User login
DLCO found to predict outcomes in subset of COPD patients
Use of diffusing capacity of the lung for carbon monoxide may be a useful prognostic tool in patients with chronic pulmonary disease who develop pulmonary hypertension, results from a single-center retrospective cohort study found.
“Historically, COPD-PH was thought to develop as the severity of airflow obstruction, measured by Forced Expiratory Volume in one second (FEV1), and subsequent chronic hypoxemia progressed,” authors led by Aparna Balasubramanian, MD, wrote in a study published online in CHEST. “However, airflow obstruction has increasingly been noted to be insufficient in predicting clinical outcomes in the general COPD population.”
Dr. Balasubramanian of the Johns Hopkins University Division of Pulmonary and Critical Care, Baltimore, and colleagues went on to note that, while studies in COPD-PH have identified hemodynamic measures as better predictors of prognosis, these metrics require right-heart catheterization (RHC), an invasive procedure that carries its own risks. “An alternative noninvasive measure of interest is diffusing capacity of the lung for carbon monoxide (DLCO). DLCO is a measure of gas exchange reflective of the complex interactions occurring at the alveolar-capillary interface, including morphologic changes in the pulmonary vasculature,” they wrote. “Recent work by our group in a large COPD cohort has demonstrated that DLCO is an indicator of disease morbidity beyond that represented by airflow obstruction or by CT evidence of emphysema alone. This may be particularly relevant for those with COPD-PH.”
The study population consisted of 71 patients enrolled in the Johns Hopkins Pulmonary Hypertension Registry between January 2000 and January 2018, all of whom had right-heart catheterization (RHC)–proven PH and pulmonary function testing (PFT) data within 1 year of diagnostic RHC. The researchers calculated transplant-free survival from index RHC and used Cox proportional hazard methods to determine transplant-free survival with age, pulmonary vascular resistance, FEV1, oxygen use, and N-terminal pro-brain natriuretic peptide included as covariates.
The average age of patients was 65 years, 66% were female, their average body mass index was 28.3 kg/m2, and the mean number of pack-years smoked was 44. On unadjusted analysis, the transplant-free survival was 87% at 1 year, 60% at 3 years, and 51% at 5 years. Survival was associated with reduced DLCO across the observed range of pulmonary artery pressures and pulmonary vascular resistance. The researchers found that severe DLCO impairment was associated with poorer survival (P less than .001), and when they adjusted for covariates, they found that mortality increased by 4% for every percent predicted decrease in DLCO (hazard ratio, 1.04).
“This study demonstrates that DLCO, a readily available, inexpensive, noninvasive measurement, is a strong independent predictor of mortality in COPD patients with PH,” the authors concluded. “The presented findings suggest that DLCO should be considered for inclusion in prognostic tools for COPD-PH.”
Dr. Balasubramanian and associates acknowledged certain limitations of the study, including its modest sample size and single-center design and the fact that the cohort underwent subspecialty referral and invasive testing, thereby limiting its generalizability to the larger COPD population. “The findings do, however, offer insight into clinical and physiologic characteristics at one extreme of the pulmonary vascular disease spectrum among COPD patients, and generate hypotheses regarding measures that warrant further exploration in the larger COPD population,” they wrote.
The study was supported by National Heart, Lung and Blood Institute. One of the study authors has served as a consultant to GlaxoSmithKline and Celgene and receives royalties from UpToDate for authorship. Another study author has served as a consultant for Arena, Actelion, Liquidia, and United Therapeutics, and has served on the Scientific Leadership Council of the Pulmonary Hypertension Association. He also serves on the Rare Disease Advisory Panel of the Patient Centered Outcomes Research Institute. The other study authors reported having no disclosures.
SOURCE: Balasubramanian A et al. CHEST. 2020 Mar 14. doi: 10.1016/j.chest.2020.02.047.
Use of diffusing capacity of the lung for carbon monoxide may be a useful prognostic tool in patients with chronic pulmonary disease who develop pulmonary hypertension, results from a single-center retrospective cohort study found.
“Historically, COPD-PH was thought to develop as the severity of airflow obstruction, measured by Forced Expiratory Volume in one second (FEV1), and subsequent chronic hypoxemia progressed,” authors led by Aparna Balasubramanian, MD, wrote in a study published online in CHEST. “However, airflow obstruction has increasingly been noted to be insufficient in predicting clinical outcomes in the general COPD population.”
Dr. Balasubramanian of the Johns Hopkins University Division of Pulmonary and Critical Care, Baltimore, and colleagues went on to note that, while studies in COPD-PH have identified hemodynamic measures as better predictors of prognosis, these metrics require right-heart catheterization (RHC), an invasive procedure that carries its own risks. “An alternative noninvasive measure of interest is diffusing capacity of the lung for carbon monoxide (DLCO). DLCO is a measure of gas exchange reflective of the complex interactions occurring at the alveolar-capillary interface, including morphologic changes in the pulmonary vasculature,” they wrote. “Recent work by our group in a large COPD cohort has demonstrated that DLCO is an indicator of disease morbidity beyond that represented by airflow obstruction or by CT evidence of emphysema alone. This may be particularly relevant for those with COPD-PH.”
The study population consisted of 71 patients enrolled in the Johns Hopkins Pulmonary Hypertension Registry between January 2000 and January 2018, all of whom had right-heart catheterization (RHC)–proven PH and pulmonary function testing (PFT) data within 1 year of diagnostic RHC. The researchers calculated transplant-free survival from index RHC and used Cox proportional hazard methods to determine transplant-free survival with age, pulmonary vascular resistance, FEV1, oxygen use, and N-terminal pro-brain natriuretic peptide included as covariates.
The average age of patients was 65 years, 66% were female, their average body mass index was 28.3 kg/m2, and the mean number of pack-years smoked was 44. On unadjusted analysis, the transplant-free survival was 87% at 1 year, 60% at 3 years, and 51% at 5 years. Survival was associated with reduced DLCO across the observed range of pulmonary artery pressures and pulmonary vascular resistance. The researchers found that severe DLCO impairment was associated with poorer survival (P less than .001), and when they adjusted for covariates, they found that mortality increased by 4% for every percent predicted decrease in DLCO (hazard ratio, 1.04).
“This study demonstrates that DLCO, a readily available, inexpensive, noninvasive measurement, is a strong independent predictor of mortality in COPD patients with PH,” the authors concluded. “The presented findings suggest that DLCO should be considered for inclusion in prognostic tools for COPD-PH.”
Dr. Balasubramanian and associates acknowledged certain limitations of the study, including its modest sample size and single-center design and the fact that the cohort underwent subspecialty referral and invasive testing, thereby limiting its generalizability to the larger COPD population. “The findings do, however, offer insight into clinical and physiologic characteristics at one extreme of the pulmonary vascular disease spectrum among COPD patients, and generate hypotheses regarding measures that warrant further exploration in the larger COPD population,” they wrote.
The study was supported by National Heart, Lung and Blood Institute. One of the study authors has served as a consultant to GlaxoSmithKline and Celgene and receives royalties from UpToDate for authorship. Another study author has served as a consultant for Arena, Actelion, Liquidia, and United Therapeutics, and has served on the Scientific Leadership Council of the Pulmonary Hypertension Association. He also serves on the Rare Disease Advisory Panel of the Patient Centered Outcomes Research Institute. The other study authors reported having no disclosures.
SOURCE: Balasubramanian A et al. CHEST. 2020 Mar 14. doi: 10.1016/j.chest.2020.02.047.
Use of diffusing capacity of the lung for carbon monoxide may be a useful prognostic tool in patients with chronic pulmonary disease who develop pulmonary hypertension, results from a single-center retrospective cohort study found.
“Historically, COPD-PH was thought to develop as the severity of airflow obstruction, measured by Forced Expiratory Volume in one second (FEV1), and subsequent chronic hypoxemia progressed,” authors led by Aparna Balasubramanian, MD, wrote in a study published online in CHEST. “However, airflow obstruction has increasingly been noted to be insufficient in predicting clinical outcomes in the general COPD population.”
Dr. Balasubramanian of the Johns Hopkins University Division of Pulmonary and Critical Care, Baltimore, and colleagues went on to note that, while studies in COPD-PH have identified hemodynamic measures as better predictors of prognosis, these metrics require right-heart catheterization (RHC), an invasive procedure that carries its own risks. “An alternative noninvasive measure of interest is diffusing capacity of the lung for carbon monoxide (DLCO). DLCO is a measure of gas exchange reflective of the complex interactions occurring at the alveolar-capillary interface, including morphologic changes in the pulmonary vasculature,” they wrote. “Recent work by our group in a large COPD cohort has demonstrated that DLCO is an indicator of disease morbidity beyond that represented by airflow obstruction or by CT evidence of emphysema alone. This may be particularly relevant for those with COPD-PH.”
The study population consisted of 71 patients enrolled in the Johns Hopkins Pulmonary Hypertension Registry between January 2000 and January 2018, all of whom had right-heart catheterization (RHC)–proven PH and pulmonary function testing (PFT) data within 1 year of diagnostic RHC. The researchers calculated transplant-free survival from index RHC and used Cox proportional hazard methods to determine transplant-free survival with age, pulmonary vascular resistance, FEV1, oxygen use, and N-terminal pro-brain natriuretic peptide included as covariates.
The average age of patients was 65 years, 66% were female, their average body mass index was 28.3 kg/m2, and the mean number of pack-years smoked was 44. On unadjusted analysis, the transplant-free survival was 87% at 1 year, 60% at 3 years, and 51% at 5 years. Survival was associated with reduced DLCO across the observed range of pulmonary artery pressures and pulmonary vascular resistance. The researchers found that severe DLCO impairment was associated with poorer survival (P less than .001), and when they adjusted for covariates, they found that mortality increased by 4% for every percent predicted decrease in DLCO (hazard ratio, 1.04).
“This study demonstrates that DLCO, a readily available, inexpensive, noninvasive measurement, is a strong independent predictor of mortality in COPD patients with PH,” the authors concluded. “The presented findings suggest that DLCO should be considered for inclusion in prognostic tools for COPD-PH.”
Dr. Balasubramanian and associates acknowledged certain limitations of the study, including its modest sample size and single-center design and the fact that the cohort underwent subspecialty referral and invasive testing, thereby limiting its generalizability to the larger COPD population. “The findings do, however, offer insight into clinical and physiologic characteristics at one extreme of the pulmonary vascular disease spectrum among COPD patients, and generate hypotheses regarding measures that warrant further exploration in the larger COPD population,” they wrote.
The study was supported by National Heart, Lung and Blood Institute. One of the study authors has served as a consultant to GlaxoSmithKline and Celgene and receives royalties from UpToDate for authorship. Another study author has served as a consultant for Arena, Actelion, Liquidia, and United Therapeutics, and has served on the Scientific Leadership Council of the Pulmonary Hypertension Association. He also serves on the Rare Disease Advisory Panel of the Patient Centered Outcomes Research Institute. The other study authors reported having no disclosures.
SOURCE: Balasubramanian A et al. CHEST. 2020 Mar 14. doi: 10.1016/j.chest.2020.02.047.
FROM CHEST
Trial undertaken to better predict pulmonary hypertension prognosis
A research team at Vanderbilt University Medical Center has begun a trial to compare the value of tracking daily activity and the Six Minute Walk Distance to predict pulmonary hypertension prognosis. The Longitudinal Pulmonary Vascular Disease Phenomics Program (L-PVDOMICS), a prospective, longitudinal, observational study will track daily activity and patient-reported outcomes in participants enrolled. Patients with pulmonary hypertension and healthy participants will undergo activity monitoring for 12 weeks once a year for 4 years. Metrics will include patient-reported outcomes including quality of life (emphasis-10, Minnesota Living with Heart Failure, and SF-36 surveys), medication changes, hospitalization, and death.
The study is designed to establish the clinical utility of daily activity tracking in patients with pulmonary hypertension and to identify clinical factors associated with reduced daily activity. Five hundred patients are expected to enroll and the estimated closing date is June 2023. The hypothesis for the study is that daily activity will have stronger prognostic value after 12 weeks than the Six Minute Walk Distance in patients with pulmonary hypertension. Participants will wear an accelerometer to record activity level to determine daily activities and will also engage in the Six Minute Walk Distance Test.
Individuals that are pregnant or have been hospitalized within the past 3 months will be excluded. Participants are currently being recruited.
The trial sponsor is Vanderbilt University Medical Center.
A research team at Vanderbilt University Medical Center has begun a trial to compare the value of tracking daily activity and the Six Minute Walk Distance to predict pulmonary hypertension prognosis. The Longitudinal Pulmonary Vascular Disease Phenomics Program (L-PVDOMICS), a prospective, longitudinal, observational study will track daily activity and patient-reported outcomes in participants enrolled. Patients with pulmonary hypertension and healthy participants will undergo activity monitoring for 12 weeks once a year for 4 years. Metrics will include patient-reported outcomes including quality of life (emphasis-10, Minnesota Living with Heart Failure, and SF-36 surveys), medication changes, hospitalization, and death.
The study is designed to establish the clinical utility of daily activity tracking in patients with pulmonary hypertension and to identify clinical factors associated with reduced daily activity. Five hundred patients are expected to enroll and the estimated closing date is June 2023. The hypothesis for the study is that daily activity will have stronger prognostic value after 12 weeks than the Six Minute Walk Distance in patients with pulmonary hypertension. Participants will wear an accelerometer to record activity level to determine daily activities and will also engage in the Six Minute Walk Distance Test.
Individuals that are pregnant or have been hospitalized within the past 3 months will be excluded. Participants are currently being recruited.
The trial sponsor is Vanderbilt University Medical Center.
A research team at Vanderbilt University Medical Center has begun a trial to compare the value of tracking daily activity and the Six Minute Walk Distance to predict pulmonary hypertension prognosis. The Longitudinal Pulmonary Vascular Disease Phenomics Program (L-PVDOMICS), a prospective, longitudinal, observational study will track daily activity and patient-reported outcomes in participants enrolled. Patients with pulmonary hypertension and healthy participants will undergo activity monitoring for 12 weeks once a year for 4 years. Metrics will include patient-reported outcomes including quality of life (emphasis-10, Minnesota Living with Heart Failure, and SF-36 surveys), medication changes, hospitalization, and death.
The study is designed to establish the clinical utility of daily activity tracking in patients with pulmonary hypertension and to identify clinical factors associated with reduced daily activity. Five hundred patients are expected to enroll and the estimated closing date is June 2023. The hypothesis for the study is that daily activity will have stronger prognostic value after 12 weeks than the Six Minute Walk Distance in patients with pulmonary hypertension. Participants will wear an accelerometer to record activity level to determine daily activities and will also engage in the Six Minute Walk Distance Test.
Individuals that are pregnant or have been hospitalized within the past 3 months will be excluded. Participants are currently being recruited.
The trial sponsor is Vanderbilt University Medical Center.
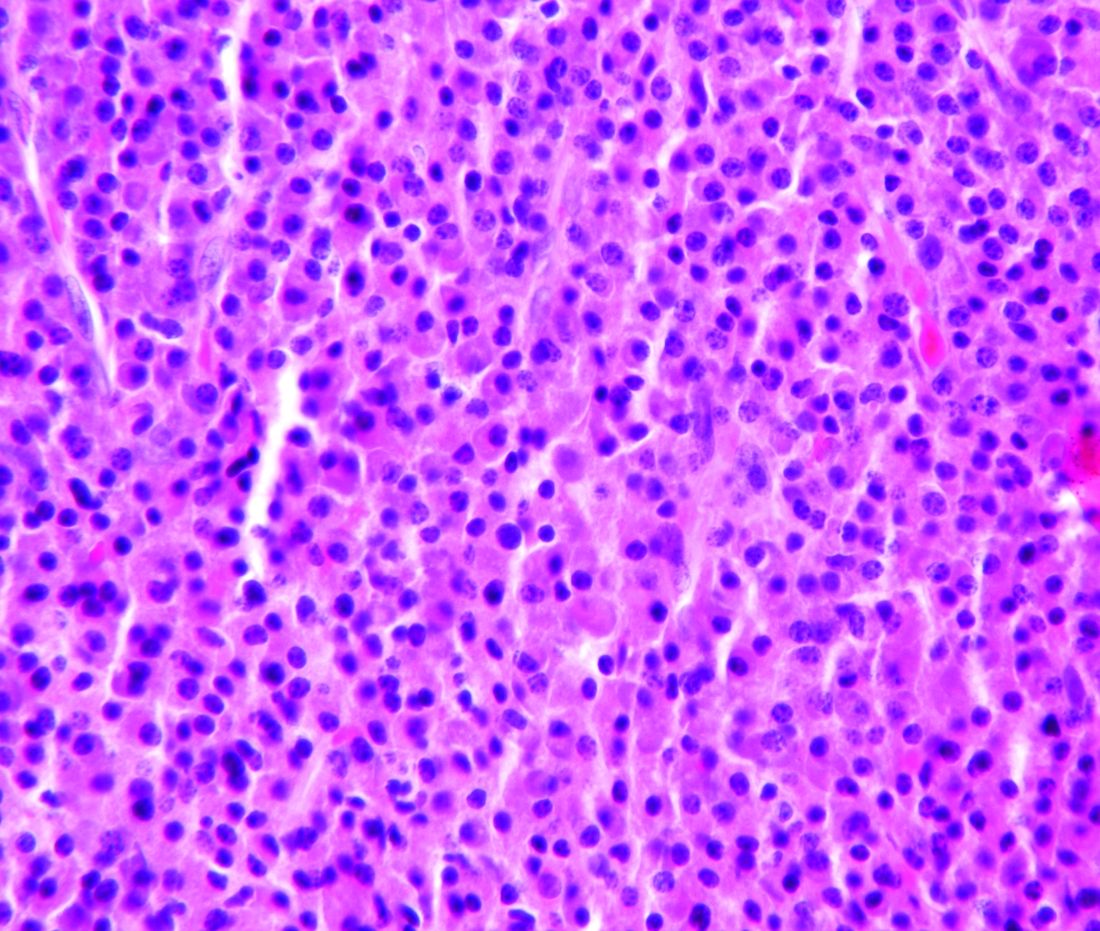
FDA OKs new drug for triple-negative breast cancer
The US Food and Drug Administration (FDA) granted accelerated approval to sacituzumab govitecan (Trodelvy, Immunomedics) for the treatment of metastatic triple-negative breast cancer (TNBC).
Eligible patients must have received at least two prior therapies.
TNBC is so-called because it lacks the three cellular targets present in more common forms of breast cancer. It is usually treated with chemotherapy.
Sacituzumab govitecan offers a new approach – and it has a target.
Given intravenously, the new drug is an antibody-drug conjugate in which SN-38, an active metabolite of the chemotherapy drug irinotecan (multiple brands), is coupled to a monoclonal antibody that targets an antigen that has high expression in TNBC and induces cancer cell growth.
