User login
Caring for Patients with OCD in a Pandemic
When a mass trauma or disaster hit, mental health clinicians often focus on encouraging resilience. In the middle of the COVID-19 pandemic, however, interventions that maintain calm, build community, and sustain hope may take priority, according to a working group of clinical experts from the International College of Obsessive Compulsive Spectrum Disorders and the Obsessive-Compulsive and Related Disorders Research Network of the European College of Neuropsychopharmacology.
While the COVID-19 pandemic has tested everyone, “[p]erhaps no group of individuals with mental illness is as directly affected by the worsening outbreak of COVID-19 as people living with obsessive-compulsive disorder (OCD),” say the group members, who include clinicians from Stanford University, University of California, and VAHCS in Palo Alto. “Paradoxically, they are ‘experts by experience’ in attempting to avert dangers through enacting compulsive behaviors.”
Consequently, coronavirus may become all these patients think about. Some who have contamination-related OCD may express doubts about the rationality of their therapies, while other patients have told their clinicians they were “right all along.” Moreover, people with OCD can be inflexible at “unlearning” danger responses and are thus conditioned to prolonged virus-induced distress and anxiety.
In response to the emerging crisis and growing calls from patients and clinicians, the working group produced a consensus statement with the aim of delivering “pragmatic guidance” for the treatment of OCD under COVID-19 conditions. Their report covers the issues they judged currently most relevant for clinicians.
Stipulating that the best available treatments for most patients are likely to include evidence-based pharmacotherapy and modifying or pausing cognitive behavioral therapy (CBT) in conjunction with enhanced supportive therapies, the panel also recommends:
- Using telemedicine, including telephone or video calls, but be aware of the patient’s circumstances: For some, poverty makes it hard to stay home. Regularly check on patients who are likely to engage in particularly harmful decontamination rituals or behaviors. The added benefit of video calling is that it helps the therapist perform a visual risk evaluation—which is especially valuable for patients living alone—to determine the condition of the patient's hands, presence of food in the fridge or cupboard, etc.
- Taking a careful history, clarifying the extent to which the symptoms represent a rational or exaggerated reaction to recent highly stressful events, or a worsening of the OCD. Don’t assume that every patient with contamination fears related to germs and illness will necessarily be excessively concerned about COVID-19.
- Assessing suicide risk. Factors such as a recent increase in OCD severity, experiencing a family member found positive for COVID-19, or finding the effects of quarantine or isolation distressing have anecdotally been shown to raise suicide risk.
- Providing balanced information about the known risks and impact of COVID-19 on physical and mental health. This includes the difficulties managing uncertainty associated with the virus, which might be particularly challenging for some people with OCD, hypochondriasis or anxiety. Patients need to understand that this health crisis may persist for some time, and they will need to manage their stress levels over that time (eg, by putting into play long-term routines of mindfulness techniques, exercise and structure).
- Inquiring about Internet usage and news consumption. Some patients spend hours a day watching television and online media sources, which may significantly exacerbate OCD and anxiety symptoms. Offer a balanced approach (eg, individuals should not spend more than a half-hour in the morning and at night to stay informed about the pandemic, to minimize the triggering of symptoms). Suggest trusted sources to avoid myths, rumors and misinformation.
- Identifying and discouraging high-risk obsessive-compulsive behaviors, such as washing in water that is too hot or bleach, or total fasting. Some patients, as a result of doubt or uncertainty about whether food in the house is contaminated, respond by throwing everything away and consequently have little or nothing to eat. Encourage eating and drinking to maintain health.
Keeping people calm and reducing the risk of depression using supportive techniques are an essential element of care. Nevertheless, the group says, clinicians should still try to find ways to help patients foster resilience towards obsessional thinking and compulsive acts.
“We are aware this guidance marks a change in practice for many clinicians treating OCD,” they note. “Temporarily modifying or pausing in vivo CBT with ERP [exposure response prevention] for contamination-related OCD, … is a difficult decision to make, but as with any treatment, the benefits and risks need to be balanced up and clear messages that take public health into account need to be given at this time of heightened risk of infection, to avoid confusion. On the other hand, many forms of CBT can be continued with modification for safety as needed.”
Understanding the impact of a pandemic like COVID-19 on patients with mental health disorders can provide important insights into the environmental determinants, the panel says. They urge research-active groups to investigate the effects of such changes on health outcomes—as well as exploring ways to address the expected rise in incidence of OCD once the pandemic is over.
When a mass trauma or disaster hit, mental health clinicians often focus on encouraging resilience. In the middle of the COVID-19 pandemic, however, interventions that maintain calm, build community, and sustain hope may take priority, according to a working group of clinical experts from the International College of Obsessive Compulsive Spectrum Disorders and the Obsessive-Compulsive and Related Disorders Research Network of the European College of Neuropsychopharmacology.
While the COVID-19 pandemic has tested everyone, “[p]erhaps no group of individuals with mental illness is as directly affected by the worsening outbreak of COVID-19 as people living with obsessive-compulsive disorder (OCD),” say the group members, who include clinicians from Stanford University, University of California, and VAHCS in Palo Alto. “Paradoxically, they are ‘experts by experience’ in attempting to avert dangers through enacting compulsive behaviors.”
Consequently, coronavirus may become all these patients think about. Some who have contamination-related OCD may express doubts about the rationality of their therapies, while other patients have told their clinicians they were “right all along.” Moreover, people with OCD can be inflexible at “unlearning” danger responses and are thus conditioned to prolonged virus-induced distress and anxiety.
In response to the emerging crisis and growing calls from patients and clinicians, the working group produced a consensus statement with the aim of delivering “pragmatic guidance” for the treatment of OCD under COVID-19 conditions. Their report covers the issues they judged currently most relevant for clinicians.
Stipulating that the best available treatments for most patients are likely to include evidence-based pharmacotherapy and modifying or pausing cognitive behavioral therapy (CBT) in conjunction with enhanced supportive therapies, the panel also recommends:
- Using telemedicine, including telephone or video calls, but be aware of the patient’s circumstances: For some, poverty makes it hard to stay home. Regularly check on patients who are likely to engage in particularly harmful decontamination rituals or behaviors. The added benefit of video calling is that it helps the therapist perform a visual risk evaluation—which is especially valuable for patients living alone—to determine the condition of the patient's hands, presence of food in the fridge or cupboard, etc.
- Taking a careful history, clarifying the extent to which the symptoms represent a rational or exaggerated reaction to recent highly stressful events, or a worsening of the OCD. Don’t assume that every patient with contamination fears related to germs and illness will necessarily be excessively concerned about COVID-19.
- Assessing suicide risk. Factors such as a recent increase in OCD severity, experiencing a family member found positive for COVID-19, or finding the effects of quarantine or isolation distressing have anecdotally been shown to raise suicide risk.
- Providing balanced information about the known risks and impact of COVID-19 on physical and mental health. This includes the difficulties managing uncertainty associated with the virus, which might be particularly challenging for some people with OCD, hypochondriasis or anxiety. Patients need to understand that this health crisis may persist for some time, and they will need to manage their stress levels over that time (eg, by putting into play long-term routines of mindfulness techniques, exercise and structure).
- Inquiring about Internet usage and news consumption. Some patients spend hours a day watching television and online media sources, which may significantly exacerbate OCD and anxiety symptoms. Offer a balanced approach (eg, individuals should not spend more than a half-hour in the morning and at night to stay informed about the pandemic, to minimize the triggering of symptoms). Suggest trusted sources to avoid myths, rumors and misinformation.
- Identifying and discouraging high-risk obsessive-compulsive behaviors, such as washing in water that is too hot or bleach, or total fasting. Some patients, as a result of doubt or uncertainty about whether food in the house is contaminated, respond by throwing everything away and consequently have little or nothing to eat. Encourage eating and drinking to maintain health.
Keeping people calm and reducing the risk of depression using supportive techniques are an essential element of care. Nevertheless, the group says, clinicians should still try to find ways to help patients foster resilience towards obsessional thinking and compulsive acts.
“We are aware this guidance marks a change in practice for many clinicians treating OCD,” they note. “Temporarily modifying or pausing in vivo CBT with ERP [exposure response prevention] for contamination-related OCD, … is a difficult decision to make, but as with any treatment, the benefits and risks need to be balanced up and clear messages that take public health into account need to be given at this time of heightened risk of infection, to avoid confusion. On the other hand, many forms of CBT can be continued with modification for safety as needed.”
Understanding the impact of a pandemic like COVID-19 on patients with mental health disorders can provide important insights into the environmental determinants, the panel says. They urge research-active groups to investigate the effects of such changes on health outcomes—as well as exploring ways to address the expected rise in incidence of OCD once the pandemic is over.
When a mass trauma or disaster hit, mental health clinicians often focus on encouraging resilience. In the middle of the COVID-19 pandemic, however, interventions that maintain calm, build community, and sustain hope may take priority, according to a working group of clinical experts from the International College of Obsessive Compulsive Spectrum Disorders and the Obsessive-Compulsive and Related Disorders Research Network of the European College of Neuropsychopharmacology.
While the COVID-19 pandemic has tested everyone, “[p]erhaps no group of individuals with mental illness is as directly affected by the worsening outbreak of COVID-19 as people living with obsessive-compulsive disorder (OCD),” say the group members, who include clinicians from Stanford University, University of California, and VAHCS in Palo Alto. “Paradoxically, they are ‘experts by experience’ in attempting to avert dangers through enacting compulsive behaviors.”
Consequently, coronavirus may become all these patients think about. Some who have contamination-related OCD may express doubts about the rationality of their therapies, while other patients have told their clinicians they were “right all along.” Moreover, people with OCD can be inflexible at “unlearning” danger responses and are thus conditioned to prolonged virus-induced distress and anxiety.
