User login
Terminating an employee
I’ve written more than once about the private practitioner’s least favorite task. Now, new federal worker protection laws are making terminations even more difficult, even when they’re justified; however, that’s still no excuse for keeping an employee that should be replaced.
Once you make the decision to replace an employee, be sure that you have legitimate grounds and assemble as much documentation as you can. Record all terminable transgressions in the employee’s permanent record and document all verbal and written warnings. This is essential; you must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights were violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age – if the employee is over 40. You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusing to take a lie detector test, and reporting Occupational Safety and Health Administration violations.
You also can’t terminate someone for refusing to commit an illegal act – such as filing false insurance claims – or for exercising a legal right – such as voting or participating in a political demonstration.
While you cannot fire an alcohol abuser unless he or she is caught drinking at work, many forms of illegal drug use are legitimate causes for termination. Other laws may apply, depending on where you live. When in doubt, contact your attorney, state labor department, or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waiver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance – which I covered in detail a few months ago – to your umbrella policy, since lawsuits are always a possibility, despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon, you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend. Ask your manager or another trusted employee to be present to reduce the risk of subsequent disputes over what was discussed.
I’ve been asked to share exactly what I say; so for what it’s worth, here it is: “We have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So today we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, despite all your “hopes,” but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on. Make it clear, when necessary, that the decision has already been made, so arguing or pleading will change nothing.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain everything. They should hear it from you, not some distorted version via the rumor mill. You don’t have to divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
I’ve written more than once about the private practitioner’s least favorite task. Now, new federal worker protection laws are making terminations even more difficult, even when they’re justified; however, that’s still no excuse for keeping an employee that should be replaced.
Once you make the decision to replace an employee, be sure that you have legitimate grounds and assemble as much documentation as you can. Record all terminable transgressions in the employee’s permanent record and document all verbal and written warnings. This is essential; you must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights were violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age – if the employee is over 40. You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusing to take a lie detector test, and reporting Occupational Safety and Health Administration violations.
You also can’t terminate someone for refusing to commit an illegal act – such as filing false insurance claims – or for exercising a legal right – such as voting or participating in a political demonstration.
While you cannot fire an alcohol abuser unless he or she is caught drinking at work, many forms of illegal drug use are legitimate causes for termination. Other laws may apply, depending on where you live. When in doubt, contact your attorney, state labor department, or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waiver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance – which I covered in detail a few months ago – to your umbrella policy, since lawsuits are always a possibility, despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon, you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend. Ask your manager or another trusted employee to be present to reduce the risk of subsequent disputes over what was discussed.
I’ve been asked to share exactly what I say; so for what it’s worth, here it is: “We have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So today we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, despite all your “hopes,” but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on. Make it clear, when necessary, that the decision has already been made, so arguing or pleading will change nothing.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain everything. They should hear it from you, not some distorted version via the rumor mill. You don’t have to divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
I’ve written more than once about the private practitioner’s least favorite task. Now, new federal worker protection laws are making terminations even more difficult, even when they’re justified; however, that’s still no excuse for keeping an employee that should be replaced.
Once you make the decision to replace an employee, be sure that you have legitimate grounds and assemble as much documentation as you can. Record all terminable transgressions in the employee’s permanent record and document all verbal and written warnings. This is essential; you must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights were violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age – if the employee is over 40. You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusing to take a lie detector test, and reporting Occupational Safety and Health Administration violations.
You also can’t terminate someone for refusing to commit an illegal act – such as filing false insurance claims – or for exercising a legal right – such as voting or participating in a political demonstration.
While you cannot fire an alcohol abuser unless he or she is caught drinking at work, many forms of illegal drug use are legitimate causes for termination. Other laws may apply, depending on where you live. When in doubt, contact your attorney, state labor department, or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waiver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance – which I covered in detail a few months ago – to your umbrella policy, since lawsuits are always a possibility, despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon, you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend. Ask your manager or another trusted employee to be present to reduce the risk of subsequent disputes over what was discussed.
I’ve been asked to share exactly what I say; so for what it’s worth, here it is: “We have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So today we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, despite all your “hopes,” but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on. Make it clear, when necessary, that the decision has already been made, so arguing or pleading will change nothing.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain everything. They should hear it from you, not some distorted version via the rumor mill. You don’t have to divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Exercise type matters for fall prevention among elderly
according to a Cochrane Review meta-analysis of 108 randomized controlled trials.
Exercise has been shown to prevent falls in older people, but given the potential consequences, the investigators thought an up-to-date synthesis of the evidence was in order. The analysis focused on people living independently who had not recently been discharged from a hospital. The trials involved 23,407 subjects from 25 countries. The review was exhaustive; the final report is almost 600 pages long (Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2).
The type of exercise matters. The researchers cited “high-certainty evidence” that exercise involving balance and functional training reduces falls. “Tai chi may also prevent falls,” they noted, adding that they were uncertain of the effect of dance, walking, and resistance training by itself. There was no evidence to determine the effects of flexibility or endurance exercises, added the researchers, led by Cathie Sherrington, PhD, of the University of Sydney Institute for Musculoskeletal Health.
Functional exercise mimics everyday movement, with the goal of improving performance. Multidirectional lunges are an example, helping the body prepare for vacuuming, yard work, and other common activities.
“Exercise [programs] carried out in group classes or done at home prescribed by a health professional ... or a trained exercise leader were effective. Exercises were mostly done while standing as this better enhances balance and the ability to do daily activities such as standing up from a low chair or climbing stairs,” according to a Cochrane press release regarding the study.
Overall, exercise reduced the number of falls by 23%, and the number of fallers by 15%, with high-certainty evidence.
Exercise also brought down the number of people facing fall fractures by over 27%, the number of people requiring medical attention for a fall by 39%, and the number ending up in the hospital for a fall by 22%.
Balance and functional exercises reduced the rate of falls by 24%, and the number of fallers by 13%. The effects were even greater when resistance exercises were added to the mix; drops in fall rates and the number of people experiencing falls were 34% and 22%, respectively. There was low-certainty evidence that tai chi reduces the rate of falls by 19% and the number of people experiencing falls by 20%.
Despite fall prevention, “exercise may make little important difference to health-related quality of life;” when results were converted to EQ-5D and 36-Item Short Form Survey scores, “the respective 95% [confidence intervals] were much smaller than minimally important differences,” the investigators said.
