User login
Paying Doctors Differently
Something is happening out there. Can you feel it?
It is like a small tremor before an earthquake or a brief lightning flash before a thunderstorm. It’s the signal that alerts us something is coming without indicating what it might be—ominous, promising, or revolutionary.
Our ossified, dysfunctional nonsystem of incentivizing the behavior of healthcare professionals gradually is eroding, even as the haves—the over-rewarded—cling to the past or rush to create the next procedure or modality to run by the insurance industry guardians of the dollar. The days of the system of paying for care in an a la carte manner—by the unit of the visit or performance of the procedure without consequence or reward for appropriate indications or demonstration of expected outcomes—clearly are numbered.
What will replace the current imperfect approach is not clear or perfect, but there are discernible, inexorable trends.
Performance Will Matter
Few sectors of our economy have been so devoid of standards—or, more to the point, of rewards for better service or outcomes—than healthcare.
Could you imagine paying the same for a 2008 Lexus as you would for a 1995 Toyota? Could you imagine a pricing system that couldn’t recognize or properly reward the difference between Motel 6 and the Ritz Carlton, excusing the inability to differentiate them by saying they both have beds, sheets, towels, and indoor plumbing? Today, the worst orthopedist in the country and the best are paid the same fee for a hip replacement—whether it’s indicated or not. Most patients or purchasers of healthcare have no way to know which is which.
Performance measurement and standards are here, and while imperfect and evolving, they will be with us throughout the rest of our professional careers. Whether you are in the “process” or “outcomes” camp, you and your institution will be measured. The carrot or the stick can take many forms.
Right now, it is much more than about just reporting. Disturbingly, only 30% of physicians have participated in the first round of the Physician Quality Reporting Initiative (PQRI). Look for Medicare to apply financial pressure on physicians who do not report.
On the hospital side, reporting has focused as much on embarrassment as anything. In April, every hospital received its mortality statistics for pneumonia from the Centers for Medicare and Medicaid Services (CMS). In July, these numbers will be made public. Look for a flurry of indignation and activity as hospitals try to regain the trust of their patients and assure them they indeed can manage something as basic to their core mission as pneumonia. SHM will be developing strategies to help hospitalists help their hospitals improve their performance.
Much has been made of paying for performance—and this may drive change at the hospital level. Yet, it is doubtful individual physicians will substantially change their work flow or processes, or purchase new systems for measurement, just to get an extra dollar or two for better glycemic control of their patients. What may carry more weight is if lack of performance means some physicians, or even hospitals, are restricted from performing certain procedures or caring for certain illnesses.
Bundling Episodes of Care
A move is afoot to change the unit of healthcare delivery. SHM has been in discussions with MedPAC, which advises CMS on changes to the reimbursement system, about aggregating a continuum of care as a “bundled” episode of care.
More than 15 years ago, the implementation of diagnosis-related groups (DRGs) moved hospital thinking from a la carte charging for each aspirin to managing the use of resources for the entire hospital stay, since their reimbursement was fixed. The DRG payment system as much as anything has encouraged hospitals to develop and support hospital medicine groups. Bundling would extend and expand a DRG-like concept to physicians.
Think of a future where physicians are not reimbursed for an admission work-up, three daily visits, and a discharge summary. Instead, they’d receive a global fee that might include the hospital care, transitions to the outpatient provider, and measurement of performance that might include patient satisfaction and a low readmission rate.
If we look at healthcare from the patient’s viewpoint, this is the kind of service for which they’re crying out. They want to move away from a system that even with the best providers leads to each expert doing his or her individual part well, but with voltage drops and white spaces as the patient moves through an uncoordinated non-system.
Hospitalists are in a unique position to be successful, especially as we look for strategies that align our performance with strong and engaged outpatient physicians and when we fully engage the entire healthcare team.
A Team Sport
Bundling and rewards driven by demonstrable performance create interlinking responsibilities for care among multiple physicians (primary care physicians, emergency physicians, surgeons, subspecialists, and hospitalists), as well as allied health professionals (registered nurses, nurse practitioners, physician assistants, pharmacists, therapists, social workers, and case managers).
While the makeup of the team is important, the environment in which it performs is most crucial for success. A system of healthcare delivery that focuses on and supports best practices and nudges—or forces—providers to make the right choice is of prime importance. In the end, a good system of care and one or two members of the team can save the entire enterprise, leading to the best outcome for the patient.
By the same token, a dysfunctional outlier on the team can sink everyone, including the patient. Think of the “new” healthcare as a crew team that needs a well-made boat (i.e., the system of care), a good coxswain (accountable physician), and a group of rowers, each of whom know and execute their roles. One rower can sink seven Olympians.
We are all in the boat together. We need to be clear where the finish line is and how best to get there. The future is in sight, and we need to continue to shape our role in helping the rest of the team get there. We must do this for ourselves, our profession, and—most of all—our patients today and tomorrow. TH
Dr. Wellikson is CEO of SHM.
Something is happening out there. Can you feel it?
It is like a small tremor before an earthquake or a brief lightning flash before a thunderstorm. It’s the signal that alerts us something is coming without indicating what it might be—ominous, promising, or revolutionary.
Our ossified, dysfunctional nonsystem of incentivizing the behavior of healthcare professionals gradually is eroding, even as the haves—the over-rewarded—cling to the past or rush to create the next procedure or modality to run by the insurance industry guardians of the dollar. The days of the system of paying for care in an a la carte manner—by the unit of the visit or performance of the procedure without consequence or reward for appropriate indications or demonstration of expected outcomes—clearly are numbered.
What will replace the current imperfect approach is not clear or perfect, but there are discernible, inexorable trends.
Performance Will Matter
Few sectors of our economy have been so devoid of standards—or, more to the point, of rewards for better service or outcomes—than healthcare.
Could you imagine paying the same for a 2008 Lexus as you would for a 1995 Toyota? Could you imagine a pricing system that couldn’t recognize or properly reward the difference between Motel 6 and the Ritz Carlton, excusing the inability to differentiate them by saying they both have beds, sheets, towels, and indoor plumbing? Today, the worst orthopedist in the country and the best are paid the same fee for a hip replacement—whether it’s indicated or not. Most patients or purchasers of healthcare have no way to know which is which.
Performance measurement and standards are here, and while imperfect and evolving, they will be with us throughout the rest of our professional careers. Whether you are in the “process” or “outcomes” camp, you and your institution will be measured. The carrot or the stick can take many forms.
Right now, it is much more than about just reporting. Disturbingly, only 30% of physicians have participated in the first round of the Physician Quality Reporting Initiative (PQRI). Look for Medicare to apply financial pressure on physicians who do not report.
On the hospital side, reporting has focused as much on embarrassment as anything. In April, every hospital received its mortality statistics for pneumonia from the Centers for Medicare and Medicaid Services (CMS). In July, these numbers will be made public. Look for a flurry of indignation and activity as hospitals try to regain the trust of their patients and assure them they indeed can manage something as basic to their core mission as pneumonia. SHM will be developing strategies to help hospitalists help their hospitals improve their performance.
Much has been made of paying for performance—and this may drive change at the hospital level. Yet, it is doubtful individual physicians will substantially change their work flow or processes, or purchase new systems for measurement, just to get an extra dollar or two for better glycemic control of their patients. What may carry more weight is if lack of performance means some physicians, or even hospitals, are restricted from performing certain procedures or caring for certain illnesses.
Bundling Episodes of Care
A move is afoot to change the unit of healthcare delivery. SHM has been in discussions with MedPAC, which advises CMS on changes to the reimbursement system, about aggregating a continuum of care as a “bundled” episode of care.
More than 15 years ago, the implementation of diagnosis-related groups (DRGs) moved hospital thinking from a la carte charging for each aspirin to managing the use of resources for the entire hospital stay, since their reimbursement was fixed. The DRG payment system as much as anything has encouraged hospitals to develop and support hospital medicine groups. Bundling would extend and expand a DRG-like concept to physicians.
Think of a future where physicians are not reimbursed for an admission work-up, three daily visits, and a discharge summary. Instead, they’d receive a global fee that might include the hospital care, transitions to the outpatient provider, and measurement of performance that might include patient satisfaction and a low readmission rate.
If we look at healthcare from the patient’s viewpoint, this is the kind of service for which they’re crying out. They want to move away from a system that even with the best providers leads to each expert doing his or her individual part well, but with voltage drops and white spaces as the patient moves through an uncoordinated non-system.
Hospitalists are in a unique position to be successful, especially as we look for strategies that align our performance with strong and engaged outpatient physicians and when we fully engage the entire healthcare team.
A Team Sport
Bundling and rewards driven by demonstrable performance create interlinking responsibilities for care among multiple physicians (primary care physicians, emergency physicians, surgeons, subspecialists, and hospitalists), as well as allied health professionals (registered nurses, nurse practitioners, physician assistants, pharmacists, therapists, social workers, and case managers).
While the makeup of the team is important, the environment in which it performs is most crucial for success. A system of healthcare delivery that focuses on and supports best practices and nudges—or forces—providers to make the right choice is of prime importance. In the end, a good system of care and one or two members of the team can save the entire enterprise, leading to the best outcome for the patient.
By the same token, a dysfunctional outlier on the team can sink everyone, including the patient. Think of the “new” healthcare as a crew team that needs a well-made boat (i.e., the system of care), a good coxswain (accountable physician), and a group of rowers, each of whom know and execute their roles. One rower can sink seven Olympians.
We are all in the boat together. We need to be clear where the finish line is and how best to get there. The future is in sight, and we need to continue to shape our role in helping the rest of the team get there. We must do this for ourselves, our profession, and—most of all—our patients today and tomorrow. TH
Dr. Wellikson is CEO of SHM.
Something is happening out there. Can you feel it?
It is like a small tremor before an earthquake or a brief lightning flash before a thunderstorm. It’s the signal that alerts us something is coming without indicating what it might be—ominous, promising, or revolutionary.
Our ossified, dysfunctional nonsystem of incentivizing the behavior of healthcare professionals gradually is eroding, even as the haves—the over-rewarded—cling to the past or rush to create the next procedure or modality to run by the insurance industry guardians of the dollar. The days of the system of paying for care in an a la carte manner—by the unit of the visit or performance of the procedure without consequence or reward for appropriate indications or demonstration of expected outcomes—clearly are numbered.
What will replace the current imperfect approach is not clear or perfect, but there are discernible, inexorable trends.
Performance Will Matter
Few sectors of our economy have been so devoid of standards—or, more to the point, of rewards for better service or outcomes—than healthcare.
Could you imagine paying the same for a 2008 Lexus as you would for a 1995 Toyota? Could you imagine a pricing system that couldn’t recognize or properly reward the difference between Motel 6 and the Ritz Carlton, excusing the inability to differentiate them by saying they both have beds, sheets, towels, and indoor plumbing? Today, the worst orthopedist in the country and the best are paid the same fee for a hip replacement—whether it’s indicated or not. Most patients or purchasers of healthcare have no way to know which is which.
Performance measurement and standards are here, and while imperfect and evolving, they will be with us throughout the rest of our professional careers. Whether you are in the “process” or “outcomes” camp, you and your institution will be measured. The carrot or the stick can take many forms.
Right now, it is much more than about just reporting. Disturbingly, only 30% of physicians have participated in the first round of the Physician Quality Reporting Initiative (PQRI). Look for Medicare to apply financial pressure on physicians who do not report.
On the hospital side, reporting has focused as much on embarrassment as anything. In April, every hospital received its mortality statistics for pneumonia from the Centers for Medicare and Medicaid Services (CMS). In July, these numbers will be made public. Look for a flurry of indignation and activity as hospitals try to regain the trust of their patients and assure them they indeed can manage something as basic to their core mission as pneumonia. SHM will be developing strategies to help hospitalists help their hospitals improve their performance.
Much has been made of paying for performance—and this may drive change at the hospital level. Yet, it is doubtful individual physicians will substantially change their work flow or processes, or purchase new systems for measurement, just to get an extra dollar or two for better glycemic control of their patients. What may carry more weight is if lack of performance means some physicians, or even hospitals, are restricted from performing certain procedures or caring for certain illnesses.
Bundling Episodes of Care
A move is afoot to change the unit of healthcare delivery. SHM has been in discussions with MedPAC, which advises CMS on changes to the reimbursement system, about aggregating a continuum of care as a “bundled” episode of care.
More than 15 years ago, the implementation of diagnosis-related groups (DRGs) moved hospital thinking from a la carte charging for each aspirin to managing the use of resources for the entire hospital stay, since their reimbursement was fixed. The DRG payment system as much as anything has encouraged hospitals to develop and support hospital medicine groups. Bundling would extend and expand a DRG-like concept to physicians.
Think of a future where physicians are not reimbursed for an admission work-up, three daily visits, and a discharge summary. Instead, they’d receive a global fee that might include the hospital care, transitions to the outpatient provider, and measurement of performance that might include patient satisfaction and a low readmission rate.
If we look at healthcare from the patient’s viewpoint, this is the kind of service for which they’re crying out. They want to move away from a system that even with the best providers leads to each expert doing his or her individual part well, but with voltage drops and white spaces as the patient moves through an uncoordinated non-system.
Hospitalists are in a unique position to be successful, especially as we look for strategies that align our performance with strong and engaged outpatient physicians and when we fully engage the entire healthcare team.
A Team Sport
Bundling and rewards driven by demonstrable performance create interlinking responsibilities for care among multiple physicians (primary care physicians, emergency physicians, surgeons, subspecialists, and hospitalists), as well as allied health professionals (registered nurses, nurse practitioners, physician assistants, pharmacists, therapists, social workers, and case managers).
While the makeup of the team is important, the environment in which it performs is most crucial for success. A system of healthcare delivery that focuses on and supports best practices and nudges—or forces—providers to make the right choice is of prime importance. In the end, a good system of care and one or two members of the team can save the entire enterprise, leading to the best outcome for the patient.
By the same token, a dysfunctional outlier on the team can sink everyone, including the patient. Think of the “new” healthcare as a crew team that needs a well-made boat (i.e., the system of care), a good coxswain (accountable physician), and a group of rowers, each of whom know and execute their roles. One rower can sink seven Olympians.
We are all in the boat together. We need to be clear where the finish line is and how best to get there. The future is in sight, and we need to continue to shape our role in helping the rest of the team get there. We must do this for ourselves, our profession, and—most of all—our patients today and tomorrow. TH
Dr. Wellikson is CEO of SHM.
What is the best choice for prophylaxis against VTE in medical inpatients?
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
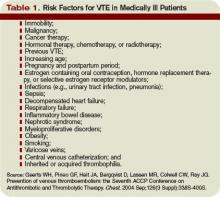
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.
Generalist
Medical generalists tell a sad story. Their steadily declining numbers reflect a compensation system that still rewards specialists handsomely at generalists’ expense.
Even though the venerable relative value unit (RVU)-based reimbursement system was intended to equalize pay between primary care’s cognitive work and specialists’ procedure-driven high pay, it hasn’t. Since 1992, when Medicare started paying physicians using RVUs based on the resources used, the specialist-generalist gap remains. RVUs comprise three factors:
- Work (55%);
- Practice expense (42%); and
- Malpractice insurance (3%).
Arguably, generalist RVUs have risen and proceduralist RVUs have decreased. However, generalists argue this skewed pay scale still causes residents to shun internal medicine, hospital medicine, family practice, general pediatrics, and general surgery. Is that true?
Hospitalists and RVUs
Although RVUs don’t always figure into hospitalist compensation, they can have an effect. Vibhu Sharma, MD, of SUNY Downstate Medical Center’s section director, hospital medicine program, heads a 13-hospitalist group employed by the medical center and carries extensive teaching responsibilities.
RVUs don’t currently factor into his hospitalists’ pay but that’s becoming troublesome to Dr. Sharma. “We’d make a lot more money if RVUs were factored in, but they aren’t because we’re a teaching hospital,” he says. “Our group is only four years old, and we aren’t ready to push for it.”
Without the RVU productivity component, Dr. Sharma says he’s at a disadvantage when recruiting. Internal medicine, family practice, and other generalists “stuck with the perception that specialization is a better career option,” he says. “If payers paid us the same as non-invasive cardiologists there’d be a lot more hospitalists.”
Boosts in compensation will be slow in coming, says Dr. Sharma, because hospitalists have demonstrated only modest cost savings and LOS decreases. He adds: “Today nobody wants to be a hospitalist for the rest of their career. We perceive that the patient care we deliver isn’t well compensated, and that the RVU gap between generalists and sub-specialists can never be closed.” As for RVUs, he sees the hospital eventually adding an RVU bonus component. For now, it bumps up hospitalist salaries when the group complains.
The three-member pediatric hospitalist group at Kentucky Children’s Hospital also doesn’t use RVUs, either for compensation or as a productivity proxy. Jeff Bennett, MD, its lead hospitalist, says pediatric outcomes data aren’t robust enough to establish proper RVU benchmarks. He adds that adult RVUs are “denser” than pediatric RVUs because of lower acuity and fewer procedures with children’s illnesses. Additionally, productivity measures don’t affect pediatrics significantly because children’s hospitals “are at the bottom of the funnel,” he says. “We have to take every kid who comes our way. Pediatric hospitals tend not to be competitive. There are four hospitals in town competing for adult patients, while we’re the only tertiary care hospital for 300 miles.”
Compounding the problem is that determining pediatric hospitalist compensation is problematic. With only 2,200 pediatric hospitalists versus 20,000 who work with adults, compensation packages tend to idiosyncratic. “Compensation is important, but RVUs won’t figure into pediatrics for a while,” says Dr. Bennett. “People chose hospital medicine from residency because they’re itching for inpatient work, with its complexity and sharp edges. The shine dims quickly, though, because they are protected during residency and then have full responsibility as hospitalists.”
David Dale, MD, director of the University of Washington’s internal medicine residency program, and American College of Physicians’ president, says hospitalist careers loom large for his annual crop of 35 to 40 residents—but RVUs don’t. “For them it’s an easy transition, a guaranteed salary versus establishing a small business,” he says. “The office practice is where the RVUs really impact generalists. We have a hard job preparing residents for those reimbursement issues.”
Dr. Dale says between two-thirds and three-quarters of his residents become hospitalists, although that’s often not their final career destination. “Some don’t treat hospitalist medicine as a long-term career because the work is hard and the hours are stressful. Many are waiting for a fellowship track to specialization.”
The General Surgeon
A 2007 article by Josef Fischer, MD, in the Journal of the American Medical Association raises questions about the dwindling general surgeon cadre.1 Dr. Fischer posits that RVUs can’t boost surgeons’ incomes because surgeons can’t increase utilization when reimbursement decreases.
For example, since patients have only one gallbladder and indications for removal are constant, there’s no way to increase surgical RVUs. He says this unattractive RVU scheme dissuades residents from general surgery careers.
