User login
Single negative colonoscopy predicts low colorectal cancer risk
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
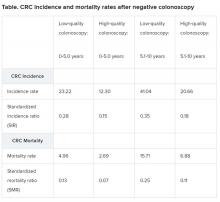
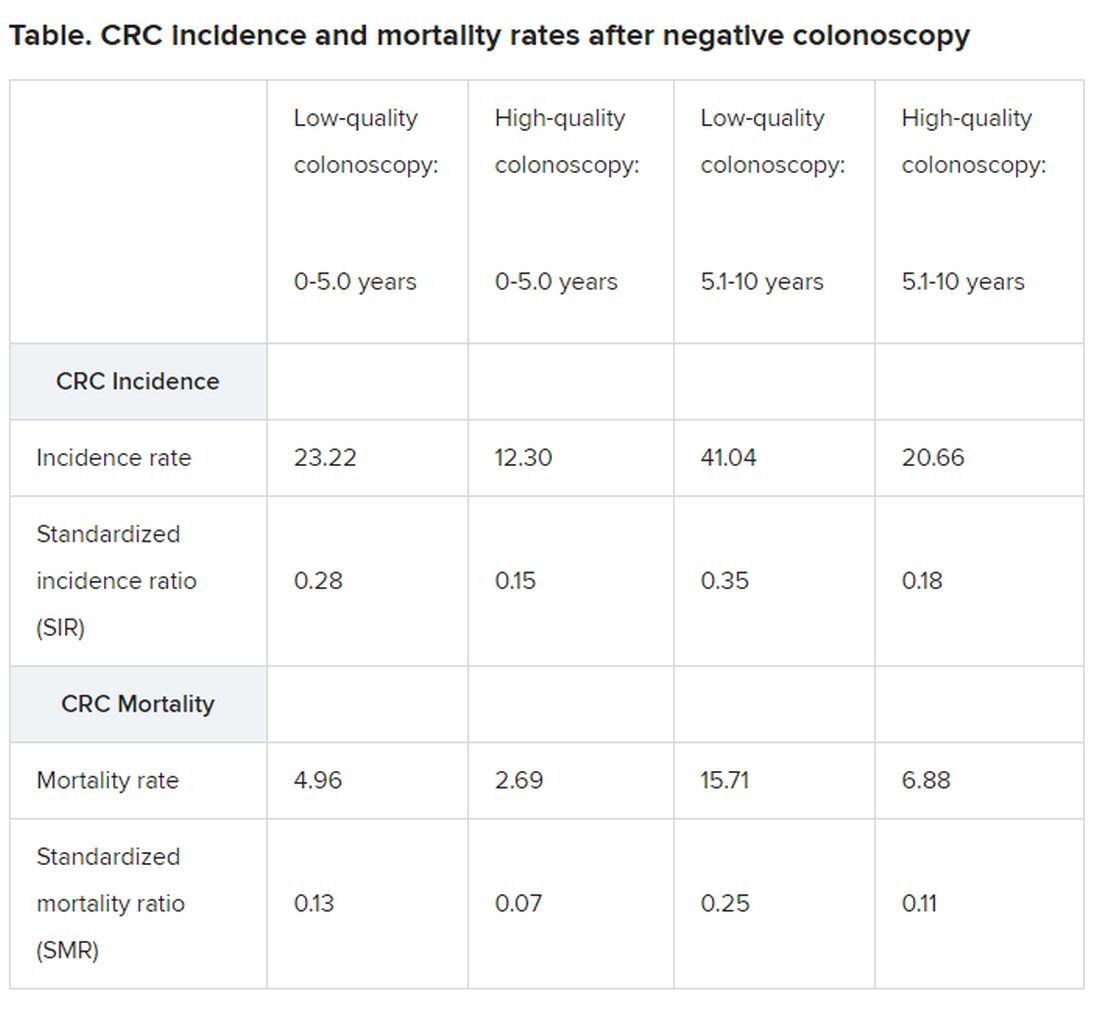
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
Robotic and manual total knee arthroplasty found at least comparable
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
FROM aaos 2020
Movement-based yoga ‘viable’ for depression in many mental disorders
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Psychiatrists assess geriatric harm from social distancing
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
Suicide often associated with bullying in LGBTQ youth
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
FROM JAMA PEDIATRICS
Primary care practices struggle to survive despite visit rebound
Primary care practices are facing an existential threat, and they need government help now if they are to survive.
That was the main message at a teleconference held on May 20 to announce the results of a study showing that outpatient visits have rebounded across the United States. Having dropped 60% from their prepandemic level in early April, office visits are now significantly higher but are still 30% less than the baseline, on average, according to new data from the Commonwealth Fund, Harvard University, and Phreesia, a health information technology firm.
The outpatient visits study shows that most of the recovery was attributable to a rise in in-person visits, not telehealth encounters, which have plateaued. The rebound was more pronounced in some regions, like the South and Southwest, than in others, such as New England and the Mid-Atlantic.
the study shows. While some other specialties have seen a greater drop-off in visits, speakers at the news conference drew reporters’ attention to the financial plight of primary care.
“Primary care practices are in dire straits, and their ability to treat patients is under threat,” said Melinda Abrams, MS, senior vice president of delivery system reform and international innovations for the Commonwealth Fund. “In the long term, an investment in primary care will ensure we have primary care, because we are concerned about its collapse.”
Health policy experts from the Commonwealth Fund and other organizations, she said, propose that the next round of federal economic stimulus funding include recovery resources dedicated to primary care practices, especially small practices and those in underserved areas. She said the money should be distributed immediately through Medicare and Medicaid in supplemental monthly payments.
Up to now, Ms. Abrams said, no money in any of the federal rescue packages has been specifically earmarked for primary care.
Close permanently?
Farzad Mostashari, MD, CEO of Aledade and former national coordinator for health information technology at the U.S. Department of Health & Human Services, agreed primary care needs immediate help.
Aledade’s customers for population health management services, he noted, are some of the most forward-looking and technologically savvy primary care groups. “Nevertheless, those practices are suffering,” Dr. Mostashari said. “Many of them are at risk financially. There has been a massive 60%-70% drop in face-to-face visits. About 40% of visits are telehealth, but the practices are still down 30% or more in visits. And they’re losing ancillary revenues from procedures and labs.”
The financial devastation of the pandemic is causing some physicians to question whether they will be able to stay in practice. A recent survey from the California Healthcare Foundation found that a third of California primary care doctors are worried their practices will be forced to close permanently because of the financial impact of COVID-19. Many doctors said their practices had furloughed or laid off staff or that they’d been forced to take pay cuts.