In response to the emerging crisis and growing calls from patients and clinicians, the working group produced a consensus statement with the aim of delivering “pragmatic guidance” for the treatment of OCD under COVID-19 conditions. Their report covers the issues they judged currently most relevant for clinicians.
Stipulating that the best available treatments for most patients are likely to include evidence-based pharmacotherapy and modifying or pausing cognitive behavioral therapy (CBT) in conjunction with enhanced supportive therapies, the panel also recommends:
- Using telemedicine, including telephone or video calls, but be aware of the patient’s circumstances: For some, poverty makes it hard to stay home. Regularly check on patients who are likely to engage in particularly harmful decontamination rituals or behaviors. The added benefit of video calling is that it helps the therapist perform a visual risk evaluation—which is especially valuable for patients living alone—to determine the condition of the patient's hands, presence of food in the fridge or cupboard, etc.
- Taking a careful history, clarifying the extent to which the symptoms represent a rational or exaggerated reaction to recent highly stressful events, or a worsening of the OCD. Don’t assume that every patient with contamination fears related to germs and illness will necessarily be excessively concerned about COVID-19.
- Assessing suicide risk. Factors such as a recent increase in OCD severity, experiencing a family member found positive for COVID-19, or finding the effects of quarantine or isolation distressing have anecdotally been shown to raise suicide risk.
- Providing balanced information about the known risks and impact of COVID-19 on physical and mental health. This includes the difficulties managing uncertainty associated with the virus, which might be particularly challenging for some people with OCD, hypochondriasis or anxiety. Patients need to understand that this health crisis may persist for some time, and they will need to manage their stress levels over that time (eg, by putting into play long-term routines of mindfulness techniques, exercise and structure).
- Inquiring about Internet usage and news consumption. Some patients spend hours a day watching television and online media sources, which may significantly exacerbate OCD and anxiety symptoms. Offer a balanced approach (eg, individuals should not spend more than a half-hour in the morning and at night to stay informed about the pandemic, to minimize the triggering of symptoms). Suggest trusted sources to avoid myths, rumors and misinformation.
- Identifying and discouraging high-risk obsessive-compulsive behaviors, such as washing in water that is too hot or bleach, or total fasting. Some patients, as a result of doubt or uncertainty about whether food in the house is contaminated, respond by throwing everything away and consequently have little or nothing to eat. Encourage eating and drinking to maintain health.
Keeping people calm and reducing the risk of depression using supportive techniques are an essential element of care. Nevertheless, the group says, clinicians should still try to find ways to help patients foster resilience towards obsessional thinking and compulsive acts.
“We are aware this guidance marks a change in practice for many clinicians treating OCD,” they note. “Temporarily modifying or pausing in vivo CBT with ERP [exposure response prevention] for contamination-related OCD, … is a difficult decision to make, but as with any treatment, the benefits and risks need to be balanced up and clear messages that take public health into account need to be given at this time of heightened risk of infection, to avoid confusion. On the other hand, many forms of CBT can be continued with modification for safety as needed.”
Understanding the impact of a pandemic like COVID-19 on patients with mental health disorders can provide important insights into the environmental determinants, the panel says. They urge research-active groups to investigate the effects of such changes on health outcomes—as well as exploring ways to address the expected rise in incidence of OCD once the pandemic is over.
AGS issues pandemic resource allocation recommendations amid ageism concerns
The American Geriatrics Society has issued policy recommendations aimed at protecting seniors from ageism when it comes to resource allocation in the current context of treating patients infected with COVID-19.
“The AGS is deeply concerned about Timothy W. Farrell, MD, University of Utah, Salt Lake City, and colleagues wrote in an AGS position statement published online in the Journal of the American Geriatrics Society.
“In particular, rationing strategies that are solely, or predominantly, based on age cutoffs could lead to persistent beliefs that older adults’ lives are less valuable than others or are even expendable, and contribute to already rampant ageism,” the authors continued. “Unless the injustice in these strategies is corrected, this will be a persistent issue if there is a resurgence of COVID-19 cases, a pandemic caused by a different virus in the future, or a different type of disaster where resources are scarce.”
To counter a potential bias against the elderly population should scarce resources force rationing decisions, AGS has made recommendations and strategies that health care systems should incorporate into a policy framework.
One principle in the AGS statement is clear: “Age per se should never be used as a means for a categorical exclusion from therapeutic interventions that represent the standard of care. ... Likewise, specific age-based cutoffs should not be used in resource allocation strategies.”
Peter Angelos, MD, chief of endocrine surgery at the University of Chicago, applauded the position statement.
“It is a well-written statement and I do think that it appropriately suggests that age in and of itself is not a good predictor of who is at greatest risk if infected with coronavirus,” Dr. Angelos, who also serves as the associate director of the MacLean Center for Clinical Medical Ethics, said in an interview.
He suggested a scenario in which a younger person could have multiple comorbidities that could put that individual at a higher risk of death because of complications from COVID-19 (or another pandemic in the future), compared with an older patient who is otherwise a healthy individual with a lower risk of death.
“For that reason, I agree with the authors that there should not be an arbitrary cutoff of age for which we don’t treat people or we limit treatment.”
Rather, the authors state that the primary allocation method in emergency circumstances that require rationing because of lack of resources should “equally weigh in-hospital survival and severe comorbidities contributing to short-term (<6 months) mortality.”
When assessing comorbidities, “the disparate impact of social determinants of health including culture, ethnicity, socioeconomic status, and other factors should be considered.”
AGS’s position statement adds that criteria such as “life-years saved” and “long-term predicted life expectancy” should not be used as they tend to disadvantage older adults.
The organization noted that institutions “should develop resource allocation strategies that are transparent, applied uniformly, and developed with forethought and input from multiple disciplines including ethics, medicine, law, and nursing. These strategies should be used consistently when making emergency decisions.” The AGS called for institutions to frequently review these strategies to ensure they are updated with the most recent evidence and to identify any issues of bias that may emerge.
Dr. Angelos stressed that these guidelines should be developed in a transparent and open fashion. He also highlighted the AGS recommendation of the use of triage officers or triage committees to make the determination about resource allocation should those decisions need to be made.
“We don’t want caregivers who are at the bedside taking care of patients to have the responsibility to say ‘We are going to treat one person as opposed to another person,’ ” he said. “You want to have those decisions made by a team that is separate from the bedside caregivers.”
He agreed with the statement authors that the goal of the triage committee decisions should be to maximize lives saved as opposed to life-years saved. Dr. Angelos noted that his institution’s plan focuses on lives saved should the need for resource rationing come to pass.
In addition to institutional strategies, AGS also emphasized in the position statement that older adults should develop individual care plans that include lists of medical conditions, medications, health care providers, and advance directives. The statement also noted that about only 50% of adults over age 60 years have complete advance directives, a rate Dr. Farrell and colleagues state is “unacceptably low.”
“Advance care planning should not be limited to the purview of only the primary care, geriatrics, or palliative care health professional, and urgent efforts should be made to discuss patient preferences before an emergent need arises,” the paper states, noting that specialists need to be a part of the conversation.
However, the position statement is clear that, while AGS is encouraging providers to talk about advance care planning with their patients, “providers should not pressure, even subtly, patients to engage in advance care planning or change to Do Not Resuscitate/Do Not Intubate (DNR/DNI) status with the intent to conserve health resources.”
Dr. Angelos reiterated this point and suggested that advance directive conversations need to be happening and happening more often.
“This current pandemic has forced us all to realize that, even in well-resourced societies like the United States, we may be faced with situations of absolute scarcity, so we ought to have these conversations up front so that we are not put in a position where we have to make decisions, and those decisions may not be well thought out and may not be ethically justifiable,” he said.
SOURCE: Farrell TW et al. J Am Geriat Soc. 2020 May 6; doi: 10.1111/jgs.16537.
The American Geriatrics Society has issued policy recommendations aimed at protecting seniors from ageism when it comes to resource allocation in the current context of treating patients infected with COVID-19.
“The AGS is deeply concerned about Timothy W. Farrell, MD, University of Utah, Salt Lake City, and colleagues wrote in an AGS position statement published online in the Journal of the American Geriatrics Society.
“In particular, rationing strategies that are solely, or predominantly, based on age cutoffs could lead to persistent beliefs that older adults’ lives are less valuable than others or are even expendable, and contribute to already rampant ageism,” the authors continued. “Unless the injustice in these strategies is corrected, this will be a persistent issue if there is a resurgence of COVID-19 cases, a pandemic caused by a different virus in the future, or a different type of disaster where resources are scarce.”
To counter a potential bias against the elderly population should scarce resources force rationing decisions, AGS has made recommendations and strategies that health care systems should incorporate into a policy framework.
One principle in the AGS statement is clear: “Age per se should never be used as a means for a categorical exclusion from therapeutic interventions that represent the standard of care. ... Likewise, specific age-based cutoffs should not be used in resource allocation strategies.”
Peter Angelos, MD, chief of endocrine surgery at the University of Chicago, applauded the position statement.
“It is a well-written statement and I do think that it appropriately suggests that age in and of itself is not a good predictor of who is at greatest risk if infected with coronavirus,” Dr. Angelos, who also serves as the associate director of the MacLean Center for Clinical Medical Ethics, said in an interview.
He suggested a scenario in which a younger person could have multiple comorbidities that could put that individual at a higher risk of death because of complications from COVID-19 (or another pandemic in the future), compared with an older patient who is otherwise a healthy individual with a lower risk of death.
“For that reason, I agree with the authors that there should not be an arbitrary cutoff of age for which we don’t treat people or we limit treatment.”
