User login
Minority-serving hospitals had similar survival after liver cancer surgery
Overall survival after liver cancer surgery was similar regardless of whether patients were treated at minority-serving hospitals or at hospitals with proportionally fewer African American or Hispanic patients, investigators have found.
“[T]reatment of racial minorities is largely restricted to a subset of hospitals, often referred to as minority-serving hospitals. We sought to examine whether racial and ethnic minorities with hepatocellular carcinoma receive their surgical care at minority-serving hospitals, and whether treatment at minority-serving hospitals is associated with differences in overall survival,” explained Winta T. Mehtsun, MD, MPH, of Dana-Farber Cancer Institute in Boston and associates in an abstract released as part of the annual Digestive Disease Week.®
Hepatocellular carcinoma continues to have a low 5-year survival rate and exhibits marked racial and ethnic disparities in diagnosis, treatment, and outcomes. In a recent study of Surveillance Epidemiology and End Results (SEER) data, African American patients with hepatocellular carcinoma were significantly younger at diagnosis, were more likely to have metastatic disease, and were less likely to receive surgical treatment compared with whites (Am J Prevent Med 2018;55:S40-48). Among patients with early-stage liver cancer, Hispanic and African American patients are less likely to receive curative therapy and die sooner, on average, than do other patients (Clin Gastroenterol Hepatol. 2019;17:551-9).
Minority-serving hospitals also have improved significantly less over time on measures of critical care, length of stay, and mortality, but whether these issues extend to hepatocellular carcinoma remains unclear. Therefore, Dr. Mehtsun and her associates studied all 2,609 patients in the National Cancer Database who received surgical resection (not transplantation or local therapy) for nonmetastatic hepatocellular carcinoma between 2004 and 2014. They compared survival at minority-serving hospitals – those in the top 10% based on the proportion of patients who were African American or Hispanic – with survival at other hospitals.
“There was no association between minority-serving hospital and overall survival,” the researchers reported (multivariable hazard ratio for death, 0.89; 95% confidence interval, 0.72-1.11). In contrast, survival was significantly shorter among patients with more advanced disease (HR, 2.5; 95% CI, 2.1-2.8), patients who were treated at a community cancer program (HR, 1.7; 95% CI, 1.3-2.4), and patients whose Charlson Comorbidity Index was greater than 2 (HR, 1.2; 95% CI, 1.1-1.4).
Stage at diagnosis, comorbidities, and sex were not significantly related to hospital type, the investigators noted. A total of 298 patients (11%) were treated at minority-serving hospitals. Patients treated at minority-serving hospitals were significantly more likely to be uninsured (11% vs. 4% at other hospitals) and significantly less likely to be treated at an academic center (55% vs. 69%; both P less than .001).
Dr. Mehtsun reported having no relevant conflicts of interest.
SOURCE: Mehtsun WT et al. DDW 2020, Abstract Tu2043.
Overall survival after liver cancer surgery was similar regardless of whether patients were treated at minority-serving hospitals or at hospitals with proportionally fewer African American or Hispanic patients, investigators have found.
“[T]reatment of racial minorities is largely restricted to a subset of hospitals, often referred to as minority-serving hospitals. We sought to examine whether racial and ethnic minorities with hepatocellular carcinoma receive their surgical care at minority-serving hospitals, and whether treatment at minority-serving hospitals is associated with differences in overall survival,” explained Winta T. Mehtsun, MD, MPH, of Dana-Farber Cancer Institute in Boston and associates in an abstract released as part of the annual Digestive Disease Week.®
Hepatocellular carcinoma continues to have a low 5-year survival rate and exhibits marked racial and ethnic disparities in diagnosis, treatment, and outcomes. In a recent study of Surveillance Epidemiology and End Results (SEER) data, African American patients with hepatocellular carcinoma were significantly younger at diagnosis, were more likely to have metastatic disease, and were less likely to receive surgical treatment compared with whites (Am J Prevent Med 2018;55:S40-48). Among patients with early-stage liver cancer, Hispanic and African American patients are less likely to receive curative therapy and die sooner, on average, than do other patients (Clin Gastroenterol Hepatol. 2019;17:551-9).
Minority-serving hospitals also have improved significantly less over time on measures of critical care, length of stay, and mortality, but whether these issues extend to hepatocellular carcinoma remains unclear. Therefore, Dr. Mehtsun and her associates studied all 2,609 patients in the National Cancer Database who received surgical resection (not transplantation or local therapy) for nonmetastatic hepatocellular carcinoma between 2004 and 2014. They compared survival at minority-serving hospitals – those in the top 10% based on the proportion of patients who were African American or Hispanic – with survival at other hospitals.
“There was no association between minority-serving hospital and overall survival,” the researchers reported (multivariable hazard ratio for death, 0.89; 95% confidence interval, 0.72-1.11). In contrast, survival was significantly shorter among patients with more advanced disease (HR, 2.5; 95% CI, 2.1-2.8), patients who were treated at a community cancer program (HR, 1.7; 95% CI, 1.3-2.4), and patients whose Charlson Comorbidity Index was greater than 2 (HR, 1.2; 95% CI, 1.1-1.4).
Stage at diagnosis, comorbidities, and sex were not significantly related to hospital type, the investigators noted. A total of 298 patients (11%) were treated at minority-serving hospitals. Patients treated at minority-serving hospitals were significantly more likely to be uninsured (11% vs. 4% at other hospitals) and significantly less likely to be treated at an academic center (55% vs. 69%; both P less than .001).
Dr. Mehtsun reported having no relevant conflicts of interest.
SOURCE: Mehtsun WT et al. DDW 2020, Abstract Tu2043.
Overall survival after liver cancer surgery was similar regardless of whether patients were treated at minority-serving hospitals or at hospitals with proportionally fewer African American or Hispanic patients, investigators have found.
“[T]reatment of racial minorities is largely restricted to a subset of hospitals, often referred to as minority-serving hospitals. We sought to examine whether racial and ethnic minorities with hepatocellular carcinoma receive their surgical care at minority-serving hospitals, and whether treatment at minority-serving hospitals is associated with differences in overall survival,” explained Winta T. Mehtsun, MD, MPH, of Dana-Farber Cancer Institute in Boston and associates in an abstract released as part of the annual Digestive Disease Week.®
Hepatocellular carcinoma continues to have a low 5-year survival rate and exhibits marked racial and ethnic disparities in diagnosis, treatment, and outcomes. In a recent study of Surveillance Epidemiology and End Results (SEER) data, African American patients with hepatocellular carcinoma were significantly younger at diagnosis, were more likely to have metastatic disease, and were less likely to receive surgical treatment compared with whites (Am J Prevent Med 2018;55:S40-48). Among patients with early-stage liver cancer, Hispanic and African American patients are less likely to receive curative therapy and die sooner, on average, than do other patients (Clin Gastroenterol Hepatol. 2019;17:551-9).
Minority-serving hospitals also have improved significantly less over time on measures of critical care, length of stay, and mortality, but whether these issues extend to hepatocellular carcinoma remains unclear. Therefore, Dr. Mehtsun and her associates studied all 2,609 patients in the National Cancer Database who received surgical resection (not transplantation or local therapy) for nonmetastatic hepatocellular carcinoma between 2004 and 2014. They compared survival at minority-serving hospitals – those in the top 10% based on the proportion of patients who were African American or Hispanic – with survival at other hospitals.
“There was no association between minority-serving hospital and overall survival,” the researchers reported (multivariable hazard ratio for death, 0.89; 95% confidence interval, 0.72-1.11). In contrast, survival was significantly shorter among patients with more advanced disease (HR, 2.5; 95% CI, 2.1-2.8), patients who were treated at a community cancer program (HR, 1.7; 95% CI, 1.3-2.4), and patients whose Charlson Comorbidity Index was greater than 2 (HR, 1.2; 95% CI, 1.1-1.4).
Stage at diagnosis, comorbidities, and sex were not significantly related to hospital type, the investigators noted. A total of 298 patients (11%) were treated at minority-serving hospitals. Patients treated at minority-serving hospitals were significantly more likely to be uninsured (11% vs. 4% at other hospitals) and significantly less likely to be treated at an academic center (55% vs. 69%; both P less than .001).
Dr. Mehtsun reported having no relevant conflicts of interest.
SOURCE: Mehtsun WT et al. DDW 2020, Abstract Tu2043.