Serious adverse events occurred in participants in one of the 27 trials that reported adverse events. These two serious adverse events were a pelvic stress fracture and an inguinal hernia surgery. Most of the other adverse events reported, all non-serious, were musculoskeletal.
On average, participants were 76 years old, and 77% were women. Disease specific trials – such as exercise for stroke rehabilitation – were excluded.
The work was supported primarily by the Cochrane Bone, Joint and Muscle Trauma Group, based at the University of Manchester, England, and Cochrane’s Acute and Emergency Care Network. There were no industry disclosures.
SOURCE: Sherrington C et al. Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2.
according to a Cochrane Review meta-analysis of 108 randomized controlled trials.
Exercise has been shown to prevent falls in older people, but given the potential consequences, the investigators thought an up-to-date synthesis of the evidence was in order. The analysis focused on people living independently who had not recently been discharged from a hospital. The trials involved 23,407 subjects from 25 countries. The review was exhaustive; the final report is almost 600 pages long (Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2).
The type of exercise matters. The researchers cited “high-certainty evidence” that exercise involving balance and functional training reduces falls. “Tai chi may also prevent falls,” they noted, adding that they were uncertain of the effect of dance, walking, and resistance training by itself. There was no evidence to determine the effects of flexibility or endurance exercises, added the researchers, led by Cathie Sherrington, PhD, of the University of Sydney Institute for Musculoskeletal Health.
Functional exercise mimics everyday movement, with the goal of improving performance. Multidirectional lunges are an example, helping the body prepare for vacuuming, yard work, and other common activities.
“Exercise [programs] carried out in group classes or done at home prescribed by a health professional ... or a trained exercise leader were effective. Exercises were mostly done while standing as this better enhances balance and the ability to do daily activities such as standing up from a low chair or climbing stairs,” according to a Cochrane press release regarding the study.
Overall, exercise reduced the number of falls by 23%, and the number of fallers by 15%, with high-certainty evidence.
Exercise also brought down the number of people facing fall fractures by over 27%, the number of people requiring medical attention for a fall by 39%, and the number ending up in the hospital for a fall by 22%.
Balance and functional exercises reduced the rate of falls by 24%, and the number of fallers by 13%. The effects were even greater when resistance exercises were added to the mix; drops in fall rates and the number of people experiencing falls were 34% and 22%, respectively. There was low-certainty evidence that tai chi reduces the rate of falls by 19% and the number of people experiencing falls by 20%.
Despite fall prevention, “exercise may make little important difference to health-related quality of life;” when results were converted to EQ-5D and 36-Item Short Form Survey scores, “the respective 95% [confidence intervals] were much smaller than minimally important differences,” the investigators said.
Serious adverse events occurred in participants in one of the 27 trials that reported adverse events. These two serious adverse events were a pelvic stress fracture and an inguinal hernia surgery. Most of the other adverse events reported, all non-serious, were musculoskeletal.
On average, participants were 76 years old, and 77% were women. Disease specific trials – such as exercise for stroke rehabilitation – were excluded.
The work was supported primarily by the Cochrane Bone, Joint and Muscle Trauma Group, based at the University of Manchester, England, and Cochrane’s Acute and Emergency Care Network. There were no industry disclosures.
SOURCE: Sherrington C et al. Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2.
according to a Cochrane Review meta-analysis of 108 randomized controlled trials.
Exercise has been shown to prevent falls in older people, but given the potential consequences, the investigators thought an up-to-date synthesis of the evidence was in order. The analysis focused on people living independently who had not recently been discharged from a hospital. The trials involved 23,407 subjects from 25 countries. The review was exhaustive; the final report is almost 600 pages long (Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2).
The type of exercise matters. The researchers cited “high-certainty evidence” that exercise involving balance and functional training reduces falls. “Tai chi may also prevent falls,” they noted, adding that they were uncertain of the effect of dance, walking, and resistance training by itself. There was no evidence to determine the effects of flexibility or endurance exercises, added the researchers, led by Cathie Sherrington, PhD, of the University of Sydney Institute for Musculoskeletal Health.
Functional exercise mimics everyday movement, with the goal of improving performance. Multidirectional lunges are an example, helping the body prepare for vacuuming, yard work, and other common activities.
“Exercise [programs] carried out in group classes or done at home prescribed by a health professional ... or a trained exercise leader were effective. Exercises were mostly done while standing as this better enhances balance and the ability to do daily activities such as standing up from a low chair or climbing stairs,” according to a Cochrane press release regarding the study.
Overall, exercise reduced the number of falls by 23%, and the number of fallers by 15%, with high-certainty evidence.
Exercise also brought down the number of people facing fall fractures by over 27%, the number of people requiring medical attention for a fall by 39%, and the number ending up in the hospital for a fall by 22%.
Balance and functional exercises reduced the rate of falls by 24%, and the number of fallers by 13%. The effects were even greater when resistance exercises were added to the mix; drops in fall rates and the number of people experiencing falls were 34% and 22%, respectively. There was low-certainty evidence that tai chi reduces the rate of falls by 19% and the number of people experiencing falls by 20%.
Despite fall prevention, “exercise may make little important difference to health-related quality of life;” when results were converted to EQ-5D and 36-Item Short Form Survey scores, “the respective 95% [confidence intervals] were much smaller than minimally important differences,” the investigators said.
Serious adverse events occurred in participants in one of the 27 trials that reported adverse events. These two serious adverse events were a pelvic stress fracture and an inguinal hernia surgery. Most of the other adverse events reported, all non-serious, were musculoskeletal.
On average, participants were 76 years old, and 77% were women. Disease specific trials – such as exercise for stroke rehabilitation – were excluded.
The work was supported primarily by the Cochrane Bone, Joint and Muscle Trauma Group, based at the University of Manchester, England, and Cochrane’s Acute and Emergency Care Network. There were no industry disclosures.
SOURCE: Sherrington C et al. Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2.
FROM COCHRANE DATABASE OF SYSTEMATIC REVIEWS
Key clinical point: Exercise helps elderly people avoid falls, especially if it focuses on balance and mimics daily activities.
Major finding: Balance and functional exercises reduce the rate of falls by 24%, and the number of fallers by 13%. The effects were even greater when resistance exercises were added to the mix; drops in fall rates and the number of people experiencing falls were 34% and 22%, respectively.
Study details: A meta-analysis of 108 randomized, controlled trials.
