User login
Intranasal DHE shows promise in migraine
, according to results from a phase 3 clinical trial. In development by Impel NeuroPharma, the new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE.
“Our analysis of the data suggests that nothing new or untoward seemed to be happening as a result of delivering DHE to the upper nasal space,” Stephen Shrewsbury, MD, chief medical officer of Impel NeuroPharma, said in an interview. The company released key results from its phase 3 clinical trial, while a poster examining patient satisfaction was presented by Dr. Shrewsbury at the virtual annual meeting of the American Headache Society.
An improved intranasal formulation
The product isn’t the first effort to develop an inhaled form of DHE. An inhaled version called Migranal, marketed by Bausch Health, delivers DHE to the front part of the nose, where it may be lost to the upper lip or down the throat, according to Dr. Shrewsbury. Impel’s formulation (INP104) delivers the drug to the upper nasal space, where an earlier phase 1 trial demonstrated it could achieve higher serum concentrations compared with Migranal.
In 2018, MAP Pharmaceuticals came close to a product, but it was ultimately rejected by the Food and Drug Administration because DHE was not stable in the propellant used in the formulation. This time is different, said Dr. Shrewsbury, who was chief medical officer at MAP before joining Impel. The new device holds DHE and the propellant in separate compartments until they are combined right before use, which should circumvent stability problems.
Dr. Shrewsbury believes that patients will welcome an inhaled version of DHE. “People with migraines don’t want to have to go into hospital or even an infusion center if they can help it,” he said.
The study was one of a number of presentations at the AHS meeting that focused on novel delivery methods for established drugs. “The idea of taking things that we know work and improving upon them, both in terms of formulation and then delivery, that’s a common theme. My impression is that this will be an interesting arrow to have in our sling,” said Andrew Charles, MD, professor of neurology and director of the UCLA Goldberg Migraine Program, who was not involved in the study.
Open-label trial results
The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). Maximum doses included two per day and three per week.
There were no new safety signals or concern trends in nasal safety findings. 15.0% of patients experienced nasal congestion, 6.8% nausea, 5.1% nasal discomfort, and 5.1% unpleasant taste.
A total of 66.3% of participants reported pain relief by 2 hours (severe or moderate pain reduced to mild or none, or mild pain reduced to none) following a dose, and 38% had freedom from pain. 16.3% reported pain relief onset at 15 minutes, with continued improvement over time. During weeks 21-24 of the study, 98.4% and 95% of patients reporting no recurrence of their migraine or use of rescue medications during the 24- and 48-hour periods after using INP104. “Once they got rid of the pain, it didn’t come back, and that’s been one of the shortcomings of many of the available oral therapies – although some of them can be quite effective, that effect can wear off and people can find their migraine comes back within a 24- or 48-hour period,” said Dr. Shrewsbury.
The drug was also rated as convenient, with 83.6% of participants strongly agreeing (50%) or agreeing (33.6%) that it is easy to use.
“It certainly looks like compliance will be good. The possibility is that this will be quite useful,” said Dr. Charles, who is also enthusiastic about some of the other drug formulations announced at the meeting. “It really is just fun times for us as clinicians to be able to have so many different options for patients,” he said.
Dr. Shrewsbury is an employee of Impel NeuroPharma, which funded the study.* Dr. Charles consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
SOURCE: Shrewsbury S, et al. AHS 2020. Abstract 832509.
*Correction, 6/19/20: An earlier version of this article misstated the name of Impel NeuroPharma.
, according to results from a phase 3 clinical trial. In development by Impel NeuroPharma, the new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE.
“Our analysis of the data suggests that nothing new or untoward seemed to be happening as a result of delivering DHE to the upper nasal space,” Stephen Shrewsbury, MD, chief medical officer of Impel NeuroPharma, said in an interview. The company released key results from its phase 3 clinical trial, while a poster examining patient satisfaction was presented by Dr. Shrewsbury at the virtual annual meeting of the American Headache Society.
An improved intranasal formulation
The product isn’t the first effort to develop an inhaled form of DHE. An inhaled version called Migranal, marketed by Bausch Health, delivers DHE to the front part of the nose, where it may be lost to the upper lip or down the throat, according to Dr. Shrewsbury. Impel’s formulation (INP104) delivers the drug to the upper nasal space, where an earlier phase 1 trial demonstrated it could achieve higher serum concentrations compared with Migranal.
In 2018, MAP Pharmaceuticals came close to a product, but it was ultimately rejected by the Food and Drug Administration because DHE was not stable in the propellant used in the formulation. This time is different, said Dr. Shrewsbury, who was chief medical officer at MAP before joining Impel. The new device holds DHE and the propellant in separate compartments until they are combined right before use, which should circumvent stability problems.
Dr. Shrewsbury believes that patients will welcome an inhaled version of DHE. “People with migraines don’t want to have to go into hospital or even an infusion center if they can help it,” he said.
The study was one of a number of presentations at the AHS meeting that focused on novel delivery methods for established drugs. “The idea of taking things that we know work and improving upon them, both in terms of formulation and then delivery, that’s a common theme. My impression is that this will be an interesting arrow to have in our sling,” said Andrew Charles, MD, professor of neurology and director of the UCLA Goldberg Migraine Program, who was not involved in the study.
Open-label trial results
The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). Maximum doses included two per day and three per week.
There were no new safety signals or concern trends in nasal safety findings. 15.0% of patients experienced nasal congestion, 6.8% nausea, 5.1% nasal discomfort, and 5.1% unpleasant taste.
A total of 66.3% of participants reported pain relief by 2 hours (severe or moderate pain reduced to mild or none, or mild pain reduced to none) following a dose, and 38% had freedom from pain. 16.3% reported pain relief onset at 15 minutes, with continued improvement over time. During weeks 21-24 of the study, 98.4% and 95% of patients reporting no recurrence of their migraine or use of rescue medications during the 24- and 48-hour periods after using INP104. “Once they got rid of the pain, it didn’t come back, and that’s been one of the shortcomings of many of the available oral therapies – although some of them can be quite effective, that effect can wear off and people can find their migraine comes back within a 24- or 48-hour period,” said Dr. Shrewsbury.
The drug was also rated as convenient, with 83.6% of participants strongly agreeing (50%) or agreeing (33.6%) that it is easy to use.
“It certainly looks like compliance will be good. The possibility is that this will be quite useful,” said Dr. Charles, who is also enthusiastic about some of the other drug formulations announced at the meeting. “It really is just fun times for us as clinicians to be able to have so many different options for patients,” he said.
Dr. Shrewsbury is an employee of Impel NeuroPharma, which funded the study.* Dr. Charles consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
SOURCE: Shrewsbury S, et al. AHS 2020. Abstract 832509.
*Correction, 6/19/20: An earlier version of this article misstated the name of Impel NeuroPharma.
, according to results from a phase 3 clinical trial. In development by Impel NeuroPharma, the new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE.
“Our analysis of the data suggests that nothing new or untoward seemed to be happening as a result of delivering DHE to the upper nasal space,” Stephen Shrewsbury, MD, chief medical officer of Impel NeuroPharma, said in an interview. The company released key results from its phase 3 clinical trial, while a poster examining patient satisfaction was presented by Dr. Shrewsbury at the virtual annual meeting of the American Headache Society.