FROM DDW 2020
Commonalities challenge the threshold of high-frequency episodic and low-frequency chronic migraine
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
FROM AHS 2020
The evolution of “COVIDists”
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).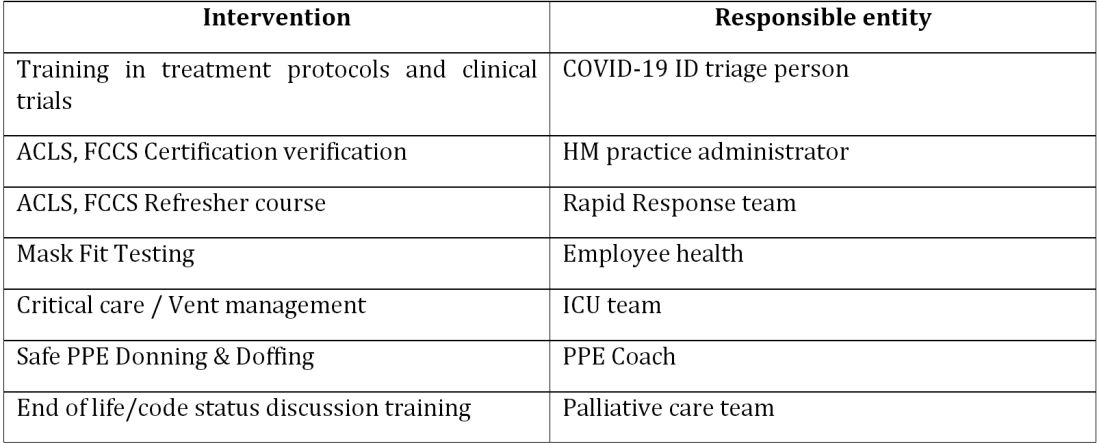
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).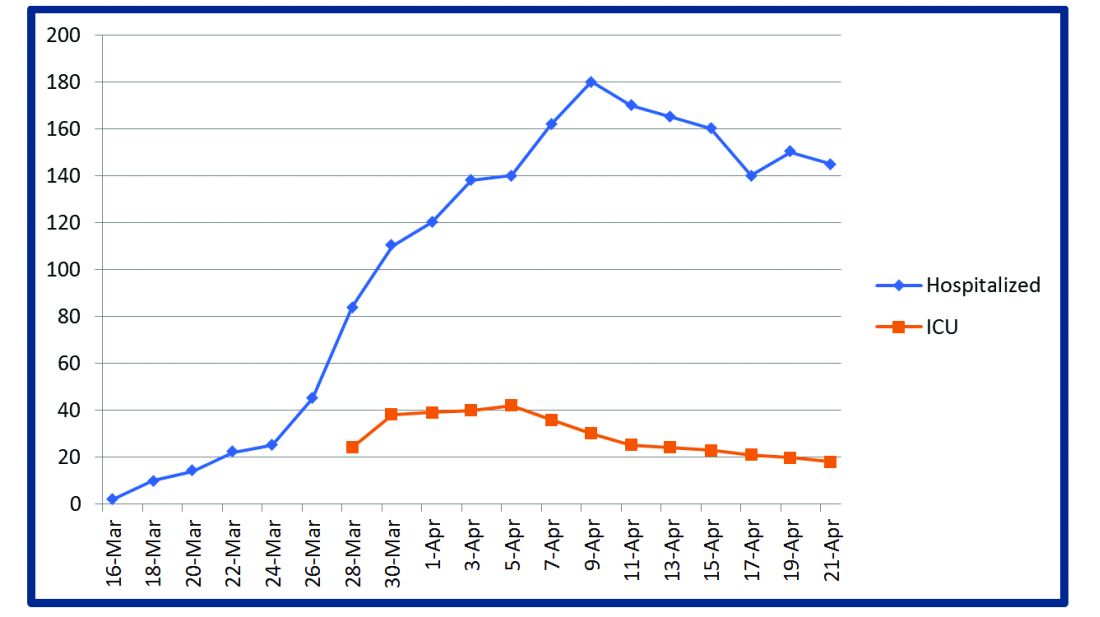
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU. 
The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at Venkatrao.MedarametlaMD@Baystatehealth.org. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
Adapting to the demands placed on hospital resources by COVID-19
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).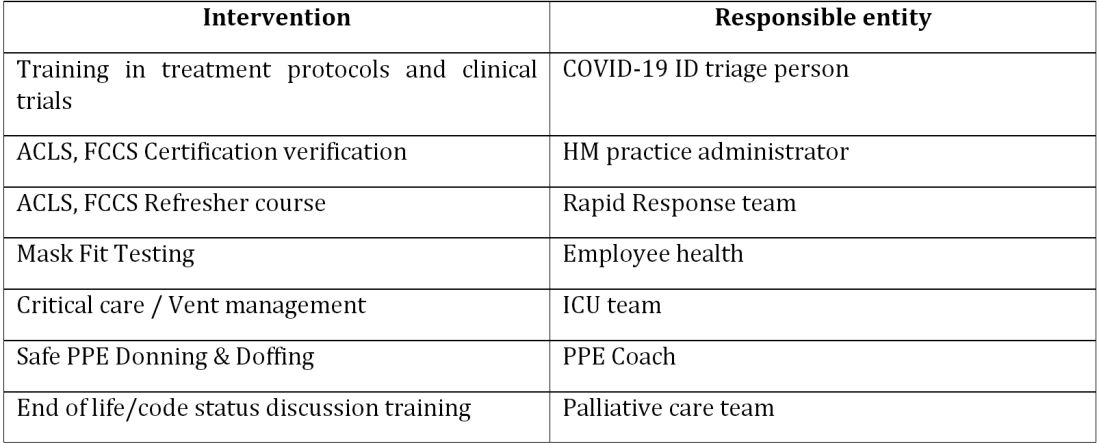
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).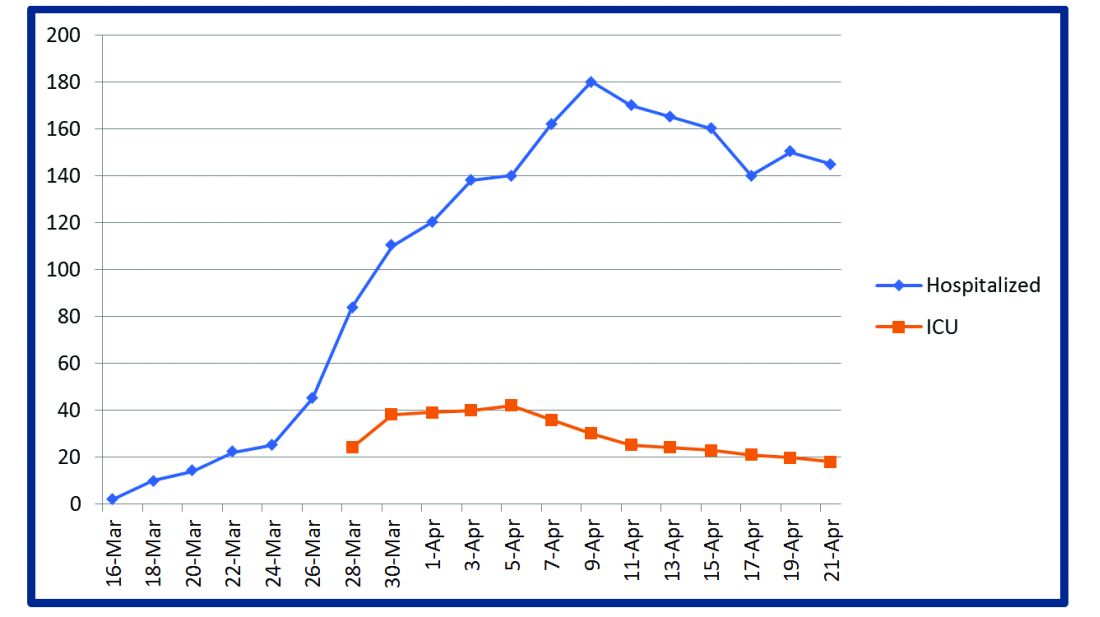
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU. 
The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at Venkatrao.MedarametlaMD@Baystatehealth.org. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).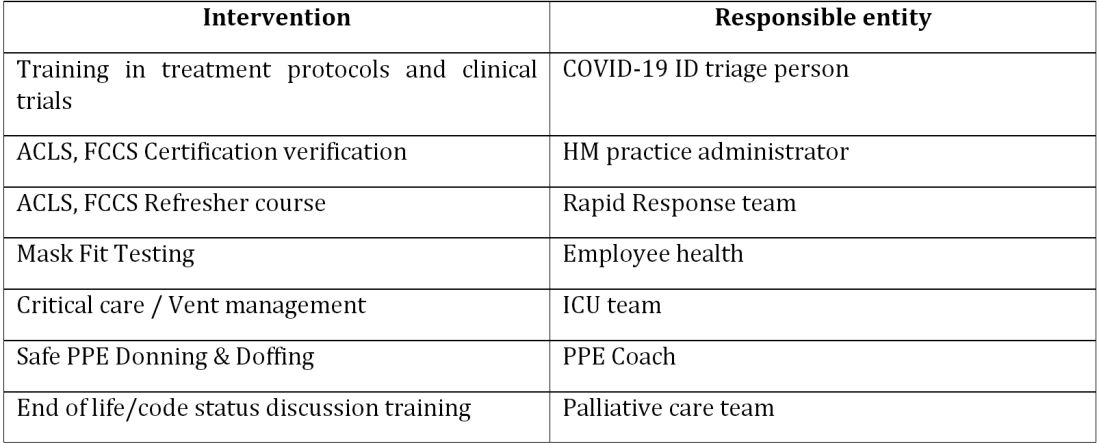
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).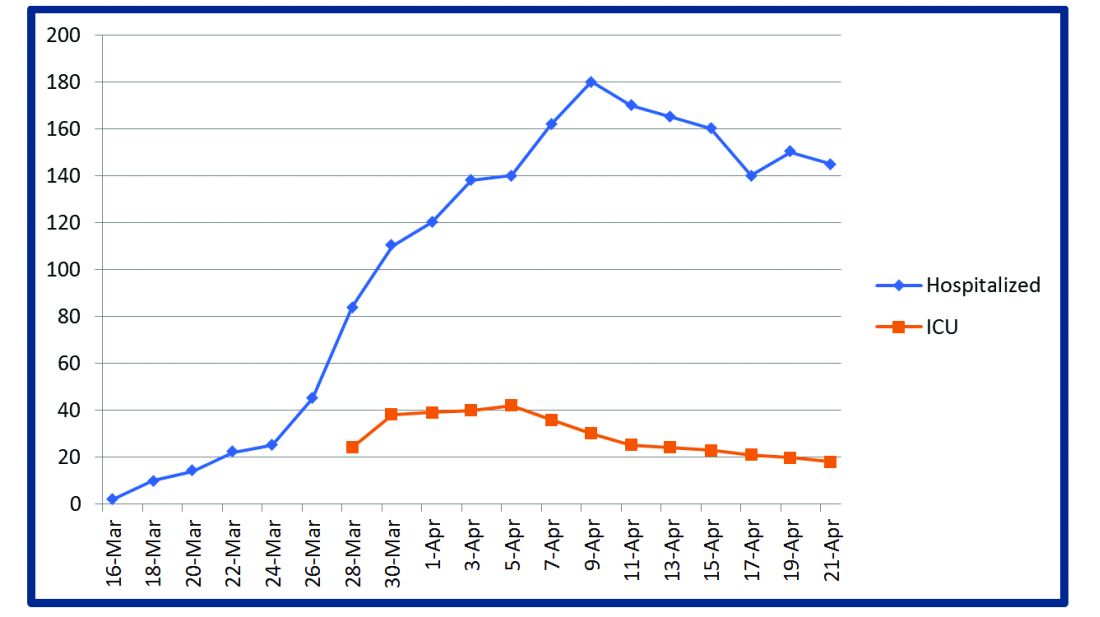
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU. 
