User login
COVID-19: What will happen to physician income this year?
“At a combined system and hospital board meeting yesterday, there was a financial presentation,” said a cardiologist in Minnesota, who declined to be named. “We have ‘salary support’ through May 16, which means we will be receiving base pay at our 2019 level. After May 16, I think it’s fairly certain salaries will be decreased.”
A general internist in the same area added: “The system has decided to pay physicians and other employees for 8 weeks, until May 15, and they are borrowing about $150 million to do this. We don’t know what will happen after May 15, but we are supposed to have an update in early May.”
Physician income is of huge interest, and many aspects of it are discussed in Medscape’s Physician Compensation Report 2020, just released.
The worst may be yet to come
Of all the categories of physicians, “I am worried about private practices the most,” said Travis Singleton, senior vice president at Merritt Hawkins, a physician search firm. “They don’t have a financial cushion, and will start seeing big drops in revenue at the end of May.”
“A lot of the A/R [accounts receivables] for practices come within 30 days, and very little comes in after 90 days,” said Terrence R. McWilliams, MD, chief clinical consultant at HSG Advisors, a consultancy for not-for-profit hospitals and their employed physician networks around the country. “So private practices are reaching the point where prior A/R will start to dwindle and they will start feeling the decline in new claims submissions.”
Large practices may have a bigger financial cushion, but in many cases, they also have more liabilities. “We don’t know the financial loss yet, but I think it’s been devastating,” said Paul M. Yonover, MD, a urologist at UroPartners, a large single-specialty practice in Chicago with 62 urologists. “In fact, the financial loss may well be larger than our loss in volume, because we have to support our own surgery center, pathology lab, radiation center, and other in-house services.”
Employed physicians in limbo
In contrast to physicians in private practices, many employed physicians at hospitals and health systems have been shielded from the impact of COVID-19 – at least for now.
“The experiences of employed physicians are very mixed,” said Mr. Singleton at Merritt Hawkins. “Some health systems have reduced physicians’ pay by 20%, but other systems have been putting off any reductions.”
Hospitals and health systems are struggling. “Stopping elective surgeries deeply affected hospitals,” said Ryan Inman, founder of Physician Wealth Services in San Diego. “With fewer elective surgeries, they have much less income coming in. Some big hospitals that are pillars of their community are under great financial stress.”
“Hospitals’ patient volumes have fallen by 50%-90%,” Mr. McWilliams reported. “Lower volume means lower pay for employed physicians, who are paid by straight productivity or other models that require high volumes. However, some health systems have intervened to make sure these physicians get some money.”
Base pay is often safe for now, but quarterly bonuses are on the chopping block. “Employed physicians are often getting a guaranteed salary for a month or two, but no bonuses or extra distributions,” said Joel Greenwald, MD, a financial adviser for physicians in St. Louis Park, Minn., a state mecca for physician employment. “They’ve been told that they will continue to get their base salary but forget about the quarterly bonuses. This amounts to salary reductions of 10%-30%.”
Ensuring payment for these doctors means lowering their productivity benchmarks, but the benchmarks might still be too high for these times. An internist at a large health system in Minneapolis–St. Paul reports that, at a lunch meeting, employed doctors learned that payment benchmarks will be reduced to 70% of their 2019 monthly average.
“I am seeing nowhere near 70% of what I was seeing last year,” he said in an interview, asking that his name not be used. “Given how slow things have been, I am probably closer to 30%, but have not been given any data on this, so I am guessing at this point.”
Adapting to a brave new world
Even as they face a dark financial future, physicians have had to completely revamp the way they practice medicine – a cumbersome process that, in itself, incurred some financial losses. They had to obtain masks and other PPE, reposition or even close down their waiting rooms, cut back on unneeded staff, and adapt to telemedicine.
“It’s been an incredibly challenging time,” said Dr. Yonover, the Chicago urologist. “As a doctor. I cannot avoid contact, and it’s not totally clear yet how the virus spreads. But I don’t have the option of closing the door. As a practice owner, you’re responsible for the health and well-being of employees, patients, and the business.”
“A practice’s daily routine is somewhat slower and costlier,” said David N. Gans, MSHA, senior fellow at the Medical Group Management Association (MGMA), which represents group practices. “Between each patient, you have to clean a lot more than previously, and you have to stock up on PPE such as masks and gowns. PPE used to be limited to infectious patients, but now it’s universal.”
At PA Clinical Network, a clinically integrated network in Pennsylvania, volume fell 40%-50% and income fell 30%-50% from late March to late April, according to Jaan Sidorov, MD, an internist who is CEO of the network, which has 158 physicians in a variety of specialties working in 54 practices around the state.
“Revenue went down but it didn’t crash,” he said. “And our physicians pivoted very quickly. They adapted to telehealth and applied for the federal loan programs. They didn’t use waiting rooms. In some cases, staff was out in the parking lot, putting stethoscopes through patients’ windows.”
“None of the practices closed, not even temporarily,” Dr. Sidorov said. “But clearly this cannot go forever without having serious consequences.”
How much can telemedicine help?
Telemedicine has been a lifeline for many struggling practices. “As much as 20%-40% of a practice’s losses can be recouped through telemedicine, depending on variables like patients’ attitudes,” said Mr. Singleton at Merritt Hawkins.
The rise in telemedicine was made possible by a temporary relaxation of the limits on telemedicine payments by Medicare and many private payers. Medicare is currently paying the same rates for telemedicine as it does for in-office visits.
In a recent MGMA Stat survey, 97% of practices reported that they had taken up telemedicine, according to Mr. Gans. He estimates that 80% of primary care could be converted to telemedicine, including medication refills, ongoing care of chronic patients, and recording patients’ vital signs from home.
Some primary care physicians are now using telemedicine for 100% of their visits. “I voluntarily closed my practice weeks ago except for virtual visits due to the risk of exposure for my patients,” a doctor in South Carolina told the Primary Care Collaborative in mid-April. “I continue to pay my staff out of pocket but have reduced hours and am not receiving any income myself.”
However, Mr. Inman of Physician Wealth Services said family medicine clients using telemedicine for all of their patients are earning less per visit, even though the Medicare reimbursement is the same as for an office visit. “They earn less because they cannot charge for any ancillaries, such as labs or imaging,” he said.
“Telemedicine has its limits,” Mr. Singleton said. It cannot replace elective surgeries, and even in primary care practices, “there is a lot of work for which patients have to come in, such as physicals or providing vaccines,” he said. “I know of one doctor who has refrigerator full of vaccines to give out. That pays his bills.”
In many cases, “telemedicine” simply means using the phone, with no video. Many patients can only use the phone, and Medicare now reimburses for some kinds of phone visits. In a mid-April survey of primary care providers, 44% were using the telephone for the majority of their visits, and 14% were not using video at all. Medicare recently decided to pay physicians the same amount for telephone visits as in-person visits.
Financial boosts will run out soon
Many private practices are surviving only because they have managed to tap into new federal programs that can finance them for the short-term. Here are the main examples:
Receiving advance Medicare payments. Through the Medicare Accelerated and Advance Payment Program, physicians can be paid up to 3 months of their average Medicare reimbursement in advance. However, repayment starts 120 days after receiving the money and must be completed within 210 days.
Obtaining a federal loan. Under the Paycheck Protection Program (PPP), which is available to all kinds of small businesses, practices can apply for up to 2.5 times their average monthly payroll costs.
PPP money can be used for payroll, rent, mortgage interest, or utility payments for up to 8 weeks. The loan will be entirely forgiven as long as the rules are followed. For example, three quarters of the money must go to payroll, and laid-off employees must be rehired by June 30.
There was such a rush for the first round of PPP loans that many physicians failed to get the loan. “Many of my physician clients applied for the loan as soon as they could, but none of them got it,” said Mr. Inman, the San Diego financial adviser. “We are hoping that the next round of funding will provide them some relief.” The second round started on April 27.
Physicians who have already obtained the PPP loan are very relieved. “This loan made it possible for us to pay our employees,” said George W. Monks, MD, a dermatologist in Tulsa, Okla., and president of the Oklahoma Medical Association.
Staff benefiting from higher unemployment payments. Many practices and hospitals are laying off their staff so that they can collect unemployment benefits. This is a good time to do that because the federal government has boosted unemployment payments by $600 a week, creating a total benefit that is greater than many people earned at their regular jobs.
This extra boost ends in July, but practices with PPP loans will have to rehire their laid-off workers a month before that. Getting laid-off staffers to come back in is going to be critical, and some practices are already having a hard time convincing them to come back, said Michael La Penna, a physician practice manager in Grand Rapids, Mich.
“They are finding that those people don’t want to come back in yet,” he said. “In many cases they have to care for children at home or have been getting generous unemployment checks.”
The problem with all these temporary financial boosts is that they will disappear within weeks or months from now. Mr. La Penna is concerned that the sudden loss of this support could send some practices spinning into bankruptcy. “Unless volume gets better very soon, time is running out for a lot of practices,” he said.
Hospitals, which also have been depending on federal assistance, may run out of money, too. Daniel Wrenne, a financial planner for physicians in Lexington, Ky., said smaller hospitals are particularly vulnerable because they lack the capital. He said a friend who is an attorney for hospitals predicted that 25% of small regional hospitals “won’t make it through this.”
Such financial turmoil might prompt many physicians to retire or find a new job, said Gary Price, MD, a plastic surgeon in New Haven, Conn., and president of the Physicians Foundation, an advocacy group for the profession. In a survey of doctors by the Physicians Foundation and Merritt Hawkins, released on April 21, 18% planned to retire, temporarily close their practices, or opt out of patient care, and another 14%, presumably employed physicians, planned to change jobs.
Is recovery around the corner?
In early May, practices in many parts of the country were seeing the possibility of a return to normal business – or at least what could pass for normal in these unusual times.
“From mid-March to mid-April, hospitals and practices were in panic mode,” said MGMA’s Mr. Gans. “They were focusing on the here and now. But from mid-April to mid-May, they could begin looking at the big picture and decide how they will get back into business.”
Surgeons devastated by bans on elective surgeries might see a bounce in cases, as the backlog of patients comes back in. By late April, 10 states reinstituted elective surgeries, including California, Arizona, Georgia, Indiana, Colorado, and Oklahoma, and New York has reinstituted elective surgeries for some counties.
Dr. Price said he hopes to reopen his plastic surgery practice by the end of June. “If it takes longer than that, I’m not sure that the practice will survive.” His PPP loan would have run out and he would have to lay off his staff. “At that point, ongoing viability of practice would become a real question.”
Dr. Monks said he hopes a lot more patients will come to his dermatology practice. As of the end of April, “we’re starting to see an uptick in the number of patients wanting to come in,” he said. “They seem to be more comfortable with the new world we’re living in.
“Viewing the backlog of cases that haven’t been attended to,” Dr. Monks added, “I think we’ll be really busy for a while.”
But Mr. La Penna said he thinks the expected backlog of elective patients will be more like a trickle than a flood. “Many patients aren’t going to want to return that fast,” he said. “They may have a condition that makes exposure to COVID-19 more risky, like diabetes or high blood pressure, or they’re elderly, or they live in a household with one of these risk groups.”
Andrew Musbach, cofounder of MD Wealth Management in Chelsea, Mich., said he expects a slow recovery for primary care physicians as well. “Even when the lockdowns are over, not everyone is going to feel comfortable coming to a hospital or visiting a doctor’s office unless it’s absolutely necessary,” he said.
Getting back to normal patient volumes will involve finding better ways to protect patients and staff from COVID-19, Dr. Yonover said. At his urology practice, “we take all the usual precautions, but nothing yet has made it dramatically easier to protect patients and staff,” he said. “Rapid, accurate testing for COVID-19 would change the landscape, but I have no idea when that will come.”
Mr. Wrenne advises his physician clients that a financial recovery will take months. “I tell them to plan for 6 months, until October, before income returns to pre–COVID-19 levels. Reimbursement lags appointments by as much as 3 months, plus it will probably take the economy 2-3 months more to get back to normal.”
“We are facing a recession, and how long it will last is anyone’s guess,” said Alex Kilian, a physician wealth manager at Aldrich Wealth in San Diego. “The federal government’s efforts to stimulate the economy is keeping it from crashing, but there are no real signs that it will actually pick up. It may take years for the travel and entertainment industries to come back.”
A recession means patients will have less spending power, and health care sectors like laser eye surgery may be damaged for years to come, said John B. Pinto, an ophthalmology practice management consultant in San Diego. “[That kind of surgery] is purely elective and relatively costly,” he said. “When people get back to work, they are going to be building up their savings and avoiding new debt. They won’t be having [laser eye surgery].”
“There won’t be any quick return to normal for me,” said Dr. Price, the Connecticut plastic surgeon. “The damage this time will probably be worse than in the Great Recession. Back then, plastic surgery was off by 20%, but this time you have the extra problem of patients reluctant to come into medical offices.”
“To get patients to come in, facilities are going to have to convince patients that they are safe,” Mr. Singleton said. “That may mean undertaking some marketing and promotion, and hospitals tend to be much better at that than practices.”
What a new wave of COVID-19 would mean
Some states have begun reopening public places, which could signal patients to return to doctors’ offices even though doctors’ offices were never officially closed. Oklahoma, for example, reopened restaurants, movie theaters, and sports venues on May 1.
Dr. Monks, president of the Oklahoma Medical Association, said his group opposes states reopening. “The governor’s order is too hasty and overly ambitious,” he said. “Oklahoma has seen an ongoing growth in the number of cases, hospitalizations, and deaths in the past week alone [in late April].”
The concern is that opening up public places too soon would create a new wave of COVID-19, which would not only be a public health disaster, but also a financial disaster for physicians. Doctors would be back where they were in March, but unlike in March, they would not benefit from revenues from previously busy times.
Mr. Pinto said the number of COVID-19 cases will rise and fall in the next 2 years, forcing states to reenact new bans on public gatherings and on elective surgeries until the numbers subside again.
Mr. Pinto said authorities in Singapore have successfully handled such waves of the disease through short bans that are tantamount to tapping the brakes of a car. “As the car gathers speed down the hill, you tap the brake,” he said. “I suspect we’ll be seeing a lot of brake-tapping until a vaccine can be developed and distributed.”
Gary LeRoy, MD, president of the American Academy of Family Physicians, recalled the worldwide Spanish Flu pandemic a century ago. “People were allowed out of their houses after 2 months, and the flu spiked up again,” he said. “I hope we don’t make that mistake this time.”
Dr. LeRoy said it’s not possible to predict how the COVID-19 crisis will play out. “What will the future be like? I don’t know the answer,” he said. “The information we learn in next hours, days, or months will probably change everything.”
A version of this article originally appeared on Medscape.com.
“At a combined system and hospital board meeting yesterday, there was a financial presentation,” said a cardiologist in Minnesota, who declined to be named. “We have ‘salary support’ through May 16, which means we will be receiving base pay at our 2019 level. After May 16, I think it’s fairly certain salaries will be decreased.”
A general internist in the same area added: “The system has decided to pay physicians and other employees for 8 weeks, until May 15, and they are borrowing about $150 million to do this. We don’t know what will happen after May 15, but we are supposed to have an update in early May.”
Physician income is of huge interest, and many aspects of it are discussed in Medscape’s Physician Compensation Report 2020, just released.
The worst may be yet to come
Of all the categories of physicians, “I am worried about private practices the most,” said Travis Singleton, senior vice president at Merritt Hawkins, a physician search firm. “They don’t have a financial cushion, and will start seeing big drops in revenue at the end of May.”
“A lot of the A/R [accounts receivables] for practices come within 30 days, and very little comes in after 90 days,” said Terrence R. McWilliams, MD, chief clinical consultant at HSG Advisors, a consultancy for not-for-profit hospitals and their employed physician networks around the country. “So private practices are reaching the point where prior A/R will start to dwindle and they will start feeling the decline in new claims submissions.”
Large practices may have a bigger financial cushion, but in many cases, they also have more liabilities. “We don’t know the financial loss yet, but I think it’s been devastating,” said Paul M. Yonover, MD, a urologist at UroPartners, a large single-specialty practice in Chicago with 62 urologists. “In fact, the financial loss may well be larger than our loss in volume, because we have to support our own surgery center, pathology lab, radiation center, and other in-house services.”
Employed physicians in limbo
In contrast to physicians in private practices, many employed physicians at hospitals and health systems have been shielded from the impact of COVID-19 – at least for now.
“The experiences of employed physicians are very mixed,” said Mr. Singleton at Merritt Hawkins. “Some health systems have reduced physicians’ pay by 20%, but other systems have been putting off any reductions.”
Hospitals and health systems are struggling. “Stopping elective surgeries deeply affected hospitals,” said Ryan Inman, founder of Physician Wealth Services in San Diego. “With fewer elective surgeries, they have much less income coming in. Some big hospitals that are pillars of their community are under great financial stress.”
“Hospitals’ patient volumes have fallen by 50%-90%,” Mr. McWilliams reported. “Lower volume means lower pay for employed physicians, who are paid by straight productivity or other models that require high volumes. However, some health systems have intervened to make sure these physicians get some money.”
Base pay is often safe for now, but quarterly bonuses are on the chopping block. “Employed physicians are often getting a guaranteed salary for a month or two, but no bonuses or extra distributions,” said Joel Greenwald, MD, a financial adviser for physicians in St. Louis Park, Minn., a state mecca for physician employment. “They’ve been told that they will continue to get their base salary but forget about the quarterly bonuses. This amounts to salary reductions of 10%-30%.”
Ensuring payment for these doctors means lowering their productivity benchmarks, but the benchmarks might still be too high for these times. An internist at a large health system in Minneapolis–St. Paul reports that, at a lunch meeting, employed doctors learned that payment benchmarks will be reduced to 70% of their 2019 monthly average.
“I am seeing nowhere near 70% of what I was seeing last year,” he said in an interview, asking that his name not be used. “Given how slow things have been, I am probably closer to 30%, but have not been given any data on this, so I am guessing at this point.”
Adapting to a brave new world
Even as they face a dark financial future, physicians have had to completely revamp the way they practice medicine – a cumbersome process that, in itself, incurred some financial losses. They had to obtain masks and other PPE, reposition or even close down their waiting rooms, cut back on unneeded staff, and adapt to telemedicine.
“It’s been an incredibly challenging time,” said Dr. Yonover, the Chicago urologist. “As a doctor. I cannot avoid contact, and it’s not totally clear yet how the virus spreads. But I don’t have the option of closing the door. As a practice owner, you’re responsible for the health and well-being of employees, patients, and the business.”
“A practice’s daily routine is somewhat slower and costlier,” said David N. Gans, MSHA, senior fellow at the Medical Group Management Association (MGMA), which represents group practices. “Between each patient, you have to clean a lot more than previously, and you have to stock up on PPE such as masks and gowns. PPE used to be limited to infectious patients, but now it’s universal.”
At PA Clinical Network, a clinically integrated network in Pennsylvania, volume fell 40%-50% and income fell 30%-50% from late March to late April, according to Jaan Sidorov, MD, an internist who is CEO of the network, which has 158 physicians in a variety of specialties working in 54 practices around the state.
“Revenue went down but it didn’t crash,” he said. “And our physicians pivoted very quickly. They adapted to telehealth and applied for the federal loan programs. They didn’t use waiting rooms. In some cases, staff was out in the parking lot, putting stethoscopes through patients’ windows.”
“None of the practices closed, not even temporarily,” Dr. Sidorov said. “But clearly this cannot go forever without having serious consequences.”
How much can telemedicine help?
Telemedicine has been a lifeline for many struggling practices. “As much as 20%-40% of a practice’s losses can be recouped through telemedicine, depending on variables like patients’ attitudes,” said Mr. Singleton at Merritt Hawkins.
The rise in telemedicine was made possible by a temporary relaxation of the limits on telemedicine payments by Medicare and many private payers. Medicare is currently paying the same rates for telemedicine as it does for in-office visits.
In a recent MGMA Stat survey, 97% of practices reported that they had taken up telemedicine, according to Mr. Gans. He estimates that 80% of primary care could be converted to telemedicine, including medication refills, ongoing care of chronic patients, and recording patients’ vital signs from home.
Some primary care physicians are now using telemedicine for 100% of their visits. “I voluntarily closed my practice weeks ago except for virtual visits due to the risk of exposure for my patients,” a doctor in South Carolina told the Primary Care Collaborative in mid-April. “I continue to pay my staff out of pocket but have reduced hours and am not receiving any income myself.”
However, Mr. Inman of Physician Wealth Services said family medicine clients using telemedicine for all of their patients are earning less per visit, even though the Medicare reimbursement is the same as for an office visit. “They earn less because they cannot charge for any ancillaries, such as labs or imaging,” he said.
“Telemedicine has its limits,” Mr. Singleton said. It cannot replace elective surgeries, and even in primary care practices, “there is a lot of work for which patients have to come in, such as physicals or providing vaccines,” he said. “I know of one doctor who has refrigerator full of vaccines to give out. That pays his bills.”
In many cases, “telemedicine” simply means using the phone, with no video. Many patients can only use the phone, and Medicare now reimburses for some kinds of phone visits. In a mid-April survey of primary care providers, 44% were using the telephone for the majority of their visits, and 14% were not using video at all. Medicare recently decided to pay physicians the same amount for telephone visits as in-person visits.
Financial boosts will run out soon
Many private practices are surviving only because they have managed to tap into new federal programs that can finance them for the short-term. Here are the main examples:
Receiving advance Medicare payments. Through the Medicare Accelerated and Advance Payment Program, physicians can be paid up to 3 months of their average Medicare reimbursement in advance. However, repayment starts 120 days after receiving the money and must be completed within 210 days.
Obtaining a federal loan. Under the Paycheck Protection Program (PPP), which is available to all kinds of small businesses, practices can apply for up to 2.5 times their average monthly payroll costs.
PPP money can be used for payroll, rent, mortgage interest, or utility payments for up to 8 weeks. The loan will be entirely forgiven as long as the rules are followed. For example, three quarters of the money must go to payroll, and laid-off employees must be rehired by June 30.