An improved intranasal formulation
The product isn’t the first effort to develop an inhaled form of DHE. An inhaled version called Migranal, marketed by Bausch Health, delivers DHE to the front part of the nose, where it may be lost to the upper lip or down the throat, according to Dr. Shrewsbury. Impel’s formulation (INP104) delivers the drug to the upper nasal space, where an earlier phase 1 trial demonstrated it could achieve higher serum concentrations compared with Migranal.
In 2018, MAP Pharmaceuticals came close to a product, but it was ultimately rejected by the Food and Drug Administration because DHE was not stable in the propellant used in the formulation. This time is different, said Dr. Shrewsbury, who was chief medical officer at MAP before joining Impel. The new device holds DHE and the propellant in separate compartments until they are combined right before use, which should circumvent stability problems.
Dr. Shrewsbury believes that patients will welcome an inhaled version of DHE. “People with migraines don’t want to have to go into hospital or even an infusion center if they can help it,” he said.
The study was one of a number of presentations at the AHS meeting that focused on novel delivery methods for established drugs. “The idea of taking things that we know work and improving upon them, both in terms of formulation and then delivery, that’s a common theme. My impression is that this will be an interesting arrow to have in our sling,” said Andrew Charles, MD, professor of neurology and director of the UCLA Goldberg Migraine Program, who was not involved in the study.
Open-label trial results
The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). Maximum doses included two per day and three per week.
There were no new safety signals or concern trends in nasal safety findings. 15.0% of patients experienced nasal congestion, 6.8% nausea, 5.1% nasal discomfort, and 5.1% unpleasant taste.
A total of 66.3% of participants reported pain relief by 2 hours (severe or moderate pain reduced to mild or none, or mild pain reduced to none) following a dose, and 38% had freedom from pain. 16.3% reported pain relief onset at 15 minutes, with continued improvement over time. During weeks 21-24 of the study, 98.4% and 95% of patients reporting no recurrence of their migraine or use of rescue medications during the 24- and 48-hour periods after using INP104. “Once they got rid of the pain, it didn’t come back, and that’s been one of the shortcomings of many of the available oral therapies – although some of them can be quite effective, that effect can wear off and people can find their migraine comes back within a 24- or 48-hour period,” said Dr. Shrewsbury.
The drug was also rated as convenient, with 83.6% of participants strongly agreeing (50%) or agreeing (33.6%) that it is easy to use.
“It certainly looks like compliance will be good. The possibility is that this will be quite useful,” said Dr. Charles, who is also enthusiastic about some of the other drug formulations announced at the meeting. “It really is just fun times for us as clinicians to be able to have so many different options for patients,” he said.
Dr. Shrewsbury is an employee of Impel NeuroPharma, which funded the study.* Dr. Charles consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
SOURCE: Shrewsbury S, et al. AHS 2020. Abstract 832509.
*Correction, 6/19/20: An earlier version of this article misstated the name of Impel NeuroPharma.
FROM AHS 2020
CheckMate 9LA: ‘Doing better’ for stage IV/recurrent NSCLC
Data from the CheckMate 9LA study suggest the combination amplifies the rapid response expected from chemotherapy and the long-term benefit from immunotherapy. Furthermore, the very limited exposure to chemotherapy appears to mitigate long-term risks.
Martin Reck, MD, PhD, of LungenClinic Grosshansdorf in Germany, reported the data as part of the American Society of Clinical Oncology virtual scientific program (Abstract 9501).
A prior trial, CheckMate 227, demonstrated that nivolumab plus ipilimumab improved overall survival (OS) and durability of response in comparison with conventional chemotherapy in advanced NSCLC, regardless of PD-L1 expression (N Engl J Med 2019; 381:2020-31).
In CheckMate 9LA, researchers tested whether adding a limited course of chemotherapy – just two cycles – could improve outcomes further. Dr. Reck reported that, at the first preplanned interim analysis, the combination met its primary goal of improving OS as well as meeting multiple secondary endpoints.
Details of CheckMate 9LA
CheckMate 9LA included 719 treatment-naive patients with histologically confirmed stage IV or recurrent NSCLC and no known sensitizing alterations in EGFR or ALK. All patients had an Eastern Cooperative Oncology Group performance status of 0 or 1.
Patients received either nivolumab plus ipilimumab at standard NSCLC doses plus two cycles of chemotherapy or chemotherapy alone for four cycles.
The chemotherapy regimen was tailored by histology. Pemetrexed plus either cisplatin or carboplatin, with optional pemetrexed maintenance, was administered to patients with non-squamous histology. Paclitaxel plus carboplatin was chosen for patients with squamous disease.
If there was no disease progression or unacceptable toxicity, patients receiving nivolumab plus ipilimumab could continue immunotherapy for up to 2 years.
Patients were stratified by PD-L1 expression (< 1% vs. ≥ 1%), gender, and histology (squamous vs. non-squamous). Tumor and clinical characteristics were balanced across the trial arms.
The primary endpoint was OS, with secondary endpoints of progression-free survival, objective response rate by blinded independent central review, and efficacy by PD-L1 subgroups. Exploratory endpoints included safety/tolerability.
Results prompt FDA approval
Dr. Reck and colleagues found significantly better OS with nivolumab-ipilimumab plus chemotherapy, in comparison with chemotherapy alone (hazard ratio, 0.69; P = .0006).
With longer follow-up (minimum 12.7 months), nivolumab-ipilimumab plus chemotherapy continued to provide longer OS compared with chemotherapy alone. The median OS was 15.6 months and 10.9 months, respectively (HR, 0.66).
Despite more patients receiving subsequent systemic therapy in the chemotherapy-alone arm (34% of whom eventually received an immune checkpoint inhibitor), the immunotherapy-chemotherapy arm still yielded superior OS in the overall population.
One-year OS rates were 63% in the immunotherapy arm and 47% in the chemotherapy-alone arm.
Statistically significant improvements in progression-free survival and objective response rate were seen. The median response duration was 11.3 months in the immunotherapy arm and 5.6 months in the chemotherapy-alone arm.
Benefit was consistent by all efficacy measures and in all subgroups, including by PD-L1 expression and histology.
Based on the strength of these results, in May, the Food and Drug Administration approved nivolumab plus ipilimumab and two cycles of platinum-doublet chemotherapy for the frontline treatment of patients with metastatic or recurrent NSCLC with no EGFR or ALK genomic tumor aberrations.
Challenges to overcome
In the forest plots for OS, the 70 patients who were 75 years of age and older had inferior survival with the combination regimen, compared with chemotherapy alone.
Grade 3-4 treatment-related toxicity was reported in 47% of patients in the immunotherapy arm and 38% of those in the chemotherapy-alone arm.
With nivolumab-ipilimumab plus chemotherapy, more adverse events were considered serious (25.4% vs. 15%). Furthermore, grade 3-4 adverse events led to a higher rate of treatment discontinuation in the immunotherapy arm than in the chemotherapy-alone arm (16% vs. 5%).
Although cross-trial comparisons are treacherous, in CheckMate 227, only 12% of patients receiving nivolumab plus ipilimumab stopped treatment because of a grade 3-4 adverse event.
Better by design
In the updated analysis of CheckMate 227 (ASCO 2020, Abstract 9500), the nivolumab-ipilimumab regimen showed inferior OS results for the first 6 months of treatment, with more disease progression during that time. However, at 6 months, the OS curves crossed over to become consistently superior for the immunotherapy regimen thereafter.
