User login
Update on duodenoscope reprocessing and infection control
Infection transmission from duodenoscopes is a serious and complex issue for our patients and our practices.
As previously shared with our members late last year, the U.S. Food and Drug Administration (FDA) reported on preliminary data from manufacturer testing of duodenoscopes following reprocessing (cleaning). The report showed that, in about 5% of cases, samples tested positive for “high concern” bacteria after the scopes had been reprocessed as recommended. According to FDA, these are bacteria that are more often associated with disease. The final results and more granular detail are expected later this year.
This is a serious and complex issue for our patients and our practices. Duodenoscopes are necessary for performing endoscopic retrograde cholangiopancreatography (ERCP). This minimally invasive procedure is typically performed in patients with diseases of the liver, pancreas, and gallbladder and obviates the necessity for more morbid surgical and radiologic procedures.
A recent article in The New York Times reviewing this issue largely understated the value of duodenoscopes and the procedure for which they are used. This is a potentially life-saving procedure for nearly 700,000 patients each year in the United States. When a doctor recommends ERCP, it often is because the patient is seriously ill, and the benefits of the procedure far outweigh the risks. ERCPs also spare patients more invasive alternatives, including surgery. Withdrawal of these instruments from the marketplace is simply not feasible and would be a major step backward in our ability to treat common and complex disease in the most beneficial manner.
We do agree and support the identification and development of safe and effective solutions that eliminate risk of infection transmission as a top priority. This cannot happen overnight: We cannot adopt new technologies, such as disposable duodenoscopes, without first understanding the new and unintentional risks we may be introducing to our patients such as an increased risk of procedural failure, perforation, or pancreatitis.
The GI societies have been working closely with FDA and industry to identify and properly vet potential solutions. FDA has already reviewed and cleared new reprocessing and sterilization technologies and revised designs for some duodenoscopes; all are intended to enhance ease of cleaning and reprocessing, thereby improving safety from transmitted infection. Other redesigns and new technologies for endoscope reprocessing, as well as single-use instruments, are in the pipeline. All of these options, and others, will likely enter the marketplace in the coming months and years after FDA vetting and approval and with postmarketing studies to ensure the efficacy of the technology and patient safety.
AGA is currently seeking feedback from AGA members to provide to FDA for consideration as they make upcoming review and approval decisions. If you are concerned about losing access to ERCP, a valuable procedure, please share your comments in the AGA Community. We will be sharing these comments with FDA to ensure their decisions reflect the needs of our members.
Since it was discovered several years ago that cases of infection transmission associated with duodenoscopes had been experienced by hospitals in the United States and Europe, health care organizations across the board recognized the need to escalate infection control efforts and to swiftly identify and disseminate best practices. FDA, the Centers for Disease Control and Prevention, state and local health departments, scope manufacturers, and medical societies have collaborated continuously to determine best practices for identifying and reporting sources of infection and effectively cleaning equipment.
Since this problem was identified, vigilance has been raised and infection rates have improved. As with all medical procedures, physicians should discuss the risks and benefits with their patients who require ERCP.
This article was developed in collaboration with American Society for Gastrointestinal Endoscopy (ASGE) and the Society of Gastroenterology Nurses and Associates (SGNA).
Infection transmission from duodenoscopes is a serious and complex issue for our patients and our practices.
As previously shared with our members late last year, the U.S. Food and Drug Administration (FDA) reported on preliminary data from manufacturer testing of duodenoscopes following reprocessing (cleaning). The report showed that, in about 5% of cases, samples tested positive for “high concern” bacteria after the scopes had been reprocessed as recommended. According to FDA, these are bacteria that are more often associated with disease. The final results and more granular detail are expected later this year.
This is a serious and complex issue for our patients and our practices. Duodenoscopes are necessary for performing endoscopic retrograde cholangiopancreatography (ERCP). This minimally invasive procedure is typically performed in patients with diseases of the liver, pancreas, and gallbladder and obviates the necessity for more morbid surgical and radiologic procedures.
A recent article in The New York Times reviewing this issue largely understated the value of duodenoscopes and the procedure for which they are used. This is a potentially life-saving procedure for nearly 700,000 patients each year in the United States. When a doctor recommends ERCP, it often is because the patient is seriously ill, and the benefits of the procedure far outweigh the risks. ERCPs also spare patients more invasive alternatives, including surgery. Withdrawal of these instruments from the marketplace is simply not feasible and would be a major step backward in our ability to treat common and complex disease in the most beneficial manner.
We do agree and support the identification and development of safe and effective solutions that eliminate risk of infection transmission as a top priority. This cannot happen overnight: We cannot adopt new technologies, such as disposable duodenoscopes, without first understanding the new and unintentional risks we may be introducing to our patients such as an increased risk of procedural failure, perforation, or pancreatitis.
The GI societies have been working closely with FDA and industry to identify and properly vet potential solutions. FDA has already reviewed and cleared new reprocessing and sterilization technologies and revised designs for some duodenoscopes; all are intended to enhance ease of cleaning and reprocessing, thereby improving safety from transmitted infection. Other redesigns and new technologies for endoscope reprocessing, as well as single-use instruments, are in the pipeline. All of these options, and others, will likely enter the marketplace in the coming months and years after FDA vetting and approval and with postmarketing studies to ensure the efficacy of the technology and patient safety.
AGA is currently seeking feedback from AGA members to provide to FDA for consideration as they make upcoming review and approval decisions. If you are concerned about losing access to ERCP, a valuable procedure, please share your comments in the AGA Community. We will be sharing these comments with FDA to ensure their decisions reflect the needs of our members.
Since it was discovered several years ago that cases of infection transmission associated with duodenoscopes had been experienced by hospitals in the United States and Europe, health care organizations across the board recognized the need to escalate infection control efforts and to swiftly identify and disseminate best practices. FDA, the Centers for Disease Control and Prevention, state and local health departments, scope manufacturers, and medical societies have collaborated continuously to determine best practices for identifying and reporting sources of infection and effectively cleaning equipment.
Since this problem was identified, vigilance has been raised and infection rates have improved. As with all medical procedures, physicians should discuss the risks and benefits with their patients who require ERCP.
This article was developed in collaboration with American Society for Gastrointestinal Endoscopy (ASGE) and the Society of Gastroenterology Nurses and Associates (SGNA).
Infection transmission from duodenoscopes is a serious and complex issue for our patients and our practices.
As previously shared with our members late last year, the U.S. Food and Drug Administration (FDA) reported on preliminary data from manufacturer testing of duodenoscopes following reprocessing (cleaning). The report showed that, in about 5% of cases, samples tested positive for “high concern” bacteria after the scopes had been reprocessed as recommended. According to FDA, these are bacteria that are more often associated with disease. The final results and more granular detail are expected later this year.
This is a serious and complex issue for our patients and our practices. Duodenoscopes are necessary for performing endoscopic retrograde cholangiopancreatography (ERCP). This minimally invasive procedure is typically performed in patients with diseases of the liver, pancreas, and gallbladder and obviates the necessity for more morbid surgical and radiologic procedures.
A recent article in The New York Times reviewing this issue largely understated the value of duodenoscopes and the procedure for which they are used. This is a potentially life-saving procedure for nearly 700,000 patients each year in the United States. When a doctor recommends ERCP, it often is because the patient is seriously ill, and the benefits of the procedure far outweigh the risks. ERCPs also spare patients more invasive alternatives, including surgery. Withdrawal of these instruments from the marketplace is simply not feasible and would be a major step backward in our ability to treat common and complex disease in the most beneficial manner.
We do agree and support the identification and development of safe and effective solutions that eliminate risk of infection transmission as a top priority. This cannot happen overnight: We cannot adopt new technologies, such as disposable duodenoscopes, without first understanding the new and unintentional risks we may be introducing to our patients such as an increased risk of procedural failure, perforation, or pancreatitis.
The GI societies have been working closely with FDA and industry to identify and properly vet potential solutions. FDA has already reviewed and cleared new reprocessing and sterilization technologies and revised designs for some duodenoscopes; all are intended to enhance ease of cleaning and reprocessing, thereby improving safety from transmitted infection. Other redesigns and new technologies for endoscope reprocessing, as well as single-use instruments, are in the pipeline. All of these options, and others, will likely enter the marketplace in the coming months and years after FDA vetting and approval and with postmarketing studies to ensure the efficacy of the technology and patient safety.
AGA is currently seeking feedback from AGA members to provide to FDA for consideration as they make upcoming review and approval decisions. If you are concerned about losing access to ERCP, a valuable procedure, please share your comments in the AGA Community. We will be sharing these comments with FDA to ensure their decisions reflect the needs of our members.
Since it was discovered several years ago that cases of infection transmission associated with duodenoscopes had been experienced by hospitals in the United States and Europe, health care organizations across the board recognized the need to escalate infection control efforts and to swiftly identify and disseminate best practices. FDA, the Centers for Disease Control and Prevention, state and local health departments, scope manufacturers, and medical societies have collaborated continuously to determine best practices for identifying and reporting sources of infection and effectively cleaning equipment.
Since this problem was identified, vigilance has been raised and infection rates have improved. As with all medical procedures, physicians should discuss the risks and benefits with their patients who require ERCP.
This article was developed in collaboration with American Society for Gastrointestinal Endoscopy (ASGE) and the Society of Gastroenterology Nurses and Associates (SGNA).
Fibrosis severity and cirrhosis drive patient-reported outcomes with NASH
Patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis reported lower quality of life that is worsened in those who develop cirrhosis, based on data from 1,667 individuals.
NASH is becoming an increasingly common cause of liver disease, cirrhosis, and hepatocellular carcinoma and can have a negative effect on patients’ quality of life and other patient-reported outcomes (PROs), but studies of the impact on PROs in these patients are limited, wrote Zobair M. Younossi, MD, of the Inova Health System, Falls Church, Va., and colleagues.
In a study published in Clinical Gastroenterology and Hepatology, the researchers reviewed data from 870 adults with NASH cirrhosis and 797 with NASH and bridging fibrosis. The average age of the patients was 58 years, 73% were white, 40% were male, 52% had cirrhosis, and 74% had diabetes.
The researchers used four tools to assess quality of life: the SF-36 (36-Item Short Form Health Survey), the EQ-5D (Euroqol, a generic health questionnaire), the CLDQ-NASH (Chronic Liver Disease Questionnaire-NASH), and the WPAI:SHP (Work Productivity and Activity Impairment: Specific Health Problem).
The SF-36 score is based on eight domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health.
Overall, patients with NASH and cirrhosis had significantly lower scores on domains of the SF-36 that related to physical function, compared with bridging fibrosis patients (70.3 vs. 73.6), as well as role physical (71.6 vs. 75.4) and bodily pain (65.0 vs. 68.6). The other areas of significant impairment in NASH patients with cirrhosis, compared with NASH patients with fibrosis, appeared in four domains of the disease-specific CLDQ-NASH: activity, emotional, fatigue, and worry. In addition, the EQ-5D utility score was significantly lower in cirrhosis patients, compared with fibrosis patients.
Older age, male sex, Asian race, and U.S. location of study enrollment were independent predictors of higher PRO scores in a multivariate analysis, while black race, history of smoking, history of diabetes, higher body mass index, cirrhosis, and history of comorbidities that were gastrointestinal, musculoskeletal, psychiatric, or neurologic were independent predictors of lower PRO scores in patients with advanced fibrosis and NASH.
WPAI:SHP scores, which focused on work productivity impairment and absenteeism, were not significantly different between the groups.
The study findings were limited by several factors including the specific nature of the study population and absence of non-NASH controls, the potential of false positives because of the use of self-reports, and the lack of longitudinal data, the researchers said. The results should be verified in a larger, diverse patient population, the researchers noted, but the data highlight the impairment in quality of life and productivity among patients with NASH and “can inform patients, clinicians, payers, and policymakers about the total burden of the disease and also the comprehensive benefit of treatment,” they concluded.
The study was supported by Gilead Sciences. Dr. Younossi disclosed relationships with Gilead Sciences, as well as Intercept, NovoNordisk, BMS, Allergan/Tobira, Terns, Viking, AbbVie, Novartis, and Quest Diagnostics.
SOURCE: Younossi ZM et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2019.02.024.
Patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis reported lower quality of life that is worsened in those who develop cirrhosis, based on data from 1,667 individuals.
NASH is becoming an increasingly common cause of liver disease, cirrhosis, and hepatocellular carcinoma and can have a negative effect on patients’ quality of life and other patient-reported outcomes (PROs), but studies of the impact on PROs in these patients are limited, wrote Zobair M. Younossi, MD, of the Inova Health System, Falls Church, Va., and colleagues.
In a study published in Clinical Gastroenterology and Hepatology, the researchers reviewed data from 870 adults with NASH cirrhosis and 797 with NASH and bridging fibrosis. The average age of the patients was 58 years, 73% were white, 40% were male, 52% had cirrhosis, and 74% had diabetes.
The researchers used four tools to assess quality of life: the SF-36 (36-Item Short Form Health Survey), the EQ-5D (Euroqol, a generic health questionnaire), the CLDQ-NASH (Chronic Liver Disease Questionnaire-NASH), and the WPAI:SHP (Work Productivity and Activity Impairment: Specific Health Problem).
The SF-36 score is based on eight domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health.
Overall, patients with NASH and cirrhosis had significantly lower scores on domains of the SF-36 that related to physical function, compared with bridging fibrosis patients (70.3 vs. 73.6), as well as role physical (71.6 vs. 75.4) and bodily pain (65.0 vs. 68.6). The other areas of significant impairment in NASH patients with cirrhosis, compared with NASH patients with fibrosis, appeared in four domains of the disease-specific CLDQ-NASH: activity, emotional, fatigue, and worry. In addition, the EQ-5D utility score was significantly lower in cirrhosis patients, compared with fibrosis patients.
Older age, male sex, Asian race, and U.S. location of study enrollment were independent predictors of higher PRO scores in a multivariate analysis, while black race, history of smoking, history of diabetes, higher body mass index, cirrhosis, and history of comorbidities that were gastrointestinal, musculoskeletal, psychiatric, or neurologic were independent predictors of lower PRO scores in patients with advanced fibrosis and NASH.
WPAI:SHP scores, which focused on work productivity impairment and absenteeism, were not significantly different between the groups.
The study findings were limited by several factors including the specific nature of the study population and absence of non-NASH controls, the potential of false positives because of the use of self-reports, and the lack of longitudinal data, the researchers said. The results should be verified in a larger, diverse patient population, the researchers noted, but the data highlight the impairment in quality of life and productivity among patients with NASH and “can inform patients, clinicians, payers, and policymakers about the total burden of the disease and also the comprehensive benefit of treatment,” they concluded.
The study was supported by Gilead Sciences. Dr. Younossi disclosed relationships with Gilead Sciences, as well as Intercept, NovoNordisk, BMS, Allergan/Tobira, Terns, Viking, AbbVie, Novartis, and Quest Diagnostics.
SOURCE: Younossi ZM et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2019.02.024.
Patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis reported lower quality of life that is worsened in those who develop cirrhosis, based on data from 1,667 individuals.
NASH is becoming an increasingly common cause of liver disease, cirrhosis, and hepatocellular carcinoma and can have a negative effect on patients’ quality of life and other patient-reported outcomes (PROs), but studies of the impact on PROs in these patients are limited, wrote Zobair M. Younossi, MD, of the Inova Health System, Falls Church, Va., and colleagues.
In a study published in Clinical Gastroenterology and Hepatology, the researchers reviewed data from 870 adults with NASH cirrhosis and 797 with NASH and bridging fibrosis. The average age of the patients was 58 years, 73% were white, 40% were male, 52% had cirrhosis, and 74% had diabetes.
The researchers used four tools to assess quality of life: the SF-36 (36-Item Short Form Health Survey), the EQ-5D (Euroqol, a generic health questionnaire), the CLDQ-NASH (Chronic Liver Disease Questionnaire-NASH), and the WPAI:SHP (Work Productivity and Activity Impairment: Specific Health Problem).
The SF-36 score is based on eight domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health.
Overall, patients with NASH and cirrhosis had significantly lower scores on domains of the SF-36 that related to physical function, compared with bridging fibrosis patients (70.3 vs. 73.6), as well as role physical (71.6 vs. 75.4) and bodily pain (65.0 vs. 68.6). The other areas of significant impairment in NASH patients with cirrhosis, compared with NASH patients with fibrosis, appeared in four domains of the disease-specific CLDQ-NASH: activity, emotional, fatigue, and worry. In addition, the EQ-5D utility score was significantly lower in cirrhosis patients, compared with fibrosis patients.