Similarly, a recent survey by the Patient-Centered Primary Care Collaborative found that 13% of practices predicted closure within the next month and that 20% have already had temporary closures. Forty-two percent of the practices have laid off or furloughed staff, and 51% are uncertain about their financial future through June.
Primary care is essential
A pandemic-related reduction in the number of primary care physicians would exacerbate what many observers view as a nationwide shortage of primary care. Right now, the health care system badly needs all the primary care doctors it has, Ms. Abrams and Dr. Mostashari said.
Decades of research have shown that strong primary care is associated with better outcomes, lower per capita costs, and greater equity, Ms. Abrams noted. In addition, she said, dedicated support for primary care during the pandemic will help ensure that doctors meet the needs of patients with chronic diseases so they don’t have to be hospitalized.
Moreover, with proper support, primary care physicians can expand COVID-19 testing “so we can reopen the economy and perhaps prevent or contain the second wave of the virus,” she said.
Dr. Mostashari pointed out that primary care providers are on the front line of the pandemic. Although much attention has been rightfully given to those who treat COVID-19 patients in hospitals, he observed, “before those patients are admitted, they need to see primary care physicians. ... We have to maintain the primary care first line of defense. When the CDC says if you’re having symptoms, call your doctor, someone has to pick up the phone at the other end.”
In addition, he said, “there’s a hidden pandemic of untreated chronic conditions we should all be worried about. We know primary care is important because if you don’t do prevention, you’ll pay the price in heart attacks and strokes and kidney failure, and we’ve seen a dramatic decline in primary care services. In New York City, some people who have avoided necessary care have had bad outcomes, including in-home cardiac death.”
Dr. Mostashari also argued that the negative financial impact of COVID-19 could lead to a further consolidation of the industry as health systems and private equity investors take over failing practices. Past experience suggests that that would result in “a lack of choice, a lack of competition, and a lack of access” in many cases, he said.
The best long-term solution, he said, is to pay primary care physicians capitation instead of on a fee-for-service basis so that they’re not dependent on income from face-to-face visits.
In the short term, however, they need direct cash payments, Dr. Mostashari said. He called on Congress to allocate at least $15 billion to bolster the viability of primary care practices.
Telehealth levels off
One of the key findings of the outpatient visits study is that telehealth encounters, after soaring in the early days of the pandemic, have leveled off. After hitting a peak of 14% of all visits in mid-April, telehealth visits now make up about 12% of the total.
Study coauthor Ateev Mehrotra, MD, MPH, an associate professor of health policy and medicine at Harvard Medical School, Boston, said he’d expected the use of telehealth to continue rising. The fact that it hasn’t, he told reporters at the news conference, may be related to the different ways in which practices conduct virtual encounters.
“Some practices are using HIPAA-compliant [telehealth] platforms and training their patients on how to use those platforms,” Dr. Mehrotra noted. “Other clinics are mainly just phoning patients. You could envision those practices could easily revert back to in-person visits, because a phone call is going to be limited in many cases. Also, practices need to know whether payers will keep covering telehealth after the pandemic is over.”
The study shows that in-person visits, which declined more than total visits in March and early April, are now increasing at about the same rate as total visits. However, in-person visits are still down by more than 40%.
Asked whether financially vulnerable practices will be able to afford the safeguards that medical societies recommend to resume in-person visits, Dr. Mostashari pointed out that Medicare is now paying $28 to collect a COVID-19 specimen from a patient.
“Just the cost of changing PPE, plus disinfecting the room or setting up a separate room or testing facility: Those expenses are not included. We should have better accounting on what it actually costs to run a practice in the time of COVID. It’s not the same as their earlier operating costs.”
Dr. Mehrotra agreed. “You also can’t have 20 people in your waiting room or the throughput you had previously. So the number of patients you’ll be able to see will be lower because of appropriate restrictions.”
A version of this article originally appeared on Medscape.com.
Primary care practices are facing an existential threat, and they need government help now if they are to survive.
That was the main message at a teleconference held on May 20 to announce the results of a study showing that outpatient visits have rebounded across the United States. Having dropped 60% from their prepandemic level in early April, office visits are now significantly higher but are still 30% less than the baseline, on average, according to new data from the Commonwealth Fund, Harvard University, and Phreesia, a health information technology firm.
The outpatient visits study shows that most of the recovery was attributable to a rise in in-person visits, not telehealth encounters, which have plateaued. The rebound was more pronounced in some regions, like the South and Southwest, than in others, such as New England and the Mid-Atlantic.
the study shows. While some other specialties have seen a greater drop-off in visits, speakers at the news conference drew reporters’ attention to the financial plight of primary care.
“Primary care practices are in dire straits, and their ability to treat patients is under threat,” said Melinda Abrams, MS, senior vice president of delivery system reform and international innovations for the Commonwealth Fund. “In the long term, an investment in primary care will ensure we have primary care, because we are concerned about its collapse.”
Health policy experts from the Commonwealth Fund and other organizations, she said, propose that the next round of federal economic stimulus funding include recovery resources dedicated to primary care practices, especially small practices and those in underserved areas. She said the money should be distributed immediately through Medicare and Medicaid in supplemental monthly payments.
Up to now, Ms. Abrams said, no money in any of the federal rescue packages has been specifically earmarked for primary care.
Close permanently?
Farzad Mostashari, MD, CEO of Aledade and former national coordinator for health information technology at the U.S. Department of Health & Human Services, agreed primary care needs immediate help.
Aledade’s customers for population health management services, he noted, are some of the most forward-looking and technologically savvy primary care groups. “Nevertheless, those practices are suffering,” Dr. Mostashari said. “Many of them are at risk financially. There has been a massive 60%-70% drop in face-to-face visits. About 40% of visits are telehealth, but the practices are still down 30% or more in visits. And they’re losing ancillary revenues from procedures and labs.”
The financial devastation of the pandemic is causing some physicians to question whether they will be able to stay in practice. A recent survey from the California Healthcare Foundation found that a third of California primary care doctors are worried their practices will be forced to close permanently because of the financial impact of COVID-19. Many doctors said their practices had furloughed or laid off staff or that they’d been forced to take pay cuts.
Similarly, a recent survey by the Patient-Centered Primary Care Collaborative found that 13% of practices predicted closure within the next month and that 20% have already had temporary closures. Forty-two percent of the practices have laid off or furloughed staff, and 51% are uncertain about their financial future through June.
Primary care is essential
A pandemic-related reduction in the number of primary care physicians would exacerbate what many observers view as a nationwide shortage of primary care. Right now, the health care system badly needs all the primary care doctors it has, Ms. Abrams and Dr. Mostashari said.
Decades of research have shown that strong primary care is associated with better outcomes, lower per capita costs, and greater equity, Ms. Abrams noted. In addition, she said, dedicated support for primary care during the pandemic will help ensure that doctors meet the needs of patients with chronic diseases so they don’t have to be hospitalized.