Rather, the authors state that the primary allocation method in emergency circumstances that require rationing because of lack of resources should “equally weigh in-hospital survival and severe comorbidities contributing to short-term (<6 months) mortality.”
When assessing comorbidities, “the disparate impact of social determinants of health including culture, ethnicity, socioeconomic status, and other factors should be considered.”
AGS’s position statement adds that criteria such as “life-years saved” and “long-term predicted life expectancy” should not be used as they tend to disadvantage older adults.
The organization noted that institutions “should develop resource allocation strategies that are transparent, applied uniformly, and developed with forethought and input from multiple disciplines including ethics, medicine, law, and nursing. These strategies should be used consistently when making emergency decisions.” The AGS called for institutions to frequently review these strategies to ensure they are updated with the most recent evidence and to identify any issues of bias that may emerge.
Dr. Angelos stressed that these guidelines should be developed in a transparent and open fashion. He also highlighted the AGS recommendation of the use of triage officers or triage committees to make the determination about resource allocation should those decisions need to be made.
“We don’t want caregivers who are at the bedside taking care of patients to have the responsibility to say ‘We are going to treat one person as opposed to another person,’ ” he said. “You want to have those decisions made by a team that is separate from the bedside caregivers.”
He agreed with the statement authors that the goal of the triage committee decisions should be to maximize lives saved as opposed to life-years saved. Dr. Angelos noted that his institution’s plan focuses on lives saved should the need for resource rationing come to pass.
In addition to institutional strategies, AGS also emphasized in the position statement that older adults should develop individual care plans that include lists of medical conditions, medications, health care providers, and advance directives. The statement also noted that about only 50% of adults over age 60 years have complete advance directives, a rate Dr. Farrell and colleagues state is “unacceptably low.”
“Advance care planning should not be limited to the purview of only the primary care, geriatrics, or palliative care health professional, and urgent efforts should be made to discuss patient preferences before an emergent need arises,” the paper states, noting that specialists need to be a part of the conversation.
However, the position statement is clear that, while AGS is encouraging providers to talk about advance care planning with their patients, “providers should not pressure, even subtly, patients to engage in advance care planning or change to Do Not Resuscitate/Do Not Intubate (DNR/DNI) status with the intent to conserve health resources.”
Dr. Angelos reiterated this point and suggested that advance directive conversations need to be happening and happening more often.
“This current pandemic has forced us all to realize that, even in well-resourced societies like the United States, we may be faced with situations of absolute scarcity, so we ought to have these conversations up front so that we are not put in a position where we have to make decisions, and those decisions may not be well thought out and may not be ethically justifiable,” he said.
SOURCE: Farrell TW et al. J Am Geriat Soc. 2020 May 6; doi: 10.1111/jgs.16537.
The American Geriatrics Society has issued policy recommendations aimed at protecting seniors from ageism when it comes to resource allocation in the current context of treating patients infected with COVID-19.
“The AGS is deeply concerned about Timothy W. Farrell, MD, University of Utah, Salt Lake City, and colleagues wrote in an AGS position statement published online in the Journal of the American Geriatrics Society.
“In particular, rationing strategies that are solely, or predominantly, based on age cutoffs could lead to persistent beliefs that older adults’ lives are less valuable than others or are even expendable, and contribute to already rampant ageism,” the authors continued. “Unless the injustice in these strategies is corrected, this will be a persistent issue if there is a resurgence of COVID-19 cases, a pandemic caused by a different virus in the future, or a different type of disaster where resources are scarce.”
To counter a potential bias against the elderly population should scarce resources force rationing decisions, AGS has made recommendations and strategies that health care systems should incorporate into a policy framework.
One principle in the AGS statement is clear: “Age per se should never be used as a means for a categorical exclusion from therapeutic interventions that represent the standard of care. ... Likewise, specific age-based cutoffs should not be used in resource allocation strategies.”
Peter Angelos, MD, chief of endocrine surgery at the University of Chicago, applauded the position statement.
“It is a well-written statement and I do think that it appropriately suggests that age in and of itself is not a good predictor of who is at greatest risk if infected with coronavirus,” Dr. Angelos, who also serves as the associate director of the MacLean Center for Clinical Medical Ethics, said in an interview.
He suggested a scenario in which a younger person could have multiple comorbidities that could put that individual at a higher risk of death because of complications from COVID-19 (or another pandemic in the future), compared with an older patient who is otherwise a healthy individual with a lower risk of death.
“For that reason, I agree with the authors that there should not be an arbitrary cutoff of age for which we don’t treat people or we limit treatment.”
Rather, the authors state that the primary allocation method in emergency circumstances that require rationing because of lack of resources should “equally weigh in-hospital survival and severe comorbidities contributing to short-term (<6 months) mortality.”
When assessing comorbidities, “the disparate impact of social determinants of health including culture, ethnicity, socioeconomic status, and other factors should be considered.”
AGS’s position statement adds that criteria such as “life-years saved” and “long-term predicted life expectancy” should not be used as they tend to disadvantage older adults.
The organization noted that institutions “should develop resource allocation strategies that are transparent, applied uniformly, and developed with forethought and input from multiple disciplines including ethics, medicine, law, and nursing. These strategies should be used consistently when making emergency decisions.” The AGS called for institutions to frequently review these strategies to ensure they are updated with the most recent evidence and to identify any issues of bias that may emerge.
Dr. Angelos stressed that these guidelines should be developed in a transparent and open fashion. He also highlighted the AGS recommendation of the use of triage officers or triage committees to make the determination about resource allocation should those decisions need to be made.
“We don’t want caregivers who are at the bedside taking care of patients to have the responsibility to say ‘We are going to treat one person as opposed to another person,’ ” he said. “You want to have those decisions made by a team that is separate from the bedside caregivers.”
He agreed with the statement authors that the goal of the triage committee decisions should be to maximize lives saved as opposed to life-years saved. Dr. Angelos noted that his institution’s plan focuses on lives saved should the need for resource rationing come to pass.
In addition to institutional strategies, AGS also emphasized in the position statement that older adults should develop individual care plans that include lists of medical conditions, medications, health care providers, and advance directives. The statement also noted that about only 50% of adults over age 60 years have complete advance directives, a rate Dr. Farrell and colleagues state is “unacceptably low.”
“Advance care planning should not be limited to the purview of only the primary care, geriatrics, or palliative care health professional, and urgent efforts should be made to discuss patient preferences before an emergent need arises,” the paper states, noting that specialists need to be a part of the conversation.
However, the position statement is clear that, while AGS is encouraging providers to talk about advance care planning with their patients, “providers should not pressure, even subtly, patients to engage in advance care planning or change to Do Not Resuscitate/Do Not Intubate (DNR/DNI) status with the intent to conserve health resources.”
Dr. Angelos reiterated this point and suggested that advance directive conversations need to be happening and happening more often.
“This current pandemic has forced us all to realize that, even in well-resourced societies like the United States, we may be faced with situations of absolute scarcity, so we ought to have these conversations up front so that we are not put in a position where we have to make decisions, and those decisions may not be well thought out and may not be ethically justifiable,” he said.
SOURCE: Farrell TW et al. J Am Geriat Soc. 2020 May 6; doi: 10.1111/jgs.16537.
FROM JOURNAL OF THE AMERICAN GERIATRIC SOCIETY
Audrey Hepburn’s lessons for a COVID clinic
Queues of patients wait to clear security and enter the sterile area at every medical office. Water bottles are allowed, fevers and visitors are not. Those who fail clearance or who are afraid to be seen in person must be treated virtually. In this context, virtually means by telephone or video, yet, aptly, it also means “nearly or almost,” as in we can nearly or almost treat them these ways. We’ve emerged safely, but we’ve lost sensibility. Because of this, what’s important in the doctor-patient relationships will drift a bit. Clinical acumen and technical skill won’t be enough. Successful practices will also have grace.
If your image of grace is Audrey Hepburn gliding along Fifth Avenue in a long black dress and elbow-length gloves, you’re in the right place. Ms. Hepburn embodied elegance and decorum and there are lessons to be drawn from her. Piling your hair high and donning oversized sunglasses along with your face mask would be to miss the point here though. Ms. Hepburn dressed exquisitely, yes, but her grace came from what wearing a difficult-to-walk-in dress meant to us, not to her. Appearance, self-control, and warmth are what made her charismatic.
To appear urbane requires effort; it’s the effort that we appreciate in someone who is graceful. When you’re thoughtful about how you look, you plan ahead, you work to look polished. In effect, you’re saying: “As my patient, you’re important enough for me to be well dressed.” It is a visible signal of all the unobservable work you’ve done to care for them. This is more critical now that our faces are covered and concern for infection means wearing shabby hospital scrubs rather than shirt and tie.
Effort is also required for telephone and video visits. In them, our doctor-patient connection is diminished – no matter how high definition, it’s a virtual affair. Ms. Hepburn would no doubt take the time to ensure she appeared professional, well lit, with a pleasing background. She’d plan for the call to be done in a quiet location and without distraction.
Whether in person or by phone, grace, as Ms. Hepburn demonstrated, is physical awareness and body control. She would often be completely still when someone is speaking, showing a countenance of warmth. She’d pause after the other person completed a thought and before replying. In doing so, she conveyed that she was present and engaged in what was being said. It is that confidence and ease of manner we perceived as grace.
I thought about this the other day during a mixed clinic of telephone and face-to-face visits. I had on my wrinkle-free scrubs (I could do better). I was listening to a patient describe all possible triggers for her hand dermatitis. My urge to interrupt grew with each paragraph of her storytelling. “Be patient,” I thought, “be at ease with her rambling. ... When she stops, thank her as if you were looking her in the eye acknowledging how interesting her observations were.” This is not just good manners, it’s the essence of grace: The art of showing how important others are to you.