Disclosures: The work was supported by Cochrane. There were no industry disclosures.
Source: Sherrington C et al. Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424. doi: 10.1002/14651858.CD012424.pub2.
She Won’t Quit—But Will Her Heart?
ANSWER
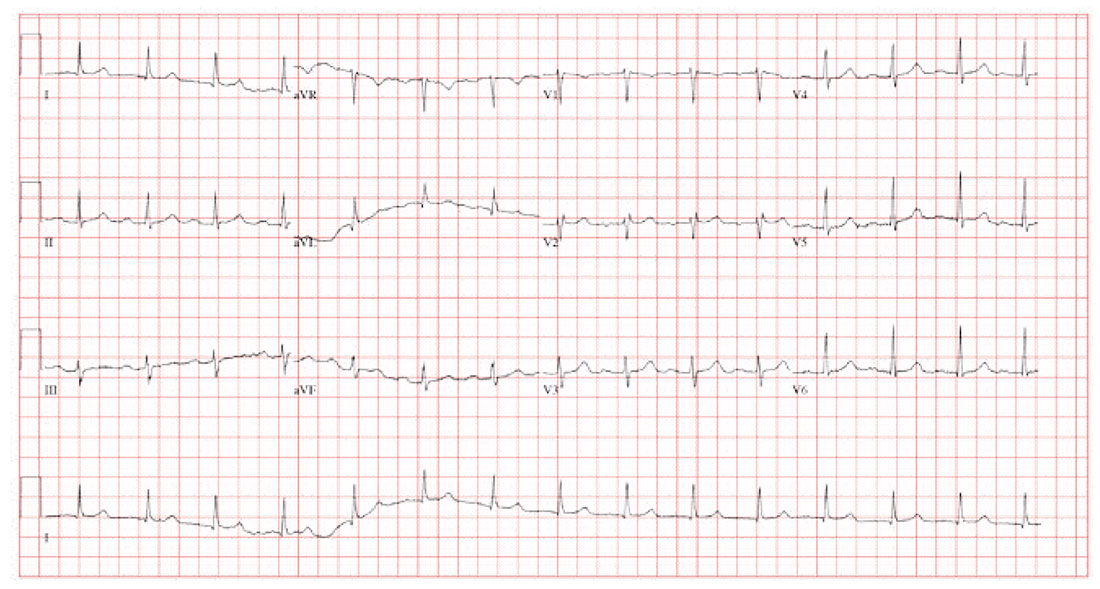
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
A 58-year-old woman presents for preoperative workup for surgical repair of a distal left tibial fracture sustained while snowshoeing. She had been descending a side slope when she lost her footing. Her left snowshoe became entangled in a large granite rock, which defined the lateral wall of the path she was traversing. She has no prior orthopedic injuries.
Cardiac history is remarkable for hypertension, palpitations, and two episodes of paroxysmal atrial fibrillation. A Holter monitor, worn to help determine the etiology of her palpitations, captured the atrial fibrillation episodes, each of which was cardioverted within 48 hours of onset without complication. Following the second cardioversion, about 6 months ago, a novel oral anticoagulation agent was recommended, but she refused to take it because she felt such medication would interfere with her active lifestyle.
The patient is otherwise quite healthy and has been personally active in her preventive health maintenance.
Her current medications include lisinopril (5 mg/d) and aspirin (81 mg/d). She also takes a multivitamin daily. In the past 24 hours, she has taken two doses of acetaminophen/oxycodone (325/5 mg) for left ankle pain. She has no drug allergies.
The patient, an immigration attorney for a prominent law firm, is divorced and has no children. She works as a Zumba instructor on the weekends and has run 3 marathons within the past 2 years. She has never smoked or used recreational drugs, but she does partake in one or two glasses of wine with friends on weekends.
Family history is remarkable for hypertension in both parents and two of her three siblings. All are alive and otherwise healthy.
Review of systems reveals no current problems. She states she went through menopause about 10 years ago and was recommended to start estrogen therapy but refused this treatment.
Vital signs include a blood pressure of 118/88 mm Hg; pulse, 90 beats/min; temperature, 98.4°F; and O2 saturation, 98% on room air. Her weight is 129 lb, and her height, 64 in.
Physical exam reveals a healthy, athletic woman in no distress. She wears an orthopedic boot on her left foot, but it isn’t removed to examine the affected ankle. She wears contact lenses and has a posterior lingual brace on her lower teeth.
The HEENT exam is normal. The neck is supple without masses. There is no thyromegaly, carotid bruits, or jugular venous distention. The lungs are clear in all fields. The breasts are symmetrical without palpable nodules.
Cardiac exam is remarkable for a regular rate and rhythm at 90 beats/min. There is a soft end-systolic murmur consistent with mild mitral regurgitation. S1 and S2 are of normal intensity, and there are no extra heart sounds.
The abdomen is nontender with no organomegaly; the patient proudly shows her core strength and “a hint of a six-pack.” The genitourinary exam is deferred. Peripheral pulses are strong and equal bilaterally. The neurologic exam is grossly intact.
A preoperative chest x-ray is performed; results are pending.
The ECG shows a ventricular rate of 89 beats/min; PR interval, 232 ms; QRS duration, 82 ms; QT/QTc interval, 364/442 ms; P axis, 86°; R axis, 23°
Pregnant women want genome guidance
Also today, a look at asthma, obesity, and the risk for severe sleep apnea in children, new questions about the role that antinuclear antibodies are playing in systemic lupus erythematosus, and the lifetime cost of tobacco is nearly $2 million per smoker.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, a look at asthma, obesity, and the risk for severe sleep apnea in children, new questions about the role that antinuclear antibodies are playing in systemic lupus erythematosus, and the lifetime cost of tobacco is nearly $2 million per smoker.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, a look at asthma, obesity, and the risk for severe sleep apnea in children, new questions about the role that antinuclear antibodies are playing in systemic lupus erythematosus, and the lifetime cost of tobacco is nearly $2 million per smoker.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Interactive parenting, life skill intervention improves self-esteem in teen mothers
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
lfranki@mdedge.com
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
lfranki@mdedge.com
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
lfranki@mdedge.com
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
FROM PEDIATRICS
DAAs reduce mortality, cancer risk in HCV study
Direct-acting antivirals significantly decrease risk of hepatocellular carcinoma and mortality in persons with hepatitis C, according to results of the first prospective, longitudinal study to evaluate the effect of the drugs on complications related to the infection.