There was such a rush for the first round of PPP loans that many physicians failed to get the loan. “Many of my physician clients applied for the loan as soon as they could, but none of them got it,” said Mr. Inman, the San Diego financial adviser. “We are hoping that the next round of funding will provide them some relief.” The second round started on April 27.
Physicians who have already obtained the PPP loan are very relieved. “This loan made it possible for us to pay our employees,” said George W. Monks, MD, a dermatologist in Tulsa, Okla., and president of the Oklahoma Medical Association.
Staff benefiting from higher unemployment payments. Many practices and hospitals are laying off their staff so that they can collect unemployment benefits. This is a good time to do that because the federal government has boosted unemployment payments by $600 a week, creating a total benefit that is greater than many people earned at their regular jobs.
This extra boost ends in July, but practices with PPP loans will have to rehire their laid-off workers a month before that. Getting laid-off staffers to come back in is going to be critical, and some practices are already having a hard time convincing them to come back, said Michael La Penna, a physician practice manager in Grand Rapids, Mich.
“They are finding that those people don’t want to come back in yet,” he said. “In many cases they have to care for children at home or have been getting generous unemployment checks.”
The problem with all these temporary financial boosts is that they will disappear within weeks or months from now. Mr. La Penna is concerned that the sudden loss of this support could send some practices spinning into bankruptcy. “Unless volume gets better very soon, time is running out for a lot of practices,” he said.
Hospitals, which also have been depending on federal assistance, may run out of money, too. Daniel Wrenne, a financial planner for physicians in Lexington, Ky., said smaller hospitals are particularly vulnerable because they lack the capital. He said a friend who is an attorney for hospitals predicted that 25% of small regional hospitals “won’t make it through this.”
Such financial turmoil might prompt many physicians to retire or find a new job, said Gary Price, MD, a plastic surgeon in New Haven, Conn., and president of the Physicians Foundation, an advocacy group for the profession. In a survey of doctors by the Physicians Foundation and Merritt Hawkins, released on April 21, 18% planned to retire, temporarily close their practices, or opt out of patient care, and another 14%, presumably employed physicians, planned to change jobs.
Is recovery around the corner?
In early May, practices in many parts of the country were seeing the possibility of a return to normal business – or at least what could pass for normal in these unusual times.
“From mid-March to mid-April, hospitals and practices were in panic mode,” said MGMA’s Mr. Gans. “They were focusing on the here and now. But from mid-April to mid-May, they could begin looking at the big picture and decide how they will get back into business.”
Surgeons devastated by bans on elective surgeries might see a bounce in cases, as the backlog of patients comes back in. By late April, 10 states reinstituted elective surgeries, including California, Arizona, Georgia, Indiana, Colorado, and Oklahoma, and New York has reinstituted elective surgeries for some counties.
Dr. Price said he hopes to reopen his plastic surgery practice by the end of June. “If it takes longer than that, I’m not sure that the practice will survive.” His PPP loan would have run out and he would have to lay off his staff. “At that point, ongoing viability of practice would become a real question.”
Dr. Monks said he hopes a lot more patients will come to his dermatology practice. As of the end of April, “we’re starting to see an uptick in the number of patients wanting to come in,” he said. “They seem to be more comfortable with the new world we’re living in.
“Viewing the backlog of cases that haven’t been attended to,” Dr. Monks added, “I think we’ll be really busy for a while.”
But Mr. La Penna said he thinks the expected backlog of elective patients will be more like a trickle than a flood. “Many patients aren’t going to want to return that fast,” he said. “They may have a condition that makes exposure to COVID-19 more risky, like diabetes or high blood pressure, or they’re elderly, or they live in a household with one of these risk groups.”
Andrew Musbach, cofounder of MD Wealth Management in Chelsea, Mich., said he expects a slow recovery for primary care physicians as well. “Even when the lockdowns are over, not everyone is going to feel comfortable coming to a hospital or visiting a doctor’s office unless it’s absolutely necessary,” he said.
Getting back to normal patient volumes will involve finding better ways to protect patients and staff from COVID-19, Dr. Yonover said. At his urology practice, “we take all the usual precautions, but nothing yet has made it dramatically easier to protect patients and staff,” he said. “Rapid, accurate testing for COVID-19 would change the landscape, but I have no idea when that will come.”
Mr. Wrenne advises his physician clients that a financial recovery will take months. “I tell them to plan for 6 months, until October, before income returns to pre–COVID-19 levels. Reimbursement lags appointments by as much as 3 months, plus it will probably take the economy 2-3 months more to get back to normal.”
“We are facing a recession, and how long it will last is anyone’s guess,” said Alex Kilian, a physician wealth manager at Aldrich Wealth in San Diego. “The federal government’s efforts to stimulate the economy is keeping it from crashing, but there are no real signs that it will actually pick up. It may take years for the travel and entertainment industries to come back.”
A recession means patients will have less spending power, and health care sectors like laser eye surgery may be damaged for years to come, said John B. Pinto, an ophthalmology practice management consultant in San Diego. “[That kind of surgery] is purely elective and relatively costly,” he said. “When people get back to work, they are going to be building up their savings and avoiding new debt. They won’t be having [laser eye surgery].”
“There won’t be any quick return to normal for me,” said Dr. Price, the Connecticut plastic surgeon. “The damage this time will probably be worse than in the Great Recession. Back then, plastic surgery was off by 20%, but this time you have the extra problem of patients reluctant to come into medical offices.”
“To get patients to come in, facilities are going to have to convince patients that they are safe,” Mr. Singleton said. “That may mean undertaking some marketing and promotion, and hospitals tend to be much better at that than practices.”
What a new wave of COVID-19 would mean
Some states have begun reopening public places, which could signal patients to return to doctors’ offices even though doctors’ offices were never officially closed. Oklahoma, for example, reopened restaurants, movie theaters, and sports venues on May 1.
Dr. Monks, president of the Oklahoma Medical Association, said his group opposes states reopening. “The governor’s order is too hasty and overly ambitious,” he said. “Oklahoma has seen an ongoing growth in the number of cases, hospitalizations, and deaths in the past week alone [in late April].”
The concern is that opening up public places too soon would create a new wave of COVID-19, which would not only be a public health disaster, but also a financial disaster for physicians. Doctors would be back where they were in March, but unlike in March, they would not benefit from revenues from previously busy times.
Mr. Pinto said the number of COVID-19 cases will rise and fall in the next 2 years, forcing states to reenact new bans on public gatherings and on elective surgeries until the numbers subside again.
Mr. Pinto said authorities in Singapore have successfully handled such waves of the disease through short bans that are tantamount to tapping the brakes of a car. “As the car gathers speed down the hill, you tap the brake,” he said. “I suspect we’ll be seeing a lot of brake-tapping until a vaccine can be developed and distributed.”
Gary LeRoy, MD, president of the American Academy of Family Physicians, recalled the worldwide Spanish Flu pandemic a century ago. “People were allowed out of their houses after 2 months, and the flu spiked up again,” he said. “I hope we don’t make that mistake this time.”
Dr. LeRoy said it’s not possible to predict how the COVID-19 crisis will play out. “What will the future be like? I don’t know the answer,” he said. “The information we learn in next hours, days, or months will probably change everything.”
A version of this article originally appeared on Medscape.com.
“At a combined system and hospital board meeting yesterday, there was a financial presentation,” said a cardiologist in Minnesota, who declined to be named. “We have ‘salary support’ through May 16, which means we will be receiving base pay at our 2019 level. After May 16, I think it’s fairly certain salaries will be decreased.”
A general internist in the same area added: “The system has decided to pay physicians and other employees for 8 weeks, until May 15, and they are borrowing about $150 million to do this. We don’t know what will happen after May 15, but we are supposed to have an update in early May.”
Physician income is of huge interest, and many aspects of it are discussed in Medscape’s Physician Compensation Report 2020, just released.
The worst may be yet to come
Of all the categories of physicians, “I am worried about private practices the most,” said Travis Singleton, senior vice president at Merritt Hawkins, a physician search firm. “They don’t have a financial cushion, and will start seeing big drops in revenue at the end of May.”
“A lot of the A/R [accounts receivables] for practices come within 30 days, and very little comes in after 90 days,” said Terrence R. McWilliams, MD, chief clinical consultant at HSG Advisors, a consultancy for not-for-profit hospitals and their employed physician networks around the country. “So private practices are reaching the point where prior A/R will start to dwindle and they will start feeling the decline in new claims submissions.”
Large practices may have a bigger financial cushion, but in many cases, they also have more liabilities. “We don’t know the financial loss yet, but I think it’s been devastating,” said Paul M. Yonover, MD, a urologist at UroPartners, a large single-specialty practice in Chicago with 62 urologists. “In fact, the financial loss may well be larger than our loss in volume, because we have to support our own surgery center, pathology lab, radiation center, and other in-house services.”
Employed physicians in limbo
In contrast to physicians in private practices, many employed physicians at hospitals and health systems have been shielded from the impact of COVID-19 – at least for now.
“The experiences of employed physicians are very mixed,” said Mr. Singleton at Merritt Hawkins. “Some health systems have reduced physicians’ pay by 20%, but other systems have been putting off any reductions.”
Hospitals and health systems are struggling. “Stopping elective surgeries deeply affected hospitals,” said Ryan Inman, founder of Physician Wealth Services in San Diego. “With fewer elective surgeries, they have much less income coming in. Some big hospitals that are pillars of their community are under great financial stress.”
“Hospitals’ patient volumes have fallen by 50%-90%,” Mr. McWilliams reported. “Lower volume means lower pay for employed physicians, who are paid by straight productivity or other models that require high volumes. However, some health systems have intervened to make sure these physicians get some money.”
Base pay is often safe for now, but quarterly bonuses are on the chopping block. “Employed physicians are often getting a guaranteed salary for a month or two, but no bonuses or extra distributions,” said Joel Greenwald, MD, a financial adviser for physicians in St. Louis Park, Minn., a state mecca for physician employment. “They’ve been told that they will continue to get their base salary but forget about the quarterly bonuses. This amounts to salary reductions of 10%-30%.”
Ensuring payment for these doctors means lowering their productivity benchmarks, but the benchmarks might still be too high for these times. An internist at a large health system in Minneapolis–St. Paul reports that, at a lunch meeting, employed doctors learned that payment benchmarks will be reduced to 70% of their 2019 monthly average.
“I am seeing nowhere near 70% of what I was seeing last year,” he said in an interview, asking that his name not be used. “Given how slow things have been, I am probably closer to 30%, but have not been given any data on this, so I am guessing at this point.”
Adapting to a brave new world
Even as they face a dark financial future, physicians have had to completely revamp the way they practice medicine – a cumbersome process that, in itself, incurred some financial losses. They had to obtain masks and other PPE, reposition or even close down their waiting rooms, cut back on unneeded staff, and adapt to telemedicine.
“It’s been an incredibly challenging time,” said Dr. Yonover, the Chicago urologist. “As a doctor. I cannot avoid contact, and it’s not totally clear yet how the virus spreads. But I don’t have the option of closing the door. As a practice owner, you’re responsible for the health and well-being of employees, patients, and the business.”
“A practice’s daily routine is somewhat slower and costlier,” said David N. Gans, MSHA, senior fellow at the Medical Group Management Association (MGMA), which represents group practices. “Between each patient, you have to clean a lot more than previously, and you have to stock up on PPE such as masks and gowns. PPE used to be limited to infectious patients, but now it’s universal.”
At PA Clinical Network, a clinically integrated network in Pennsylvania, volume fell 40%-50% and income fell 30%-50% from late March to late April, according to Jaan Sidorov, MD, an internist who is CEO of the network, which has 158 physicians in a variety of specialties working in 54 practices around the state.
“Revenue went down but it didn’t crash,” he said. “And our physicians pivoted very quickly. They adapted to telehealth and applied for the federal loan programs. They didn’t use waiting rooms. In some cases, staff was out in the parking lot, putting stethoscopes through patients’ windows.”
“None of the practices closed, not even temporarily,” Dr. Sidorov said. “But clearly this cannot go forever without having serious consequences.”
How much can telemedicine help?
Telemedicine has been a lifeline for many struggling practices. “As much as 20%-40% of a practice’s losses can be recouped through telemedicine, depending on variables like patients’ attitudes,” said Mr. Singleton at Merritt Hawkins.
The rise in telemedicine was made possible by a temporary relaxation of the limits on telemedicine payments by Medicare and many private payers. Medicare is currently paying the same rates for telemedicine as it does for in-office visits.
In a recent MGMA Stat survey, 97% of practices reported that they had taken up telemedicine, according to Mr. Gans. He estimates that 80% of primary care could be converted to telemedicine, including medication refills, ongoing care of chronic patients, and recording patients’ vital signs from home.
Some primary care physicians are now using telemedicine for 100% of their visits. “I voluntarily closed my practice weeks ago except for virtual visits due to the risk of exposure for my patients,” a doctor in South Carolina told the Primary Care Collaborative in mid-April. “I continue to pay my staff out of pocket but have reduced hours and am not receiving any income myself.”
However, Mr. Inman of Physician Wealth Services said family medicine clients using telemedicine for all of their patients are earning less per visit, even though the Medicare reimbursement is the same as for an office visit. “They earn less because they cannot charge for any ancillaries, such as labs or imaging,” he said.
“Telemedicine has its limits,” Mr. Singleton said. It cannot replace elective surgeries, and even in primary care practices, “there is a lot of work for which patients have to come in, such as physicals or providing vaccines,” he said. “I know of one doctor who has refrigerator full of vaccines to give out. That pays his bills.”
In many cases, “telemedicine” simply means using the phone, with no video. Many patients can only use the phone, and Medicare now reimburses for some kinds of phone visits. In a mid-April survey of primary care providers, 44% were using the telephone for the majority of their visits, and 14% were not using video at all. Medicare recently decided to pay physicians the same amount for telephone visits as in-person visits.
Financial boosts will run out soon
Many private practices are surviving only because they have managed to tap into new federal programs that can finance them for the short-term. Here are the main examples:
Receiving advance Medicare payments. Through the Medicare Accelerated and Advance Payment Program, physicians can be paid up to 3 months of their average Medicare reimbursement in advance. However, repayment starts 120 days after receiving the money and must be completed within 210 days.
Obtaining a federal loan. Under the Paycheck Protection Program (PPP), which is available to all kinds of small businesses, practices can apply for up to 2.5 times their average monthly payroll costs.
PPP money can be used for payroll, rent, mortgage interest, or utility payments for up to 8 weeks. The loan will be entirely forgiven as long as the rules are followed. For example, three quarters of the money must go to payroll, and laid-off employees must be rehired by June 30.
There was such a rush for the first round of PPP loans that many physicians failed to get the loan. “Many of my physician clients applied for the loan as soon as they could, but none of them got it,” said Mr. Inman, the San Diego financial adviser. “We are hoping that the next round of funding will provide them some relief.” The second round started on April 27.
Physicians who have already obtained the PPP loan are very relieved. “This loan made it possible for us to pay our employees,” said George W. Monks, MD, a dermatologist in Tulsa, Okla., and president of the Oklahoma Medical Association.
Staff benefiting from higher unemployment payments. Many practices and hospitals are laying off their staff so that they can collect unemployment benefits. This is a good time to do that because the federal government has boosted unemployment payments by $600 a week, creating a total benefit that is greater than many people earned at their regular jobs.
This extra boost ends in July, but practices with PPP loans will have to rehire their laid-off workers a month before that. Getting laid-off staffers to come back in is going to be critical, and some practices are already having a hard time convincing them to come back, said Michael La Penna, a physician practice manager in Grand Rapids, Mich.
“They are finding that those people don’t want to come back in yet,” he said. “In many cases they have to care for children at home or have been getting generous unemployment checks.”
The problem with all these temporary financial boosts is that they will disappear within weeks or months from now. Mr. La Penna is concerned that the sudden loss of this support could send some practices spinning into bankruptcy. “Unless volume gets better very soon, time is running out for a lot of practices,” he said.
Hospitals, which also have been depending on federal assistance, may run out of money, too. Daniel Wrenne, a financial planner for physicians in Lexington, Ky., said smaller hospitals are particularly vulnerable because they lack the capital. He said a friend who is an attorney for hospitals predicted that 25% of small regional hospitals “won’t make it through this.”
Such financial turmoil might prompt many physicians to retire or find a new job, said Gary Price, MD, a plastic surgeon in New Haven, Conn., and president of the Physicians Foundation, an advocacy group for the profession. In a survey of doctors by the Physicians Foundation and Merritt Hawkins, released on April 21, 18% planned to retire, temporarily close their practices, or opt out of patient care, and another 14%, presumably employed physicians, planned to change jobs.
Is recovery around the corner?
In early May, practices in many parts of the country were seeing the possibility of a return to normal business – or at least what could pass for normal in these unusual times.
“From mid-March to mid-April, hospitals and practices were in panic mode,” said MGMA’s Mr. Gans. “They were focusing on the here and now. But from mid-April to mid-May, they could begin looking at the big picture and decide how they will get back into business.”
Surgeons devastated by bans on elective surgeries might see a bounce in cases, as the backlog of patients comes back in. By late April, 10 states reinstituted elective surgeries, including California, Arizona, Georgia, Indiana, Colorado, and Oklahoma, and New York has reinstituted elective surgeries for some counties.
Dr. Price said he hopes to reopen his plastic surgery practice by the end of June. “If it takes longer than that, I’m not sure that the practice will survive.” His PPP loan would have run out and he would have to lay off his staff. “At that point, ongoing viability of practice would become a real question.”
Dr. Monks said he hopes a lot more patients will come to his dermatology practice. As of the end of April, “we’re starting to see an uptick in the number of patients wanting to come in,” he said. “They seem to be more comfortable with the new world we’re living in.
“Viewing the backlog of cases that haven’t been attended to,” Dr. Monks added, “I think we’ll be really busy for a while.”
But Mr. La Penna said he thinks the expected backlog of elective patients will be more like a trickle than a flood. “Many patients aren’t going to want to return that fast,” he said. “They may have a condition that makes exposure to COVID-19 more risky, like diabetes or high blood pressure, or they’re elderly, or they live in a household with one of these risk groups.”
Andrew Musbach, cofounder of MD Wealth Management in Chelsea, Mich., said he expects a slow recovery for primary care physicians as well. “Even when the lockdowns are over, not everyone is going to feel comfortable coming to a hospital or visiting a doctor’s office unless it’s absolutely necessary,” he said.
Getting back to normal patient volumes will involve finding better ways to protect patients and staff from COVID-19, Dr. Yonover said. At his urology practice, “we take all the usual precautions, but nothing yet has made it dramatically easier to protect patients and staff,” he said. “Rapid, accurate testing for COVID-19 would change the landscape, but I have no idea when that will come.”
Mr. Wrenne advises his physician clients that a financial recovery will take months. “I tell them to plan for 6 months, until October, before income returns to pre–COVID-19 levels. Reimbursement lags appointments by as much as 3 months, plus it will probably take the economy 2-3 months more to get back to normal.”
“We are facing a recession, and how long it will last is anyone’s guess,” said Alex Kilian, a physician wealth manager at Aldrich Wealth in San Diego. “The federal government’s efforts to stimulate the economy is keeping it from crashing, but there are no real signs that it will actually pick up. It may take years for the travel and entertainment industries to come back.”
A recession means patients will have less spending power, and health care sectors like laser eye surgery may be damaged for years to come, said John B. Pinto, an ophthalmology practice management consultant in San Diego. “[That kind of surgery] is purely elective and relatively costly,” he said. “When people get back to work, they are going to be building up their savings and avoiding new debt. They won’t be having [laser eye surgery].”
“There won’t be any quick return to normal for me,” said Dr. Price, the Connecticut plastic surgeon. “The damage this time will probably be worse than in the Great Recession. Back then, plastic surgery was off by 20%, but this time you have the extra problem of patients reluctant to come into medical offices.”
“To get patients to come in, facilities are going to have to convince patients that they are safe,” Mr. Singleton said. “That may mean undertaking some marketing and promotion, and hospitals tend to be much better at that than practices.”
What a new wave of COVID-19 would mean
Some states have begun reopening public places, which could signal patients to return to doctors’ offices even though doctors’ offices were never officially closed. Oklahoma, for example, reopened restaurants, movie theaters, and sports venues on May 1.
Dr. Monks, president of the Oklahoma Medical Association, said his group opposes states reopening. “The governor’s order is too hasty and overly ambitious,” he said. “Oklahoma has seen an ongoing growth in the number of cases, hospitalizations, and deaths in the past week alone [in late April].”
The concern is that opening up public places too soon would create a new wave of COVID-19, which would not only be a public health disaster, but also a financial disaster for physicians. Doctors would be back where they were in March, but unlike in March, they would not benefit from revenues from previously busy times.
Mr. Pinto said the number of COVID-19 cases will rise and fall in the next 2 years, forcing states to reenact new bans on public gatherings and on elective surgeries until the numbers subside again.
Mr. Pinto said authorities in Singapore have successfully handled such waves of the disease through short bans that are tantamount to tapping the brakes of a car. “As the car gathers speed down the hill, you tap the brake,” he said. “I suspect we’ll be seeing a lot of brake-tapping until a vaccine can be developed and distributed.”
Gary LeRoy, MD, president of the American Academy of Family Physicians, recalled the worldwide Spanish Flu pandemic a century ago. “People were allowed out of their houses after 2 months, and the flu spiked up again,” he said. “I hope we don’t make that mistake this time.”
Dr. LeRoy said it’s not possible to predict how the COVID-19 crisis will play out. “What will the future be like? I don’t know the answer,” he said. “The information we learn in next hours, days, or months will probably change everything.”
A version of this article originally appeared on Medscape.com.
Managing Trichomonas vaginalis infections
CASE Woman with malodorous vaginal discharge
A 26-year-old nulligravid woman with 2 current sexual partners requests evaluation because she has a yellow-green frothy vaginal discharge that is slightly malodorous. One of her sexual partners has noted a similar discharge from his urethra. On physical examination, the clinician notes that the patient’s discharge emanates from the vaginal mucosa, and the exocervix has multiple punctate hemorrhages. Considerations in this case include:
- What is the most likely diagnosis?
- How should this patient be evaluated and treated?
- Should the patient’s sexual partners be treated?
