharmacological options. Exp Opin Pharmacother. 2004;5(4):713-725.
Physician burnout: Signs and solutions
CASE
Dr. Peter D is a mid-career family physician in a group practice that recently adopted an electronic health record system. Although he realizes he is now competent at computerized medicine, he has far less of the one-on-one patient contact that he once found so gratifying about the field of medicine.
Others in the practice have similar concerns, but they suggest that everyone ought to “go along to get along.” To manage the increasing demands of his case load and the required documentation, Dr. D has begun staying late to finish charting, which is negatively impacting his family life.
Dr. D finds himself burdened by record keeping that is increasingly complicated and insurance company demands that are onerous. Pharmaceutical prior authorizations that previously had been mildly bothersome are now a full-on burden. More often than not, he finds himself becoming irritable over extra requests and administrative demands, impatient with some patients and staff, and extremely fatigued at the end of workdays. Simply put, he finds that practicing medicine is far less enjoyable than it once was. He takes the Maslach Burnout Inventory, and his score indicates that he has moderate burnout.
Physician burnout has been a growing concern in recent decades.1 Characterized by varying degrees of job dissatisfaction, cynicism, emotional exhaustion, clinical inefficiency, and depression, physician burnout can impede effective patient care, cause significant health issues among physicians, diminish professional gratification and feelings of accomplishment, and financially burden society as a whole. Here we present the information you need to recognize burnout in yourself and colleagues and address the problem on personal, organizational, and legislative levels.
A problem that affects physicians of all ages
Physician burnout has been recognized to present anywhere on a spectrum, manifesting as ineffectiveness, overextension, disengagement, and/or an inability to practice.2 Such features may lead to feelings of professional inadequacy among even the highest functioning physicians.
Burnout occurs in all stages of medical life—as students, residents, and practicing physicians.3-6 Due to pressures in excess of coping capacity, some physicians will suffer from alcohol or other drug abuse, depression, and/or suicidal thinking.7 Stress and burnout can also result in musculoskeletal disorders, immune system dysfunction, cardiac pathology, and a shorter lifespan.8
Not only do individual practitioners suffer consequences from burnout, but it also compromises health care delivery. In 2018, the Medscape National Physician Burnout and Depression Report surveyed 15,000 physicians from 29 specialties; 33% of the respondents said that they were more easily frustrated by patients, and 32% reported less personal engagement.9 Burnout adversely impacts care, patient satisfaction, productivity, physician retention, retirement, and income, as well.6 Safety during clinical practice deteriorates because of an increase in medical error rates.10 Resultant emotional distress for physicians creates a vicious cycle.10
[polldaddy:10427848]
Continue to: These issues negatively impact...
These issues negatively impact practice enthusiasm and may engender self-doubt.11 They may lead to absenteeism or, worse, to abandoning the profession, further contributing to physician shortages.12 The financial impact of physician burnout in lost revenue in 2018 was about $17 billion, according to the National Taskforce for Humanity in Medicine.13
How prevalent is physician burnout?
Between October 2012 and March 2013, the American Society of Clinical Oncology surveyed US oncologists and found that 45% had evidence of burnout.14 In another survey of US physicians from all specialties conducted in 2011, at least 1 symptom of burnout was documented in nearly 46% of respondents.15 By 2014, this percentage increased to 54%.16
In 2018, the Medscape National Physician Burnout and Depression Report indicated that 42% of physicians admitted to some burnout, while 12% said they were unhappy at work, and 3% reported being clinically depressed.9 About 48% of female practitioners reported burnout vs 38% of male peers.9 Work-related distress varies between specialties, with internists, family physicians, intensivists, neurologists, and gynecologists more affected than those from other specialties.9
Causes and contributing factors
Job stress generally increases with changes in the workplace. This can be heightened in the health care workplace, which demands perfection and leaves little room for emotional issues. Loss of autonomy, time constraints associated with clinical care, electronic health record (EHR) documentation, and disorganized workflow tend to contribute to provider dissatisfaction and stress, as do ethical disagreements about patient care between physicians and leadership.10,17 Fear of reprisal for speaking up about such issues can further exacerbate the problem. Some older physicians may have difficulty with technology and computerized record keeping. Reduced patient contact due to increasing reliance on computers can diminish physicians’ job satisfaction. And managing recurrent or difficult-to-treat ailments can result in compassion fatigue, diminished empathy, and emotional disengagement.
Burnout in the health care workplace is inconsistently addressed, despite negative professional and personal ramifications. The reasons include denial, uncertainty about monetary implications, and lack of corrective programs by decision-making organizations and/or employers.6 American medicine has lacked the political and financial will to implement strategies to mitigate burnout. Improvement requires changes on the part of government, physician groups, and the population at large.
The answer?
A multipronged approach
Identifying burnout is the first step in management. The 22-item Maslach Burnout Inventory (MBI) is a self-reporting questionnaire, reliable at detecting and assessing burnout severity.18 It screens 3 main domains: emotional exhaustion, depersonalization, and diminished feelings of accomplishment. The American Medical Association recommends the 10-item Zero Burnout Program—the “Mini Z Survey”—as being quicker and more convenient.19
Once the problem is recognized, experts suggest adopting a multipronged approach to prevention and intervention by using personal, organizational, and legislative strategies.20
Continue to: On a personal level...
On a personal level, it’s important to identify stressors and employ stress-reduction and coping skills, such as mindfulness and/or reflection.21 Mindfulness programs may help to minimize exhaustion, increase compassion, and improve understanding of other people’s feelings.22 Such programs are widely available and may be accessed through the Internet, mental health centers, or by contacting psychiatric or psychological services.
Other self-care methods include ensuring adequate sleep, nutrition, exercise, and enjoyable activities. If a physician who is suffering from burnout is taking any prescription or over-the-counter drugs or supplements, it is important to be self-aware of the potential for misuse of medications. Of course, one should never self-prescribe controlled drugs, such as opiates and sedatives. Consumption of alcohol must be well-controlled, without excesses, and drinking near bedtime is ill-advised. The use of illegal substances should be avoided.
Pursuing aspects of health care that are meaningful and that increase patient contact time can boost enthusiasm, as can focusing on the positives aspects of one’s career.23 Continuing medical education can enhance self-esteem and promote a sense of purpose.24
Peer support. Practice partners may assist their colleagues by alerting them to signs of burnout, offering timely intervention suggestions, and monitoring the effectiveness of strategies. Physicians should discuss stress and burnout with their peers; camaraderie within a practice group is helpful.
