User login
Fine-tune staging for better SCC risk stratification
ORLANDO – When caring for individuals with sun-damaged skin, dermatologists need comfort with the full spectrum of photo-related skin disease. From assessment and treatment of actinic keratoses (AKs) and field cancerization, to long-term follow-up of cutaneous squamous cell carcinomas (SCCs), appropriate treatment and staging can improve patient quality of life and reduce health care costs, Vishal Patel, MD, said at the Orlando Dermatology Aesthetic and Clinical Conference.
said Dr. Patel, director of cutaneous oncology at George Washington University Cancer Center, Washington. On the other hand, he added, “field disease can be a marker for invasive squamous cell carcinoma risk, and it requires field treatment.” Treatment that reduces field disease is primary prevention because it decreases the formation of invasive SCC, he noted.
“But this level of disease – AKs and SCC in situ – doesn’t kill people,” he emphasized. “I want to leave you with an ability to stage this disease,” said Dr. Patel, noting that SCC mortality may eventually surpass melanoma mortality as deaths from the latter decline and numbers of older Americans with high ultraviolet light exposure and other risk factors climb.
While the majority of AKs regress within 5 years, he looks at the total burden of AKs as a marker for field cancerization “because having less than five in situ or actinic lesions puts you at less than a 1% risk of squamous cell carcinoma formation. Having more than 20 increases that risk 20-fold to 20%,” he said. “That’s the way we need to start thinking about this: Is this a disease – or a symptom?”
Rather than thinking of each AK or SCC in situ as a separate disease event, “the disease we need to be focusing on and treating is field cancerization,” he continued. Within this context, “we should not be thinking that … we need to be aggressive in our management,” which is what results in high costs.
“The reality is that this is a big quality of life issue for our patients. So what do we do?” Field treatment is appropriate for field disease, he said. Dr. Patel said that at GW only field treatment is used; destructive treatment for AKs and SCC in situ is not used. In the absence of patient and lesion characteristics that elevate risk,“surgery is really not the standard of care for in situ lesions for us,” he commented.
“We start by discerning the field disease from the invasive disease” with an initial round of field treatment and, if needed, adjunctive oral chemoprophylaxis. “We lather, rinse, and repeat” the field therapy, continuously if needed, Dr. Patel said.
“We like to do that because we can then identify those specific lesions we want to go after. No cryosurgery, no destructive therapy, because we run the risk of burying those tumors under the scar. They may recur and make it more difficult to accurately stage them in the future,” he noted.
“I like to be more sophisticated in thinking about our approach to the outcomes of these individual lesions,” he said. When it comes to excising lesions that have been biopsied and show invasive SCC, “disc excision may be a more cost-effective way to treat many low-risk SCCs,” he noted. In any case, “removal with clear surgical margins is key.”
Primary tumors with such low-risk attributes as diameter under a centimeter and thickness under 2 mm; well-defined borders; location on the trunk, neck, or extremities; well-differentiated histology; and lack of perineural invasion can all be considered for a disc technique, especially if the patient is immunocompetent without background chronic inflammation or a history of prior radiation therapy.
Staging SCCs, said Dr. Patel, is where things really get tricky. Older staging systems for SCC “led us to overtreat nonaggressive disease and undertreat aggressive disease. I think we have the responsibility to lead the charge to having a more sophisticated approach.” For example, patients whose tumors were staged T2 in the American Joint Commission on Cancer (AJCC) 7 classification system were most likely to have poor outcomes – in part because so few tumors were staged higher – which meant AJCC 7 didn’t provide adequate differentiation for useful risk prognostication.
A group of researchers at the Brigham and Women’s Hospital (BWH), Boston, “came up with a better system to better differentiate those T2 tumors into a high-risk and a low-risk subtype,” according to Dr. Patel.
With use of validated risk factors, the investigators applied a long list of risk factors to 2,000 tumors to see which risk factors, taken individually, were really contributing to poor outcomes. Eventually, four risk factors that made the most difference were identified: size greater than 2 cm, poor tumor differentiation, perineural invasion greater than 0.1 mm in diameter, and tumor invasion beyond subcutaneous fat. “I really want to highlight the size portion of those risk factors,” said Dr. Patel. “Something I’d like you to do in your clinical practice is to measure and document the size of the lesion. … That really, clearly helps” with risk prognostication.
These four factors were then used to break out a T2a stage for tumors with one risk factor and a T2b stage for tumors with two or three risk factors. Tumors with no risk factors are stage T1, and those with all four risk factors are stage T3. In situ SCC is T0.
Applying this new staging system to a 2,000-patient cohort with SCC yielded clear separation in outcomes including recurrence, nodal metastasis, disease-specific death, and overall survival between patients with the T2a and T2b tumors (P less than .001 for all; J Clin Oncol. 2014 Feb 1;32[4]:327-34).
While AJCC 8 is “significantly better” than AJCC 7 in its incorporation of meaningful risk factors into the SCC staging system, “it still underperforms in comparison” with the BWH staging system using the 2000 patient cohort, he said. Recent work has shown the BWH classification system to have superior specificity and positive predictive value in detecting nodal metastasis and disease-specific death in higher-grade tumors. But both BWH and AJCC 8 need further refinement.
“So what are the staging pearls to take home?” Dr. Patel asked. “First, utilize a staging system.” “Staging of SCC utilizing should be done routinely. Most data seems to suggest that the BWH system appears to outperform AJCC 8, and it is what we currently use routinely at GW,” he said.
Patients who are T1 by BWH criteria, with no risk factors, are at low or even no risk, he noted. He pointed out that of the nearly 1,400 patients who met T1 criteria, there were just eight local recurrences, one nodal metastasis, and no distant metastases or deaths. Knowing this should guide physicians on a treatment path that will reduce costs and provide patients with peace of mind, he said.
In the BWH schema, T2a patients fared almost as well, with a 2% risk of nodal metastasis and an overall 1% risk of disease-specific death. “T2a disease is low risk, in my mind. Most of these patients will go on to do well,” he said.
By contrast, “there may be a number of tumors that you are missing” that are candidates for close follow-up if the BWH criteria are not being used, said Dr. Patel. These are the T2b tumors. “For those patients, we want to aggressively follow them and think about a more aggressive management plan.”
The bottom line is that BWH T2b and T3 tumors are both high risk, and management needs to acknowledge this, he said. The current protocol in our cutaneous oncology program includes using routine radiologic nodal staging in patients with BWH stage 2b and above SCCs and considering sentinel lymph node biopsy for certain individuals.
For patients with BWH T2b and T3 tumors, dermatologists should give consideration to tertiary care or cancer center referrals so they have access to the full spectrum of diagnostic and therapeutic modalities and the opportunity to participate in clinical trials, Dr. Patel said.
Dr. Patel reported that he is a speaker for Regeneron/Sanofi and a cofounder of the Skin Cancer Outcomes (SCOUT) consortium.
This article was updated 2/9/2019
ORLANDO – When caring for individuals with sun-damaged skin, dermatologists need comfort with the full spectrum of photo-related skin disease. From assessment and treatment of actinic keratoses (AKs) and field cancerization, to long-term follow-up of cutaneous squamous cell carcinomas (SCCs), appropriate treatment and staging can improve patient quality of life and reduce health care costs, Vishal Patel, MD, said at the Orlando Dermatology Aesthetic and Clinical Conference.
said Dr. Patel, director of cutaneous oncology at George Washington University Cancer Center, Washington. On the other hand, he added, “field disease can be a marker for invasive squamous cell carcinoma risk, and it requires field treatment.” Treatment that reduces field disease is primary prevention because it decreases the formation of invasive SCC, he noted.
“But this level of disease – AKs and SCC in situ – doesn’t kill people,” he emphasized. “I want to leave you with an ability to stage this disease,” said Dr. Patel, noting that SCC mortality may eventually surpass melanoma mortality as deaths from the latter decline and numbers of older Americans with high ultraviolet light exposure and other risk factors climb.
While the majority of AKs regress within 5 years, he looks at the total burden of AKs as a marker for field cancerization “because having less than five in situ or actinic lesions puts you at less than a 1% risk of squamous cell carcinoma formation. Having more than 20 increases that risk 20-fold to 20%,” he said. “That’s the way we need to start thinking about this: Is this a disease – or a symptom?”
Rather than thinking of each AK or SCC in situ as a separate disease event, “the disease we need to be focusing on and treating is field cancerization,” he continued. Within this context, “we should not be thinking that … we need to be aggressive in our management,” which is what results in high costs.
“The reality is that this is a big quality of life issue for our patients. So what do we do?” Field treatment is appropriate for field disease, he said. Dr. Patel said that at GW only field treatment is used; destructive treatment for AKs and SCC in situ is not used. In the absence of patient and lesion characteristics that elevate risk,“surgery is really not the standard of care for in situ lesions for us,” he commented.
“We start by discerning the field disease from the invasive disease” with an initial round of field treatment and, if needed, adjunctive oral chemoprophylaxis. “We lather, rinse, and repeat” the field therapy, continuously if needed, Dr. Patel said.
“We like to do that because we can then identify those specific lesions we want to go after. No cryosurgery, no destructive therapy, because we run the risk of burying those tumors under the scar. They may recur and make it more difficult to accurately stage them in the future,” he noted.
“I like to be more sophisticated in thinking about our approach to the outcomes of these individual lesions,” he said. When it comes to excising lesions that have been biopsied and show invasive SCC, “disc excision may be a more cost-effective way to treat many low-risk SCCs,” he noted. In any case, “removal with clear surgical margins is key.”
Primary tumors with such low-risk attributes as diameter under a centimeter and thickness under 2 mm; well-defined borders; location on the trunk, neck, or extremities; well-differentiated histology; and lack of perineural invasion can all be considered for a disc technique, especially if the patient is immunocompetent without background chronic inflammation or a history of prior radiation therapy.
Staging SCCs, said Dr. Patel, is where things really get tricky. Older staging systems for SCC “led us to overtreat nonaggressive disease and undertreat aggressive disease. I think we have the responsibility to lead the charge to having a more sophisticated approach.” For example, patients whose tumors were staged T2 in the American Joint Commission on Cancer (AJCC) 7 classification system were most likely to have poor outcomes – in part because so few tumors were staged higher – which meant AJCC 7 didn’t provide adequate differentiation for useful risk prognostication.
A group of researchers at the Brigham and Women’s Hospital (BWH), Boston, “came up with a better system to better differentiate those T2 tumors into a high-risk and a low-risk subtype,” according to Dr. Patel.
With use of validated risk factors, the investigators applied a long list of risk factors to 2,000 tumors to see which risk factors, taken individually, were really contributing to poor outcomes. Eventually, four risk factors that made the most difference were identified: size greater than 2 cm, poor tumor differentiation, perineural invasion greater than 0.1 mm in diameter, and tumor invasion beyond subcutaneous fat. “I really want to highlight the size portion of those risk factors,” said Dr. Patel. “Something I’d like you to do in your clinical practice is to measure and document the size of the lesion. … That really, clearly helps” with risk prognostication.