This clinical scenario is most consistent with a trichomonas infection, although other conditions, including bacterial vaginosis, gonorrhea, and chlamydia infection, must be considered in the differential diagnosis.
In this article, we examine the microbiology, epidemiology, clinical manifestations, and diagnosis and treatment of this common sexually transmitted infection (STI).
The causative microbe
Trichomonas vaginalis is a free-living flagellated protozoan that accounts for almost half of all nonviral STIs globally. It has a predilection for the mucosal epithelium of the genitourinary tract, including the vagina and urethra. Humans are the only known host for T vaginalis. The infection is transmitted through sexual intercourse, and the organism reproduces through binary fission in the lower genital tract of women and in the urethra and prostate of men.
This anaerobic trophozoite has 4 flagella anteriorly and 1 flagellum that projects posteriorly, with an undulating membrane that gives its characteristic motile appearance on saline microscopy.1
T vaginalis infection causes major mechanical stress on epithelial cells, which results in disruption of the plasma cell membrane and, ultimately, cell death. The necrotic cell fragments are then phagocytosed by trichomonads, thus accelerating the infection.2
Groups at risk
Trichomonal infections are not reportable to public health authorities, which makes assessing the true prevalence of infection difficult.
The World Health Organization estimated the incidence of infection to be more than 156 million cases globally in 2016, with a prevalence of 110.4 million people at any one time.3
The 2013-2014 National Health and Nutrition Examination Survey tested 4,057 men and women aged 18 to 59 years for T vaginalis and found a prevalence of 0.5% among men and 1.8% among women.4 The prevalence increased with age. There was a disproportionate burden of trichomonas infections in the non-Hispanic black population, with 4.2% of black men and 8.9% of black women affected.4
Targeted screening of urogenital samples for T vaginalis in a population of US women undergoing Chlamydia trachomatis/Neisseria gonorrhoeae screening demonstrated prevalence rates of 8.7%, 6.7%, and 1.7% for T vaginalis, C trachomatis, and N gonorrhoeae, respectively.5
Differences in prevalence estimates may be due to differences in the varying sensitivity of each testing modality and patient populations. In one study, nucleic acid amplification testing (NAAT) for T vaginalis detected rates as high as 11.3% in women and 6.1% in men undergoing evaluations at STI clinics.6
Continue to: Clinical manifestations of infection...
Clinical manifestations of infection
Most cases of T vaginalis remain in an asymptomatic carrier state, with up to 85% of women and 77% of men reporting no clinical symptoms.1 However, approximately one-third of asymptomatic carriers will experience symptoms within 6 months of infection acquisition. This latency in appearance of clinical symptoms certainly contributes to the high transmission rate of T vaginalis.
Infected men may experience purulent urethritis, dysuria, and postcoital pruritus. Common clinical symptoms in women include abnormal vaginal discharge that may be malodorous, purulent, thin, frothy, and yellow-green, as well as symptoms of dyspareunia and vulvar irritation. Punctate hemorrhages in the cervix (colpitis macularis) and vaginal walls (macular vaginitis) give the characteristic “strawberry appearance,” but these findings are seen in only 2% of affected women.7
Complications in ObGyn patients
Although T vaginalis once was regarded as more of an annoyance than a public health issue, awareness of the infection’s ramifications has increased in recent years. Because of these complications, treatment of both symptomatic and asymptomatic patients is clearly indicated.
Complications of trichomonal infection in men include balanoposthitis, epididymitis, prostatitis, urethritis, and infertility.7 In women, complications include infections of the adnexa, endometrium, and vestibular glands, as well as cervical neoplasia and increased co-infection rates with other STIs, such as bacterial vaginosis, chlamydia infection, gonorrhea, syphilis, and herpes simplex virus type 2.1
Infection in pregnancy. Adverse outcomes in pregnant women with T vaginalis infections at mid-gestation include low birth weight, preterm premature rupture of membranes, preterm delivery, and postpartum endometritis.8 A disproportionately larger share of the low birth weight rate associated with T vaginalis infections occurs in black women compared with white and Hispanic women.8 Perinatal transmission to newborns can cause fever; respiratory difficulties; urinary tract infections; nasal discharge; and, in female infants, vaginal discharge.9,10
Co-infection concerns. The increased rate of co-infection with human immunodeficiency virus type 1 (HIV-1) and T vaginalis is a major concern.11 One study found a higher concentration of HIV-1 in semen samples from men with T vaginalis and symptomatic urethritis.12 Further, T vaginalis was found in 17.4% of women with HIV screened at a public clinic in California, with almost 38% of black women affected.13 Trichomoniasis can increase the risk of HIV-1 acquisition by 1.52-fold (95% confidence interval, 1.04- to 2.24-fold), pointing toward a potential amplifying effect of T vaginalis on HIV transmission rates.14 This association may be based at least in part on the organism’s ability to cause microulcerations in the genital and urinary tract epithelium, thus creating pathways for other microorganisms to enter the vascular system.
Making the diagnosis
The nonspecific symptoms of T vaginalis create a wide differential to consider. Vaginal discharge may be due to bacterial vaginosis, vulvovaginal candidiasis, physiologic discharge, atrophy, and nonspecific inflammation. The presence of malodorous and discolored discharge increases the likelihood of bacterial vaginosis or T vaginalis infection. Pruritus often is associated with candidiasis co-infection.
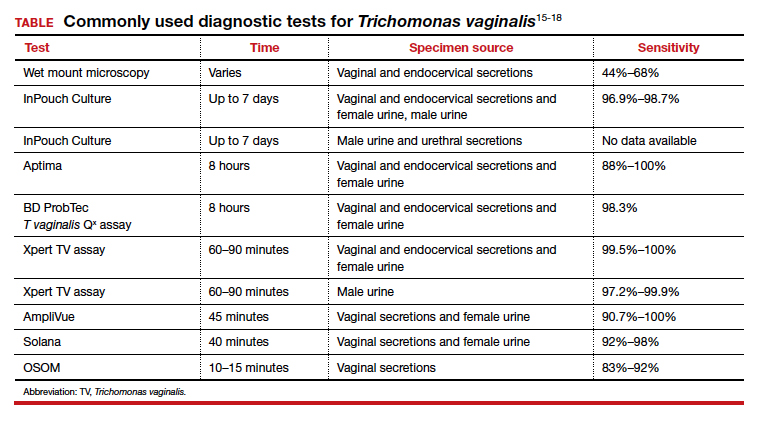
The diagnosis of trichomoniasis can be confirmed in the outpatient office with the use of saline microscopy, an inexpensive test that is based on observation of motile trichomonads in a wet mount of vaginal fluid. The sensitivity of the wet mount ranges from 44% to 68% compared with culture. Culture, traditionally using Diamond’s medium, has a sensitivity of 81% to 94% and was long the gold standard; however, culture has been replaced largely by molecular and antigen testing.
Three US Food and Drug Administration (FDA)-approved NAATs for T vaginalis currently are on the market; all can detect co-infection with gonorrhea and chlamydia from the same specimen. These tests include the Aptima T vaginalis rRNA target assay (Hologic, Bedford, Massachusetts) and the BD ProbTec T vaginalis Qx (TVQ) amplified DNA assay (BD Diagnostics, Baltimore, Maryland), both of which require up to 8 hours to yield results. The Xpert T vaginalis (TV) assay (Cepheid, Sunnyvale, California) is the first NAAT that is FDA approved for use with male urine (in addition to female urine), and it yields results in 60 to 90 minutes. Sensitivity for these NAAT assays ranges from 88% to 100%.15
Point-of-care testing is preferred for rapid diagnosis and for helping the clinician provide same-visit treatment for STIs. The Solana trichomonas assay (Quidel, San Diego, California) detects T vaginalis DNA and can yield results within 40 minutes, but it requires specialized equipment for running the samples. The AmpliVue trichomonas assay (Quidel, San Diego, California) is similar to the Solana assay but it is contained within a small handheld cartridge that does not require additional equipment. Sensitivities are 92% to 98% for Solona and 90.7% to 100% for AmpliVue. The OSOM trichomonas rapid test (Sekisui, Framingham, Massachusetts) uses antigen-detection immunochromatography to provide results in 10 to 15 minutes, with 83% to 92% sensitivity and 99% specificity for vaginal specimens.15,16
Continue to: The TABLE provides a summary...
The TABLE provides a summary of the clinical performance of the various tests for T vaginalis. 15-18
Treatment options
The 5-nitroimidazole agents, which include metronidazole and tinidazole, are the preferred agents for the treatment of trichomoniasis.
Dosing regimen. While a single oral dose of metronidazole 2 g has long been the mainstay of treatment for T vaginalis, this regimen recently has been questioned, at least in women, due to the high posttreatment positive rate of T vaginalis, which ranges from 5% to 37%.19,20 These cases may be due to reinfection by untreated sexual partners. They also may result from treatment failure, however, specifically inadequate treatment time.21 Overall, patients treated with single-dose metronidazole are 1.87 times more likely to experience treatment failure compared with those treated with a multidose regimen.19 Since many cases of T vaginalis infection are associated with bacterial vaginosis co-infection, recommending metronidazole 500 mg twice daily for 7 days is beneficial because this course provides optimal treatment for both infections.
Treatment during pregnancy. In the minds of some investigators, treatment of T vaginalis in asymptomatic pregnant women is problematic. One study demonstrated a similar to slightly increased risk of preterm delivery for metronidazole-treated patients compared with a placebo-treated group.22 Limitations of the study included atypical treatment dosing (2 doses of metronidazole 2 g given 48 hours apart at 16 to 23 weeks’ gestation and repeated at 24 to 29 weeks’ gestation) and a latency between the last dose of metronidazole and preterm delivery.22
We believe that all pregnant women, symptomatic or asymptomatic, should be treated because of the sexually transmitted nature of the infection and the probability that most asymptomatic carriers ultimately become symptomatic.
Cost of treatment. Generic oral metronidazole is very inexpensive. The approximate retail price for 14 metronidazole 500-mg tablets is $15.69 (www.goodrx.com). By contrast, a single-dose course of tinidazole (four 500-mg tablets) costs approximately $45. Accordingly, we reserve tinidazole for patients who have experienced a treatment failure with metronidazole or who cannot tolerate metronidazole.
Drug‒alcohol interaction. With both metronidazole and tinidazole, patients must abstain from alcohol during treatment and for 72 hours after completing therapy because these drugs have a disulfiram-like reaction with ethanol.
- Kissinger P. Epidemiology and treatment of trichomoniasis. Curr Infect Dis Rep. 2015;17:484.
- Midlej V, Benchimol M. Trichomonas vaginalis kills and eats—evidence for phagocytic activity as a cytopathic effect. Parasitology. 2010;137:65-76.
- Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97:548–562P.
- Patel EU, Gaydos CA, Packman ZR, et al. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin Infect Dis. 2018;67:211-217.
- Ginocchio CC, Chapin K, Smith JS, et al. Prevalence of Trichomonas vaginalis and coinfection with Chlamydia trachomatis and Neisseria gonorrhoeae in the United States as determined by the Aptima Trichomonas vaginalis nucleic acid amplification assay. J Clin Microbiol. 2012;50:2601-2608.
- Schwebke J, Merriweather A, Massingale S, et al. Screening for Trichomonas vaginalis in a large high-risk population: prevalence among men and women determined by nucleic acid amplification testing. Sex Transm Dis. 2018;45:e23-e24.
- Petrin D, Delgaty K, Bhatt R, et al. Clinical and microbiological aspects of Trichomonas vaginalis. Clin Microbiol Rev. 1998;11:300-317.
- Cotch MF, Pastorek JG II, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex Transm Dis. 1997;24:353-360.
- Smith LM, Wang M, Zangwill K, et al. Trichomonas vaginalis infection in a premature newborn. J Perinatol. 2002;22:502-503.
- Temesvári P, Kerekes A, Tege A, et al. Demonstration of Trichomonas vaginalis in tracheal aspirates in infants with early respiratory failure. J Matern Fetal Neonatal Med. 2002;11:347-349.
- Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89:426-433.
- Cohen MS, Hoffman IF, Royce RA, et al; AIDSCAP Malawi Research Group. Reduction of concentration of HIV-1 in semen after treatment of urethritis: implications for prevention of sexual transmission of HIV-1. Lancet. 1997;349:1868-1873.
- Sorvillo F, Kovacs A, Kerndt P, et al. Risk factors for trichomoniasis among women with human immunodeficiency virus (HIV) infection at a public clinic in Los Angeles County, California: implications for HIV prevention. Am J Trop Med Hyg. 1998;58:495-500.
- McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195:698-702.
- Van Gerwen OT, Muzny CA. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Res. 2019;8:F1000 Faculty Rev-1666.
- Gaydos CA, Klausner JD, Pai NP, et al. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex Transm Infect. 2017;93(S4):S31-S35.
- Rivers CA, Muzny CA, Schwebke JR. Diagnostic rates differ on the basis of the number of read days with the use of the InPouch culture system for Trichomonas vaginalis screening. J Clin Microbiol. 2013;51:3875-3876.
- Van Der Pol B, Williams JA, Taylor SN, et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper System. J Clin Microbiol. 2014;52:885-889.
- Howe K, Kissinger P. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44:29-34.
- Duff P. Should the length of treatment for trichomoniasis in women be reconsidered? OBG Manag. 2017;29(3):48-49.
- Krashin JW, Koumans EH, Bradshaw-Sydnor AC, et al. Trichomonas vaginalis prevalence, incidence, risk factors and antibiotic-resistance in an adolescent population. Sex Transm Dis. 2010;37:440-444.
- Klebanoff MA, Carey JC, Hauth JC, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487-493.
CASE Woman with malodorous vaginal discharge
A 26-year-old nulligravid woman with 2 current sexual partners requests evaluation because she has a yellow-green frothy vaginal discharge that is slightly malodorous. One of her sexual partners has noted a similar discharge from his urethra. On physical examination, the clinician notes that the patient’s discharge emanates from the vaginal mucosa, and the exocervix has multiple punctate hemorrhages. Considerations in this case include:
- What is the most likely diagnosis?
- How should this patient be evaluated and treated?
- Should the patient’s sexual partners be treated?
This clinical scenario is most consistent with a trichomonas infection, although other conditions, including bacterial vaginosis, gonorrhea, and chlamydia infection, must be considered in the differential diagnosis.
In this article, we examine the microbiology, epidemiology, clinical manifestations, and diagnosis and treatment of this common sexually transmitted infection (STI).
The causative microbe
Trichomonas vaginalis is a free-living flagellated protozoan that accounts for almost half of all nonviral STIs globally. It has a predilection for the mucosal epithelium of the genitourinary tract, including the vagina and urethra. Humans are the only known host for T vaginalis. The infection is transmitted through sexual intercourse, and the organism reproduces through binary fission in the lower genital tract of women and in the urethra and prostate of men.
This anaerobic trophozoite has 4 flagella anteriorly and 1 flagellum that projects posteriorly, with an undulating membrane that gives its characteristic motile appearance on saline microscopy.1
T vaginalis infection causes major mechanical stress on epithelial cells, which results in disruption of the plasma cell membrane and, ultimately, cell death. The necrotic cell fragments are then phagocytosed by trichomonads, thus accelerating the infection.2
Groups at risk
Trichomonal infections are not reportable to public health authorities, which makes assessing the true prevalence of infection difficult.
The World Health Organization estimated the incidence of infection to be more than 156 million cases globally in 2016, with a prevalence of 110.4 million people at any one time.3
The 2013-2014 National Health and Nutrition Examination Survey tested 4,057 men and women aged 18 to 59 years for T vaginalis and found a prevalence of 0.5% among men and 1.8% among women.4 The prevalence increased with age. There was a disproportionate burden of trichomonas infections in the non-Hispanic black population, with 4.2% of black men and 8.9% of black women affected.4
Targeted screening of urogenital samples for T vaginalis in a population of US women undergoing Chlamydia trachomatis/Neisseria gonorrhoeae screening demonstrated prevalence rates of 8.7%, 6.7%, and 1.7% for T vaginalis, C trachomatis, and N gonorrhoeae, respectively.5
Differences in prevalence estimates may be due to differences in the varying sensitivity of each testing modality and patient populations. In one study, nucleic acid amplification testing (NAAT) for T vaginalis detected rates as high as 11.3% in women and 6.1% in men undergoing evaluations at STI clinics.6
Continue to: Clinical manifestations of infection...
Clinical manifestations of infection
Most cases of T vaginalis remain in an asymptomatic carrier state, with up to 85% of women and 77% of men reporting no clinical symptoms.1 However, approximately one-third of asymptomatic carriers will experience symptoms within 6 months of infection acquisition. This latency in appearance of clinical symptoms certainly contributes to the high transmission rate of T vaginalis.
Infected men may experience purulent urethritis, dysuria, and postcoital pruritus. Common clinical symptoms in women include abnormal vaginal discharge that may be malodorous, purulent, thin, frothy, and yellow-green, as well as symptoms of dyspareunia and vulvar irritation. Punctate hemorrhages in the cervix (colpitis macularis) and vaginal walls (macular vaginitis) give the characteristic “strawberry appearance,” but these findings are seen in only 2% of affected women.7
Complications in ObGyn patients
Although T vaginalis once was regarded as more of an annoyance than a public health issue, awareness of the infection’s ramifications has increased in recent years. Because of these complications, treatment of both symptomatic and asymptomatic patients is clearly indicated.
Complications of trichomonal infection in men include balanoposthitis, epididymitis, prostatitis, urethritis, and infertility.7 In women, complications include infections of the adnexa, endometrium, and vestibular glands, as well as cervical neoplasia and increased co-infection rates with other STIs, such as bacterial vaginosis, chlamydia infection, gonorrhea, syphilis, and herpes simplex virus type 2.1
Infection in pregnancy. Adverse outcomes in pregnant women with T vaginalis infections at mid-gestation include low birth weight, preterm premature rupture of membranes, preterm delivery, and postpartum endometritis.8 A disproportionately larger share of the low birth weight rate associated with T vaginalis infections occurs in black women compared with white and Hispanic women.8 Perinatal transmission to newborns can cause fever; respiratory difficulties; urinary tract infections; nasal discharge; and, in female infants, vaginal discharge.9,10
Co-infection concerns. The increased rate of co-infection with human immunodeficiency virus type 1 (HIV-1) and T vaginalis is a major concern.11 One study found a higher concentration of HIV-1 in semen samples from men with T vaginalis and symptomatic urethritis.12 Further, T vaginalis was found in 17.4% of women with HIV screened at a public clinic in California, with almost 38% of black women affected.13 Trichomoniasis can increase the risk of HIV-1 acquisition by 1.52-fold (95% confidence interval, 1.04- to 2.24-fold), pointing toward a potential amplifying effect of T vaginalis on HIV transmission rates.14 This association may be based at least in part on the organism’s ability to cause microulcerations in the genital and urinary tract epithelium, thus creating pathways for other microorganisms to enter the vascular system.
Making the diagnosis
The nonspecific symptoms of T vaginalis create a wide differential to consider. Vaginal discharge may be due to bacterial vaginosis, vulvovaginal candidiasis, physiologic discharge, atrophy, and nonspecific inflammation. The presence of malodorous and discolored discharge increases the likelihood of bacterial vaginosis or T vaginalis infection. Pruritus often is associated with candidiasis co-infection.
The diagnosis of trichomoniasis can be confirmed in the outpatient office with the use of saline microscopy, an inexpensive test that is based on observation of motile trichomonads in a wet mount of vaginal fluid. The sensitivity of the wet mount ranges from 44% to 68% compared with culture. Culture, traditionally using Diamond’s medium, has a sensitivity of 81% to 94% and was long the gold standard; however, culture has been replaced largely by molecular and antigen testing.
Three US Food and Drug Administration (FDA)-approved NAATs for T vaginalis currently are on the market; all can detect co-infection with gonorrhea and chlamydia from the same specimen. These tests include the Aptima T vaginalis rRNA target assay (Hologic, Bedford, Massachusetts) and the BD ProbTec T vaginalis Qx (TVQ) amplified DNA assay (BD Diagnostics, Baltimore, Maryland), both of which require up to 8 hours to yield results. The Xpert T vaginalis (TV) assay (Cepheid, Sunnyvale, California) is the first NAAT that is FDA approved for use with male urine (in addition to female urine), and it yields results in 60 to 90 minutes. Sensitivity for these NAAT assays ranges from 88% to 100%.15
Point-of-care testing is preferred for rapid diagnosis and for helping the clinician provide same-visit treatment for STIs. The Solana trichomonas assay (Quidel, San Diego, California) detects T vaginalis DNA and can yield results within 40 minutes, but it requires specialized equipment for running the samples. The AmpliVue trichomonas assay (Quidel, San Diego, California) is similar to the Solana assay but it is contained within a small handheld cartridge that does not require additional equipment. Sensitivities are 92% to 98% for Solona and 90.7% to 100% for AmpliVue. The OSOM trichomonas rapid test (Sekisui, Framingham, Massachusetts) uses antigen-detection immunochromatography to provide results in 10 to 15 minutes, with 83% to 92% sensitivity and 99% specificity for vaginal specimens.15,16
Continue to: The TABLE provides a summary...
The TABLE provides a summary of the clinical performance of the various tests for T vaginalis. 15-18
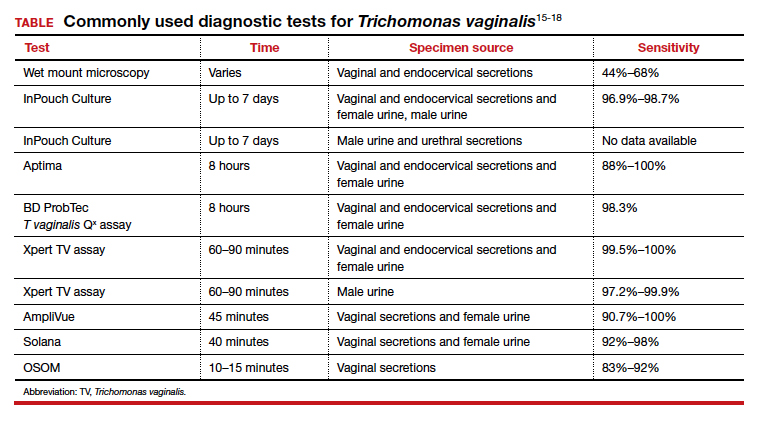
Treatment options
The 5-nitroimidazole agents, which include metronidazole and tinidazole, are the preferred agents for the treatment of trichomoniasis.