Professional coaches or counselors may be engaged to mitigate workplace distress. Coaching is best instituted collegially with pre-identified goals in order to minimize stigmatization.
Continue to: Professional societies and medical boards
Professional societies and medical boards. Reporting requirements by medical boards tend to stigmatize those seeking professional assistance. But that could change if all of us—through our participation in these organizations—pursue change.
Specifically, organizations and related societies could assist with better guidance and policy adjustment (see “Resources”). State medical boards could, for example, increase education of, and outreach to, physicians about mental health issues, while maintaining confidentiality.25 Medical organizations could regularly survey their membership to identify burnout early and identify personal, social, and institutional shortcomings that contribute to physician burnout. In addition, hospital quality improvement committees that monitor health care delivery appropriateness could take steps toward change as well.
SIDEBAR
Resources to help combat burnout
- National Academy of Medicine Action Collaborative on Clinician Well- Being and Resilience: https://nam.edu/initiatives/clinician-resilience-and-well-being/
- The Schwartz Center for Compassionate Healthcare: http://www.theschwartzcenter.org
- NEJM Catalyst: http://catalyst.nejm.org/posts?q=burnout
- The American Medical Association, Joy in Medicine: https://www.ama-assn.org/search?search=joy+in+medicine
- Agency for Healthcare Research and Quality: https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
- Accreditation Council for Graduate Medical Education Tools and Resources for Resident and Faculty Member Well-Being: https://www.acgme.org/What-We-Do/Initiatives/Physician-Well-Being/Resources
The American Medical Association (AMA) just recently announced that they are launching a new effort to fight the causes of physician burnout. The AMA’s Practice Transformation Inititative26 seeks to fill the knowledge gaps regarding effective interventions to reduce burnout. AMA’s leadership indicates that the initiative will focus on “improving joy in medicine by using validated assessment tools to measure burnout; field-testing interventions that are designed to improve workflows, applying practice science research methodology to evaluate impact, and sharing best practices within an AMA-facilitated learning community.”26
Stanford’s example. Stanford University instituted a ‘time bank’ program, to help their academic medical faculty balance work and life and reduce stress. They essentially offer services, such as home food delivery and house cleaning, in return for hours spent in the clinic.27
Reorganizing and reprioritizing. Prioritizing physician wellness as a quality indicator and instituting a committee to advocate for wellness can help attenuate burnout.28,29 Specific measures include minimizing rushed, overloaded scheduling and allowing more clinical contact time with patients. Using nursing and office staff to streamline workflow is also helpful.29 The University of Colorado’s “Ambulatory Process Excellence Model” strives to assist doctors by increasing the medical assistant-to-clinician ratio, yielding better productivity.23 Medical assistants are increasingly handling tasks such as data entry, medication reconciliation, and preventive care, to allow physicians more time to focus on medical decision-making.23
Continue to: The role of the EHR
The role of the EHR. One important way to boost professional morale is to simplify and shorten the EHR. The complexity of and reduced patient contact caused by today’s record-keeping systems is the source of great frustration among many physicians. In addition, many patients dislike the disproportionate attention paid by physicians to the computer during office visits, further compromising physician-patient relationships. Improving documentation methodology and/or employing medical assistant scribes can be helpful.30,31 (See “Advanced team-based care: How we made it work” at http://bit.ly/2lNaB5Q.)
Legislation with physician input can mandate policies for more appropriate work environments. A good way to initiate improvement and reform strategies is to contact local medical societies and political representatives. Federal and state collaboration to reduce physician shortages in selected specialties or geographic regions can improve work-related stress. This might be attained by expanding residency programs, using telemedicine in underserved regions, and employing more physician assistants.32
Health insurance. Enhancing universal access to affordable medical care, including pharmaceutical coverage, would alleviate stress for physicians and patients alike.33 Health insurance regulation to decrease paperwork and simplify coverage would decrease physician workload. Standardized policy requirements, fewer exclusionary rules, and simplified prescribing guidelines (including having less cumbersome prescription pre-authorizations and greater standardization of drug formularies by different payer sources or insurance plans) would facilitate better clinical management.
CASE
Dr. D begins by discussing his concerns with his colleagues in the group practice and finds he is not alone. Many of the concerns of the group center around brief, rushed appointments that diminish relationships with patients, a lack of autonomy, and the fear of medical malpractice. Several older physicians acknowledge that they just want to retire.
To address the patient contact and documentation issues, the group decides to hire scribes. They also decide to bring their concerns to the next county medical society meeting. The end result: They petitioned their state medical association to host presentations about mitigating burnout, to hold roundtable discussions, and to establish panels focused on remedying the situation.
Continue to: With this accomplished...
With this accomplished, Dr. D’s anxieties lessened. He surveyed relevant literature and shared tips for improving professional time management with his partners. In a hopeful mood, he volunteered to address burnout prevention at the next statewide medical meeting. He felt it was a good start.
CORRESPONDENCE
Steven Lippmann, MD, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
1. Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263-1269.
2. Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burnout Research. 2016;3:89-100.
3. Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Int Med. 2008;149:334-341.
4. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
5. Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463-471.
6. Shanafelt TD, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
7. Cottler LB, Ajinkya S, Merlo LJ, et al. Lifetime psychiatric and substance use disorders among impaired physicians in a physicians health program. J Addict Med. 2013;7:108-112.
8. Consiglio C. Interpersonal strain at work: a new burnout facet relevant for the health of hospital staff. Burnout Res. 2014;1:69-75.
9. Peckham C. Medscape National Physician Burnout and Depression Report 2018. January 12, 2018. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235. Accessed October 4, 2019.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527-533.
12. Suñer-Soler R, Grau-Martin A, Flichtentrei D, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burnout Research. 2014;1:82-89.
13. National Taskforce for Humanity in Healthcare. Position paper: The business case for humanity in healthcare. April 2018. https://www.vocera.com/public/pdf/NTHBusinessCase_final003.pdf. Accessed October 4, 2019.
14. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678-686.
15. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Int Med. 2012;172:1377-1385.
16. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90;1600-1613.
17. Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151:28-36.
18. Maslach C, Jackson SE. The measurement of experienced burnout. J Occcup Behav. 1981;2:99-113.
19. Linzer M, Guzman-Corrales L, Poplau S. Physician Burnout: improve physician satisfaction and patient outcomes. June 5, 2015. https://www.stepsforward.org/modules/physician-burnout. Accessed October 4, 2019.
