User login
Hospital medicine grows globally
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
In transgender care, questions are the answer
New York OBGYN Zoe I. Rodriguez, MD, a pioneer in the care of transgender people, has witnessed a remarkable evolution in medicine.
Years ago, providers knew little to nothing about the unique needs of transgender patients. Now, Dr. Rodriguez said, “there’s tremendous interest in being able to competently treat and address transgender individuals.”
But increased awareness has come with a dose of worry. Providers are often afraid they’ll say or do the wrong thing.
Dr. Rodriguez, who is an assistant professor at the Icahn School of Medicine at Mount Sinai, New York, will help hospitalists gain confidence in treating transgender patients at an HM19 session on Tuesday. “I hope to eliminate this element of fear,” she said. “It’s just really about treating people with respect and dignity and having the knowledge to care for them appropriately.”
The United States is home to an estimated 1.4 million transgender people, and every one has a preferred name and preferred pronouns. It’s crucial for physicians to understand name and pronoun preferences and use them, Dr. Rodriguez said.
At her practice, an intake form asks patients how they wish to be addressed. “I know this information by the time I walk into the exam room,” she said.
For hospitalists, she said, getting this information beforehand may not be possible. In that case, she said, ask questions of the patient and don’t be afraid to get it wrong.
“Mistakes happen all the time,” Dr. Rodriguez said. “People will correct you if you misgender them or call them other than their preferred name. As long as the mistakes are not willful, apologize and move on.”
It’s also important to understand the special needs that transgender patients may – or may not – have. For example, not every transgender patient takes hormones. Even if a patient does, the hormones may not affect as many body processes as you might assume, Dr. Rodriguez said.
Also, not every transgender person has had surgery. However, it can be helpful to understand what surgery entails. “If they get their surgery done in Thailand, a popular destination, and they need treatment in Topeka for an issue related to their surgery, it would be good for the hospitalist to understand what’s done during the surgery.”
In her session, Dr. Rodriguez will also talk about creating an LGBT-friendly environment. “These patients are already feeling very vulnerable and marginalized within these vast health systems,” she said. “It makes a big difference to know that someone is there and gets it.”
Dr. Rodriguez also plans to emphasize the importance of staying aware and up to date about transgender issues. “It’s a continuum,” she said. “There will be more evolution as people come up with new terminologies and words to describe their gender expression and identity. It will be crucially important for physicians to be aware and respectful.”
What Hospitalists Need to Know About Caring for Transgender Patients
Tuesday, 3:50 - 4:30 p.m.
Maryland A/1-3
New York OBGYN Zoe I. Rodriguez, MD, a pioneer in the care of transgender people, has witnessed a remarkable evolution in medicine.
Years ago, providers knew little to nothing about the unique needs of transgender patients. Now, Dr. Rodriguez said, “there’s tremendous interest in being able to competently treat and address transgender individuals.”
But increased awareness has come with a dose of worry. Providers are often afraid they’ll say or do the wrong thing.
Dr. Rodriguez, who is an assistant professor at the Icahn School of Medicine at Mount Sinai, New York, will help hospitalists gain confidence in treating transgender patients at an HM19 session on Tuesday. “I hope to eliminate this element of fear,” she said. “It’s just really about treating people with respect and dignity and having the knowledge to care for them appropriately.”
The United States is home to an estimated 1.4 million transgender people, and every one has a preferred name and preferred pronouns. It’s crucial for physicians to understand name and pronoun preferences and use them, Dr. Rodriguez said.
At her practice, an intake form asks patients how they wish to be addressed. “I know this information by the time I walk into the exam room,” she said.
For hospitalists, she said, getting this information beforehand may not be possible. In that case, she said, ask questions of the patient and don’t be afraid to get it wrong.
“Mistakes happen all the time,” Dr. Rodriguez said. “People will correct you if you misgender them or call them other than their preferred name. As long as the mistakes are not willful, apologize and move on.”
It’s also important to understand the special needs that transgender patients may – or may not – have. For example, not every transgender patient takes hormones. Even if a patient does, the hormones may not affect as many body processes as you might assume, Dr. Rodriguez said.