“Metastatic triple-negative breast cancer is an aggressive form of breast cancer with limited treatment options,” observed Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research in a press statement. “There is intense interest in finding new medications” for this patient population, he added.
The new approval is based on safety and efficacy results from a phase 1/2 clinical trial of 108 patients (median age, 56 years) who had received at least two prior treatments for metastatic disease.
The overall response rate was 33% (n = 36), including three complete responses. Median duration of response was 7.7 months. Of responders, 55.6% maintained their response for at least 6 months and 16.7% for at least 12 months.
Median progression-free survival was 5.5 months, and median overall survival was 13.0 months.
The study data were published last year in the New England Journal of Medicine.
“It’s not every day that we see this sort of clinical activity in this aggressive subtype of breast cancer,” said senior study author Kevin Kalinsky, MD, in an interview at that time. He is a medical oncologist at New York–Presbyterian Hospital and Columbia University Medical Center in New York City.
The most common side effects of the new therapy were nausea, neutropenia, diarrhea, fatigue, anemia, vomiting, alopecia, constipation, decreased appetite, rash, and abdominal pain.
No peripheral neuropathy of grade 3 or higher was reported.
In the study, patients received sacituzumab govitecan intravenously (10 mg/kg body weight) on days 1 and 8 of each 21-day cycle until disease progression or unacceptable toxicity.
The 108 participants received a mean 18.7 doses of sacituzumab govitecan, or 9.6 cycles. The median duration of exposure was 5.1 months.
Three patients discontinued treatment because of adverse events, and two patients discontinued because of drug-related events.
The prescribing information includes a boxed warning regarding the risks of severe neutropenia and severe diarrhea. Blood cell counts should be monitored during treatment and granulocyte-colony stimulating factor (G-CSF) therapy should be considered. Anti-infective treatment should be initiated in the event of febrile neutropenia. Patients with reduced uridine diphosphate-glucuronosyltransferase 1A1 (UGT1A1) activity are at increased risk for neutropenia following initiation of treatment.
The new drug can also cause hypersensitivity reactions including severe anaphylactic reactions.
Women who are pregnant should not take sacituzumab govitecan.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) granted accelerated approval to sacituzumab govitecan (Trodelvy, Immunomedics) for the treatment of metastatic triple-negative breast cancer (TNBC).
Eligible patients must have received at least two prior therapies.
TNBC is so-called because it lacks the three cellular targets present in more common forms of breast cancer. It is usually treated with chemotherapy.
Sacituzumab govitecan offers a new approach – and it has a target.
Given intravenously, the new drug is an antibody-drug conjugate in which SN-38, an active metabolite of the chemotherapy drug irinotecan (multiple brands), is coupled to a monoclonal antibody that targets an antigen that has high expression in TNBC and induces cancer cell growth.
“Metastatic triple-negative breast cancer is an aggressive form of breast cancer with limited treatment options,” observed Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research in a press statement. “There is intense interest in finding new medications” for this patient population, he added.
The new approval is based on safety and efficacy results from a phase 1/2 clinical trial of 108 patients (median age, 56 years) who had received at least two prior treatments for metastatic disease.
The overall response rate was 33% (n = 36), including three complete responses. Median duration of response was 7.7 months. Of responders, 55.6% maintained their response for at least 6 months and 16.7% for at least 12 months.
Median progression-free survival was 5.5 months, and median overall survival was 13.0 months.
The study data were published last year in the New England Journal of Medicine.
“It’s not every day that we see this sort of clinical activity in this aggressive subtype of breast cancer,” said senior study author Kevin Kalinsky, MD, in an interview at that time. He is a medical oncologist at New York–Presbyterian Hospital and Columbia University Medical Center in New York City.
The most common side effects of the new therapy were nausea, neutropenia, diarrhea, fatigue, anemia, vomiting, alopecia, constipation, decreased appetite, rash, and abdominal pain.
No peripheral neuropathy of grade 3 or higher was reported.
In the study, patients received sacituzumab govitecan intravenously (10 mg/kg body weight) on days 1 and 8 of each 21-day cycle until disease progression or unacceptable toxicity.
The 108 participants received a mean 18.7 doses of sacituzumab govitecan, or 9.6 cycles. The median duration of exposure was 5.1 months.
Three patients discontinued treatment because of adverse events, and two patients discontinued because of drug-related events.
The prescribing information includes a boxed warning regarding the risks of severe neutropenia and severe diarrhea. Blood cell counts should be monitored during treatment and granulocyte-colony stimulating factor (G-CSF) therapy should be considered. Anti-infective treatment should be initiated in the event of febrile neutropenia. Patients with reduced uridine diphosphate-glucuronosyltransferase 1A1 (UGT1A1) activity are at increased risk for neutropenia following initiation of treatment.
The new drug can also cause hypersensitivity reactions including severe anaphylactic reactions.
Women who are pregnant should not take sacituzumab govitecan.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) granted accelerated approval to sacituzumab govitecan (Trodelvy, Immunomedics) for the treatment of metastatic triple-negative breast cancer (TNBC).
Eligible patients must have received at least two prior therapies.
TNBC is so-called because it lacks the three cellular targets present in more common forms of breast cancer. It is usually treated with chemotherapy.
Sacituzumab govitecan offers a new approach – and it has a target.
Given intravenously, the new drug is an antibody-drug conjugate in which SN-38, an active metabolite of the chemotherapy drug irinotecan (multiple brands), is coupled to a monoclonal antibody that targets an antigen that has high expression in TNBC and induces cancer cell growth.
“Metastatic triple-negative breast cancer is an aggressive form of breast cancer with limited treatment options,” observed Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research in a press statement. “There is intense interest in finding new medications” for this patient population, he added.
The new approval is based on safety and efficacy results from a phase 1/2 clinical trial of 108 patients (median age, 56 years) who had received at least two prior treatments for metastatic disease.
The overall response rate was 33% (n = 36), including three complete responses. Median duration of response was 7.7 months. Of responders, 55.6% maintained their response for at least 6 months and 16.7% for at least 12 months.
Median progression-free survival was 5.5 months, and median overall survival was 13.0 months.
The study data were published last year in the New England Journal of Medicine.
“It’s not every day that we see this sort of clinical activity in this aggressive subtype of breast cancer,” said senior study author Kevin Kalinsky, MD, in an interview at that time. He is a medical oncologist at New York–Presbyterian Hospital and Columbia University Medical Center in New York City.
The most common side effects of the new therapy were nausea, neutropenia, diarrhea, fatigue, anemia, vomiting, alopecia, constipation, decreased appetite, rash, and abdominal pain.
No peripheral neuropathy of grade 3 or higher was reported.
In the study, patients received sacituzumab govitecan intravenously (10 mg/kg body weight) on days 1 and 8 of each 21-day cycle until disease progression or unacceptable toxicity.
The 108 participants received a mean 18.7 doses of sacituzumab govitecan, or 9.6 cycles. The median duration of exposure was 5.1 months.
Three patients discontinued treatment because of adverse events, and two patients discontinued because of drug-related events.
The prescribing information includes a boxed warning regarding the risks of severe neutropenia and severe diarrhea. Blood cell counts should be monitored during treatment and granulocyte-colony stimulating factor (G-CSF) therapy should be considered. Anti-infective treatment should be initiated in the event of febrile neutropenia. Patients with reduced uridine diphosphate-glucuronosyltransferase 1A1 (UGT1A1) activity are at increased risk for neutropenia following initiation of treatment.
The new drug can also cause hypersensitivity reactions including severe anaphylactic reactions.
Women who are pregnant should not take sacituzumab govitecan.
This article first appeared on Medscape.com.
Private equity: Salvation or death sentence?
The dermatologist had been in practice just a few years when he was approached by a private equity group. This was around 2015, when dermatology was just starting to buzz about investor buyouts. He was curious, so he agreed to meet with the company.
“They approached me with the idea that they could help me grow my practice, help my patients, and cut down overhead,” said the northern Alabama dermatologist, who asked that his name not be used. Over a lavish dinner, the investors lauded the clinician for his business acumen and for having built a great practice so quickly. They made an enticing buyout offer.
Before agreeing, he thought it over. He told the investors he wanted a few more years on his own before he’d consider a buyout. They encouraged him to think about it some more. He did, but the answer was still no.
Suddenly, the investors became aggressive and threatening. “They told me, ‘you have just made the biggest mistake of your early career. We’re going to make sure that our practice swallows you up, and if we can’t take you over and put you out of business, we’re going to buy up everyone around you so you can’t survive,’ ” said the dermatologist.
Surprisingly, the experience did not sour him on private equity – he even entertained a successor company’s offer. But he’s become more circumspect. “It has the potential to do good,” he said, adding that such financial support could help him pay employees, keep the lights on, and improve care. But the investors’ emphasis on profit is not appealing, he said.
“I’m going to have to have good proof that it’s truly going to improve patient care and outcomes. And I haven’t seen that yet,” he said.
Salvation or death sentence?
Depending on whom you ask, the continuing growth of private equity purchases of dermatology practices is either the death – or salvation – of the specialty.
Many dermatologists question whether the financial backers will invest in quality of care, or if they just will hire mid-level providers to churn out procedures to plump up revenues.
Neither the controversy nor the acquisitions show any sign of abating.
The American Academy of Dermatology has hosted debates on the topic at its annual meetings – and was to do so in 2020 until COVID-19 led to the meeting’s cancellation. AAD has not weighed in with any official policy and is not releasing data it may be collecting on the potential impact of private equity ownership. The organization provided a statement from President George J. Hruza, MD, who said, “the AAD supports a member’s right to choose the model that works best for them,” adding that the Academy “expects its members to provide safe and effective patient care, regardless of a dermatologist’s practice setting.” Dr. Hruza sold his Chesterfield, Mo., practice to United Skin Specialists, a private equity–backed company, in 2016, and still works at the same practice.
Some have said the acquisitions need to stop. “Until meaningful data are available on what happens to the quality of care and affordability for patients and payers, dermatologists should stop selling their practices to private equity firms, and legislators should prohibit such transactions,” wrote Joshua M. Sharfstein, MD, and Jamar Slocum, MD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, in an editorial in July (JAMA Dermatol. 2019;155[9]:1007-8).
Although he acknowledged that he has not tracked the issue closely and that little data exist on the impact on quality or cost, Dr. Sharfstein has not changed his tune. “I think there are enough warning signs to say we should put the brakes on,” he said in an interview.
“For what reason?” asked Betsy Wernli, MD, president of Forefront Dermatology, an investor-owned group based in Manitowoc, Wis. She said it seems that “on this topic, we abandon our scientific foundations and default to emotion and anecdote,” she said in an interview. “Having capital, and an investor that supports us has allowed us to perform better patient care,” she said. Dermatologist variance across all practices and practice models should be cause for more concern, she added.
Sailesh Konda, MD, has been an outspoken critic. Dr. Konda, medical director and clinical assistant professor in the department of dermatology at the University of Florida, Gainesville, and colleagues detailed the complicated financial machinations of private equity in the Journal of the American Academy of Dermatology. They showed that private investors seemed to hone in on buying outlier practices that performed high numbers of procedures. The paper – first made public in the fall of 2018 – created an uproar, especially among private equity companies. It was initially removed from the website in conjunction with a request from the editor that its conclusions be altered to be less harsh on private equity, according to the New York Times. The paper was eventually published in 2019 (J Am Acad Dermatol. Jul;81[1]:287-296.e8).
Dr. Konda has spoken at various dermatology forums and health care gatherings on private equity. He told the Times that he had given 16 talks to health care groups in 2018, and he was due to speak to a health care investors’ group in 2020. But he would not comment on the record for this story.
Brett Coldiron, MD, a former president of the AAD, also has been critical. He believes investor-owners push for more biopsies, freezing of actinic keratoses, Moh’s surgery, and other well-paying procedures. “I’m convinced that private equity may be the undoing of our specialty,” Dr. Coldiron said in an interview.
In a paper titled, “Private Equity Acquisition of Physician Practices,” published in the Annals of Internal Medicine in January 2019, Lawrence Casalino, MD, PhD, chief of the division of health policy and economics at New York’s Weill Cornell Medicine, and colleagues wrote that “private equity firms focus on specialties with high potential for additional income from elective procedures and ancillary services,” and that “dermatology has been a major focus” (Ann Intern Med. 2019;170[2]:114-5).
And in a viewpoint published in JAMA in February 2019, first-year medical student Suhas Gondi and Zirui Song, MD, PhD, both of Harvard Medical School, Boston, concluded that investor-owned practices could drive up overall health spending in part because they extract better reimbursement from insurers (JAMA. 2019;321[11]:1047-8).
Access could also become an issue if the companies drive smaller independent practices out of business, they wrote.
On the other hand, they said, “these investments may also benefit patients and bring more efficiency to a system burdened with waste.” The authors called for more research and “thoughtful regulation” to enhance the potential positives while mitigating the negatives.
So far, the acquisitions have largely escaped the notice of regulators or lawmakers. Congress has made noises about targeting specialty practices owned by private equity as a means of taming surprise medical bills, but that legislation has been stymied.
Dr. Coldiron is convinced that private investors will eventually be tripped up by state laws that prohibit the corporate practice of medicine.
Leslie Baumann, MD, who sold her Miami practice in October 2019 to the investor-owned Skin and Cancer Associates, said critics are too cynical. “What if these private equity firms are going to actually make our specialty better?” she asked in an interview.
What makes dermatology attractive?
Private equity has been acquiring specialty practices since at least 2009, with an acceleration over the last 5 years. Dermatology has been a frequent target, in part because so many dermatologists were in independent or small group private practices, making them ripe for takeover.
A 2015 report on the specialty by Cegedim, a company that provides information technology support to health care, found that the majority of practices had fewer than five physicians and that 57% of the practices were independent.
But more dermatologists are choosing employment. In a 2018 Medscape survey, 57% of dermatologists reported they were employed, while 49% were self-employed.
During 2013-2016, investors bought 35 dermatology practices – comprising 334 physicians, according to one study published in February (JAMA. 2020;323[7]:663-5). Investors bought 69 anesthesiology practices, 43 emergency medicine practices, and 39 family medicine practices during the same period.
Harvard’s Mr. Gondi and Dr. Song estimated that dermatology practices accounted for 15% of investor purchases in 2015 and 2016, even though dermatologists make up just 1% of U.S. clinicians.
In another paper published in JAMA Dermatology, Sally Tan, MD, and colleagues at Brigham and Women’s Hospital, Boston, and Harvard medical and business schools, estimated that, in 2019, at least 184 practices, comprising 381 clinics, were owned by 17 private equity groups and that the acquisitions had been accelerating: from 5 in 2012 to 59 in 2017 to 34 in the first 5 months of 2018 (JAMA Dermatol. 2019;155[9]:1013-21).
“It’s a very attractive area for investors because they know that the future is bright for dermatology,” said Reuven Porges, MD, CEO of Ft. Lauderdale-based Skin and Cancer Associates, which is owned by a private investor. Because dermatology involves providing many ancillary services and cash-only cosmetic services, “it has tremendous potential to continue to be successful in the future regardless of what health care changes are coming,” Dr. Porges said in an interview.
Investors also see promise in dermatology in the United States because “there’s a huge supply demand mismatch,” said Vance Vanier, MD, a cofounding managing partner at Chicago Pacific Founders, the private equity owner of Pinnacle Dermatology, which has 52 locations in Illinois, Indiana, Michigan, Minnesota, and Tennessee.
Theoretically, when investors handle billing, insurance negotiations, and health information technology, it gives clinicians more time to practice, Dr. Vanier said in an interview.
“Once that doctor is freed up to not do administrative tasks and focus on patient care, then, if they want to, they can see more patients and be more responsive to their needs,” he said.
Dr. Vanier said investor acquisitions are here to stay. “This is a trend that could go on for another 50 years before any saturation point is hit,” he said. “It’s a $2 trillion market. It’s hard to wrap your head around how enormous health care services is,” he said.
Dermatology acquisitions will be driven by the continuing imbalance of physician supply and patient demand; the financial pressure on newly graduating physicians who have big debt loads; the requirements for investment in health information technology to report quality metrics; and an aging population, Dr. Vanier said.
In a JAMA Dermatology viewpoint, Jack Resneck Jr., MD, professor of dermatology, University of California, San Francisco, listed many of the same factors – plus a skin cancer epidemic – as fueling dermatology acquisitions (JAMA Dermatol. 2018;154[1]:13-4).
Medical practices – not just dermatology practices – also offer a pure financial play. “Acquisitions of smaller practices provide a major arbitrage opportunity,” Dr. Casalino and colleagues said in the January 2019 Annals of Internal Medicine paper. In a merger of smaller practices into larger, the smaller practice’s valuation immediately becomes that of the bigger one, they wrote.
Could the bottom fall out?
Creating giant groups through consolidation is a main aim for private equity.
Skin and Cancer Associates, founded in 1971, was a large entity, with 25 practices. But for a long time, its leaders had wanted to become a regional or a national player, said Dr. Porges. Those leaders asked Dr. Porges – who helped take his former radiology practice through a private equity purchase – to help them attract investors. In March 2018, Susquehanna Private Capital signed on as a “partner” with Skin and Cancer Associates.
It has since almost doubled in size, with 40 locations and 60 dermatologists, all in Florida, Dr. Porges said. “The only limiting factor for growing it as fast as we want, is really money,” he said.
Consolidation is just an initial step. Most investors have a finite timeline for cashing out. “The ultimate goal is often to realize a profitable secondary sale in three to seven years to another PE investor (or even a publicly traded entity),” Dr. Resneck wrote in the 2018 JAMA Dermatology paper.
Not all private equity companies are the same, said Dr. Wernli, of Forefront. Dermatologists can investigate a company’s “hold period” – how long they keep an investment before trading – and the strength of its capitalization before deciding to sell, she said.
Since 2016, Forefront has been owned by the Ontario Municipal Employee Retirement System (OMERS), a pension fund for the province’s public workers. OMERS bought Forefront from Varsity Healthcare Partners, which had owned the dermatology group for just 2 years.
Dr. Wernli said OMERS is a good, solid investor. “They have unlimited resources to invest so they don’t have to quickly flip a company to satisfy an investment in another company,” she said.
Some investor-backed dermatology practices have gone belly up. In 2012, WestWind Investors bought DermOne, based in Toms River, N.J. But by early 2018, the business had fallen apart, and some practices – in North Carolina, New Jersey, Texas, and Virginia – just shut their doors.
Long Island City, N.Y.–based Schweiger Dermatology Group, backed by private equity, snapped up nine of the New Jersey DermOne practices in March 2018.
Another private equity–backed company, U.S. Dermatology Partners, defaulted on a $377 million loan in January 2020. As reported by Bloomberg, the company had $340 million in revenue in 2018. U.S. Dermatology’s owners are reportedly working out a recapitalization or debt-for-equity swap with the lenders.