Our world needs grace more than ever and what better place to start but with us. In pleasing, assisting, and honoring them, our patients can be reassured that we can and will care for them. Make Ms. Hepburn proud.
“For beautiful eyes, look for the good in others; for beautiful lips, speak only words of kindness; and for poise, walk with the knowledge that you are never alone.” – Audrey Hepburn
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He has no disclosures related to this column. Write to him at dermnews@mdedge.com .
Queues of patients wait to clear security and enter the sterile area at every medical office. Water bottles are allowed, fevers and visitors are not. Those who fail clearance or who are afraid to be seen in person must be treated virtually. In this context, virtually means by telephone or video, yet, aptly, it also means “nearly or almost,” as in we can nearly or almost treat them these ways. We’ve emerged safely, but we’ve lost sensibility. Because of this, what’s important in the doctor-patient relationships will drift a bit. Clinical acumen and technical skill won’t be enough. Successful practices will also have grace.
If your image of grace is Audrey Hepburn gliding along Fifth Avenue in a long black dress and elbow-length gloves, you’re in the right place. Ms. Hepburn embodied elegance and decorum and there are lessons to be drawn from her. Piling your hair high and donning oversized sunglasses along with your face mask would be to miss the point here though. Ms. Hepburn dressed exquisitely, yes, but her grace came from what wearing a difficult-to-walk-in dress meant to us, not to her. Appearance, self-control, and warmth are what made her charismatic.
To appear urbane requires effort; it’s the effort that we appreciate in someone who is graceful. When you’re thoughtful about how you look, you plan ahead, you work to look polished. In effect, you’re saying: “As my patient, you’re important enough for me to be well dressed.” It is a visible signal of all the unobservable work you’ve done to care for them. This is more critical now that our faces are covered and concern for infection means wearing shabby hospital scrubs rather than shirt and tie.
Effort is also required for telephone and video visits. In them, our doctor-patient connection is diminished – no matter how high definition, it’s a virtual affair. Ms. Hepburn would no doubt take the time to ensure she appeared professional, well lit, with a pleasing background. She’d plan for the call to be done in a quiet location and without distraction.
Whether in person or by phone, grace, as Ms. Hepburn demonstrated, is physical awareness and body control. She would often be completely still when someone is speaking, showing a countenance of warmth. She’d pause after the other person completed a thought and before replying. In doing so, she conveyed that she was present and engaged in what was being said. It is that confidence and ease of manner we perceived as grace.
I thought about this the other day during a mixed clinic of telephone and face-to-face visits. I had on my wrinkle-free scrubs (I could do better). I was listening to a patient describe all possible triggers for her hand dermatitis. My urge to interrupt grew with each paragraph of her storytelling. “Be patient,” I thought, “be at ease with her rambling. ... When she stops, thank her as if you were looking her in the eye acknowledging how interesting her observations were.” This is not just good manners, it’s the essence of grace: The art of showing how important others are to you.
Our world needs grace more than ever and what better place to start but with us. In pleasing, assisting, and honoring them, our patients can be reassured that we can and will care for them. Make Ms. Hepburn proud.
“For beautiful eyes, look for the good in others; for beautiful lips, speak only words of kindness; and for poise, walk with the knowledge that you are never alone.” – Audrey Hepburn
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He has no disclosures related to this column. Write to him at dermnews@mdedge.com .
Queues of patients wait to clear security and enter the sterile area at every medical office. Water bottles are allowed, fevers and visitors are not. Those who fail clearance or who are afraid to be seen in person must be treated virtually. In this context, virtually means by telephone or video, yet, aptly, it also means “nearly or almost,” as in we can nearly or almost treat them these ways. We’ve emerged safely, but we’ve lost sensibility. Because of this, what’s important in the doctor-patient relationships will drift a bit. Clinical acumen and technical skill won’t be enough. Successful practices will also have grace.
If your image of grace is Audrey Hepburn gliding along Fifth Avenue in a long black dress and elbow-length gloves, you’re in the right place. Ms. Hepburn embodied elegance and decorum and there are lessons to be drawn from her. Piling your hair high and donning oversized sunglasses along with your face mask would be to miss the point here though. Ms. Hepburn dressed exquisitely, yes, but her grace came from what wearing a difficult-to-walk-in dress meant to us, not to her. Appearance, self-control, and warmth are what made her charismatic.
To appear urbane requires effort; it’s the effort that we appreciate in someone who is graceful. When you’re thoughtful about how you look, you plan ahead, you work to look polished. In effect, you’re saying: “As my patient, you’re important enough for me to be well dressed.” It is a visible signal of all the unobservable work you’ve done to care for them. This is more critical now that our faces are covered and concern for infection means wearing shabby hospital scrubs rather than shirt and tie.
Effort is also required for telephone and video visits. In them, our doctor-patient connection is diminished – no matter how high definition, it’s a virtual affair. Ms. Hepburn would no doubt take the time to ensure she appeared professional, well lit, with a pleasing background. She’d plan for the call to be done in a quiet location and without distraction.
Whether in person or by phone, grace, as Ms. Hepburn demonstrated, is physical awareness and body control. She would often be completely still when someone is speaking, showing a countenance of warmth. She’d pause after the other person completed a thought and before replying. In doing so, she conveyed that she was present and engaged in what was being said. It is that confidence and ease of manner we perceived as grace.
I thought about this the other day during a mixed clinic of telephone and face-to-face visits. I had on my wrinkle-free scrubs (I could do better). I was listening to a patient describe all possible triggers for her hand dermatitis. My urge to interrupt grew with each paragraph of her storytelling. “Be patient,” I thought, “be at ease with her rambling. ... When she stops, thank her as if you were looking her in the eye acknowledging how interesting her observations were.” This is not just good manners, it’s the essence of grace: The art of showing how important others are to you.
Our world needs grace more than ever and what better place to start but with us. In pleasing, assisting, and honoring them, our patients can be reassured that we can and will care for them. Make Ms. Hepburn proud.
“For beautiful eyes, look for the good in others; for beautiful lips, speak only words of kindness; and for poise, walk with the knowledge that you are never alone.” – Audrey Hepburn
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He has no disclosures related to this column. Write to him at dermnews@mdedge.com .
3 new latent TB preventive regimens dramatically cut Tx time
References
- Sterling TR, Njie G, Zenner D, et al. Guidelines for the treatment of latent tubercular infection: recommendations from the National Tuberculosis Controllers Association and the CDC, 2020. MMWR Recomm Rep. 2020;69:1-11.
- USPSTF. Latent tuberculosis screening [final recommendation statement]. Published September 6, 2016. www.uspreventiveservicestaskforce.org/uspstf/recommendation/latent-tuberculosis-infection-screening. Accessed May 19, 2020.
- CDC. Tuberculosis (TB): data and statistics. Updated September 6, 2019. www.cdc.gov/tb/statistics/default.htm. Accessed May 19, 2020.
References
- Sterling TR, Njie G, Zenner D, et al. Guidelines for the treatment of latent tubercular infection: recommendations from the National Tuberculosis Controllers Association and the CDC, 2020. MMWR Recomm Rep. 2020;69:1-11.
- USPSTF. Latent tuberculosis screening [final recommendation statement]. Published September 6, 2016. www.uspreventiveservicestaskforce.org/uspstf/recommendation/latent-tuberculosis-infection-screening. Accessed May 19, 2020.
- CDC. Tuberculosis (TB): data and statistics. Updated September 6, 2019. www.cdc.gov/tb/statistics/default.htm. Accessed May 19, 2020.
References
- Sterling TR, Njie G, Zenner D, et al. Guidelines for the treatment of latent tubercular infection: recommendations from the National Tuberculosis Controllers Association and the CDC, 2020. MMWR Recomm Rep. 2020;69:1-11.
- USPSTF. Latent tuberculosis screening [final recommendation statement]. Published September 6, 2016. www.uspreventiveservicestaskforce.org/uspstf/recommendation/latent-tuberculosis-infection-screening. Accessed May 19, 2020.
- CDC. Tuberculosis (TB): data and statistics. Updated September 6, 2019. www.cdc.gov/tb/statistics/default.htm. Accessed May 19, 2020.
Novel program for preventing addiction-related suicide
A single 3-hour-long group psychosocial intervention designed specifically for patients in intensive outpatient programs for addiction treatment to prevent future suicide resulted in significantly improved knowledge and attitudes regarding suicide that persisted at 6 months of follow-up in a large multicenter randomized effectiveness study, reported Richard K. Ries, MD.
There is an enormous unmet need for evidence-based strategies for preventing addiction-related suicide, since people with substance use disorders have a 10-fold increased risk of suicide. Based upon these new study findings, the Preventing Addiction Related Suicide (PARS) program can now be considered the first such evidence-based intervention for this extremely high-risk population, Dr. Ries said at the virtual annual meeting of the American Association of Suicidology.
“We’ve shown that suicide prevention in intensive outpatient program addiction groups is feasible, easy to train, and highly rated by counselors, and I’d say it’s very adaptable, easy to go national in almost any addiction treatment program, right out of the box,” said Dr. Ries, professor of psychiatry at the University of Washington, Seattle, and director of outpatient psychiatry as well as the psychiatry addiction division at Harborview Medical Center.
The workbook-based PARS program developed by Dr. Ries and colleagues adapted empirically supported suicide prevention best practices from other settings for use in group-based intensive outpatient addiction treatment, which is the most common form of treatment for chemical dependency in the United States. Dr. Ries recognized the need for a program such as PARS because addiction counselors often feel out of their depth regarding suicide-related issues.
he explained. “We designed the PARS intervention to be integrated right into the counselors’ workflow. They get trained right in their setting in a one-shot deal that takes 2-3 hours. The training was highly rated by counselors as acceptable and effective in their day-to-day work, not ivory tower-type stuff.”