Dr. Fischer’s concerns don’t faze David Joyce, CEO of Morrisville, N.C.-based Delphi Healthcare Partners, which has three surgicalist programs nationally. Each employs two general surgeons working two weeks on, two weeks off, covering indigent and unassigned patients.
On average, each sees eight patients daily, two requiring surgery. The surgicalists all are either age 50 to 55 or under 35 and reject the hassles of office-based practices at both ends of the career ladder. They earn fixed salaries; Delphi uses RVUs for reimbursement but not for productivity bonuses.
“RVUs aren’t very important in our surgicalist equation, which is a winning situation for everyone involved,” Joyce says. “Private-practice surgeons are thrilled because they don’t cover call and can build their practices. The hospitals do well and don’t mind kicking in several hundred thousand dollars to cover surgicalist compensation.
“In our Charleston, W. Va., program the hospital derived $1.6 million above our program’s cost because the private docs did more surgeries, our surgicalists do what they were trained to do and are well compensated. It’s great,” he says.
Delphi surgicalist Richard Fogle, MD, works at Thomas Memorial Hospital in South Charleston, W. Va., and doesn’t think about RVUs. “The problem with surgeons is lifestyle,” he asserts. “If you have 10 surgeons, you cover call once every 10 days. With three surgeons it’s once every three days.”
Delphi solved his hospital’s problem by recruiting him and another surgicalist. “Before we came most general surgeons had left,” Dr. Fogle says. “Now, two have come back, and four more have settled here. We’re not competing with them for business, and they can build their office practices — particularly with outpatient procedures.”
As a surgicalist, Dr. Fogle, doesn’t miss spending 50% of revenues on office overhead, or leaving 20 patients sitting in his office while answering a hospital page. “I keep waiting for the other shoe to drop, but it hasn’t,” he says of his freedom to practice surgery unfettered by office busyness. He’s happy with the compensation but has a bone to pick with the RVU system. “RVUs are too low for general surgery, and anyone who discounts the cognitive part of surgery procedures is seriously mistaken,” he says.
Different Strokes
John Marcelis, MD, an Erickson Retirement Communities regional medical director of 19 providers in four communities, gives the RVU discussion another twist. He practices at Ann’s Choice in Warminster, Pa., with four other physicians, each of whom acts as the group’s hospitalist once every five weeks.
Previously he spent 10 years at the University of Pennsylvania hospital system, where RVUs figured in significantly and volume was highly rewarded. Taking a huge pay cut to practice at Erickson, he happily left the RVU treadmill. “I didn’t like seeing patients at RVU factories,” he recalls. “At Erickson, we have half-hour office visits and see our hospitalized patients as needed. An RVU system doesn’t compute with us.”
Dr. Marcelis, who lost sleep when he was part of an RVU system, sees a bimodal curve of doctors—some thrive on RVUs, others don’t. “There are some doctors who want to see 50 MIs in a day,” he says. “They relish the high-volume intensity. ‘Bring ’em on,’ they say. RVU systems work well for them. For doctors who value longitudinal relationships with patients, RVUs don’t work well.”
He doesn’t see the cognitive vs. procedure gap leading to RVUs ever closing: “There’s a pool of dollars, and shifting 5% from procedures to cognitive work can’t change things. If payers lower RVUs for procedures, specialists will just do more procedures.” TH
Marlene Piturro is a medical writer based in New York.
Reference
- Fischer J. The impending disappearance of the general surgeon. JAMA. 2007;298:2191-2193.
Medical generalists tell a sad story. Their steadily declining numbers reflect a compensation system that still rewards specialists handsomely at generalists’ expense.
Even though the venerable relative value unit (RVU)-based reimbursement system was intended to equalize pay between primary care’s cognitive work and specialists’ procedure-driven high pay, it hasn’t. Since 1992, when Medicare started paying physicians using RVUs based on the resources used, the specialist-generalist gap remains. RVUs comprise three factors:
- Work (55%);
- Practice expense (42%); and
- Malpractice insurance (3%).
Arguably, generalist RVUs have risen and proceduralist RVUs have decreased. However, generalists argue this skewed pay scale still causes residents to shun internal medicine, hospital medicine, family practice, general pediatrics, and general surgery. Is that true?
Hospitalists and RVUs
Although RVUs don’t always figure into hospitalist compensation, they can have an effect. Vibhu Sharma, MD, of SUNY Downstate Medical Center’s section director, hospital medicine program, heads a 13-hospitalist group employed by the medical center and carries extensive teaching responsibilities.
RVUs don’t currently factor into his hospitalists’ pay but that’s becoming troublesome to Dr. Sharma. “We’d make a lot more money if RVUs were factored in, but they aren’t because we’re a teaching hospital,” he says. “Our group is only four years old, and we aren’t ready to push for it.”
Without the RVU productivity component, Dr. Sharma says he’s at a disadvantage when recruiting. Internal medicine, family practice, and other generalists “stuck with the perception that specialization is a better career option,” he says. “If payers paid us the same as non-invasive cardiologists there’d be a lot more hospitalists.”
Boosts in compensation will be slow in coming, says Dr. Sharma, because hospitalists have demonstrated only modest cost savings and LOS decreases. He adds: “Today nobody wants to be a hospitalist for the rest of their career. We perceive that the patient care we deliver isn’t well compensated, and that the RVU gap between generalists and sub-specialists can never be closed.” As for RVUs, he sees the hospital eventually adding an RVU bonus component. For now, it bumps up hospitalist salaries when the group complains.
The three-member pediatric hospitalist group at Kentucky Children’s Hospital also doesn’t use RVUs, either for compensation or as a productivity proxy. Jeff Bennett, MD, its lead hospitalist, says pediatric outcomes data aren’t robust enough to establish proper RVU benchmarks. He adds that adult RVUs are “denser” than pediatric RVUs because of lower acuity and fewer procedures with children’s illnesses. Additionally, productivity measures don’t affect pediatrics significantly because children’s hospitals “are at the bottom of the funnel,” he says. “We have to take every kid who comes our way. Pediatric hospitals tend not to be competitive. There are four hospitals in town competing for adult patients, while we’re the only tertiary care hospital for 300 miles.”
Compounding the problem is that determining pediatric hospitalist compensation is problematic. With only 2,200 pediatric hospitalists versus 20,000 who work with adults, compensation packages tend to idiosyncratic. “Compensation is important, but RVUs won’t figure into pediatrics for a while,” says Dr. Bennett. “People chose hospital medicine from residency because they’re itching for inpatient work, with its complexity and sharp edges. The shine dims quickly, though, because they are protected during residency and then have full responsibility as hospitalists.”
David Dale, MD, director of the University of Washington’s internal medicine residency program, and American College of Physicians’ president, says hospitalist careers loom large for his annual crop of 35 to 40 residents—but RVUs don’t. “For them it’s an easy transition, a guaranteed salary versus establishing a small business,” he says. “The office practice is where the RVUs really impact generalists. We have a hard job preparing residents for those reimbursement issues.”
Dr. Dale says between two-thirds and three-quarters of his residents become hospitalists, although that’s often not their final career destination. “Some don’t treat hospitalist medicine as a long-term career because the work is hard and the hours are stressful. Many are waiting for a fellowship track to specialization.”
The General Surgeon
A 2007 article by Josef Fischer, MD, in the Journal of the American Medical Association raises questions about the dwindling general surgeon cadre.1 Dr. Fischer posits that RVUs can’t boost surgeons’ incomes because surgeons can’t increase utilization when reimbursement decreases.
For example, since patients have only one gallbladder and indications for removal are constant, there’s no way to increase surgical RVUs. He says this unattractive RVU scheme dissuades residents from general surgery careers.
Dr. Fischer’s concerns don’t faze David Joyce, CEO of Morrisville, N.C.-based Delphi Healthcare Partners, which has three surgicalist programs nationally. Each employs two general surgeons working two weeks on, two weeks off, covering indigent and unassigned patients.
On average, each sees eight patients daily, two requiring surgery. The surgicalists all are either age 50 to 55 or under 35 and reject the hassles of office-based practices at both ends of the career ladder. They earn fixed salaries; Delphi uses RVUs for reimbursement but not for productivity bonuses.
“RVUs aren’t very important in our surgicalist equation, which is a winning situation for everyone involved,” Joyce says. “Private-practice surgeons are thrilled because they don’t cover call and can build their practices. The hospitals do well and don’t mind kicking in several hundred thousand dollars to cover surgicalist compensation.
“In our Charleston, W. Va., program the hospital derived $1.6 million above our program’s cost because the private docs did more surgeries, our surgicalists do what they were trained to do and are well compensated. It’s great,” he says.
Delphi surgicalist Richard Fogle, MD, works at Thomas Memorial Hospital in South Charleston, W. Va., and doesn’t think about RVUs. “The problem with surgeons is lifestyle,” he asserts. “If you have 10 surgeons, you cover call once every 10 days. With three surgeons it’s once every three days.”
Delphi solved his hospital’s problem by recruiting him and another surgicalist. “Before we came most general surgeons had left,” Dr. Fogle says. “Now, two have come back, and four more have settled here. We’re not competing with them for business, and they can build their office practices — particularly with outpatient procedures.”
As a surgicalist, Dr. Fogle, doesn’t miss spending 50% of revenues on office overhead, or leaving 20 patients sitting in his office while answering a hospital page. “I keep waiting for the other shoe to drop, but it hasn’t,” he says of his freedom to practice surgery unfettered by office busyness. He’s happy with the compensation but has a bone to pick with the RVU system. “RVUs are too low for general surgery, and anyone who discounts the cognitive part of surgery procedures is seriously mistaken,” he says.
Different Strokes
John Marcelis, MD, an Erickson Retirement Communities regional medical director of 19 providers in four communities, gives the RVU discussion another twist. He practices at Ann’s Choice in Warminster, Pa., with four other physicians, each of whom acts as the group’s hospitalist once every five weeks.
Previously he spent 10 years at the University of Pennsylvania hospital system, where RVUs figured in significantly and volume was highly rewarded. Taking a huge pay cut to practice at Erickson, he happily left the RVU treadmill. “I didn’t like seeing patients at RVU factories,” he recalls. “At Erickson, we have half-hour office visits and see our hospitalized patients as needed. An RVU system doesn’t compute with us.”
Dr. Marcelis, who lost sleep when he was part of an RVU system, sees a bimodal curve of doctors—some thrive on RVUs, others don’t. “There are some doctors who want to see 50 MIs in a day,” he says. “They relish the high-volume intensity. ‘Bring ’em on,’ they say. RVU systems work well for them. For doctors who value longitudinal relationships with patients, RVUs don’t work well.”
He doesn’t see the cognitive vs. procedure gap leading to RVUs ever closing: “There’s a pool of dollars, and shifting 5% from procedures to cognitive work can’t change things. If payers lower RVUs for procedures, specialists will just do more procedures.” TH
Marlene Piturro is a medical writer based in New York.
Reference
- Fischer J. The impending disappearance of the general surgeon. JAMA. 2007;298:2191-2193.
Medical generalists tell a sad story. Their steadily declining numbers reflect a compensation system that still rewards specialists handsomely at generalists’ expense.
Even though the venerable relative value unit (RVU)-based reimbursement system was intended to equalize pay between primary care’s cognitive work and specialists’ procedure-driven high pay, it hasn’t. Since 1992, when Medicare started paying physicians using RVUs based on the resources used, the specialist-generalist gap remains. RVUs comprise three factors:
- Work (55%);
- Practice expense (42%); and
- Malpractice insurance (3%).
Arguably, generalist RVUs have risen and proceduralist RVUs have decreased. However, generalists argue this skewed pay scale still causes residents to shun internal medicine, hospital medicine, family practice, general pediatrics, and general surgery. Is that true?
Hospitalists and RVUs
Although RVUs don’t always figure into hospitalist compensation, they can have an effect. Vibhu Sharma, MD, of SUNY Downstate Medical Center’s section director, hospital medicine program, heads a 13-hospitalist group employed by the medical center and carries extensive teaching responsibilities.
RVUs don’t currently factor into his hospitalists’ pay but that’s becoming troublesome to Dr. Sharma. “We’d make a lot more money if RVUs were factored in, but they aren’t because we’re a teaching hospital,” he says. “Our group is only four years old, and we aren’t ready to push for it.”
Without the RVU productivity component, Dr. Sharma says he’s at a disadvantage when recruiting. Internal medicine, family practice, and other generalists “stuck with the perception that specialization is a better career option,” he says. “If payers paid us the same as non-invasive cardiologists there’d be a lot more hospitalists.”
Boosts in compensation will be slow in coming, says Dr. Sharma, because hospitalists have demonstrated only modest cost savings and LOS decreases. He adds: “Today nobody wants to be a hospitalist for the rest of their career. We perceive that the patient care we deliver isn’t well compensated, and that the RVU gap between generalists and sub-specialists can never be closed.” As for RVUs, he sees the hospital eventually adding an RVU bonus component. For now, it bumps up hospitalist salaries when the group complains.
The three-member pediatric hospitalist group at Kentucky Children’s Hospital also doesn’t use RVUs, either for compensation or as a productivity proxy. Jeff Bennett, MD, its lead hospitalist, says pediatric outcomes data aren’t robust enough to establish proper RVU benchmarks. He adds that adult RVUs are “denser” than pediatric RVUs because of lower acuity and fewer procedures with children’s illnesses. Additionally, productivity measures don’t affect pediatrics significantly because children’s hospitals “are at the bottom of the funnel,” he says. “We have to take every kid who comes our way. Pediatric hospitals tend not to be competitive. There are four hospitals in town competing for adult patients, while we’re the only tertiary care hospital for 300 miles.”
Compounding the problem is that determining pediatric hospitalist compensation is problematic. With only 2,200 pediatric hospitalists versus 20,000 who work with adults, compensation packages tend to idiosyncratic. “Compensation is important, but RVUs won’t figure into pediatrics for a while,” says Dr. Bennett. “People chose hospital medicine from residency because they’re itching for inpatient work, with its complexity and sharp edges. The shine dims quickly, though, because they are protected during residency and then have full responsibility as hospitalists.”
David Dale, MD, director of the University of Washington’s internal medicine residency program, and American College of Physicians’ president, says hospitalist careers loom large for his annual crop of 35 to 40 residents—but RVUs don’t. “For them it’s an easy transition, a guaranteed salary versus establishing a small business,” he says. “The office practice is where the RVUs really impact generalists. We have a hard job preparing residents for those reimbursement issues.”
Dr. Dale says between two-thirds and three-quarters of his residents become hospitalists, although that’s often not their final career destination. “Some don’t treat hospitalist medicine as a long-term career because the work is hard and the hours are stressful. Many are waiting for a fellowship track to specialization.”
The General Surgeon
A 2007 article by Josef Fischer, MD, in the Journal of the American Medical Association raises questions about the dwindling general surgeon cadre.1 Dr. Fischer posits that RVUs can’t boost surgeons’ incomes because surgeons can’t increase utilization when reimbursement decreases.
For example, since patients have only one gallbladder and indications for removal are constant, there’s no way to increase surgical RVUs. He says this unattractive RVU scheme dissuades residents from general surgery careers.
Dr. Fischer’s concerns don’t faze David Joyce, CEO of Morrisville, N.C.-based Delphi Healthcare Partners, which has three surgicalist programs nationally. Each employs two general surgeons working two weeks on, two weeks off, covering indigent and unassigned patients.
On average, each sees eight patients daily, two requiring surgery. The surgicalists all are either age 50 to 55 or under 35 and reject the hassles of office-based practices at both ends of the career ladder. They earn fixed salaries; Delphi uses RVUs for reimbursement but not for productivity bonuses.
“RVUs aren’t very important in our surgicalist equation, which is a winning situation for everyone involved,” Joyce says. “Private-practice surgeons are thrilled because they don’t cover call and can build their practices. The hospitals do well and don’t mind kicking in several hundred thousand dollars to cover surgicalist compensation.
“In our Charleston, W. Va., program the hospital derived $1.6 million above our program’s cost because the private docs did more surgeries, our surgicalists do what they were trained to do and are well compensated. It’s great,” he says.
Delphi surgicalist Richard Fogle, MD, works at Thomas Memorial Hospital in South Charleston, W. Va., and doesn’t think about RVUs. “The problem with surgeons is lifestyle,” he asserts. “If you have 10 surgeons, you cover call once every 10 days. With three surgeons it’s once every three days.”
Delphi solved his hospital’s problem by recruiting him and another surgicalist. “Before we came most general surgeons had left,” Dr. Fogle says. “Now, two have come back, and four more have settled here. We’re not competing with them for business, and they can build their office practices — particularly with outpatient procedures.”
As a surgicalist, Dr. Fogle, doesn’t miss spending 50% of revenues on office overhead, or leaving 20 patients sitting in his office while answering a hospital page. “I keep waiting for the other shoe to drop, but it hasn’t,” he says of his freedom to practice surgery unfettered by office busyness. He’s happy with the compensation but has a bone to pick with the RVU system. “RVUs are too low for general surgery, and anyone who discounts the cognitive part of surgery procedures is seriously mistaken,” he says.
Different Strokes
John Marcelis, MD, an Erickson Retirement Communities regional medical director of 19 providers in four communities, gives the RVU discussion another twist. He practices at Ann’s Choice in Warminster, Pa., with four other physicians, each of whom acts as the group’s hospitalist once every five weeks.
Previously he spent 10 years at the University of Pennsylvania hospital system, where RVUs figured in significantly and volume was highly rewarded. Taking a huge pay cut to practice at Erickson, he happily left the RVU treadmill. “I didn’t like seeing patients at RVU factories,” he recalls. “At Erickson, we have half-hour office visits and see our hospitalized patients as needed. An RVU system doesn’t compute with us.”
Dr. Marcelis, who lost sleep when he was part of an RVU system, sees a bimodal curve of doctors—some thrive on RVUs, others don’t. “There are some doctors who want to see 50 MIs in a day,” he says. “They relish the high-volume intensity. ‘Bring ’em on,’ they say. RVU systems work well for them. For doctors who value longitudinal relationships with patients, RVUs don’t work well.”
He doesn’t see the cognitive vs. procedure gap leading to RVUs ever closing: “There’s a pool of dollars, and shifting 5% from procedures to cognitive work can’t change things. If payers lower RVUs for procedures, specialists will just do more procedures.” TH
Marlene Piturro is a medical writer based in New York.
Reference
- Fischer J. The impending disappearance of the general surgeon. JAMA. 2007;298:2191-2193.
Choose Your Exam Rules
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
No Fee for Errors
State governments, private payors, Medicare, and hospitals have reached the same conclusion: Hospitals should not charge for preventable medical errors.
