User login
Examining bias
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
First-episode psychosis in the time of COVID-19
Patients may need more than weekly teletherapy
In response to COVID-19, we have seen a rapid transformation to virtually delivered mental health care, essential for the prevention and treatment of various mental health conditions during an isolating and stress-inducing pandemic. Yet teletherapy and virtual medication management alone may not adequately address the needs of some of the populations we serve.
Take Jackson, whose name and details have been changed for privacy. A year ago, Jackson, in his last year of high school, began hearing voices that others could not hear. After becoming increasingly withdrawn, his father sought out treatment for him and learned that Jackson was experiencing his first episode of psychosis.
Psychosis involves disruptions in the way one processes thoughts and feelings or behaves, and includes delusions – or unusual beliefs – and hallucinations, meaning seeing and hearing things that others cannot. “First-episode psychosis” (FEP) simply refers to the first time an individual experiences this. It typically occurs between one’s teenage years and their 20s. Whereas some individuals recover from their first episode and may not experience another, others go on to experience recurrence, and sometimes a waxing and waning illness course.
Jackson enrolled in a comprehensive mental health program that not only includes a psychiatrist, but also therapists who provide case management services, as well as a peer specialist; this is someone with lived experience navigating mental illness. The program also includes an employment and education specialist and family and group therapy sessions. His team helped him identify and work toward his personal recovery goals: graduating from high school, obtaining a job, and maintaining a strong relationship with his father.
One hundred thousand adolescents and young adults like Jackson experience FEP each year, and now, in the wake of COVID-19, they probably have more limited access to the kind of support that can be vital to recovery.
Studies have shown that untreated psychosis can detrimentally affect quality of life in several ways, including by negatively affecting interpersonal relationships, interfering with obtaining or maintaining employment, and increasing the risk for problematic substance use. The psychosocial effects of COVID-19 could compound problems that individuals navigating psychosis already face, such as stigmatization, social isolation, and unemployment. On top of this, individuals who experience additional marginalization and downstream effects of systematic discriminatory practices by virtue of their race or ethnicity, immigration status, or language bear the brunt of some of this pandemic’s worst health inequities.
Early and efficacious treatment is critically important for individuals experiencing psychosis. Evidence shows that engagement in coordinated specialty care (CSC) specifically can improve outcomes, including the likelihood of being engaged in school or work and lower rates of hospitalization. CSC is a team-based approach that utilizes the unique skills of every team member to support an individual in reaching their recovery goals, whether it’s starting or finishing college or building a new relationship.
Unlike traditional treatment goals, which often focus on “symptom reduction,” recovery-oriented care is about supporting an individual in obtaining a sense of satisfaction, meaning, and purpose in life. It also supports navigating such experiences as a job interview or a date. These key, multifaceted components must be made accessible and adapted during these times.
For individuals like Jackson, it is crucial to be able to continue accessing quality CSC, even during our current pandemic. Lisa Dixon, MD, a professor of psychiatry at Columbia University, leads ONTrackNY, a statewide FEP program. She states that “effective, recovery-oriented treatment can make such a huge difference in the lives of these young people who are at a potential inflection point in their lives. Creative, collaborative clinicians can maintain connection and support.”
So how can we adapt CSC during this time? In addition to virtualized medication management and individual therapy, other components of CSC can be creatively adapted for online platforms. Group sessions can be completed virtually, from family to peer-led. Though the unemployment rate continues to rise, we can still help participants with a desire to work find employers that are offering remote work or navigate the risks of potential COVID-19 work exposures if remote options aren’t available. We can also support their developing skills to be used once other employers that pose less risk reopen.
For those in school, virtual education support can provide study skills, ways to cope with transition to an online classroom, or help with obtaining tutoring. Nutritionists can work remotely to provide support and creatively use online platforms for real-time feedback in a participant’s kitchen. Virtual case management is even more essential in the wake of COVID-19, from assistance with applying for unemployment insurance and financial aid to obtaining health insurance or determining eligibility.
For those without access to virtual platforms, individual and group telephone sessions and text check-ins can provide meaningful opportunities for continued engagement. For those who are unstably housed or have limited privacy in housing, teams must generate ideas of where to have remote sessions, such as a nearby park.
In a world now dominated by virtual care, it is critically important that individuals needing to see a clinician in person still be able to do so. Whether it is due to an acute crisis or to administer a long-acting injection medication, it is our responsibility to thoughtfully and judiciously remain available to patients, using appropriate personal protective equipment and precautions.
Jackson is one of many young people in recovery from psychosis. He is not defined by or limited by his experiences, but rather is navigating the possibilities that lie ahead of him, defining for himself who he wants to be in this world as it evolves. In the midst of COVID-19, as we seek to innovate – from how we exercise to how we throw birthday parties – let’s also be innovative in how we provide care and support for individuals experiencing psychosis.
This article first appeared on Medscape.com.
Patients may need more than weekly teletherapy
Patients may need more than weekly teletherapy
In response to COVID-19, we have seen a rapid transformation to virtually delivered mental health care, essential for the prevention and treatment of various mental health conditions during an isolating and stress-inducing pandemic. Yet teletherapy and virtual medication management alone may not adequately address the needs of some of the populations we serve.
Take Jackson, whose name and details have been changed for privacy. A year ago, Jackson, in his last year of high school, began hearing voices that others could not hear. After becoming increasingly withdrawn, his father sought out treatment for him and learned that Jackson was experiencing his first episode of psychosis.
Psychosis involves disruptions in the way one processes thoughts and feelings or behaves, and includes delusions – or unusual beliefs – and hallucinations, meaning seeing and hearing things that others cannot. “First-episode psychosis” (FEP) simply refers to the first time an individual experiences this. It typically occurs between one’s teenage years and their 20s. Whereas some individuals recover from their first episode and may not experience another, others go on to experience recurrence, and sometimes a waxing and waning illness course.
Jackson enrolled in a comprehensive mental health program that not only includes a psychiatrist, but also therapists who provide case management services, as well as a peer specialist; this is someone with lived experience navigating mental illness. The program also includes an employment and education specialist and family and group therapy sessions. His team helped him identify and work toward his personal recovery goals: graduating from high school, obtaining a job, and maintaining a strong relationship with his father.
One hundred thousand adolescents and young adults like Jackson experience FEP each year, and now, in the wake of COVID-19, they probably have more limited access to the kind of support that can be vital to recovery.
Studies have shown that untreated psychosis can detrimentally affect quality of life in several ways, including by negatively affecting interpersonal relationships, interfering with obtaining or maintaining employment, and increasing the risk for problematic substance use. The psychosocial effects of COVID-19 could compound problems that individuals navigating psychosis already face, such as stigmatization, social isolation, and unemployment. On top of this, individuals who experience additional marginalization and downstream effects of systematic discriminatory practices by virtue of their race or ethnicity, immigration status, or language bear the brunt of some of this pandemic’s worst health inequities.
Early and efficacious treatment is critically important for individuals experiencing psychosis. Evidence shows that engagement in coordinated specialty care (CSC) specifically can improve outcomes, including the likelihood of being engaged in school or work and lower rates of hospitalization. CSC is a team-based approach that utilizes the unique skills of every team member to support an individual in reaching their recovery goals, whether it’s starting or finishing college or building a new relationship.
Unlike traditional treatment goals, which often focus on “symptom reduction,” recovery-oriented care is about supporting an individual in obtaining a sense of satisfaction, meaning, and purpose in life. It also supports navigating such experiences as a job interview or a date. These key, multifaceted components must be made accessible and adapted during these times.
For individuals like Jackson, it is crucial to be able to continue accessing quality CSC, even during our current pandemic. Lisa Dixon, MD, a professor of psychiatry at Columbia University, leads ONTrackNY, a statewide FEP program. She states that “effective, recovery-oriented treatment can make such a huge difference in the lives of these young people who are at a potential inflection point in their lives. Creative, collaborative clinicians can maintain connection and support.”
So how can we adapt CSC during this time? In addition to virtualized medication management and individual therapy, other components of CSC can be creatively adapted for online platforms. Group sessions can be completed virtually, from family to peer-led. Though the unemployment rate continues to rise, we can still help participants with a desire to work find employers that are offering remote work or navigate the risks of potential COVID-19 work exposures if remote options aren’t available. We can also support their developing skills to be used once other employers that pose less risk reopen.