Older age, male sex, Asian race, and U.S. location of study enrollment were independent predictors of higher PRO scores in a multivariate analysis, while black race, history of smoking, history of diabetes, higher body mass index, cirrhosis, and history of comorbidities that were gastrointestinal, musculoskeletal, psychiatric, or neurologic were independent predictors of lower PRO scores in patients with advanced fibrosis and NASH.
WPAI:SHP scores, which focused on work productivity impairment and absenteeism, were not significantly different between the groups.
The study findings were limited by several factors including the specific nature of the study population and absence of non-NASH controls, the potential of false positives because of the use of self-reports, and the lack of longitudinal data, the researchers said. The results should be verified in a larger, diverse patient population, the researchers noted, but the data highlight the impairment in quality of life and productivity among patients with NASH and “can inform patients, clinicians, payers, and policymakers about the total burden of the disease and also the comprehensive benefit of treatment,” they concluded.
The study was supported by Gilead Sciences. Dr. Younossi disclosed relationships with Gilead Sciences, as well as Intercept, NovoNordisk, BMS, Allergan/Tobira, Terns, Viking, AbbVie, Novartis, and Quest Diagnostics.
SOURCE: Younossi ZM et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2019.02.024.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
8 new insights about diet and gut health
Three experts share their takeaways from the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
During your 4 years of medical school, you likely received only 4 hours of nutrition training. Yet we know diet is integral to the care of GI patients. That’s why AGA focused the 2019 James W. Freston Conference on the topic of food.
Our course directors William Chey, MD, AGAF, Sheila E. Crowe, MD, AGAF, and Gerard E. Mullin, MD, AGAF, share eight points from the meeting that stuck with them and can help all practicing GIs as they consider dietary treatments for their patients.
• 1. Personalized nutrition is important. Genetic differences lead to differences in health outcomes. One size or recommendation does not fit all. This is why certain diets only work on certain people. There is no one diet for all and for all disease states. Genetic tests can be helpful, but they rely on reporting that isn’t readily available yet.
• 2. Dietary therapy is key to managing eosinophilic esophagitis (EoE). EoE is becoming more and more prevalent. Genes can’t change that fast, but epigenetic factors can, and the evidence seems to be in food. EoE is not an IgE-mediated disease and therefore most allergy tests will not prove useful; however, food is often the trigger — most common, dairy. Dietary therapy is likely the best way to manage. You want to reduce the number of eliminated foods by way of a reintroduction protocol. The six-food elimination diet is standard, though some are moving to a four-food elimination diet (dairy, wheat, egg and soy).
• 3. There has been a reported increase in those with food allergies, sensitivities, celiac disease, and other adverse reactions to food. Many of the food allergy tests available are not helpful. In addition, many afflicted patients are conducting self-imposed diets rather than working with a GI, allergist, or dietitian. This needs to change.
• 4. There is currently insufficient evidence to support a gluten-free diet for irritable bowel syndrome (IBS). It is possible that fructans, more than gluten, are causing the GI issues. Typically, the low-FODMAP diet is beneficial to IBS patients if done correctly with the guidance of a dietitian; however, not everyone with IBS improves on it. All the steps are important though, including reintroduction and maintenance.
•5. When working with patients on the low-FODMAP or other restrictive diets, it is important to know their food and eating history. Avoidance/Restrictive Food Intake Disorder (ARFID) is something we need to be aware of when it comes to patients with a history or likelihood to develop disordered eating/eating disorders. The patient team may need to include an eating disorder therapist.
•6. The general population in the U.S. has increased the adoption of a gluten-free diet although the number of cases of celiac disease has not increased. Many have self-reported gluten sensitivities. Those that have removed gluten following trends are more at risk of bowel irregularity (low fiber), weight gain, and disordered eating. Celiac disease is not a do-it-yourself disease, patients will be best served working with a dietitian and GI.
• 7. Food can induce symptoms in patients with inflammatory bowel disease (IBD). It can also trigger gut inflammation resulting in incident or relapse. There is experimental plausibility for some factors of the relationship to be causal and we may be able to modify the diet to prevent and manage IBD.
• 8. The focus on nutrition education must continue! Nutrition should be a required part of continuing medical education for physicians. And physicians should work with dietitians to improve the care of GI patients.
For resources to help your patients understand how diet and nutrition can affect their digestive health, visit the AGA GI Patient Center, gastro.org/patient. Each disease-based resource provides tips from leading experts on the role of diet in managing GI health.
The 2019 James W. Freston Single Topic Conference took place Aug. 9 and 10 in Chicago. The Freston conference is the only conference organized by the AGA Institute Council in which the agenda is determined through an open call for proposals from AGA membership. The purpose of the conference is to focus on scientific dialogue, present opportunities for scientific collaboration, and explore new ideas that may lead to enhanced patient therapies or potential opportunities for cures of digestive diseases. The 2019 conference was sponsored by the AGA Institute Council Obesity, Metabolism & Nutrition Section. Vice chair of the section, Dr. Gerard Mullin, served as co-course director.
Three experts share their takeaways from the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
During your 4 years of medical school, you likely received only 4 hours of nutrition training. Yet we know diet is integral to the care of GI patients. That’s why AGA focused the 2019 James W. Freston Conference on the topic of food.
Our course directors William Chey, MD, AGAF, Sheila E. Crowe, MD, AGAF, and Gerard E. Mullin, MD, AGAF, share eight points from the meeting that stuck with them and can help all practicing GIs as they consider dietary treatments for their patients.
• 1. Personalized nutrition is important. Genetic differences lead to differences in health outcomes. One size or recommendation does not fit all. This is why certain diets only work on certain people. There is no one diet for all and for all disease states. Genetic tests can be helpful, but they rely on reporting that isn’t readily available yet.
• 2. Dietary therapy is key to managing eosinophilic esophagitis (EoE). EoE is becoming more and more prevalent. Genes can’t change that fast, but epigenetic factors can, and the evidence seems to be in food. EoE is not an IgE-mediated disease and therefore most allergy tests will not prove useful; however, food is often the trigger — most common, dairy. Dietary therapy is likely the best way to manage. You want to reduce the number of eliminated foods by way of a reintroduction protocol. The six-food elimination diet is standard, though some are moving to a four-food elimination diet (dairy, wheat, egg and soy).
• 3. There has been a reported increase in those with food allergies, sensitivities, celiac disease, and other adverse reactions to food. Many of the food allergy tests available are not helpful. In addition, many afflicted patients are conducting self-imposed diets rather than working with a GI, allergist, or dietitian. This needs to change.
• 4. There is currently insufficient evidence to support a gluten-free diet for irritable bowel syndrome (IBS). It is possible that fructans, more than gluten, are causing the GI issues. Typically, the low-FODMAP diet is beneficial to IBS patients if done correctly with the guidance of a dietitian; however, not everyone with IBS improves on it. All the steps are important though, including reintroduction and maintenance.
•5. When working with patients on the low-FODMAP or other restrictive diets, it is important to know their food and eating history. Avoidance/Restrictive Food Intake Disorder (ARFID) is something we need to be aware of when it comes to patients with a history or likelihood to develop disordered eating/eating disorders. The patient team may need to include an eating disorder therapist.
•6. The general population in the U.S. has increased the adoption of a gluten-free diet although the number of cases of celiac disease has not increased. Many have self-reported gluten sensitivities. Those that have removed gluten following trends are more at risk of bowel irregularity (low fiber), weight gain, and disordered eating. Celiac disease is not a do-it-yourself disease, patients will be best served working with a dietitian and GI.
• 7. Food can induce symptoms in patients with inflammatory bowel disease (IBD). It can also trigger gut inflammation resulting in incident or relapse. There is experimental plausibility for some factors of the relationship to be causal and we may be able to modify the diet to prevent and manage IBD.
• 8. The focus on nutrition education must continue! Nutrition should be a required part of continuing medical education for physicians. And physicians should work with dietitians to improve the care of GI patients.
For resources to help your patients understand how diet and nutrition can affect their digestive health, visit the AGA GI Patient Center, gastro.org/patient. Each disease-based resource provides tips from leading experts on the role of diet in managing GI health.
The 2019 James W. Freston Single Topic Conference took place Aug. 9 and 10 in Chicago. The Freston conference is the only conference organized by the AGA Institute Council in which the agenda is determined through an open call for proposals from AGA membership. The purpose of the conference is to focus on scientific dialogue, present opportunities for scientific collaboration, and explore new ideas that may lead to enhanced patient therapies or potential opportunities for cures of digestive diseases. The 2019 conference was sponsored by the AGA Institute Council Obesity, Metabolism & Nutrition Section. Vice chair of the section, Dr. Gerard Mullin, served as co-course director.
Three experts share their takeaways from the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
During your 4 years of medical school, you likely received only 4 hours of nutrition training. Yet we know diet is integral to the care of GI patients. That’s why AGA focused the 2019 James W. Freston Conference on the topic of food.
Our course directors William Chey, MD, AGAF, Sheila E. Crowe, MD, AGAF, and Gerard E. Mullin, MD, AGAF, share eight points from the meeting that stuck with them and can help all practicing GIs as they consider dietary treatments for their patients.
• 1. Personalized nutrition is important. Genetic differences lead to differences in health outcomes. One size or recommendation does not fit all. This is why certain diets only work on certain people. There is no one diet for all and for all disease states. Genetic tests can be helpful, but they rely on reporting that isn’t readily available yet.
• 2. Dietary therapy is key to managing eosinophilic esophagitis (EoE). EoE is becoming more and more prevalent. Genes can’t change that fast, but epigenetic factors can, and the evidence seems to be in food. EoE is not an IgE-mediated disease and therefore most allergy tests will not prove useful; however, food is often the trigger — most common, dairy. Dietary therapy is likely the best way to manage. You want to reduce the number of eliminated foods by way of a reintroduction protocol. The six-food elimination diet is standard, though some are moving to a four-food elimination diet (dairy, wheat, egg and soy).
• 3. There has been a reported increase in those with food allergies, sensitivities, celiac disease, and other adverse reactions to food. Many of the food allergy tests available are not helpful. In addition, many afflicted patients are conducting self-imposed diets rather than working with a GI, allergist, or dietitian. This needs to change.
• 4. There is currently insufficient evidence to support a gluten-free diet for irritable bowel syndrome (IBS). It is possible that fructans, more than gluten, are causing the GI issues. Typically, the low-FODMAP diet is beneficial to IBS patients if done correctly with the guidance of a dietitian; however, not everyone with IBS improves on it. All the steps are important though, including reintroduction and maintenance.
•5. When working with patients on the low-FODMAP or other restrictive diets, it is important to know their food and eating history. Avoidance/Restrictive Food Intake Disorder (ARFID) is something we need to be aware of when it comes to patients with a history or likelihood to develop disordered eating/eating disorders. The patient team may need to include an eating disorder therapist.
•6. The general population in the U.S. has increased the adoption of a gluten-free diet although the number of cases of celiac disease has not increased. Many have self-reported gluten sensitivities. Those that have removed gluten following trends are more at risk of bowel irregularity (low fiber), weight gain, and disordered eating. Celiac disease is not a do-it-yourself disease, patients will be best served working with a dietitian and GI.
• 7. Food can induce symptoms in patients with inflammatory bowel disease (IBD). It can also trigger gut inflammation resulting in incident or relapse. There is experimental plausibility for some factors of the relationship to be causal and we may be able to modify the diet to prevent and manage IBD.
• 8. The focus on nutrition education must continue! Nutrition should be a required part of continuing medical education for physicians. And physicians should work with dietitians to improve the care of GI patients.
For resources to help your patients understand how diet and nutrition can affect their digestive health, visit the AGA GI Patient Center, gastro.org/patient. Each disease-based resource provides tips from leading experts on the role of diet in managing GI health.
The 2019 James W. Freston Single Topic Conference took place Aug. 9 and 10 in Chicago. The Freston conference is the only conference organized by the AGA Institute Council in which the agenda is determined through an open call for proposals from AGA membership. The purpose of the conference is to focus on scientific dialogue, present opportunities for scientific collaboration, and explore new ideas that may lead to enhanced patient therapies or potential opportunities for cures of digestive diseases. The 2019 conference was sponsored by the AGA Institute Council Obesity, Metabolism & Nutrition Section. Vice chair of the section, Dr. Gerard Mullin, served as co-course director.
Management of Refractory Pain From Hereditary Cutaneous Leiomyomas With Nifedipine and Gabapentin
To the Editor:
Leiomyomas are benign smooth muscle tumors. There are 3 types of cutaneous leiomyomas: (1) piloleiomyomas, arising from the arrector pili muscles; (2) angioleiomyomas, arising from the muscles surrounding dermal blood vessels; and (3) leiomyomas of the external genitalia, arising from the dartoic, vulvar, or mammary smooth muscles.1 There is no gender predilection for cutaneous leiomyomas, and lesions present on average at approximately 40 to 45 years of age.2
Piloleiomyomas are the most common type of cutaneous leiomyomas and typically present as red-brown papules and nodules on the trunk, arms, and legs.3 Piloleiomyomas often are associated with spontaneous or induced pain (eg, with cold exposure). The pain associated with piloleiomyomas can be severely debilitating to patients and may have a considerable impact on their quality of life.
A 40-year-old woman presented to our clinic with numerous widespread, painful, red-brown papules and nodules on the head, neck, chest, abdomen, back, arms, and legs of 6 years’ duration that were increasing in number (Figure 1). She had a history of uterine leiomyomas and type 2 renal papillary carcinoma following a left nephrectomy at 38 years of age. The patient’s mother had a history of similar skin lesions as well as uterine cancer. Multiple excisional biopsies were performed, all of which showed piloleiomyomas on histopathology (Figure 2). The pain associated with the patient’s extensive cutaneous leiomyomas considerably impaired her quality of life. Although she experienced pain in all affected areas of the body, the pain was the worst in the upper arms. She reported having requested a nerve ablation procedure from an outside pain management clinic, which was denied for unknown reasons.
Two years prior to the current presentation, the patient had been treated by a pain management specialist with gabapentin 300 mg twice daily as needed for pain associated with leiomyomas. The patient followed this regimen approximately 3 times weekly for the preceding 1 to 2 years with reduction in her pain symptoms; however, the painful episodes became more frequent and severe over time. The patient reported being unable to further increase the gabapentin dosing frequency because it made her too drowsy and impacted her ability to work a job that required heavy lifting. Thus, the patient requested additional therapy and was subsequently treated at our clinic with numerous excisional biopsies of the most painful lesions during the 2 years prior to her current presentation.
When the patient re-presented to our clinic, she requested additional lesion excisions given that she had experienced some pain relief from this treatment modality in the past; however, these prior excisions only resulted in local pain relief limited to the site of the excision. Because of the extent of the lesions and the patient’s inability to tolerate pain from the lidocaine injections, we did not feel multiple excisions were a practical treatment option. The patient subsequently was offered a trial of cryotherapy for symptom relief based on a reported case in which this modality was successfully used.4 After discussing the risks and benefits associated with this treatment, cryotherapy was attempted on a few of the leiomyomas on the patient’s right shoulder; however, she experienced severe pain during cryotherapy treatment, and the procedure had to be aborted.
We then increased the patient’s gabapentin regimen to 300 mg in the morning and 600 mg in the evening, as tolerated. The patient reported that she was better able to tolerate the sedating side effects of the increased dose of gabapentin because she had stopped working due to her severe pain episodes. We also added oral nifedipine 10 mg 3 times daily, as needed. Within 30 minutes of starting this treatment regimen, the pain associated with the lesions remarkably improved (10/10 severity before starting treatment vs 3/10 after starting treatment). Her pain levels remained stable (3/10 severity) during 3 weeks of treatment with this combination regimen, but unfortunately she developed headaches and malaise, which she associated with the nifedipine at the 3 times daily dose.
The patient was able to better tolerate the nifedipine after reducing the dose to once daily on an as-needed basis. On average, the patient took nifedipine once every 3 days; however, she reported that she had to periodically increase the frequency of the nifedipine to once daily for up to 2 weeks at a time for periods of more frequent pain flares. The patient reported a consistent pattern of the breakthrough symptoms rapidly improving with each dose of nifedipine, though she did feel that taking consistent gabapentin enhanced baseline symptom control. The patient also noticed on a few occasions when she did not have access to her nifedipine that her pain would flare to 10/10 severity and would decrease to 4/10 severity 30 minutes after restarting nifedipine at 10 mg once daily. She experienced breakthrough pain due to exacerbating factors including her menstrual cycle; exposure to the sun and cold temperatures or water; excessive physical activity; and mild trauma. Due to exacerbations from sun exposure, the patient often wore long-sleeved shirts, which helped reduce the severity of the pain episodes while she was outdoors.
The exact mechanism for the pain associated with cutaneous leiomyomas is unknown but is thought to be due to infringement of the lesion on the surrounding cutaneous nerves. In addition, norepinephrine activates alpha receptors on the smooth muscle to contract through an influx of ions such as calcium. When smooth muscle contracts, the compression of nerves likely is worsened.