One of the latest entities to join this trend is Washington state. Early this year, healthcare associations there passed a resolution saying Washington healthcare providers no longer will charge for preventable hospital errors. The resolution applies to 28 “never events” published by the National Quality Forum (NQF). These are medical errors that clearly are identifiable, preventable, serious in their consequences for patients, and indicative of a real problem in the safety and credibility of a healthcare facility. (For a complete list of events, visit NQF’s Web site (www.qualityforum.org/pdf/news/prSeriousReportableEvents10-15-06.pdf).
Hospitals in Massachusetts, Minnesota, Pennsylvania, and Vermont have adopted similar policies. Private insurers Aetna, Wellpoint, and Blue Cross Blue Shield each are taking steps toward refusing payment for treatment resulting from serious medical errors in hospitals.
Amid these decisions, the American Hospital Association (AHA) released a quality advisory Feb. 12, recommending hospitals implement a no-charge policy for serious adverse errors.
“There’s certainly been a lot of conversation about aligning payment around outcomes,” says Nancy E. Foster, the AHA’s vice president for quality and patient safety policy. “Most of those conversations have focused on reward for doing the right thing, but there were certainly parts of those conversations based on the notion of who’s responsible and who pays when something that was preventable did happen.”
Even the federal government has gotten involved. Beginning in October, the Centers for Medicare and Medicaid Services (CMS) plans to no longer reimburse for specific preventable conditions.
CMS “Stop Payments”
If Congress approves Medicare’s plan, the CMS will not pay any extra-care costs for eight conditions unless they were present upon admission—and it prohibits hospitals from charging patients for such conditions. The conditions include three “never events”:
- Objects left in the body during surgery (“never event”);
- Air embolism (“never event”);
- Blood incompatibility (“never event”);
- Falls;
- Catheter-associated urinary tract infections;
- Pressure ulcers (decubitus ulcers);
- Vascular catheter-associated infection; and
- Surgical site infection after coronary artery bypass graft surgery (mediastinitis).
Next year, the CMS plans to add more conditions to the no-pay list. The most likely additions are ventilator-associated pneumonia, staphylococcus aureus septicemia, deep-vein thrombosis (DVT), and pulmonary embolism.
The CMS rule obviously directly affects hospital income, which will affect hospital processes and staff.
“As hospitalists, this affects us,” says Winthrop F. Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., director of hospital medicine at Catholic Health East, and co-founder of SHM. “It’s another thing showcasing the value of hospitalists because we tend to document well. When a patient comes in with DVT or a pressure ulcer, we tend to document that, and that will help our hospitals.”
Other physicians may balk at hospital requests to amend or add to their notes to ensure payment, but, says Dr. Whitcomb: “Hospitalists understand the requirement for documentation. If you’re not a hospitalist, you may not be happy to be asked to change your documentation so that the hospital can get paid more, but we understand how important this is.”
Hospitals likely will continue to closely oversee physician documentation on Medicare patients.
“At our hospital, we [already] work with coders,” Dr. Whitcomb says. “I’ve heard of this more and more. They round with us now on every Medicare patient and review the charts. They actually write a formal note that prompts us to document accurately—they may ask us to amend that something was present on admission.” Dr. Whitcomb’s hospital has a paper-based system for this information; an electronic system will include this type of prompt. “Electronic prompts can be customized, but they can also be ignored; prompt fatigue is a big issue,” Dr. Whitcomb warns.
Another potential effect on hospitalists will be involvement in hospital efforts to prevent the eight conditions.
“The CMS change is definitely going to up the ante for quality improvement and patient safety work, no matter who undertakes it,” Dr. Whitcomb says. “It should expand opportunities for hospitalists to work in [quality improvement]. Hospitalists may end up leading teams to specifically address certain never events. The good news is, it gets right at the bottom line of the hospital, so nonclinicians like administrators in the financial office will immediately understand the importance of work like this.”
Leaving a sponge inside a patient is clearly a preventable medical error—but what about pressure ulcers? Or DVT?
In his “Wachter’s World” blog post of Feb. 11 (www.wachtersworld.org), Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, addressed the CMS rule.
“For some of the events on the Medicare list, particularly the infections (such as catheter-related bloodstream infections), there is good evidence that the vast majority of events can be prevented,” Dr. Wachter wrote. “For others, such as pressure ulcers and falls, although some commonsensical practices have been widely promoted (particularly through IHI’s 5 Million Lives campaign), the evidence linking adherence to ‘prevention practices’ and reductions in adverse events is tenuous. These adverse events should stay off the list until the evidence is stronger.”
In spite of his misgivings, Dr. Wachter is a strong proponent of the trend toward nonpayment for preventable errors. “We’ve already seen hospitals putting far more resources into trying to prevent line infections, falls, and [pressure ulcers] than they were before,” he says. “And remember that the dollars at stake are relatively small. The extra payments for “Complicating Conditions” (CC) are not enormous, and many patients who have one CC have more than one; in which case, the hospital will still receive the extra payment even if the adverse event-related payment is denied. So, in essence the policy is creating an unusual amount of patient safety momentum for a relatively small displacement of dollars – a pretty clever trick.”
For more information on the CMS rule, read “Medicare’s decision to withhold payment for hospital errors: the devil is in the details,” by Dr. Wachter, Nancy Foster, and Adams Dudley, MD, in the February 2008 Joint Commission Journal of Quality and Patient Safety. TH
Jane Jerrard is a medical writer based in Chicago.
State governments, private payors, Medicare, and hospitals have reached the same conclusion: Hospitals should not charge for preventable medical errors.
One of the latest entities to join this trend is Washington state. Early this year, healthcare associations there passed a resolution saying Washington healthcare providers no longer will charge for preventable hospital errors. The resolution applies to 28 “never events” published by the National Quality Forum (NQF). These are medical errors that clearly are identifiable, preventable, serious in their consequences for patients, and indicative of a real problem in the safety and credibility of a healthcare facility. (For a complete list of events, visit NQF’s Web site (www.qualityforum.org/pdf/news/prSeriousReportableEvents10-15-06.pdf).
Hospitals in Massachusetts, Minnesota, Pennsylvania, and Vermont have adopted similar policies. Private insurers Aetna, Wellpoint, and Blue Cross Blue Shield each are taking steps toward refusing payment for treatment resulting from serious medical errors in hospitals.
Amid these decisions, the American Hospital Association (AHA) released a quality advisory Feb. 12, recommending hospitals implement a no-charge policy for serious adverse errors.
“There’s certainly been a lot of conversation about aligning payment around outcomes,” says Nancy E. Foster, the AHA’s vice president for quality and patient safety policy. “Most of those conversations have focused on reward for doing the right thing, but there were certainly parts of those conversations based on the notion of who’s responsible and who pays when something that was preventable did happen.”
Even the federal government has gotten involved. Beginning in October, the Centers for Medicare and Medicaid Services (CMS) plans to no longer reimburse for specific preventable conditions.
CMS “Stop Payments”
If Congress approves Medicare’s plan, the CMS will not pay any extra-care costs for eight conditions unless they were present upon admission—and it prohibits hospitals from charging patients for such conditions. The conditions include three “never events”:
- Objects left in the body during surgery (“never event”);
- Air embolism (“never event”);
- Blood incompatibility (“never event”);
- Falls;
- Catheter-associated urinary tract infections;
- Pressure ulcers (decubitus ulcers);
- Vascular catheter-associated infection; and
- Surgical site infection after coronary artery bypass graft surgery (mediastinitis).
Next year, the CMS plans to add more conditions to the no-pay list. The most likely additions are ventilator-associated pneumonia, staphylococcus aureus septicemia, deep-vein thrombosis (DVT), and pulmonary embolism.
The CMS rule obviously directly affects hospital income, which will affect hospital processes and staff.
“As hospitalists, this affects us,” says Winthrop F. Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., director of hospital medicine at Catholic Health East, and co-founder of SHM. “It’s another thing showcasing the value of hospitalists because we tend to document well. When a patient comes in with DVT or a pressure ulcer, we tend to document that, and that will help our hospitals.”
Other physicians may balk at hospital requests to amend or add to their notes to ensure payment, but, says Dr. Whitcomb: “Hospitalists understand the requirement for documentation. If you’re not a hospitalist, you may not be happy to be asked to change your documentation so that the hospital can get paid more, but we understand how important this is.”
Hospitals likely will continue to closely oversee physician documentation on Medicare patients.
“At our hospital, we [already] work with coders,” Dr. Whitcomb says. “I’ve heard of this more and more. They round with us now on every Medicare patient and review the charts. They actually write a formal note that prompts us to document accurately—they may ask us to amend that something was present on admission.” Dr. Whitcomb’s hospital has a paper-based system for this information; an electronic system will include this type of prompt. “Electronic prompts can be customized, but they can also be ignored; prompt fatigue is a big issue,” Dr. Whitcomb warns.
Another potential effect on hospitalists will be involvement in hospital efforts to prevent the eight conditions.
“The CMS change is definitely going to up the ante for quality improvement and patient safety work, no matter who undertakes it,” Dr. Whitcomb says. “It should expand opportunities for hospitalists to work in [quality improvement]. Hospitalists may end up leading teams to specifically address certain never events. The good news is, it gets right at the bottom line of the hospital, so nonclinicians like administrators in the financial office will immediately understand the importance of work like this.”
Leaving a sponge inside a patient is clearly a preventable medical error—but what about pressure ulcers? Or DVT?
In his “Wachter’s World” blog post of Feb. 11 (www.wachtersworld.org), Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, addressed the CMS rule.
“For some of the events on the Medicare list, particularly the infections (such as catheter-related bloodstream infections), there is good evidence that the vast majority of events can be prevented,” Dr. Wachter wrote. “For others, such as pressure ulcers and falls, although some commonsensical practices have been widely promoted (particularly through IHI’s 5 Million Lives campaign), the evidence linking adherence to ‘prevention practices’ and reductions in adverse events is tenuous. These adverse events should stay off the list until the evidence is stronger.”
In spite of his misgivings, Dr. Wachter is a strong proponent of the trend toward nonpayment for preventable errors. “We’ve already seen hospitals putting far more resources into trying to prevent line infections, falls, and [pressure ulcers] than they were before,” he says. “And remember that the dollars at stake are relatively small. The extra payments for “Complicating Conditions” (CC) are not enormous, and many patients who have one CC have more than one; in which case, the hospital will still receive the extra payment even if the adverse event-related payment is denied. So, in essence the policy is creating an unusual amount of patient safety momentum for a relatively small displacement of dollars – a pretty clever trick.”
For more information on the CMS rule, read “Medicare’s decision to withhold payment for hospital errors: the devil is in the details,” by Dr. Wachter, Nancy Foster, and Adams Dudley, MD, in the February 2008 Joint Commission Journal of Quality and Patient Safety. TH
Jane Jerrard is a medical writer based in Chicago.
State governments, private payors, Medicare, and hospitals have reached the same conclusion: Hospitals should not charge for preventable medical errors.
One of the latest entities to join this trend is Washington state. Early this year, healthcare associations there passed a resolution saying Washington healthcare providers no longer will charge for preventable hospital errors. The resolution applies to 28 “never events” published by the National Quality Forum (NQF). These are medical errors that clearly are identifiable, preventable, serious in their consequences for patients, and indicative of a real problem in the safety and credibility of a healthcare facility. (For a complete list of events, visit NQF’s Web site (www.qualityforum.org/pdf/news/prSeriousReportableEvents10-15-06.pdf).
Hospitals in Massachusetts, Minnesota, Pennsylvania, and Vermont have adopted similar policies. Private insurers Aetna, Wellpoint, and Blue Cross Blue Shield each are taking steps toward refusing payment for treatment resulting from serious medical errors in hospitals.
Amid these decisions, the American Hospital Association (AHA) released a quality advisory Feb. 12, recommending hospitals implement a no-charge policy for serious adverse errors.
“There’s certainly been a lot of conversation about aligning payment around outcomes,” says Nancy E. Foster, the AHA’s vice president for quality and patient safety policy. “Most of those conversations have focused on reward for doing the right thing, but there were certainly parts of those conversations based on the notion of who’s responsible and who pays when something that was preventable did happen.”
Even the federal government has gotten involved. Beginning in October, the Centers for Medicare and Medicaid Services (CMS) plans to no longer reimburse for specific preventable conditions.
CMS “Stop Payments”
If Congress approves Medicare’s plan, the CMS will not pay any extra-care costs for eight conditions unless they were present upon admission—and it prohibits hospitals from charging patients for such conditions. The conditions include three “never events”:
- Objects left in the body during surgery (“never event”);
- Air embolism (“never event”);
- Blood incompatibility (“never event”);
- Falls;
- Catheter-associated urinary tract infections;
- Pressure ulcers (decubitus ulcers);
- Vascular catheter-associated infection; and
- Surgical site infection after coronary artery bypass graft surgery (mediastinitis).
Next year, the CMS plans to add more conditions to the no-pay list. The most likely additions are ventilator-associated pneumonia, staphylococcus aureus septicemia, deep-vein thrombosis (DVT), and pulmonary embolism.
The CMS rule obviously directly affects hospital income, which will affect hospital processes and staff.
“As hospitalists, this affects us,” says Winthrop F. Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., director of hospital medicine at Catholic Health East, and co-founder of SHM. “It’s another thing showcasing the value of hospitalists because we tend to document well. When a patient comes in with DVT or a pressure ulcer, we tend to document that, and that will help our hospitals.”
Other physicians may balk at hospital requests to amend or add to their notes to ensure payment, but, says Dr. Whitcomb: “Hospitalists understand the requirement for documentation. If you’re not a hospitalist, you may not be happy to be asked to change your documentation so that the hospital can get paid more, but we understand how important this is.”
Hospitals likely will continue to closely oversee physician documentation on Medicare patients.
“At our hospital, we [already] work with coders,” Dr. Whitcomb says. “I’ve heard of this more and more. They round with us now on every Medicare patient and review the charts. They actually write a formal note that prompts us to document accurately—they may ask us to amend that something was present on admission.” Dr. Whitcomb’s hospital has a paper-based system for this information; an electronic system will include this type of prompt. “Electronic prompts can be customized, but they can also be ignored; prompt fatigue is a big issue,” Dr. Whitcomb warns.
Another potential effect on hospitalists will be involvement in hospital efforts to prevent the eight conditions.
“The CMS change is definitely going to up the ante for quality improvement and patient safety work, no matter who undertakes it,” Dr. Whitcomb says. “It should expand opportunities for hospitalists to work in [quality improvement]. Hospitalists may end up leading teams to specifically address certain never events. The good news is, it gets right at the bottom line of the hospital, so nonclinicians like administrators in the financial office will immediately understand the importance of work like this.”
Leaving a sponge inside a patient is clearly a preventable medical error—but what about pressure ulcers? Or DVT?
In his “Wachter’s World” blog post of Feb. 11 (www.wachtersworld.org), Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, addressed the CMS rule.
“For some of the events on the Medicare list, particularly the infections (such as catheter-related bloodstream infections), there is good evidence that the vast majority of events can be prevented,” Dr. Wachter wrote. “For others, such as pressure ulcers and falls, although some commonsensical practices have been widely promoted (particularly through IHI’s 5 Million Lives campaign), the evidence linking adherence to ‘prevention practices’ and reductions in adverse events is tenuous. These adverse events should stay off the list until the evidence is stronger.”
In spite of his misgivings, Dr. Wachter is a strong proponent of the trend toward nonpayment for preventable errors. “We’ve already seen hospitals putting far more resources into trying to prevent line infections, falls, and [pressure ulcers] than they were before,” he says. “And remember that the dollars at stake are relatively small. The extra payments for “Complicating Conditions” (CC) are not enormous, and many patients who have one CC have more than one; in which case, the hospital will still receive the extra payment even if the adverse event-related payment is denied. So, in essence the policy is creating an unusual amount of patient safety momentum for a relatively small displacement of dollars – a pretty clever trick.”
For more information on the CMS rule, read “Medicare’s decision to withhold payment for hospital errors: the devil is in the details,” by Dr. Wachter, Nancy Foster, and Adams Dudley, MD, in the February 2008 Joint Commission Journal of Quality and Patient Safety. TH
Jane Jerrard is a medical writer based in Chicago.
Mentorship Essentials
You may have had a mentor as a resident and possibly in your first year as a hospitalist, but don’t count out these valuable resources as you continue in your career. And don’t count out mentors who may come from other walks of life.
“It’s natural for physicians to look toward other physicians for guidance,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare, Nashville. “For physicians, including hospitalists, their natural inclination is to seek mentors who are physicians or have a similar training background. While there are many great physician mentors, you may be limiting yourself and missing opportunities that come from broader mentoring.”
Informal mentoring relationships are an excellent way to learn all sorts of leadership skills, from the subtle—like handling complains about a physician’s constant body odor—to hard skills, such as putting together a budget for your department or practice.
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, Nashville
Management Mentors
Dr. Holman identified people at various stages in his career who could impart skills he sought, from a vice president of [human relations] for an integrated health system who steered him on personnel management and leadership development, to a carpenter-turned-attorney who helped him hone critical thinking skills.
“Talking to a mentor can show you the fresh side of new or old situations,” says Dr. Holman. “And you can feel comfortable telling them things that you wouldn’t tell anyone else. [When] you don’t work together, it provides a safe harbor to express ideas and opinions you normally wouldn’t.”
Mary Jo Gorman, MD, MBA, chief executive officer of Advanced ICU Care in St. Louis, Mo., agrees. “If you want someone to bounce ideas off of, try to find someone outside your organization,” she advises. She recommends physician organizations such as SHM: “Find someone who will listen, can keep their mouth shut and give you some honest feedback. For that reason, I’m a fan of professional coaches and career counselors. They provide an objective and unbiased audience and can suggest straightforward ways to manage sensitive issues.”
You also can find valuable mentors inside your workplace. “An often overlooked resource for hospitalist leaders is the other managers in their facilities,” says Dr. Gorman. “When I was a new manager, one of my mentors was the director of nursing. We could toss ideas back and forth, and she knew the politics and the personalities of the place, knew what mattered and what didn’t, and could steer me in the right direction.”
The managers and directors you work with, regardless of whether they’re physicians, are likely to have a lot of management experience, and can be resources for on-the-spot advice and guidance.
“Depending on the situation, even a chief operating officer or CEO of your hospital can give you good ideas and help you,” adds Dr. Gorman. “You’re a hospitalist; they’re supposed to be on your side. And they may be just five or 10 years older than you, but they have a lot of people management experience under their belts.”
They’re Everywhere
If you look beyond physicians and other healthcare professionals, finding an informal mentor is simply a matter of keeping your eyes and your mind open.
“You find a mentor by being in different situations,” Dr. Holman says. “Take advantage of getting to know people in different spheres, see what makes them tick that you can learn and apply to yourself.”