For those in school, virtual education support can provide study skills, ways to cope with transition to an online classroom, or help with obtaining tutoring. Nutritionists can work remotely to provide support and creatively use online platforms for real-time feedback in a participant’s kitchen. Virtual case management is even more essential in the wake of COVID-19, from assistance with applying for unemployment insurance and financial aid to obtaining health insurance or determining eligibility.
For those without access to virtual platforms, individual and group telephone sessions and text check-ins can provide meaningful opportunities for continued engagement. For those who are unstably housed or have limited privacy in housing, teams must generate ideas of where to have remote sessions, such as a nearby park.
In a world now dominated by virtual care, it is critically important that individuals needing to see a clinician in person still be able to do so. Whether it is due to an acute crisis or to administer a long-acting injection medication, it is our responsibility to thoughtfully and judiciously remain available to patients, using appropriate personal protective equipment and precautions.
Jackson is one of many young people in recovery from psychosis. He is not defined by or limited by his experiences, but rather is navigating the possibilities that lie ahead of him, defining for himself who he wants to be in this world as it evolves. In the midst of COVID-19, as we seek to innovate – from how we exercise to how we throw birthday parties – let’s also be innovative in how we provide care and support for individuals experiencing psychosis.
This article first appeared on Medscape.com.
In response to COVID-19, we have seen a rapid transformation to virtually delivered mental health care, essential for the prevention and treatment of various mental health conditions during an isolating and stress-inducing pandemic. Yet teletherapy and virtual medication management alone may not adequately address the needs of some of the populations we serve.
Take Jackson, whose name and details have been changed for privacy. A year ago, Jackson, in his last year of high school, began hearing voices that others could not hear. After becoming increasingly withdrawn, his father sought out treatment for him and learned that Jackson was experiencing his first episode of psychosis.
Psychosis involves disruptions in the way one processes thoughts and feelings or behaves, and includes delusions – or unusual beliefs – and hallucinations, meaning seeing and hearing things that others cannot. “First-episode psychosis” (FEP) simply refers to the first time an individual experiences this. It typically occurs between one’s teenage years and their 20s. Whereas some individuals recover from their first episode and may not experience another, others go on to experience recurrence, and sometimes a waxing and waning illness course.
Jackson enrolled in a comprehensive mental health program that not only includes a psychiatrist, but also therapists who provide case management services, as well as a peer specialist; this is someone with lived experience navigating mental illness. The program also includes an employment and education specialist and family and group therapy sessions. His team helped him identify and work toward his personal recovery goals: graduating from high school, obtaining a job, and maintaining a strong relationship with his father.
One hundred thousand adolescents and young adults like Jackson experience FEP each year, and now, in the wake of COVID-19, they probably have more limited access to the kind of support that can be vital to recovery.
Studies have shown that untreated psychosis can detrimentally affect quality of life in several ways, including by negatively affecting interpersonal relationships, interfering with obtaining or maintaining employment, and increasing the risk for problematic substance use. The psychosocial effects of COVID-19 could compound problems that individuals navigating psychosis already face, such as stigmatization, social isolation, and unemployment. On top of this, individuals who experience additional marginalization and downstream effects of systematic discriminatory practices by virtue of their race or ethnicity, immigration status, or language bear the brunt of some of this pandemic’s worst health inequities.
Early and efficacious treatment is critically important for individuals experiencing psychosis. Evidence shows that engagement in coordinated specialty care (CSC) specifically can improve outcomes, including the likelihood of being engaged in school or work and lower rates of hospitalization. CSC is a team-based approach that utilizes the unique skills of every team member to support an individual in reaching their recovery goals, whether it’s starting or finishing college or building a new relationship.
Unlike traditional treatment goals, which often focus on “symptom reduction,” recovery-oriented care is about supporting an individual in obtaining a sense of satisfaction, meaning, and purpose in life. It also supports navigating such experiences as a job interview or a date. These key, multifaceted components must be made accessible and adapted during these times.
For individuals like Jackson, it is crucial to be able to continue accessing quality CSC, even during our current pandemic. Lisa Dixon, MD, a professor of psychiatry at Columbia University, leads ONTrackNY, a statewide FEP program. She states that “effective, recovery-oriented treatment can make such a huge difference in the lives of these young people who are at a potential inflection point in their lives. Creative, collaborative clinicians can maintain connection and support.”
So how can we adapt CSC during this time? In addition to virtualized medication management and individual therapy, other components of CSC can be creatively adapted for online platforms. Group sessions can be completed virtually, from family to peer-led. Though the unemployment rate continues to rise, we can still help participants with a desire to work find employers that are offering remote work or navigate the risks of potential COVID-19 work exposures if remote options aren’t available. We can also support their developing skills to be used once other employers that pose less risk reopen.
For those in school, virtual education support can provide study skills, ways to cope with transition to an online classroom, or help with obtaining tutoring. Nutritionists can work remotely to provide support and creatively use online platforms for real-time feedback in a participant’s kitchen. Virtual case management is even more essential in the wake of COVID-19, from assistance with applying for unemployment insurance and financial aid to obtaining health insurance or determining eligibility.
For those without access to virtual platforms, individual and group telephone sessions and text check-ins can provide meaningful opportunities for continued engagement. For those who are unstably housed or have limited privacy in housing, teams must generate ideas of where to have remote sessions, such as a nearby park.
In a world now dominated by virtual care, it is critically important that individuals needing to see a clinician in person still be able to do so. Whether it is due to an acute crisis or to administer a long-acting injection medication, it is our responsibility to thoughtfully and judiciously remain available to patients, using appropriate personal protective equipment and precautions.
Jackson is one of many young people in recovery from psychosis. He is not defined by or limited by his experiences, but rather is navigating the possibilities that lie ahead of him, defining for himself who he wants to be in this world as it evolves. In the midst of COVID-19, as we seek to innovate – from how we exercise to how we throw birthday parties – let’s also be innovative in how we provide care and support for individuals experiencing psychosis.
This article first appeared on Medscape.com.
NSAID/triptan combination improves treatment-resistant migraine
The combination (AXS-07), in development by Axsome Therapeutics, was also safe and well tolerated, according to Cedric O’Gorman, MD, Axsome senior vice president for clinical development and medical affairs. It was tested in subjects who had inadequately responded to previous treatment and who had an average of 2-8 migraines per month.
The therapy combines 10-mg rizatriptan with 20-mg meloxicam delivered by the company’s MoSEIC technology. “Treatment with AXS-07 resulted in rapid, sustained, substantial, and statistically significant effect as compared with rizatriptan and placebo. The enhanced effect of AXS-07 may be especially relevant for patients with more difficult-to-treat migraine,” said Dr. O’Gorman during a presentation of the study at the virtual annual meeting of the American Headache Society.
Matthew Robbins, MD, said in an interview, “This combination may be particularly useful for patients who want to take an oral medication but still need rapid and sustained pain freedom.” Dr. Robbins is the neurology residency program director at New York Presbyterian Hospital and an associate professor of neurology at Weill Cornell Medicine, New York. He was not involved in the research.
The study randomized 1,594 patients 2:2:2:1 to AXS-07, rizatriptan alone, MoSEIC meloxicam alone, or placebo, which could be administered immediately after a migraine event. Between 35% and 40% of participants across the groups had previously used triptans. The mean migraine treatment optimization questionnaire (mTOQ4) score was 3.6, indicating that the population was made up of people with poor responses to medication. Among patients in the study group, 37%-43% had severe pain intensity, 41%-47% were obese, and 35%-37% had morning migraine.
At 2 hours, more patients in the AXS-07 group than in the placebo group were pain free (19.9% vs. 6.7%; P < 0.001). They were also more likely to experience freedom from the most bothersome symptom at 2 hours (36.9% vs. 24.4%; P = 0.002). Secondary outcome measures favored the AXS-07 group when compared with the rizatriptan-only group, including 1-hour pain relief (44% vs. 37%; P = 0.04), 2- to 24-hour sustained pain relief (53% vs. 44%; P = 0.006), 2- to 48-hour sustained pain relief (47% vs. 37%; P = 0.003), 2- to 24-hour sustained pain freedom (16% vs. 11%; P = 0.038), 2- to 48-hour sustained pain freedom (15% vs. 8.8%; P = 0.003), rescue medication use (23% vs. 35%; P < 0.001), a rating of much or very much improved on the Patient Global Impression of Change (PGI-C) scale (47% vs. 39%; P = 0.022), and functional improvement at 24 hours (64% vs. 56%; P = 0.027).