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272-2281.
21. Nedrow A, Steckler NA, Hardman J. Physician resilience and burnout: can you make the switch? Fam Prac Manag. 2013;20:25-30.
22. Verweij H, van Ravesteijn H, van Hooff MLM, et al. Mindfulness-based stress reduction for residents: a randomized controlled trial. J Gen Intern Med. 2018;33:429-436.
23. Wright AA, Katz IT. Beyond burnout – redesigning care to restore meaning and sanity for physicians. N Eng J Med. 2018;378:309-311.
24. Shanafelt TD, Gorringe G, Menaker R, et. al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432-440.
25. Hengerer A, Kishore S. 2017. Breaking a culture of silence: the role of state medical boards. National Academy of Medicine, Washington DC. https://nam.edu/breaking-a-culture-of-silence-the-role-of-state-medical-boards/. Accessed October 4, 2019.
26. American Medical Association. AMA fights burnout with new practice transformation initiative. September 5, 2019. https://www.ama-assn.org/press-center/press-releases/ama-fights-burnout-new-practice-transformation-initiative. Accessed September 5, 2019.
27. Schulte B. Time in the bank: a Stanford plan to save doctors from burnout. The Washington Post. https://www.washingtonpost.com/news/inspired-life/wp/2015/08/20/the-innovative-stanford-program-thats-saving-emergency-room-doctors-from-burnout/?utm_term=.838c930e8de7. Accessed October 4, 2019.
28. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721.
29. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
30. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Info Assoc. 2014;21:E100-E106.
31. Bodenheimer T, Willard-Grace R, Ghorob A. Expanding the roles of medical assistants: who does what in primary care? JAMA Intern Med. 2014;174:1025-1026.
32. Mangiofico G. Physician shortage requires multi-prong solution. January 26, 2018. Am J Manag Care. https://www.ajmc.com/contributor/dr-gary-mangiofico/2018/01/physician-shortage-requires-multiprong-solution. Accessed October 4, 2019.
33. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
CASE
Dr. Peter D is a mid-career family physician in a group practice that recently adopted an electronic health record system. Although he realizes he is now competent at computerized medicine, he has far less of the one-on-one patient contact that he once found so gratifying about the field of medicine.
Others in the practice have similar concerns, but they suggest that everyone ought to “go along to get along.” To manage the increasing demands of his case load and the required documentation, Dr. D has begun staying late to finish charting, which is negatively impacting his family life.
Dr. D finds himself burdened by record keeping that is increasingly complicated and insurance company demands that are onerous. Pharmaceutical prior authorizations that previously had been mildly bothersome are now a full-on burden. More often than not, he finds himself becoming irritable over extra requests and administrative demands, impatient with some patients and staff, and extremely fatigued at the end of workdays. Simply put, he finds that practicing medicine is far less enjoyable than it once was. He takes the Maslach Burnout Inventory, and his score indicates that he has moderate burnout.
Physician burnout has been a growing concern in recent decades.1 Characterized by varying degrees of job dissatisfaction, cynicism, emotional exhaustion, clinical inefficiency, and depression, physician burnout can impede effective patient care, cause significant health issues among physicians, diminish professional gratification and feelings of accomplishment, and financially burden society as a whole. Here we present the information you need to recognize burnout in yourself and colleagues and address the problem on personal, organizational, and legislative levels.
A problem that affects physicians of all ages
Physician burnout has been recognized to present anywhere on a spectrum, manifesting as ineffectiveness, overextension, disengagement, and/or an inability to practice.2 Such features may lead to feelings of professional inadequacy among even the highest functioning physicians.
Burnout occurs in all stages of medical life—as students, residents, and practicing physicians.3-6 Due to pressures in excess of coping capacity, some physicians will suffer from alcohol or other drug abuse, depression, and/or suicidal thinking.7 Stress and burnout can also result in musculoskeletal disorders, immune system dysfunction, cardiac pathology, and a shorter lifespan.8
Not only do individual practitioners suffer consequences from burnout, but it also compromises health care delivery. In 2018, the Medscape National Physician Burnout and Depression Report surveyed 15,000 physicians from 29 specialties; 33% of the respondents said that they were more easily frustrated by patients, and 32% reported less personal engagement.9 Burnout adversely impacts care, patient satisfaction, productivity, physician retention, retirement, and income, as well.6 Safety during clinical practice deteriorates because of an increase in medical error rates.10 Resultant emotional distress for physicians creates a vicious cycle.10
[polldaddy:10427848]
Continue to: These issues negatively impact...
These issues negatively impact practice enthusiasm and may engender self-doubt.11 They may lead to absenteeism or, worse, to abandoning the profession, further contributing to physician shortages.12 The financial impact of physician burnout in lost revenue in 2018 was about $17 billion, according to the National Taskforce for Humanity in Medicine.13
How prevalent is physician burnout?
Between October 2012 and March 2013, the American Society of Clinical Oncology surveyed US oncologists and found that 45% had evidence of burnout.14 In another survey of US physicians from all specialties conducted in 2011, at least 1 symptom of burnout was documented in nearly 46% of respondents.15 By 2014, this percentage increased to 54%.16
In 2018, the Medscape National Physician Burnout and Depression Report indicated that 42% of physicians admitted to some burnout, while 12% said they were unhappy at work, and 3% reported being clinically depressed.9 About 48% of female practitioners reported burnout vs 38% of male peers.9 Work-related distress varies between specialties, with internists, family physicians, intensivists, neurologists, and gynecologists more affected than those from other specialties.9
Causes and contributing factors
Job stress generally increases with changes in the workplace. This can be heightened in the health care workplace, which demands perfection and leaves little room for emotional issues. Loss of autonomy, time constraints associated with clinical care, electronic health record (EHR) documentation, and disorganized workflow tend to contribute to provider dissatisfaction and stress, as do ethical disagreements about patient care between physicians and leadership.10,17 Fear of reprisal for speaking up about such issues can further exacerbate the problem. Some older physicians may have difficulty with technology and computerized record keeping. Reduced patient contact due to increasing reliance on computers can diminish physicians’ job satisfaction. And managing recurrent or difficult-to-treat ailments can result in compassion fatigue, diminished empathy, and emotional disengagement.