Consider all aspects of your life outside the workplace—your neighborhood, your church, your children’s school, any organizations you volunteer for, or social venues. Even your family—does anyone have management or business experience?
Keep your options open for learning from others, but if you have a specific area where you want to gain knowledge, you can search your circle of acquaintances to see who might be able to fill in that gap.
“Outside of healthcare, my personal accountant was a huge help,” says Dr. Gorman. “He sat down with me and helped me understand the financials I was supposed to do. You may have to pay for this service, but if you’re just asking for a few hours of their time and you have a good relationship, they’ll help you out.”
Regardless of what you want to learn, keep in mind that mentors can come in any shape and form. “A mentor can be someone younger than you, someone less well educated,” Dr. Holman points out. “What matters is when you recognize the value of the perspectives they bring.”
In fact, Dr. Holman says, he deliberately looks for people who are a little different from himself. “We tend to gravitate to those who are like us, but [in mentoring] this doesn’t lend itself to the greatest growth long-term,” he explains.
Make Mentoring Work
When you target someone as a potential mentor, it’s best to start with occasional questions and keep the relationship casual.
“My experience—and this is supported by literature—is that mentoring relationships are most solid when they form naturally,” Dr. Holman says. “The mentorship arena lends itself to flexibility and informal structure.”
Dr. Gorman agrees, suggesting that you not even mention “the M word.” “In my experience, asking someone flat out if they’ll be your mentor doesn’t really work,” Dr. Gorman says. “It sounds like a big commitment, and they shy away from it. Instead, I’d say just keep going back to the same people for guidance. Find those people who will listen to you and give you some help.”
Once you establish a mentoring relationship, try to find a way to return the favor—at least by being a good mentee.
“It’s particularly rewarding when mentoring is not one-sided, when each person has something to bring to the table,” Dr. Holman says. “Though it may be mostly one-sided, it’s good to be able to give some advice or counsel in return.”
Dr. Gorman adds that a good mentee either will act on advice or address why they didn’t. “No one likes to give advice just to see you blow it off, or head straight into a situation they warned you against,” she stresses. “Be respectful of their time, and be prepared when you present a problem. And be sure to thank them. You don’t have to send flowers or anything, just a verbal thank you for their time.”
No matter what stage your career is in, you can always pick up new skills and perspectives—particularly if you’re in a leadership position. Even if you feel you’re well established, finding new mentors can only make you better at what you do.
“You should always look for someone to learn from,” Dr. Gorman says. “They’re out there, no matter where you are or what you’re doing. Throw out some questions and see who you hit it off with, who gives you sound advice.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
You may have had a mentor as a resident and possibly in your first year as a hospitalist, but don’t count out these valuable resources as you continue in your career. And don’t count out mentors who may come from other walks of life.
“It’s natural for physicians to look toward other physicians for guidance,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare, Nashville. “For physicians, including hospitalists, their natural inclination is to seek mentors who are physicians or have a similar training background. While there are many great physician mentors, you may be limiting yourself and missing opportunities that come from broader mentoring.”
Informal mentoring relationships are an excellent way to learn all sorts of leadership skills, from the subtle—like handling complains about a physician’s constant body odor—to hard skills, such as putting together a budget for your department or practice.
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, Nashville
Management Mentors
Dr. Holman identified people at various stages in his career who could impart skills he sought, from a vice president of [human relations] for an integrated health system who steered him on personnel management and leadership development, to a carpenter-turned-attorney who helped him hone critical thinking skills.
“Talking to a mentor can show you the fresh side of new or old situations,” says Dr. Holman. “And you can feel comfortable telling them things that you wouldn’t tell anyone else. [When] you don’t work together, it provides a safe harbor to express ideas and opinions you normally wouldn’t.”
Mary Jo Gorman, MD, MBA, chief executive officer of Advanced ICU Care in St. Louis, Mo., agrees. “If you want someone to bounce ideas off of, try to find someone outside your organization,” she advises. She recommends physician organizations such as SHM: “Find someone who will listen, can keep their mouth shut and give you some honest feedback. For that reason, I’m a fan of professional coaches and career counselors. They provide an objective and unbiased audience and can suggest straightforward ways to manage sensitive issues.”
You also can find valuable mentors inside your workplace. “An often overlooked resource for hospitalist leaders is the other managers in their facilities,” says Dr. Gorman. “When I was a new manager, one of my mentors was the director of nursing. We could toss ideas back and forth, and she knew the politics and the personalities of the place, knew what mattered and what didn’t, and could steer me in the right direction.”
The managers and directors you work with, regardless of whether they’re physicians, are likely to have a lot of management experience, and can be resources for on-the-spot advice and guidance.
“Depending on the situation, even a chief operating officer or CEO of your hospital can give you good ideas and help you,” adds Dr. Gorman. “You’re a hospitalist; they’re supposed to be on your side. And they may be just five or 10 years older than you, but they have a lot of people management experience under their belts.”
They’re Everywhere
If you look beyond physicians and other healthcare professionals, finding an informal mentor is simply a matter of keeping your eyes and your mind open.
“You find a mentor by being in different situations,” Dr. Holman says. “Take advantage of getting to know people in different spheres, see what makes them tick that you can learn and apply to yourself.”
Consider all aspects of your life outside the workplace—your neighborhood, your church, your children’s school, any organizations you volunteer for, or social venues. Even your family—does anyone have management or business experience?
Keep your options open for learning from others, but if you have a specific area where you want to gain knowledge, you can search your circle of acquaintances to see who might be able to fill in that gap.
“Outside of healthcare, my personal accountant was a huge help,” says Dr. Gorman. “He sat down with me and helped me understand the financials I was supposed to do. You may have to pay for this service, but if you’re just asking for a few hours of their time and you have a good relationship, they’ll help you out.”
Regardless of what you want to learn, keep in mind that mentors can come in any shape and form. “A mentor can be someone younger than you, someone less well educated,” Dr. Holman points out. “What matters is when you recognize the value of the perspectives they bring.”
In fact, Dr. Holman says, he deliberately looks for people who are a little different from himself. “We tend to gravitate to those who are like us, but [in mentoring] this doesn’t lend itself to the greatest growth long-term,” he explains.
Make Mentoring Work
When you target someone as a potential mentor, it’s best to start with occasional questions and keep the relationship casual.
“My experience—and this is supported by literature—is that mentoring relationships are most solid when they form naturally,” Dr. Holman says. “The mentorship arena lends itself to flexibility and informal structure.”
Dr. Gorman agrees, suggesting that you not even mention “the M word.” “In my experience, asking someone flat out if they’ll be your mentor doesn’t really work,” Dr. Gorman says. “It sounds like a big commitment, and they shy away from it. Instead, I’d say just keep going back to the same people for guidance. Find those people who will listen to you and give you some help.”
Once you establish a mentoring relationship, try to find a way to return the favor—at least by being a good mentee.
“It’s particularly rewarding when mentoring is not one-sided, when each person has something to bring to the table,” Dr. Holman says. “Though it may be mostly one-sided, it’s good to be able to give some advice or counsel in return.”
Dr. Gorman adds that a good mentee either will act on advice or address why they didn’t. “No one likes to give advice just to see you blow it off, or head straight into a situation they warned you against,” she stresses. “Be respectful of their time, and be prepared when you present a problem. And be sure to thank them. You don’t have to send flowers or anything, just a verbal thank you for their time.”
No matter what stage your career is in, you can always pick up new skills and perspectives—particularly if you’re in a leadership position. Even if you feel you’re well established, finding new mentors can only make you better at what you do.
“You should always look for someone to learn from,” Dr. Gorman says. “They’re out there, no matter where you are or what you’re doing. Throw out some questions and see who you hit it off with, who gives you sound advice.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
You may have had a mentor as a resident and possibly in your first year as a hospitalist, but don’t count out these valuable resources as you continue in your career. And don’t count out mentors who may come from other walks of life.
“It’s natural for physicians to look toward other physicians for guidance,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare, Nashville. “For physicians, including hospitalists, their natural inclination is to seek mentors who are physicians or have a similar training background. While there are many great physician mentors, you may be limiting yourself and missing opportunities that come from broader mentoring.”
Informal mentoring relationships are an excellent way to learn all sorts of leadership skills, from the subtle—like handling complains about a physician’s constant body odor—to hard skills, such as putting together a budget for your department or practice.
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, Nashville
Management Mentors
Dr. Holman identified people at various stages in his career who could impart skills he sought, from a vice president of [human relations] for an integrated health system who steered him on personnel management and leadership development, to a carpenter-turned-attorney who helped him hone critical thinking skills.
“Talking to a mentor can show you the fresh side of new or old situations,” says Dr. Holman. “And you can feel comfortable telling them things that you wouldn’t tell anyone else. [When] you don’t work together, it provides a safe harbor to express ideas and opinions you normally wouldn’t.”
Mary Jo Gorman, MD, MBA, chief executive officer of Advanced ICU Care in St. Louis, Mo., agrees. “If you want someone to bounce ideas off of, try to find someone outside your organization,” she advises. She recommends physician organizations such as SHM: “Find someone who will listen, can keep their mouth shut and give you some honest feedback. For that reason, I’m a fan of professional coaches and career counselors. They provide an objective and unbiased audience and can suggest straightforward ways to manage sensitive issues.”
You also can find valuable mentors inside your workplace. “An often overlooked resource for hospitalist leaders is the other managers in their facilities,” says Dr. Gorman. “When I was a new manager, one of my mentors was the director of nursing. We could toss ideas back and forth, and she knew the politics and the personalities of the place, knew what mattered and what didn’t, and could steer me in the right direction.”
The managers and directors you work with, regardless of whether they’re physicians, are likely to have a lot of management experience, and can be resources for on-the-spot advice and guidance.
“Depending on the situation, even a chief operating officer or CEO of your hospital can give you good ideas and help you,” adds Dr. Gorman. “You’re a hospitalist; they’re supposed to be on your side. And they may be just five or 10 years older than you, but they have a lot of people management experience under their belts.”
They’re Everywhere
If you look beyond physicians and other healthcare professionals, finding an informal mentor is simply a matter of keeping your eyes and your mind open.
“You find a mentor by being in different situations,” Dr. Holman says. “Take advantage of getting to know people in different spheres, see what makes them tick that you can learn and apply to yourself.”
Consider all aspects of your life outside the workplace—your neighborhood, your church, your children’s school, any organizations you volunteer for, or social venues. Even your family—does anyone have management or business experience?
Keep your options open for learning from others, but if you have a specific area where you want to gain knowledge, you can search your circle of acquaintances to see who might be able to fill in that gap.
“Outside of healthcare, my personal accountant was a huge help,” says Dr. Gorman. “He sat down with me and helped me understand the financials I was supposed to do. You may have to pay for this service, but if you’re just asking for a few hours of their time and you have a good relationship, they’ll help you out.”
Regardless of what you want to learn, keep in mind that mentors can come in any shape and form. “A mentor can be someone younger than you, someone less well educated,” Dr. Holman points out. “What matters is when you recognize the value of the perspectives they bring.”
In fact, Dr. Holman says, he deliberately looks for people who are a little different from himself. “We tend to gravitate to those who are like us, but [in mentoring] this doesn’t lend itself to the greatest growth long-term,” he explains.
Make Mentoring Work
When you target someone as a potential mentor, it’s best to start with occasional questions and keep the relationship casual.
“My experience—and this is supported by literature—is that mentoring relationships are most solid when they form naturally,” Dr. Holman says. “The mentorship arena lends itself to flexibility and informal structure.”
Dr. Gorman agrees, suggesting that you not even mention “the M word.” “In my experience, asking someone flat out if they’ll be your mentor doesn’t really work,” Dr. Gorman says. “It sounds like a big commitment, and they shy away from it. Instead, I’d say just keep going back to the same people for guidance. Find those people who will listen to you and give you some help.”
Once you establish a mentoring relationship, try to find a way to return the favor—at least by being a good mentee.
“It’s particularly rewarding when mentoring is not one-sided, when each person has something to bring to the table,” Dr. Holman says. “Though it may be mostly one-sided, it’s good to be able to give some advice or counsel in return.”
Dr. Gorman adds that a good mentee either will act on advice or address why they didn’t. “No one likes to give advice just to see you blow it off, or head straight into a situation they warned you against,” she stresses. “Be respectful of their time, and be prepared when you present a problem. And be sure to thank them. You don’t have to send flowers or anything, just a verbal thank you for their time.”
No matter what stage your career is in, you can always pick up new skills and perspectives—particularly if you’re in a leadership position. Even if you feel you’re well established, finding new mentors can only make you better at what you do.
“You should always look for someone to learn from,” Dr. Gorman says. “They’re out there, no matter where you are or what you’re doing. Throw out some questions and see who you hit it off with, who gives you sound advice.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Nurse Ratios Suffer
Several studies have linked lower nurse-to-patient ratios with fewer medical errors and deaths, better overall treatment, and reduced rates of nurse burnout. These findings led California, in 1999, to pass the country’s first law mandating a minimum nurse-to-patient staffing ratio.
By 2004, the mandated ratio was one licensed nurse for every six patients; that was decreased in 2005 to one nurse for every five patients. Since then, similar bills have been passed or proposed in at least 25 more states. The benefits to patients and nurses of these improved ratios are clear. However, their effect on hospitalists, other staff members, and hospitals have not been widely studied. Further, the mandates often do not come with additional money to implement them.
In this month’s issue of the Journal of Hospital Medicine, Patrick Conway, MD, and colleagues examine nurse staffing trends in California hospitals since the mandate went into effect. They were particularly interested in what they called “safety net” hospitals: urban, government-owned, resource-poor institutions with at least 36% of patients uninsured or on Medicaid.
Dr. Conway, a pediatric hospitalist and assistant professor of pediatrics at the Cincinnati Children’s Hospital Medical Center, and his coauthors hypothesized that cash-strapped hospitals would find it hard to meet the mandate and might shortchange other programs in an effort to comply. Laudable as such legislation might be, “we wanted to make it clear to hospitalists and hospitals that the ratios could have an impact on other goals they wanted to achieve, such as meeting pay-for-performance targets,” he says.
Using financial data from the California Office of Statewide Health Planning and Development, they examined staffing trends on adult general medical surgical units in short-term, acute-care general hospitals from 1993 to 2004, the most recent years for which complete data was available. For 2003 and 2004, they also analyzed staff ratios according to five characteristics: hospital ownership (profit, nonprofit, government-owned), market competitiveness, teaching status, location (urban vs. rural), and whether or not the hospital met the definition of a safety net facility.
From 1993-99, nurse staffing ratios remained flat; they rose steadily thereafter. Not surprisingly, the largest increase occurred between 2003 and 2004, the year implementation was slated to go into effect. During that period, the median ratio for all hospitals studied went from less than one nurse per four patients to more than 1:4, exceeding the mandated figure. Fewer than 25% of hospitals fell short of the minimum mandate of 1:5.
However, further analysis reveals more nuances. The mandate requires a minimum ratio of licensed nurses to patients; those nurses can be registered nurses (RNs), licensed vocational nurses (LVNs), or a combination. In 2004, only 2.4% of hospitals fell below the mandated minimum for that year of 1:6, compared with 5% from the year before—but 11.4% were below 1:5 (RNs plus LVNs). When RNs only were considered, 29.5% of hospitals fell short of one for every five patients.
Further, some states are considering a minimum mandate of one licensed nurse per every four patients—yet 40.4% of the hospitals in this study did not meet that standard. “This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased,” the authors point out.
The finding that nearly 30% of hospitals had less than one registered nurse for every five patients was surprising, says Dr. Conway, whose wife is a registered nurse. In other words, “if you or I or our parents were admitted to a hospital, your chances are about one in three that they will have less than one nurse for every five patients. That means each nurse has less time to spend per patient.”
For-profit hospitals, non-teaching hospitals, and hospitals in urban or more competitive locations fared best at achieving the mandated ratios. However, hospitals with high Medicaid or uninsured populations were significantly more likely to fall below the minimum ratios than their more affluent counterparts and did not achieve the marked gains in staffing ratios achieved in other facilities.
All in all, more than 20% of safety net hospitals failed to achieve the 2004 mandate of 1:5, compared with about 12% of the other types of hospitals.
Of the safety net hospitals that did achieve the mandate, one wonders what types of tradeoffs they had to make, Dr. Conway adds: “Are they closing emergency rooms? Investing less in new equipment and facilities? Hiring less-trained staff? This study raises those questions, although it doesn’t answer them.”
More and more, hospitalists are being held responsible for quality improvement programs and outcomes measures within hospitals. The targets monitored often are those most strongly influenced by nurse presence, such as the number of central line infections, pressure ulcers, urinary tract infections, ventilator-acquired pneumonia, and similar conditions.
On the other hand, “no one has yet studied what happens when a hospital goes from a ratio of 1:5 to 1:4,” Dr. Conway says. It is possible that the [patient] gains realized may not be large enough to justify the compromises a hospital might have to make in other areas to meet that goal. “We must determine what the tradeoffs are and identify optimal nurse staffing ratios. Adequate nurse staffing is a significant key to achieving a successful team management approach in a hospital.” TH
Norra MacReady is a medical writer based in California.
Editor’s note: Dr. Conway was featured in the February 2008 issue (p. 28) as a member of the White House Fellows Program.
Several studies have linked lower nurse-to-patient ratios with fewer medical errors and deaths, better overall treatment, and reduced rates of nurse burnout. These findings led California, in 1999, to pass the country’s first law mandating a minimum nurse-to-patient staffing ratio.
By 2004, the mandated ratio was one licensed nurse for every six patients; that was decreased in 2005 to one nurse for every five patients. Since then, similar bills have been passed or proposed in at least 25 more states. The benefits to patients and nurses of these improved ratios are clear. However, their effect on hospitalists, other staff members, and hospitals have not been widely studied. Further, the mandates often do not come with additional money to implement them.
In this month’s issue of the Journal of Hospital Medicine, Patrick Conway, MD, and colleagues examine nurse staffing trends in California hospitals since the mandate went into effect. They were particularly interested in what they called “safety net” hospitals: urban, government-owned, resource-poor institutions with at least 36% of patients uninsured or on Medicaid.
Dr. Conway, a pediatric hospitalist and assistant professor of pediatrics at the Cincinnati Children’s Hospital Medical Center, and his coauthors hypothesized that cash-strapped hospitals would find it hard to meet the mandate and might shortchange other programs in an effort to comply. Laudable as such legislation might be, “we wanted to make it clear to hospitalists and hospitals that the ratios could have an impact on other goals they wanted to achieve, such as meeting pay-for-performance targets,” he says.