“The percentage of patients achieving pain relief with AXS-07 was numerically greater than with rizatriptan at every time point measure, starting at 15 minutes, and was statistically significant by 60 minutes. This is significant because rizatriptan is widely recognized as the fastest-acting and one of the most effective oral triptans,” said Dr. O’Gorman.
The frequency of adverse events was 11.0% in the AXS-07, 15.4% in the rizatriptan group, 11.5% in the meloxicam group, and 6.0% in the placebo group.
“The added benefit of this study was the demonstration of efficacy in patients who have previously failed other acute treatments. We know that ineffective acute treatments are a likely risk factor for the progression of episodic migraine to chronic migraine, and the more options that we have for our patients, the better,” Dr. Robbins commented.
He remains concerned about cost and access, however. A limited number of tablets per month for acute treatments prompt clinicians to prescribe the medications individually and advise patients to take them in combination. “Rizatriptan is generally available in 12 monthly tablets by many coverage plans, and I would hope that, if ultimately FDA approved, a similar allotment is made affordable and accessible,” he said.
The study was funded by Axsome Therapeutics. Dr. O’Gorman is an employee of Axsome. Dr. Robbins has no relevant financial disclosures.
SOURCE: O’Gorman C et al. AHS 2020, Abstract 840673.
The combination (AXS-07), in development by Axsome Therapeutics, was also safe and well tolerated, according to Cedric O’Gorman, MD, Axsome senior vice president for clinical development and medical affairs. It was tested in subjects who had inadequately responded to previous treatment and who had an average of 2-8 migraines per month.
The therapy combines 10-mg rizatriptan with 20-mg meloxicam delivered by the company’s MoSEIC technology. “Treatment with AXS-07 resulted in rapid, sustained, substantial, and statistically significant effect as compared with rizatriptan and placebo. The enhanced effect of AXS-07 may be especially relevant for patients with more difficult-to-treat migraine,” said Dr. O’Gorman during a presentation of the study at the virtual annual meeting of the American Headache Society.
Matthew Robbins, MD, said in an interview, “This combination may be particularly useful for patients who want to take an oral medication but still need rapid and sustained pain freedom.” Dr. Robbins is the neurology residency program director at New York Presbyterian Hospital and an associate professor of neurology at Weill Cornell Medicine, New York. He was not involved in the research.
The study randomized 1,594 patients 2:2:2:1 to AXS-07, rizatriptan alone, MoSEIC meloxicam alone, or placebo, which could be administered immediately after a migraine event. Between 35% and 40% of participants across the groups had previously used triptans. The mean migraine treatment optimization questionnaire (mTOQ4) score was 3.6, indicating that the population was made up of people with poor responses to medication. Among patients in the study group, 37%-43% had severe pain intensity, 41%-47% were obese, and 35%-37% had morning migraine.
At 2 hours, more patients in the AXS-07 group than in the placebo group were pain free (19.9% vs. 6.7%; P < 0.001). They were also more likely to experience freedom from the most bothersome symptom at 2 hours (36.9% vs. 24.4%; P = 0.002). Secondary outcome measures favored the AXS-07 group when compared with the rizatriptan-only group, including 1-hour pain relief (44% vs. 37%; P = 0.04), 2- to 24-hour sustained pain relief (53% vs. 44%; P = 0.006), 2- to 48-hour sustained pain relief (47% vs. 37%; P = 0.003), 2- to 24-hour sustained pain freedom (16% vs. 11%; P = 0.038), 2- to 48-hour sustained pain freedom (15% vs. 8.8%; P = 0.003), rescue medication use (23% vs. 35%; P < 0.001), a rating of much or very much improved on the Patient Global Impression of Change (PGI-C) scale (47% vs. 39%; P = 0.022), and functional improvement at 24 hours (64% vs. 56%; P = 0.027).
“The percentage of patients achieving pain relief with AXS-07 was numerically greater than with rizatriptan at every time point measure, starting at 15 minutes, and was statistically significant by 60 minutes. This is significant because rizatriptan is widely recognized as the fastest-acting and one of the most effective oral triptans,” said Dr. O’Gorman.
The frequency of adverse events was 11.0% in the AXS-07, 15.4% in the rizatriptan group, 11.5% in the meloxicam group, and 6.0% in the placebo group.
“The added benefit of this study was the demonstration of efficacy in patients who have previously failed other acute treatments. We know that ineffective acute treatments are a likely risk factor for the progression of episodic migraine to chronic migraine, and the more options that we have for our patients, the better,” Dr. Robbins commented.
He remains concerned about cost and access, however. A limited number of tablets per month for acute treatments prompt clinicians to prescribe the medications individually and advise patients to take them in combination. “Rizatriptan is generally available in 12 monthly tablets by many coverage plans, and I would hope that, if ultimately FDA approved, a similar allotment is made affordable and accessible,” he said.
The study was funded by Axsome Therapeutics. Dr. O’Gorman is an employee of Axsome. Dr. Robbins has no relevant financial disclosures.
SOURCE: O’Gorman C et al. AHS 2020, Abstract 840673.
The combination (AXS-07), in development by Axsome Therapeutics, was also safe and well tolerated, according to Cedric O’Gorman, MD, Axsome senior vice president for clinical development and medical affairs. It was tested in subjects who had inadequately responded to previous treatment and who had an average of 2-8 migraines per month.
The therapy combines 10-mg rizatriptan with 20-mg meloxicam delivered by the company’s MoSEIC technology. “Treatment with AXS-07 resulted in rapid, sustained, substantial, and statistically significant effect as compared with rizatriptan and placebo. The enhanced effect of AXS-07 may be especially relevant for patients with more difficult-to-treat migraine,” said Dr. O’Gorman during a presentation of the study at the virtual annual meeting of the American Headache Society.
Matthew Robbins, MD, said in an interview, “This combination may be particularly useful for patients who want to take an oral medication but still need rapid and sustained pain freedom.” Dr. Robbins is the neurology residency program director at New York Presbyterian Hospital and an associate professor of neurology at Weill Cornell Medicine, New York. He was not involved in the research.
The study randomized 1,594 patients 2:2:2:1 to AXS-07, rizatriptan alone, MoSEIC meloxicam alone, or placebo, which could be administered immediately after a migraine event. Between 35% and 40% of participants across the groups had previously used triptans. The mean migraine treatment optimization questionnaire (mTOQ4) score was 3.6, indicating that the population was made up of people with poor responses to medication. Among patients in the study group, 37%-43% had severe pain intensity, 41%-47% were obese, and 35%-37% had morning migraine.
At 2 hours, more patients in the AXS-07 group than in the placebo group were pain free (19.9% vs. 6.7%; P < 0.001). They were also more likely to experience freedom from the most bothersome symptom at 2 hours (36.9% vs. 24.4%; P = 0.002). Secondary outcome measures favored the AXS-07 group when compared with the rizatriptan-only group, including 1-hour pain relief (44% vs. 37%; P = 0.04), 2- to 24-hour sustained pain relief (53% vs. 44%; P = 0.006), 2- to 48-hour sustained pain relief (47% vs. 37%; P = 0.003), 2- to 24-hour sustained pain freedom (16% vs. 11%; P = 0.038), 2- to 48-hour sustained pain freedom (15% vs. 8.8%; P = 0.003), rescue medication use (23% vs. 35%; P < 0.001), a rating of much or very much improved on the Patient Global Impression of Change (PGI-C) scale (47% vs. 39%; P = 0.022), and functional improvement at 24 hours (64% vs. 56%; P = 0.027).
“The percentage of patients achieving pain relief with AXS-07 was numerically greater than with rizatriptan at every time point measure, starting at 15 minutes, and was statistically significant by 60 minutes. This is significant because rizatriptan is widely recognized as the fastest-acting and one of the most effective oral triptans,” said Dr. O’Gorman.
The frequency of adverse events was 11.0% in the AXS-07, 15.4% in the rizatriptan group, 11.5% in the meloxicam group, and 6.0% in the placebo group.