Dr. Wernli said that financial problems aren’t unique to investor-owned practices and that doctors could still be out of a job if a private practice goes under.
“A private practice can also default on their loans that they’ve used to fund their own personal practice, leaving employed physicians in the same situation,” she said.
Patients are likely to be in the dark, however, until the doors close.
Pressure on practices
Private equity is changing the shape of practice for both those who work for investor-owned businesses and those still out on their own.
The Alabama dermatologist, for instance, said it has made it harder for him to recruit new doctors, who are offered big signing bonuses and a steady income by the investor-owned practices. “They’re skewing the numbers,” he said, adding that residents are now expecting a big payment and benefits.
Dr. Baumann said that when she was on her own, she had trouble finding and recruiting good dermatologists. But it has become easier since she’d sold to Skin and Cancer Associates, she said, noting that Dr. Porges recently found a qualified candidate for her to interview a week after she put in a request.
Another dermatologist in a Midwestern metropolitan practice – who did not want his name used – said that when it came time for him to increase his equity stake, his older partner, who was near retirement and had explored selling to private equity – wanted four-and-a-half times the price that had been discussed when he joined the practice.
The younger partner believes the private equity offers inflated the practice’s valuation in his partner’s mind. He ended up leaving the practice.
Many dermatologists have been led to believe that their practices are worth more than they might be, according to Dr. Coldiron. “I think a lot of these doctors that sell out are deluded. They think that they’re getting a lot of money and they’re not,” he said.
Typically, investors may offer three or four times earnings before interest, taxes, depreciation and amortization (EBITDA). The money paid out is taxed at the capital gains rate, which provides some savings. “But you have to pay that all back, because when they sign you up, you become an employee,” Dr. Coldiron said.
Doctors often agree to work for 5 years, but during that period, their base salary is decreased while the buyout cash is meted out to them, he added. A chunk of the buyout usually is also given as equity, but that equity is worthless unless the investor sells to another entity.
Pinnacle Dermatology doesn’t want doctors to retire immediately upon an acquisition, said Dr. Vanier of Chicago Pacific Founders. “We want to find physician partners who want to keep working,” he said. “We strongly believe if you don’t have strong physician leadership, experienced physician leadership, that your odds of success go down.”
Chicago Pacific also believes physicians should have an ownership interest, he said. It allows them to share in the eventual financial rewards – whether that’s 5 or 20 years later, said Dr. Vanier.
Dr. Coldiron sees other pressures that skew practice styles and can harm patient care. Clinicians in investor-owned practices are often urged to refer all dermatopathology to labs owned by the practice and often, a Moh’s surgeon is employed to service all the practices – sometimes even being flown in from elsewhere, he claimed.
That takes away the clinician’s autonomy in terms of referring where he or she feels appropriate and also could harm pathologists and Moh’s surgeons that depend on those referral streams, he added.
In their paper, Mr. Gondi and Dr. Song wrote that this practice is concerning because “keeping referrals within the practice may render referral patterns less responsive to patient needs or preference.”
Procedure factories?
Many critics say investor-backed practices are goosing revenues by hiring more mid-level providers – such as nurse practitioners and physician assistants – and getting them to perform more procedures.
Midlevel practitioners do more biopsies than dermatologists do to get a diagnosis, according to Dr. Coldiron.
A 2018 JAMA Dermatology study appears to back that up. Physician assistants needed to conduct 3.9 biopsies to diagnose one skin cancer, compared to 3.3 for dermatologists. For a single melanoma, the number needed to biopsy was 39.4 for PAs and 25.4 for dermatologists (JAMA Dermatol. 2018;154[5]:569-73).
Skin biopsies have almost doubled in the last decade, said Dr. Coldiron. “The skin cancer epidemic would account for only half of that,” he said.
“The ultimate loser is the patient – because the patient doesn’t get the highest quality care and the patient has unnecessary things done to him or her,” he said. But, he said, he could not directly tie the biopsy increase to the rise of private equity.
Forefront tracks the number of biopsies per patient done by every dermatologist in its network – to make sure that no one is outside the norms set by the Centers for Medicare and Medicaid Services, said Dr. Wernli. And she said biopsies declined after the group was bought by private equity.
Dr. Baumann said the average number of biopsies per patient at Skin and Cancer Associates in 2019 was 0.20 – less than the 0.30 average reported by Medicare that same year.
The rising use of mid-level providers existed long before private equity came on the scene, said Dr. Wernli. “There’s not enough board-certified dermatologists to satisfy need,” she said, noting that, in addition, many clinicians won’t serve rural areas. “If we don’t move and extend ourselves, there will be someone who fills our shoes,” she said, adding that Forefront has 1 mid-level for every 1.5 to 2 dermatologists.
Skin and Cancer Associates has 55 doctors and 29 physician assistants, said Dr. Baumann, adding that she had not been pressured to add any mid-level providers to her practice.
Excitement about sale shot down
Dr. Wernli and Dr. Baumann both have been happy with their decision to ally with private equity. For Dr. Baumann, however, her move was tinged by online attacks that reflected the strong opinions on the topic.
She began looking into selling her practice when one of her businesses – Skin Type Solutions – began taking off. Both her clinical practice and research business were thriving. She had two children at home and was having a hard time keeping up with the administrative end of her businesses.
None of her partners nor any groups in Miami showed interest in purchasing the practice, so she began researching private equity. She spoke with seven companies before settling on Skin and Cancer Associates. They had “a long track record of successfully running practices,” said Dr. Baumann, adding that “the doctors who work there are happy, and I respect the quality of the physicians and the organization.”
When she closed the deal in October 2019, she agreed to stay on for 5 years and signed a noncompete clause that she deems “very reasonable.” Among the perks she cites: being able to consult via telemedicine with an expert on pigmented lesions; quick and easy referrals to a Moh’s surgeon; being able to train residents; and having paid personal time off.
It’s less responsibility and the same or better job satisfaction, she said.
But when she shared the news on a private Facebook group for board-certified dermatologists, she was vilified. Of some 195 comments, about half were “mean,” said Dr. Baumann.
“I was shocked about how strongly everybody feels,” she said. Those commenting accused her of doing it for the money or said that her move was contributing to the ruination of dermatology.
“I just defended myself,” she said. “For me, it was my time.”
Dr. Coldiron and Dr. Baumann are members of the Dermatology News editorial advisory board.
The dermatologist had been in practice just a few years when he was approached by a private equity group. This was around 2015, when dermatology was just starting to buzz about investor buyouts. He was curious, so he agreed to meet with the company.
“They approached me with the idea that they could help me grow my practice, help my patients, and cut down overhead,” said the northern Alabama dermatologist, who asked that his name not be used. Over a lavish dinner, the investors lauded the clinician for his business acumen and for having built a great practice so quickly. They made an enticing buyout offer.
Before agreeing, he thought it over. He told the investors he wanted a few more years on his own before he’d consider a buyout. They encouraged him to think about it some more. He did, but the answer was still no.
Suddenly, the investors became aggressive and threatening. “They told me, ‘you have just made the biggest mistake of your early career. We’re going to make sure that our practice swallows you up, and if we can’t take you over and put you out of business, we’re going to buy up everyone around you so you can’t survive,’ ” said the dermatologist.
Surprisingly, the experience did not sour him on private equity – he even entertained a successor company’s offer. But he’s become more circumspect. “It has the potential to do good,” he said, adding that such financial support could help him pay employees, keep the lights on, and improve care. But the investors’ emphasis on profit is not appealing, he said.
“I’m going to have to have good proof that it’s truly going to improve patient care and outcomes. And I haven’t seen that yet,” he said.
Salvation or death sentence?
Depending on whom you ask, the continuing growth of private equity purchases of dermatology practices is either the death – or salvation – of the specialty.
Many dermatologists question whether the financial backers will invest in quality of care, or if they just will hire mid-level providers to churn out procedures to plump up revenues.
Neither the controversy nor the acquisitions show any sign of abating.
The American Academy of Dermatology has hosted debates on the topic at its annual meetings – and was to do so in 2020 until COVID-19 led to the meeting’s cancellation. AAD has not weighed in with any official policy and is not releasing data it may be collecting on the potential impact of private equity ownership. The organization provided a statement from President George J. Hruza, MD, who said, “the AAD supports a member’s right to choose the model that works best for them,” adding that the Academy “expects its members to provide safe and effective patient care, regardless of a dermatologist’s practice setting.” Dr. Hruza sold his Chesterfield, Mo., practice to United Skin Specialists, a private equity–backed company, in 2016, and still works at the same practice.
Some have said the acquisitions need to stop. “Until meaningful data are available on what happens to the quality of care and affordability for patients and payers, dermatologists should stop selling their practices to private equity firms, and legislators should prohibit such transactions,” wrote Joshua M. Sharfstein, MD, and Jamar Slocum, MD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, in an editorial in July (JAMA Dermatol. 2019;155[9]:1007-8).
Although he acknowledged that he has not tracked the issue closely and that little data exist on the impact on quality or cost, Dr. Sharfstein has not changed his tune. “I think there are enough warning signs to say we should put the brakes on,” he said in an interview.
“For what reason?” asked Betsy Wernli, MD, president of Forefront Dermatology, an investor-owned group based in Manitowoc, Wis. She said it seems that “on this topic, we abandon our scientific foundations and default to emotion and anecdote,” she said in an interview. “Having capital, and an investor that supports us has allowed us to perform better patient care,” she said. Dermatologist variance across all practices and practice models should be cause for more concern, she added.
Sailesh Konda, MD, has been an outspoken critic. Dr. Konda, medical director and clinical assistant professor in the department of dermatology at the University of Florida, Gainesville, and colleagues detailed the complicated financial machinations of private equity in the Journal of the American Academy of Dermatology. They showed that private investors seemed to hone in on buying outlier practices that performed high numbers of procedures. The paper – first made public in the fall of 2018 – created an uproar, especially among private equity companies. It was initially removed from the website in conjunction with a request from the editor that its conclusions be altered to be less harsh on private equity, according to the New York Times. The paper was eventually published in 2019 (J Am Acad Dermatol. Jul;81[1]:287-296.e8).
Dr. Konda has spoken at various dermatology forums and health care gatherings on private equity. He told the Times that he had given 16 talks to health care groups in 2018, and he was due to speak to a health care investors’ group in 2020. But he would not comment on the record for this story.
Brett Coldiron, MD, a former president of the AAD, also has been critical. He believes investor-owners push for more biopsies, freezing of actinic keratoses, Moh’s surgery, and other well-paying procedures. “I’m convinced that private equity may be the undoing of our specialty,” Dr. Coldiron said in an interview.
In a paper titled, “Private Equity Acquisition of Physician Practices,” published in the Annals of Internal Medicine in January 2019, Lawrence Casalino, MD, PhD, chief of the division of health policy and economics at New York’s Weill Cornell Medicine, and colleagues wrote that “private equity firms focus on specialties with high potential for additional income from elective procedures and ancillary services,” and that “dermatology has been a major focus” (Ann Intern Med. 2019;170[2]:114-5).
And in a viewpoint published in JAMA in February 2019, first-year medical student Suhas Gondi and Zirui Song, MD, PhD, both of Harvard Medical School, Boston, concluded that investor-owned practices could drive up overall health spending in part because they extract better reimbursement from insurers (JAMA. 2019;321[11]:1047-8).
Access could also become an issue if the companies drive smaller independent practices out of business, they wrote.
On the other hand, they said, “these investments may also benefit patients and bring more efficiency to a system burdened with waste.” The authors called for more research and “thoughtful regulation” to enhance the potential positives while mitigating the negatives.
So far, the acquisitions have largely escaped the notice of regulators or lawmakers. Congress has made noises about targeting specialty practices owned by private equity as a means of taming surprise medical bills, but that legislation has been stymied.
Dr. Coldiron is convinced that private investors will eventually be tripped up by state laws that prohibit the corporate practice of medicine.
Leslie Baumann, MD, who sold her Miami practice in October 2019 to the investor-owned Skin and Cancer Associates, said critics are too cynical. “What if these private equity firms are going to actually make our specialty better?” she asked in an interview.
What makes dermatology attractive?
Private equity has been acquiring specialty practices since at least 2009, with an acceleration over the last 5 years. Dermatology has been a frequent target, in part because so many dermatologists were in independent or small group private practices, making them ripe for takeover.
A 2015 report on the specialty by Cegedim, a company that provides information technology support to health care, found that the majority of practices had fewer than five physicians and that 57% of the practices were independent.
But more dermatologists are choosing employment. In a 2018 Medscape survey, 57% of dermatologists reported they were employed, while 49% were self-employed.
During 2013-2016, investors bought 35 dermatology practices – comprising 334 physicians, according to one study published in February (JAMA. 2020;323[7]:663-5). Investors bought 69 anesthesiology practices, 43 emergency medicine practices, and 39 family medicine practices during the same period.
Harvard’s Mr. Gondi and Dr. Song estimated that dermatology practices accounted for 15% of investor purchases in 2015 and 2016, even though dermatologists make up just 1% of U.S. clinicians.
In another paper published in JAMA Dermatology, Sally Tan, MD, and colleagues at Brigham and Women’s Hospital, Boston, and Harvard medical and business schools, estimated that, in 2019, at least 184 practices, comprising 381 clinics, were owned by 17 private equity groups and that the acquisitions had been accelerating: from 5 in 2012 to 59 in 2017 to 34 in the first 5 months of 2018 (JAMA Dermatol. 2019;155[9]:1013-21).
“It’s a very attractive area for investors because they know that the future is bright for dermatology,” said Reuven Porges, MD, CEO of Ft. Lauderdale-based Skin and Cancer Associates, which is owned by a private investor. Because dermatology involves providing many ancillary services and cash-only cosmetic services, “it has tremendous potential to continue to be successful in the future regardless of what health care changes are coming,” Dr. Porges said in an interview.
Investors also see promise in dermatology in the United States because “there’s a huge supply demand mismatch,” said Vance Vanier, MD, a cofounding managing partner at Chicago Pacific Founders, the private equity owner of Pinnacle Dermatology, which has 52 locations in Illinois, Indiana, Michigan, Minnesota, and Tennessee.
Theoretically, when investors handle billing, insurance negotiations, and health information technology, it gives clinicians more time to practice, Dr. Vanier said in an interview.
“Once that doctor is freed up to not do administrative tasks and focus on patient care, then, if they want to, they can see more patients and be more responsive to their needs,” he said.
Dr. Vanier said investor acquisitions are here to stay. “This is a trend that could go on for another 50 years before any saturation point is hit,” he said. “It’s a $2 trillion market. It’s hard to wrap your head around how enormous health care services is,” he said.
Dermatology acquisitions will be driven by the continuing imbalance of physician supply and patient demand; the financial pressure on newly graduating physicians who have big debt loads; the requirements for investment in health information technology to report quality metrics; and an aging population, Dr. Vanier said.
In a JAMA Dermatology viewpoint, Jack Resneck Jr., MD, professor of dermatology, University of California, San Francisco, listed many of the same factors – plus a skin cancer epidemic – as fueling dermatology acquisitions (JAMA Dermatol. 2018;154[1]:13-4).
Medical practices – not just dermatology practices – also offer a pure financial play. “Acquisitions of smaller practices provide a major arbitrage opportunity,” Dr. Casalino and colleagues said in the January 2019 Annals of Internal Medicine paper. In a merger of smaller practices into larger, the smaller practice’s valuation immediately becomes that of the bigger one, they wrote.
Could the bottom fall out?
Creating giant groups through consolidation is a main aim for private equity.
Skin and Cancer Associates, founded in 1971, was a large entity, with 25 practices. But for a long time, its leaders had wanted to become a regional or a national player, said Dr. Porges. Those leaders asked Dr. Porges – who helped take his former radiology practice through a private equity purchase – to help them attract investors. In March 2018, Susquehanna Private Capital signed on as a “partner” with Skin and Cancer Associates.
It has since almost doubled in size, with 40 locations and 60 dermatologists, all in Florida, Dr. Porges said. “The only limiting factor for growing it as fast as we want, is really money,” he said.
Consolidation is just an initial step. Most investors have a finite timeline for cashing out. “The ultimate goal is often to realize a profitable secondary sale in three to seven years to another PE investor (or even a publicly traded entity),” Dr. Resneck wrote in the 2018 JAMA Dermatology paper.
Not all private equity companies are the same, said Dr. Wernli, of Forefront. Dermatologists can investigate a company’s “hold period” – how long they keep an investment before trading – and the strength of its capitalization before deciding to sell, she said.
Since 2016, Forefront has been owned by the Ontario Municipal Employee Retirement System (OMERS), a pension fund for the province’s public workers. OMERS bought Forefront from Varsity Healthcare Partners, which had owned the dermatology group for just 2 years.
Dr. Wernli said OMERS is a good, solid investor. “They have unlimited resources to invest so they don’t have to quickly flip a company to satisfy an investment in another company,” she said.
Some investor-backed dermatology practices have gone belly up. In 2012, WestWind Investors bought DermOne, based in Toms River, N.J. But by early 2018, the business had fallen apart, and some practices – in North Carolina, New Jersey, Texas, and Virginia – just shut their doors.
Long Island City, N.Y.–based Schweiger Dermatology Group, backed by private equity, snapped up nine of the New Jersey DermOne practices in March 2018.
Another private equity–backed company, U.S. Dermatology Partners, defaulted on a $377 million loan in January 2020. As reported by Bloomberg, the company had $340 million in revenue in 2018. U.S. Dermatology’s owners are reportedly working out a recapitalization or debt-for-equity swap with the lenders.
Dr. Wernli said that financial problems aren’t unique to investor-owned practices and that doctors could still be out of a job if a private practice goes under.
“A private practice can also default on their loans that they’ve used to fund their own personal practice, leaving employed physicians in the same situation,” she said.
Patients are likely to be in the dark, however, until the doors close.
Pressure on practices
Private equity is changing the shape of practice for both those who work for investor-owned businesses and those still out on their own.
The Alabama dermatologist, for instance, said it has made it harder for him to recruit new doctors, who are offered big signing bonuses and a steady income by the investor-owned practices. “They’re skewing the numbers,” he said, adding that residents are now expecting a big payment and benefits.
Dr. Baumann said that when she was on her own, she had trouble finding and recruiting good dermatologists. But it has become easier since she’d sold to Skin and Cancer Associates, she said, noting that Dr. Porges recently found a qualified candidate for her to interview a week after she put in a request.
Another dermatologist in a Midwestern metropolitan practice – who did not want his name used – said that when it came time for him to increase his equity stake, his older partner, who was near retirement and had explored selling to private equity – wanted four-and-a-half times the price that had been discussed when he joined the practice.
The younger partner believes the private equity offers inflated the practice’s valuation in his partner’s mind. He ended up leaving the practice.