Dosing regimen. While a single oral dose of metronidazole 2 g has long been the mainstay of treatment for T vaginalis, this regimen recently has been questioned, at least in women, due to the high posttreatment positive rate of T vaginalis, which ranges from 5% to 37%.19,20 These cases may be due to reinfection by untreated sexual partners. They also may result from treatment failure, however, specifically inadequate treatment time.21 Overall, patients treated with single-dose metronidazole are 1.87 times more likely to experience treatment failure compared with those treated with a multidose regimen.19 Since many cases of T vaginalis infection are associated with bacterial vaginosis co-infection, recommending metronidazole 500 mg twice daily for 7 days is beneficial because this course provides optimal treatment for both infections.
Treatment during pregnancy. In the minds of some investigators, treatment of T vaginalis in asymptomatic pregnant women is problematic. One study demonstrated a similar to slightly increased risk of preterm delivery for metronidazole-treated patients compared with a placebo-treated group.22 Limitations of the study included atypical treatment dosing (2 doses of metronidazole 2 g given 48 hours apart at 16 to 23 weeks’ gestation and repeated at 24 to 29 weeks’ gestation) and a latency between the last dose of metronidazole and preterm delivery.22
We believe that all pregnant women, symptomatic or asymptomatic, should be treated because of the sexually transmitted nature of the infection and the probability that most asymptomatic carriers ultimately become symptomatic.
Cost of treatment. Generic oral metronidazole is very inexpensive. The approximate retail price for 14 metronidazole 500-mg tablets is $15.69 (www.goodrx.com). By contrast, a single-dose course of tinidazole (four 500-mg tablets) costs approximately $45. Accordingly, we reserve tinidazole for patients who have experienced a treatment failure with metronidazole or who cannot tolerate metronidazole.
Drug‒alcohol interaction. With both metronidazole and tinidazole, patients must abstain from alcohol during treatment and for 72 hours after completing therapy because these drugs have a disulfiram-like reaction with ethanol.
CASE Woman with malodorous vaginal discharge
A 26-year-old nulligravid woman with 2 current sexual partners requests evaluation because she has a yellow-green frothy vaginal discharge that is slightly malodorous. One of her sexual partners has noted a similar discharge from his urethra. On physical examination, the clinician notes that the patient’s discharge emanates from the vaginal mucosa, and the exocervix has multiple punctate hemorrhages. Considerations in this case include:
- What is the most likely diagnosis?
- How should this patient be evaluated and treated?
- Should the patient’s sexual partners be treated?
This clinical scenario is most consistent with a trichomonas infection, although other conditions, including bacterial vaginosis, gonorrhea, and chlamydia infection, must be considered in the differential diagnosis.
In this article, we examine the microbiology, epidemiology, clinical manifestations, and diagnosis and treatment of this common sexually transmitted infection (STI).
The causative microbe
Trichomonas vaginalis is a free-living flagellated protozoan that accounts for almost half of all nonviral STIs globally. It has a predilection for the mucosal epithelium of the genitourinary tract, including the vagina and urethra. Humans are the only known host for T vaginalis. The infection is transmitted through sexual intercourse, and the organism reproduces through binary fission in the lower genital tract of women and in the urethra and prostate of men.
This anaerobic trophozoite has 4 flagella anteriorly and 1 flagellum that projects posteriorly, with an undulating membrane that gives its characteristic motile appearance on saline microscopy.1
T vaginalis infection causes major mechanical stress on epithelial cells, which results in disruption of the plasma cell membrane and, ultimately, cell death. The necrotic cell fragments are then phagocytosed by trichomonads, thus accelerating the infection.2
Groups at risk
Trichomonal infections are not reportable to public health authorities, which makes assessing the true prevalence of infection difficult.
The World Health Organization estimated the incidence of infection to be more than 156 million cases globally in 2016, with a prevalence of 110.4 million people at any one time.3
The 2013-2014 National Health and Nutrition Examination Survey tested 4,057 men and women aged 18 to 59 years for T vaginalis and found a prevalence of 0.5% among men and 1.8% among women.4 The prevalence increased with age. There was a disproportionate burden of trichomonas infections in the non-Hispanic black population, with 4.2% of black men and 8.9% of black women affected.4
Targeted screening of urogenital samples for T vaginalis in a population of US women undergoing Chlamydia trachomatis/Neisseria gonorrhoeae screening demonstrated prevalence rates of 8.7%, 6.7%, and 1.7% for T vaginalis, C trachomatis, and N gonorrhoeae, respectively.5
Differences in prevalence estimates may be due to differences in the varying sensitivity of each testing modality and patient populations. In one study, nucleic acid amplification testing (NAAT) for T vaginalis detected rates as high as 11.3% in women and 6.1% in men undergoing evaluations at STI clinics.6
Continue to: Clinical manifestations of infection...
Clinical manifestations of infection
Most cases of T vaginalis remain in an asymptomatic carrier state, with up to 85% of women and 77% of men reporting no clinical symptoms.1 However, approximately one-third of asymptomatic carriers will experience symptoms within 6 months of infection acquisition. This latency in appearance of clinical symptoms certainly contributes to the high transmission rate of T vaginalis.
Infected men may experience purulent urethritis, dysuria, and postcoital pruritus. Common clinical symptoms in women include abnormal vaginal discharge that may be malodorous, purulent, thin, frothy, and yellow-green, as well as symptoms of dyspareunia and vulvar irritation. Punctate hemorrhages in the cervix (colpitis macularis) and vaginal walls (macular vaginitis) give the characteristic “strawberry appearance,” but these findings are seen in only 2% of affected women.7
Complications in ObGyn patients
Although T vaginalis once was regarded as more of an annoyance than a public health issue, awareness of the infection’s ramifications has increased in recent years. Because of these complications, treatment of both symptomatic and asymptomatic patients is clearly indicated.
Complications of trichomonal infection in men include balanoposthitis, epididymitis, prostatitis, urethritis, and infertility.7 In women, complications include infections of the adnexa, endometrium, and vestibular glands, as well as cervical neoplasia and increased co-infection rates with other STIs, such as bacterial vaginosis, chlamydia infection, gonorrhea, syphilis, and herpes simplex virus type 2.1
Infection in pregnancy. Adverse outcomes in pregnant women with T vaginalis infections at mid-gestation include low birth weight, preterm premature rupture of membranes, preterm delivery, and postpartum endometritis.8 A disproportionately larger share of the low birth weight rate associated with T vaginalis infections occurs in black women compared with white and Hispanic women.8 Perinatal transmission to newborns can cause fever; respiratory difficulties; urinary tract infections; nasal discharge; and, in female infants, vaginal discharge.9,10
Co-infection concerns. The increased rate of co-infection with human immunodeficiency virus type 1 (HIV-1) and T vaginalis is a major concern.11 One study found a higher concentration of HIV-1 in semen samples from men with T vaginalis and symptomatic urethritis.12 Further, T vaginalis was found in 17.4% of women with HIV screened at a public clinic in California, with almost 38% of black women affected.13 Trichomoniasis can increase the risk of HIV-1 acquisition by 1.52-fold (95% confidence interval, 1.04- to 2.24-fold), pointing toward a potential amplifying effect of T vaginalis on HIV transmission rates.14 This association may be based at least in part on the organism’s ability to cause microulcerations in the genital and urinary tract epithelium, thus creating pathways for other microorganisms to enter the vascular system.
Making the diagnosis
The nonspecific symptoms of T vaginalis create a wide differential to consider. Vaginal discharge may be due to bacterial vaginosis, vulvovaginal candidiasis, physiologic discharge, atrophy, and nonspecific inflammation. The presence of malodorous and discolored discharge increases the likelihood of bacterial vaginosis or T vaginalis infection. Pruritus often is associated with candidiasis co-infection.
The diagnosis of trichomoniasis can be confirmed in the outpatient office with the use of saline microscopy, an inexpensive test that is based on observation of motile trichomonads in a wet mount of vaginal fluid. The sensitivity of the wet mount ranges from 44% to 68% compared with culture. Culture, traditionally using Diamond’s medium, has a sensitivity of 81% to 94% and was long the gold standard; however, culture has been replaced largely by molecular and antigen testing.
Three US Food and Drug Administration (FDA)-approved NAATs for T vaginalis currently are on the market; all can detect co-infection with gonorrhea and chlamydia from the same specimen. These tests include the Aptima T vaginalis rRNA target assay (Hologic, Bedford, Massachusetts) and the BD ProbTec T vaginalis Qx (TVQ) amplified DNA assay (BD Diagnostics, Baltimore, Maryland), both of which require up to 8 hours to yield results. The Xpert T vaginalis (TV) assay (Cepheid, Sunnyvale, California) is the first NAAT that is FDA approved for use with male urine (in addition to female urine), and it yields results in 60 to 90 minutes. Sensitivity for these NAAT assays ranges from 88% to 100%.15
Point-of-care testing is preferred for rapid diagnosis and for helping the clinician provide same-visit treatment for STIs. The Solana trichomonas assay (Quidel, San Diego, California) detects T vaginalis DNA and can yield results within 40 minutes, but it requires specialized equipment for running the samples. The AmpliVue trichomonas assay (Quidel, San Diego, California) is similar to the Solana assay but it is contained within a small handheld cartridge that does not require additional equipment. Sensitivities are 92% to 98% for Solona and 90.7% to 100% for AmpliVue. The OSOM trichomonas rapid test (Sekisui, Framingham, Massachusetts) uses antigen-detection immunochromatography to provide results in 10 to 15 minutes, with 83% to 92% sensitivity and 99% specificity for vaginal specimens.15,16
Continue to: The TABLE provides a summary...
The TABLE provides a summary of the clinical performance of the various tests for T vaginalis. 15-18
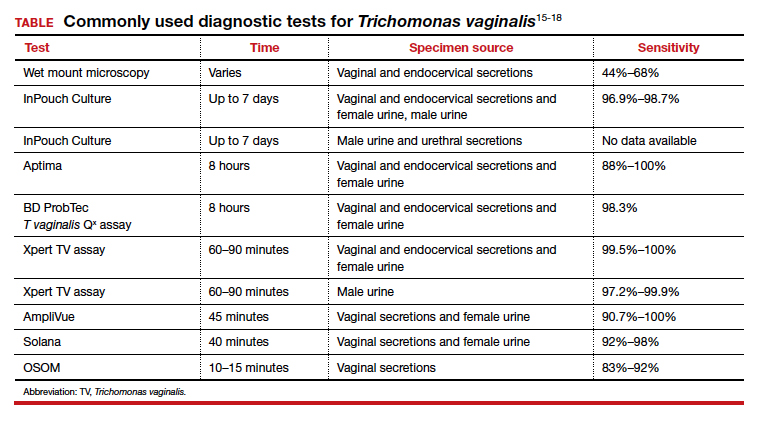
Treatment options
The 5-nitroimidazole agents, which include metronidazole and tinidazole, are the preferred agents for the treatment of trichomoniasis.
Dosing regimen. While a single oral dose of metronidazole 2 g has long been the mainstay of treatment for T vaginalis, this regimen recently has been questioned, at least in women, due to the high posttreatment positive rate of T vaginalis, which ranges from 5% to 37%.19,20 These cases may be due to reinfection by untreated sexual partners. They also may result from treatment failure, however, specifically inadequate treatment time.21 Overall, patients treated with single-dose metronidazole are 1.87 times more likely to experience treatment failure compared with those treated with a multidose regimen.19 Since many cases of T vaginalis infection are associated with bacterial vaginosis co-infection, recommending metronidazole 500 mg twice daily for 7 days is beneficial because this course provides optimal treatment for both infections.
Treatment during pregnancy. In the minds of some investigators, treatment of T vaginalis in asymptomatic pregnant women is problematic. One study demonstrated a similar to slightly increased risk of preterm delivery for metronidazole-treated patients compared with a placebo-treated group.22 Limitations of the study included atypical treatment dosing (2 doses of metronidazole 2 g given 48 hours apart at 16 to 23 weeks’ gestation and repeated at 24 to 29 weeks’ gestation) and a latency between the last dose of metronidazole and preterm delivery.22
We believe that all pregnant women, symptomatic or asymptomatic, should be treated because of the sexually transmitted nature of the infection and the probability that most asymptomatic carriers ultimately become symptomatic.
Cost of treatment. Generic oral metronidazole is very inexpensive. The approximate retail price for 14 metronidazole 500-mg tablets is $15.69 (www.goodrx.com). By contrast, a single-dose course of tinidazole (four 500-mg tablets) costs approximately $45. Accordingly, we reserve tinidazole for patients who have experienced a treatment failure with metronidazole or who cannot tolerate metronidazole.
Drug‒alcohol interaction. With both metronidazole and tinidazole, patients must abstain from alcohol during treatment and for 72 hours after completing therapy because these drugs have a disulfiram-like reaction with ethanol.
- Kissinger P. Epidemiology and treatment of trichomoniasis. Curr Infect Dis Rep. 2015;17:484.
- Midlej V, Benchimol M. Trichomonas vaginalis kills and eats—evidence for phagocytic activity as a cytopathic effect. Parasitology. 2010;137:65-76.
- Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97:548–562P.
- Patel EU, Gaydos CA, Packman ZR, et al. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin Infect Dis. 2018;67:211-217.
- Ginocchio CC, Chapin K, Smith JS, et al. Prevalence of Trichomonas vaginalis and coinfection with Chlamydia trachomatis and Neisseria gonorrhoeae in the United States as determined by the Aptima Trichomonas vaginalis nucleic acid amplification assay. J Clin Microbiol. 2012;50:2601-2608.
- Schwebke J, Merriweather A, Massingale S, et al. Screening for Trichomonas vaginalis in a large high-risk population: prevalence among men and women determined by nucleic acid amplification testing. Sex Transm Dis. 2018;45:e23-e24.
- Petrin D, Delgaty K, Bhatt R, et al. Clinical and microbiological aspects of Trichomonas vaginalis. Clin Microbiol Rev. 1998;11:300-317.
- Cotch MF, Pastorek JG II, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex Transm Dis. 1997;24:353-360.
- Smith LM, Wang M, Zangwill K, et al. Trichomonas vaginalis infection in a premature newborn. J Perinatol. 2002;22:502-503.
- Temesvári P, Kerekes A, Tege A, et al. Demonstration of Trichomonas vaginalis in tracheal aspirates in infants with early respiratory failure. J Matern Fetal Neonatal Med. 2002;11:347-349.
- Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89:426-433.
- Cohen MS, Hoffman IF, Royce RA, et al; AIDSCAP Malawi Research Group. Reduction of concentration of HIV-1 in semen after treatment of urethritis: implications for prevention of sexual transmission of HIV-1. Lancet. 1997;349:1868-1873.
- Sorvillo F, Kovacs A, Kerndt P, et al. Risk factors for trichomoniasis among women with human immunodeficiency virus (HIV) infection at a public clinic in Los Angeles County, California: implications for HIV prevention. Am J Trop Med Hyg. 1998;58:495-500.
- McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195:698-702.
- Van Gerwen OT, Muzny CA. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Res. 2019;8:F1000 Faculty Rev-1666.
- Gaydos CA, Klausner JD, Pai NP, et al. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex Transm Infect. 2017;93(S4):S31-S35.
- Rivers CA, Muzny CA, Schwebke JR. Diagnostic rates differ on the basis of the number of read days with the use of the InPouch culture system for Trichomonas vaginalis screening. J Clin Microbiol. 2013;51:3875-3876.
- Van Der Pol B, Williams JA, Taylor SN, et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper System. J Clin Microbiol. 2014;52:885-889.
- Howe K, Kissinger P. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44:29-34.
- Duff P. Should the length of treatment for trichomoniasis in women be reconsidered? OBG Manag. 2017;29(3):48-49.
- Krashin JW, Koumans EH, Bradshaw-Sydnor AC, et al. Trichomonas vaginalis prevalence, incidence, risk factors and antibiotic-resistance in an adolescent population. Sex Transm Dis. 2010;37:440-444.
- Klebanoff MA, Carey JC, Hauth JC, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487-493.
- Kissinger P. Epidemiology and treatment of trichomoniasis. Curr Infect Dis Rep. 2015;17:484.
- Midlej V, Benchimol M. Trichomonas vaginalis kills and eats—evidence for phagocytic activity as a cytopathic effect. Parasitology. 2010;137:65-76.
- Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97:548–562P.
- Patel EU, Gaydos CA, Packman ZR, et al. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin Infect Dis. 2018;67:211-217.
- Ginocchio CC, Chapin K, Smith JS, et al. Prevalence of Trichomonas vaginalis and coinfection with Chlamydia trachomatis and Neisseria gonorrhoeae in the United States as determined by the Aptima Trichomonas vaginalis nucleic acid amplification assay. J Clin Microbiol. 2012;50:2601-2608.
- Schwebke J, Merriweather A, Massingale S, et al. Screening for Trichomonas vaginalis in a large high-risk population: prevalence among men and women determined by nucleic acid amplification testing. Sex Transm Dis. 2018;45:e23-e24.
- Petrin D, Delgaty K, Bhatt R, et al. Clinical and microbiological aspects of Trichomonas vaginalis. Clin Microbiol Rev. 1998;11:300-317.
- Cotch MF, Pastorek JG II, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex Transm Dis. 1997;24:353-360.
- Smith LM, Wang M, Zangwill K, et al. Trichomonas vaginalis infection in a premature newborn. J Perinatol. 2002;22:502-503.
- Temesvári P, Kerekes A, Tege A, et al. Demonstration of Trichomonas vaginalis in tracheal aspirates in infants with early respiratory failure. J Matern Fetal Neonatal Med. 2002;11:347-349.
- Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89:426-433.
- Cohen MS, Hoffman IF, Royce RA, et al; AIDSCAP Malawi Research Group. Reduction of concentration of HIV-1 in semen after treatment of urethritis: implications for prevention of sexual transmission of HIV-1. Lancet. 1997;349:1868-1873.
- Sorvillo F, Kovacs A, Kerndt P, et al. Risk factors for trichomoniasis among women with human immunodeficiency virus (HIV) infection at a public clinic in Los Angeles County, California: implications for HIV prevention. Am J Trop Med Hyg. 1998;58:495-500.
- McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195:698-702.
- Van Gerwen OT, Muzny CA. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Res. 2019;8:F1000 Faculty Rev-1666.
- Gaydos CA, Klausner JD, Pai NP, et al. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex Transm Infect. 2017;93(S4):S31-S35.
- Rivers CA, Muzny CA, Schwebke JR. Diagnostic rates differ on the basis of the number of read days with the use of the InPouch culture system for Trichomonas vaginalis screening. J Clin Microbiol. 2013;51:3875-3876.
- Van Der Pol B, Williams JA, Taylor SN, et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper System. J Clin Microbiol. 2014;52:885-889.
- Howe K, Kissinger P. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44:29-34.
- Duff P. Should the length of treatment for trichomoniasis in women be reconsidered? OBG Manag. 2017;29(3):48-49.
- Krashin JW, Koumans EH, Bradshaw-Sydnor AC, et al. Trichomonas vaginalis prevalence, incidence, risk factors and antibiotic-resistance in an adolescent population. Sex Transm Dis. 2010;37:440-444.
- Klebanoff MA, Carey JC, Hauth JC, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487-493.
Gastrointestinal symptoms affected one in four patients hospitalized with COVID-19
Gastrointestinal symptoms affected 26% of hospital employees hospitalized with presumptive COVID-19 infection, according to the results of a study from Wuhan, China.
Among nonmedical personnel in the study (median age, 62 years), 63% of those with GI symptoms were female (P = .03), wrote Zili Zhou of Huazhong University of Science and Technology, Wuhan, China, and associates. they noted. However, “most patients were still hospitalized at the time of [manuscript] submission, [which made it] difficult to further assess the correlation between GI symptoms and clinical outcomes,” they wrote in Gastroenterology.
Reverse transcriptase polymerase chain reaction has detected COVID-19 in patients’ stool, and COVID-19’s primary receptor for cellular entry, the angiotensin converting enzyme 2 (ACE2) receptor, “is highly expressed not only in lung AT2 cells but also in absorptive enterocytes in the ileum and colon,” the investigators wrote. They compared laboratory and clinical findings among 254 adults with and without GI symptoms who were admitted to Wuhan’s main hospital with presumptive COVID-19 pneumonia between December 20, 2019, and February 9, 2020. All patients were employed by the hospital.
Gastrointestinal symptoms affected 26% of patients and most commonly included diarrhea (18%), nausea (8%), vomiting (6%), and abdominal pain (2%), the researchers reported. Arrhythmias and shock were rare, affecting less than 0.5% of patients. A total of 16 patients (6%) died.
The 161 nonmedical staff in the study were older and, therefore, were evaluated separately from medical staff (respective medians, 36 and 62 years; interquartile ranges, 31-41 years and 49-69 years). Among nonmedical staff, GI symptoms correlated with significantly lower hemoglobin levels (117 g/L [range, 106-127] vs. 133 g/L [range, 114-141], P = .03), and significantly higher levels of C-reactive protein (7.3 mg [range, 2.9-6.6] vs. 3.8 mg (1.8-5.8), P = .021) and alanine aminotransferase (64.1 U/L [range, 51.2-64.4] vs. 46.6 U/L [range, 31.9-61.2]; P = .049). Gastrointestinal symptoms also correlated significantly with fatigue, sore throat, and dizziness. Although the nonmedical cohort included five more males than females, females made up nearly two-thirds (63%) of individuals with GI symptoms (P = .03).
Although 25% of medical staff in the study had GI symptoms, GI symptoms did not correlate with other symptoms or with laboratory findings. This might be because “most of the infected medical staff were younger nurses without comorbidities,” the investigators wrote. “In addition, there [was] less delay from the onset of symptoms to hospital admission.”