“The added benefit of this study was the demonstration of efficacy in patients who have previously failed other acute treatments. We know that ineffective acute treatments are a likely risk factor for the progression of episodic migraine to chronic migraine, and the more options that we have for our patients, the better,” Dr. Robbins commented.
He remains concerned about cost and access, however. A limited number of tablets per month for acute treatments prompt clinicians to prescribe the medications individually and advise patients to take them in combination. “Rizatriptan is generally available in 12 monthly tablets by many coverage plans, and I would hope that, if ultimately FDA approved, a similar allotment is made affordable and accessible,” he said.
The study was funded by Axsome Therapeutics. Dr. O’Gorman is an employee of Axsome. Dr. Robbins has no relevant financial disclosures.
SOURCE: O’Gorman C et al. AHS 2020, Abstract 840673.
FROM AHS 2020
Lung ultrasound works well in children with COVID-19
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
FROM PEDIATRICS
Assessing Spinal Muscular Atrophy Across the Patient Journey

Click here to read.
Supplement Faculty
Perry Shieh, MD, PhD
Professor
Department of Neurology
David Geffen School
of Medicine at UCLA
Ronald Reagan UCLA
Medical Center
Los Angeles, CA
Sally Dunaway Young, PT, DPT
Physical Therapist
and Clinical Research
Evaluator/Manager
Stanford University School
of Medicine
Stanford, CA

Click here to read.
Supplement Faculty
Perry Shieh, MD, PhD
Professor
Department of Neurology
David Geffen School
of Medicine at UCLA
Ronald Reagan UCLA
Medical Center
Los Angeles, CA
Sally Dunaway Young, PT, DPT
Physical Therapist
and Clinical Research
Evaluator/Manager
Stanford University School
of Medicine
Stanford, CA

Click here to read.
Supplement Faculty
Perry Shieh, MD, PhD
Professor
Department of Neurology
David Geffen School
of Medicine at UCLA
Ronald Reagan UCLA
Medical Center
Los Angeles, CA
Sally Dunaway Young, PT, DPT
Physical Therapist
and Clinical Research
Evaluator/Manager
Stanford University School
of Medicine
Stanford, CA
CGRPs in real world: Similar efficacy, more AEs
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
FROM AHS 2020
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
ID dermatology: Advancements, but new challenges, over 50 years
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”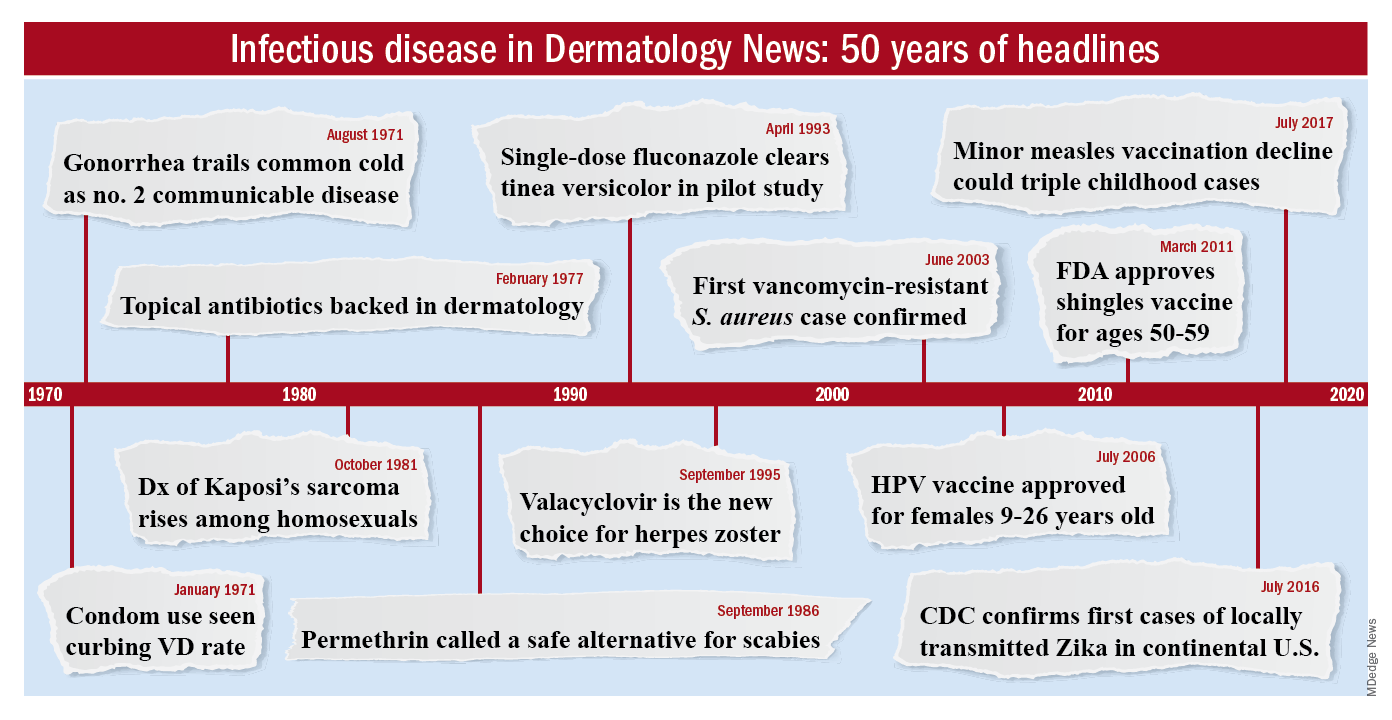
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”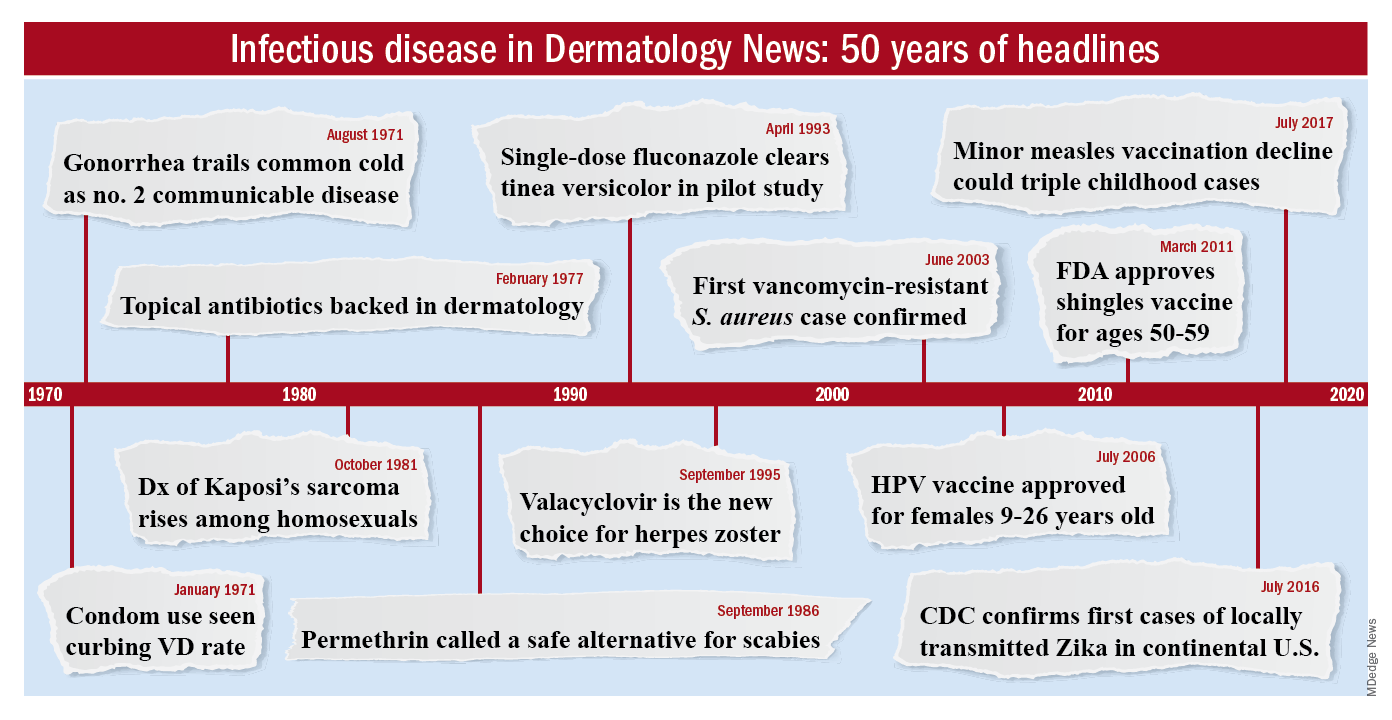
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”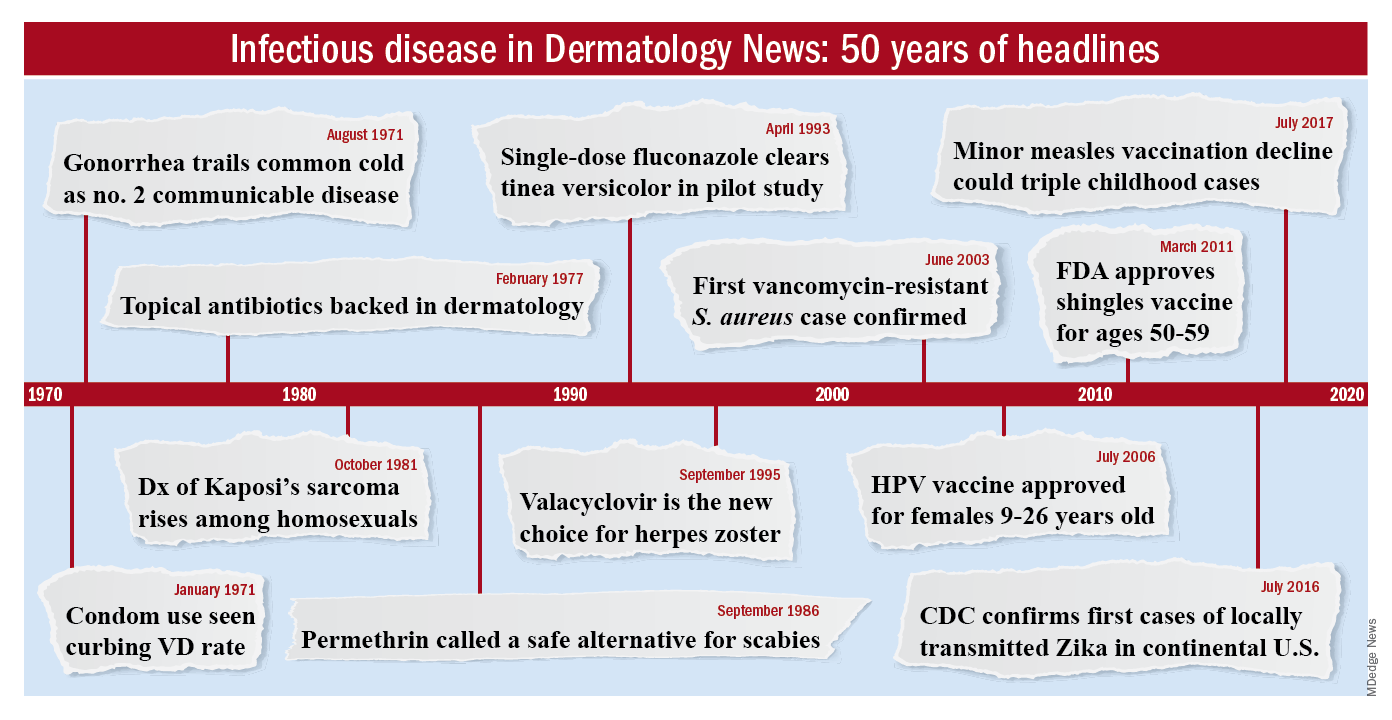
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
What presents as deep erythematous papules, pustules, and may form an annular or circular plaque?
Scrapings of the child’s rash were analyzed with potassium hydroxide (KOH) under microscopy which revealed multiple septate hyphae.
She was diagnosed with Majocchi’s granuloma. The fungal culture was positive for Trichophyton rubrum.
Majocchi’s granuloma (MG) is cutaneous mycosis in which the fungal infection goes deeper into the hair follicle causing granulomatous folliculitis and perifolliculitis.1 It was first described by Domenico Majocchi in 1883, and he named the condition “granuloma tricofitico.”2
It is commonly caused by T. rubrum but also can be caused by T. mentagrophytes, T. tonsurans, T. verrucosum, Microsporum canis, and Epidermophyton floccosum.2,3 Patients at risk for developing this infection include those previously treated with topical corticosteroids, immunosuppressed patients, patients with areas under occlusion, and those with areas traumatized by shaving. This infection is most commonly seen in the lower extremities, but can happen anywhere in the body. The lesions present as deep erythematous papules, pustules, and may form an annular or circular plaque as seen on our patient.