Using financial data from the California Office of Statewide Health Planning and Development, they examined staffing trends on adult general medical surgical units in short-term, acute-care general hospitals from 1993 to 2004, the most recent years for which complete data was available. For 2003 and 2004, they also analyzed staff ratios according to five characteristics: hospital ownership (profit, nonprofit, government-owned), market competitiveness, teaching status, location (urban vs. rural), and whether or not the hospital met the definition of a safety net facility.
From 1993-99, nurse staffing ratios remained flat; they rose steadily thereafter. Not surprisingly, the largest increase occurred between 2003 and 2004, the year implementation was slated to go into effect. During that period, the median ratio for all hospitals studied went from less than one nurse per four patients to more than 1:4, exceeding the mandated figure. Fewer than 25% of hospitals fell short of the minimum mandate of 1:5.
However, further analysis reveals more nuances. The mandate requires a minimum ratio of licensed nurses to patients; those nurses can be registered nurses (RNs), licensed vocational nurses (LVNs), or a combination. In 2004, only 2.4% of hospitals fell below the mandated minimum for that year of 1:6, compared with 5% from the year before—but 11.4% were below 1:5 (RNs plus LVNs). When RNs only were considered, 29.5% of hospitals fell short of one for every five patients.
Further, some states are considering a minimum mandate of one licensed nurse per every four patients—yet 40.4% of the hospitals in this study did not meet that standard. “This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased,” the authors point out.
The finding that nearly 30% of hospitals had less than one registered nurse for every five patients was surprising, says Dr. Conway, whose wife is a registered nurse. In other words, “if you or I or our parents were admitted to a hospital, your chances are about one in three that they will have less than one nurse for every five patients. That means each nurse has less time to spend per patient.”
For-profit hospitals, non-teaching hospitals, and hospitals in urban or more competitive locations fared best at achieving the mandated ratios. However, hospitals with high Medicaid or uninsured populations were significantly more likely to fall below the minimum ratios than their more affluent counterparts and did not achieve the marked gains in staffing ratios achieved in other facilities.
All in all, more than 20% of safety net hospitals failed to achieve the 2004 mandate of 1:5, compared with about 12% of the other types of hospitals.
Of the safety net hospitals that did achieve the mandate, one wonders what types of tradeoffs they had to make, Dr. Conway adds: “Are they closing emergency rooms? Investing less in new equipment and facilities? Hiring less-trained staff? This study raises those questions, although it doesn’t answer them.”
More and more, hospitalists are being held responsible for quality improvement programs and outcomes measures within hospitals. The targets monitored often are those most strongly influenced by nurse presence, such as the number of central line infections, pressure ulcers, urinary tract infections, ventilator-acquired pneumonia, and similar conditions.
On the other hand, “no one has yet studied what happens when a hospital goes from a ratio of 1:5 to 1:4,” Dr. Conway says. It is possible that the [patient] gains realized may not be large enough to justify the compromises a hospital might have to make in other areas to meet that goal. “We must determine what the tradeoffs are and identify optimal nurse staffing ratios. Adequate nurse staffing is a significant key to achieving a successful team management approach in a hospital.” TH
Norra MacReady is a medical writer based in California.
Editor’s note: Dr. Conway was featured in the February 2008 issue (p. 28) as a member of the White House Fellows Program.
Several studies have linked lower nurse-to-patient ratios with fewer medical errors and deaths, better overall treatment, and reduced rates of nurse burnout. These findings led California, in 1999, to pass the country’s first law mandating a minimum nurse-to-patient staffing ratio.
By 2004, the mandated ratio was one licensed nurse for every six patients; that was decreased in 2005 to one nurse for every five patients. Since then, similar bills have been passed or proposed in at least 25 more states. The benefits to patients and nurses of these improved ratios are clear. However, their effect on hospitalists, other staff members, and hospitals have not been widely studied. Further, the mandates often do not come with additional money to implement them.
In this month’s issue of the Journal of Hospital Medicine, Patrick Conway, MD, and colleagues examine nurse staffing trends in California hospitals since the mandate went into effect. They were particularly interested in what they called “safety net” hospitals: urban, government-owned, resource-poor institutions with at least 36% of patients uninsured or on Medicaid.
Dr. Conway, a pediatric hospitalist and assistant professor of pediatrics at the Cincinnati Children’s Hospital Medical Center, and his coauthors hypothesized that cash-strapped hospitals would find it hard to meet the mandate and might shortchange other programs in an effort to comply. Laudable as such legislation might be, “we wanted to make it clear to hospitalists and hospitals that the ratios could have an impact on other goals they wanted to achieve, such as meeting pay-for-performance targets,” he says.
Using financial data from the California Office of Statewide Health Planning and Development, they examined staffing trends on adult general medical surgical units in short-term, acute-care general hospitals from 1993 to 2004, the most recent years for which complete data was available. For 2003 and 2004, they also analyzed staff ratios according to five characteristics: hospital ownership (profit, nonprofit, government-owned), market competitiveness, teaching status, location (urban vs. rural), and whether or not the hospital met the definition of a safety net facility.
From 1993-99, nurse staffing ratios remained flat; they rose steadily thereafter. Not surprisingly, the largest increase occurred between 2003 and 2004, the year implementation was slated to go into effect. During that period, the median ratio for all hospitals studied went from less than one nurse per four patients to more than 1:4, exceeding the mandated figure. Fewer than 25% of hospitals fell short of the minimum mandate of 1:5.
However, further analysis reveals more nuances. The mandate requires a minimum ratio of licensed nurses to patients; those nurses can be registered nurses (RNs), licensed vocational nurses (LVNs), or a combination. In 2004, only 2.4% of hospitals fell below the mandated minimum for that year of 1:6, compared with 5% from the year before—but 11.4% were below 1:5 (RNs plus LVNs). When RNs only were considered, 29.5% of hospitals fell short of one for every five patients.
Further, some states are considering a minimum mandate of one licensed nurse per every four patients—yet 40.4% of the hospitals in this study did not meet that standard. “This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased,” the authors point out.
The finding that nearly 30% of hospitals had less than one registered nurse for every five patients was surprising, says Dr. Conway, whose wife is a registered nurse. In other words, “if you or I or our parents were admitted to a hospital, your chances are about one in three that they will have less than one nurse for every five patients. That means each nurse has less time to spend per patient.”
For-profit hospitals, non-teaching hospitals, and hospitals in urban or more competitive locations fared best at achieving the mandated ratios. However, hospitals with high Medicaid or uninsured populations were significantly more likely to fall below the minimum ratios than their more affluent counterparts and did not achieve the marked gains in staffing ratios achieved in other facilities.
All in all, more than 20% of safety net hospitals failed to achieve the 2004 mandate of 1:5, compared with about 12% of the other types of hospitals.
Of the safety net hospitals that did achieve the mandate, one wonders what types of tradeoffs they had to make, Dr. Conway adds: “Are they closing emergency rooms? Investing less in new equipment and facilities? Hiring less-trained staff? This study raises those questions, although it doesn’t answer them.”
More and more, hospitalists are being held responsible for quality improvement programs and outcomes measures within hospitals. The targets monitored often are those most strongly influenced by nurse presence, such as the number of central line infections, pressure ulcers, urinary tract infections, ventilator-acquired pneumonia, and similar conditions.
On the other hand, “no one has yet studied what happens when a hospital goes from a ratio of 1:5 to 1:4,” Dr. Conway says. It is possible that the [patient] gains realized may not be large enough to justify the compromises a hospital might have to make in other areas to meet that goal. “We must determine what the tradeoffs are and identify optimal nurse staffing ratios. Adequate nurse staffing is a significant key to achieving a successful team management approach in a hospital.” TH
Norra MacReady is a medical writer based in California.
Editor’s note: Dr. Conway was featured in the February 2008 issue (p. 28) as a member of the White House Fellows Program.
Protect the Platelets
The frequency of drug-induced thrombocytopenia (DIT) in acutely ill patients is thought to be up to 25%, making it a common problem.1,2
Hundreds of drugs have been identified as causing DIT, due to either accelerated immune-mediated platelet destruction, decreased platelet production (bone marrow suppression), or platelet aggregation. The latter is the case in heparin-induced thrombocytopenia and thrombosis (HITT). DIT should be suspected in any patient who presents with acute thrombocytopenia from an unknown cause.3
Normal adult platelet counts usually are in the range of 140,000 to 450,000/mm3. A patient who presents with severe thrombocytopenia (less than 20,000 platelets/mm3) should strongly be suspected as having a drug-induced cause.
A patient also can present with moderate to severe thrombocytopenia (less than 50,000 platelets/mm3) and spontaneous bleeding from a drug-induced cause. The spontaneous bleeding can take the form of simple petechiae or ecchymoses, as well as mucosal bleeding or life-threatening intracranial or gastrointestinal hemorrhage. It may also present itself as bleeding around catheter insertion sites.
When DIT occurs, platelet count usually falls within two to three days of taking a drug that’s been taken before, or seven or more days after starting a drug the patient has not been exposed to. Once the offending drug is discontinued, platelet counts usually recover within 10 days.
Exclusions of other causes of thrombocytopenia, such as inflammatory processes and congenital disorders, as well as nondrug causes including sepsis, malignancy, extensive burns, chronic alcoholism, human immunodeficiency virus, splenomegaly, and disseminated intravascular coagulation, become part of the differential diagnosis.
Generally, the frequency and severity of bleeding manifestations correlate with the actual platelet count. Patients with a platelet count of less than 50,000/mm3 have an increased risk of spontaneous hemorrhage, but the severity may vary. Other risk factors include advanced age, bleeding history, and general bleeding diatheses.
A thorough physical examination and drug history are essential. Agents commonly associated with thrombocytopenia should be identified first followed by a more extensive review for other causes. A careful drug history should include prescriptions, over-the-counter medications (specifically quinine and acetaminophen), dietary supplements, folk remedies, other complementary and alternative therapies, and vaccinations.
The Agents
The top two suspects for DIT are antineoplastic agents and heparin. After these two, the agents most frequently associated with DIT development include:
- Quinine/quinidine;
- Phenytoin;
- Sulfonamide antibiotics;
- Cimetidine;
- Ranitidine;
- Rifampin/rifampicin;
- Carbamazepine;
- Thiazide diuretics;
- Penicillin;
- Oral antidiabetic drugs;
- Nonsteroidal anti-inflammatory drugs;
- Gold salts; and
- Procainamide.
A complete list of all case reports describing DIT, organized by generic
drug names, is available online at http://w3.ouhsc.edu/platelets/ditp.html.4
Management
Removal of the potentially offending agent, if known, is prudent before clinically significant bleeding occurs. If the offending agent is not discontinued, the platelet count will continue to decrease and bleeding will become more severe. If necessary, an alternate agent with a similar pharmacologic effect can be started. Daily platelet count monitoring is also recommended for management. Rare cases may require platelet transfusions, intravenous immunoglobulin therapy or plasmapheresis.
A complete blood count and peripheral blood smear may provide important indications into the mechanism of the disorder, but they’re not necessary for patient management. TH
Michele B Kaufman, PharmD, BSc, is a registere pharmacist based in New York City.
References
- Visentin GP, Liu CY. Drug-induced thrombocytopenia. Hematol Oncol Clin N Am. 2007;21:685-696.
- Wazny LD, Ariano RE. Evaluation and management of drug-induced thrombocytopenia in the acutely ill patient. Pharmacother. 2000;20(3):292-307.
- Aster RH, Bougie DW. Drug-induced thrombocytopenia. N Engl J Med. 2007;357(6):580-587.
- Majhail NS, Lichtin AE. What is the best way to determine if thrombocytopenia in a patient on multiple medications is drug-induced? Cleve Clin J Med. 2002;69(3):259-262.
The frequency of drug-induced thrombocytopenia (DIT) in acutely ill patients is thought to be up to 25%, making it a common problem.1,2
Hundreds of drugs have been identified as causing DIT, due to either accelerated immune-mediated platelet destruction, decreased platelet production (bone marrow suppression), or platelet aggregation. The latter is the case in heparin-induced thrombocytopenia and thrombosis (HITT). DIT should be suspected in any patient who presents with acute thrombocytopenia from an unknown cause.3
Normal adult platelet counts usually are in the range of 140,000 to 450,000/mm3. A patient who presents with severe thrombocytopenia (less than 20,000 platelets/mm3) should strongly be suspected as having a drug-induced cause.
A patient also can present with moderate to severe thrombocytopenia (less than 50,000 platelets/mm3) and spontaneous bleeding from a drug-induced cause. The spontaneous bleeding can take the form of simple petechiae or ecchymoses, as well as mucosal bleeding or life-threatening intracranial or gastrointestinal hemorrhage. It may also present itself as bleeding around catheter insertion sites.
When DIT occurs, platelet count usually falls within two to three days of taking a drug that’s been taken before, or seven or more days after starting a drug the patient has not been exposed to. Once the offending drug is discontinued, platelet counts usually recover within 10 days.
Exclusions of other causes of thrombocytopenia, such as inflammatory processes and congenital disorders, as well as nondrug causes including sepsis, malignancy, extensive burns, chronic alcoholism, human immunodeficiency virus, splenomegaly, and disseminated intravascular coagulation, become part of the differential diagnosis.
Generally, the frequency and severity of bleeding manifestations correlate with the actual platelet count. Patients with a platelet count of less than 50,000/mm3 have an increased risk of spontaneous hemorrhage, but the severity may vary. Other risk factors include advanced age, bleeding history, and general bleeding diatheses.
A thorough physical examination and drug history are essential. Agents commonly associated with thrombocytopenia should be identified first followed by a more extensive review for other causes. A careful drug history should include prescriptions, over-the-counter medications (specifically quinine and acetaminophen), dietary supplements, folk remedies, other complementary and alternative therapies, and vaccinations.
The Agents
The top two suspects for DIT are antineoplastic agents and heparin. After these two, the agents most frequently associated with DIT development include:
- Quinine/quinidine;
- Phenytoin;
- Sulfonamide antibiotics;
- Cimetidine;
- Ranitidine;
- Rifampin/rifampicin;
- Carbamazepine;
- Thiazide diuretics;
- Penicillin;
- Oral antidiabetic drugs;
- Nonsteroidal anti-inflammatory drugs;
- Gold salts; and
- Procainamide.
A complete list of all case reports describing DIT, organized by generic
drug names, is available online at http://w3.ouhsc.edu/platelets/ditp.html.4
Management
Removal of the potentially offending agent, if known, is prudent before clinically significant bleeding occurs. If the offending agent is not discontinued, the platelet count will continue to decrease and bleeding will become more severe. If necessary, an alternate agent with a similar pharmacologic effect can be started. Daily platelet count monitoring is also recommended for management. Rare cases may require platelet transfusions, intravenous immunoglobulin therapy or plasmapheresis.
A complete blood count and peripheral blood smear may provide important indications into the mechanism of the disorder, but they’re not necessary for patient management. TH
Michele B Kaufman, PharmD, BSc, is a registere pharmacist based in New York City.
References
- Visentin GP, Liu CY. Drug-induced thrombocytopenia. Hematol Oncol Clin N Am. 2007;21:685-696.
- Wazny LD, Ariano RE. Evaluation and management of drug-induced thrombocytopenia in the acutely ill patient. Pharmacother. 2000;20(3):292-307.
- Aster RH, Bougie DW. Drug-induced thrombocytopenia. N Engl J Med. 2007;357(6):580-587.
- Majhail NS, Lichtin AE. What is the best way to determine if thrombocytopenia in a patient on multiple medications is drug-induced? Cleve Clin J Med. 2002;69(3):259-262.
The frequency of drug-induced thrombocytopenia (DIT) in acutely ill patients is thought to be up to 25%, making it a common problem.1,2
Hundreds of drugs have been identified as causing DIT, due to either accelerated immune-mediated platelet destruction, decreased platelet production (bone marrow suppression), or platelet aggregation. The latter is the case in heparin-induced thrombocytopenia and thrombosis (HITT). DIT should be suspected in any patient who presents with acute thrombocytopenia from an unknown cause.3
Normal adult platelet counts usually are in the range of 140,000 to 450,000/mm3. A patient who presents with severe thrombocytopenia (less than 20,000 platelets/mm3) should strongly be suspected as having a drug-induced cause.
A patient also can present with moderate to severe thrombocytopenia (less than 50,000 platelets/mm3) and spontaneous bleeding from a drug-induced cause. The spontaneous bleeding can take the form of simple petechiae or ecchymoses, as well as mucosal bleeding or life-threatening intracranial or gastrointestinal hemorrhage. It may also present itself as bleeding around catheter insertion sites.
When DIT occurs, platelet count usually falls within two to three days of taking a drug that’s been taken before, or seven or more days after starting a drug the patient has not been exposed to. Once the offending drug is discontinued, platelet counts usually recover within 10 days.
Exclusions of other causes of thrombocytopenia, such as inflammatory processes and congenital disorders, as well as nondrug causes including sepsis, malignancy, extensive burns, chronic alcoholism, human immunodeficiency virus, splenomegaly, and disseminated intravascular coagulation, become part of the differential diagnosis.
Generally, the frequency and severity of bleeding manifestations correlate with the actual platelet count. Patients with a platelet count of less than 50,000/mm3 have an increased risk of spontaneous hemorrhage, but the severity may vary. Other risk factors include advanced age, bleeding history, and general bleeding diatheses.
A thorough physical examination and drug history are essential. Agents commonly associated with thrombocytopenia should be identified first followed by a more extensive review for other causes. A careful drug history should include prescriptions, over-the-counter medications (specifically quinine and acetaminophen), dietary supplements, folk remedies, other complementary and alternative therapies, and vaccinations.
The Agents
The top two suspects for DIT are antineoplastic agents and heparin. After these two, the agents most frequently associated with DIT development include:
- Quinine/quinidine;
- Phenytoin;
- Sulfonamide antibiotics;
- Cimetidine;
- Ranitidine;
- Rifampin/rifampicin;
- Carbamazepine;
- Thiazide diuretics;
- Penicillin;
- Oral antidiabetic drugs;
- Nonsteroidal anti-inflammatory drugs;
- Gold salts; and
- Procainamide.
A complete list of all case reports describing DIT, organized by generic
drug names, is available online at http://w3.ouhsc.edu/platelets/ditp.html.4
Management
Removal of the potentially offending agent, if known, is prudent before clinically significant bleeding occurs. If the offending agent is not discontinued, the platelet count will continue to decrease and bleeding will become more severe. If necessary, an alternate agent with a similar pharmacologic effect can be started. Daily platelet count monitoring is also recommended for management. Rare cases may require platelet transfusions, intravenous immunoglobulin therapy or plasmapheresis.
A complete blood count and peripheral blood smear may provide important indications into the mechanism of the disorder, but they’re not necessary for patient management. TH
Michele B Kaufman, PharmD, BSc, is a registere pharmacist based in New York City.