Many dermatologists have been led to believe that their practices are worth more than they might be, according to Dr. Coldiron. “I think a lot of these doctors that sell out are deluded. They think that they’re getting a lot of money and they’re not,” he said.
Typically, investors may offer three or four times earnings before interest, taxes, depreciation and amortization (EBITDA). The money paid out is taxed at the capital gains rate, which provides some savings. “But you have to pay that all back, because when they sign you up, you become an employee,” Dr. Coldiron said.
Doctors often agree to work for 5 years, but during that period, their base salary is decreased while the buyout cash is meted out to them, he added. A chunk of the buyout usually is also given as equity, but that equity is worthless unless the investor sells to another entity.
Pinnacle Dermatology doesn’t want doctors to retire immediately upon an acquisition, said Dr. Vanier of Chicago Pacific Founders. “We want to find physician partners who want to keep working,” he said. “We strongly believe if you don’t have strong physician leadership, experienced physician leadership, that your odds of success go down.”
Chicago Pacific also believes physicians should have an ownership interest, he said. It allows them to share in the eventual financial rewards – whether that’s 5 or 20 years later, said Dr. Vanier.
Dr. Coldiron sees other pressures that skew practice styles and can harm patient care. Clinicians in investor-owned practices are often urged to refer all dermatopathology to labs owned by the practice and often, a Moh’s surgeon is employed to service all the practices – sometimes even being flown in from elsewhere, he claimed.
That takes away the clinician’s autonomy in terms of referring where he or she feels appropriate and also could harm pathologists and Moh’s surgeons that depend on those referral streams, he added.
In their paper, Mr. Gondi and Dr. Song wrote that this practice is concerning because “keeping referrals within the practice may render referral patterns less responsive to patient needs or preference.”
Procedure factories?
Many critics say investor-backed practices are goosing revenues by hiring more mid-level providers – such as nurse practitioners and physician assistants – and getting them to perform more procedures.
Midlevel practitioners do more biopsies than dermatologists do to get a diagnosis, according to Dr. Coldiron.
A 2018 JAMA Dermatology study appears to back that up. Physician assistants needed to conduct 3.9 biopsies to diagnose one skin cancer, compared to 3.3 for dermatologists. For a single melanoma, the number needed to biopsy was 39.4 for PAs and 25.4 for dermatologists (JAMA Dermatol. 2018;154[5]:569-73).
Skin biopsies have almost doubled in the last decade, said Dr. Coldiron. “The skin cancer epidemic would account for only half of that,” he said.
“The ultimate loser is the patient – because the patient doesn’t get the highest quality care and the patient has unnecessary things done to him or her,” he said. But, he said, he could not directly tie the biopsy increase to the rise of private equity.
Forefront tracks the number of biopsies per patient done by every dermatologist in its network – to make sure that no one is outside the norms set by the Centers for Medicare and Medicaid Services, said Dr. Wernli. And she said biopsies declined after the group was bought by private equity.
Dr. Baumann said the average number of biopsies per patient at Skin and Cancer Associates in 2019 was 0.20 – less than the 0.30 average reported by Medicare that same year.
The rising use of mid-level providers existed long before private equity came on the scene, said Dr. Wernli. “There’s not enough board-certified dermatologists to satisfy need,” she said, noting that, in addition, many clinicians won’t serve rural areas. “If we don’t move and extend ourselves, there will be someone who fills our shoes,” she said, adding that Forefront has 1 mid-level for every 1.5 to 2 dermatologists.
Skin and Cancer Associates has 55 doctors and 29 physician assistants, said Dr. Baumann, adding that she had not been pressured to add any mid-level providers to her practice.
Excitement about sale shot down
Dr. Wernli and Dr. Baumann both have been happy with their decision to ally with private equity. For Dr. Baumann, however, her move was tinged by online attacks that reflected the strong opinions on the topic.
She began looking into selling her practice when one of her businesses – Skin Type Solutions – began taking off. Both her clinical practice and research business were thriving. She had two children at home and was having a hard time keeping up with the administrative end of her businesses.
None of her partners nor any groups in Miami showed interest in purchasing the practice, so she began researching private equity. She spoke with seven companies before settling on Skin and Cancer Associates. They had “a long track record of successfully running practices,” said Dr. Baumann, adding that “the doctors who work there are happy, and I respect the quality of the physicians and the organization.”
When she closed the deal in October 2019, she agreed to stay on for 5 years and signed a noncompete clause that she deems “very reasonable.” Among the perks she cites: being able to consult via telemedicine with an expert on pigmented lesions; quick and easy referrals to a Moh’s surgeon; being able to train residents; and having paid personal time off.
It’s less responsibility and the same or better job satisfaction, she said.
But when she shared the news on a private Facebook group for board-certified dermatologists, she was vilified. Of some 195 comments, about half were “mean,” said Dr. Baumann.
“I was shocked about how strongly everybody feels,” she said. Those commenting accused her of doing it for the money or said that her move was contributing to the ruination of dermatology.
“I just defended myself,” she said. “For me, it was my time.”
Dr. Coldiron and Dr. Baumann are members of the Dermatology News editorial advisory board.
The dermatologist had been in practice just a few years when he was approached by a private equity group. This was around 2015, when dermatology was just starting to buzz about investor buyouts. He was curious, so he agreed to meet with the company.
“They approached me with the idea that they could help me grow my practice, help my patients, and cut down overhead,” said the northern Alabama dermatologist, who asked that his name not be used. Over a lavish dinner, the investors lauded the clinician for his business acumen and for having built a great practice so quickly. They made an enticing buyout offer.
Before agreeing, he thought it over. He told the investors he wanted a few more years on his own before he’d consider a buyout. They encouraged him to think about it some more. He did, but the answer was still no.
Suddenly, the investors became aggressive and threatening. “They told me, ‘you have just made the biggest mistake of your early career. We’re going to make sure that our practice swallows you up, and if we can’t take you over and put you out of business, we’re going to buy up everyone around you so you can’t survive,’ ” said the dermatologist.
Surprisingly, the experience did not sour him on private equity – he even entertained a successor company’s offer. But he’s become more circumspect. “It has the potential to do good,” he said, adding that such financial support could help him pay employees, keep the lights on, and improve care. But the investors’ emphasis on profit is not appealing, he said.
“I’m going to have to have good proof that it’s truly going to improve patient care and outcomes. And I haven’t seen that yet,” he said.
Salvation or death sentence?
Depending on whom you ask, the continuing growth of private equity purchases of dermatology practices is either the death – or salvation – of the specialty.
Many dermatologists question whether the financial backers will invest in quality of care, or if they just will hire mid-level providers to churn out procedures to plump up revenues.
Neither the controversy nor the acquisitions show any sign of abating.
The American Academy of Dermatology has hosted debates on the topic at its annual meetings – and was to do so in 2020 until COVID-19 led to the meeting’s cancellation. AAD has not weighed in with any official policy and is not releasing data it may be collecting on the potential impact of private equity ownership. The organization provided a statement from President George J. Hruza, MD, who said, “the AAD supports a member’s right to choose the model that works best for them,” adding that the Academy “expects its members to provide safe and effective patient care, regardless of a dermatologist’s practice setting.” Dr. Hruza sold his Chesterfield, Mo., practice to United Skin Specialists, a private equity–backed company, in 2016, and still works at the same practice.
Some have said the acquisitions need to stop. “Until meaningful data are available on what happens to the quality of care and affordability for patients and payers, dermatologists should stop selling their practices to private equity firms, and legislators should prohibit such transactions,” wrote Joshua M. Sharfstein, MD, and Jamar Slocum, MD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, in an editorial in July (JAMA Dermatol. 2019;155[9]:1007-8).
Although he acknowledged that he has not tracked the issue closely and that little data exist on the impact on quality or cost, Dr. Sharfstein has not changed his tune. “I think there are enough warning signs to say we should put the brakes on,” he said in an interview.
“For what reason?” asked Betsy Wernli, MD, president of Forefront Dermatology, an investor-owned group based in Manitowoc, Wis. She said it seems that “on this topic, we abandon our scientific foundations and default to emotion and anecdote,” she said in an interview. “Having capital, and an investor that supports us has allowed us to perform better patient care,” she said. Dermatologist variance across all practices and practice models should be cause for more concern, she added.
Sailesh Konda, MD, has been an outspoken critic. Dr. Konda, medical director and clinical assistant professor in the department of dermatology at the University of Florida, Gainesville, and colleagues detailed the complicated financial machinations of private equity in the Journal of the American Academy of Dermatology. They showed that private investors seemed to hone in on buying outlier practices that performed high numbers of procedures. The paper – first made public in the fall of 2018 – created an uproar, especially among private equity companies. It was initially removed from the website in conjunction with a request from the editor that its conclusions be altered to be less harsh on private equity, according to the New York Times. The paper was eventually published in 2019 (J Am Acad Dermatol. Jul;81[1]:287-296.e8).
Dr. Konda has spoken at various dermatology forums and health care gatherings on private equity. He told the Times that he had given 16 talks to health care groups in 2018, and he was due to speak to a health care investors’ group in 2020. But he would not comment on the record for this story.
Brett Coldiron, MD, a former president of the AAD, also has been critical. He believes investor-owners push for more biopsies, freezing of actinic keratoses, Moh’s surgery, and other well-paying procedures. “I’m convinced that private equity may be the undoing of our specialty,” Dr. Coldiron said in an interview.
In a paper titled, “Private Equity Acquisition of Physician Practices,” published in the Annals of Internal Medicine in January 2019, Lawrence Casalino, MD, PhD, chief of the division of health policy and economics at New York’s Weill Cornell Medicine, and colleagues wrote that “private equity firms focus on specialties with high potential for additional income from elective procedures and ancillary services,” and that “dermatology has been a major focus” (Ann Intern Med. 2019;170[2]:114-5).
And in a viewpoint published in JAMA in February 2019, first-year medical student Suhas Gondi and Zirui Song, MD, PhD, both of Harvard Medical School, Boston, concluded that investor-owned practices could drive up overall health spending in part because they extract better reimbursement from insurers (JAMA. 2019;321[11]:1047-8).
Access could also become an issue if the companies drive smaller independent practices out of business, they wrote.
On the other hand, they said, “these investments may also benefit patients and bring more efficiency to a system burdened with waste.” The authors called for more research and “thoughtful regulation” to enhance the potential positives while mitigating the negatives.
So far, the acquisitions have largely escaped the notice of regulators or lawmakers. Congress has made noises about targeting specialty practices owned by private equity as a means of taming surprise medical bills, but that legislation has been stymied.
Dr. Coldiron is convinced that private investors will eventually be tripped up by state laws that prohibit the corporate practice of medicine.
Leslie Baumann, MD, who sold her Miami practice in October 2019 to the investor-owned Skin and Cancer Associates, said critics are too cynical. “What if these private equity firms are going to actually make our specialty better?” she asked in an interview.
What makes dermatology attractive?
Private equity has been acquiring specialty practices since at least 2009, with an acceleration over the last 5 years. Dermatology has been a frequent target, in part because so many dermatologists were in independent or small group private practices, making them ripe for takeover.
A 2015 report on the specialty by Cegedim, a company that provides information technology support to health care, found that the majority of practices had fewer than five physicians and that 57% of the practices were independent.
But more dermatologists are choosing employment. In a 2018 Medscape survey, 57% of dermatologists reported they were employed, while 49% were self-employed.
During 2013-2016, investors bought 35 dermatology practices – comprising 334 physicians, according to one study published in February (JAMA. 2020;323[7]:663-5). Investors bought 69 anesthesiology practices, 43 emergency medicine practices, and 39 family medicine practices during the same period.
Harvard’s Mr. Gondi and Dr. Song estimated that dermatology practices accounted for 15% of investor purchases in 2015 and 2016, even though dermatologists make up just 1% of U.S. clinicians.
In another paper published in JAMA Dermatology, Sally Tan, MD, and colleagues at Brigham and Women’s Hospital, Boston, and Harvard medical and business schools, estimated that, in 2019, at least 184 practices, comprising 381 clinics, were owned by 17 private equity groups and that the acquisitions had been accelerating: from 5 in 2012 to 59 in 2017 to 34 in the first 5 months of 2018 (JAMA Dermatol. 2019;155[9]:1013-21).
“It’s a very attractive area for investors because they know that the future is bright for dermatology,” said Reuven Porges, MD, CEO of Ft. Lauderdale-based Skin and Cancer Associates, which is owned by a private investor. Because dermatology involves providing many ancillary services and cash-only cosmetic services, “it has tremendous potential to continue to be successful in the future regardless of what health care changes are coming,” Dr. Porges said in an interview.
Investors also see promise in dermatology in the United States because “there’s a huge supply demand mismatch,” said Vance Vanier, MD, a cofounding managing partner at Chicago Pacific Founders, the private equity owner of Pinnacle Dermatology, which has 52 locations in Illinois, Indiana, Michigan, Minnesota, and Tennessee.
Theoretically, when investors handle billing, insurance negotiations, and health information technology, it gives clinicians more time to practice, Dr. Vanier said in an interview.
“Once that doctor is freed up to not do administrative tasks and focus on patient care, then, if they want to, they can see more patients and be more responsive to their needs,” he said.
Dr. Vanier said investor acquisitions are here to stay. “This is a trend that could go on for another 50 years before any saturation point is hit,” he said. “It’s a $2 trillion market. It’s hard to wrap your head around how enormous health care services is,” he said.
Dermatology acquisitions will be driven by the continuing imbalance of physician supply and patient demand; the financial pressure on newly graduating physicians who have big debt loads; the requirements for investment in health information technology to report quality metrics; and an aging population, Dr. Vanier said.
In a JAMA Dermatology viewpoint, Jack Resneck Jr., MD, professor of dermatology, University of California, San Francisco, listed many of the same factors – plus a skin cancer epidemic – as fueling dermatology acquisitions (JAMA Dermatol. 2018;154[1]:13-4).
Medical practices – not just dermatology practices – also offer a pure financial play. “Acquisitions of smaller practices provide a major arbitrage opportunity,” Dr. Casalino and colleagues said in the January 2019 Annals of Internal Medicine paper. In a merger of smaller practices into larger, the smaller practice’s valuation immediately becomes that of the bigger one, they wrote.
Could the bottom fall out?
Creating giant groups through consolidation is a main aim for private equity.
Skin and Cancer Associates, founded in 1971, was a large entity, with 25 practices. But for a long time, its leaders had wanted to become a regional or a national player, said Dr. Porges. Those leaders asked Dr. Porges – who helped take his former radiology practice through a private equity purchase – to help them attract investors. In March 2018, Susquehanna Private Capital signed on as a “partner” with Skin and Cancer Associates.
It has since almost doubled in size, with 40 locations and 60 dermatologists, all in Florida, Dr. Porges said. “The only limiting factor for growing it as fast as we want, is really money,” he said.
Consolidation is just an initial step. Most investors have a finite timeline for cashing out. “The ultimate goal is often to realize a profitable secondary sale in three to seven years to another PE investor (or even a publicly traded entity),” Dr. Resneck wrote in the 2018 JAMA Dermatology paper.
Not all private equity companies are the same, said Dr. Wernli, of Forefront. Dermatologists can investigate a company’s “hold period” – how long they keep an investment before trading – and the strength of its capitalization before deciding to sell, she said.
Since 2016, Forefront has been owned by the Ontario Municipal Employee Retirement System (OMERS), a pension fund for the province’s public workers. OMERS bought Forefront from Varsity Healthcare Partners, which had owned the dermatology group for just 2 years.
Dr. Wernli said OMERS is a good, solid investor. “They have unlimited resources to invest so they don’t have to quickly flip a company to satisfy an investment in another company,” she said.
Some investor-backed dermatology practices have gone belly up. In 2012, WestWind Investors bought DermOne, based in Toms River, N.J. But by early 2018, the business had fallen apart, and some practices – in North Carolina, New Jersey, Texas, and Virginia – just shut their doors.
Long Island City, N.Y.–based Schweiger Dermatology Group, backed by private equity, snapped up nine of the New Jersey DermOne practices in March 2018.
Another private equity–backed company, U.S. Dermatology Partners, defaulted on a $377 million loan in January 2020. As reported by Bloomberg, the company had $340 million in revenue in 2018. U.S. Dermatology’s owners are reportedly working out a recapitalization or debt-for-equity swap with the lenders.
Dr. Wernli said that financial problems aren’t unique to investor-owned practices and that doctors could still be out of a job if a private practice goes under.
“A private practice can also default on their loans that they’ve used to fund their own personal practice, leaving employed physicians in the same situation,” she said.
Patients are likely to be in the dark, however, until the doors close.
Pressure on practices
Private equity is changing the shape of practice for both those who work for investor-owned businesses and those still out on their own.
The Alabama dermatologist, for instance, said it has made it harder for him to recruit new doctors, who are offered big signing bonuses and a steady income by the investor-owned practices. “They’re skewing the numbers,” he said, adding that residents are now expecting a big payment and benefits.
Dr. Baumann said that when she was on her own, she had trouble finding and recruiting good dermatologists. But it has become easier since she’d sold to Skin and Cancer Associates, she said, noting that Dr. Porges recently found a qualified candidate for her to interview a week after she put in a request.
Another dermatologist in a Midwestern metropolitan practice – who did not want his name used – said that when it came time for him to increase his equity stake, his older partner, who was near retirement and had explored selling to private equity – wanted four-and-a-half times the price that had been discussed when he joined the practice.
The younger partner believes the private equity offers inflated the practice’s valuation in his partner’s mind. He ended up leaving the practice.
Many dermatologists have been led to believe that their practices are worth more than they might be, according to Dr. Coldiron. “I think a lot of these doctors that sell out are deluded. They think that they’re getting a lot of money and they’re not,” he said.
Typically, investors may offer three or four times earnings before interest, taxes, depreciation and amortization (EBITDA). The money paid out is taxed at the capital gains rate, which provides some savings. “But you have to pay that all back, because when they sign you up, you become an employee,” Dr. Coldiron said.
Doctors often agree to work for 5 years, but during that period, their base salary is decreased while the buyout cash is meted out to them, he added. A chunk of the buyout usually is also given as equity, but that equity is worthless unless the investor sells to another entity.
Pinnacle Dermatology doesn’t want doctors to retire immediately upon an acquisition, said Dr. Vanier of Chicago Pacific Founders. “We want to find physician partners who want to keep working,” he said. “We strongly believe if you don’t have strong physician leadership, experienced physician leadership, that your odds of success go down.”
Chicago Pacific also believes physicians should have an ownership interest, he said. It allows them to share in the eventual financial rewards – whether that’s 5 or 20 years later, said Dr. Vanier.
Dr. Coldiron sees other pressures that skew practice styles and can harm patient care. Clinicians in investor-owned practices are often urged to refer all dermatopathology to labs owned by the practice and often, a Moh’s surgeon is employed to service all the practices – sometimes even being flown in from elsewhere, he claimed.