Burnout in the health care workplace is inconsistently addressed, despite negative professional and personal ramifications. The reasons include denial, uncertainty about monetary implications, and lack of corrective programs by decision-making organizations and/or employers.6 American medicine has lacked the political and financial will to implement strategies to mitigate burnout. Improvement requires changes on the part of government, physician groups, and the population at large.
The answer?
A multipronged approach
Identifying burnout is the first step in management. The 22-item Maslach Burnout Inventory (MBI) is a self-reporting questionnaire, reliable at detecting and assessing burnout severity.18 It screens 3 main domains: emotional exhaustion, depersonalization, and diminished feelings of accomplishment. The American Medical Association recommends the 10-item Zero Burnout Program—the “Mini Z Survey”—as being quicker and more convenient.19
Once the problem is recognized, experts suggest adopting a multipronged approach to prevention and intervention by using personal, organizational, and legislative strategies.20
Continue to: On a personal level...
On a personal level, it’s important to identify stressors and employ stress-reduction and coping skills, such as mindfulness and/or reflection.21 Mindfulness programs may help to minimize exhaustion, increase compassion, and improve understanding of other people’s feelings.22 Such programs are widely available and may be accessed through the Internet, mental health centers, or by contacting psychiatric or psychological services.
Other self-care methods include ensuring adequate sleep, nutrition, exercise, and enjoyable activities. If a physician who is suffering from burnout is taking any prescription or over-the-counter drugs or supplements, it is important to be self-aware of the potential for misuse of medications. Of course, one should never self-prescribe controlled drugs, such as opiates and sedatives. Consumption of alcohol must be well-controlled, without excesses, and drinking near bedtime is ill-advised. The use of illegal substances should be avoided.
Pursuing aspects of health care that are meaningful and that increase patient contact time can boost enthusiasm, as can focusing on the positives aspects of one’s career.23 Continuing medical education can enhance self-esteem and promote a sense of purpose.24
Peer support. Practice partners may assist their colleagues by alerting them to signs of burnout, offering timely intervention suggestions, and monitoring the effectiveness of strategies. Physicians should discuss stress and burnout with their peers; camaraderie within a practice group is helpful.
Professional coaches or counselors may be engaged to mitigate workplace distress. Coaching is best instituted collegially with pre-identified goals in order to minimize stigmatization.
Continue to: Professional societies and medical boards
Professional societies and medical boards. Reporting requirements by medical boards tend to stigmatize those seeking professional assistance. But that could change if all of us—through our participation in these organizations—pursue change.
Specifically, organizations and related societies could assist with better guidance and policy adjustment (see “Resources”). State medical boards could, for example, increase education of, and outreach to, physicians about mental health issues, while maintaining confidentiality.25 Medical organizations could regularly survey their membership to identify burnout early and identify personal, social, and institutional shortcomings that contribute to physician burnout. In addition, hospital quality improvement committees that monitor health care delivery appropriateness could take steps toward change as well.
SIDEBAR
Resources to help combat burnout
- National Academy of Medicine Action Collaborative on Clinician Well- Being and Resilience: https://nam.edu/initiatives/clinician-resilience-and-well-being/
- The Schwartz Center for Compassionate Healthcare: http://www.theschwartzcenter.org
- NEJM Catalyst: http://catalyst.nejm.org/posts?q=burnout
- The American Medical Association, Joy in Medicine: https://www.ama-assn.org/search?search=joy+in+medicine
- Agency for Healthcare Research and Quality: https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
- Accreditation Council for Graduate Medical Education Tools and Resources for Resident and Faculty Member Well-Being: https://www.acgme.org/What-We-Do/Initiatives/Physician-Well-Being/Resources
The American Medical Association (AMA) just recently announced that they are launching a new effort to fight the causes of physician burnout. The AMA’s Practice Transformation Inititative26 seeks to fill the knowledge gaps regarding effective interventions to reduce burnout. AMA’s leadership indicates that the initiative will focus on “improving joy in medicine by using validated assessment tools to measure burnout; field-testing interventions that are designed to improve workflows, applying practice science research methodology to evaluate impact, and sharing best practices within an AMA-facilitated learning community.”26
Stanford’s example. Stanford University instituted a ‘time bank’ program, to help their academic medical faculty balance work and life and reduce stress. They essentially offer services, such as home food delivery and house cleaning, in return for hours spent in the clinic.27
Reorganizing and reprioritizing. Prioritizing physician wellness as a quality indicator and instituting a committee to advocate for wellness can help attenuate burnout.28,29 Specific measures include minimizing rushed, overloaded scheduling and allowing more clinical contact time with patients. Using nursing and office staff to streamline workflow is also helpful.29 The University of Colorado’s “Ambulatory Process Excellence Model” strives to assist doctors by increasing the medical assistant-to-clinician ratio, yielding better productivity.23 Medical assistants are increasingly handling tasks such as data entry, medication reconciliation, and preventive care, to allow physicians more time to focus on medical decision-making.23
Continue to: The role of the EHR
The role of the EHR. One important way to boost professional morale is to simplify and shorten the EHR. The complexity of and reduced patient contact caused by today’s record-keeping systems is the source of great frustration among many physicians. In addition, many patients dislike the disproportionate attention paid by physicians to the computer during office visits, further compromising physician-patient relationships. Improving documentation methodology and/or employing medical assistant scribes can be helpful.30,31 (See “Advanced team-based care: How we made it work” at http://bit.ly/2lNaB5Q.)
Legislation with physician input can mandate policies for more appropriate work environments. A good way to initiate improvement and reform strategies is to contact local medical societies and political representatives. Federal and state collaboration to reduce physician shortages in selected specialties or geographic regions can improve work-related stress. This might be attained by expanding residency programs, using telemedicine in underserved regions, and employing more physician assistants.32
Health insurance. Enhancing universal access to affordable medical care, including pharmaceutical coverage, would alleviate stress for physicians and patients alike.33 Health insurance regulation to decrease paperwork and simplify coverage would decrease physician workload. Standardized policy requirements, fewer exclusionary rules, and simplified prescribing guidelines (including having less cumbersome prescription pre-authorizations and greater standardization of drug formularies by different payer sources or insurance plans) would facilitate better clinical management.
CASE
Dr. D begins by discussing his concerns with his colleagues in the group practice and finds he is not alone. Many of the concerns of the group center around brief, rushed appointments that diminish relationships with patients, a lack of autonomy, and the fear of medical malpractice. Several older physicians acknowledge that they just want to retire.