A KOH test of skin scrapings and hair extractions often can reveal fungal hyphae. Identification of the pathogen can be performed with culture or polymerase chain reaction of skin samples. If the diagnosis is uncertain or the KOH is negative, a skin biopsy can be performed. Histopathologic examination reveals perifollicular granulomas with associated dermal abscesses. Giant cells may be observed. MG is associated with chronic inflammation with lymphocytes, macrophages, epithelioid cells, and scattered multinucleated giant cells.2,3
The differential diagnosis for these lesions in children includes other granulomatous conditions such as granulomatous rosacea, sarcoidosis, and granuloma faciale, as well as bacterial or atypical mycobacterial infections, cutaneous leishmaniasis, and eosinophilic pustular folliculitis.
Treatment of MG requires systemic treatment with griseofulvin, itraconazole, or terbinafine for at least 4-8 weeks or until all the lesions have resolved. Our patient was treated with 6 weeks of high-dose griseofulvin with resolution of her lesions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Dermatol Online J. 2018 Dec 15;24(12):13030/qt89k4t6wj.
2. Med Mycol. 2012 Jul;50(5):449-57.
3. Clin Microbiol Rev. 2011 Apr;24(2):247-80.
Scrapings of the child’s rash were analyzed with potassium hydroxide (KOH) under microscopy which revealed multiple septate hyphae.
She was diagnosed with Majocchi’s granuloma. The fungal culture was positive for Trichophyton rubrum.
Majocchi’s granuloma (MG) is cutaneous mycosis in which the fungal infection goes deeper into the hair follicle causing granulomatous folliculitis and perifolliculitis.1 It was first described by Domenico Majocchi in 1883, and he named the condition “granuloma tricofitico.”2
It is commonly caused by T. rubrum but also can be caused by T. mentagrophytes, T. tonsurans, T. verrucosum, Microsporum canis, and Epidermophyton floccosum.2,3 Patients at risk for developing this infection include those previously treated with topical corticosteroids, immunosuppressed patients, patients with areas under occlusion, and those with areas traumatized by shaving. This infection is most commonly seen in the lower extremities, but can happen anywhere in the body. The lesions present as deep erythematous papules, pustules, and may form an annular or circular plaque as seen on our patient.
A KOH test of skin scrapings and hair extractions often can reveal fungal hyphae. Identification of the pathogen can be performed with culture or polymerase chain reaction of skin samples. If the diagnosis is uncertain or the KOH is negative, a skin biopsy can be performed. Histopathologic examination reveals perifollicular granulomas with associated dermal abscesses. Giant cells may be observed. MG is associated with chronic inflammation with lymphocytes, macrophages, epithelioid cells, and scattered multinucleated giant cells.2,3
The differential diagnosis for these lesions in children includes other granulomatous conditions such as granulomatous rosacea, sarcoidosis, and granuloma faciale, as well as bacterial or atypical mycobacterial infections, cutaneous leishmaniasis, and eosinophilic pustular folliculitis.
Treatment of MG requires systemic treatment with griseofulvin, itraconazole, or terbinafine for at least 4-8 weeks or until all the lesions have resolved. Our patient was treated with 6 weeks of high-dose griseofulvin with resolution of her lesions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Dermatol Online J. 2018 Dec 15;24(12):13030/qt89k4t6wj.
2. Med Mycol. 2012 Jul;50(5):449-57.
3. Clin Microbiol Rev. 2011 Apr;24(2):247-80.
Scrapings of the child’s rash were analyzed with potassium hydroxide (KOH) under microscopy which revealed multiple septate hyphae.
She was diagnosed with Majocchi’s granuloma. The fungal culture was positive for Trichophyton rubrum.