For the overall cohort, the most prevalent symptoms were fever (84%), fatigue (52%), productive cough (42%), dry cough (42%), and myalgia (34%). Although these symptoms are typical of COVID-19 infection, most patients were not tested for the virus, “which will inevitably lead to several patients without [COVID-19 pneumonia] being included,” the investigators noted.
The National Nature Science Foundation of China provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Zhou Z et al. Gastroenterology. 2020 Mar 18. doi: 10.1053/j.gastro.2020.03.020.
Gastrointestinal symptoms affected 26% of hospital employees hospitalized with presumptive COVID-19 infection, according to the results of a study from Wuhan, China.
Among nonmedical personnel in the study (median age, 62 years), 63% of those with GI symptoms were female (P = .03), wrote Zili Zhou of Huazhong University of Science and Technology, Wuhan, China, and associates. they noted. However, “most patients were still hospitalized at the time of [manuscript] submission, [which made it] difficult to further assess the correlation between GI symptoms and clinical outcomes,” they wrote in Gastroenterology.
Reverse transcriptase polymerase chain reaction has detected COVID-19 in patients’ stool, and COVID-19’s primary receptor for cellular entry, the angiotensin converting enzyme 2 (ACE2) receptor, “is highly expressed not only in lung AT2 cells but also in absorptive enterocytes in the ileum and colon,” the investigators wrote. They compared laboratory and clinical findings among 254 adults with and without GI symptoms who were admitted to Wuhan’s main hospital with presumptive COVID-19 pneumonia between December 20, 2019, and February 9, 2020. All patients were employed by the hospital.
Gastrointestinal symptoms affected 26% of patients and most commonly included diarrhea (18%), nausea (8%), vomiting (6%), and abdominal pain (2%), the researchers reported. Arrhythmias and shock were rare, affecting less than 0.5% of patients. A total of 16 patients (6%) died.
The 161 nonmedical staff in the study were older and, therefore, were evaluated separately from medical staff (respective medians, 36 and 62 years; interquartile ranges, 31-41 years and 49-69 years). Among nonmedical staff, GI symptoms correlated with significantly lower hemoglobin levels (117 g/L [range, 106-127] vs. 133 g/L [range, 114-141], P = .03), and significantly higher levels of C-reactive protein (7.3 mg [range, 2.9-6.6] vs. 3.8 mg (1.8-5.8), P = .021) and alanine aminotransferase (64.1 U/L [range, 51.2-64.4] vs. 46.6 U/L [range, 31.9-61.2]; P = .049). Gastrointestinal symptoms also correlated significantly with fatigue, sore throat, and dizziness. Although the nonmedical cohort included five more males than females, females made up nearly two-thirds (63%) of individuals with GI symptoms (P = .03).
Although 25% of medical staff in the study had GI symptoms, GI symptoms did not correlate with other symptoms or with laboratory findings. This might be because “most of the infected medical staff were younger nurses without comorbidities,” the investigators wrote. “In addition, there [was] less delay from the onset of symptoms to hospital admission.”
For the overall cohort, the most prevalent symptoms were fever (84%), fatigue (52%), productive cough (42%), dry cough (42%), and myalgia (34%). Although these symptoms are typical of COVID-19 infection, most patients were not tested for the virus, “which will inevitably lead to several patients without [COVID-19 pneumonia] being included,” the investigators noted.
The National Nature Science Foundation of China provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Zhou Z et al. Gastroenterology. 2020 Mar 18. doi: 10.1053/j.gastro.2020.03.020.
Gastrointestinal symptoms affected 26% of hospital employees hospitalized with presumptive COVID-19 infection, according to the results of a study from Wuhan, China.
Among nonmedical personnel in the study (median age, 62 years), 63% of those with GI symptoms were female (P = .03), wrote Zili Zhou of Huazhong University of Science and Technology, Wuhan, China, and associates. they noted. However, “most patients were still hospitalized at the time of [manuscript] submission, [which made it] difficult to further assess the correlation between GI symptoms and clinical outcomes,” they wrote in Gastroenterology.
Reverse transcriptase polymerase chain reaction has detected COVID-19 in patients’ stool, and COVID-19’s primary receptor for cellular entry, the angiotensin converting enzyme 2 (ACE2) receptor, “is highly expressed not only in lung AT2 cells but also in absorptive enterocytes in the ileum and colon,” the investigators wrote. They compared laboratory and clinical findings among 254 adults with and without GI symptoms who were admitted to Wuhan’s main hospital with presumptive COVID-19 pneumonia between December 20, 2019, and February 9, 2020. All patients were employed by the hospital.
Gastrointestinal symptoms affected 26% of patients and most commonly included diarrhea (18%), nausea (8%), vomiting (6%), and abdominal pain (2%), the researchers reported. Arrhythmias and shock were rare, affecting less than 0.5% of patients. A total of 16 patients (6%) died.
The 161 nonmedical staff in the study were older and, therefore, were evaluated separately from medical staff (respective medians, 36 and 62 years; interquartile ranges, 31-41 years and 49-69 years). Among nonmedical staff, GI symptoms correlated with significantly lower hemoglobin levels (117 g/L [range, 106-127] vs. 133 g/L [range, 114-141], P = .03), and significantly higher levels of C-reactive protein (7.3 mg [range, 2.9-6.6] vs. 3.8 mg (1.8-5.8), P = .021) and alanine aminotransferase (64.1 U/L [range, 51.2-64.4] vs. 46.6 U/L [range, 31.9-61.2]; P = .049). Gastrointestinal symptoms also correlated significantly with fatigue, sore throat, and dizziness. Although the nonmedical cohort included five more males than females, females made up nearly two-thirds (63%) of individuals with GI symptoms (P = .03).
Although 25% of medical staff in the study had GI symptoms, GI symptoms did not correlate with other symptoms or with laboratory findings. This might be because “most of the infected medical staff were younger nurses without comorbidities,” the investigators wrote. “In addition, there [was] less delay from the onset of symptoms to hospital admission.”
For the overall cohort, the most prevalent symptoms were fever (84%), fatigue (52%), productive cough (42%), dry cough (42%), and myalgia (34%). Although these symptoms are typical of COVID-19 infection, most patients were not tested for the virus, “which will inevitably lead to several patients without [COVID-19 pneumonia] being included,” the investigators noted.
The National Nature Science Foundation of China provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Zhou Z et al. Gastroenterology. 2020 Mar 18. doi: 10.1053/j.gastro.2020.03.020.
FROM GASTROENTEROLOGY
Experts recommend slow, steady approach to reopening laser and cosmetic surgery practices

“People talk about reinventing the wheel,” Jeffrey S. Dover, MD, codirector of SkinCare Physicians in Chestnut Hill, Mass., said during an hour-long webinar on May 5 sponsored by the American Society for Laser Medicine and Surgery. “In this case, we’re inventing the wheel; no one’s ever done this before – not in our lifetimes. The last pandemic was over 100 years ago, when there wasn’t aesthetic medicine.”
Dr. Dover joined a panel of four other experts from around the country to discuss how to reopen practices safely and effectively. Paul M. Friedman, MD, director of the Houston Cosmetic Dermatology & Laser Center, moderated the event.
In Florida, which reopened certain businesses on May 4, 2020, Jill S. Waibel, MD, plans to start at 25% capacity at Miami Dermatology and Laser Institute, and build from there. “We’re trying to take care of skin cancer patients first,” said Dr. Waibel, a dermatologist who owns the practice. “Then we’re going to start doing less aggressive cosmetic procedures like injectables, nonablative procedures. We’ll move into the more aggressive procedures as we ease back into it. We really want to see what’s going to happen 2-3 weeks down the line now that things are starting to open up.”
In Maryland, where state officials announced on May 6 that guidelines would be issued to allow for nonmedical procedures, Elizabeth L. Tanzi, MD, founder and director of Capital Laser & Skin Care in Chevy Chase, expects things to “look very different” once her practice reopens. “We are taking it very slowly,” she said. “Teledermatology for acne and other follow-ups is not something we did before, but it is certainly something that we’ll continue.”
The way she sees it, having the proper personal protective equipment is a key part of any reopening discussion. “I am not going near anyone’s face without an N95 mask that fits well, and without a face shield,” she said. “If you’re delegating these procedures to people that you don’t trust to be wearing the PPE correctly, then you shouldn’t be delegating them, because a key is the PPE. You have to assume that everyone has the virus at every time.”
In Ardmore, Pa., the Main Line Center for Laser Surgery remains closed because of current state regulations. When practice director Eric F. Bernstein, MD, gets the green light to reopen, patients will undergo a consultation by phone or videoconference and pay their bill before they set foot in the office. “We’re on the second floor, so patients can take a stairwell and avoid the elevator,” Dr. Bernstein said. “They’ll come in, not check in at the desk; go right to the room. There will be one treater and one assistant. If the patient doesn’t come in with a mask, we’ll supply one. It’s going to be a very different process. People are setting their hours longer because they’re going to be seeing fewer people. There will be no sitting in the waiting room.”
In the COVID-19 epicenter, Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, has been performing Mohs procedures and treating children with vascular malformations, but everything else is on hold. “Once the governor [Andrew Cuomo] lifts the stay-at-home restrictions, we’ll ease into things,” he said. “The issue of performing more invasive procedures – like ablative fractional resurfacing – is something that we are concerned about. I’m concerned about any laser that has environmental plume. For example, with our tattoo-removal procedures, I intend to treat every patient through a gel for the short term, and perhaps even for the long term. One can do that safely, and that eliminates the plume altogether.”
At the center, Dr. Geronemus added, “we do a fair amount of ablative fractional resurfacing and some fully ablative resurfacing. I intend to use large facial shields with these patients. We do use vacuum in each room as it stands right now, not only with electrosurgery, but we’ll be adding that to laser procedures as well. That will be helpful.”
In Chestnut Hill, Mass., Dr. Dover and his colleagues plan to practice what he termed “universal COVID precaution” by wearing a face mask, goggles, or a face shield, gloves, and protective clothing when necessary. “We are not going to do any ablative procedures, no procedures with plume, and we’re going to try and eliminate risk as much as we can,” he said. “We will have no waiting room; the patients will walk right to an exam room. They’ll be prescreened on the phone. The only thing they’ll have done when they first come in is to have their temperature taken, and they’ll be checked in and out with the doctor and the nurse in the room, and that’s it. There will be no other extraneous people to help to eliminate risk. We’re cutting our schedules down by 75% so that we can socially distance within our practice,” Dr. Dover said.
Dr. Dover served as lead author on “A path to resume aesthetic care: Executive summary of Project AesCert guidance supplement – practical considerations for aesthetic medicine professionals supporting clinic preparedness in response to the SARS-CoV-2 outbreak,” which was published online in Facial Plastic Surgery & Aesthetic Medicine (2002 May 5. doi: 10.1089/fpsam.2020.0239). His coauthors included a facial plastic surgeon and three infectious disease experts.
Dr. Dover said, “We took the advice of these experts in infectious diseases, who said, ‘we don’t know all the right answers [to resuming aesthetic care]. We can mitigate risk, but we cannot eliminate risk. You have to treat every patient in your office as if they’re COVID-19 positive. If you do that, you’ll have a safe office. It’ll be the safest place in your world, safer than a grocery store, where you have no idea who you’re standing beside.’ ”
“The problem with this virus, compared to, say, SARS-CoV-1, is that these patients are positive and shedding virus 2-3 days before they get a fever,” he added. “With SARS-CoV-1, they had a fever first and then they shed virus. What I learned was, treat everybody with universal precautions.” The document includes tips for communicating with patient about expectations for office visits, clinic schedule management, cleaning procedures, PPE, treatment room set-up, and employee health screening and training.
During the webinar, an ASLMS member posed a question to the panelists about their comfort level in performing mechanical microneedling and radiofrequency (RF) microneedling procedures as aesthetic practices begin to reopen. “Generally, there’s no plume with microneedling with or without RF,” Dr. Geronemus said. “Depending upon the procedure that you’re doing, some of the microneedling procedures are very bloody; that may carry a risk unto itself. Other procedures where you’re using a thermal component have less bleeding. I’m more inclined to proceed with an RF with microneedling procedure and less inclined to proceed with a bloody, more aggressive microneedling procedure.”
Dr. Waibel emphasized the importance of disinfecting the microneedling device between uses. “If you have disposable needle cartridges, I think it’s a lot safer than if you have to clean [them],” she said. “We know that COVID-19 can live up to 3 hours, at least in a lab scenario, so you don’t want to transmit it from patient to patient. If someone has COVID-19 on their nose, and you microneedle over it, and that’s not completely disinfected, you could spread it to the next patient. We have really amped up our cleaning in between rooms. We have a whole crew that cleans every surface with [disinfectant wipes] and 90% alcohol.”
With reported shortages of N95 in many health care settings, some panelists said that they plan to reuse masks until the supply chain improves. Dr. Dover said that one option is to “use a mask, label it, number it, drop it in into a paper bag or into a [sealed plastic food container] upside down without touching the front of it,” he said. “If it sits for a week and you see patients 5 days a week, that mask will be dried out and highly effective a week later. That’s what we’re going to do until there is a big supply of them.”
The pandemic has also thrown a monkey wrench into aesthetic and medical dermatology clinical research efforts. According to Dr. Dover, many aesthetic studies have been shut down, “and most companies are giving us little guidance,” he said. “As they figure things out, they ask us to do things over and over again. So, I hope that clinical research will improve because of COVID-19 in the long term, but in the short term, it’s been a bit of a nightmare.”
Dr. Geronemus added that, in order to fulfill criteria for most studies, clinicians are required to see patients in a certain number of days. “We’re out of protocol in many different studies, so we’re requesting that protocols be amended and that the FDA [Food and Drug Administration] and the sponsors will consider opportunities to make those changes,” he said. “We’ll do as much as we can virtually, but if you’re studying an acne scar, you really need to see the patient [in person].”
Strict social distancing measures are also disrupting agreements that dermatologists may have had with trainees and fellows before the pandemic hit. “We’ve had to send letters and e-mails to people who were planning visits and preceptorships,” Dr. Dover said. “Even with our fellows, we’re going to have to figure out a way to practice so as not to complicate the issue in the room. The more people in the room, the more risk there is for transmitting disease. It’s really an issue.”
Dr. Tanzi limits everyone in the room during procedures. “We’re screening patients beforehand and telling them no family members, unless there’s a disability; no kids, unless it’s a kid coming in for acne treatment and they have to bring their parent; no drivers – they can wait outside,” she said.
Another ASLMS member asked the panelists if they plan to incorporate an informed consent form for COVID-19 risk into their practices, similar to the one developed by the American Society of Plastic Surgeons. “That’s a tough one,” Dr. Waibel said. “Before patients enter our practice, we take their temperature and ask them several COVID-related symptoms and contact questions – which they validate as true.”
Dr. Geronemus said that he will consider the idea. “The downside is logistical,” he said. “Patients sign so many forms already; they’re complaining that it takes so long to get into see me, and my hand is tired from signing so many forms.’”
Dr. Dover said that he and his colleagues are planning to use a COVID-19 risk consent form. “I’d err on the side of yes rather than on the side of no, because you’re better off overdoing it than underdoing it,” he said. “This is not the time for shortcuts.”
dbrunk@mdedge.com

“People talk about reinventing the wheel,” Jeffrey S. Dover, MD, codirector of SkinCare Physicians in Chestnut Hill, Mass., said during an hour-long webinar on May 5 sponsored by the American Society for Laser Medicine and Surgery. “In this case, we’re inventing the wheel; no one’s ever done this before – not in our lifetimes. The last pandemic was over 100 years ago, when there wasn’t aesthetic medicine.”
Dr. Dover joined a panel of four other experts from around the country to discuss how to reopen practices safely and effectively. Paul M. Friedman, MD, director of the Houston Cosmetic Dermatology & Laser Center, moderated the event.
In Florida, which reopened certain businesses on May 4, 2020, Jill S. Waibel, MD, plans to start at 25% capacity at Miami Dermatology and Laser Institute, and build from there. “We’re trying to take care of skin cancer patients first,” said Dr. Waibel, a dermatologist who owns the practice. “Then we’re going to start doing less aggressive cosmetic procedures like injectables, nonablative procedures. We’ll move into the more aggressive procedures as we ease back into it. We really want to see what’s going to happen 2-3 weeks down the line now that things are starting to open up.”
In Maryland, where state officials announced on May 6 that guidelines would be issued to allow for nonmedical procedures, Elizabeth L. Tanzi, MD, founder and director of Capital Laser & Skin Care in Chevy Chase, expects things to “look very different” once her practice reopens. “We are taking it very slowly,” she said. “Teledermatology for acne and other follow-ups is not something we did before, but it is certainly something that we’ll continue.”
The way she sees it, having the proper personal protective equipment is a key part of any reopening discussion. “I am not going near anyone’s face without an N95 mask that fits well, and without a face shield,” she said. “If you’re delegating these procedures to people that you don’t trust to be wearing the PPE correctly, then you shouldn’t be delegating them, because a key is the PPE. You have to assume that everyone has the virus at every time.”
In Ardmore, Pa., the Main Line Center for Laser Surgery remains closed because of current state regulations. When practice director Eric F. Bernstein, MD, gets the green light to reopen, patients will undergo a consultation by phone or videoconference and pay their bill before they set foot in the office. “We’re on the second floor, so patients can take a stairwell and avoid the elevator,” Dr. Bernstein said. “They’ll come in, not check in at the desk; go right to the room. There will be one treater and one assistant. If the patient doesn’t come in with a mask, we’ll supply one. It’s going to be a very different process. People are setting their hours longer because they’re going to be seeing fewer people. There will be no sitting in the waiting room.”
In the COVID-19 epicenter, Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, has been performing Mohs procedures and treating children with vascular malformations, but everything else is on hold. “Once the governor [Andrew Cuomo] lifts the stay-at-home restrictions, we’ll ease into things,” he said. “The issue of performing more invasive procedures – like ablative fractional resurfacing – is something that we are concerned about. I’m concerned about any laser that has environmental plume. For example, with our tattoo-removal procedures, I intend to treat every patient through a gel for the short term, and perhaps even for the long term. One can do that safely, and that eliminates the plume altogether.”
At the center, Dr. Geronemus added, “we do a fair amount of ablative fractional resurfacing and some fully ablative resurfacing. I intend to use large facial shields with these patients. We do use vacuum in each room as it stands right now, not only with electrosurgery, but we’ll be adding that to laser procedures as well. That will be helpful.”
In Chestnut Hill, Mass., Dr. Dover and his colleagues plan to practice what he termed “universal COVID precaution” by wearing a face mask, goggles, or a face shield, gloves, and protective clothing when necessary. “We are not going to do any ablative procedures, no procedures with plume, and we’re going to try and eliminate risk as much as we can,” he said. “We will have no waiting room; the patients will walk right to an exam room. They’ll be prescreened on the phone. The only thing they’ll have done when they first come in is to have their temperature taken, and they’ll be checked in and out with the doctor and the nurse in the room, and that’s it. There will be no other extraneous people to help to eliminate risk. We’re cutting our schedules down by 75% so that we can socially distance within our practice,” Dr. Dover said.
Dr. Dover served as lead author on “A path to resume aesthetic care: Executive summary of Project AesCert guidance supplement – practical considerations for aesthetic medicine professionals supporting clinic preparedness in response to the SARS-CoV-2 outbreak,” which was published online in Facial Plastic Surgery & Aesthetic Medicine (2002 May 5. doi: 10.1089/fpsam.2020.0239). His coauthors included a facial plastic surgeon and three infectious disease experts.
Dr. Dover said, “We took the advice of these experts in infectious diseases, who said, ‘we don’t know all the right answers [to resuming aesthetic care]. We can mitigate risk, but we cannot eliminate risk. You have to treat every patient in your office as if they’re COVID-19 positive. If you do that, you’ll have a safe office. It’ll be the safest place in your world, safer than a grocery store, where you have no idea who you’re standing beside.’ ”
“The problem with this virus, compared to, say, SARS-CoV-1, is that these patients are positive and shedding virus 2-3 days before they get a fever,” he added. “With SARS-CoV-1, they had a fever first and then they shed virus. What I learned was, treat everybody with universal precautions.” The document includes tips for communicating with patient about expectations for office visits, clinic schedule management, cleaning procedures, PPE, treatment room set-up, and employee health screening and training.
During the webinar, an ASLMS member posed a question to the panelists about their comfort level in performing mechanical microneedling and radiofrequency (RF) microneedling procedures as aesthetic practices begin to reopen. “Generally, there’s no plume with microneedling with or without RF,” Dr. Geronemus said. “Depending upon the procedure that you’re doing, some of the microneedling procedures are very bloody; that may carry a risk unto itself. Other procedures where you’re using a thermal component have less bleeding. I’m more inclined to proceed with an RF with microneedling procedure and less inclined to proceed with a bloody, more aggressive microneedling procedure.”
Dr. Waibel emphasized the importance of disinfecting the microneedling device between uses. “If you have disposable needle cartridges, I think it’s a lot safer than if you have to clean [them],” she said. “We know that COVID-19 can live up to 3 hours, at least in a lab scenario, so you don’t want to transmit it from patient to patient. If someone has COVID-19 on their nose, and you microneedle over it, and that’s not completely disinfected, you could spread it to the next patient. We have really amped up our cleaning in between rooms. We have a whole crew that cleans every surface with [disinfectant wipes] and 90% alcohol.”
With reported shortages of N95 in many health care settings, some panelists said that they plan to reuse masks until the supply chain improves. Dr. Dover said that one option is to “use a mask, label it, number it, drop it in into a paper bag or into a [sealed plastic food container] upside down without touching the front of it,” he said. “If it sits for a week and you see patients 5 days a week, that mask will be dried out and highly effective a week later. That’s what we’re going to do until there is a big supply of them.”
The pandemic has also thrown a monkey wrench into aesthetic and medical dermatology clinical research efforts. According to Dr. Dover, many aesthetic studies have been shut down, “and most companies are giving us little guidance,” he said. “As they figure things out, they ask us to do things over and over again. So, I hope that clinical research will improve because of COVID-19 in the long term, but in the short term, it’s been a bit of a nightmare.”