Compared with no treatment, DAA therapy cut risk of hepatocellular carcinoma by about one-third and all-cause mortality by about half in the study, which included about 10,000 adult patients with chronic hepatitis C virus (HCV) infection treated at 1 of 32 hepatology centers in France (NCT01953458).
There were no signs of increased risk of hepatocellular carcinoma during treatment with DAAs, providing more evidence refuting earlier, single-center reports that had suggested an increased incidence early after treatment. These findings also counterbalance a recent Cochrane review that could not confirm or reject a potential benefit of drugs on long-term morbidity and mortality.
Results of the study, published in the Lancet, are based on analysis of 9,895 patients, including 7,344 who started DAA treatment and 2,551 who remained untreated at a median follow-up of more than 31 months. The median patient age was 56 years, and 53% were men.
Treatment with DAAs reduced risk of hepatocellular carcinoma when compared with no DAA treatment, with a hazard ratio of 0.66 (95% confidence interval, 0.46-0.93), and reduced risk of all-cause mortality, with an HR of 0.48 (95% CI, 0.33-0.70), investigators reported in a multivariable analysis that adjusted for variables including age, sex, fibrosis score, HCV genotype, alcohol use, and more.
“These inverse associations persisted in the subgroup of patients who achieved a sustained virological response, whereas those who did not achieve a sustained virological response were a higher risk for hepatocellular carcinoma,” said the investigators, led by Fabrice Carrat, PhD, of Sorbonne Université, Institut National de la Santé et de la Recherche Médicale (INSERM), Paris.
Sustained virologic response was observed in 94% of patients who had known response status and sufficient follow-up, investigators said.
In patients with cirrhosis at baseline, DAA treatment had a similarly strong association with reduced hepatocellular carcinoma and mortality, with a sustained virologic response rate of 92% in those for whom sufficient data was available, they said.
There was no evidence for an increased risk of hepatocellular carcinoma on treatment, with an adjusted HR of 0.74 (95% CI, 0.49-1.13; P = 0.17), they added.
“Our results support urgent treatment of patients with advanced liver disease and extension of the follow-up of treated patients with less severe disease to assess the long-term clinical effect of direct-acting antiviral treatment,” Dr. Carrat and colleagues said in a commentary on their results.
However, the long-term effect of DAAs on liver decompensation has yet to be clarified, they added, noting that their study excluded patients with decompensated cirrhosis or a history of hepatocellular carcinoma.
Funding for the study came from INSERM, Agence Nationale de la Recherche, DGS (Direction Générale de la Santé), MSD, Janssen, Gilead, AbbVie, Bristol-Myers Squibb, and Roche. Dr. Carrat reported personal fees from Imaxio not related to the present study. Coauthors provided additional disclosures related to Gilead, AbbVie, Bristol-Myers Squibb, MSD, and Janssen, among others.
SOURCE: Carrat F et al. Lancet. 2019 Feb 11. doi: 10.1016/S0140-6736(18)32111-1
This study provides “substantive evidence” that curing hepatitis C virus with all-oral direct-acting antiviral regimens provides clinical benefits, according to Raymond T. Chung, MD, and his coauthors of a related editorial.
Investigators in this study provide the best evidence so far in support of guidelines that advise direct-acting antiviral (DAA) treatment for all patients with chronic hepatitis C virus (HCV) infection, the editorial’s authors stated.
Results of the French study provide a strong counterpoint to the findings of a recent Cochrane review of DAA trials that could not confirm or reject whether DAAs had effects on long-term morbidity and mortality related to HCV, added Dr. Chung and his coauthors. “Finally, they provide credence to the achievability of the goals set out by the World Health Organization (WHO), not only to eliminate HCV but also to substantially reduce its complications.”
The WHO targets were established in light of earlier evidence that sustained virologic responses are linked to reductions in hepatocellular carcinoma, liver transplantation, and mortality, they said.
“In view of the high sustained virological response and excellent tolerability achieved with DAAs, it seemed highly plausible to envision reductions in chronic HCV infection–related complications with these drugs,” they said in reference to the study by Carrat and colleagues.
This editorial appearing in the Lancet was authored by Jacinta A. Holmes, Stephanie M. Rutledge, and Raymond T. Chung of the Liver Center, Gastrointestinal Division, Massachusetts General Hospital, Boston. Dr. Chung provided disclosures related to AbbVie, Gilead, Merck, Bristol-Myers Squibb, Roche, Janssen, and Boehringer Ingelheim.
This study provides “substantive evidence” that curing hepatitis C virus with all-oral direct-acting antiviral regimens provides clinical benefits, according to Raymond T. Chung, MD, and his coauthors of a related editorial.
Investigators in this study provide the best evidence so far in support of guidelines that advise direct-acting antiviral (DAA) treatment for all patients with chronic hepatitis C virus (HCV) infection, the editorial’s authors stated.
Results of the French study provide a strong counterpoint to the findings of a recent Cochrane review of DAA trials that could not confirm or reject whether DAAs had effects on long-term morbidity and mortality related to HCV, added Dr. Chung and his coauthors. “Finally, they provide credence to the achievability of the goals set out by the World Health Organization (WHO), not only to eliminate HCV but also to substantially reduce its complications.”
The WHO targets were established in light of earlier evidence that sustained virologic responses are linked to reductions in hepatocellular carcinoma, liver transplantation, and mortality, they said.
“In view of the high sustained virological response and excellent tolerability achieved with DAAs, it seemed highly plausible to envision reductions in chronic HCV infection–related complications with these drugs,” they said in reference to the study by Carrat and colleagues.
This editorial appearing in the Lancet was authored by Jacinta A. Holmes, Stephanie M. Rutledge, and Raymond T. Chung of the Liver Center, Gastrointestinal Division, Massachusetts General Hospital, Boston. Dr. Chung provided disclosures related to AbbVie, Gilead, Merck, Bristol-Myers Squibb, Roche, Janssen, and Boehringer Ingelheim.
This study provides “substantive evidence” that curing hepatitis C virus with all-oral direct-acting antiviral regimens provides clinical benefits, according to Raymond T. Chung, MD, and his coauthors of a related editorial.
Investigators in this study provide the best evidence so far in support of guidelines that advise direct-acting antiviral (DAA) treatment for all patients with chronic hepatitis C virus (HCV) infection, the editorial’s authors stated.