The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at Venkatrao.MedarametlaMD@Baystatehealth.org. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
First-in-kind anti-CD47 antibody shows promise for MDS and AML treatment
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
FROM ASCO 2020
Daily Recap: Lung ultrasound helps diagnose COVID-19 in kids, first treatment approved for adult-onset Still’s disease
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
New health policy and advocacy committee (HPAC)
What a privilege it has been over the last several months to participate as staff support along with Jenny Nemkovich and Michelle Kosobucki to CHEST’s new Health Policy and Advocacy Committee (HPAC). The opportunity to serve on a committee of CHEST from the perspective of staff rather than in a volunteer/leadership role has been very enlightening and clearly a learning experience.
Background
As most know, CHEST in the summer of 2019 made the decision to proactively strengthen our position in the areas of public policy, both advocacy and the regulatory space.
This decision will provide CHEST with the mechanism to have greater control over determining and influencing the pulmonary, critical care, and sleep agenda that directly impacts our members and our patients. Adding this piece to the CHEST portfolio is particularly fortuitous in light of the increased advocacy needs in this COVID-19 environment. Having recently completed the acquisition of NAMDRC, CHEST has jump-started our return to this space. While this acquisition does not represent a single source solution, it does represent a key component to a comprehensive approach to policy and advocacy. The rich experience of our new colleagues from NAMDRC brings incredible value and insights to our efforts.
Health policy and advocacy committee
The initial composition of the HPAC is made up of equal numbers of members drawn from the NAMDRC leadership pool, as well as members of both the CHEST Foundation Board of Trustees and the Board of Regents of the College. This group represents a very energetic, talented, and diverse group. Experience in the space of policy and advocacy in areas such as home ventilation, oxygen issues, telemedicine, and pulmonary rehab reimbursement is blended with presidential leadership of both the CHEST Foundation and CHEST, as well as talent in areas such as coding and reimbursement, social media applications, and also leadership representing our NetWorks.
Policy priorities
Having had three virtual meetings, the HPAC has initially been focusing on developing and discussing an initial group of policy priorities. These topics are being vetted and held to a rigorous discussion, including what success looks like in these areas, potential barriers or obstacles to making an impact, and who could represent important collaborative partners in these areas. These priorities will be coupled with an effort to define short-term and longer term performance indicators to help try to assess meaningful impact. Once these are better defined, we plan to reach out to our CHEST NetWorks, partners in Industry, sister societies, and friends in patient advocacy groups to get their input and, when appropriate, their collaboration. The BOR will be kept informed and eventually comment and hopefully endorse these policy priorities.
Member engagement
In my opinion, our approach in this area of policy and advocacy is somewhat unique in the associational arena. Rather than policy staff driving the agenda, we are following the example of other committees at CHEST in having volunteers and leadership developing the “what” and staff creating the “how.” At that point, a team of leadership/staff will deliver the product. I feel that this somewhat “bottom up” approach will lead to much more productive and effective member engagement and a growing group of advocacy aware and committed members.
Washington watchline
To complement the work of HPAC and better communicate important issues related to policy and advocacy, our Publications team, led by Nicki Augustyn, has taken over the production of what was NAMDRC’s valuable periodical, the Washington Watchline. Under the editorship for many years of past CHEST President, Jim Mathers, MD, FCCP, this resource has been a valuable and respected source of information for NAMDRC membership. The June edition has recently been published.
Spring meeting, 2021
The HPAC’s Chair and Vice-Chair, Drs. Neil Freedman and Jim Lamberti, are serving as the Program Directors for our first meeting that will blend the NAMDRC perspective and experience in a program around policy and advocacy with the traditional expertise in education delivery of CHEST. This meeting will be in conjunction with our Spring Leadership meetings in Sonoma, California. Save the date, as this promises to be a great meeting, with unique educational opportunities and policy and advocacy insights.
Thanks again to the members of HPAC and to Bob Musacchio for giving me an opportunity to provide staff assistance in this exciting new endeavor for CHEST.
What a privilege it has been over the last several months to participate as staff support along with Jenny Nemkovich and Michelle Kosobucki to CHEST’s new Health Policy and Advocacy Committee (HPAC). The opportunity to serve on a committee of CHEST from the perspective of staff rather than in a volunteer/leadership role has been very enlightening and clearly a learning experience.
Background
As most know, CHEST in the summer of 2019 made the decision to proactively strengthen our position in the areas of public policy, both advocacy and the regulatory space.
This decision will provide CHEST with the mechanism to have greater control over determining and influencing the pulmonary, critical care, and sleep agenda that directly impacts our members and our patients. Adding this piece to the CHEST portfolio is particularly fortuitous in light of the increased advocacy needs in this COVID-19 environment. Having recently completed the acquisition of NAMDRC, CHEST has jump-started our return to this space. While this acquisition does not represent a single source solution, it does represent a key component to a comprehensive approach to policy and advocacy. The rich experience of our new colleagues from NAMDRC brings incredible value and insights to our efforts.
Health policy and advocacy committee
The initial composition of the HPAC is made up of equal numbers of members drawn from the NAMDRC leadership pool, as well as members of both the CHEST Foundation Board of Trustees and the Board of Regents of the College. This group represents a very energetic, talented, and diverse group. Experience in the space of policy and advocacy in areas such as home ventilation, oxygen issues, telemedicine, and pulmonary rehab reimbursement is blended with presidential leadership of both the CHEST Foundation and CHEST, as well as talent in areas such as coding and reimbursement, social media applications, and also leadership representing our NetWorks.
Policy priorities
Having had three virtual meetings, the HPAC has initially been focusing on developing and discussing an initial group of policy priorities. These topics are being vetted and held to a rigorous discussion, including what success looks like in these areas, potential barriers or obstacles to making an impact, and who could represent important collaborative partners in these areas. These priorities will be coupled with an effort to define short-term and longer term performance indicators to help try to assess meaningful impact. Once these are better defined, we plan to reach out to our CHEST NetWorks, partners in Industry, sister societies, and friends in patient advocacy groups to get their input and, when appropriate, their collaboration. The BOR will be kept informed and eventually comment and hopefully endorse these policy priorities.
Member engagement
In my opinion, our approach in this area of policy and advocacy is somewhat unique in the associational arena. Rather than policy staff driving the agenda, we are following the example of other committees at CHEST in having volunteers and leadership developing the “what” and staff creating the “how.” At that point, a team of leadership/staff will deliver the product. I feel that this somewhat “bottom up” approach will lead to much more productive and effective member engagement and a growing group of advocacy aware and committed members.
Washington watchline
To complement the work of HPAC and better communicate important issues related to policy and advocacy, our Publications team, led by Nicki Augustyn, has taken over the production of what was NAMDRC’s valuable periodical, the Washington Watchline. Under the editorship for many years of past CHEST President, Jim Mathers, MD, FCCP, this resource has been a valuable and respected source of information for NAMDRC membership. The June edition has recently been published.
Spring meeting, 2021
The HPAC’s Chair and Vice-Chair, Drs. Neil Freedman and Jim Lamberti, are serving as the Program Directors for our first meeting that will blend the NAMDRC perspective and experience in a program around policy and advocacy with the traditional expertise in education delivery of CHEST. This meeting will be in conjunction with our Spring Leadership meetings in Sonoma, California. Save the date, as this promises to be a great meeting, with unique educational opportunities and policy and advocacy insights.
Thanks again to the members of HPAC and to Bob Musacchio for giving me an opportunity to provide staff assistance in this exciting new endeavor for CHEST.
What a privilege it has been over the last several months to participate as staff support along with Jenny Nemkovich and Michelle Kosobucki to CHEST’s new Health Policy and Advocacy Committee (HPAC). The opportunity to serve on a committee of CHEST from the perspective of staff rather than in a volunteer/leadership role has been very enlightening and clearly a learning experience.
Background
As most know, CHEST in the summer of 2019 made the decision to proactively strengthen our position in the areas of public policy, both advocacy and the regulatory space.
This decision will provide CHEST with the mechanism to have greater control over determining and influencing the pulmonary, critical care, and sleep agenda that directly impacts our members and our patients. Adding this piece to the CHEST portfolio is particularly fortuitous in light of the increased advocacy needs in this COVID-19 environment. Having recently completed the acquisition of NAMDRC, CHEST has jump-started our return to this space. While this acquisition does not represent a single source solution, it does represent a key component to a comprehensive approach to policy and advocacy. The rich experience of our new colleagues from NAMDRC brings incredible value and insights to our efforts.
Health policy and advocacy committee
The initial composition of the HPAC is made up of equal numbers of members drawn from the NAMDRC leadership pool, as well as members of both the CHEST Foundation Board of Trustees and the Board of Regents of the College. This group represents a very energetic, talented, and diverse group. Experience in the space of policy and advocacy in areas such as home ventilation, oxygen issues, telemedicine, and pulmonary rehab reimbursement is blended with presidential leadership of both the CHEST Foundation and CHEST, as well as talent in areas such as coding and reimbursement, social media applications, and also leadership representing our NetWorks.
Policy priorities
Having had three virtual meetings, the HPAC has initially been focusing on developing and discussing an initial group of policy priorities. These topics are being vetted and held to a rigorous discussion, including what success looks like in these areas, potential barriers or obstacles to making an impact, and who could represent important collaborative partners in these areas. These priorities will be coupled with an effort to define short-term and longer term performance indicators to help try to assess meaningful impact. Once these are better defined, we plan to reach out to our CHEST NetWorks, partners in Industry, sister societies, and friends in patient advocacy groups to get their input and, when appropriate, their collaboration. The BOR will be kept informed and eventually comment and hopefully endorse these policy priorities.
Member engagement
In my opinion, our approach in this area of policy and advocacy is somewhat unique in the associational arena. Rather than policy staff driving the agenda, we are following the example of other committees at CHEST in having volunteers and leadership developing the “what” and staff creating the “how.” At that point, a team of leadership/staff will deliver the product. I feel that this somewhat “bottom up” approach will lead to much more productive and effective member engagement and a growing group of advocacy aware and committed members.
Washington watchline
To complement the work of HPAC and better communicate important issues related to policy and advocacy, our Publications team, led by Nicki Augustyn, has taken over the production of what was NAMDRC’s valuable periodical, the Washington Watchline. Under the editorship for many years of past CHEST President, Jim Mathers, MD, FCCP, this resource has been a valuable and respected source of information for NAMDRC membership. The June edition has recently been published.
Spring meeting, 2021
The HPAC’s Chair and Vice-Chair, Drs. Neil Freedman and Jim Lamberti, are serving as the Program Directors for our first meeting that will blend the NAMDRC perspective and experience in a program around policy and advocacy with the traditional expertise in education delivery of CHEST. This meeting will be in conjunction with our Spring Leadership meetings in Sonoma, California. Save the date, as this promises to be a great meeting, with unique educational opportunities and policy and advocacy insights.