Platinum-based chemotherapy is thought to augment antitumor immunity by inducing immunogenic cell death, increasing tumor neoantigen expression, and disturbing the immunosuppressive tumor microenvironment that prevents immune detection.
Therefore, CheckMate 9LA incorporated a short exposure to chemotherapy for the patients receiving nivolumab-ipilimumab in an effort to attain rapid disease control and retain the durable OS benefit that was seen with dual immunotherapy in CheckMate 227.
Indeed, in CheckMate 9LA, the Kaplan-Meier curves in both the initial and follow-up OS analyses diverged early in favor of the nivolumab-ipilimumab plus chemotherapy regimen and never crossed the curve for chemotherapy alone. Progressive disease was observed in fewer patients with the immunotherapy combination than with chemotherapy alone.
Longer follow-up needed
In recent years, a large number of treatment options for stage IV NSCLC patients have emerged. In the current report of CheckMate 9LA, the OS curve extended only to 27 months.
As was noted by invited discussant Benjamin Levy, MD, of Johns Hopkins University in Baltimore, it may be premature to put the regimen of two cycles of chemotherapy plus dual checkpoint/CTLA4 blockade in its proper context until follow-up extends for 3-5 years.
It would be ideal to know whether the tail of the OS curve will flatten out.
Do the best you can
Clinical investigators have a responsibility to retain the successes of prior regimens while overcoming the challenges of adverse events. New regimens also need to be practical when applied in general oncology practice.
In 2014, the American poet Maya Angelou advised, “Do the best you can until you know better. Then, when you know better, do better.” In many regards, the immunotherapy-chemotherapy combination tested in CheckMate 9LA appears to do better than preceding regimens.
Further refinements in dose, schedule, and supportive care, as well as real-time reporting of and response to patient-reported outcomes, will likely help us build on the CheckMate 9LA regimen and do even better.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Reck M et al. ASCO 2020, Abstract 9501.
Data from the CheckMate 9LA study suggest the combination amplifies the rapid response expected from chemotherapy and the long-term benefit from immunotherapy. Furthermore, the very limited exposure to chemotherapy appears to mitigate long-term risks.
Martin Reck, MD, PhD, of LungenClinic Grosshansdorf in Germany, reported the data as part of the American Society of Clinical Oncology virtual scientific program (Abstract 9501).
A prior trial, CheckMate 227, demonstrated that nivolumab plus ipilimumab improved overall survival (OS) and durability of response in comparison with conventional chemotherapy in advanced NSCLC, regardless of PD-L1 expression (N Engl J Med 2019; 381:2020-31).
In CheckMate 9LA, researchers tested whether adding a limited course of chemotherapy – just two cycles – could improve outcomes further. Dr. Reck reported that, at the first preplanned interim analysis, the combination met its primary goal of improving OS as well as meeting multiple secondary endpoints.
Details of CheckMate 9LA
CheckMate 9LA included 719 treatment-naive patients with histologically confirmed stage IV or recurrent NSCLC and no known sensitizing alterations in EGFR or ALK. All patients had an Eastern Cooperative Oncology Group performance status of 0 or 1.
Patients received either nivolumab plus ipilimumab at standard NSCLC doses plus two cycles of chemotherapy or chemotherapy alone for four cycles.
The chemotherapy regimen was tailored by histology. Pemetrexed plus either cisplatin or carboplatin, with optional pemetrexed maintenance, was administered to patients with non-squamous histology. Paclitaxel plus carboplatin was chosen for patients with squamous disease.
If there was no disease progression or unacceptable toxicity, patients receiving nivolumab plus ipilimumab could continue immunotherapy for up to 2 years.
Patients were stratified by PD-L1 expression (< 1% vs. ≥ 1%), gender, and histology (squamous vs. non-squamous). Tumor and clinical characteristics were balanced across the trial arms.
The primary endpoint was OS, with secondary endpoints of progression-free survival, objective response rate by blinded independent central review, and efficacy by PD-L1 subgroups. Exploratory endpoints included safety/tolerability.
Results prompt FDA approval
Dr. Reck and colleagues found significantly better OS with nivolumab-ipilimumab plus chemotherapy, in comparison with chemotherapy alone (hazard ratio, 0.69; P = .0006).
With longer follow-up (minimum 12.7 months), nivolumab-ipilimumab plus chemotherapy continued to provide longer OS compared with chemotherapy alone. The median OS was 15.6 months and 10.9 months, respectively (HR, 0.66).
Despite more patients receiving subsequent systemic therapy in the chemotherapy-alone arm (34% of whom eventually received an immune checkpoint inhibitor), the immunotherapy-chemotherapy arm still yielded superior OS in the overall population.
One-year OS rates were 63% in the immunotherapy arm and 47% in the chemotherapy-alone arm.
Statistically significant improvements in progression-free survival and objective response rate were seen. The median response duration was 11.3 months in the immunotherapy arm and 5.6 months in the chemotherapy-alone arm.
Benefit was consistent by all efficacy measures and in all subgroups, including by PD-L1 expression and histology.
Based on the strength of these results, in May, the Food and Drug Administration approved nivolumab plus ipilimumab and two cycles of platinum-doublet chemotherapy for the frontline treatment of patients with metastatic or recurrent NSCLC with no EGFR or ALK genomic tumor aberrations.
Challenges to overcome
In the forest plots for OS, the 70 patients who were 75 years of age and older had inferior survival with the combination regimen, compared with chemotherapy alone.
Grade 3-4 treatment-related toxicity was reported in 47% of patients in the immunotherapy arm and 38% of those in the chemotherapy-alone arm.
With nivolumab-ipilimumab plus chemotherapy, more adverse events were considered serious (25.4% vs. 15%). Furthermore, grade 3-4 adverse events led to a higher rate of treatment discontinuation in the immunotherapy arm than in the chemotherapy-alone arm (16% vs. 5%).
Although cross-trial comparisons are treacherous, in CheckMate 227, only 12% of patients receiving nivolumab plus ipilimumab stopped treatment because of a grade 3-4 adverse event.
Better by design
In the updated analysis of CheckMate 227 (ASCO 2020, Abstract 9500), the nivolumab-ipilimumab regimen showed inferior OS results for the first 6 months of treatment, with more disease progression during that time. However, at 6 months, the OS curves crossed over to become consistently superior for the immunotherapy regimen thereafter.
Platinum-based chemotherapy is thought to augment antitumor immunity by inducing immunogenic cell death, increasing tumor neoantigen expression, and disturbing the immunosuppressive tumor microenvironment that prevents immune detection.
Therefore, CheckMate 9LA incorporated a short exposure to chemotherapy for the patients receiving nivolumab-ipilimumab in an effort to attain rapid disease control and retain the durable OS benefit that was seen with dual immunotherapy in CheckMate 227.
Indeed, in CheckMate 9LA, the Kaplan-Meier curves in both the initial and follow-up OS analyses diverged early in favor of the nivolumab-ipilimumab plus chemotherapy regimen and never crossed the curve for chemotherapy alone. Progressive disease was observed in fewer patients with the immunotherapy combination than with chemotherapy alone.
Longer follow-up needed
In recent years, a large number of treatment options for stage IV NSCLC patients have emerged. In the current report of CheckMate 9LA, the OS curve extended only to 27 months.
As was noted by invited discussant Benjamin Levy, MD, of Johns Hopkins University in Baltimore, it may be premature to put the regimen of two cycles of chemotherapy plus dual checkpoint/CTLA4 blockade in its proper context until follow-up extends for 3-5 years.