Majocchi’s granuloma (MG) is cutaneous mycosis in which the fungal infection goes deeper into the hair follicle causing granulomatous folliculitis and perifolliculitis.1 It was first described by Domenico Majocchi in 1883, and he named the condition “granuloma tricofitico.”2
It is commonly caused by T. rubrum but also can be caused by T. mentagrophytes, T. tonsurans, T. verrucosum, Microsporum canis, and Epidermophyton floccosum.2,3 Patients at risk for developing this infection include those previously treated with topical corticosteroids, immunosuppressed patients, patients with areas under occlusion, and those with areas traumatized by shaving. This infection is most commonly seen in the lower extremities, but can happen anywhere in the body. The lesions present as deep erythematous papules, pustules, and may form an annular or circular plaque as seen on our patient.
A KOH test of skin scrapings and hair extractions often can reveal fungal hyphae. Identification of the pathogen can be performed with culture or polymerase chain reaction of skin samples. If the diagnosis is uncertain or the KOH is negative, a skin biopsy can be performed. Histopathologic examination reveals perifollicular granulomas with associated dermal abscesses. Giant cells may be observed. MG is associated with chronic inflammation with lymphocytes, macrophages, epithelioid cells, and scattered multinucleated giant cells.2,3
The differential diagnosis for these lesions in children includes other granulomatous conditions such as granulomatous rosacea, sarcoidosis, and granuloma faciale, as well as bacterial or atypical mycobacterial infections, cutaneous leishmaniasis, and eosinophilic pustular folliculitis.
Treatment of MG requires systemic treatment with griseofulvin, itraconazole, or terbinafine for at least 4-8 weeks or until all the lesions have resolved. Our patient was treated with 6 weeks of high-dose griseofulvin with resolution of her lesions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. Dermatol Online J. 2018 Dec 15;24(12):13030/qt89k4t6wj.
2. Med Mycol. 2012 Jul;50(5):449-57.
3. Clin Microbiol Rev. 2011 Apr;24(2):247-80.
A 3-year-old girl with a known history of eczema presented to our dermatology clinic for evaluation of a persistent rash for about a year on the right cheek.
The mother reported she was treating the lesions with hydrocortisone cream 2.5% as instructed previously for her eczema. Initially the rash got partially better but then started getting worse again. The area was itchy.
The child was later seen in the emergency department, where she was recommended to treat the area with a combination cream of terbinafine 1% and betamethasone dipropionate 0.05%. The mother applied this cream as instructed for 3 weeks with some improvement of the lesions on the cheek.
A few weeks later, pimples started coming back. The mother tried the medication again but this time it was not helpful and the rash continued to expand.
The mother reported having a rash on her hand months back, which she successfully treated with the combination cream provided at the emergency department. They have no pets at home.
The child has a little sister who also has mild eczema.
She goes to day care and dances ballet.
VERTIS-CV: Ertugliflozin’s CV outcomes trial confirms SGLT2i benefits
The cardiovascular outcome trial results for a fourth sodium-glucose cotransporter 2 (SGLT2) inhibitor, ertugliflozin, were most notable for their consistency with the four prior, similar trials run on the three other drugs from this class on the U.S. market, canagliflozin, dapagliflozin, and empagliflozin, further solidifying the important role this drug class has recently taken on for patients with type 2 diabetes.
But the ertugliflozin results, which showed statistically significant superiority to placebo for just one endpoint, hospitalization for heart failure, made it unclear whether clinicians will regard ertugliflozin as the top agent from this class to prescribe.
“Our big takeaway is that the findings are consistent with what’s been seen in the other studies” of cardiovascular and renal outcomes in the EMPA-REG OUTCOME study of empagliflozin (N Engl J Med. 2015 Nov 26;373[22]:2117-28 ), the CANVAS (N Engl J Med. 2017 Aug 17;377[7]:644-57) and CREDENCE (N Engl J Med. 2019 June 13;380[24]:2295-306 ) studies of canagliflozin, and the DECLARE-TIMI 58 trial with dapagliflozin (N Engl J Med. 2019 Jan 24;380[4]:347-57), Christopher P. Cannon, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
The cardiovascular outcome trials (CVOTs), mandated in 2008 by Food and Drug Administration guidance for type 2 diabetes drugs that is now in the process of undergoing an update, have had the main goal of proving safety, and the primary endpoint of the new ertugliflozin trial, VERTIS-CV, was noninferiority to placebo when used on top of standard type 2 diabetes medications for the combined endpoint of cardiovascular death, nonfatal MI, or nonfatal stroke.
Key findings
Both of the tested dosages of ertugliflozin, 5 mg and 15 mg daily, met this endpoint, with event rates over a median 3.0 years of follow-up that ran very close to the placebo rate, clearly proving noninferiority. But the results showed no suggestion of superiority in a study that randomized 5,499 patients to either of the ertugliflozin regimens and 2,747 to placebo, reported Dr. Cannon, a cardiologist and professor of medicine at Harvard Medical School, Boston.
The primary outcome also showed similar event rates for each component of the composite endpoint, and subgroup analysis showed consistent results from ertugliflozin, compared with placebo, regardless of study-cohort subdivision by demographic, clinical, or treatment factors.
The trial design called for a hierarchical sequence of secondary-outcome superiority analyses, starting with the impact of ertugliflozin on cardiovascular death or heart failure hospitalization, and for this outcome ertugliflozin showed a point estimate of a 12% relative risk reduction, compared with placebo-treated patients, but this difference was not statistically significant. This meant that all subsequent superiority analyses in this trial could only be hypothesis generating and not definitive.
This negated the statistical validity of the only statistically significant treatment difference between ertugliflozin and placebo seen in VERTIS-CV, for the outcome of hospitalization for heart failure, where ertugliflozin treatment cut this outcome by 30%, compared with placebo patients. The rate of cardiovascular death alone, as well as a renal composite endpoint each showed no statistically significant benefit of ertugliflozin, compared with placebo, although the renal endpoint came close, with ertugliflozin reducing the combined rate of renal death, need for dialysis, need for renal transplant, or a doubling of serum creatinine from baseline by 19%, compared with placebo (P = .08).
How results compare with prior CVOTs
In some ways, these results seemed to contrast with outcomes from the CVOTs for the other SGLT2 inhibitors, which all showed at least two statistically significant benefits for major endpoints when compared with placebo.
As summarized in a new meta-analysis of all the CVOTs by Darren K. McGuire, MD, a cardiologist and professor of medicine at the University of Texas, Dallas, both empagliflozin and canagliflozin showed statistically significant superiority compared with placebo for their trial’s primary, combined major cardiovascular adverse event endpoint, but dapagliflozin and ertugliflozin did not. Empagliflozin was the sole SGLT2 inhibitor to show a statistically significant cut in cardiovascular deaths, compared with placebo.
The primary, composite renal efficacy endpoints used in these trials were hardest to compare because they differed from study to study, but unlike ertugliflozin, all the other three drugs in the class showed a statistically significant improvement, compared with placebo, for their respective renal outcomes. On the other hand, the pattern of estimated glomerular filtration rates measured at multiple times during the various trials showed a high level of consistency across the CVOTs.
The greatest consistently among the major endpoints across the trials was for heart failure hospitalization. All four agents showed statistically significant improvements, compared with placebo, and all four had roughly equal magnitudes of effect, a cut in event rates by about one-third.
“The greatest magnitude of benefit is for reductions in heart failure hospitalizations and for renal outcomes,” with the heart failure outcomes the “most consistent” across the studies and the renal outcomes “largely consistent,” concluded Dr. McGuire. All together, the five CVOTs for these four SGLT2 inhibitors involved more than 46,000 patients.
“A lot of data suggest these are all class effects,” that are roughly similar across all four of these SGLT2 inhibitors, commented Mark E. Cooper, MBBS, a professor and head of the department of diabetes at Monash University, Melbourne, and designated discussant for the study.
There was “clear homogeneity” between the VERTIS-CV results for hospitalization for heart failure and the other CVOTs, he noted. “I think there is a difference” in the cardiovascular death outcomes, specifically the sole statistically significant, 38% relative risk reduction with empagliflozin that stood out from the other CVOTs, but this difference is “totally unexplained,” added Dr. Cooper. “To really determine differences you’d need head-to-head studies that are unlikely to happen.”