References
- Visentin GP, Liu CY. Drug-induced thrombocytopenia. Hematol Oncol Clin N Am. 2007;21:685-696.
- Wazny LD, Ariano RE. Evaluation and management of drug-induced thrombocytopenia in the acutely ill patient. Pharmacother. 2000;20(3):292-307.
- Aster RH, Bougie DW. Drug-induced thrombocytopenia. N Engl J Med. 2007;357(6):580-587.
- Majhail NS, Lichtin AE. What is the best way to determine if thrombocytopenia in a patient on multiple medications is drug-induced? Cleve Clin J Med. 2002;69(3):259-262.
In the Literature
Literature at a Glance
A guide to this month’s studies.
- Physiologic doses of corticosteroids provide no clear benefit to patients with septic shock.
- Endovascular vs. open repair of abdominal aortic aneurysms is associated with fewer short-term deaths but complications and higher late reinterventions.
- Neither intensive insulin nor use of colloid over crystalloid improves mortality or organ failure outcomes in sepsis.
- Surgical cure for diabetes shows promise at two-year follow-up.
- Delayed defibrillation negatively affects survival.
- Right-ventricular enlargement in patients with acute PE is not associated with increased mortality.
- Periprocedural interruption of warfarin therapy presents low risk of thromboembolism.
- Minor leg injury increases risk of developing venous thrombosis threefold.
- Oral vs. parenteral antibiotics for pediatric pyelonephritis.
Do Physiologic Doses of Hydrocortisone Benefit Patients With Septic Shock?
Background: Meta-analyses and guidelines advocate the use of physiologic dose steroids in patients exhibiting septic shock. However, recommendations are largely based on the results of a single trial where benefits were seen only in patients without a response to corticotropin.
Study design: Multicenter, randomized, double-blind, placebo-controlled study.
Setting: Fifty-two participating ICUs in nine countries.
Synopsis: A total of 499 patients with evidence of infection or a systemic inflammatory response characterized by refractory hypotension were randomly selected to receive either an 11-day tapering dose of hydrocortisone or a placebo. The primary outcome was death from any cause at 28 days. A corticotropin stimulation test was conducted on every patient to assess adrenal function. There were no differences in death rates or duration of hospitalization between study arms. Overall, there were 86 deaths in the hydrocortisone group and 78 deaths in the placebo group (p=0.51). Also, response to corticotropin appeared to have little bearing on outcomes.
The study was underpowered due to low enrollment and a lower-than-expected death rate. Nevertheless, this is the largest trial to date examining the role of steroids in the management of septic shock and calls into question the strength of prior data and published guidelines.
Bottom line: This study failed to demonstrate a clinically or statistically significant treatment effect from the administration of physiologic-dose steroids in patients with septic shock.
Citation: Sprung C, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111-124.
Does Open or Endovascular Repair of Abdominal Aortic Aneurysm Benefit the Medicare Population?
Background: Randomized controlled trials (RCT) have shown a perioperative survival benefit of endovascular repair over open repair with fewer complications and shorter recovery. There is concern that late morbidity may be increased with endovascular repair. Patients enrolled in the trials were highly selected at specialty centers, so the results may not reflect actual practice.
Study design: Retrospective, propensity-matched, observational cohort study.
Synopsis: 22,830 patients were matched in each cohort. Patients were eligible if they had an abdominal aortic aneurysm repair without rupture and excluded if they were enrolled in health maintenance organizations.
Outcomes included death within 30 days and late survival, perioperative complications, aneurysm rupture, reintervention, and laparotomy-related complications. The average age was 76, and 20% were women. Perioperative mortality was lower after endovascular repair (1.2% vs. 4.8%, p<0.001), and older patients had a greater benefit. Late survival was similar. By four years, rupture was more likely in the endovascular group (1.8% vs. 0.5%, p<0.001), as was reintervention (9% vs. 1.7%, p<0.001).
In contrast, by four years, surgery for laparotomy-related complications was more likely in the open-repair group (9.7% v 4.1%, p<0.001), as was hospitalization for bowel obstruction or abdominal-wall hernia (14.2% v 8.1%, p<0.001). Limitations included the non-randomized design and use of administrative data for important categorical variables including medical co-morbidities.
Bottom line: As compared with open repair, endovascular repair of abdominal aortic aneurysm is associated with lower short-term death and complications and higher late reinterventions. This is balanced by an increase in laparotomy-related reinterventions after open repair.
Citation: Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008 Jan 31;358(5):464-474.
What Therapy Improves Outcomes in ICU Patients With Severe Sepsis or Septic Shock?
Background: Evidence suggests lower mortality with intensive insulin therapy in post-surgical cardiac patients. There is no proven benefit for non-surgical ICU patients. Despite lack of data, intensive insulin in severe sepsis has been widely advocated. Little is known to guide the use of colloid or crystalloid for fluid resuscitation in sepsis.
Study design: Multicenter, two-by-two factorial, open-label trial.
Setting: Multidisciplinary ICUs at 18 academic tertiary hospitals in Germany.
Synopsis: Data were analyzed for 537 patients with severe sepsis. They were randomly selected to receive intensive insulin therapy (n=247) or conventional insulin therapy (290), with either 10% hydroxyethyl starch (HES) (262) or modified Ringer’s lactate (LR) (275) for fluid resuscitation.
Co-primary endpoints were all-cause mortality at 28 days and morbidity as measured by the mean score on the Sequential Organ Failure Assessment (SOFA). The trial was stopped early for safety reasons. Intensive insulin therapy was terminated due to an increased number of hypoglycemic events in the intensive-therapy group compared with conventional therapy (12.1% vs. 2.1%, p<0.001), and there was no difference in mortality between groups at 28 and 90 days.
Interim analysis of 600 patients showed patients given HES had higher incidence of renal failure compared with LR (34.9% vs. 22.8%, p=0.002), required more days of renal replacement therapy, had lower median platelets and received more units of packed red cells. There was a trend toward higher rate of death at 90 days in those treated with HES (41% vs. 33.9%, p=0.09).
Bottom line: Intensive insulin therapy in ICU patients with severe sepsis and septic shock does not improve mortality and increases hypoglycemia and ICU length of stay. Use of colloid over crystalloid should be avoided, showing a trend toward increased death at 90 days, higher rates of acute renal failure, and need for renal replacement therapy..
Citation: Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125-139.
How Does Laparoscopic Adjustable Gastric Banding Affect Obese Adults With Type 2 Diabetes?
Background: Observational studies related surgical weight loss to improved glycemic control, but clinical trials did not test this relationship. The current trial examined this hypothesis.
Study design: Unmasked, randomized controlled trial.
Setting: University Obesity Research Center, Australia.
Synopsis: Sixty adults age 20-60 with body-mass index (BMI) of 30-40 and diagnosed with diabetes mellitus type 2 (DM2) within two years of recruitment were randomized into conventional therapy and surgical groups.
While both groups were treated similarly, only the surgical group received laparoscopic adjustable gastric banding. Primary outcome was remission of DM2 (a fasting glucose less than 126 mg/dl, HbA1C less than 6.2%, and off all hypoglycemic agents). At two years, 73% in the surgical group compared with 13% in the conventional group attained this outcome (relative risk [RR] 5.5, 95% confidence interval [CI] 2.2-14.0; p<0.001). Compared with the conventional group, the surgical group demonstrated statistically significant improvements in several secondary outcomes including mean body weight, waist circumference, insulin resistance, and lipids.
The limitations of the study are that it examined a small number of patients with shorter duration of DM2 and a shorter follow-up. The lower surgical complication rates cannot be generalized to other centers.
Bottom line: This study is a step forward in examining the relationship of surgical weight loss and remission of DM2. However, large multicenter trials with longer periods of follow-up in diverse group of patients would result in a better understanding of this relationship.
Citation: Dixon JB, O’Brien PE, Playfair J, et. al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299(3):316-323.
What is the Prevalence of Delayed Defibrillation and its Association With Survival to Discharge?
Background: Despite advances in resuscitation, survival rates following cardiac arrest remain low. Previous studies observed the effect of the timing of defibrillation on survival. This study examined the magnitude of delayed defibrillation and its association with survival in adults who sustained cardiac arrest specifically from ventricular fibrillation and pulseless ventricular tachycardia.
Study design: National Registry of Cardiopulmonary Resuscitation (NRCPR), a multicenter prospective cohort.
Setting: 369 U.S. hospitals providing acute care.
Synopsis: Data from NRCPR relating to 6,789 cardiac arrests secondary to ventricular fibrillation or pulseless ventricular tachycardia, at 369 hospitals in hospitalized adults were analyzed. Delayed defibrillation was defined as occurring more than two minutes from the identification of ventricular fibrillation or pulseless ventricular tachycardia to the administration of the first shock to the patient.
Delayed defibrillation occurred in 2,045 (30.1%) subjects. A lower proportion of subjects who received delayed defibrillation (22.2%) compared with those who received defibrillation in two minutes or less (39.3%) survived to hospital discharge. This was statistically significant (adjusted odds ratio [OR] 0.48, 95% CI 0.42 to 0.54; p<0.01).
Bottom line: This study not only reported that delayed defibrillation was prevalent in adult hospitalized patients, but also reinforced the importance of defibrillation within two minutes of identification of cardiac arrest secondary to ventricular fibrillation and pulseless ventricular tachycardia for better survival outcomes.
Citation: Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
Does Right-Ventricle Enlargement in Acute PE Increase In-hospital Death From PE or All-cause Mortality?
Background: Previous studies have shown conflicting results regarding the risk of death with right-ventricular enlargement in acute pulmonary embolism (PE). The role of thrombolysis in hemodynamically stable patients with acute PE and right-ventricular enlargement remains controversial.
Study design: Retrospective analysis of prospective cohort study.
Setting: Academic centers housing inpatients and outpatients in the United States and Canada.
Synopsis: Patients enrolled in PIOPED II who were diagnosed with acute PE and had multidetector computed tomographic (CT) angiography were retrospectively reviewed for the presence of right-ventricular enlargement. Study determined that 181 patients had PE and a CT, and 157 were adequate for measurement of right-ventricular size. PE treatment was anticoagulation in 138, anticoagulation and inferior vena cava filter in 15, inferior vena cava filter alone in two, and thrombolysis in two.
Right-ventricular enlargement was found in 78 (50%) patients; 76 were treated with anticoagulation alone or in combination with inferior vena cava filter. For patients with and without right-ventricular enlargement, there was no difference in in-hospital death from PE (0% vs. 1.3%) or all-cause mortality (2.6% vs. 2.5%). The results were unchanged when examined for septal motion abnormality and previous cardiopulmonary disease.
Bottom line: In hemodynamically stable patients with acute pulmonary embolism, right ventricular enlargement does not increase mortality. Further, thrombolytic therapy is unlikely to improve outcomes.
Citation: Stein PD, Beemath A, Matti F, et al. Enlarged right ventricle without shock in acute pulmonary embolus: prognosis. Am J Med. 2008;121:34-42.
What Are Short-term Thromboembolism, Hemorrhage Risks When Interrupting Warfarin Therapy for Procedures?
Background: The risks of thromboembolism and hemorrhage during the periprocedural interruption of warfarin therapy are not known. The risks and benefits of heparin bridging therapy are not well described.
Study design: Multicenter, prospective, observational cohort study.
Setting: Community-based physician practices.
Synopsis: Patients were eligible if they were on long-term warfarin and underwent outpatient procedures requiring interruption of therapy. The primary outcomes were thromboembolism or hemorrhage within 30 days of therapy interruption. In all, 1,024 eligible patients (7.1% considered high risk) had 1,293 interruptions of warfarin therapy. The most common procedures were colonoscopy (25.1%), oral or dental surgery (24.9%), and ophthalmologic surgery (8.9%). Warfarin interruption was five or fewer days in 83.8% of episodes.
Thromboembolism occurred in seven (0.7%) patients, and major or clinically significant bleeding occurred in 23 (0.6%, and 1.7%, respectively) patients. Periprocedural bridging with heparin was used in 88 (8.6%) patients. Of the patients who received periprocedural heparin therapy, none had thromboembolism, and 14 (13%) had bleeding episodes.
Bottom line: In patients whose warfarin therapy is interrupted to undergo outpatient procedures, the risk of thromboembolism is low and the hemorrhagic risk of heparin bridging therapy is significant.
Citation: Garcia DA, Regan S, Henault LE, et al. Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med. 2008;168(1):63-69.
Are Minor Injuries an Independent Risk Factor For Development of DVT?
Background: Prior studies focus on major injuries as a risk factor for deep-vein thrombosis (DVT) and PE. However, major injury is often associated with other risks for venous thrombosis, such as surgery, plaster casting, hospitalization, and extended bed rest. Risk of DVT with minor injuries that don’t lead to these factors is unknown.
Study design: Large population-based case-control study.
Setting: Six anticoagulation clinics in the Netherlands.
Synopsis: 2,471 consecutive cases (patients with first episode of DVT or PE) and 3,534 controls (partners of cases or random digit dialing contacts) were enrolled. Participants were mailed a questionnaire, including a list of eight common injuries.
Participants with history of cast, surgery, recent hospitalization, extended bed rest, or prior history of cancer were excluded. A subset of patients and controls underwent DNA and blood collection to evaluate for presence of a hypercoagulable state. Of the cases, 289 (11.7%) had a minor injury within three months of the index date, compared with 154 (4.4%) of controls, representing a threefold increased risk of DVT/PE with minor injury (OR 3.1). Partial ruptures of muscles or ligaments in the leg (OR 10.9), multiple simultaneous injuries (OR 9.9), and injury within four weeks of presentation (OR 4.0), were associated with increased risk of DVT/PE.
Patients found to be Factor V Leiden carriers with injury had an almost 50-fold increased risk of venous thromboembolism (VTE) compared with non-carriers without injury (OR 49.7). Authors appropriately address possible limitations, including recall and referral bias.
Bottom line: Minor leg injury is associated with threefold risk of DVT/PE, especially in the four weeks following injury. Providers should consider short-term prophylactic treatment in patients with Factor V Leiden or high-risk injuries.
Citation: Van Stralen KJ, Rosendaal FR, Doggen CJ. Minor injuries as a risk factor for venous thrombosis. Arch Intern Med. 2008;168(1):21-26.
Is Oral Amox-Clav Non-inferior to IV Antibiotics in Pediatric Pyelonephritis?
Background: Present guidelines recommend initial treatment for pediatric pyelonephritis to be a parenteral third-generation cephalosporin followed by oral antibiotics. One prior randomly selected controlled trial compared oral antibiotics only with antibiotics started parenterally, but there was a higher-than-usual incidence of vesicoureteral reflux and female gender in the study.
Study design: Non-inferiority, multicenter, random, open label, controlled trial.
Setting: Twenty-eight pediatric units in northeast Italy from 2000-2005
Synopsis: 502 children age 1 month to less than 7 years with a clinical diagnosis of first occurrence of acute pyelonephritis according to urinalysis and urine culture (requiring two concordant consecutive tests) with at least two of the following conditions: fever of 38 degrees C or more or elevated erythrocyte sedimentation rate (ESR) or c-reactive protein (CRP), and elevated neutrophil count were randomized to receive oral amoxicillin-clavulanate (AC) or parenteral ceftriaxone followed by oral AC. Exclusion criteria were sepsis, dehydration, vomiting, and creatinine clearance of 70 ml/min or less.
Also, 400 children had dimercaptosuccinic acid (DMSA) scintigraphy within 10 days of study entry. Meantime, 223 had repeat DMSA at one year, and 177 had normal scans at study entry so were not repeated. At one year, 20% of patients were lost to follow-up. The primary outcome was renal scarring at one year. Secondary outcomes included time to fever defervescence, reduction in inflammatory indices, and percentage with sterile urine after 72 hours. Intention to treat analysis showed no significant differences between oral (n=244) and parenteral (n=258) treatment, both in the primary outcome 13.7% vs. 17.7% (95% CI, -11.1% to 3.1%), and secondary outcomes.
Bottom line: Treatment with oral antibiotics is as effective as parenteral then oral treatment for first episode of acute pediatric pyelonephritis.
Citation: Montini G, Toffolo A, Zucchetta P, et al. Antibiotic treatment for pyelonephritis in children: multicentre randomised controlled non-inferiority trial. BMJ. 2007 Aug 25;335(7616):386.
Literature at a Glance
A guide to this month’s studies.
- Physiologic doses of corticosteroids provide no clear benefit to patients with septic shock.
- Endovascular vs. open repair of abdominal aortic aneurysms is associated with fewer short-term deaths but complications and higher late reinterventions.
- Neither intensive insulin nor use of colloid over crystalloid improves mortality or organ failure outcomes in sepsis.
- Surgical cure for diabetes shows promise at two-year follow-up.
- Delayed defibrillation negatively affects survival.
- Right-ventricular enlargement in patients with acute PE is not associated with increased mortality.
- Periprocedural interruption of warfarin therapy presents low risk of thromboembolism.
- Minor leg injury increases risk of developing venous thrombosis threefold.
- Oral vs. parenteral antibiotics for pediatric pyelonephritis.
Do Physiologic Doses of Hydrocortisone Benefit Patients With Septic Shock?
Background: Meta-analyses and guidelines advocate the use of physiologic dose steroids in patients exhibiting septic shock. However, recommendations are largely based on the results of a single trial where benefits were seen only in patients without a response to corticotropin.
Study design: Multicenter, randomized, double-blind, placebo-controlled study.
Setting: Fifty-two participating ICUs in nine countries.
Synopsis: A total of 499 patients with evidence of infection or a systemic inflammatory response characterized by refractory hypotension were randomly selected to receive either an 11-day tapering dose of hydrocortisone or a placebo. The primary outcome was death from any cause at 28 days. A corticotropin stimulation test was conducted on every patient to assess adrenal function. There were no differences in death rates or duration of hospitalization between study arms. Overall, there were 86 deaths in the hydrocortisone group and 78 deaths in the placebo group (p=0.51). Also, response to corticotropin appeared to have little bearing on outcomes.
The study was underpowered due to low enrollment and a lower-than-expected death rate. Nevertheless, this is the largest trial to date examining the role of steroids in the management of septic shock and calls into question the strength of prior data and published guidelines.
Bottom line: This study failed to demonstrate a clinically or statistically significant treatment effect from the administration of physiologic-dose steroids in patients with septic shock.
Citation: Sprung C, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111-124.
Does Open or Endovascular Repair of Abdominal Aortic Aneurysm Benefit the Medicare Population?
Background: Randomized controlled trials (RCT) have shown a perioperative survival benefit of endovascular repair over open repair with fewer complications and shorter recovery. There is concern that late morbidity may be increased with endovascular repair. Patients enrolled in the trials were highly selected at specialty centers, so the results may not reflect actual practice.