These four factors were then used to break out a T2a stage for tumors with one risk factor and a T2b stage for tumors with two or three risk factors. Tumors with no risk factors are stage T1, and those with all four risk factors are stage T3. In situ SCC is T0.
Applying this new staging system to a 2,000-patient cohort with SCC yielded clear separation in outcomes including recurrence, nodal metastasis, disease-specific death, and overall survival between patients with the T2a and T2b tumors (P less than .001 for all; J Clin Oncol. 2014 Feb 1;32[4]:327-34).
While AJCC 8 is “significantly better” than AJCC 7 in its incorporation of meaningful risk factors into the SCC staging system, “it still underperforms in comparison” with the BWH staging system using the 2000 patient cohort, he said. Recent work has shown the BWH classification system to have superior specificity and positive predictive value in detecting nodal metastasis and disease-specific death in higher-grade tumors. But both BWH and AJCC 8 need further refinement.
“So what are the staging pearls to take home?” Dr. Patel asked. “First, utilize a staging system.” “Staging of SCC utilizing should be done routinely. Most data seems to suggest that the BWH system appears to outperform AJCC 8, and it is what we currently use routinely at GW,” he said.
Patients who are T1 by BWH criteria, with no risk factors, are at low or even no risk, he noted. He pointed out that of the nearly 1,400 patients who met T1 criteria, there were just eight local recurrences, one nodal metastasis, and no distant metastases or deaths. Knowing this should guide physicians on a treatment path that will reduce costs and provide patients with peace of mind, he said.
In the BWH schema, T2a patients fared almost as well, with a 2% risk of nodal metastasis and an overall 1% risk of disease-specific death. “T2a disease is low risk, in my mind. Most of these patients will go on to do well,” he said.
By contrast, “there may be a number of tumors that you are missing” that are candidates for close follow-up if the BWH criteria are not being used, said Dr. Patel. These are the T2b tumors. “For those patients, we want to aggressively follow them and think about a more aggressive management plan.”
The bottom line is that BWH T2b and T3 tumors are both high risk, and management needs to acknowledge this, he said. The current protocol in our cutaneous oncology program includes using routine radiologic nodal staging in patients with BWH stage 2b and above SCCs and considering sentinel lymph node biopsy for certain individuals.
For patients with BWH T2b and T3 tumors, dermatologists should give consideration to tertiary care or cancer center referrals so they have access to the full spectrum of diagnostic and therapeutic modalities and the opportunity to participate in clinical trials, Dr. Patel said.
Dr. Patel reported that he is a speaker for Regeneron/Sanofi and a cofounder of the Skin Cancer Outcomes (SCOUT) consortium.
This article was updated 2/9/2019
ORLANDO – When caring for individuals with sun-damaged skin, dermatologists need comfort with the full spectrum of photo-related skin disease. From assessment and treatment of actinic keratoses (AKs) and field cancerization, to long-term follow-up of cutaneous squamous cell carcinomas (SCCs), appropriate treatment and staging can improve patient quality of life and reduce health care costs, Vishal Patel, MD, said at the Orlando Dermatology Aesthetic and Clinical Conference.
said Dr. Patel, director of cutaneous oncology at George Washington University Cancer Center, Washington. On the other hand, he added, “field disease can be a marker for invasive squamous cell carcinoma risk, and it requires field treatment.” Treatment that reduces field disease is primary prevention because it decreases the formation of invasive SCC, he noted.
“But this level of disease – AKs and SCC in situ – doesn’t kill people,” he emphasized. “I want to leave you with an ability to stage this disease,” said Dr. Patel, noting that SCC mortality may eventually surpass melanoma mortality as deaths from the latter decline and numbers of older Americans with high ultraviolet light exposure and other risk factors climb.
While the majority of AKs regress within 5 years, he looks at the total burden of AKs as a marker for field cancerization “because having less than five in situ or actinic lesions puts you at less than a 1% risk of squamous cell carcinoma formation. Having more than 20 increases that risk 20-fold to 20%,” he said. “That’s the way we need to start thinking about this: Is this a disease – or a symptom?”
Rather than thinking of each AK or SCC in situ as a separate disease event, “the disease we need to be focusing on and treating is field cancerization,” he continued. Within this context, “we should not be thinking that … we need to be aggressive in our management,” which is what results in high costs.
“The reality is that this is a big quality of life issue for our patients. So what do we do?” Field treatment is appropriate for field disease, he said. Dr. Patel said that at GW only field treatment is used; destructive treatment for AKs and SCC in situ is not used. In the absence of patient and lesion characteristics that elevate risk,“surgery is really not the standard of care for in situ lesions for us,” he commented.
“We start by discerning the field disease from the invasive disease” with an initial round of field treatment and, if needed, adjunctive oral chemoprophylaxis. “We lather, rinse, and repeat” the field therapy, continuously if needed, Dr. Patel said.
“We like to do that because we can then identify those specific lesions we want to go after. No cryosurgery, no destructive therapy, because we run the risk of burying those tumors under the scar. They may recur and make it more difficult to accurately stage them in the future,” he noted.
“I like to be more sophisticated in thinking about our approach to the outcomes of these individual lesions,” he said. When it comes to excising lesions that have been biopsied and show invasive SCC, “disc excision may be a more cost-effective way to treat many low-risk SCCs,” he noted. In any case, “removal with clear surgical margins is key.”
Primary tumors with such low-risk attributes as diameter under a centimeter and thickness under 2 mm; well-defined borders; location on the trunk, neck, or extremities; well-differentiated histology; and lack of perineural invasion can all be considered for a disc technique, especially if the patient is immunocompetent without background chronic inflammation or a history of prior radiation therapy.
Staging SCCs, said Dr. Patel, is where things really get tricky. Older staging systems for SCC “led us to overtreat nonaggressive disease and undertreat aggressive disease. I think we have the responsibility to lead the charge to having a more sophisticated approach.” For example, patients whose tumors were staged T2 in the American Joint Commission on Cancer (AJCC) 7 classification system were most likely to have poor outcomes – in part because so few tumors were staged higher – which meant AJCC 7 didn’t provide adequate differentiation for useful risk prognostication.
A group of researchers at the Brigham and Women’s Hospital (BWH), Boston, “came up with a better system to better differentiate those T2 tumors into a high-risk and a low-risk subtype,” according to Dr. Patel.
With use of validated risk factors, the investigators applied a long list of risk factors to 2,000 tumors to see which risk factors, taken individually, were really contributing to poor outcomes. Eventually, four risk factors that made the most difference were identified: size greater than 2 cm, poor tumor differentiation, perineural invasion greater than 0.1 mm in diameter, and tumor invasion beyond subcutaneous fat. “I really want to highlight the size portion of those risk factors,” said Dr. Patel. “Something I’d like you to do in your clinical practice is to measure and document the size of the lesion. … That really, clearly helps” with risk prognostication.
These four factors were then used to break out a T2a stage for tumors with one risk factor and a T2b stage for tumors with two or three risk factors. Tumors with no risk factors are stage T1, and those with all four risk factors are stage T3. In situ SCC is T0.
Applying this new staging system to a 2,000-patient cohort with SCC yielded clear separation in outcomes including recurrence, nodal metastasis, disease-specific death, and overall survival between patients with the T2a and T2b tumors (P less than .001 for all; J Clin Oncol. 2014 Feb 1;32[4]:327-34).
While AJCC 8 is “significantly better” than AJCC 7 in its incorporation of meaningful risk factors into the SCC staging system, “it still underperforms in comparison” with the BWH staging system using the 2000 patient cohort, he said. Recent work has shown the BWH classification system to have superior specificity and positive predictive value in detecting nodal metastasis and disease-specific death in higher-grade tumors. But both BWH and AJCC 8 need further refinement.
“So what are the staging pearls to take home?” Dr. Patel asked. “First, utilize a staging system.” “Staging of SCC utilizing should be done routinely. Most data seems to suggest that the BWH system appears to outperform AJCC 8, and it is what we currently use routinely at GW,” he said.
Patients who are T1 by BWH criteria, with no risk factors, are at low or even no risk, he noted. He pointed out that of the nearly 1,400 patients who met T1 criteria, there were just eight local recurrences, one nodal metastasis, and no distant metastases or deaths. Knowing this should guide physicians on a treatment path that will reduce costs and provide patients with peace of mind, he said.
In the BWH schema, T2a patients fared almost as well, with a 2% risk of nodal metastasis and an overall 1% risk of disease-specific death. “T2a disease is low risk, in my mind. Most of these patients will go on to do well,” he said.
By contrast, “there may be a number of tumors that you are missing” that are candidates for close follow-up if the BWH criteria are not being used, said Dr. Patel. These are the T2b tumors. “For those patients, we want to aggressively follow them and think about a more aggressive management plan.”
The bottom line is that BWH T2b and T3 tumors are both high risk, and management needs to acknowledge this, he said. The current protocol in our cutaneous oncology program includes using routine radiologic nodal staging in patients with BWH stage 2b and above SCCs and considering sentinel lymph node biopsy for certain individuals.
For patients with BWH T2b and T3 tumors, dermatologists should give consideration to tertiary care or cancer center referrals so they have access to the full spectrum of diagnostic and therapeutic modalities and the opportunity to participate in clinical trials, Dr. Patel said.
Dr. Patel reported that he is a speaker for Regeneron/Sanofi and a cofounder of the Skin Cancer Outcomes (SCOUT) consortium.
This article was updated 2/9/2019
EXPERT ANALYSIS FROM ODAC 2019
Years in practice, burnout risk linked in otolaryngology
CORONADO, CALIF. – Otolaryngologists and otolaryngology nurse practitioners at the Cleveland Clinic who have been practicing for 6-10 years are at the highest risk for burnout, while those who have been practicing for more than 10 are at the lowest risk.
The finding comes from a cross-sectional survey published in Otolaryngology–Head and Neck Surgery designed to evaluate the presence of burnout among 52 otolaryngology clinicians and to compare results among faculty, trainees, and advanced practice practitioners.
“Other studies have shown that work-life balance can contribute to burnout symptoms, including low spouse support, having young children at home, and a decreased satisfaction with work-life balance,” Michael S. Benninger, MD, said at the Triological Society’s Combined Sections Meeting. “We wanted to know if there was difference within our group among people at different points in their career.”
In a study led by Katie Geelan-Hansen, MD, Dr. Benninger, who chairs the Head and Neck Institute at the Cleveland Clinic, and his colleagues administered the Maslach Burnout Inventory (MBI) and questions regarding work stressors specific to that department to 52 employees (Otolaryngol Head Neck Surg. 2018;159[2]:254-7). The questions focused on domains of emotional exhaustion, depersonalization, and a sense of personal accomplishment.
Of the 52 surveys distributed, 42 participants (85%) completed the survey. The researchers found that respondents who had worked for 6-10 years had higher MBI scores on emotional exhaustion, compared with their peers who had worked for 5 years or fewer, and those who had worked for more than 10 years (18.18, compared with 15.78 and 14.68, respectively; P = .63). A similar association was observed for MBI scores on depersonalization (15.14, compared with 14.72 and 9.68; P = .07). MBI scores on personal accomplishment were similar between the two groups (39, compared with 38.33 and 40.84; P = .5).