That takes away the clinician’s autonomy in terms of referring where he or she feels appropriate and also could harm pathologists and Moh’s surgeons that depend on those referral streams, he added.
In their paper, Mr. Gondi and Dr. Song wrote that this practice is concerning because “keeping referrals within the practice may render referral patterns less responsive to patient needs or preference.”
Procedure factories?
Many critics say investor-backed practices are goosing revenues by hiring more mid-level providers – such as nurse practitioners and physician assistants – and getting them to perform more procedures.
Midlevel practitioners do more biopsies than dermatologists do to get a diagnosis, according to Dr. Coldiron.
A 2018 JAMA Dermatology study appears to back that up. Physician assistants needed to conduct 3.9 biopsies to diagnose one skin cancer, compared to 3.3 for dermatologists. For a single melanoma, the number needed to biopsy was 39.4 for PAs and 25.4 for dermatologists (JAMA Dermatol. 2018;154[5]:569-73).
Skin biopsies have almost doubled in the last decade, said Dr. Coldiron. “The skin cancer epidemic would account for only half of that,” he said.
“The ultimate loser is the patient – because the patient doesn’t get the highest quality care and the patient has unnecessary things done to him or her,” he said. But, he said, he could not directly tie the biopsy increase to the rise of private equity.
Forefront tracks the number of biopsies per patient done by every dermatologist in its network – to make sure that no one is outside the norms set by the Centers for Medicare and Medicaid Services, said Dr. Wernli. And she said biopsies declined after the group was bought by private equity.
Dr. Baumann said the average number of biopsies per patient at Skin and Cancer Associates in 2019 was 0.20 – less than the 0.30 average reported by Medicare that same year.
The rising use of mid-level providers existed long before private equity came on the scene, said Dr. Wernli. “There’s not enough board-certified dermatologists to satisfy need,” she said, noting that, in addition, many clinicians won’t serve rural areas. “If we don’t move and extend ourselves, there will be someone who fills our shoes,” she said, adding that Forefront has 1 mid-level for every 1.5 to 2 dermatologists.
Skin and Cancer Associates has 55 doctors and 29 physician assistants, said Dr. Baumann, adding that she had not been pressured to add any mid-level providers to her practice.
Excitement about sale shot down
Dr. Wernli and Dr. Baumann both have been happy with their decision to ally with private equity. For Dr. Baumann, however, her move was tinged by online attacks that reflected the strong opinions on the topic.
She began looking into selling her practice when one of her businesses – Skin Type Solutions – began taking off. Both her clinical practice and research business were thriving. She had two children at home and was having a hard time keeping up with the administrative end of her businesses.
None of her partners nor any groups in Miami showed interest in purchasing the practice, so she began researching private equity. She spoke with seven companies before settling on Skin and Cancer Associates. They had “a long track record of successfully running practices,” said Dr. Baumann, adding that “the doctors who work there are happy, and I respect the quality of the physicians and the organization.”
When she closed the deal in October 2019, she agreed to stay on for 5 years and signed a noncompete clause that she deems “very reasonable.” Among the perks she cites: being able to consult via telemedicine with an expert on pigmented lesions; quick and easy referrals to a Moh’s surgeon; being able to train residents; and having paid personal time off.
It’s less responsibility and the same or better job satisfaction, she said.
But when she shared the news on a private Facebook group for board-certified dermatologists, she was vilified. Of some 195 comments, about half were “mean,” said Dr. Baumann.
“I was shocked about how strongly everybody feels,” she said. Those commenting accused her of doing it for the money or said that her move was contributing to the ruination of dermatology.
“I just defended myself,” she said. “For me, it was my time.”
Dr. Coldiron and Dr. Baumann are members of the Dermatology News editorial advisory board.
Combo therapy with melflufen promising in small r/r multiple myeloma study
Small phase 1 and phase 2 multi-center, open label studies of melflufen toxicity and efficacy in combination with dexamethasone showed significant benefits in overall response rate in patients with relapsed/refractory multiple myeloma. A report on these studies was published in Lancet Hematology.
The studies enrolled patients aged 18 years and older with relapsed/refractory multiple myeloma (MM), who had received two or more previous lines of therapy and were refractory to their last line of therapy. All patients had an Eastern Cooperative Oncology Group performance status of 2 or less.
Phase 1 was a dose-tolerance study of 23 patients, which found that the maximum tolerated dose tested of intravenous infusion of melflufen was 40 mg for 30 min on day 1 in 21-day cycles plus oral dexamethasone at 40 mg weekly.
In phase 2, 45 patients were tested at the maximum tolerated dose (40 mg) identified in phase 1 in combination with dexamethasone and 13 patients were treated with melflufen as a single agent (ClinicalTrials.gov, NCT01897714). The single-agent arm of the study was discontinued for ethical reasons once evidence became available of the benefit of combination therapy in comparison.
In phase 2, patients treated with combination therapy achieved an overall response rate of 31% (14/45 patients) and a clinical benefit rate of 49% (22/45 patients). In the phase 2 single-agent cohort, the overall response rate was 8% (1/13 patients) and the clinical benefit rate was 23% (3/13 patients) before this aspect of the study was discontinued.
In terms of adverse events, among the 45 phase 2 combination–treatment patients, the most common grade 3-4 adverse events were clinically manageable thrombocytopenia (62% of patients) and neutropenia (58%) In addition, 24 serious adverse events were reported in 38% patients, most commonly pneumonia (11%).
Because of the benefits seen and the need for relapsed/refractory MM treatments, further studies on melflufen in combination therapies are ongoing, according to the researchers “with encouraging early results to date”: NCT03151811, NCT02963493, and NCT03481556.
“Melflufen represents a novel treatment concept with a unique mechanism of action that might find future use in combinations with key partners, such as proteasome inhibitors and monoclonal antibodies,” the researchers concluded.
The study was sponsored by Oncopeptides AB. The authors received funding from a variety of pharmaceutical companies.
SOURCE: Richardson PG et al. Lancet Hematol. 2020; doi.org/10.1016/S2352-3026(20)30044-2.
Small phase 1 and phase 2 multi-center, open label studies of melflufen toxicity and efficacy in combination with dexamethasone showed significant benefits in overall response rate in patients with relapsed/refractory multiple myeloma. A report on these studies was published in Lancet Hematology.
The studies enrolled patients aged 18 years and older with relapsed/refractory multiple myeloma (MM), who had received two or more previous lines of therapy and were refractory to their last line of therapy. All patients had an Eastern Cooperative Oncology Group performance status of 2 or less.
Phase 1 was a dose-tolerance study of 23 patients, which found that the maximum tolerated dose tested of intravenous infusion of melflufen was 40 mg for 30 min on day 1 in 21-day cycles plus oral dexamethasone at 40 mg weekly.
In phase 2, 45 patients were tested at the maximum tolerated dose (40 mg) identified in phase 1 in combination with dexamethasone and 13 patients were treated with melflufen as a single agent (ClinicalTrials.gov, NCT01897714). The single-agent arm of the study was discontinued for ethical reasons once evidence became available of the benefit of combination therapy in comparison.
In phase 2, patients treated with combination therapy achieved an overall response rate of 31% (14/45 patients) and a clinical benefit rate of 49% (22/45 patients). In the phase 2 single-agent cohort, the overall response rate was 8% (1/13 patients) and the clinical benefit rate was 23% (3/13 patients) before this aspect of the study was discontinued.
In terms of adverse events, among the 45 phase 2 combination–treatment patients, the most common grade 3-4 adverse events were clinically manageable thrombocytopenia (62% of patients) and neutropenia (58%) In addition, 24 serious adverse events were reported in 38% patients, most commonly pneumonia (11%).
Because of the benefits seen and the need for relapsed/refractory MM treatments, further studies on melflufen in combination therapies are ongoing, according to the researchers “with encouraging early results to date”: NCT03151811, NCT02963493, and NCT03481556.
“Melflufen represents a novel treatment concept with a unique mechanism of action that might find future use in combinations with key partners, such as proteasome inhibitors and monoclonal antibodies,” the researchers concluded.
The study was sponsored by Oncopeptides AB. The authors received funding from a variety of pharmaceutical companies.
SOURCE: Richardson PG et al. Lancet Hematol. 2020; doi.org/10.1016/S2352-3026(20)30044-2.
Small phase 1 and phase 2 multi-center, open label studies of melflufen toxicity and efficacy in combination with dexamethasone showed significant benefits in overall response rate in patients with relapsed/refractory multiple myeloma. A report on these studies was published in Lancet Hematology.
The studies enrolled patients aged 18 years and older with relapsed/refractory multiple myeloma (MM), who had received two or more previous lines of therapy and were refractory to their last line of therapy. All patients had an Eastern Cooperative Oncology Group performance status of 2 or less.
Phase 1 was a dose-tolerance study of 23 patients, which found that the maximum tolerated dose tested of intravenous infusion of melflufen was 40 mg for 30 min on day 1 in 21-day cycles plus oral dexamethasone at 40 mg weekly.
In phase 2, 45 patients were tested at the maximum tolerated dose (40 mg) identified in phase 1 in combination with dexamethasone and 13 patients were treated with melflufen as a single agent (ClinicalTrials.gov, NCT01897714). The single-agent arm of the study was discontinued for ethical reasons once evidence became available of the benefit of combination therapy in comparison.
In phase 2, patients treated with combination therapy achieved an overall response rate of 31% (14/45 patients) and a clinical benefit rate of 49% (22/45 patients). In the phase 2 single-agent cohort, the overall response rate was 8% (1/13 patients) and the clinical benefit rate was 23% (3/13 patients) before this aspect of the study was discontinued.
In terms of adverse events, among the 45 phase 2 combination–treatment patients, the most common grade 3-4 adverse events were clinically manageable thrombocytopenia (62% of patients) and neutropenia (58%) In addition, 24 serious adverse events were reported in 38% patients, most commonly pneumonia (11%).
Because of the benefits seen and the need for relapsed/refractory MM treatments, further studies on melflufen in combination therapies are ongoing, according to the researchers “with encouraging early results to date”: NCT03151811, NCT02963493, and NCT03481556.
“Melflufen represents a novel treatment concept with a unique mechanism of action that might find future use in combinations with key partners, such as proteasome inhibitors and monoclonal antibodies,” the researchers concluded.
The study was sponsored by Oncopeptides AB. The authors received funding from a variety of pharmaceutical companies.
SOURCE: Richardson PG et al. Lancet Hematol. 2020; doi.org/10.1016/S2352-3026(20)30044-2.
FROM THE LANCET HEMATOLOGY
Financial incentives affect the adoption of biosimilars
during the same time period in 2015-2019, according to an analysis published in Arthritis and Rheumatology.
The use of the biosimilars also was associated with cost savings at the VAMC, but not at the academic medical center, which illustrates that insufficient financial incentives can delay the adoption of biosimilars and the health care system’s realization of cost savings, according to the authors.
Medicare, which is not allowed to negotiate drug prices, is one of the largest payers for infused therapies. Medicare reimbursement for infused therapies is based on the latter’s average selling price (ASP) during the previous quarter. Institutions may negotiate purchase prices with drug manufacturers and receive Medicare reimbursement. Biosimilars generally have lower ASPs than their corresponding reference therapies, and biosimilar manufacturers may have less room to negotiate prices than reference therapy manufacturers. Consequently, a given institution might have a greater incentive to use reference products than to use biosimilars.
An examination of pharmacy data
The VA negotiates drug prices for all of its medical centers and has mandated that clinicians prefer biosimilars to their corresponding reference therapies, so Joshua F. Baker, MD, of the University of Pennsylvania and the Corporal Michael J. Crescenz VAMC, both in Philadelphia, and his colleagues hypothesized that the adoption of biosimilars had proceeded more quickly at a VAMC than at a nearby academic medical center.
The investigators examined pharmacy data from the University of Pennsylvania Health System (UPHS) electronic medical record and the Corporal Michael J. Crescenz VAMC to compare the frequency of prescribing biosimilars at these sites between Jan. 1, 2015, and May 31, 2019. Dr. Baker and his associates focused specifically on reference infliximab (Remicade) and the reference noninfusion therapies filgrastim (Neupogen) and pegfilgrastim (Neulasta) and on biosimilars of these therapies (infliximab-dyyb [Inflectra], infliximab-abda [Renflexis], filgrastim-sndz [Zarxio], and pegfilgrastim-jmdb [Fulphila]).
Because Medicare was the predominant payer, the researchers estimated reimbursement for reference and biosimilar infliximabs according to the Medicare Part B reimbursement policy. They defined an institution’s incentive to use a given therapy as the difference between the reimbursement and acquisition cost for that therapy. Dr. Baker and colleagues compared the incentives for UPHS with those for the VAMC.
VAMC saved 81% of reference product cost
The researchers identified 15,761 infusions of infliximab at UPHS and 446 at the VAMC during the study period. The proportion of infusions that used the reference product was 99% at UPHS and 62% at the VAMC. ASPs for biosimilar infliximab have been consistently lower than those for the reference product since July 2017. In December 2017, the VAMC switched to the biosimilar infliximab.
Institutional incentives based on Medicare Part B reimbursement and acquisitions costs for reference and biosimilar infliximab have been similar since 2018. In 2019, the institutional incentive favored the reference product by $49-$64 per 100-mg vial. But at the VAMC, the cost per 100-mg vial was $623.48 for the reference product and $115.58 for the biosimilar Renflexis. Purchasing the biosimilar thus yielded a savings of 81%. The current costs for the therapies are $546 and $116, respectively.
In addition, Dr. Baker and colleagues identified 46,683 orders for filgrastim or pegfilgrastim at UPHS. Approximately 90% of the orders were for either of the two reference products despite the ASP of biosimilar filgrastim being approximately 40% lower than that of its reference product. At the VAMC, about 88% of orders were for the reference products. Biosimilars became available in 2016. UPHS began using them at a modest rate, but their adoption was greater at the VAMC, which designated them as preferred products.
Tendering and a nationwide policy mandating use of biosimilars have resulted in financial savings for the VAMC, wrote Dr. Baker and colleagues. “These data suggest that, with current Medicare Part B reimbursement policy, the absence of financial incentives to encourage use of infliximab biosimilars has resulted in slower uptake of biosimilar use at institutions outside of the VA system. The implications of this are a slower reduction in costs to the health care system, since decreases in ASP over time are predicated on negotiations at the institutional level, which have been gradual and stepwise. ...
“Although some of our results may not be applicable to other geographical regions of the U.S., the comparison of two affiliated institutions in geographical proximity and with shared health care providers is a strength,” they continued. “Our findings should be replicated using national VAMC data or data from other health care systems.”
The researchers said that their findings may not apply to noninfused therapies, which are not covered under Medicare Part B, and they did not directly study the impact of pharmacy benefit managers. However, they noted that their data on filgrastim and pegfilgrastim support the hypothesis that pharmacy benefit managers receive “incentives that continue to promote the use of reference products that have higher manufacturer’s list prices, which likely will limit the uptake of both infused and injectable biosimilar therapies over time.” They said that “this finding has important implications for when noninfused biosimilars (e.g. etanercept and adalimumab) are eventually introduced to the U.S. market.”
European governments incentivize use of biosimilars
Government and institutional incentives have increased the adoption of biosimilars in Europe, wrote Guro Lovik Goll, MD, and Tore Kristian Kvien, MD, of the department of rheumatology at Diakonhjemmet Hospital in Oslo, in an accompanying editorial. Norway and Denmark have annual national tender systems in which biosimilars and reference products compete. The price of infliximab biosimilar was 39% lower than the reference product in 2014 and 69% lower in 2015. “Competition has caused dramatically lower prices both for biosimilars and also for the originator drugs competing with them,” wrote the authors.
In 2015, the government of Denmark mandated that patients on infliximab be switched to a biosimilar, and patients in Norway also have been switched to biosimilars. The use of etanercept in Norway increased by 40% from 2016 to 2019, and the use of infliximab has increased by more than threefold since 2015. “In Norway, the consequence of competition, national tenders, and availability of biosimilars have led to better access to therapy for more people in need of biologic drugs, while at the same time showing a total cost reduction of biologics for use in rheumatology, gastroenterology, and dermatology,” wrote the authors.
Health care costs $10,000 per capita in the United States, compared with $5,300 for other wealthy countries in the Organization for Economic Cooperation and Development. Low life expectancy and high infant mortality in the U.S. indicate that high costs are not associated with better outcomes. “As Americans seem to lose out on the cost-cutting potential of biosimilars, this missed opportunity is set to get even more expensive,” the authors concluded.
The U.S. Department of Veterans Affairs, the National Institutes of Health, and the American Diabetes Association contributed funding for the study. Dr. Baker reported receiving consulting fees from Bristol-Myers Squibb and Gilead, and another author reported receiving research support paid to his institution by Pfizer and UCB, as well as receiving consulting fees from nine pharmaceutical companies. Dr. Goll and Dr. Kvien both reported receiving fees for speaking and/or consulting from numerous pharmaceutical companies, including Pfizer.
AGA is taking the lead in educating health care providers and patients about biosimilars and how they can be used for IBD patient care. Learn more at www.gastro.org/biosimilars.
SOURCES: Baker JF et al. Arthritis Rheumatol. 2020 Apr 6. doi: 10.1002/art.41277.
during the same time period in 2015-2019, according to an analysis published in Arthritis and Rheumatology.
The use of the biosimilars also was associated with cost savings at the VAMC, but not at the academic medical center, which illustrates that insufficient financial incentives can delay the adoption of biosimilars and the health care system’s realization of cost savings, according to the authors.
Medicare, which is not allowed to negotiate drug prices, is one of the largest payers for infused therapies. Medicare reimbursement for infused therapies is based on the latter’s average selling price (ASP) during the previous quarter. Institutions may negotiate purchase prices with drug manufacturers and receive Medicare reimbursement. Biosimilars generally have lower ASPs than their corresponding reference therapies, and biosimilar manufacturers may have less room to negotiate prices than reference therapy manufacturers. Consequently, a given institution might have a greater incentive to use reference products than to use biosimilars.
An examination of pharmacy data
The VA negotiates drug prices for all of its medical centers and has mandated that clinicians prefer biosimilars to their corresponding reference therapies, so Joshua F. Baker, MD, of the University of Pennsylvania and the Corporal Michael J. Crescenz VAMC, both in Philadelphia, and his colleagues hypothesized that the adoption of biosimilars had proceeded more quickly at a VAMC than at a nearby academic medical center.
The investigators examined pharmacy data from the University of Pennsylvania Health System (UPHS) electronic medical record and the Corporal Michael J. Crescenz VAMC to compare the frequency of prescribing biosimilars at these sites between Jan. 1, 2015, and May 31, 2019. Dr. Baker and his associates focused specifically on reference infliximab (Remicade) and the reference noninfusion therapies filgrastim (Neupogen) and pegfilgrastim (Neulasta) and on biosimilars of these therapies (infliximab-dyyb [Inflectra], infliximab-abda [Renflexis], filgrastim-sndz [Zarxio], and pegfilgrastim-jmdb [Fulphila]).