It would be ideal to know whether the tail of the OS curve will flatten out.
Do the best you can
Clinical investigators have a responsibility to retain the successes of prior regimens while overcoming the challenges of adverse events. New regimens also need to be practical when applied in general oncology practice.
In 2014, the American poet Maya Angelou advised, “Do the best you can until you know better. Then, when you know better, do better.” In many regards, the immunotherapy-chemotherapy combination tested in CheckMate 9LA appears to do better than preceding regimens.
Further refinements in dose, schedule, and supportive care, as well as real-time reporting of and response to patient-reported outcomes, will likely help us build on the CheckMate 9LA regimen and do even better.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Reck M et al. ASCO 2020, Abstract 9501.
Data from the CheckMate 9LA study suggest the combination amplifies the rapid response expected from chemotherapy and the long-term benefit from immunotherapy. Furthermore, the very limited exposure to chemotherapy appears to mitigate long-term risks.
Martin Reck, MD, PhD, of LungenClinic Grosshansdorf in Germany, reported the data as part of the American Society of Clinical Oncology virtual scientific program (Abstract 9501).
A prior trial, CheckMate 227, demonstrated that nivolumab plus ipilimumab improved overall survival (OS) and durability of response in comparison with conventional chemotherapy in advanced NSCLC, regardless of PD-L1 expression (N Engl J Med 2019; 381:2020-31).
In CheckMate 9LA, researchers tested whether adding a limited course of chemotherapy – just two cycles – could improve outcomes further. Dr. Reck reported that, at the first preplanned interim analysis, the combination met its primary goal of improving OS as well as meeting multiple secondary endpoints.
Details of CheckMate 9LA
CheckMate 9LA included 719 treatment-naive patients with histologically confirmed stage IV or recurrent NSCLC and no known sensitizing alterations in EGFR or ALK. All patients had an Eastern Cooperative Oncology Group performance status of 0 or 1.
Patients received either nivolumab plus ipilimumab at standard NSCLC doses plus two cycles of chemotherapy or chemotherapy alone for four cycles.
The chemotherapy regimen was tailored by histology. Pemetrexed plus either cisplatin or carboplatin, with optional pemetrexed maintenance, was administered to patients with non-squamous histology. Paclitaxel plus carboplatin was chosen for patients with squamous disease.
If there was no disease progression or unacceptable toxicity, patients receiving nivolumab plus ipilimumab could continue immunotherapy for up to 2 years.
Patients were stratified by PD-L1 expression (< 1% vs. ≥ 1%), gender, and histology (squamous vs. non-squamous). Tumor and clinical characteristics were balanced across the trial arms.
The primary endpoint was OS, with secondary endpoints of progression-free survival, objective response rate by blinded independent central review, and efficacy by PD-L1 subgroups. Exploratory endpoints included safety/tolerability.
Results prompt FDA approval
Dr. Reck and colleagues found significantly better OS with nivolumab-ipilimumab plus chemotherapy, in comparison with chemotherapy alone (hazard ratio, 0.69; P = .0006).
With longer follow-up (minimum 12.7 months), nivolumab-ipilimumab plus chemotherapy continued to provide longer OS compared with chemotherapy alone. The median OS was 15.6 months and 10.9 months, respectively (HR, 0.66).
Despite more patients receiving subsequent systemic therapy in the chemotherapy-alone arm (34% of whom eventually received an immune checkpoint inhibitor), the immunotherapy-chemotherapy arm still yielded superior OS in the overall population.
One-year OS rates were 63% in the immunotherapy arm and 47% in the chemotherapy-alone arm.
Statistically significant improvements in progression-free survival and objective response rate were seen. The median response duration was 11.3 months in the immunotherapy arm and 5.6 months in the chemotherapy-alone arm.
Benefit was consistent by all efficacy measures and in all subgroups, including by PD-L1 expression and histology.
Based on the strength of these results, in May, the Food and Drug Administration approved nivolumab plus ipilimumab and two cycles of platinum-doublet chemotherapy for the frontline treatment of patients with metastatic or recurrent NSCLC with no EGFR or ALK genomic tumor aberrations.
Challenges to overcome
In the forest plots for OS, the 70 patients who were 75 years of age and older had inferior survival with the combination regimen, compared with chemotherapy alone.
Grade 3-4 treatment-related toxicity was reported in 47% of patients in the immunotherapy arm and 38% of those in the chemotherapy-alone arm.
With nivolumab-ipilimumab plus chemotherapy, more adverse events were considered serious (25.4% vs. 15%). Furthermore, grade 3-4 adverse events led to a higher rate of treatment discontinuation in the immunotherapy arm than in the chemotherapy-alone arm (16% vs. 5%).
Although cross-trial comparisons are treacherous, in CheckMate 227, only 12% of patients receiving nivolumab plus ipilimumab stopped treatment because of a grade 3-4 adverse event.
Better by design
In the updated analysis of CheckMate 227 (ASCO 2020, Abstract 9500), the nivolumab-ipilimumab regimen showed inferior OS results for the first 6 months of treatment, with more disease progression during that time. However, at 6 months, the OS curves crossed over to become consistently superior for the immunotherapy regimen thereafter.
Platinum-based chemotherapy is thought to augment antitumor immunity by inducing immunogenic cell death, increasing tumor neoantigen expression, and disturbing the immunosuppressive tumor microenvironment that prevents immune detection.
Therefore, CheckMate 9LA incorporated a short exposure to chemotherapy for the patients receiving nivolumab-ipilimumab in an effort to attain rapid disease control and retain the durable OS benefit that was seen with dual immunotherapy in CheckMate 227.
Indeed, in CheckMate 9LA, the Kaplan-Meier curves in both the initial and follow-up OS analyses diverged early in favor of the nivolumab-ipilimumab plus chemotherapy regimen and never crossed the curve for chemotherapy alone. Progressive disease was observed in fewer patients with the immunotherapy combination than with chemotherapy alone.
Longer follow-up needed
In recent years, a large number of treatment options for stage IV NSCLC patients have emerged. In the current report of CheckMate 9LA, the OS curve extended only to 27 months.
As was noted by invited discussant Benjamin Levy, MD, of Johns Hopkins University in Baltimore, it may be premature to put the regimen of two cycles of chemotherapy plus dual checkpoint/CTLA4 blockade in its proper context until follow-up extends for 3-5 years.
It would be ideal to know whether the tail of the OS curve will flatten out.
Do the best you can
Clinical investigators have a responsibility to retain the successes of prior regimens while overcoming the challenges of adverse events. New regimens also need to be practical when applied in general oncology practice.
In 2014, the American poet Maya Angelou advised, “Do the best you can until you know better. Then, when you know better, do better.” In many regards, the immunotherapy-chemotherapy combination tested in CheckMate 9LA appears to do better than preceding regimens.
Further refinements in dose, schedule, and supportive care, as well as real-time reporting of and response to patient-reported outcomes, will likely help us build on the CheckMate 9LA regimen and do even better.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Reck M et al. ASCO 2020, Abstract 9501.
FROM ASCO 2020
VIALE-A confirms survival benefit for venetoclax-azacitidine in hard-to-treat AML
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
FROM EHA CONGRESS
FDA makes Ilaris the first approved treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA), making it the first approved treatment for AOSD, according to an FDA announcement.