Results of the French study provide a strong counterpoint to the findings of a recent Cochrane review of DAA trials that could not confirm or reject whether DAAs had effects on long-term morbidity and mortality related to HCV, added Dr. Chung and his coauthors. “Finally, they provide credence to the achievability of the goals set out by the World Health Organization (WHO), not only to eliminate HCV but also to substantially reduce its complications.”
The WHO targets were established in light of earlier evidence that sustained virologic responses are linked to reductions in hepatocellular carcinoma, liver transplantation, and mortality, they said.
“In view of the high sustained virological response and excellent tolerability achieved with DAAs, it seemed highly plausible to envision reductions in chronic HCV infection–related complications with these drugs,” they said in reference to the study by Carrat and colleagues.
This editorial appearing in the Lancet was authored by Jacinta A. Holmes, Stephanie M. Rutledge, and Raymond T. Chung of the Liver Center, Gastrointestinal Division, Massachusetts General Hospital, Boston. Dr. Chung provided disclosures related to AbbVie, Gilead, Merck, Bristol-Myers Squibb, Roche, Janssen, and Boehringer Ingelheim.
Direct-acting antivirals significantly decrease risk of hepatocellular carcinoma and mortality in persons with hepatitis C, according to results of the first prospective, longitudinal study to evaluate the effect of the drugs on complications related to the infection.
Compared with no treatment, DAA therapy cut risk of hepatocellular carcinoma by about one-third and all-cause mortality by about half in the study, which included about 10,000 adult patients with chronic hepatitis C virus (HCV) infection treated at 1 of 32 hepatology centers in France (NCT01953458).
There were no signs of increased risk of hepatocellular carcinoma during treatment with DAAs, providing more evidence refuting earlier, single-center reports that had suggested an increased incidence early after treatment. These findings also counterbalance a recent Cochrane review that could not confirm or reject a potential benefit of drugs on long-term morbidity and mortality.
Results of the study, published in the Lancet, are based on analysis of 9,895 patients, including 7,344 who started DAA treatment and 2,551 who remained untreated at a median follow-up of more than 31 months. The median patient age was 56 years, and 53% were men.
Treatment with DAAs reduced risk of hepatocellular carcinoma when compared with no DAA treatment, with a hazard ratio of 0.66 (95% confidence interval, 0.46-0.93), and reduced risk of all-cause mortality, with an HR of 0.48 (95% CI, 0.33-0.70), investigators reported in a multivariable analysis that adjusted for variables including age, sex, fibrosis score, HCV genotype, alcohol use, and more.
“These inverse associations persisted in the subgroup of patients who achieved a sustained virological response, whereas those who did not achieve a sustained virological response were a higher risk for hepatocellular carcinoma,” said the investigators, led by Fabrice Carrat, PhD, of Sorbonne Université, Institut National de la Santé et de la Recherche Médicale (INSERM), Paris.
Sustained virologic response was observed in 94% of patients who had known response status and sufficient follow-up, investigators said.
In patients with cirrhosis at baseline, DAA treatment had a similarly strong association with reduced hepatocellular carcinoma and mortality, with a sustained virologic response rate of 92% in those for whom sufficient data was available, they said.
There was no evidence for an increased risk of hepatocellular carcinoma on treatment, with an adjusted HR of 0.74 (95% CI, 0.49-1.13; P = 0.17), they added.
“Our results support urgent treatment of patients with advanced liver disease and extension of the follow-up of treated patients with less severe disease to assess the long-term clinical effect of direct-acting antiviral treatment,” Dr. Carrat and colleagues said in a commentary on their results.
However, the long-term effect of DAAs on liver decompensation has yet to be clarified, they added, noting that their study excluded patients with decompensated cirrhosis or a history of hepatocellular carcinoma.
Funding for the study came from INSERM, Agence Nationale de la Recherche, DGS (Direction Générale de la Santé), MSD, Janssen, Gilead, AbbVie, Bristol-Myers Squibb, and Roche. Dr. Carrat reported personal fees from Imaxio not related to the present study. Coauthors provided additional disclosures related to Gilead, AbbVie, Bristol-Myers Squibb, MSD, and Janssen, among others.
SOURCE: Carrat F et al. Lancet. 2019 Feb 11. doi: 10.1016/S0140-6736(18)32111-1
Direct-acting antivirals significantly decrease risk of hepatocellular carcinoma and mortality in persons with hepatitis C, according to results of the first prospective, longitudinal study to evaluate the effect of the drugs on complications related to the infection.
Compared with no treatment, DAA therapy cut risk of hepatocellular carcinoma by about one-third and all-cause mortality by about half in the study, which included about 10,000 adult patients with chronic hepatitis C virus (HCV) infection treated at 1 of 32 hepatology centers in France (NCT01953458).
There were no signs of increased risk of hepatocellular carcinoma during treatment with DAAs, providing more evidence refuting earlier, single-center reports that had suggested an increased incidence early after treatment. These findings also counterbalance a recent Cochrane review that could not confirm or reject a potential benefit of drugs on long-term morbidity and mortality.
Results of the study, published in the Lancet, are based on analysis of 9,895 patients, including 7,344 who started DAA treatment and 2,551 who remained untreated at a median follow-up of more than 31 months. The median patient age was 56 years, and 53% were men.
Treatment with DAAs reduced risk of hepatocellular carcinoma when compared with no DAA treatment, with a hazard ratio of 0.66 (95% confidence interval, 0.46-0.93), and reduced risk of all-cause mortality, with an HR of 0.48 (95% CI, 0.33-0.70), investigators reported in a multivariable analysis that adjusted for variables including age, sex, fibrosis score, HCV genotype, alcohol use, and more.
“These inverse associations persisted in the subgroup of patients who achieved a sustained virological response, whereas those who did not achieve a sustained virological response were a higher risk for hepatocellular carcinoma,” said the investigators, led by Fabrice Carrat, PhD, of Sorbonne Université, Institut National de la Santé et de la Recherche Médicale (INSERM), Paris.
Sustained virologic response was observed in 94% of patients who had known response status and sufficient follow-up, investigators said.
In patients with cirrhosis at baseline, DAA treatment had a similarly strong association with reduced hepatocellular carcinoma and mortality, with a sustained virologic response rate of 92% in those for whom sufficient data was available, they said.
There was no evidence for an increased risk of hepatocellular carcinoma on treatment, with an adjusted HR of 0.74 (95% CI, 0.49-1.13; P = 0.17), they added.