Thanks again to the members of HPAC and to Bob Musacchio for giving me an opportunity to provide staff assistance in this exciting new endeavor for CHEST.
Virtual visits for patients with neuromuscular respiratory failure in the time of COVID-19: A potential bright spot from the pandemic
On March 17, 2020, I entered my patients electronic medical record and hit the “Connect with Zoom” button in her Epic (Epic Systems Corporation) chart. About 20 seconds later, the face of my 28-year-old patient with advanced spinal muscular atrophy type 2 (SMA-2) appeared virtually and not live for the first time since I had met her some 10 years previously. She appeared well and her history supported that. We spent most of the time reviewing recent events and surveying her home ventilation equipment. She felt well and sleep was of good quality. She was performing her normal activities without dyspnea. Her mechanical insufflator-exsufflator was working fine, although she used it only as needed, and she was performing lung volume recruitment maneuvers with a resuscitator bag three times a day with assistance. Her mask for nocturnal NPPV was getting old, and she showed me where the straps were fraying. We noted that her bilevel device was now 8 years old and that she needed a new one. We concluded our conversation in 20 minutes and she blurted out: “Wow, that was easy. Thanks, Dr. Benditt.” I got off the phone and put in the order for a new mask and bilevel device with our clinic respiratory therapist. She received the equipment 48 hours later and sent an electronic message through her chart to let me know it had arrived. A total of five in-person visits including me and other providers had been cancelled and replaced by virtual visits. She has made one visit to the hospital in the last 3 months for an intrathecal nusinersen (Spinraza) injection that was done with a COVID-19 prescreening and full PPE.
One week prior to our virtual visit, my university hospital had reduced in-person clinic visits to those deemed absolutely necessary due to the COVID-19 pandemic. Visits considered absolutely necessary included such patients as postoperative transplant visits and preoperative evaluations for urgent surgeries. All other patient visits were canceled with plans to reschedule them once the COVID-19 pandemic was controlled. As the breadth and depth of the pandemic became apparent, a very rapid ramp-up of “virtual visits” via telemedicine capacity was rolled out. I had not previously used telemedicine, and the learning curve was steep, although once in place, the technology was straightforward from the provider perspective. The telemedicine visits for our hospital for the entire year of 2019 totaled about 800. In the month of April of 2020 we engaged in 40,000 telemedicine visits. This explosive growth of telemedicine implementation has occurred around the country and world during the COVID-19 pandemic (Olayiwola JN, et al. JMIR Public Health Surveill. 2020, May 29. doi: 10.2196/19045). This recent growth of telemedicine in the US has been fueled by the need for social distancing and quarantine, the lack of universal testing and COVID-19 case tracking, and the realization by CMS that coverage of telemedicine services had to be expanded rapidly to allow for continued patient care in the setting of stay-at-home orders. A rapid role out of application technology support and online training classes for health-care providers was undertaken. Privileges for telemedicine virtual visits were approved when providers completed the informational online modules and set up their HIPPA compliant Zoom accounts (Zoom Video Communications, San Jose, CA). All of us had minor stumbles initially with the equipment, software, and getting the patients connected online. After four or five visits, the process started to click and has become rather routine. Many providers and patients found this quite a positive development in terms of patient-provider visits but a question arose almost immediately: “Will this continue to be supported by insurers and allow us to integrate this practice into our outpatient clinic setting once the pandemic was controlled?” Time with tell, but an opportunity has presented itself.
For patients with neuromuscular disease and respiratory failure, telemedicine is a technology that may be particularly attractive for a number of reasons. First, patients with neuromuscular respiratory failure are likely at a particularly high risk of death if they develop full-blown COVID-19 infection. Development of acute respiratory distress syndrome (ARDS) on top of underlying neuromuscular respiratory failure is likely to be particularly deadly, although, very fortunately, there are no published reports of widespread infections in patients with neuromuscular respiratory disease. We have known for many decades that pneumonia is the leading cause of death for these patients. Second, patients with neuromuscular respiratory failure often find it quite difficult to come to the hospital for clinic visits. Mobilizing equipment, caregivers, and transportation can take days to arrange. For this reason, many neuromuscular clinics provide a multidisciplinary/multi-provider half-day visit to reduce the need to come into the hospital for multiple separate visits. Lastly, there are relatively few respiratory health-care providers in the United States and around the world who focus on patients with neuromuscular respiratory disease. Many neuromuscular clinics and providers will, therefore, have a very wide patient catchment area. For instance, my practice, based in Seattle, Washington, includes patients from Alaska, Montana, Idaho, and Wyoming. In-person hospital visits more than once per year may be virtually impossible.
Telemedicine is a methodology that has long been considered helpful in the arena of home ventilation and, in fact, we have been using some telemedicine technologies for some time (Casavant DW, et al. J Telemed Telecare. 2014;20[8]:441). Telemedicine (telehealth) includes the use of electronic information and communications technologies to provide and support health care when distance separates the participants. For instance, monitoring of nocturnal ventilation via downloads from Internet-connected noninvasive or invasive ventilation devices, overnight oximetry, and even phone calls from durable medical equipment providers during a home visit would be considered telemedicine. Many of us have been using these methods for many years. It is really the face-to-face “virtual visit” frequency that the COVID-19 pandemic has accelerated. This is a crucial advance in the process of telehealth because we may be able to reduce visits to our clinics from once every 3 to 6 months to perhaps once per year if support for virtual visits by insurers continues and if home monitoring can expand to include accurate home measurement of patient CO2 levels by either end-tidal CO2, transcutaneous CO2, or point of care arterial or capillary blood gases, as well as home pulmonary function monitoring. Measurement of CO2 levels and pulmonary function has generally been done at the hospital or in the clinic although there is no reason that with home visit support from appropriate services (that might even include durable medical equipment companies) that this could not be accomplished. This is not to say that there are not hurdles to the application of telehealth in the neuromuscular disease and home ventilation population. Not all patients have the equipment or technology savvy to participate in virtual visits, and not all insurers cover these visits even now during COVID-19. However, I imagine a future where a significant number of visits for patients with neuromuscular respiratory disease and home ventilation needs could be performed virtually. I envision that this would reduce patient and home caregiver travel burdens, make more efficient use of health-care provider time, expand the number of patients that a neuromuscular respiratory disease practitioner could serve, and perhaps reduce health-care expenditures per patient. This may be a real health-care bright spot in the huge difficulties of COVID-19. Fingers crossed.
Dr. Benditt is Medical Director of Respiratory Care Services and Professor of Medicine, University of Washington Medical Center, Seattle, Washington.
On March 17, 2020, I entered my patients electronic medical record and hit the “Connect with Zoom” button in her Epic (Epic Systems Corporation) chart. About 20 seconds later, the face of my 28-year-old patient with advanced spinal muscular atrophy type 2 (SMA-2) appeared virtually and not live for the first time since I had met her some 10 years previously. She appeared well and her history supported that. We spent most of the time reviewing recent events and surveying her home ventilation equipment. She felt well and sleep was of good quality. She was performing her normal activities without dyspnea. Her mechanical insufflator-exsufflator was working fine, although she used it only as needed, and she was performing lung volume recruitment maneuvers with a resuscitator bag three times a day with assistance. Her mask for nocturnal NPPV was getting old, and she showed me where the straps were fraying. We noted that her bilevel device was now 8 years old and that she needed a new one. We concluded our conversation in 20 minutes and she blurted out: “Wow, that was easy. Thanks, Dr. Benditt.” I got off the phone and put in the order for a new mask and bilevel device with our clinic respiratory therapist. She received the equipment 48 hours later and sent an electronic message through her chart to let me know it had arrived. A total of five in-person visits including me and other providers had been cancelled and replaced by virtual visits. She has made one visit to the hospital in the last 3 months for an intrathecal nusinersen (Spinraza) injection that was done with a COVID-19 prescreening and full PPE.
One week prior to our virtual visit, my university hospital had reduced in-person clinic visits to those deemed absolutely necessary due to the COVID-19 pandemic. Visits considered absolutely necessary included such patients as postoperative transplant visits and preoperative evaluations for urgent surgeries. All other patient visits were canceled with plans to reschedule them once the COVID-19 pandemic was controlled. As the breadth and depth of the pandemic became apparent, a very rapid ramp-up of “virtual visits” via telemedicine capacity was rolled out. I had not previously used telemedicine, and the learning curve was steep, although once in place, the technology was straightforward from the provider perspective. The telemedicine visits for our hospital for the entire year of 2019 totaled about 800. In the month of April of 2020 we engaged in 40,000 telemedicine visits. This explosive growth of telemedicine implementation has occurred around the country and world during the COVID-19 pandemic (Olayiwola JN, et al. JMIR Public Health Surveill. 2020, May 29. doi: 10.2196/19045). This recent growth of telemedicine in the US has been fueled by the need for social distancing and quarantine, the lack of universal testing and COVID-19 case tracking, and the realization by CMS that coverage of telemedicine services had to be expanded rapidly to allow for continued patient care in the setting of stay-at-home orders. A rapid role out of application technology support and online training classes for health-care providers was undertaken. Privileges for telemedicine virtual visits were approved when providers completed the informational online modules and set up their HIPPA compliant Zoom accounts (Zoom Video Communications, San Jose, CA). All of us had minor stumbles initially with the equipment, software, and getting the patients connected online. After four or five visits, the process started to click and has become rather routine. Many providers and patients found this quite a positive development in terms of patient-provider visits but a question arose almost immediately: “Will this continue to be supported by insurers and allow us to integrate this practice into our outpatient clinic setting once the pandemic was controlled?” Time with tell, but an opportunity has presented itself.