Once the counselors were trained in PARS, they then trained their alcohol- and drug-addicted patients. Elements of the PARS program include information on suicide risk and protective factors, myths and facts about suicide, action steps to take when warning signs of suicide are observed, and local crisis resources.
The effectiveness study was a randomized, stepped-wedge cluster design intervention that included 905 patients in 15 busy community group–based intensive outpatient addiction treatment programs in Western Washington. Patients were randomized to counselor-delivered PARS or treatment as usual, with follow-up assessments at 2 weeks and 1, 3, and 6 months.
There was no attempt to enrich the study population for suicidality by prescreening potential enrollees, since participation in a drug and alcohol treatment program already places an individual in a high-risk group. For example, 74% of study participants indicated they had thought of suicide at least once in the past year, compared with a background rate of 4% in the U.S. general population. And 29% of study participants reported a lifetime history of one or more suicide attempts, versus roughly 5% in the general population.
Dr. Ries’ coinvestigator, Katherine Anne Comtois, PhD, MPH, presented the study results. The three key outcomes were improvement on structured measures of suicide knowledge, attitudes, and help-seeking behavior. The PARS recipients showed statistically significant improvement compared with baseline on two of the three: they displayed greater knowledge about suicide and its close relationship with addiction, and less stigmatization and other maladaptive attitudes toward suicide. Scores on all three measures remained unchanged over time in the control group.
“Overall, we had small to medium effect sizes, comparable to what you might see in studies measuring antidepressant effect sizes. I think these were meaningful improvements in knowledge and attitudes,” said Dr. Comtois of the University of Washington.
The PARS group showed a small increase in the third endpoint – willingness to seek professional help for themselves, friends, or family if depressed or suicidal, but this didn’t achieve statistical significance. However, Dr. Comtois noted that the study outcomes were assessed per protocol using an intent-to-treat analysis. This likely underestimated the true effectiveness of the PARS intervention, given that 40% of patients randomized to PARS didn’t actually attend the intervention session.
“People with drug and alcohol problems have complicated lives,” she said by way of explanation for the high no-show rate.
The investigators are now performing a per-protocol analysis of the data, restricted to those subjects who actually attended their session. A long-term look at suicide events and outcomes in the study population is planned.
Dr. Ries and Dr. Comtois reported having no financial conflicts regarding the study, which was funded by a multiyear grant from the National Institute on Drug Abuse.
A single 3-hour-long group psychosocial intervention designed specifically for patients in intensive outpatient programs for addiction treatment to prevent future suicide resulted in significantly improved knowledge and attitudes regarding suicide that persisted at 6 months of follow-up in a large multicenter randomized effectiveness study, reported Richard K. Ries, MD.
There is an enormous unmet need for evidence-based strategies for preventing addiction-related suicide, since people with substance use disorders have a 10-fold increased risk of suicide. Based upon these new study findings, the Preventing Addiction Related Suicide (PARS) program can now be considered the first such evidence-based intervention for this extremely high-risk population, Dr. Ries said at the virtual annual meeting of the American Association of Suicidology.
“We’ve shown that suicide prevention in intensive outpatient program addiction groups is feasible, easy to train, and highly rated by counselors, and I’d say it’s very adaptable, easy to go national in almost any addiction treatment program, right out of the box,” said Dr. Ries, professor of psychiatry at the University of Washington, Seattle, and director of outpatient psychiatry as well as the psychiatry addiction division at Harborview Medical Center.
The workbook-based PARS program developed by Dr. Ries and colleagues adapted empirically supported suicide prevention best practices from other settings for use in group-based intensive outpatient addiction treatment, which is the most common form of treatment for chemical dependency in the United States. Dr. Ries recognized the need for a program such as PARS because addiction counselors often feel out of their depth regarding suicide-related issues.
he explained. “We designed the PARS intervention to be integrated right into the counselors’ workflow. They get trained right in their setting in a one-shot deal that takes 2-3 hours. The training was highly rated by counselors as acceptable and effective in their day-to-day work, not ivory tower-type stuff.”
Once the counselors were trained in PARS, they then trained their alcohol- and drug-addicted patients. Elements of the PARS program include information on suicide risk and protective factors, myths and facts about suicide, action steps to take when warning signs of suicide are observed, and local crisis resources.
The effectiveness study was a randomized, stepped-wedge cluster design intervention that included 905 patients in 15 busy community group–based intensive outpatient addiction treatment programs in Western Washington. Patients were randomized to counselor-delivered PARS or treatment as usual, with follow-up assessments at 2 weeks and 1, 3, and 6 months.
There was no attempt to enrich the study population for suicidality by prescreening potential enrollees, since participation in a drug and alcohol treatment program already places an individual in a high-risk group. For example, 74% of study participants indicated they had thought of suicide at least once in the past year, compared with a background rate of 4% in the U.S. general population. And 29% of study participants reported a lifetime history of one or more suicide attempts, versus roughly 5% in the general population.
Dr. Ries’ coinvestigator, Katherine Anne Comtois, PhD, MPH, presented the study results. The three key outcomes were improvement on structured measures of suicide knowledge, attitudes, and help-seeking behavior. The PARS recipients showed statistically significant improvement compared with baseline on two of the three: they displayed greater knowledge about suicide and its close relationship with addiction, and less stigmatization and other maladaptive attitudes toward suicide. Scores on all three measures remained unchanged over time in the control group.
“Overall, we had small to medium effect sizes, comparable to what you might see in studies measuring antidepressant effect sizes. I think these were meaningful improvements in knowledge and attitudes,” said Dr. Comtois of the University of Washington.
The PARS group showed a small increase in the third endpoint – willingness to seek professional help for themselves, friends, or family if depressed or suicidal, but this didn’t achieve statistical significance. However, Dr. Comtois noted that the study outcomes were assessed per protocol using an intent-to-treat analysis. This likely underestimated the true effectiveness of the PARS intervention, given that 40% of patients randomized to PARS didn’t actually attend the intervention session.
“People with drug and alcohol problems have complicated lives,” she said by way of explanation for the high no-show rate.
The investigators are now performing a per-protocol analysis of the data, restricted to those subjects who actually attended their session. A long-term look at suicide events and outcomes in the study population is planned.
Dr. Ries and Dr. Comtois reported having no financial conflicts regarding the study, which was funded by a multiyear grant from the National Institute on Drug Abuse.
A single 3-hour-long group psychosocial intervention designed specifically for patients in intensive outpatient programs for addiction treatment to prevent future suicide resulted in significantly improved knowledge and attitudes regarding suicide that persisted at 6 months of follow-up in a large multicenter randomized effectiveness study, reported Richard K. Ries, MD.
There is an enormous unmet need for evidence-based strategies for preventing addiction-related suicide, since people with substance use disorders have a 10-fold increased risk of suicide. Based upon these new study findings, the Preventing Addiction Related Suicide (PARS) program can now be considered the first such evidence-based intervention for this extremely high-risk population, Dr. Ries said at the virtual annual meeting of the American Association of Suicidology.
“We’ve shown that suicide prevention in intensive outpatient program addiction groups is feasible, easy to train, and highly rated by counselors, and I’d say it’s very adaptable, easy to go national in almost any addiction treatment program, right out of the box,” said Dr. Ries, professor of psychiatry at the University of Washington, Seattle, and director of outpatient psychiatry as well as the psychiatry addiction division at Harborview Medical Center.
The workbook-based PARS program developed by Dr. Ries and colleagues adapted empirically supported suicide prevention best practices from other settings for use in group-based intensive outpatient addiction treatment, which is the most common form of treatment for chemical dependency in the United States. Dr. Ries recognized the need for a program such as PARS because addiction counselors often feel out of their depth regarding suicide-related issues.
he explained. “We designed the PARS intervention to be integrated right into the counselors’ workflow. They get trained right in their setting in a one-shot deal that takes 2-3 hours. The training was highly rated by counselors as acceptable and effective in their day-to-day work, not ivory tower-type stuff.”
Once the counselors were trained in PARS, they then trained their alcohol- and drug-addicted patients. Elements of the PARS program include information on suicide risk and protective factors, myths and facts about suicide, action steps to take when warning signs of suicide are observed, and local crisis resources.
The effectiveness study was a randomized, stepped-wedge cluster design intervention that included 905 patients in 15 busy community group–based intensive outpatient addiction treatment programs in Western Washington. Patients were randomized to counselor-delivered PARS or treatment as usual, with follow-up assessments at 2 weeks and 1, 3, and 6 months.
There was no attempt to enrich the study population for suicidality by prescreening potential enrollees, since participation in a drug and alcohol treatment program already places an individual in a high-risk group. For example, 74% of study participants indicated they had thought of suicide at least once in the past year, compared with a background rate of 4% in the U.S. general population. And 29% of study participants reported a lifetime history of one or more suicide attempts, versus roughly 5% in the general population.
Dr. Ries’ coinvestigator, Katherine Anne Comtois, PhD, MPH, presented the study results. The three key outcomes were improvement on structured measures of suicide knowledge, attitudes, and help-seeking behavior. The PARS recipients showed statistically significant improvement compared with baseline on two of the three: they displayed greater knowledge about suicide and its close relationship with addiction, and less stigmatization and other maladaptive attitudes toward suicide. Scores on all three measures remained unchanged over time in the control group.
“Overall, we had small to medium effect sizes, comparable to what you might see in studies measuring antidepressant effect sizes. I think these were meaningful improvements in knowledge and attitudes,” said Dr. Comtois of the University of Washington.