Also, not every transgender person has had surgery. However, it can be helpful to understand what surgery entails. “If they get their surgery done in Thailand, a popular destination, and they need treatment in Topeka for an issue related to their surgery, it would be good for the hospitalist to understand what’s done during the surgery.”
In her session, Dr. Rodriguez will also talk about creating an LGBT-friendly environment. “These patients are already feeling very vulnerable and marginalized within these vast health systems,” she said. “It makes a big difference to know that someone is there and gets it.”
Dr. Rodriguez also plans to emphasize the importance of staying aware and up to date about transgender issues. “It’s a continuum,” she said. “There will be more evolution as people come up with new terminologies and words to describe their gender expression and identity. It will be crucially important for physicians to be aware and respectful.”
What Hospitalists Need to Know About Caring for Transgender Patients
Tuesday, 3:50 - 4:30 p.m.
Maryland A/1-3
New York OBGYN Zoe I. Rodriguez, MD, a pioneer in the care of transgender people, has witnessed a remarkable evolution in medicine.
Years ago, providers knew little to nothing about the unique needs of transgender patients. Now, Dr. Rodriguez said, “there’s tremendous interest in being able to competently treat and address transgender individuals.”
But increased awareness has come with a dose of worry. Providers are often afraid they’ll say or do the wrong thing.
Dr. Rodriguez, who is an assistant professor at the Icahn School of Medicine at Mount Sinai, New York, will help hospitalists gain confidence in treating transgender patients at an HM19 session on Tuesday. “I hope to eliminate this element of fear,” she said. “It’s just really about treating people with respect and dignity and having the knowledge to care for them appropriately.”
The United States is home to an estimated 1.4 million transgender people, and every one has a preferred name and preferred pronouns. It’s crucial for physicians to understand name and pronoun preferences and use them, Dr. Rodriguez said.
At her practice, an intake form asks patients how they wish to be addressed. “I know this information by the time I walk into the exam room,” she said.
For hospitalists, she said, getting this information beforehand may not be possible. In that case, she said, ask questions of the patient and don’t be afraid to get it wrong.
“Mistakes happen all the time,” Dr. Rodriguez said. “People will correct you if you misgender them or call them other than their preferred name. As long as the mistakes are not willful, apologize and move on.”
It’s also important to understand the special needs that transgender patients may – or may not – have. For example, not every transgender patient takes hormones. Even if a patient does, the hormones may not affect as many body processes as you might assume, Dr. Rodriguez said.
Also, not every transgender person has had surgery. However, it can be helpful to understand what surgery entails. “If they get their surgery done in Thailand, a popular destination, and they need treatment in Topeka for an issue related to their surgery, it would be good for the hospitalist to understand what’s done during the surgery.”
In her session, Dr. Rodriguez will also talk about creating an LGBT-friendly environment. “These patients are already feeling very vulnerable and marginalized within these vast health systems,” she said. “It makes a big difference to know that someone is there and gets it.”
Dr. Rodriguez also plans to emphasize the importance of staying aware and up to date about transgender issues. “It’s a continuum,” she said. “There will be more evolution as people come up with new terminologies and words to describe their gender expression and identity. It will be crucially important for physicians to be aware and respectful.”
What Hospitalists Need to Know About Caring for Transgender Patients
Tuesday, 3:50 - 4:30 p.m.