There are a limited number of case reports in the literature that have demonstrated successful treatment of the pain associated with cutaneous leiomyomas. Previously reported treatment modalities have included phenoxybenzamine, an alpha-blocking agent that may reduce pain through its antiadrenergic effects2; nitroglycerin, a venous and arterial dilator that may reduce pain by decreasing muscle oxygen requirements2; gabapentin, an antiepileptic and analgesic medication with structural similarity to the gamma-aminobutyric acid neurotransmitter for which the exact mechanism of action is unknown3; botulinum toxin, a neuromuscular blocker that prevents the release of presynaptic acetylcholine and may decrease neuropathic pain by reducing hyperactive nerves5,6; hyoscine butylbromide and topical hyoscine hydrobromide, both antispasmodics that may reduce pain through their anticholinergic effects, which relax smooth muscle7,8; and the CO2 laser, a treatment that has been utilized for its resurfacing, excisional, and ablative properties.9,10
Calcium channel blockers such as amlodipine, verapamil, and nifedipine also have been used to treat the pain associated with piloleiomyomas.11 Calcium ion channel antagonists inhibit the influx of calcium ions across the cell membrane; therefore, nifedipine and other calcium channel blockers may prevent the smooth muscle contraction that is hypothesized to cause pain in patients with cutaneous leiomyomas.12
Mean plasma concentration of nifedipine has been shown to reach maximum values of 160 +/− 49 µg/L after 30 to 60 minutes following oral administration of 10 mg of nifedipine.13 After 8 hours, the mean concentration drops to 3.4 +/− 1.2 µg/L. The clinical response in our patient appeared consistent with the reported pharmacokinetics of the drug, as she was able to consistently obtain considerable reduction in her pain symptoms within 30 minutes of starting nifedipine, coinciding with the period of time it takes for the nifedipine to reach maximum plasma concentrations.13
Interestingly, our patient had worsening pain episodes associated with sun exposure, which typically is not reported as one of the usual triggers for cutaneous leiomyomas. We are not aware of any described mechanisms that would explain this phenomenon.
Importantly, any patient presenting with multiple cutaneous and uterine (if female) leiomyomas should be screened for hereditary leiomyomatosis and renal cell carcinoma syndrome (HLRCC), an autosomal-dominant disorder linked to a mutation in the fumarate hydratase tumor suppressor gene. Clinically, HLRCC patients typically present with multiple cutaneous leiomyomas, uterine leiomyomas, and renal cell cancer (most often type 2 papillary renal cell carcinoma).14 Hereditary leiomyomatosis and renal cell carcinoma syndrome (also known as multiple cutaneous and uterine leiomyomatosis syndrome) previously was thought to be a separate disease entity from Reed syndrome; however, after the same mutation in the fumarate hydratase tumor suppressor gene was found to be responsible for both Reed syndrome and HLRCC, they are now thought to be the same disease process.15
Diagnosis of HLRCC is likely when the patient meets the major criterion of multiple cutaneous piloleiomyomas confirmed histopathologically. Clinical diagnosis of HLRCC is suspected if 2 or more of the following minor criteria are present: type 2 papillary renal cell carcinoma before 40 years of age; onset of severely symptomatic (requiring surgery) uterine fibroids before 40 years of age in females; and first-degree family member who meets 1 or more of these criteria.15 At the time of presentation, the patient met clinical criteria for HLRCC, including multiple cutaneous leiomyomas (major criterion) and type 2 papillary renal cell carcinoma before 40 years of age (minor criterion). The patient also had a history of uterine leiomyomas, but these lesions did not fulfill the criterion of being severely symptomatic requiring surgery. Furthermore, the patient’s mother had similar cutaneous leiomyomas and a history of uterine cancer, which fulfilled additional minor criterion, consistent with an autosomal-dominant inheritance pattern (with variable penetrance) seen in HLRCC. An important issue for counseling and monitoring patients is that premenopausal women with HLRCC are at an increased risk of developing uterine leiomyosarcoma.15 Our patient followed up with an oncologist for tumor surveillance and subsequently underwent genetic testing, which revealed a mutation in the fumarate hydratase gene.
Treatment of painful cutaneous leiomyomas, particularly in patients with HLRCC, remains a therapeutic challenge. Although surgical and/or destructive treatments can provide pain relief for patients who have a limited number of lesions, these options are impracticable when a patient has numerous widespread leiomyomas; therefore, systemic therapies may be more beneficial. Clinicians should be aware of nifedipine, which may be used in combination with gabapentin as a viable treatment option in the management of acute and breakthrough pain associated with cutaneous leiomyomas.
Acknowledgment
The a
- Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002;46:477-494.
- Raj S, Calonje E, Kraus M, et al. Cutaneous pilar leiomyoma: clinicopathologic analysis of 53 lesions in 45 patients. Am J Dermatopathol. 1997;19:2-9.
- Alam M, Rabinowitz AD, Engler DE. Gabapentin treatment of multiple piloleiomyoma-related pain. J Am Acad Dermatol. 2002;46:S27-S29.
- Basendwh MA, Fatani M, Baltow B. Reed’s syndrome: a case of multiple cutaneous leiomyomas treated with liquid nitrogen cryotherapy. Case Rep Dermatol. 2016;8:65-70.
- Sifaki MK, Krueger-Krasagakis S, Koutsopoulos A, et al. Botulinum toxin type A–treatment of a patient with multiple cutaneous piloleiomyomas. Dermatology. 2008;218:44-47.
- Onder M, Adıs¸en E. A new indication of botulinum toxin: leiomyoma-related pain. J Am Acad Dermatol. 2009;60:325-328.
- Kaliyadan F, Manoj J, Dharmaratnam AD. Multiple cutaneous leiomyomas: pain relief with pulsed hysocine butyl bromide. Indian J Dermatol. 2009;54:72.
- Archer CB, Whittaker S, Greaves MW. Pharmacological modulation of cold‐induced pain in cutaneous leiomyomata. Br J Dermatol. 1988;118:255-260.
- Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26:319-322.
- Michajłowski I, Błaz˙ewicz I, Karpinsky G, et al. Successful treatment of multiple cutaneous leiomyomas with carbon dioxide laser ablation. Postepy Dermatol Alergol. 2015;32:480-482.
- Archer CB, Greaves MW. Assessment of treatment for painful cutaneous leiomyomas. J Am Acad Dermatol. 1987;17:141-142.
- Thompson JA. Therapy for painful cutaneous leiomyomas. J Am Acad Dermatol. 1985;13:865-867.
- Raemsch KD, Sommer J. Pharmacokinetics and metabolism of nifedipine. Hypertension. 1983;5(4 pt 2):II18-II24.
- Toro JR, Nickerson ML, Wei MH, et al. Mutations in the fumarate hydratase gene cause hereditary leiomyomatosis and renal cell cancer in families in North America. Am J Hum Genet. 2003;73:95-106.
- Smit DL, Mensenkamp AR, Badeloe S, et al. Hereditary leiomyomatosis and renal cell cancer in families referred for fumarate hydratase germline mutation analysis. Clin Genet. 2011;79:49-59.
To the Editor:
Leiomyomas are benign smooth muscle tumors. There are 3 types of cutaneous leiomyomas: (1) piloleiomyomas, arising from the arrector pili muscles; (2) angioleiomyomas, arising from the muscles surrounding dermal blood vessels; and (3) leiomyomas of the external genitalia, arising from the dartoic, vulvar, or mammary smooth muscles.1 There is no gender predilection for cutaneous leiomyomas, and lesions present on average at approximately 40 to 45 years of age.2
Piloleiomyomas are the most common type of cutaneous leiomyomas and typically present as red-brown papules and nodules on the trunk, arms, and legs.3 Piloleiomyomas often are associated with spontaneous or induced pain (eg, with cold exposure). The pain associated with piloleiomyomas can be severely debilitating to patients and may have a considerable impact on their quality of life.
A 40-year-old woman presented to our clinic with numerous widespread, painful, red-brown papules and nodules on the head, neck, chest, abdomen, back, arms, and legs of 6 years’ duration that were increasing in number (Figure 1). She had a history of uterine leiomyomas and type 2 renal papillary carcinoma following a left nephrectomy at 38 years of age. The patient’s mother had a history of similar skin lesions as well as uterine cancer. Multiple excisional biopsies were performed, all of which showed piloleiomyomas on histopathology (Figure 2). The pain associated with the patient’s extensive cutaneous leiomyomas considerably impaired her quality of life. Although she experienced pain in all affected areas of the body, the pain was the worst in the upper arms. She reported having requested a nerve ablation procedure from an outside pain management clinic, which was denied for unknown reasons.
Two years prior to the current presentation, the patient had been treated by a pain management specialist with gabapentin 300 mg twice daily as needed for pain associated with leiomyomas. The patient followed this regimen approximately 3 times weekly for the preceding 1 to 2 years with reduction in her pain symptoms; however, the painful episodes became more frequent and severe over time. The patient reported being unable to further increase the gabapentin dosing frequency because it made her too drowsy and impacted her ability to work a job that required heavy lifting. Thus, the patient requested additional therapy and was subsequently treated at our clinic with numerous excisional biopsies of the most painful lesions during the 2 years prior to her current presentation.
When the patient re-presented to our clinic, she requested additional lesion excisions given that she had experienced some pain relief from this treatment modality in the past; however, these prior excisions only resulted in local pain relief limited to the site of the excision. Because of the extent of the lesions and the patient’s inability to tolerate pain from the lidocaine injections, we did not feel multiple excisions were a practical treatment option. The patient subsequently was offered a trial of cryotherapy for symptom relief based on a reported case in which this modality was successfully used.4 After discussing the risks and benefits associated with this treatment, cryotherapy was attempted on a few of the leiomyomas on the patient’s right shoulder; however, she experienced severe pain during cryotherapy treatment, and the procedure had to be aborted.
We then increased the patient’s gabapentin regimen to 300 mg in the morning and 600 mg in the evening, as tolerated. The patient reported that she was better able to tolerate the sedating side effects of the increased dose of gabapentin because she had stopped working due to her severe pain episodes. We also added oral nifedipine 10 mg 3 times daily, as needed. Within 30 minutes of starting this treatment regimen, the pain associated with the lesions remarkably improved (10/10 severity before starting treatment vs 3/10 after starting treatment). Her pain levels remained stable (3/10 severity) during 3 weeks of treatment with this combination regimen, but unfortunately she developed headaches and malaise, which she associated with the nifedipine at the 3 times daily dose.
The patient was able to better tolerate the nifedipine after reducing the dose to once daily on an as-needed basis. On average, the patient took nifedipine once every 3 days; however, she reported that she had to periodically increase the frequency of the nifedipine to once daily for up to 2 weeks at a time for periods of more frequent pain flares. The patient reported a consistent pattern of the breakthrough symptoms rapidly improving with each dose of nifedipine, though she did feel that taking consistent gabapentin enhanced baseline symptom control. The patient also noticed on a few occasions when she did not have access to her nifedipine that her pain would flare to 10/10 severity and would decrease to 4/10 severity 30 minutes after restarting nifedipine at 10 mg once daily. She experienced breakthrough pain due to exacerbating factors including her menstrual cycle; exposure to the sun and cold temperatures or water; excessive physical activity; and mild trauma. Due to exacerbations from sun exposure, the patient often wore long-sleeved shirts, which helped reduce the severity of the pain episodes while she was outdoors.
The exact mechanism for the pain associated with cutaneous leiomyomas is unknown but is thought to be due to infringement of the lesion on the surrounding cutaneous nerves. In addition, norepinephrine activates alpha receptors on the smooth muscle to contract through an influx of ions such as calcium. When smooth muscle contracts, the compression of nerves likely is worsened.
There are a limited number of case reports in the literature that have demonstrated successful treatment of the pain associated with cutaneous leiomyomas. Previously reported treatment modalities have included phenoxybenzamine, an alpha-blocking agent that may reduce pain through its antiadrenergic effects2; nitroglycerin, a venous and arterial dilator that may reduce pain by decreasing muscle oxygen requirements2; gabapentin, an antiepileptic and analgesic medication with structural similarity to the gamma-aminobutyric acid neurotransmitter for which the exact mechanism of action is unknown3; botulinum toxin, a neuromuscular blocker that prevents the release of presynaptic acetylcholine and may decrease neuropathic pain by reducing hyperactive nerves5,6; hyoscine butylbromide and topical hyoscine hydrobromide, both antispasmodics that may reduce pain through their anticholinergic effects, which relax smooth muscle7,8; and the CO2 laser, a treatment that has been utilized for its resurfacing, excisional, and ablative properties.9,10
Calcium channel blockers such as amlodipine, verapamil, and nifedipine also have been used to treat the pain associated with piloleiomyomas.11 Calcium ion channel antagonists inhibit the influx of calcium ions across the cell membrane; therefore, nifedipine and other calcium channel blockers may prevent the smooth muscle contraction that is hypothesized to cause pain in patients with cutaneous leiomyomas.12
Mean plasma concentration of nifedipine has been shown to reach maximum values of 160 +/− 49 µg/L after 30 to 60 minutes following oral administration of 10 mg of nifedipine.13 After 8 hours, the mean concentration drops to 3.4 +/− 1.2 µg/L. The clinical response in our patient appeared consistent with the reported pharmacokinetics of the drug, as she was able to consistently obtain considerable reduction in her pain symptoms within 30 minutes of starting nifedipine, coinciding with the period of time it takes for the nifedipine to reach maximum plasma concentrations.13
Interestingly, our patient had worsening pain episodes associated with sun exposure, which typically is not reported as one of the usual triggers for cutaneous leiomyomas. We are not aware of any described mechanisms that would explain this phenomenon.
Importantly, any patient presenting with multiple cutaneous and uterine (if female) leiomyomas should be screened for hereditary leiomyomatosis and renal cell carcinoma syndrome (HLRCC), an autosomal-dominant disorder linked to a mutation in the fumarate hydratase tumor suppressor gene. Clinically, HLRCC patients typically present with multiple cutaneous leiomyomas, uterine leiomyomas, and renal cell cancer (most often type 2 papillary renal cell carcinoma).14 Hereditary leiomyomatosis and renal cell carcinoma syndrome (also known as multiple cutaneous and uterine leiomyomatosis syndrome) previously was thought to be a separate disease entity from Reed syndrome; however, after the same mutation in the fumarate hydratase tumor suppressor gene was found to be responsible for both Reed syndrome and HLRCC, they are now thought to be the same disease process.15
Diagnosis of HLRCC is likely when the patient meets the major criterion of multiple cutaneous piloleiomyomas confirmed histopathologically. Clinical diagnosis of HLRCC is suspected if 2 or more of the following minor criteria are present: type 2 papillary renal cell carcinoma before 40 years of age; onset of severely symptomatic (requiring surgery) uterine fibroids before 40 years of age in females; and first-degree family member who meets 1 or more of these criteria.15 At the time of presentation, the patient met clinical criteria for HLRCC, including multiple cutaneous leiomyomas (major criterion) and type 2 papillary renal cell carcinoma before 40 years of age (minor criterion). The patient also had a history of uterine leiomyomas, but these lesions did not fulfill the criterion of being severely symptomatic requiring surgery. Furthermore, the patient’s mother had similar cutaneous leiomyomas and a history of uterine cancer, which fulfilled additional minor criterion, consistent with an autosomal-dominant inheritance pattern (with variable penetrance) seen in HLRCC. An important issue for counseling and monitoring patients is that premenopausal women with HLRCC are at an increased risk of developing uterine leiomyosarcoma.15 Our patient followed up with an oncologist for tumor surveillance and subsequently underwent genetic testing, which revealed a mutation in the fumarate hydratase gene.
Treatment of painful cutaneous leiomyomas, particularly in patients with HLRCC, remains a therapeutic challenge. Although surgical and/or destructive treatments can provide pain relief for patients who have a limited number of lesions, these options are impracticable when a patient has numerous widespread leiomyomas; therefore, systemic therapies may be more beneficial. Clinicians should be aware of nifedipine, which may be used in combination with gabapentin as a viable treatment option in the management of acute and breakthrough pain associated with cutaneous leiomyomas.
Acknowledgment
The a
To the Editor:
Leiomyomas are benign smooth muscle tumors. There are 3 types of cutaneous leiomyomas: (1) piloleiomyomas, arising from the arrector pili muscles; (2) angioleiomyomas, arising from the muscles surrounding dermal blood vessels; and (3) leiomyomas of the external genitalia, arising from the dartoic, vulvar, or mammary smooth muscles.1 There is no gender predilection for cutaneous leiomyomas, and lesions present on average at approximately 40 to 45 years of age.2
Piloleiomyomas are the most common type of cutaneous leiomyomas and typically present as red-brown papules and nodules on the trunk, arms, and legs.3 Piloleiomyomas often are associated with spontaneous or induced pain (eg, with cold exposure). The pain associated with piloleiomyomas can be severely debilitating to patients and may have a considerable impact on their quality of life.