Study design: Retrospective, propensity-matched, observational cohort study.
Synopsis: 22,830 patients were matched in each cohort. Patients were eligible if they had an abdominal aortic aneurysm repair without rupture and excluded if they were enrolled in health maintenance organizations.
Outcomes included death within 30 days and late survival, perioperative complications, aneurysm rupture, reintervention, and laparotomy-related complications. The average age was 76, and 20% were women. Perioperative mortality was lower after endovascular repair (1.2% vs. 4.8%, p<0.001), and older patients had a greater benefit. Late survival was similar. By four years, rupture was more likely in the endovascular group (1.8% vs. 0.5%, p<0.001), as was reintervention (9% vs. 1.7%, p<0.001).
In contrast, by four years, surgery for laparotomy-related complications was more likely in the open-repair group (9.7% v 4.1%, p<0.001), as was hospitalization for bowel obstruction or abdominal-wall hernia (14.2% v 8.1%, p<0.001). Limitations included the non-randomized design and use of administrative data for important categorical variables including medical co-morbidities.
Bottom line: As compared with open repair, endovascular repair of abdominal aortic aneurysm is associated with lower short-term death and complications and higher late reinterventions. This is balanced by an increase in laparotomy-related reinterventions after open repair.
Citation: Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008 Jan 31;358(5):464-474.
What Therapy Improves Outcomes in ICU Patients With Severe Sepsis or Septic Shock?
Background: Evidence suggests lower mortality with intensive insulin therapy in post-surgical cardiac patients. There is no proven benefit for non-surgical ICU patients. Despite lack of data, intensive insulin in severe sepsis has been widely advocated. Little is known to guide the use of colloid or crystalloid for fluid resuscitation in sepsis.
Study design: Multicenter, two-by-two factorial, open-label trial.
Setting: Multidisciplinary ICUs at 18 academic tertiary hospitals in Germany.
Synopsis: Data were analyzed for 537 patients with severe sepsis. They were randomly selected to receive intensive insulin therapy (n=247) or conventional insulin therapy (290), with either 10% hydroxyethyl starch (HES) (262) or modified Ringer’s lactate (LR) (275) for fluid resuscitation.
Co-primary endpoints were all-cause mortality at 28 days and morbidity as measured by the mean score on the Sequential Organ Failure Assessment (SOFA). The trial was stopped early for safety reasons. Intensive insulin therapy was terminated due to an increased number of hypoglycemic events in the intensive-therapy group compared with conventional therapy (12.1% vs. 2.1%, p<0.001), and there was no difference in mortality between groups at 28 and 90 days.
Interim analysis of 600 patients showed patients given HES had higher incidence of renal failure compared with LR (34.9% vs. 22.8%, p=0.002), required more days of renal replacement therapy, had lower median platelets and received more units of packed red cells. There was a trend toward higher rate of death at 90 days in those treated with HES (41% vs. 33.9%, p=0.09).
Bottom line: Intensive insulin therapy in ICU patients with severe sepsis and septic shock does not improve mortality and increases hypoglycemia and ICU length of stay. Use of colloid over crystalloid should be avoided, showing a trend toward increased death at 90 days, higher rates of acute renal failure, and need for renal replacement therapy..
Citation: Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125-139.
How Does Laparoscopic Adjustable Gastric Banding Affect Obese Adults With Type 2 Diabetes?
Background: Observational studies related surgical weight loss to improved glycemic control, but clinical trials did not test this relationship. The current trial examined this hypothesis.
Study design: Unmasked, randomized controlled trial.
Setting: University Obesity Research Center, Australia.
Synopsis: Sixty adults age 20-60 with body-mass index (BMI) of 30-40 and diagnosed with diabetes mellitus type 2 (DM2) within two years of recruitment were randomized into conventional therapy and surgical groups.
While both groups were treated similarly, only the surgical group received laparoscopic adjustable gastric banding. Primary outcome was remission of DM2 (a fasting glucose less than 126 mg/dl, HbA1C less than 6.2%, and off all hypoglycemic agents). At two years, 73% in the surgical group compared with 13% in the conventional group attained this outcome (relative risk [RR] 5.5, 95% confidence interval [CI] 2.2-14.0; p<0.001). Compared with the conventional group, the surgical group demonstrated statistically significant improvements in several secondary outcomes including mean body weight, waist circumference, insulin resistance, and lipids.
The limitations of the study are that it examined a small number of patients with shorter duration of DM2 and a shorter follow-up. The lower surgical complication rates cannot be generalized to other centers.
Bottom line: This study is a step forward in examining the relationship of surgical weight loss and remission of DM2. However, large multicenter trials with longer periods of follow-up in diverse group of patients would result in a better understanding of this relationship.
Citation: Dixon JB, O’Brien PE, Playfair J, et. al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299(3):316-323.
What is the Prevalence of Delayed Defibrillation and its Association With Survival to Discharge?
Background: Despite advances in resuscitation, survival rates following cardiac arrest remain low. Previous studies observed the effect of the timing of defibrillation on survival. This study examined the magnitude of delayed defibrillation and its association with survival in adults who sustained cardiac arrest specifically from ventricular fibrillation and pulseless ventricular tachycardia.
Study design: National Registry of Cardiopulmonary Resuscitation (NRCPR), a multicenter prospective cohort.
Setting: 369 U.S. hospitals providing acute care.
Synopsis: Data from NRCPR relating to 6,789 cardiac arrests secondary to ventricular fibrillation or pulseless ventricular tachycardia, at 369 hospitals in hospitalized adults were analyzed. Delayed defibrillation was defined as occurring more than two minutes from the identification of ventricular fibrillation or pulseless ventricular tachycardia to the administration of the first shock to the patient.
Delayed defibrillation occurred in 2,045 (30.1%) subjects. A lower proportion of subjects who received delayed defibrillation (22.2%) compared with those who received defibrillation in two minutes or less (39.3%) survived to hospital discharge. This was statistically significant (adjusted odds ratio [OR] 0.48, 95% CI 0.42 to 0.54; p<0.01).
Bottom line: This study not only reported that delayed defibrillation was prevalent in adult hospitalized patients, but also reinforced the importance of defibrillation within two minutes of identification of cardiac arrest secondary to ventricular fibrillation and pulseless ventricular tachycardia for better survival outcomes.
Citation: Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
Does Right-Ventricle Enlargement in Acute PE Increase In-hospital Death From PE or All-cause Mortality?
Background: Previous studies have shown conflicting results regarding the risk of death with right-ventricular enlargement in acute pulmonary embolism (PE). The role of thrombolysis in hemodynamically stable patients with acute PE and right-ventricular enlargement remains controversial.
Study design: Retrospective analysis of prospective cohort study.
Setting: Academic centers housing inpatients and outpatients in the United States and Canada.
Synopsis: Patients enrolled in PIOPED II who were diagnosed with acute PE and had multidetector computed tomographic (CT) angiography were retrospectively reviewed for the presence of right-ventricular enlargement. Study determined that 181 patients had PE and a CT, and 157 were adequate for measurement of right-ventricular size. PE treatment was anticoagulation in 138, anticoagulation and inferior vena cava filter in 15, inferior vena cava filter alone in two, and thrombolysis in two.
Right-ventricular enlargement was found in 78 (50%) patients; 76 were treated with anticoagulation alone or in combination with inferior vena cava filter. For patients with and without right-ventricular enlargement, there was no difference in in-hospital death from PE (0% vs. 1.3%) or all-cause mortality (2.6% vs. 2.5%). The results were unchanged when examined for septal motion abnormality and previous cardiopulmonary disease.
Bottom line: In hemodynamically stable patients with acute pulmonary embolism, right ventricular enlargement does not increase mortality. Further, thrombolytic therapy is unlikely to improve outcomes.
Citation: Stein PD, Beemath A, Matti F, et al. Enlarged right ventricle without shock in acute pulmonary embolus: prognosis. Am J Med. 2008;121:34-42.
What Are Short-term Thromboembolism, Hemorrhage Risks When Interrupting Warfarin Therapy for Procedures?
Background: The risks of thromboembolism and hemorrhage during the periprocedural interruption of warfarin therapy are not known. The risks and benefits of heparin bridging therapy are not well described.
Study design: Multicenter, prospective, observational cohort study.
Setting: Community-based physician practices.
Synopsis: Patients were eligible if they were on long-term warfarin and underwent outpatient procedures requiring interruption of therapy. The primary outcomes were thromboembolism or hemorrhage within 30 days of therapy interruption. In all, 1,024 eligible patients (7.1% considered high risk) had 1,293 interruptions of warfarin therapy. The most common procedures were colonoscopy (25.1%), oral or dental surgery (24.9%), and ophthalmologic surgery (8.9%). Warfarin interruption was five or fewer days in 83.8% of episodes.
Thromboembolism occurred in seven (0.7%) patients, and major or clinically significant bleeding occurred in 23 (0.6%, and 1.7%, respectively) patients. Periprocedural bridging with heparin was used in 88 (8.6%) patients. Of the patients who received periprocedural heparin therapy, none had thromboembolism, and 14 (13%) had bleeding episodes.
Bottom line: In patients whose warfarin therapy is interrupted to undergo outpatient procedures, the risk of thromboembolism is low and the hemorrhagic risk of heparin bridging therapy is significant.
Citation: Garcia DA, Regan S, Henault LE, et al. Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med. 2008;168(1):63-69.
Are Minor Injuries an Independent Risk Factor For Development of DVT?
Background: Prior studies focus on major injuries as a risk factor for deep-vein thrombosis (DVT) and PE. However, major injury is often associated with other risks for venous thrombosis, such as surgery, plaster casting, hospitalization, and extended bed rest. Risk of DVT with minor injuries that don’t lead to these factors is unknown.
Study design: Large population-based case-control study.
Setting: Six anticoagulation clinics in the Netherlands.
Synopsis: 2,471 consecutive cases (patients with first episode of DVT or PE) and 3,534 controls (partners of cases or random digit dialing contacts) were enrolled. Participants were mailed a questionnaire, including a list of eight common injuries.
Participants with history of cast, surgery, recent hospitalization, extended bed rest, or prior history of cancer were excluded. A subset of patients and controls underwent DNA and blood collection to evaluate for presence of a hypercoagulable state. Of the cases, 289 (11.7%) had a minor injury within three months of the index date, compared with 154 (4.4%) of controls, representing a threefold increased risk of DVT/PE with minor injury (OR 3.1). Partial ruptures of muscles or ligaments in the leg (OR 10.9), multiple simultaneous injuries (OR 9.9), and injury within four weeks of presentation (OR 4.0), were associated with increased risk of DVT/PE.
Patients found to be Factor V Leiden carriers with injury had an almost 50-fold increased risk of venous thromboembolism (VTE) compared with non-carriers without injury (OR 49.7). Authors appropriately address possible limitations, including recall and referral bias.
Bottom line: Minor leg injury is associated with threefold risk of DVT/PE, especially in the four weeks following injury. Providers should consider short-term prophylactic treatment in patients with Factor V Leiden or high-risk injuries.
Citation: Van Stralen KJ, Rosendaal FR, Doggen CJ. Minor injuries as a risk factor for venous thrombosis. Arch Intern Med. 2008;168(1):21-26.
Is Oral Amox-Clav Non-inferior to IV Antibiotics in Pediatric Pyelonephritis?
Background: Present guidelines recommend initial treatment for pediatric pyelonephritis to be a parenteral third-generation cephalosporin followed by oral antibiotics. One prior randomly selected controlled trial compared oral antibiotics only with antibiotics started parenterally, but there was a higher-than-usual incidence of vesicoureteral reflux and female gender in the study.
Study design: Non-inferiority, multicenter, random, open label, controlled trial.
Setting: Twenty-eight pediatric units in northeast Italy from 2000-2005
Synopsis: 502 children age 1 month to less than 7 years with a clinical diagnosis of first occurrence of acute pyelonephritis according to urinalysis and urine culture (requiring two concordant consecutive tests) with at least two of the following conditions: fever of 38 degrees C or more or elevated erythrocyte sedimentation rate (ESR) or c-reactive protein (CRP), and elevated neutrophil count were randomized to receive oral amoxicillin-clavulanate (AC) or parenteral ceftriaxone followed by oral AC. Exclusion criteria were sepsis, dehydration, vomiting, and creatinine clearance of 70 ml/min or less.
Also, 400 children had dimercaptosuccinic acid (DMSA) scintigraphy within 10 days of study entry. Meantime, 223 had repeat DMSA at one year, and 177 had normal scans at study entry so were not repeated. At one year, 20% of patients were lost to follow-up. The primary outcome was renal scarring at one year. Secondary outcomes included time to fever defervescence, reduction in inflammatory indices, and percentage with sterile urine after 72 hours. Intention to treat analysis showed no significant differences between oral (n=244) and parenteral (n=258) treatment, both in the primary outcome 13.7% vs. 17.7% (95% CI, -11.1% to 3.1%), and secondary outcomes.
Bottom line: Treatment with oral antibiotics is as effective as parenteral then oral treatment for first episode of acute pediatric pyelonephritis.
Citation: Montini G, Toffolo A, Zucchetta P, et al. Antibiotic treatment for pyelonephritis in children: multicentre randomised controlled non-inferiority trial. BMJ. 2007 Aug 25;335(7616):386.
Literature at a Glance
A guide to this month’s studies.
- Physiologic doses of corticosteroids provide no clear benefit to patients with septic shock.
- Endovascular vs. open repair of abdominal aortic aneurysms is associated with fewer short-term deaths but complications and higher late reinterventions.
- Neither intensive insulin nor use of colloid over crystalloid improves mortality or organ failure outcomes in sepsis.
- Surgical cure for diabetes shows promise at two-year follow-up.
- Delayed defibrillation negatively affects survival.
- Right-ventricular enlargement in patients with acute PE is not associated with increased mortality.
- Periprocedural interruption of warfarin therapy presents low risk of thromboembolism.
- Minor leg injury increases risk of developing venous thrombosis threefold.
- Oral vs. parenteral antibiotics for pediatric pyelonephritis.
Do Physiologic Doses of Hydrocortisone Benefit Patients With Septic Shock?
Background: Meta-analyses and guidelines advocate the use of physiologic dose steroids in patients exhibiting septic shock. However, recommendations are largely based on the results of a single trial where benefits were seen only in patients without a response to corticotropin.
Study design: Multicenter, randomized, double-blind, placebo-controlled study.
Setting: Fifty-two participating ICUs in nine countries.
Synopsis: A total of 499 patients with evidence of infection or a systemic inflammatory response characterized by refractory hypotension were randomly selected to receive either an 11-day tapering dose of hydrocortisone or a placebo. The primary outcome was death from any cause at 28 days. A corticotropin stimulation test was conducted on every patient to assess adrenal function. There were no differences in death rates or duration of hospitalization between study arms. Overall, there were 86 deaths in the hydrocortisone group and 78 deaths in the placebo group (p=0.51). Also, response to corticotropin appeared to have little bearing on outcomes.
The study was underpowered due to low enrollment and a lower-than-expected death rate. Nevertheless, this is the largest trial to date examining the role of steroids in the management of septic shock and calls into question the strength of prior data and published guidelines.
Bottom line: This study failed to demonstrate a clinically or statistically significant treatment effect from the administration of physiologic-dose steroids in patients with septic shock.
Citation: Sprung C, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111-124.
Does Open or Endovascular Repair of Abdominal Aortic Aneurysm Benefit the Medicare Population?
Background: Randomized controlled trials (RCT) have shown a perioperative survival benefit of endovascular repair over open repair with fewer complications and shorter recovery. There is concern that late morbidity may be increased with endovascular repair. Patients enrolled in the trials were highly selected at specialty centers, so the results may not reflect actual practice.
Study design: Retrospective, propensity-matched, observational cohort study.
Synopsis: 22,830 patients were matched in each cohort. Patients were eligible if they had an abdominal aortic aneurysm repair without rupture and excluded if they were enrolled in health maintenance organizations.
Outcomes included death within 30 days and late survival, perioperative complications, aneurysm rupture, reintervention, and laparotomy-related complications. The average age was 76, and 20% were women. Perioperative mortality was lower after endovascular repair (1.2% vs. 4.8%, p<0.001), and older patients had a greater benefit. Late survival was similar. By four years, rupture was more likely in the endovascular group (1.8% vs. 0.5%, p<0.001), as was reintervention (9% vs. 1.7%, p<0.001).
In contrast, by four years, surgery for laparotomy-related complications was more likely in the open-repair group (9.7% v 4.1%, p<0.001), as was hospitalization for bowel obstruction or abdominal-wall hernia (14.2% v 8.1%, p<0.001). Limitations included the non-randomized design and use of administrative data for important categorical variables including medical co-morbidities.
Bottom line: As compared with open repair, endovascular repair of abdominal aortic aneurysm is associated with lower short-term death and complications and higher late reinterventions. This is balanced by an increase in laparotomy-related reinterventions after open repair.
Citation: Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008 Jan 31;358(5):464-474.
What Therapy Improves Outcomes in ICU Patients With Severe Sepsis or Septic Shock?
Background: Evidence suggests lower mortality with intensive insulin therapy in post-surgical cardiac patients. There is no proven benefit for non-surgical ICU patients. Despite lack of data, intensive insulin in severe sepsis has been widely advocated. Little is known to guide the use of colloid or crystalloid for fluid resuscitation in sepsis.
Study design: Multicenter, two-by-two factorial, open-label trial.
Setting: Multidisciplinary ICUs at 18 academic tertiary hospitals in Germany.
Synopsis: Data were analyzed for 537 patients with severe sepsis. They were randomly selected to receive intensive insulin therapy (n=247) or conventional insulin therapy (290), with either 10% hydroxyethyl starch (HES) (262) or modified Ringer’s lactate (LR) (275) for fluid resuscitation.
Co-primary endpoints were all-cause mortality at 28 days and morbidity as measured by the mean score on the Sequential Organ Failure Assessment (SOFA). The trial was stopped early for safety reasons. Intensive insulin therapy was terminated due to an increased number of hypoglycemic events in the intensive-therapy group compared with conventional therapy (12.1% vs. 2.1%, p<0.001), and there was no difference in mortality between groups at 28 and 90 days.
Interim analysis of 600 patients showed patients given HES had higher incidence of renal failure compared with LR (34.9% vs. 22.8%, p=0.002), required more days of renal replacement therapy, had lower median platelets and received more units of packed red cells. There was a trend toward higher rate of death at 90 days in those treated with HES (41% vs. 33.9%, p=0.09).
Bottom line: Intensive insulin therapy in ICU patients with severe sepsis and septic shock does not improve mortality and increases hypoglycemia and ICU length of stay. Use of colloid over crystalloid should be avoided, showing a trend toward increased death at 90 days, higher rates of acute renal failure, and need for renal replacement therapy..