Moreover, with proper support, primary care physicians can expand COVID-19 testing “so we can reopen the economy and perhaps prevent or contain the second wave of the virus,” she said.
Dr. Mostashari pointed out that primary care providers are on the front line of the pandemic. Although much attention has been rightfully given to those who treat COVID-19 patients in hospitals, he observed, “before those patients are admitted, they need to see primary care physicians. ... We have to maintain the primary care first line of defense. When the CDC says if you’re having symptoms, call your doctor, someone has to pick up the phone at the other end.”
In addition, he said, “there’s a hidden pandemic of untreated chronic conditions we should all be worried about. We know primary care is important because if you don’t do prevention, you’ll pay the price in heart attacks and strokes and kidney failure, and we’ve seen a dramatic decline in primary care services. In New York City, some people who have avoided necessary care have had bad outcomes, including in-home cardiac death.”
Dr. Mostashari also argued that the negative financial impact of COVID-19 could lead to a further consolidation of the industry as health systems and private equity investors take over failing practices. Past experience suggests that that would result in “a lack of choice, a lack of competition, and a lack of access” in many cases, he said.
The best long-term solution, he said, is to pay primary care physicians capitation instead of on a fee-for-service basis so that they’re not dependent on income from face-to-face visits.
In the short term, however, they need direct cash payments, Dr. Mostashari said. He called on Congress to allocate at least $15 billion to bolster the viability of primary care practices.
Telehealth levels off
One of the key findings of the outpatient visits study is that telehealth encounters, after soaring in the early days of the pandemic, have leveled off. After hitting a peak of 14% of all visits in mid-April, telehealth visits now make up about 12% of the total.
Study coauthor Ateev Mehrotra, MD, MPH, an associate professor of health policy and medicine at Harvard Medical School, Boston, said he’d expected the use of telehealth to continue rising. The fact that it hasn’t, he told reporters at the news conference, may be related to the different ways in which practices conduct virtual encounters.
“Some practices are using HIPAA-compliant [telehealth] platforms and training their patients on how to use those platforms,” Dr. Mehrotra noted. “Other clinics are mainly just phoning patients. You could envision those practices could easily revert back to in-person visits, because a phone call is going to be limited in many cases. Also, practices need to know whether payers will keep covering telehealth after the pandemic is over.”
The study shows that in-person visits, which declined more than total visits in March and early April, are now increasing at about the same rate as total visits. However, in-person visits are still down by more than 40%.
Asked whether financially vulnerable practices will be able to afford the safeguards that medical societies recommend to resume in-person visits, Dr. Mostashari pointed out that Medicare is now paying $28 to collect a COVID-19 specimen from a patient.
“Just the cost of changing PPE, plus disinfecting the room or setting up a separate room or testing facility: Those expenses are not included. We should have better accounting on what it actually costs to run a practice in the time of COVID. It’s not the same as their earlier operating costs.”
Dr. Mehrotra agreed. “You also can’t have 20 people in your waiting room or the throughput you had previously. So the number of patients you’ll be able to see will be lower because of appropriate restrictions.”
A version of this article originally appeared on Medscape.com.
Primary care practices are facing an existential threat, and they need government help now if they are to survive.
That was the main message at a teleconference held on May 20 to announce the results of a study showing that outpatient visits have rebounded across the United States. Having dropped 60% from their prepandemic level in early April, office visits are now significantly higher but are still 30% less than the baseline, on average, according to new data from the Commonwealth Fund, Harvard University, and Phreesia, a health information technology firm.
The outpatient visits study shows that most of the recovery was attributable to a rise in in-person visits, not telehealth encounters, which have plateaued. The rebound was more pronounced in some regions, like the South and Southwest, than in others, such as New England and the Mid-Atlantic.
the study shows. While some other specialties have seen a greater drop-off in visits, speakers at the news conference drew reporters’ attention to the financial plight of primary care.
“Primary care practices are in dire straits, and their ability to treat patients is under threat,” said Melinda Abrams, MS, senior vice president of delivery system reform and international innovations for the Commonwealth Fund. “In the long term, an investment in primary care will ensure we have primary care, because we are concerned about its collapse.”
Health policy experts from the Commonwealth Fund and other organizations, she said, propose that the next round of federal economic stimulus funding include recovery resources dedicated to primary care practices, especially small practices and those in underserved areas. She said the money should be distributed immediately through Medicare and Medicaid in supplemental monthly payments.
Up to now, Ms. Abrams said, no money in any of the federal rescue packages has been specifically earmarked for primary care.
Close permanently?
Farzad Mostashari, MD, CEO of Aledade and former national coordinator for health information technology at the U.S. Department of Health & Human Services, agreed primary care needs immediate help.
Aledade’s customers for population health management services, he noted, are some of the most forward-looking and technologically savvy primary care groups. “Nevertheless, those practices are suffering,” Dr. Mostashari said. “Many of them are at risk financially. There has been a massive 60%-70% drop in face-to-face visits. About 40% of visits are telehealth, but the practices are still down 30% or more in visits. And they’re losing ancillary revenues from procedures and labs.”
The financial devastation of the pandemic is causing some physicians to question whether they will be able to stay in practice. A recent survey from the California Healthcare Foundation found that a third of California primary care doctors are worried their practices will be forced to close permanently because of the financial impact of COVID-19. Many doctors said their practices had furloughed or laid off staff or that they’d been forced to take pay cuts.
Similarly, a recent survey by the Patient-Centered Primary Care Collaborative found that 13% of practices predicted closure within the next month and that 20% have already had temporary closures. Forty-two percent of the practices have laid off or furloughed staff, and 51% are uncertain about their financial future through June.
Primary care is essential
A pandemic-related reduction in the number of primary care physicians would exacerbate what many observers view as a nationwide shortage of primary care. Right now, the health care system badly needs all the primary care doctors it has, Ms. Abrams and Dr. Mostashari said.
Decades of research have shown that strong primary care is associated with better outcomes, lower per capita costs, and greater equity, Ms. Abrams noted. In addition, she said, dedicated support for primary care during the pandemic will help ensure that doctors meet the needs of patients with chronic diseases so they don’t have to be hospitalized.
Moreover, with proper support, primary care physicians can expand COVID-19 testing “so we can reopen the economy and perhaps prevent or contain the second wave of the virus,” she said.
Dr. Mostashari pointed out that primary care providers are on the front line of the pandemic. Although much attention has been rightfully given to those who treat COVID-19 patients in hospitals, he observed, “before those patients are admitted, they need to see primary care physicians. ... We have to maintain the primary care first line of defense. When the CDC says if you’re having symptoms, call your doctor, someone has to pick up the phone at the other end.”