To address the patient contact and documentation issues, the group decides to hire scribes. They also decide to bring their concerns to the next county medical society meeting. The end result: They petitioned their state medical association to host presentations about mitigating burnout, to hold roundtable discussions, and to establish panels focused on remedying the situation.
Continue to: With this accomplished...
With this accomplished, Dr. D’s anxieties lessened. He surveyed relevant literature and shared tips for improving professional time management with his partners. In a hopeful mood, he volunteered to address burnout prevention at the next statewide medical meeting. He felt it was a good start.
CORRESPONDENCE
Steven Lippmann, MD, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
CASE
Dr. Peter D is a mid-career family physician in a group practice that recently adopted an electronic health record system. Although he realizes he is now competent at computerized medicine, he has far less of the one-on-one patient contact that he once found so gratifying about the field of medicine.
Others in the practice have similar concerns, but they suggest that everyone ought to “go along to get along.” To manage the increasing demands of his case load and the required documentation, Dr. D has begun staying late to finish charting, which is negatively impacting his family life.
Dr. D finds himself burdened by record keeping that is increasingly complicated and insurance company demands that are onerous. Pharmaceutical prior authorizations that previously had been mildly bothersome are now a full-on burden. More often than not, he finds himself becoming irritable over extra requests and administrative demands, impatient with some patients and staff, and extremely fatigued at the end of workdays. Simply put, he finds that practicing medicine is far less enjoyable than it once was. He takes the Maslach Burnout Inventory, and his score indicates that he has moderate burnout.
Physician burnout has been a growing concern in recent decades.1 Characterized by varying degrees of job dissatisfaction, cynicism, emotional exhaustion, clinical inefficiency, and depression, physician burnout can impede effective patient care, cause significant health issues among physicians, diminish professional gratification and feelings of accomplishment, and financially burden society as a whole. Here we present the information you need to recognize burnout in yourself and colleagues and address the problem on personal, organizational, and legislative levels.
A problem that affects physicians of all ages
Physician burnout has been recognized to present anywhere on a spectrum, manifesting as ineffectiveness, overextension, disengagement, and/or an inability to practice.2 Such features may lead to feelings of professional inadequacy among even the highest functioning physicians.
Burnout occurs in all stages of medical life—as students, residents, and practicing physicians.3-6 Due to pressures in excess of coping capacity, some physicians will suffer from alcohol or other drug abuse, depression, and/or suicidal thinking.7 Stress and burnout can also result in musculoskeletal disorders, immune system dysfunction, cardiac pathology, and a shorter lifespan.8
Not only do individual practitioners suffer consequences from burnout, but it also compromises health care delivery. In 2018, the Medscape National Physician Burnout and Depression Report surveyed 15,000 physicians from 29 specialties; 33% of the respondents said that they were more easily frustrated by patients, and 32% reported less personal engagement.9 Burnout adversely impacts care, patient satisfaction, productivity, physician retention, retirement, and income, as well.6 Safety during clinical practice deteriorates because of an increase in medical error rates.10 Resultant emotional distress for physicians creates a vicious cycle.10
[polldaddy:10427848]
Continue to: These issues negatively impact...
These issues negatively impact practice enthusiasm and may engender self-doubt.11 They may lead to absenteeism or, worse, to abandoning the profession, further contributing to physician shortages.12 The financial impact of physician burnout in lost revenue in 2018 was about $17 billion, according to the National Taskforce for Humanity in Medicine.13
How prevalent is physician burnout?
Between October 2012 and March 2013, the American Society of Clinical Oncology surveyed US oncologists and found that 45% had evidence of burnout.14 In another survey of US physicians from all specialties conducted in 2011, at least 1 symptom of burnout was documented in nearly 46% of respondents.15 By 2014, this percentage increased to 54%.16
In 2018, the Medscape National Physician Burnout and Depression Report indicated that 42% of physicians admitted to some burnout, while 12% said they were unhappy at work, and 3% reported being clinically depressed.9 About 48% of female practitioners reported burnout vs 38% of male peers.9 Work-related distress varies between specialties, with internists, family physicians, intensivists, neurologists, and gynecologists more affected than those from other specialties.9
Causes and contributing factors
Job stress generally increases with changes in the workplace. This can be heightened in the health care workplace, which demands perfection and leaves little room for emotional issues. Loss of autonomy, time constraints associated with clinical care, electronic health record (EHR) documentation, and disorganized workflow tend to contribute to provider dissatisfaction and stress, as do ethical disagreements about patient care between physicians and leadership.10,17 Fear of reprisal for speaking up about such issues can further exacerbate the problem. Some older physicians may have difficulty with technology and computerized record keeping. Reduced patient contact due to increasing reliance on computers can diminish physicians’ job satisfaction. And managing recurrent or difficult-to-treat ailments can result in compassion fatigue, diminished empathy, and emotional disengagement.
Burnout in the health care workplace is inconsistently addressed, despite negative professional and personal ramifications. The reasons include denial, uncertainty about monetary implications, and lack of corrective programs by decision-making organizations and/or employers.6 American medicine has lacked the political and financial will to implement strategies to mitigate burnout. Improvement requires changes on the part of government, physician groups, and the population at large.
The answer?
A multipronged approach
Identifying burnout is the first step in management. The 22-item Maslach Burnout Inventory (MBI) is a self-reporting questionnaire, reliable at detecting and assessing burnout severity.18 It screens 3 main domains: emotional exhaustion, depersonalization, and diminished feelings of accomplishment. The American Medical Association recommends the 10-item Zero Burnout Program—the “Mini Z Survey”—as being quicker and more convenient.19
Once the problem is recognized, experts suggest adopting a multipronged approach to prevention and intervention by using personal, organizational, and legislative strategies.20
Continue to: On a personal level...
On a personal level, it’s important to identify stressors and employ stress-reduction and coping skills, such as mindfulness and/or reflection.21 Mindfulness programs may help to minimize exhaustion, increase compassion, and improve understanding of other people’s feelings.22 Such programs are widely available and may be accessed through the Internet, mental health centers, or by contacting psychiatric or psychological services.
Other self-care methods include ensuring adequate sleep, nutrition, exercise, and enjoyable activities. If a physician who is suffering from burnout is taking any prescription or over-the-counter drugs or supplements, it is important to be self-aware of the potential for misuse of medications. Of course, one should never self-prescribe controlled drugs, such as opiates and sedatives. Consumption of alcohol must be well-controlled, without excesses, and drinking near bedtime is ill-advised. The use of illegal substances should be avoided.