Citation: Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125-139.
How Does Laparoscopic Adjustable Gastric Banding Affect Obese Adults With Type 2 Diabetes?
Background: Observational studies related surgical weight loss to improved glycemic control, but clinical trials did not test this relationship. The current trial examined this hypothesis.
Study design: Unmasked, randomized controlled trial.
Setting: University Obesity Research Center, Australia.
Synopsis: Sixty adults age 20-60 with body-mass index (BMI) of 30-40 and diagnosed with diabetes mellitus type 2 (DM2) within two years of recruitment were randomized into conventional therapy and surgical groups.
While both groups were treated similarly, only the surgical group received laparoscopic adjustable gastric banding. Primary outcome was remission of DM2 (a fasting glucose less than 126 mg/dl, HbA1C less than 6.2%, and off all hypoglycemic agents). At two years, 73% in the surgical group compared with 13% in the conventional group attained this outcome (relative risk [RR] 5.5, 95% confidence interval [CI] 2.2-14.0; p<0.001). Compared with the conventional group, the surgical group demonstrated statistically significant improvements in several secondary outcomes including mean body weight, waist circumference, insulin resistance, and lipids.
The limitations of the study are that it examined a small number of patients with shorter duration of DM2 and a shorter follow-up. The lower surgical complication rates cannot be generalized to other centers.
Bottom line: This study is a step forward in examining the relationship of surgical weight loss and remission of DM2. However, large multicenter trials with longer periods of follow-up in diverse group of patients would result in a better understanding of this relationship.
Citation: Dixon JB, O’Brien PE, Playfair J, et. al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299(3):316-323.
What is the Prevalence of Delayed Defibrillation and its Association With Survival to Discharge?
Background: Despite advances in resuscitation, survival rates following cardiac arrest remain low. Previous studies observed the effect of the timing of defibrillation on survival. This study examined the magnitude of delayed defibrillation and its association with survival in adults who sustained cardiac arrest specifically from ventricular fibrillation and pulseless ventricular tachycardia.
Study design: National Registry of Cardiopulmonary Resuscitation (NRCPR), a multicenter prospective cohort.
Setting: 369 U.S. hospitals providing acute care.
Synopsis: Data from NRCPR relating to 6,789 cardiac arrests secondary to ventricular fibrillation or pulseless ventricular tachycardia, at 369 hospitals in hospitalized adults were analyzed. Delayed defibrillation was defined as occurring more than two minutes from the identification of ventricular fibrillation or pulseless ventricular tachycardia to the administration of the first shock to the patient.
Delayed defibrillation occurred in 2,045 (30.1%) subjects. A lower proportion of subjects who received delayed defibrillation (22.2%) compared with those who received defibrillation in two minutes or less (39.3%) survived to hospital discharge. This was statistically significant (adjusted odds ratio [OR] 0.48, 95% CI 0.42 to 0.54; p<0.01).
Bottom line: This study not only reported that delayed defibrillation was prevalent in adult hospitalized patients, but also reinforced the importance of defibrillation within two minutes of identification of cardiac arrest secondary to ventricular fibrillation and pulseless ventricular tachycardia for better survival outcomes.
Citation: Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
Does Right-Ventricle Enlargement in Acute PE Increase In-hospital Death From PE or All-cause Mortality?
Background: Previous studies have shown conflicting results regarding the risk of death with right-ventricular enlargement in acute pulmonary embolism (PE). The role of thrombolysis in hemodynamically stable patients with acute PE and right-ventricular enlargement remains controversial.
Study design: Retrospective analysis of prospective cohort study.
Setting: Academic centers housing inpatients and outpatients in the United States and Canada.
Synopsis: Patients enrolled in PIOPED II who were diagnosed with acute PE and had multidetector computed tomographic (CT) angiography were retrospectively reviewed for the presence of right-ventricular enlargement. Study determined that 181 patients had PE and a CT, and 157 were adequate for measurement of right-ventricular size. PE treatment was anticoagulation in 138, anticoagulation and inferior vena cava filter in 15, inferior vena cava filter alone in two, and thrombolysis in two.
Right-ventricular enlargement was found in 78 (50%) patients; 76 were treated with anticoagulation alone or in combination with inferior vena cava filter. For patients with and without right-ventricular enlargement, there was no difference in in-hospital death from PE (0% vs. 1.3%) or all-cause mortality (2.6% vs. 2.5%). The results were unchanged when examined for septal motion abnormality and previous cardiopulmonary disease.
Bottom line: In hemodynamically stable patients with acute pulmonary embolism, right ventricular enlargement does not increase mortality. Further, thrombolytic therapy is unlikely to improve outcomes.
Citation: Stein PD, Beemath A, Matti F, et al. Enlarged right ventricle without shock in acute pulmonary embolus: prognosis. Am J Med. 2008;121:34-42.
What Are Short-term Thromboembolism, Hemorrhage Risks When Interrupting Warfarin Therapy for Procedures?
Background: The risks of thromboembolism and hemorrhage during the periprocedural interruption of warfarin therapy are not known. The risks and benefits of heparin bridging therapy are not well described.
Study design: Multicenter, prospective, observational cohort study.
Setting: Community-based physician practices.
Synopsis: Patients were eligible if they were on long-term warfarin and underwent outpatient procedures requiring interruption of therapy. The primary outcomes were thromboembolism or hemorrhage within 30 days of therapy interruption. In all, 1,024 eligible patients (7.1% considered high risk) had 1,293 interruptions of warfarin therapy. The most common procedures were colonoscopy (25.1%), oral or dental surgery (24.9%), and ophthalmologic surgery (8.9%). Warfarin interruption was five or fewer days in 83.8% of episodes.
Thromboembolism occurred in seven (0.7%) patients, and major or clinically significant bleeding occurred in 23 (0.6%, and 1.7%, respectively) patients. Periprocedural bridging with heparin was used in 88 (8.6%) patients. Of the patients who received periprocedural heparin therapy, none had thromboembolism, and 14 (13%) had bleeding episodes.
Bottom line: In patients whose warfarin therapy is interrupted to undergo outpatient procedures, the risk of thromboembolism is low and the hemorrhagic risk of heparin bridging therapy is significant.
Citation: Garcia DA, Regan S, Henault LE, et al. Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med. 2008;168(1):63-69.
Are Minor Injuries an Independent Risk Factor For Development of DVT?
Background: Prior studies focus on major injuries as a risk factor for deep-vein thrombosis (DVT) and PE. However, major injury is often associated with other risks for venous thrombosis, such as surgery, plaster casting, hospitalization, and extended bed rest. Risk of DVT with minor injuries that don’t lead to these factors is unknown.
Study design: Large population-based case-control study.
Setting: Six anticoagulation clinics in the Netherlands.
Synopsis: 2,471 consecutive cases (patients with first episode of DVT or PE) and 3,534 controls (partners of cases or random digit dialing contacts) were enrolled. Participants were mailed a questionnaire, including a list of eight common injuries.
Participants with history of cast, surgery, recent hospitalization, extended bed rest, or prior history of cancer were excluded. A subset of patients and controls underwent DNA and blood collection to evaluate for presence of a hypercoagulable state. Of the cases, 289 (11.7%) had a minor injury within three months of the index date, compared with 154 (4.4%) of controls, representing a threefold increased risk of DVT/PE with minor injury (OR 3.1). Partial ruptures of muscles or ligaments in the leg (OR 10.9), multiple simultaneous injuries (OR 9.9), and injury within four weeks of presentation (OR 4.0), were associated with increased risk of DVT/PE.
Patients found to be Factor V Leiden carriers with injury had an almost 50-fold increased risk of venous thromboembolism (VTE) compared with non-carriers without injury (OR 49.7). Authors appropriately address possible limitations, including recall and referral bias.
Bottom line: Minor leg injury is associated with threefold risk of DVT/PE, especially in the four weeks following injury. Providers should consider short-term prophylactic treatment in patients with Factor V Leiden or high-risk injuries.
Citation: Van Stralen KJ, Rosendaal FR, Doggen CJ. Minor injuries as a risk factor for venous thrombosis. Arch Intern Med. 2008;168(1):21-26.
Is Oral Amox-Clav Non-inferior to IV Antibiotics in Pediatric Pyelonephritis?
Background: Present guidelines recommend initial treatment for pediatric pyelonephritis to be a parenteral third-generation cephalosporin followed by oral antibiotics. One prior randomly selected controlled trial compared oral antibiotics only with antibiotics started parenterally, but there was a higher-than-usual incidence of vesicoureteral reflux and female gender in the study.
Study design: Non-inferiority, multicenter, random, open label, controlled trial.
Setting: Twenty-eight pediatric units in northeast Italy from 2000-2005
Synopsis: 502 children age 1 month to less than 7 years with a clinical diagnosis of first occurrence of acute pyelonephritis according to urinalysis and urine culture (requiring two concordant consecutive tests) with at least two of the following conditions: fever of 38 degrees C or more or elevated erythrocyte sedimentation rate (ESR) or c-reactive protein (CRP), and elevated neutrophil count were randomized to receive oral amoxicillin-clavulanate (AC) or parenteral ceftriaxone followed by oral AC. Exclusion criteria were sepsis, dehydration, vomiting, and creatinine clearance of 70 ml/min or less.
Also, 400 children had dimercaptosuccinic acid (DMSA) scintigraphy within 10 days of study entry. Meantime, 223 had repeat DMSA at one year, and 177 had normal scans at study entry so were not repeated. At one year, 20% of patients were lost to follow-up. The primary outcome was renal scarring at one year. Secondary outcomes included time to fever defervescence, reduction in inflammatory indices, and percentage with sterile urine after 72 hours. Intention to treat analysis showed no significant differences between oral (n=244) and parenteral (n=258) treatment, both in the primary outcome 13.7% vs. 17.7% (95% CI, -11.1% to 3.1%), and secondary outcomes.
Bottom line: Treatment with oral antibiotics is as effective as parenteral then oral treatment for first episode of acute pediatric pyelonephritis.
Citation: Montini G, Toffolo A, Zucchetta P, et al. Antibiotic treatment for pyelonephritis in children: multicentre randomised controlled non-inferiority trial. BMJ. 2007 Aug 25;335(7616):386.
VTE Protocol Among Winning Posters
The best and brightest thinking from today’s hospitalists was on display in the poster presentations in San Diego. Of 265 abstracts submitted to the Research, Innovations and Clinical Vignettes (RIV) Competition, 195 were accepted for poster presentations.
“The quality and quantity of abstract submissions increases every year,” said Sylvia McKean, MD, course director of Hospital Medicine 2008.
Best in Show
“It’s been a banner year for the poster presentations,” said Jeffrey Greenwald, MD, hospital medicine unit director, Boston Medical Center, as he announced the winning abstracts during the President’s Lunch on April 5:
- Research: “Prevention of Hospital-Acquired Venous Thromboembolism: Prospective Validation of a VTE Risk Assessment Model and Protocol, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
- Innovations: “Can Tissue Models Be Used to Teach Central Line Placement? Phase II of the Procedure Patient Safety Initiative (PPSI), Annie R. Harrington, MD, Cedars-Sinai Medical Center, Los Angeles; and
- Clinical Vignettes: “A Case of Salty Voluminous Urine, Twylla Tassava, MD, Saint Joseph Mercy Hospital, Ann Arbor, Mich.
Other Notable Works
Param Dedhia, MD, presented research he conducted with colleagues from Johns Hopkins Bayview Medical Center titled “Safe STEPS: Safe and Successful Transition of Elderly Patients.” The group developed an interdisciplinary, multifaceted intervention in this area, which included:
- A history and physical exam tailored to geriatric patients;
- A “fast facts fax” to communicate with the primary care physician;
- An interdisciplinary team worksheet for centralized input;
- A medical evaluation including a detailed review with the pharmacist; and?
- A pre-discharge appointment.
The results: A 15-question survey showed a 60% to 90% jump in patient satisfaction. A health assessment by self-report showed improvement as well, and the number of revisits and readmissions dropped from 10% to 3%.
“The Impact of Fragmentation of Hospitalist Care on Length of Stay and Post-Discharge Issues” was presented by Kenneth R. Epstein, MD, MBA, of IPC-The Hospitalist Company. Dr. Epstein and his colleagues used an observational study of data from IPC’s billing and clinical database on inpatient admissions with pneumonia with complications and heart failure and shock. They wanted to see if fragmented hospitalist care—care provided by more than one hospitalist—affected outcomes for these patients.
Using a fragmentation formula that included the number of days as an inpatient and the number of hospitalists who provided care, they found that for every 10% increase in fragmentation, the length of stay increased 0.45 days for pneumonia patients and 0.38 days for heart failure patients.
The country’s first fellowship for physician assistants (PA) specializing in hospital medicine was detailed in “The Mayo Clinic Arizona Post-Graduate PA Fellowship in Hospital Internal Medicine.” Kristen K. Will, MHPE, PA-C, co-program director of clinic’s PA Fellowship Program, outlined how her institution initiated the fellowship in October. The program will train one PA using hospital medicine-specific clinical rotations, didactic instruction, and teaching modules.
The best and brightest thinking from today’s hospitalists was on display in the poster presentations in San Diego. Of 265 abstracts submitted to the Research, Innovations and Clinical Vignettes (RIV) Competition, 195 were accepted for poster presentations.
“The quality and quantity of abstract submissions increases every year,” said Sylvia McKean, MD, course director of Hospital Medicine 2008.
Best in Show
“It’s been a banner year for the poster presentations,” said Jeffrey Greenwald, MD, hospital medicine unit director, Boston Medical Center, as he announced the winning abstracts during the President’s Lunch on April 5:
- Research: “Prevention of Hospital-Acquired Venous Thromboembolism: Prospective Validation of a VTE Risk Assessment Model and Protocol, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
- Innovations: “Can Tissue Models Be Used to Teach Central Line Placement? Phase II of the Procedure Patient Safety Initiative (PPSI), Annie R. Harrington, MD, Cedars-Sinai Medical Center, Los Angeles; and
- Clinical Vignettes: “A Case of Salty Voluminous Urine, Twylla Tassava, MD, Saint Joseph Mercy Hospital, Ann Arbor, Mich.
Other Notable Works
Param Dedhia, MD, presented research he conducted with colleagues from Johns Hopkins Bayview Medical Center titled “Safe STEPS: Safe and Successful Transition of Elderly Patients.” The group developed an interdisciplinary, multifaceted intervention in this area, which included:
- A history and physical exam tailored to geriatric patients;
- A “fast facts fax” to communicate with the primary care physician;
- An interdisciplinary team worksheet for centralized input;
- A medical evaluation including a detailed review with the pharmacist; and?
- A pre-discharge appointment.
The results: A 15-question survey showed a 60% to 90% jump in patient satisfaction. A health assessment by self-report showed improvement as well, and the number of revisits and readmissions dropped from 10% to 3%.
“The Impact of Fragmentation of Hospitalist Care on Length of Stay and Post-Discharge Issues” was presented by Kenneth R. Epstein, MD, MBA, of IPC-The Hospitalist Company. Dr. Epstein and his colleagues used an observational study of data from IPC’s billing and clinical database on inpatient admissions with pneumonia with complications and heart failure and shock. They wanted to see if fragmented hospitalist care—care provided by more than one hospitalist—affected outcomes for these patients.
Using a fragmentation formula that included the number of days as an inpatient and the number of hospitalists who provided care, they found that for every 10% increase in fragmentation, the length of stay increased 0.45 days for pneumonia patients and 0.38 days for heart failure patients.
The country’s first fellowship for physician assistants (PA) specializing in hospital medicine was detailed in “The Mayo Clinic Arizona Post-Graduate PA Fellowship in Hospital Internal Medicine.” Kristen K. Will, MHPE, PA-C, co-program director of clinic’s PA Fellowship Program, outlined how her institution initiated the fellowship in October. The program will train one PA using hospital medicine-specific clinical rotations, didactic instruction, and teaching modules.
The best and brightest thinking from today’s hospitalists was on display in the poster presentations in San Diego. Of 265 abstracts submitted to the Research, Innovations and Clinical Vignettes (RIV) Competition, 195 were accepted for poster presentations.
“The quality and quantity of abstract submissions increases every year,” said Sylvia McKean, MD, course director of Hospital Medicine 2008.
Best in Show
“It’s been a banner year for the poster presentations,” said Jeffrey Greenwald, MD, hospital medicine unit director, Boston Medical Center, as he announced the winning abstracts during the President’s Lunch on April 5:
- Research: “Prevention of Hospital-Acquired Venous Thromboembolism: Prospective Validation of a VTE Risk Assessment Model and Protocol, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
- Innovations: “Can Tissue Models Be Used to Teach Central Line Placement? Phase II of the Procedure Patient Safety Initiative (PPSI), Annie R. Harrington, MD, Cedars-Sinai Medical Center, Los Angeles; and
- Clinical Vignettes: “A Case of Salty Voluminous Urine, Twylla Tassava, MD, Saint Joseph Mercy Hospital, Ann Arbor, Mich.
Other Notable Works
Param Dedhia, MD, presented research he conducted with colleagues from Johns Hopkins Bayview Medical Center titled “Safe STEPS: Safe and Successful Transition of Elderly Patients.” The group developed an interdisciplinary, multifaceted intervention in this area, which included:
- A history and physical exam tailored to geriatric patients;
- A “fast facts fax” to communicate with the primary care physician;
- An interdisciplinary team worksheet for centralized input;
- A medical evaluation including a detailed review with the pharmacist; and?
- A pre-discharge appointment.
The results: A 15-question survey showed a 60% to 90% jump in patient satisfaction. A health assessment by self-report showed improvement as well, and the number of revisits and readmissions dropped from 10% to 3%.
“The Impact of Fragmentation of Hospitalist Care on Length of Stay and Post-Discharge Issues” was presented by Kenneth R. Epstein, MD, MBA, of IPC-The Hospitalist Company. Dr. Epstein and his colleagues used an observational study of data from IPC’s billing and clinical database on inpatient admissions with pneumonia with complications and heart failure and shock. They wanted to see if fragmented hospitalist care—care provided by more than one hospitalist—affected outcomes for these patients.
Using a fragmentation formula that included the number of days as an inpatient and the number of hospitalists who provided care, they found that for every 10% increase in fragmentation, the length of stay increased 0.45 days for pneumonia patients and 0.38 days for heart failure patients.
The country’s first fellowship for physician assistants (PA) specializing in hospital medicine was detailed in “The Mayo Clinic Arizona Post-Graduate PA Fellowship in Hospital Internal Medicine.” Kristen K. Will, MHPE, PA-C, co-program director of clinic’s PA Fellowship Program, outlined how her institution initiated the fellowship in October. The program will train one PA using hospital medicine-specific clinical rotations, didactic instruction, and teaching modules.