The results of new SGLT2 inhibitor meta-analysis appeared to also “support contemporary society recommendations to prioritize the use of SGLT2 inhibitors independent of glucose-control considerations in patients with type 2 diabetes with or at high risk for cardiovascular and renal complications,” said Dr. McGuire.
“The guidelines have it right. Now it’s on us to implement these treatments to appropriate patients,” concluded Dr. Cannon.
Study details
VERTIS-CV (Cardiovascular Outcomes Following Ertugliflozin Treatment in Type 2 Diabetes Mellitus Participants With Vascular Disease) enrolled and followed patients with type 2 diabetes and established atherosclerotic cardiovascular disease at 531 centers in 34 countries during December 2013–December 2019. Other effects from ertugliflozin recorded during the trial were consistent with prior studies of the drug, which is already FDA approved for glycemic control: Compared with placebo, ertugliflozin treatment reduced hemoglobin A1c by an average of 0.5% after 1 year, cut average body weight by about 2.5 kg after 1 year with additional modest weight loss, during subsequent years on the drug, and reduced systolic blood pressure by about 3 mm Hg after 1 year.
The drug’s safety profile was generally reassuring and consistent with prior studies of this drug and others in the class, with overall no increase in total adverse events or serious adverse events, compared with placebo, and modestly increased rates of urinary tract and mycotic genital infections.
VERTIS-CV was sponsored by Merck and Pfizer, the companies that market ertugliflozin (Steglatro). Dr. Cannon has received research funding and fees from Merck and Pfizer and from several other companies. Dr. McGuire has received honoraria from Merck, has been a consultant to Pfizer, and has had similar relationships with several other companies. Dr. Cooper has been an advisor to and received honoraria from Merck. He has also received honoraria from or been an adviser to AstraZeneca, Boehringer Ingelheim, Lilly, MundiPharma, Novartis, Reata, and Servier, and he has received research funding from Boehringer Ingelheim and Novo Nordisk.
The cardiovascular outcome trial results for a fourth sodium-glucose cotransporter 2 (SGLT2) inhibitor, ertugliflozin, were most notable for their consistency with the four prior, similar trials run on the three other drugs from this class on the U.S. market, canagliflozin, dapagliflozin, and empagliflozin, further solidifying the important role this drug class has recently taken on for patients with type 2 diabetes.
But the ertugliflozin results, which showed statistically significant superiority to placebo for just one endpoint, hospitalization for heart failure, made it unclear whether clinicians will regard ertugliflozin as the top agent from this class to prescribe.
“Our big takeaway is that the findings are consistent with what’s been seen in the other studies” of cardiovascular and renal outcomes in the EMPA-REG OUTCOME study of empagliflozin (N Engl J Med. 2015 Nov 26;373[22]:2117-28 ), the CANVAS (N Engl J Med. 2017 Aug 17;377[7]:644-57) and CREDENCE (N Engl J Med. 2019 June 13;380[24]:2295-306 ) studies of canagliflozin, and the DECLARE-TIMI 58 trial with dapagliflozin (N Engl J Med. 2019 Jan 24;380[4]:347-57), Christopher P. Cannon, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
The cardiovascular outcome trials (CVOTs), mandated in 2008 by Food and Drug Administration guidance for type 2 diabetes drugs that is now in the process of undergoing an update, have had the main goal of proving safety, and the primary endpoint of the new ertugliflozin trial, VERTIS-CV, was noninferiority to placebo when used on top of standard type 2 diabetes medications for the combined endpoint of cardiovascular death, nonfatal MI, or nonfatal stroke.
Key findings
Both of the tested dosages of ertugliflozin, 5 mg and 15 mg daily, met this endpoint, with event rates over a median 3.0 years of follow-up that ran very close to the placebo rate, clearly proving noninferiority. But the results showed no suggestion of superiority in a study that randomized 5,499 patients to either of the ertugliflozin regimens and 2,747 to placebo, reported Dr. Cannon, a cardiologist and professor of medicine at Harvard Medical School, Boston.
The primary outcome also showed similar event rates for each component of the composite endpoint, and subgroup analysis showed consistent results from ertugliflozin, compared with placebo, regardless of study-cohort subdivision by demographic, clinical, or treatment factors.
The trial design called for a hierarchical sequence of secondary-outcome superiority analyses, starting with the impact of ertugliflozin on cardiovascular death or heart failure hospitalization, and for this outcome ertugliflozin showed a point estimate of a 12% relative risk reduction, compared with placebo-treated patients, but this difference was not statistically significant. This meant that all subsequent superiority analyses in this trial could only be hypothesis generating and not definitive.
This negated the statistical validity of the only statistically significant treatment difference between ertugliflozin and placebo seen in VERTIS-CV, for the outcome of hospitalization for heart failure, where ertugliflozin treatment cut this outcome by 30%, compared with placebo patients. The rate of cardiovascular death alone, as well as a renal composite endpoint each showed no statistically significant benefit of ertugliflozin, compared with placebo, although the renal endpoint came close, with ertugliflozin reducing the combined rate of renal death, need for dialysis, need for renal transplant, or a doubling of serum creatinine from baseline by 19%, compared with placebo (P = .08).
How results compare with prior CVOTs
In some ways, these results seemed to contrast with outcomes from the CVOTs for the other SGLT2 inhibitors, which all showed at least two statistically significant benefits for major endpoints when compared with placebo.
As summarized in a new meta-analysis of all the CVOTs by Darren K. McGuire, MD, a cardiologist and professor of medicine at the University of Texas, Dallas, both empagliflozin and canagliflozin showed statistically significant superiority compared with placebo for their trial’s primary, combined major cardiovascular adverse event endpoint, but dapagliflozin and ertugliflozin did not. Empagliflozin was the sole SGLT2 inhibitor to show a statistically significant cut in cardiovascular deaths, compared with placebo.
The primary, composite renal efficacy endpoints used in these trials were hardest to compare because they differed from study to study, but unlike ertugliflozin, all the other three drugs in the class showed a statistically significant improvement, compared with placebo, for their respective renal outcomes. On the other hand, the pattern of estimated glomerular filtration rates measured at multiple times during the various trials showed a high level of consistency across the CVOTs.
The greatest consistently among the major endpoints across the trials was for heart failure hospitalization. All four agents showed statistically significant improvements, compared with placebo, and all four had roughly equal magnitudes of effect, a cut in event rates by about one-third.
“The greatest magnitude of benefit is for reductions in heart failure hospitalizations and for renal outcomes,” with the heart failure outcomes the “most consistent” across the studies and the renal outcomes “largely consistent,” concluded Dr. McGuire. All together, the five CVOTs for these four SGLT2 inhibitors involved more than 46,000 patients.
“A lot of data suggest these are all class effects,” that are roughly similar across all four of these SGLT2 inhibitors, commented Mark E. Cooper, MBBS, a professor and head of the department of diabetes at Monash University, Melbourne, and designated discussant for the study.
There was “clear homogeneity” between the VERTIS-CV results for hospitalization for heart failure and the other CVOTs, he noted. “I think there is a difference” in the cardiovascular death outcomes, specifically the sole statistically significant, 38% relative risk reduction with empagliflozin that stood out from the other CVOTs, but this difference is “totally unexplained,” added Dr. Cooper. “To really determine differences you’d need head-to-head studies that are unlikely to happen.”
The results of new SGLT2 inhibitor meta-analysis appeared to also “support contemporary society recommendations to prioritize the use of SGLT2 inhibitors independent of glucose-control considerations in patients with type 2 diabetes with or at high risk for cardiovascular and renal complications,” said Dr. McGuire.
“The guidelines have it right. Now it’s on us to implement these treatments to appropriate patients,” concluded Dr. Cannon.
Study details
VERTIS-CV (Cardiovascular Outcomes Following Ertugliflozin Treatment in Type 2 Diabetes Mellitus Participants With Vascular Disease) enrolled and followed patients with type 2 diabetes and established atherosclerotic cardiovascular disease at 531 centers in 34 countries during December 2013–December 2019. Other effects from ertugliflozin recorded during the trial were consistent with prior studies of the drug, which is already FDA approved for glycemic control: Compared with placebo, ertugliflozin treatment reduced hemoglobin A1c by an average of 0.5% after 1 year, cut average body weight by about 2.5 kg after 1 year with additional modest weight loss, during subsequent years on the drug, and reduced systolic blood pressure by about 3 mm Hg after 1 year.