Pursuing aspects of health care that are meaningful and that increase patient contact time can boost enthusiasm, as can focusing on the positives aspects of one’s career.23 Continuing medical education can enhance self-esteem and promote a sense of purpose.24
Peer support. Practice partners may assist their colleagues by alerting them to signs of burnout, offering timely intervention suggestions, and monitoring the effectiveness of strategies. Physicians should discuss stress and burnout with their peers; camaraderie within a practice group is helpful.
Professional coaches or counselors may be engaged to mitigate workplace distress. Coaching is best instituted collegially with pre-identified goals in order to minimize stigmatization.
Continue to: Professional societies and medical boards
Professional societies and medical boards. Reporting requirements by medical boards tend to stigmatize those seeking professional assistance. But that could change if all of us—through our participation in these organizations—pursue change.
Specifically, organizations and related societies could assist with better guidance and policy adjustment (see “Resources”). State medical boards could, for example, increase education of, and outreach to, physicians about mental health issues, while maintaining confidentiality.25 Medical organizations could regularly survey their membership to identify burnout early and identify personal, social, and institutional shortcomings that contribute to physician burnout. In addition, hospital quality improvement committees that monitor health care delivery appropriateness could take steps toward change as well.
SIDEBAR
Resources to help combat burnout
- National Academy of Medicine Action Collaborative on Clinician Well- Being and Resilience: https://nam.edu/initiatives/clinician-resilience-and-well-being/
- The Schwartz Center for Compassionate Healthcare: http://www.theschwartzcenter.org
- NEJM Catalyst: http://catalyst.nejm.org/posts?q=burnout
- The American Medical Association, Joy in Medicine: https://www.ama-assn.org/search?search=joy+in+medicine
- Agency for Healthcare Research and Quality: https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
- Accreditation Council for Graduate Medical Education Tools and Resources for Resident and Faculty Member Well-Being: https://www.acgme.org/What-We-Do/Initiatives/Physician-Well-Being/Resources
The American Medical Association (AMA) just recently announced that they are launching a new effort to fight the causes of physician burnout. The AMA’s Practice Transformation Inititative26 seeks to fill the knowledge gaps regarding effective interventions to reduce burnout. AMA’s leadership indicates that the initiative will focus on “improving joy in medicine by using validated assessment tools to measure burnout; field-testing interventions that are designed to improve workflows, applying practice science research methodology to evaluate impact, and sharing best practices within an AMA-facilitated learning community.”26
Stanford’s example. Stanford University instituted a ‘time bank’ program, to help their academic medical faculty balance work and life and reduce stress. They essentially offer services, such as home food delivery and house cleaning, in return for hours spent in the clinic.27
Reorganizing and reprioritizing. Prioritizing physician wellness as a quality indicator and instituting a committee to advocate for wellness can help attenuate burnout.28,29 Specific measures include minimizing rushed, overloaded scheduling and allowing more clinical contact time with patients. Using nursing and office staff to streamline workflow is also helpful.29 The University of Colorado’s “Ambulatory Process Excellence Model” strives to assist doctors by increasing the medical assistant-to-clinician ratio, yielding better productivity.23 Medical assistants are increasingly handling tasks such as data entry, medication reconciliation, and preventive care, to allow physicians more time to focus on medical decision-making.23
Continue to: The role of the EHR
The role of the EHR. One important way to boost professional morale is to simplify and shorten the EHR. The complexity of and reduced patient contact caused by today’s record-keeping systems is the source of great frustration among many physicians. In addition, many patients dislike the disproportionate attention paid by physicians to the computer during office visits, further compromising physician-patient relationships. Improving documentation methodology and/or employing medical assistant scribes can be helpful.30,31 (See “Advanced team-based care: How we made it work” at http://bit.ly/2lNaB5Q.)
Legislation with physician input can mandate policies for more appropriate work environments. A good way to initiate improvement and reform strategies is to contact local medical societies and political representatives. Federal and state collaboration to reduce physician shortages in selected specialties or geographic regions can improve work-related stress. This might be attained by expanding residency programs, using telemedicine in underserved regions, and employing more physician assistants.32
Health insurance. Enhancing universal access to affordable medical care, including pharmaceutical coverage, would alleviate stress for physicians and patients alike.33 Health insurance regulation to decrease paperwork and simplify coverage would decrease physician workload. Standardized policy requirements, fewer exclusionary rules, and simplified prescribing guidelines (including having less cumbersome prescription pre-authorizations and greater standardization of drug formularies by different payer sources or insurance plans) would facilitate better clinical management.
CASE
Dr. D begins by discussing his concerns with his colleagues in the group practice and finds he is not alone. Many of the concerns of the group center around brief, rushed appointments that diminish relationships with patients, a lack of autonomy, and the fear of medical malpractice. Several older physicians acknowledge that they just want to retire.
To address the patient contact and documentation issues, the group decides to hire scribes. They also decide to bring their concerns to the next county medical society meeting. The end result: They petitioned their state medical association to host presentations about mitigating burnout, to hold roundtable discussions, and to establish panels focused on remedying the situation.
Continue to: With this accomplished...
With this accomplished, Dr. D’s anxieties lessened. He surveyed relevant literature and shared tips for improving professional time management with his partners. In a hopeful mood, he volunteered to address burnout prevention at the next statewide medical meeting. He felt it was a good start.
CORRESPONDENCE
Steven Lippmann, MD, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; steven.lippmann@louisville.edu.
1. Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263-1269.
2. Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burnout Research. 2016;3:89-100.
3. Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Int Med. 2008;149:334-341.
4. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
5. Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463-471.
6. Shanafelt TD, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
7. Cottler LB, Ajinkya S, Merlo LJ, et al. Lifetime psychiatric and substance use disorders among impaired physicians in a physicians health program. J Addict Med. 2013;7:108-112.
8. Consiglio C. Interpersonal strain at work: a new burnout facet relevant for the health of hospital staff. Burnout Res. 2014;1:69-75.
9. Peckham C. Medscape National Physician Burnout and Depression Report 2018. January 12, 2018. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235. Accessed October 4, 2019.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527-533.
12. Suñer-Soler R, Grau-Martin A, Flichtentrei D, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burnout Research. 2014;1:82-89.
13. National Taskforce for Humanity in Healthcare. Position paper: The business case for humanity in healthcare. April 2018. https://www.vocera.com/public/pdf/NTHBusinessCase_final003.pdf. Accessed October 4, 2019.
14. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678-686.
15. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Int Med. 2012;172:1377-1385.
16. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90;1600-1613.
17. Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151:28-36.
18. Maslach C, Jackson SE. The measurement of experienced burnout. J Occcup Behav. 1981;2:99-113.
19. Linzer M, Guzman-Corrales L, Poplau S. Physician Burnout: improve physician satisfaction and patient outcomes. June 5, 2015. https://www.stepsforward.org/modules/physician-burnout. Accessed October 4, 2019.
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272-2281.
21. Nedrow A, Steckler NA, Hardman J. Physician resilience and burnout: can you make the switch? Fam Prac Manag. 2013;20:25-30.
22. Verweij H, van Ravesteijn H, van Hooff MLM, et al. Mindfulness-based stress reduction for residents: a randomized controlled trial. J Gen Intern Med. 2018;33:429-436.
23. Wright AA, Katz IT. Beyond burnout – redesigning care to restore meaning and sanity for physicians. N Eng J Med. 2018;378:309-311.
24. Shanafelt TD, Gorringe G, Menaker R, et. al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432-440.
25. Hengerer A, Kishore S. 2017. Breaking a culture of silence: the role of state medical boards. National Academy of Medicine, Washington DC. https://nam.edu/breaking-a-culture-of-silence-the-role-of-state-medical-boards/. Accessed October 4, 2019.
26. American Medical Association. AMA fights burnout with new practice transformation initiative. September 5, 2019. https://www.ama-assn.org/press-center/press-releases/ama-fights-burnout-new-practice-transformation-initiative. Accessed September 5, 2019.
27. Schulte B. Time in the bank: a Stanford plan to save doctors from burnout. The Washington Post. https://www.washingtonpost.com/news/inspired-life/wp/2015/08/20/the-innovative-stanford-program-thats-saving-emergency-room-doctors-from-burnout/?utm_term=.838c930e8de7. Accessed October 4, 2019.
28. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721.
29. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
30. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Info Assoc. 2014;21:E100-E106.
31. Bodenheimer T, Willard-Grace R, Ghorob A. Expanding the roles of medical assistants: who does what in primary care? JAMA Intern Med. 2014;174:1025-1026.
32. Mangiofico G. Physician shortage requires multi-prong solution. January 26, 2018. Am J Manag Care. https://www.ajmc.com/contributor/dr-gary-mangiofico/2018/01/physician-shortage-requires-multiprong-solution. Accessed October 4, 2019.
33. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
1. Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263-1269.
2. Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burnout Research. 2016;3:89-100.
3. Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Int Med. 2008;149:334-341.
4. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
5. Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463-471.
6. Shanafelt TD, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
7. Cottler LB, Ajinkya S, Merlo LJ, et al. Lifetime psychiatric and substance use disorders among impaired physicians in a physicians health program. J Addict Med. 2013;7:108-112.
8. Consiglio C. Interpersonal strain at work: a new burnout facet relevant for the health of hospital staff. Burnout Res. 2014;1:69-75.
9. Peckham C. Medscape National Physician Burnout and Depression Report 2018. January 12, 2018. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235. Accessed October 4, 2019.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527-533.
12. Suñer-Soler R, Grau-Martin A, Flichtentrei D, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burnout Research. 2014;1:82-89.
13. National Taskforce for Humanity in Healthcare. Position paper: The business case for humanity in healthcare. April 2018. https://www.vocera.com/public/pdf/NTHBusinessCase_final003.pdf. Accessed October 4, 2019.
14. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678-686.
15. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Int Med. 2012;172:1377-1385.
16. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90;1600-1613.
17. Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151:28-36.
18. Maslach C, Jackson SE. The measurement of experienced burnout. J Occcup Behav. 1981;2:99-113.
19. Linzer M, Guzman-Corrales L, Poplau S. Physician Burnout: improve physician satisfaction and patient outcomes. June 5, 2015. https://www.stepsforward.org/modules/physician-burnout. Accessed October 4, 2019.
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272-2281.
21. Nedrow A, Steckler NA, Hardman J. Physician resilience and burnout: can you make the switch? Fam Prac Manag. 2013;20:25-30.
22. Verweij H, van Ravesteijn H, van Hooff MLM, et al. Mindfulness-based stress reduction for residents: a randomized controlled trial. J Gen Intern Med. 2018;33:429-436.
23. Wright AA, Katz IT. Beyond burnout – redesigning care to restore meaning and sanity for physicians. N Eng J Med. 2018;378:309-311.
24. Shanafelt TD, Gorringe G, Menaker R, et. al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432-440.
25. Hengerer A, Kishore S. 2017. Breaking a culture of silence: the role of state medical boards. National Academy of Medicine, Washington DC. https://nam.edu/breaking-a-culture-of-silence-the-role-of-state-medical-boards/. Accessed October 4, 2019.
26. American Medical Association. AMA fights burnout with new practice transformation initiative. September 5, 2019. https://www.ama-assn.org/press-center/press-releases/ama-fights-burnout-new-practice-transformation-initiative. Accessed September 5, 2019.
27. Schulte B. Time in the bank: a Stanford plan to save doctors from burnout. The Washington Post. https://www.washingtonpost.com/news/inspired-life/wp/2015/08/20/the-innovative-stanford-program-thats-saving-emergency-room-doctors-from-burnout/?utm_term=.838c930e8de7. Accessed October 4, 2019.
28. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721.
29. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
30. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Info Assoc. 2014;21:E100-E106.
31. Bodenheimer T, Willard-Grace R, Ghorob A. Expanding the roles of medical assistants: who does what in primary care? JAMA Intern Med. 2014;174:1025-1026.
32. Mangiofico G. Physician shortage requires multi-prong solution. January 26, 2018. Am J Manag Care. https://www.ajmc.com/contributor/dr-gary-mangiofico/2018/01/physician-shortage-requires-multiprong-solution. Accessed October 4, 2019.
33. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
Overdoses are driving down life expectancy
The average life expectancy in the United States declined from 78.9 years in 2014 to 78.6 years in 2017.1 The 2017 figure—78.6 years—means life expectancy is shorter in the United States than in other countries.1 The decline is due, in part, to the drug overdose epidemic in the United States.2 In 2017, 70,237 people died by drug overdose2—with prescription drugs, heroin, and opioids (especially fentanyl) being the major threats.3 From 2016 to 2017, overdoses from synthetic opioids, such as fentanyl, fentanyl analogs, and tramadol, increased from 6.2 to 9 per 100,000 people.2
These statistics should motivate all health care professionals to improve the general public’s health metrics, especially when treating patients with substance use disorders. But to best do so, we need a collaborative effort across many professions—not just health care providers, but also public health officials, elected government leaders, and law enforcement. To better define what this would entail, we suggest ways in which these groups could expand their roles to help reduce overdose deaths.
Health care professionals:
- implement safer opioid prescribing for patients who have chronic pain;
- educate patients about the risks of opioid use;
- consider alternative therapies for pain management; and
- utilize electronic databases to monitor controlled substance prescribing.
Public health officials:
- expand naloxone distribution; and
- enhance harm reduction (eg, syringe exchange programs, substance abuse treatment options).
Government leaders:
- draft legislation that allows the use of better interventions for treating individuals with drug dependence or those who overdose; and
- improve criminal justice approaches so that laws are less punitive and more therapeutic for individuals who suffer from drug dependence.
Law enforcement:
- supply naltrexone kits to first responders and provide appropriate training.
Kuldeep Ghosh, MD, MS
Rajashekhar Yeruva, MD
Steven Lippmann, MD
Louisville, Ky
1. National Center for Health Statistics. Table 15. Life expectancy at birth, at age 65, and at age 75, by sex, race, and Hispanic origin: United States, selected years 1900-2015. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/hus/2016/015.pdf. Published 2016. Accessed April 24, 2019.
2. Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2017. NCHS Data Brief No 329. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published November 2019. Accessed April 24, 2019.
3. United States Drug Enforcement Administration. DEA releases 2018 National Drug Threat Assessment. https://www.dea.gov/press-releases/2018/11/02/dea-releases-2018-national-drug-threat-assessment-0. Published November 2, 2018. Accessed April 24, 2019.
The average life expectancy in the United States declined from 78.9 years in 2014 to 78.6 years in 2017.1 The 2017 figure—78.6 years—means life expectancy is shorter in the United States than in other countries.1 The decline is due, in part, to the drug overdose epidemic in the United States.2 In 2017, 70,237 people died by drug overdose2—with prescription drugs, heroin, and opioids (especially fentanyl) being the major threats.3 From 2016 to 2017, overdoses from synthetic opioids, such as fentanyl, fentanyl analogs, and tramadol, increased from 6.2 to 9 per 100,000 people.2
These statistics should motivate all health care professionals to improve the general public’s health metrics, especially when treating patients with substance use disorders. But to best do so, we need a collaborative effort across many professions—not just health care providers, but also public health officials, elected government leaders, and law enforcement. To better define what this would entail, we suggest ways in which these groups could expand their roles to help reduce overdose deaths.
Health care professionals:
- implement safer opioid prescribing for patients who have chronic pain;
- educate patients about the risks of opioid use;
- consider alternative therapies for pain management; and
- utilize electronic databases to monitor controlled substance prescribing.
Public health officials:
- expand naloxone distribution; and
- enhance harm reduction (eg, syringe exchange programs, substance abuse treatment options).
Government leaders:
- draft legislation that allows the use of better interventions for treating individuals with drug dependence or those who overdose; and
- improve criminal justice approaches so that laws are less punitive and more therapeutic for individuals who suffer from drug dependence.
Law enforcement:
- supply naltrexone kits to first responders and provide appropriate training.
Kuldeep Ghosh, MD, MS
Rajashekhar Yeruva, MD
Steven Lippmann, MD
Louisville, Ky
The average life expectancy in the United States declined from 78.9 years in 2014 to 78.6 years in 2017.1 The 2017 figure—78.6 years—means life expectancy is shorter in the United States than in other countries.1 The decline is due, in part, to the drug overdose epidemic in the United States.2 In 2017, 70,237 people died by drug overdose2—with prescription drugs, heroin, and opioids (especially fentanyl) being the major threats.3 From 2016 to 2017, overdoses from synthetic opioids, such as fentanyl, fentanyl analogs, and tramadol, increased from 6.2 to 9 per 100,000 people.2
These statistics should motivate all health care professionals to improve the general public’s health metrics, especially when treating patients with substance use disorders. But to best do so, we need a collaborative effort across many professions—not just health care providers, but also public health officials, elected government leaders, and law enforcement. To better define what this would entail, we suggest ways in which these groups could expand their roles to help reduce overdose deaths.
Health care professionals:
- implement safer opioid prescribing for patients who have chronic pain;
- educate patients about the risks of opioid use;
- consider alternative therapies for pain management; and
- utilize electronic databases to monitor controlled substance prescribing.
Public health officials:
- expand naloxone distribution; and
- enhance harm reduction (eg, syringe exchange programs, substance abuse treatment options).
Government leaders:
- draft legislation that allows the use of better interventions for treating individuals with drug dependence or those who overdose; and
- improve criminal justice approaches so that laws are less punitive and more therapeutic for individuals who suffer from drug dependence.
Law enforcement:
- supply naltrexone kits to first responders and provide appropriate training.
Kuldeep Ghosh, MD, MS
Rajashekhar Yeruva, MD
Steven Lippmann, MD
Louisville, Ky
1. National Center for Health Statistics. Table 15. Life expectancy at birth, at age 65, and at age 75, by sex, race, and Hispanic origin: United States, selected years 1900-2015. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/hus/2016/015.pdf. Published 2016. Accessed April 24, 2019.
2. Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2017. NCHS Data Brief No 329. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published November 2019. Accessed April 24, 2019.
3. United States Drug Enforcement Administration. DEA releases 2018 National Drug Threat Assessment. https://www.dea.gov/press-releases/2018/11/02/dea-releases-2018-national-drug-threat-assessment-0. Published November 2, 2018. Accessed April 24, 2019.
1. National Center for Health Statistics. Table 15. Life expectancy at birth, at age 65, and at age 75, by sex, race, and Hispanic origin: United States, selected years 1900-2015. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/hus/2016/015.pdf. Published 2016. Accessed April 24, 2019.
2. Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2017. NCHS Data Brief No 329. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published November 2019. Accessed April 24, 2019.
3. United States Drug Enforcement Administration. DEA releases 2018 National Drug Threat Assessment. https://www.dea.gov/press-releases/2018/11/02/dea-releases-2018-national-drug-threat-assessment-0. Published November 2, 2018. Accessed April 24, 2019.