For patients with neuromuscular disease and respiratory failure, telemedicine is a technology that may be particularly attractive for a number of reasons. First, patients with neuromuscular respiratory failure are likely at a particularly high risk of death if they develop full-blown COVID-19 infection. Development of acute respiratory distress syndrome (ARDS) on top of underlying neuromuscular respiratory failure is likely to be particularly deadly, although, very fortunately, there are no published reports of widespread infections in patients with neuromuscular respiratory disease. We have known for many decades that pneumonia is the leading cause of death for these patients. Second, patients with neuromuscular respiratory failure often find it quite difficult to come to the hospital for clinic visits. Mobilizing equipment, caregivers, and transportation can take days to arrange. For this reason, many neuromuscular clinics provide a multidisciplinary/multi-provider half-day visit to reduce the need to come into the hospital for multiple separate visits. Lastly, there are relatively few respiratory health-care providers in the United States and around the world who focus on patients with neuromuscular respiratory disease. Many neuromuscular clinics and providers will, therefore, have a very wide patient catchment area. For instance, my practice, based in Seattle, Washington, includes patients from Alaska, Montana, Idaho, and Wyoming. In-person hospital visits more than once per year may be virtually impossible.
Telemedicine is a methodology that has long been considered helpful in the arena of home ventilation and, in fact, we have been using some telemedicine technologies for some time (Casavant DW, et al. J Telemed Telecare. 2014;20[8]:441). Telemedicine (telehealth) includes the use of electronic information and communications technologies to provide and support health care when distance separates the participants. For instance, monitoring of nocturnal ventilation via downloads from Internet-connected noninvasive or invasive ventilation devices, overnight oximetry, and even phone calls from durable medical equipment providers during a home visit would be considered telemedicine. Many of us have been using these methods for many years. It is really the face-to-face “virtual visit” frequency that the COVID-19 pandemic has accelerated. This is a crucial advance in the process of telehealth because we may be able to reduce visits to our clinics from once every 3 to 6 months to perhaps once per year if support for virtual visits by insurers continues and if home monitoring can expand to include accurate home measurement of patient CO2 levels by either end-tidal CO2, transcutaneous CO2, or point of care arterial or capillary blood gases, as well as home pulmonary function monitoring. Measurement of CO2 levels and pulmonary function has generally been done at the hospital or in the clinic although there is no reason that with home visit support from appropriate services (that might even include durable medical equipment companies) that this could not be accomplished. This is not to say that there are not hurdles to the application of telehealth in the neuromuscular disease and home ventilation population. Not all patients have the equipment or technology savvy to participate in virtual visits, and not all insurers cover these visits even now during COVID-19. However, I imagine a future where a significant number of visits for patients with neuromuscular respiratory disease and home ventilation needs could be performed virtually. I envision that this would reduce patient and home caregiver travel burdens, make more efficient use of health-care provider time, expand the number of patients that a neuromuscular respiratory disease practitioner could serve, and perhaps reduce health-care expenditures per patient. This may be a real health-care bright spot in the huge difficulties of COVID-19. Fingers crossed.
Dr. Benditt is Medical Director of Respiratory Care Services and Professor of Medicine, University of Washington Medical Center, Seattle, Washington.
On March 17, 2020, I entered my patients electronic medical record and hit the “Connect with Zoom” button in her Epic (Epic Systems Corporation) chart. About 20 seconds later, the face of my 28-year-old patient with advanced spinal muscular atrophy type 2 (SMA-2) appeared virtually and not live for the first time since I had met her some 10 years previously. She appeared well and her history supported that. We spent most of the time reviewing recent events and surveying her home ventilation equipment. She felt well and sleep was of good quality. She was performing her normal activities without dyspnea. Her mechanical insufflator-exsufflator was working fine, although she used it only as needed, and she was performing lung volume recruitment maneuvers with a resuscitator bag three times a day with assistance. Her mask for nocturnal NPPV was getting old, and she showed me where the straps were fraying. We noted that her bilevel device was now 8 years old and that she needed a new one. We concluded our conversation in 20 minutes and she blurted out: “Wow, that was easy. Thanks, Dr. Benditt.” I got off the phone and put in the order for a new mask and bilevel device with our clinic respiratory therapist. She received the equipment 48 hours later and sent an electronic message through her chart to let me know it had arrived. A total of five in-person visits including me and other providers had been cancelled and replaced by virtual visits. She has made one visit to the hospital in the last 3 months for an intrathecal nusinersen (Spinraza) injection that was done with a COVID-19 prescreening and full PPE.
One week prior to our virtual visit, my university hospital had reduced in-person clinic visits to those deemed absolutely necessary due to the COVID-19 pandemic. Visits considered absolutely necessary included such patients as postoperative transplant visits and preoperative evaluations for urgent surgeries. All other patient visits were canceled with plans to reschedule them once the COVID-19 pandemic was controlled. As the breadth and depth of the pandemic became apparent, a very rapid ramp-up of “virtual visits” via telemedicine capacity was rolled out. I had not previously used telemedicine, and the learning curve was steep, although once in place, the technology was straightforward from the provider perspective. The telemedicine visits for our hospital for the entire year of 2019 totaled about 800. In the month of April of 2020 we engaged in 40,000 telemedicine visits. This explosive growth of telemedicine implementation has occurred around the country and world during the COVID-19 pandemic (Olayiwola JN, et al. JMIR Public Health Surveill. 2020, May 29. doi: 10.2196/19045). This recent growth of telemedicine in the US has been fueled by the need for social distancing and quarantine, the lack of universal testing and COVID-19 case tracking, and the realization by CMS that coverage of telemedicine services had to be expanded rapidly to allow for continued patient care in the setting of stay-at-home orders. A rapid role out of application technology support and online training classes for health-care providers was undertaken. Privileges for telemedicine virtual visits were approved when providers completed the informational online modules and set up their HIPPA compliant Zoom accounts (Zoom Video Communications, San Jose, CA). All of us had minor stumbles initially with the equipment, software, and getting the patients connected online. After four or five visits, the process started to click and has become rather routine. Many providers and patients found this quite a positive development in terms of patient-provider visits but a question arose almost immediately: “Will this continue to be supported by insurers and allow us to integrate this practice into our outpatient clinic setting once the pandemic was controlled?” Time with tell, but an opportunity has presented itself.
For patients with neuromuscular disease and respiratory failure, telemedicine is a technology that may be particularly attractive for a number of reasons. First, patients with neuromuscular respiratory failure are likely at a particularly high risk of death if they develop full-blown COVID-19 infection. Development of acute respiratory distress syndrome (ARDS) on top of underlying neuromuscular respiratory failure is likely to be particularly deadly, although, very fortunately, there are no published reports of widespread infections in patients with neuromuscular respiratory disease. We have known for many decades that pneumonia is the leading cause of death for these patients. Second, patients with neuromuscular respiratory failure often find it quite difficult to come to the hospital for clinic visits. Mobilizing equipment, caregivers, and transportation can take days to arrange. For this reason, many neuromuscular clinics provide a multidisciplinary/multi-provider half-day visit to reduce the need to come into the hospital for multiple separate visits. Lastly, there are relatively few respiratory health-care providers in the United States and around the world who focus on patients with neuromuscular respiratory disease. Many neuromuscular clinics and providers will, therefore, have a very wide patient catchment area. For instance, my practice, based in Seattle, Washington, includes patients from Alaska, Montana, Idaho, and Wyoming. In-person hospital visits more than once per year may be virtually impossible.
Telemedicine is a methodology that has long been considered helpful in the arena of home ventilation and, in fact, we have been using some telemedicine technologies for some time (Casavant DW, et al. J Telemed Telecare. 2014;20[8]:441). Telemedicine (telehealth) includes the use of electronic information and communications technologies to provide and support health care when distance separates the participants. For instance, monitoring of nocturnal ventilation via downloads from Internet-connected noninvasive or invasive ventilation devices, overnight oximetry, and even phone calls from durable medical equipment providers during a home visit would be considered telemedicine. Many of us have been using these methods for many years. It is really the face-to-face “virtual visit” frequency that the COVID-19 pandemic has accelerated. This is a crucial advance in the process of telehealth because we may be able to reduce visits to our clinics from once every 3 to 6 months to perhaps once per year if support for virtual visits by insurers continues and if home monitoring can expand to include accurate home measurement of patient CO2 levels by either end-tidal CO2, transcutaneous CO2, or point of care arterial or capillary blood gases, as well as home pulmonary function monitoring. Measurement of CO2 levels and pulmonary function has generally been done at the hospital or in the clinic although there is no reason that with home visit support from appropriate services (that might even include durable medical equipment companies) that this could not be accomplished. This is not to say that there are not hurdles to the application of telehealth in the neuromuscular disease and home ventilation population. Not all patients have the equipment or technology savvy to participate in virtual visits, and not all insurers cover these visits even now during COVID-19. However, I imagine a future where a significant number of visits for patients with neuromuscular respiratory disease and home ventilation needs could be performed virtually. I envision that this would reduce patient and home caregiver travel burdens, make more efficient use of health-care provider time, expand the number of patients that a neuromuscular respiratory disease practitioner could serve, and perhaps reduce health-care expenditures per patient. This may be a real health-care bright spot in the huge difficulties of COVID-19. Fingers crossed.
Dr. Benditt is Medical Director of Respiratory Care Services and Professor of Medicine, University of Washington Medical Center, Seattle, Washington.
New definitions of hypertension reveal new preeclampsia risks
according to results from a large retrospective cohort study.
In a 2017 guideline, the American College of Cardiology and American Heart Association changed clinical definitions of hypertension in adults. People previously deemed to have prehypertension were classed as having elevated blood pressure (systolic BP 120-129 mm Hg and diastolic BP >80 mm Hg) or stage 1 hypertension (systolic 130-139 mm Hg or diastolic 80-89 mm Hg).
And while hypertension as earlier defined (at or above systolic 140 mm Hg or at or above diastolic 90 mm Hg; now called stage 2 hypertension) has been long associated with adverse maternal and fetal effects, it was unclear whether lesser elevations in blood pressure also are linked to the same.
For their research published in Obstetrics & Gynecology, Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby and had two or more prenatal appointments before week 20 of pregnancy. The women in the study were seen at the same institution over a 3-year period ending in 2018. Three-quarters of the cohort had normal blood pressure, while 14% had elevated blood pressure and 5% had stage 1 hypertension before 20 weeks. Another 6% of the cohort had stage 2 hypertension.
The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did with 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Both term and preterm preeclampsia were factors in women with stage 1 and stage 2 hypertension, but preterm preeclampsia was associated with a higher risk. Although black race was associated with a higher risk of preeclampsia, the pattern of increasing risk with higher blood pressure category was similar in both black and white women.