“Our results support urgent treatment of patients with advanced liver disease and extension of the follow-up of treated patients with less severe disease to assess the long-term clinical effect of direct-acting antiviral treatment,” Dr. Carrat and colleagues said in a commentary on their results.
However, the long-term effect of DAAs on liver decompensation has yet to be clarified, they added, noting that their study excluded patients with decompensated cirrhosis or a history of hepatocellular carcinoma.
Funding for the study came from INSERM, Agence Nationale de la Recherche, DGS (Direction Générale de la Santé), MSD, Janssen, Gilead, AbbVie, Bristol-Myers Squibb, and Roche. Dr. Carrat reported personal fees from Imaxio not related to the present study. Coauthors provided additional disclosures related to Gilead, AbbVie, Bristol-Myers Squibb, MSD, and Janssen, among others.
SOURCE: Carrat F et al. Lancet. 2019 Feb 11. doi: 10.1016/S0140-6736(18)32111-1
FROM THE LANCET
Key clinical point:
Major finding: DAAs reduced risk of hepatocellular carcinoma (HR, 0.66; 95% confidence interval, 0.46-0.93) and all-cause mortality (HR, 0.48; 95% CI, 0.33-0.70).
Study details: A prospective study including about 10,000 adults with chronic HCV infection enrolled at 1 of 32 centers in France.
Disclosures: Funding for the study came from INSERM, Agence Nationale de la Recherche, DGS (Direction Générale de la Santé), MSD, Janssen, Gilead, AbbVie, Bristol-Myers Squibb, and Roche. Dr. Carrat reported personal fees from Imaxio not related to the present study. Coauthors provided additional disclosures related to the study pharma sponsors among others.
Source: Carrat F et al. Lancet. 2019 Feb 11. doi: 10.1016/20S0140-6736(18)32111-1.
Watchful waiting up for low-risk prostate cancer
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
FROM JAMA
Key clinical point: Conservative management for low-risk localized prostate cancer is up, in line with guidelines, while radical prostatectomy use has increased in high-risk disease despite a lack of new high-level evidence to support that approach.
Major finding: In men with low-risk disease, active surveillance or watchful waiting increased from 14.5% in 2010 to 42.1% in 2015, while in high-risk disease, radical prostatectomy increased from 38.0% to 42.8%
Study details: Analysis including 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database.
Disclosures: Study authors reported disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, Astellas, and the National Institutes of Health.
Source: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Quick Byte: Needle-free injections
A start-up operating out of MIT in Cambridge, Mass., called Portal Instruments has developed a needleless injection system.
The device, called PRIME, delivers medication into the bloodstream in a high-pressure stream that travels at Mach 0.7 – the speed of a jet. The makers signed a commercial deal in December 2017, and the device is expected to be available soon.
Reference
1. Kerrigan S. The 16 Most Remarkable Healthcare Innovations, Events, and Discoveries of 2018 For World Health Day. https://interestingengineering.com/the-16-most-remarkable-healthcare-innovations-events-and-discoveries-of-2018-for-world-health-day. April 7, 2018. Accessed June 4, 2018.
A start-up operating out of MIT in Cambridge, Mass., called Portal Instruments has developed a needleless injection system.
The device, called PRIME, delivers medication into the bloodstream in a high-pressure stream that travels at Mach 0.7 – the speed of a jet. The makers signed a commercial deal in December 2017, and the device is expected to be available soon.
Reference
1. Kerrigan S. The 16 Most Remarkable Healthcare Innovations, Events, and Discoveries of 2018 For World Health Day. https://interestingengineering.com/the-16-most-remarkable-healthcare-innovations-events-and-discoveries-of-2018-for-world-health-day. April 7, 2018. Accessed June 4, 2018.
A start-up operating out of MIT in Cambridge, Mass., called Portal Instruments has developed a needleless injection system.
The device, called PRIME, delivers medication into the bloodstream in a high-pressure stream that travels at Mach 0.7 – the speed of a jet. The makers signed a commercial deal in December 2017, and the device is expected to be available soon.
Reference
1. Kerrigan S. The 16 Most Remarkable Healthcare Innovations, Events, and Discoveries of 2018 For World Health Day. https://interestingengineering.com/the-16-most-remarkable-healthcare-innovations-events-and-discoveries-of-2018-for-world-health-day. April 7, 2018. Accessed June 4, 2018.
United States now over 100 measles cases for the year
according to the Centers for Disease Control and Prevention.
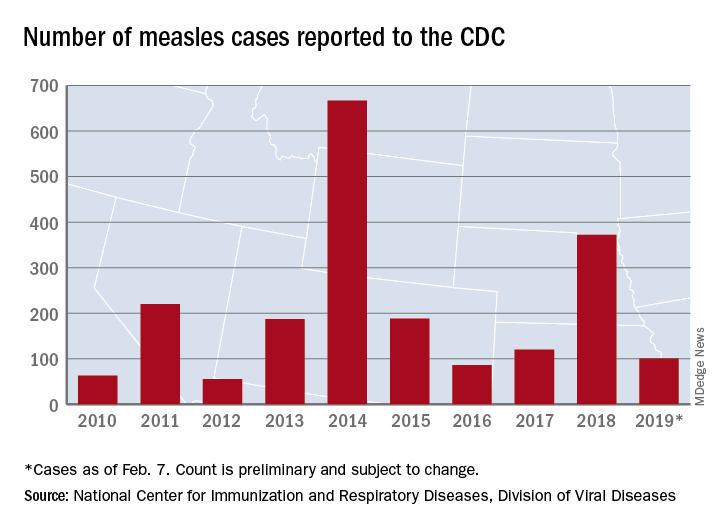
Just over half of the cases in 2019 have occurred in Clark County, Wash., which has reported 53 cases. That outbreak led Gov. Jay Inslee to declare a public health emergency for the entire state on Jan. 25.
The cases in Washington represent one of the five outbreaks – the CDC defines an outbreak as three or more cases – that have occurred so far this year, with three reported in New York State (Rockland County, Monroe County, and New York City) and one in Texas, which has been spread out over five counties, the CDC reported Feb. 11.
“These outbreaks are linked to travelers who brought measles back from other countries such as Israel and Ukraine, where large measles outbreaks are occurring,” the CDC noted. The other states with confirmed cases are California, Colorado, Connecticut, Georgia, Illinois, New Jersey, and Oregon.