Dr. Geronemus added that, in order to fulfill criteria for most studies, clinicians are required to see patients in a certain number of days. “We’re out of protocol in many different studies, so we’re requesting that protocols be amended and that the FDA [Food and Drug Administration] and the sponsors will consider opportunities to make those changes,” he said. “We’ll do as much as we can virtually, but if you’re studying an acne scar, you really need to see the patient [in person].”
Strict social distancing measures are also disrupting agreements that dermatologists may have had with trainees and fellows before the pandemic hit. “We’ve had to send letters and e-mails to people who were planning visits and preceptorships,” Dr. Dover said. “Even with our fellows, we’re going to have to figure out a way to practice so as not to complicate the issue in the room. The more people in the room, the more risk there is for transmitting disease. It’s really an issue.”
Dr. Tanzi limits everyone in the room during procedures. “We’re screening patients beforehand and telling them no family members, unless there’s a disability; no kids, unless it’s a kid coming in for acne treatment and they have to bring their parent; no drivers – they can wait outside,” she said.
Another ASLMS member asked the panelists if they plan to incorporate an informed consent form for COVID-19 risk into their practices, similar to the one developed by the American Society of Plastic Surgeons. “That’s a tough one,” Dr. Waibel said. “Before patients enter our practice, we take their temperature and ask them several COVID-related symptoms and contact questions – which they validate as true.”
Dr. Geronemus said that he will consider the idea. “The downside is logistical,” he said. “Patients sign so many forms already; they’re complaining that it takes so long to get into see me, and my hand is tired from signing so many forms.’”
Dr. Dover said that he and his colleagues are planning to use a COVID-19 risk consent form. “I’d err on the side of yes rather than on the side of no, because you’re better off overdoing it than underdoing it,” he said. “This is not the time for shortcuts.”
dbrunk@mdedge.com

“People talk about reinventing the wheel,” Jeffrey S. Dover, MD, codirector of SkinCare Physicians in Chestnut Hill, Mass., said during an hour-long webinar on May 5 sponsored by the American Society for Laser Medicine and Surgery. “In this case, we’re inventing the wheel; no one’s ever done this before – not in our lifetimes. The last pandemic was over 100 years ago, when there wasn’t aesthetic medicine.”
Dr. Dover joined a panel of four other experts from around the country to discuss how to reopen practices safely and effectively. Paul M. Friedman, MD, director of the Houston Cosmetic Dermatology & Laser Center, moderated the event.
In Florida, which reopened certain businesses on May 4, 2020, Jill S. Waibel, MD, plans to start at 25% capacity at Miami Dermatology and Laser Institute, and build from there. “We’re trying to take care of skin cancer patients first,” said Dr. Waibel, a dermatologist who owns the practice. “Then we’re going to start doing less aggressive cosmetic procedures like injectables, nonablative procedures. We’ll move into the more aggressive procedures as we ease back into it. We really want to see what’s going to happen 2-3 weeks down the line now that things are starting to open up.”
In Maryland, where state officials announced on May 6 that guidelines would be issued to allow for nonmedical procedures, Elizabeth L. Tanzi, MD, founder and director of Capital Laser & Skin Care in Chevy Chase, expects things to “look very different” once her practice reopens. “We are taking it very slowly,” she said. “Teledermatology for acne and other follow-ups is not something we did before, but it is certainly something that we’ll continue.”
The way she sees it, having the proper personal protective equipment is a key part of any reopening discussion. “I am not going near anyone’s face without an N95 mask that fits well, and without a face shield,” she said. “If you’re delegating these procedures to people that you don’t trust to be wearing the PPE correctly, then you shouldn’t be delegating them, because a key is the PPE. You have to assume that everyone has the virus at every time.”
In Ardmore, Pa., the Main Line Center for Laser Surgery remains closed because of current state regulations. When practice director Eric F. Bernstein, MD, gets the green light to reopen, patients will undergo a consultation by phone or videoconference and pay their bill before they set foot in the office. “We’re on the second floor, so patients can take a stairwell and avoid the elevator,” Dr. Bernstein said. “They’ll come in, not check in at the desk; go right to the room. There will be one treater and one assistant. If the patient doesn’t come in with a mask, we’ll supply one. It’s going to be a very different process. People are setting their hours longer because they’re going to be seeing fewer people. There will be no sitting in the waiting room.”
In the COVID-19 epicenter, Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, has been performing Mohs procedures and treating children with vascular malformations, but everything else is on hold. “Once the governor [Andrew Cuomo] lifts the stay-at-home restrictions, we’ll ease into things,” he said. “The issue of performing more invasive procedures – like ablative fractional resurfacing – is something that we are concerned about. I’m concerned about any laser that has environmental plume. For example, with our tattoo-removal procedures, I intend to treat every patient through a gel for the short term, and perhaps even for the long term. One can do that safely, and that eliminates the plume altogether.”
At the center, Dr. Geronemus added, “we do a fair amount of ablative fractional resurfacing and some fully ablative resurfacing. I intend to use large facial shields with these patients. We do use vacuum in each room as it stands right now, not only with electrosurgery, but we’ll be adding that to laser procedures as well. That will be helpful.”
In Chestnut Hill, Mass., Dr. Dover and his colleagues plan to practice what he termed “universal COVID precaution” by wearing a face mask, goggles, or a face shield, gloves, and protective clothing when necessary. “We are not going to do any ablative procedures, no procedures with plume, and we’re going to try and eliminate risk as much as we can,” he said. “We will have no waiting room; the patients will walk right to an exam room. They’ll be prescreened on the phone. The only thing they’ll have done when they first come in is to have their temperature taken, and they’ll be checked in and out with the doctor and the nurse in the room, and that’s it. There will be no other extraneous people to help to eliminate risk. We’re cutting our schedules down by 75% so that we can socially distance within our practice,” Dr. Dover said.
Dr. Dover served as lead author on “A path to resume aesthetic care: Executive summary of Project AesCert guidance supplement – practical considerations for aesthetic medicine professionals supporting clinic preparedness in response to the SARS-CoV-2 outbreak,” which was published online in Facial Plastic Surgery & Aesthetic Medicine (2002 May 5. doi: 10.1089/fpsam.2020.0239). His coauthors included a facial plastic surgeon and three infectious disease experts.
Dr. Dover said, “We took the advice of these experts in infectious diseases, who said, ‘we don’t know all the right answers [to resuming aesthetic care]. We can mitigate risk, but we cannot eliminate risk. You have to treat every patient in your office as if they’re COVID-19 positive. If you do that, you’ll have a safe office. It’ll be the safest place in your world, safer than a grocery store, where you have no idea who you’re standing beside.’ ”
“The problem with this virus, compared to, say, SARS-CoV-1, is that these patients are positive and shedding virus 2-3 days before they get a fever,” he added. “With SARS-CoV-1, they had a fever first and then they shed virus. What I learned was, treat everybody with universal precautions.” The document includes tips for communicating with patient about expectations for office visits, clinic schedule management, cleaning procedures, PPE, treatment room set-up, and employee health screening and training.
During the webinar, an ASLMS member posed a question to the panelists about their comfort level in performing mechanical microneedling and radiofrequency (RF) microneedling procedures as aesthetic practices begin to reopen. “Generally, there’s no plume with microneedling with or without RF,” Dr. Geronemus said. “Depending upon the procedure that you’re doing, some of the microneedling procedures are very bloody; that may carry a risk unto itself. Other procedures where you’re using a thermal component have less bleeding. I’m more inclined to proceed with an RF with microneedling procedure and less inclined to proceed with a bloody, more aggressive microneedling procedure.”
Dr. Waibel emphasized the importance of disinfecting the microneedling device between uses. “If you have disposable needle cartridges, I think it’s a lot safer than if you have to clean [them],” she said. “We know that COVID-19 can live up to 3 hours, at least in a lab scenario, so you don’t want to transmit it from patient to patient. If someone has COVID-19 on their nose, and you microneedle over it, and that’s not completely disinfected, you could spread it to the next patient. We have really amped up our cleaning in between rooms. We have a whole crew that cleans every surface with [disinfectant wipes] and 90% alcohol.”
With reported shortages of N95 in many health care settings, some panelists said that they plan to reuse masks until the supply chain improves. Dr. Dover said that one option is to “use a mask, label it, number it, drop it in into a paper bag or into a [sealed plastic food container] upside down without touching the front of it,” he said. “If it sits for a week and you see patients 5 days a week, that mask will be dried out and highly effective a week later. That’s what we’re going to do until there is a big supply of them.”
The pandemic has also thrown a monkey wrench into aesthetic and medical dermatology clinical research efforts. According to Dr. Dover, many aesthetic studies have been shut down, “and most companies are giving us little guidance,” he said. “As they figure things out, they ask us to do things over and over again. So, I hope that clinical research will improve because of COVID-19 in the long term, but in the short term, it’s been a bit of a nightmare.”
Dr. Geronemus added that, in order to fulfill criteria for most studies, clinicians are required to see patients in a certain number of days. “We’re out of protocol in many different studies, so we’re requesting that protocols be amended and that the FDA [Food and Drug Administration] and the sponsors will consider opportunities to make those changes,” he said. “We’ll do as much as we can virtually, but if you’re studying an acne scar, you really need to see the patient [in person].”
Strict social distancing measures are also disrupting agreements that dermatologists may have had with trainees and fellows before the pandemic hit. “We’ve had to send letters and e-mails to people who were planning visits and preceptorships,” Dr. Dover said. “Even with our fellows, we’re going to have to figure out a way to practice so as not to complicate the issue in the room. The more people in the room, the more risk there is for transmitting disease. It’s really an issue.”
Dr. Tanzi limits everyone in the room during procedures. “We’re screening patients beforehand and telling them no family members, unless there’s a disability; no kids, unless it’s a kid coming in for acne treatment and they have to bring their parent; no drivers – they can wait outside,” she said.
Another ASLMS member asked the panelists if they plan to incorporate an informed consent form for COVID-19 risk into their practices, similar to the one developed by the American Society of Plastic Surgeons. “That’s a tough one,” Dr. Waibel said. “Before patients enter our practice, we take their temperature and ask them several COVID-related symptoms and contact questions – which they validate as true.”
Dr. Geronemus said that he will consider the idea. “The downside is logistical,” he said. “Patients sign so many forms already; they’re complaining that it takes so long to get into see me, and my hand is tired from signing so many forms.’”
Dr. Dover said that he and his colleagues are planning to use a COVID-19 risk consent form. “I’d err on the side of yes rather than on the side of no, because you’re better off overdoing it than underdoing it,” he said. “This is not the time for shortcuts.”
dbrunk@mdedge.com
Incidental finding on brain MRI seen in 5% of older patients
New research shows that Knowing the expected prevalence of such incidental findings in the older general population is “extremely useful” for both researchers and clinicians, said study co-author Sarah Elisabeth Keuss, MBChB, clinical research associate, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK.
“In research, the knowledge helps to inform study protocols regarding how to manage incidental findings and enables study participants to be appropriately informed,” said Dr. Keuss. Greater awareness also helps clinicians make decisions about whether or not to scan a patient, she said, adding that imaging is increasingly available to them. It allows clinicians to counsel patients regarding the probability of an incidental finding and balance that risk against the potential benefits of having a test.
The research is being presented online as part of the American Academy of Neurology 2020 Science Highlights. The incidental findings also were published last year in BMJ Open.
The new findings are from the first wave of data collection for the Insight 46 study, a neuroimaging substudy of the MRC National Survey of Health and Development (NSHD) 1946 British birth cohort, a broadly representative sample of the population born in mainland Britain during 1946. The research uses detailed brain imaging, cognitive testing, and blood and other biomarkers to investigate genetic and life-course factors associated with Alzheimer’s disease and cerebrovascular disease.
The current study included 502 individuals, aged about 71 years at the time of the analysis, and 49% were women. Almost all (93.8%) participants underwent 1-day MRI scans. Some 4.5% of these participants had an incidental finding of brain abnormality as per a prespecified standardized protocol.
Suspected vascular malformations were present in 1.9%, and suspected intracranial mass lesions were present in 1.5%. The single most common vascular abnormality was a suspected cerebral aneurysm, which affected 1.1% of participants.
Suspected meningiomas were the most common intracranial lesion, affecting 0.6% of study participants.
Action plan
Participants and their primary care provider were informed of findings “that were deemed to be potentially serious, or life-threatening, or could have a major impact on quality of life,” said Dr. Keuss. Relevant experts “came up with a recommended clinical action plan to help the primary care provider decide what should be the next course of action with regard to investigation or referral to another specialist,” said Dr. Keuss.
The new results are important for clinical decision-making, said Dr. Keuss. “Clinicians should consider the possibility of detecting an incidental finding whenever they’re requesting a brain scan. They should balance that risk against the possible benefits of recommending a test.”
The prevalence of incidental findings on MRI reported in the literature varies because of different methods used to review scans. “However, comparing our study with similar studies, the prevalence of the key findings with regard to aneurysms and intracranial mass lesions are very similar,” said Dr. Keuss.
Dr. Keuss and colleagues do not recommend all elderly patients get a brain scan.
“We don’t know what the long-term consequences are of being informed you have an incidental finding of an abnormality; we don’t know if it improves their outcome, and it potentially could cause anxiety,” said Dr. Keuss.
Psychological impact
The researchers have not looked at the psychological impact of negative findings on study participants, but they could do so at a later date.
“It would be very important to look into that given the potential to cause anxiety,” said Dr. Keuss. “It’s important to find out the potential negative consequences to inform researchers in future about how best to manage these findings.”
From blood tests, the analysis found that more than a third (34.6%) of participants had at least one related abnormality. The most common of these were kidney impairment (about 9%), thyroid function abnormalities (between 4% and 5%), anemia (about 4%), and low vitamin B12 levels (about 3%).
However, few of these reached the prespecified threshold for urgent action, and Dr. Keuss noted these findings were not the focus of her AAN presentation.
A strength of the study was that participants were almost the exact same age.
Important issue
Commenting on the research, David S. Liebeskind, MD, professor of neurology and director, Neurovascular Imaging Research Core, University of California, Los Angeles, said it raises “a very interesting” and “important” public health issue.
“The question is whether we do things based around individual symptomatic status, or at a larger level in terms of public health, screening the larger population to figure out who is at risk for any particular disease or disorder.”
From the standpoint of imaging technologies like MRI that show details about brain structures, experts debate whether the population should be screened “before something occurs,” said Dr. Liebeskind. “Imaging has the capacity to tell us a tremendous amount; whether this implies we should therefore image everybody is a larger public health question.”
The issue is “fraught with a lot of difficulty and complexity” as treatment paradigms tend to be “built around symptomatic status,” he said. “When we sit in the office or with a patient at the bedside, we usually focus on that individual patient and not necessarily on the larger public.”
Dr. Liebeskind noted that the question of whether to put the emphasis on the individual patient or the public at large is also being discussed during the current COVID-19 pandemic.
He wasn’t surprised that the study uncovered incidental findings in almost 5% of the sample. “If you take an 80-year-old and study their brain, a good chunk, if not half or more, will have some abnormality,” he said.
Drs. Keuss and Liebeskind have reported no relevant financial relationships.
This article first appeared on Medscape.com.
New research shows that Knowing the expected prevalence of such incidental findings in the older general population is “extremely useful” for both researchers and clinicians, said study co-author Sarah Elisabeth Keuss, MBChB, clinical research associate, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK.
“In research, the knowledge helps to inform study protocols regarding how to manage incidental findings and enables study participants to be appropriately informed,” said Dr. Keuss. Greater awareness also helps clinicians make decisions about whether or not to scan a patient, she said, adding that imaging is increasingly available to them. It allows clinicians to counsel patients regarding the probability of an incidental finding and balance that risk against the potential benefits of having a test.
The research is being presented online as part of the American Academy of Neurology 2020 Science Highlights. The incidental findings also were published last year in BMJ Open.
The new findings are from the first wave of data collection for the Insight 46 study, a neuroimaging substudy of the MRC National Survey of Health and Development (NSHD) 1946 British birth cohort, a broadly representative sample of the population born in mainland Britain during 1946. The research uses detailed brain imaging, cognitive testing, and blood and other biomarkers to investigate genetic and life-course factors associated with Alzheimer’s disease and cerebrovascular disease.
The current study included 502 individuals, aged about 71 years at the time of the analysis, and 49% were women. Almost all (93.8%) participants underwent 1-day MRI scans. Some 4.5% of these participants had an incidental finding of brain abnormality as per a prespecified standardized protocol.
Suspected vascular malformations were present in 1.9%, and suspected intracranial mass lesions were present in 1.5%. The single most common vascular abnormality was a suspected cerebral aneurysm, which affected 1.1% of participants.
Suspected meningiomas were the most common intracranial lesion, affecting 0.6% of study participants.
Action plan
Participants and their primary care provider were informed of findings “that were deemed to be potentially serious, or life-threatening, or could have a major impact on quality of life,” said Dr. Keuss. Relevant experts “came up with a recommended clinical action plan to help the primary care provider decide what should be the next course of action with regard to investigation or referral to another specialist,” said Dr. Keuss.
The new results are important for clinical decision-making, said Dr. Keuss. “Clinicians should consider the possibility of detecting an incidental finding whenever they’re requesting a brain scan. They should balance that risk against the possible benefits of recommending a test.”
The prevalence of incidental findings on MRI reported in the literature varies because of different methods used to review scans. “However, comparing our study with similar studies, the prevalence of the key findings with regard to aneurysms and intracranial mass lesions are very similar,” said Dr. Keuss.
Dr. Keuss and colleagues do not recommend all elderly patients get a brain scan.
“We don’t know what the long-term consequences are of being informed you have an incidental finding of an abnormality; we don’t know if it improves their outcome, and it potentially could cause anxiety,” said Dr. Keuss.
Psychological impact
The researchers have not looked at the psychological impact of negative findings on study participants, but they could do so at a later date.
“It would be very important to look into that given the potential to cause anxiety,” said Dr. Keuss. “It’s important to find out the potential negative consequences to inform researchers in future about how best to manage these findings.”
From blood tests, the analysis found that more than a third (34.6%) of participants had at least one related abnormality. The most common of these were kidney impairment (about 9%), thyroid function abnormalities (between 4% and 5%), anemia (about 4%), and low vitamin B12 levels (about 3%).
However, few of these reached the prespecified threshold for urgent action, and Dr. Keuss noted these findings were not the focus of her AAN presentation.
A strength of the study was that participants were almost the exact same age.
Important issue
Commenting on the research, David S. Liebeskind, MD, professor of neurology and director, Neurovascular Imaging Research Core, University of California, Los Angeles, said it raises “a very interesting” and “important” public health issue.
“The question is whether we do things based around individual symptomatic status, or at a larger level in terms of public health, screening the larger population to figure out who is at risk for any particular disease or disorder.”
From the standpoint of imaging technologies like MRI that show details about brain structures, experts debate whether the population should be screened “before something occurs,” said Dr. Liebeskind. “Imaging has the capacity to tell us a tremendous amount; whether this implies we should therefore image everybody is a larger public health question.”
The issue is “fraught with a lot of difficulty and complexity” as treatment paradigms tend to be “built around symptomatic status,” he said. “When we sit in the office or with a patient at the bedside, we usually focus on that individual patient and not necessarily on the larger public.”
Dr. Liebeskind noted that the question of whether to put the emphasis on the individual patient or the public at large is also being discussed during the current COVID-19 pandemic.
He wasn’t surprised that the study uncovered incidental findings in almost 5% of the sample. “If you take an 80-year-old and study their brain, a good chunk, if not half or more, will have some abnormality,” he said.
Drs. Keuss and Liebeskind have reported no relevant financial relationships.
This article first appeared on Medscape.com.
New research shows that Knowing the expected prevalence of such incidental findings in the older general population is “extremely useful” for both researchers and clinicians, said study co-author Sarah Elisabeth Keuss, MBChB, clinical research associate, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK.
“In research, the knowledge helps to inform study protocols regarding how to manage incidental findings and enables study participants to be appropriately informed,” said Dr. Keuss. Greater awareness also helps clinicians make decisions about whether or not to scan a patient, she said, adding that imaging is increasingly available to them. It allows clinicians to counsel patients regarding the probability of an incidental finding and balance that risk against the potential benefits of having a test.
The research is being presented online as part of the American Academy of Neurology 2020 Science Highlights. The incidental findings also were published last year in BMJ Open.
The new findings are from the first wave of data collection for the Insight 46 study, a neuroimaging substudy of the MRC National Survey of Health and Development (NSHD) 1946 British birth cohort, a broadly representative sample of the population born in mainland Britain during 1946. The research uses detailed brain imaging, cognitive testing, and blood and other biomarkers to investigate genetic and life-course factors associated with Alzheimer’s disease and cerebrovascular disease.
The current study included 502 individuals, aged about 71 years at the time of the analysis, and 49% were women. Almost all (93.8%) participants underwent 1-day MRI scans. Some 4.5% of these participants had an incidental finding of brain abnormality as per a prespecified standardized protocol.
Suspected vascular malformations were present in 1.9%, and suspected intracranial mass lesions were present in 1.5%. The single most common vascular abnormality was a suspected cerebral aneurysm, which affected 1.1% of participants.
Suspected meningiomas were the most common intracranial lesion, affecting 0.6% of study participants.
Action plan
Participants and their primary care provider were informed of findings “that were deemed to be potentially serious, or life-threatening, or could have a major impact on quality of life,” said Dr. Keuss. Relevant experts “came up with a recommended clinical action plan to help the primary care provider decide what should be the next course of action with regard to investigation or referral to another specialist,” said Dr. Keuss.
The new results are important for clinical decision-making, said Dr. Keuss. “Clinicians should consider the possibility of detecting an incidental finding whenever they’re requesting a brain scan. They should balance that risk against the possible benefits of recommending a test.”
The prevalence of incidental findings on MRI reported in the literature varies because of different methods used to review scans. “However, comparing our study with similar studies, the prevalence of the key findings with regard to aneurysms and intracranial mass lesions are very similar,” said Dr. Keuss.
Dr. Keuss and colleagues do not recommend all elderly patients get a brain scan.
“We don’t know what the long-term consequences are of being informed you have an incidental finding of an abnormality; we don’t know if it improves their outcome, and it potentially could cause anxiety,” said Dr. Keuss.