The drug’s safety profile was generally reassuring and consistent with prior studies of this drug and others in the class, with overall no increase in total adverse events or serious adverse events, compared with placebo, and modestly increased rates of urinary tract and mycotic genital infections.
VERTIS-CV was sponsored by Merck and Pfizer, the companies that market ertugliflozin (Steglatro). Dr. Cannon has received research funding and fees from Merck and Pfizer and from several other companies. Dr. McGuire has received honoraria from Merck, has been a consultant to Pfizer, and has had similar relationships with several other companies. Dr. Cooper has been an advisor to and received honoraria from Merck. He has also received honoraria from or been an adviser to AstraZeneca, Boehringer Ingelheim, Lilly, MundiPharma, Novartis, Reata, and Servier, and he has received research funding from Boehringer Ingelheim and Novo Nordisk.
The cardiovascular outcome trial results for a fourth sodium-glucose cotransporter 2 (SGLT2) inhibitor, ertugliflozin, were most notable for their consistency with the four prior, similar trials run on the three other drugs from this class on the U.S. market, canagliflozin, dapagliflozin, and empagliflozin, further solidifying the important role this drug class has recently taken on for patients with type 2 diabetes.
But the ertugliflozin results, which showed statistically significant superiority to placebo for just one endpoint, hospitalization for heart failure, made it unclear whether clinicians will regard ertugliflozin as the top agent from this class to prescribe.
“Our big takeaway is that the findings are consistent with what’s been seen in the other studies” of cardiovascular and renal outcomes in the EMPA-REG OUTCOME study of empagliflozin (N Engl J Med. 2015 Nov 26;373[22]:2117-28 ), the CANVAS (N Engl J Med. 2017 Aug 17;377[7]:644-57) and CREDENCE (N Engl J Med. 2019 June 13;380[24]:2295-306 ) studies of canagliflozin, and the DECLARE-TIMI 58 trial with dapagliflozin (N Engl J Med. 2019 Jan 24;380[4]:347-57), Christopher P. Cannon, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
The cardiovascular outcome trials (CVOTs), mandated in 2008 by Food and Drug Administration guidance for type 2 diabetes drugs that is now in the process of undergoing an update, have had the main goal of proving safety, and the primary endpoint of the new ertugliflozin trial, VERTIS-CV, was noninferiority to placebo when used on top of standard type 2 diabetes medications for the combined endpoint of cardiovascular death, nonfatal MI, or nonfatal stroke.
Key findings
Both of the tested dosages of ertugliflozin, 5 mg and 15 mg daily, met this endpoint, with event rates over a median 3.0 years of follow-up that ran very close to the placebo rate, clearly proving noninferiority. But the results showed no suggestion of superiority in a study that randomized 5,499 patients to either of the ertugliflozin regimens and 2,747 to placebo, reported Dr. Cannon, a cardiologist and professor of medicine at Harvard Medical School, Boston.
The primary outcome also showed similar event rates for each component of the composite endpoint, and subgroup analysis showed consistent results from ertugliflozin, compared with placebo, regardless of study-cohort subdivision by demographic, clinical, or treatment factors.
The trial design called for a hierarchical sequence of secondary-outcome superiority analyses, starting with the impact of ertugliflozin on cardiovascular death or heart failure hospitalization, and for this outcome ertugliflozin showed a point estimate of a 12% relative risk reduction, compared with placebo-treated patients, but this difference was not statistically significant. This meant that all subsequent superiority analyses in this trial could only be hypothesis generating and not definitive.
This negated the statistical validity of the only statistically significant treatment difference between ertugliflozin and placebo seen in VERTIS-CV, for the outcome of hospitalization for heart failure, where ertugliflozin treatment cut this outcome by 30%, compared with placebo patients. The rate of cardiovascular death alone, as well as a renal composite endpoint each showed no statistically significant benefit of ertugliflozin, compared with placebo, although the renal endpoint came close, with ertugliflozin reducing the combined rate of renal death, need for dialysis, need for renal transplant, or a doubling of serum creatinine from baseline by 19%, compared with placebo (P = .08).
How results compare with prior CVOTs
In some ways, these results seemed to contrast with outcomes from the CVOTs for the other SGLT2 inhibitors, which all showed at least two statistically significant benefits for major endpoints when compared with placebo.
As summarized in a new meta-analysis of all the CVOTs by Darren K. McGuire, MD, a cardiologist and professor of medicine at the University of Texas, Dallas, both empagliflozin and canagliflozin showed statistically significant superiority compared with placebo for their trial’s primary, combined major cardiovascular adverse event endpoint, but dapagliflozin and ertugliflozin did not. Empagliflozin was the sole SGLT2 inhibitor to show a statistically significant cut in cardiovascular deaths, compared with placebo.
The primary, composite renal efficacy endpoints used in these trials were hardest to compare because they differed from study to study, but unlike ertugliflozin, all the other three drugs in the class showed a statistically significant improvement, compared with placebo, for their respective renal outcomes. On the other hand, the pattern of estimated glomerular filtration rates measured at multiple times during the various trials showed a high level of consistency across the CVOTs.
The greatest consistently among the major endpoints across the trials was for heart failure hospitalization. All four agents showed statistically significant improvements, compared with placebo, and all four had roughly equal magnitudes of effect, a cut in event rates by about one-third.
“The greatest magnitude of benefit is for reductions in heart failure hospitalizations and for renal outcomes,” with the heart failure outcomes the “most consistent” across the studies and the renal outcomes “largely consistent,” concluded Dr. McGuire. All together, the five CVOTs for these four SGLT2 inhibitors involved more than 46,000 patients.
“A lot of data suggest these are all class effects,” that are roughly similar across all four of these SGLT2 inhibitors, commented Mark E. Cooper, MBBS, a professor and head of the department of diabetes at Monash University, Melbourne, and designated discussant for the study.
There was “clear homogeneity” between the VERTIS-CV results for hospitalization for heart failure and the other CVOTs, he noted. “I think there is a difference” in the cardiovascular death outcomes, specifically the sole statistically significant, 38% relative risk reduction with empagliflozin that stood out from the other CVOTs, but this difference is “totally unexplained,” added Dr. Cooper. “To really determine differences you’d need head-to-head studies that are unlikely to happen.”
The results of new SGLT2 inhibitor meta-analysis appeared to also “support contemporary society recommendations to prioritize the use of SGLT2 inhibitors independent of glucose-control considerations in patients with type 2 diabetes with or at high risk for cardiovascular and renal complications,” said Dr. McGuire.
“The guidelines have it right. Now it’s on us to implement these treatments to appropriate patients,” concluded Dr. Cannon.
Study details
VERTIS-CV (Cardiovascular Outcomes Following Ertugliflozin Treatment in Type 2 Diabetes Mellitus Participants With Vascular Disease) enrolled and followed patients with type 2 diabetes and established atherosclerotic cardiovascular disease at 531 centers in 34 countries during December 2013–December 2019. Other effects from ertugliflozin recorded during the trial were consistent with prior studies of the drug, which is already FDA approved for glycemic control: Compared with placebo, ertugliflozin treatment reduced hemoglobin A1c by an average of 0.5% after 1 year, cut average body weight by about 2.5 kg after 1 year with additional modest weight loss, during subsequent years on the drug, and reduced systolic blood pressure by about 3 mm Hg after 1 year.
The drug’s safety profile was generally reassuring and consistent with prior studies of this drug and others in the class, with overall no increase in total adverse events or serious adverse events, compared with placebo, and modestly increased rates of urinary tract and mycotic genital infections.
VERTIS-CV was sponsored by Merck and Pfizer, the companies that market ertugliflozin (Steglatro). Dr. Cannon has received research funding and fees from Merck and Pfizer and from several other companies. Dr. McGuire has received honoraria from Merck, has been a consultant to Pfizer, and has had similar relationships with several other companies. Dr. Cooper has been an advisor to and received honoraria from Merck. He has also received honoraria from or been an adviser to AstraZeneca, Boehringer Ingelheim, Lilly, MundiPharma, Novartis, Reata, and Servier, and he has received research funding from Boehringer Ingelheim and Novo Nordisk.
FROM ADA 2020