In addition, he said, “there’s a hidden pandemic of untreated chronic conditions we should all be worried about. We know primary care is important because if you don’t do prevention, you’ll pay the price in heart attacks and strokes and kidney failure, and we’ve seen a dramatic decline in primary care services. In New York City, some people who have avoided necessary care have had bad outcomes, including in-home cardiac death.”
Dr. Mostashari also argued that the negative financial impact of COVID-19 could lead to a further consolidation of the industry as health systems and private equity investors take over failing practices. Past experience suggests that that would result in “a lack of choice, a lack of competition, and a lack of access” in many cases, he said.
The best long-term solution, he said, is to pay primary care physicians capitation instead of on a fee-for-service basis so that they’re not dependent on income from face-to-face visits.
In the short term, however, they need direct cash payments, Dr. Mostashari said. He called on Congress to allocate at least $15 billion to bolster the viability of primary care practices.
Telehealth levels off
One of the key findings of the outpatient visits study is that telehealth encounters, after soaring in the early days of the pandemic, have leveled off. After hitting a peak of 14% of all visits in mid-April, telehealth visits now make up about 12% of the total.
Study coauthor Ateev Mehrotra, MD, MPH, an associate professor of health policy and medicine at Harvard Medical School, Boston, said he’d expected the use of telehealth to continue rising. The fact that it hasn’t, he told reporters at the news conference, may be related to the different ways in which practices conduct virtual encounters.
“Some practices are using HIPAA-compliant [telehealth] platforms and training their patients on how to use those platforms,” Dr. Mehrotra noted. “Other clinics are mainly just phoning patients. You could envision those practices could easily revert back to in-person visits, because a phone call is going to be limited in many cases. Also, practices need to know whether payers will keep covering telehealth after the pandemic is over.”
The study shows that in-person visits, which declined more than total visits in March and early April, are now increasing at about the same rate as total visits. However, in-person visits are still down by more than 40%.
Asked whether financially vulnerable practices will be able to afford the safeguards that medical societies recommend to resume in-person visits, Dr. Mostashari pointed out that Medicare is now paying $28 to collect a COVID-19 specimen from a patient.
“Just the cost of changing PPE, plus disinfecting the room or setting up a separate room or testing facility: Those expenses are not included. We should have better accounting on what it actually costs to run a practice in the time of COVID. It’s not the same as their earlier operating costs.”
Dr. Mehrotra agreed. “You also can’t have 20 people in your waiting room or the throughput you had previously. So the number of patients you’ll be able to see will be lower because of appropriate restrictions.”
A version of this article originally appeared on Medscape.com.
Biologic approved for atopic dermatitis in children
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
Family physicians have lowest incentive bonuses, survey finds
according to the Medscape Family Medicine Physician Compensation Report 2020.
This year’s survey was the first to ask about bonuses, and it showed strong contrasts between specialties. Family physicians’ bonuses averaged $24,000, whereas orthopedists’ were four times higher, at $96,000.
Two-thirds of family physicians (67%), similar to physicians overall, reported that bonuses had no influence on the number of hours worked.
More than half of all physicians in the survey (56%) said they got such bonuses.
Family physicians’ pay was up $3,000 from last year, to $234,000, but still ranked near the bottom in comparison with other specialties. Only physicians in public health/preventive medicine and pediatrics made less, both at $232,000.
The top four specialties in pay were the same this year as they were last year and ranked in the same order: Orthopedists made the most, at $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000).
However, the compensation picture is changing for all physicians. This report reflects data gathered between Oct. 4, 2019, and Feb. 10, 2020. Since that time, the COVID-19 crisis has reversed income gains for physicians overall. In a study from the Medical Group Management Association, researchers estimated that more than half of medical practices reported a drop in revenue by early April of 55% and a drop in patient volume of 60%.
Male family physicians continue to make more than their female colleagues, with this year’s difference at 26% ($257,000 vs. $205,000). Male specialists overall in the survey made 31% more than their female counterparts.
Few claims denied
A bright spot in compensation was that family physicians have among the lowest rates (14%) of claims that are denied or that need to be resubmitted. Plastic surgeons have twice that rate (28%) of rejected claims.
The survey authors noted, “One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.”
Family physicians were in the middle of the pack as far as how much time was spent on paperwork. On average, they spent 15.9 hours a week on the tasks. Intensivists spent the most, at 19.1 hours each week, and ophthalmologists spent the least, at 9.8 hours per week.
Although 73% of physicians overall said they had no plans to stop accepting new and current Medicare and Medicaid patients, only 65% of family physicians answered that way. Seventeen percent said they would stop taking new Medicare patients, and 9% said they wouldn’t take new Medicaid patients; 15% had not made those decisions yet.
Rules and regulations are the biggest challenges
Asked about their biggest challenges, 29% of family physicians put “having so many rules and regulations” at the top. Next came working with an electronic health records system, followed by dealing with difficult patients.
The biggest reward, they said again this year, was “gratitude/relationships with patients” (34% ranked it at the top), followed by “knowing I’m making the world a better place” (25%), “being very good at what I do/finding answers, diagnoses” (18%), and “making good money at a job that I like” (10%).
Most family practices employ advanced practice providers (62% employed NPs, and 43% employed PAs). Fewer than one-third employed neither.
Of the family medicine physicians who did work with advanced practice providers in their offices, half (50%) said they improved profitability, 45% said they had no effect, and 5% said they decreased profitability.
A version of this article originally appeared on Medscape.com.
according to the Medscape Family Medicine Physician Compensation Report 2020.
This year’s survey was the first to ask about bonuses, and it showed strong contrasts between specialties. Family physicians’ bonuses averaged $24,000, whereas orthopedists’ were four times higher, at $96,000.
Two-thirds of family physicians (67%), similar to physicians overall, reported that bonuses had no influence on the number of hours worked.
More than half of all physicians in the survey (56%) said they got such bonuses.
Family physicians’ pay was up $3,000 from last year, to $234,000, but still ranked near the bottom in comparison with other specialties. Only physicians in public health/preventive medicine and pediatrics made less, both at $232,000.
The top four specialties in pay were the same this year as they were last year and ranked in the same order: Orthopedists made the most, at $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000).
However, the compensation picture is changing for all physicians. This report reflects data gathered between Oct. 4, 2019, and Feb. 10, 2020. Since that time, the COVID-19 crisis has reversed income gains for physicians overall. In a study from the Medical Group Management Association, researchers estimated that more than half of medical practices reported a drop in revenue by early April of 55% and a drop in patient volume of 60%.
Male family physicians continue to make more than their female colleagues, with this year’s difference at 26% ($257,000 vs. $205,000). Male specialists overall in the survey made 31% more than their female counterparts.