A 40-year-old woman presented to our clinic with numerous widespread, painful, red-brown papules and nodules on the head, neck, chest, abdomen, back, arms, and legs of 6 years’ duration that were increasing in number (Figure 1). She had a history of uterine leiomyomas and type 2 renal papillary carcinoma following a left nephrectomy at 38 years of age. The patient’s mother had a history of similar skin lesions as well as uterine cancer. Multiple excisional biopsies were performed, all of which showed piloleiomyomas on histopathology (Figure 2). The pain associated with the patient’s extensive cutaneous leiomyomas considerably impaired her quality of life. Although she experienced pain in all affected areas of the body, the pain was the worst in the upper arms. She reported having requested a nerve ablation procedure from an outside pain management clinic, which was denied for unknown reasons.
Two years prior to the current presentation, the patient had been treated by a pain management specialist with gabapentin 300 mg twice daily as needed for pain associated with leiomyomas. The patient followed this regimen approximately 3 times weekly for the preceding 1 to 2 years with reduction in her pain symptoms; however, the painful episodes became more frequent and severe over time. The patient reported being unable to further increase the gabapentin dosing frequency because it made her too drowsy and impacted her ability to work a job that required heavy lifting. Thus, the patient requested additional therapy and was subsequently treated at our clinic with numerous excisional biopsies of the most painful lesions during the 2 years prior to her current presentation.
When the patient re-presented to our clinic, she requested additional lesion excisions given that she had experienced some pain relief from this treatment modality in the past; however, these prior excisions only resulted in local pain relief limited to the site of the excision. Because of the extent of the lesions and the patient’s inability to tolerate pain from the lidocaine injections, we did not feel multiple excisions were a practical treatment option. The patient subsequently was offered a trial of cryotherapy for symptom relief based on a reported case in which this modality was successfully used.4 After discussing the risks and benefits associated with this treatment, cryotherapy was attempted on a few of the leiomyomas on the patient’s right shoulder; however, she experienced severe pain during cryotherapy treatment, and the procedure had to be aborted.
We then increased the patient’s gabapentin regimen to 300 mg in the morning and 600 mg in the evening, as tolerated. The patient reported that she was better able to tolerate the sedating side effects of the increased dose of gabapentin because she had stopped working due to her severe pain episodes. We also added oral nifedipine 10 mg 3 times daily, as needed. Within 30 minutes of starting this treatment regimen, the pain associated with the lesions remarkably improved (10/10 severity before starting treatment vs 3/10 after starting treatment). Her pain levels remained stable (3/10 severity) during 3 weeks of treatment with this combination regimen, but unfortunately she developed headaches and malaise, which she associated with the nifedipine at the 3 times daily dose.
The patient was able to better tolerate the nifedipine after reducing the dose to once daily on an as-needed basis. On average, the patient took nifedipine once every 3 days; however, she reported that she had to periodically increase the frequency of the nifedipine to once daily for up to 2 weeks at a time for periods of more frequent pain flares. The patient reported a consistent pattern of the breakthrough symptoms rapidly improving with each dose of nifedipine, though she did feel that taking consistent gabapentin enhanced baseline symptom control. The patient also noticed on a few occasions when she did not have access to her nifedipine that her pain would flare to 10/10 severity and would decrease to 4/10 severity 30 minutes after restarting nifedipine at 10 mg once daily. She experienced breakthrough pain due to exacerbating factors including her menstrual cycle; exposure to the sun and cold temperatures or water; excessive physical activity; and mild trauma. Due to exacerbations from sun exposure, the patient often wore long-sleeved shirts, which helped reduce the severity of the pain episodes while she was outdoors.
The exact mechanism for the pain associated with cutaneous leiomyomas is unknown but is thought to be due to infringement of the lesion on the surrounding cutaneous nerves. In addition, norepinephrine activates alpha receptors on the smooth muscle to contract through an influx of ions such as calcium. When smooth muscle contracts, the compression of nerves likely is worsened.
There are a limited number of case reports in the literature that have demonstrated successful treatment of the pain associated with cutaneous leiomyomas. Previously reported treatment modalities have included phenoxybenzamine, an alpha-blocking agent that may reduce pain through its antiadrenergic effects2; nitroglycerin, a venous and arterial dilator that may reduce pain by decreasing muscle oxygen requirements2; gabapentin, an antiepileptic and analgesic medication with structural similarity to the gamma-aminobutyric acid neurotransmitter for which the exact mechanism of action is unknown3; botulinum toxin, a neuromuscular blocker that prevents the release of presynaptic acetylcholine and may decrease neuropathic pain by reducing hyperactive nerves5,6; hyoscine butylbromide and topical hyoscine hydrobromide, both antispasmodics that may reduce pain through their anticholinergic effects, which relax smooth muscle7,8; and the CO2 laser, a treatment that has been utilized for its resurfacing, excisional, and ablative properties.9,10
Calcium channel blockers such as amlodipine, verapamil, and nifedipine also have been used to treat the pain associated with piloleiomyomas.11 Calcium ion channel antagonists inhibit the influx of calcium ions across the cell membrane; therefore, nifedipine and other calcium channel blockers may prevent the smooth muscle contraction that is hypothesized to cause pain in patients with cutaneous leiomyomas.12
Mean plasma concentration of nifedipine has been shown to reach maximum values of 160 +/− 49 µg/L after 30 to 60 minutes following oral administration of 10 mg of nifedipine.13 After 8 hours, the mean concentration drops to 3.4 +/− 1.2 µg/L. The clinical response in our patient appeared consistent with the reported pharmacokinetics of the drug, as she was able to consistently obtain considerable reduction in her pain symptoms within 30 minutes of starting nifedipine, coinciding with the period of time it takes for the nifedipine to reach maximum plasma concentrations.13
Interestingly, our patient had worsening pain episodes associated with sun exposure, which typically is not reported as one of the usual triggers for cutaneous leiomyomas. We are not aware of any described mechanisms that would explain this phenomenon.
Importantly, any patient presenting with multiple cutaneous and uterine (if female) leiomyomas should be screened for hereditary leiomyomatosis and renal cell carcinoma syndrome (HLRCC), an autosomal-dominant disorder linked to a mutation in the fumarate hydratase tumor suppressor gene. Clinically, HLRCC patients typically present with multiple cutaneous leiomyomas, uterine leiomyomas, and renal cell cancer (most often type 2 papillary renal cell carcinoma).14 Hereditary leiomyomatosis and renal cell carcinoma syndrome (also known as multiple cutaneous and uterine leiomyomatosis syndrome) previously was thought to be a separate disease entity from Reed syndrome; however, after the same mutation in the fumarate hydratase tumor suppressor gene was found to be responsible for both Reed syndrome and HLRCC, they are now thought to be the same disease process.15
Diagnosis of HLRCC is likely when the patient meets the major criterion of multiple cutaneous piloleiomyomas confirmed histopathologically. Clinical diagnosis of HLRCC is suspected if 2 or more of the following minor criteria are present: type 2 papillary renal cell carcinoma before 40 years of age; onset of severely symptomatic (requiring surgery) uterine fibroids before 40 years of age in females; and first-degree family member who meets 1 or more of these criteria.15 At the time of presentation, the patient met clinical criteria for HLRCC, including multiple cutaneous leiomyomas (major criterion) and type 2 papillary renal cell carcinoma before 40 years of age (minor criterion). The patient also had a history of uterine leiomyomas, but these lesions did not fulfill the criterion of being severely symptomatic requiring surgery. Furthermore, the patient’s mother had similar cutaneous leiomyomas and a history of uterine cancer, which fulfilled additional minor criterion, consistent with an autosomal-dominant inheritance pattern (with variable penetrance) seen in HLRCC. An important issue for counseling and monitoring patients is that premenopausal women with HLRCC are at an increased risk of developing uterine leiomyosarcoma.15 Our patient followed up with an oncologist for tumor surveillance and subsequently underwent genetic testing, which revealed a mutation in the fumarate hydratase gene.
Treatment of painful cutaneous leiomyomas, particularly in patients with HLRCC, remains a therapeutic challenge. Although surgical and/or destructive treatments can provide pain relief for patients who have a limited number of lesions, these options are impracticable when a patient has numerous widespread leiomyomas; therefore, systemic therapies may be more beneficial. Clinicians should be aware of nifedipine, which may be used in combination with gabapentin as a viable treatment option in the management of acute and breakthrough pain associated with cutaneous leiomyomas.
Acknowledgment
The a
- Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002;46:477-494.
- Raj S, Calonje E, Kraus M, et al. Cutaneous pilar leiomyoma: clinicopathologic analysis of 53 lesions in 45 patients. Am J Dermatopathol. 1997;19:2-9.
- Alam M, Rabinowitz AD, Engler DE. Gabapentin treatment of multiple piloleiomyoma-related pain. J Am Acad Dermatol. 2002;46:S27-S29.
- Basendwh MA, Fatani M, Baltow B. Reed’s syndrome: a case of multiple cutaneous leiomyomas treated with liquid nitrogen cryotherapy. Case Rep Dermatol. 2016;8:65-70.
- Sifaki MK, Krueger-Krasagakis S, Koutsopoulos A, et al. Botulinum toxin type A–treatment of a patient with multiple cutaneous piloleiomyomas. Dermatology. 2008;218:44-47.
- Onder M, Adıs¸en E. A new indication of botulinum toxin: leiomyoma-related pain. J Am Acad Dermatol. 2009;60:325-328.
- Kaliyadan F, Manoj J, Dharmaratnam AD. Multiple cutaneous leiomyomas: pain relief with pulsed hysocine butyl bromide. Indian J Dermatol. 2009;54:72.
- Archer CB, Whittaker S, Greaves MW. Pharmacological modulation of cold‐induced pain in cutaneous leiomyomata. Br J Dermatol. 1988;118:255-260.
- Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26:319-322.
- Michajłowski I, Błaz˙ewicz I, Karpinsky G, et al. Successful treatment of multiple cutaneous leiomyomas with carbon dioxide laser ablation. Postepy Dermatol Alergol. 2015;32:480-482.
- Archer CB, Greaves MW. Assessment of treatment for painful cutaneous leiomyomas. J Am Acad Dermatol. 1987;17:141-142.
- Thompson JA. Therapy for painful cutaneous leiomyomas. J Am Acad Dermatol. 1985;13:865-867.
- Raemsch KD, Sommer J. Pharmacokinetics and metabolism of nifedipine. Hypertension. 1983;5(4 pt 2):II18-II24.
- Toro JR, Nickerson ML, Wei MH, et al. Mutations in the fumarate hydratase gene cause hereditary leiomyomatosis and renal cell cancer in families in North America. Am J Hum Genet. 2003;73:95-106.
- Smit DL, Mensenkamp AR, Badeloe S, et al. Hereditary leiomyomatosis and renal cell cancer in families referred for fumarate hydratase germline mutation analysis. Clin Genet. 2011;79:49-59.
- Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002;46:477-494.
- Raj S, Calonje E, Kraus M, et al. Cutaneous pilar leiomyoma: clinicopathologic analysis of 53 lesions in 45 patients. Am J Dermatopathol. 1997;19:2-9.
- Alam M, Rabinowitz AD, Engler DE. Gabapentin treatment of multiple piloleiomyoma-related pain. J Am Acad Dermatol. 2002;46:S27-S29.
- Basendwh MA, Fatani M, Baltow B. Reed’s syndrome: a case of multiple cutaneous leiomyomas treated with liquid nitrogen cryotherapy. Case Rep Dermatol. 2016;8:65-70.
- Sifaki MK, Krueger-Krasagakis S, Koutsopoulos A, et al. Botulinum toxin type A–treatment of a patient with multiple cutaneous piloleiomyomas. Dermatology. 2008;218:44-47.
- Onder M, Adıs¸en E. A new indication of botulinum toxin: leiomyoma-related pain. J Am Acad Dermatol. 2009;60:325-328.
- Kaliyadan F, Manoj J, Dharmaratnam AD. Multiple cutaneous leiomyomas: pain relief with pulsed hysocine butyl bromide. Indian J Dermatol. 2009;54:72.
- Archer CB, Whittaker S, Greaves MW. Pharmacological modulation of cold‐induced pain in cutaneous leiomyomata. Br J Dermatol. 1988;118:255-260.
- Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26:319-322.
- Michajłowski I, Błaz˙ewicz I, Karpinsky G, et al. Successful treatment of multiple cutaneous leiomyomas with carbon dioxide laser ablation. Postepy Dermatol Alergol. 2015;32:480-482.
- Archer CB, Greaves MW. Assessment of treatment for painful cutaneous leiomyomas. J Am Acad Dermatol. 1987;17:141-142.
- Thompson JA. Therapy for painful cutaneous leiomyomas. J Am Acad Dermatol. 1985;13:865-867.
- Raemsch KD, Sommer J. Pharmacokinetics and metabolism of nifedipine. Hypertension. 1983;5(4 pt 2):II18-II24.
- Toro JR, Nickerson ML, Wei MH, et al. Mutations in the fumarate hydratase gene cause hereditary leiomyomatosis and renal cell cancer in families in North America. Am J Hum Genet. 2003;73:95-106.
- Smit DL, Mensenkamp AR, Badeloe S, et al. Hereditary leiomyomatosis and renal cell cancer in families referred for fumarate hydratase germline mutation analysis. Clin Genet. 2011;79:49-59.
Practice Points
- Cutaneous leiomyomas (piloleiomyomas) are benign smooth muscle tumors derived from the arrector pili muscle.
- Patients presenting with multiple cutaneous leiomyomas should be evaluated for hereditary leiomyomatosis and renal cell carcinoma syndrome, an autosomal-dominant disorder, which also predisposes to the development of symptomatic uterine fibroids and uterine leiomyosarcoma.
- Cutaneous leiomyomas may be a source of considerable pain, which may respond to treatment with nifedipine in combination with gabapentin.
Clip closure reduced bleeding after large lesion resection
Use of clip closure significantly reduced delayed bleeding in patients who underwent resections for large colorectal lesions, based on data from 235 individuals.
Source: American Gastroenterological Association
“Closure of a mucosal defect with clips after resection has long been considered to reduce the risk of bleeding,” but evidence to support this practice is limited, wrote Eduardo Albéniz, MD, of the Public University of Navarra (Spain), and colleagues.
In a study published in Gastroenterology, the researchers identified 235 consecutive patients who had resections of large nonpedunculated colorectal lesions from May 2016 to June 2018. Patients had an average or high risk of delayed bleeding and were randomized to receive scar closure with either 11-mm through-the-scope clips (119 patients) or no clip (116 patients).
Delayed bleeding occurred in 14 control patients (12.1%), compared with 6 clip patients (5%), for a risk reduction of 7%. The clip group included 68 cases (57%) of complete closure and 33 cases (28%) with partial closure, as well as 18 cases of failure to close (15%); only 1 case of delayed bleeding occurred in the clip group after completion of clip closure. On average, six clips were needed for complete closure.
None of the patients who experienced delayed bleeding required surgical or angiographic intervention, although 15 of the 20 patients with bleeding underwent additional endoscopy. Other adverse events included immediate bleeding in 21 clip patients and 18 controls that was managed with snare soft-tip coagulation. No deaths were reported in connection with the study.
Demographics were similar between the two groups, but the subset of patients with complete closure included more individuals aged 75 years and older and more cases with smaller polyps, compared with other subgroups, the researchers noted.
The study findings were limited by several factors, including the difficulty in predicting delayed bleeding, the potential for selection bias given the timing of patient randomization, the lack of information about polyps that were excluded from treatment, and the difficulty in completely closing the mucosal defects, the researchers noted. However, the results suggest that complete clip closure, despite its challenges, “displays a clear trend to reduce delayed bleeding risk,” and is worth an attempt.
The study was supported by the Spanish Society of Digestive Endoscopy. The researchers had no financial conflicts to disclose. MicroTech (Nanjing, China) contributed the clips used in the study.
SOURCE: Albéniz E et al. Gastroenterology. 2019 Jul 27. doi: 10.1053/j.gastro.2019.07.037.
With the advent of routine submucosal lifting prior to endoscopic mucosal resection, perforation now occurs less commonly; however, delayed bleeding following resection remains problematic given the aging population and increasing use of antithrombotic agents. In this study, clip closure resulted in a decrease in post-polypectomy bleeding in patients deemed to be at high risk (at least 8%) for delayed bleeding.