In a video released Feb. 1, Surgeon General Jerome Adams stressed the importance of getting vaccinated and noted that an infected person can transmit the measles virus up to 4 days before he or she develops symptoms.
according to the Centers for Disease Control and Prevention.
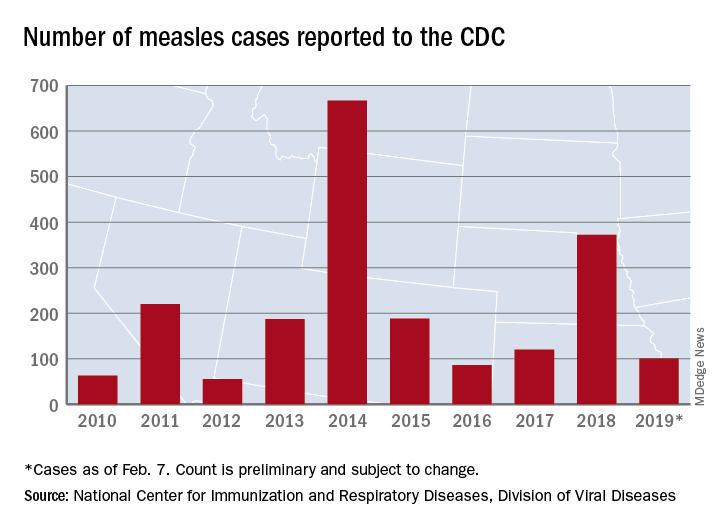
Just over half of the cases in 2019 have occurred in Clark County, Wash., which has reported 53 cases. That outbreak led Gov. Jay Inslee to declare a public health emergency for the entire state on Jan. 25.
The cases in Washington represent one of the five outbreaks – the CDC defines an outbreak as three or more cases – that have occurred so far this year, with three reported in New York State (Rockland County, Monroe County, and New York City) and one in Texas, which has been spread out over five counties, the CDC reported Feb. 11.
“These outbreaks are linked to travelers who brought measles back from other countries such as Israel and Ukraine, where large measles outbreaks are occurring,” the CDC noted. The other states with confirmed cases are California, Colorado, Connecticut, Georgia, Illinois, New Jersey, and Oregon.
In a video released Feb. 1, Surgeon General Jerome Adams stressed the importance of getting vaccinated and noted that an infected person can transmit the measles virus up to 4 days before he or she develops symptoms.
according to the Centers for Disease Control and Prevention.
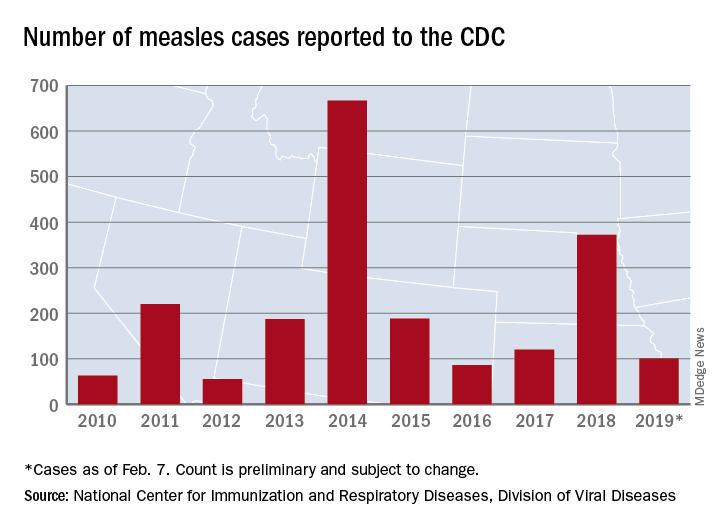
Just over half of the cases in 2019 have occurred in Clark County, Wash., which has reported 53 cases. That outbreak led Gov. Jay Inslee to declare a public health emergency for the entire state on Jan. 25.
The cases in Washington represent one of the five outbreaks – the CDC defines an outbreak as three or more cases – that have occurred so far this year, with three reported in New York State (Rockland County, Monroe County, and New York City) and one in Texas, which has been spread out over five counties, the CDC reported Feb. 11.
“These outbreaks are linked to travelers who brought measles back from other countries such as Israel and Ukraine, where large measles outbreaks are occurring,” the CDC noted. The other states with confirmed cases are California, Colorado, Connecticut, Georgia, Illinois, New Jersey, and Oregon.
In a video released Feb. 1, Surgeon General Jerome Adams stressed the importance of getting vaccinated and noted that an infected person can transmit the measles virus up to 4 days before he or she develops symptoms.