The approval comes under a Priority Review designation that used “comparable pharmacokinetic exposure and extrapolation of established efficacy of canakinumab in patients with sJIA, as well as the safety of canakinumab in patients with AOSD and other diseases,” the FDA said.
The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab.
AOSD and sJIA share certain similarities, such as fever, arthritis, rash, and elevated markers of inflammation, which has led to suspicion that they are part of a continuum rather than wholly distinct, according to the agency. In addition, the role of interleukin-1 is well established in both diseases and is blocked by canakinumab.
The most common side effects (occurring in greater than 10% of patients) in sJIA studies included infections, abdominal pain, and injection-site reactions. Serious infections (e.g., pneumonia, varicella, gastroenteritis, measles, sepsis, otitis media, sinusitis, adenovirus, lymph node abscess, pharyngitis) were observed in approximately 4%-5%, according to the full prescribing information.
Canakinumab is also approved for the periodic fever syndromes of cryopyrin-associated periodic syndromes in adults and children aged 4 years and older (including familial cold auto-inflammatory syndrome and Muckle-Wells syndrome), tumor necrosis factor receptor associated periodic syndrome in adult and pediatric patients, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency in adult and pediatric patients, and familial Mediterranean fever in adult and pediatric patients.
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA), making it the first approved treatment for AOSD, according to an FDA announcement.
The approval comes under a Priority Review designation that used “comparable pharmacokinetic exposure and extrapolation of established efficacy of canakinumab in patients with sJIA, as well as the safety of canakinumab in patients with AOSD and other diseases,” the FDA said.
The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab.
AOSD and sJIA share certain similarities, such as fever, arthritis, rash, and elevated markers of inflammation, which has led to suspicion that they are part of a continuum rather than wholly distinct, according to the agency. In addition, the role of interleukin-1 is well established in both diseases and is blocked by canakinumab.
The most common side effects (occurring in greater than 10% of patients) in sJIA studies included infections, abdominal pain, and injection-site reactions. Serious infections (e.g., pneumonia, varicella, gastroenteritis, measles, sepsis, otitis media, sinusitis, adenovirus, lymph node abscess, pharyngitis) were observed in approximately 4%-5%, according to the full prescribing information.
Canakinumab is also approved for the periodic fever syndromes of cryopyrin-associated periodic syndromes in adults and children aged 4 years and older (including familial cold auto-inflammatory syndrome and Muckle-Wells syndrome), tumor necrosis factor receptor associated periodic syndrome in adult and pediatric patients, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency in adult and pediatric patients, and familial Mediterranean fever in adult and pediatric patients.
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA), making it the first approved treatment for AOSD, according to an FDA announcement.
The approval comes under a Priority Review designation that used “comparable pharmacokinetic exposure and extrapolation of established efficacy of canakinumab in patients with sJIA, as well as the safety of canakinumab in patients with AOSD and other diseases,” the FDA said.
The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab.
AOSD and sJIA share certain similarities, such as fever, arthritis, rash, and elevated markers of inflammation, which has led to suspicion that they are part of a continuum rather than wholly distinct, according to the agency. In addition, the role of interleukin-1 is well established in both diseases and is blocked by canakinumab.
The most common side effects (occurring in greater than 10% of patients) in sJIA studies included infections, abdominal pain, and injection-site reactions. Serious infections (e.g., pneumonia, varicella, gastroenteritis, measles, sepsis, otitis media, sinusitis, adenovirus, lymph node abscess, pharyngitis) were observed in approximately 4%-5%, according to the full prescribing information.
Canakinumab is also approved for the periodic fever syndromes of cryopyrin-associated periodic syndromes in adults and children aged 4 years and older (including familial cold auto-inflammatory syndrome and Muckle-Wells syndrome), tumor necrosis factor receptor associated periodic syndrome in adult and pediatric patients, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency in adult and pediatric patients, and familial Mediterranean fever in adult and pediatric patients.
Preventing arrhythmias and QTc prolongation in COVID-19 patients on psychotropics
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Face mask type matters when sterilizing, study finds
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
Ecchymotic patches
This patient’s circular ecchymotic patches were due to cupping. One of the clues that this was iatrogenic was the regular and repeated pattern on the skin.
Cupping is a centuries old treatment for pain relief (among other things) that involves applying glass globes or other hollow materials to the skin to create a vacuum. Traditionally, this vacuum is created by heating the air inside the vessel and then holding the vessel in place as the air cools. Practitioners may also use more modern instruments to induce the vacuum that are similar to those used to assist in vaginal deliveries. The mechanical devices leave these circular ecchymotic marks. The ecchymosis fades over time, and this procedure has been shown to significantly reduce myofascial neck and back pain in small trials.
It is important to recognize geometric patterns that are iatrogenic or due to abuse when evaluating skin findings. If skin findings do not follow dermatomal distributions, typical exanthem, or other classic patterns or presentations, there is the possibility that the pattern may be the result of neglect or abuse. On inspection, consider whether an odd pattern may have been caused from a belt buckle, striking instrument, furniture, medical equipment, or a hand strike.
This patient’s findings were consistent with his history of visiting a physical therapist for cupping. No treatment was required; the patient’s back pain from his car accident was improving, and the cupping marks were not troubling him.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Wang YT, Qi Y, Tang FY, et al. The effect of cupping therapy for low back pain: a meta-analysis based on existing randomized controlled trials. J Back Musculoskelet Rehabil. 2017;30:1187-1195.
This patient’s circular ecchymotic patches were due to cupping. One of the clues that this was iatrogenic was the regular and repeated pattern on the skin.
Cupping is a centuries old treatment for pain relief (among other things) that involves applying glass globes or other hollow materials to the skin to create a vacuum. Traditionally, this vacuum is created by heating the air inside the vessel and then holding the vessel in place as the air cools. Practitioners may also use more modern instruments to induce the vacuum that are similar to those used to assist in vaginal deliveries. The mechanical devices leave these circular ecchymotic marks. The ecchymosis fades over time, and this procedure has been shown to significantly reduce myofascial neck and back pain in small trials.
It is important to recognize geometric patterns that are iatrogenic or due to abuse when evaluating skin findings. If skin findings do not follow dermatomal distributions, typical exanthem, or other classic patterns or presentations, there is the possibility that the pattern may be the result of neglect or abuse. On inspection, consider whether an odd pattern may have been caused from a belt buckle, striking instrument, furniture, medical equipment, or a hand strike.
This patient’s findings were consistent with his history of visiting a physical therapist for cupping. No treatment was required; the patient’s back pain from his car accident was improving, and the cupping marks were not troubling him.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
This patient’s circular ecchymotic patches were due to cupping. One of the clues that this was iatrogenic was the regular and repeated pattern on the skin.
Cupping is a centuries old treatment for pain relief (among other things) that involves applying glass globes or other hollow materials to the skin to create a vacuum. Traditionally, this vacuum is created by heating the air inside the vessel and then holding the vessel in place as the air cools. Practitioners may also use more modern instruments to induce the vacuum that are similar to those used to assist in vaginal deliveries. The mechanical devices leave these circular ecchymotic marks. The ecchymosis fades over time, and this procedure has been shown to significantly reduce myofascial neck and back pain in small trials.