The PARS group showed a small increase in the third endpoint – willingness to seek professional help for themselves, friends, or family if depressed or suicidal, but this didn’t achieve statistical significance. However, Dr. Comtois noted that the study outcomes were assessed per protocol using an intent-to-treat analysis. This likely underestimated the true effectiveness of the PARS intervention, given that 40% of patients randomized to PARS didn’t actually attend the intervention session.
“People with drug and alcohol problems have complicated lives,” she said by way of explanation for the high no-show rate.
The investigators are now performing a per-protocol analysis of the data, restricted to those subjects who actually attended their session. A long-term look at suicide events and outcomes in the study population is planned.
Dr. Ries and Dr. Comtois reported having no financial conflicts regarding the study, which was funded by a multiyear grant from the National Institute on Drug Abuse.
FROM AAS20
Unexpected Consequence of COVID-19: Veteran Cirrhosis Hospitalizations Decline
Cirrhosis hospitalizations are declining during the coronavirus pandemic, according to researchers from the University of Pennsylvania and Corporal Michael J. Crescenz US Department of Veterans Affairs Medical Center in Philadelphia. They found a “clear drop-off” among patients who ordinarily would meet acute care criteria.
Using data from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort, the researchers collected data that included length of stay, type of hospital, and region for 7,216 patients and 12,467 hospitalizations between January 1 and April 15 in 2019 and 2020. They designated 3 2020 subgroups: pre-COVID (before February 29), early COVID (February 29 - March 25), and late COVID (March 26 - April 15). The breakpoints were chosen because the Veterans Health Administration announced a COVID-19 Response Plan on March 23 that was implemented widely within 3 days.
Analyzing the differences in data from the 2 years, the researchers found weekly cirrhosis hospitalizations were on average 159.5 fewer in the late-COVID era, while admissions for end-stage liver disease were significantly higher. Patients also had shorter lengths of stay in 2020 when compared with 2019 (median, 2 days vs 3), and fewer hospital transfers (7.5% vs 11.1%).
The late-COVID era also was characterized by significantly fewer academic hospital admissions (63.6% vs 68.1% pre-COVID). And more patients were discharged to home in the late-COVID era (91.1% vs 88.8% pre-COVID) and fewer to facilities (5.1% vs 9.0% pre-COVID).
The changes likely reflect initiatives to preserve inpatient resources, the researchers say. “Importantly,” they suggest, their findings probably “parallel changes in other inpatient resource-intensive conditions,” such as congestive heart failure, chronic obstructive pulmonary disease, and myocardial infarction.
The pandemic response also may be sending conflicting messages to people who already have serious illnesses: Patients may be following guidance encouraging them to stay home, or avoiding going to the hospital until their symptoms are severe, perhaps from fears about COVID-19.
It is unclear how these patients are being managed, the researchers add. “Given the baseline vulnerability of patients with cirrhosis, it is likely that many do not currently have adequate healthcare access.”
Cirrhosis hospitalizations are declining during the coronavirus pandemic, according to researchers from the University of Pennsylvania and Corporal Michael J. Crescenz US Department of Veterans Affairs Medical Center in Philadelphia. They found a “clear drop-off” among patients who ordinarily would meet acute care criteria.
Using data from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort, the researchers collected data that included length of stay, type of hospital, and region for 7,216 patients and 12,467 hospitalizations between January 1 and April 15 in 2019 and 2020. They designated 3 2020 subgroups: pre-COVID (before February 29), early COVID (February 29 - March 25), and late COVID (March 26 - April 15). The breakpoints were chosen because the Veterans Health Administration announced a COVID-19 Response Plan on March 23 that was implemented widely within 3 days.
Analyzing the differences in data from the 2 years, the researchers found weekly cirrhosis hospitalizations were on average 159.5 fewer in the late-COVID era, while admissions for end-stage liver disease were significantly higher. Patients also had shorter lengths of stay in 2020 when compared with 2019 (median, 2 days vs 3), and fewer hospital transfers (7.5% vs 11.1%).
The late-COVID era also was characterized by significantly fewer academic hospital admissions (63.6% vs 68.1% pre-COVID). And more patients were discharged to home in the late-COVID era (91.1% vs 88.8% pre-COVID) and fewer to facilities (5.1% vs 9.0% pre-COVID).
The changes likely reflect initiatives to preserve inpatient resources, the researchers say. “Importantly,” they suggest, their findings probably “parallel changes in other inpatient resource-intensive conditions,” such as congestive heart failure, chronic obstructive pulmonary disease, and myocardial infarction.
The pandemic response also may be sending conflicting messages to people who already have serious illnesses: Patients may be following guidance encouraging them to stay home, or avoiding going to the hospital until their symptoms are severe, perhaps from fears about COVID-19.
It is unclear how these patients are being managed, the researchers add. “Given the baseline vulnerability of patients with cirrhosis, it is likely that many do not currently have adequate healthcare access.”
Cirrhosis hospitalizations are declining during the coronavirus pandemic, according to researchers from the University of Pennsylvania and Corporal Michael J. Crescenz US Department of Veterans Affairs Medical Center in Philadelphia. They found a “clear drop-off” among patients who ordinarily would meet acute care criteria.
Using data from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort, the researchers collected data that included length of stay, type of hospital, and region for 7,216 patients and 12,467 hospitalizations between January 1 and April 15 in 2019 and 2020. They designated 3 2020 subgroups: pre-COVID (before February 29), early COVID (February 29 - March 25), and late COVID (March 26 - April 15). The breakpoints were chosen because the Veterans Health Administration announced a COVID-19 Response Plan on March 23 that was implemented widely within 3 days.
Analyzing the differences in data from the 2 years, the researchers found weekly cirrhosis hospitalizations were on average 159.5 fewer in the late-COVID era, while admissions for end-stage liver disease were significantly higher. Patients also had shorter lengths of stay in 2020 when compared with 2019 (median, 2 days vs 3), and fewer hospital transfers (7.5% vs 11.1%).
The late-COVID era also was characterized by significantly fewer academic hospital admissions (63.6% vs 68.1% pre-COVID). And more patients were discharged to home in the late-COVID era (91.1% vs 88.8% pre-COVID) and fewer to facilities (5.1% vs 9.0% pre-COVID).
The changes likely reflect initiatives to preserve inpatient resources, the researchers say. “Importantly,” they suggest, their findings probably “parallel changes in other inpatient resource-intensive conditions,” such as congestive heart failure, chronic obstructive pulmonary disease, and myocardial infarction.
The pandemic response also may be sending conflicting messages to people who already have serious illnesses: Patients may be following guidance encouraging them to stay home, or avoiding going to the hospital until their symptoms are severe, perhaps from fears about COVID-19.
It is unclear how these patients are being managed, the researchers add. “Given the baseline vulnerability of patients with cirrhosis, it is likely that many do not currently have adequate healthcare access.”
Vitamin D: A low-hanging fruit in COVID-19?
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Migraine Management: What Primary Care Providers Need to Know
Migraine is a long-term, disabling neurologic disease that has a severe impact on the lives of patients living with it.1-3 Patients who experience frequent migraine attacks may require a multidisciplinary approach, which includes a combination of acute and preventive modalities as well as behavioral interventions as part of their treatment plan.4
This sponsored content shares ways in which patients with migraine may successfully manage their conditions and minimize impact on their lives with the support of their health care teams within primary care.4
References:
1 Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Neurology. 2007;68(5):343-349.
2 Buse DC, Rupnow MFT, Lipton RB. Mayo Clin Proc. 2009;84(5):422-435.
3 GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Lancet. 2018;392(10159):1789-1858.
4 American Headache Society. Headache. 2019;59(1):1-18.
USA-334-83662
Migraine is a long-term, disabling neurologic disease that has a severe impact on the lives of patients living with it.1-3 Patients who experience frequent migraine attacks may require a multidisciplinary approach, which includes a combination of acute and preventive modalities as well as behavioral interventions as part of their treatment plan.4
This sponsored content shares ways in which patients with migraine may successfully manage their conditions and minimize impact on their lives with the support of their health care teams within primary care.4
References:
1 Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Neurology. 2007;68(5):343-349.
2 Buse DC, Rupnow MFT, Lipton RB. Mayo Clin Proc. 2009;84(5):422-435.
3 GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Lancet. 2018;392(10159):1789-1858.
4 American Headache Society. Headache. 2019;59(1):1-18.
USA-334-83662
Migraine is a long-term, disabling neurologic disease that has a severe impact on the lives of patients living with it.1-3 Patients who experience frequent migraine attacks may require a multidisciplinary approach, which includes a combination of acute and preventive modalities as well as behavioral interventions as part of their treatment plan.4
This sponsored content shares ways in which patients with migraine may successfully manage their conditions and minimize impact on their lives with the support of their health care teams within primary care.4
References:
1 Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Neurology. 2007;68(5):343-349.
2 Buse DC, Rupnow MFT, Lipton RB. Mayo Clin Proc. 2009;84(5):422-435.
3 GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Lancet. 2018;392(10159):1789-1858.
4 American Headache Society. Headache. 2019;59(1):1-18.
USA-334-83662
TNF inhibitors may dampen COVID-19 severity
Patients on a tumor necrosis factor inhibitor for their rheumatic disease when they became infected with COVID-19 were markedly less likely to subsequently require hospitalization, according to intriguing early evidence from the COVID-19 Global Rheumatology Alliance Registry.