Researchers also looked at gestational diabetes, severe maternal morbidity, neonatal morbidity, and placental abruption as secondary outcomes. They found the risk of gestational diabetes increased in a stepwise fashion as blood pressure increased, compared with normotensive women. Higher risk of severe maternal and neonatal morbidities was seen only in women with stage 2 hypertension. Placental abruption was rare in this cohort and the odds were not increased in any group.
The findings “highlight the importance of early pregnancy BP elevations, which may reflect prepregnancy BP status,” and suggest that the new guidelines “can identify women early in pregnancy who may benefit from increased surveillance,” Dr. Sutton and colleagues wrote.
Although randomized trials will be needed to identify the best prevention and management strategies for this patient group, they added, some clinicians may want to consider low-dose aspirin – an intervention shown to safely reduce preeclampsia risk among women with stage 2 hypertension – for women with elevated BP or stage 1 hypertension.
Dr. Sutton and colleagues acknowledged that its retrospective design is among the limitations of their study, and that use of antihypertensive medications could not be captured in their study.
Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy which are not well studied” in comparison to nonpregnant hypertensive states.
“Are these seemingly normal blood pressures associated with poor outcomes, maternal or neonatal? I think that this paper strongly tells us yes,” Dr. Santillan added. “But does that mean we have to do more aggressive blood pressure monitoring, seeing your doctor every month or so? Maybe we should change the way we’re treating people early on in gestation.”
The question of whether aspirin helps reduce preeclampsia risk in women with elevated blood pressure or stage 1 hypertension needs to be resolved in studies, Dr. Santillan said. But because of its favorable risk profile, “if I consider that if a patient has significant risk factors for developing preeclampsia, baby aspirin is fine.”
Postpregnancy blood pressure management is something that should also be reconsidered in light of the findings, Dr. Santillan said. Half of women with preeclampsia will have chronic hypertension after they deliver, increasing their risk of adverse cardiovascular outcomes later in life. But because most are young and otherwise healthy, they often are lost to follow-up.
“I think this paper has helped open up that conversation, that there is probably a link between what we’re doing in pregnancy to what we should be doing in the postpartum period,” he said.
Dr. Sutton and colleagues’ study received funding from the Richard King Mellon Foundation, the American Heart Association; and the National Institutes of Health. None of its authors had relevant disclosures. Dr. Santillan disclosed holding U.S. and international patents for preeclampsia prediction, diagnosis, and treatment.
SOURCE: Sutton et al. Obstet Gynecol. 2020;136:129-39.
according to results from a large retrospective cohort study.
In a 2017 guideline, the American College of Cardiology and American Heart Association changed clinical definitions of hypertension in adults. People previously deemed to have prehypertension were classed as having elevated blood pressure (systolic BP 120-129 mm Hg and diastolic BP >80 mm Hg) or stage 1 hypertension (systolic 130-139 mm Hg or diastolic 80-89 mm Hg).
And while hypertension as earlier defined (at or above systolic 140 mm Hg or at or above diastolic 90 mm Hg; now called stage 2 hypertension) has been long associated with adverse maternal and fetal effects, it was unclear whether lesser elevations in blood pressure also are linked to the same.
For their research published in Obstetrics & Gynecology, Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby and had two or more prenatal appointments before week 20 of pregnancy. The women in the study were seen at the same institution over a 3-year period ending in 2018. Three-quarters of the cohort had normal blood pressure, while 14% had elevated blood pressure and 5% had stage 1 hypertension before 20 weeks. Another 6% of the cohort had stage 2 hypertension.
The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did with 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Both term and preterm preeclampsia were factors in women with stage 1 and stage 2 hypertension, but preterm preeclampsia was associated with a higher risk. Although black race was associated with a higher risk of preeclampsia, the pattern of increasing risk with higher blood pressure category was similar in both black and white women.
Researchers also looked at gestational diabetes, severe maternal morbidity, neonatal morbidity, and placental abruption as secondary outcomes. They found the risk of gestational diabetes increased in a stepwise fashion as blood pressure increased, compared with normotensive women. Higher risk of severe maternal and neonatal morbidities was seen only in women with stage 2 hypertension. Placental abruption was rare in this cohort and the odds were not increased in any group.
The findings “highlight the importance of early pregnancy BP elevations, which may reflect prepregnancy BP status,” and suggest that the new guidelines “can identify women early in pregnancy who may benefit from increased surveillance,” Dr. Sutton and colleagues wrote.
Although randomized trials will be needed to identify the best prevention and management strategies for this patient group, they added, some clinicians may want to consider low-dose aspirin – an intervention shown to safely reduce preeclampsia risk among women with stage 2 hypertension – for women with elevated BP or stage 1 hypertension.
Dr. Sutton and colleagues acknowledged that its retrospective design is among the limitations of their study, and that use of antihypertensive medications could not be captured in their study.
Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy which are not well studied” in comparison to nonpregnant hypertensive states.
“Are these seemingly normal blood pressures associated with poor outcomes, maternal or neonatal? I think that this paper strongly tells us yes,” Dr. Santillan added. “But does that mean we have to do more aggressive blood pressure monitoring, seeing your doctor every month or so? Maybe we should change the way we’re treating people early on in gestation.”
The question of whether aspirin helps reduce preeclampsia risk in women with elevated blood pressure or stage 1 hypertension needs to be resolved in studies, Dr. Santillan said. But because of its favorable risk profile, “if I consider that if a patient has significant risk factors for developing preeclampsia, baby aspirin is fine.”
Postpregnancy blood pressure management is something that should also be reconsidered in light of the findings, Dr. Santillan said. Half of women with preeclampsia will have chronic hypertension after they deliver, increasing their risk of adverse cardiovascular outcomes later in life. But because most are young and otherwise healthy, they often are lost to follow-up.
“I think this paper has helped open up that conversation, that there is probably a link between what we’re doing in pregnancy to what we should be doing in the postpartum period,” he said.
Dr. Sutton and colleagues’ study received funding from the Richard King Mellon Foundation, the American Heart Association; and the National Institutes of Health. None of its authors had relevant disclosures. Dr. Santillan disclosed holding U.S. and international patents for preeclampsia prediction, diagnosis, and treatment.
SOURCE: Sutton et al. Obstet Gynecol. 2020;136:129-39.
according to results from a large retrospective cohort study.
In a 2017 guideline, the American College of Cardiology and American Heart Association changed clinical definitions of hypertension in adults. People previously deemed to have prehypertension were classed as having elevated blood pressure (systolic BP 120-129 mm Hg and diastolic BP >80 mm Hg) or stage 1 hypertension (systolic 130-139 mm Hg or diastolic 80-89 mm Hg).
And while hypertension as earlier defined (at or above systolic 140 mm Hg or at or above diastolic 90 mm Hg; now called stage 2 hypertension) has been long associated with adverse maternal and fetal effects, it was unclear whether lesser elevations in blood pressure also are linked to the same.
For their research published in Obstetrics & Gynecology, Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby and had two or more prenatal appointments before week 20 of pregnancy. The women in the study were seen at the same institution over a 3-year period ending in 2018. Three-quarters of the cohort had normal blood pressure, while 14% had elevated blood pressure and 5% had stage 1 hypertension before 20 weeks. Another 6% of the cohort had stage 2 hypertension.
The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did with 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Both term and preterm preeclampsia were factors in women with stage 1 and stage 2 hypertension, but preterm preeclampsia was associated with a higher risk. Although black race was associated with a higher risk of preeclampsia, the pattern of increasing risk with higher blood pressure category was similar in both black and white women.
Researchers also looked at gestational diabetes, severe maternal morbidity, neonatal morbidity, and placental abruption as secondary outcomes. They found the risk of gestational diabetes increased in a stepwise fashion as blood pressure increased, compared with normotensive women. Higher risk of severe maternal and neonatal morbidities was seen only in women with stage 2 hypertension. Placental abruption was rare in this cohort and the odds were not increased in any group.
The findings “highlight the importance of early pregnancy BP elevations, which may reflect prepregnancy BP status,” and suggest that the new guidelines “can identify women early in pregnancy who may benefit from increased surveillance,” Dr. Sutton and colleagues wrote.
Although randomized trials will be needed to identify the best prevention and management strategies for this patient group, they added, some clinicians may want to consider low-dose aspirin – an intervention shown to safely reduce preeclampsia risk among women with stage 2 hypertension – for women with elevated BP or stage 1 hypertension.
Dr. Sutton and colleagues acknowledged that its retrospective design is among the limitations of their study, and that use of antihypertensive medications could not be captured in their study.
Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy which are not well studied” in comparison to nonpregnant hypertensive states.
“Are these seemingly normal blood pressures associated with poor outcomes, maternal or neonatal? I think that this paper strongly tells us yes,” Dr. Santillan added. “But does that mean we have to do more aggressive blood pressure monitoring, seeing your doctor every month or so? Maybe we should change the way we’re treating people early on in gestation.”
The question of whether aspirin helps reduce preeclampsia risk in women with elevated blood pressure or stage 1 hypertension needs to be resolved in studies, Dr. Santillan said. But because of its favorable risk profile, “if I consider that if a patient has significant risk factors for developing preeclampsia, baby aspirin is fine.”
Postpregnancy blood pressure management is something that should also be reconsidered in light of the findings, Dr. Santillan said. Half of women with preeclampsia will have chronic hypertension after they deliver, increasing their risk of adverse cardiovascular outcomes later in life. But because most are young and otherwise healthy, they often are lost to follow-up.
“I think this paper has helped open up that conversation, that there is probably a link between what we’re doing in pregnancy to what we should be doing in the postpartum period,” he said.
Dr. Sutton and colleagues’ study received funding from the Richard King Mellon Foundation, the American Heart Association; and the National Institutes of Health. None of its authors had relevant disclosures. Dr. Santillan disclosed holding U.S. and international patents for preeclampsia prediction, diagnosis, and treatment.
SOURCE: Sutton et al. Obstet Gynecol. 2020;136:129-39.
FROM OBSTETRICS & GYNECOLOGY
New registry focuses on rheumatic immune-related AEs of cancer therapy
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
FROM THE EULAR 2020 E-CONGRESS
Dapagliflozin’s T2D renal protection extends to ‘fast decline’ of eGFR
Treatment of patients with type 2 diabetes with the SGLT2 inhibitor dapagliflozin led to a significant drop in the occurrence of ‘fast decline’ of renal function in more than 15,000 patients enrolled in the drug’s main cardiovascular outcome trial, another example of the potent renal protective effects of agents from this drug class.