Few claims denied
A bright spot in compensation was that family physicians have among the lowest rates (14%) of claims that are denied or that need to be resubmitted. Plastic surgeons have twice that rate (28%) of rejected claims.
The survey authors noted, “One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.”
Family physicians were in the middle of the pack as far as how much time was spent on paperwork. On average, they spent 15.9 hours a week on the tasks. Intensivists spent the most, at 19.1 hours each week, and ophthalmologists spent the least, at 9.8 hours per week.
Although 73% of physicians overall said they had no plans to stop accepting new and current Medicare and Medicaid patients, only 65% of family physicians answered that way. Seventeen percent said they would stop taking new Medicare patients, and 9% said they wouldn’t take new Medicaid patients; 15% had not made those decisions yet.
Rules and regulations are the biggest challenges
Asked about their biggest challenges, 29% of family physicians put “having so many rules and regulations” at the top. Next came working with an electronic health records system, followed by dealing with difficult patients.
The biggest reward, they said again this year, was “gratitude/relationships with patients” (34% ranked it at the top), followed by “knowing I’m making the world a better place” (25%), “being very good at what I do/finding answers, diagnoses” (18%), and “making good money at a job that I like” (10%).
Most family practices employ advanced practice providers (62% employed NPs, and 43% employed PAs). Fewer than one-third employed neither.
Of the family medicine physicians who did work with advanced practice providers in their offices, half (50%) said they improved profitability, 45% said they had no effect, and 5% said they decreased profitability.
A version of this article originally appeared on Medscape.com.
according to the Medscape Family Medicine Physician Compensation Report 2020.
This year’s survey was the first to ask about bonuses, and it showed strong contrasts between specialties. Family physicians’ bonuses averaged $24,000, whereas orthopedists’ were four times higher, at $96,000.
Two-thirds of family physicians (67%), similar to physicians overall, reported that bonuses had no influence on the number of hours worked.
More than half of all physicians in the survey (56%) said they got such bonuses.
Family physicians’ pay was up $3,000 from last year, to $234,000, but still ranked near the bottom in comparison with other specialties. Only physicians in public health/preventive medicine and pediatrics made less, both at $232,000.
The top four specialties in pay were the same this year as they were last year and ranked in the same order: Orthopedists made the most, at $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000).
However, the compensation picture is changing for all physicians. This report reflects data gathered between Oct. 4, 2019, and Feb. 10, 2020. Since that time, the COVID-19 crisis has reversed income gains for physicians overall. In a study from the Medical Group Management Association, researchers estimated that more than half of medical practices reported a drop in revenue by early April of 55% and a drop in patient volume of 60%.
Male family physicians continue to make more than their female colleagues, with this year’s difference at 26% ($257,000 vs. $205,000). Male specialists overall in the survey made 31% more than their female counterparts.
Few claims denied
A bright spot in compensation was that family physicians have among the lowest rates (14%) of claims that are denied or that need to be resubmitted. Plastic surgeons have twice that rate (28%) of rejected claims.
The survey authors noted, “One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.”
Family physicians were in the middle of the pack as far as how much time was spent on paperwork. On average, they spent 15.9 hours a week on the tasks. Intensivists spent the most, at 19.1 hours each week, and ophthalmologists spent the least, at 9.8 hours per week.
Although 73% of physicians overall said they had no plans to stop accepting new and current Medicare and Medicaid patients, only 65% of family physicians answered that way. Seventeen percent said they would stop taking new Medicare patients, and 9% said they wouldn’t take new Medicaid patients; 15% had not made those decisions yet.
Rules and regulations are the biggest challenges
Asked about their biggest challenges, 29% of family physicians put “having so many rules and regulations” at the top. Next came working with an electronic health records system, followed by dealing with difficult patients.
The biggest reward, they said again this year, was “gratitude/relationships with patients” (34% ranked it at the top), followed by “knowing I’m making the world a better place” (25%), “being very good at what I do/finding answers, diagnoses” (18%), and “making good money at a job that I like” (10%).
Most family practices employ advanced practice providers (62% employed NPs, and 43% employed PAs). Fewer than one-third employed neither.
Of the family medicine physicians who did work with advanced practice providers in their offices, half (50%) said they improved profitability, 45% said they had no effect, and 5% said they decreased profitability.
A version of this article originally appeared on Medscape.com.
Social isolation tied to higher risk of cardiovascular events, death
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
FROM EAN 2020
More evidence hydroxychloroquine is ineffective, harmful in COVID-19
Hydroxychloroquine and chloroquine, with or without azithromycin or clarithromycin, offer no benefit in treating patients with COVID-19 and, instead, are associated with ventricular arrhythmias and higher rates of mortality, according to a major new international study.
In the largest observational study of its kind, including close to 100,000 people in 671 hospitals on six continents, investigators compared outcomes in 15,000 patients with COVID-19 treated with hydroxychloroquine and chloroquine alone or in combination with a macrolide with 80,000 control patients with COVID-19 not receiving these agents.
Treatment with any of these medications, either alone or in combination, was associated with increased death during hospitalization; compared with about 10% in control group patients, mortality rates ranged from more than 16% to almost 24% in the treated groups.
Patients treated with hydroxychloroquine plus a macrolide showed the highest rates of serious cardiac arrhythmias, and, even after accounting for demographic factors and comorbidities, this combination was found to be associated with a more than 5-fold increase in the risk of developing a serious arrhythmia while in the hospital.
“In this real-world study, the biggest yet, we looked at 100,000 patients [with COVID-19] across six continents and found not the slightest hint of benefits and only risks, and the data is pretty straightforward,” study coauthor Frank Ruschitzka, MD, director of the Heart Center at University Hospital, Zürich, said in an interview. The study was published online May 22 in The Lancet.
‘Inconclusive’ evidence
The absence of an effective treatment for COVID-19 has led to the “repurposing” of the antimalarial drug chloroquine and its analogue hydroxychloroquine, which is used for treating autoimmune disease, but this approach is based on anecdotal evidence or open-label randomized trials that have been “largely inconclusive,” the authors wrote.
Additional agents used to treat COVID-19 are second-generation macrolides (azithromycin or clarithromycin), in combination with chloroquine or hydroxychloroquine, “despite limited evidence” and the risk for ventricular arrhythmias, the authors noted.
“Our primary question was whether there was any associated benefits of the use of hydroxychloroquine, chloroquine, or a combined regimen with macrolides in treating COVID-19, and — if there was no benefit — would there be harm?” lead author Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine, Brigham and Women’s Hospital, Boston, said in an interview.