Maryland A/1-3
MIPS: Nearly 20% of small/solo practices took a pay cut in first year
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
ABIM contests class-action lawsuit, asks judge to dismiss
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
‘Update in HM’ highlights top research
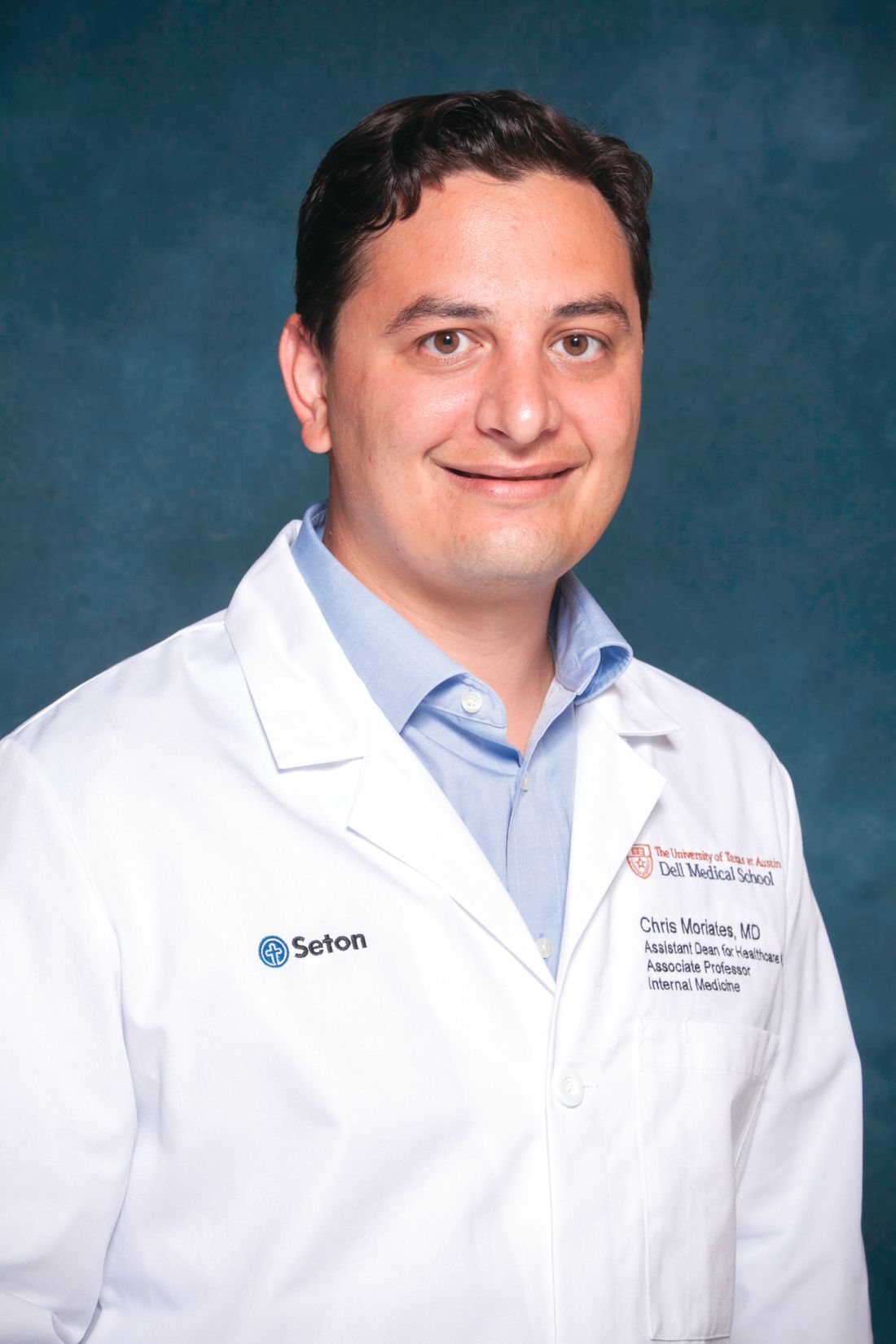
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
What’s your favorite aspect of HM19?
Attendees explain what they enjoy about the Annual Conference.

Attendees explain what they enjoy about the Annual Conference.

Attendees explain what they enjoy about the Annual Conference.

Female radiation oncologists taking in smaller Medicare payments
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
FROM JAMA NETWORK OPEN
Surge of gabapentinoids for pain lacks supporting evidence
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
FROM JAMA INTERNAL MEDICINE
Long-acting injectables noninferior to tablet integrase for HIV
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
REPORTING FROM CROI 2019
When Can You Stop Dialysis?
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.