Among patients with type 2 diabetes enrolled in the DECLARE-TIMI 58 trial, the incidence of a fast decline in renal function, defined as a drop in estimated glomerular filtration rate (eGFR) of at least 3 mL/min per 1.73 m2, was 27% among patients treated with dapagliflozin and 37% in control patients who received placebo, a statistically significant difference for this post-hoc analysis, Itamar Raz, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
This finding, which adds to a long list of other renal function parameters reported to have been improved by treatment with sodium-glucose cotransporter 2 (SGLT2) inhibitors, “emphasizes the value of SGLT2 inhibitors as an important component of both prevention and treatment of chronic kidney disease among patients with type 2 diabetes,” said Dr. Raz, a diabetes researcher and professor of medicine at Hadassah University Hospital in Jerusalem.
The primary, prespecified renal outcomes in DECLARE-TIMI 58 were a cardiorenal composite outcome of sustained decline of at least 40% in eGFR to less than 60 mL/min per 1.73 m2, end-stage renal disease (defined as dialysis for at least 90 days, kidney transplantation, or confirmed sustained eGFR of less than 15 mL/min per 1.73 m2), or death from renal or cardiovascular causes; and a second prespecified renal-specific composite outcome that was the same except for excluding death from cardiovascular causes. The results showed that the cardiorenal outcome dropped by a statistically significant 24% with dapagliflozin treatment relative to control patients, and the renal-specific outcome fell by a statistically significant 47% with dapagliflozin relative to control patients (Lancet Diab Endocrinol. 2019 Aug 1;7[8];606-17).
The new findings on the incidence of fast decline in renal function help to further flesh out the scope of renal benefit exerted by SGLT2 inhibitors like dapagliflozin in patients with type 2 diabetes, said experts. Fast decline is a relatively recently devised measure of a high-risk, precipitous loss of renal function that has been defined as a drop of either 3 or 5 mL/min per 1.73 m2 per year (Kidney Int. 2017 Jun;91[6]:1300-11); for this analysis Dr. Raz and his associates used the less stringent definition.
Finding and treating ‘fast decliners’
The new report from Dr. Raz “confirms the original [renal] findings and looks to expand them to a particularly high risk group: the fast decliners,” commented Robert A. Gabbay, MD, chief science & medical officer of the ADA. “In some ways, the group of patients that we need to find a better treatment for most are those whose GFR declines quickly. We don’t always know who they are until after the fact, and studies have been looking for markers that might prospectively identify them,” he said in an interview.
The new analysis showed that dapagliflozin “was effective in this subgroup of patients. Furthermore, it didn’t matter if they had significant baseline disease or not. Even people with normal kidney function [at baseline] who were still fast decliners fared better with the drug than without it. This suggests that, if it can be confirmed in a prospective study, dapagliflozin might be effective very early in the course of treatment if we can identify who will be the fast decliners.”
Dr. Raz and his associates had the data necessary to calculate the rates of eGFR decline during the full follow-up period for 15,012 of the 17,160 patients enrolled in DECLARE-TIMI 58, and they found that 4,788 (32%) were fast decliners and 10,224 had a slower rate of renal deterioration. The average annual decline in eGFR during the period from 6 months after study entry through 4 years was 6.3 mL/min per 1.73 m2 per year (median of 5.1 mL/min per 1.73 m2 per year) among the fast decliners, and zero (median of 0.6 mL/min per 1.73 m2 per year) among the other patients.
Overcoming dapagliflozin’s initial eGFR reduction
The researchers focused on the 6-month to 4-year period of treatment as more representative of the impact of dapagliflozin because the SGLT2 inhibitors have an established pattern of triggering an initial, moderate decline in eGFR over roughly the first 6 months on the drug, which is similar to what happens to patients who start treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker.
“Some patients get as much as a 10% decline in eGFR” when SGLT2 inhibitor treatment starts, but “patients do better over time even with this initial hit,” the same way they do on drugs that act on the renin-angiotensin system, explained Silvio E. Inzucchi, MD, an endocrinologist and professor of medicine at Yale University in New Haven who has extensively studied the SGLT2 inhibitors.
The analyses reported by Dr. Raz showed that the protection against fast decline during the 6-month to 4-year period with dapagliflozin treatment was consistent across a range of patient subgroups regardless of age, duration of their type 2 diabetes, their baseline level of hyperglycemia, and their baseline eGFR. Nearly half the patients enrolled in DECLARE-TIMI 58 had an eGFR at baseline of at least 91 mL/min per 1.73 m2 and in this subgroup the incidence of fast decliners was 23% with dapagliflozin and 31% on placebo. Among the 45% of patients who began with an eGFR of 60-90 mL/min per 1.73 m2 the fast-decliner incidence was 32% and 43% when on or off dapagliflozin. Among the 7% of patients who entered with an eGFR below 60 mL/min per 1.73 m2, the fast-decliner incidence was 25% on dapagliflozin and 36% among controls. All the between-group differences were statistically significant.
The incidence of fast decliners was also lower with dapagliflozin treatment when the analysis included the entire first 4 years on treatment, including the first 6 months when SGLT2s usually spikes a loss of renal function. For the entire 4-year period, fast decline occurred among 34% of patients on dapagliflozin and in 37% of control patients, a statistically significant difference.
The mechanisms behind the consistent renal-protective effects of the SGLT2 inhibitors remain unclear right now, but likely seem related to the “perfect” diuretic action the drugs produce, said Dr. Inzucchi. “They’re not as hugely effective as diuretics, but they’re gentler.” While the SGLT2 inhibitors cause a modest amount of fluid loss ”for some reason they don’t activate the compensatory mechanisms that prevent further reductions in plasma volume,” a property that manifests as little or no change in catecholamines or renin-angiotensin activity, which sets this diuretic action apart from what happens with conventional diuretic drugs, he said in an interview.
In DECLARE-TIMI 58 treatment with dapagliflozin met its primary safety outcome of noninferiority to placebo with respect to major adverse cardiovascular events. The results failed to show statistically significant superiority for one of the primary efficacy endpoints, the rate of major adverse coronary events, but they did show significantly better performance for the second primary efficacy outcome of the rate of cardiovascular death or hospitalization for heart failure, which occurred in 4.9% of patients treated with dapagliflozin and in 5.8% of the control patients during a median follow-up of 4.2 years (N Engl J Med. 2019 Jan 24;380[4]:347-57).
DECLARE-TIMI 58 was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Raz has been an advisor to and speaker on behalf of AstraZeneca as well as several other companies. Dr. Gabbay had no relevant disclosures. Dr. Inzucchi has been a consultant to AstraZeneca, and also to Abbott, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
SOURCE: Raz I et al. ADA 2020, Abstract 303-OR.
Treatment of patients with type 2 diabetes with the SGLT2 inhibitor dapagliflozin led to a significant drop in the occurrence of ‘fast decline’ of renal function in more than 15,000 patients enrolled in the drug’s main cardiovascular outcome trial, another example of the potent renal protective effects of agents from this drug class.
Among patients with type 2 diabetes enrolled in the DECLARE-TIMI 58 trial, the incidence of a fast decline in renal function, defined as a drop in estimated glomerular filtration rate (eGFR) of at least 3 mL/min per 1.73 m2, was 27% among patients treated with dapagliflozin and 37% in control patients who received placebo, a statistically significant difference for this post-hoc analysis, Itamar Raz, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
This finding, which adds to a long list of other renal function parameters reported to have been improved by treatment with sodium-glucose cotransporter 2 (SGLT2) inhibitors, “emphasizes the value of SGLT2 inhibitors as an important component of both prevention and treatment of chronic kidney disease among patients with type 2 diabetes,” said Dr. Raz, a diabetes researcher and professor of medicine at Hadassah University Hospital in Jerusalem.
The primary, prespecified renal outcomes in DECLARE-TIMI 58 were a cardiorenal composite outcome of sustained decline of at least 40% in eGFR to less than 60 mL/min per 1.73 m2, end-stage renal disease (defined as dialysis for at least 90 days, kidney transplantation, or confirmed sustained eGFR of less than 15 mL/min per 1.73 m2), or death from renal or cardiovascular causes; and a second prespecified renal-specific composite outcome that was the same except for excluding death from cardiovascular causes. The results showed that the cardiorenal outcome dropped by a statistically significant 24% with dapagliflozin treatment relative to control patients, and the renal-specific outcome fell by a statistically significant 47% with dapagliflozin relative to control patients (Lancet Diab Endocrinol. 2019 Aug 1;7[8];606-17).
The new findings on the incidence of fast decline in renal function help to further flesh out the scope of renal benefit exerted by SGLT2 inhibitors like dapagliflozin in patients with type 2 diabetes, said experts. Fast decline is a relatively recently devised measure of a high-risk, precipitous loss of renal function that has been defined as a drop of either 3 or 5 mL/min per 1.73 m2 per year (Kidney Int. 2017 Jun;91[6]:1300-11); for this analysis Dr. Raz and his associates used the less stringent definition.
Finding and treating ‘fast decliners’
The new report from Dr. Raz “confirms the original [renal] findings and looks to expand them to a particularly high risk group: the fast decliners,” commented Robert A. Gabbay, MD, chief science & medical officer of the ADA. “In some ways, the group of patients that we need to find a better treatment for most are those whose GFR declines quickly. We don’t always know who they are until after the fact, and studies have been looking for markers that might prospectively identify them,” he said in an interview.
The new analysis showed that dapagliflozin “was effective in this subgroup of patients. Furthermore, it didn’t matter if they had significant baseline disease or not. Even people with normal kidney function [at baseline] who were still fast decliners fared better with the drug than without it. This suggests that, if it can be confirmed in a prospective study, dapagliflozin might be effective very early in the course of treatment if we can identify who will be the fast decliners.”
Dr. Raz and his associates had the data necessary to calculate the rates of eGFR decline during the full follow-up period for 15,012 of the 17,160 patients enrolled in DECLARE-TIMI 58, and they found that 4,788 (32%) were fast decliners and 10,224 had a slower rate of renal deterioration. The average annual decline in eGFR during the period from 6 months after study entry through 4 years was 6.3 mL/min per 1.73 m2 per year (median of 5.1 mL/min per 1.73 m2 per year) among the fast decliners, and zero (median of 0.6 mL/min per 1.73 m2 per year) among the other patients.