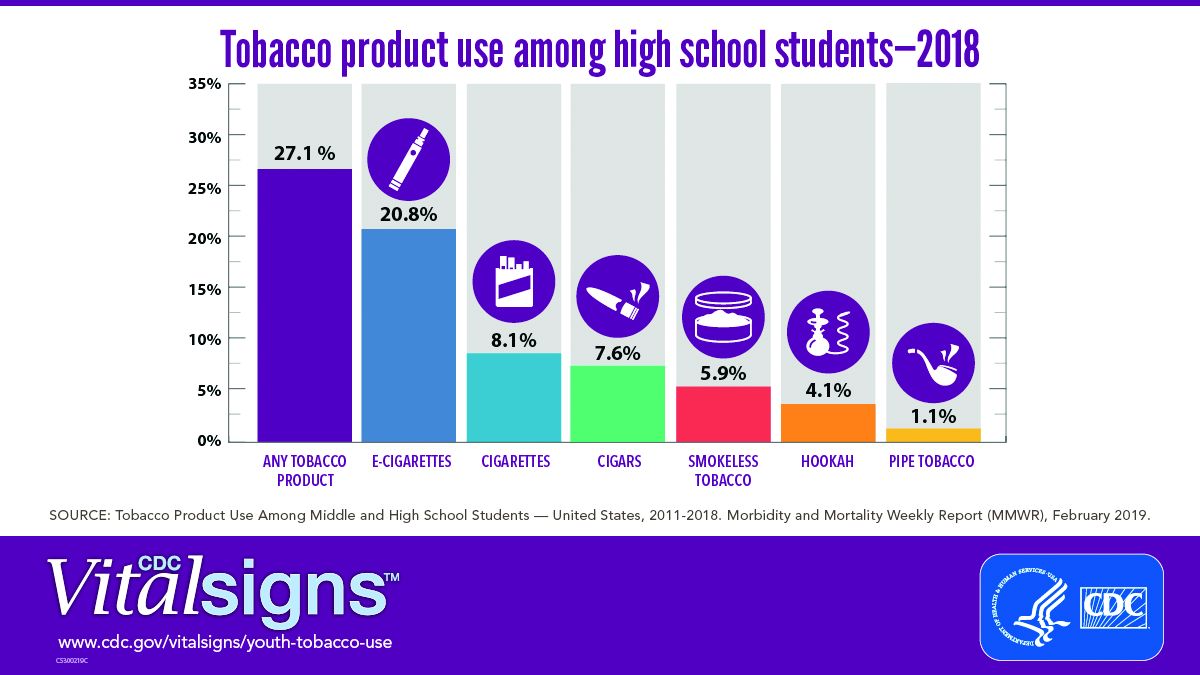
E-cig use reverses progress in reducing tobacco use in teens
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
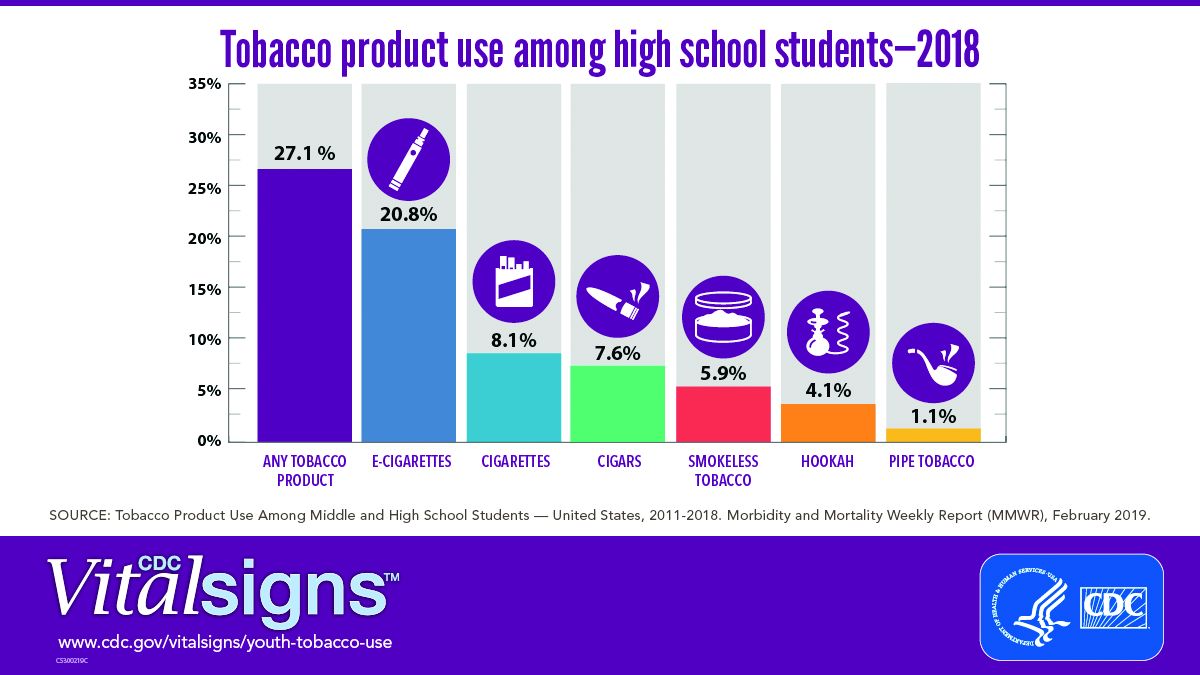
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
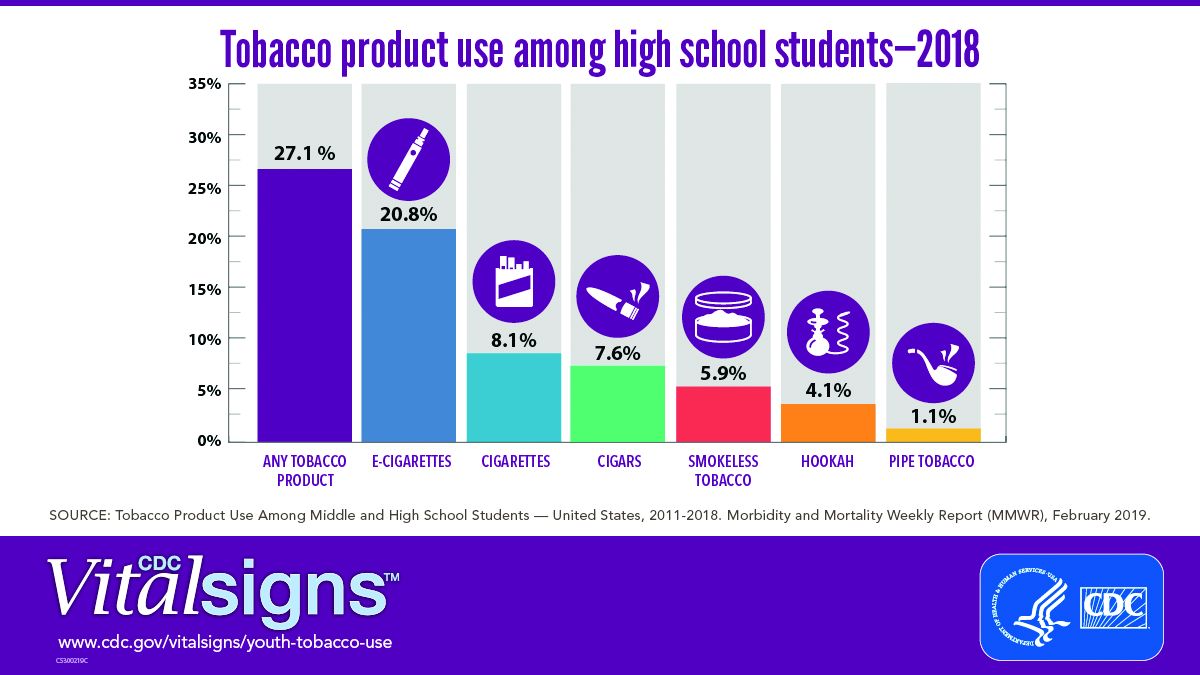
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
FROM CDC VITAL SIGNS REPORT