The protective benefit of clip closure was seen almost exclusively in patients who had complete closure of the defect, which was achieved in only 57% of procedures. Clinical efficacy is largely driven by endoscopist skill level and the ability to achieve complete closure. Notably, defects that were successfully clipped were smaller in size, had better accessibility, and were technically easier. Defining such procedural factors a priori is important and may influence whether one should attempt clip closure if complete clip closure is unlikely. Interestingly, the bleeding rate was higher in the control group in lesions proximal to the transverse colon, where clip closure is likely to be most beneficial and cost effective, based on emerging data. It’s worth noting that the clips used in this study were relatively small (11 mm), and not currently available in the United States, although most endoscopic clips function similarly.
Studies such as this provide evidenced-based medicine to endoscopic practice. Hemostatic clips were introduced nearly 20 years ago without evidence for their effectiveness. Future studies are needed, such as those that compare electrocautery-based resection of high-risk polyps with standard clips to over-the-scope clips, and those that compare electrocautery-based resection to cold snare resection.
Todd H. Baron, MD, is a gastroenterologist based at the University of North Carolina, Chapel Hill. He is a speaker and consultant for Olympus, Boston Scientific, and Cook Endoscopy.
With the advent of routine submucosal lifting prior to endoscopic mucosal resection, perforation now occurs less commonly; however, delayed bleeding following resection remains problematic given the aging population and increasing use of antithrombotic agents. In this study, clip closure resulted in a decrease in post-polypectomy bleeding in patients deemed to be at high risk (at least 8%) for delayed bleeding.
The protective benefit of clip closure was seen almost exclusively in patients who had complete closure of the defect, which was achieved in only 57% of procedures. Clinical efficacy is largely driven by endoscopist skill level and the ability to achieve complete closure. Notably, defects that were successfully clipped were smaller in size, had better accessibility, and were technically easier. Defining such procedural factors a priori is important and may influence whether one should attempt clip closure if complete clip closure is unlikely. Interestingly, the bleeding rate was higher in the control group in lesions proximal to the transverse colon, where clip closure is likely to be most beneficial and cost effective, based on emerging data. It’s worth noting that the clips used in this study were relatively small (11 mm), and not currently available in the United States, although most endoscopic clips function similarly.
Studies such as this provide evidenced-based medicine to endoscopic practice. Hemostatic clips were introduced nearly 20 years ago without evidence for their effectiveness. Future studies are needed, such as those that compare electrocautery-based resection of high-risk polyps with standard clips to over-the-scope clips, and those that compare electrocautery-based resection to cold snare resection.
Todd H. Baron, MD, is a gastroenterologist based at the University of North Carolina, Chapel Hill. He is a speaker and consultant for Olympus, Boston Scientific, and Cook Endoscopy.
With the advent of routine submucosal lifting prior to endoscopic mucosal resection, perforation now occurs less commonly; however, delayed bleeding following resection remains problematic given the aging population and increasing use of antithrombotic agents. In this study, clip closure resulted in a decrease in post-polypectomy bleeding in patients deemed to be at high risk (at least 8%) for delayed bleeding.
The protective benefit of clip closure was seen almost exclusively in patients who had complete closure of the defect, which was achieved in only 57% of procedures. Clinical efficacy is largely driven by endoscopist skill level and the ability to achieve complete closure. Notably, defects that were successfully clipped were smaller in size, had better accessibility, and were technically easier. Defining such procedural factors a priori is important and may influence whether one should attempt clip closure if complete clip closure is unlikely. Interestingly, the bleeding rate was higher in the control group in lesions proximal to the transverse colon, where clip closure is likely to be most beneficial and cost effective, based on emerging data. It’s worth noting that the clips used in this study were relatively small (11 mm), and not currently available in the United States, although most endoscopic clips function similarly.
Studies such as this provide evidenced-based medicine to endoscopic practice. Hemostatic clips were introduced nearly 20 years ago without evidence for their effectiveness. Future studies are needed, such as those that compare electrocautery-based resection of high-risk polyps with standard clips to over-the-scope clips, and those that compare electrocautery-based resection to cold snare resection.
Todd H. Baron, MD, is a gastroenterologist based at the University of North Carolina, Chapel Hill. He is a speaker and consultant for Olympus, Boston Scientific, and Cook Endoscopy.
Use of clip closure significantly reduced delayed bleeding in patients who underwent resections for large colorectal lesions, based on data from 235 individuals.
Source: American Gastroenterological Association
“Closure of a mucosal defect with clips after resection has long been considered to reduce the risk of bleeding,” but evidence to support this practice is limited, wrote Eduardo Albéniz, MD, of the Public University of Navarra (Spain), and colleagues.
In a study published in Gastroenterology, the researchers identified 235 consecutive patients who had resections of large nonpedunculated colorectal lesions from May 2016 to June 2018. Patients had an average or high risk of delayed bleeding and were randomized to receive scar closure with either 11-mm through-the-scope clips (119 patients) or no clip (116 patients).
Delayed bleeding occurred in 14 control patients (12.1%), compared with 6 clip patients (5%), for a risk reduction of 7%. The clip group included 68 cases (57%) of complete closure and 33 cases (28%) with partial closure, as well as 18 cases of failure to close (15%); only 1 case of delayed bleeding occurred in the clip group after completion of clip closure. On average, six clips were needed for complete closure.
None of the patients who experienced delayed bleeding required surgical or angiographic intervention, although 15 of the 20 patients with bleeding underwent additional endoscopy. Other adverse events included immediate bleeding in 21 clip patients and 18 controls that was managed with snare soft-tip coagulation. No deaths were reported in connection with the study.
Demographics were similar between the two groups, but the subset of patients with complete closure included more individuals aged 75 years and older and more cases with smaller polyps, compared with other subgroups, the researchers noted.
The study findings were limited by several factors, including the difficulty in predicting delayed bleeding, the potential for selection bias given the timing of patient randomization, the lack of information about polyps that were excluded from treatment, and the difficulty in completely closing the mucosal defects, the researchers noted. However, the results suggest that complete clip closure, despite its challenges, “displays a clear trend to reduce delayed bleeding risk,” and is worth an attempt.
The study was supported by the Spanish Society of Digestive Endoscopy. The researchers had no financial conflicts to disclose. MicroTech (Nanjing, China) contributed the clips used in the study.
SOURCE: Albéniz E et al. Gastroenterology. 2019 Jul 27. doi: 10.1053/j.gastro.2019.07.037.
Use of clip closure significantly reduced delayed bleeding in patients who underwent resections for large colorectal lesions, based on data from 235 individuals.
Source: American Gastroenterological Association
“Closure of a mucosal defect with clips after resection has long been considered to reduce the risk of bleeding,” but evidence to support this practice is limited, wrote Eduardo Albéniz, MD, of the Public University of Navarra (Spain), and colleagues.
In a study published in Gastroenterology, the researchers identified 235 consecutive patients who had resections of large nonpedunculated colorectal lesions from May 2016 to June 2018. Patients had an average or high risk of delayed bleeding and were randomized to receive scar closure with either 11-mm through-the-scope clips (119 patients) or no clip (116 patients).
Delayed bleeding occurred in 14 control patients (12.1%), compared with 6 clip patients (5%), for a risk reduction of 7%. The clip group included 68 cases (57%) of complete closure and 33 cases (28%) with partial closure, as well as 18 cases of failure to close (15%); only 1 case of delayed bleeding occurred in the clip group after completion of clip closure. On average, six clips were needed for complete closure.
None of the patients who experienced delayed bleeding required surgical or angiographic intervention, although 15 of the 20 patients with bleeding underwent additional endoscopy. Other adverse events included immediate bleeding in 21 clip patients and 18 controls that was managed with snare soft-tip coagulation. No deaths were reported in connection with the study.
Demographics were similar between the two groups, but the subset of patients with complete closure included more individuals aged 75 years and older and more cases with smaller polyps, compared with other subgroups, the researchers noted.
The study findings were limited by several factors, including the difficulty in predicting delayed bleeding, the potential for selection bias given the timing of patient randomization, the lack of information about polyps that were excluded from treatment, and the difficulty in completely closing the mucosal defects, the researchers noted. However, the results suggest that complete clip closure, despite its challenges, “displays a clear trend to reduce delayed bleeding risk,” and is worth an attempt.
The study was supported by the Spanish Society of Digestive Endoscopy. The researchers had no financial conflicts to disclose. MicroTech (Nanjing, China) contributed the clips used in the study.
SOURCE: Albéniz E et al. Gastroenterology. 2019 Jul 27. doi: 10.1053/j.gastro.2019.07.037.
FROM GASTROENTEROLOGY
Three distinct scenarios for treating facial redness with lasers and light
SAN DIEGO – In the clinical experience of J. Stuart Nelson, MD, PhD,
“There’s the patient with telangiectasia without diffuse redness, the patient who has telangiectasia with diffuse redness, and the patient who has diffuse redness,” Dr. Nelson said at the annual Masters of Aesthetics Symposium. “Because the vessel sizes are different, your approach to the clinical management of each one of these patients is going to be very different.”
For patients with telangiectasia without the redness, using pulsed dye lasers with a wavelength of 585-600 nm can be effective. “If someone has a single isolated telangiectasia, it’s the simplest thing you’ll do that day in your office,” said Dr. Nelson, professor of surgery and biomedical engineering at the Beckman Laser Institute and Medical Clinic at the University of California, Irvine. “It’s like Tiger Woods putting for a 2-foot birdie. Similarly, with the millisecond green devices, you can focus the laser beam onto the spot and you will see the blood vessels go away in real time.”
Treating patients who have telangiectasia and diffuse redness requires two steps. First, treat the larger telangiectasia with pulse durations of 20 ms, he said, and then treat the global background redness with shorter pulse durations (of 3 ms and 6 ms). “You can do this with pulse dye lasers and with green millisecond devices,” he noted.
For patients who present with diffuse global redness, “you don’t have to worry about the larger blood vessels, so you’re not going to be using the long pulse durations of the laser exposure,” said Dr. Nelson, past president of the American Society for Laser Medicine and Surgery. “You’re going to be using much shorter pulse durations, because you’re targeting blood vessels that are much smaller. You’re trying to tease out that background redness.”
If you’re concerned about how a particular patient will fare, consider performing a test spot. “This allows you to check for any unusual tissue reaction and to gauge the potential success of the laser treatment you’re doing,” he said. “It allows the patient to sort of experience the swelling and healing process they’re going to be going through.”
Dr. Nelson advised against applying a “cookbook” approach to using lasers and light sources in dermatology. “Don’t memorize treatment parameters,” he said. “What you really need to do is look for the clinical endpoints. What is the tissue response you want to see? You also want to exercise caution in patients who are tanned. The epidermal melanin absorption by tanned patients can be significant, even with some of the cooling technologies we have.”
Dr. Nelson reported having intellectual property rights with Syneron/Candela.
SAN DIEGO – In the clinical experience of J. Stuart Nelson, MD, PhD,
“There’s the patient with telangiectasia without diffuse redness, the patient who has telangiectasia with diffuse redness, and the patient who has diffuse redness,” Dr. Nelson said at the annual Masters of Aesthetics Symposium. “Because the vessel sizes are different, your approach to the clinical management of each one of these patients is going to be very different.”
For patients with telangiectasia without the redness, using pulsed dye lasers with a wavelength of 585-600 nm can be effective. “If someone has a single isolated telangiectasia, it’s the simplest thing you’ll do that day in your office,” said Dr. Nelson, professor of surgery and biomedical engineering at the Beckman Laser Institute and Medical Clinic at the University of California, Irvine. “It’s like Tiger Woods putting for a 2-foot birdie. Similarly, with the millisecond green devices, you can focus the laser beam onto the spot and you will see the blood vessels go away in real time.”
Treating patients who have telangiectasia and diffuse redness requires two steps. First, treat the larger telangiectasia with pulse durations of 20 ms, he said, and then treat the global background redness with shorter pulse durations (of 3 ms and 6 ms). “You can do this with pulse dye lasers and with green millisecond devices,” he noted.
For patients who present with diffuse global redness, “you don’t have to worry about the larger blood vessels, so you’re not going to be using the long pulse durations of the laser exposure,” said Dr. Nelson, past president of the American Society for Laser Medicine and Surgery. “You’re going to be using much shorter pulse durations, because you’re targeting blood vessels that are much smaller. You’re trying to tease out that background redness.”
If you’re concerned about how a particular patient will fare, consider performing a test spot. “This allows you to check for any unusual tissue reaction and to gauge the potential success of the laser treatment you’re doing,” he said. “It allows the patient to sort of experience the swelling and healing process they’re going to be going through.”
Dr. Nelson advised against applying a “cookbook” approach to using lasers and light sources in dermatology. “Don’t memorize treatment parameters,” he said. “What you really need to do is look for the clinical endpoints. What is the tissue response you want to see? You also want to exercise caution in patients who are tanned. The epidermal melanin absorption by tanned patients can be significant, even with some of the cooling technologies we have.”
Dr. Nelson reported having intellectual property rights with Syneron/Candela.
SAN DIEGO – In the clinical experience of J. Stuart Nelson, MD, PhD,
“There’s the patient with telangiectasia without diffuse redness, the patient who has telangiectasia with diffuse redness, and the patient who has diffuse redness,” Dr. Nelson said at the annual Masters of Aesthetics Symposium. “Because the vessel sizes are different, your approach to the clinical management of each one of these patients is going to be very different.”
For patients with telangiectasia without the redness, using pulsed dye lasers with a wavelength of 585-600 nm can be effective. “If someone has a single isolated telangiectasia, it’s the simplest thing you’ll do that day in your office,” said Dr. Nelson, professor of surgery and biomedical engineering at the Beckman Laser Institute and Medical Clinic at the University of California, Irvine. “It’s like Tiger Woods putting for a 2-foot birdie. Similarly, with the millisecond green devices, you can focus the laser beam onto the spot and you will see the blood vessels go away in real time.”
Treating patients who have telangiectasia and diffuse redness requires two steps. First, treat the larger telangiectasia with pulse durations of 20 ms, he said, and then treat the global background redness with shorter pulse durations (of 3 ms and 6 ms). “You can do this with pulse dye lasers and with green millisecond devices,” he noted.
For patients who present with diffuse global redness, “you don’t have to worry about the larger blood vessels, so you’re not going to be using the long pulse durations of the laser exposure,” said Dr. Nelson, past president of the American Society for Laser Medicine and Surgery. “You’re going to be using much shorter pulse durations, because you’re targeting blood vessels that are much smaller. You’re trying to tease out that background redness.”
If you’re concerned about how a particular patient will fare, consider performing a test spot. “This allows you to check for any unusual tissue reaction and to gauge the potential success of the laser treatment you’re doing,” he said. “It allows the patient to sort of experience the swelling and healing process they’re going to be going through.”
Dr. Nelson advised against applying a “cookbook” approach to using lasers and light sources in dermatology. “Don’t memorize treatment parameters,” he said. “What you really need to do is look for the clinical endpoints. What is the tissue response you want to see? You also want to exercise caution in patients who are tanned. The epidermal melanin absorption by tanned patients can be significant, even with some of the cooling technologies we have.”
Dr. Nelson reported having intellectual property rights with Syneron/Candela.
EXPERT ANALYSIS FROM MOA 2019
Medical boards change or consider amending mental health-related licensing questions
Delicia M. Haynes, MD, wants the Florida Board of Medicine to take another look at how its licensing applications query physicians about their mental health history. Her state’s board is one of several nationwide that has, in recent years, mulled whether the phrasing of its questions poses an unintended hurdle for physicians who need help for conditions such as depression.
The Federation of State Medical Boards (FSMB) recommends limiting such queries, if they must be asked, to questions about potential current impairment. But the Florida license application takes a more sweeping approach that may discourage physicians from seeking treatment, Dr. Haynes, founder and CEO of Family First Health Center in Daytona Beach, Fla., said in a video. She describes herself as a direct primary care physician.
In the video, which was posted on YouTube in January, 2019, Dr. Haynes discussed her own experience with having been treated for depression and then needing to report that to the state board. Florida’s license application asks if physicians have been treated within the past 5 years for a mental disorder that has impaired the ability to practice medicine. Those who have had such a condition may need to give the board an explanation providing the names of the physicians, therapists, and counselors they have seen, as well as details and dates for the institutions where they received treatment.
State medical boards play a critical role in protecting people from physicians whose current mental health conditions may risk harming patients, Dr. Haynes said. But they must balance that against the consequences of overly intrusive questioning. Florida’s current application wording may deter physicians from seeking care if they develop conditions such as depression, she said.
“It’s the fear of what’s going to happen if I have to check yes,” Dr. Haynes said in her YouTube video. Physicians will wonder how getting treatment could put their license and their employment at risk, she added.
“It’s really important that [state medical boards] are asking the questions that matter and those questions are questions that talk about impairment, and not just having a history,” Dr. Haynes said.