Overcoming dapagliflozin’s initial eGFR reduction
The researchers focused on the 6-month to 4-year period of treatment as more representative of the impact of dapagliflozin because the SGLT2 inhibitors have an established pattern of triggering an initial, moderate decline in eGFR over roughly the first 6 months on the drug, which is similar to what happens to patients who start treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker.
“Some patients get as much as a 10% decline in eGFR” when SGLT2 inhibitor treatment starts, but “patients do better over time even with this initial hit,” the same way they do on drugs that act on the renin-angiotensin system, explained Silvio E. Inzucchi, MD, an endocrinologist and professor of medicine at Yale University in New Haven who has extensively studied the SGLT2 inhibitors.
The analyses reported by Dr. Raz showed that the protection against fast decline during the 6-month to 4-year period with dapagliflozin treatment was consistent across a range of patient subgroups regardless of age, duration of their type 2 diabetes, their baseline level of hyperglycemia, and their baseline eGFR. Nearly half the patients enrolled in DECLARE-TIMI 58 had an eGFR at baseline of at least 91 mL/min per 1.73 m2 and in this subgroup the incidence of fast decliners was 23% with dapagliflozin and 31% on placebo. Among the 45% of patients who began with an eGFR of 60-90 mL/min per 1.73 m2 the fast-decliner incidence was 32% and 43% when on or off dapagliflozin. Among the 7% of patients who entered with an eGFR below 60 mL/min per 1.73 m2, the fast-decliner incidence was 25% on dapagliflozin and 36% among controls. All the between-group differences were statistically significant.
The incidence of fast decliners was also lower with dapagliflozin treatment when the analysis included the entire first 4 years on treatment, including the first 6 months when SGLT2s usually spikes a loss of renal function. For the entire 4-year period, fast decline occurred among 34% of patients on dapagliflozin and in 37% of control patients, a statistically significant difference.
The mechanisms behind the consistent renal-protective effects of the SGLT2 inhibitors remain unclear right now, but likely seem related to the “perfect” diuretic action the drugs produce, said Dr. Inzucchi. “They’re not as hugely effective as diuretics, but they’re gentler.” While the SGLT2 inhibitors cause a modest amount of fluid loss ”for some reason they don’t activate the compensatory mechanisms that prevent further reductions in plasma volume,” a property that manifests as little or no change in catecholamines or renin-angiotensin activity, which sets this diuretic action apart from what happens with conventional diuretic drugs, he said in an interview.
In DECLARE-TIMI 58 treatment with dapagliflozin met its primary safety outcome of noninferiority to placebo with respect to major adverse cardiovascular events. The results failed to show statistically significant superiority for one of the primary efficacy endpoints, the rate of major adverse coronary events, but they did show significantly better performance for the second primary efficacy outcome of the rate of cardiovascular death or hospitalization for heart failure, which occurred in 4.9% of patients treated with dapagliflozin and in 5.8% of the control patients during a median follow-up of 4.2 years (N Engl J Med. 2019 Jan 24;380[4]:347-57).
DECLARE-TIMI 58 was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Raz has been an advisor to and speaker on behalf of AstraZeneca as well as several other companies. Dr. Gabbay had no relevant disclosures. Dr. Inzucchi has been a consultant to AstraZeneca, and also to Abbott, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
SOURCE: Raz I et al. ADA 2020, Abstract 303-OR.
Treatment of patients with type 2 diabetes with the SGLT2 inhibitor dapagliflozin led to a significant drop in the occurrence of ‘fast decline’ of renal function in more than 15,000 patients enrolled in the drug’s main cardiovascular outcome trial, another example of the potent renal protective effects of agents from this drug class.
Among patients with type 2 diabetes enrolled in the DECLARE-TIMI 58 trial, the incidence of a fast decline in renal function, defined as a drop in estimated glomerular filtration rate (eGFR) of at least 3 mL/min per 1.73 m2, was 27% among patients treated with dapagliflozin and 37% in control patients who received placebo, a statistically significant difference for this post-hoc analysis, Itamar Raz, MD, said at the virtual annual scientific sessions of the American Diabetes Association.
This finding, which adds to a long list of other renal function parameters reported to have been improved by treatment with sodium-glucose cotransporter 2 (SGLT2) inhibitors, “emphasizes the value of SGLT2 inhibitors as an important component of both prevention and treatment of chronic kidney disease among patients with type 2 diabetes,” said Dr. Raz, a diabetes researcher and professor of medicine at Hadassah University Hospital in Jerusalem.
The primary, prespecified renal outcomes in DECLARE-TIMI 58 were a cardiorenal composite outcome of sustained decline of at least 40% in eGFR to less than 60 mL/min per 1.73 m2, end-stage renal disease (defined as dialysis for at least 90 days, kidney transplantation, or confirmed sustained eGFR of less than 15 mL/min per 1.73 m2), or death from renal or cardiovascular causes; and a second prespecified renal-specific composite outcome that was the same except for excluding death from cardiovascular causes. The results showed that the cardiorenal outcome dropped by a statistically significant 24% with dapagliflozin treatment relative to control patients, and the renal-specific outcome fell by a statistically significant 47% with dapagliflozin relative to control patients (Lancet Diab Endocrinol. 2019 Aug 1;7[8];606-17).
The new findings on the incidence of fast decline in renal function help to further flesh out the scope of renal benefit exerted by SGLT2 inhibitors like dapagliflozin in patients with type 2 diabetes, said experts. Fast decline is a relatively recently devised measure of a high-risk, precipitous loss of renal function that has been defined as a drop of either 3 or 5 mL/min per 1.73 m2 per year (Kidney Int. 2017 Jun;91[6]:1300-11); for this analysis Dr. Raz and his associates used the less stringent definition.
Finding and treating ‘fast decliners’
The new report from Dr. Raz “confirms the original [renal] findings and looks to expand them to a particularly high risk group: the fast decliners,” commented Robert A. Gabbay, MD, chief science & medical officer of the ADA. “In some ways, the group of patients that we need to find a better treatment for most are those whose GFR declines quickly. We don’t always know who they are until after the fact, and studies have been looking for markers that might prospectively identify them,” he said in an interview.
The new analysis showed that dapagliflozin “was effective in this subgroup of patients. Furthermore, it didn’t matter if they had significant baseline disease or not. Even people with normal kidney function [at baseline] who were still fast decliners fared better with the drug than without it. This suggests that, if it can be confirmed in a prospective study, dapagliflozin might be effective very early in the course of treatment if we can identify who will be the fast decliners.”
Dr. Raz and his associates had the data necessary to calculate the rates of eGFR decline during the full follow-up period for 15,012 of the 17,160 patients enrolled in DECLARE-TIMI 58, and they found that 4,788 (32%) were fast decliners and 10,224 had a slower rate of renal deterioration. The average annual decline in eGFR during the period from 6 months after study entry through 4 years was 6.3 mL/min per 1.73 m2 per year (median of 5.1 mL/min per 1.73 m2 per year) among the fast decliners, and zero (median of 0.6 mL/min per 1.73 m2 per year) among the other patients.
Overcoming dapagliflozin’s initial eGFR reduction
The researchers focused on the 6-month to 4-year period of treatment as more representative of the impact of dapagliflozin because the SGLT2 inhibitors have an established pattern of triggering an initial, moderate decline in eGFR over roughly the first 6 months on the drug, which is similar to what happens to patients who start treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker.
“Some patients get as much as a 10% decline in eGFR” when SGLT2 inhibitor treatment starts, but “patients do better over time even with this initial hit,” the same way they do on drugs that act on the renin-angiotensin system, explained Silvio E. Inzucchi, MD, an endocrinologist and professor of medicine at Yale University in New Haven who has extensively studied the SGLT2 inhibitors.
The analyses reported by Dr. Raz showed that the protection against fast decline during the 6-month to 4-year period with dapagliflozin treatment was consistent across a range of patient subgroups regardless of age, duration of their type 2 diabetes, their baseline level of hyperglycemia, and their baseline eGFR. Nearly half the patients enrolled in DECLARE-TIMI 58 had an eGFR at baseline of at least 91 mL/min per 1.73 m2 and in this subgroup the incidence of fast decliners was 23% with dapagliflozin and 31% on placebo. Among the 45% of patients who began with an eGFR of 60-90 mL/min per 1.73 m2 the fast-decliner incidence was 32% and 43% when on or off dapagliflozin. Among the 7% of patients who entered with an eGFR below 60 mL/min per 1.73 m2, the fast-decliner incidence was 25% on dapagliflozin and 36% among controls. All the between-group differences were statistically significant.
The incidence of fast decliners was also lower with dapagliflozin treatment when the analysis included the entire first 4 years on treatment, including the first 6 months when SGLT2s usually spikes a loss of renal function. For the entire 4-year period, fast decline occurred among 34% of patients on dapagliflozin and in 37% of control patients, a statistically significant difference.
The mechanisms behind the consistent renal-protective effects of the SGLT2 inhibitors remain unclear right now, but likely seem related to the “perfect” diuretic action the drugs produce, said Dr. Inzucchi. “They’re not as hugely effective as diuretics, but they’re gentler.” While the SGLT2 inhibitors cause a modest amount of fluid loss ”for some reason they don’t activate the compensatory mechanisms that prevent further reductions in plasma volume,” a property that manifests as little or no change in catecholamines or renin-angiotensin activity, which sets this diuretic action apart from what happens with conventional diuretic drugs, he said in an interview.
In DECLARE-TIMI 58 treatment with dapagliflozin met its primary safety outcome of noninferiority to placebo with respect to major adverse cardiovascular events. The results failed to show statistically significant superiority for one of the primary efficacy endpoints, the rate of major adverse coronary events, but they did show significantly better performance for the second primary efficacy outcome of the rate of cardiovascular death or hospitalization for heart failure, which occurred in 4.9% of patients treated with dapagliflozin and in 5.8% of the control patients during a median follow-up of 4.2 years (N Engl J Med. 2019 Jan 24;380[4]:347-57).
DECLARE-TIMI 58 was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Raz has been an advisor to and speaker on behalf of AstraZeneca as well as several other companies. Dr. Gabbay had no relevant disclosures. Dr. Inzucchi has been a consultant to AstraZeneca, and also to Abbott, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
SOURCE: Raz I et al. ADA 2020, Abstract 303-OR.
FROM ADA 2020