It is important to recognize geometric patterns that are iatrogenic or due to abuse when evaluating skin findings. If skin findings do not follow dermatomal distributions, typical exanthem, or other classic patterns or presentations, there is the possibility that the pattern may be the result of neglect or abuse. On inspection, consider whether an odd pattern may have been caused from a belt buckle, striking instrument, furniture, medical equipment, or a hand strike.
This patient’s findings were consistent with his history of visiting a physical therapist for cupping. No treatment was required; the patient’s back pain from his car accident was improving, and the cupping marks were not troubling him.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Wang YT, Qi Y, Tang FY, et al. The effect of cupping therapy for low back pain: a meta-analysis based on existing randomized controlled trials. J Back Musculoskelet Rehabil. 2017;30:1187-1195.
Wang YT, Qi Y, Tang FY, et al. The effect of cupping therapy for low back pain: a meta-analysis based on existing randomized controlled trials. J Back Musculoskelet Rehabil. 2017;30:1187-1195.
Coronavirus impact on medical education: Thoughts from two GI fellows’ perspectives
Introduction
We are living in an unprecedented time. During March 2020, in response to the COVID-19 (coronavirus disease 2019) outbreak, our institution removed all medical students from rotations with direct patient contact to prioritize their safety and well-being, following recommendations made by the Association of American Medical Colleges (AAMC).1 Similarly, we as gastroenterology fellows experienced an upheaval in our usual schedules and routines. Some of us were redeployed to other areas of the hospital, such as inpatient wards and emergency departments, to meet the needs of our patients and our health system. These changes were difficult, not only because we were practicing in different roles, but also because unknown situations commonly incite fear and anxiety.
Among the repercussions of the COVID-19 pandemic were the changes thrust upon medical students who suddenly found themselves without clinical exposure (both on core clerkships and electives) for the duration of the academic year.2 We too lost many of our educational and teaching opportunities as we adapted to our changing circumstances and new reality. Therefore, . We used the lessons we learned because of the changes in our own medical education to anticipate the best ways to provide learning opportunities for our students.
GI fellows’ experiences
The changes to our schedules and lack of in-person educational conferences seemingly happened overnight – the shock of being pulled from clinics, consults, and endoscopy left us feeling scared and lonely. We were quickly transitioned from knowing our roles and responsibilities as GI providers to taking over care for hospitalist patients as the “primary team,” working in the COVID emergency department (ED), and losing our clinic space. Redeployment to other clinical environments was anxiety-provoking. Self-doubt and fear were the most cited concerns as we asked ourselves: Do I remember enough general medicine to be an effective hospitalist? How do I place admission orders or perform a medication reconciliation on discharge? What can I expect in the COVID ED? Will I have to intubate someone? What about possible PPE shortages? Are my family members safe at home? Should I stay in a hotel? Do we have estimates on how long this will last?
Clinical schedules were reconfigured to consolidate the use of inpatient fellows and allow for reserves of fellows to be redeployed if needed. Schedules for the following 7 days were made just 48 hours prior to the start of each workweek. The anticipation and fear of the unknown were perhaps the hardest parts of the changes in our clinical learning environment. Little time was provided to make child care arrangements, coordinate with the schedules of significant others, or review topics and skills we might need in the next week that had gone unused for some time.
Our conference schedule was pared down considerably as fellows and attendings adjusted to their new responsibilities and a virtual platform for fellows’ education. While the transition to online lectures was seamless, the spirit of conference certainly changed. Impromptu questions and conversations that oftentimes arise organically during case conferences no longer occurred as virtual meetings do not offer the same space to foster these discussions as we awkwardly muted and unmuted ourselves. Participation in lectures seemed disjointed, which translated in some ways to less effective learning opportunities. Our involvement in endoscopy was also removed as only urgent cases were being performed and PPE conservation was of the utmost priority. This was especially concerning for third-year fellows on the cusp of graduation who would soon be independent practitioners without recent procedural practice. In general, the fellowship felt isolated and uncertain, which our program director addressed with weekly virtual COVID-19 “happy hour” updates.
GI fellows’ contribution
As our program encouraged us to come together during this time to support each other, we realized that while our clinical duties may look different during the COVID-19 crisis, our responsibility to learners was more important than ever. At many academic institutions, GI fellows are referred to as “the face of the division” owed in large part to our consistent presence on consult services and roles as teachers for medical students and residents who rotate with us. In an effort to assist the medical school’s charge to rapidly generate at-home curriculum for our students, we created an online curriculum for medical students to complete during the time they were previously scheduled to rotate with us on consults either as third- or fourth-year students.
We designed a series of interactive podcasts covering six topics that are commonly encountered issues on the GI consult service: upper GI bleeding, lower GI bleeding, biliary sepsis, acute pancreatitis, chronic diarrhea with a new diagnosis of inflammatory bowel disease, as well as cirrhosis and its associated complications.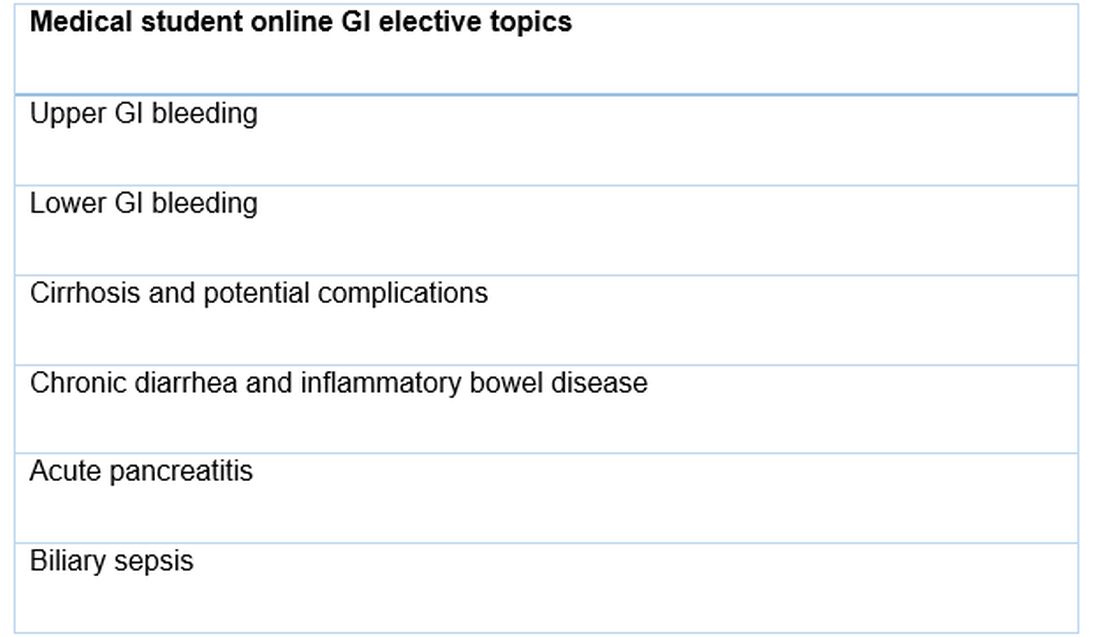
Conclusion
The COVID-19 pandemic brought about significant change in the daily activities of GI fellows including new responsibilities and a great need for adaptation. We hope that the lessons the COVID-19 pandemic has taught us – to think of others and make our talents available to those who need them, to look for ways to adapt to challenges, to live in the present but focus on the future, and to spread creativity when able – will continue long after the curve has flattened.