“People who are more mature in their practice tend to have less burnout,” Dr. Benninger said. “That may be because they’ve found a place of homeostasis. They’ve figured out how to maximize their efficiency, and they may have more support.
“The people who tend to be the biggest concern are those 6 -10 years into the field. I recommend that you focus on that group. It’s a transitional time in their careers. It’s a time when there’s some insecurity; they’re being asked to do a lot more.” It remains unclear if male or female respondents had a higher level of burnout, he added, although other surveys have suggested that female physicians have a higher level of burnout, compared with male physicians.
“Our overall evaluation of burnout was lower than what you see from national statistics,” Dr. Benninger said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “We have had a wellness officer [at Cleveland Clinic] for a long time. We have a group of people on our clinic’s board of governors who any staff can go to in order to vent issues on a private basis. All of those things help, but I am seeing an escalating unsatisfaction with the workload and the work environment. We’re looking at other things. Expectation setting and rewarding people are also important.”
He reported having no relevant financial disclosures.
SOURCE: Benninger MS et al. Triological CSM, Abstracts.
CORONADO, CALIF. – Otolaryngologists and otolaryngology nurse practitioners at the Cleveland Clinic who have been practicing for 6-10 years are at the highest risk for burnout, while those who have been practicing for more than 10 are at the lowest risk.
The finding comes from a cross-sectional survey published in Otolaryngology–Head and Neck Surgery designed to evaluate the presence of burnout among 52 otolaryngology clinicians and to compare results among faculty, trainees, and advanced practice practitioners.
“Other studies have shown that work-life balance can contribute to burnout symptoms, including low spouse support, having young children at home, and a decreased satisfaction with work-life balance,” Michael S. Benninger, MD, said at the Triological Society’s Combined Sections Meeting. “We wanted to know if there was difference within our group among people at different points in their career.”
In a study led by Katie Geelan-Hansen, MD, Dr. Benninger, who chairs the Head and Neck Institute at the Cleveland Clinic, and his colleagues administered the Maslach Burnout Inventory (MBI) and questions regarding work stressors specific to that department to 52 employees (Otolaryngol Head Neck Surg. 2018;159[2]:254-7). The questions focused on domains of emotional exhaustion, depersonalization, and a sense of personal accomplishment.
Of the 52 surveys distributed, 42 participants (85%) completed the survey. The researchers found that respondents who had worked for 6-10 years had higher MBI scores on emotional exhaustion, compared with their peers who had worked for 5 years or fewer, and those who had worked for more than 10 years (18.18, compared with 15.78 and 14.68, respectively; P = .63). A similar association was observed for MBI scores on depersonalization (15.14, compared with 14.72 and 9.68; P = .07). MBI scores on personal accomplishment were similar between the two groups (39, compared with 38.33 and 40.84; P = .5).
“People who are more mature in their practice tend to have less burnout,” Dr. Benninger said. “That may be because they’ve found a place of homeostasis. They’ve figured out how to maximize their efficiency, and they may have more support.
“The people who tend to be the biggest concern are those 6 -10 years into the field. I recommend that you focus on that group. It’s a transitional time in their careers. It’s a time when there’s some insecurity; they’re being asked to do a lot more.” It remains unclear if male or female respondents had a higher level of burnout, he added, although other surveys have suggested that female physicians have a higher level of burnout, compared with male physicians.
“Our overall evaluation of burnout was lower than what you see from national statistics,” Dr. Benninger said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “We have had a wellness officer [at Cleveland Clinic] for a long time. We have a group of people on our clinic’s board of governors who any staff can go to in order to vent issues on a private basis. All of those things help, but I am seeing an escalating unsatisfaction with the workload and the work environment. We’re looking at other things. Expectation setting and rewarding people are also important.”
He reported having no relevant financial disclosures.
SOURCE: Benninger MS et al. Triological CSM, Abstracts.
CORONADO, CALIF. – Otolaryngologists and otolaryngology nurse practitioners at the Cleveland Clinic who have been practicing for 6-10 years are at the highest risk for burnout, while those who have been practicing for more than 10 are at the lowest risk.
The finding comes from a cross-sectional survey published in Otolaryngology–Head and Neck Surgery designed to evaluate the presence of burnout among 52 otolaryngology clinicians and to compare results among faculty, trainees, and advanced practice practitioners.
“Other studies have shown that work-life balance can contribute to burnout symptoms, including low spouse support, having young children at home, and a decreased satisfaction with work-life balance,” Michael S. Benninger, MD, said at the Triological Society’s Combined Sections Meeting. “We wanted to know if there was difference within our group among people at different points in their career.”
In a study led by Katie Geelan-Hansen, MD, Dr. Benninger, who chairs the Head and Neck Institute at the Cleveland Clinic, and his colleagues administered the Maslach Burnout Inventory (MBI) and questions regarding work stressors specific to that department to 52 employees (Otolaryngol Head Neck Surg. 2018;159[2]:254-7). The questions focused on domains of emotional exhaustion, depersonalization, and a sense of personal accomplishment.
Of the 52 surveys distributed, 42 participants (85%) completed the survey. The researchers found that respondents who had worked for 6-10 years had higher MBI scores on emotional exhaustion, compared with their peers who had worked for 5 years or fewer, and those who had worked for more than 10 years (18.18, compared with 15.78 and 14.68, respectively; P = .63). A similar association was observed for MBI scores on depersonalization (15.14, compared with 14.72 and 9.68; P = .07). MBI scores on personal accomplishment were similar between the two groups (39, compared with 38.33 and 40.84; P = .5).
“People who are more mature in their practice tend to have less burnout,” Dr. Benninger said. “That may be because they’ve found a place of homeostasis. They’ve figured out how to maximize their efficiency, and they may have more support.
“The people who tend to be the biggest concern are those 6 -10 years into the field. I recommend that you focus on that group. It’s a transitional time in their careers. It’s a time when there’s some insecurity; they’re being asked to do a lot more.” It remains unclear if male or female respondents had a higher level of burnout, he added, although other surveys have suggested that female physicians have a higher level of burnout, compared with male physicians.
“Our overall evaluation of burnout was lower than what you see from national statistics,” Dr. Benninger said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “We have had a wellness officer [at Cleveland Clinic] for a long time. We have a group of people on our clinic’s board of governors who any staff can go to in order to vent issues on a private basis. All of those things help, but I am seeing an escalating unsatisfaction with the workload and the work environment. We’re looking at other things. Expectation setting and rewarding people are also important.”
He reported having no relevant financial disclosures.
SOURCE: Benninger MS et al. Triological CSM, Abstracts.
REPORTING FROM TRIOLOGICAL CSM
Eltrombopag ‘cannot be recommended’ during AML induction
The thrombopoietic agent eltrombopag (Promacta) did more harm than good when given to adults with acute myeloid leukemia (AML) during standard induction chemotherapy, results of a randomized phase 2 trial show.
Patients who were randomly assigned to receive standard induction chemotherapy with daunorubicin and cytarabine plus eltrombopag had a higher incidence of serious adverse events and death from hemorrhage within 30 days of the last eltrombopag dose, compared with patients who received chemotherapy and placebo, reported Noelle Frey, MD, from the University of Pennsylvania in Philadelphia, and colleagues.
“Overall survival was also numerically longer in the placebo group, compared with the eltrombopag group. It remains unclear why there were more deaths, particularly due to hemorrhage within 30 days after the last dose of treatment, in the eltrombopag group,” they wrote in the Lancet Haematology.
The investigators had expected better results, based on eltrombopag’s demonstrated efficacy against thrombocytopenia (a common feature of AML, exacerbated by chemotherapy), and because of evidence suggesting that the thrombopoietin-receptor agonist might also have antileukemic properties.
They set out to test the safety, tolerability, and efficacy of eltrombopag added to standard induction therapy in patients with treatment-naive AML of any subtype except M3 (acute promyelocytic leukemia) or M7 (acute megakaryocytic leukemia).
Patients received chemotherapy with daunorubicin in a bolus intravenous infusion at a dose of 90 mg/m2 on days 1-3 for patients 18-60 years of age, or 60 mg/m2 for patients older than 60 years, plus cytarabine continuous intravenous infusion at a dose of 100 mg/m2 on days 1-7. The 148 patients were randomized in groups of 74 each to receive either eltrombopag 200 mg (100 mg for patients of east Asian heritage) or placebo, once daily.
Eltrombopag was continued until platelet counts were 200 × 109/L or higher, remission, or 42 days after the start of induction chemotherapy.
Grade 3 or 4 adverse events occurring in 10% or more of patients – a primary endpoint – were febrile neutropenia, which occurred in 42% of patients receiving eltrombopag, compared with 39% receiving placebo, decreased white blood cell count in 11% vs. 7%, and hypophosphatemia in 4% and 13%, respectively,
Serious adverse events occurred in 34% of patients on eltrombopag, compared with 20% on placebo. Similarly, 53% of patients receiving eltrombopag died, compared with 41% of patients receiving the placebo.
Most of the deaths were attributable to AML, including 19 patients (26%) on eltrombopag and 10 (14%) on placebo. Eleven patients on eltrombopag and four on placebo died within 30 days of the last dose of study treatment.
Hemorrhage accounted for the deaths of five patients on eltrombopag and three on placebo, and sepsis accounted for the deaths of five and six patients, respectively.
Both the incidence of thromboembolic events and mean change in left ventricular ejection fraction were similar between the groups.
Median overall survival was 15.4 months in the eltrombopag group vs. 25.7 months in the placebo group, although this difference was not statistically significant, likely because of the sample size.
The investigators were at a loss to explain why the eltrombopag-treated patients had numerically worse outcomes.
“In the present study, eltrombopag did not improve the time to platelet recovery or the incidences of grade 3-4 thrombocytopenia, neutropenia, or anemia, compared with placebo. Furthermore, the study did not reveal any differences in investigator-assessed response to treatment. These findings were unexpected given outcomes from previous studies of eltrombopag monotherapy in patients with myelodysplastic syndromes or acute myeloid leukemia,” they wrote.
Although the reasons behind the findings are unclear, “the data from this trial do not support a favorable benefit-risk profile for eltrombopag in combination with induction chemotherapy in patients with acute myeloid leukemia,” the investigators wrote.
The study was funded by Novartis. Dr. Frey reported nonfinancial support from Novartis during the conduct of the study and consultancy fees from Novartis outside of the submitted work. Multiple coauthors reported similar relationships with Novartis and/or other companies.
SOURCE: Frey N et al. Lancet Haematol. 2019 Jan 28. doi: 10.1016/S2352-3026(18)30231-X.
The thrombopoietic agent eltrombopag (Promacta) did more harm than good when given to adults with acute myeloid leukemia (AML) during standard induction chemotherapy, results of a randomized phase 2 trial show.
Patients who were randomly assigned to receive standard induction chemotherapy with daunorubicin and cytarabine plus eltrombopag had a higher incidence of serious adverse events and death from hemorrhage within 30 days of the last eltrombopag dose, compared with patients who received chemotherapy and placebo, reported Noelle Frey, MD, from the University of Pennsylvania in Philadelphia, and colleagues.