Psychological impact
The researchers have not looked at the psychological impact of negative findings on study participants, but they could do so at a later date.
“It would be very important to look into that given the potential to cause anxiety,” said Dr. Keuss. “It’s important to find out the potential negative consequences to inform researchers in future about how best to manage these findings.”
From blood tests, the analysis found that more than a third (34.6%) of participants had at least one related abnormality. The most common of these were kidney impairment (about 9%), thyroid function abnormalities (between 4% and 5%), anemia (about 4%), and low vitamin B12 levels (about 3%).
However, few of these reached the prespecified threshold for urgent action, and Dr. Keuss noted these findings were not the focus of her AAN presentation.
A strength of the study was that participants were almost the exact same age.
Important issue
Commenting on the research, David S. Liebeskind, MD, professor of neurology and director, Neurovascular Imaging Research Core, University of California, Los Angeles, said it raises “a very interesting” and “important” public health issue.
“The question is whether we do things based around individual symptomatic status, or at a larger level in terms of public health, screening the larger population to figure out who is at risk for any particular disease or disorder.”
From the standpoint of imaging technologies like MRI that show details about brain structures, experts debate whether the population should be screened “before something occurs,” said Dr. Liebeskind. “Imaging has the capacity to tell us a tremendous amount; whether this implies we should therefore image everybody is a larger public health question.”
The issue is “fraught with a lot of difficulty and complexity” as treatment paradigms tend to be “built around symptomatic status,” he said. “When we sit in the office or with a patient at the bedside, we usually focus on that individual patient and not necessarily on the larger public.”
Dr. Liebeskind noted that the question of whether to put the emphasis on the individual patient or the public at large is also being discussed during the current COVID-19 pandemic.
He wasn’t surprised that the study uncovered incidental findings in almost 5% of the sample. “If you take an 80-year-old and study their brain, a good chunk, if not half or more, will have some abnormality,” he said.
Drs. Keuss and Liebeskind have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Pediatric OCD: A case for vigilance
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at pdnews@mdedge.com.
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at pdnews@mdedge.com.
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at pdnews@mdedge.com.
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
AGA Clinical Practice Update: Functional heartburn
Recognizing the presence of functional heartburn is vital to prevent unnecessary acid-suppressive therapy and invasive antireflux treatments, which are ineffective and “might even lead to harm,” cautions a new clinical practice update from the American Gastroenterological Association.
Proton pump inhibitors (PPIs) “have no therapeutic value in functional heartburn,” unless patients also have gastroesophageal reflux disease (GERD), Ronnie Fass, MD, of MetroHealth System in Cleveland, and coauthors wrote in Gastroenterology. If clinical work-up finds no clear evidence of GERD, “an attempt to discontinue PPI therapy is warranted,” they added. Likewise, antireflux surgery and endoscopic treatments for GERD “have no therapeutic benefit in functional heartburn and should not be recommended.” However, histamine2 receptor antagonists (H2RAs) “may have an independent benefit in functional heartburn from an esophageal pain modulatory effect.”
Heartburn consists of burning or discomfort that radiates retrosternally from the epigastrium. Patients may report reflux, regurgitation, chest pain or discomfort, fullness, water brash, belching, or a sour and bitter taste in the mouth. Functional heartburn is heartburn that persists after at least 3 months of maximal (double-dose) PPIs taken before meals. Confirming functional heartburn requires high-resolution manometry to rule out major esophageal motor disorders, esophageal endoscopy with biopsy to rule out structural abnormalities and mucosal disorders (e.g., erosive esophagitis, Barrett’s esophagus, and eosinophilic esophagitis), and either pH monitoring while off PPI therapy or pH-impedance monitoring on therapy if patients have proven GERD. According to the clinical practice update, pH studies should document physiological acid exposure in the distal esophagus that is unlinked to symptoms (i.e., both a negative symptom index and a negative symptom association probability).
Functional heartburn resembles GERD, but symptoms are unrelated to acid exposure. Balloon distension studies indicate that patients with functional heartburn experience both esophageal and rectal hypersensitivity. Anxiety and mood disorders also are highly prevalent, and patients “will likely not improve unless esophageal perception and underlying affective disorders are adequately managed,” Dr. Fass and coauthors emphasized.
In keeping with this approach, limited evidence from clinical trials supports the first-line use of neuromodulator therapies, including selective serotonin reuptake inhibitors, tricyclic antidepressants, the serotonin 4 receptor antagonist tegaserod, and H2RAs (e.g., cimetidine, famotidine, nizatidine). The only SSRI studied thus far in functional heartburn is fluoxetine. In a placebo-controlled trial of patients with normal endoscopy and heartburn that had not responded to once-daily PPI therapy, 6 weeks of fluoxetine (20 mg daily) significantly outperformed double-dose omeprazole (P < .001) for the primary endpoint of heartburn-free days. “This superior therapeutic effect of fluoxetine was seen only in the subset of patients with a normal pH test,” the experts noted.
In another placebo-controlled trial, the neuromodulator tegaserod (a serotonin 5-HT4 receptor partial agonist) significantly improved tolerance of esophageal pressure during balloon distension and significantly decreased heartburn, regurgitation, and associated distress among patients with functional heartburn. Melatonin, which “also has a pain modulatory effect in the gastrointestinal tract,” significantly improved symptom-related quality of life, compared with nortriptyline and placebo in a randomized, three-arm trial. The patients on melatonin received a 6-mg dose at bedtime for 3 months.
Acupuncture and hypnotherapy also have shown benefit in small studies of functional heartburn patients and may be appropriate as monotherapy or adjunctive treatment, according to the clinical practice update. In a small randomized study, 10 acupuncture sessions delivered over 4 weeks significantly improved daytime and nighttime heartburn and acid regurgitation scores, compared with double-dose PPI. “Mean general health score was significantly improved only in those receiving acupuncture,” the experts noted. Hypnotherapy, the only psychological intervention to have been studied in functional heartburn, was associated with significant improvements in symptoms, visceral anxiety, and quality of life in an uncontrolled study of nine patients.
Although the overall prevalence of functional heartburn is unclear, it has been detected in 21%-39% of PPI-refractory patients evaluated with pH-impedance monitoring, Dr. Fass and associates wrote. Because functional heartburn and GERD can co-occur, some patients with functional heartburn may develop long-term complications of GERD, such as Barrett’s esophagus or peptic stricture. However, the experts noted, “this is anticipated to be rare, and the vast majority of patients with functional heartburn will have compromised quality of life, rather than organic complications over time.
Dr. Fass reported receiving consulting, research, and speaking fees from Ironwood, Takeda, and Salix, among other pharmaceutical companies; Dr. Zerbib received consulting fees from Reckitt Benckiser; and Dr. Gyawali received teaching and consulting fees from Medtronic, Diversatek, and Ironwood.
SOURCE: Fass R et al. Gastroenterology. 2020 Feb 1. doi: 10.1053/j.gastro.2020.01.034.
This story was updated on 6/11/2020.
Recognizing the presence of functional heartburn is vital to prevent unnecessary acid-suppressive therapy and invasive antireflux treatments, which are ineffective and “might even lead to harm,” cautions a new clinical practice update from the American Gastroenterological Association.
Proton pump inhibitors (PPIs) “have no therapeutic value in functional heartburn,” unless patients also have gastroesophageal reflux disease (GERD), Ronnie Fass, MD, of MetroHealth System in Cleveland, and coauthors wrote in Gastroenterology. If clinical work-up finds no clear evidence of GERD, “an attempt to discontinue PPI therapy is warranted,” they added. Likewise, antireflux surgery and endoscopic treatments for GERD “have no therapeutic benefit in functional heartburn and should not be recommended.” However, histamine2 receptor antagonists (H2RAs) “may have an independent benefit in functional heartburn from an esophageal pain modulatory effect.”
Heartburn consists of burning or discomfort that radiates retrosternally from the epigastrium. Patients may report reflux, regurgitation, chest pain or discomfort, fullness, water brash, belching, or a sour and bitter taste in the mouth. Functional heartburn is heartburn that persists after at least 3 months of maximal (double-dose) PPIs taken before meals. Confirming functional heartburn requires high-resolution manometry to rule out major esophageal motor disorders, esophageal endoscopy with biopsy to rule out structural abnormalities and mucosal disorders (e.g., erosive esophagitis, Barrett’s esophagus, and eosinophilic esophagitis), and either pH monitoring while off PPI therapy or pH-impedance monitoring on therapy if patients have proven GERD. According to the clinical practice update, pH studies should document physiological acid exposure in the distal esophagus that is unlinked to symptoms (i.e., both a negative symptom index and a negative symptom association probability).
Functional heartburn resembles GERD, but symptoms are unrelated to acid exposure. Balloon distension studies indicate that patients with functional heartburn experience both esophageal and rectal hypersensitivity. Anxiety and mood disorders also are highly prevalent, and patients “will likely not improve unless esophageal perception and underlying affective disorders are adequately managed,” Dr. Fass and coauthors emphasized.
In keeping with this approach, limited evidence from clinical trials supports the first-line use of neuromodulator therapies, including selective serotonin reuptake inhibitors, tricyclic antidepressants, the serotonin 4 receptor antagonist tegaserod, and H2RAs (e.g., cimetidine, famotidine, nizatidine). The only SSRI studied thus far in functional heartburn is fluoxetine. In a placebo-controlled trial of patients with normal endoscopy and heartburn that had not responded to once-daily PPI therapy, 6 weeks of fluoxetine (20 mg daily) significantly outperformed double-dose omeprazole (P < .001) for the primary endpoint of heartburn-free days. “This superior therapeutic effect of fluoxetine was seen only in the subset of patients with a normal pH test,” the experts noted.
In another placebo-controlled trial, the neuromodulator tegaserod (a serotonin 5-HT4 receptor partial agonist) significantly improved tolerance of esophageal pressure during balloon distension and significantly decreased heartburn, regurgitation, and associated distress among patients with functional heartburn. Melatonin, which “also has a pain modulatory effect in the gastrointestinal tract,” significantly improved symptom-related quality of life, compared with nortriptyline and placebo in a randomized, three-arm trial. The patients on melatonin received a 6-mg dose at bedtime for 3 months.
Acupuncture and hypnotherapy also have shown benefit in small studies of functional heartburn patients and may be appropriate as monotherapy or adjunctive treatment, according to the clinical practice update. In a small randomized study, 10 acupuncture sessions delivered over 4 weeks significantly improved daytime and nighttime heartburn and acid regurgitation scores, compared with double-dose PPI. “Mean general health score was significantly improved only in those receiving acupuncture,” the experts noted. Hypnotherapy, the only psychological intervention to have been studied in functional heartburn, was associated with significant improvements in symptoms, visceral anxiety, and quality of life in an uncontrolled study of nine patients.
Although the overall prevalence of functional heartburn is unclear, it has been detected in 21%-39% of PPI-refractory patients evaluated with pH-impedance monitoring, Dr. Fass and associates wrote. Because functional heartburn and GERD can co-occur, some patients with functional heartburn may develop long-term complications of GERD, such as Barrett’s esophagus or peptic stricture. However, the experts noted, “this is anticipated to be rare, and the vast majority of patients with functional heartburn will have compromised quality of life, rather than organic complications over time.
Dr. Fass reported receiving consulting, research, and speaking fees from Ironwood, Takeda, and Salix, among other pharmaceutical companies; Dr. Zerbib received consulting fees from Reckitt Benckiser; and Dr. Gyawali received teaching and consulting fees from Medtronic, Diversatek, and Ironwood.
SOURCE: Fass R et al. Gastroenterology. 2020 Feb 1. doi: 10.1053/j.gastro.2020.01.034.
This story was updated on 6/11/2020.
Recognizing the presence of functional heartburn is vital to prevent unnecessary acid-suppressive therapy and invasive antireflux treatments, which are ineffective and “might even lead to harm,” cautions a new clinical practice update from the American Gastroenterological Association.
Proton pump inhibitors (PPIs) “have no therapeutic value in functional heartburn,” unless patients also have gastroesophageal reflux disease (GERD), Ronnie Fass, MD, of MetroHealth System in Cleveland, and coauthors wrote in Gastroenterology. If clinical work-up finds no clear evidence of GERD, “an attempt to discontinue PPI therapy is warranted,” they added. Likewise, antireflux surgery and endoscopic treatments for GERD “have no therapeutic benefit in functional heartburn and should not be recommended.” However, histamine2 receptor antagonists (H2RAs) “may have an independent benefit in functional heartburn from an esophageal pain modulatory effect.”
Heartburn consists of burning or discomfort that radiates retrosternally from the epigastrium. Patients may report reflux, regurgitation, chest pain or discomfort, fullness, water brash, belching, or a sour and bitter taste in the mouth. Functional heartburn is heartburn that persists after at least 3 months of maximal (double-dose) PPIs taken before meals. Confirming functional heartburn requires high-resolution manometry to rule out major esophageal motor disorders, esophageal endoscopy with biopsy to rule out structural abnormalities and mucosal disorders (e.g., erosive esophagitis, Barrett’s esophagus, and eosinophilic esophagitis), and either pH monitoring while off PPI therapy or pH-impedance monitoring on therapy if patients have proven GERD. According to the clinical practice update, pH studies should document physiological acid exposure in the distal esophagus that is unlinked to symptoms (i.e., both a negative symptom index and a negative symptom association probability).
Functional heartburn resembles GERD, but symptoms are unrelated to acid exposure. Balloon distension studies indicate that patients with functional heartburn experience both esophageal and rectal hypersensitivity. Anxiety and mood disorders also are highly prevalent, and patients “will likely not improve unless esophageal perception and underlying affective disorders are adequately managed,” Dr. Fass and coauthors emphasized.
In keeping with this approach, limited evidence from clinical trials supports the first-line use of neuromodulator therapies, including selective serotonin reuptake inhibitors, tricyclic antidepressants, the serotonin 4 receptor antagonist tegaserod, and H2RAs (e.g., cimetidine, famotidine, nizatidine). The only SSRI studied thus far in functional heartburn is fluoxetine. In a placebo-controlled trial of patients with normal endoscopy and heartburn that had not responded to once-daily PPI therapy, 6 weeks of fluoxetine (20 mg daily) significantly outperformed double-dose omeprazole (P < .001) for the primary endpoint of heartburn-free days. “This superior therapeutic effect of fluoxetine was seen only in the subset of patients with a normal pH test,” the experts noted.
In another placebo-controlled trial, the neuromodulator tegaserod (a serotonin 5-HT4 receptor partial agonist) significantly improved tolerance of esophageal pressure during balloon distension and significantly decreased heartburn, regurgitation, and associated distress among patients with functional heartburn. Melatonin, which “also has a pain modulatory effect in the gastrointestinal tract,” significantly improved symptom-related quality of life, compared with nortriptyline and placebo in a randomized, three-arm trial. The patients on melatonin received a 6-mg dose at bedtime for 3 months.
Acupuncture and hypnotherapy also have shown benefit in small studies of functional heartburn patients and may be appropriate as monotherapy or adjunctive treatment, according to the clinical practice update. In a small randomized study, 10 acupuncture sessions delivered over 4 weeks significantly improved daytime and nighttime heartburn and acid regurgitation scores, compared with double-dose PPI. “Mean general health score was significantly improved only in those receiving acupuncture,” the experts noted. Hypnotherapy, the only psychological intervention to have been studied in functional heartburn, was associated with significant improvements in symptoms, visceral anxiety, and quality of life in an uncontrolled study of nine patients.
Although the overall prevalence of functional heartburn is unclear, it has been detected in 21%-39% of PPI-refractory patients evaluated with pH-impedance monitoring, Dr. Fass and associates wrote. Because functional heartburn and GERD can co-occur, some patients with functional heartburn may develop long-term complications of GERD, such as Barrett’s esophagus or peptic stricture. However, the experts noted, “this is anticipated to be rare, and the vast majority of patients with functional heartburn will have compromised quality of life, rather than organic complications over time.
Dr. Fass reported receiving consulting, research, and speaking fees from Ironwood, Takeda, and Salix, among other pharmaceutical companies; Dr. Zerbib received consulting fees from Reckitt Benckiser; and Dr. Gyawali received teaching and consulting fees from Medtronic, Diversatek, and Ironwood.
SOURCE: Fass R et al. Gastroenterology. 2020 Feb 1. doi: 10.1053/j.gastro.2020.01.034.
This story was updated on 6/11/2020.
FROM GASTROENTEROLOGY
New ‘atlas’ maps links between mental disorders, physical illnesses
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Endocrinologists adapt to telehealth, deferrals during COVID-19
James V. Hennessey, MD, has been working from home, like so many others, since the lockdowns went into effect. The director of clinical endocrinology at Beth Israel Deaconess Medical Center in Boston has felt surprisingly heartened by his experience.
“So far, these [video-based] discussions have been reassuring,” he said in an interview. “The images generating the referral have been available for review, and we’ve been able to reassure the patients that there are no danger signs in their histories.” Dr. Hennessey noted that for patients who agree to thyroid nodule consultations via video consult, the arrangement has allowed for the assessment of difficulty swallowing and other obvious difficulties.
While Dr. Hennessey has not yet encountered anything serious during his virtual consults, such as a rapidly growing anaplastic thyroid cancer, “it will only take some time before we hear of one, I’m sure,” he observed.
Surprisingly productive
During the COVID-19 pandemic, many physicians have been forced to innovate and turn aspects of their practices virtual. Use of telehealth services has increased by 50% in the United States since the start of the pandemic, according to research by Frost and Sullivan consultants. Three endocrinologists report that telehealth, although not always ideal, may provide more information than expected.
Recent recommendations say physicians should defer biopsies of asymptomatic thyroid nodules until the risk for COVID-19 has passed. As a result, some patients may experience increased anxiety because of such delays. But cases determined to require more urgent care should not be delayed, says the guidance.
Trevor E. Angell, MD, concurred that it’s possible to safely defer thyroid nodule assessment. “I would agree that with appropriate risk stratification by symptom assessment, ultrasound, and lab testing, thyroid nodules can be safely triaged for delayed evaluation,” said Dr. Angell, an assistant professor of clinical medicine and associate medical director of the thyroid center at the University of Southern California, in Los Angeles.
“I have found that patients with thyroid nodules that are not highly suspicious are reasonably reassured that the delay in obtaining FNA [fine needle aspiration] is very unlikely to have an impact on the ultimate outcome,” he said in an interview.
But he does have concerns that many of the investigations needed to make a decision about whether treatment can be deferred are also on hold.
“In many settings, including my own institution, nonurgent radiology studies are not being performed,” he noted. And “patients are reluctant to go to an ultrasound evaluation or a laboratory to perform testing” because of worries about COVID-19. “For possible thyroid nodules that have not yet been evaluated, this presents difficulty in getting the accurate ultrasound risk stratification and/or calcitonin testing that would help determine the need for immediate FNA biopsy or surgical consideration.”
And for patients in whom surgery has already been recommended, because of “indeterminate FNA cytology or suspicious molecular test result,” there is likely to be even more anxiety, Dr. Angell said.
“Most patients happy” with video visits
Victor J. Bernet, MD, American Thyroid Association president-elect, noted that, while his practice already had planned to start doing some video visits in April, the process was by necessity jump-started in March.
“Currently, about 90%-95% of our appointments are video visit or phone-call based,” he said in an interview. “Most patients seem to actually be happy with the video visit experience,” he said. “Some patients were very happy that they were given the opportunity to not have to come into the clinic in person at this point in time.”
Dr. Bernet agreed that video consults can be productive in identifying some important clinical information. “I have had at least a few patients with obvious goiter or nodule,” said Dr. Bernet, an associate professor and chair of the division of endocrinology at the Mayo Clinic in Jacksonville, Fla. “I also had a patient with hyperthyroidism from Graves disease and we were able to assess her for tremor over video.”
In the latter case, “we had the patient place a sheet of paper on the top of her hand while her arm was extended, which is the technique that can be used in person as well, and helps amplify the ability to detect if a fine tremor is present.”
“It was obvious that this patient had a tremor by video,” Dr. Bernet said.
In addition to tremor, video visits can be helpful in “looking for the presence of thyroid eye disease, enlarged thyroid, and possibly even skin changes.” Video may also be useful in evaluating respiratory effort and some cognitive behaviors, Dr. Bernet noted.
Starting to think about elective procedures again
As centers in the United States begin to reopen and permit elective procedures again, patients being considered for FNAs will likely be reintroduced according to the level of need, Dr. Hennessey noted. “Those with clear indications for FNA will be the first (to be scheduled),” while those who had very-low-risk findings, such as small nodules and cysts, “have already been deferred to 6- or 12-month follow-up ultrasounds, and decisions regarding FNAs will be made based on clinical course.”
Dr. Angell agrees that efforts to address the most urgent cases once centers reopen will be of the utmost importance. “To the greatest extent possible, providers should work together to coordinate the rescheduling of patients for FNA or surgery to avoid any further delay for those at most risk,” he said.Dr. Hennessey, Dr. Angell, and Dr. Bernet have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
James V. Hennessey, MD, has been working from home, like so many others, since the lockdowns went into effect. The director of clinical endocrinology at Beth Israel Deaconess Medical Center in Boston has felt surprisingly heartened by his experience.
“So far, these [video-based] discussions have been reassuring,” he said in an interview. “The images generating the referral have been available for review, and we’ve been able to reassure the patients that there are no danger signs in their histories.” Dr. Hennessey noted that for patients who agree to thyroid nodule consultations via video consult, the arrangement has allowed for the assessment of difficulty swallowing and other obvious difficulties.
While Dr. Hennessey has not yet encountered anything serious during his virtual consults, such as a rapidly growing anaplastic thyroid cancer, “it will only take some time before we hear of one, I’m sure,” he observed.
Surprisingly productive
During the COVID-19 pandemic, many physicians have been forced to innovate and turn aspects of their practices virtual. Use of telehealth services has increased by 50% in the United States since the start of the pandemic, according to research by Frost and Sullivan consultants. Three endocrinologists report that telehealth, although not always ideal, may provide more information than expected.
Recent recommendations say physicians should defer biopsies of asymptomatic thyroid nodules until the risk for COVID-19 has passed. As a result, some patients may experience increased anxiety because of such delays. But cases determined to require more urgent care should not be delayed, says the guidance.