References
1. Murphy B. American Medical Association website. https://www.ama-assn.org/residents-students/medical-school-life/online-learning-during-covid-19-tips-help-med-students. Apr 3, 2020.
2. Murphy B. American Medical Association website. https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools. Mar 20, 2020.
3. “H5P: Create, share and reuse interactive HTML5 content in your browser.” H5P website. https://h5p.org.
Dr. Bhavsar-Burke and Dr. Jansson-Knodell are GI fellows in the division of gastroenterology and hepatology, department of medicine, Indiana University, Indianapolis. The authors have no conflicts of interest.
Introduction
We are living in an unprecedented time. During March 2020, in response to the COVID-19 (coronavirus disease 2019) outbreak, our institution removed all medical students from rotations with direct patient contact to prioritize their safety and well-being, following recommendations made by the Association of American Medical Colleges (AAMC).1 Similarly, we as gastroenterology fellows experienced an upheaval in our usual schedules and routines. Some of us were redeployed to other areas of the hospital, such as inpatient wards and emergency departments, to meet the needs of our patients and our health system. These changes were difficult, not only because we were practicing in different roles, but also because unknown situations commonly incite fear and anxiety.
Among the repercussions of the COVID-19 pandemic were the changes thrust upon medical students who suddenly found themselves without clinical exposure (both on core clerkships and electives) for the duration of the academic year.2 We too lost many of our educational and teaching opportunities as we adapted to our changing circumstances and new reality. Therefore, . We used the lessons we learned because of the changes in our own medical education to anticipate the best ways to provide learning opportunities for our students.
GI fellows’ experiences
The changes to our schedules and lack of in-person educational conferences seemingly happened overnight – the shock of being pulled from clinics, consults, and endoscopy left us feeling scared and lonely. We were quickly transitioned from knowing our roles and responsibilities as GI providers to taking over care for hospitalist patients as the “primary team,” working in the COVID emergency department (ED), and losing our clinic space. Redeployment to other clinical environments was anxiety-provoking. Self-doubt and fear were the most cited concerns as we asked ourselves: Do I remember enough general medicine to be an effective hospitalist? How do I place admission orders or perform a medication reconciliation on discharge? What can I expect in the COVID ED? Will I have to intubate someone? What about possible PPE shortages? Are my family members safe at home? Should I stay in a hotel? Do we have estimates on how long this will last?
Clinical schedules were reconfigured to consolidate the use of inpatient fellows and allow for reserves of fellows to be redeployed if needed. Schedules for the following 7 days were made just 48 hours prior to the start of each workweek. The anticipation and fear of the unknown were perhaps the hardest parts of the changes in our clinical learning environment. Little time was provided to make child care arrangements, coordinate with the schedules of significant others, or review topics and skills we might need in the next week that had gone unused for some time.
Our conference schedule was pared down considerably as fellows and attendings adjusted to their new responsibilities and a virtual platform for fellows’ education. While the transition to online lectures was seamless, the spirit of conference certainly changed. Impromptu questions and conversations that oftentimes arise organically during case conferences no longer occurred as virtual meetings do not offer the same space to foster these discussions as we awkwardly muted and unmuted ourselves. Participation in lectures seemed disjointed, which translated in some ways to less effective learning opportunities. Our involvement in endoscopy was also removed as only urgent cases were being performed and PPE conservation was of the utmost priority. This was especially concerning for third-year fellows on the cusp of graduation who would soon be independent practitioners without recent procedural practice. In general, the fellowship felt isolated and uncertain, which our program director addressed with weekly virtual COVID-19 “happy hour” updates.
GI fellows’ contribution
As our program encouraged us to come together during this time to support each other, we realized that while our clinical duties may look different during the COVID-19 crisis, our responsibility to learners was more important than ever. At many academic institutions, GI fellows are referred to as “the face of the division” owed in large part to our consistent presence on consult services and roles as teachers for medical students and residents who rotate with us. In an effort to assist the medical school’s charge to rapidly generate at-home curriculum for our students, we created an online curriculum for medical students to complete during the time they were previously scheduled to rotate with us on consults either as third- or fourth-year students.
We designed a series of interactive podcasts covering six topics that are commonly encountered issues on the GI consult service: upper GI bleeding, lower GI bleeding, biliary sepsis, acute pancreatitis, chronic diarrhea with a new diagnosis of inflammatory bowel disease, as well as cirrhosis and its associated complications.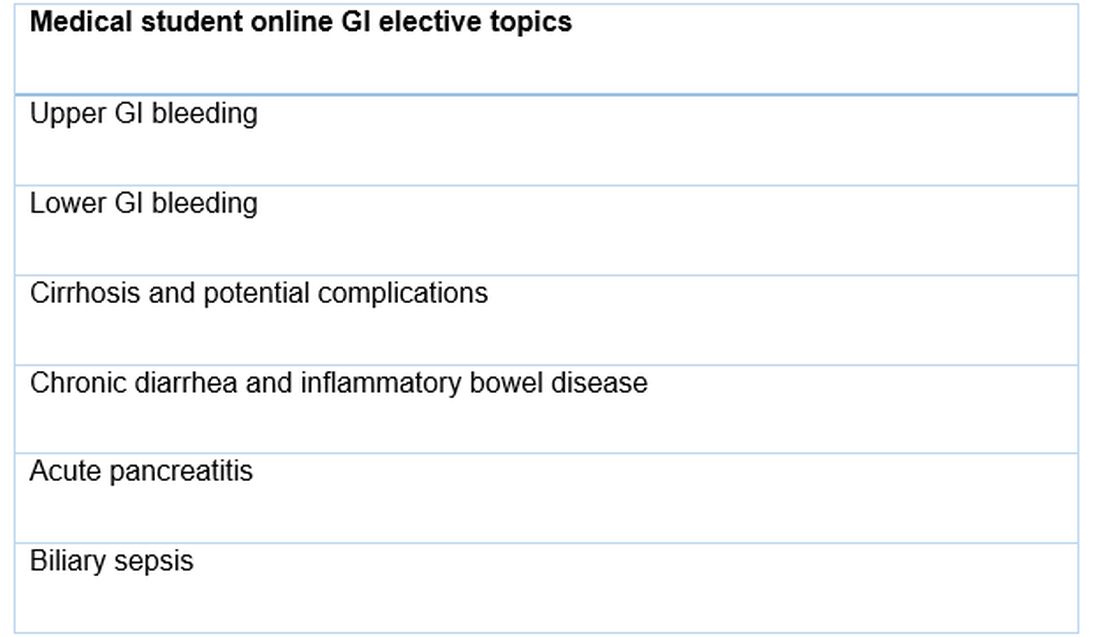
Conclusion
The COVID-19 pandemic brought about significant change in the daily activities of GI fellows including new responsibilities and a great need for adaptation. We hope that the lessons the COVID-19 pandemic has taught us – to think of others and make our talents available to those who need them, to look for ways to adapt to challenges, to live in the present but focus on the future, and to spread creativity when able – will continue long after the curve has flattened.
References
1. Murphy B. American Medical Association website. https://www.ama-assn.org/residents-students/medical-school-life/online-learning-during-covid-19-tips-help-med-students. Apr 3, 2020.
2. Murphy B. American Medical Association website. https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools. Mar 20, 2020.
3. “H5P: Create, share and reuse interactive HTML5 content in your browser.” H5P website. https://h5p.org.