“Overall survival was also numerically longer in the placebo group, compared with the eltrombopag group. It remains unclear why there were more deaths, particularly due to hemorrhage within 30 days after the last dose of treatment, in the eltrombopag group,” they wrote in the Lancet Haematology.
The investigators had expected better results, based on eltrombopag’s demonstrated efficacy against thrombocytopenia (a common feature of AML, exacerbated by chemotherapy), and because of evidence suggesting that the thrombopoietin-receptor agonist might also have antileukemic properties.
They set out to test the safety, tolerability, and efficacy of eltrombopag added to standard induction therapy in patients with treatment-naive AML of any subtype except M3 (acute promyelocytic leukemia) or M7 (acute megakaryocytic leukemia).
Patients received chemotherapy with daunorubicin in a bolus intravenous infusion at a dose of 90 mg/m2 on days 1-3 for patients 18-60 years of age, or 60 mg/m2 for patients older than 60 years, plus cytarabine continuous intravenous infusion at a dose of 100 mg/m2 on days 1-7. The 148 patients were randomized in groups of 74 each to receive either eltrombopag 200 mg (100 mg for patients of east Asian heritage) or placebo, once daily.
Eltrombopag was continued until platelet counts were 200 × 109/L or higher, remission, or 42 days after the start of induction chemotherapy.
Grade 3 or 4 adverse events occurring in 10% or more of patients – a primary endpoint – were febrile neutropenia, which occurred in 42% of patients receiving eltrombopag, compared with 39% receiving placebo, decreased white blood cell count in 11% vs. 7%, and hypophosphatemia in 4% and 13%, respectively,
Serious adverse events occurred in 34% of patients on eltrombopag, compared with 20% on placebo. Similarly, 53% of patients receiving eltrombopag died, compared with 41% of patients receiving the placebo.
Most of the deaths were attributable to AML, including 19 patients (26%) on eltrombopag and 10 (14%) on placebo. Eleven patients on eltrombopag and four on placebo died within 30 days of the last dose of study treatment.
Hemorrhage accounted for the deaths of five patients on eltrombopag and three on placebo, and sepsis accounted for the deaths of five and six patients, respectively.
Both the incidence of thromboembolic events and mean change in left ventricular ejection fraction were similar between the groups.
Median overall survival was 15.4 months in the eltrombopag group vs. 25.7 months in the placebo group, although this difference was not statistically significant, likely because of the sample size.
The investigators were at a loss to explain why the eltrombopag-treated patients had numerically worse outcomes.
“In the present study, eltrombopag did not improve the time to platelet recovery or the incidences of grade 3-4 thrombocytopenia, neutropenia, or anemia, compared with placebo. Furthermore, the study did not reveal any differences in investigator-assessed response to treatment. These findings were unexpected given outcomes from previous studies of eltrombopag monotherapy in patients with myelodysplastic syndromes or acute myeloid leukemia,” they wrote.
Although the reasons behind the findings are unclear, “the data from this trial do not support a favorable benefit-risk profile for eltrombopag in combination with induction chemotherapy in patients with acute myeloid leukemia,” the investigators wrote.
The study was funded by Novartis. Dr. Frey reported nonfinancial support from Novartis during the conduct of the study and consultancy fees from Novartis outside of the submitted work. Multiple coauthors reported similar relationships with Novartis and/or other companies.
SOURCE: Frey N et al. Lancet Haematol. 2019 Jan 28. doi: 10.1016/S2352-3026(18)30231-X.
The thrombopoietic agent eltrombopag (Promacta) did more harm than good when given to adults with acute myeloid leukemia (AML) during standard induction chemotherapy, results of a randomized phase 2 trial show.
Patients who were randomly assigned to receive standard induction chemotherapy with daunorubicin and cytarabine plus eltrombopag had a higher incidence of serious adverse events and death from hemorrhage within 30 days of the last eltrombopag dose, compared with patients who received chemotherapy and placebo, reported Noelle Frey, MD, from the University of Pennsylvania in Philadelphia, and colleagues.
“Overall survival was also numerically longer in the placebo group, compared with the eltrombopag group. It remains unclear why there were more deaths, particularly due to hemorrhage within 30 days after the last dose of treatment, in the eltrombopag group,” they wrote in the Lancet Haematology.
The investigators had expected better results, based on eltrombopag’s demonstrated efficacy against thrombocytopenia (a common feature of AML, exacerbated by chemotherapy), and because of evidence suggesting that the thrombopoietin-receptor agonist might also have antileukemic properties.
They set out to test the safety, tolerability, and efficacy of eltrombopag added to standard induction therapy in patients with treatment-naive AML of any subtype except M3 (acute promyelocytic leukemia) or M7 (acute megakaryocytic leukemia).
Patients received chemotherapy with daunorubicin in a bolus intravenous infusion at a dose of 90 mg/m2 on days 1-3 for patients 18-60 years of age, or 60 mg/m2 for patients older than 60 years, plus cytarabine continuous intravenous infusion at a dose of 100 mg/m2 on days 1-7. The 148 patients were randomized in groups of 74 each to receive either eltrombopag 200 mg (100 mg for patients of east Asian heritage) or placebo, once daily.
Eltrombopag was continued until platelet counts were 200 × 109/L or higher, remission, or 42 days after the start of induction chemotherapy.
Grade 3 or 4 adverse events occurring in 10% or more of patients – a primary endpoint – were febrile neutropenia, which occurred in 42% of patients receiving eltrombopag, compared with 39% receiving placebo, decreased white blood cell count in 11% vs. 7%, and hypophosphatemia in 4% and 13%, respectively,
Serious adverse events occurred in 34% of patients on eltrombopag, compared with 20% on placebo. Similarly, 53% of patients receiving eltrombopag died, compared with 41% of patients receiving the placebo.
Most of the deaths were attributable to AML, including 19 patients (26%) on eltrombopag and 10 (14%) on placebo. Eleven patients on eltrombopag and four on placebo died within 30 days of the last dose of study treatment.
Hemorrhage accounted for the deaths of five patients on eltrombopag and three on placebo, and sepsis accounted for the deaths of five and six patients, respectively.
Both the incidence of thromboembolic events and mean change in left ventricular ejection fraction were similar between the groups.
Median overall survival was 15.4 months in the eltrombopag group vs. 25.7 months in the placebo group, although this difference was not statistically significant, likely because of the sample size.
The investigators were at a loss to explain why the eltrombopag-treated patients had numerically worse outcomes.
“In the present study, eltrombopag did not improve the time to platelet recovery or the incidences of grade 3-4 thrombocytopenia, neutropenia, or anemia, compared with placebo. Furthermore, the study did not reveal any differences in investigator-assessed response to treatment. These findings were unexpected given outcomes from previous studies of eltrombopag monotherapy in patients with myelodysplastic syndromes or acute myeloid leukemia,” they wrote.
Although the reasons behind the findings are unclear, “the data from this trial do not support a favorable benefit-risk profile for eltrombopag in combination with induction chemotherapy in patients with acute myeloid leukemia,” the investigators wrote.
The study was funded by Novartis. Dr. Frey reported nonfinancial support from Novartis during the conduct of the study and consultancy fees from Novartis outside of the submitted work. Multiple coauthors reported similar relationships with Novartis and/or other companies.
SOURCE: Frey N et al. Lancet Haematol. 2019 Jan 28. doi: 10.1016/S2352-3026(18)30231-X.
FROM LANCET HAEMATOLOGY
Key clinical point:
Major finding: Overall survival was shorter for patients assigned to eltrombopag than placebo, at 15.4 months versus 25.7 months. The difference was not statistically significant.
Study details: Randomized phase 2 trial in 148 adults with treatment-naive acute myeloid leukemia.
Disclosures: The study was funded by Novartis. Dr. Frey reported nonfinancial support from Novartis during the conduct of the study and consultancy fees from Novartis outside of the submitted work. Multiple coauthors reported similar relationships with Novartis and other companies.
Source: Frey N et al. Lancet Haematol. 2019 Jan 28. doi: 10.1016/S2352-3026(18)30231-X.
Most U.S. tPA-eligible stroke patients now get treated within an hour
HONOLULU – The speed at which eligible U.S. patients with acute ischemic stroke receive thrombolytic therapy has surged in recent years, and .
By the second half of last year, 75% of acute ischemic stroke patients treated at any of the 913 U.S. hospitals in the Get With The Guidelines-Stroke program received intravenous tissue plasminogen activator (tPA; Alteplase) within 60 minutes of their hospital arrival (their door-to-needle time (DTN), and 52% received tPA with a DTN time of 45 minutes or less. These levels met the treatment-speed goals set by the second phase of the Target: Stroke program, which called for delivering tPA to 75% of appropriate stroke patients within a DTN time of 60 minutes, and within 45 minutes in at least 50% of patients, Gregg C. Fonarow, MD, and his associates reported at the International Stroke Conference, sponsored by the American Heart Association.
The analyses they reported also documented how these most recent gains in thrombolytic speed played out in improved patient outcomes. During phase 2 of Target: Stroke, which ran from January 2014 to September 2018, 85,078 U.S. patients received tPA at one of the participating hospitals. During those 4 years, the rate of in-hospital mortality was 6.0%, half the patients were discharged home, 53% could ambulate independently, and the rate of intracerebral hemorrhage (ICH) was 3.5%. The researchers compared these clinical event rates with the rates from 24,603 tPA-treated patients during 2003-2009, before the Target: Stroke campaign began. After adjustment for many potential confounders, the more recently treated cohort had a 31% relative risk reduction in in-hospital mortality, a 43% relative increase in being discharged home, a 40% relative increase in independent ambulation, and a 32% relative risk reduction in the rate of symptomatic ICH. All these between-group differences were statistically significant.
“We were hoping that, by improving DTN times we could achieve improved outcomes, but often in quality-improvement research – even when the process of care improves – the gains in outcomes don’t necessarily match expectations. Fortunately, with Target: Stroke, the remarkable improvements in timely treatment translated to remarkable improvements in clinical outcomes,” Dr. Fonarow said in an interview. “These are substantial, clinically relevant improvements in clinical outcomes for patients with acute ischemic stroke. As a result of the program, more than 100,000 acute ischemic stroke patients received much more timely acute ischemic stroke care and achieved far better clinical outcomes.”
During the 2003-2018 period reviewed, the percentage of presenting acute ischemic stroke patients who received tPA treatment at the 913 Get With The Guidelines hospitals that participated in the Target: Stroke program (and so had reviewable data) throughout all three periods rose from 6% during 2003-2009 (prestudy) to 8% during 2010-2013 (phase 1), and to 12% during 2014-2018 (phase 2). The percentages of these patients who received the drug within 60 minutes were 27% during 2003-2009, 43% during 2010-2013, and 68% during the entire 2014-2018 period, culminating in the 75% rate during July-September 2018, reported Dr. Fonarow, professor of medicine and cochief of cardiology at the University of California, Los Angeles.