The investigators used data from a multinational registry comprising 671 hospitals that included patients (n = 96,032; mean age 53.8 years; 46.3% female) who had been hospitalized between Dec. 20, 2019, and April 14, 2020, with confirmed COVID-19 infection.
They also collected data about demographics, underlying comorbidities, and medical history, and medications that patients were taking at baseline.
Patients receiving treatment (n = 14,888) were divided into four groups: those receiving chloroquine alone (n = 1,868), those receiving chloroquine with a macrolide (n = 3,783), those receiving hydroxychloroquine alone (n = 3,016) and those receiving hydroxychloroquine with a macrolide (n = 6,221).
The remaining patients not treated with these regimens (n = 81,144) were regarded as the control group.
Most patients (65.9%) came from North America, followed by Europe (17.39%), Asia (7.9%), Africa (4.6%), South America (3.7%), and Australia (0.6%). Most (66.9%) were white, followed by patients of Asian origin (14.1%), black patients (9.4%), and Hispanic patients (6.2%).
Comorbidities and underlying conditions included obesity, hyperlipidemia, and hypertension in about 30%.
Comorbidities and underlying conditions
The investigators conducted multiple analyses to control for confounding variables, including Cox proportional hazards regression and propensity score matching analyses.
“In an observational study, there is always a chance of residual confounding, which is why we did propensity score based matched analyses,” Dr. Ruschitzka explained.
No significant differences were found in distribution of demographics and comorbidities between the groups.
As good as it gets
“We found no benefit in any of the four treatment regimens for hospitalized patients with COVID-19, but we did notice higher rates of death and serious ventricular arrhythmias in these patients, compared to the controls,” Dr. Mehra reported.
Of the patients in the control group, roughly 9.3% died during their hospitalization, compared with 16.4% of patients treated with chloroquine alone, 18.0% of those treated with hydroxychloroquine alone, 22.2% of those treated with chloroquine and a macrolide, and 23.8% of those treated with hydroxychloroquine and a macrolide.
After accounting for confounding variables, the researchers estimated that the excess mortality risk attributable to use of the drug regimen ranged from 34% to 45%.
Patients treated with any of the four regimens sustained more serious arrhythmias, compared with those in the control group (0.35), with the biggest increase seen in the group treated with the combination of hydroxychloroquine plus a macrolide (8.1%), followed by chloroquine with a macrolide (6.5%), hydroxychloroquine alone (6.1%), and chloroquine alone (4.3%).
“We were fairly reassured that, although the study was observational, the signals were robust and consistent across all regions of the world in diverse populations, and we did not see any muting of that signal, depending on region,” Dr. Mehra said.
“Two months ago, we were all scratching our heads about how to treat patients with COVID-19, and then came a drug [hydroxychloroquine] with some anecdotal evidence, but now we have 2 months more experience, and we looked to science to provide some answer,” Dr. Ruschitzka said.
“Although this was not a randomized, controlled trial, so we do not have a definite answer, the data provided in this [large, multinational] real-world study is as good as it gets and the best data we have,” he concluded.
“Let the science speak for itself”
Commenting on the study in an interview, Christian Funck-Brentano, MD, from the Hospital Pitié-Salpêtrière and Sorbonne University, both in Paris, said that, although the study is observational and therefore not as reliable as a randomized controlled trial, it is “nevertheless well-documented, studied a huge amount of people, and utilized several sensitivity methods, all of which showed the same results.”
Dr. Funck-Brentano, who is the coauthor of an accompanying editorial in The Lancet and was not involved with the study, said that “we now have no evidence that hydroxychloroquine and chloroquine alone or in combination with a macrolide do any good and we have potential evidence that they do harm and kill people.”
Also commenting on the study in an interview, David Holtgrave, PhD, dean of the School of Public Health at the State University of New York at Albany, said that, “while no one observational study alone would lead to a firm clinical recommendation, I think it is helpful for physicians and public health officials to be aware of the findings of the peer-reviewed observational studies to date and the National Institutes of Health COVID-19 treatment guidelines and the Food and Drug Administration’s statement of drug safety concern about hydroxychloroquine to inform their decision-making as we await the results of randomized clinical trials of these drugs for the treatment of COVID-19,” said Dr. Holtgrave, who was not involved with the study.
He added that, to his knowledge, there are “still no published studies of prophylactic use of these drugs to prevent COVID-19.”
Dr. Mehra emphasized that a cardinal principle of practicing medicine is “first do no harm” and “even in situations where you believe a desperate disease calls for desperate measures, responsible physicians should take a step back and ask if we are doing harm, and until we can say we aren’t, I don’t think it’s wise to push something like this in the absence of good efficacy data.”
Dr. Ruschitzka added that those who are encouraging the use of these agents “should review their decision based on today’s data and let the science speak for itself.”
The study was supported by the William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston. Dr. Mehra reported personal fees from Abbott, Medtronic, Janssen, Mesoblast, Portola, Bayer, Baim Institute for Clinical Research, NuPulseCV, FineHeart, Leviticus, Roivant, and Triple Gene. Dr. Ruschitzka was paid for time spent as a committee member for clinical trials, advisory boards, other forms of consulting, and lectures or presentations; these payments were made directly to the University of Zürich and no personal payments were received in relation to these trials or other activities. Dr. Funck-Brentano, his coauthor, and Dr. Holtgrave declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Hydroxychloroquine and chloroquine, with or without azithromycin or clarithromycin, offer no benefit in treating patients with COVID-19 and, instead, are associated with ventricular arrhythmias and higher rates of mortality, according to a major new international study.
In the largest observational study of its kind, including close to 100,000 people in 671 hospitals on six continents, investigators compared outcomes in 15,000 patients with COVID-19 treated with hydroxychloroquine and chloroquine alone or in combination with a macrolide with 80,000 control patients with COVID-19 not receiving these agents.
Treatment with any of these medications, either alone or in combination, was associated with increased death during hospitalization; compared with about 10% in control group patients, mortality rates ranged from more than 16% to almost 24% in the treated groups.
Patients treated with hydroxychloroquine plus a macrolide showed the highest rates of serious cardiac arrhythmias, and, even after accounting for demographic factors and comorbidities, this combination was found to be associated with a more than 5-fold increase in the risk of developing a serious arrhythmia while in the hospital.
“In this real-world study, the biggest yet, we looked at 100,000 patients [with COVID-19] across six continents and found not the slightest hint of benefits and only risks, and the data is pretty straightforward,” study coauthor Frank Ruschitzka, MD, director of the Heart Center at University Hospital, Zürich, said in an interview. The study was published online May 22 in The Lancet.
‘Inconclusive’ evidence
The absence of an effective treatment for COVID-19 has led to the “repurposing” of the antimalarial drug chloroquine and its analogue hydroxychloroquine, which is used for treating autoimmune disease, but this approach is based on anecdotal evidence or open-label randomized trials that have been “largely inconclusive,” the authors wrote.