Trevor E. Angell, MD, concurred that it’s possible to safely defer thyroid nodule assessment. “I would agree that with appropriate risk stratification by symptom assessment, ultrasound, and lab testing, thyroid nodules can be safely triaged for delayed evaluation,” said Dr. Angell, an assistant professor of clinical medicine and associate medical director of the thyroid center at the University of Southern California, in Los Angeles.
“I have found that patients with thyroid nodules that are not highly suspicious are reasonably reassured that the delay in obtaining FNA [fine needle aspiration] is very unlikely to have an impact on the ultimate outcome,” he said in an interview.
But he does have concerns that many of the investigations needed to make a decision about whether treatment can be deferred are also on hold.
“In many settings, including my own institution, nonurgent radiology studies are not being performed,” he noted. And “patients are reluctant to go to an ultrasound evaluation or a laboratory to perform testing” because of worries about COVID-19. “For possible thyroid nodules that have not yet been evaluated, this presents difficulty in getting the accurate ultrasound risk stratification and/or calcitonin testing that would help determine the need for immediate FNA biopsy or surgical consideration.”
And for patients in whom surgery has already been recommended, because of “indeterminate FNA cytology or suspicious molecular test result,” there is likely to be even more anxiety, Dr. Angell said.
“Most patients happy” with video visits
Victor J. Bernet, MD, American Thyroid Association president-elect, noted that, while his practice already had planned to start doing some video visits in April, the process was by necessity jump-started in March.
“Currently, about 90%-95% of our appointments are video visit or phone-call based,” he said in an interview. “Most patients seem to actually be happy with the video visit experience,” he said. “Some patients were very happy that they were given the opportunity to not have to come into the clinic in person at this point in time.”
Dr. Bernet agreed that video consults can be productive in identifying some important clinical information. “I have had at least a few patients with obvious goiter or nodule,” said Dr. Bernet, an associate professor and chair of the division of endocrinology at the Mayo Clinic in Jacksonville, Fla. “I also had a patient with hyperthyroidism from Graves disease and we were able to assess her for tremor over video.”
In the latter case, “we had the patient place a sheet of paper on the top of her hand while her arm was extended, which is the technique that can be used in person as well, and helps amplify the ability to detect if a fine tremor is present.”
“It was obvious that this patient had a tremor by video,” Dr. Bernet said.
In addition to tremor, video visits can be helpful in “looking for the presence of thyroid eye disease, enlarged thyroid, and possibly even skin changes.” Video may also be useful in evaluating respiratory effort and some cognitive behaviors, Dr. Bernet noted.
Starting to think about elective procedures again
As centers in the United States begin to reopen and permit elective procedures again, patients being considered for FNAs will likely be reintroduced according to the level of need, Dr. Hennessey noted. “Those with clear indications for FNA will be the first (to be scheduled),” while those who had very-low-risk findings, such as small nodules and cysts, “have already been deferred to 6- or 12-month follow-up ultrasounds, and decisions regarding FNAs will be made based on clinical course.”
Dr. Angell agrees that efforts to address the most urgent cases once centers reopen will be of the utmost importance. “To the greatest extent possible, providers should work together to coordinate the rescheduling of patients for FNA or surgery to avoid any further delay for those at most risk,” he said.Dr. Hennessey, Dr. Angell, and Dr. Bernet have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
James V. Hennessey, MD, has been working from home, like so many others, since the lockdowns went into effect. The director of clinical endocrinology at Beth Israel Deaconess Medical Center in Boston has felt surprisingly heartened by his experience.
“So far, these [video-based] discussions have been reassuring,” he said in an interview. “The images generating the referral have been available for review, and we’ve been able to reassure the patients that there are no danger signs in their histories.” Dr. Hennessey noted that for patients who agree to thyroid nodule consultations via video consult, the arrangement has allowed for the assessment of difficulty swallowing and other obvious difficulties.
While Dr. Hennessey has not yet encountered anything serious during his virtual consults, such as a rapidly growing anaplastic thyroid cancer, “it will only take some time before we hear of one, I’m sure,” he observed.
Surprisingly productive
During the COVID-19 pandemic, many physicians have been forced to innovate and turn aspects of their practices virtual. Use of telehealth services has increased by 50% in the United States since the start of the pandemic, according to research by Frost and Sullivan consultants. Three endocrinologists report that telehealth, although not always ideal, may provide more information than expected.
Recent recommendations say physicians should defer biopsies of asymptomatic thyroid nodules until the risk for COVID-19 has passed. As a result, some patients may experience increased anxiety because of such delays. But cases determined to require more urgent care should not be delayed, says the guidance.
Trevor E. Angell, MD, concurred that it’s possible to safely defer thyroid nodule assessment. “I would agree that with appropriate risk stratification by symptom assessment, ultrasound, and lab testing, thyroid nodules can be safely triaged for delayed evaluation,” said Dr. Angell, an assistant professor of clinical medicine and associate medical director of the thyroid center at the University of Southern California, in Los Angeles.
“I have found that patients with thyroid nodules that are not highly suspicious are reasonably reassured that the delay in obtaining FNA [fine needle aspiration] is very unlikely to have an impact on the ultimate outcome,” he said in an interview.
But he does have concerns that many of the investigations needed to make a decision about whether treatment can be deferred are also on hold.
“In many settings, including my own institution, nonurgent radiology studies are not being performed,” he noted. And “patients are reluctant to go to an ultrasound evaluation or a laboratory to perform testing” because of worries about COVID-19. “For possible thyroid nodules that have not yet been evaluated, this presents difficulty in getting the accurate ultrasound risk stratification and/or calcitonin testing that would help determine the need for immediate FNA biopsy or surgical consideration.”
And for patients in whom surgery has already been recommended, because of “indeterminate FNA cytology or suspicious molecular test result,” there is likely to be even more anxiety, Dr. Angell said.
“Most patients happy” with video visits
Victor J. Bernet, MD, American Thyroid Association president-elect, noted that, while his practice already had planned to start doing some video visits in April, the process was by necessity jump-started in March.
“Currently, about 90%-95% of our appointments are video visit or phone-call based,” he said in an interview. “Most patients seem to actually be happy with the video visit experience,” he said. “Some patients were very happy that they were given the opportunity to not have to come into the clinic in person at this point in time.”
Dr. Bernet agreed that video consults can be productive in identifying some important clinical information. “I have had at least a few patients with obvious goiter or nodule,” said Dr. Bernet, an associate professor and chair of the division of endocrinology at the Mayo Clinic in Jacksonville, Fla. “I also had a patient with hyperthyroidism from Graves disease and we were able to assess her for tremor over video.”
In the latter case, “we had the patient place a sheet of paper on the top of her hand while her arm was extended, which is the technique that can be used in person as well, and helps amplify the ability to detect if a fine tremor is present.”
“It was obvious that this patient had a tremor by video,” Dr. Bernet said.
In addition to tremor, video visits can be helpful in “looking for the presence of thyroid eye disease, enlarged thyroid, and possibly even skin changes.” Video may also be useful in evaluating respiratory effort and some cognitive behaviors, Dr. Bernet noted.
Starting to think about elective procedures again
As centers in the United States begin to reopen and permit elective procedures again, patients being considered for FNAs will likely be reintroduced according to the level of need, Dr. Hennessey noted. “Those with clear indications for FNA will be the first (to be scheduled),” while those who had very-low-risk findings, such as small nodules and cysts, “have already been deferred to 6- or 12-month follow-up ultrasounds, and decisions regarding FNAs will be made based on clinical course.”
Dr. Angell agrees that efforts to address the most urgent cases once centers reopen will be of the utmost importance. “To the greatest extent possible, providers should work together to coordinate the rescheduling of patients for FNA or surgery to avoid any further delay for those at most risk,” he said.Dr. Hennessey, Dr. Angell, and Dr. Bernet have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The third surge: Are we prepared for the non-COVID crisis?
Over the last several weeks, hospitals and health systems have focused on the COVID-19 epidemic, preparing and expanding bed capacities for the surge of admissions both in intensive care and medical units. An indirect impact of this has been the reduction in outpatient staffing and resources, with the shifting of staff for inpatient care. Many areas seem to have passed the peak in the number of cases and are now seeing a plateau or downward trend in the admissions to acute care facilities.
During this period, there has been a noticeable downtrend in patients being evaluated in the ED, or admitted for decompensation of chronic conditions like heart failure, COPD and diabetes mellitus, or such acute conditions as stroke and MI. Studies from Italy and Spain, and closer to home from Atlanta and Boston, point to a significant decrease in numbers of ST-elevation myocardial infarction (STEMI) admissions.1 Duke Health saw a decrease in stroke admissions in their hospitals by 34%.2
One could argue that these patients are in fact presenting with COVID-19 or similar symptoms as is evidenced by the studies linking the severity of SARS-Co-V2 infection to chronic conditions like diabetes mellitus and obesity.2 On the other hand, the message of social isolation and avoidance of nonurgent visits could lead to delays in care resulting in patients presenting sicker and in advanced stages.3 Also, this has not been limited to the adult population. For example, reports indicate that visits to WakeMed’s pediatric emergency rooms in Wake County, N.C., were down by 60%.2
We could well be seeing a calm before the storm. While it is anticipated that there may be a second surge of COVID-19 cases, health systems would do well to be prepared for the “third surge,” consisting of patients coming in with chronic medical conditions for which they have been, so far, avoiding follow-up and managing at home, and acute medical conditions with delayed diagnoses. The impact could likely be more in the subset of patients with limited access to health care, including medications and follow-up, resulting in a disproportionate burden on safety-net hospitals.
Compounding this issue would be the economic impact of the current crisis on health systems, their staffing, and resources. Several major organizations have already proposed budget cuts and reduction of the workforce, raising significant concerns about the future of health care workers who put their lives at risk during this pandemic.4 There is no guarantee that the federal funding provided by the stimulus packages will save jobs in the health care industry. This problem needs new leadership thinking, and every organization that puts employees over profits margins will have a long-term impact on communities.
Another area of concern is a shift in resources and workflow from ambulatory to inpatient settings for the COVID-19 pandemic, and the need for revamping the ambulatory services with reshifting the workforce. As COVID-19 cases plateau, the resurgence of non-COVID–related admissions will require additional help in inpatient settings. Prioritizing the ambulatory services based on financial benefits versus patient outcomes is also a major challenge to leadership.5
Lastly, the current health care crisis has led to significant stress, both emotional and physical, among frontline caregivers, increasing the risk of burnout.6 How leadership helps health care workers to cope with these stressors, and the resources they provide, is going to play a key role in long term retention of their talent, and will reflect on the organizational culture. Though it might seem trivial, posttraumatic stress disorder related to this is already obvious, and health care leadership needs to put every effort in providing the resources to help prevent burnout, in partnership with national organizations like the Society of Hospital Medicine and the American College of Physicians.
The expansion of telemedicine has provided a unique opportunity to address several of these issues while maintaining the nonpharmacologic interventions to fight the epidemic, and keeping the cost curve as low as possible.7 Extension of these services to all ambulatory service lines, including home health and therapy, is the next big step in the new health care era. Virtual check-ins by physicians, advance practice clinicians, and home care nurses could help alleviate the concerns regarding delays in care of patients with chronic conditions, and help identify those at risk. This would also be of help with staffing shortages, and possibly provide much needed support to frontline providers.
Dr. Prasad is currently medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He was previously quality and utilization officer and chief of the medical staff at Aurora Sinai Medical Center. Dr. Prasad is cochair of SHM’s IT Special Interest Group, sits on the HQPS Committee, and is president of SHM’s Wisconsin Chapter. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist in the UMMC School of Medicine.
References
1. Wood S. TCTMD. 2020 Apr 2. “The mystery of the missing STEMIs during the COVID-19 pandemic.”
2. Stradling R. The News & Observer. 2020 Apr 21. “Fewer people are going to Triangle [N.C.] emergency rooms, and that could be a bad thing.”
3. Kasanagottu K. USA Today. 2020 Apr 15. “Don’t delay care for chronic illness over coronavirus. It’s bad for you and for hospitals.”
4. Snowbeck C. The Star Tribune. 2020 Apr 11. “Mayo Clinic cutting pay for more than 20,000 workers.”
5. LaPointe J. RevCycle Intelligence. 2020 Mar 31. “How much will the COVID-19 pandemic cost hospitals?”
6. Gavidia M. AJMC. 2020 Mar 31. “Sleep, physician burnout linked amid COVID-19 pandemic.”
7. Hollander JE and Carr BG. N Engl J Med. 2020 Apr 30;382(18):1679-81. “Virtually perfect? Telemedicine for COVID-19.”
Over the last several weeks, hospitals and health systems have focused on the COVID-19 epidemic, preparing and expanding bed capacities for the surge of admissions both in intensive care and medical units. An indirect impact of this has been the reduction in outpatient staffing and resources, with the shifting of staff for inpatient care. Many areas seem to have passed the peak in the number of cases and are now seeing a plateau or downward trend in the admissions to acute care facilities.
During this period, there has been a noticeable downtrend in patients being evaluated in the ED, or admitted for decompensation of chronic conditions like heart failure, COPD and diabetes mellitus, or such acute conditions as stroke and MI. Studies from Italy and Spain, and closer to home from Atlanta and Boston, point to a significant decrease in numbers of ST-elevation myocardial infarction (STEMI) admissions.1 Duke Health saw a decrease in stroke admissions in their hospitals by 34%.2
One could argue that these patients are in fact presenting with COVID-19 or similar symptoms as is evidenced by the studies linking the severity of SARS-Co-V2 infection to chronic conditions like diabetes mellitus and obesity.2 On the other hand, the message of social isolation and avoidance of nonurgent visits could lead to delays in care resulting in patients presenting sicker and in advanced stages.3 Also, this has not been limited to the adult population. For example, reports indicate that visits to WakeMed’s pediatric emergency rooms in Wake County, N.C., were down by 60%.2
We could well be seeing a calm before the storm. While it is anticipated that there may be a second surge of COVID-19 cases, health systems would do well to be prepared for the “third surge,” consisting of patients coming in with chronic medical conditions for which they have been, so far, avoiding follow-up and managing at home, and acute medical conditions with delayed diagnoses. The impact could likely be more in the subset of patients with limited access to health care, including medications and follow-up, resulting in a disproportionate burden on safety-net hospitals.
Compounding this issue would be the economic impact of the current crisis on health systems, their staffing, and resources. Several major organizations have already proposed budget cuts and reduction of the workforce, raising significant concerns about the future of health care workers who put their lives at risk during this pandemic.4 There is no guarantee that the federal funding provided by the stimulus packages will save jobs in the health care industry. This problem needs new leadership thinking, and every organization that puts employees over profits margins will have a long-term impact on communities.
Another area of concern is a shift in resources and workflow from ambulatory to inpatient settings for the COVID-19 pandemic, and the need for revamping the ambulatory services with reshifting the workforce. As COVID-19 cases plateau, the resurgence of non-COVID–related admissions will require additional help in inpatient settings. Prioritizing the ambulatory services based on financial benefits versus patient outcomes is also a major challenge to leadership.5
Lastly, the current health care crisis has led to significant stress, both emotional and physical, among frontline caregivers, increasing the risk of burnout.6 How leadership helps health care workers to cope with these stressors, and the resources they provide, is going to play a key role in long term retention of their talent, and will reflect on the organizational culture. Though it might seem trivial, posttraumatic stress disorder related to this is already obvious, and health care leadership needs to put every effort in providing the resources to help prevent burnout, in partnership with national organizations like the Society of Hospital Medicine and the American College of Physicians.
The expansion of telemedicine has provided a unique opportunity to address several of these issues while maintaining the nonpharmacologic interventions to fight the epidemic, and keeping the cost curve as low as possible.7 Extension of these services to all ambulatory service lines, including home health and therapy, is the next big step in the new health care era. Virtual check-ins by physicians, advance practice clinicians, and home care nurses could help alleviate the concerns regarding delays in care of patients with chronic conditions, and help identify those at risk. This would also be of help with staffing shortages, and possibly provide much needed support to frontline providers.
Dr. Prasad is currently medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He was previously quality and utilization officer and chief of the medical staff at Aurora Sinai Medical Center. Dr. Prasad is cochair of SHM’s IT Special Interest Group, sits on the HQPS Committee, and is president of SHM’s Wisconsin Chapter. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist in the UMMC School of Medicine.
References
1. Wood S. TCTMD. 2020 Apr 2. “The mystery of the missing STEMIs during the COVID-19 pandemic.”
2. Stradling R. The News & Observer. 2020 Apr 21. “Fewer people are going to Triangle [N.C.] emergency rooms, and that could be a bad thing.”
3. Kasanagottu K. USA Today. 2020 Apr 15. “Don’t delay care for chronic illness over coronavirus. It’s bad for you and for hospitals.”
4. Snowbeck C. The Star Tribune. 2020 Apr 11. “Mayo Clinic cutting pay for more than 20,000 workers.”
5. LaPointe J. RevCycle Intelligence. 2020 Mar 31. “How much will the COVID-19 pandemic cost hospitals?”
6. Gavidia M. AJMC. 2020 Mar 31. “Sleep, physician burnout linked amid COVID-19 pandemic.”
7. Hollander JE and Carr BG. N Engl J Med. 2020 Apr 30;382(18):1679-81. “Virtually perfect? Telemedicine for COVID-19.”
Over the last several weeks, hospitals and health systems have focused on the COVID-19 epidemic, preparing and expanding bed capacities for the surge of admissions both in intensive care and medical units. An indirect impact of this has been the reduction in outpatient staffing and resources, with the shifting of staff for inpatient care. Many areas seem to have passed the peak in the number of cases and are now seeing a plateau or downward trend in the admissions to acute care facilities.
During this period, there has been a noticeable downtrend in patients being evaluated in the ED, or admitted for decompensation of chronic conditions like heart failure, COPD and diabetes mellitus, or such acute conditions as stroke and MI. Studies from Italy and Spain, and closer to home from Atlanta and Boston, point to a significant decrease in numbers of ST-elevation myocardial infarction (STEMI) admissions.1 Duke Health saw a decrease in stroke admissions in their hospitals by 34%.2
One could argue that these patients are in fact presenting with COVID-19 or similar symptoms as is evidenced by the studies linking the severity of SARS-Co-V2 infection to chronic conditions like diabetes mellitus and obesity.2 On the other hand, the message of social isolation and avoidance of nonurgent visits could lead to delays in care resulting in patients presenting sicker and in advanced stages.3 Also, this has not been limited to the adult population. For example, reports indicate that visits to WakeMed’s pediatric emergency rooms in Wake County, N.C., were down by 60%.2
We could well be seeing a calm before the storm. While it is anticipated that there may be a second surge of COVID-19 cases, health systems would do well to be prepared for the “third surge,” consisting of patients coming in with chronic medical conditions for which they have been, so far, avoiding follow-up and managing at home, and acute medical conditions with delayed diagnoses. The impact could likely be more in the subset of patients with limited access to health care, including medications and follow-up, resulting in a disproportionate burden on safety-net hospitals.
Compounding this issue would be the economic impact of the current crisis on health systems, their staffing, and resources. Several major organizations have already proposed budget cuts and reduction of the workforce, raising significant concerns about the future of health care workers who put their lives at risk during this pandemic.4 There is no guarantee that the federal funding provided by the stimulus packages will save jobs in the health care industry. This problem needs new leadership thinking, and every organization that puts employees over profits margins will have a long-term impact on communities.
Another area of concern is a shift in resources and workflow from ambulatory to inpatient settings for the COVID-19 pandemic, and the need for revamping the ambulatory services with reshifting the workforce. As COVID-19 cases plateau, the resurgence of non-COVID–related admissions will require additional help in inpatient settings. Prioritizing the ambulatory services based on financial benefits versus patient outcomes is also a major challenge to leadership.5
Lastly, the current health care crisis has led to significant stress, both emotional and physical, among frontline caregivers, increasing the risk of burnout.6 How leadership helps health care workers to cope with these stressors, and the resources they provide, is going to play a key role in long term retention of their talent, and will reflect on the organizational culture. Though it might seem trivial, posttraumatic stress disorder related to this is already obvious, and health care leadership needs to put every effort in providing the resources to help prevent burnout, in partnership with national organizations like the Society of Hospital Medicine and the American College of Physicians.
The expansion of telemedicine has provided a unique opportunity to address several of these issues while maintaining the nonpharmacologic interventions to fight the epidemic, and keeping the cost curve as low as possible.7 Extension of these services to all ambulatory service lines, including home health and therapy, is the next big step in the new health care era. Virtual check-ins by physicians, advance practice clinicians, and home care nurses could help alleviate the concerns regarding delays in care of patients with chronic conditions, and help identify those at risk. This would also be of help with staffing shortages, and possibly provide much needed support to frontline providers.
Dr. Prasad is currently medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He was previously quality and utilization officer and chief of the medical staff at Aurora Sinai Medical Center. Dr. Prasad is cochair of SHM’s IT Special Interest Group, sits on the HQPS Committee, and is president of SHM’s Wisconsin Chapter. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist in the UMMC School of Medicine.
References
1. Wood S. TCTMD. 2020 Apr 2. “The mystery of the missing STEMIs during the COVID-19 pandemic.”
2. Stradling R. The News & Observer. 2020 Apr 21. “Fewer people are going to Triangle [N.C.] emergency rooms, and that could be a bad thing.”
3. Kasanagottu K. USA Today. 2020 Apr 15. “Don’t delay care for chronic illness over coronavirus. It’s bad for you and for hospitals.”
4. Snowbeck C. The Star Tribune. 2020 Apr 11. “Mayo Clinic cutting pay for more than 20,000 workers.”
5. LaPointe J. RevCycle Intelligence. 2020 Mar 31. “How much will the COVID-19 pandemic cost hospitals?”
6. Gavidia M. AJMC. 2020 Mar 31. “Sleep, physician burnout linked amid COVID-19 pandemic.”
7. Hollander JE and Carr BG. N Engl J Med. 2020 Apr 30;382(18):1679-81. “Virtually perfect? Telemedicine for COVID-19.”