Dr. Fonarow attributed the drop in the rate of ICH – from 5.7% during 2003-2009, to 4.4% during 2010-2013, and down to 3.5% during 2014-2018 – to the faster delivery of tPA. “With faster treatment, there is less ischemic brain and vascular damage and thus a lower likelihood of ICH as a complication of tPA,” he explained.
The Target: Stroke program achieved these gains in speedier thrombolytic treatment (and better recognition of eligible patients) through educational and promotional activities including dissemination of best practices. Notable best practices have included EMS prenotification of hospitals before they arrive with a stroke patient, direct transport of patients to a brain imaging scanner, premix of tPA, initiation of tPA in the brain imaging suite, and prompt data feedback, Dr. Fonarow said.
The Get With The Guidelines-Stroke and Target: Stroke programs now involve more than 2,100 U.S. hospitals, and they are able to deliver emergency care to roughly 70% of U.S. acute ischemic stroke patients, he noted.
With achievement of Target: Stroke’s phase 2 goals, the program announced its launch of a third phase, with new treatment goals: Initiation of thrombolytic treatment to 85% of eligible patients within 60 minutes, to 75% within 45 minutes, and to 50% within 30 minutes. The phase 3 Target: Stroke program also for the first time includes treatment goals for delivery of endovascular thrombectomy treatment.
SOURCE: Fonarow GC et al. ISC 2019, Abstract LBP9.
The Target: Stroke and Get With The Guidelines-Stroke programs should be commended for the very impressive achievements they have made in improved delivery of thrombolytic therapy to acute ischemic stroke patients. What’s happened over the past decade in the speed of delivery of tissue plasminogen activator for treating U.S. stroke patients has been a real success story.
Programs like Get With The Guidelines and Target: Stroke have proven their value, but a significant barrier remains to bringing this program to all U.S. stroke patients and to all U.S. hospitals that treat stroke patients. That barrier is resources. Participating hospitals need to meet certain data-collection standards, but some U.S. hospitals do not have the resources to do this.
Bruce Ovbiagele, MD , is a neurologist and chief of staff for the San Francisco Veterans Affairs Health Care System. He had no disclosures. He made these comments in an interview.
The Target: Stroke and Get With The Guidelines-Stroke programs should be commended for the very impressive achievements they have made in improved delivery of thrombolytic therapy to acute ischemic stroke patients. What’s happened over the past decade in the speed of delivery of tissue plasminogen activator for treating U.S. stroke patients has been a real success story.
Programs like Get With The Guidelines and Target: Stroke have proven their value, but a significant barrier remains to bringing this program to all U.S. stroke patients and to all U.S. hospitals that treat stroke patients. That barrier is resources. Participating hospitals need to meet certain data-collection standards, but some U.S. hospitals do not have the resources to do this.
Bruce Ovbiagele, MD , is a neurologist and chief of staff for the San Francisco Veterans Affairs Health Care System. He had no disclosures. He made these comments in an interview.
The Target: Stroke and Get With The Guidelines-Stroke programs should be commended for the very impressive achievements they have made in improved delivery of thrombolytic therapy to acute ischemic stroke patients. What’s happened over the past decade in the speed of delivery of tissue plasminogen activator for treating U.S. stroke patients has been a real success story.
Programs like Get With The Guidelines and Target: Stroke have proven their value, but a significant barrier remains to bringing this program to all U.S. stroke patients and to all U.S. hospitals that treat stroke patients. That barrier is resources. Participating hospitals need to meet certain data-collection standards, but some U.S. hospitals do not have the resources to do this.
Bruce Ovbiagele, MD , is a neurologist and chief of staff for the San Francisco Veterans Affairs Health Care System. He had no disclosures. He made these comments in an interview.
HONOLULU – The speed at which eligible U.S. patients with acute ischemic stroke receive thrombolytic therapy has surged in recent years, and .
By the second half of last year, 75% of acute ischemic stroke patients treated at any of the 913 U.S. hospitals in the Get With The Guidelines-Stroke program received intravenous tissue plasminogen activator (tPA; Alteplase) within 60 minutes of their hospital arrival (their door-to-needle time (DTN), and 52% received tPA with a DTN time of 45 minutes or less. These levels met the treatment-speed goals set by the second phase of the Target: Stroke program, which called for delivering tPA to 75% of appropriate stroke patients within a DTN time of 60 minutes, and within 45 minutes in at least 50% of patients, Gregg C. Fonarow, MD, and his associates reported at the International Stroke Conference, sponsored by the American Heart Association.
The analyses they reported also documented how these most recent gains in thrombolytic speed played out in improved patient outcomes. During phase 2 of Target: Stroke, which ran from January 2014 to September 2018, 85,078 U.S. patients received tPA at one of the participating hospitals. During those 4 years, the rate of in-hospital mortality was 6.0%, half the patients were discharged home, 53% could ambulate independently, and the rate of intracerebral hemorrhage (ICH) was 3.5%. The researchers compared these clinical event rates with the rates from 24,603 tPA-treated patients during 2003-2009, before the Target: Stroke campaign began. After adjustment for many potential confounders, the more recently treated cohort had a 31% relative risk reduction in in-hospital mortality, a 43% relative increase in being discharged home, a 40% relative increase in independent ambulation, and a 32% relative risk reduction in the rate of symptomatic ICH. All these between-group differences were statistically significant.
“We were hoping that, by improving DTN times we could achieve improved outcomes, but often in quality-improvement research – even when the process of care improves – the gains in outcomes don’t necessarily match expectations. Fortunately, with Target: Stroke, the remarkable improvements in timely treatment translated to remarkable improvements in clinical outcomes,” Dr. Fonarow said in an interview. “These are substantial, clinically relevant improvements in clinical outcomes for patients with acute ischemic stroke. As a result of the program, more than 100,000 acute ischemic stroke patients received much more timely acute ischemic stroke care and achieved far better clinical outcomes.”
During the 2003-2018 period reviewed, the percentage of presenting acute ischemic stroke patients who received tPA treatment at the 913 Get With The Guidelines hospitals that participated in the Target: Stroke program (and so had reviewable data) throughout all three periods rose from 6% during 2003-2009 (prestudy) to 8% during 2010-2013 (phase 1), and to 12% during 2014-2018 (phase 2). The percentages of these patients who received the drug within 60 minutes were 27% during 2003-2009, 43% during 2010-2013, and 68% during the entire 2014-2018 period, culminating in the 75% rate during July-September 2018, reported Dr. Fonarow, professor of medicine and cochief of cardiology at the University of California, Los Angeles.
Dr. Fonarow attributed the drop in the rate of ICH – from 5.7% during 2003-2009, to 4.4% during 2010-2013, and down to 3.5% during 2014-2018 – to the faster delivery of tPA. “With faster treatment, there is less ischemic brain and vascular damage and thus a lower likelihood of ICH as a complication of tPA,” he explained.
The Target: Stroke program achieved these gains in speedier thrombolytic treatment (and better recognition of eligible patients) through educational and promotional activities including dissemination of best practices. Notable best practices have included EMS prenotification of hospitals before they arrive with a stroke patient, direct transport of patients to a brain imaging scanner, premix of tPA, initiation of tPA in the brain imaging suite, and prompt data feedback, Dr. Fonarow said.
The Get With The Guidelines-Stroke and Target: Stroke programs now involve more than 2,100 U.S. hospitals, and they are able to deliver emergency care to roughly 70% of U.S. acute ischemic stroke patients, he noted.
With achievement of Target: Stroke’s phase 2 goals, the program announced its launch of a third phase, with new treatment goals: Initiation of thrombolytic treatment to 85% of eligible patients within 60 minutes, to 75% within 45 minutes, and to 50% within 30 minutes. The phase 3 Target: Stroke program also for the first time includes treatment goals for delivery of endovascular thrombectomy treatment.
SOURCE: Fonarow GC et al. ISC 2019, Abstract LBP9.
HONOLULU – The speed at which eligible U.S. patients with acute ischemic stroke receive thrombolytic therapy has surged in recent years, and .
By the second half of last year, 75% of acute ischemic stroke patients treated at any of the 913 U.S. hospitals in the Get With The Guidelines-Stroke program received intravenous tissue plasminogen activator (tPA; Alteplase) within 60 minutes of their hospital arrival (their door-to-needle time (DTN), and 52% received tPA with a DTN time of 45 minutes or less. These levels met the treatment-speed goals set by the second phase of the Target: Stroke program, which called for delivering tPA to 75% of appropriate stroke patients within a DTN time of 60 minutes, and within 45 minutes in at least 50% of patients, Gregg C. Fonarow, MD, and his associates reported at the International Stroke Conference, sponsored by the American Heart Association.
The analyses they reported also documented how these most recent gains in thrombolytic speed played out in improved patient outcomes. During phase 2 of Target: Stroke, which ran from January 2014 to September 2018, 85,078 U.S. patients received tPA at one of the participating hospitals. During those 4 years, the rate of in-hospital mortality was 6.0%, half the patients were discharged home, 53% could ambulate independently, and the rate of intracerebral hemorrhage (ICH) was 3.5%. The researchers compared these clinical event rates with the rates from 24,603 tPA-treated patients during 2003-2009, before the Target: Stroke campaign began. After adjustment for many potential confounders, the more recently treated cohort had a 31% relative risk reduction in in-hospital mortality, a 43% relative increase in being discharged home, a 40% relative increase in independent ambulation, and a 32% relative risk reduction in the rate of symptomatic ICH. All these between-group differences were statistically significant.
“We were hoping that, by improving DTN times we could achieve improved outcomes, but often in quality-improvement research – even when the process of care improves – the gains in outcomes don’t necessarily match expectations. Fortunately, with Target: Stroke, the remarkable improvements in timely treatment translated to remarkable improvements in clinical outcomes,” Dr. Fonarow said in an interview. “These are substantial, clinically relevant improvements in clinical outcomes for patients with acute ischemic stroke. As a result of the program, more than 100,000 acute ischemic stroke patients received much more timely acute ischemic stroke care and achieved far better clinical outcomes.”
During the 2003-2018 period reviewed, the percentage of presenting acute ischemic stroke patients who received tPA treatment at the 913 Get With The Guidelines hospitals that participated in the Target: Stroke program (and so had reviewable data) throughout all three periods rose from 6% during 2003-2009 (prestudy) to 8% during 2010-2013 (phase 1), and to 12% during 2014-2018 (phase 2). The percentages of these patients who received the drug within 60 minutes were 27% during 2003-2009, 43% during 2010-2013, and 68% during the entire 2014-2018 period, culminating in the 75% rate during July-September 2018, reported Dr. Fonarow, professor of medicine and cochief of cardiology at the University of California, Los Angeles.
Dr. Fonarow attributed the drop in the rate of ICH – from 5.7% during 2003-2009, to 4.4% during 2010-2013, and down to 3.5% during 2014-2018 – to the faster delivery of tPA. “With faster treatment, there is less ischemic brain and vascular damage and thus a lower likelihood of ICH as a complication of tPA,” he explained.