Because Medicare was the predominant payer, the researchers estimated reimbursement for reference and biosimilar infliximabs according to the Medicare Part B reimbursement policy. They defined an institution’s incentive to use a given therapy as the difference between the reimbursement and acquisition cost for that therapy. Dr. Baker and colleagues compared the incentives for UPHS with those for the VAMC.
VAMC saved 81% of reference product cost
The researchers identified 15,761 infusions of infliximab at UPHS and 446 at the VAMC during the study period. The proportion of infusions that used the reference product was 99% at UPHS and 62% at the VAMC. ASPs for biosimilar infliximab have been consistently lower than those for the reference product since July 2017. In December 2017, the VAMC switched to the biosimilar infliximab.
Institutional incentives based on Medicare Part B reimbursement and acquisitions costs for reference and biosimilar infliximab have been similar since 2018. In 2019, the institutional incentive favored the reference product by $49-$64 per 100-mg vial. But at the VAMC, the cost per 100-mg vial was $623.48 for the reference product and $115.58 for the biosimilar Renflexis. Purchasing the biosimilar thus yielded a savings of 81%. The current costs for the therapies are $546 and $116, respectively.
In addition, Dr. Baker and colleagues identified 46,683 orders for filgrastim or pegfilgrastim at UPHS. Approximately 90% of the orders were for either of the two reference products despite the ASP of biosimilar filgrastim being approximately 40% lower than that of its reference product. At the VAMC, about 88% of orders were for the reference products. Biosimilars became available in 2016. UPHS began using them at a modest rate, but their adoption was greater at the VAMC, which designated them as preferred products.
Tendering and a nationwide policy mandating use of biosimilars have resulted in financial savings for the VAMC, wrote Dr. Baker and colleagues. “These data suggest that, with current Medicare Part B reimbursement policy, the absence of financial incentives to encourage use of infliximab biosimilars has resulted in slower uptake of biosimilar use at institutions outside of the VA system. The implications of this are a slower reduction in costs to the health care system, since decreases in ASP over time are predicated on negotiations at the institutional level, which have been gradual and stepwise. ...
“Although some of our results may not be applicable to other geographical regions of the U.S., the comparison of two affiliated institutions in geographical proximity and with shared health care providers is a strength,” they continued. “Our findings should be replicated using national VAMC data or data from other health care systems.”
The researchers said that their findings may not apply to noninfused therapies, which are not covered under Medicare Part B, and they did not directly study the impact of pharmacy benefit managers. However, they noted that their data on filgrastim and pegfilgrastim support the hypothesis that pharmacy benefit managers receive “incentives that continue to promote the use of reference products that have higher manufacturer’s list prices, which likely will limit the uptake of both infused and injectable biosimilar therapies over time.” They said that “this finding has important implications for when noninfused biosimilars (e.g. etanercept and adalimumab) are eventually introduced to the U.S. market.”
European governments incentivize use of biosimilars
Government and institutional incentives have increased the adoption of biosimilars in Europe, wrote Guro Lovik Goll, MD, and Tore Kristian Kvien, MD, of the department of rheumatology at Diakonhjemmet Hospital in Oslo, in an accompanying editorial. Norway and Denmark have annual national tender systems in which biosimilars and reference products compete. The price of infliximab biosimilar was 39% lower than the reference product in 2014 and 69% lower in 2015. “Competition has caused dramatically lower prices both for biosimilars and also for the originator drugs competing with them,” wrote the authors.
In 2015, the government of Denmark mandated that patients on infliximab be switched to a biosimilar, and patients in Norway also have been switched to biosimilars. The use of etanercept in Norway increased by 40% from 2016 to 2019, and the use of infliximab has increased by more than threefold since 2015. “In Norway, the consequence of competition, national tenders, and availability of biosimilars have led to better access to therapy for more people in need of biologic drugs, while at the same time showing a total cost reduction of biologics for use in rheumatology, gastroenterology, and dermatology,” wrote the authors.
Health care costs $10,000 per capita in the United States, compared with $5,300 for other wealthy countries in the Organization for Economic Cooperation and Development. Low life expectancy and high infant mortality in the U.S. indicate that high costs are not associated with better outcomes. “As Americans seem to lose out on the cost-cutting potential of biosimilars, this missed opportunity is set to get even more expensive,” the authors concluded.
The U.S. Department of Veterans Affairs, the National Institutes of Health, and the American Diabetes Association contributed funding for the study. Dr. Baker reported receiving consulting fees from Bristol-Myers Squibb and Gilead, and another author reported receiving research support paid to his institution by Pfizer and UCB, as well as receiving consulting fees from nine pharmaceutical companies. Dr. Goll and Dr. Kvien both reported receiving fees for speaking and/or consulting from numerous pharmaceutical companies, including Pfizer.
AGA is taking the lead in educating health care providers and patients about biosimilars and how they can be used for IBD patient care. Learn more at www.gastro.org/biosimilars.
SOURCES: Baker JF et al. Arthritis Rheumatol. 2020 Apr 6. doi: 10.1002/art.41277.
during the same time period in 2015-2019, according to an analysis published in Arthritis and Rheumatology.
The use of the biosimilars also was associated with cost savings at the VAMC, but not at the academic medical center, which illustrates that insufficient financial incentives can delay the adoption of biosimilars and the health care system’s realization of cost savings, according to the authors.
Medicare, which is not allowed to negotiate drug prices, is one of the largest payers for infused therapies. Medicare reimbursement for infused therapies is based on the latter’s average selling price (ASP) during the previous quarter. Institutions may negotiate purchase prices with drug manufacturers and receive Medicare reimbursement. Biosimilars generally have lower ASPs than their corresponding reference therapies, and biosimilar manufacturers may have less room to negotiate prices than reference therapy manufacturers. Consequently, a given institution might have a greater incentive to use reference products than to use biosimilars.
An examination of pharmacy data
The VA negotiates drug prices for all of its medical centers and has mandated that clinicians prefer biosimilars to their corresponding reference therapies, so Joshua F. Baker, MD, of the University of Pennsylvania and the Corporal Michael J. Crescenz VAMC, both in Philadelphia, and his colleagues hypothesized that the adoption of biosimilars had proceeded more quickly at a VAMC than at a nearby academic medical center.
The investigators examined pharmacy data from the University of Pennsylvania Health System (UPHS) electronic medical record and the Corporal Michael J. Crescenz VAMC to compare the frequency of prescribing biosimilars at these sites between Jan. 1, 2015, and May 31, 2019. Dr. Baker and his associates focused specifically on reference infliximab (Remicade) and the reference noninfusion therapies filgrastim (Neupogen) and pegfilgrastim (Neulasta) and on biosimilars of these therapies (infliximab-dyyb [Inflectra], infliximab-abda [Renflexis], filgrastim-sndz [Zarxio], and pegfilgrastim-jmdb [Fulphila]).
Because Medicare was the predominant payer, the researchers estimated reimbursement for reference and biosimilar infliximabs according to the Medicare Part B reimbursement policy. They defined an institution’s incentive to use a given therapy as the difference between the reimbursement and acquisition cost for that therapy. Dr. Baker and colleagues compared the incentives for UPHS with those for the VAMC.
VAMC saved 81% of reference product cost
The researchers identified 15,761 infusions of infliximab at UPHS and 446 at the VAMC during the study period. The proportion of infusions that used the reference product was 99% at UPHS and 62% at the VAMC. ASPs for biosimilar infliximab have been consistently lower than those for the reference product since July 2017. In December 2017, the VAMC switched to the biosimilar infliximab.
Institutional incentives based on Medicare Part B reimbursement and acquisitions costs for reference and biosimilar infliximab have been similar since 2018. In 2019, the institutional incentive favored the reference product by $49-$64 per 100-mg vial. But at the VAMC, the cost per 100-mg vial was $623.48 for the reference product and $115.58 for the biosimilar Renflexis. Purchasing the biosimilar thus yielded a savings of 81%. The current costs for the therapies are $546 and $116, respectively.
In addition, Dr. Baker and colleagues identified 46,683 orders for filgrastim or pegfilgrastim at UPHS. Approximately 90% of the orders were for either of the two reference products despite the ASP of biosimilar filgrastim being approximately 40% lower than that of its reference product. At the VAMC, about 88% of orders were for the reference products. Biosimilars became available in 2016. UPHS began using them at a modest rate, but their adoption was greater at the VAMC, which designated them as preferred products.
Tendering and a nationwide policy mandating use of biosimilars have resulted in financial savings for the VAMC, wrote Dr. Baker and colleagues. “These data suggest that, with current Medicare Part B reimbursement policy, the absence of financial incentives to encourage use of infliximab biosimilars has resulted in slower uptake of biosimilar use at institutions outside of the VA system. The implications of this are a slower reduction in costs to the health care system, since decreases in ASP over time are predicated on negotiations at the institutional level, which have been gradual and stepwise. ...
“Although some of our results may not be applicable to other geographical regions of the U.S., the comparison of two affiliated institutions in geographical proximity and with shared health care providers is a strength,” they continued. “Our findings should be replicated using national VAMC data or data from other health care systems.”
The researchers said that their findings may not apply to noninfused therapies, which are not covered under Medicare Part B, and they did not directly study the impact of pharmacy benefit managers. However, they noted that their data on filgrastim and pegfilgrastim support the hypothesis that pharmacy benefit managers receive “incentives that continue to promote the use of reference products that have higher manufacturer’s list prices, which likely will limit the uptake of both infused and injectable biosimilar therapies over time.” They said that “this finding has important implications for when noninfused biosimilars (e.g. etanercept and adalimumab) are eventually introduced to the U.S. market.”
European governments incentivize use of biosimilars
Government and institutional incentives have increased the adoption of biosimilars in Europe, wrote Guro Lovik Goll, MD, and Tore Kristian Kvien, MD, of the department of rheumatology at Diakonhjemmet Hospital in Oslo, in an accompanying editorial. Norway and Denmark have annual national tender systems in which biosimilars and reference products compete. The price of infliximab biosimilar was 39% lower than the reference product in 2014 and 69% lower in 2015. “Competition has caused dramatically lower prices both for biosimilars and also for the originator drugs competing with them,” wrote the authors.
In 2015, the government of Denmark mandated that patients on infliximab be switched to a biosimilar, and patients in Norway also have been switched to biosimilars. The use of etanercept in Norway increased by 40% from 2016 to 2019, and the use of infliximab has increased by more than threefold since 2015. “In Norway, the consequence of competition, national tenders, and availability of biosimilars have led to better access to therapy for more people in need of biologic drugs, while at the same time showing a total cost reduction of biologics for use in rheumatology, gastroenterology, and dermatology,” wrote the authors.
Health care costs $10,000 per capita in the United States, compared with $5,300 for other wealthy countries in the Organization for Economic Cooperation and Development. Low life expectancy and high infant mortality in the U.S. indicate that high costs are not associated with better outcomes. “As Americans seem to lose out on the cost-cutting potential of biosimilars, this missed opportunity is set to get even more expensive,” the authors concluded.
The U.S. Department of Veterans Affairs, the National Institutes of Health, and the American Diabetes Association contributed funding for the study. Dr. Baker reported receiving consulting fees from Bristol-Myers Squibb and Gilead, and another author reported receiving research support paid to his institution by Pfizer and UCB, as well as receiving consulting fees from nine pharmaceutical companies. Dr. Goll and Dr. Kvien both reported receiving fees for speaking and/or consulting from numerous pharmaceutical companies, including Pfizer.
AGA is taking the lead in educating health care providers and patients about biosimilars and how they can be used for IBD patient care. Learn more at www.gastro.org/biosimilars.
SOURCES: Baker JF et al. Arthritis Rheumatol. 2020 Apr 6. doi: 10.1002/art.41277.
FROM ARTHRITIS & RHEUMATOLOGY
Sacroiliac bone marrow edema on MRI may be common postpartum
A “strikingly high number” of women have bone marrow edema on MRI of the sacroiliac joints postpartum, according to a prospective study of 35 patients published in Annals of the Rheumatic Diseases. Postpartum sacroiliac bone marrow edema decreases over time. Its occurrence may be associated with a shorter duration of labor and a lack of epidural anesthesia, the researchers wrote.
Sacroiliac bone marrow edema in postpartum women “persists mainly in subjects older than 30 years,” noted Thomas Renson, MD, of Ghent (Belgium) University Hospital and colleagues. “When suspecting AxSpA [axial spondyloarthritis], our data indicate the need to wait at least 6 months to perform an MRI [of the sacroiliac joints] in postpartum women and, if positive, repeat the MRI after 12 months.”
Sacroiliac bone marrow edema is a hallmark of axSpA. However, recent studies of young, active people without the disease have found a high prevalence of bone marrow edema meeting the Assessment of SpondyloArthritis International Society (ASAS) definition of a positive MRI for sacroiliitis. Researchers have reported sacroiliac bone marrow edema in women during pregnancy and after childbirth, but prior studies have not assessed the trajectory of sacroiliac bone marrow edema after delivery, Dr. Renson and his colleagues said.
To study this question, the researchers recruited 35 subjects from the department of obstetrics at Ghent University Hospital. All participants were aged 18-45 years and had an uncomplicated, vaginal childbirth. The investigators excluded patients with a diagnosis of spondyloarthritis, inflammatory bowel disease, severe scoliosis, treatment with anti–tumor necrosis factor-alpha agents, any contraindication for MRI, childbirth through cesarean section, or pregnancy with more than one fetus.
Researchers performed a baseline MRI within 10 days of when patients gave birth and another MRI after 6 months. If the second MRI fulfilled the ASAS definition of a positive MRI for sacroiliitis, another MRI was performed at 12 months. Bone marrow edema was scored using the Spondyloarthritis Research Consortium of Canada (SPARCC) method.
In all, 77% of the patients had sacroiliac bone marrow edema on MRI an average of 5 days postpartum, and 60% fulfilled the ASAS definition of a positive MRI. After 6 months, 46% had bone marrow edema on MRI, and 15% had a positive MRI according to the ASAS definition. After 12 months, MRI was positive in 12% of the subjects. There was a high prevalence of bone marrow edema “even in subjects without back pain,” the researchers said.
“Four subjects would have fulfilled the ASAS classification criteria if there was a suspicion of axSpA: Three fulfilled the ASAS definition of a positive MRI for sacroiliitis and had inflammatory back pain, [and] one had chronic back pain, a positive MRI, and skin psoriasis,” the researchers wrote.
Misdiagnosis of axSpA based on MRI findings entails risks, the authors noted. NSAIDs may be less effective in patients who do not have axSpA, and patients may be “subsequently more likely to receive ineffective biological therapy, which has significant potential side effects and encompasses high socioeconomic costs,” the investigators said.
The study was supported by an ASAS research grant. The authors declared having no competing interests.
SOURCE: Renson T et al. Ann Rheum Dis. 2020 Apr 16. doi: 10.1136/annrheumdis-2020-217095.
A “strikingly high number” of women have bone marrow edema on MRI of the sacroiliac joints postpartum, according to a prospective study of 35 patients published in Annals of the Rheumatic Diseases. Postpartum sacroiliac bone marrow edema decreases over time. Its occurrence may be associated with a shorter duration of labor and a lack of epidural anesthesia, the researchers wrote.
Sacroiliac bone marrow edema in postpartum women “persists mainly in subjects older than 30 years,” noted Thomas Renson, MD, of Ghent (Belgium) University Hospital and colleagues. “When suspecting AxSpA [axial spondyloarthritis], our data indicate the need to wait at least 6 months to perform an MRI [of the sacroiliac joints] in postpartum women and, if positive, repeat the MRI after 12 months.”
Sacroiliac bone marrow edema is a hallmark of axSpA. However, recent studies of young, active people without the disease have found a high prevalence of bone marrow edema meeting the Assessment of SpondyloArthritis International Society (ASAS) definition of a positive MRI for sacroiliitis. Researchers have reported sacroiliac bone marrow edema in women during pregnancy and after childbirth, but prior studies have not assessed the trajectory of sacroiliac bone marrow edema after delivery, Dr. Renson and his colleagues said.
To study this question, the researchers recruited 35 subjects from the department of obstetrics at Ghent University Hospital. All participants were aged 18-45 years and had an uncomplicated, vaginal childbirth. The investigators excluded patients with a diagnosis of spondyloarthritis, inflammatory bowel disease, severe scoliosis, treatment with anti–tumor necrosis factor-alpha agents, any contraindication for MRI, childbirth through cesarean section, or pregnancy with more than one fetus.
Researchers performed a baseline MRI within 10 days of when patients gave birth and another MRI after 6 months. If the second MRI fulfilled the ASAS definition of a positive MRI for sacroiliitis, another MRI was performed at 12 months. Bone marrow edema was scored using the Spondyloarthritis Research Consortium of Canada (SPARCC) method.
In all, 77% of the patients had sacroiliac bone marrow edema on MRI an average of 5 days postpartum, and 60% fulfilled the ASAS definition of a positive MRI. After 6 months, 46% had bone marrow edema on MRI, and 15% had a positive MRI according to the ASAS definition. After 12 months, MRI was positive in 12% of the subjects. There was a high prevalence of bone marrow edema “even in subjects without back pain,” the researchers said.
“Four subjects would have fulfilled the ASAS classification criteria if there was a suspicion of axSpA: Three fulfilled the ASAS definition of a positive MRI for sacroiliitis and had inflammatory back pain, [and] one had chronic back pain, a positive MRI, and skin psoriasis,” the researchers wrote.
Misdiagnosis of axSpA based on MRI findings entails risks, the authors noted. NSAIDs may be less effective in patients who do not have axSpA, and patients may be “subsequently more likely to receive ineffective biological therapy, which has significant potential side effects and encompasses high socioeconomic costs,” the investigators said.
The study was supported by an ASAS research grant. The authors declared having no competing interests.
SOURCE: Renson T et al. Ann Rheum Dis. 2020 Apr 16. doi: 10.1136/annrheumdis-2020-217095.
A “strikingly high number” of women have bone marrow edema on MRI of the sacroiliac joints postpartum, according to a prospective study of 35 patients published in Annals of the Rheumatic Diseases. Postpartum sacroiliac bone marrow edema decreases over time. Its occurrence may be associated with a shorter duration of labor and a lack of epidural anesthesia, the researchers wrote.
Sacroiliac bone marrow edema in postpartum women “persists mainly in subjects older than 30 years,” noted Thomas Renson, MD, of Ghent (Belgium) University Hospital and colleagues. “When suspecting AxSpA [axial spondyloarthritis], our data indicate the need to wait at least 6 months to perform an MRI [of the sacroiliac joints] in postpartum women and, if positive, repeat the MRI after 12 months.”