Members of Florida’s board of medicine last year favorably discussed making such a change during a rules/legislative committee meeting, but have not yet implemented it. The board has postponed further discussion of this topic until its December meeting, said Brad Dalton, a spokesman for the Florida Department of Health.
Dr. Haynes said in an email that she will continue to press for changes in her state’s licensing application.
There’s been a wave of reconsideration of these kinds of questions, spurred by FSMB efforts, which included the board’s offering specific advice to state medical boards about questions on licensing applications as part of a set of recommendations on addressing physician wellness and burnout last year in a report.
Boards have the option of omitting or dropping specific inquiries about mental health. But if they choose to retain this question, FSMB recommends using this phrasing: “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner? (Yes/No)” the report says.
The staff of the Medical Board of California cited FSMB’s recommendation in a January 2019 report about revising the state’s approach to asking physicians about their mental health. In May 2019, the board voted unanimously to revise its questions on physicians’ mental health, narrowing its inquiry on the licensing application to focus on current impairment.
“There are many doctors who do not seek treatment or find it threatening to seek treatment, because they are concerned that they may lose their license,” Peter Yellowlees, MBBS, MD, chief wellness officer and a professor of psychiatry at University of California, Davis, said in a public comment offered at the meeting. “This is ultimately all about patient safety.”
said Joe Knickrehm, a spokesman for the FSMB. Over the past few years, Kentucky, New Hampshire, New Mexico, North Carolina, North Dakota, Ohio, Vermont and Washington have made changes to their licensing questions, he added.
Still, state boards are not moving quickly enough to remove or revise these questions about mental health, said Katherine J. Gold, MD MSW, associate professor in the department of family medicine at University of Michigan, Ann Arbor. She has studied how these queries can deter physicians from seeking treatment for mental illness. A past treatment for postpartum depression may have no bearing on a physician’s practice, yet members of many state medical boards hesitate to alter their approach, she noted.
Groups including the American Medical Association (AMA) and the American Psychiatric Association also have pushed in recent years for changes in state rules about what a physician has to disclose about mental health, with the FSMB taking a lead in these efforts. In many cases, physicians face questions about their mental health that are beyond the limits of standards set by the Americans With Disabilities Act, according to an article published this year in the FSMB’s Journal of Medical Regulation. As of 2017, a review of questions on initial licensure applications for all 50 states and the District of Columbia showed that 32 licensing boards ask questions beyond the limits of ADA standards, the article said.
Consequences of “reporting stable and easily treatable conditions such as anxiety or depression to a state licensing board can range from a physician simply being required to submit a letter from their primary care provider documenting fitness to practice, to a request to appear before the board, to being required to undergo and pay for an examination by a board-appointed physician,” wrote Catherine M. Welcher, an AMA senior policy analyst, and coauthors of the paper, including Humayun J. Chaudhry, DO, FSMB’s CEO.
Nearly 40% of physicians surveyed about medical licensing questions (2,325 of 5,829) indicated they would be reluctant to seek formal medical care for a mental health condition because of potential repercussions, Liselotte N. Dyrbye, MD, and coauthors reported in 2017 in the Mayo Clinic Proceedings.
“You’re sort of stuck. You recognize you have a problem and you want to seek care so that you can get better, but if you do that, you might have to tell the board,” Dr. Dyrbye said in an interview. “You could be mandated potentially to have an outside psychiatric evaluation, to have your personal medical records reviewed by people other than your personal physician.”
Rising levels of burnout among physicians make it critical to remove obstacles to care, said Arthur S. Hengerer, MD, a former chair of the FSMB who has been a leader in efforts to revise medical licensing questions.
“The only thing that really brings joy to medicine are the relationships you develop with patients, the trust that comes from that, and when you can’t develop relationships because you can’t spend the time, because you are clicking and documenting, it hurts,” said Andrew Lamb, MD, who aided in successful efforts to change North Carolina’s licensing questions.
North Carolina approached this issue in steps. In 2017, it removed a question about mental health from its annual physician license renewal form. In 2018, the North Carolina Medical Board voted to drop questions about mental and physical health from physician license applications.
“It’s hoped that removing this question will encourage clinicians to get the help they need, without fear it will compromise their chances to obtain a professional license,” the board said in an annual report.
Other states are retaining these questions, but allowing physicians to check “no” if they are in an approved program for mental health treatment. The North Dakota Board of Medicine took this approach.
“Because our mission is protection of the public, we didn’t feel that we could eliminate that question,” Bonnie Storbakken, JD, executive secretary of the North Dakota Board of Medicine, said in an interview.
The North Dakota board voted in March 2018 to change its question on mental health after the FSMB spurred a national dialogue on this issue, she said. The North Dakota board opted to allow physicians to check ‘no’ on the question about current mental health and or substance issues if they had voluntarily sought assistance from the North Dakota Professional Health Program or a professional health program in another state. The approach preserves anonymity. The question as previously phrased made some physicians feel they had to report their treatment, she said.
In Alabama, physicians also have the option to check “no” on questions about whether they are undergoing mental health treatment if they are participating in a professional assistance program. Mark Jackson, executive director of the Medical Association of Alabama, said he hopes more states give physicians this option for seeking help not only with mental health issues, but with addiction as well.
“You need to get people in and get them help and not jeopardize their career in the process. Society in general has got that problem going on and physicians are not immune from that,” Mr. Jackson said. “Hopefully other states will see that we need to do something to make sure that the physician population is taken care of.”
Pamela Wible, MD, an advocate for physicians’ mental health, did her own review of state board’s licensing questions. In an assessment posted on her website, Dr. Wible, who practices family medicine, gives 13 states an “A” grade for having no mental health questions or one or two straightforward current questions about impairment that do not mention mental health. “Connecticut, Hawaii, Michigan, and New York are the most physician-friendly of all states with no mental health or impairment questions,” Dr. Wible wrote.
The Texas Medical Board earned a “C” grade in Dr. Wible’s survey. In May 2019, that board’s chairman, Sherif Zaafran, MD, wrote about how his organization had taken a new look at the licensing questions, which were last revised in 2014. While the board has not decided on any immediate changes, it is “maintaining an open dialogue to address future concerns,” Dr. Zaafran wrote in the board’s bulletin.
The Texas Medical Board’s physician licensing form, as posted on its website, includes a broadly phrased question on mental health: “Within the past five (5) years, have you been diagnosed with or treated for any: psychotic disorder, delusional disorder, mood disorder, major depression, personality disorder, or any other mental condition which impaired or does impair your behavior, judgment, or ability to function in school or work?”
Physicians who have had treatment for mental health conditions then must submit another form. They may have to provide details on diagnosis, prognosis, and medications prescribed. Compliance requirements include counseling records, contracts with impairment support groups, and records on file with law enforcement agencies and licensing agencies.
State officials are trying to figure out how best to learn of potential impairments that could pose a risk for patients, without scaring physicians away from getting the care they themselves need said Stephen ‘Brint’ Carlton, JD, executive director of the Texas Medical Board.
Delicia M. Haynes, MD, wants the Florida Board of Medicine to take another look at how its licensing applications query physicians about their mental health history. Her state’s board is one of several nationwide that has, in recent years, mulled whether the phrasing of its questions poses an unintended hurdle for physicians who need help for conditions such as depression.
The Federation of State Medical Boards (FSMB) recommends limiting such queries, if they must be asked, to questions about potential current impairment. But the Florida license application takes a more sweeping approach that may discourage physicians from seeking treatment, Dr. Haynes, founder and CEO of Family First Health Center in Daytona Beach, Fla., said in a video. She describes herself as a direct primary care physician.
In the video, which was posted on YouTube in January, 2019, Dr. Haynes discussed her own experience with having been treated for depression and then needing to report that to the state board. Florida’s license application asks if physicians have been treated within the past 5 years for a mental disorder that has impaired the ability to practice medicine. Those who have had such a condition may need to give the board an explanation providing the names of the physicians, therapists, and counselors they have seen, as well as details and dates for the institutions where they received treatment.
State medical boards play a critical role in protecting people from physicians whose current mental health conditions may risk harming patients, Dr. Haynes said. But they must balance that against the consequences of overly intrusive questioning. Florida’s current application wording may deter physicians from seeking care if they develop conditions such as depression, she said.
“It’s the fear of what’s going to happen if I have to check yes,” Dr. Haynes said in her YouTube video. Physicians will wonder how getting treatment could put their license and their employment at risk, she added.
“It’s really important that [state medical boards] are asking the questions that matter and those questions are questions that talk about impairment, and not just having a history,” Dr. Haynes said.
Members of Florida’s board of medicine last year favorably discussed making such a change during a rules/legislative committee meeting, but have not yet implemented it. The board has postponed further discussion of this topic until its December meeting, said Brad Dalton, a spokesman for the Florida Department of Health.
Dr. Haynes said in an email that she will continue to press for changes in her state’s licensing application.
There’s been a wave of reconsideration of these kinds of questions, spurred by FSMB efforts, which included the board’s offering specific advice to state medical boards about questions on licensing applications as part of a set of recommendations on addressing physician wellness and burnout last year in a report.
Boards have the option of omitting or dropping specific inquiries about mental health. But if they choose to retain this question, FSMB recommends using this phrasing: “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner? (Yes/No)” the report says.
The staff of the Medical Board of California cited FSMB’s recommendation in a January 2019 report about revising the state’s approach to asking physicians about their mental health. In May 2019, the board voted unanimously to revise its questions on physicians’ mental health, narrowing its inquiry on the licensing application to focus on current impairment.
“There are many doctors who do not seek treatment or find it threatening to seek treatment, because they are concerned that they may lose their license,” Peter Yellowlees, MBBS, MD, chief wellness officer and a professor of psychiatry at University of California, Davis, said in a public comment offered at the meeting. “This is ultimately all about patient safety.”
said Joe Knickrehm, a spokesman for the FSMB. Over the past few years, Kentucky, New Hampshire, New Mexico, North Carolina, North Dakota, Ohio, Vermont and Washington have made changes to their licensing questions, he added.
Still, state boards are not moving quickly enough to remove or revise these questions about mental health, said Katherine J. Gold, MD MSW, associate professor in the department of family medicine at University of Michigan, Ann Arbor. She has studied how these queries can deter physicians from seeking treatment for mental illness. A past treatment for postpartum depression may have no bearing on a physician’s practice, yet members of many state medical boards hesitate to alter their approach, she noted.
Groups including the American Medical Association (AMA) and the American Psychiatric Association also have pushed in recent years for changes in state rules about what a physician has to disclose about mental health, with the FSMB taking a lead in these efforts. In many cases, physicians face questions about their mental health that are beyond the limits of standards set by the Americans With Disabilities Act, according to an article published this year in the FSMB’s Journal of Medical Regulation. As of 2017, a review of questions on initial licensure applications for all 50 states and the District of Columbia showed that 32 licensing boards ask questions beyond the limits of ADA standards, the article said.
Consequences of “reporting stable and easily treatable conditions such as anxiety or depression to a state licensing board can range from a physician simply being required to submit a letter from their primary care provider documenting fitness to practice, to a request to appear before the board, to being required to undergo and pay for an examination by a board-appointed physician,” wrote Catherine M. Welcher, an AMA senior policy analyst, and coauthors of the paper, including Humayun J. Chaudhry, DO, FSMB’s CEO.
Nearly 40% of physicians surveyed about medical licensing questions (2,325 of 5,829) indicated they would be reluctant to seek formal medical care for a mental health condition because of potential repercussions, Liselotte N. Dyrbye, MD, and coauthors reported in 2017 in the Mayo Clinic Proceedings.
“You’re sort of stuck. You recognize you have a problem and you want to seek care so that you can get better, but if you do that, you might have to tell the board,” Dr. Dyrbye said in an interview. “You could be mandated potentially to have an outside psychiatric evaluation, to have your personal medical records reviewed by people other than your personal physician.”
Rising levels of burnout among physicians make it critical to remove obstacles to care, said Arthur S. Hengerer, MD, a former chair of the FSMB who has been a leader in efforts to revise medical licensing questions.
“The only thing that really brings joy to medicine are the relationships you develop with patients, the trust that comes from that, and when you can’t develop relationships because you can’t spend the time, because you are clicking and documenting, it hurts,” said Andrew Lamb, MD, who aided in successful efforts to change North Carolina’s licensing questions.
North Carolina approached this issue in steps. In 2017, it removed a question about mental health from its annual physician license renewal form. In 2018, the North Carolina Medical Board voted to drop questions about mental and physical health from physician license applications.
“It’s hoped that removing this question will encourage clinicians to get the help they need, without fear it will compromise their chances to obtain a professional license,” the board said in an annual report.
Other states are retaining these questions, but allowing physicians to check “no” if they are in an approved program for mental health treatment. The North Dakota Board of Medicine took this approach.
“Because our mission is protection of the public, we didn’t feel that we could eliminate that question,” Bonnie Storbakken, JD, executive secretary of the North Dakota Board of Medicine, said in an interview.
The North Dakota board voted in March 2018 to change its question on mental health after the FSMB spurred a national dialogue on this issue, she said. The North Dakota board opted to allow physicians to check ‘no’ on the question about current mental health and or substance issues if they had voluntarily sought assistance from the North Dakota Professional Health Program or a professional health program in another state. The approach preserves anonymity. The question as previously phrased made some physicians feel they had to report their treatment, she said.
In Alabama, physicians also have the option to check “no” on questions about whether they are undergoing mental health treatment if they are participating in a professional assistance program. Mark Jackson, executive director of the Medical Association of Alabama, said he hopes more states give physicians this option for seeking help not only with mental health issues, but with addiction as well.
“You need to get people in and get them help and not jeopardize their career in the process. Society in general has got that problem going on and physicians are not immune from that,” Mr. Jackson said. “Hopefully other states will see that we need to do something to make sure that the physician population is taken care of.”
Pamela Wible, MD, an advocate for physicians’ mental health, did her own review of state board’s licensing questions. In an assessment posted on her website, Dr. Wible, who practices family medicine, gives 13 states an “A” grade for having no mental health questions or one or two straightforward current questions about impairment that do not mention mental health. “Connecticut, Hawaii, Michigan, and New York are the most physician-friendly of all states with no mental health or impairment questions,” Dr. Wible wrote.
The Texas Medical Board earned a “C” grade in Dr. Wible’s survey. In May 2019, that board’s chairman, Sherif Zaafran, MD, wrote about how his organization had taken a new look at the licensing questions, which were last revised in 2014. While the board has not decided on any immediate changes, it is “maintaining an open dialogue to address future concerns,” Dr. Zaafran wrote in the board’s bulletin.
The Texas Medical Board’s physician licensing form, as posted on its website, includes a broadly phrased question on mental health: “Within the past five (5) years, have you been diagnosed with or treated for any: psychotic disorder, delusional disorder, mood disorder, major depression, personality disorder, or any other mental condition which impaired or does impair your behavior, judgment, or ability to function in school or work?”
Physicians who have had treatment for mental health conditions then must submit another form. They may have to provide details on diagnosis, prognosis, and medications prescribed. Compliance requirements include counseling records, contracts with impairment support groups, and records on file with law enforcement agencies and licensing agencies.
State officials are trying to figure out how best to learn of potential impairments that could pose a risk for patients, without scaring physicians away from getting the care they themselves need said Stephen ‘Brint’ Carlton, JD, executive director of the Texas Medical Board.
Delicia M. Haynes, MD, wants the Florida Board of Medicine to take another look at how its licensing applications query physicians about their mental health history. Her state’s board is one of several nationwide that has, in recent years, mulled whether the phrasing of its questions poses an unintended hurdle for physicians who need help for conditions such as depression.
The Federation of State Medical Boards (FSMB) recommends limiting such queries, if they must be asked, to questions about potential current impairment. But the Florida license application takes a more sweeping approach that may discourage physicians from seeking treatment, Dr. Haynes, founder and CEO of Family First Health Center in Daytona Beach, Fla., said in a video. She describes herself as a direct primary care physician.
In the video, which was posted on YouTube in January, 2019, Dr. Haynes discussed her own experience with having been treated for depression and then needing to report that to the state board. Florida’s license application asks if physicians have been treated within the past 5 years for a mental disorder that has impaired the ability to practice medicine. Those who have had such a condition may need to give the board an explanation providing the names of the physicians, therapists, and counselors they have seen, as well as details and dates for the institutions where they received treatment.
State medical boards play a critical role in protecting people from physicians whose current mental health conditions may risk harming patients, Dr. Haynes said. But they must balance that against the consequences of overly intrusive questioning. Florida’s current application wording may deter physicians from seeking care if they develop conditions such as depression, she said.
“It’s the fear of what’s going to happen if I have to check yes,” Dr. Haynes said in her YouTube video. Physicians will wonder how getting treatment could put their license and their employment at risk, she added.