The Target: Stroke program achieved these gains in speedier thrombolytic treatment (and better recognition of eligible patients) through educational and promotional activities including dissemination of best practices. Notable best practices have included EMS prenotification of hospitals before they arrive with a stroke patient, direct transport of patients to a brain imaging scanner, premix of tPA, initiation of tPA in the brain imaging suite, and prompt data feedback, Dr. Fonarow said.
The Get With The Guidelines-Stroke and Target: Stroke programs now involve more than 2,100 U.S. hospitals, and they are able to deliver emergency care to roughly 70% of U.S. acute ischemic stroke patients, he noted.
With achievement of Target: Stroke’s phase 2 goals, the program announced its launch of a third phase, with new treatment goals: Initiation of thrombolytic treatment to 85% of eligible patients within 60 minutes, to 75% within 45 minutes, and to 50% within 30 minutes. The phase 3 Target: Stroke program also for the first time includes treatment goals for delivery of endovascular thrombectomy treatment.
SOURCE: Fonarow GC et al. ISC 2019, Abstract LBP9.
REPORTING FROM ISC 2019
Key clinical point: In late 2018, the Target: Stroke program met its phase 2 goal for timely delivery of thrombolytic therapy to acute ischemic stroke patients.
Major finding: In September 2018, 75% of eligible stroke patients underwent thrombolysis within 60 minutes of hospital arrival, and 52% within 45 minutes.
Study details: Review of data collected from 154,221 U.S. stroke patients treated with thrombolysis during 2003-2018.
Disclosures: Target: Stroke has received funding from Boehringer Ingelheim, Janssen, Bristol-Myers Squibb/Sanofi, and Merck. Dr. Fonarow had no relevant disclosures.
Source: Fonarow GC et al. ISC 2019, Abstract LBP9.
PD-1 blockade plus CD19 CAR T boosts CAR T-cell persistence
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
REPORTING FROM ASH 2018
Key clinical point: Major finding: Three of six patients with poor CAR T-cell persistence had a complete response after treatment with the combination therapy. Study details: A clinical study of 14 patients with relapsed B-ALL.
Disclosures: Dr. Maude reported financial relationships with Novartis.
Source: Li AM et al. ASH 2018, Abstract 556.
How to get surgical-like results using MitraClip
SNOWMASS, COLO. – Achieving optimal surgical-like results via transcatheter repair of primary mitral regurgitation using the MitraClip in prohibitively high-surgical-risk patients becomes much more likely by taking into account key predictive anatomic and procedural features as well as the major comorbidities influencing outcome, Paul Sorajja, MD, said at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
. Dr. Sorajja was first author of a study of 1-year outcomes in 2,952 patients with MR in the Society of Thoracic Surgery/American College of Cardiology Transcatheter Valve Therapy Registry (STS/ACC TVT) who were commercially treated with the MitraClip, at present the only transcatheter device approved for this indication. Sixty-two percent had a surgical-like result, and their 1-year mortality rate of 21.7% was significantly lower than the 29.2% rate for patients with residual grade 2 MR and the 48.9% mortality in patients left with grade 3 or 4 MR.
It’s noteworthy that even though the acute procedural success rate – defined as residual grade 2 or less MR – was impressively high at 91.8% in this group of nearly 3,000 patients, roughly one in five in the overall series was rehospitalized for heart failure within 1 year, and one in four was dead. So there remains considerable room for improvement in long-term outcomes of transcatheter repair of MR, said Dr. Sorajja, director of the Center of Valve and Structural Heart Disease at the Minneapolis Heart Institute.
Anatomic predictors of good short-term outcome
“There are specific anatomic criteria, but an easier way to think about whether your patient could get an optimal result is to remember the physical limits of this therapy. What I teach is 1-2-5-50: the MitraClip device is about 1 cm tall, about 2 cm wide, and you need about 5 mm of leaflet inside the clip to create coaptation for MR reduction. And if you do that, you will reduce the mitral valve area by about 50%, so you have to be very careful in patients with small valve areas because you can worsen mitral stenosis,” the cardiologist explained.
Only two transechocardiographic views are needed to know if a patient will have a good result with the MitraClip. A bicommissural view traversing the valve medial to lateral shows where the MR jet is; if it’s in the middle of the mitral valve, that’s favorable because it means the interventionalist has a lot of freedom to operate. Then, going orthogonal from the bicommissural view to get an anterior-posterior view allows the operator to get a good look at the valve leaflets and apply the 1-2-5 rule to determine if the leaflet approximation is favorable, he continued.
Some mitral valve anatomy variants make it challenging to get surgical-like results with a transcatheter repair. These include calcified leaflets, large gaps between leaflets, Barlow’s valves, and small leaflets. Be aware of key success-limiting comorbidities.
In the STS/ACC TVT registry study, severe tricuspid regurgitation, present in 10% of patients preprocedurally, virtually doubled the adjusted risk of 1-year mortality in multivariate analyses.
“Tricuspid regurgitation is one of the most common concomitant lesions. And the presence of tricuspid regurgitation is ominous,” Dr. Sorajja said. “Treatment of concomitant lesions such as this is going to be necessary for us to get a truly surgical-like result in outcomes.”
Toward this end, he put in a plug to consider referring patients with severe tricuspid regurgitation for enrollment in the TRILUMINATE II trial, the pivotal U.S. trial for the investigational Tri-Clip device for transcatheter tricuspid valve repair, for which he is coprincipal investigator. The trial, pitting the Tri-Clip against medical therapy, is due to start in the spring of 2019.
In multivariate analyses of the MitraClip registry study, other predictors of the combined endpoint of death and rehospitalization for heart failure at 1 year, in addition to severe tricuspid regurgitation, included dialysis, with an adjusted 2.09-fold increased risk; moderate or severe lung disease, with a 1.28-fold risk; postprocedural residual MR; diminished left ventricular ejection fraction; and advanced age (J Am Coll Cardiol. 2017 Nov 7;70[19]:2315-27).
Case experience counts
In a soon-to-be-published more up-to-date analysis of more than 12,000 MitraClip patients in the STS/ACC TVT registry, which captures all U.S. commercial use of the device for its approved indication, Dr. Sorajja and his coinvestigators documented a procedural truism: The more cases an interventionalist performs, the better the results. However, even inexperienced users of the MitraClip were able to obtain at least moderate results – that is, residual grade 2 or less MR – 90% of the time or more.
“There is some change with greater experience, but it’s actually quite small,” according to Dr. Sorajja.
However, optimal results – grade 0 or 1 MR – are another matter entirely.
“For grade 1 or less, the learning curve is much steeper. It plateaus somewhere between 50 and 75 cases. In other words, in most cases you can get to moderate MR, but getting to grade 1 requires more experience. That relationship between case experience and outcome also applies to complication rates and case time,” he said.
Although at present the MitraClip is the only Food and Drug Administration–approved transcatheter device for MR repair, there are many others in the developmental pipeline, the he noted.
Dr. Sorajja reported receiving research funding from Abbott Structural, Boston Scientific, Edwards Lifesciences, and Medtronic, and serving as a consultant to those companies and several others.
SNOWMASS, COLO. – Achieving optimal surgical-like results via transcatheter repair of primary mitral regurgitation using the MitraClip in prohibitively high-surgical-risk patients becomes much more likely by taking into account key predictive anatomic and procedural features as well as the major comorbidities influencing outcome, Paul Sorajja, MD, said at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
. Dr. Sorajja was first author of a study of 1-year outcomes in 2,952 patients with MR in the Society of Thoracic Surgery/American College of Cardiology Transcatheter Valve Therapy Registry (STS/ACC TVT) who were commercially treated with the MitraClip, at present the only transcatheter device approved for this indication. Sixty-two percent had a surgical-like result, and their 1-year mortality rate of 21.7% was significantly lower than the 29.2% rate for patients with residual grade 2 MR and the 48.9% mortality in patients left with grade 3 or 4 MR.
It’s noteworthy that even though the acute procedural success rate – defined as residual grade 2 or less MR – was impressively high at 91.8% in this group of nearly 3,000 patients, roughly one in five in the overall series was rehospitalized for heart failure within 1 year, and one in four was dead. So there remains considerable room for improvement in long-term outcomes of transcatheter repair of MR, said Dr. Sorajja, director of the Center of Valve and Structural Heart Disease at the Minneapolis Heart Institute.
Anatomic predictors of good short-term outcome
“There are specific anatomic criteria, but an easier way to think about whether your patient could get an optimal result is to remember the physical limits of this therapy. What I teach is 1-2-5-50: the MitraClip device is about 1 cm tall, about 2 cm wide, and you need about 5 mm of leaflet inside the clip to create coaptation for MR reduction. And if you do that, you will reduce the mitral valve area by about 50%, so you have to be very careful in patients with small valve areas because you can worsen mitral stenosis,” the cardiologist explained.
Only two transechocardiographic views are needed to know if a patient will have a good result with the MitraClip. A bicommissural view traversing the valve medial to lateral shows where the MR jet is; if it’s in the middle of the mitral valve, that’s favorable because it means the interventionalist has a lot of freedom to operate. Then, going orthogonal from the bicommissural view to get an anterior-posterior view allows the operator to get a good look at the valve leaflets and apply the 1-2-5 rule to determine if the leaflet approximation is favorable, he continued.
Some mitral valve anatomy variants make it challenging to get surgical-like results with a transcatheter repair. These include calcified leaflets, large gaps between leaflets, Barlow’s valves, and small leaflets. Be aware of key success-limiting comorbidities.
In the STS/ACC TVT registry study, severe tricuspid regurgitation, present in 10% of patients preprocedurally, virtually doubled the adjusted risk of 1-year mortality in multivariate analyses.
“Tricuspid regurgitation is one of the most common concomitant lesions. And the presence of tricuspid regurgitation is ominous,” Dr. Sorajja said. “Treatment of concomitant lesions such as this is going to be necessary for us to get a truly surgical-like result in outcomes.”
Toward this end, he put in a plug to consider referring patients with severe tricuspid regurgitation for enrollment in the TRILUMINATE II trial, the pivotal U.S. trial for the investigational Tri-Clip device for transcatheter tricuspid valve repair, for which he is coprincipal investigator. The trial, pitting the Tri-Clip against medical therapy, is due to start in the spring of 2019.
In multivariate analyses of the MitraClip registry study, other predictors of the combined endpoint of death and rehospitalization for heart failure at 1 year, in addition to severe tricuspid regurgitation, included dialysis, with an adjusted 2.09-fold increased risk; moderate or severe lung disease, with a 1.28-fold risk; postprocedural residual MR; diminished left ventricular ejection fraction; and advanced age (J Am Coll Cardiol. 2017 Nov 7;70[19]:2315-27).
Case experience counts
In a soon-to-be-published more up-to-date analysis of more than 12,000 MitraClip patients in the STS/ACC TVT registry, which captures all U.S. commercial use of the device for its approved indication, Dr. Sorajja and his coinvestigators documented a procedural truism: The more cases an interventionalist performs, the better the results. However, even inexperienced users of the MitraClip were able to obtain at least moderate results – that is, residual grade 2 or less MR – 90% of the time or more.
“There is some change with greater experience, but it’s actually quite small,” according to Dr. Sorajja.