Dr. Bhavsar-Burke and Dr. Jansson-Knodell are GI fellows in the division of gastroenterology and hepatology, department of medicine, Indiana University, Indianapolis. The authors have no conflicts of interest.
Introduction
We are living in an unprecedented time. During March 2020, in response to the COVID-19 (coronavirus disease 2019) outbreak, our institution removed all medical students from rotations with direct patient contact to prioritize their safety and well-being, following recommendations made by the Association of American Medical Colleges (AAMC).1 Similarly, we as gastroenterology fellows experienced an upheaval in our usual schedules and routines. Some of us were redeployed to other areas of the hospital, such as inpatient wards and emergency departments, to meet the needs of our patients and our health system. These changes were difficult, not only because we were practicing in different roles, but also because unknown situations commonly incite fear and anxiety.
Among the repercussions of the COVID-19 pandemic were the changes thrust upon medical students who suddenly found themselves without clinical exposure (both on core clerkships and electives) for the duration of the academic year.2 We too lost many of our educational and teaching opportunities as we adapted to our changing circumstances and new reality. Therefore, . We used the lessons we learned because of the changes in our own medical education to anticipate the best ways to provide learning opportunities for our students.
GI fellows’ experiences
The changes to our schedules and lack of in-person educational conferences seemingly happened overnight – the shock of being pulled from clinics, consults, and endoscopy left us feeling scared and lonely. We were quickly transitioned from knowing our roles and responsibilities as GI providers to taking over care for hospitalist patients as the “primary team,” working in the COVID emergency department (ED), and losing our clinic space. Redeployment to other clinical environments was anxiety-provoking. Self-doubt and fear were the most cited concerns as we asked ourselves: Do I remember enough general medicine to be an effective hospitalist? How do I place admission orders or perform a medication reconciliation on discharge? What can I expect in the COVID ED? Will I have to intubate someone? What about possible PPE shortages? Are my family members safe at home? Should I stay in a hotel? Do we have estimates on how long this will last?
Clinical schedules were reconfigured to consolidate the use of inpatient fellows and allow for reserves of fellows to be redeployed if needed. Schedules for the following 7 days were made just 48 hours prior to the start of each workweek. The anticipation and fear of the unknown were perhaps the hardest parts of the changes in our clinical learning environment. Little time was provided to make child care arrangements, coordinate with the schedules of significant others, or review topics and skills we might need in the next week that had gone unused for some time.
Our conference schedule was pared down considerably as fellows and attendings adjusted to their new responsibilities and a virtual platform for fellows’ education. While the transition to online lectures was seamless, the spirit of conference certainly changed. Impromptu questions and conversations that oftentimes arise organically during case conferences no longer occurred as virtual meetings do not offer the same space to foster these discussions as we awkwardly muted and unmuted ourselves. Participation in lectures seemed disjointed, which translated in some ways to less effective learning opportunities. Our involvement in endoscopy was also removed as only urgent cases were being performed and PPE conservation was of the utmost priority. This was especially concerning for third-year fellows on the cusp of graduation who would soon be independent practitioners without recent procedural practice. In general, the fellowship felt isolated and uncertain, which our program director addressed with weekly virtual COVID-19 “happy hour” updates.
GI fellows’ contribution
As our program encouraged us to come together during this time to support each other, we realized that while our clinical duties may look different during the COVID-19 crisis, our responsibility to learners was more important than ever. At many academic institutions, GI fellows are referred to as “the face of the division” owed in large part to our consistent presence on consult services and roles as teachers for medical students and residents who rotate with us. In an effort to assist the medical school’s charge to rapidly generate at-home curriculum for our students, we created an online curriculum for medical students to complete during the time they were previously scheduled to rotate with us on consults either as third- or fourth-year students.
We designed a series of interactive podcasts covering six topics that are commonly encountered issues on the GI consult service: upper GI bleeding, lower GI bleeding, biliary sepsis, acute pancreatitis, chronic diarrhea with a new diagnosis of inflammatory bowel disease, as well as cirrhosis and its associated complications.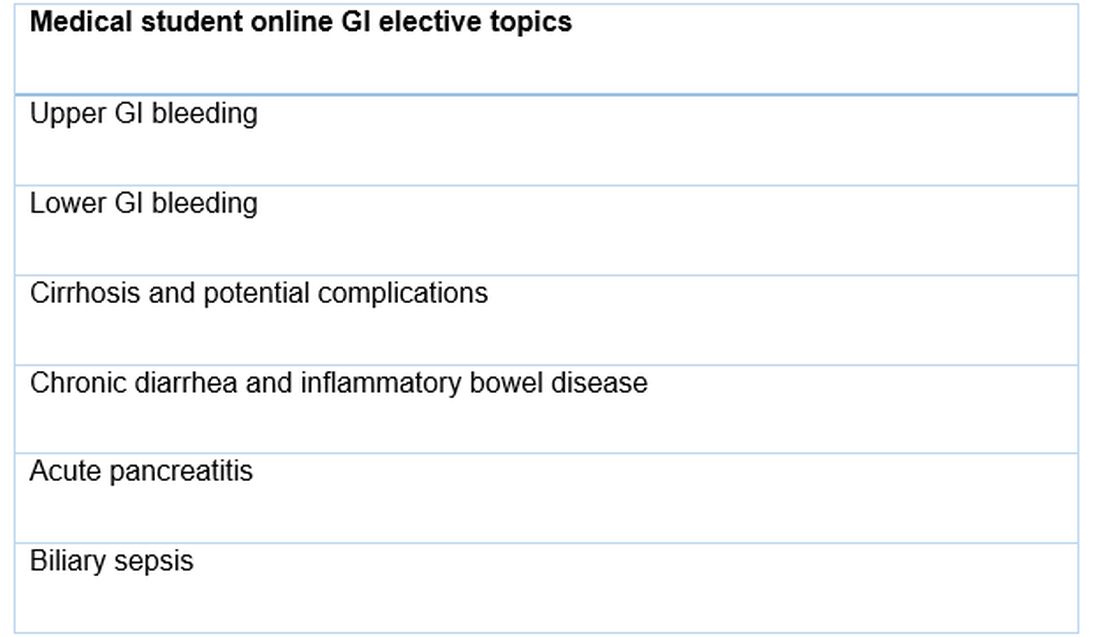
Conclusion
The COVID-19 pandemic brought about significant change in the daily activities of GI fellows including new responsibilities and a great need for adaptation. We hope that the lessons the COVID-19 pandemic has taught us – to think of others and make our talents available to those who need them, to look for ways to adapt to challenges, to live in the present but focus on the future, and to spread creativity when able – will continue long after the curve has flattened.
References
1. Murphy B. American Medical Association website. https://www.ama-assn.org/residents-students/medical-school-life/online-learning-during-covid-19-tips-help-med-students. Apr 3, 2020.
2. Murphy B. American Medical Association website. https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools. Mar 20, 2020.
3. “H5P: Create, share and reuse interactive HTML5 content in your browser.” H5P website. https://h5p.org.
Dr. Bhavsar-Burke and Dr. Jansson-Knodell are GI fellows in the division of gastroenterology and hepatology, department of medicine, Indiana University, Indianapolis. The authors have no conflicts of interest.
Daily Recap 6/17
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Getting unstuck: Helping patients with behavior change
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at pdnews@mdedge.com.
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at pdnews@mdedge.com.
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at pdnews@mdedge.com.
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).