Additional agents used to treat COVID-19 are second-generation macrolides (azithromycin or clarithromycin), in combination with chloroquine or hydroxychloroquine, “despite limited evidence” and the risk for ventricular arrhythmias, the authors noted.
“Our primary question was whether there was any associated benefits of the use of hydroxychloroquine, chloroquine, or a combined regimen with macrolides in treating COVID-19, and — if there was no benefit — would there be harm?” lead author Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine, Brigham and Women’s Hospital, Boston, said in an interview.
The investigators used data from a multinational registry comprising 671 hospitals that included patients (n = 96,032; mean age 53.8 years; 46.3% female) who had been hospitalized between Dec. 20, 2019, and April 14, 2020, with confirmed COVID-19 infection.
They also collected data about demographics, underlying comorbidities, and medical history, and medications that patients were taking at baseline.
Patients receiving treatment (n = 14,888) were divided into four groups: those receiving chloroquine alone (n = 1,868), those receiving chloroquine with a macrolide (n = 3,783), those receiving hydroxychloroquine alone (n = 3,016) and those receiving hydroxychloroquine with a macrolide (n = 6,221).
The remaining patients not treated with these regimens (n = 81,144) were regarded as the control group.
Most patients (65.9%) came from North America, followed by Europe (17.39%), Asia (7.9%), Africa (4.6%), South America (3.7%), and Australia (0.6%). Most (66.9%) were white, followed by patients of Asian origin (14.1%), black patients (9.4%), and Hispanic patients (6.2%).
Comorbidities and underlying conditions included obesity, hyperlipidemia, and hypertension in about 30%.
Comorbidities and underlying conditions
The investigators conducted multiple analyses to control for confounding variables, including Cox proportional hazards regression and propensity score matching analyses.
“In an observational study, there is always a chance of residual confounding, which is why we did propensity score based matched analyses,” Dr. Ruschitzka explained.
No significant differences were found in distribution of demographics and comorbidities between the groups.
As good as it gets
“We found no benefit in any of the four treatment regimens for hospitalized patients with COVID-19, but we did notice higher rates of death and serious ventricular arrhythmias in these patients, compared to the controls,” Dr. Mehra reported.
Of the patients in the control group, roughly 9.3% died during their hospitalization, compared with 16.4% of patients treated with chloroquine alone, 18.0% of those treated with hydroxychloroquine alone, 22.2% of those treated with chloroquine and a macrolide, and 23.8% of those treated with hydroxychloroquine and a macrolide.
After accounting for confounding variables, the researchers estimated that the excess mortality risk attributable to use of the drug regimen ranged from 34% to 45%.
Patients treated with any of the four regimens sustained more serious arrhythmias, compared with those in the control group (0.35), with the biggest increase seen in the group treated with the combination of hydroxychloroquine plus a macrolide (8.1%), followed by chloroquine with a macrolide (6.5%), hydroxychloroquine alone (6.1%), and chloroquine alone (4.3%).
“We were fairly reassured that, although the study was observational, the signals were robust and consistent across all regions of the world in diverse populations, and we did not see any muting of that signal, depending on region,” Dr. Mehra said.
“Two months ago, we were all scratching our heads about how to treat patients with COVID-19, and then came a drug [hydroxychloroquine] with some anecdotal evidence, but now we have 2 months more experience, and we looked to science to provide some answer,” Dr. Ruschitzka said.
“Although this was not a randomized, controlled trial, so we do not have a definite answer, the data provided in this [large, multinational] real-world study is as good as it gets and the best data we have,” he concluded.
“Let the science speak for itself”
Commenting on the study in an interview, Christian Funck-Brentano, MD, from the Hospital Pitié-Salpêtrière and Sorbonne University, both in Paris, said that, although the study is observational and therefore not as reliable as a randomized controlled trial, it is “nevertheless well-documented, studied a huge amount of people, and utilized several sensitivity methods, all of which showed the same results.”
Dr. Funck-Brentano, who is the coauthor of an accompanying editorial in The Lancet and was not involved with the study, said that “we now have no evidence that hydroxychloroquine and chloroquine alone or in combination with a macrolide do any good and we have potential evidence that they do harm and kill people.”
Also commenting on the study in an interview, David Holtgrave, PhD, dean of the School of Public Health at the State University of New York at Albany, said that, “while no one observational study alone would lead to a firm clinical recommendation, I think it is helpful for physicians and public health officials to be aware of the findings of the peer-reviewed observational studies to date and the National Institutes of Health COVID-19 treatment guidelines and the Food and Drug Administration’s statement of drug safety concern about hydroxychloroquine to inform their decision-making as we await the results of randomized clinical trials of these drugs for the treatment of COVID-19,” said Dr. Holtgrave, who was not involved with the study.
He added that, to his knowledge, there are “still no published studies of prophylactic use of these drugs to prevent COVID-19.”
Dr. Mehra emphasized that a cardinal principle of practicing medicine is “first do no harm” and “even in situations where you believe a desperate disease calls for desperate measures, responsible physicians should take a step back and ask if we are doing harm, and until we can say we aren’t, I don’t think it’s wise to push something like this in the absence of good efficacy data.”
Dr. Ruschitzka added that those who are encouraging the use of these agents “should review their decision based on today’s data and let the science speak for itself.”
The study was supported by the William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston. Dr. Mehra reported personal fees from Abbott, Medtronic, Janssen, Mesoblast, Portola, Bayer, Baim Institute for Clinical Research, NuPulseCV, FineHeart, Leviticus, Roivant, and Triple Gene. Dr. Ruschitzka was paid for time spent as a committee member for clinical trials, advisory boards, other forms of consulting, and lectures or presentations; these payments were made directly to the University of Zürich and no personal payments were received in relation to these trials or other activities. Dr. Funck-Brentano, his coauthor, and Dr. Holtgrave declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Hydroxychloroquine and chloroquine, with or without azithromycin or clarithromycin, offer no benefit in treating patients with COVID-19 and, instead, are associated with ventricular arrhythmias and higher rates of mortality, according to a major new international study.
In the largest observational study of its kind, including close to 100,000 people in 671 hospitals on six continents, investigators compared outcomes in 15,000 patients with COVID-19 treated with hydroxychloroquine and chloroquine alone or in combination with a macrolide with 80,000 control patients with COVID-19 not receiving these agents.
Treatment with any of these medications, either alone or in combination, was associated with increased death during hospitalization; compared with about 10% in control group patients, mortality rates ranged from more than 16% to almost 24% in the treated groups.