However, optimal results – grade 0 or 1 MR – are another matter entirely.
“For grade 1 or less, the learning curve is much steeper. It plateaus somewhere between 50 and 75 cases. In other words, in most cases you can get to moderate MR, but getting to grade 1 requires more experience. That relationship between case experience and outcome also applies to complication rates and case time,” he said.
Although at present the MitraClip is the only Food and Drug Administration–approved transcatheter device for MR repair, there are many others in the developmental pipeline, the he noted.
Dr. Sorajja reported receiving research funding from Abbott Structural, Boston Scientific, Edwards Lifesciences, and Medtronic, and serving as a consultant to those companies and several others.
SNOWMASS, COLO. – Achieving optimal surgical-like results via transcatheter repair of primary mitral regurgitation using the MitraClip in prohibitively high-surgical-risk patients becomes much more likely by taking into account key predictive anatomic and procedural features as well as the major comorbidities influencing outcome, Paul Sorajja, MD, said at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
. Dr. Sorajja was first author of a study of 1-year outcomes in 2,952 patients with MR in the Society of Thoracic Surgery/American College of Cardiology Transcatheter Valve Therapy Registry (STS/ACC TVT) who were commercially treated with the MitraClip, at present the only transcatheter device approved for this indication. Sixty-two percent had a surgical-like result, and their 1-year mortality rate of 21.7% was significantly lower than the 29.2% rate for patients with residual grade 2 MR and the 48.9% mortality in patients left with grade 3 or 4 MR.
It’s noteworthy that even though the acute procedural success rate – defined as residual grade 2 or less MR – was impressively high at 91.8% in this group of nearly 3,000 patients, roughly one in five in the overall series was rehospitalized for heart failure within 1 year, and one in four was dead. So there remains considerable room for improvement in long-term outcomes of transcatheter repair of MR, said Dr. Sorajja, director of the Center of Valve and Structural Heart Disease at the Minneapolis Heart Institute.
Anatomic predictors of good short-term outcome
“There are specific anatomic criteria, but an easier way to think about whether your patient could get an optimal result is to remember the physical limits of this therapy. What I teach is 1-2-5-50: the MitraClip device is about 1 cm tall, about 2 cm wide, and you need about 5 mm of leaflet inside the clip to create coaptation for MR reduction. And if you do that, you will reduce the mitral valve area by about 50%, so you have to be very careful in patients with small valve areas because you can worsen mitral stenosis,” the cardiologist explained.
Only two transechocardiographic views are needed to know if a patient will have a good result with the MitraClip. A bicommissural view traversing the valve medial to lateral shows where the MR jet is; if it’s in the middle of the mitral valve, that’s favorable because it means the interventionalist has a lot of freedom to operate. Then, going orthogonal from the bicommissural view to get an anterior-posterior view allows the operator to get a good look at the valve leaflets and apply the 1-2-5 rule to determine if the leaflet approximation is favorable, he continued.
Some mitral valve anatomy variants make it challenging to get surgical-like results with a transcatheter repair. These include calcified leaflets, large gaps between leaflets, Barlow’s valves, and small leaflets. Be aware of key success-limiting comorbidities.
In the STS/ACC TVT registry study, severe tricuspid regurgitation, present in 10% of patients preprocedurally, virtually doubled the adjusted risk of 1-year mortality in multivariate analyses.
“Tricuspid regurgitation is one of the most common concomitant lesions. And the presence of tricuspid regurgitation is ominous,” Dr. Sorajja said. “Treatment of concomitant lesions such as this is going to be necessary for us to get a truly surgical-like result in outcomes.”
Toward this end, he put in a plug to consider referring patients with severe tricuspid regurgitation for enrollment in the TRILUMINATE II trial, the pivotal U.S. trial for the investigational Tri-Clip device for transcatheter tricuspid valve repair, for which he is coprincipal investigator. The trial, pitting the Tri-Clip against medical therapy, is due to start in the spring of 2019.
In multivariate analyses of the MitraClip registry study, other predictors of the combined endpoint of death and rehospitalization for heart failure at 1 year, in addition to severe tricuspid regurgitation, included dialysis, with an adjusted 2.09-fold increased risk; moderate or severe lung disease, with a 1.28-fold risk; postprocedural residual MR; diminished left ventricular ejection fraction; and advanced age (J Am Coll Cardiol. 2017 Nov 7;70[19]:2315-27).
Case experience counts
In a soon-to-be-published more up-to-date analysis of more than 12,000 MitraClip patients in the STS/ACC TVT registry, which captures all U.S. commercial use of the device for its approved indication, Dr. Sorajja and his coinvestigators documented a procedural truism: The more cases an interventionalist performs, the better the results. However, even inexperienced users of the MitraClip were able to obtain at least moderate results – that is, residual grade 2 or less MR – 90% of the time or more.
“There is some change with greater experience, but it’s actually quite small,” according to Dr. Sorajja.
However, optimal results – grade 0 or 1 MR – are another matter entirely.
“For grade 1 or less, the learning curve is much steeper. It plateaus somewhere between 50 and 75 cases. In other words, in most cases you can get to moderate MR, but getting to grade 1 requires more experience. That relationship between case experience and outcome also applies to complication rates and case time,” he said.
Although at present the MitraClip is the only Food and Drug Administration–approved transcatheter device for MR repair, there are many others in the developmental pipeline, the he noted.
Dr. Sorajja reported receiving research funding from Abbott Structural, Boston Scientific, Edwards Lifesciences, and Medtronic, and serving as a consultant to those companies and several others.
EXPERT ANALYSIS FROM ACC SNOWMASS 2019
Apply for VAM Travel Awards
Applications are due Feb. 27 for travel scholarships to attend the Vascular Annual Meeting. Available is a resident/medical student award and a diversity medical student award. Recipients are eligible to receive complimentary meeting registration plus a travel scholarship. They also get to participate in the Scholarship Program, including the hugely popular simulation training. Students and residents, please apply. And SVS members, urge the students you know to apply, as well.
Applications are due Feb. 27 for travel scholarships to attend the Vascular Annual Meeting. Available is a resident/medical student award and a diversity medical student award. Recipients are eligible to receive complimentary meeting registration plus a travel scholarship. They also get to participate in the Scholarship Program, including the hugely popular simulation training. Students and residents, please apply. And SVS members, urge the students you know to apply, as well.
Applications are due Feb. 27 for travel scholarships to attend the Vascular Annual Meeting. Available is a resident/medical student award and a diversity medical student award. Recipients are eligible to receive complimentary meeting registration plus a travel scholarship. They also get to participate in the Scholarship Program, including the hugely popular simulation training. Students and residents, please apply. And SVS members, urge the students you know to apply, as well.
Flu activity hits seasonal high
Influenza activity increased for the third consecutive week and has now reached its highest point for the 2018-2019 flu season, according to the Centers for Disease Control and Prevention.
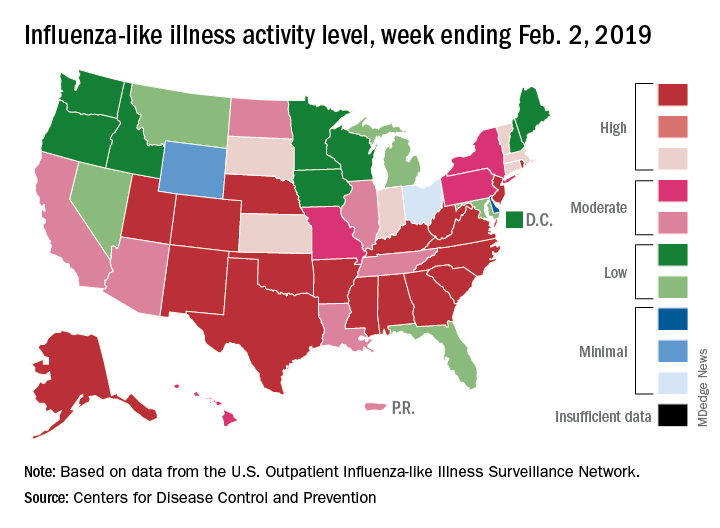
The proportion of outpatient visits for influenza-like illness (ILI) hit 4.3% for the week ending Feb. 2, which topped the previous high of 4.0% that was reached in late December (the national baseline rate is 2.2%). Outpatient ILI visits then dipped down to 3.1% after 2 weeks of decreases before rising again in mid-January, the CDC’s influenza division reported Feb. 8.
Season-high activity also was seen at the state level for the week ending Feb. 2. There were 18 states at level 10 on the CDC’s 1-10 scale of ILI activity, which was up from 16 the week before, and a total of 24 states were in the high range from 8-10, compared with 23 for the previous week. The geographic spread of influenza was reported as widespread in 47 states and Puerto Rico, the CDC said.
Four flu-related pediatric deaths were reported during the week ending Feb. 2, two of which occurred the previous week, which brings the total for the 2018-2019 season to 28, the CDC said.
There were 158 flu-related deaths among all ages during the week ending Jan. 26 – the latest for which such data are available – with reporting almost 75% complete. The previous week saw 177 overall flu deaths, with reporting for that week over 90% complete. During the corresponding weeks of the very severe 2017-2018 flu season, the overall death totals were 1,448 and 1,626, CDC data show.
Influenza activity increased for the third consecutive week and has now reached its highest point for the 2018-2019 flu season, according to the Centers for Disease Control and Prevention.
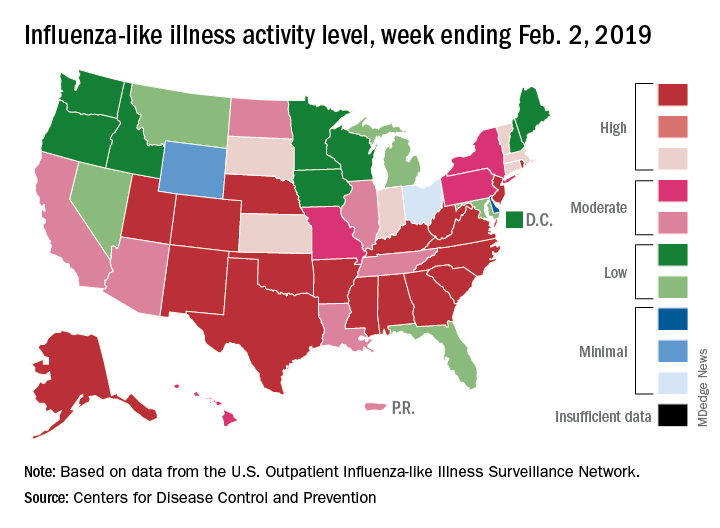
The proportion of outpatient visits for influenza-like illness (ILI) hit 4.3% for the week ending Feb. 2, which topped the previous high of 4.0% that was reached in late December (the national baseline rate is 2.2%). Outpatient ILI visits then dipped down to 3.1% after 2 weeks of decreases before rising again in mid-January, the CDC’s influenza division reported Feb. 8.