Sacroiliac bone marrow edema is a hallmark of axSpA. However, recent studies of young, active people without the disease have found a high prevalence of bone marrow edema meeting the Assessment of SpondyloArthritis International Society (ASAS) definition of a positive MRI for sacroiliitis. Researchers have reported sacroiliac bone marrow edema in women during pregnancy and after childbirth, but prior studies have not assessed the trajectory of sacroiliac bone marrow edema after delivery, Dr. Renson and his colleagues said.
To study this question, the researchers recruited 35 subjects from the department of obstetrics at Ghent University Hospital. All participants were aged 18-45 years and had an uncomplicated, vaginal childbirth. The investigators excluded patients with a diagnosis of spondyloarthritis, inflammatory bowel disease, severe scoliosis, treatment with anti–tumor necrosis factor-alpha agents, any contraindication for MRI, childbirth through cesarean section, or pregnancy with more than one fetus.
Researchers performed a baseline MRI within 10 days of when patients gave birth and another MRI after 6 months. If the second MRI fulfilled the ASAS definition of a positive MRI for sacroiliitis, another MRI was performed at 12 months. Bone marrow edema was scored using the Spondyloarthritis Research Consortium of Canada (SPARCC) method.
In all, 77% of the patients had sacroiliac bone marrow edema on MRI an average of 5 days postpartum, and 60% fulfilled the ASAS definition of a positive MRI. After 6 months, 46% had bone marrow edema on MRI, and 15% had a positive MRI according to the ASAS definition. After 12 months, MRI was positive in 12% of the subjects. There was a high prevalence of bone marrow edema “even in subjects without back pain,” the researchers said.
“Four subjects would have fulfilled the ASAS classification criteria if there was a suspicion of axSpA: Three fulfilled the ASAS definition of a positive MRI for sacroiliitis and had inflammatory back pain, [and] one had chronic back pain, a positive MRI, and skin psoriasis,” the researchers wrote.
Misdiagnosis of axSpA based on MRI findings entails risks, the authors noted. NSAIDs may be less effective in patients who do not have axSpA, and patients may be “subsequently more likely to receive ineffective biological therapy, which has significant potential side effects and encompasses high socioeconomic costs,” the investigators said.
The study was supported by an ASAS research grant. The authors declared having no competing interests.
SOURCE: Renson T et al. Ann Rheum Dis. 2020 Apr 16. doi: 10.1136/annrheumdis-2020-217095.
FROM ANNALS OF THE RHEUMATIC DISEASES
Methotrexate adherence: It’s worse than you think
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
REPORTING FROM RWCS 2020
Are patients with epilepsy at increased risk of COVID-19 infection?
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
Innovation and Knowledge Sharing Can Transform COVID-19 Infection Prevention Response
Emerging studies on coronavirus disease 2019 (COVID-19) confirm high rates of infection among healthcare workers (HCWs).1 As widespread community transmission increases, frontline HCWs, such as hospitalists, are at particularly high risk of exposure to people with undiagnosed COVID-19. Although there is no known effective treatment for COVID-19, early detection is vital to decreasing ongoing transmission through contact tracing and quarantine. However, lack of adequate testing capacity prevented basic public health interventions from curbing the pandemic at an earlier stage. As a result, given high rates of presumed community transmission of COVID-19 and evidence for asymptomatic transmission, there have been moves toward the use of universal personal protective equipment (PPE). This strategy is challenging to implement because of the acute PPE shortage, which has resulted in an urgent need to embrace innovation in infection prevention.
The current pandemic has resulted in an unprecedented volume of data being generated and disseminated, with the potential to impact real-time responses in geographically disparate regions. Here, we focus on the potential for innovation and knowledge sharing from an infection prevention perspective, which could enhance frontline HCW safety in the current COVID-19 pandemic.
DIAGNOSIS MATTERS
Every outbreak begins and ends with a diagnostic test. Widespread population testing coupled with intensive contact tracing had the potential to curb national epidemics if it had been implemented in time. In the United States, which now has the highest number of COVID-19 cases worldwide, there were technical difficulties with the first diagnostic test developed by the Centers for Disease Control and Prevention (CDC) and subsequent delays in scaling up access to COVID-19 diagnostic testing.2 The strategy of initially reserving testing only for those who were critically ill meant that by the time patients with COVID-19 were being diagnosed, widespread community spread had occurred because of the lack of detection of individuals with less severe or asymptomatic infections.
In contrast, scaled-up testing in South Korea has helped limit the spread and consequences of COVID-19. The use of drive-through testing centers enabled safe and efficient testing, while minimizing the risk to HCWs and eliminating the possibility of cross infection among people being tested.3 Although outdoor testing is not feasible in all settings, this approach avoids resources and time typically needed for ventilation (typically a negative pressure room with 12 air changes per hour would be used) and cleaning of specimen collection rooms.
The other major diagnostic gap is the ability to identify individuals who have recovered from COVID-19 and are immune. There is an urgent need to develop and scale up a rapid serological test that avoids cross-reactivity with other coronaviruses. Ideally, this test would permit testing of HCWs to determine who is likely immune and can therefore return safely to work.
RETHINKING PPE
There has been a massive and rapid increase in the need for PPE globally because of overwhelmed health systems having to care for large numbers of patients with suspected or confirmed COVID-19. This has been exacerbated by public fear, which has led to panic buying of medical face masks (primarily used to protect others from infections with a droplet mode of transmission) and filtering facepiece half-mask respirators, which include N95 respirators (used to protect the wearer from infections with an airborne mode of transmission).
COVID-19 is thought to be predominantly spread by transmission of respiratory droplets (>5 and <10 μm in diameter), which occurs when people are in close contact (within 1 meter) with others who typically (but not always) have respiratory symptoms such as cough or sneeze or with fomites that have come into contact with an infected person. This is in contrast to infectious diseases such as tuberculosis (TB) or measles, which are spread by airborne transmission of virus suspended in droplet nuclei (<5 μm in diameter), which can remain in the air for prolonged periods of time and can be transmitted over distances greater than 1 meter.4
While World Health Organization (WHO) and CDC infection prevention guidance have cited droplet transmission as the primary mode of transmission for COVID-19, current CDC guidelines state that respirators are preferred for the care of patients with known or suspected COVID-19, given the potential for opportunistic airborne transmission.5 However, in the setting of respirator shortages, it is recommended that these should be prioritized for HCWs caring for patients with COVID-19 in the context of aerosol-generating procedures or other patients with infections spread by airborne transmission such as TB or varicella until the supply chain is restored. Of note, optimal use of respirators requires fit testing, which is often lacking in nursing homes and outpatient facilities, as well as more widely in resource-limited countries.
Universal masking (use of surgical mask) for HCWs caring for any patient irrespective of symptoms or presenting complaint has also been implemented by many large hospital systems in recent days. Although universal masking adds to the burden of the PPE shortage, in settings with widespread community transmission and given increasing evidence6 demonstrating transmission from people with asymptomatic and presymptomatic infection, universal masking may be useful to decrease transmission. However, particularly in the setting of PPE shortages, it is important to understand that surgical masks are designed to be single use and that dampness and frequent adjustment of the mask affects their effectiveness.
As urgent attempts to coordinate and increase PPE manufacture are being made by health systems, in conjunction with private partnerships, there has also been a burst of public campaigns to sew cloth masks to mitigate the real-time shortages. Although it is likely that cloth masks provide inadequate protection in comparison with surgical masks,7 evidence does suggest that cloth masks provide some degree of protection from the spread of respiratory viruses,8 particularly if these are replaced promptly when damp or damaged and if combined with other interventions such as hand hygiene. This has led to recommendations for the general public in various countries to wear cloth face coverings in public settings, particularly where social distancing may be harder to maintain, but these are not recommended for use by HCWs in healthcare settings.
INNOVATION IN INFECTION PREVENTION
Strategies to navigate the PPE shortage in the era of COVID-19 include importing, reclaiming, reusing, and repurposing PPE; generating and extending supply; eliminating nonessential services; reducing patient contact; and using nonhuman services such as drones to deliver equipment and undertake tasks such as decontamination.9,10 Multidisciplinary teams are working on creative ways to use existing resources to make effective PPE, including alternatives to N95 respirators. An outbreak simulation study at Emory University in Atlanta, Georgia, and the University of Texas Health Science Center at Houston in Texas demonstrated that HCWs could be rapidly trained and fit tested to use elastomeric half-mask respirators, which are reusable.11 A multidisciplinary team at Boston Children’s Hospital in Massachusetts has developed and completed a small pilot study of a reusable elastomeric respirator made using an anesthesia facemask, antimicrobial filter, and elastic straps.12
Given evidence that suggests that COVID-19 involves a component of airborne transmission,13 in addition to droplet spread and surface (fomite) contamination,14 using known infection prevention techniques that work to decrease airborne transmission of other respiratory infectious diseases should also be considered. Germicidal ultraviolet (GUV) air disinfection rapidly disinfects upper room air, which is then continually exchanged with contaminated lower-room air. GUV air disinfection has been demonstrated to be a safe and cost-effective intervention, with an efficacy of approximately 80% for decreasing TB transmission.15 GUV air disinfection is also effective against airborne influenza and measles and may play a role in surface decontamination by accelerating viral inactivation. Enabling GUV in high-risk areas such as the emergency department or intensive care unit could be a high-yield intervention to decrease transmission of COVID-19.
HCWs exposed to other respiratory infections such as influenza or TB may receive preventive therapy to reduce the risk of developing disease. High rates of COVID-19 in HCWs have prompted several initiatives to evaluate innovative approaches to decreasing this risk. Multiple studies are underway to determine whether hydroxychloroquine could be used for pre- or postexposure prophylaxis to prevent COVID-19. Another multisite trial will evaluate whether the BCG vaccine, primarily used to reduce the risk of TB, provides protection against COVID-19 in HCWs, driven by data suggesting a correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19.16
DATA GENERATION AND KNOWLEDGE SHARING
Infection prevention efforts can benefit from the unprecedented amount of data on COVID-19 that is being generated and shared. Successful examples of the rapid intensification of infection prevention measures to decrease transmission in healthcare facilities should be emulated. The hospital authority of Hong Kong implemented a bundle of measures focused on early recognition, isolation, notification, and molecular diagnostics for people being evaluated for COVID-19.17 They subsequently broadened the clinical and epidemiological criteria of surveillance as the outbreak evolved and intensified PPE recommendations to all HCWs (face masks for all and N95 respirators for those performing aerosol-generating procedures), which appears to have resulted in no cases of HCW infection or nosocomial transmission.
Data characterizing the extent of occupational infections in HCWs during acute and chronic epidemics is often lacking and subject to wide variability in reporting, which limits its impact. For example, HCWs in high TB incidence countries have at least twice the risk of developing TB, compared with the general population. Although there are still major gaps in national data collection regarding the incidence of occupational TB, recent attempts by WHO to systematically record this data have resulted in increasing prioritization of this group as an at-risk population who may benefit from TB preventive therapy. We strongly advocate that health systems systematically record and share longitudinal data on numbers of HCWs infected with COVID-19. This transparency will facilitate urgent action to replenish and sustain resources such as PPE and enable institutions to share and adapt successful infection prevention strategies. Examples such as the prevention of central line- associated bloodstream infections demonstrate the potential impact of national collaborative efforts to strengthen infection prevention, although further effort is needed to optimize knowledge sharing in the context of outbreaks.
CONCLUSIONS
The cost of not investing in public health pandemic preparedness including measures to protect HCWs is now widely apparent. HCWs have a right to safety in their workplaces as they fulfil their duty of care to patients.18 Rapid scale-up of diagnostic testing capacity, and bundles of infection prevention interventions including universal masking and drive-through testing, can safeguard HCWs and the patients they serve in the current COVID-19 pandemic. Re-establishing immediate access to quality-assured PPE is imperative to reduce the individual and workforce consequences of HCWs developing COVID-19 or other infectious diseases like TB that are continuously a threat to the workforce. Meanwhile, innovative approaches such as repurposing resources to develop PPE and use of GUV air disinfection may help to mitigate PPE shortages, and use of preventive therapies may also decrease COVID-19 risk in HCWs. Reliable surveillance data on HCW infection rates can help identify and track gaps in infection prevention, as well as identify strategies that impact this outcome. Ultimately greater top-down political commitment is urgently needed to ensure that frontline HCWs have the necessary resources to address the current pandemic and to sustain these interventions to protect HCWs in the future.
1. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11)1061-1069. https://doi.org/10.1001/jama.2020.1585.
2. Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus. JAMA. 2020. https://doi.org/10.1001/jama.2020.3864.
3. Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35(11):e123. https://doi.org/10.3346/jkms.2020.35.e123.
4. World Health Organization. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific Brief, March 29, 2020. https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed April 5, 2020.
5. Centers for Disease Control and Prevention. CDC Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed April 5, 2020.
6. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377-381. https://doi.org/10.15585/mmwr.mm6913e1.
7. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577. https://doi.org/10.1136/bmjopen-2014-006577.
8. van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3(7):e2618. https://doi.org/10.1371/journal.pone.0002618.
9. Livingston E, Desai A, Berkwits M. Sourcing Personal Protective Equipment During the COVID-19 Pandemic. JAMA. 2020. https://doi.org/10.1001/jama.2020.5317.
10. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3429.
11. Pompeii LA, Kraft CS, Brownsword EA, et al. Training and fit testing of health care personnel for reusable elastomeric half-mask respirators compared with disposable N95 respirators. JAMA. 2020;e204806. https://doi.org/10.1001/jama.2020.4806.
12. Boston Children’s Hospital. Surgical Innovation Fellowship. https://www.childrenshospital.org/research/departments-divisions-programs/departments/surgery/surgical-innovation-fellowship. Accessed April 5, 2020.
13. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. https://doi.org/10.1056/NEJMc2004973.
14. Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;e203227. https://doi.org/10.1001/jama.2020.3227.
15. Mphaphlele M, Dharmadhikari AS, Jensen PA, et al. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. Am J Respir Crit Care Med. 2015;192(4):477-484. https://doi.org/10.1164/rccm.201501-0060OC.
16. Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. medRxiv. 2020. https://doi.org/10.1101/2020.03.24.20042937 .
17. Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020. https://doi.org/10.1017/ice.2020.58.
18. Antommaria AHM. Conflicting duties and reciprocal obligations during a pandemic. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3425.
Emerging studies on coronavirus disease 2019 (COVID-19) confirm high rates of infection among healthcare workers (HCWs).1 As widespread community transmission increases, frontline HCWs, such as hospitalists, are at particularly high risk of exposure to people with undiagnosed COVID-19. Although there is no known effective treatment for COVID-19, early detection is vital to decreasing ongoing transmission through contact tracing and quarantine. However, lack of adequate testing capacity prevented basic public health interventions from curbing the pandemic at an earlier stage. As a result, given high rates of presumed community transmission of COVID-19 and evidence for asymptomatic transmission, there have been moves toward the use of universal personal protective equipment (PPE). This strategy is challenging to implement because of the acute PPE shortage, which has resulted in an urgent need to embrace innovation in infection prevention.
The current pandemic has resulted in an unprecedented volume of data being generated and disseminated, with the potential to impact real-time responses in geographically disparate regions. Here, we focus on the potential for innovation and knowledge sharing from an infection prevention perspective, which could enhance frontline HCW safety in the current COVID-19 pandemic.
DIAGNOSIS MATTERS
Every outbreak begins and ends with a diagnostic test. Widespread population testing coupled with intensive contact tracing had the potential to curb national epidemics if it had been implemented in time. In the United States, which now has the highest number of COVID-19 cases worldwide, there were technical difficulties with the first diagnostic test developed by the Centers for Disease Control and Prevention (CDC) and subsequent delays in scaling up access to COVID-19 diagnostic testing.2 The strategy of initially reserving testing only for those who were critically ill meant that by the time patients with COVID-19 were being diagnosed, widespread community spread had occurred because of the lack of detection of individuals with less severe or asymptomatic infections.
In contrast, scaled-up testing in South Korea has helped limit the spread and consequences of COVID-19. The use of drive-through testing centers enabled safe and efficient testing, while minimizing the risk to HCWs and eliminating the possibility of cross infection among people being tested.3 Although outdoor testing is not feasible in all settings, this approach avoids resources and time typically needed for ventilation (typically a negative pressure room with 12 air changes per hour would be used) and cleaning of specimen collection rooms.
The other major diagnostic gap is the ability to identify individuals who have recovered from COVID-19 and are immune. There is an urgent need to develop and scale up a rapid serological test that avoids cross-reactivity with other coronaviruses. Ideally, this test would permit testing of HCWs to determine who is likely immune and can therefore return safely to work.
RETHINKING PPE
There has been a massive and rapid increase in the need for PPE globally because of overwhelmed health systems having to care for large numbers of patients with suspected or confirmed COVID-19. This has been exacerbated by public fear, which has led to panic buying of medical face masks (primarily used to protect others from infections with a droplet mode of transmission) and filtering facepiece half-mask respirators, which include N95 respirators (used to protect the wearer from infections with an airborne mode of transmission).
COVID-19 is thought to be predominantly spread by transmission of respiratory droplets (>5 and <10 μm in diameter), which occurs when people are in close contact (within 1 meter) with others who typically (but not always) have respiratory symptoms such as cough or sneeze or with fomites that have come into contact with an infected person. This is in contrast to infectious diseases such as tuberculosis (TB) or measles, which are spread by airborne transmission of virus suspended in droplet nuclei (<5 μm in diameter), which can remain in the air for prolonged periods of time and can be transmitted over distances greater than 1 meter.4
While World Health Organization (WHO) and CDC infection prevention guidance have cited droplet transmission as the primary mode of transmission for COVID-19, current CDC guidelines state that respirators are preferred for the care of patients with known or suspected COVID-19, given the potential for opportunistic airborne transmission.5 However, in the setting of respirator shortages, it is recommended that these should be prioritized for HCWs caring for patients with COVID-19 in the context of aerosol-generating procedures or other patients with infections spread by airborne transmission such as TB or varicella until the supply chain is restored. Of note, optimal use of respirators requires fit testing, which is often lacking in nursing homes and outpatient facilities, as well as more widely in resource-limited countries.
Universal masking (use of surgical mask) for HCWs caring for any patient irrespective of symptoms or presenting complaint has also been implemented by many large hospital systems in recent days. Although universal masking adds to the burden of the PPE shortage, in settings with widespread community transmission and given increasing evidence6 demonstrating transmission from people with asymptomatic and presymptomatic infection, universal masking may be useful to decrease transmission. However, particularly in the setting of PPE shortages, it is important to understand that surgical masks are designed to be single use and that dampness and frequent adjustment of the mask affects their effectiveness.