On the other hand, those registry patients who were on 10 mg of prednisone or more daily when they got infected were more than twice as likely to be hospitalized than were those who were not on corticosteroids, even after controlling for the severity of their rheumatic disease and other potential confounders, Jinoos Yazdany, MD, reported at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
“We saw a signal with moderate to high-dose steroids. I think it’s something we’re going to have to keep an eye out on as more data come in,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
The global registry launched on March 24, 2020, and was quickly embraced by rheumatologists from around the world. By May 12, the registry included more than 1,300 patients with a range of rheumatic diseases, all with confirmed COVID-19 infection as a requisite for enrollment; the cases were submitted by more than 300 rheumatologists in 40 countries. The registry is supported by the ACR and European League Against Rheumatism.
Dr. Yazdany, a member of the registry steering committee, described the project’s two main goals: To learn the outcomes of COVID-19–infected patients with various rheumatic diseases and to make inferences regarding the impact of the immunosuppressive and antimalarial medications widely prescribed by rheumatologists.
She presented soon-to-be-published data on the characteristics and disposition of the first 600 patients, 46% of whom were hospitalized and 9% died. A caveat regarding the registry, she noted, is that these are observational data and thus potentially subject to unrecognized confounders. Also, the registry population is skewed toward the sicker end of the COVID-19 disease spectrum because while all participants have confirmed infection, testing for the infection has been notoriously uneven. Many people are infected asymptomatically and thus may not undergo testing even where readily available.
Early key findings from registry
The risk factors for more severe infection resulting in hospitalization in patients with rheumatic diseases are by and large the same drivers described in the general population: older age and comorbid conditions including diabetes, hypertension, cardiovascular disease, obesity, chronic kidney disease, and lung disease. Notably, however, patients on the equivalent of 10 mg/day of prednisone or more were at a 105% increased risk for hospitalization, compared with those not on corticosteroids after adjustment for age, comorbid conditions, and rheumatic disease severity.
Patients on a background tumor necrosis factor (TNF) inhibitor had an adjusted 60% reduction in risk of hospitalization. This apparent protective effect against more severe COVID-19 disease is mechanistically plausible: In animal studies, being on a TNF inhibitor has been associated with less severe infection following exposure to influenza virus, Dr. Yazdany observed.
COVID-infected patients on any biologic disease-modifying antirheumatic drug had a 54% decreased risk of hospitalization. However, in this early analysis, the study was sufficiently powered only to specifically assess the impact of TNF inhibitors, since those agents were by far the most commonly used biologics. As the registry grows, it will be possible to analyze the impact of other antirheumatic medications.
Being on hydroxychloroquine or other antimalarials at the time of COVID-19 infection had no impact on hospitalization.
The only rheumatic disease diagnosis with an odds of hospitalization significantly different from that of RA patients was systemic lupus erythematosus (SLE). Lupus patients were at 80% increased risk of hospitalization. Although this was a statistically significant difference, Dr. Yazdany cautioned against making too much of it because of the strong potential for unmeasured confounding. In particular, lupus patients as a group are known to rate on the lower end of measures of social determinants of health, a status that is an established major risk factor for COVID-19 disease.
“A strength of the global registry has been that it provides timely data that’s been very helpful for rheumatologists to rapidly dispel misinformation that has been spread about hydroxychloroquine, especially statements about lupus patients not getting COVID-19. We know from these data that’s not true,” she said.
Being on background NSAIDs at the time of SARS-CoV-2 infection was not associated with increased risk of hospitalization; in fact, NSAID users were 36% less likely to be hospitalized for their COVID-19 disease, although this difference didn’t reach statistical significance.
Dr. Yazdany urged her fellow rheumatologists to enter their cases on the registry website: rheum-covid.org. There they can also join the registry mailing list and receive weekly updates.
Other recent insights on COVID-19 in rheumatology
An as-yet unpublished U.K. observational study involving electronic health record data on 17 million people included 885,000 individuals with RA, SLE, or psoriasis. After extensive statistical controlling for the known risk factors for severe COVID-19 infection, including a measure of socioeconomic deprivation, the group with one of these autoimmune diseases had an adjusted, statistically significant 23% increased risk of hospital death because of COVID-19 infection.
“This is the largest study of its kind to date. There’s potential for unmeasured confounding and selection bias here due to who gets tested. We’ll have to see where this study lands, but I think it does suggest there’s a slightly higher mortality risk in COVID-infected patients with rheumatic disease,” according to Dr. Yazdany.
On the other hand, there have been at least eight recently published patient surveys and case series of patients with rheumatic diseases in areas of the world hardest hit by the pandemic, and they paint a consistent picture.
“What we’ve learned from these studies was the infection rate was generally in the ballpark of people in the region. It doesn’t seem like there’s a dramatically higher infection rate in people with rheumatic disease in these surveys. The hospitalized rheumatology patients had many of the familiar comorbidities. This is the first glance at how likely people are to become infected and how they fared, and I think overall the data have been quite reassuring,” she said.
Dr. Yazdany reported serving as a consultant to AstraZeneca and Eli Lilly and receiving research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Centers for Disease Control and Prevention.
Patients on a tumor necrosis factor inhibitor for their rheumatic disease when they became infected with COVID-19 were markedly less likely to subsequently require hospitalization, according to intriguing early evidence from the COVID-19 Global Rheumatology Alliance Registry.
On the other hand, those registry patients who were on 10 mg of prednisone or more daily when they got infected were more than twice as likely to be hospitalized than were those who were not on corticosteroids, even after controlling for the severity of their rheumatic disease and other potential confounders, Jinoos Yazdany, MD, reported at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
“We saw a signal with moderate to high-dose steroids. I think it’s something we’re going to have to keep an eye out on as more data come in,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
The global registry launched on March 24, 2020, and was quickly embraced by rheumatologists from around the world. By May 12, the registry included more than 1,300 patients with a range of rheumatic diseases, all with confirmed COVID-19 infection as a requisite for enrollment; the cases were submitted by more than 300 rheumatologists in 40 countries. The registry is supported by the ACR and European League Against Rheumatism.
Dr. Yazdany, a member of the registry steering committee, described the project’s two main goals: To learn the outcomes of COVID-19–infected patients with various rheumatic diseases and to make inferences regarding the impact of the immunosuppressive and antimalarial medications widely prescribed by rheumatologists.
She presented soon-to-be-published data on the characteristics and disposition of the first 600 patients, 46% of whom were hospitalized and 9% died. A caveat regarding the registry, she noted, is that these are observational data and thus potentially subject to unrecognized confounders. Also, the registry population is skewed toward the sicker end of the COVID-19 disease spectrum because while all participants have confirmed infection, testing for the infection has been notoriously uneven. Many people are infected asymptomatically and thus may not undergo testing even where readily available.
Early key findings from registry
The risk factors for more severe infection resulting in hospitalization in patients with rheumatic diseases are by and large the same drivers described in the general population: older age and comorbid conditions including diabetes, hypertension, cardiovascular disease, obesity, chronic kidney disease, and lung disease. Notably, however, patients on the equivalent of 10 mg/day of prednisone or more were at a 105% increased risk for hospitalization, compared with those not on corticosteroids after adjustment for age, comorbid conditions, and rheumatic disease severity.
Patients on a background tumor necrosis factor (TNF) inhibitor had an adjusted 60% reduction in risk of hospitalization. This apparent protective effect against more severe COVID-19 disease is mechanistically plausible: In animal studies, being on a TNF inhibitor has been associated with less severe infection following exposure to influenza virus, Dr. Yazdany observed.
COVID-infected patients on any biologic disease-modifying antirheumatic drug had a 54% decreased risk of hospitalization. However, in this early analysis, the study was sufficiently powered only to specifically assess the impact of TNF inhibitors, since those agents were by far the most commonly used biologics. As the registry grows, it will be possible to analyze the impact of other antirheumatic medications.
Being on hydroxychloroquine or other antimalarials at the time of COVID-19 infection had no impact on hospitalization.
The only rheumatic disease diagnosis with an odds of hospitalization significantly different from that of RA patients was systemic lupus erythematosus (SLE). Lupus patients were at 80% increased risk of hospitalization. Although this was a statistically significant difference, Dr. Yazdany cautioned against making too much of it because of the strong potential for unmeasured confounding. In particular, lupus patients as a group are known to rate on the lower end of measures of social determinants of health, a status that is an established major risk factor for COVID-19 disease.
“A strength of the global registry has been that it provides timely data that’s been very helpful for rheumatologists to rapidly dispel misinformation that has been spread about hydroxychloroquine, especially statements about lupus patients not getting COVID-19. We know from these data that’s not true,” she said.
Being on background NSAIDs at the time of SARS-CoV-2 infection was not associated with increased risk of hospitalization; in fact, NSAID users were 36% less likely to be hospitalized for their COVID-19 disease, although this difference didn’t reach statistical significance.
Dr. Yazdany urged her fellow rheumatologists to enter their cases on the registry website: rheum-covid.org. There they can also join the registry mailing list and receive weekly updates.
Other recent insights on COVID-19 in rheumatology
An as-yet unpublished U.K. observational study involving electronic health record data on 17 million people included 885,000 individuals with RA, SLE, or psoriasis. After extensive statistical controlling for the known risk factors for severe COVID-19 infection, including a measure of socioeconomic deprivation, the group with one of these autoimmune diseases had an adjusted, statistically significant 23% increased risk of hospital death because of COVID-19 infection.
“This is the largest study of its kind to date. There’s potential for unmeasured confounding and selection bias here due to who gets tested. We’ll have to see where this study lands, but I think it does suggest there’s a slightly higher mortality risk in COVID-infected patients with rheumatic disease,” according to Dr. Yazdany.
On the other hand, there have been at least eight recently published patient surveys and case series of patients with rheumatic diseases in areas of the world hardest hit by the pandemic, and they paint a consistent picture.