“It’s really important that [state medical boards] are asking the questions that matter and those questions are questions that talk about impairment, and not just having a history,” Dr. Haynes said.
Members of Florida’s board of medicine last year favorably discussed making such a change during a rules/legislative committee meeting, but have not yet implemented it. The board has postponed further discussion of this topic until its December meeting, said Brad Dalton, a spokesman for the Florida Department of Health.
Dr. Haynes said in an email that she will continue to press for changes in her state’s licensing application.
There’s been a wave of reconsideration of these kinds of questions, spurred by FSMB efforts, which included the board’s offering specific advice to state medical boards about questions on licensing applications as part of a set of recommendations on addressing physician wellness and burnout last year in a report.
Boards have the option of omitting or dropping specific inquiries about mental health. But if they choose to retain this question, FSMB recommends using this phrasing: “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner? (Yes/No)” the report says.
The staff of the Medical Board of California cited FSMB’s recommendation in a January 2019 report about revising the state’s approach to asking physicians about their mental health. In May 2019, the board voted unanimously to revise its questions on physicians’ mental health, narrowing its inquiry on the licensing application to focus on current impairment.
“There are many doctors who do not seek treatment or find it threatening to seek treatment, because they are concerned that they may lose their license,” Peter Yellowlees, MBBS, MD, chief wellness officer and a professor of psychiatry at University of California, Davis, said in a public comment offered at the meeting. “This is ultimately all about patient safety.”
said Joe Knickrehm, a spokesman for the FSMB. Over the past few years, Kentucky, New Hampshire, New Mexico, North Carolina, North Dakota, Ohio, Vermont and Washington have made changes to their licensing questions, he added.
Still, state boards are not moving quickly enough to remove or revise these questions about mental health, said Katherine J. Gold, MD MSW, associate professor in the department of family medicine at University of Michigan, Ann Arbor. She has studied how these queries can deter physicians from seeking treatment for mental illness. A past treatment for postpartum depression may have no bearing on a physician’s practice, yet members of many state medical boards hesitate to alter their approach, she noted.
Groups including the American Medical Association (AMA) and the American Psychiatric Association also have pushed in recent years for changes in state rules about what a physician has to disclose about mental health, with the FSMB taking a lead in these efforts. In many cases, physicians face questions about their mental health that are beyond the limits of standards set by the Americans With Disabilities Act, according to an article published this year in the FSMB’s Journal of Medical Regulation. As of 2017, a review of questions on initial licensure applications for all 50 states and the District of Columbia showed that 32 licensing boards ask questions beyond the limits of ADA standards, the article said.
Consequences of “reporting stable and easily treatable conditions such as anxiety or depression to a state licensing board can range from a physician simply being required to submit a letter from their primary care provider documenting fitness to practice, to a request to appear before the board, to being required to undergo and pay for an examination by a board-appointed physician,” wrote Catherine M. Welcher, an AMA senior policy analyst, and coauthors of the paper, including Humayun J. Chaudhry, DO, FSMB’s CEO.
Nearly 40% of physicians surveyed about medical licensing questions (2,325 of 5,829) indicated they would be reluctant to seek formal medical care for a mental health condition because of potential repercussions, Liselotte N. Dyrbye, MD, and coauthors reported in 2017 in the Mayo Clinic Proceedings.
“You’re sort of stuck. You recognize you have a problem and you want to seek care so that you can get better, but if you do that, you might have to tell the board,” Dr. Dyrbye said in an interview. “You could be mandated potentially to have an outside psychiatric evaluation, to have your personal medical records reviewed by people other than your personal physician.”
Rising levels of burnout among physicians make it critical to remove obstacles to care, said Arthur S. Hengerer, MD, a former chair of the FSMB who has been a leader in efforts to revise medical licensing questions.
“The only thing that really brings joy to medicine are the relationships you develop with patients, the trust that comes from that, and when you can’t develop relationships because you can’t spend the time, because you are clicking and documenting, it hurts,” said Andrew Lamb, MD, who aided in successful efforts to change North Carolina’s licensing questions.
North Carolina approached this issue in steps. In 2017, it removed a question about mental health from its annual physician license renewal form. In 2018, the North Carolina Medical Board voted to drop questions about mental and physical health from physician license applications.
“It’s hoped that removing this question will encourage clinicians to get the help they need, without fear it will compromise their chances to obtain a professional license,” the board said in an annual report.
Other states are retaining these questions, but allowing physicians to check “no” if they are in an approved program for mental health treatment. The North Dakota Board of Medicine took this approach.
“Because our mission is protection of the public, we didn’t feel that we could eliminate that question,” Bonnie Storbakken, JD, executive secretary of the North Dakota Board of Medicine, said in an interview.
The North Dakota board voted in March 2018 to change its question on mental health after the FSMB spurred a national dialogue on this issue, she said. The North Dakota board opted to allow physicians to check ‘no’ on the question about current mental health and or substance issues if they had voluntarily sought assistance from the North Dakota Professional Health Program or a professional health program in another state. The approach preserves anonymity. The question as previously phrased made some physicians feel they had to report their treatment, she said.
In Alabama, physicians also have the option to check “no” on questions about whether they are undergoing mental health treatment if they are participating in a professional assistance program. Mark Jackson, executive director of the Medical Association of Alabama, said he hopes more states give physicians this option for seeking help not only with mental health issues, but with addiction as well.
“You need to get people in and get them help and not jeopardize their career in the process. Society in general has got that problem going on and physicians are not immune from that,” Mr. Jackson said. “Hopefully other states will see that we need to do something to make sure that the physician population is taken care of.”
Pamela Wible, MD, an advocate for physicians’ mental health, did her own review of state board’s licensing questions. In an assessment posted on her website, Dr. Wible, who practices family medicine, gives 13 states an “A” grade for having no mental health questions or one or two straightforward current questions about impairment that do not mention mental health. “Connecticut, Hawaii, Michigan, and New York are the most physician-friendly of all states with no mental health or impairment questions,” Dr. Wible wrote.
The Texas Medical Board earned a “C” grade in Dr. Wible’s survey. In May 2019, that board’s chairman, Sherif Zaafran, MD, wrote about how his organization had taken a new look at the licensing questions, which were last revised in 2014. While the board has not decided on any immediate changes, it is “maintaining an open dialogue to address future concerns,” Dr. Zaafran wrote in the board’s bulletin.
The Texas Medical Board’s physician licensing form, as posted on its website, includes a broadly phrased question on mental health: “Within the past five (5) years, have you been diagnosed with or treated for any: psychotic disorder, delusional disorder, mood disorder, major depression, personality disorder, or any other mental condition which impaired or does impair your behavior, judgment, or ability to function in school or work?”
Physicians who have had treatment for mental health conditions then must submit another form. They may have to provide details on diagnosis, prognosis, and medications prescribed. Compliance requirements include counseling records, contracts with impairment support groups, and records on file with law enforcement agencies and licensing agencies.
State officials are trying to figure out how best to learn of potential impairments that could pose a risk for patients, without scaring physicians away from getting the care they themselves need said Stephen ‘Brint’ Carlton, JD, executive director of the Texas Medical Board.
TKI preserved lung function in patients with fibrosing interstitial disease
MADRID – according to findings from a phase 3, placebo-controlled trial presented at the annual congress of the European Respiratory Society.
The trial, called INBUILD, enrolled patients who had a progressive lung disease with a fibrosing phenotype, such as interstitial pneumonia with autoimmune features (IPAF) or noninterstitial pneumonia (NSIP), on the premise that these conditions might share a pathology responsive to a common therapy, explained Kevin R. Flaherty, MD, of National Jewish Health, Denver. The INBUILD trial was a randomized, double-blind, placebo-controlled, parallel-group trial conducted at 153 sites in 15 countries. A total of 663 patients underwent randomization and received at least one dose of nintedanib (332) or placebo (331).
Patients with fibrosing lung disease affecting more than 10% of lung volume were randomized to 150 mg twice daily of nintedanib, which inhibits intracellular growth factors implicated in fibrosis and is already indicated for IPF, or matching placebo.
On the primary endpoint of change in forced vital capacity (FVC) at 52 weeks, those in the nintedanib arm lost lung function at a rate that was less than half that of those randomized to placebo (–80.8 vs. –187.8 mL/year; P less than .001).
In a preplanned stratification, the protection from nintedanib against a decline in lung function was found to be at least as good in those with a usual interstitial pneumonia (UIP-like) pattern of fibrosis on baseline imaging (–82.9 vs. –211.1 mL/year), compared with those with other fibrotic patterns (–79.0 vs. –154.2 mL/year). The UIP-like subgroup represented about 60% of those enrolled.
“The relative protection from decline in lung function supports the hypothesis that progressive fibrosing interstitial lung diseases have a similar pathobiologic mechanism,” said Dr. Flaherty. Results from the INBUILD were published simultaneously with his ERS presentation (N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681).
The curves documenting change of lung function in favor of nintedanib relative to placebo separated within 12 weeks of treatment initiation, according to Dr. Flaherty. The ERS-invited discussant, Martin Kolb, MD, PhD, professor of respirology, McMaster University, Hamilton, Ont., called the reductions in loss of lung function “profound” and “very impactful.”
However, despite these reductions, there was no significant difference in quality of life as measured with the King’s Brief Interstitial Lung Disease (KBILD) questionnaire, which was a secondary outcome. The problem was that there was little change in KBILD in either group at 52 weeks, limiting the ability to show differences.
The rates of death were numerically lower at 52 weeks in the nintedanib arm for the study overall (4.8% vs. 5.1%) and for the UIP-like subgroup (5.3% vs. 7.8%), but the differences did not reach statistical significance.
A suggestion of benefit was derived from a design feature of INBUILD that called for patients to remain on blinded therapy until all enrolled patients completed the trial. When the effect of nintedanib was evaluated in this extended analysis, the event curves for the combined endpoint of interstitial lung disease or death separated and approached significance.
In this extended analysis, which suggests that clinical benefit is likely to accrue after longer periods of treatment, “we saw similar trends when we looked at mortality as an independent outcome,” Dr. Flaherty reported.
More patients in the nintedanib group discontinued therapy because of adverse events (19.6% vs. 10.3%), but Dr. Flaherty characterized the rate of serious adverse events as “similar.” He made this statement even though several adverse events, particularly those involving the gastrointestinal tract, such as diarrhea (66.9% vs. 23.9%), nausea (28.9% vs. 9.4%), vomiting (18.4% vs. 5.1%), and abdominal pain (10.2% vs. 2.4%), were higher in the nintedanib arm.
The INBUILD trial demonstrates that nintedanib preserves lung function in fibrosing lung diseases other than IPF. In his review of this paper, Dr. Kolb pointed out that non-IPF etiologies represent about 75% of interstitial lung diseases. For these patients “we have no drugs, so there is a big medical need.”
Dr. Flaherty reports no potential conflicts of interest. The study was funded by Boehringer-Ingelheim, which produces nintedanib.
SOURCE: Flaherty KR et al. N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681.
MADRID – according to findings from a phase 3, placebo-controlled trial presented at the annual congress of the European Respiratory Society.
The trial, called INBUILD, enrolled patients who had a progressive lung disease with a fibrosing phenotype, such as interstitial pneumonia with autoimmune features (IPAF) or noninterstitial pneumonia (NSIP), on the premise that these conditions might share a pathology responsive to a common therapy, explained Kevin R. Flaherty, MD, of National Jewish Health, Denver. The INBUILD trial was a randomized, double-blind, placebo-controlled, parallel-group trial conducted at 153 sites in 15 countries. A total of 663 patients underwent randomization and received at least one dose of nintedanib (332) or placebo (331).
Patients with fibrosing lung disease affecting more than 10% of lung volume were randomized to 150 mg twice daily of nintedanib, which inhibits intracellular growth factors implicated in fibrosis and is already indicated for IPF, or matching placebo.
On the primary endpoint of change in forced vital capacity (FVC) at 52 weeks, those in the nintedanib arm lost lung function at a rate that was less than half that of those randomized to placebo (–80.8 vs. –187.8 mL/year; P less than .001).
In a preplanned stratification, the protection from nintedanib against a decline in lung function was found to be at least as good in those with a usual interstitial pneumonia (UIP-like) pattern of fibrosis on baseline imaging (–82.9 vs. –211.1 mL/year), compared with those with other fibrotic patterns (–79.0 vs. –154.2 mL/year). The UIP-like subgroup represented about 60% of those enrolled.
“The relative protection from decline in lung function supports the hypothesis that progressive fibrosing interstitial lung diseases have a similar pathobiologic mechanism,” said Dr. Flaherty. Results from the INBUILD were published simultaneously with his ERS presentation (N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681).
The curves documenting change of lung function in favor of nintedanib relative to placebo separated within 12 weeks of treatment initiation, according to Dr. Flaherty. The ERS-invited discussant, Martin Kolb, MD, PhD, professor of respirology, McMaster University, Hamilton, Ont., called the reductions in loss of lung function “profound” and “very impactful.”
However, despite these reductions, there was no significant difference in quality of life as measured with the King’s Brief Interstitial Lung Disease (KBILD) questionnaire, which was a secondary outcome. The problem was that there was little change in KBILD in either group at 52 weeks, limiting the ability to show differences.
The rates of death were numerically lower at 52 weeks in the nintedanib arm for the study overall (4.8% vs. 5.1%) and for the UIP-like subgroup (5.3% vs. 7.8%), but the differences did not reach statistical significance.
A suggestion of benefit was derived from a design feature of INBUILD that called for patients to remain on blinded therapy until all enrolled patients completed the trial. When the effect of nintedanib was evaluated in this extended analysis, the event curves for the combined endpoint of interstitial lung disease or death separated and approached significance.
In this extended analysis, which suggests that clinical benefit is likely to accrue after longer periods of treatment, “we saw similar trends when we looked at mortality as an independent outcome,” Dr. Flaherty reported.
More patients in the nintedanib group discontinued therapy because of adverse events (19.6% vs. 10.3%), but Dr. Flaherty characterized the rate of serious adverse events as “similar.” He made this statement even though several adverse events, particularly those involving the gastrointestinal tract, such as diarrhea (66.9% vs. 23.9%), nausea (28.9% vs. 9.4%), vomiting (18.4% vs. 5.1%), and abdominal pain (10.2% vs. 2.4%), were higher in the nintedanib arm.
The INBUILD trial demonstrates that nintedanib preserves lung function in fibrosing lung diseases other than IPF. In his review of this paper, Dr. Kolb pointed out that non-IPF etiologies represent about 75% of interstitial lung diseases. For these patients “we have no drugs, so there is a big medical need.”
Dr. Flaherty reports no potential conflicts of interest. The study was funded by Boehringer-Ingelheim, which produces nintedanib.
SOURCE: Flaherty KR et al. N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681.
MADRID – according to findings from a phase 3, placebo-controlled trial presented at the annual congress of the European Respiratory Society.
The trial, called INBUILD, enrolled patients who had a progressive lung disease with a fibrosing phenotype, such as interstitial pneumonia with autoimmune features (IPAF) or noninterstitial pneumonia (NSIP), on the premise that these conditions might share a pathology responsive to a common therapy, explained Kevin R. Flaherty, MD, of National Jewish Health, Denver. The INBUILD trial was a randomized, double-blind, placebo-controlled, parallel-group trial conducted at 153 sites in 15 countries. A total of 663 patients underwent randomization and received at least one dose of nintedanib (332) or placebo (331).
Patients with fibrosing lung disease affecting more than 10% of lung volume were randomized to 150 mg twice daily of nintedanib, which inhibits intracellular growth factors implicated in fibrosis and is already indicated for IPF, or matching placebo.
On the primary endpoint of change in forced vital capacity (FVC) at 52 weeks, those in the nintedanib arm lost lung function at a rate that was less than half that of those randomized to placebo (–80.8 vs. –187.8 mL/year; P less than .001).
In a preplanned stratification, the protection from nintedanib against a decline in lung function was found to be at least as good in those with a usual interstitial pneumonia (UIP-like) pattern of fibrosis on baseline imaging (–82.9 vs. –211.1 mL/year), compared with those with other fibrotic patterns (–79.0 vs. –154.2 mL/year). The UIP-like subgroup represented about 60% of those enrolled.
“The relative protection from decline in lung function supports the hypothesis that progressive fibrosing interstitial lung diseases have a similar pathobiologic mechanism,” said Dr. Flaherty. Results from the INBUILD were published simultaneously with his ERS presentation (N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681).
The curves documenting change of lung function in favor of nintedanib relative to placebo separated within 12 weeks of treatment initiation, according to Dr. Flaherty. The ERS-invited discussant, Martin Kolb, MD, PhD, professor of respirology, McMaster University, Hamilton, Ont., called the reductions in loss of lung function “profound” and “very impactful.”