As urgent attempts to coordinate and increase PPE manufacture are being made by health systems, in conjunction with private partnerships, there has also been a burst of public campaigns to sew cloth masks to mitigate the real-time shortages. Although it is likely that cloth masks provide inadequate protection in comparison with surgical masks,7 evidence does suggest that cloth masks provide some degree of protection from the spread of respiratory viruses,8 particularly if these are replaced promptly when damp or damaged and if combined with other interventions such as hand hygiene. This has led to recommendations for the general public in various countries to wear cloth face coverings in public settings, particularly where social distancing may be harder to maintain, but these are not recommended for use by HCWs in healthcare settings.
INNOVATION IN INFECTION PREVENTION
Strategies to navigate the PPE shortage in the era of COVID-19 include importing, reclaiming, reusing, and repurposing PPE; generating and extending supply; eliminating nonessential services; reducing patient contact; and using nonhuman services such as drones to deliver equipment and undertake tasks such as decontamination.9,10 Multidisciplinary teams are working on creative ways to use existing resources to make effective PPE, including alternatives to N95 respirators. An outbreak simulation study at Emory University in Atlanta, Georgia, and the University of Texas Health Science Center at Houston in Texas demonstrated that HCWs could be rapidly trained and fit tested to use elastomeric half-mask respirators, which are reusable.11 A multidisciplinary team at Boston Children’s Hospital in Massachusetts has developed and completed a small pilot study of a reusable elastomeric respirator made using an anesthesia facemask, antimicrobial filter, and elastic straps.12
Given evidence that suggests that COVID-19 involves a component of airborne transmission,13 in addition to droplet spread and surface (fomite) contamination,14 using known infection prevention techniques that work to decrease airborne transmission of other respiratory infectious diseases should also be considered. Germicidal ultraviolet (GUV) air disinfection rapidly disinfects upper room air, which is then continually exchanged with contaminated lower-room air. GUV air disinfection has been demonstrated to be a safe and cost-effective intervention, with an efficacy of approximately 80% for decreasing TB transmission.15 GUV air disinfection is also effective against airborne influenza and measles and may play a role in surface decontamination by accelerating viral inactivation. Enabling GUV in high-risk areas such as the emergency department or intensive care unit could be a high-yield intervention to decrease transmission of COVID-19.
HCWs exposed to other respiratory infections such as influenza or TB may receive preventive therapy to reduce the risk of developing disease. High rates of COVID-19 in HCWs have prompted several initiatives to evaluate innovative approaches to decreasing this risk. Multiple studies are underway to determine whether hydroxychloroquine could be used for pre- or postexposure prophylaxis to prevent COVID-19. Another multisite trial will evaluate whether the BCG vaccine, primarily used to reduce the risk of TB, provides protection against COVID-19 in HCWs, driven by data suggesting a correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19.16
DATA GENERATION AND KNOWLEDGE SHARING
Infection prevention efforts can benefit from the unprecedented amount of data on COVID-19 that is being generated and shared. Successful examples of the rapid intensification of infection prevention measures to decrease transmission in healthcare facilities should be emulated. The hospital authority of Hong Kong implemented a bundle of measures focused on early recognition, isolation, notification, and molecular diagnostics for people being evaluated for COVID-19.17 They subsequently broadened the clinical and epidemiological criteria of surveillance as the outbreak evolved and intensified PPE recommendations to all HCWs (face masks for all and N95 respirators for those performing aerosol-generating procedures), which appears to have resulted in no cases of HCW infection or nosocomial transmission.
Data characterizing the extent of occupational infections in HCWs during acute and chronic epidemics is often lacking and subject to wide variability in reporting, which limits its impact. For example, HCWs in high TB incidence countries have at least twice the risk of developing TB, compared with the general population. Although there are still major gaps in national data collection regarding the incidence of occupational TB, recent attempts by WHO to systematically record this data have resulted in increasing prioritization of this group as an at-risk population who may benefit from TB preventive therapy. We strongly advocate that health systems systematically record and share longitudinal data on numbers of HCWs infected with COVID-19. This transparency will facilitate urgent action to replenish and sustain resources such as PPE and enable institutions to share and adapt successful infection prevention strategies. Examples such as the prevention of central line- associated bloodstream infections demonstrate the potential impact of national collaborative efforts to strengthen infection prevention, although further effort is needed to optimize knowledge sharing in the context of outbreaks.
CONCLUSIONS
The cost of not investing in public health pandemic preparedness including measures to protect HCWs is now widely apparent. HCWs have a right to safety in their workplaces as they fulfil their duty of care to patients.18 Rapid scale-up of diagnostic testing capacity, and bundles of infection prevention interventions including universal masking and drive-through testing, can safeguard HCWs and the patients they serve in the current COVID-19 pandemic. Re-establishing immediate access to quality-assured PPE is imperative to reduce the individual and workforce consequences of HCWs developing COVID-19 or other infectious diseases like TB that are continuously a threat to the workforce. Meanwhile, innovative approaches such as repurposing resources to develop PPE and use of GUV air disinfection may help to mitigate PPE shortages, and use of preventive therapies may also decrease COVID-19 risk in HCWs. Reliable surveillance data on HCW infection rates can help identify and track gaps in infection prevention, as well as identify strategies that impact this outcome. Ultimately greater top-down political commitment is urgently needed to ensure that frontline HCWs have the necessary resources to address the current pandemic and to sustain these interventions to protect HCWs in the future.
Emerging studies on coronavirus disease 2019 (COVID-19) confirm high rates of infection among healthcare workers (HCWs).1 As widespread community transmission increases, frontline HCWs, such as hospitalists, are at particularly high risk of exposure to people with undiagnosed COVID-19. Although there is no known effective treatment for COVID-19, early detection is vital to decreasing ongoing transmission through contact tracing and quarantine. However, lack of adequate testing capacity prevented basic public health interventions from curbing the pandemic at an earlier stage. As a result, given high rates of presumed community transmission of COVID-19 and evidence for asymptomatic transmission, there have been moves toward the use of universal personal protective equipment (PPE). This strategy is challenging to implement because of the acute PPE shortage, which has resulted in an urgent need to embrace innovation in infection prevention.
The current pandemic has resulted in an unprecedented volume of data being generated and disseminated, with the potential to impact real-time responses in geographically disparate regions. Here, we focus on the potential for innovation and knowledge sharing from an infection prevention perspective, which could enhance frontline HCW safety in the current COVID-19 pandemic.
DIAGNOSIS MATTERS
Every outbreak begins and ends with a diagnostic test. Widespread population testing coupled with intensive contact tracing had the potential to curb national epidemics if it had been implemented in time. In the United States, which now has the highest number of COVID-19 cases worldwide, there were technical difficulties with the first diagnostic test developed by the Centers for Disease Control and Prevention (CDC) and subsequent delays in scaling up access to COVID-19 diagnostic testing.2 The strategy of initially reserving testing only for those who were critically ill meant that by the time patients with COVID-19 were being diagnosed, widespread community spread had occurred because of the lack of detection of individuals with less severe or asymptomatic infections.
In contrast, scaled-up testing in South Korea has helped limit the spread and consequences of COVID-19. The use of drive-through testing centers enabled safe and efficient testing, while minimizing the risk to HCWs and eliminating the possibility of cross infection among people being tested.3 Although outdoor testing is not feasible in all settings, this approach avoids resources and time typically needed for ventilation (typically a negative pressure room with 12 air changes per hour would be used) and cleaning of specimen collection rooms.
The other major diagnostic gap is the ability to identify individuals who have recovered from COVID-19 and are immune. There is an urgent need to develop and scale up a rapid serological test that avoids cross-reactivity with other coronaviruses. Ideally, this test would permit testing of HCWs to determine who is likely immune and can therefore return safely to work.
RETHINKING PPE
There has been a massive and rapid increase in the need for PPE globally because of overwhelmed health systems having to care for large numbers of patients with suspected or confirmed COVID-19. This has been exacerbated by public fear, which has led to panic buying of medical face masks (primarily used to protect others from infections with a droplet mode of transmission) and filtering facepiece half-mask respirators, which include N95 respirators (used to protect the wearer from infections with an airborne mode of transmission).
COVID-19 is thought to be predominantly spread by transmission of respiratory droplets (>5 and <10 μm in diameter), which occurs when people are in close contact (within 1 meter) with others who typically (but not always) have respiratory symptoms such as cough or sneeze or with fomites that have come into contact with an infected person. This is in contrast to infectious diseases such as tuberculosis (TB) or measles, which are spread by airborne transmission of virus suspended in droplet nuclei (<5 μm in diameter), which can remain in the air for prolonged periods of time and can be transmitted over distances greater than 1 meter.4
While World Health Organization (WHO) and CDC infection prevention guidance have cited droplet transmission as the primary mode of transmission for COVID-19, current CDC guidelines state that respirators are preferred for the care of patients with known or suspected COVID-19, given the potential for opportunistic airborne transmission.5 However, in the setting of respirator shortages, it is recommended that these should be prioritized for HCWs caring for patients with COVID-19 in the context of aerosol-generating procedures or other patients with infections spread by airborne transmission such as TB or varicella until the supply chain is restored. Of note, optimal use of respirators requires fit testing, which is often lacking in nursing homes and outpatient facilities, as well as more widely in resource-limited countries.
Universal masking (use of surgical mask) for HCWs caring for any patient irrespective of symptoms or presenting complaint has also been implemented by many large hospital systems in recent days. Although universal masking adds to the burden of the PPE shortage, in settings with widespread community transmission and given increasing evidence6 demonstrating transmission from people with asymptomatic and presymptomatic infection, universal masking may be useful to decrease transmission. However, particularly in the setting of PPE shortages, it is important to understand that surgical masks are designed to be single use and that dampness and frequent adjustment of the mask affects their effectiveness.
As urgent attempts to coordinate and increase PPE manufacture are being made by health systems, in conjunction with private partnerships, there has also been a burst of public campaigns to sew cloth masks to mitigate the real-time shortages. Although it is likely that cloth masks provide inadequate protection in comparison with surgical masks,7 evidence does suggest that cloth masks provide some degree of protection from the spread of respiratory viruses,8 particularly if these are replaced promptly when damp or damaged and if combined with other interventions such as hand hygiene. This has led to recommendations for the general public in various countries to wear cloth face coverings in public settings, particularly where social distancing may be harder to maintain, but these are not recommended for use by HCWs in healthcare settings.
INNOVATION IN INFECTION PREVENTION
Strategies to navigate the PPE shortage in the era of COVID-19 include importing, reclaiming, reusing, and repurposing PPE; generating and extending supply; eliminating nonessential services; reducing patient contact; and using nonhuman services such as drones to deliver equipment and undertake tasks such as decontamination.9,10 Multidisciplinary teams are working on creative ways to use existing resources to make effective PPE, including alternatives to N95 respirators. An outbreak simulation study at Emory University in Atlanta, Georgia, and the University of Texas Health Science Center at Houston in Texas demonstrated that HCWs could be rapidly trained and fit tested to use elastomeric half-mask respirators, which are reusable.11 A multidisciplinary team at Boston Children’s Hospital in Massachusetts has developed and completed a small pilot study of a reusable elastomeric respirator made using an anesthesia facemask, antimicrobial filter, and elastic straps.12
Given evidence that suggests that COVID-19 involves a component of airborne transmission,13 in addition to droplet spread and surface (fomite) contamination,14 using known infection prevention techniques that work to decrease airborne transmission of other respiratory infectious diseases should also be considered. Germicidal ultraviolet (GUV) air disinfection rapidly disinfects upper room air, which is then continually exchanged with contaminated lower-room air. GUV air disinfection has been demonstrated to be a safe and cost-effective intervention, with an efficacy of approximately 80% for decreasing TB transmission.15 GUV air disinfection is also effective against airborne influenza and measles and may play a role in surface decontamination by accelerating viral inactivation. Enabling GUV in high-risk areas such as the emergency department or intensive care unit could be a high-yield intervention to decrease transmission of COVID-19.
HCWs exposed to other respiratory infections such as influenza or TB may receive preventive therapy to reduce the risk of developing disease. High rates of COVID-19 in HCWs have prompted several initiatives to evaluate innovative approaches to decreasing this risk. Multiple studies are underway to determine whether hydroxychloroquine could be used for pre- or postexposure prophylaxis to prevent COVID-19. Another multisite trial will evaluate whether the BCG vaccine, primarily used to reduce the risk of TB, provides protection against COVID-19 in HCWs, driven by data suggesting a correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19.16
DATA GENERATION AND KNOWLEDGE SHARING
Infection prevention efforts can benefit from the unprecedented amount of data on COVID-19 that is being generated and shared. Successful examples of the rapid intensification of infection prevention measures to decrease transmission in healthcare facilities should be emulated. The hospital authority of Hong Kong implemented a bundle of measures focused on early recognition, isolation, notification, and molecular diagnostics for people being evaluated for COVID-19.17 They subsequently broadened the clinical and epidemiological criteria of surveillance as the outbreak evolved and intensified PPE recommendations to all HCWs (face masks for all and N95 respirators for those performing aerosol-generating procedures), which appears to have resulted in no cases of HCW infection or nosocomial transmission.
Data characterizing the extent of occupational infections in HCWs during acute and chronic epidemics is often lacking and subject to wide variability in reporting, which limits its impact. For example, HCWs in high TB incidence countries have at least twice the risk of developing TB, compared with the general population. Although there are still major gaps in national data collection regarding the incidence of occupational TB, recent attempts by WHO to systematically record this data have resulted in increasing prioritization of this group as an at-risk population who may benefit from TB preventive therapy. We strongly advocate that health systems systematically record and share longitudinal data on numbers of HCWs infected with COVID-19. This transparency will facilitate urgent action to replenish and sustain resources such as PPE and enable institutions to share and adapt successful infection prevention strategies. Examples such as the prevention of central line- associated bloodstream infections demonstrate the potential impact of national collaborative efforts to strengthen infection prevention, although further effort is needed to optimize knowledge sharing in the context of outbreaks.
CONCLUSIONS
The cost of not investing in public health pandemic preparedness including measures to protect HCWs is now widely apparent. HCWs have a right to safety in their workplaces as they fulfil their duty of care to patients.18 Rapid scale-up of diagnostic testing capacity, and bundles of infection prevention interventions including universal masking and drive-through testing, can safeguard HCWs and the patients they serve in the current COVID-19 pandemic. Re-establishing immediate access to quality-assured PPE is imperative to reduce the individual and workforce consequences of HCWs developing COVID-19 or other infectious diseases like TB that are continuously a threat to the workforce. Meanwhile, innovative approaches such as repurposing resources to develop PPE and use of GUV air disinfection may help to mitigate PPE shortages, and use of preventive therapies may also decrease COVID-19 risk in HCWs. Reliable surveillance data on HCW infection rates can help identify and track gaps in infection prevention, as well as identify strategies that impact this outcome. Ultimately greater top-down political commitment is urgently needed to ensure that frontline HCWs have the necessary resources to address the current pandemic and to sustain these interventions to protect HCWs in the future.
1. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11)1061-1069. https://doi.org/10.1001/jama.2020.1585.
2. Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus. JAMA. 2020. https://doi.org/10.1001/jama.2020.3864.
3. Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35(11):e123. https://doi.org/10.3346/jkms.2020.35.e123.
4. World Health Organization. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific Brief, March 29, 2020. https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed April 5, 2020.
5. Centers for Disease Control and Prevention. CDC Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed April 5, 2020.
6. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377-381. https://doi.org/10.15585/mmwr.mm6913e1.
7. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577. https://doi.org/10.1136/bmjopen-2014-006577.
8. van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3(7):e2618. https://doi.org/10.1371/journal.pone.0002618.
9. Livingston E, Desai A, Berkwits M. Sourcing Personal Protective Equipment During the COVID-19 Pandemic. JAMA. 2020. https://doi.org/10.1001/jama.2020.5317.
10. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3429.
11. Pompeii LA, Kraft CS, Brownsword EA, et al. Training and fit testing of health care personnel for reusable elastomeric half-mask respirators compared with disposable N95 respirators. JAMA. 2020;e204806. https://doi.org/10.1001/jama.2020.4806.
12. Boston Children’s Hospital. Surgical Innovation Fellowship. https://www.childrenshospital.org/research/departments-divisions-programs/departments/surgery/surgical-innovation-fellowship. Accessed April 5, 2020.
13. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. https://doi.org/10.1056/NEJMc2004973.
14. Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;e203227. https://doi.org/10.1001/jama.2020.3227.
15. Mphaphlele M, Dharmadhikari AS, Jensen PA, et al. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. Am J Respir Crit Care Med. 2015;192(4):477-484. https://doi.org/10.1164/rccm.201501-0060OC.
16. Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. medRxiv. 2020. https://doi.org/10.1101/2020.03.24.20042937 .
17. Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020. https://doi.org/10.1017/ice.2020.58.
18. Antommaria AHM. Conflicting duties and reciprocal obligations during a pandemic. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3425.
1. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11)1061-1069. https://doi.org/10.1001/jama.2020.1585.
2. Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus. JAMA. 2020. https://doi.org/10.1001/jama.2020.3864.
3. Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35(11):e123. https://doi.org/10.3346/jkms.2020.35.e123.
4. World Health Organization. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific Brief, March 29, 2020. https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed April 5, 2020.
5. Centers for Disease Control and Prevention. CDC Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed April 5, 2020.
6. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377-381. https://doi.org/10.15585/mmwr.mm6913e1.
7. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577. https://doi.org/10.1136/bmjopen-2014-006577.
8. van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3(7):e2618. https://doi.org/10.1371/journal.pone.0002618.
9. Livingston E, Desai A, Berkwits M. Sourcing Personal Protective Equipment During the COVID-19 Pandemic. JAMA. 2020. https://doi.org/10.1001/jama.2020.5317.
10. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3429.
11. Pompeii LA, Kraft CS, Brownsword EA, et al. Training and fit testing of health care personnel for reusable elastomeric half-mask respirators compared with disposable N95 respirators. JAMA. 2020;e204806. https://doi.org/10.1001/jama.2020.4806.
12. Boston Children’s Hospital. Surgical Innovation Fellowship. https://www.childrenshospital.org/research/departments-divisions-programs/departments/surgery/surgical-innovation-fellowship. Accessed April 5, 2020.
13. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. https://doi.org/10.1056/NEJMc2004973.
14. Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;e203227. https://doi.org/10.1001/jama.2020.3227.
15. Mphaphlele M, Dharmadhikari AS, Jensen PA, et al. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. Am J Respir Crit Care Med. 2015;192(4):477-484. https://doi.org/10.1164/rccm.201501-0060OC.
16. Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. medRxiv. 2020. https://doi.org/10.1101/2020.03.24.20042937 .
17. Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020. https://doi.org/10.1017/ice.2020.58.
18. Antommaria AHM. Conflicting duties and reciprocal obligations during a pandemic. J Hosp Med. 2020;15(5):xxx-xxx. https://doi.org/10.12788/jhm.3425.
© 2020 Society of Hospital Medicine