Season-high activity also was seen at the state level for the week ending Feb. 2. There were 18 states at level 10 on the CDC’s 1-10 scale of ILI activity, which was up from 16 the week before, and a total of 24 states were in the high range from 8-10, compared with 23 for the previous week. The geographic spread of influenza was reported as widespread in 47 states and Puerto Rico, the CDC said.
Four flu-related pediatric deaths were reported during the week ending Feb. 2, two of which occurred the previous week, which brings the total for the 2018-2019 season to 28, the CDC said.
There were 158 flu-related deaths among all ages during the week ending Jan. 26 – the latest for which such data are available – with reporting almost 75% complete. The previous week saw 177 overall flu deaths, with reporting for that week over 90% complete. During the corresponding weeks of the very severe 2017-2018 flu season, the overall death totals were 1,448 and 1,626, CDC data show.
Influenza activity increased for the third consecutive week and has now reached its highest point for the 2018-2019 flu season, according to the Centers for Disease Control and Prevention.
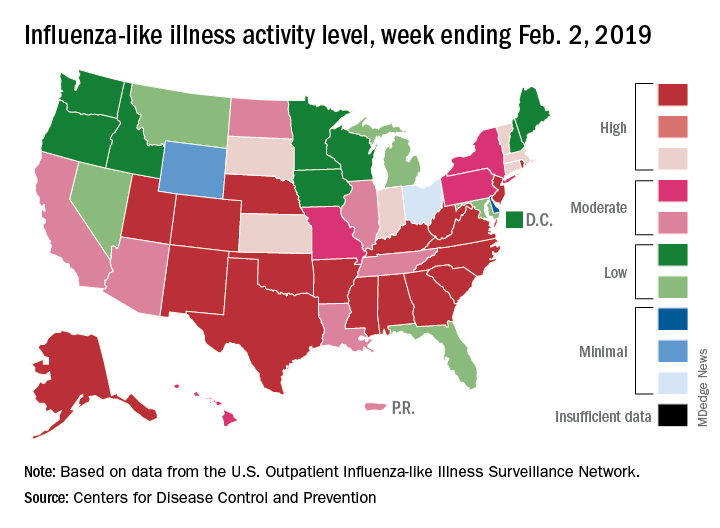
The proportion of outpatient visits for influenza-like illness (ILI) hit 4.3% for the week ending Feb. 2, which topped the previous high of 4.0% that was reached in late December (the national baseline rate is 2.2%). Outpatient ILI visits then dipped down to 3.1% after 2 weeks of decreases before rising again in mid-January, the CDC’s influenza division reported Feb. 8.
Season-high activity also was seen at the state level for the week ending Feb. 2. There were 18 states at level 10 on the CDC’s 1-10 scale of ILI activity, which was up from 16 the week before, and a total of 24 states were in the high range from 8-10, compared with 23 for the previous week. The geographic spread of influenza was reported as widespread in 47 states and Puerto Rico, the CDC said.
Four flu-related pediatric deaths were reported during the week ending Feb. 2, two of which occurred the previous week, which brings the total for the 2018-2019 season to 28, the CDC said.
There were 158 flu-related deaths among all ages during the week ending Jan. 26 – the latest for which such data are available – with reporting almost 75% complete. The previous week saw 177 overall flu deaths, with reporting for that week over 90% complete. During the corresponding weeks of the very severe 2017-2018 flu season, the overall death totals were 1,448 and 1,626, CDC data show.
In search of an ear
On our way up north to go backcountry skiing with another couple, we stopped at a roadside restaurant/tavern for lunch. We seated ourselves and, after a long 10 minutes, our waitperson arrived like a tornado, looking frazzled. She offered an apology and the first installment of her tale of woe. Before taking our order, she explained it all began when her car wouldn’t start, and then her day care provider called to say that she was sick and our server would have to find some other arrangement for the day. When our meal finally arrived, it looked appetizing but didn’t quite match our order. Again, our waitperson apologized, adding that it has been a particularly hard week because her husband was out of town and not around to help with her three children.
Had we been dining at a high-end restaurant with a white tablecloth and a candle, we would have considered our server’s behavior unprofessional and off-putting. However, we were in no hurry as the light snow had turned to a ski-unfriendly drizzle. While our original intent had been to simply have lunch, we accepted our role as a sympathetic audience for this unfortunate woman. In fact, we asked a few open-ended questions to help the cathartic process along.
The need to share one’s troubles seems to be a universal human trait. Our server had no illusions that we were going to provide any solutions to her problems. Nor was she seeking any expression of sympathy beyond our patience. However, I’m sure that unburdening herself by telling the story made her feel better, at least temporarily. Hopefully, there would be additional understanding diners to help her through the day.
For many people, the workplace serves as a therapeutic outlet where they can share their troubles and concerns. At times, the whining can be annoying to coworkers but in general, woe sharing is a harmless and valuable perk of having a job. Unless, of course, one’s job is primarily serving the public.
As physicians we are accustomed listening to our patients’ troubles. However, our job is not one of those that affords much opportunity to unburden ourselves of our own concerns. The patients assume that we are the problem solvers and don’t have any of our own. Or, if we do have some troubles, their office visit is not the time for us to share them.
The occasional sharing, such as that we are running late because we’ve had a flat on the way to the office, is harmless and can remind patients that we are human. But one must be careful stay off the slippery slope that leads to unprofessional oversharing.
Without that luxury of a workplace that allows for occasional catharsis, physicians have an additional risk for burnout. There are no easy solutions. Sharing with patients is unprofessional. Our peers are as busy as we are and probably don’t have the time to listen. Or at least they don’t seem to have the time. And then there is that ego-vulnerability issue where we are hesitant to reveal to anyone, be they staff or peers, that we have a soft underbelly.
I don’t have any easy answers to the problem beyond the usual suggestion that, Personally, I have to admit that, when my bad day was the result of an accumulation of minor bumps, I would follow our waitperson’s example and share them selectively with patients whom I deluded myself into believing had the time and concern to listen. It probably was unprofessional, but it made me feel better.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
On our way up north to go backcountry skiing with another couple, we stopped at a roadside restaurant/tavern for lunch. We seated ourselves and, after a long 10 minutes, our waitperson arrived like a tornado, looking frazzled. She offered an apology and the first installment of her tale of woe. Before taking our order, she explained it all began when her car wouldn’t start, and then her day care provider called to say that she was sick and our server would have to find some other arrangement for the day. When our meal finally arrived, it looked appetizing but didn’t quite match our order. Again, our waitperson apologized, adding that it has been a particularly hard week because her husband was out of town and not around to help with her three children.
Had we been dining at a high-end restaurant with a white tablecloth and a candle, we would have considered our server’s behavior unprofessional and off-putting. However, we were in no hurry as the light snow had turned to a ski-unfriendly drizzle. While our original intent had been to simply have lunch, we accepted our role as a sympathetic audience for this unfortunate woman. In fact, we asked a few open-ended questions to help the cathartic process along.
The need to share one’s troubles seems to be a universal human trait. Our server had no illusions that we were going to provide any solutions to her problems. Nor was she seeking any expression of sympathy beyond our patience. However, I’m sure that unburdening herself by telling the story made her feel better, at least temporarily. Hopefully, there would be additional understanding diners to help her through the day.
For many people, the workplace serves as a therapeutic outlet where they can share their troubles and concerns. At times, the whining can be annoying to coworkers but in general, woe sharing is a harmless and valuable perk of having a job. Unless, of course, one’s job is primarily serving the public.
As physicians we are accustomed listening to our patients’ troubles. However, our job is not one of those that affords much opportunity to unburden ourselves of our own concerns. The patients assume that we are the problem solvers and don’t have any of our own. Or, if we do have some troubles, their office visit is not the time for us to share them.
The occasional sharing, such as that we are running late because we’ve had a flat on the way to the office, is harmless and can remind patients that we are human. But one must be careful stay off the slippery slope that leads to unprofessional oversharing.
Without that luxury of a workplace that allows for occasional catharsis, physicians have an additional risk for burnout. There are no easy solutions. Sharing with patients is unprofessional. Our peers are as busy as we are and probably don’t have the time to listen. Or at least they don’t seem to have the time. And then there is that ego-vulnerability issue where we are hesitant to reveal to anyone, be they staff or peers, that we have a soft underbelly.
I don’t have any easy answers to the problem beyond the usual suggestion that, Personally, I have to admit that, when my bad day was the result of an accumulation of minor bumps, I would follow our waitperson’s example and share them selectively with patients whom I deluded myself into believing had the time and concern to listen. It probably was unprofessional, but it made me feel better.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
On our way up north to go backcountry skiing with another couple, we stopped at a roadside restaurant/tavern for lunch. We seated ourselves and, after a long 10 minutes, our waitperson arrived like a tornado, looking frazzled. She offered an apology and the first installment of her tale of woe. Before taking our order, she explained it all began when her car wouldn’t start, and then her day care provider called to say that she was sick and our server would have to find some other arrangement for the day. When our meal finally arrived, it looked appetizing but didn’t quite match our order. Again, our waitperson apologized, adding that it has been a particularly hard week because her husband was out of town and not around to help with her three children.
Had we been dining at a high-end restaurant with a white tablecloth and a candle, we would have considered our server’s behavior unprofessional and off-putting. However, we were in no hurry as the light snow had turned to a ski-unfriendly drizzle. While our original intent had been to simply have lunch, we accepted our role as a sympathetic audience for this unfortunate woman. In fact, we asked a few open-ended questions to help the cathartic process along.
The need to share one’s troubles seems to be a universal human trait. Our server had no illusions that we were going to provide any solutions to her problems. Nor was she seeking any expression of sympathy beyond our patience. However, I’m sure that unburdening herself by telling the story made her feel better, at least temporarily. Hopefully, there would be additional understanding diners to help her through the day.
For many people, the workplace serves as a therapeutic outlet where they can share their troubles and concerns. At times, the whining can be annoying to coworkers but in general, woe sharing is a harmless and valuable perk of having a job. Unless, of course, one’s job is primarily serving the public.
As physicians we are accustomed listening to our patients’ troubles. However, our job is not one of those that affords much opportunity to unburden ourselves of our own concerns. The patients assume that we are the problem solvers and don’t have any of our own. Or, if we do have some troubles, their office visit is not the time for us to share them.
The occasional sharing, such as that we are running late because we’ve had a flat on the way to the office, is harmless and can remind patients that we are human. But one must be careful stay off the slippery slope that leads to unprofessional oversharing.
Without that luxury of a workplace that allows for occasional catharsis, physicians have an additional risk for burnout. There are no easy solutions. Sharing with patients is unprofessional. Our peers are as busy as we are and probably don’t have the time to listen. Or at least they don’t seem to have the time. And then there is that ego-vulnerability issue where we are hesitant to reveal to anyone, be they staff or peers, that we have a soft underbelly.
I don’t have any easy answers to the problem beyond the usual suggestion that, Personally, I have to admit that, when my bad day was the result of an accumulation of minor bumps, I would follow our waitperson’s example and share them selectively with patients whom I deluded myself into believing had the time and concern to listen. It probably was unprofessional, but it made me feel better.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Woman loses hands and feet after cystectomy
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.