However, despite these reductions, there was no significant difference in quality of life as measured with the King’s Brief Interstitial Lung Disease (KBILD) questionnaire, which was a secondary outcome. The problem was that there was little change in KBILD in either group at 52 weeks, limiting the ability to show differences.
The rates of death were numerically lower at 52 weeks in the nintedanib arm for the study overall (4.8% vs. 5.1%) and for the UIP-like subgroup (5.3% vs. 7.8%), but the differences did not reach statistical significance.
A suggestion of benefit was derived from a design feature of INBUILD that called for patients to remain on blinded therapy until all enrolled patients completed the trial. When the effect of nintedanib was evaluated in this extended analysis, the event curves for the combined endpoint of interstitial lung disease or death separated and approached significance.
In this extended analysis, which suggests that clinical benefit is likely to accrue after longer periods of treatment, “we saw similar trends when we looked at mortality as an independent outcome,” Dr. Flaherty reported.
More patients in the nintedanib group discontinued therapy because of adverse events (19.6% vs. 10.3%), but Dr. Flaherty characterized the rate of serious adverse events as “similar.” He made this statement even though several adverse events, particularly those involving the gastrointestinal tract, such as diarrhea (66.9% vs. 23.9%), nausea (28.9% vs. 9.4%), vomiting (18.4% vs. 5.1%), and abdominal pain (10.2% vs. 2.4%), were higher in the nintedanib arm.
The INBUILD trial demonstrates that nintedanib preserves lung function in fibrosing lung diseases other than IPF. In his review of this paper, Dr. Kolb pointed out that non-IPF etiologies represent about 75% of interstitial lung diseases. For these patients “we have no drugs, so there is a big medical need.”
Dr. Flaherty reports no potential conflicts of interest. The study was funded by Boehringer-Ingelheim, which produces nintedanib.
SOURCE: Flaherty KR et al. N Engl J Med. 2019 Sep 29. doi: 10.1056/NEJMoa1908681.
REPORTING FROM ERS 2019
Direct-acting antiviral therapy boosts survival for infected HCC patients
Direct-acting antiviral (DAA) therapy significantly reduced the risk of death in patients with hepatitis C infections and a history of hepatocellular carcinoma, based on data from 797 individuals.
Previous studies have reported a benefit of direct-acting antiviral (DAA) therapy for reducing mortality in patients with hepatocellular carcinoma (HCC), but data on its impact in patients with complete responses to HCC therapy are limited, wrote Amit G. Singal, MD, of the University of Texas, Dallas, and colleagues.
In a study published in Gastroenterology, the researchers identified adult HCC patients who achieved complete treatment response between January 2013 and December 2017. The study included patients from 31 locations in the United States and Canada. Complete response to treatment was defined as “disappearance of arterial enhancement from all HCC lesions on contrast-enhanced cross-sectional imaging.”
A total of 383 (48.1%) of patients were randomized to DAA therapy, and 414 (51.9%) did not receive DAA treatment for their HCV infection after complete response to prior HCC therapy.
A total of 43 deaths occurred among DAA patients over 941 person-years of follow-up, compared with 103 deaths over 527 person-years of follow-up for the untreated controls. Overall, DAA therapy was associated with a significantly reduced risk of death (hazard ratio, 0.54), compared with no therapy. Of note, patients with a sustained virologic response showed a reduced risk of death (HR, 0.29), but those without a sustained virologic response to DAA therapy did not (HR, 1.13).
The findings support those from previous studies suggesting that DAA therapy may reduce mortality in patients with a history of HCC, the researchers said.
The study findings were limited by several factors, including potential confounding if DAA was given to patients with better prognoses, the researchers noted. Other limitations include the use of imaging in routine clinical care rather than centralized review, the loss of approximately 9% of the patients to follow-up, and the lack of data on hepatic decompensation during follow-up, the researchers said. However, the results were strengthened by the multicenter design, large cohort, and inclusion of untreated controls, and support the use of DAA therapies as “likely beneficial in HCV-infected patients with a history of HCC,” they concluded.
The study was funded in part by the National Cancer Institute and AbbVie. Dr. Singal disclosed relationships with companies including AbbVie, Gilead, Bayer, Eisai, Wako Diagnostics, Exact Sciences, Exelixis, Roche, Glycotest, and Bristol-Myers Squibb.
SOURCE: Singal AG et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.07.040.
Direct-acting antiviral (DAA) therapy significantly reduced the risk of death in patients with hepatitis C infections and a history of hepatocellular carcinoma, based on data from 797 individuals.
Previous studies have reported a benefit of direct-acting antiviral (DAA) therapy for reducing mortality in patients with hepatocellular carcinoma (HCC), but data on its impact in patients with complete responses to HCC therapy are limited, wrote Amit G. Singal, MD, of the University of Texas, Dallas, and colleagues.
In a study published in Gastroenterology, the researchers identified adult HCC patients who achieved complete treatment response between January 2013 and December 2017. The study included patients from 31 locations in the United States and Canada. Complete response to treatment was defined as “disappearance of arterial enhancement from all HCC lesions on contrast-enhanced cross-sectional imaging.”
A total of 383 (48.1%) of patients were randomized to DAA therapy, and 414 (51.9%) did not receive DAA treatment for their HCV infection after complete response to prior HCC therapy.
A total of 43 deaths occurred among DAA patients over 941 person-years of follow-up, compared with 103 deaths over 527 person-years of follow-up for the untreated controls. Overall, DAA therapy was associated with a significantly reduced risk of death (hazard ratio, 0.54), compared with no therapy. Of note, patients with a sustained virologic response showed a reduced risk of death (HR, 0.29), but those without a sustained virologic response to DAA therapy did not (HR, 1.13).
The findings support those from previous studies suggesting that DAA therapy may reduce mortality in patients with a history of HCC, the researchers said.
The study findings were limited by several factors, including potential confounding if DAA was given to patients with better prognoses, the researchers noted. Other limitations include the use of imaging in routine clinical care rather than centralized review, the loss of approximately 9% of the patients to follow-up, and the lack of data on hepatic decompensation during follow-up, the researchers said. However, the results were strengthened by the multicenter design, large cohort, and inclusion of untreated controls, and support the use of DAA therapies as “likely beneficial in HCV-infected patients with a history of HCC,” they concluded.
The study was funded in part by the National Cancer Institute and AbbVie. Dr. Singal disclosed relationships with companies including AbbVie, Gilead, Bayer, Eisai, Wako Diagnostics, Exact Sciences, Exelixis, Roche, Glycotest, and Bristol-Myers Squibb.
SOURCE: Singal AG et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.07.040.
Direct-acting antiviral (DAA) therapy significantly reduced the risk of death in patients with hepatitis C infections and a history of hepatocellular carcinoma, based on data from 797 individuals.
Previous studies have reported a benefit of direct-acting antiviral (DAA) therapy for reducing mortality in patients with hepatocellular carcinoma (HCC), but data on its impact in patients with complete responses to HCC therapy are limited, wrote Amit G. Singal, MD, of the University of Texas, Dallas, and colleagues.
In a study published in Gastroenterology, the researchers identified adult HCC patients who achieved complete treatment response between January 2013 and December 2017. The study included patients from 31 locations in the United States and Canada. Complete response to treatment was defined as “disappearance of arterial enhancement from all HCC lesions on contrast-enhanced cross-sectional imaging.”
A total of 383 (48.1%) of patients were randomized to DAA therapy, and 414 (51.9%) did not receive DAA treatment for their HCV infection after complete response to prior HCC therapy.
A total of 43 deaths occurred among DAA patients over 941 person-years of follow-up, compared with 103 deaths over 527 person-years of follow-up for the untreated controls. Overall, DAA therapy was associated with a significantly reduced risk of death (hazard ratio, 0.54), compared with no therapy. Of note, patients with a sustained virologic response showed a reduced risk of death (HR, 0.29), but those without a sustained virologic response to DAA therapy did not (HR, 1.13).
The findings support those from previous studies suggesting that DAA therapy may reduce mortality in patients with a history of HCC, the researchers said.
The study findings were limited by several factors, including potential confounding if DAA was given to patients with better prognoses, the researchers noted. Other limitations include the use of imaging in routine clinical care rather than centralized review, the loss of approximately 9% of the patients to follow-up, and the lack of data on hepatic decompensation during follow-up, the researchers said. However, the results were strengthened by the multicenter design, large cohort, and inclusion of untreated controls, and support the use of DAA therapies as “likely beneficial in HCV-infected patients with a history of HCC,” they concluded.
The study was funded in part by the National Cancer Institute and AbbVie. Dr. Singal disclosed relationships with companies including AbbVie, Gilead, Bayer, Eisai, Wako Diagnostics, Exact Sciences, Exelixis, Roche, Glycotest, and Bristol-Myers Squibb.
SOURCE: Singal AG et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.07.040.
FROM GASTROENTEROLOGY
NICUs admitting more normal-weight newborns
Almost half of the newborns admitted to U.S. neonatal intensive care units in 2017 were of normal birth weight, according to a new report from the Dartmouth Institute for Health Policy & Clinical Practice.
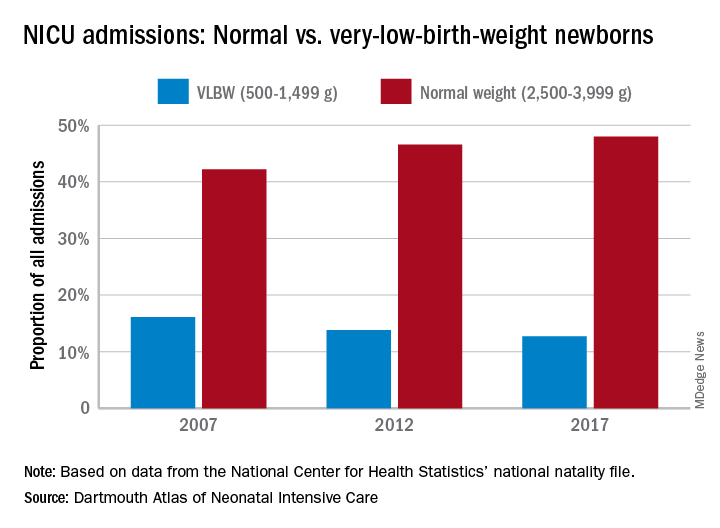
The proportion of NICU admissions involving normal-weight (2,500-3,999 g) newborns increased from 42% in 2007 to 48% in 2017, investigators said in the Dartmouth Atlas of Neonatal Intensive Care. Over that same period, admissions of very-low-birth-weight (500-1,499 g) babies dropped from 16% to 13% of the total.
Those changes were part of a larger, longer-term trend. “The expansion of NICUs and beds in recent decades has been associated with changes in the newborn population receiving NICU care,” the investigators said in the report.
The number of NICU beds increased by 65% from 1995 to 2013, and the number of neonatologists rose by 75% from 1996 to 2013. “At the same time, ” they said in a written statement.
The increases in NICU and neonatologist supply, however, did not always follow the need for such care. Areas of the country with high rates of newborn prematurity, or of risk factors such as low maternal education levels or high cesarean section rates, do not have higher supplies of NICU beds or neonatologists, the researchers noted.
“We should not spare a dollar in providing the best care for newborns. But spending more doesn’t help infants if they could receive the care they need in a maternity unit or home with their mothers. It is very troubling that such a valuable and expensive health care resource is not distributed where it is needed,” said principal author David C. Goodman, MD, of the Dartmouth Institute for Health Policy & Clinical Practice in Lebanon, N.H.
Almost half of the newborns admitted to U.S. neonatal intensive care units in 2017 were of normal birth weight, according to a new report from the Dartmouth Institute for Health Policy & Clinical Practice.
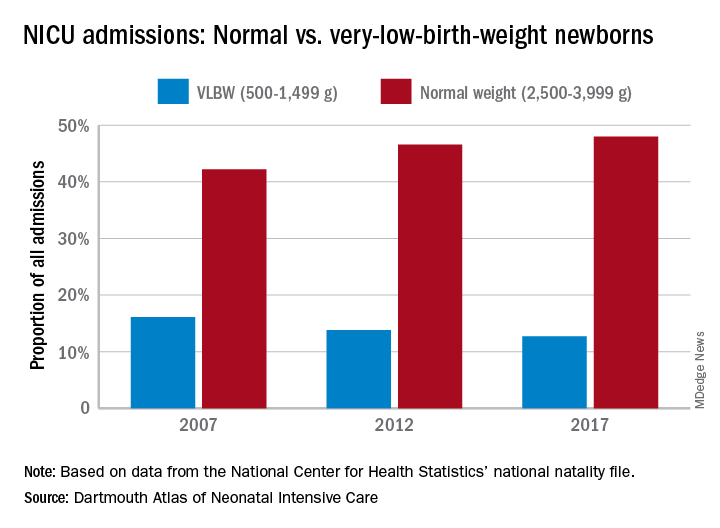
The proportion of NICU admissions involving normal-weight (2,500-3,999 g) newborns increased from 42% in 2007 to 48% in 2017, investigators said in the Dartmouth Atlas of Neonatal Intensive Care. Over that same period, admissions of very-low-birth-weight (500-1,499 g) babies dropped from 16% to 13% of the total.
Those changes were part of a larger, longer-term trend. “The expansion of NICUs and beds in recent decades has been associated with changes in the newborn population receiving NICU care,” the investigators said in the report.
The number of NICU beds increased by 65% from 1995 to 2013, and the number of neonatologists rose by 75% from 1996 to 2013. “At the same time, ” they said in a written statement.
The increases in NICU and neonatologist supply, however, did not always follow the need for such care. Areas of the country with high rates of newborn prematurity, or of risk factors such as low maternal education levels or high cesarean section rates, do not have higher supplies of NICU beds or neonatologists, the researchers noted.
“We should not spare a dollar in providing the best care for newborns. But spending more doesn’t help infants if they could receive the care they need in a maternity unit or home with their mothers. It is very troubling that such a valuable and expensive health care resource is not distributed where it is needed,” said principal author David C. Goodman, MD, of the Dartmouth Institute for Health Policy & Clinical Practice in Lebanon, N.H.
Almost half of the newborns admitted to U.S. neonatal intensive care units in 2017 were of normal birth weight, according to a new report from the Dartmouth Institute for Health Policy & Clinical Practice.
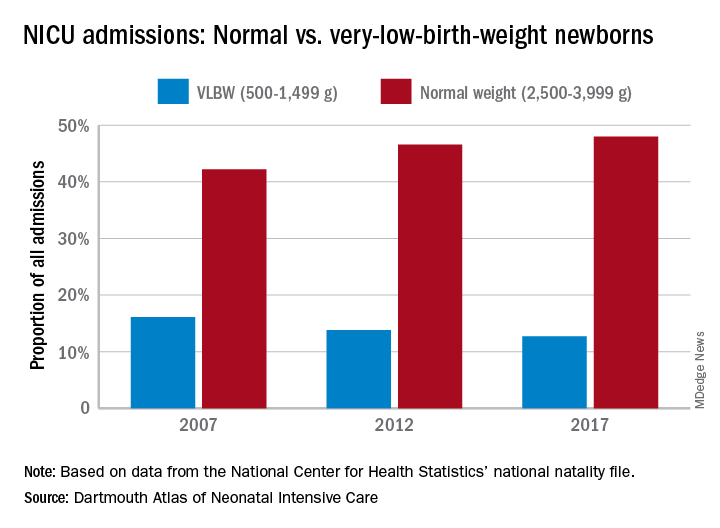
The proportion of NICU admissions involving normal-weight (2,500-3,999 g) newborns increased from 42% in 2007 to 48% in 2017, investigators said in the Dartmouth Atlas of Neonatal Intensive Care. Over that same period, admissions of very-low-birth-weight (500-1,499 g) babies dropped from 16% to 13% of the total.
Those changes were part of a larger, longer-term trend. “The expansion of NICUs and beds in recent decades has been associated with changes in the newborn population receiving NICU care,” the investigators said in the report.
The number of NICU beds increased by 65% from 1995 to 2013, and the number of neonatologists rose by 75% from 1996 to 2013. “At the same time, ” they said in a written statement.
The increases in NICU and neonatologist supply, however, did not always follow the need for such care. Areas of the country with high rates of newborn prematurity, or of risk factors such as low maternal education levels or high cesarean section rates, do not have higher supplies of NICU beds or neonatologists, the researchers noted.
“We should not spare a dollar in providing the best care for newborns. But spending more doesn’t help infants if they could receive the care they need in a maternity unit or home with their mothers. It is very troubling that such a valuable and expensive health care resource is not distributed where it is needed,” said principal author David C. Goodman, MD, of the Dartmouth Institute for Health Policy & Clinical Practice in Lebanon, N.H.