“What we’ve learned from these studies was the infection rate was generally in the ballpark of people in the region. It doesn’t seem like there’s a dramatically higher infection rate in people with rheumatic disease in these surveys. The hospitalized rheumatology patients had many of the familiar comorbidities. This is the first glance at how likely people are to become infected and how they fared, and I think overall the data have been quite reassuring,” she said.
Dr. Yazdany reported serving as a consultant to AstraZeneca and Eli Lilly and receiving research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Centers for Disease Control and Prevention.
Patients on a tumor necrosis factor inhibitor for their rheumatic disease when they became infected with COVID-19 were markedly less likely to subsequently require hospitalization, according to intriguing early evidence from the COVID-19 Global Rheumatology Alliance Registry.
On the other hand, those registry patients who were on 10 mg of prednisone or more daily when they got infected were more than twice as likely to be hospitalized than were those who were not on corticosteroids, even after controlling for the severity of their rheumatic disease and other potential confounders, Jinoos Yazdany, MD, reported at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
“We saw a signal with moderate to high-dose steroids. I think it’s something we’re going to have to keep an eye out on as more data come in,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
The global registry launched on March 24, 2020, and was quickly embraced by rheumatologists from around the world. By May 12, the registry included more than 1,300 patients with a range of rheumatic diseases, all with confirmed COVID-19 infection as a requisite for enrollment; the cases were submitted by more than 300 rheumatologists in 40 countries. The registry is supported by the ACR and European League Against Rheumatism.
Dr. Yazdany, a member of the registry steering committee, described the project’s two main goals: To learn the outcomes of COVID-19–infected patients with various rheumatic diseases and to make inferences regarding the impact of the immunosuppressive and antimalarial medications widely prescribed by rheumatologists.
She presented soon-to-be-published data on the characteristics and disposition of the first 600 patients, 46% of whom were hospitalized and 9% died. A caveat regarding the registry, she noted, is that these are observational data and thus potentially subject to unrecognized confounders. Also, the registry population is skewed toward the sicker end of the COVID-19 disease spectrum because while all participants have confirmed infection, testing for the infection has been notoriously uneven. Many people are infected asymptomatically and thus may not undergo testing even where readily available.
Early key findings from registry
The risk factors for more severe infection resulting in hospitalization in patients with rheumatic diseases are by and large the same drivers described in the general population: older age and comorbid conditions including diabetes, hypertension, cardiovascular disease, obesity, chronic kidney disease, and lung disease. Notably, however, patients on the equivalent of 10 mg/day of prednisone or more were at a 105% increased risk for hospitalization, compared with those not on corticosteroids after adjustment for age, comorbid conditions, and rheumatic disease severity.
Patients on a background tumor necrosis factor (TNF) inhibitor had an adjusted 60% reduction in risk of hospitalization. This apparent protective effect against more severe COVID-19 disease is mechanistically plausible: In animal studies, being on a TNF inhibitor has been associated with less severe infection following exposure to influenza virus, Dr. Yazdany observed.
COVID-infected patients on any biologic disease-modifying antirheumatic drug had a 54% decreased risk of hospitalization. However, in this early analysis, the study was sufficiently powered only to specifically assess the impact of TNF inhibitors, since those agents were by far the most commonly used biologics. As the registry grows, it will be possible to analyze the impact of other antirheumatic medications.
Being on hydroxychloroquine or other antimalarials at the time of COVID-19 infection had no impact on hospitalization.
The only rheumatic disease diagnosis with an odds of hospitalization significantly different from that of RA patients was systemic lupus erythematosus (SLE). Lupus patients were at 80% increased risk of hospitalization. Although this was a statistically significant difference, Dr. Yazdany cautioned against making too much of it because of the strong potential for unmeasured confounding. In particular, lupus patients as a group are known to rate on the lower end of measures of social determinants of health, a status that is an established major risk factor for COVID-19 disease.
“A strength of the global registry has been that it provides timely data that’s been very helpful for rheumatologists to rapidly dispel misinformation that has been spread about hydroxychloroquine, especially statements about lupus patients not getting COVID-19. We know from these data that’s not true,” she said.
Being on background NSAIDs at the time of SARS-CoV-2 infection was not associated with increased risk of hospitalization; in fact, NSAID users were 36% less likely to be hospitalized for their COVID-19 disease, although this difference didn’t reach statistical significance.
Dr. Yazdany urged her fellow rheumatologists to enter their cases on the registry website: rheum-covid.org. There they can also join the registry mailing list and receive weekly updates.
Other recent insights on COVID-19 in rheumatology
An as-yet unpublished U.K. observational study involving electronic health record data on 17 million people included 885,000 individuals with RA, SLE, or psoriasis. After extensive statistical controlling for the known risk factors for severe COVID-19 infection, including a measure of socioeconomic deprivation, the group with one of these autoimmune diseases had an adjusted, statistically significant 23% increased risk of hospital death because of COVID-19 infection.
“This is the largest study of its kind to date. There’s potential for unmeasured confounding and selection bias here due to who gets tested. We’ll have to see where this study lands, but I think it does suggest there’s a slightly higher mortality risk in COVID-infected patients with rheumatic disease,” according to Dr. Yazdany.
On the other hand, there have been at least eight recently published patient surveys and case series of patients with rheumatic diseases in areas of the world hardest hit by the pandemic, and they paint a consistent picture.
“What we’ve learned from these studies was the infection rate was generally in the ballpark of people in the region. It doesn’t seem like there’s a dramatically higher infection rate in people with rheumatic disease in these surveys. The hospitalized rheumatology patients had many of the familiar comorbidities. This is the first glance at how likely people are to become infected and how they fared, and I think overall the data have been quite reassuring,” she said.
Dr. Yazdany reported serving as a consultant to AstraZeneca and Eli Lilly and receiving research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Centers for Disease Control and Prevention.
REPORTING FROM SOTA 2020
Antibody testing suggests COVID-19 cases are being missed
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
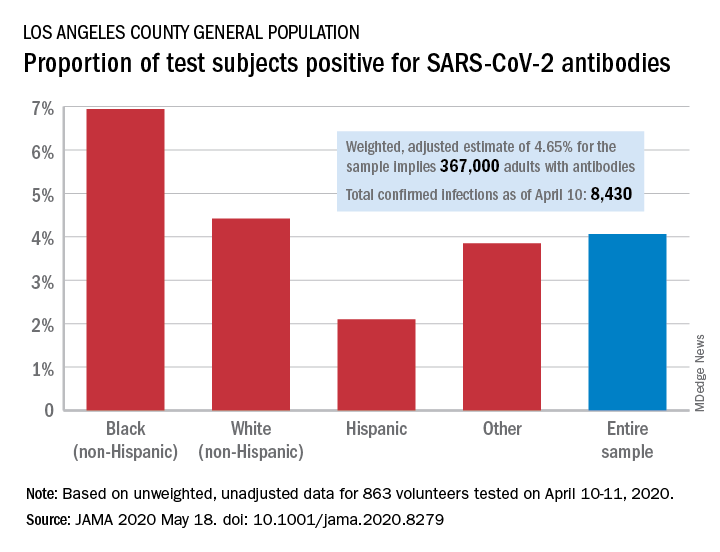
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
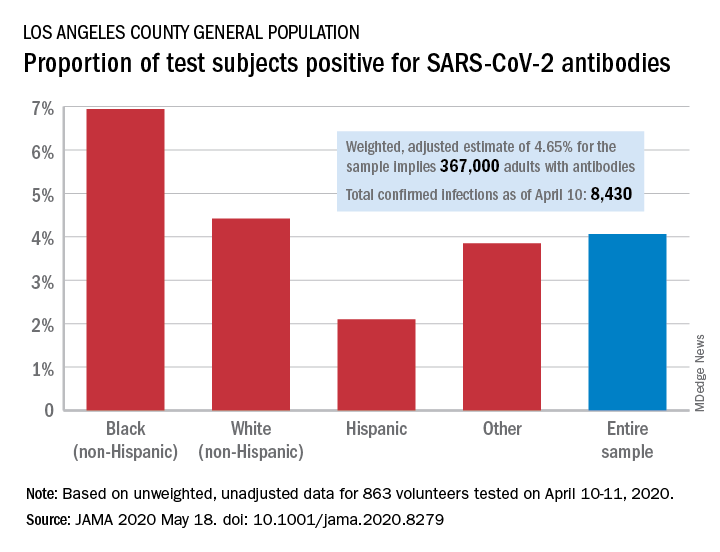
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
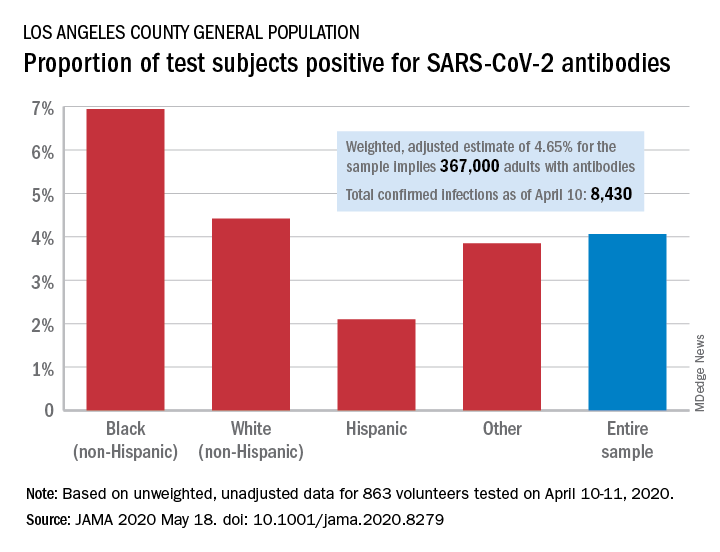
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
FROM JAMA