Patients treated with hydroxychloroquine plus a macrolide showed the highest rates of serious cardiac arrhythmias, and, even after accounting for demographic factors and comorbidities, this combination was found to be associated with a more than 5-fold increase in the risk of developing a serious arrhythmia while in the hospital.
“In this real-world study, the biggest yet, we looked at 100,000 patients [with COVID-19] across six continents and found not the slightest hint of benefits and only risks, and the data is pretty straightforward,” study coauthor Frank Ruschitzka, MD, director of the Heart Center at University Hospital, Zürich, said in an interview. The study was published online May 22 in The Lancet.
‘Inconclusive’ evidence
The absence of an effective treatment for COVID-19 has led to the “repurposing” of the antimalarial drug chloroquine and its analogue hydroxychloroquine, which is used for treating autoimmune disease, but this approach is based on anecdotal evidence or open-label randomized trials that have been “largely inconclusive,” the authors wrote.
Additional agents used to treat COVID-19 are second-generation macrolides (azithromycin or clarithromycin), in combination with chloroquine or hydroxychloroquine, “despite limited evidence” and the risk for ventricular arrhythmias, the authors noted.
“Our primary question was whether there was any associated benefits of the use of hydroxychloroquine, chloroquine, or a combined regimen with macrolides in treating COVID-19, and — if there was no benefit — would there be harm?” lead author Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine, Brigham and Women’s Hospital, Boston, said in an interview.
The investigators used data from a multinational registry comprising 671 hospitals that included patients (n = 96,032; mean age 53.8 years; 46.3% female) who had been hospitalized between Dec. 20, 2019, and April 14, 2020, with confirmed COVID-19 infection.
They also collected data about demographics, underlying comorbidities, and medical history, and medications that patients were taking at baseline.
Patients receiving treatment (n = 14,888) were divided into four groups: those receiving chloroquine alone (n = 1,868), those receiving chloroquine with a macrolide (n = 3,783), those receiving hydroxychloroquine alone (n = 3,016) and those receiving hydroxychloroquine with a macrolide (n = 6,221).
The remaining patients not treated with these regimens (n = 81,144) were regarded as the control group.
Most patients (65.9%) came from North America, followed by Europe (17.39%), Asia (7.9%), Africa (4.6%), South America (3.7%), and Australia (0.6%). Most (66.9%) were white, followed by patients of Asian origin (14.1%), black patients (9.4%), and Hispanic patients (6.2%).
Comorbidities and underlying conditions included obesity, hyperlipidemia, and hypertension in about 30%.
Comorbidities and underlying conditions
The investigators conducted multiple analyses to control for confounding variables, including Cox proportional hazards regression and propensity score matching analyses.
“In an observational study, there is always a chance of residual confounding, which is why we did propensity score based matched analyses,” Dr. Ruschitzka explained.
No significant differences were found in distribution of demographics and comorbidities between the groups.
As good as it gets
“We found no benefit in any of the four treatment regimens for hospitalized patients with COVID-19, but we did notice higher rates of death and serious ventricular arrhythmias in these patients, compared to the controls,” Dr. Mehra reported.
Of the patients in the control group, roughly 9.3% died during their hospitalization, compared with 16.4% of patients treated with chloroquine alone, 18.0% of those treated with hydroxychloroquine alone, 22.2% of those treated with chloroquine and a macrolide, and 23.8% of those treated with hydroxychloroquine and a macrolide.
After accounting for confounding variables, the researchers estimated that the excess mortality risk attributable to use of the drug regimen ranged from 34% to 45%.
Patients treated with any of the four regimens sustained more serious arrhythmias, compared with those in the control group (0.35), with the biggest increase seen in the group treated with the combination of hydroxychloroquine plus a macrolide (8.1%), followed by chloroquine with a macrolide (6.5%), hydroxychloroquine alone (6.1%), and chloroquine alone (4.3%).
“We were fairly reassured that, although the study was observational, the signals were robust and consistent across all regions of the world in diverse populations, and we did not see any muting of that signal, depending on region,” Dr. Mehra said.
“Two months ago, we were all scratching our heads about how to treat patients with COVID-19, and then came a drug [hydroxychloroquine] with some anecdotal evidence, but now we have 2 months more experience, and we looked to science to provide some answer,” Dr. Ruschitzka said.
“Although this was not a randomized, controlled trial, so we do not have a definite answer, the data provided in this [large, multinational] real-world study is as good as it gets and the best data we have,” he concluded.
“Let the science speak for itself”
Commenting on the study in an interview, Christian Funck-Brentano, MD, from the Hospital Pitié-Salpêtrière and Sorbonne University, both in Paris, said that, although the study is observational and therefore not as reliable as a randomized controlled trial, it is “nevertheless well-documented, studied a huge amount of people, and utilized several sensitivity methods, all of which showed the same results.”
Dr. Funck-Brentano, who is the coauthor of an accompanying editorial in The Lancet and was not involved with the study, said that “we now have no evidence that hydroxychloroquine and chloroquine alone or in combination with a macrolide do any good and we have potential evidence that they do harm and kill people.”
Also commenting on the study in an interview, David Holtgrave, PhD, dean of the School of Public Health at the State University of New York at Albany, said that, “while no one observational study alone would lead to a firm clinical recommendation, I think it is helpful for physicians and public health officials to be aware of the findings of the peer-reviewed observational studies to date and the National Institutes of Health COVID-19 treatment guidelines and the Food and Drug Administration’s statement of drug safety concern about hydroxychloroquine to inform their decision-making as we await the results of randomized clinical trials of these drugs for the treatment of COVID-19,” said Dr. Holtgrave, who was not involved with the study.
He added that, to his knowledge, there are “still no published studies of prophylactic use of these drugs to prevent COVID-19.”
Dr. Mehra emphasized that a cardinal principle of practicing medicine is “first do no harm” and “even in situations where you believe a desperate disease calls for desperate measures, responsible physicians should take a step back and ask if we are doing harm, and until we can say we aren’t, I don’t think it’s wise to push something like this in the absence of good efficacy data.”
Dr. Ruschitzka added that those who are encouraging the use of these agents “should review their decision based on today’s data and let the science speak for itself.”
The study was supported by the William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston. Dr. Mehra reported personal fees from Abbott, Medtronic, Janssen, Mesoblast, Portola, Bayer, Baim Institute for Clinical Research, NuPulseCV, FineHeart, Leviticus, Roivant, and Triple Gene. Dr. Ruschitzka was paid for time spent as a committee member for clinical trials, advisory boards, other forms of consulting, and lectures or presentations; these payments were made directly to the University of Zürich and no personal payments were received in relation to these trials or other activities. Dr. Funck-Brentano, his coauthor, and Dr. Holtgrave declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.